2013 APDIM Spring Meeting Poster Reception - Alliance for ...
2013 APDIM Spring Meeting Poster Reception - Alliance for ...
2013 APDIM Spring Meeting Poster Reception - Alliance for ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
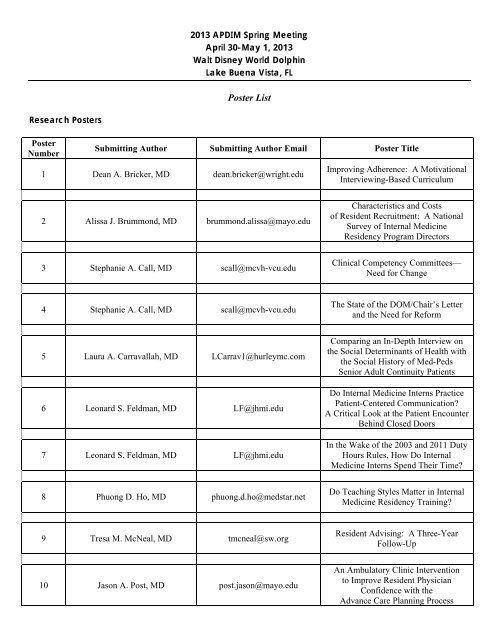
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong><br />
April 30-May 1, <strong>2013</strong><br />
Walt Disney World Dolphin<br />
Lake Buena Vista, FL<br />
<strong>Poster</strong> List<br />
Research <strong>Poster</strong>s<br />
<strong>Poster</strong><br />
Number<br />
Submitting Author Submitting Author Email <strong>Poster</strong> Title<br />
1 Dean A. Bricker, MD dean.bricker@wright.edu<br />
Improving Adherence: A Motivational<br />
Interviewing-Based Curriculum<br />
2 Alissa J. Brummond, MD brummond.alissa@mayo.edu<br />
Characteristics and Costs<br />
of Resident Recruitment: A National<br />
Survey of Internal Medicine<br />
Residency Program Directors<br />
3 Stephanie A. Call, MD scall@mcvh-vcu.edu<br />
Clinical Competency Committees—<br />
Need <strong>for</strong> Change<br />
4 Stephanie A. Call, MD scall@mcvh-vcu.edu<br />
The State of the DOM/Chair’s Letter<br />
and the Need <strong>for</strong> Re<strong>for</strong>m<br />
5 Laura A. Carravallah, MD LCarrav1@hurleymc.com<br />
6 Leonard S. Feldman, MD LF@jhmi.edu<br />
7 Leonard S. Feldman, MD LF@jhmi.edu<br />
Comparing an In-Depth Interview on<br />
the Social Determinants of Health with<br />
the Social History of Med-Peds<br />
Senior Adult Continuity Patients<br />
Do Internal Medicine Interns Practice<br />
Patient-Centered Communication?<br />
A Critical Look at the Patient Encounter<br />
Behind Closed Doors<br />
In the Wake of the 2003 and 2011 Duty<br />
Hours Rules, How Do Internal<br />
Medicine Interns Spend Their Time?<br />
8 Phuong D. Ho, MD phuong.d.ho@medstar.net<br />
Do Teaching Styles Matter in Internal<br />
Medicine Residency Training?<br />
9 Tresa M. McNeal, MD tmcneal@sw.org<br />
Resident Advising: A Three-Year<br />
Follow-Up<br />
10 Jason A. Post, MD post.jason@mayo.edu<br />
An Ambulatory Clinic Intervention<br />
to Improve Resident Physician<br />
Confidence with the<br />
Advance Care Planning Process
11 Ruby P. Shah, MD ruby.shah@ucdmc.ucdavis.edu<br />
12 Sara L. Swenson, MD swensosl@sutterhealth.org<br />
13 Kris G. Thomas, MD thomas.kris@mayo.edu<br />
Generalist Career Outcomes<br />
of University of Cali<strong>for</strong>nia Davis<br />
Graduates: A Longitudinal Study<br />
Thinking of Quitting: Predictors<br />
of Considering Resignation Among<br />
Internal Medicine Program Directors<br />
The Educational Innovations Project<br />
(EIP)—Association Between Residency<br />
Program Participation and<br />
Medical Education Publications<br />
14 Heather A. Thompson Buum, MD thomp057@umn.edu<br />
Duty Hours Monitoring Revisited:<br />
Self-Report May Not Be Adequate<br />
15 Laurel Fick, MD lbfick@stvincent.org<br />
Patient Census: What is Optimal<br />
<strong>for</strong> Educational Satisfaction<br />
and Quality of Care Balance?<br />
Programmatic Innovation <strong>Poster</strong>s<br />
<strong>Poster</strong><br />
Number<br />
Submitting Author Submitting Author Email <strong>Poster</strong> Title<br />
16 Laurel Fick, MD lbfick@stvincent.org<br />
The Triple Threat—Novel<br />
Hospitalist-Track Electives<br />
17 Alisa Duran-Nelson, MD duran012@umn.edu<br />
Procedural Competence:<br />
From See One, Do One, Teach One<br />
to an Entrustable Professional Activity<br />
18 Ola Al Sous, MD alsouso@trinity-health.org<br />
Transition of Care: A New Curriculum<br />
to Enhance Safer Hospital Discharges<br />
19 Sandy Balwan, MD sbalwan@NSHS.edu<br />
Transitional Care: A Novel,<br />
Narrative Initiative<br />
20 Poonam Beniwal-Patel, MD pbeniwal@mcw.edu<br />
Night Float Cards:<br />
An Educational Endeavor<br />
21 Christina R. Bergin, MD christina.bergin@bannerhealth.com<br />
22 Steffanie R. Campbell, MD Steffanie.Campbell@bcm.edu<br />
Improving Patient Satisfaction<br />
Outcomes, Resident Interpersonal<br />
Communication Skills,<br />
and Resident Feedback<br />
Does the Time<br />
of Educational Conference Impact<br />
Patient Discharge Times?<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> List Page 2
23 Amy F. Matthews amatthews@uchc.edu<br />
24 Brian M. Cohee, MD brian.m.cohee.mil@health.mil<br />
25 Jennifer A. Corbelli, MD corbellija@upmc.edu<br />
Incorporating a Longitudinal<br />
Subspecialty Continuity Clinic<br />
into Internal Medicine Training<br />
Achieving Balance on the Inpatient<br />
Internal Medicine Wards:<br />
A Per<strong>for</strong>mance Improvement Project<br />
to Restructure Resident Work Hours<br />
at a Tertiary Care Center<br />
Breast Cancer Screening and Prevention<br />
in Primary Care: A Novel Curricular<br />
Intervention <strong>for</strong> Medicine Housestaff<br />
26 Nathan E. Derhammer, MD nderhammer@lumc.edu Chief Resident Leadership Academy<br />
27 Christopher Dittus, DO cdittus@nshs.edu<br />
28 Scott R. Friedstrom, MD friedstrom@yahoo.com<br />
29 Brian J. Hanson, MD hans3829@umn.edu<br />
“The Chief’s Seminar”:<br />
Motivating New Residents<br />
to Master Clinical Reasoning<br />
Objectification and Meaningful<br />
Implementation of a Medicine<br />
Curriculum Designed to Produce the<br />
Next Generation of Physician Leaders<br />
Innovative and Successful<br />
Evidence-Based Morning Report<br />
Linked to Resident-Led Journal Club<br />
30 Katherine Harris, MD harriski@healthcare.uiowa.edu<br />
Tea(ch) Time: An Afternoon Approach<br />
to Morning Report<br />
31 Saba A. Hasan, MD shasan@capitalhealth.org<br />
“You Must Be the Change You Wish<br />
to See in the World.” -Mahatma Gandhi<br />
32 Stephen J. Knaus, MD sjknaus@stvincent.org<br />
33 Tasha Kouvatsos, MD tasha.kouvatsos@gmail.com<br />
Ambulatory Case Conference—<br />
A Novel Approach<br />
to Outpatient Education<br />
Morbidity and Mortality Conference<br />
Working Group—<br />
Resident Driven Change<br />
34 Gina Luciano, MD gina.luciano@baystatehealth.org The July Transition—Making It Easier<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> List Page 3
35 Srikrishna V. Malayala, MD varun_msk@yahoo.com<br />
36 Jared Moore, MD jared.moore@osumc.edu<br />
A Refined Patient Safety and Quality<br />
Improvement Curriculum <strong>for</strong> Internal<br />
Medicine Residents—Based<br />
on a Six-Year Feedback and Review<br />
Preparing Residents <strong>for</strong> Team-Based<br />
Patient Care: The Development<br />
and Implementation<br />
of a Resident Leadership<br />
and Management Training Program<br />
37 Brandon R. Murguia, MD Brandon.Murguia@dignityhealth.org<br />
The Next Step in Collaborative Care:<br />
Medical-Legal Partnerships<br />
38 Moyna H. Ng, MD mng3@nshs.edu<br />
Improving Resident Documentation:<br />
Coding and Billing Practices<br />
with a Practical Tutorial<br />
39 Kerri L. Palamara, MD kpalamara@partners.org<br />
Ambulatory Clinician-Educator<br />
Rotation <strong>for</strong> Primary Care Residents<br />
40 Kerri L. Palamara, MD kpalamara@partners.org<br />
41 David Paje, MD DPAJE1@hfhs.org<br />
42 Anne G. Pereira, MD anne.pereira@hcmed.org<br />
43 Seth Politano, DO politano@usc.edu<br />
44 Patrick A. Rendon, MD prendon@salud.unm.edu<br />
45 Eileen E. Reynolds, MD ereynold@bidmc.harvard.edu<br />
46 Lloyd Rucker, MD lrucker@uci.edu<br />
Less Sinking and More Swimming:<br />
Resident Primary Care<br />
Immersion Blocks<br />
Training Residents <strong>for</strong> Independent<br />
Inpatient Practice (TRIIP): Ongoing<br />
Development of a Novel Clinical<br />
Rotation Using PDCA<br />
and Milestones to Improve<br />
Education in Hospital Medicine<br />
Remediating Residents in Transition:<br />
Individualizing the<br />
Learner-Manager-Teacher Model<br />
Training Homework: Does a Structured<br />
Reading and Testing Program<br />
Improve Per<strong>for</strong>mance<br />
on the ABIM In-Training Exam?<br />
“Intern Boot Camp”:<br />
Case-Based Interactive Curriculum<br />
<strong>for</strong> the New Intern<br />
Hospital Practice Profiles:<br />
Improving Training by Linking Patient<br />
Outcomes to Resident Practice<br />
Best Cases Create Best Case Scenario:<br />
Educational Competition<br />
to Improve Resident Experience<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> List Page 4
47 Lloyd Rucker, MD lrucker@uci.edu<br />
Cost Awareness Curriculum<br />
<strong>for</strong> Residents<br />
48 Bindu K. Swaroop, MD bkswaroop@yahoo.com<br />
49 Adam Sawatsky, MD sawatskyap@upmc.edu<br />
A Resident-Driven<br />
Mini-Lecture Curriculum<br />
<strong>for</strong> Inpatient Internal Medicine<br />
The Last Lecture? Uniting Resident<br />
Preferences and Principles<br />
of Adult Learning to Improve<br />
the Noon Conference Lecture Series<br />
50 Michael P. Stevens, MD mstevens@mcvh-vcu.edu<br />
It’s All in the Execution: Description<br />
of a Duty Hours Monitoring Process<br />
51 Vishnu Laalitha Surapaneni, MD<br />
VishnuLaalitha.Surapaneni<br />
@UHhospitals.org<br />
Optimizing Resident Handoffs<br />
52 Tabassum Salam, MD tsalam@christianacare.org<br />
53 David B. Sweet, MD sweetd@summahealth.org<br />
54 Hailey Vincent, MD hvincent@sw.org<br />
Raising Resident Awareness of Their<br />
Role in Quality and Safety<br />
Through Patient Safety Discussions<br />
Resident-Led Decision Support<br />
Huddles to Improve Risk Factors<br />
<strong>for</strong> Patients with Diabetes<br />
Hands-On Quality Improvement:<br />
A Curriculum <strong>for</strong> Team-Based,<br />
Resident-Led Projects Training<br />
Residents in Quality Improvement<br />
Using Small Groups<br />
and Resident-Initiated Projects<br />
55 Bennett S. Vogelman, MD bsv@medicine.wisc.edu<br />
Outcomes from a Three-Year QI<br />
Residency Education Program<br />
56 Ekterina A. Vypritskaya, MD evypritskaya@capitalhealth.org<br />
57 Eric J. Warm, MD warmej@ucmail.uc.edu<br />
“If You Listen Carefully to the Patient,<br />
They Will Tell You the Diagnosis.”<br />
-Sir William Osler<br />
A Novel Assessment System Created<br />
by Mapping Milestones<br />
to Entrustable Professional Activities<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> List Page 5
Research <strong>Poster</strong> Abstracts<br />
<strong>Poster</strong> Number: 1<br />
<strong>Poster</strong> Title: Improving Adherence: A Motivational Interviewing-Based Curriculum<br />
Authors and Affiliate Institutions: Dean Bricker, Paul Hershberger, Wright State University Boonshoft School of<br />
Medicine<br />
Submitting Author<br />
Dean A. Bricker, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
Wright State University Boonshoft School of Medicine<br />
Weber CHE Building, Second Floor<br />
128 East Apple Street<br />
Dayton, OH 45409-2902<br />
Telephone: (937) 510-2663<br />
Email: dean.bricker@wright.edu<br />
Background: Nonadherence to prescribed treatments is both common and costly. With a prevalence of 50% or<br />
greater, residents encounter nonadherence multiple times each day, yet few programs provide specific training on<br />
this topic. The patient-provider relationship affects medication adherence. Thus we sought train providers to<br />
engage patients in a more patient-centered fashion emphasizing how medications are discussed. We targeted<br />
understanding motivational interviewing, use of open-ended questions and reflective statement as a means to have<br />
patients talk about their barriers to adherence.<br />
Aim: To develop and evaluate a motivational interviewing-based curriculum designed to enhance resident<br />
knowledge and skills <strong>for</strong> promoting patient adherence.<br />
Methods: The curriculum consisted of 4 half-day training modules that occurred once per week during an<br />
ambulatory block rotation. Each block typically included 6 learners: 2 IM R1, 2 FM R1, and 2 sixth year pharmacy<br />
students. The first session involved interactive discussion of factual content: 1) the scope of the adherence<br />
problem, 2) barriers to adherence, 3) collaborative care principles, 4) self-management plans, and 5) motivational<br />
interviewing philosophy/techniques. The second module emphasized skills practice utilizing role plays. In the third<br />
module, learners interviewed a standardized patient and the interviews were video recorded. The group also<br />
reviewed video of each learner with one of her/his real patients. The final session included review of the<br />
standardized patient videos. We used a 20-question quiz to assess learner’s knowledge and a 6-item survey to<br />
assess skills confidence. We evaluated our video review <strong>for</strong>m <strong>for</strong> inter-rater reliability and used it to assess videorecorded<br />
interviews.<br />
Results: Fifty-nine learners completed the curriculum in 2011-12. Knowledge scores improved from 11.6 (58%<br />
correct) to 16.1 (80.0% correct) at course completion (p < 0.001). Confidence improved <strong>for</strong> all items surveyed (p <<br />
0.001) at course completion. We demonstrated good inter-rater reliability <strong>for</strong> our interview skills assessment <strong>for</strong>m<br />
with regard to use of open-ended versus closed questions. Learner’s showed improvements in the open-question:<br />
closed-question ratios from early rotation compared with scores <strong>for</strong> interviewing a standardized patient at course<br />
completion (ratio 1.14 vs. 1.84; p = 0.023).<br />
Discussion or Conclusion: Learners demonstrated improvements in knowledge and confidence as well as some<br />
elements of motivational interviewing skills.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 1
<strong>2013</strong> Mayo Foundation <strong>for</strong> Medical Education and Research<br />
Characteristics and Costs of Resident Recruitment: A National Survey of<br />
Internal Medicine Residency Program Directors<br />
Alissa Brummond MD, 1 Susan Sefcik MD, 2 Andrew J. Halvorsen MS, 1 Saima Chaudhry MD MSHS, 3 Vineet Arora MD MAPP, 4 Mike Adams MD, 5 Maria Lucarelli MD, 6 Furman S. McDonald MD MPH, 1 Darcy A. Reed, MD MPH 1<br />
1 Department of Medicine, Mayo Clinic College of Medicine, 2 St. Lukes University Health Network, 3 North Shore-Long Island Jewish Hofstra School of Medicine, 4 University of Chicago Prtizker School of Medicine,<br />
5 Georgetown University School of Medicine, 6 Ohio State University Medical Center<br />
Background<br />
• Interest in internal medicine is declining and<br />
resources <strong>for</strong> residency recruitment are limited.<br />
• New regulations requiring programs to place all, or<br />
none, of their positions within NRMP are anticipated<br />
to increase recruitment costs; yet, costs of<br />
recruitment to U.S. residency programs have not<br />
been comprehensively examined.<br />
• The objective of this study was to describe<br />
recruitment to U.S. internal medicine residency<br />
programs and to estimate associated costs.<br />
Methods<br />
Cross-sectional survey of 353 U.S. categorical internal<br />
medicine residency program directors. Recruitment<br />
costs were estimated as the sum of the annual<br />
recruitment budget (food, hotels, supplies, etc.) and the<br />
percentage ef<strong>for</strong>t dedicated to recruitment by residency<br />
personnel multiplied by national salary data.<br />
Results<br />
• Surveys were returned by 270 (76.5%) program<br />
directors.<br />
• Programs received a mean (SD) of 2,314 (1579)<br />
applications and conducted 10 (4) interviews per<br />
resident position.<br />
• The estimated median (IQR) total cost of<br />
recruitment was $148,345 ($95,966-234,704) per<br />
program and $9,899 ($6,494-13,271) per<br />
matriculate.<br />
• In multivariate analysis, PGY1 class size (β=<br />
+$6,073; p
<strong>Poster</strong> Number: 2<br />
<strong>Poster</strong> Title: Characteristics and Costs of Resident Recruitment: A National Survey of Internal Medicine<br />
Residency Program Directors<br />
Authors and Affiliate Institutions: Alissa Brummond, Andrew Halvorsen, Furman McDonald, Darcy Reed,<br />
Mayo Clinic College of Medicine; Susan Sefcik, St. Luke’s of Bethlehem; Saima Chaudhry, Hofstra North Shore-<br />
LIJ School of Medicine at Hofstra University; Vineet M Arora, University of Chicago Pritzker School of Medicine;<br />
Mike Adams, Georgetown University School of Medicine; Stephanie Call, Virginia Commonwealth University<br />
Medical College of Virginia; Maria Lucarelli, Ohio State University College of Medicine<br />
Submitting Author<br />
Alissa J. Brummond, MD<br />
PGY 2 Resident<br />
Department of Internal Medicine<br />
Mayo Clinic College of Medicine<br />
200 First Street, SW<br />
Rochester, MN 55905<br />
Telephone: (507) 284-6391<br />
Email: brummond.alissa@mayo.edu<br />
Background: Interest in internal medicine is declining and resources <strong>for</strong> residency recruitment are limited. New<br />
regulations requiring programs to place all, or none, of their positions within National Resident Matching Program<br />
(NRMP) are anticipated to increase recruitment costs, yet costs of recruitment to U.S. residency programs have not<br />
been comprehensively examined.<br />
Aim: To describe recruitment to U.S. internal medicine residency programs and to estimate associated costs.<br />
Methods: Design: Cross-sectional survey Setting: U.S. categorical internal medicine residency programs<br />
Participants: 353 program directors Measures: Recruitment costs were estimated as the sum of the annual<br />
recruitment budget (food, hotels, supplies, etc.) and the percentage ef<strong>for</strong>t dedicated to recruitment by residency<br />
personnel multiplied by national salary data.<br />
Results: Surveys were returned by 270 (76.5%) program directors. Programs received a mean (SD) of 2,314<br />
(1579) applications and conducted 10 (4) interviews per resident position. The estimated median (IQR) total cost<br />
of recruitment was $148,345 ($95,966-234,704) per program and $9,899 ($6,494-13,271) per matriculate. In<br />
multivariate analysis, postgraduate year one (PGY1) class size (β= +$6,073; p
<strong>Poster</strong> Number: 3<br />
<strong>Poster</strong> Title: Clinical Competency Committees—Need <strong>for</strong> Change<br />
Authors and Affiliate Institutions: Stephanie Call, Virginia Commonwealth University; Jessica Salt, Gregory<br />
Kane, Jefferson Medical College of Thomas Jefferson University; Sapna Kuehl, St. Agnes Hospital; Vineet Arora,<br />
University of Chicago Pritzker School of Medicine<br />
Submitting Author<br />
Stephanie A. Call, MD<br />
Program Director<br />
Department of Internal Medicine<br />
Virginia Commonwealth University Medical College of Virginia<br />
PO Box 980509<br />
1200 East Broad Street<br />
Richmond, VA 23298<br />
Telephone: (804) 828-9726<br />
Email: scall@mcvh-vcu.edu<br />
Background: Internal medicine is implementing the Accreditation Council <strong>for</strong> Graduate Medical Education’s<br />
(ACGME) Next Accreditation System (NAS) in July of <strong>2013</strong> and is moving toward a more transparent<br />
competency-based advancement model. Despite the importance of the CCC, little is known of the best structure,<br />
authority lines, and approach to competency decisions.<br />
Aim: We describe the current variability in CCC characteristics.<br />
Methods: Questions regarding structure, function, authority and perceived effectiveness of Internal Medicine<br />
program CCCs were included on the 2011 annual <strong>APDIM</strong> Program Director (PD) survey. Data from the survey<br />
was merged in a de-identified database with publicly available data from the ACGME and ABIM. Descriptive<br />
statistics were per<strong>for</strong>med using SPSS; chi-squared tests were used to assess <strong>for</strong> differences.<br />
