National Medical Policy - Health Net
National Medical Policy - Health Net
National Medical Policy - Health Net
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
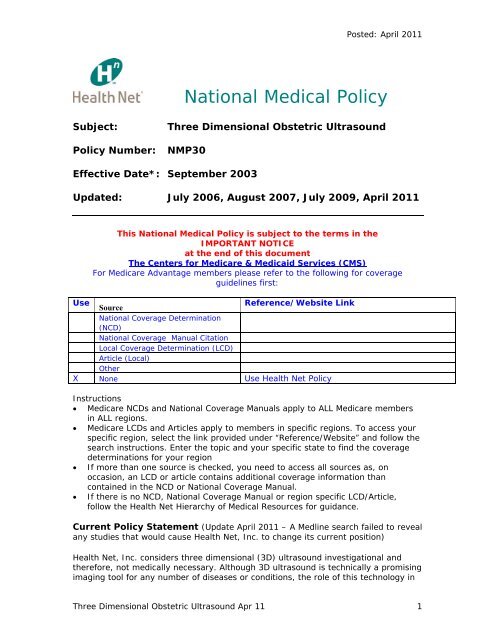
Posted: April 2011<br />
<strong>National</strong> <strong>Medical</strong> <strong>Policy</strong><br />
Subject:<br />
<strong>Policy</strong> Number:<br />
Three Dimensional Obstetric Ultrasound<br />
NMP30<br />
Effective Date*: September 2003<br />
Updated: July 2006, August 2007, July 2009, April 2011<br />
This <strong>National</strong> <strong>Medical</strong> <strong>Policy</strong> is subject to the terms in the<br />
IMPORTANT NOTICE<br />
at the end of this document<br />
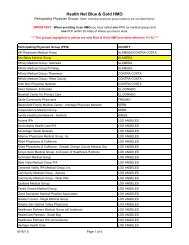
The Centers for Medicare & Medicaid Services (CMS)<br />
For Medicare Advantage members please refer to the following for coverage<br />
guidelines first:<br />
Use<br />
Source<br />
Reference/Website Link<br />
<strong>National</strong> Coverage Determination<br />
(NCD)<br />
<strong>National</strong> Coverage Manual Citation<br />
Local Coverage Determination (LCD)<br />
Article (Local)<br />
Other<br />
X None Use <strong>Health</strong> <strong>Net</strong> <strong>Policy</strong><br />
Instructions<br />
• Medicare NCDs and <strong>National</strong> Coverage Manuals apply to ALL Medicare members<br />
in ALL regions.<br />
• Medicare LCDs and Articles apply to members in specific regions. To access your<br />
specific region, select the link provided under “Reference/Website” and follow the<br />
search instructions. Enter the topic and your specific state to find the coverage<br />
determinations for your region<br />
• If more than one source is checked, you need to access all sources as, on<br />
occasion, an LCD or article contains additional coverage information than<br />
contained in the NCD or <strong>National</strong> Coverage Manual.<br />
• If there is no NCD, <strong>National</strong> Coverage Manual or region specific LCD/Article,<br />
follow the <strong>Health</strong> <strong>Net</strong> Hierarchy of <strong>Medical</strong> Resources for guidance.<br />
Current <strong>Policy</strong> Statement (Update April 2011 – A Medline search failed to reveal<br />
any studies that would cause <strong>Health</strong> <strong>Net</strong>, Inc. to change its current position)<br />
<strong>Health</strong> <strong>Net</strong>, Inc. considers three dimensional (3D) ultrasound investigational and<br />
therefore, not medically necessary. Although 3D ultrasound is technically a promising<br />
imaging tool for any number of diseases or conditions, the role of this technology in<br />
Three Dimensional Obstetric Ultrasound Apr 11 1
Posted: April 2011<br />
reaching the correct diagnosis has not been clearly translated into clinical<br />
improvement of patient outcome.<br />
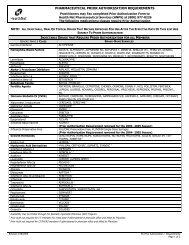
Codes Related To This <strong>Policy</strong><br />
ICD-9 Codes<br />
V22.0-V22.2 Normal pregnancy<br />
V23.0-V23.9 Supervision of high-risk pregnancy<br />
CPT Codes<br />
76375<br />
Coronal sagittal, multiplanar, oblique, 3-Dimensional and/or<br />
holographic reconstruction of computerized tomography,<br />
magnetic resonance imaging, or other topographic modality<br />
(may be considered medically unnecessary and denied if<br />
equivalent information to that obtained from the test has<br />
already been provided by another procedure (magnetic<br />
resonance imaging, ultrasound, angiography, etc.), or could be<br />
provided by a standard CT Scan (2-Dimensional) without<br />
reconstruction (deleted 12/31/05)<br />
76376 3D rendering with interpretation and reporting of computed<br />
tomography, magnetic resonance imaging, ultrasound, or other<br />
tomographic modality; not requiring image post processing on<br />
an independent workstation<br />
76377 3D rendering with interpretation and reporting of computed<br />
tomography, magnetic resonance imaging, ultrasound, or other<br />
tomographic modality; requiring image post processing on an<br />
independent workstation<br />
HCPCS Codes<br />
N/A<br />
Scientific Rationale – Update July 2009<br />
Ultrasonography in pregnancy should be performed only when there is a valid<br />
medical indication. The American College of Obstetrics and Gynecology (ACOG)<br />
[2009] stated, "The use of either two-dimensional or three-dimensional<br />
ultrasonography only to view the fetus, obtain a picture of the fetus, or determine<br />
the fetal sex without a medical indication is inappropriate and contrary to responsible<br />
medical practice."<br />
Current guidelines on ultrasonography in pregnancy from the American College of<br />
Obstetricians and Gynecologists (2009) state: "The technical advantages of 3-<br />
dimensional ultrasonography include its ability to acquire and manipulate an infinite<br />
number of planes and to display ultrasound planes traditionally inaccessible by 2-<br />
dimensional ultrasonography. Despite these technical advantages, proof of a clinical<br />
