Wksp 307_Mariotti - Alliance for Academic Internal Medicine
Wksp 307_Mariotti - Alliance for Academic Internal Medicine
Wksp 307_Mariotti - Alliance for Academic Internal Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Ambulatory Redesign in<br />
Residency Training<br />
PCMH Model<br />
APDIM<br />
Spring 2011<br />
Jennifer <strong>Mariotti</strong>, DO, FACP<br />
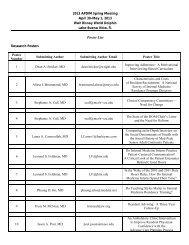
Workshop / Presentation<br />
■<br />
■<br />
■<br />
■<br />
Goal - Provide an individualized map <strong>for</strong> residency practice and<br />
ambulatory educational re<strong>for</strong>m grounded in quality improvement<br />
Template provided<br />
– Work through the document as we discuss different topics<br />
– Consider your program / experience<br />
• Action plan on potential changes / learnings<br />
– Map out your tangible “to do” next steps<br />
Collaborative learning<br />
– Open <strong>for</strong>um / sharing of ideas and concepts<br />
Change your current framework<br />
– Cause you to think differently about your residents ambulatory experience<br />
– Reflect honestly and openly<br />
• Training environment and the culture <strong>for</strong> improvement
■ Key areas?<br />
Clear Expectations<br />
■ One major take away?<br />
■ Review of our learnings / literature<br />
■ Tools utilized / Resources<br />
My Background<br />
■ Related Experience<br />
– Associate Program Director<br />
• <strong>Internal</strong> <strong>Medicine</strong><br />
• PD – Osteopathic Internship<br />
– Medical Director – Residency Clinic<br />
• PCMH / Residency Collaborative Participation<br />
– Quality Leader<br />
• Department of <strong>Medicine</strong> - LVHN<br />
• IHI OS GME Interest Group Facilitator
■<br />
Overview<br />
National call <strong>for</strong> residency redesign - ambulatory education<br />
■ Key element - Develop a core model –<br />
– Quality improvement culture within residency practice<br />
– Achieve high quality clinical outcomes in an educational environment<br />
■<br />
How do you do this?<br />
– Integrate residents into the quality improvement mechanism<br />
• Achieve sustainability<br />
– New models of resident scheduling<br />
– Continuity of care / Modified open access<br />
– EMR implementation<br />
– Patient centered medical home (PCMH) model concepts<br />
• Certification – Should you / Why would you / When<br />
– Key quality data metrics – Resident considerations<br />
– Integration of PBLI and SBP competencies<br />
– Balance / navigate system change vs. educational opportunities<br />
■<br />
■<br />
Charting Course - Roadmap<br />
National call <strong>for</strong> residency redesign - ambulatory education<br />
– Changes in practice of medicine<br />
• Chronic care / population p management – Separate outpt / inpt<br />
– Work hour restrictions<br />
– Shortage of PCPs<br />
– Increasing focus on patient safety<br />
Educational Experience<br />
– Dysfunctional residency practices<br />
– Poor clinical experiences<br />
– Low ambulatory primary care matriculation<br />
– Emphasize inpatient medicine / Ambulatory is an “add on”<br />
– Strong use of “clinics”<br />
• Primary venue <strong>for</strong> ambulatory medicine<br />
• Common – dysfunctional settings<br />
The “ICU” of ambulatory care<br />
1 Meyers F et al.Redesigning Residency training in internal medicine: The Consensus Report AAIM Redesign Task Force. <strong>Academic</strong> <strong>Medicine</strong>. 2007;82(12):1211-1219.<br />
2 Fitzgibbons J,et al. Redesigning Residency education in <strong>Internal</strong> <strong>Medicine</strong>: APDIM position paper. Annals of <strong>Internal</strong> <strong>Medicine</strong>. 2006;144(12):920-926.<br />
3 Batalden P,et al General Competencies and Accreditation in Graduate Medical Education. Health Affairs. 2002; 21(5):103-111.<br />
4.Holmboe E,et al. Re<strong>for</strong>ming <strong>Internal</strong> <strong>Medicine</strong> Residency Training: A Report from SGIM JGIM. 2005;20:1165-1172.<br />
5 Keirns C. et al. The unintended consequences of training residents in dysfunctional setting. Acad Med. 2008;83:498-502.