Results: The survey response rate was 68.5% (n=261). The average size of a CCC was 12.3 members; this varied<br />
with program characteristics. PD was most frequent chair of the CCC (59%), followed by Associate PD (23%),<br />
core faculty (12%), other (5%). PDs appointed the chair in 89.7% of programs; this varied by program size. A<br />
large majority of programs (79%) did not require <strong>for</strong>mal training of the CCC faculty. PDs reported the following<br />
CCC roles: remediation of residents (97.3%), advancement decisions (92.7%), assessment development (54.4%),<br />
biannual review process (49.8%), remediation of faculty (28.7%). Only 19% of programs reported a <strong>for</strong>mal process<br />
<strong>for</strong> granting residents more autonomy; this did not vary by program characteristics. The PD completed the ABIM<br />
tracking <strong>for</strong>m in 84% of programs, determined by PD alone in 40%. Only 11% of programs reported that the CCC<br />
made these decisions alone. One fourth of all programs reported that “every year I graduate at least one resident<br />
about whom I have concerns regarding their ability to practice independently.” Half of all programs reported that<br />
“each year I advance at least one resident about whom I have concerns regarding their ability to handle additional<br />
responsibility.”<br />
Discussion or Conclusion: Based on this data, it is clear that the structure, <strong>for</strong>mat, function, authority and<br />
effectiveness of these committees must change in order to enhance our ability to effectively evaluate, train, and<br />
ensure that every Internal Medicine residency graduate is ready <strong>for</strong> independent practice.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 3
<strong>Poster</strong> Number: 4<br />
<strong>Poster</strong> Title: The State of the DOM/Chair’s Letter and the Need <strong>for</strong> Re<strong>for</strong>m<br />
Authors and Affiliate Institutions: Ryan Vega, Georgia McIntosh, Maia LaVallee, Stephanie Call, Virginia<br />
Commonwealth University School of Medicine; Valerie Lang, University of Rochester School of Medicine and<br />
Dentistry<br />
Submitting Author<br />
Stephanie A. Call, MD<br />
Program Director<br />
Department of Internal Medicine<br />
Virginia Commonwealth University Medical College of Virginia<br />
PO Box 980509<br />
1200 East Broad Street<br />
Richmond, VA 23298<br />
Telephone: (804) 828-9726<br />
Email: scall@mcvh-vcu.edu<br />
Background: Internal Medicine Program Directors regard the Department of Medicine (DOM) letter as a valuable<br />
piece of in<strong>for</strong>mation in a residency applicant’s portfolio. An AAIM joint task <strong>for</strong>ce of Clerkship Directors and<br />
Program Directors recently developed a proposed set of guidelines <strong>for</strong> letter content.<br />
Aim: Our aim in this survey was to assess current variability in content and <strong>for</strong>mat of DOM letters.<br />
Methods: We identified DOM letters from our program’s pool of US LCME-accredited allopathic school<br />
graduating applicants in the NRMP 2012 and <strong>2013</strong> match seasons. We randomly selected one letter from each<br />
school <strong>for</strong> review. Letters were de-identified and then reviewed <strong>for</strong> content. We extracted data on 14 variables<br />
regarding length, structure, and content, including variables identified by the recently proposed guideline <strong>for</strong> DOM<br />
letter content. Data was managed and analyzed in Microsoft Excel. Descriptive statistics were per<strong>for</strong>med.<br />
Results: From our applicant pool, we accessed 116 of the 141 currently LCME accredited or provisionally<br />
accredited US allopathic schools (82%). There was significant variability in the content and quality of the letters.<br />
Regarding clerkship and letter descriptions, 89% met the recommended length; 37% contained a statement<br />
regarding letter preparation; 37% described the clerkship structure and content; 22% contained in<strong>for</strong>mation on<br />
grading policies; 23% contained a grade distribution <strong>for</strong> the clerkship. Regarding individual per<strong>for</strong>mance, 68%<br />
included the final clerkship grade; 19% included NBME shelf exam score; 78% contained some <strong>for</strong>m of detailed<br />
narrative on per<strong>for</strong>mance or verbatim comments. Only 11% of letters included a summary paragraph with student’s<br />
comparative rank. Only 20% of the letters included in<strong>for</strong>mation about students’ per<strong>for</strong>mance on the sub-internship<br />
rotation. Approximately 65% of letters included personal or historical in<strong>for</strong>mation which is not recommended in the<br />
guidelines. In total, only 44% of letters reviewed contained at least 5 of the criteria from the proposed guidelines.<br />
Discussion or Conclusion: There is significant variability in the content of the DOM letter. Based on<br />
recommendations of a national organization, key pieces are missing in a large proportion of letters. As this<br />
document is considered a critical piece of in<strong>for</strong>mation <strong>for</strong> program directors in the review of Internal Medicine<br />
candidates, there is a significant need <strong>for</strong> re<strong>for</strong>m in and standardization of letter content.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 4
Comparing an In-Depth Interview on the Social Determinants of Health<br />
with the Social History of Med-Peds Senior Adult Continuity Patients<br />
Laura Carravallah, Jowhara Zindani, Sunil Meruga, Gopesh K Singh, Nick Lecea, Vijay Naraparaju<br />
Hurley Medical Center, Flint, Michigan<br />
Michigan State University College of Human Medicine, East Lansing, Michigan<br />
BACKGROUND<br />
The impact of socioeconomic factors on health status is well<br />
delineated in the literature, and while estimates vary, most agree<br />
that social determinants may in fact play a greater role than biology,<br />
medical care and health behaviors combined. (Tarlov,1999)<br />
Determinants of Health<br />
Source: Dahlgren, G and Whitehead, M. 1991<br />
Literature Search<br />
Only one study (Griffith, et a, 1995) addressed the content and adequacy of<br />
the collection of social history by residents.<br />
Griffith and colleagues found that the residents had an answer <strong>for</strong> only 29%<br />
of the basic social history (excluding health habits) of their inpatients –<br />
residents who had primary responsibilty <strong>for</strong> the patient had slightly better<br />
recall..<br />
No studies compared a comprehensive independent patient interview with<br />
resident documentation and recall.<br />
No studies evaluated the adequacy and the relevance of social history<br />
obtained in the ambulatory setting by residents<br />
It is possible that increased contact and “ownership” of patients in<br />
continuity clinic may af<strong>for</strong>d better resident knowledge of these social<br />
determinants.<br />
ACGME - Internal Medicine Milestones<br />
We believe that the knowledge skills and attitudes required of the<br />
residents to successfully collect a history of social determinants is<br />
pertinent to the following Milestones:<br />
11. Transitions patients effectively within and across health delivery systems. (SBP4)<br />
Aspirational: Anticipates needs of patient, caregivers and future care providers and takes<br />
appropriate steps to address those needs<br />
18. Responds to each patient’s unique characteristics and needs. (PROF-3)<br />
Ready <strong>for</strong> Unsupervised Practice: Recognizes and accounts <strong>for</strong> the unique characteristics<br />
and needs of the patient/ caregiver; Appropriately modifies care plan to account <strong>for</strong> a<br />
patient’s unique characteristics and needs<br />
20. Communicates effectively with patients and caregivers. (ICS-1)<br />
Ready <strong>for</strong> Unsupervised Practice: Quickly establishes a therapeutic relationship with<br />
patients and caregivers, including persons of different socioeconomic and cultural<br />
backgrounds<br />
PURPOSE<br />
Source: Tarlov, 1999, also cited by CDC<br />
The “Social History” is a required part of the medical history, but the<br />
items are not standardized, and often include little more than the<br />
health habits of the patient.<br />
Estimate the prevalence of various social health<br />
determinants in our underserved adult continuity clinic<br />
population<br />
Determine the concordance of resident documentation and<br />
knowledge with this in<strong>for</strong>mation<br />
Determine resident and preceptor rating of the importance<br />
of these factors <strong>for</strong> patient’s care<br />
METHODS<br />
Setting<br />
Med-Peds Continuity Clinic situated in a federally subsidized<br />
Federally Qualified Health Center (FQHC) located in the northern<br />
part of Flint, MI.<br />
Subjects<br />
Patients – adult continuity clinic patients<br />
• Age ≥ 30 years with ≥ 1 chronic disease<br />
• Seen by same resident <strong>for</strong> > 3 times in 2 years<br />
• No active malignancy<br />
Residents – Med-Peds senior residents – PGY-3 & -4<br />
Study Procedure<br />
Study Interview Tool<br />
Sources <strong>for</strong> patient questionnaire<br />
Southwest Baltimore Community Health Survey (SWB)<br />
Multilevel Assessment Instrument (MAI)<br />
Cali<strong>for</strong>nia Health Interview Survey (CHIS-2009)<br />
Psychosocial Adjustment to Illness Scale (PAIS)<br />
Instrument Activities of Daily Living Scale (IADL)<br />
Bright Futures<br />
Rapid Estimate of Adult Literacy in Medicine (REALM-R)<br />
Categories<br />
physical environment<br />
activities of daily living<br />
social support systems<br />
spirituality and faith<br />
community<br />
adequate finances<br />
access to health care<br />
dependent care<br />
recreation<br />
transportation<br />
housing<br />
police, fire and<br />
security<br />
employment<br />
opportunity<br />
RESULTS<br />
occupational health<br />
education, including<br />
health literacy<br />
substance use<br />
mental health<br />
legal concerns<br />
Nutrition<br />
Residents<br />
8 senior residents (4 PGY-3 & 4 PGY-4) completed the interview.<br />
25% Female and 75% Male, all International Medical Graduates<br />
Patients<br />
25 adult continuity clinic patients<br />
60% Female and 40% Male, Ages 30-66 years (mean 49 years)<br />
56% Black, 40% White, and 4% Other<br />
80% HTN, 32% COPD, 28% DM, 20% arthritis, 12% CAD/CHF,<br />
8% CKD, 4% asthma<br />
Resident Knowledge and Importance of<br />
“Traditional” Social History > 90%:<br />
marital status<br />
social support<br />
employment<br />
insurance<br />
prescription<br />
drug coverage<br />
tobacco<br />
alcohol abuse<br />
prescription drug<br />
abuse<br />
street drug abuse<br />
Prevalence<br />
History of Abuse<br />
56%<br />
Unemployment<br />
56%<br />
Lack of<br />
Transportation<br />
46%<br />
Cannot Af<strong>for</strong>d<br />
Dental Care<br />
46%<br />
Financial Issues<br />
40%<br />
Discrimination<br />
40%<br />
Poor Health<br />
Literacy<br />
33%<br />
Lack of Sidewalks /<br />
Street Lights<br />
33%<br />
Legal Problems<br />
32%<br />
Cannot Af<strong>for</strong>d<br />
Eye Care<br />
56%<br />
Resident<br />
Documentation /<br />
Knowledge<br />
48%<br />
Chart<br />
76%<br />
Chart<br />
48%<br />
Chart<br />
60%<br />
Chart<br />
28%<br />
Chart<br />
16%<br />
Chart<br />
20%<br />
Chart<br />
0%<br />
Chart<br />
32%<br />
Chart<br />
76%<br />
Resident<br />
100%<br />
Resident<br />
76%<br />
Resident<br />
40%<br />
Resident<br />
72%<br />
Resident<br />
40%<br />
Resident<br />
48%<br />
Resident<br />
24%<br />
Resident<br />
72%<br />
Resident<br />
80% 80%<br />
Chart<br />
Resident<br />
Resident & Faculty<br />
Perceived Clinical<br />
Importance <strong>for</strong> the<br />
Specific Patient<br />
100% 100%<br />
Resident<br />
Faculty<br />
92% 100%<br />
Resident<br />
Faculty<br />
100% 100%<br />
Resident<br />
80%<br />
Resident<br />
84%<br />
Resident<br />
Faculty<br />
36%<br />
Faculty<br />
100%<br />
Faculty<br />
76% 80%<br />
Resident<br />
Faculty<br />
96% 100%<br />
Resident<br />
48%<br />
Resident<br />
Faculty<br />
80%<br />
Faculty<br />
64% 60%<br />
Resident<br />
Faculty<br />
84% 80%<br />
Resident<br />
Faculty<br />
DISCUSSION<br />
This pilot study shows that continuity patients seen by our<br />
residents in an FQHC face considerable health stress stemming<br />
from socioeconomic condition.<br />
Traditional social history questions provided very narrow<br />
in<strong>for</strong>mation. Similar to the study by Griffith, et al (1995), issues<br />
considered important in managing the patient were often missed.<br />
Residents in this study have improved their collection of social<br />
history as compared to the 1995 Griffith, et al study both in<br />
breadth and depth (vs. 30%). This may relate to the continuity<br />
clinic venue, as Griffith found that the accuracy residents<br />
improved with their level of primary responsibility <strong>for</strong> that patient.<br />
For the majority of the social determinants missed, residents and<br />
faculty rated the importance similarly<br />
Limitations of this pilot include: small sample size, single<br />
institution, semi-qualitative analysis, social desirability bias (both<br />
patients and residents), and lack of a comprehensive validated<br />
questionnaire <strong>for</strong> all categories.<br />
Conclusion and Next Steps<br />
We believe that we have gained valuable insight about the patient<br />
population we serve. Residents felt that most of these issues are<br />
important, but were unaware of many of these barriers affecting<br />
adherence and outcomes. It is clearly not feasible to do an hourlong<br />
interview on social determinants on every patient, but this<br />
study will allow us to prioritize our social history to those issues<br />
that are most prevalent and important <strong>for</strong> our patients.<br />
We have now converted to an EHR and we will be able to use this<br />
in<strong>for</strong>mation to develop templates that may allow us to obtain a<br />
more efficient and effective history. Current planned areas to<br />
improve education and data collection include: health literacy,<br />
transportation, nutrition (including food security) and<br />
environmental factors. We will re-audit after implementation.<br />
We also plan to have our residents do a comprehensive interview<br />
on one of their continuity patients and write a reflection as a<br />
method to enhance empathy. Correlation of accuracy of social<br />
history and scales measuring resident empathy may also give<br />
further insights.<br />
REFERENCES<br />
1. Griffith, C.H., Rich, E. C., and Wilson, J.F. (1995). Housestaff’s Knowledge of Their<br />
Patients’ Social Histories. Acad Med, 70(1), 64-66.<br />
2. Griffith, C.H., Wilson, J.F., and Rich, E.C., A Randomized Trial of Providing House Staff<br />
with Patient Social History In<strong>for</strong>mation: Effect on Patient Outcomes. Eval Health Prof,<br />
21(3), 362-376.<br />
3. Morgan-Hopkins Center <strong>for</strong> Health Disparities Solutions. SOUTH WEST BALTIMORE<br />
COMMUNITY HEALTH SURVEY (SWB). Rev. 4/2/2004. Johns Hopkins Bloomberg<br />
School of Public Health, Baltimore, MD<br />
4. Davis TC, Long SW, Jackson RH, et al. Rapid Estimate of Adult Literacy in Medicine<br />
(REALM-R) in Rapid estimate of adult literacyin medicine: a shortened screening<br />
instrument. Fam Med. 1993;25:391–5<br />
5. Lawton, MP, Moss, M, Fulcomer, M, Kleban M.Multi-Level Assessment Instrument (MAI)<br />
Manual <strong>for</strong> Full-length MAI. Madlyn and Leonard Abramson Center <strong>for</strong> Jewish Life<br />
6. Accreditation Council on Graduate Medical Education (ACGME). Program Requirements<br />
<strong>for</strong> Graduate Medical Education in Internal Medicine. July 1, 2009, pg. 18<br />
7. TarlovTARLOV, A. R. (1999), Public Policy Frameworks <strong>for</strong> Improving Population Health.<br />
Annals of the New York Academy of Sciences, 896: 281–293. doi: 10.1111/j.1749-<br />
6632.1999.tb08123<br />
8. CDC http://www.cdc.gov/socialdeterminants/FAQ.html accessed 4/24/<strong>2013</strong>
<strong>Poster</strong> Number: 5<br />
<strong>Poster</strong> Title: Comparing an In-Depth Interview on the Social Determinants of Health with the Social History of<br />
Med-Peds Senior Adult Continuity Patients<br />
Authors and Affiliate Institutions: Laura Carravallah, Sunil Meruga, Gopesh K Singh, Nick Lecea, Vijay<br />
Naraparaju, Hurley Medical Center/Michigan State University; Jowhara Zindani, Michigan State University<br />
College of Human Medicine; Gergana Kodjebacheva, University of Michigan Medical School<br />
Submitting Author<br />
Laura A. Carravallah, MD<br />
Program Director<br />
Department of Internal Medicine and Pediatrics<br />
Hurley Medical Center/Michigan State University College of Human Medicine<br />
3AW Combined Med-Peds Education<br />
One Hurley Plaza<br />
Flint, MI 48503<br />
Telephone: (810) 262-9283<br />
Email: LCarrav1@hurleymc.com<br />
Background: The impact of socioeconomic factors on health status is well delineated in the literature, but it is<br />
unknown how often residents elicit a comprehensive social history, nor the impact of any omissions on patient<br />
outcomes. While Griffith et al (1995) found that social histories in the inpatient setting were inadequate; this has<br />
not been studied in continuity clinic.<br />
Aim: To examine the resident recognition and assessment of importance of key psychosocial variables that may<br />
impact on the management our continuity patients.<br />
Methods: Senior resident adult continuity patients with chronic disease were invited to participate in a detailed<br />
interview on the social determinants of health compiled from questionnaires in the literature. After all interviews<br />
were completed, a chart audit assessed adequacy of documentation and the continuity resident was also quizzed<br />
about positive findings found in the interview. The resident and a faculty preceptor were asked to rate the clinical<br />
importance of that in<strong>for</strong>mation <strong>for</strong> that individual patient.<br />
Results: Twenty-five patients of 8 senior residents completed the interview. Major social problems identified<br />
include difficulties with employment (56%), transportation (46%), abuse (44%), finances (40%), medications<br />
(40%), discrimination (36%), health literacy (33%), legal system (32%), and health care access, particularly dental<br />
and eye. Documentation and resident knowledge was deficient, especially in the areas of physical environment<br />
(24%), discrimination (40%) and health illiteracy (48%). The greatest discrepancy between resident rating of<br />
importance vs. resident knowledge was around health illiteracy (96% vs.48%), discrimination (76% vs. 40%), and<br />
transportation and abuse (both 100% vs. 76%). Faculty ratings of importance were within 10% of the residents’<br />
with the exception of lack of streetlights/sidewalks (80% vs. 48%) and dental care (36% vs. 80%).<br />
Discussion or Conclusion: This pilot study shows that continuity patients seen by our residents face considerable<br />
health stress stemming from socioeconomic conditions. Traditional social history questions provided very narrow<br />
in<strong>for</strong>mation. While knowledge and documentation was better than in the inpatient sample in Griffith’s study, room<br />
