Tunnel Intersection in Combined Anatomic Reconstruction ... - Healio
Tunnel Intersection in Combined Anatomic Reconstruction ... - Healio
Tunnel Intersection in Combined Anatomic Reconstruction ... - Healio
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
n the cutt<strong>in</strong>g edge<br />
Section Editor: Bennie G.P. L<strong>in</strong>deque, MD<br />
<strong>Tunnel</strong> <strong>Intersection</strong> <strong>in</strong> Comb<strong>in</strong>ed<br />
<strong>Anatomic</strong> <strong>Reconstruction</strong> of the ACL<br />
and Posterolateral Corner<br />
Steven J. Narvy, MD; Michael P. Hall, MD; Ronald S. Kvitne, MD; James E. Tibone, MD<br />
Abstract: Femoral tunnel <strong>in</strong>tersection <strong>in</strong> comb<strong>in</strong>ed anterior cruciate<br />
ligament and posterolateral corner reconstruction has been<br />
reported to be high. The purpose of this study was to exam<strong>in</strong>e the<br />
risk of <strong>in</strong>tersection between an anatomic femoral anterior cruciate<br />
ligament tunnel created with a retrograde ream<strong>in</strong>g device and<br />
femoral lateral collateral ligament reconstruction tunnels of vary<strong>in</strong>g<br />
trajectory <strong>in</strong> a synthetic femur model.<br />
Injuries to the posterolateral<br />
corner (PLC) of the knee are<br />
<strong>in</strong>frequent but can cause severe<br />
disability due to damage<br />
to the articular cartilage and<br />
persistent <strong>in</strong>stability. 1 Although<br />
<strong>in</strong>jury to the posterolateral<br />
structures can occur <strong>in</strong> isolation,<br />
coexist<strong>in</strong>g <strong>in</strong>jury to other<br />
structures, such as the menisci<br />
or the cruciate ligaments, is<br />
common. 2-4 Unrecognized<br />
posterolateral rotatory <strong>in</strong>stability<br />
has been shown to be a<br />
major cause of anterior cruciate<br />
ligament (ACL) reconstruction<br />
failure. 1,5,6 This has led to an <strong>in</strong>creased<br />
awareness of comb<strong>in</strong>ed<br />
<strong>in</strong>juries and <strong>in</strong>creased numbers<br />
of comb<strong>in</strong>ed ACL and PLC reconstructions.<br />
Numerous authors have<br />
published various surgical<br />
techniques for PLC reconstruction.<br />
3,7-18 Many tunnel configurations<br />
have been proposed,<br />
<strong>in</strong>clud<strong>in</strong>g a neutral lateral tunnel<br />
orig<strong>in</strong>at<strong>in</strong>g at the isometric po<strong>in</strong>t<br />
of the lateral epicondyle 14,15 and<br />
tunnels orig<strong>in</strong>at<strong>in</strong>g from the anatomic<br />
orig<strong>in</strong> of the lateral collateral<br />
ligament (LCL). 19<br />
The authors are from the Department of Orthopaedic Surgery (SJN,<br />
JET), Keck School of Medic<strong>in</strong>e, University of Southern California; and the<br />
Kerlan-Jobe Orthopaedic Cl<strong>in</strong>ic (MPH, RSK, JET), Los Angeles, California.<br />
The authors have no relevant f<strong>in</strong>ancial relationships to disclose.<br />
Correspondence should be addressed to: Ronald S. Kvitne, MD, Kerlan-<br />
Jobe Orthopaedic Cl<strong>in</strong>ic, 6801 Park Terrace, Los Angeles, CA 90045<br />
(drkvitne@aol.com).<br />