advantage of 3-dimensional ultrasonography in prenatal diagnosis in general is still<br />
lacking. Potential areas of promise include fetal facial anomalies, neural tube<br />
defects, and skeletal malformations where 3-dimensional ultrasonography may be<br />
helpful in diagnosis as an adjunct to, but not a replacement for, 2-dimensional<br />
ultrasonography. Until clinical evidence shows a clear advantage to conventional 2-<br />
dimensional ultrasonography, 3-dimensional ultrasonography is not considered a<br />
required modality at this time."<br />
Three Dimensional Obstetric Ultrasound Apr 11 2
Posted: April 2011<br />
Scientific Rationale – Update August 2007<br />
According to the American College of Obstetrics and Gynecology (ACOG) practice<br />
bulletin, Ultrasonography in Pregnancy, “Proof of a clear advantage of 3-dimensional<br />
ultrasonography in prenatal diagnosis is not present when compared with 2-<br />
dimensional imaging by an experienced clinician. Therefore, 3-dimensional imaging is<br />
not considered a required modality at this time.”<br />
Wang et al. (2007) investigated the prenatal diagnostic accuracy of two-dimensional<br />
ultrasound (2DUS) alone versus 2DUS in conjunction with three-dimensional<br />
ultrasonography (3DUS) including orthogonal display (OGD) and three-dimensional<br />
extended imaging for cleft lip and primary palate. Fetuses being suspected of having<br />
a facial cleft by previous ultrasound examination or family history were examined<br />
sequentially with 2DUS and then 3DUS. Of a total of 30 infants, 22 had cleft lip and<br />
nine also had cleft palate at birth. The use of 2DUS with or without 3DUS correctly<br />
identified all cases of cleft lips prenatally. However, the use of 2DUS in conjunction<br />
with 3DUS correctly identified more cleft primary palate than 2DUS alone (88.9% vs<br />
22.2%). Cleft primary palate was well demonstrated in both the multi-slice view<br />
(MSV) and OGD modes. In one case, a cleft palate was shown in the MSV mode but<br />
not in the Oblique view(OBV) mode. All the unaffected fetuses were reported as no<br />
cleft palate with the use of MSV mode. The investigator concluded the combined<br />
approach of 2DUS and 3DUS with both OGD and MSV modes significantly improved<br />
the prenatal detection rate for a cleft palate compared with 2DUS alone (88.9% vs<br />
22.2%) without decreasing the specificity.<br />
Goncalves et al. (2005) performed a review of the published literature on 3-<br />
dimensional ultrasound (3DUS) and 4-dimensional ultrasound (4DUS) in obstetrics to<br />
determine whether 3DUS adds diagnostic information to what is currently provided<br />
by 2-dimensional ultrasound (2DUS) and, if so, in what areas. A PubMed search<br />
found 525 articles reporting on the use of 3DUS or 4DUS in obstetrics related to the<br />
subject of the review. Articles describing technical developments, clinical studies,<br />
reviews, editorials, and studies on fetal behavior or maternal-fetal bonding were<br />
reviewed. The reviewers found that three-dimensional ultrasound provides<br />
additional diagnostic information for the diagnosis of facial anomalies, especially<br />
facial clefts. They also found evidence that 3DUS provides additional diagnostic<br />
information in neural tube defects and skeletal malformations. Large studies<br />
comparing 2DUS and 3DUS for the diagnosis of congenital anomalies have not<br />
provided conclusive results. They noted preliminary evidence suggests that<br />
sonographic tomography may decrease the examination time of the obstetric<br />
ultrasound examination, with minimal impact on the visualization rates of anatomic<br />
structures. The reviewers concluded three-dimensional ultrasound provides<br />
additional diagnostic information for the diagnosis of facial anomalies, evaluation of<br />
neural tube defects, and skeletal malformations. Additional research is needed to<br />
determine the clinical role of 3DUS and 4DUS for the diagnosis of congenital heart<br />
disease and central nervous system anomalies. Future studies should determine<br />
whether the information contained in the volume data set, by itself, is sufficient to<br />
evaluate fetal biometric measurements and diagnose congenital anomalies.<br />
In a prospective randomized pilot study among low risk women with singleton<br />
fetuses in the second and third trimester, Lapaire et al. (2007) assessed the impact<br />
of three-dimensional (3D) versus two-dimensional (2D) ultrasound (US) on<br />
maternal-fetal bonding. Sixty women were randomized to either 2D US or 3D US<br />
and the effects were recorded with standardized questionnaires. Although the<br />
Three Dimensional Obstetric Ultrasound Apr 11 3
Posted: April 2011<br />
quality of 2D US, assessed by the examinator, was superior to 3D US, maternal<br />
recognition was higher with 3-D US. With 2D US, nulliparous patients had<br />
significantly more difficulties visualizing the fetus, than multiparous. However, the<br />
maternal preference of 3D US had no significant impact on maternal-fetal bonding.<br />