<strong>for</strong> improvement remains. This study will help to focus education and screening protocols on important areas most<br />
often missed. Next steps will be to embed these protocols into our electronic health record.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 5
Do internal medicine interns practice etiquette-based communication?<br />
A critical look at the inpatient encounter<br />
Lauren Block, MD, MPH, Lindsey Hutzler, Robert Habicht, MD, Albert W. Wu, MD, MPH, Sanjay V. Desai, MD, Kathryn Novello Silva,<br />
MD, Timothy Niessen, MD, MPH, Nora Oliver, MD, and Leonard Feldman, MD<br />
Background<br />
• Institute of Medicine patient-centered care definition:<br />
• “Care that is respectful of and responsive to individual patient preferences, needs, and<br />
values, and ensuring that patient values guide all clinical decisions”<br />
• Etiquette-based medicine definition:<br />
• Term coined by Kahn<br />
• Subset of patient-centered communication<br />
• Includes simple behaviors that convey professionalism and respect to patients<br />
• Patient-centered communication may improve patient outcomes:<br />
• Make it easier <strong>for</strong> patients to disclose illness-related in<strong>for</strong>mation<br />
• May impact patient perceptions of safety, patient anxiety, patient satisfaction, functional<br />
status, and compliance with medical recommendations<br />
Behavior<br />
Introducing self<br />
Introducing role<br />
Sitting down<br />
Touching the patient<br />
Providing a name<br />
Results<br />
Observed behaviors and definitions<br />
Uses term “doctor”, “resident”, “intern”, or “medical team”<br />
Definition<br />
Sitting on the bed, in a chair, or crouching if no chair was available during at least part of the encounter<br />
Any <strong>for</strong>m of physical contact that occurred at least once during the encounter including shaking a patient’s hand, touching a<br />
patient on the shoulder, or per<strong>for</strong>ming any part of the physical exam.<br />
Frequency of per<strong>for</strong>ming behaviors during patient encounters by intern gender and shift type<br />
Total encounters N (%) Introduced self Introduced role Sat down Touched patient<br />
Conclusions<br />
•Internal medicine residents did not routinely practice behaviors comprising etiquettebased<br />
communication<br />
•Interns introduced themselves to patients in fewer than half of all observed encounters<br />
•Interns sat down with patients in fewer than 10% of encounters<br />
•Residents did not touch the patient in one third of visits, including during admitting<br />
shifts<br />
•We observed a high degree of variation between interns in per<strong>for</strong>mance of these<br />
behaviors<br />
•While interns believed they were practicing etiquette-based communication, as<br />
defined by Kahn, only a minority actually were<br />
Limitations<br />
• We sought to understand whether etiquette-based communication behaviors are practiced<br />
by trainees.<br />
• Study design and setting<br />
Specific hypotheses<br />
Methods<br />
• Cross-sectional prospective inpatient study incorporating direct observation of<br />
residents<br />
Overall 732 (100%) 40% 36% 9% 64%<br />
JHH 373 (51%) 35%*† 29%*† 10% 62%*<br />
UMD 359 (49%) 45% 44% 8% 69%<br />
Male 284 (39%) 39% 35% 9% 64%<br />
Female 448 (61%) 41% 38% 10% 67%<br />
Day shift 551 (75%) 37%* 34%* 9% 65%<br />
Night shift 181 (25%) 48% 45% 12% 67%<br />
Admitting shift 377 (52%) 46%* 42%* 10% 63% *<br />
Non-admitting shift 355 (48%) 34% 30% 9% 69%<br />
*<br />
•Study limited to two institutions in Baltimore, which limits external validity<br />
•Using non-medical observers may have caused measurement error<br />
•All 732 patient encounters were assessed, regardless of whether the resident had<br />
seen the patient previously or was leading the discussion on rounds<br />
•Hawthorne effect, change in behavior due to observation, is also possible<br />
•Survey was conducted 6 months after observations and limited to only 1 program<br />
Implications<br />
• PGY-1 residents in two internal medicine programs in Baltimore during January, 2012<br />
• Total of 29 interns observed (27% of interns in the two programs)<br />
• * p
<strong>Poster</strong> Number: 6<br />
<strong>Poster</strong> Title: Do Internal Medicine Interns Practice Patient-Centered Communication? A Critical Look at the<br />
Patient Encounter Behind Closed Doors<br />
Authors and Affiliate Institutions: Leonard Feldman, Lauren Block, Albert W Wu, Sanjay V Desai, Timothy<br />
Niessen, Lindsey Hutzler, Johns Hopkins University School of Medicine; Robert Habicht, University of Maryland<br />
School of Medicine<br />
Submitting Author<br />
Leonard S. Feldman, MD<br />
Assistant Professor<br />
Division of General Internal Medicine<br />
Department of Internal Medicine and Pediatrics<br />
Johns Hopkins University School of Medicine<br />
600 North Wolfe Street<br />
Nelson 215<br />
Baltimore, MD 21287<br />
Telephone: (443) 287-3135<br />
Email: LF@jhmi.edu<br />
Background: Patient-centered communication strategies are associated with positive outcomes, including patient<br />
satisfaction.<br />
Aim: We sought to understand whether such behaviors are practiced by residents.<br />
Methods: Cross-sectional study design using direct observation of twenty-nine first-year medicine residents at two<br />
internal medicine programs who were observed during clinical encounters over one month of patient care. We<br />
evaluated how often four key “etiquette-based” communication strategies are practiced: introducing one’s self;<br />
introducing one’s role in the patient’s care; touching the patient; and sitting down with the patient.<br />
Results: A total of 732 patient encounters were observed during 118 intern shifts. Overall, interns introduced<br />
themselves 40% of the time and their role 36% of the time. Interns sat down with patients during 9% of visits, and<br />
touched patients on 64% of visits. All four behaviors were per<strong>for</strong>med during 5% of encounters. Ten percent of the<br />
interns almost always practiced the behaviors, averaging three or more behaviors per encounter, while 14%<br />
averaged less than one.<br />
Discussion or Conclusion: Resident physicians introduced themselves to patients, explained their role, and sat<br />
down with patients infrequently during observed inpatient encounters. Interns touched patients during a majority of<br />
visits, but rarely per<strong>for</strong>med all four behaviors in the same encounter. There was a high degree of variability among<br />
interns in per<strong>for</strong>mance of these behaviors. These behaviors, termed “etiquette-based medicine,” are easy to per<strong>for</strong>m<br />
yet are not widely practiced. Since trainee behaviors may persist when they enter independent practice,<br />
interventions to facilitate etiquette-based communication during residency are warranted.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 6
Background<br />
In the Wake of the 2003 and 2011 Duty Hours Regulations,<br />
How Do Internal Medicine Interns Spend Their Time?<br />
Lauren Block MD, Kevin Wang, Timothy Niessen MD, Sanjay Desai MD, Albert Wu MD, Robert Habicht MD, Leonard Feldman MD<br />
Johns Hopkins University and University of Maryland Medical Center, Baltimore MD<br />
Results<br />
Conclusions<br />
• New ACGME requirements highlight importance of interaction with patients:<br />
• “For the resident, the essential learning activity is interaction with patients under the<br />
guidance and supervision of faculty members who give value, context, and meaning to<br />
those interactions”<br />
• New work hour rules may reduce time spent with patients<br />
• Efficiency may be prioritized over quality care<br />
• More frequent handoffs could increase medical errors<br />
• Health system changes may improve efficiency and safety but require more “screen” time<br />
• Expansion of electronic medical records and allied health professional teams may ease<br />
some resident clinical burden<br />
• Shorter hospital shifts could mean increased wakefulness and efficiency<br />
• Prior time motion studies in 1989 and 1997 found that residents spent more time charting<br />
than they do with patients; findings upheld in meta-analysis<br />
• Residents spent significant time engaging in basic activities: sleeping and eating<br />
Specific hypotheses<br />
• Relative to prior time motion studies, internal medicine residents will spend:<br />
• Less face-to-face time directly interacting with patients, and less time sleeping<br />
• More indirect patient care time: patient handoffs, accessing the medical record, and<br />
discussing patients with other physicians<br />
Methods<br />
Time spent by activity category<br />
63.6%<br />
9.3%<br />
12.3%<br />
• Nearly 2/3 of time spent in indirect patient care<br />
• Only 12.3% of time spent in direct patient care<br />
14.7%<br />
Comparison to historical studies<br />
Patient care<br />
Education<br />
Indirect pt care<br />
Misc<br />
Study Shift Direct pt care Indirect pt care Education Basic<br />
schedule<br />
Lurie, 1989 Night 22-31% 20-34% n/a 34-46%<br />
Lurie, 1993 Day/night 27-39% 20-42% n/a 11-40%<br />
Moore, 2000 Night 14% 43% n/a 42%<br />
Current study Day/night 12% 64% 15% 9%<br />
Percent of time spent in each activity by institution<br />
Total JH UMD<br />
Total time (hours) 873 439 (50.3%) 434 (49.7%)<br />
Activity<br />
Direct patient care 12.3% 11.4% 13.3%*<br />
Initial patient evaluation 3.8% 3.6% 4.1%<br />
Follow-up patient visit 7.2% 6.5% 7.8%*+<br />
Patient education 0.1% 0.1% 0.1%<br />
Family meeting 0.5% 0.4% 0.6%<br />
Procedures 0.7% 0.8% 0.6%<br />
Procedure consent 0.04% 0.05% 0.03%<br />
Education 14.7% 18.8% 10.6%*<br />
Educational conferences 2.3% 2.8% 1.8%<br />
Reading about medicine 2.1% 2.8% 1.3%*+<br />
Rounds 9.7% 12.2% 7.3%*+<br />
Teaching students 0.6% 1% 0.3%<br />
Indirect patient care 63.6% 61.2% 66.1%*<br />
Reviewing patient chart 14.5% 14.7% 14.3%<br />
Writing notes 16.1% 13.1% 19.1%<br />
Talking with providers 20% 20.5% 19.5%<br />
Paperwork 3.8% 1.5% 6.1%*+<br />
Writing orders 6.4% 7.3% 5.4%<br />
Handoffs 2.9% 4% 1.7%*+<br />
Transport
<strong>Poster</strong> Number: 7<br />
<strong>Poster</strong> Title: In the Wake of the 2003 and 2011 Duty Hours Rules, How Do Internal Medicine Interns Spend Their<br />
Time?<br />
Authors and Affiliate Institutions: Leonard Feldman, Lauren Block, Albert W Wu, Sanjay V Desai, Timothy<br />
Niessen, Kevin Wang, Johns Hopkins University School of Medicine; Robert Habicht, Kathryn Novello Silva,<br />
Nora Oliver, University of Maryland School of Medicine<br />
Submitting Author<br />
Leonard S. Feldman, MD<br />
Assistant Professor<br />
Division of General Internal Medicine<br />
Department of Internal Medicine and Pediatrics<br />
Johns Hopkins University School of Medicine<br />
600 North Wolfe Street<br />
Nelson 215<br />
Baltimore, MD 21287<br />
Telephone: (443) 287-3135<br />
Email: LF@jhmi.edu<br />
Background: The 2003 and 2011 ACGME common program requirements compress busy inpatient schedules and<br />
increase intern supervision at the same time that residents wrestle with the effects of electronic medical record<br />
systems, including documentation needs and availability of an ever-increasing amount of stored patient data.<br />
Aim: In light of this environment, we conducted a time motion study to determine how internal medicine residents<br />
spend their time in the hospital.<br />
Methods: Descriptive, observational study on inpatient ward rotations at two internal medicine residency programs<br />
at large academic medical centers in Baltimore, MD during January, 2012. Twenty-nine interns from the two<br />
residency programs participated. The primary outcome was percent of time spent in direct patient care (talking with<br />
and examining patients). Secondary outcomes included percent of time spent in indirect patient care, education, and<br />
miscellaneous activities (eating, sleeping, and walking). Results were analyzed using multilevel regression analysis<br />
adjusted <strong>for</strong> clustering at the observer and intern levels.<br />
Results: Interns were observed <strong>for</strong> a total of 439 hours at Site 1 and 434 hours at Site 2. Interns spent 12% of their<br />
time in direct patient care, 64% in indirect patient care, 15% in educational activities, and 9% in miscellaneous<br />
activities. Computer utilization occupied 40% of their time. There was no significant difference in time spent in<br />
these activities between the two sites.<br />
Discussion or Conclusion: Interns today spend a minority of their work time in direct contact with patients.<br />
Compared with interns in time motion studies prior to 2003, interns in our study spent less time in direct patient<br />
care and sleeping, and proportionally more time talking with other providers and documenting. Reduced work<br />
hours in the setting of increasing complexity of medical inpatients, growing volume of patient data, and increased<br />
supervision may limit the amount of time interns spend with patients.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 7
<strong>Poster</strong> Number: 8<br />
<strong>Poster</strong> Title: Do Teaching Styles Matter in Internal Medicine Residency Training?<br />
Authors and Affiliate Institutions: Phuong Ho, Burton Lee, Sailaja Pindiprolu, Washington Hospital Center<br />
Submitting Author<br />
Phuong D. Ho, MD<br />
Fellow<br />
Division of Pulmonary and Critical Care<br />
Department of Medicine<br />
MedStar Washington Hospital Center<br />
110 Irving Street, NW<br />
Washington, DC 20010<br />
Telephone: (202) 877-7856<br />
Email: phuong.d.ho@medstar.net<br />
Background: Deslauriers et al. demonstrated that a model that included pre-class reading assignments and quizzes,<br />
small group active learning, and targeted in-class instruction and feedback increased learning1. This has been the<br />
teaching model in our MICU <strong>for</strong> the past 10 years. The same attendings also taught on the pulmonary elective<br />
using traditional daily rounds with bedside teaching and ad hoc talks. This is supplemented by traditional didactic<br />
noon conferences.<br />
Aim: To assess whether these different styles affected In-Training Exam (ITE) scores.<br />
Methods: Retrospective review of 1st and 3rd year ITE results <strong>for</strong> the past five years. We collected each<br />
resident’s % of overall questions and combined pulmonary/critical care (PCC) questions answered correctly. Using<br />
the objectives, we divided the PCC questions into pulmonary and critical care, and determined the % correct <strong>for</strong><br />
each. We reviewed their schedules to determine whether they had MICU and pulmonary rotations. We compared<br />
the % of questions answered correctly (overall, PCC, pulmonary only, and critical care only) with their exposure to<br />
the MICU and pulmonary electives.<br />
Results: A total of 95 residents (190 ITE score reports) were included. While all residents had at least 2 MICU<br />
rotations, only 43% had a pulmonary rotation by their 3rd year ITE. Overall ITE, PCC, pulmonary only and<br />
critical care only scores all significantly improved from year 1 to year 3. There was a greater improvement in<br />
critical care only scores vs. pulmonary only scores (17.0% vs. 8.3%, p= 0.004) and this difference was statistically<br />
significant. In addition, the improvement in critical care only scores was greater than the improvement in the<br />
overall scores (17.0% vs. 9.2%, p=0.001). There was no difference in 3rd year ITE overall, PCC, pulmonary<br />
only or critical care only scores between residents who had and did not have a pulmonary elective. In addition,<br />
having a pulmonary rotation also made no difference on rates of improvement on ITE overall, PCC, pulmonary<br />
only or critical care only questions between the 1st year and 3rd year ITEs.<br />
Discussion or Conclusion: These results suggest that pre-assigned reading, small group interactive problem<br />
solving and direct feedback is more effective than rounds and conferences. We hope to change the educational<br />
structure on pulmonary to emulate the MICU model.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 8
Resident Advising: A Three-Year Follow-Up<br />
Tresa M McNeal, MD 1,2 , Austin Metting, MD 1,2 , Maybelline Lezama, MD 1,2 , Curtis Mirkes, DO 1,2<br />
1<br />
Texas A&M Health Science Center College of Medicine, 2 Scott & White Healthcare, Temple, Texas<br />
Introduction<br />
A resident advising program can serve a useful purpose in providing<br />
guidance to residents on many potential topics. The July 2009<br />
ACGME guidelines charged internal medicine residencies with the<br />
“development of an effective resident advising program.” (II.A.4.t.)<br />
Residencies throughout the U.S. have instituted advising programs<br />
within different frameworks at their institutions.<br />
Background<br />
The Scott & White Healthcare/Texas A&M Health Science Center<br />
(S&W/TAMHSC) Internal Medicine Residency pairs incoming<br />
interns with faculty advisors in the intern’s area of interest. The<br />
resident advising requirement has now been in effect <strong>for</strong> 3 years so<br />
we surveyed internal medicine residents and recent graduates at<br />
S&W/TAMHSA to determine the effects of the program.<br />
Suggestions <strong>for</strong> dealing with<br />
stressors<br />
Work‐life balance<br />
Subspecialty/job application<br />
Scholarly activity<br />
What to look <strong>for</strong> in a practice<br />
Topics Discussed with<br />
Advisors<br />
2012 all respondents<br />
2012 PGY4<br />
2012 PGY3<br />
2012 PGY2<br />
Results<br />
26 of 32 (91%) total surveys were returned<br />
• 10 PGY-2 (63%)<br />
• 10 PGY-3 (63%)<br />
• 6 PGY-4 (43%)<br />
There were 13 male and 13 female responses.<br />
92% were com<strong>for</strong>table contacting their advisor with concerns.<br />
42% shared interests with their advisor outside of medicine.<br />
88% stated that most communication with their advisor was in person.<br />
Most commonly discussed topics were (multiple responses were allowed):<br />
• Subspecialty or job application (58%)<br />
• Work-life balance (50%)<br />
• What to look <strong>for</strong> in a practice (50%)<br />
• Scholarly activity (50%)<br />
15% of all respondents felt that that their interaction with their advisor was not<br />
adequate.<br />
Of the recent graduates who responded, 50% reported that they<br />
changed their career direction based on interactions with their<br />
advisor.<br />
Methods<br />
A 12-question, multiple choice response and free text survey was sent<br />
to 32 PGY-2 and PGY-3 residents and 14 PGY-4 recent graduates at<br />
the TAM/HSC Internal Medicine Residency Program in October<br />
2012 with a goal of program evaluation and improvement. Questions<br />
centered on discovering resident perceptions regarding the advising<br />
program in terms of the usefulness of these interactions as well as<br />
suggestions <strong>for</strong> improvement. Results were collected and analyzed<br />
<strong>for</strong> any trends in responses.<br />
Board preparation<br />
0 10 20 30 40 50 60 70<br />
Percent of Residents Indicating Each Topic Discussed with<br />
their Advisor (multiple responses allowed)<br />
Conclusion<br />
Based on results from this small number of respondents, the resident advising<br />
program is serving a useful purpose in guiding residents through career<br />
development. Future directions may include a multi-institutional survey regarding<br />
resident advising programs.