doi: 10.3928/01477447-20130624-07<br />
In the sett<strong>in</strong>g of comb<strong>in</strong>ed<br />
ligament reconstruction procedures,<br />
the close proximity of<br />
ACL and LCL tunnels <strong>in</strong> the<br />
lateral femoral condyle can<br />
cause bone weaken<strong>in</strong>g and tunnel<br />
collision, particularly when<br />
perform<strong>in</strong>g double-bundle<br />
ACL reconstruction. 20,21 This<br />
can compromise graft function.<br />
Accord<strong>in</strong>gly, the safest LCL<br />
tunnel trajectory has been recommended<br />
to avoid any proximal<br />
angulation <strong>in</strong> the coronal<br />
plane. 4,6 However, when creat<strong>in</strong>g<br />
a concomitant, parallel<br />
tunnel for a popliteal tendon<br />
reconstruction, this trajectory<br />
may risk damage to the articular<br />
cartilage of the lateral femoral<br />
condyle or trochlea. 6 In addition,<br />
this contradicts several<br />
popular PLC reconstruction<br />
techniques that recommend<br />
proximal and anterior angulation<br />
of both tunnels. 7,22<br />
The accuracy of ACL tunnel<br />
placement is also important <strong>in</strong><br />
comb<strong>in</strong>ed ligament reconstruction.<br />
Gaditoka et al 23 recently<br />
compared transtibial ACL tunnel<br />
creation to outside-<strong>in</strong> and<br />
anteromedial portal techniques<br />
<strong>in</strong> a cadaver model and noted<br />
statistically significant improvements<br />
<strong>in</strong> the percentage of<br />
coverage of the ACL footpr<strong>in</strong>t<br />
by the femoral tunnel with the<br />
anteromedial portal and outside<strong>in</strong><br />
techniques. The center of the<br />
outside-<strong>in</strong> tunnel was found to<br />
most closely replicate the center<br />
of the ACL footpr<strong>in</strong>t. In addition,<br />
the exit po<strong>in</strong>t of outside-<strong>in</strong><br />
tunnels on the lateral femoral<br />
condyle was farther away from<br />
the LCL orig<strong>in</strong> (particularly <strong>in</strong><br />
the anterior direction) than the<br />
anteromedial portal tunnels.<br />
This <strong>in</strong>creased ability of outside-<strong>in</strong><br />
tunnel creation to replicate<br />
the center of the ACL footpr<strong>in</strong>t<br />
and to better control tunnel<br />
trajectory relative to the lateral<br />
epicondyle may be cl<strong>in</strong>ically<br />
relevant <strong>in</strong> the reconstruction of<br />
a multiligament-<strong>in</strong>jured knee.<br />
The purpose of this study<br />
was to exam<strong>in</strong>e the risk of <strong>in</strong>tersection<br />
between an anatomic<br />
femoral ACL tunnel created<br />
with an outside-<strong>in</strong> ream<strong>in</strong>g device<br />
(FlipCutter; Arthrex, Inc,<br />
Naples, Florida) and femoral<br />
LCL reconstruction tunnels of<br />
vary<strong>in</strong>g trajectory <strong>in</strong> a synthetic<br />
femur model and to identify the<br />
best trajectory for safe tunnel<br />
JULY 2013 | Volume 36 • Number 7 529
n the cutt<strong>in</strong>g edge<br />
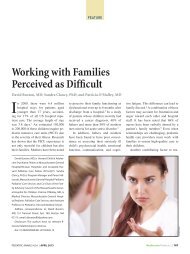
2A<br />
Figure 2: Anterior (axial) (A) and proximal (coronal) (B) angulation of the lateral collateral ligament tunnel.<br />
2B<br />