The investigator concluded ultrasound had no significant effect on maternal-fetal<br />
bonding. Three-dimensional images may facilitate recognition of the fetus, but 3D US<br />
did not have higher impact on maternal-fetal bonding. This finding may be a reason<br />
not to consider 3D ultrasound for routine scanning<br />
According to the American Institute of Ultrasound in Medicine, “Currently, twodimensional<br />
(2D) gray-scale real-time sonography is the primary method of<br />
medically indicated anatomic imaging with ultrasound. The term three-dimensional<br />
(3D) ultrasound refers to the acquisition of imaging data from a volume of tissue.<br />
This volumetric data can be displayed as slabs of varying thickness, multiplanar<br />
reconstruction or as a rendered image. The 2D display remains the primary method<br />
of image presentation regardless of the method of acquisition. While 3D ultrasound<br />
may be helpful in diagnosis, it is currently an adjunct to, but not a replacement for<br />
2D ultrasound. As with any developing technology, its clinical value may improve and<br />
its diagnostic role will be periodically re-evaluated”<br />
Scientific Rationale<br />
Two-dimensional (2D) sonography is the traditional way we have been using<br />
ultrasound in all areas of medicine to display normal and abnormal anatomy. More<br />
recently, three dimensional (3D) ultrasound has emerged as the novel sonographic<br />
method that can enhance diagnostic capability over standard 2D ultrasound. Even<br />
though this ability to display a 3D image may become one of the most powerful<br />
recent advances in sonography, critics of the technique feel that three-dimensional<br />
ultrasound has been over rated and that the training afforded to 2D sonographers<br />
enables them to perform 3D reconstructions in their mind’s eye, with similar results<br />
as those described with actual 3D displays.<br />
Numerous studies conducted on the use of 3D ultrasound demonstrate that this noninvasive<br />
method is technically feasible and suggest potential benefits for some of the<br />
proposed indications. However, there is a paucity of high quality direct evidence<br />
demonstrating the impact on diagnostic thinking and therapeutic decision-making. In<br />
addition, the techniques of acquiring the capabilities to perform 3D ultrasound,<br />
appropriate patient selection criteria, and interpreting the results are not well<br />
standardized. There is no adequate evidence that 3D ultrasound can prevent or<br />
retard the development and/or progression of the long-term complications of any<br />
diseases or conditions; nor is there evidence that 3D ultrasound can prolong the life<br />
of patients. Prospective clinical studies are needed to determine the clinical value of<br />
3D ultrasound over standard 2D ultrasound in the assessment of patients. The<br />
following enumerates the potential uses of 3D ultrasound.<br />
2D ultrasound is used routinely in obstetrics and gynecology. Today, nearly all<br />
pregnant women undergo at least one ultrasound during her pregnancy. These<br />
ultrasounds are designed to assess fetal well-being and gestational age. The<br />
traditional 2D ultrasound uses high-frequency sound waves to bounce off the<br />
surfaces and structures of the fetus producing echos, which can be assessed on the<br />
video screen. Although clinicians are generally adept at using this information, the<br />
image remains distorted and vague to say the least. In the last couple of years, the<br />
creation of 3D ultrasound for use in obstetrics has come to fruition. 3D ultrasound is<br />
Three Dimensional Obstetric Ultrasound Apr 11 4
Posted: April 2011<br />
done the same way as the traditional ultrasound with the addition of software to<br />
enhance the image and produce a three dimensional image.<br />
A further benefit of 3D ultrasonography is that it can provide caregivers in primary<br />
facilities with less experience and expertise in ultrasonography an opportunity for<br />
remote referrals and consultations for complicated cases. 3D images can be digitally<br />
stored with the complete data set conveyed by an Internet connection from the<br />
primary caregiver to experts across the world. This allows the consultant to have an<br />
entirety of imaging information required to make a diagnosis. Furthermore, the online<br />
transmission enables feedback and interaction with a specialist at the time of or<br />
immediately after an ultrasonographic examination, thus limiting the need for further<br />
referrals. Telemedicine has only begun to demonstrate itself as a useful tool and 3D<br />
ultrasonography is ideally suited to promote this upcoming aspect of care in<br />
medicine. Imaging physicians already use 3D volume imaging techniques in CT and<br />
MR and are likely to become comfortable working in a volume or multiplanar<br />
environment in ultrasound as well.<br />
One of the most consistently used justifications for the use of obstetric<br />