<strong>Poster</strong> Number: 9<br />
<strong>Poster</strong> Title: Resident Advising: A Three-Year Follow-Up<br />
Authors and Affiliate Institutions: Tresa M McNeal, Maybelline Lezama, Austin Metting, Curtis R Mirkes,<br />
Texas A&M University College of Medicine<br />
Submitting Author<br />
Tresa M. McNeal, MD<br />
Assistant Professor, Associate Program Director<br />
Division of Inpatient Medicine<br />
Department of Internal Medicine<br />
Texas A&M University College of Medicine<br />
2401 South 31st Street<br />
Temple, TX 76508<br />
Telephone: (254) 724-8797<br />
Email: tmcneal@sw.org<br />
Background: A resident advising program can serve a useful purpose in providing guidance to residents on many<br />
potential topics. The July 2009 ACGME guidelines charged internal medicine residencies with the “development of<br />
an effective resident advising program.” (II.A.4.t.) Residencies throughout the U.S. have instituted advising<br />
programs within different frameworks at their institutions. The Scott & White Healthcare/Texas A&M Health<br />
Science Center (S&W/TAMHSC) Internal Medicine Residency matches incoming interns with faculty advisors in<br />
the intern’s area of interest.<br />
Aim: The resident advising requirement has now been in effect <strong>for</strong> 3 years so we surveyed internal medicine<br />
residents and recent graduates at S&W/TAMHSC to determine the effects of the program.<br />
Methods: A 12-question, multiple choice response and free text survey was sent to 32 PGY-2 and PGY-3 residents<br />
and 14 PGY-4 recent graduates at the S&W/TAMHSC internal medicine residency program in October 2012 with a<br />
goal of program evaluation and improvement. Questions centered on discovering resident perceptions regarding<br />
the advising programs in terms of the usefulness of these interactions as well as suggestions <strong>for</strong> improvement.<br />
Results were collected and analyzed <strong>for</strong> any trends in responses.<br />
Results: A total of 26 surveys were returned, 10 each of PGY-2 and 3 responses and 6 PGY-4 responses. There<br />
were an equal number of responses from male and female residents and recent graduates. Overall, only 15% felt<br />
that the interaction with their advisor was not adequate to meet their career development needs. Ninety-two percent<br />
would feel com<strong>for</strong>table contacting their advisor with a concern. Interestingly, 42% of respondents reported not only<br />
having similar interests as their advisor within medicine but also outside of medicine. The topic most commonly<br />
discussed with advisors was subspecialty or job application with 58% of respondents indicating this. The majority<br />
(88%) indicated that they typically communicated in person although 27% also communicate with text messaging.<br />
Of the recent graduates who responded, 50% reported that they changed their career direction based on interactions<br />
with their advisor.<br />
Discussion or Conclusion: Based on results from this small number of respondents, the resident advising program<br />
is serving a useful purpose in guiding residents through career development. Future directions may include a multiinstitutional<br />
survey regarding resident advising programs.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 9
<strong>Poster</strong> Number: 10<br />
<strong>Poster</strong> Title: An Ambulatory Clinic Intervention to Improve Resident Physician Confidence with the Advance<br />
Care Planning Process<br />
Authors and Affiliate Institutions: Ericka Tung, Jason Post, Mark Wieland, John Bundrick, Thomas Jaeger,<br />
Karen Mauck, Matthew Thomas, Kris Thomas, Mayo Clinic Rochester; Brandon Verdoorn, University of Colorado<br />
School of Medicine<br />
Submitting Author<br />
Jason A. Post, MD<br />
Instructor<br />
Department of Medicine<br />
Mayo Clinic Rochester<br />
200 First Street, SW<br />
Rochester, MN 55905<br />
Telephone: (507) 284-2511<br />
Email: post.jason@mayo.edu<br />
Background: Primary care providers play a key role in advance care planning (ACP), yet studies indicate many<br />
providers lack ACP training and feel uncom<strong>for</strong>table discussing end of life care.<br />
Aim: To assess internal medicine (IM) residents’ ACP practices and improve resident confidence with ACP<br />
utilizing a multifaceted educational intervention.<br />
Methods: During one continuity clinic session in January 2012, residents participated in a quality review of ACP,<br />
including small group discussion, guided self-reflection, didactic teaching, and ACP chart audit on their patients<br />
aged ≥65. Patient and provider variables were collected to explore associations between these measures and<br />
documentation of ACP. A pre- and post-intervention survey assessed resident confidence with ACP activities.<br />
Descriptive statistics were generated <strong>for</strong> survey results and chart audits. Fisher’s exact test was utilized to compare<br />
pre and post-intervention survey results. Multivariate logistic regression models were used to determine<br />
associations between ACP completion and patient and provider variables. This study was deemed exempt by Mayo<br />
Clinic’s IRB.<br />
Results: Of 144 categorical IM residents, 106 (74%) participated in the sessions, of which 92% completed pre-post<br />
surveys and guided chart audit (873 charts reviewed, mean 8.6 charts per resident). Only 24% of audited patients<br />
had an advance directive (AD) on file; 11% had ACP documentation at the last comprehensive examination; and<br />
28% of ACP documentation was reported of “no clinical utility.” Senior residents were less likely to document<br />
ACP (OR 0.21, p
<strong>Poster</strong> Number: 11<br />
<strong>Poster</strong> Title: Generalist Career Outcomes of University of Cali<strong>for</strong>nia Davis Graduates: A Longitudinal Study<br />
Authors and Affiliate Institutions: Ruby Shah, Anthony Bhe, Tonya Fancher, University of Cali<strong>for</strong>nia Davis,<br />
School of Medicine<br />
Submitting Author<br />
Ruby P. Shah, MD<br />
Primary Care Outcomes Research Fellow<br />
Department of Internal Medicine<br />
University of Cali<strong>for</strong>nia, Davis, School of Medicine<br />
4150 V Street, Suite 2400<br />
Sacramento, CA 95817<br />
Telephone: (916) 734-5290<br />
Email: ruby.shah@ucdmc.ucdavis.edu<br />
Background: The number of medical school graduates choosing primary care internal medicine (IM) has<br />
plummeted since 1985. UC Davis School of Medicine (UCDSOM) was founded in 1966 with an overarching goal<br />
of “maintaining one of the best generalist physician training programs in the country. However, little is known<br />
about graduates’ career outcomes.<br />
Aim: 1) To examine the number of UCDSOM graduates practicing in primary care careers or medically<br />
underserved areas post-residency; and 2) to determine if educational experiences at UCDSOM are associated with<br />
graduates entering these careers.<br />
Methods: We conducted a longitudinal cohort study of all UCDSOM graduates from 2004-2008 (N=454) and<br />
determined their post-residency practice specialty and practice setting. Using logistic regression, we examined the<br />
association between post-residency career setting or specialty adjusting <strong>for</strong> research experience during medical<br />
school, student run clinic participation, gender, race, ability to speak more than one language, total dollar debt at<br />
graduation, , and per<strong>for</strong>mance on the MCAT, USMLE 1 and 2.<br />
Results: We found that post-residency 27.9% of UCDSOM graduates were practicing primary care and 37.2%<br />
were in medically underserved areas; 6.6% were in primary care IM and 12% were practicing IM sub-specialties.<br />
We found that graduates who participated in a student-run clinic (OR 2.15, 95% CI 1.16-3.99) and women<br />
graduates (OR 1.83, 95% CI 1.09-3.07) were more likely to be in primary care careers post-residency. Graduates<br />
who participated in research experiences during medical school were less likely to be in primary care careers (OR<br />
0.52, 95% CI 0.32-0.86). There was no significant association between debt at graduation and eventual practice in<br />
primary care or medically underserved areas. Graduates who speak more than one language were more likely to<br />
practice in medically underserved areas (OR 1.91, 95% CI 1.14-3.23). Student race, per<strong>for</strong>mance on the MCAT or<br />
USMLE, research activity or participation in student run clinics during medical school were not associated with<br />
post-residency practice in medically underserved areas.<br />
Discussion or Conclusion: Many students participate in UCDSOM student run clinics and go on to practice<br />
primary care. Gender, ability to speak more than one language, and research experience are also associated with<br />
career outcomes which is consistent with prior studies. Program directors seeking to identify applicants who are<br />
likely to enter primary care or medically underserved areas may choose to focus on these characteristics.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 11
Flight Risk: Predictors of Contemplating Resignation Among Internal Medicine Program Directors<br />
Sara L. Swenson, MD † , Richard Shaw, PhD † , Vineet M. Arora, MD ‡ , Andrew J. Halvorsen, MS € , Michael Adams, MD*, Kevin T. Hinchey, MD**, Sandhya Wahi‐Gururaj, MD***, Furman S. McDonald, MD, MPH € <strong>APDIM</strong> Survey Committee<br />
† Cali<strong>for</strong>nia Pacific Medical Center,<br />
‡ University of Chicago Pritzker School of Medicine, *Georgetown University School of Medicine, **Baystate Medical Center, ***University of Nevada School of Medicine,<br />
€ Mayo Clinic College of Medicine<br />
Introduction<br />
National internal medicine program directors exhibit high<br />
job turnover with almost 40% of program directors<br />
reporting three or fewer years in the job in 2010. Fiscal<br />
constraints and regulatory requirements may heighten<br />
pressures on program directors. We hypothesized that<br />
program directors’ perceptions of support by key<br />
institutional leaders might play an important role in job<br />
sustainability.<br />
Discussion<br />
• large national sample<br />
Strengths<br />
Limitations<br />
• unknown predictive value of primary outcome variable<br />
• institutional support questions not previously validated<br />
Methods<br />
National survey of 365 internal medicine program directors<br />
in August‐November of 2011<br />
• Response rate 72% (261/365 IM programs surveyed)<br />
Implications<br />
• increasing residency program budget transparency and institutional<br />
support by key leaders may help to mitigate high turnover among internal<br />
medicine program directors<br />
• GME organizations, such as <strong>APDIM</strong>, should consider ways to support<br />
program directors at high flight risk<br />
• Sample size <strong>for</strong> this data analysis: 244<br />
Primary outcome variable: “In the past year, have you<br />
considered resigning as program director?”<br />
Independent variables:<br />
Program director characteristics (age, sex, length of tenure,<br />
salary, time since training, percent protected time)<br />
Program characteristics (community vs. university, cycle<br />
length<br />
Perceptions of key leaders, institutional support, budgetary<br />
control<br />
Perspectives on 2011 duty hours requirements<br />
Duty hours and institutional support assessed using 5‐point Likert<br />
scale items<br />
Statistical analyses:<br />
Bivariate: Kendall’s b‐tau<br />
Multivariable logistic regression model included statistically<br />
significant (P
<strong>Poster</strong> Number: 12<br />
<strong>Poster</strong> Title: Thinking of Quitting: Predictors of Considering Resignation Among Internal Medicine Program<br />
Directors<br />
Authors and Affiliate Institutions: Sara L Swenson, Richard Shaw, Cali<strong>for</strong>nia Pacific Medical Center; Michael<br />
Adams, Georgetown University School of Medicine; Sandhya Wahi-Gururaj, University of Nevada School of<br />
Medicine (Las Vegas); Kevin Hinchey, Baystate Medical Center; Vineet Arora, University of Chicago Pritzker<br />
School of Medicine; Furman McDonald, Mayo Clinic College of Medicine<br />
Submitting Author<br />
Sara L. Swenson, MD<br />
Interim Program Director<br />
Department of Medicine<br />
Cali<strong>for</strong>nia Pacific Medical Center<br />
2351 Clay Street, Third Floor<br />
San Francisco, CA 94115<br />
Telephone: (415) 600-2767<br />
Email: swensosl@sutterhealth.org<br />
Background: Turnover among internal medicine program directors is high. Fiscal constraints and regulatory<br />
requirements may heighten pressures on program directors. We hypothesized that program directors’ perceptions of<br />
support by key institutional leaders may have an impact on job sustainability.<br />
Aim: Our study investigated how many internal medicine program directors had considered resigning from their<br />
jobs in the past year and the predictors of contemplating resigning.<br />
Methods: Using the 2011 annual <strong>APDIM</strong> survey, we asked internal medicine program directors: “in the past year,<br />
have you considered resigning as program director?” We investigated univariate and multivariable predictors of<br />
intent to resign, including program and program director characteristics and perceptions of institutional support.<br />
Institutional support items used 5-point Likert scales to assess perceptions of program director control of their<br />
budget, key institutional leaders’ valuation of service versus education, disagreements with key leaders, and support<br />
<strong>for</strong> 2011 duty hours requirements. For univariate analyses, we employed Kendall’s b-tau and ANOVA <strong>for</strong><br />
categorical and linear variables, respectively. We evaluated multivariable predictors via logistic regression.<br />
Results: Forty-six percent of respondents considered resigning as program director in 2011-12. Univariate analysis<br />
demonstrated associations between intent to resign and program director sex (female 61%, male 39%), support of<br />
duty hours regulations, and perceptions of institutional support. On multivariable analysis, independent predictors<br />
of contemplating resigning were female sex (AOR 2.37; 95% CI 1.03, 5.43), lack of philosophical support <strong>for</strong> duty<br />
hours changes (4.80; 1.36, 16.90), the perception that disagreements with key hospital leaders had a negative<br />
impact on job satisfaction (2.88; 1.09, 7.60), and lack of transparency regarding residency-related funding (0.34;<br />
0.14, 0.87). Hospital administrators were more likely to prioritize service over education (56% vs. 9%) than were<br />
department chairs (40% vs. 12%) (p
The Educational Innovations Project (EIP) - Association between Residency<br />
Program Participation and Medical Education Publications<br />
Kris G Thomas 1 , Andrew J Halvorsen 1 , Colin P West 1 , Eric J Warm 2 , Jerry Vasilias 3 , Eileen E Reynolds 4 , John G.Frohna 5 , Furman S McDonald 1<br />
1 Mayo Clinic, 2 University of Cincinnati, 3 Accreditation Council <strong>for</strong> Graduate Medical Education, 4 Beth Israel Deaconess Medical Center, 5 University of Wisconsin<br />
<br />
<br />
<br />
Background<br />
The Educational Innovations Project (EIP) is an<br />
Accreditation Council <strong>for</strong> Graduate Medical<br />
Education (ACGME) initiative meant to spur<br />
innovation and dissemination of outcomes<br />
among participating IM residency programs. 1<br />
Since its inception in 2006, a collaborative<br />
community has been established among EIP<br />
programs that may facilitate innovation and<br />
scholarship.<br />
A number of presentations and publications<br />
have been disseminated from EIP<br />
programs 2,3,4,5 though it is unclear whether<br />
education scholarship productivity of EIP<br />
programs differs from similar non-participating<br />
programs.<br />
Study Objectives<br />
• To determine if the number of education<br />
publications generated from EIP programs<br />
differs from that of similar non-EIP programs.<br />
• To compare the proportion of EIP-participating<br />
and EIP-eligible programs with at least one<br />
publication.<br />
• To determine if the impact factor of journals<br />
publishing education scholarship generated<br />
from EIP programs differs from that of similar<br />
non-EIP programs<br />
Methods<br />
Design:<br />
•Controlled cohort study comparing internal medicine GME<br />
publications from EIP-participating (n=21) and EIP-eligible (n=80)<br />
programs, using program director (PD) authorship as a surrogate<br />
marker.<br />
•During the study period, 3 programs stopped participating in EIP<br />
and 5 eligible programs withdrew accreditation, leaving 18<br />
participating and 75 eligible programs (37 and 129 PDs,<br />
respectively) <strong>for</strong> inclusion.<br />
Search Strategy:<br />
•The medical literature was searched using Pub Med via a search<br />
strategy linking all PD names from EIP-participating and EIP-eligible<br />
programs as authors AND (internal medicine[mesh] OR "graduate<br />
medical education" OR education, medical, graduate[mesh] OR<br />
internship and residency[mesh]), limited to publication dates 2002-<br />
2011.<br />
•The literature search returned 300 publications, of which 3 were<br />
excluded due to mismatched author initials, leaving 297 matched<br />
publications, 239 (80.5%) of which were authored by the PD during<br />
a year of their tenure at a program (Figure 1).<br />
Figure 1: GME publications returned by<br />
the literature search<br />
28<br />
Participating<br />
(1.6/program)<br />
84<br />
PRE-initiative<br />
(2002-2006)<br />
300 articles returned by<br />
literature search<br />
(166 PD names)<br />
61 excluded<br />
3 author initial mismatch<br />
58 outside PD years of<br />
tenure<br />
239 articles<br />
authored during<br />
PD tenures<br />
56<br />
Eligible<br />
(0.8/program)<br />
76<br />
Participating<br />
(4.2/program)<br />
155<br />
POST-initiative<br />
(2007-2011)<br />
79<br />
Eligible<br />
(1.1/program)<br />
Demographic Characteristics of EIP-<br />
Participating and EIP-Eligible Programs<br />
Number of<br />
Program<br />
Directors, Mean<br />
(SD)<br />
Years of PD<br />
Tenure, Mean (SD)<br />
% ABIM Pass<br />
Rate, Mean (SD)<br />
Approved<br />
Residency<br />
Positions, Mean<br />
(SD)<br />
EIP-Participating<br />
Programs (N=18)<br />
EIP-Eligible<br />
Programs (N=75)<br />
References<br />
P Value<br />
2.1 (0.9) 1.7 (0.8) 0.19<br />
11.0 (5.1) 11.3 (6.1) 0.86<br />
91.2 (6.7) 89.6 (7.3) 0.40<br />
101.4 (49.0) 69.5 (35.3) 0.02<br />
Region 0.17<br />
Midwest 10 (55.6%) 24 (32.0%)<br />
Northeast 4 (22.2%) 31 (41.3%)<br />
South 1 (5.6%) 12 (16.0%)<br />
West 3 (16.7%) 8 (10.7%)<br />
Type Program 0.32<br />
Community-based 0 (0.0%) 6 (8.0%)<br />
Community-based, 7 (38.9%) 40 (53.3%)<br />
University-affiliated<br />
Military 0 (0.0%) 1 (1.3%)<br />
University-based 11 (61.1%) 28 (37.3%)<br />
No government 15 (83.3%) 56 (74.7%) 0.80<br />
affiliation<br />
1. Mladenovic J, Bush R, Frohna J. Am J Med. 2009;122(4):398-404.<br />
2. Warm EJ, Schauer DP, Diers T, et al. Journal of General Internal Medicine.<br />
2008;23(7):921-6.<br />
3. Mathis BR, Warm EJ, Schauer DP, et al. Journal of General Internal Medicine.<br />
2011;26(11):1253-7.<br />
4. McCoy CP, Halvorsen AJ, Loftus CG, et al. Mayo Clin Proc. 2011;86(3):192-6.<br />
5. Tess AV, Yang JJ, Smith CC, et al. Academic Medicine. 2009;84(3):326-34.<br />
6. Nasca TJ, Philibert I, Brigham T, Flynn TC. NEJM 2012.<br />
Results: Publications from EIP and Eligible<br />
Programs and Their Program Directors (PD)<br />
Pre-EIP (2002-2006)<br />
EIP-<br />
Participating<br />
Programs<br />
(N=18)<br />
EIP-<br />
Eligible<br />
Programs<br />
(N=75)<br />
P Value<br />
Prevalence of Publication<br />
N (%) Publishing 10 (55.6%) 25 (33.3%)<br />
OR of Publication 2.5 - 0.09<br />
Number of Publications<br />
Maximum Per Program 18 8<br />
Maximum Per PD 12 8<br />
Median (IQR) Per Program 1 (0-2) 0 (0-1) 0.13<br />
Median (IQR) Per PD 0 (0-1) 0 (0-0) 0.25<br />
2011 Impact Factor, Mean (SD) 5.9 (6.5) 4.8 (6.4) 0.48<br />
Post-EIP (2007-2011)<br />
Prevalence of Publication<br />
N (%) Publishing 15 (83.3%) 25 (33.3%)<br />
OR of Publication* 10.0 - 0.0007<br />
Number of Publications<br />
Maximum Per Program 34 23<br />
Maximum Per PD 29 23<br />
Median (IQR) Per Program 2 (1-4) 0 (0-1)
<strong>Poster</strong> Number: 13<br />
<strong>Poster</strong> Title: The Educational Innovations Project (EIP)—Association Between Residency Program Participation<br />
and Medical Education Publications<br />
Authors and Affiliate Institutions: Kris Thomas, Andrew Halvorsen, Colin West, Furman McDonald, Mayo<br />
Clinic College of Medicine; Eric Warm, University of Cincinnati College of Medicine; Jerry Vasilias,<br />
Accreditation Council <strong>for</strong> Graduate Medical Education; Eileen Reynolds, Harvard Medical School Beth Israel<br />
Deaconess Medical Center; John Frohna, University of Wisconsin School of Medicine<br />
Submitting Author<br />
Kris G. Thomas, MD<br />
Associate Program Director<br />
Division of Primary Care Internal Medicine<br />
Department of Internal Medicine<br />
Mayo Clinic College of Medicine<br />
200 First Street, SW<br />
Rochester, MN 55905<br />
Telephone: (507) 284-2511<br />
Email: thomas.kris@mayo.edu<br />
Background: The Educational Innovations Project (EIP) is an Accreditation Council <strong>for</strong> Graduate Medical<br />
Education (ACGME) initiative launched July 1, 2006 to spur innovation and dissemination of outcomes among<br />
internal medicine residency programs.<br />
Aim: To determine if the number of education publications generated from EIP- programs differs from similar<br />
EIP-eligible programs.<br />
Methods: We compared internal medicine GME publications from EIP-participating and EIP-eligible programs,<br />
using program director (PD) authorship as a surrogate marker. PDs from EIP-participating and EIP-eligible<br />
programs were identified using publically available data. PubMed was searched via a strategy linking PD names as<br />
authors with residency education related publications, limited to publication dates 2002-2011. The mean number of<br />
publications, median number of publications, and proportion with at least 1 publication (<strong>for</strong> both programs and<br />
PDs) were assessed across two 5-year time periods, pre-EIP (2002-06) and post-EIP (2007-11).<br />
Results: Twenty-one EIP-participating and 80 EIP-eligible programs were identified. During the study period, 3<br />
programs stopped participating in EIP and 5 eligible programs withdrew accreditation, so 18 participating and 75<br />
eligible programs (38 and 136 PDs, respectively) were included. The literature search returned 302 publications, of<br />
which 3 were excluded due to mismatched author initials, leaving 299 publications <strong>for</strong> analysis. During the pre-<br />
EIP, there were 38 publications by participating programs and 68 by eligible (Mean 2.2 vs. 0.9 publications per<br />
program, p=.22, Mean 1.2 vs. 0.5 publications per program director, p=.11). During the post-EIP, there were 94<br />
publications by participating programs and 99 by eligible (Mean 5.4 vs. 1.3 publications per program, p=.07, Mean<br />
3.0 vs. 0.8 publications per program director, p=.02). A significant increase in publications was seen among EIPparticipating<br />
programs relative to eligible (Mean change of +3.4 publications per program, p=.01, Mean change of<br />
+1.8 publications per PD, p=.02), while publications from eligible programs remained unchanged (Mean +0.4<br />
publications per program, p=.20, Mean +0.2 per PD, p=.17). Analysis by medians and proportion with at least 1<br />
publication (per program and per PD) were similar.<br />
Discussion or Conclusion: These data support plans by GME leaders to replicate and generalize successful<br />
elements of EIP in support of innovation and scholarly dissemination throughout residency programs nationally.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 13
<strong>Poster</strong> Number: 14<br />
<strong>Poster</strong> Title: Duty Hours Monitoring Revisited: Self-Report May Not Be Adequate<br />
Authors and Affiliate Institutions: Heather Thompson Buum, Alisa Duran-Nelson, L James Nixon, Jeremiah<br />
Menk, University of Minnesota Medical School<br />
Submitting Author<br />
Heather A. Thompson Buum, MD<br />
Associate Program Director<br />
Division of General Internal Medicine<br />
Department of Internal Medicine<br />
University of Minnesota Medical School<br />
MMC 284<br />
420 Delaware Street, SE<br />
Minneapolis, MN 55455<br />
Telephone: (612) 626-5868<br />
Email: thomp057@umn.edu<br />
Background: Monitoring compliance with duty hour regulations requires an accurate method of reporting. While<br />
self-report is a generally accepted practice, it has not been validated. Only three studies to date have been<br />
published evaluating the accuracy of self-report compared to another measure of resident activity. These studies<br />
concluded that self-report was accurate, but were limited by small numbers of residents and relatively brief study<br />
periods.<br />
Aim: We sought to verify the accuracy of daily self-reported duty hours data logged via an electronic reporting<br />
system, the Residency Management Suite (RMS), as well as validate RMS as a tool <strong>for</strong> tracking duty hours<br />
violations.<br />
Methods: Twenty-eight weeks of parking data and self-reported RMS data <strong>for</strong> 136 resident rotations were<br />
compared, spanning from December 12, 2011 to June 27, 2012. An intercept-only model with a random effect <strong>for</strong><br />
correlation within person was used to compare the hours parked per day versus self-report hours. The number of<br />
duty hour violations in the two sets of data was compared using McNemar’s test.<br />
Results: The daily mean self-report hours was 0.745 longer than the mean hours parked (95% CI: [0.538--0.953], p<br />
< 0.001), a difference likely accounted <strong>for</strong> by offsite continuity clinics. No significant difference was detected<br />
regarding the 80-hour violations in the two sets of data; however, a greater number of 8-hour and 16-hour violations<br />
were observed in the parking card data compared to self-report data (p
<strong>Poster</strong> Number: 15<br />
<strong>Poster</strong> Title: Patient Census: What is Optimal <strong>for</strong> Educational Satisfaction and Quality of Care Balance?<br />
Authors and Affiliate Institutions: Megan Ramsey, Laurel Fick, St. Vincent Hospital and Health Care Center<br />
Submitting Author<br />
Laurel Fick, MD<br />
Associate Program Director<br />
Division of Internal Medicine<br />
Department of Medical Education<br />
St. Vincent Hospital and Health Care Center<br />
2001 West 86th Street<br />
Three North, Medical Education<br />
Indianapolis, IN 46260<br />
Telephone: (317) 338-7622<br />
Email: lbfick@stvincent.org<br />
Background: To our knowledge there have been no previous studies correlating daily patient census with<br />
educational satisfaction and perceived patient care quality in the teaching hospital setting.<br />
Aim: The purpose of this study was to determine the teaching census that provides the best balance of quality<br />
patient care and educational satisfaction as perceived by teaching faculty and resident physicians.<br />
Methods: This IRB-approved study surveyed hospitalist faculty and Internal Medicine residents at our mediumsized<br />
community-based training program at a tertiary care hospital in the Midwest. The electronic survey tool<br />
asked each respondent to identify the daily team patient census at which the quality of patient care/education<br />
balance is optimal as well as the census at which this balance becomes suboptimal. It then asked the physicians to<br />
qualify how his or her overall work experience is affected by patient census and to state if they had ever had a poor<br />
patient outcome they attributed to being overextended from a high census.<br />
Results: Seventy-two percent of academic hospitalists and 64% of residents completed the survey. Among<br />
faculty, 95% responded that the census at which the patient care/educational balance is optimal is 12-15 <strong>for</strong> a team<br />
consisting of one resident and two interns. Sixty-seven percent of residents agreed that an optimal census is 12-15.<br />
For teams consisting of 1 resident or intern, 77% of faculty and 65% of residents felt that an optimal census was 12<br />
or less. In both surveys only 1 respondent felt that a census over 15 was optimal. Nearly one hundred percent of<br />
hospitalists and residents felt faculty teaching decreased, quality of care decreased, career satisfaction decreased<br />
when the census was high. Thirty-eight percent of faculty and 51% of residents attributed a poor patient outcome to<br />
being overextended from a high census.<br />
Discussion or Conclusion: This pilot study suggests that the current ACGME census caps may be higher than is<br />
optimal <strong>for</strong> balancing educational satisfaction and quality patient care. A team census cap of 15 patients (<strong>for</strong> one<br />
resident/two intern teams) may be more favorable <strong>for</strong> training programs of similar size and structure. Most<br />
concerning is the high percentage of physicians that felt a poor patient outcome was related to high census. It<br />
would be interesting to objectively study this perception in the future.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 15
Introduction<br />
The Triple Threat: Novel Hospitalist‐Track Electives<br />
Kapil Mehta MD, Teresa Hogue MD, Laurel Fick MD, FACP<br />
St. Vincent Hospital‐ Indianapolis<br />
Advanced Hospitalist Medicine<br />
Results<br />
Hospitalists are increasingly involved in hospital<br />
operations, administration, and practicing in distinctive<br />
areas of medicine. Given this trend, our Curriculum<br />
Committee created three new electives <strong>for</strong> our Internal<br />
Medicine Hospitalist Track to facilitate the development of<br />
diverse yet uniquely trained physicians.<br />
Administrative Medicine<br />
Two to four-week elective that offers senior residents<br />
exposure to the business and quality aspects of hospital<br />
leadership.<br />
Experiences include:<br />
• Hospital Operations: Quality Assurance,<br />
Regulatory Compliance, Business Development<br />
and Lean Methodology, Per<strong>for</strong>mance Metrics<br />
• Patient Safety: Medication Safety, Principles of a<br />
High Reliability Organization(HRO)<br />
• Principles of physician leadership<br />
• Legislative Medicine<br />
• Hospital <strong>Meeting</strong>s/Committee management<br />
Four- week elective that offers residents a “menu” of 1-2<br />
week sub-rotations based on their interest and perceived<br />
need <strong>for</strong> additional training.<br />
Current options <strong>for</strong> experiences include:<br />
•Pre-Operative Medicine<br />
• Observation Unit Medicine<br />
• Advanced Neurology<br />
• Inpatient Geriatrics<br />
• Orthopedic Hospitalist Medicine<br />
• Inpatient Billing and Coding<br />
In<strong>for</strong>matics<br />
Two to four-week elective with the Chief In<strong>for</strong>matics Officer<br />
and In<strong>for</strong>mation Technology (IT) team to participate in<br />
the development and implementation of the electronic<br />
health record and to learn how IT enables the effective<br />
collection of data to develop medical knowledge and to<br />
facilitate the delivery of patient care.<br />
“This rotation allowed me to get exposure to prepare <strong>for</strong><br />
being a hospitalist. I feel more com<strong>for</strong>table with<br />
billing/coding, and made the transition much smoother.<br />
Due to this rotation, I also developed interest in preoperative<br />
medicine and am currently doing pre-operative<br />
consultations/risk assessment.”<br />
To date one graduate who completed these electives has<br />
begun a hospitalist career involving both administrative<br />
medicine and in<strong>for</strong>matics .<br />
Conclusions<br />
These elective rotations are easy to implement and<br />
customizable based on the facilities, staffing, resident<br />
interest, and specialty options unique to each residency<br />
program and/or hospital. Future directions may include<br />
development of an Administrative Medicine Track.