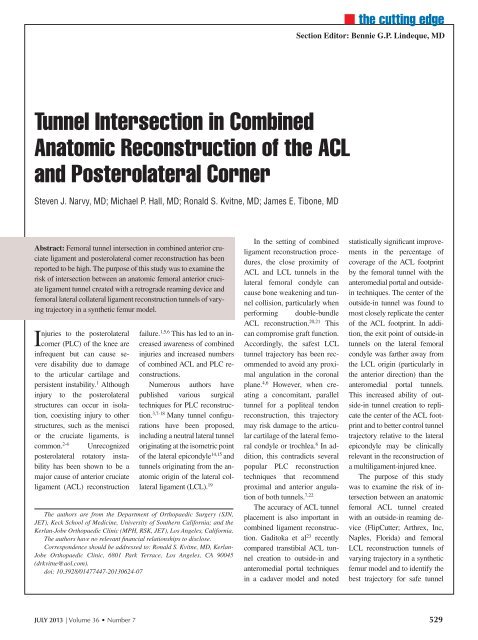
Figure 1: Photograph show<strong>in</strong>g the anterior cruciate<br />
ligament tunnel.<br />
placement. The authors hypothesized<br />
that us<strong>in</strong>g a retrograde<br />
ACL tunnel creation technique<br />
would reduce the risk of tunnel<br />
<strong>in</strong>tersection and allow for a<br />
greater range of acceptable tunnel<br />
positions.<br />
Materials and Methods<br />
Eighteen solid foam synthetic<br />
femurs (Pacific Research<br />
Laboratories, Inc, Vachon,<br />
Wash<strong>in</strong>gton) were used as the<br />
model for tunnel creation. N<strong>in</strong>e<br />
were size large (36-mm lateral<br />
femoral condyle), and 9 were<br />
size medium (28-mm lateral<br />
femoral condyle). These synthetic<br />
femurs were mounted<br />
proximally to a custom-made<br />
frame, and anatomic ACL tunnels<br />
were drilled retrograde<br />
from the ACL footpr<strong>in</strong>t us<strong>in</strong>g<br />
the FlipCutter set at 110°<br />
and angled 45° anterior <strong>in</strong> the<br />
axial plane (Figure 1). Entry<br />
po<strong>in</strong>ts on the lateral femoral<br />
cortex were standardized at<br />
4 cm proximal to the articular<br />
surface <strong>in</strong> the midpo<strong>in</strong>t <strong>in</strong><br />
1<br />
the anteroposterior<br />
plane of the femur<br />
(just anterior to the<br />
superiormost aspect<br />
of the lateral<br />
epicondyle), and<br />
drill<strong>in</strong>g angle was<br />
confirmed us<strong>in</strong>g a goniometer.<br />
Several studies have noted <strong>in</strong>creased<br />
tunnel collision with<br />
30 mm ACL tunnels compared<br />
with 25 mm tunnels 4,6 ; a 10-mm<br />
tunnel was therefore reamed<br />
to 25 mm deep us<strong>in</strong>g the calibration<br />
mechanism on the<br />
FlipCutter to prevent confound<strong>in</strong>g<br />
due to tunnel depth.<br />
Lateral collateral ligament<br />
tunnels were then created at the<br />
anatomic proximal attachment<br />
of the LCL (1.4 mm proximal<br />
and 3.1 mm posterior to the<br />
lateral epicondyle). 19 Previous<br />
studies have shown that lateral<br />
tunnel trajectories greater than<br />
40° <strong>in</strong> either the axial plane or<br />
coronal plane can result <strong>in</strong> elliptical<br />
tunnels and th<strong>in</strong>ned cortices<br />
about the tunnel open<strong>in</strong>g 4 ;<br />
accord<strong>in</strong>gly, tunnel trajectories<br />
were limited to this range. From<br />
the LCL start<strong>in</strong>g po<strong>in</strong>t, 8-mm<br />
tunnels were drilled to a depth of<br />
25 mm at either 0°, 20°, or 40°<br />
of angulation <strong>in</strong> either the proximal<br />
plane or the anterior plane<br />
(Figure 2). Specimens without<br />
obvious tunnel convergence underwent<br />
computed tomography<br />
(CT) scan with 3-dimensional<br />
reconstruction (2-mm cuts)<br />
(Aquilion16; Toshiba Medical<br />
Systems, Tust<strong>in</strong>, California) to<br />
determ<strong>in</strong>e the distance between<br />
the created tunnels or to determ<strong>in</strong>e<br />
whether an occult tunnel<br />
collision existed (Figures 3, 4).<br />
Radiographic measurements<br />
were conducted us<strong>in</strong>g the computer’s<br />