Quality Improvement<br />
“Every system is perfectly designed to get<br />
the results it gets”<br />
■<br />
■<br />
■<br />
■<br />
Mechanism <strong>for</strong> Change<br />
QI Committee<br />
Practice Trans<strong>for</strong>mation<br />
– DRIVER: On your own, Collaborative, Consultation<br />
Working group<br />
– Residency versus Practice<br />
• Focus defines the members<br />
Regular meetings<br />
– Leader – QI experience / ownership<br />
• Integrates with Residency / Practice / Faculty<br />
Prioritize projects<br />
– Start small and grow as you develop<br />
– Complete full PDCA as a group<br />
• Encourages sustainability<br />
– Tangible metrics / monitor and showcase
Quality Improvement<br />
■ Resources<br />
– Infrastructure – People / Knowledge<br />
• Faculty / key leader development<br />
• Tools <strong>for</strong> QI<br />
– Lean methods / A3 concepts / etc.<br />
– Resources –<br />
» IHI open school<br />
» ACMQ – American college of medical quality<br />
» APDIM<br />
»TJC<br />
Quality Improvement<br />
■ Resources<br />
– Infrastructure - Team<br />
• Key areas should be represented<br />
• Want engagement (sometimes opponents are best)<br />
• Multiple residents / consistent presence<br />
• Faculty – Core if possible<br />
– Ensure consistent and productive meetings<br />
• Define goals together / need a safe culture
Quality Improvement<br />
■ Resources<br />
– I/S needs<br />
• Analyst / Support liaison<br />
– Key to success – need strong relationship<br />
• Database <strong>for</strong> enterprise in<strong>for</strong>mation<br />
• Business Intelligence tools <strong>for</strong> analysis<br />
• Understanding of data management in system<br />
■<br />
Redesign - What do you do?<br />
National call <strong>for</strong> residency redesign - ambulatory education<br />