Programmatic Innovation <strong>Poster</strong> Abstracts<br />
<strong>Poster</strong> Number: 16<br />
<strong>Poster</strong> Title: The Triple Threat—Novel Hospitalist-Track Electives<br />
Authors and Affiliate Institutions: Kapil Mehta, Teresa Hogue, Laurel Fick, St. Vincent Hospital and Health<br />
Care Center<br />
Submitting Author<br />
Laurel Fick, MD<br />
Associate Program Director<br />
Division of Internal Medicine<br />
Department of Medical Education<br />
St. Vincent Hospital and Health Care Center<br />
2001 West 86th Street<br />
Three North, Medical Education<br />
Indianapolis, IN 46260<br />
Telephone: (317) 338-7622<br />
Email: lbfick@stvincent.org<br />
Discussion of How the Problem was Identified and Explored: Hospitalists are increasingly involved in hospital<br />
operations, administration, and practicing in distinctive areas of medicine. Given this trend, in 2011 our Curriculum<br />
Committee created three new electives <strong>for</strong> our Internal Medicine Hospitalist Track to facilitate the development of<br />
diverse yet uniquely trained physicians.<br />
Description of the Innovation: Administrative Medicine- Two to four-week elective that offers senior residents<br />
exposure to the business and quality aspects of hospital leadership. Residents rotate with the Hospitalist Director<br />
and obtain experience in Hospital Operations, Patient and Medication Safety, Leadership, and Legislative<br />
Medicine. In<strong>for</strong>matics- Two to four-week elective with the Chief In<strong>for</strong>matics Officer and In<strong>for</strong>mation<br />
Technology (IT) team to participate in the development and implementation of the electronic health record and to<br />
learn how IT enables the effective collection of data to develop medical knowledge and to facilitate the delivery of<br />
patient care. Advanced Hospitalist Medicine (AHM)- Four- week elective that offers residents a “menu” of 1-2<br />
week sub-rotations based on their interest and perceived need <strong>for</strong> additional training. Current options <strong>for</strong><br />
experiences include: o Pre-Operative Medicine o Observation Medicine o Advanced Neurology o Inpatient<br />
Geriatrics o Orthopedic Hospitalist Medicine o Inpatient Billing and Coding.<br />
Results to Date: Post-rotation surveys were administered to all rotators with positive results. Administrative<br />
medicine (2 rotators to date) and In<strong>for</strong>matics (1 rotator to date) each had an average of 5 (on a 5 point Likert scale)<br />
when asked if this rotation was valuable <strong>for</strong> the resident’s medical education, 4 out of 5 when asked if the rotation<br />
was organized sufficiently. To date, one rotator <strong>for</strong> both of the above rotations has since completed residency has<br />
entered into a career including both administrative and in<strong>for</strong>matics responsibilities. AHM (10 rotators to date)-<br />
All sub-rotations achieved at least a 5 (on 1-6 Likert scale) when asked “The components of this rotation provided<br />
knowledge and experiences missing in other rotations of the required residency curriculum.”. There were no<br />
negative comments or scores <strong>for</strong> any sub-rotation or the rotation as a whole. Free text comments were extremely<br />
positive <strong>for</strong> all three novel rotations.<br />
Discussion/Reflection/Lessons Learned: Our program identified a need <strong>for</strong> advanced experiences in<br />
administrative medicine, in<strong>for</strong>matics, and hospitalist medicine and created three novel electives with very positive<br />
results to date. These elective rotations are easy to implement and customizable based on the facilities, staffing,<br />
resident interest, and specialty options unique to each residency program and/or hospital.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 16
<strong>Poster</strong> Number: 17<br />
<strong>Poster</strong> Title: Procedural Competence: From See One, Do One, Teach One to an Entrustable Professional Activity<br />
Authors and Affiliate Institutions: Alisa Duran-Nelson, Sophia P Gladding, L James Nixon, University of<br />
Minnesota Medical School<br />
Submitting Author<br />
Alisa Duran-Nelson, MD<br />
Assistant Professor<br />
Department of Medicine<br />
University of Minnesota Medical School<br />
420 Delaware Street, SE<br />
MMC 284<br />
Minneapolis, MN 55455<br />
Telephone: (612) 626-4603<br />
Email: duran012@umn.edu<br />
Discussion of How the Problem was Identified and Explored: The ACGME’s Outcome Project launched a<br />
transition from focusing on the processes to the outcomes of training. The ACGME competencies have been refined<br />
to program specific developmental milestones to be achieved by trainees during their training. Educational leaders<br />
have looked to Entrustable Professional Activities (EPAs) as a framework to tie these concepts together. We have<br />
been challenged with creating EPAs that support the development and assessment of our trainees in areas of<br />
essential clinical practice.<br />
Description of the Innovation: Our educational committee, composed of educators with expertise in competencybased<br />
education and assessment, developed a Procedural EPA. Using levels of entrustment described previously by<br />
Ten Cate (reference), we defined criteria <strong>for</strong> advancement to each level of entrustment. The criteria included:<br />
assessment environment (simulated vs. actual), assessment by procedural checklist and/or knowledge test, level of<br />
assistance required of instructor (hands on, verbal, no assistance), and resident’s self-assessment of confidence <strong>for</strong><br />
each procedure. We piloted this EPA with 32 interns in our Beside Ultrasound Course. In this course, we train<br />
residents in simulated ultrasound-guided procedures including: central venous catheters, arterial lines, paracentesis<br />
and thoracentesis. For advancement to level 2 entrustment, each intern had to pass the knowledge test at the end of<br />
the course, and correctly complete all four procedures under the supervision of instructors.<br />
Results to Date: One hundred percent of our interns correctly completed the required procedures in the simulation<br />
environment and passed the knowledge assessment at the end of the course. Consequently, all of the interns<br />
advanced to level 2 entrustment (able to per<strong>for</strong>m in actual practice under full supervision) <strong>for</strong> the procedures.<br />
Discussion/Reflection/Lessons Learned: Residents’ ability to per<strong>for</strong>m common procedures independently by<br />
graduation is a critical outcome of residency training. Until now little has been done to assess residents’ procedural<br />
competence beyond logging of procedures. Our Procedural EPA demands careful observation and assessment of<br />
residents’ skills, and purposeful entrustment as skills develop. While we only piloted initial advancement to Level<br />
2 entrustment, time will yield more in<strong>for</strong>mation on the number of procedures needed <strong>for</strong> advancement, rates of<br />
progression <strong>for</strong> residents to higher levels of entrustment, as well as patient outcomes and complications reported <strong>for</strong><br />
residents at different levels of entrustment.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 17
Transitions of Care: A New Curriculum to Promote Safer Hospital Discharges<br />
O. Al Sous, K. Ramdeen *, V. Abiraj, M. Akce, J. Hopper<br />
St. Joseph Mercy Hospital, Ann Arbor, Michigan, USA<br />
*University of North Dakota<br />
Introduction<br />
Background<br />
Objectives<br />
Process Description<br />
Results<br />
Care coordination,<br />
including transitions<br />
of care, has been<br />
recognized by the<br />
Institute of<br />
Medicine as a<br />
national priority<br />
area <strong>for</strong> quality<br />
improvement. (1)<br />
Ineffective<br />
handovers at<br />
hospital discharge<br />
seriously impede the<br />
quality and safety of<br />
patient care, as well<br />
as pose a significant<br />
financial burden. (2)<br />
Safe hospital<br />
discharge is always a<br />
major concern,<br />
particularly in the<br />
early academic year<br />
when new interns<br />
and residents are<br />
practicing their roles<br />
<strong>for</strong> the very first<br />
time. The potential<br />
<strong>for</strong> error is high<br />
during this period;<br />
we developed a onemonth<br />
Transitions<br />
of Care (TOC)<br />
rotation <strong>for</strong> the<br />
early PGY-2 year.<br />
The St. Joseph<br />
Mercy Hospital<br />
Internal Medicine<br />
Residency is a<br />
community program<br />
in a 537-bed<br />
tertiary care<br />
hospital in Ann<br />
Arbor, Michigan.<br />
There are 61<br />
residents including<br />
categorical and<br />
preliminary internal<br />
medicine and<br />
transitional year<br />
residents.<br />
Our Medicine<br />
Teaching Service<br />
(MTS) hospital<br />
ward team consists<br />
of one supervising<br />
physician, one<br />
senior resident,<br />
three interns and<br />
one or two medical<br />
students. Clinical<br />
rounds are preceded<br />
by brief case<br />
management<br />
rounds; where early<br />
discharge planning<br />
takes place.<br />
• To deliver high quality care to hospital patients.<br />
• To avoid preventable re-admissions.<br />
• To ensure resident reflective learning on transitions of care.<br />
• To incorporate ACGME requirement <strong>for</strong> systems-based practice.<br />
Expectations<br />
• Work within the MTS team and lead case management rounds<br />
and early discharge planning.<br />
• Provide patients with in-depth education about disease processes,<br />
preventive measures, medication changes and vaccination updates.<br />
• On admission, ensure accurate medication reconciliation and<br />
primary care physician (PCP) notification.<br />
• Assess appropriateness of discharge location.<br />
• Provide one on one intern supervision of the discharge process,<br />
including medication reconciliation, in<strong>for</strong>mative concise discharge<br />
summaries, patient counseling about new medications and follow<br />
up tests and appointments.<br />
• Follow up on any pending tests on discharge<br />
• Coordinating communication with primary care physicians and<br />
case managers regarding discharge plan.<br />
• For patients who do not have primary care physician, set up follow<br />
up appointments with the TOC resident in the resident continuity<br />
clinic.<br />
Prior to the start of the rotation, TOC residents attend an<br />
orientation led by a chief resident and in<strong>for</strong>matics specialist.<br />
Expectations, curriculum and goals are reviewed. TOC residents<br />
taught how to keep an electronic log of primary care contacts.<br />
Near the end of rotation, the TOC resident facilitates a meeting<br />
with the MTS team, attending and chief resident to discuss<br />
readmissions and analyze preventability of at least one of them.<br />
Evaluation<br />
Based on ACGME milestones using Entrustable Professional<br />
Activities (EPA):<br />
• Recognize need to advocate<br />
<strong>for</strong> individual patient needs<br />
• Provide appropriate<br />
preventive care and teach<br />
patient regarding self-care<br />
• Effectively communicate<br />
plan of care to all members<br />
of the health care team<br />
• Utilize patient-centered<br />
education strategies<br />
• Manage and coordinate<br />
care and care transitions<br />
across multiple delivery<br />
systems<br />
• Engage in collaborative<br />
communication with all<br />
members of the health<br />
care<br />
Response from residents, faculty and<br />
interdisciplinary staff has been positive.<br />
Residents commented: “Good learning<br />
experience as a bridge between relentless<br />
inpatient physician ef<strong>for</strong>ts and outpatient<br />
long term health care providers. Ensuring<br />
more patient safety by all means”, “I will<br />
be utilizing this training to incorporate<br />
in my future role as team leader”, “Made<br />
sure the inpatient plans continue in<br />
the outpatient world”, “I learnt a lot<br />
regarding coordination care plans after<br />
discharge to make sure that patients are<br />
living in a safe environment in order<br />
to prevent relapse or readmission”<br />
Conclusion<br />
Multiple transitions of care innovations have been studied but it has been<br />
difficult to draw conclusions regarding best practice. (2) As more structured<br />
modalities are explored, residency programs should prepare physicians<br />
in training to practice safe discharges and adapt concise and consistent<br />
communication between the inpatient and the outpatient settings. For the next<br />
academic year, we are planning to continue TOC training <strong>for</strong> all second year<br />
residents prior to starting their roles as team leaders. As the ward team structure<br />
evolves, the hospital ward curriculum will continue to incorporate the new<br />
ACGME transition of care competencies.<br />
References<br />
1. Priority Areas <strong>for</strong> National Action, Trans<strong>for</strong>ming Health<br />
Care Quality. Adams K, Corrigan JM, eds. 2003, The<br />
National Academies Press. Accessed at: http://www.<br />
nap.edu/openbook.php?record_id=10593<br />
2. Transitional Care: Focusing on Patients-Centered<br />
Outcomes and Simplicity. Bray-Hall, Susan T. 6,<br />
s.l.: Annals of Internal Medicine, 2012, Vol. 157.<br />
REMARKABLE MEDICINE. REMARKABLE CARE.<br />
Designed and Produced by: Debi Nichols, Graphic Designer<br />
St. Joseph Mercy Hospital – Ann Arbor, Michigan<br />
Printing Services and Graphic Design Department
<strong>Poster</strong> Number: 18<br />
<strong>Poster</strong> Title: Transition of Care: A New Curriculum to Enhance Safer Hospital Discharges<br />
Authors and Affiliate Institutions: Ola Al Sous, Khris Ramdeen, Vishal Abiraj, Mehmet Akce, John Hopper, St.<br />
Joseph Mercy Hospital<br />
Submitting Author<br />
Ola Al Sous, MD<br />
Third-Year Resident<br />
Department of Internal Medicine<br />
St. Joseph Mercy Hospital<br />
5333 McAuley Drive<br />
Suite 3009<br />
Ann Arbor, MI 48106<br />
Telephone: (904) 651-6443<br />
Email: alsouso@trinity-health.org<br />
Discussion of How the Problem was Identified and Explored: Care coordination including transition of care has<br />
been recognized by the Institute of Medicine as a national priority area <strong>for</strong> quality improvement. Ineffective<br />
handovers at hospital discharge seriously impede the quality and safety of patient care. Safe discharge is always a<br />
major concern; in particular early in the academic year when new interns and second year residents are practicing<br />
their roles <strong>for</strong> the first time. Due to the high potential <strong>for</strong> error during this period, a one-month Transition of Care<br />
(TOC) rotation was developed in the PGY-2 year, July through October. The purpose is to deliver high quality<br />
hospital discharges allowing improved patient care and reducing rate of preventable readmissions.<br />
Description of the Innovation: TOC residents work within the Medicine Teaching Service (MTS) team and lead<br />
interdisciplinary rounds. Prior to the rotation, residents attend an orientation led by a chief resident and in<strong>for</strong>matic<br />
specialist. The roles of TOC residents are to ensure: contact with primary care physicians, early discharge planning,<br />
and in-depth patient education. The TOC resident educates interns on the discharge process including medication<br />
reconciliation and in<strong>for</strong>mative concise discharge summaries. The TOC resident ensures contact with primary care<br />
physicians as well as case managers at patients discharge. Patients who do not have primary care physicians are<br />
seen by the TOC resident in the resident continuity clinic. Near the end of rotation, the TOC resident facilitates a<br />
meeting with the MTS team, attending and chief resident to analyze preventability of at least one readmission.<br />
Results to Date: Response from residents, faculty and interdisciplinary staff has been positive. Data from the first<br />
month of the rotation show improved communication with doctors and admission medication reconciliation.<br />
Discussion/Reflection/Lessons Learned: Multiple transition of care innovations have been studied but it has been<br />
difficult to draw conclusion regarding best practice. As more structured modalities are explored, residency<br />
programs should prepare physicians in training to practice safe discharges and adapt concise and consistent<br />
communication between the inpatient and the outpatient settings.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 18
<strong>Poster</strong> Number: 19<br />
<strong>Poster</strong> Title: Transitional Care: A Novel, Narrative Initiative<br />
Authors and Affiliate Institutions: Sandy Balwan, Sean LaVine, Saima Chaudhry, Steven Savella, Alexandria<br />
Atuahene, Hofstra NorthShore-LIJ School of Medicine at Hofstra University<br />
Submitting Author<br />
Sandy Balwan, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
Hofstra North Shore-LIJ School of Medicine at Hofstra University<br />
300 Community Drive<br />
Manhasset, NY 11030<br />
Telephone: (516) 562-2587<br />
Email: sbalwan@NSHS.edu<br />
Discussion of How the Problem was Identified and Explored: More than two-thirds of sentinel events in<br />
hospitals are caused by communication breakdowns, half during transitions. The ACGME requires residency<br />
programs to instruct trainees in care transitions. Traditionally the focus has been placed on intra facility transitions<br />
and less emphasis has been placed on transitions between inpatient and rehabilitation settings on discharge.<br />
Description of the Innovation: In July 2011, The Hofstra NSLIJ Residency introduced a unique transition of care<br />
experience as an alternative to classroom based education. Interns followed a patient they discharged to a<br />
rehabilitation center or skilled nursing facility (SNF). At the facility the intern reconciled discharge medications<br />
with SNF medications, identified new medical issues, and verified follow-up of pending tests or recommendations.<br />
Additionally, interns wrote a narrative on how the experience altered their understanding of transitional care,<br />
patient safety, and how it may impact their future practice. Two hospitalists evaluated each narrative and provided<br />
feedback.<br />
Results to Date: Fifty out of 60 interns participated. Interns identified a large number of changes to medications<br />
including 62% of patients having a new medication, 47% having a medication discontinued, and 28% having a<br />
change in dose or frequency. Thirty percent of patients had pending tests, 50% had new medical issues identified,<br />
and 60% required a specialty consultation. Sixty percent of interns reported their experience was very valuable in<br />
their understanding of the fragmentation in healthcare. Hospitalist evaluators identified two major themes in the<br />
intern’s reflections. First, interns reported they more fully understood the importance of handoff between facilities<br />
and identified procedures to improve it; second, interns reported more com<strong>for</strong>t in discussing nursing facilities with<br />
their patients.<br />
Discussion/Reflection/Lessons Learned: The experience provided an inexpensive, effective method of teaching<br />
transitional care that differed from traditional methods and was well received. The activity fulfills teaching in all<br />
six ACGME competencies and the entrustable professional activity (EPA) of safely discharging a patient.<br />
Hospitalist core faculty are uniquely qualified to assess and provide feedback on transitional care teaching activities<br />
in resident programs.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 19
<strong>Poster</strong> Number: 20<br />
<strong>Poster</strong> Title: Night Float Cards: An Educational Endeavor<br />
Authors and Affiliate Institution: Poonam Beniwal-Patel, Kathlyn E Fletcher, Medical College of Wisconsin<br />
Submitting Author<br />
Poonam Beniwal-Patel, MD<br />
Chief Resident<br />
Department of Internal Medicine<br />
Medical College of Wisconsin<br />
9200 West Wisconsin Avenue<br />
Cancer Center—Fifth Floor<br />
Milwaukee, WI 53226<br />
Telephone: (414) 917-2046<br />
Email: pbeniwal@mcw.edu<br />
Discussion of How the Problem was Identified and Explored: Since the implementation of the Accreditation<br />
Council <strong>for</strong> Graduate Medical Education (ACGME)’s new work hour policies in July 2011, more internal medicine<br />
residency programs have had to utilize a night float system to comply with restricted hours. With night float<br />
comprising a larger proportion of residency requirements, attention should be paid to its contribution to resident<br />
education.<br />
Description of the Innovation: We gave night float cards to each intern during their weeks as a night float. We<br />