straight-l<strong>in</strong>e measur<strong>in</strong>g<br />
tool to determ<strong>in</strong>e the tangent<br />
distance between the created<br />
tunnels.<br />
Results<br />
Overall frequency of tunnel<br />
<strong>in</strong>tersection was 3/9 (33%)<br />
<strong>in</strong> large femur specimens and<br />
5/9 (56%) <strong>in</strong> medium femur<br />
specimens (P5.34; x 2 ). Among<br />
specimens without tunnel <strong>in</strong>tersection,<br />
mean tunnel separation<br />
was 4.862.5 mm. Mean tunnel<br />
separation was 5.162.8 mm<br />
for the large-sized femora and<br />
4.362.0 mm for the mediumsized<br />
femora (P5.64; Student’s<br />
t test).<br />
At 0° of anterior angulation<br />
<strong>in</strong> the axial plane, 5 (83%)<br />
of 6 specimens were noted to<br />
have tunnel <strong>in</strong>tersection. At<br />
20° of anterior angulation, 3<br />
(50%) of 6 tunnels <strong>in</strong>tersected.<br />
Mean tunnel separation among<br />
the rema<strong>in</strong><strong>in</strong>g specimens was<br />
4.261.5 mm. No <strong>in</strong>tersection<br />
occurred with LCL tunnels created<br />
with 40° of anterior angulation,<br />
with a mean separation of<br />
5.762.6 mm.<br />
At 0° of proximal angulation,<br />
1 (17%) of 6 specimens<br />
experienced tunnel <strong>in</strong>tersection.<br />
Increas<strong>in</strong>g degrees of<br />
proximal angulation to 20° and<br />
40° produced a 50% and 66%<br />
rate of tunnel <strong>in</strong>tersection, respectively.<br />
At these higher degrees<br />
of proximal angulation,<br />
high concomitant anterior angulation<br />
to 40° prevented tunnel<br />
<strong>in</strong>tersection <strong>in</strong> both medium<br />
and large specimens.<br />
Maximum tunnel separation<br />
was noted at 40° of anterior<br />
angulation and 0° of proximal<br />
angulation (9.6 mm <strong>in</strong> the<br />
large femur and 7.2 mm <strong>in</strong> the<br />
medium femur). However, the<br />
guide p<strong>in</strong> used to drill the LCL<br />
tunnel at this trajectory violated<br />
the trochlea <strong>in</strong> both medium and<br />
large specimens (Table).<br />
Discussion<br />
This study demonstrates a<br />
decreased risk of tunnel <strong>in</strong>tersection<br />
with greater anterior<br />
angulation and an <strong>in</strong>creased<br />
risk of tunnel <strong>in</strong>tersection with<br />
530 ORTHOPEDICS | <strong>Healio</strong>.com/Orthopedics
n the cutt<strong>in</strong>g edge<br />
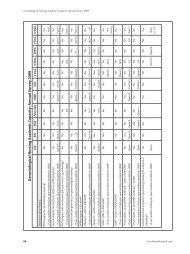
Table<br />
<strong>Tunnel</strong> Trajectory Results<br />
Figure 3: Computed tomography scan show<strong>in</strong>g<br />
divergent tunnels.<br />
Figure 4: Computed tomography scan show<strong>in</strong>g<br />
tunnel collision.<br />
3<br />
4<br />
Specimen<br />
No.<br />
Femur<br />
Size<br />
PLC Angle, deg<br />
Anterior<br />
Proximal<br />
Collision<br />
Separation<br />
on CT, mm<br />
1 Large 0 0 No 1.8<br />
2 Large 0 20 Yes<br />
3 Large 0 40 Yes<br />
4 Large 20 0 No 5.9<br />
5 Large 20 20 No 3.4<br />
6 Large 20 40 Yes<br />
Notes<br />
7 Large 40 0 No 9.6 Trochlea<br />
violated<br />
8 Large 40 20 No 6.7<br />
9 Large 40 40 No 3.4<br />
10 Medium 0 0 Yes<br />
11 Medium 0 20 Yes<br />
12 Medium 0 40 Yes<br />