■ Key element - Develop a core model –<br />
– Quality improvement culture within residency practice<br />
– Achieve high quality clinical outcomes in an educational environment<br />
■<br />
How do you do this?<br />
– Integrate residents into the quality improvement mechanism<br />
• Achieve sustainability<br />
– New models of resident scheduling<br />
– Continuity of care / Modified open access<br />
– EMR implementation<br />
– Patient centered medical home (PCMH) model concepts<br />
• Certification – Should you / Why would you / When<br />
– Key quality data metrics – Resident considerations<br />
– Integration of PBLI and SBP competencies<br />
– Balance / navigate system change vs. educational opportunities
Ambulatory Redesign<br />
■ Structure – People<br />
– Work<strong>for</strong>ce distribution / Operational structure<br />
■ Process:<br />
– Scheduling Model (*Specific Linear Order)<br />
• Resident Schedule<br />
– Team Model<br />
• Patient Schedule – Open Access model<br />
– Continuity<br />
Scheduling<br />
■ Core Structure – Residency<br />
– Scheduling Model (*Specific Linear Order)<br />
• Resident Schedule<br />
– Team Model<br />
• Patient Schedule – Open Access model<br />
– Continuity
Question<br />
Does your program follow the traditional<br />
one clinic session / week model?<br />
■ Yes<br />
■ No<br />
Question<br />
Are you satisfied with that model?<br />
■ Yes<br />
■ No<br />
■ Don’t know
Resident Scheduling<br />
■<br />
■<br />
■<br />
Separate inpatient and outpatient<br />
Strengthen ambulatory exposure / emphasis<br />
– Make outpatient medicine IMPORTANT<br />
Immersion training<br />
– Long block versus weekly concept<br />
• Year long; 4:1; 4:2 Model<br />
– Example template - Review<br />
■<br />
Model selection depends on inherent program<br />
requirements / needs<br />
Example Long-Block Schedule<br />
1 Warm E, et al. The ambulatory long block; An ACGME EIP. JGIM 23 (7); 921-6.
Example 4:1; 4:2 Schedule<br />
1 <strong>Mariotti</strong> J et al The 4:1 Schedule; A novel template. JGME. 12/10; 541-7.<br />
2 Shalaby M et al. Developing new models of ambulatory training. AAIM Insight 8:3. 12-17.<br />
The Details -<br />
Inpatient Team Structure
4:1 Theory - CMO Matrix<br />
Context Mechanism Outcome<br />
Separation of inpatient and<br />
outpatient experiences <strong>for</strong><br />
the residents<br />
Residents would have<br />
dedicated weeks in clinic<br />
Residents wouldn’t have to<br />
work in both venues at<br />
once<br />
Extra time in clinic would<br />
allow residents to learn<br />
about the clinic process<br />
- Less internal conflict<br />
- Less frustration<br />
- Less “tense” environment<br />
- Better work satisfaction<br />
- More focused learning<br />
- More efficient care<br />
- More effective care<br />
- Better satisfaction<br />
A complicated schedule -<br />
Residents split into five<br />
different cohorts<br />
Residents wouldn’t be<br />
pulled to clinic<br />
More “slots” <strong>for</strong> patients<br />
Resident staggering<br />
They would have more<br />
focused time on rotations<br />
- Enhanced continuity<br />
- Overlap on inpatient care<br />
-“Team”-feel in clinic<br />
-Tougher to find “switches”<br />
- Better rotation education<br />
- More time with preceptors<br />
4:1 Schedule Results<br />
Educational Environment Learnings<br />
• Better sense of “team” in clinic<br />
• No pressure to “get out of clinic”<br />
• Allowed residents to focus on clinic patients<br />
• “Immersion” model resident engagement<br />
in change / improvement ef<strong>for</strong>ts<br />
• Cons:<br />
• Difficult <strong>for</strong> short term follow up<br />
• Requires a team model <strong>for</strong> cross coverage
Immersion Training<br />
(Ambulatory Block) Outcomes<br />
■ Consistent research findings<br />
– Satisfaction improved<br />
• Residents, patients, faculty<br />
• Enhanced ownership and engagement<br />
– Quality Measures improved<br />
– Continuity / No-Show rates improved<br />
■ PD / Resident perspective article<br />