asked interns to enter the following in<strong>for</strong>mation on each card: patient name, question to address, source of answer,<br />
answer. The cards also had a space <strong>for</strong> the question to be answered. Each night float intern was instructed to<br />
complete at least one card per night. They could give the card to someone from a team that they had cross-covered<br />
or admitted to during the previous night or they could find the answer on their own. The cards were turned into the<br />
chief resident at the end of each month.<br />
Results to Date: A total of sixty-two night float cards were collected. We analyzed the interns’ questions by<br />
identifying the content area (i.e. cardiology) and type of question (i.e. diagnostics). The most common content<br />
areas were: cardiology (25%), general internal medicine (15%), pain (11.3%) and nephrology (11.3%). Interns<br />
most commonly asked about how to manage conditions (72%) but also commonly had questions about diagnosis<br />
(28%). There was a wide range of complexity in the interns’ questions. An example of a straight<strong>for</strong>ward question<br />
was how to treat hospital acquired pneumonia in a patient with a penicillin allergy. An example of a complex<br />
question was how to insert an arterial line. Interns used a variety of resources to find the answer to questions: on<br />
call medicine resident (74%), UpToDate/Online Source (15%), consult resident/fellow (7%) and a pharmacist (4%).<br />
Interestingly not all of the answers provided by on-call residents were correct.<br />
Discussion/Reflection/Lessons Learned: We designed a simple intervention to facilitate learning while on night<br />
float. These data identify common questions that interns encounter while on night float rotations. There is an<br />
opportunity to construct an educational tool <strong>for</strong> night float interns that incorporates the most commonly-asked<br />
questions and also encourages independent investigation into questions using different resources.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 20
Improving Patient Satisfaction Outcomes, Resident Interpersonal<br />
Communication Skills, and Resident Feedback<br />
Christina R. Bergin, Cheryl W. O'Malley, Karen Alonso, Douglas Eckhardt, and Richard Gerkin<br />
Banner Good Samaritan Medical Center/Phoenix VA Medical Center Internal Medicine Residency Program, Phoenix AZ<br />
Background<br />
• The concept of patient satisfaction is becoming increasingly important in medicine today.<br />
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS)<br />
survey has standardized the assessment and public reporting of patient satisfaction. In<br />
addition, the ValueBased Purchasing Program by the Centers <strong>for</strong> Medicare and Medicaid<br />
Services links various outcomes, including patient satisfaction, to reimbursement.<br />
• Such public attention stems from evidence that difficulties in physicianpatient<br />
communication contribute to patient dissatisfaction with medical care, malpractice suits,<br />
discontinuity of care, and reduced compliance with treatment regimens.<br />
• Conversely, improved communication and increased patient satisfaction have been<br />
linked to improved continuity of care and patient compliance, decreased readmission<br />
rates, and even improvement in various health outcomes.<br />
• To help identify members of the teaching service, an in<strong>for</strong>mation sheet describing the<br />
teaching service is provided to patients (Figure 4), and a monthly picture roster is<br />
distributed to nursing staff.<br />
• Every four months, a comprehensive report is compiled <strong>for</strong> each resident with their<br />
survey results, enabling them to identify strengths and to address any identified<br />
deficiencies, with the goal of improving per<strong>for</strong>mance (Figure 5).<br />
• A high percentage of residents reported "always" or "usually" utilizing several key<br />
strategies that can enhance patient satisfaction (Figure 9). However, other techniques<br />
remain underemployed despite discussion of their merits (Figure 10).<br />
Figure 9. Frequency of Commonly Utilized Strategies by Residents<br />
How the Problem was Identified and Explored<br />
• Residents are important providers of patient care on the inpatient teaching service, and<br />
there<strong>for</strong>e they create opportunities <strong>for</strong> directly impacting patient satisfaction.<br />
• In addition, the ACGME requires training programs to teach about systems of care and<br />
to assess trainees using multiple sources of feedback, including patients.<br />
• Our Internal Medicine residency program identified<br />
the need <strong>for</strong> more <strong>for</strong>mal resident training in patient<br />
satisfaction and interpersonal communication after a<br />
quarter in which the inpatient teaching service's<br />
score was suboptimal on the HCAHPS<br />
Communication with Doctors composite (Figure 1).<br />
• Due to HCAHPS methodology, no concrete<br />
explanation <strong>for</strong> our low score was available; nor was<br />
there specific provider feedback to help us focus our<br />
ef<strong>for</strong>ts. We there<strong>for</strong>e recognized there was an<br />
opportunity to obtain 360degree patient and nursing<br />
feedback about resident per<strong>for</strong>mance in the inpatient<br />
setting as well.<br />
Figure 1. Q4 2010 HCAHPS “Top Box” Scores,<br />
Communication with Doctors Composite<br />
Description of the Innovation<br />
• A patient satisfaction and feedback project was initiated in June 2011. Patient and<br />
nursing surveys were developed as residencyspecific feedback tools. Questions were<br />
based on both the HCAHPS Communication with Doctors composite and on several other<br />
satisfaction factors that were felt to be useful feedback items.<br />
• At the beginning of each ward month, a faculty member leads residents in an interactive<br />
session about HCAHPS and key concepts in patient satisfaction. Strategies to enhance<br />
physicianpatient communication and patient satisfaction are discussed in detail.<br />
• Residents rotating on wards distribute the surveys to patients and nurses requesting<br />
their anonymous feedback (Figures 2 and 3). Selfaddressed envelopes are also included<br />
to preserve anonymity.<br />
Figure 4. Patient In<strong>for</strong>mation Sheet<br />
• After the first year of the project, a survey was conducted assessing resident attitudes<br />
and frequency of use of suggested behaviours shown to improve patient satisfaction.<br />
Results to Date<br />
• The Internal Medicine residency service's HCAHPS top box scores improved from 52%<br />
in the fourth quarter of 2010 to 78% in the second quarter of 2012 (Figure 6).<br />
• Resident scores on the distributed programspecific patient surveys also have<br />
increased, three of these significantly (Figure 7).<br />
Figure 6. HCAHPS "Top Box" Scores, Communication with<br />
Doctors Composite<br />
• While not statistically significant, there is a trend towards residents placing more value<br />
on patient satisfaction since the inception of this project. Sixty percent of residents<br />
agreed or strongly agreed that<br />
patient satisfaction was important<br />
to them prior to the project's<br />
initiation, whereas 72% did so after<br />
participating (Figure 8).<br />
• Residents also place a priority on<br />
multisource feedback. Over 90%<br />
of residents felt it is valuable to<br />
obtain feedback from patients;<br />
84% felt it is valuable to obtain<br />
feedback from nurses (Figure 8).<br />
Figure 5. Resident Feedback Report<br />
Figure 7. Scores on Residency Program's Patient Surveys<br />
• With progression in PGY level, there was a trend towards an increased rate of:<br />
explaining their role on the team<br />
using whiteboards in patient rooms<br />
sitting down at the bedside during H&P, daily assessment, and on day of discharge<br />
Discussion<br />
• The implementation of this project has led residents to place more value on patient<br />
satisfaction than they did previously.<br />
• This program innovation has also filled a prior void in multisource feedback in the<br />
inpatient setting within our residency program. The addition of individualized patient and<br />
nursing feedback from their time on the wards has allowed <strong>for</strong> more targeted interventions<br />
to assist in the continued maturation of resident interpersonal communication skills.<br />
• Combining focused education about patient satisfaction with individualized resident<br />
feedback and the regular discussion of techniques shown to enhance communication and<br />
patient satisfaction seems to have been effective at improving patient satisfaction scores<br />
<strong>for</strong> the Internal Medicine teaching service.<br />
• This initial project has also identified other<br />
areas <strong>for</strong> focused initiatives. We added five<br />
new questions to the patient feedback tool to<br />
enhance the quality and quantity of feedback<br />
received by residents (Figure 11). We are<br />
working to improve distribution and return rates<br />
of the two feedback tools. We have added<br />
more <strong>for</strong>mal opportunities <strong>for</strong> residents to<br />
review and discuss their feedback, including a<br />
monthly small group activity <strong>for</strong> wards residents,<br />
in order to promote selfreflection, goalsetting,<br />
and peertopeer sharing of successful<br />
techniques.<br />
References<br />
Figure 10. Frequency of Less Commonly Utilized Strategies by<br />
Residents<br />
Boulding, W et al. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17:4148.<br />
Brinkman, WB et al. Effect of multisource feedback on resident communication skills and professionalism. Arch Pediatr Adolesc Med. 2007;161:4449.<br />
Cope, DW et al. Modification of residents’ behavior by preceptor feedback of patient satisfaction. J Gen Intern Med. 1986;1:394398.<br />
DiMatteo, MR. Enhancing patient adherence to medical recommendations. JAMA. 1994; 271:7983.<br />
Figure 11. New Patient Survey<br />
Reinders, ME et al. Does patient feedback improve the consultation skills of general practice trainees? A controlled trial. Medical Education. 2010;44:156164.<br />
Stewart, MA. Effective physicianpatient communication and health outcomes: a review. Can Med Assoc J. 1995;152:14231433.<br />
Figure 2. Patient Survey<br />
Figure 3. Nursing Survey<br />
Figure 8. Resident Attitudes About Patient Satisfaction and Multisource<br />
Feedback<br />
Swayden, KJ et al. Effect of sitting vs. standing on perception of provider time at bedside: a pilot study. Patient Education and Counseling. 2012;86:166171.<br />
Tan, SY. Issues in medical malpractice IX. Hawaii Medical Journal. 2007;66:7879.
<strong>Poster</strong> Number: 21<br />
<strong>Poster</strong> Title: Improving Patient Satisfaction Outcomes, Resident Interpersonal Communication Skills, and<br />
Resident Feedback<br />
Authors and Affiliate Institutions: Christina R Bergin, Cheryl W O’Malley, Karen Alonso, Douglas Eckhardt,<br />
Richard Gerkin, Banner Good Samaritan Medical Center<br />
Submitting Author<br />
Christina R. Bergin, MD<br />
Faculty/Academic Hospitalist<br />
Department of Internal Medicine<br />
Banner Good Samaritan Medical Center<br />
1111 East McDowell Road<br />
Medical Education, LL2<br />
Phoenix, AZ 85006<br />
Telephone: (602) 839-6301<br />
Email: christina.bergin@bannerhealth.com<br />
Discussion of How the Problem was Identified and Explored: Our Internal Medicine residency program<br />
identified the need <strong>for</strong> more <strong>for</strong>mal resident training in patient satisfaction after a quarter in which the inpatient<br />
teaching service’s score was suboptimal on the Hospital Consumer Assessment of Healthcare Providers and<br />
Systems (HCAHPS) survey’s Communication with Doctors composite. Due to HCAHPS methodology no concrete<br />
explanation <strong>for</strong> this or specific feedback was available. We there<strong>for</strong>e felt there was opportunity to obtain 360-<br />
degree patient and nursing feedback about resident per<strong>for</strong>mance in the inpatient setting as well.<br />
Description of the Innovation: A patient satisfaction and nursing survey project was initiated in June 2011. At<br />
the beginning of each ward month, a faculty member leads a discussion about HCAHPS and strategies to enhance<br />
patient satisfaction. Residents rotating on wards distribute surveys to patients and nurses requesting their<br />
anonymous feedback. Every four months, a comprehensive report is compiled <strong>for</strong> each resident with their survey<br />
results, enabling them to identify strengths and to address any identified deficiencies. After the first year of the<br />
project, a survey was conducted assessing resident attitudes and frequency of use of suggested behaviors shown to<br />
improve patient satisfaction.<br />
Results to Date: The Internal Medicine residency service’s HCAHPS scores improved from a mean of 52% in the<br />
fourth quarter of 2010 to a mean of 73% in the first quarter of 2012. Resident scores on the distributed patient<br />
surveys also have increased, some significantly. While not statistically significant, there is a trend towards<br />
residents placing more value on patient satisfaction since the inception of this project. Sixty percent of residents<br />
agreed or strongly agreed that patient satisfaction was important to them prior to the project’s initiation, whereas<br />
72% did so after participating. Additionally, over 90% of residents felt it is valuable to obtain feedback from<br />
patients; nearly 84% felt it is valuable to obtain feedback from nurses. A high percentage of residents reported<br />
“always” or “usually” utilizing several key strategies that enhance patient satisfaction. However, other techniques<br />
are underemployed, including sitting down at the bedside, using whiteboards in patient rooms, and distributing<br />
in<strong>for</strong>mation describing the teaching service.<br />
Discussion/Reflection/Lessons Learned: The implementation of this project has led residents to place more value<br />
on patient satisfaction and provided them with individualized patient feedback allowing <strong>for</strong> more targeted<br />
interventions. Combining these methods with the regular discussion of techniques shown to enhance patient<br />
satisfaction seems to have been effective at improving patient satisfaction scores. We would like to continue to<br />
optimize patient satisfaction and to enhance rates of patient and nursing feedback. These goals may be achieved in<br />
part by addressing the satisfaction strategies currently still underutilized, together with interventions to augment the<br />
quantity of feedback obtained.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 21
Does the time of educational conference impact patient discharge times?<br />
Steffanie Campbell, MD; Alexander M Djuricich, MD<br />
Department of Medicine, Baylor College of Medicine;<br />
Department of Medicine, Indiana University School of Medicine<br />
Introduction<br />
Background<br />
Resident workload is continually compressed due to decreasing length of<br />
stay, increasing admission acuity and overall nationwide increase in hospital<br />
admissions.<br />
This is further exacerbated by the 2003 and 2011 work hour limitations.<br />
Recent research surrounding the 2003 and 2011 work hour changes have<br />
found that residents believe the quality of their education has suffered.<br />
Despite this compression, we must still try and find time <strong>for</strong> our residents to<br />
learn the necessary medical knowledge.<br />
One patient care task vital to throughput and hospital quality measures is<br />
discharge time.<br />
It has been hypothesized that morning conferences delay patient discharge<br />
times by procuring resident working time.<br />
The purpose of this study was to determine whether moving the time of day<br />
an educational conference is scheduled impacts the time to completion of<br />
patient discharges by internal medicine teaching services.<br />
Methods<br />
Setting and participants<br />
Wishard Hospital is a county hospital in downtown Indianapolis. It has 340<br />
beds, 90 of these are dedicated to medicine patients. Wishard Hospital serves<br />
an indigent population with multiple medical comorbidities and increasingly<br />
difficult social situations. These factors make discharges <strong>for</strong> patients extremely<br />
complex and difficult.<br />
Internal Medicine Interns and Residents assigned to Wishard Hospital<br />
inpatient teaching teams during the study period. Our residency consists of 36<br />
categorical medicine residents, 14 Medicine-Pediatrics residents, and 12<br />
preliminary residents per year, <strong>for</strong> a total of 177 during the 2010-2011 academic<br />
year.<br />
Our interns and residents train at four different hospitals, to include: a county<br />
hospital – Wishard, a tertiary care hospital – University, a private hospital –<br />
Methodist and the Veterans Administration Hospital.<br />
On average each intern and resident does 3-4 months per year of inpatient<br />
medicine wards at Wishard hospital. There are five teaching teams with one<br />
resident and two interns each. There are two additional teaching teams with<br />
one resident or one intern each. The overnight admissions are done by a<br />
nightfloat team.<br />
During the three month study period during the year 2010-2011, 51 interns<br />
and residents rotated through Wishard Hospital.<br />
Discharge Times <strong>for</strong> Each Morning Report<br />
Number of Discharges<br />
Study Design<br />
Morning report-style conference <strong>for</strong> all internal medicine interns and residents<br />
at Wishard Hospital was shifted from 8:30am to 2pm during 8/23/2010<br />
through 12/12/2010.<br />
This shift occurred at the midpoint of a month long inpatient rotation in an<br />
attempt to eliminate potential differences conferred by individual resident<br />
efficiency.<br />
Teaching service medicine patient discharge times, defined as the time the<br />
discharge order set was signed, were compared during the three-months the<br />
conference time was shifted.<br />
Resident attendance was measured with resident sign-in sheets placed at<br />
each conference time.<br />
Resident satisfaction and time preference was measured using an<br />
electronically delivered survey.<br />
Conference<br />
Time<br />
Time of Day<br />
Results<br />
Discharge time <strong>for</strong> 1493 medicine patients discharged during the 8:30 am<br />
was compared to 1506 medicine patients discharged during the 2pm report<br />
time.<br />
Dependent variable was educational conference time. The independent<br />
variables were medicine patient discharge times and resident satisfaction<br />
scores. The discharge times during the 8:30am educational conference and<br />
the 2pm educational conference were graphically compared. The discharge<br />
times were also analyzed using a T-Test method with a significant P-value<br />
defined as less than 0.05.<br />
It was noted there was no significant difference in discharge time with a P<br />
value of 0.3.<br />
Mean discharge time during both designated conference times was between<br />
4:30 and 5:00 pm.<br />
All residents were sent a link to participate in the electronic survey. 42 of 51<br />
residents (82% response rate) completed the survey<br />
74% of the interns and residents that completed the survey felt the 8:30am<br />
conference time was better <strong>for</strong> rounding and education. 56% of the interns<br />
and residents that completed the survey felt the 8:30am conference time<br />
was better <strong>for</strong> patient care tasks.<br />
Conclusions<br />
As shown through our study, medical patient discharge time was not<br />
significantly influenced by time of educational conference.<br />
Educating residents when time constraints and workload continue to increase<br />
is fraught with challenges.<br />
Our data suggest that Program Directors should resist the urge from hospital<br />
administration to change educational conference times in order to maximize<br />
throughput via earlier discharge times.<br />
References<br />
Goitein L, Ludmerer K. Resident Workload-Let’s Treat the Disease, Not Just the Symptom. JAMA Intern<br />
Med, online, 3/25/<strong>2013</strong><br />
Healthcare Cost and Utilization Project net. Available at: http://hcupnet.ahrq.gov/<br />
Meyer MH, Jekowsky E, Crane FG. Applying plat<strong>for</strong>m design to improve the integration of patient services<br />
across the continuum of care. Managing Service Quality 2007; 17:23.<br />
Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a<br />
systematic review. Arch Intern Med 2012; 172:1057.<br />
O'Leary KJ, Liebovitz DM, Feinglass J, et al. Creating a better discharge summary: improvement in quality<br />
and timeliness using an electronic discharge summary. J Hosp Med 2009; 4:219.