13 Medium 20 0 No 3.2<br />
14 Medium 20 20 Yes<br />
15 Medium 20 40 Yes<br />
16 Medium 40 0 No 7.2 Trochlea<br />
violated<br />
17 Medium 40 20 No 4.4<br />
18 Medium 40 40 No 2.6<br />
Abbreviation: CT, computed tomography; deg, degrees; PLC, posterolateral corner.<br />
greater proximal angulation.<br />
These f<strong>in</strong>d<strong>in</strong>gs were particularly<br />
important <strong>in</strong> the mediumsized<br />
femora, which had overall<br />
higher rates of <strong>in</strong>tersection,<br />
likely due to the smaller available<br />
volume for travers<strong>in</strong>g tunnels.<br />
However, proximal angulation<br />
greater than 20° did not<br />
produce tunnel collision to the<br />
same extent as has been previously<br />
described. Proximal angulation<br />
of 20° or more was a<br />
safe configuration <strong>in</strong> the large<br />
femur when comb<strong>in</strong>ed with 20°<br />
of anterior angulation and was<br />
safe <strong>in</strong> both femur sizes when<br />
comb<strong>in</strong>ed with 40° of anterior<br />
angulation.<br />
Two studies have previously<br />
evaluated tunnel collision<br />
<strong>in</strong> comb<strong>in</strong>ed ACL–PLC<br />
reconstruction us<strong>in</strong>g synthetic<br />
femur models with study designs<br />
similar to that of the current<br />
study. Shuler et al 4 evaluated<br />
tunnel placement <strong>in</strong> 11<br />
synthetic femurs. The ACL<br />
tunnel was placed <strong>in</strong> a standard<br />
manner but appeared to be nonanatomic<br />
on imag<strong>in</strong>g, with the<br />
<strong>in</strong>tra-articular tunnel aperture<br />
centered over the footpr<strong>in</strong>t of<br />
the anteromedial bundle rather<br />
than between the anteromedial<br />
and posterolateral bundle footpr<strong>in</strong>ts.<br />
The LCL <strong>in</strong>sertion po<strong>in</strong>t<br />
was anatomically located on<br />
the synthetic femurs, and then<br />
tunnels of vary<strong>in</strong>g axial and<br />
coronal angulation (0°-60°)<br />
were drilled from this start<strong>in</strong>g<br />
po<strong>in</strong>t. The authors found that<br />
<strong>in</strong>creas<strong>in</strong>g the axial trajectory<br />
of the lateral tunnel from 0° to<br />
40° was protective aga<strong>in</strong>st tunnel<br />
collision and demonstrated<br />
that tunnel separation distance<br />
<strong>in</strong>creased directly with axial<br />
angulation. Coronal angulation<br />
greater than 20° produced tunnel<br />
collision <strong>in</strong> all specimens.<br />
In a separate arm of the study,<br />
the authors compared LCL tunnels<br />
drilled at 40° anterior/0°<br />
proximal to control tunnels<br />
drilled at 0° anterior/0° proximal<br />
<strong>in</strong> 7 matched cadaver knees<br />
and noted a 29% collision rate<br />
with the more anterior tunnels<br />
compared with 43% <strong>in</strong> the control<br />
group. The authors concluded<br />
that the safest configuration<br />
for tunnel placement was<br />
40° anterior and 0° proximal. 4<br />
Camarda et al 6 performed a<br />
similar study of tunnel placement<br />
when the ACL was reconstructed<br />
us<strong>in</strong>g only the<br />
posterolateral bundle tunnel of<br />