1 Warm E, et al. The ambulatory long block; An ACGME EIP. JGIM 23 (7); 921-6.<br />
2 <strong>Mariotti</strong> J et al The 4:1 Schedule; A novel template. JGME. 12/10; 541-7.<br />
3 Shalaby M et al. Developing new models of ambulatory training. AAIM Insight 8:3. 12-17.<br />
4 Thomas K et al. Alternative approaches to ambulatory training: Resident and PD perspectives. JGIM 24(8):904-10.<br />
Open Collaborative Discussion<br />
■ Other scheduling models?
Scheduling<br />
■ Core Structure – Residency<br />
– Scheduling Model (*Specific Linear Order)<br />
• Resident Schedule<br />
– Team Model<br />
• Patient Schedule – Open Access model<br />
– Continuity<br />
Question<br />
Does your outpatient resident practice function<br />
in a team model?<br />
■ Yes<br />
■ No<br />
■ Don’t know
Question<br />
If you don’t currently use a team model, did you<br />
try it in the past and find it didn’t work?<br />
■ Yes<br />
■ No<br />
■ Don’t know<br />
Team Development<br />
■ Clinical model<br />
– Team development<br />
• Three core resident teams (a, b, c)<br />
– (+/-) Staff linkage<br />
• Delineation of administrative work<br />
• Patient panels defined * Referenced later<br />
– Dedicated preceptors per team<br />
• Allowed <strong>for</strong> Attending continuity<br />
• 3 residents:1 faculty ratio<br />
– Selected faculty practice at site
Ambulatory Scheduling<br />
■ Clinical model<br />
– 6 sessions of clinic, 3 sessions other ambulatory<br />
LVPP<br />
Team schedule<br />
Session Monday Tuesday Wednesday Thursday Friday<br />
AM AB BC AC BC AB<br />
PM AC AC Education AB BC<br />
Ambulatory Scheduling<br />
■ Each team<br />
– All within same 4:1 cohort<br />
– Integration of PGY years<br />
– Separate clinical “space”<br />
■ Consideration <strong>for</strong> staffing linkage
1 Hern T. Patient Care management teams: improving continuity, office efficiency, and teamwork in a residency clinic. JGME. 09/09. 67-72<br />
Provider Team Model<br />
■ Research Findings<br />
– Improvement in ratings of:<br />
• Learning opportunities<br />
• Quality of teaching<br />
• Job satisfaction<br />
• Employee Autonomy<br />
• Staff roles<br />
• Staff attitudes toward residents<br />
– Patient care management teams<br />
• Continuity it of patient t<br />
care<br />
• Office efficiency<br />
• Team communication<br />
– Essential <strong>for</strong> continuity – Residency model<br />
1 Roth L, Effects of implementation of a team model on physician and staff perceptions of a clinic’s organizational and learning environments. FMed, 2009; 41(6):434-9.<br />
2 Hern T. Patient Care management teams: improving continuity, office efficiency, and teamwork in a residency clinic. JGME. 09/09. 67-72<br />
3 Kennedy f. Implementation of an open access scheduling system in a residency training program. FMed 2003; 35(9):666-70
Open Collaborative Discussion<br />
■ Team model considerations<br />
Scheduling<br />
■ Core Structure – Residency<br />
– Scheduling Model (*Specific Linear Order)<br />
• Resident Schedule<br />
– Team Model<br />
• Patient Schedule – Open Access model<br />
– Continuity
Question<br />
Are you familiar with the concept of an open<br />
access model (or a modified open access)?<br />
■ Yes<br />
■ No<br />
■ Maybe<br />
Question<br />
Does your outpatient resident practice schedule<br />
using an open access model (or modified)?<br />
■ Yes<br />
■ No<br />
■ Don’t know
(Modified) Open Access<br />
■<br />
■<br />
■<br />
■<br />
Defined: “Doing today’s work today”<br />
Element of PCMH (access)<br />
Scheduling model<br />
– Traditional Open Access –<br />
• Appointments are open 48 hours prior<br />
• No advanced booking<br />
– Modified Open Access –<br />
(Preferred in GME due to limited availability)<br />
• Some advance appointments<br />
– 5 week follow up / 2 week continuity / 24 hr prior acute<br />
• Consistent ambulatory scheduling allows <strong>for</strong> continuity<br />
– An appointment is an appointment – focus is on continuity<br />
A REMINDER SYSTEM is the key <strong>for</strong> chronic population continuity!<br />
– How this reminder system functions can define the success of open<br />