ultrasonography is that accurate diagnosis of fetal malformations before delivery can<br />
provide both health care providers and parents a number of management options<br />
that before the advent of this technique were unavailable. However, reports from the<br />
Routine Antenatal Diagnostic Imaging with Ultrasound (RADIUS) trial have<br />
challenged this particular tenet. These researchers indicated that screening with<br />
ultrasonography did not significantly influence the management or outcome of<br />
pregnancies complicated by congenital malformations. Its role in gynecology has not<br />
been clearly established. It may be indicated only when equivalent information<br />
resulting in clinical improvement in fetal and maternal outcome cannot be obtained<br />
by another standard test (2D ultrasound, magnetic resonance imaging, CT Scan,<br />
angiography, etc.). 3D ultrasound may be useful in differentiating between a septate<br />
and a bicornuate uterus or to determine the exact location of a malpositioned<br />
intrauterine device (IUD).<br />
The fetal brain is one of the areas where 3D ultrasound has been most helpful.<br />
Surface rendering of the skull is instrumental in evaluating the status of cranial<br />
sutures and determining whether or not an abnormal head shape is secondary to<br />
craniosynostosis. Three-dimensional surface rendering is also particularly helpful in<br />
the evaluation of other surfaces of the fetal head and face, such as the fetal ears,<br />
which are not normally focused upon using standard 2D cross sectional imaging.<br />
Surface imaging of the fetal face using 3D sonography has probably been the most<br />
notable area of study, not only in the ultrasound literature but also in the lay press<br />
where patients have been able to see the face of their unborn baby more clearly than<br />
ever before. Everyone agrees that 3D sonography of the face is not a screening<br />
technique but an adjunct to a good 2D scan. To date, it is not yet possible to detect<br />
dysmorphologic features using 3D surface rendering although it is hoped that as the<br />
techniques improve, the dysmorphologic fetal facies will be detectable. It is the<br />
evaluation of the fetal cleft lip and palate that has gotten the most attention in the<br />
literature.<br />
Three-dimensional imaging of the normal and abnormal extremities has been studied<br />
extensively using both multi-planar reconstruction and surface rendering. Several<br />
studies have described fetal skeletal dysphasia’s viewed with 3D ultrasound, where<br />
practitioners found that 3D provided additional information on affected fetuses as<br />
compared to 2D. On the other hand, other investigators have not been as<br />
Three Dimensional Obstetric Ultrasound Apr 11 5
Posted: April 2011<br />
enthusiastic about the role of 3D for fetuses with these malformations, thus requiring<br />
further investigation to come to a consensus. Opinions that 3D provides diagnostic<br />
details not available using two-dimensional ultrasound remains somewhat anecdotal<br />
and restricted to small case series. It is clear from several reports that although 3D<br />
made additional diagnostic information possible, the technique was not necessary for<br />
definitive diagnosis of spina bifida. 3D ultrasounds, however, did display the level of<br />
the defect more accurately than with conventional scanning. Scoliosis resulting from<br />
vertebral body anomalies was also recognized more easily on a single 3D rendered<br />
image whereas multiple standard 2D images were needed to make the same<br />
diagnosis.<br />
Evaluation of the fetal heart is an intense area of research, however, evaluation of<br />
the heart in 3D can be tricky and requires Doppler gated capabilities. There is still<br />
much work to be done to bring 3D imaging of the heart up to a standard currently<br />
possible using 2D operated by trained personnel. Other areas of investigation include<br />
fetal genital scanning where the fetal perineum can be visualized, although to date,<br />
the performance of 3D technology is reportedly not as good in evaluating fetal<br />
genitals than is 2D imaging alone. By far, the most important function of first<br />
trimester 3D scanning may become the evaluation of the nuchal translucency<br />
measurement of fetuses 11-14 weeks.<br />
Another important clinical application of 3D is volume measurements calculations<br />
based on 3D volume acquisition. Current literature has demonstrated the accuracy of<br />
volume based 3D ultrasonography measurement on follicle aspiration performed<br />
using transvaginal needle guided technique. Other practitioners have also shown that<br />
3D sonographic methods provide accurate measurements of serial fetal lung volume<br />
measurements for the prenatal detection of pulmonary hypoplasia, the fetal thoracolumbar<br />
spine as well as kidneys, brain, liver and heart. Additionally, at the current<br />
time fetal cardiac malformations, which remain the least identifiable of major<br />