a double-bundle technique concomitantly<br />
with reconstruction<br />
of the lateral collateral ligament<br />
<strong>in</strong> 36 synthetic femurs (18 large<br />
and 18 medium). As <strong>in</strong> the current<br />
study, 9 different guidewire<br />
JULY 2013 | Volume 36 • Number 7 531
n the cutt<strong>in</strong>g edge<br />
orientations <strong>in</strong> the anterior and<br />
proximal planes were created at<br />
20° <strong>in</strong>tervals for the LCL tunnel.<br />
6 Similar to Shuler et al, 4 the<br />
authors demonstrated a significantly<br />
higher rate of tunnel collision<br />
with proximal angulation<br />
greater than 20°. No collisions<br />
were noted when the LCL tunnel<br />
was reamed at 0° of proximal<br />
angulation, irrespective of<br />
anterior trajectory. 6<br />
Also similar to Shuler et<br />
al, 4 the current authors noted<br />
maximal tunnel separation at<br />
40° anterior and 0° proximal.<br />
This configuration resulted <strong>in</strong><br />
violation of the trochlea <strong>in</strong> both<br />
medium and large specimens,<br />
although proximal angulation<br />
to 20° at the same anterior trajectory<br />
produced satisfactory<br />
tunnel separation. This f<strong>in</strong>d<strong>in</strong>g<br />
suggests that proximal angulation<br />
may be protective of the<br />
trochlea when comb<strong>in</strong>ed with<br />
significant anterior angulation.<br />
However, the limitations of<br />
this laboratory model must be<br />
appreciated <strong>in</strong> mak<strong>in</strong>g this determ<strong>in</strong>ation.<br />
Variability of human<br />
femoral condyle size can<br />
greatly affect the risk of tunnel<br />
collision, and although 2 sizes<br />
of synthetic femur were used<br />
<strong>in</strong> the current study, <strong>in</strong> vivo<br />
tunnel creation may produce<br />
different f<strong>in</strong>d<strong>in</strong>gs. Similarly,<br />
<strong>in</strong> vivo retrograde ream<strong>in</strong>g is<br />
based on <strong>in</strong>tra-articular landmarks<br />
from the footpr<strong>in</strong>t of<br />
the ACL, which was not present<br />
<strong>in</strong> this sawbones model.<br />
Us<strong>in</strong>g a handheld goniometer<br />
for lateral tunnel placement<br />
may have an <strong>in</strong>creased risk<br />
of variability compared with<br />
a well-controlled jig. Most<br />
importantly, the small sample<br />
size limits the generalizability<br />
of the current results to <strong>in</strong><br />
vivo reconstructive procedures.<br />
Nonetheless, this study demonstrates<br />
the technical feasibility<br />
of a comb<strong>in</strong>ed ACL-PLC reconstruction<br />
us<strong>in</strong>g a retrograde<br />
ream<strong>in</strong>g device <strong>in</strong> a laboratory<br />
model. Increas<strong>in</strong>g anterior angulation<br />
when comb<strong>in</strong>ed with<br />
25-mm LCL tunnels may help<br />
avoid tunnel <strong>in</strong>tersection when<br />
perform<strong>in</strong>g such comb<strong>in</strong>ed<br />
procedures, particularly <strong>in</strong><br />
smaller-sized femora.<br />
Conclusion<br />
The results of this study provide<br />
evidence for safe LCL tunnel<br />
creation when us<strong>in</strong>g retrograde<br />