access model<br />
■ Benefits:<br />
Modified Open Access<br />
– Allows <strong>for</strong> acute changes in schedules<br />
• Necessary with residency demands<br />
– Decreases no – show rates<br />
• No-Show rate – Cut in ½<br />
– Consistent t experience across practices<br />
• Optimizes educational exposure<br />
– More patients seen / session
Open Access Model<br />
■ Tangible Process<br />
– Have resource handouts on how to<br />
transition<br />
Open Access Model<br />
■ Research Findings<br />
– Charges / revenues increased<br />
• Visits per FTE, lower no show rate<br />
– Total monthly volumes – increase<br />
– Improved satisfaction<br />
• Patient / Provider<br />
– Reduce appointment delays<br />
– Improved patient-PCP match<br />
1 Kennedy J. Implementation of an open access scheduling system in a residency training program. FMed 2003; 35(9); 666-70<br />
2 Belardi F. A controlled trial of an advanced access appointment system in a residency family medicine center. Fmed 2004;36(5):341-5
Modified Open Access<br />
(Continuity Focus)<br />
■ Need assigned preferred providers –<br />
– How many have assigned panels?<br />
• What size panel <strong>for</strong> your residents?<br />
• How do you maintain assignments?<br />
– Reports Run / Excel management / EMR assistance<br />
• Correct assignment is INTEGRAL to assessing continuity with<br />
a provider – Requires oversight!<br />
– Continuity – priority with chronic conditions<br />
• Reminder system / preferred provider system can be<br />
structured to optimize your resident experience<br />
■<br />
A helpful method to integrate PCMH principle<br />
(primary provider) within GME context<br />
Patient / Provider Continuity<br />
■ Are you able to maintain continuity<br />
between providers and patients?<br />
– Yes<br />
– No<br />
– Not sure
Patient / Provider Continuity<br />
■ Do you measure continuity?<br />
– Yes<br />
– No<br />
– Not sure<br />
Continuity<br />
■ Discussion on barriers to continuity<br />
■ Discussion on how you make it work
■ MMCI<br />
Continuity Measurement<br />
■ Provider Index<br />
■ Patient Index<br />
■ Chronic condition patients vs. everyone<br />
■ Continuity is necessary <strong>for</strong> provider<br />
population data to be “meaningful”<br />
1 Darden, P. Comparison of continuity in a resident versus private practice. Peds 2001;108;1263-1268<br />
2 Breslau N. Continuity Reexamined: Differential impact on satisfaction with medical care <strong>for</strong> disabled and normal children. Medical Care April 1982;Vol XX, No 4; 347-359<br />
3 Morgan E et al. Continuity of care and patient satisfaction in a family practice clinic. J am Board Fam Pract 2004;17:341-6.<br />
Continuity Research<br />
■ Increased satisfaction<br />
– Patient / Provider / Staff<br />
■ Decreased resource utilization / costs<br />
■ Decreased ED utilization<br />
■ Improved chronic disease recognition<br />
■ Decreased hospitalizations<br />
■ Improved clinical outcomes<br />
1 Saultz J, et al Interpersonal continuity of care and patient satisfaction: A critical review. Annals of family medicine. 2004;2(5):445-451.<br />
2 Becker M, et al A field experiment to evaluate various outcomes of continuity of physician care. AJPH. 1974;64(11):1062-1070.<br />
3 Raddish M,et al Continuity of care: Is it cost effective? Am J Managed care. 1999;5:727-734.<br />
4.Rosenblatt R,et al The effect of the doctor patient relationship on ED use among the elderly. Am J Public Health. 2000;90:97-102.<br />
5.Gill J,er al The effect of continuity of care on ED use. Arch Family <strong>Medicine</strong>. 2000;9:333-338.<br />
6.Koopman R, et al. Continuity of care and recognition of diabetes, hypertension and hypercholesterolemia. Arch <strong>Internal</strong> <strong>Medicine</strong>. 2003;163:1357-1361.<br />
7 Gill J, Mainous A. The role of provider continuity in preventing hospitalizations. Arch Family <strong>Medicine</strong>. 1998;7:352-357.<br />
8.Cabana M, Jee S. Does continuity of care improve patient outcomes? The journal of family practice. 2004;53(12):974 - 980.