malformations, have thus far had only limited benefit from this 3D technique<br />
because of motion artifact. Hypothetically, if the 3D examination demonstrates an<br />
abnormality not seen with 2D imaging, then clinical management of patients may be<br />
altered.<br />
Craniofacial abnormalities that have been identified with 3D ultrasound include cleft<br />
lip or palate, micrognathia, midface hypoplasia, facial dysmorphia, intracranial<br />
abnormalities, hypotelorism, holoprosencephaly and skull defects in the second- and<br />
third-trimester. In expert hands, a 2D ultrasound is sufficient and 3D ultrasound<br />
does not add any valuable diagnostic information. Three-dimensional ultrasound may<br />
facilitate the understanding of the lesion by the parents and facilitate communication<br />
with the plastic surgeons. However, these potential benefits need to be carefully<br />
weighed against the costs of the ultrasound instrumentation, increased examination<br />
time and training of personnel.<br />
Computer technology and software advanced sufficiently in the past five years to<br />
allow real-time reconstruction of 3D images and their visualization and manipulation<br />
on inexpensive desktop computers. Nevertheless, ultrasound imaging still suffers<br />
from several disadvantages related to its 2 dimensional nature, which 3D imaging<br />
attempts to address. Despite decades of exploration, it is only in the past five years<br />
that 3D imaging in ultrasound moved out of the research laboratory to become a<br />
commercial product for routine clinical use.<br />
Three Dimensional Obstetric Ultrasound Apr 11 6
Posted: April 2011<br />
A major advantage of 2D ultrasound is its flexibility, allowing the sonologist to<br />
manipulate the transducer and view the desired anatomical section. Paradoxically,<br />
this advantage is one of its weaknesses that 3D imaging attempts to address. Using<br />
conventional ultrasonography, only one thin slice of the patient can be viewed at any<br />
time, and the location of this image plane is controlled by physically manipulating the<br />
transducer orientation. It is difficult to place the 2D image plane at a particular<br />
location within an organ, and even more difficult to find the same location again<br />
later. Thus, 2D US is not optimal for planning or monitoring therapeutic procedures,<br />
or for performing quantitative prospective or follow-up studies.<br />
Consequently, the diagnostician or physician must mentally integrate many 2D<br />
images to form an impression of the 3D anatomy and pathology. This process is<br />
time-consuming and inefficient, but more important, variable and subjective.<br />
Most 3D ultrasound systems have used conventional ultrasound machines with 1D<br />
arrays to collect multiple 2D images and reconstruct them into 3D images. Two<br />
important criteria must be met to avoid inaccuracies or distortions: (1) the relative<br />
position and angulation of the acquired 2D images must be accurately known so that<br />
the reconstructed 3D image is not distorted; and (2)<br />
the image acquisition must be carried out rapidly and/or gated to avoid artifacts<br />
caused by respiratory, cardiac and involuntary motion.<br />
Although 3D ultrasound is a promising tool to image many anatomical sites in the<br />
fetus and the adult female, its clinical benefits are still being researched. There is no<br />
question that the pictures far exceed the surface detail of the traditional grainy,<br />
black-and-white, 2D ultrasound images. However, at the present time 3D ultrasound<br />
is rarely critical in reaching the correct diagnosis and it may take a few more years<br />
before the place of 3D ultrasound as a diagnostic tool can be defined more precisely.<br />
There are scant outcome studies and much research is needed as the 3D technology<br />
is further developed.<br />
Review History<br />
September 9, 2003<br />
July 2006<br />
August 2007<br />
July 2009<br />
April 2011<br />
<strong>Medical</strong> Advisory Council<br />
Update – no revisions<br />
Update – no revisions<br />
Update. No Revisions. Codes reviewed.<br />
Update. Added Medicare Table. No revisions.<br />
Patient Education Websites<br />
English<br />
1. American College of Radiology, Radiological Society of North America.<br />
Ultrasound: Obstetric. Available at:<br />
http://www.radiologyinfo.org/en/info.cfm?PG=obstetricus<br />
Spanish<br />
1. American College of Radiology, Radiological Society of North America.<br />
Ultrasonido obstétrico. Acesso en:<br />
http://www.radiologyinfo.org/sp/info.cfm?pg=obstetricus<br />
This policy is based on the following evidence-based guidelines:<br />
1. American College of Obstetrics and Gynecology. (ACOG) Practice Bulletin<br />
Number 58. Clinical Management Guidelines for Obstetrician-Gynecologist.<br />
Ultrasonography in Pregnancy. December 2004<br />
Three Dimensional Obstetric Ultrasound Apr 11 7
Posted: April 2011<br />
2. American Institute of Ultrasound in Medicine. 3D Technology. Nov 2005.<br />