ACL ream<strong>in</strong>g techniques<br />
<strong>in</strong> comb<strong>in</strong>ed ACL and PLC reconstruction.<br />
Forty degrees of<br />
anterior angulation of the LCL<br />
tunnel produced the lowest risk<br />
of tunnel collision but at the risk<br />
of trochlear violation without<br />
concomitant proximal angulation.<br />
Therefore, optimal tunnel<br />
orientation is recommended at<br />
40° of anterior angulation and<br />
20° of proximal angulation.<br />
References<br />
1. Covey DC. Injuries of the posterolateral<br />
corner of the knee.<br />
J Bone Jo<strong>in</strong>t Surg Am. 2001;<br />
83(1):106-118.<br />
2. LaPrade RF, Wentorf FA, Fritts<br />
H, Gundry C, Hightower CD. A<br />
prospective magnetic resonance<br />
imag<strong>in</strong>g study of the <strong>in</strong>cidence<br />
of posterolateral and multiple<br />
ligament <strong>in</strong>juries <strong>in</strong> acute knee<br />
<strong>in</strong>juries present<strong>in</strong>g with a hemarthrosis.<br />
Arthroscopy. 2007;<br />
23(12):1341-1347.<br />
3. Lee SH, Jung YB, Jung HJ, Song<br />
KS, Ko YB. Comb<strong>in</strong>ed reconstruction<br />
for posterolateral rotatory<br />
<strong>in</strong>stability with anterior cruciate<br />
ligament <strong>in</strong>juries of the knee.<br />
Knee Surg Sports Traumatol Arthrosc.<br />
2010; 18(9):1219-1225.<br />
4. Shuler MS, Jasper LE, Rauh PB,<br />
Mulligan ME, Moorman CT<br />
III. <strong>Tunnel</strong> convergence <strong>in</strong> comb<strong>in</strong>ed<br />
anterior cruciate ligament<br />
and posterolateral corner reconstruction.<br />
Arthroscopy. 2006;<br />
22(2):193-198.<br />
5. LaPrade RF, Hamilton CD,<br />
Engebretsen L. Treatment of<br />
acute and chronic comb<strong>in</strong>ed anterior<br />
cruciate ligament and posterolateral<br />
knee ligament <strong>in</strong>juries.<br />
Sports Med Arthrosc Rev. 1997;<br />
5:91-99.<br />
6. Camarda L, D’Arienzo M, Patera<br />
GP, Filosto L, LaPrade<br />
RF. Avoid<strong>in</strong>g tunnel collisions<br />
between fibular collateral ligament<br />
and ACL posterolateral<br />
bundle reconstruction. Knee Surg<br />
Sports Traumatol Arthrosc. 2011;<br />
19(4):598-603.<br />
7. LaPrade RF, Johansen S, Wentorf<br />
FA, Engebretsen L, Esterberg JL,<br />
Tso A. An analysis of an anatomical<br />
posterolateral knee reconstruction:<br />
an <strong>in</strong> vitro biomechanical<br />
study and development of a<br />
surgical technique. Am J Sports<br />
Med. 2004; 32(6):1405-1414.<br />
8. Stannard JP, Brown SL, Rob<strong>in</strong>son<br />
JT, McGw<strong>in</strong> G, Volgas DA.<br />
<strong>Reconstruction</strong> of the posterolateral<br />
corner of the knee. Arthroscopy.<br />
2005; 21(9):1051-1059.<br />
9. Bicos J, Arciero RA. Novel approach<br />
for reconstruction of the<br />
posterolateral corner us<strong>in</strong>g a free<br />
tendon graft technique. Sports<br />
Med Arthrosc. 2006; 14(1):28-<br />
36.<br />
10. Larson RV. Isometry of the lateral<br />
collateral and popliteofibular<br />
ligaments and techniques for<br />
reconstruction us<strong>in</strong>g a free semitend<strong>in</strong>osus<br />
tendon graft. Oper<br />
Tech Sports Med. 2001; 9:84-90.<br />
11. Simonian PT. Operative treatment<br />