Continuity Research<br />
■ Chronic care patients<br />
– Continuity means the most<br />
■ Acute care<br />
– Continuity less important<br />
■ Team based continuity ~ way <strong>for</strong>ward<br />
– Need to balance fast access and ability to<br />
consult a known and trusted doctor<br />
1 Mainous A. Advanced access, open access, and continuity of care: should we en<strong>for</strong>ce continuity? FMed 2009;41(1):57-8.<br />
Open Collaborative Discussion<br />
■ Open Access considerations<br />
■ Continuity considerations
■<br />
Redesign - What do you do?<br />
National call <strong>for</strong> residency redesign - ambulatory education<br />
■ Key element - Develop a core model –<br />
– Quality improvement culture within residency practice<br />
– Achieve high quality clinical outcomes in an educational environment<br />
■<br />
How do you do this?<br />
– Integrate residents into the quality improvement mechanism<br />
• Achieve sustainability<br />
– New models of resident scheduling<br />
– Continuity of care / Modified open access<br />
– EMR implementation<br />
– Patient centered medical home (PCMH) model concepts<br />
• Certification – Should you / Why would you / When<br />
– Key quality data metrics – Resident considerations<br />
– Integration of PBLI and SBP competencies<br />
– Balance / navigate system change vs. educational opportunities<br />
Ambulatory Redesign<br />
■<br />
■<br />
Structure<br />
– EMR Tool<br />
Process / Workflows (*Specific Linear Order)<br />
• Simple usage / in<strong>for</strong>mation entry<br />
– Workflow learning<br />
• Focusing entry of data (meaningful locations)<br />
– OBS fields / trackable fields<br />
• Report Generation / Data Audit / Feedback<br />
• Clinical Decision support tools (meaningful use)<br />
– Templates / Clinical reports
EMR<br />
■ What status is your practice with EMR?<br />
– Not implemented, no plans to do so<br />
– Not implemented, gearing up soon<br />
– Implemented < 1 yr ago<br />
– Implemented 2-5 yrs ago<br />
– Implemented >5 yrs ago<br />
EMR<br />
■ If implemented, how do you feel about<br />
EMR?<br />
– Hate it!<br />
– Necessary Evil, some pros and cons<br />
– Love it!<br />
– Not sure
■ First Year<br />
EMR Utilization<br />
– Simple usage / in<strong>for</strong>mation entry<br />
• Workflow learning<br />
– Ensure workflows are defined (standard)<br />
• Review in<strong>for</strong>mation with residents regularly<br />
– Difficult to expect learners to navigate<br />
Clinical Decision Support tools at this<br />
stage
EMR Implementation<br />
■ Second Year (meaningful use)<br />
– Focusing entry of data<br />
• Meaningful locations<br />
– OBS fields / trackable fields<br />
– Report Generation<br />
• Requires continuity * if using population data<br />
– Highly recommend individualized feedback<br />
– Data Audit / Feedback<br />
• Focuses residents on where to enter data to get “credit”<br />
– Will discuss at PCMH tenets / PBLI
EMR Implementation<br />
■ Second – Third Year<br />
– Utilization can move further<br />
• Clinical Decision support tools<br />
– Meaningful use<br />
• Templates / Clinical reports<br />
– Asthma / Lipids / Preoperative / etc.<br />
– Educational Tool<br />
• Solidify EBM guidelines / concepts<br />
• Guide treatment algorithms
EMR Positive Considerations<br />
■ Positive Considerations:<br />
– Personal teaching files<br />
– Per<strong>for</strong>mance reporting<br />
• Outcome / Procedure tracking<br />
– Documentation<br />
• More detail usually reported<br />
• Electronic history prompts optimized<br />
Peled J. Do electronic health records help or hinder education? PLOS <strong>Medicine</strong>. May 2009; 6(5); 1-5.<br />
EMR Educational Tool<br />
■ Research<br />
– Point of care education<br />
• New knowledge best assimilated when<br />
learned in context<br />
• Electronic order sets / template notes<br />
– Computerized CDS system<br />
• Any system to assist in decision making<br />
– Research, QI education and core<br />
competencies<br />
1 Keenan C. EMRs and their impact on resident and medical student education. <strong>Academic</strong> Psychiatry 2006;30:522-527
EMR Research / Attitudes<br />
■ Observations / Learnings<br />
– EMRs bypass synthesis of clinical in<strong>for</strong>mation<br />
• Attending knows all the case elements<br />
• Prevents learners from presenting patient data in words<br />
– Creates an educational exercise<br />
– Could cause unprocessed in<strong>for</strong>mation transfer<br />
– EMR is a distractor<br />
• “Staring into a screen”<br />
• Less interaction among patients / faculty<br />
• Faculty swiftly click through a chart to answer questions<br />
rather than pose them to learner<br />
– Robs them of questions that occur to a more seasoned<br />
clinician<br />
Peled J. Do electronic health records help or hinder education? PLOS <strong>Medicine</strong>. May 2009; 6(5); 1-5.<br />
EMR Research / Attitudes<br />
■ Observations / Learnings<br />
– Copy and Waste<br />
• Potential source of error / waste in EMR<br />
– “Readily available security”<br />
• Not checking data in advance because quick<br />
access is possible<br />
• Prevents opportunities to explore things on<br />
their own<br />
Peled J. Do electronic health records help or hinder education? PLOS <strong>Medicine</strong>. May 2009; 6(5); 1-5.
EMR Research / Attitudes<br />
■ Challenges / Barriers to EMR adoption<br />
– Time it takes to enter in<strong>for</strong>mation<br />
• Paper compared to EMR<br />
– Requires exact diagnosis / exact lab testing<br />
– Double work – paper then EMR<br />
– Intrusion on the patient / provider interaction<br />
– Potential impact on quality documentation<br />
• Could be worse if time is an issue<br />
• Ensuring note is “accurate”<br />
– Not documenting what wasn’t done<br />
• Strongly monitor the use of templates!<br />