Available at:<br />
http://www.aium.org/publications/statements/_statementSelected.asp?stateme<br />
nt=23<br />
3. Hayes <strong>Medical</strong> Technology Directory. Three-Dimensional and Four-Dimensional<br />
Ultrasound for Extrafetal and Maternal Structures in Pregnancy. July 2006<br />
4. Hayes <strong>Medical</strong> Technology Directory. Three-Dimensional and Four-Dimensional<br />
Ultrasound for Diagnosis of Fetal Head Abnormalities. Nov 2005<br />
5. Hayes <strong>Medical</strong> Technology Directory Three-Dimensional and Four-Dimensional<br />
Ultrasound for High-Risk Pregnancies and Routine Screening. Nov 2005<br />
6. American College of Obstetricians and Gynecologists (ACOG), Committee on<br />
Practice Bulletins. Obstetrics. Ultrasonography in pregnancy. ACOG Practice<br />
Bulletin No. 101. Washington, DC: ACOG; February 2009.<br />
References – Update April 2011<br />
1. Yagel S, Cohen SM, Messing B, Valsky DV. Three-dimensional and fourdimensional<br />
ultrasound applications in fetal medicine. Curr Opin Obstet Gynecol.<br />
2009;21(2):167-174.<br />
2. Chen M, Wang HF, Leung TY, et al. First trimester measurements of nasal bone<br />
length using three-dimensional ultrasound. Prenat Diagn. 2009;29(8):766-770.<br />
References – Update July 2009<br />
1. American College of Obstetricians and Gynecologists (ACOG), Committee on<br />
Practice Bulletins. Obstetrics. Ultrasonography in pregnancy. ACOG Practice<br />
Bulletin No. 98. Washington, DC: ACOG; October 2008.<br />
2. Clinical Practice Obstetrics Committee; Maternal Fetal Medicine Committee,<br />
Delaney M, Roggensack A, Leduc DC, et al. Guidelines for the management of<br />
pregnancy at 41+0 to 42+0 weeks. J Obstet Gynaecol Can. 2008;30(9):800-<br />
823.<br />
3. Chen M, Lee CP, Lam YH, et al. Comparison of nuchal and detailed morphology<br />
ultrasound examinations in early pregnancy for fetal structural abnormality<br />
screening: A randomized controlled trial. Ultrasound Obstet Gynecol.<br />
2008;31(2):136-146; discussion 146.<br />
References – Update August 2007<br />
1. Wang LM, Leung KY, Tang M. Prenatal evaluation of facial clefts by threedimensional<br />
extended imaging. Prenat Diagn. 2007 May 29;<br />
2. Lapaire O, Alder J, Peukert R, Holzgreve W, Tercanli S. Two- versus threedimensional<br />
ultrasound in the second and third trimester of pregnancy: impact<br />
on recognition and maternal-fetal bonding. A prospective pilot study. Arch<br />
Gynecol Obstet. 2007 Apr 25.<br />
3. Goncalves LF, Lee W, Espinoza J, Romero R. Three- and 4-dimensional<br />
ultrasound in obstetric practice: does it help? J Ultrasound Med. 2005<br />
Dec;24(12):1599-624.<br />
4. Towner D, Boe N, Lou K, Gilbert WM. Cervical length measurements in<br />
pregnancy are longer when measured with three-dimensional transvaginal<br />
ultrasound. J Matern Fetal Neonatal Med. 2004 Sep;16(3):167-70.<br />
References<br />
1. Salim R, Woelfer B, Backos M, et al. Reproducibility of three-dimensional<br />
ultrasound diagnosis of congenital uterine anomalies. Ultrasound Obstet<br />
Gynecol 2003; 21(6):578-82<br />
Three Dimensional Obstetric Ultrasound Apr 11 8
Posted: April 2011<br />
2. Ghi T. Two-dimensional ultrasound is accurate in the diagnosis of fetal<br />
craniofacial malformation. Ultrasound Obstet Gynecol 2002; 19(6):543-51<br />
3. Timor-Tritsch IE, Platt LD. Three-dimensional ultrasound experience in<br />
obstetrics. Curr Opin Obstet Gynecol 2002; 14(6):569-75<br />
4. Pooh RK, Pooh K. Transvaginal 3D and Doppler ultrasonography of the fetal<br />
brain. Semin Perinatol 2001; 25(1):38-43<br />
5. Kurjak A, Hafner T, Kos M, et al. Three-dimensional sonography in prenatal<br />
diagnosis: a luxury or a necessity? J Perinat Med 2000; 28(3):194-209<br />
6. Lai TH, Chang CH, Yu CH, et al. Prenatal diagnosis of alobar holoprosencephaly<br />
by two-dimensional and three-dimensional ultrasound. Prenat Diagn 2000;<br />
20(5):400-3<br />
7. Ayida G, Kennedy S, Barlow D, et al. Contrast sonography for uterine cavity<br />
assessment: A comparison of conventional two-dimensional with threedimensional<br />
transvaginal ultrasound: A pilot study. Fertil Steril 1996; 66:848<br />
8. Baba K, Okai T, Kozuma S, et al: Real-time processable three-dimensional US in<br />
obstetrics. Radiology 1997; 203:571<br />
9. Brandl H, Gritzky A, Haizinger M. Three-dimensional ultrasound: A dedicated<br />
system. Eur Radiol 1999; 9(suppl 3):S331,<br />
10. Brunner M, Obruca A, Bauer P, et al. Clinical application of volume estimation<br />
based on three-dimensional ultrasonography. Ultrasound Obstet Gynecol 1995;<br />
6:358<br />
11. Chang FM, Hsu KF, Ko HC, et al. Fetal heart volume assessment by threedimensional<br />
ultrasound. Ultrasound Obstet Gynecol 1997; 9:942<br />
12. Chang FM, Hsu KF, Ko HC, et al. Three-dimensional ultrasound assessment of<br />
fetal liver volume in normal pregnancy: A comparison of reproducibility with<br />
two-dimensional ultrasound and a search for a volume constant. Ultrasound<br />
Med Biol 1997; 23:381<br />