<strong>Poster</strong> Number: 22<br />
<strong>Poster</strong> Title: Does the Time of Educational Conference Impact Patient Discharge Times?<br />
Authors and Affiliate Institutions: Steffanie Campbell, Baylor College of Medicine; Alexander Djuricich,<br />
Indiana University School of Medicine<br />
Submitting Author<br />
Steffanie R. Campbell, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
Baylor College of Medicine<br />
One Baylor Plaza<br />
BCM 285<br />
Houston, TX 77030<br />
Telephone: (713) 798-6724<br />
Email: Steffanie.Campbell@bcm.edu<br />
Discussion of How the Problem was Identified and Explored: Changes in direct patient care time caused by the<br />
duty hour changes in 2003 and 2011 have compressed medical resident daily workload. Despite this compression,<br />
residents must still learn the necessary medical knowledge and patient care management. Thus, the timing of<br />
educational activities is imperative to optimize attendance while also assuring completion of necessary patient care<br />
tasks. One task vital to throughput is the time of discharge. The purpose of this study was to determine whether<br />
moving the time of day an educational conference is scheduled impacts the time to completion of patient discharges<br />
by internal medicine teaching services.<br />
Description of the Innovation: Morning report-style conference <strong>for</strong> internal medicine residents was shifted from<br />
8:30am to 2pm during a five-month period. This shift occurred at the midpoint of the rotation in an attempt to<br />
eliminate potential differences conferred by individual resident efficiency. Teaching service medicine patient<br />
discharge times, defined as the time the discharge order set was signed, were then obtained via the electronic<br />
medical record <strong>for</strong> this same time period. The discharge times recorded were compared <strong>for</strong> the two different<br />
educational conference times. Resident attendance and satisfaction was also measured.<br />
Results to Date: Discharge times <strong>for</strong> 1495 medicine teaching service patients demonstrated a mean discharge time<br />
between 4:30 and 5pm. The timing of the educational conference had no effect on the discharge time. There were<br />
222 discharges around 5pm during the 8:30am conference time and 201 discharges at 5pm during the 2pm<br />
conference time. Resident attendance was approximately 50% <strong>for</strong> both conference times. Satisfaction survey<br />
results <strong>for</strong> 42 residents demonstrated that 64% preferred the 8:30 am report time, and 74% felt this time was also<br />
better <strong>for</strong> education and rounding.<br />
Discussion/Reflection/Lessons Learned: Medical patient discharge time was not significantly influenced by time<br />
of educational conference. Educating residents when time constraints and workload continue to increase is fraught<br />
with challenges. Our data suggest that there are other factors beyond the timing of educational conference that may<br />
influence discharge times.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 22
<strong>Poster</strong> Number: 23<br />
<strong>Poster</strong> Title: Incorporating a Longitudinal Subspecialty Continuity Clinic into Internal Medicine Training<br />
Authors and Affiliate Institutions: Amy F Matthews, Steven V Angus, University of Connecticut School of<br />
Medicine<br />
Submitting Author<br />
Amy F. Matthews<br />
Administrative Program Coordinator<br />
Department of Medicine<br />
University of Connecticut School of Medicine<br />
263 Farmington Avenue<br />
Farmington, CT 06030<br />
Telephone: (860) 679-6297<br />
Email: amatthews@uchc.edu<br />
Discussion of How the Problem was Identified and Explored: The number of Internal Medicine Residency<br />
graduates choosing to pursue further subspecialty training in Internal Medicine has risen nearly 25% over the last<br />
10 years. Although elective block rotations and inpatient subspecialty experiences are available, these brief<br />
encounters fail to give residents true insight into what it would be like to practice in that profession. Most elective<br />
time is spent rounding on the inpatient service and per<strong>for</strong>ming subspecialty consults with different attendings,<br />
impairing the development of a true mentoring relationship between resident and attending. Additionally, patients<br />
seen on subspecialty rotations are typically seen only in the hospital with no continuity of care provided by the<br />
residents.<br />
Description of the Innovation: In an attempt to overcome these barriers, a weekly longitudinal ambulatory-based<br />
subspecialty clinic was developed as part of the PGY2/3 year curriculum. During non-call rotations, residents may<br />
elect to spend one half-day each week working with the same subspecialty mentor and seeing the same panel of<br />
patients <strong>for</strong> the duration of their ambulatory-based subspecialty continuity clinic. The typical resident attends<br />
approximately 40-50 half-day sessions in their longitudinal clinic, in addition to their 130 half-day primary care<br />
continuity clinic sessions.<br />
Results to Date: Ninety out of 155 graduates (58%) from the Internal Medicine program opted to participate in the<br />
longitudinal ambulatory-based subspecialty clinic. We found residents participating in the second clinic experience<br />
were significantly more likely to match into a fellowship than residents who did not (p=.001). Satisfaction surveys<br />
targeting residents who selected the second continuity experience and their faculty preceptors were administered<br />
anonymously and overall, residents agreed that the second clinic was a valuable component of their training (100%)<br />
and helpful in their decisions about pursuing fellowship training (93%) while 100% of faculty reported the<br />
experience was valuable to residents considering fellowships, in helping them craft stronger letters of<br />
recommendation, and choosing suitable candidates <strong>for</strong> their fellowship programs.<br />
Discussion/Reflection/Lessons Learned: A longitudinal continuity clinic based in a specialty clinic was<br />
associated with higher rates of matching into fellowships and high satisfaction ratings by faculty and residents<br />
alike. Future research should explore the experience’s clinical impact on patient care and patient satisfaction.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 23
<strong>Poster</strong> Number: 24<br />
<strong>Poster</strong> Title: Achieving Balance on the Inpatient Internal Medicine Wards: A Per<strong>for</strong>mance Improvement Project<br />
to Restructure Resident Work Hours at a Tertiary Care Center<br />
Authors and Affiliate Institutions: Brian M Cohee, Joshua D Hartzell, William T Shimeall, Walter Reed<br />
National Military Medical Center<br />
Submitting Author<br />
Brian M. Cohee, MD<br />
Pulmonary and Critical Care Medicine Fellow<br />
Department of Internal Medicine<br />
Walter Reed National Military Medical Center<br />
Pulmonary Clinic, Building Nine<br />
8901 Wisconsin Avenue<br />
Bethesda, MD 20889<br />
Telephone: (301) 295-4191<br />
Email: brian.m.cohee.mil@health.mil<br />
Discussion of How the Problem was Identified and Explored: Verbal reports from residents working under a<br />
night-float system were that on-call teams were routinely violating work hours. Also, because the majority of<br />
admissions were occurring late in the day, the night float was admitting more patients than the day teams, and these<br />
patients had rushed initial evaluations and poor continuity. Additionally, the emergency department expressed<br />
frustration over prolonged wait times <strong>for</strong> admissions.<br />
Description of the Innovation: We report the results of a quality improvement project designed to enhance our<br />
ward structure to improve continuity and better align resident resources with institutional demands. Data collection<br />
on the details of admitting intensity, disposition times, and continuity were collected during an 8-day period be<strong>for</strong>e<br />
and a 12-day period after an intervention that changed the ward team structure from a night-float system to a senior<br />
resident long-call system with a graded transition of responsibility to a night team. All housestaff and attendings<br />
that rotated on the new structure during an eight-week period were surveyed after implementation.<br />
Results to Date: The new structure improved patient continuity and resident satisfaction and sense of patient<br />
involvement. Disposition times from the emergency department were substantially improved. Survey respondents<br />
reported subjective improvements in quality of patient care and handoffs, as well as improved adherence to dutyhour<br />
regulations. The changes also resulted in a decrease of one resident on night-float responsibility without<br />
increasing other ancillary support.<br />
Discussion/Reflection/Lessons Learned: A growing body of literature exists describing how fatigue, handoffs,<br />
and work intensity affect the quality of patient care and the educational experience of residents. While many<br />
studies have examined each of the factors independently, there remains little understanding as to how these factors<br />
interplay and the best ways to optimize rotation structure to achieve the best balance. Reports of interventions<br />
designed to improve care at specific centers have occasionally yielded unexpected results, and are probably highly<br />
dependent on local factors. Designing a ward admission system around a brief but intensive assessment of the<br />
intensity of work was associated with better alignment of resident resources with work load, and resulted in<br />
improvements in continuity, emergency department disposition times, adherence with duty hours, and transitions in<br />
care.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 24
<strong>Poster</strong> Number: 25<br />
<strong>Poster</strong> Title: Breast Cancer Screening and Prevention in Primary Care: A Novel Curricular Intervention <strong>for</strong><br />
Medicine Housestaff<br />
Authors and Affiliate Institutions: Jennifer Corbelli, Melissa McNeil, University of Pittsburgh School of<br />
Medicine<br />
Submitting Author<br />
Jennifer A. Corbelli, MD<br />
Faculty<br />
Department of General Internal Medicine<br />
University of Pittsburgh School of Medicine<br />
230 McKee Place<br />
Suite 600<br />
Pittsburgh, PA 15213<br />
Telephone: (585) 781-4177<br />
Email: corbellija@upmc.edu<br />
Discussion of How the Problem was Identified and Explored: Women’s health content accounts <strong>for</strong><br />
approximately 6% of the American Board of Internal Medicine certifying examination. Yet national studies have<br />
shown that residents do not receive sufficient training in women’s health. Furthermore, prior survey research by the<br />
submitting author found that breast health knowledge among housestaff is poor: <strong>for</strong> example, fewer than 10% had<br />
ever calculated a Gail score. This educational intervention targets interns’ knowledge and skills surrounding breast<br />
health.<br />
Description of the Innovation: The curriculum is multimodal and takes place over a half-day session. Interns first<br />
take a knowledge-based pre-test. Next, they work through a 30-minute interactive web-based virtual patient case<br />
and a team-based learning session, both of which focus on a variety of breast health topics including the<br />
controversies in screening mammography, the Gail model, chemoprevention, and management of high-risk women.<br />
They then take a knowledge-based post-test. To target skill development, interns per<strong>for</strong>m a pre- and post- breast<br />
exam on the Mammacare® breast simulator, which uses specialized software to generate scores <strong>for</strong> completeness<br />
and accuracy.<br />
Results to Date: Data collection is ongoing. With existing data, interns’ pre- and post- test scores on both the<br />
knowledge assessment and the Mammacare simulator were compared. Furthermore, PGY-2s, who have not<br />
received this curriculum, took the same knowledge-based assessment, with scores compared to interns’ postcurriculum<br />
scores. A repeated measures Analysis of Covariance (ANCOVA) will be calculated, to control <strong>for</strong><br />
length of time in the program as a potential confounder. Preliminary data shows a significant improvement in<br />
interns’ post-test scores on both knowledge and skills assessments. Furthermore, data shows that interns who<br />
received this curriculum per<strong>for</strong>m significantly better on a knowledge-based assessment than PGY-2s who do not.<br />
Discussion/Reflection/Lessons Learned: Housestaff serve as the primary care physician <strong>for</strong> a panel of patients<br />
during their residency training, many of whom have numerous barriers to care. As such, housestaff are responsible<br />
<strong>for</strong> optimization of their patients’ breast health, as the majority of these patients see no other physician <strong>for</strong><br />
preventive health measures. Results to date suggest that a low-cost, low-time investment curriculum can result in a<br />
significant improvement the knowledge and skills necessary <strong>for</strong> interns to meet their patients’ breast health needs.<br />
Furthermore, interns’ superior per<strong>for</strong>mance to PGY-2s demonstrates that this topic is not being adequately<br />
delivered elsewhere in their training.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 25
<strong>Poster</strong> Number: 26<br />
<strong>Poster</strong> Title: Chief Resident Leadership Academy<br />
Authors and Affiliate Institutions: Nathan E Derhammer, Loyola University Medical Center<br />
Submitting Author<br />
Nathan E. Derhammer, MD<br />
Associate Program Director<br />
Division of Hospital Medicine<br />
Department of Internal Medicine and Pediatrics<br />
Loyola University Medical Center<br />
2160 South First Avenue<br />
Maywood, IL 60304<br />
Telephone: (708) 216-5674<br />
Email: nderhammer@lumc.edu<br />
Discussion of How the Problem was Identified and Explored: The role of chief resident is a time-honored<br />
tradition and <strong>for</strong>mative experience, as well as one that brings with it lofty expectations from program directors,<br />
residents-at-large, and individual chief residents alike. Chief residents typically lack <strong>for</strong>mal training <strong>for</strong> this<br />
uniquely challenging and important position. Our institution identified a need <strong>for</strong> preparation of incoming chief<br />
residents from all departments to refine and develop leadership skills with respect to their applicability in this<br />
multifaceted role.<br />
Description of the Innovation: Using a learner-centered curriculum driven by a leadership skills inventory<br />
completed by participants, the Chief Resident Leadership Academy is comprised of five weekly discussion-based<br />
sessions. Although conversations are guided by brief preparatory reading assignments, involvement of both<br />
educational leaders and current chief residents provides insight and expertise at a number of levels. The<br />
participation of leaders and chief residents (both active and incoming) from a variety of residency programs at our<br />
institution addresses the hidden curriculum of building professional interdepartmental relationships.<br />
Results to Date: Pilot data collected by survey demonstrated that 100% of participants in the 2012 Chief Resident<br />
Leadership Academy found the program to be both personally and professionally beneficial, relevant to their chief<br />
residency, and enhanced by the interdepartmental scope of involvement. Importantly, participants reported that the<br />
climate of the sessions promoted non-judgmental discussion and all respondents indicated that they would<br />
recommend the program to future chief residents.<br />
Discussion/Reflection/Lessons Learned: The philosophy behind the Chief Resident Leadership Academy is<br />
simple: leaders-in-training deserve the opportunity to develop their skills and identify challenges BEFORE<br />
assuming a highly regarded and highly scrutinized position such as chief resident. The individuals benefit from a<br />
heightened sense of awareness and confidence and a decreased sense of isolation when faced with the multitude of<br />
unique but recurrent issues related to chief residency. Program directors benefit from chief residents who have been<br />
imparted some degree of “institutional memory” and also offered the opportunity to reflect on strengths and<br />
weaknesses as they pertain to their role as an educational leader. Residents benefit from cohesive, confident,<br />
emotionally-intelligent leadership. Future directions of the Chief Resident Leadership Academy will include<br />
enhancing interdepartmental participation and collecting data to support the above assertions.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 26
<strong>Poster</strong> Number: 27<br />
<strong>Poster</strong> Title: “The Chief’s Seminar”: Motivating New Residents to Master Clinical Reasoning<br />
Authors and Affiliate Institutions: Christopher Dittus, Vanya Grover, Georgia Panagopoulos, Lenox Hill<br />
Hospital; Kenar Jhaveri, Hofstra North Shore-LIJ School of Medicine at Hofstra University<br />
Submitting Author<br />
Christopher Dittus, DO<br />
Chief Resident<br />
Department of Internal Medicine<br />
Lenox Hill Hospital<br />
100 East 77th Street<br />
New York, NY 10075<br />
Telephone: (917) 754-0887<br />
Email: cdittus@nshs.edu<br />
Discussion of How the Problem was Identified and Explored: Postgraduate medical education is primarily<br />
lecture-based learning, which has been unchanged <strong>for</strong> decades. Identification of multiple learning styles has<br />
modified undergraduate medical education. This has not been adequately adapted in the postgraduate medical<br />
education setting. To accommodate these changes, we propose a reproducible, interactive teaching curriculum led<br />
by chief residents.<br />
Description of the Innovation: This innovative clinical reasoning curriculum is based on three concepts – “who,<br />
what, and how.” First, the program is led by chief residents (i.e. “who”). Second, topics are presented based on the<br />
chief complaint, and not the disease itself (e.g. “dyspnea,” not “pneumonia”). This allows the resident to generate a<br />
differential and arrive at the diagnosis through structured clinical reasoning (i.e. “what”). Third, the in<strong>for</strong>mation<br />
must be conveyed using an innovative approach to engage and motivate residents (i.e. “how”). Incentives and<br />
competition are excellent motivators <strong>for</strong> residents. Specifically, each module begins with a topic-based crossword<br />
puzzle competition followed by three weekly, small-group, interactive sessions using concept maps. Data were<br />
collected via pre- and post-course five-item quizzes. The Wilcoxon Signed-Rank Test was used <strong>for</strong> statistical<br />
analysis. A six point resident survey was also distributed <strong>for</strong> evaluation of each module.<br />
Results to Date: To date, four one-month modules have been completed – Dyspnea (N=15), Chest Pain (N=13),<br />
Fever (N=14), and Abdominal Pain (N=10). Results showed a statistically significant increase in quiz scores <strong>for</strong> the<br />
Chest Pain (pre-, post-test means: 1.77, 3.08; p=0.007), Fever (2.21, 3.21; p=0.008), and Abdominal Pain (3.5, 4.3;<br />
p=0.011) modules, and a trend towards statistical significance <strong>for</strong> the Dyspnea module (2.93, 3.67; p=0.053).<br />
Additionally, the six-point resident survey demonstrated overall resident satisfaction with each instructed module.<br />
Discussion/Reflection/Lessons Learned: The results of this pilot study reveal a statistically significant increase in<br />
five-item quiz scores after attending the Chest Pain, Fever, and Abdominal Pain teaching modules. The evolving<br />
nature of this curriculum allows us to adapt the subsequent modules to improve resident education. This<br />
curriculum, based on the “who, what and how” concepts, is a novel and effective way to enhance resident education<br />
and satisfaction.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 27
<strong>Poster</strong> Number: 28<br />
<strong>Poster</strong> Title: Objectification and Meaningful Implementation of a Medicine Curriculum Designed to Produce the<br />
Next Generation of Physician Leaders<br />
Authors and Affiliate Institutions: Scott R Friedstrom, Helen Koselka, Good Samaritan Hospital; Curtis A<br />
Sheldon, Cincinnati Children’s Hospital<br />
Submitting Author<br />
Scott R. Friedstrom, MD<br />
Program Director<br />
Division of Medicine<br />
Department of Internal Medicine<br />
Good Samaritan Hospital<br />
375 Dixmyth Avenue<br />
Cincinnati, OH 45220<br />
Telephone: (513) 862-3306<br />
Email: friedstrom@yahoo.com<br />
Discussion of How the Problem was Identified and Explored: The need <strong>for</strong> program change became obvious<br />
when our board pass rate recently dropped dramatically. Using the techniques of SWOT analysis, key driver<br />
diagrams, and mind mapping, we realized that this was a symptom of a bigger problem, rather than a bump in the<br />
road. Our analysis helped us to conclude that a curriculum change was needed, but also, and more fundamentally, a<br />
culture change was necessary. This can be especially challenging <strong>for</strong> a community based program. The didactic<br />
curriculum was renovated and re-invigorated. Key faculty were identified, and a “buy-in” to this change was<br />
obtained. Support of the GME office, as well as highly placed hospital administrators, was solicited and obtained.<br />
Description of the Innovation: The didactic curriculum has been individualized <strong>for</strong> each post-graduate year. A<br />
first year interactive lecture series called “Foundations of Professionalism and Continuous Learning” has been<br />
implemented. Interns have been taught how to use mind-maps, and they are now mind-mapping “The Hitchhiker’s<br />
Guide to Internal Medicine”. These maps can be continuously updated, and are being shared on the cloud.<br />
Beginning at week 1 of PGY year 2, and continuing <strong>for</strong> 78 weeks, a theme has been chosen. In successive noon<br />
conferences during each week, the relevant chapter from a major medicine text is discussed, the same topic from a<br />
major board review book is discussed, the relevant subspecialist brings it to the bedside in a lecture, and 2-3 case<br />
scenarios are discussed to teach clinical reasoning. For each week of this curriculum, mind-maps are created. The<br />
last six months of the PGY3 year are spent in an intensive board review ef<strong>for</strong>t. We predict the mind maps will be<br />
very useful in board preparation.<br />
Results to Date: It is still early. However, our resident team placed second in the “Doctor’s Dilemma Quiz Bowl”<br />
competition of the most recent Ohio ACP chapter meeting. Last year they did not escape the first round. We have<br />
one-third more resident research projects being conducted this year when compared to last year. Be<strong>for</strong>e and after<br />
quizzes are measuring real per<strong>for</strong>mance improvement. Scores on ITEs and ABIM exams will be compared when<br />
available. But most importantly, a palpable change is in the air. Most of our residents now exhibit what Sam Keen<br />
called “fire in the belly.”<br />
Discussion/Reflection/Lessons Learned: Change is usually daunting and <strong>for</strong>eboding; this change has been<br />
exhilarating. Our new curriculum is based on fundamental principles of education, systems theory, bioethical<br />
principles, variance analysis using Donald Wheeler’s work, process improvement based on Demmings’ work, the<br />
study of conflict management based on Pues’ work, and much more. And a bonus of this ef<strong>for</strong>t is that much of this<br />
change is helping us to prepare <strong>for</strong> and implement the NAS. It has been a lot of work, but in the words of Thomas<br />
Jefferson: “I’m a great believer in luck, and I find the harder I work, the more I have of it.” We’re feeling lucky.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 28
<strong>Poster</strong> Number: 29<br />
<strong>Poster</strong> Title: Innovative and Successful Evidence-Based Morning Report Linked to Resident-Led Journal Club<br />
Authors and Affiliate Institutions: Brian Hanson, Jerrod Quarles, Anita Udayamurthy, Alison Wing, Sarah Lee,<br />
Laura Broder, Kirstin Juhl, Justin Howard, Steve Powell, Matt Lehnert, Colin Turner, Jonathan Koffel, Nacide<br />
Ercan-Fang, Minneapolis VA Medical Center<br />
Submitting Author<br />
Brian J. Hanson, MD<br />
Chief Resident<br />
Department of Internal Medicine<br />
Minneapolis VA Medical Center<br />
One Veterans Drive<br />
111 Hanson<br />
Minneapolis, MN 55417<br />
Telephone: (612) 467-7141<br />
Email: hans3829@umn.edu<br />
Discussion of How the Problem was Identified and Explored: Practice-based learning and improvement is a<br />
part of the Accreditation Committee <strong>for</strong> Graduate Medical Education’s (ACGME) core competencies. The<br />
evidence-based medicine (EBM) milestones include asking answerable questions, acquiring the best evidence,<br />
appraising the validity and usefulness, as well as applying the evidence to decision-making <strong>for</strong> individual patients.<br />