1 Ilie V. et al. Paper versus Electronic: Challenges associated with physicians usage of EMRs. Proceedings of the 40 th Hawaii IC on Social systems - 2007<br />
EMR Educational Considerations<br />
■ Educational Elements:<br />
– Faculty should actively avoid referring to source<br />
data during presentations<br />
– Faculty / learner / patient interactions should be<br />
fostered in conducive environment<br />
• Encourage face to face encounters<br />
– Copying and pasting<br />
• Could be banned<br />
Peled J. Do electronic health records help or hinder education? PLOS <strong>Medicine</strong>. May 2009; 6(5); 1-5.
EMR Educational Considerations<br />
■ Educational Elements:<br />
– Learners (Students / GME) should be<br />
encouraged to actively check labs prior to<br />
presentations<br />
– Incorporate teaching of EMR specific<br />
communication to learners<br />
• Introduce computer / adjust geography / 30<br />
second rule / share data with patients<br />
Peled J. Do electronic health records help or hinder education? PLOS <strong>Medicine</strong>. May 2009; 6(5); 1-5.<br />
■ EMR Usage<br />
Open Discussion<br />
– Discussion on Educational benefit<br />
– Goal –<br />
• Educational development versus system<br />
redesign <strong>for</strong> Quality integration<br />
i<br />
– Opportunities <strong>for</strong> data / audit feedback
Quality Improvement<br />
Data considerations <strong>for</strong> resident learners:<br />
■<br />
■<br />
■<br />
Ensuring resident’s personal data / data ownership<br />
– Will likely need team model <strong>for</strong> some metrics (pop based)<br />
– Continuity is critical be<strong>for</strong>e data can be delivered<br />
Point of care data metrics – alternative <strong>for</strong> GME<br />
learners<br />
– E.g. – foot exams / DM patient<br />
• Staff education / per<strong>for</strong>mance of monofilament<br />
• Resident per<strong>for</strong>mance and assurance of completion<br />
• Can review data and ensure done on all patients each week<br />
Population management versus individual<br />
management<br />
– Each carries different considerations<br />
Quality Improvement<br />
General data considerations:<br />
■ Process versus Outcome data metrics<br />
– Did they “do” the right thing?<br />
• DM Foot exam<br />
• Vaccination completion<br />
– Flu / Pneumovax – DM patients<br />
• Preventive maintenance<br />
– Mammography tracking<br />
• Can be facilitated by EMR / prompting / clinical decision<br />
support tools
Quality Improvement<br />
■ Process versus Outcome metrics<br />
– Did they achieve a better “outcome”<br />
• Enhanced glucose control<br />
– Better HbA1C control in a population<br />
» Truly measure after a “process” change<br />
» Clinical case mgr involvement<br />
• Patient satisfaction / Provider satisfaction<br />
– Satisfaction surveys / Press Ganey surveys<br />
• Decreased no – show rates<br />
– Implementation of open access, use of no-show letters,<br />
defined protocol that was en<strong>for</strong>ced, enhanced<br />
communication with patients (call center), notification on<br />
entering practice
■<br />
Redesign - What do you do?<br />
National call <strong>for</strong> residency redesign - ambulatory education<br />
■ Key element - Develop a core model –<br />
– Quality improvement culture within residency practice<br />
– Achieve high quality clinical outcomes in an educational environment<br />
■<br />
How do you do this?<br />
– Integrate residents into the quality improvement mechanism<br />
• Achieve sustainability<br />
– New models of resident scheduling<br />
– Continuity of care / Modified open access<br />
– EMR implementation<br />
– Patient centered medical home (PCMH) model concepts<br />
• Certification – Should you / Why would you / When<br />
– Key quality data metrics – Resident considerations<br />
– Integration of PBLI and SBP competencies<br />
– Balance / navigate system change vs. educational opportunities<br />
Ambulatory Redesign<br />
■ Structure<br />
– Patient Centered Medical Home<br />
■ Process = System change ~ Practice-wide QI<br />
mechanism<br />
– Population management<br />
– Per<strong>for</strong>mance reporting / PBLI<br />
– Balance of education versus system support
PCMH<br />
Is your residency practice certified?<br />
■ Yes<br />
■ No, but working on it<br />
■ No, no plans right now<br />
■ Not sure<br />
Patient Centered Medical Home<br />
AAFP, AAP, ACP, AOA: March, 2007<br />
■ Personal Physician<br />
■ Physician directed medical practice<br />
■ Whole person orientation<br />
■ Care – coordinated and/or integrated<br />
■ Quality of care / culture of patient safety<br />
■ Enhanced access to care<br />
■ Payment Re<strong>for</strong>m<br />
http://www.pcpcc.net/
■ Are you doing it<br />
BUT…<br />
SYSTEMATICALLY?<br />
– And<br />
ARE YOU GETTING PAID FOR IT?<br />
- And<br />
ARE YOUR LEARNERS INVOLVED?<br />
PCMH – Associated with:<br />
■ Better outcomes<br />
■ Reduced mortality<br />
■ Fewer preventable hospital admissions<br />
■ Lower utilization<br />
■ Improved patient compliance<br />
■ Lower medicare spending<br />
Evidence of Quality Summary Report, 2009 (PCPCC)
National Committee <strong>for</strong> Quality<br />
Assurance (NCQA)<br />
■ PPC – PCMH Recognition<br />
– Level 1, 2, and 3<br />
■ NCQA supported by<br />
– AAFP / AAP / ACP / AOA<br />
– Washington based not-<strong>for</strong>-profit<br />
healthcare QI organization<br />
The Joint Commission<br />
■ Primary Care Home Option<br />
– Accreditation of ambulatory health care<br />
organizations<br />
– Working with Medicare / Medicaid / Insurance<br />
carriers to ensure standards will allow <strong>for</strong><br />
recognition as PCH provider<br />
■ Starting in July 2011<br />
– Standards to be released in November ‘10, final<br />
standards in March ‘11 and on-site surveys in<br />
July ’11.