13. Downey DB, Fenster A. 3-D US: A maturing technology. Ultrasound Quarterly<br />
1998;14:25<br />
14. Feichtinger W. Transvaginal three-dimensional imaging. Fertil Steril 1998;<br />
70:374<br />
15. Thomas R, Pretorius N, Pretorius DH. Three-dimensional ultrasound imaging.<br />
UMB 1998; 24, 1243.<br />
16. Gilja OH, Hausken T, Berstad A, et al. Measurements of organ volume by<br />
ultrasonography. Proc Inst Mech Eng 1999; 213:247<br />
17. Johnson DD, Pretorius DH, Budorick NE, et al. Three-dimesnional ultrasound of<br />
the fetal lip and primary palate. Radiology 2000; 217:236<br />
18. Jurkovic D, Geipel A, Gruboeck K, et al. Three-dimensional ultrasound for the<br />
assessment of uterine anatomy and detection of congenital anomalies: A<br />
comparison with HSG and two-dimensional sonography. Ultrasound Obstet<br />
Gynecol 1995; 5:233<br />
19. Jurkovic D, Gruboeck K, Tailor A, et al. Ultrasound screening for congenital<br />
uterine anomalies. Br J Obstet Gynaecol 199; 104:1320<br />
20. Kupesic S, Kurjak A. Diagnosis and treatment outcome of the septate uterus.<br />
Croat Med J 1998; 39:185,<br />
21. Lee A, Eppel W, Sam C, et al. Intrauterine device localization by threedimensional<br />
transvaginal sonography. Ultrasound Obstet Gynecol 1997; 10:289<br />
22. Lee A, Kratochwil A, Stumpflen I, et al. Fetal lung volume determination by<br />
three-dimensional ultrasonography. Am J Obstet Gynecol 1996; 175:588<br />
23. Merz E. Three-dimensional transvaginal ultrasound in gynecological diagnosis.<br />
Ultrasound Obstet Gynecol 1999; 14:81<br />
Three Dimensional Obstetric Ultrasound Apr 11 9
Posted: April 2011<br />
24. Merz E, Weber G, Bahlmann F, et al. Application of transvaginal and abdominal<br />
three-dimensional ultrasound for the detection or exclusion of malformations of<br />
the fetal face. Ultrasound Obstet Gynecol 1997; 9:237<br />
25. Nelson TR, Pretorius DH. Three-dimensional ultrasound imaging. Ultrasound<br />
Med Biol 1998; 24:1243,<br />
26. Platt LD, Santulli T, Carlson DE, et al. Three-dimensional ultrasonography in<br />
obstetrics and gynecology: Preliminary experience. Am J Obstet Gynecol 1998;<br />
178:1199<br />
27. Session DR, Daniel SW, Dumesic DA. Three-dimensional ultrasound in<br />
gynecology. Journal of Gynecologic Techniques 1998; 4:125<br />
28. Shih JC, Shyu MK, Lee CN, et al. Antenatal depiction of the fetal ear with threedimensional<br />
ultrasonography. Obstet Gynecol 1998; 91:500<br />
29. Fenster A, Downey DB. 3-D ultrasound imaging: A review. IEEE Engineering in<br />
Medicine and Biology 1996; 15:41-51<br />
30. Fenster A, Tong S, Sherebrin S, et al. Three-dimensional ultrasound imaging.<br />
SPIE 1995; 2432:176.<br />
31. Rankin RN, Fenster A, Downey DB, et al. Three-dimensional sonographic<br />
reconstruction: techniques and diagnostic applications. AJR 1993; 161:695-702.<br />
32. Sherebrin S, Fenster A, Rankin R, Spence JD. Freehand three-dimensional<br />
ultrasound: implementation and applications. SPIE Physics of <strong>Medical</strong> Imaging<br />
1996; 2708:296-303.<br />
33. Pretorius DH, Nelson TR. Prenatal visualization of cranial sutures and<br />
fontanelles with three-dimensional ultrasonography. J Ultrasound Med 13:871-<br />
876, 1994.<br />
34. Pretorius DH, Nelson TR. Fetal face visualization using three-dimensional<br />
ultrasonography. J Ultrasound Med 14:349-356, 1995.<br />
35. Nelson TR, Pretorius DH. Three-dimensional ultrasound of fetal surface features.<br />
Ultras Obstet Gynecol 1992; 2:166.<br />
Important Notice<br />
General Purpose.<br />
<strong>Health</strong> <strong>Net</strong>'s <strong>National</strong> <strong>Medical</strong> Policies (the "Policies") are developed to assist <strong>Health</strong> <strong>Net</strong> in administering<br />
plan benefits and determining whether a particular procedure, drug, service or supply is medically<br />
necessary. The Policies are based upon a review of the available clinical information including clinical<br />
outcome studies in the peer-reviewed published medical literature, regulatory status of the drug or device,<br />
evidence-based guidelines of governmental bodies, and evidence-based guidelines and positions of select<br />
national health professional organizations. Coverage determinations are made on a case-by-case basis<br />
and are subject to all of the terms, conditions, limitations, and exclusions of the member's contract,<br />
including medical necessity requirements. <strong>Health</strong> <strong>Net</strong> may use the Policies to determine whether under the<br />
facts and circumstances of a particular case, the proposed procedure, drug, service or supply is medically<br />
necessary. The conclusion that a procedure, drug, service or supply is medically necessary does not<br />
constitute coverage. The member's contract defines which procedure, drug, service or supply is covered,<br />
excluded, limited, or subject to dollar caps. The policy provides for clearly written, reasonable and current<br />