of posterolateral knee <strong>in</strong>stability.<br />
Oper Tech Sports Med.<br />
2001; 9:76-83.<br />
12. Yoon KH, Bae DK, Ha JH, Park<br />
SW. <strong>Anatomic</strong> reconstructive<br />
surgery for posterolateral <strong>in</strong>stability<br />
of the knee. Arthroscopy.<br />
2006; 22(2):159-165.<br />
13. Latimer HA, Tibone JE, ElAttrache<br />
NS, McMahon PJ. <strong>Reconstruction</strong><br />
of the lateral collateral<br />
ligament of the knee with patellar<br />
tendon allograft. Report of a new<br />
technique <strong>in</strong> comb<strong>in</strong>ed ligament<br />
<strong>in</strong>juries. Am J Sports Med. 1998;<br />
26(5):656-662.<br />
14. Kocabey Y, Nawab A, Caborn<br />
DN, Nyland J. Posterolateral corner<br />
reconstruction us<strong>in</strong>g a hamstr<strong>in</strong>g<br />
allograft and a bioabsorbable<br />
tenodesis screw: description<br />
of a new surgical technique.<br />
Arthroscopy. 2004; 20(suppl<br />
2):159-163.<br />
15. Verma NN, Mithöfer K, Battaglia<br />
M, MacGillivray J. The dock<strong>in</strong>g<br />
technique for posterolateral<br />
corner corner reconstruction. Arthroscopy.<br />
2005; 21(2):238-242.<br />
16. McGuire DA, Wolchok JC. Posterolateral<br />
corner reconstruction.<br />
Arthroscopy. 2003; 19(7):790-<br />
793.<br />
17. Sekiya JK, Kurtz CA. Posterolateral<br />
corner reconstruction of the<br />
knee: surgical technique utiliz<strong>in</strong>g<br />
a bifid Achilles tendon allograft<br />
and a double femoral tunnel. Arthroscopy.<br />
2005; 21(11):1400.<br />
18. Kim SJ, Park IS, Cheon YM, Ryu<br />
SW. New technique for chronic<br />
posterolateral <strong>in</strong>stability of the<br />
knee: posterolateral reconstruction<br />
us<strong>in</strong>g the tibialis posterior<br />
tendon allograft. Arthroscopy.<br />
2004; 20(suppl 2):195-200.<br />
19. LaPrade RF, Ly TV, Wentorf FA,<br />
Engebretsen L. The posterolateral<br />
attachments of the knee: a<br />
qualitative and quantitative morphologic<br />
analysis of the fibular<br />
collateral ligament, popliteus tendon,<br />
popliteofibular ligament, and<br />
lateral gastrocnemius tendon. Am<br />
J Sports Med. 2003; 31:854-860.<br />
20. Albright JP, Brown AW. Management<br />
of chronic posterolateral<br />
rotatory <strong>in</strong>stability of the<br />
knee: surgical technique for the<br />
posterolateral corner sl<strong>in</strong>g procedure.<br />
Instr Course Lect. 1998;<br />
47:369-378.<br />
21. Neven E, D’Hooghe P, Bellemans<br />
J. Double-bundle anterior<br />
cruciate ligament reconstruction:<br />
a cadaveric study on the posterolateral<br />
tunnel position and safety<br />
of the lateral structures. Arthroscopy.<br />
2008; 24(4):436-440.<br />
22. Arciero RA. <strong>Anatomic</strong> posterolateral<br />
corner knee reconstruction.<br />
Arthroscopy. 2005;<br />
21(9):1147.<br />
23. Gaditoka HR, Sim JA, Hosse<strong>in</strong>i<br />
A, Gill TJ, Li G. The relationship<br />
between femoral tunnels created<br />
by the transtibial, anteromedial<br />
portal, and outside-<strong>in</strong> techniques<br />
and the anterior cruciate ligament<br />
footpr<strong>in</strong>t. Am J Sports Med.<br />
2012; 40(4):882-888.<br />
532 ORTHOPEDICS | <strong>Healio</strong>.com/Orthopedics