PCMH Focus<br />
■ Application process<br />
– Online survey to upload documents<br />
– 9 part process to accreditation<br />
• PPC 1 - Access and communication<br />
• PPC 2 - Patient tracking and registry<br />
• PPC 3 – Care management<br />
• PPC 4 – Patient self-management support<br />
• PPC 5 – Electronic prescribing<br />
• PPC 6 – Test tracking<br />
• PPC 7 – Referral tracking<br />
• PPC 8 – Per<strong>for</strong>mance reporting and improvement<br />
• PPC 9 – Advanced electronic communication<br />
PCMH Focus<br />
■ Application process<br />
– Documentation supporting per<strong>for</strong>mance<br />
– Includes:<br />
• Protocols / policies<br />
• Data reports (% demographics on charting, %<br />
active problem list, etc)<br />
– EMR is integral with this area<br />
• Screen shots of EMR / examples of<br />
documents that show protocols used<br />
• Population management reports / how used
PCMH Focus<br />
■ Collaborative insights<br />
– PAFP Family medicine residency<br />
collaborative<br />
• ~30 residency programs in state<br />
– Tandem PA-Governor collaborative<br />
– Shared resources / documents<br />
– Coaching provided / guidance<br />
– Goal – application submission<br />
PCMH Focus<br />
■<br />
■<br />
Resident involvement<br />
– In application process – limited # of resident champions<br />
– Should ideally be through core QI / PI mechanism in<br />
practice or through feedback related to initiative<br />
PCMH process facilitates QI / PI to occur – resident<br />
integration should be downstream of actual<br />
certification process but in the middle of the change<br />
ef<strong>for</strong>ts themselves<br />
– Understanding of process and certification is encouraged
Quality Improvement<br />
■ Learner involvement observations<br />
PLAN / DO<br />
– Group project / Strong faculty mentorship<br />
– Develop an infrastructure to allow them to be a<br />
member and not have to “lead” the team<br />
– “Buy in” to the project<br />
– Consistent interaction with lead faculty to guide<br />
observations and progress<br />
– Interactions allow <strong>for</strong> experiential learning<br />
Quality Improvement<br />
■ Learner involvement observations<br />
CHECK (DATA)<br />
– Needs to be “specific”<br />
• Provide the residents with key directions on where and<br />
what needs to be done<br />
• For example – review this excel file and per<strong>for</strong>m X<br />
– Needs faculty mentoring<br />
– Data management / interpretation<br />
– Chart reviews<br />
– Database maintenance
Quality Improvement<br />
■ Learner Involvement<br />
ACT<br />
– Feeding back data / changes to occur<br />
– Consistent communication key<br />
– If personal initiative – have residents be<br />
the ones to deliver the message<br />
PCMH Focus<br />
■ Do I NEED to certify my residency<br />
practice as a PCMH?<br />
– Proactive approach – health care re<strong>for</strong>m<br />
reimbursement model<br />
– Core concepts of practice trans<strong>for</strong>mation<br />
are the ultimate t goals<br />
• Areas that are emphasized align well with<br />
Residency Ambulatory Redesign<br />
– Can be used as a model / reason <strong>for</strong> re<strong>for</strong>m
PCMH Tenets &<br />
Ambulatory Redesign<br />
• PPC 1 - Access and communication<br />
– Scheduling / Modified Open Access Model<br />
• PPC 2 - Patient tracking and registry<br />
– Assignments of Preferred Provider / EMR Reporting<br />
• PPC 3 – Care management<br />
– System support providing population management<br />
• PPC 4 – Patient self-management support<br />
– Resident involvement in group visit education<br />
• PPC 5 – Electronic prescribing<br />
– EMR Provided<br />
PCMH Tenets &<br />
Ambulatory Redesign<br />
• PPC 6 – Test tracking<br />
– EMR Provided<br />
• PPC 7 – Referral tracking<br />
– EMR Provided<br />
• PPC 8 – Per<strong>for</strong>mance reporting and improvement<br />
– Data feedback to residents / PBLI / SBP<br />
• PPC 9 – Advanced electronic communication<br />
– EMR Provided<br />
d<br />
■ EMR can be viewed as independent<br />
educational tool as well
PCMH Certification Assistance<br />
■ Collaborative Support<br />
– State Sponsored / ACP / IPIP<br />
■ ACP Medical Home Builder<br />
– acponline.org/medicalhomebuilder<br />
■ Consultants<br />
■ Trans<strong>for</strong>MED<br />
– http://www.trans<strong>for</strong>med.com/<br />
Balance System Change vs.<br />
Educational Development<br />
■ Hand-in-Hand Model<br />
■ System redesign is future of primary care<br />
– Chronic Care Model<br />
– Learning how to change a larger system<br />
■ Teaching residents how to navigate<br />
– Use Clinical Decision Support Tools<br />
– Focus on medicine and allow system to support<br />
the other “tasks”<br />
• “Tasks <strong>for</strong> Staff / Decisions <strong>for</strong> Physicians”<br />
– (Dr. Warning)
Personalized Template<br />
■ What kind of QI mechanism do you<br />
have currently in your practice?<br />
– Who is your identified leader of QI?<br />
■ Check off areas that you might find<br />
helpful<br />
■ Map out your action plan <strong>for</strong> follow up<br />
■ Concepts / Ideas – “Take-away”<br />
Thank you <strong>for</strong> your time!<br />
■ Questions / Thoughts