criteria that have been approved by <strong>Health</strong> <strong>Net</strong>’s <strong>National</strong> <strong>Medical</strong> Advisory Council (MAC). The clinical<br />
criteria and medical policies provide guidelines for determining the medical necessity criteria for specific<br />
procedures, equipment, and services. In order to be eligible, all services must be medically necessary and<br />
otherwise defined in the member's benefits contract as described this " Important Notice" disclaimer. In all<br />
cases, final benefit determinations are based on the applicable contract language. To the extent there are<br />
any conflicts between medical policy guidelines and applicable contract language, the contract language<br />
prevails. <strong>Medical</strong> policy is not intended to override the policy that defines the member’s benefits, nor is it<br />
intended to dictate to providers how to practice medicine.<br />
<strong>Policy</strong> Effective Date and Defined Terms.<br />
The date of posting is not the effective date of the <strong>Policy</strong>. The <strong>Policy</strong> is effective as of the date determined<br />
by <strong>Health</strong> <strong>Net</strong>. All policies are subject to applicable legal and regulatory mandates and requirements for<br />
prior notification. If there is a discrepancy between the policy effective date and legal mandates and<br />
regulatory requirements, the requirements of law and regulation shall govern. * In some states, new or<br />
revised policies require prior notice or posting on the website before a policy is deemed effective. For<br />
Three Dimensional Obstetric Ultrasound Apr 11 10
Posted: April 2011<br />
information regarding the effective dates of Policies, contact your provider representative. The Policies do<br />
not include definitions. All terms are defined by <strong>Health</strong> <strong>Net</strong>. For information regarding the definitions of<br />
terms used in the Policies, contact your provider representative.<br />
<strong>Policy</strong> Amendment without Notice.<br />
<strong>Health</strong> <strong>Net</strong> reserves the right to amend the Policies without notice to providers or Members. In some<br />
states, new or revised policies require prior notice or website posting before an amendment is deemed<br />
effective.<br />
No <strong>Medical</strong> Advice.<br />
The Policies do not constitute medical advice. <strong>Health</strong> <strong>Net</strong> does not provide or recommend treatment to<br />
members. Members should consult with their treating physician in connection with diagnosis and<br />
treatment decisions.<br />
No Authorization or Guarantee of Coverage.<br />
The Policies do not constitute authorization or guarantee of coverage of particular procedure, drug, service<br />
or supply. Members and providers should refer to the Member contract to determine if exclusions,<br />
limitations, and dollar caps apply to a particular procedure, drug, service or supply.<br />
<strong>Policy</strong> Limitation: Member’s Contract Controls Coverage Determinations.<br />
The determination of coverage for a particular procedure, drug, service or supply is not based upon the<br />
Policies, but rather is subject to the facts of the individual clinical case, terms and conditions of the<br />
member’s contract, and requirements of applicable laws and regulations. The contract language contains<br />
specific terms and conditions, including pre-existing conditions, limitations, exclusions, benefit maximums,<br />
eligibility, and other relevant terms and conditions of coverage. In the event the Member’s contract (also<br />
known as the benefit contract, coverage document, or evidence of coverage) conflicts with the Policies,<br />
the Member’s contract shall govern. Coverage decisions are the result of the terms and conditions of the<br />
Member’s benefit contract. The Policies do not replace or amend the Member’s contract. If there is a<br />
discrepancy between the Policies and the Member’s contract, the Member’s contract shall govern.<br />
<strong>Policy</strong> Limitation: Legal and Regulatory Mandates and Requirements.<br />
The determinations of coverage for a particular procedure, drug, service or supply is subject to applicable<br />
legal and regulatory mandates and requirements. If there is a discrepancy between the Policies and legal<br />
mandates and regulatory requirements, the requirements of law and regulation shall govern.<br />
<strong>Policy</strong> Limitations: Medicare and Medicaid.<br />
Policies specifically developed to assist <strong>Health</strong> <strong>Net</strong> in administering Medicare or Medicaid plan benefits and<br />
determining coverage for a particular procedure, drug, service or supply for Medicare or Medicaid<br />
members shall not be construed to apply to any other <strong>Health</strong> <strong>Net</strong> plans and members. The Policies shall<br />
not be interpreted to limit the benefits afforded Medicare and Medicaid members by law and regulation.<br />
Three Dimensional Obstetric Ultrasound Apr 11 11