Our goal was to improve residents’ EBM skills by implementing an EBM morning report and a resident-led journal<br />
club tied directly to patient care.<br />
Description of the Innovation: We implemented an EBM morning report linked to a resident-led journal club at<br />
our institution. A clinical question in the PICO <strong>for</strong>mat is generated from the care of a current patient. A research<br />
librarian aids in the search while teaching search techniques. An article is selected to answer the clinical question<br />
and the resident critically appraises the article with the aid of an EBM mentor. Standardized instructions guide the<br />
resident through the appraisal and presentation process. A chief resident reviews presentation skills and techniques.<br />
At a subsequent morning report, the resident presents their findings and teaching points. Care is taken to apply the<br />
findings directly to patient care. The EBM mentor in addition to a clinical expert are present to guide discussion<br />
and answer questions. A questionnaire using a Likert scale from 1-5 was used to the rate quality of the journal<br />
club. A score of “5” indicated the evaluator strongly agreed with the statement and the presentation far exceeded<br />
expectations. A score of “1” indicated the evaluator strongly disagreed with the statement and the presentation was<br />
unacceptable.<br />
Results to Date: The curriculum addressed the development of a clinical question, the acquisition of relevant<br />
evidence, critical appraisal, and patient application. Over the course of three years, 38 residents led an EBM journal<br />
club. Overall, residents found EBM report to be helpful and educational. Based on the six questions, the average<br />
presenter scores were 4.53, 4.79, 4.82, 4.68, 4.62, and 4.71 <strong>for</strong> clinical relevance, coherency, presenter<br />
understanding, identifying study strengths and weaknesses, applicability, and overall presentation respectively.<br />
Discussion/Reflection/Lessons Learned: Our EBM linked resident-led journal club meets ACGME practicebased<br />
learning and improvement milestones. In addition, it has created high quality presentations. Residents present<br />
relevant in<strong>for</strong>mation in a coherent, clear, interesting and dynamic way while addressing key components of EBM.<br />
In addition, the sessions have be well attended and participation excellent. We propose that a resident driven,<br />
mentor-assisted, EBM morning report linked to a resident-led journal club can be a successful way to address<br />
current ACGME milestones.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 29
<strong>Poster</strong> Number: 30<br />
<strong>Poster</strong> Title: Tea(ch) Time: An Afternoon Approach to Morning Report<br />
Authors and Affiliate Institutions: Katherine Harris, Manish Suneja, University of Iowa Carver College of<br />
Medicine<br />
Submitting Author<br />
Katherine Harris, MD<br />
Associate Program Director<br />
Division of General Medicine<br />
Department of Internal Medicine<br />
University of Iowa Carver College of Medicine<br />
200 Hawkins Drive<br />
E 327-1 GH<br />
Iowa City, IA 52242<br />
Telephone: (319) 384-8512<br />
Email: harriski@healthcare.uiowa.edu<br />
Discussion of How the Problem was Identified and Explored: In this era of increasingly hectic time schedules<br />
and duty hour restrictions, our residency program struggled with balancing didactic teaching and traditional<br />
morning report based case presentations. Additional challenges included finding a time and venue <strong>for</strong> case based<br />
learning which would enable maximum participation of the residents/students on the inpatient wards. The goal of<br />
this project was to introduce daily case-based learning sessions to enhance diagnostic reasoning at a time and venue<br />
which would maximize inpatient resident/student participation. Initial needs assessment was done by a survey of<br />
all Internal Medicine Residents (respondents: 30/82).<br />
Description of the Innovation: Based on the survey results we piloted an afternoon session called “Tea (ch)<br />
Time” which took place at 3:00 pm in the individual team room of the presenting resident/students. At each<br />
conference a resident team presented one of their current patients selected on the basis of: 1) diagnostic dilemmas;<br />
2) interesting findings; 3) common diseases with uncommon presentations; 4) notable radiologic findings; 5) rare<br />
diagnoses. These sessions were in<strong>for</strong>mal and were moderated by two faculty members. At the end of the session the<br />
group was asked to identify two teaching points. The teaching points focused more on general principles with<br />
emphasis placed on the cognitive process behind clinical decision making.<br />
Results to Date: The resident/student attendance and participation was excellent. Feedback from the<br />
residents/students pertaining to the sessions was gathered. The major themes from comments gathered were that the<br />
learners liked the exposure to more cases, it helped them develop diagnostic reasoning skills and a systematic<br />
approach to patient care. An important and unanticipated finding was noted with the medical students surveyed.<br />
The medical students were asked if they were more likely to enter the field of Internal Medicine because of these<br />
teaching sessions and 80% replied “yes.”<br />
Discussion/Reflection/Lessons Learned: Based on the results of the survey, we plan on implementing “Tea<br />
Time” as a learning curriculum in November 2012. The Chief residents will play a large role in moderating the<br />
sessions, along with key clinical faculty on the Inpatient Wards. This will make the curriculum sustainable, as the<br />
two faculty initiating this project are unable to facilitate the meeting daily. We will be gathering data regularly to<br />
further assess resident/medical student satisfaction and gain more insight regarding the session’s effectiveness in<br />
teaching clinical reasoning on the inpatient wards.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 30
“You Must Be The Change You Wish To See In The World”- Mahatma Gandhi<br />
An Innovative Approach to Per<strong>for</strong>mance Improvement Curriculum<br />
Saba A. Hasan, MD, FACP; Ekaterina Vypritskaya, MD, FACP<br />
Abstract<br />
Methods<br />
Results<br />
Conclusion<br />
ACGME requires each resident to<br />
“evaluate per<strong>for</strong>mance data <strong>for</strong> their<br />
panels related to both chronic<br />
disease management and<br />
preventive health care, receiving<br />
faculty guidance <strong>for</strong> developing a<br />
data-based action plan and evaluate<br />
the plan at least twice a year”<br />
Objectives<br />
To develop an innovative approach<br />
to the existing Per<strong>for</strong>mance<br />
Improvement Curriculum by having<br />
residents work on their projects with<br />
an attitude of ownership and<br />
commitment.<br />
•In the past three years, residents<br />
have worked on a number of different<br />
projects, which have enhanced the<br />
care of their patients and improved<br />
patient satisfaction<br />
•The presentations have led to<br />
evidence based discussions among<br />
residents and faculty<br />
•Through the work on PI projects, the<br />
program has been able to recruit<br />
institutional resources in the clinic<br />
system<br />
•Some examples include:<br />
•introduction of weight loss clinic<br />
•appointment reminder phone<br />
calls<br />
•improved medication<br />
reconciliation<br />
•increased number of influenza<br />
and pneumovax vaccinations<br />
given<br />
•improved overall care of diabetic<br />
patients through the introduction<br />
of focused diabetic visits and a<br />
resident designed diabetic visit<br />
progress note template<br />
•Residents feel a sense of pride<br />
regarding their success with<br />
interventions and are motivated to<br />
change their strategies when faced<br />
with barriers hindering change<br />
In order to maximize the impact of<br />
the residents' Per<strong>for</strong>mance<br />
Improvement experience, the<br />
program implemented the following:<br />
•Residents make a twice yearly<br />
<strong>for</strong>mal presentation of their data to<br />
their peers and faculty<br />
•The presentation includes a brief<br />
overview of the problem, the most<br />
recent evidence based<br />
recommendations <strong>for</strong> preventive<br />
and chronic disease care, the reason<br />
the resident chose to address it in his<br />
panel of patients, review of data<br />
collected, summary of results and<br />
future plans <strong>for</strong> the project<br />
•These presentations stimulate<br />
discussions on medical care and<br />
systems based issues encountered<br />
in the continuity clinic<br />
•Through the process, the residents<br />
optimize the care of clinic patients<br />
and identify systems barriers,<br />
which are discussed with peers and<br />
clinic leadership, exploring ideas and<br />
solutions<br />
•Residents receive written<br />
feedback from faculty using an<br />
evaluation <strong>for</strong>m, which is also filed<br />
along with their project in their<br />
portfolio<br />
•In our program, the PI project<br />
exercise not only helps develop the<br />
competency of PBLI, but also<br />
Medical Knowledge,<br />
Communication and Interpersonal<br />
Skills and Systems Based Practice<br />
•It provides a <strong>for</strong>um <strong>for</strong> discussion of<br />
‘best practices’, review of recent<br />
literature/guidelines<br />
• Collaboratively develop innovative<br />
ideas to overcome the challenges<br />
to providing quality care to our clinic<br />
patients.<br />
Healthy Weight Project<br />
References:<br />
•ACGME Outcome Project. General competencies.<br />
http://www.acgme.org/outcome/comp/compmin.asp. Last accessed- May 5, 2011.<br />
•Holmboe ES, Prince L, Green M. Teaching and Improving Quality of Care in a<br />
Primary Care Internal Medicine Residency Clinic. Acad Med. 2005;80:571–73.<br />
•Djuricich AM, Ciccarelli M, Swigonski NL. A Continuous Quality Improvement<br />
Curriculum <strong>for</strong> Residents: Addressing Core Competency, Improving Systems.<br />
Acad Med. 2004;79:65–75.
<strong>Poster</strong> Number: 31<br />
<strong>Poster</strong> Title: “You Must Be the Change You Wish to See in the World.” -Mahatma Gandhi<br />
Authors and Affiliate Institutions: Saba A Hasan, Ekaterina Vypritskaya, Capital Health Regional Medical<br />
Center<br />
Submitting Author<br />
Saba A. Hasan, MD<br />
Program Director<br />
Department of Internal Medicine<br />
Capital Health Regional Medical Center<br />
750 Brunswick Avenue<br />
Trenton, NJ 08638<br />
Telephone: (609) 394-6031<br />
Email: shasan@capitalhealth.org<br />
Discussion of How the Problem was Identified and Explored: ACGME requires each resident to “evaluate<br />
per<strong>for</strong>mance data <strong>for</strong> their panels related to both chronic disease management and preventive health care, receiving<br />
faculty guidance <strong>for</strong> developing a data-based action plan and evaluate the plan at least twice a year.”<br />
Description of the Innovation: In order to maximize the impact of the resident’s Per<strong>for</strong>mance Improvement<br />
experience, the program implemented the following: •Residents make a twice yearly <strong>for</strong>mal presentation of their<br />
data to their peers and faculty •The presentation includes a brief overview of the problem, the most recent evidence<br />
based recommendations <strong>for</strong> preventive and chronic disease care, the reason the resident chose to address it in his<br />
panel of patients, review of data collected and summary of results and future plans <strong>for</strong> the project. •These<br />
presentations stimulate discussions on medical care and systems based issues encountered in the continuity clinic.<br />
•Through the process the residents optimize the care of clinic patients and identify systems barriers, which are<br />
discussed with peers and clinic leadership, exploring ideas and solutions. •Residents receive written feedback from<br />
faculty using an evaluation <strong>for</strong>m, which is also filed along with their project in their portfolio.<br />
Results to Date: In the past three years residents have worked on a number of different projects, enhancing the<br />
care of their patients, improving patient satisfaction and held evidence based discussions on the topics. Residents<br />
feel a sense of pride regarding their success with interventions and are motivated to change their strategies when<br />
faced with barriers hindering change.<br />
Discussion/Reflection/Lessons Learned: In our program, the Per<strong>for</strong>mance Improvement Project exercise not only<br />
helps develop the competency of PBLI, but also Medical Knowledge, Communication and Interpersonal Skills and<br />
Systems Based Practice. It provides a <strong>for</strong>um <strong>for</strong> discussion of ‘best practices’, review of recent literature/guidelines<br />
and collaboratively develop innovative ideas to overcome the challenges to providing quality care to our clinic<br />
patients.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 31
Ambulatory Case Conference—A Novel Approach to Outpatient Education<br />
Stephen J. Knaus MD, FACP and Laurel Fick MD, FACP<br />
St. Vincent Indianapolis Hospital<br />
Introduction<br />
Description of Innovation 2011-12 ACC Schedule Results Conclusion<br />
Evidence-based discussion of<br />
common ambulatory disease states<br />
is often missing in traditional internal<br />
medicine didactic conferences.<br />
Many institutions have successfully<br />
implemented Ambulatory Morning<br />
Report as a way to improve<br />
ambulatory education and cover<br />
ambulatory topics not covered in<br />
other parts of the conference<br />
curriculum. Our program developed<br />
an Ambulatory Case Conference to<br />
improve our resident training in<br />
common conditions encountered in<br />
ambulatory general internal<br />
medicine.<br />
Percent of Cases (n=56)<br />
Graph 1<br />
16<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
14<br />
Ambulatory Case Conference (ACC) is a<br />
30-45 minute resident-led case<br />
presentation and evidence-based<br />
discussion of an outpatient topic of the<br />
resident’s choosing—typically based on<br />
a case encountered in the resident’s<br />
ambulatory experience. This is usually<br />
followed by faculty-led topic-related<br />
MKSAP questions with group response<br />
and discussion. The conference is held<br />
every other Wednesday from 3-4pm<br />
during protected educational time and is<br />
mandatory <strong>for</strong> any resident not on<br />
vacation, nights, ICU, or inpatient<br />
general medical wards. Multiple general<br />
medicine faculty and occasionally<br />
ambulatory clinical pharmacists or<br />
subspecialists are also in attendance.<br />
Topics are diverse, ranging from<br />
women’s health to obesity treatment to<br />
sleep disorders. Topics are chosen by<br />
the resident in collaboration with the<br />
clinic director, and emphasis is placed on<br />
opportunities seen <strong>for</strong> improvement in<br />
medical knowledge and patient care,<br />
such as a women’s health focus in the<br />
fall of 2011. Workshops on ambulatory<br />
procedures, practice management<br />
topics, and quality improvement<br />
supplement the resident presentations<br />
throughout the academic year.<br />
Cases Presented by Residents at ACC by Category, July 2009-February <strong>2013</strong><br />
10 10<br />
9 9 9 9 9<br />
7<br />
5 5<br />
3<br />
2<br />
Presenter<br />
PGY-2 resident<br />
PGY-3 resident<br />
PGY-3 resident<br />
PGY-3 resident<br />
IM Faculty<br />
PGY-3 resident<br />
PGY-3 resident<br />
Clinical Pharmacist<br />
OB-GYN physician<br />
PGY-3 resident<br />
PGY-2 resident<br />
PGY-2 resident<br />
PGY-2 resident<br />
PGY-2 resident<br />
PGY-3 resident<br />
IM Faculty<br />
IM/FM Faculty<br />
PGY-3 resident<br />
PGY-2 resident<br />
PGY-2 resident<br />
Clinical Pharmacist<br />
Topic<br />
Hypertension<br />
Spondyloarthropathies<br />
Fibromyalgia<br />
Secondary amenorrhea<br />
Vaginitis<br />
Breast Cancer Screening<br />
Graves disease<br />
Oral Contraceptive Pills<br />
Cervical Cancer Screening<br />
Obstructive Sleep Apnea<br />
Weight Loss Management<br />
Chronic Low Back Pain<br />
Atrial Fibrillation<br />
Hidradenitis Suppurativa<br />
Male Hypogonadism<br />
Common Errors in<br />
Outpatient Medicine<br />
Joint Injection/Skin Biopsy<br />
Workshop<br />
Rheumatoid Arthritis<br />
Osteoporosis<br />
Psoriasis<br />
Anticoagulation<br />
Management<br />
2010-11 ACC Schedule<br />
Presenter<br />
Topic<br />
PGY-3 resident Diabetes Mellitus, Type 2<br />
PGY-3 resident<br />
Colon Cancer Screening<br />
IM Faculty<br />
Quality Improvement<br />
PGY-3 resident<br />
Subclinical Hypothyroidism<br />
PGY-2 resident<br />
Gastroesophageal Reflux<br />
Disease<br />
PGY-3 resident and IM<br />
Faculty<br />
Clinical Pharmacists<br />
PGY-3 resident<br />
PGY-2 resident<br />
PGY-2 resident<br />
PGY-3 resident<br />
PGY-3 resident<br />
PGY-2 resident<br />
Clinical Pharmacist<br />
Clinical Pharmacist<br />
PGY-2 resident<br />
Opioids <strong>for</strong> Chronic Non-<br />
Cancer Pain<br />
Drug Monitoring<br />
Osteoporosis<br />
Community-Acquired<br />
Pneumonia<br />
Dizziness<br />
Chronic Kidney Disease<br />
Acute Sinusitis<br />
Depression<br />
Getting to Know Your<br />
NSAIDs<br />
COPD Treatments<br />
Skin Cancer<br />
A survey of residents in June 2011<br />
(sixteen respondents) indicated that on<br />
a 5-point Likert scale, residents agreed<br />
that “Ambulatory Case Conference has<br />
added value to my residency training”<br />
(4.62) and that “presenting an<br />
Ambulatory Case Conference during my<br />
residency was a valuable experience”<br />
(4.44). Residents agreed that “MKSAP<br />
questions related to the ACC topic add<br />
value to the Ambulatory Case<br />
Conference session” (4.31).<br />
Ambulatory Case Conference provided<br />
an opportunity to cover ambulatory<br />
topics that were not discussed during<br />
other didactic sessions. A review of<br />
topics from 2008-2011 indicated that<br />
72% of topics presented during<br />
Ambulatory Case Conference were not<br />
presented at our daily noon conference.<br />
Topics were well distributed by category,<br />
with Endocrinology the most frequent<br />
category represented (Graph 1).<br />
2011 ACC Survey Results<br />
Based on 5-point Likert Scale<br />
ACC has added value to my internal<br />
medicine residency training<br />
MKSAP questions related to the ACC<br />
topic add value to the ACC session<br />
Procedural workshop improved my<br />
confidence in per<strong>for</strong>ming joint injections<br />
Procedural workshop improved my<br />
confidence in per<strong>for</strong>ming skin biopsies<br />
Billing/coding workshops improved the<br />
accuracy of my outpatient billing<br />
My confidence in managing outpatients<br />
on chronic opioids improved during the<br />
course of this academic year<br />
Presenting an Ambulatory Case<br />
Conference during my residency was a<br />
valuable experience<br />
Presentations by clinical pharmacists<br />
were helpful in managing my outpatients<br />
4.62<br />
4.31<br />
4.0<br />
4.12<br />
4.38<br />
3.68<br />
4.44<br />
4.53<br />
An evidence-based, multidisciplinary<br />
educational conference devoted to<br />
case-based discussion of common<br />
ambulatory diseases has improved<br />
our program’s training in ambulatory<br />
general internal medicine. It has also<br />
provided a <strong>for</strong>um <strong>for</strong> board-style<br />
review with MKSAP questions related<br />
to the topic discussed and has<br />
provided a setting to incorporate<br />
ambulatory workshops, quality<br />
improvement, and practice<br />
management topics into the residency<br />
curriculum.<br />
References<br />
Spickard A III, Ryan SP, Muldowney JA<br />
III, Farnham L. Outpatient morning<br />
report: a new conference <strong>for</strong> internal<br />
medicine residency programs. J Gen<br />
Intern Med 2000;15:822-824<br />
Wenderoth S, Pelzman F, Demopoulos<br />
B. Ambulatory morning report: can it<br />
prepare residents <strong>for</strong> the American<br />
Board of Internal Medicine Examination?<br />
J Gen Intern Med 2002;17:207-209
<strong>Poster</strong> Number: 32<br />
<strong>Poster</strong> Title: Ambulatory Case Conference—A Novel Approach to Outpatient Education<br />
Authors and Affiliate Institutions: Stephen Knaus, Laurel Fick, St. Vincent Hospital and Health Care Center<br />
Submitting Author<br />
Stephen J. Knaus, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
St. Vincent Hospital and Health Care Center<br />
2001 West 86th Street<br />
Indianapolis, IN 46268<br />
Telephone: (317) 338-7619<br />
Email: sjknaus@stvincent.org<br />
Discussion of How the Problem was Identified and Explored: Evidence-based discussion of common<br />
ambulatory disease states is often missing in traditional internal medicine didactic conferences. Many institutions<br />
have successfully implemented Ambulatory Morning Report as a way to improve ambulatory education and cover<br />
ambulatory topics not covered in other parts of the conference curriculum. Our program developed an Ambulatory<br />
Case Conference to improve our resident training in common conditions encountered in ambulatory general internal<br />
medicine.<br />
Description of the Innovation: Ambulatory Case Conference is a 30-45 minute resident-led case presentation and<br />
evidence-based discussion of an outpatient topic of the resident’s choosing—typically based on a case encountered<br />
in the resident’s ambulatory experience. This is followed by faculty-led topic-related MKSAP questions with<br />
group response and discussion. The conference is held every other Wednesday from 3-4pm during protected<br />
educational time and is mandatory <strong>for</strong> any resident not on vacation, nights, ICU, or inpatient general medical wards.<br />
Multiple general medicine faculty and occasionally ambulatory clinical pharmacists or subspecialists are also in<br />
attendance. Topics are diverse, ranging from women’s health to obesity treatment to sleep disorders (complete list<br />
available). Workshops on ambulatory procedures, practice management topics, and quality improvement<br />
supplement the resident presentations throughout the academic year.<br />
Results to Date: A survey of residents in June 2011 (sixteen respondents) indicated that on a 5-point Likert scale,<br />
residents agreed that “Ambulatory Case Conference has added value to my residency training” (4.62) and that<br />
“presenting an Ambulatory Case Conference during my residency was a valuable experience” (4.44). Residents<br />
agreed that “MKSAP questions related to the ACC topic add value to the Ambulatory Case Conference session”<br />
(4.31). Ambulatory Case Conference provided an opportunity to cover ambulatory topics that were not discussed<br />
during other didactic sessions. A review of topics from 2008-2011 indicated that 72% of topics presented during<br />
Ambulatory Case Conference were not presented at noon conference.<br />
Discussion/Reflection/Lessons Learned: An evidence-based, multidisciplinary educational conference devoted to<br />
case-based discussion of common ambulatory diseases has improved our program’s training in ambulatory general<br />
internal medicine. It has also provided a <strong>for</strong>um <strong>for</strong> board-style review with MKSAP questions related to the topic<br />
discussed and has provided a setting to incorporate ambulatory workshops, quality improvement, and practice<br />
management topics into the residency curriculum.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 32
Morbidity and Mortality Conference Working Group – Resident Driven Change<br />
Tasha Kouvatsos, MD, Emily Stewart, MD and Gretchen Diemer, MD<br />
Thomas Jefferson University, Department of Medicine, Philadelphia, PA<br />
Introduction<br />
Results<br />
The Morbidity and Mortality<br />
Conference (MMC) has been a<br />
requirement <strong>for</strong> all medical training<br />
programs by the Accreditation<br />
Council <strong>for</strong> Graduate Medical<br />
Education (ACGME) since 1983 (1).<br />
Residents graduating from ACGME<br />
accredited residency programs must<br />
demonstrate competence in practice<br />
based learning and improvement<br />
The working group meets after each MMC and monthly to discuss the<br />
systems issues and create the plan of action. The residents divide the<br />
responsibilities and provide updates to the group via email in between<br />
meetings. All education and systems interventions are presented by the<br />
participating residents at the final MMC of the year and the patient safety<br />
officers of the hospital monitor patient outcomes from the interventions.<br />
For example, one MMC highlighted a series of complications from<br />
paracentesis. The working group identified several education and systems<br />
issues and then established a multi-level action plan with supervision,<br />
education and procedural components.<br />
(PBLI) and systems-based practice<br />
(SBP) (2). The New Accreditation<br />
System has a specific emphasis<br />
on patient safety and quality<br />
improvement. Consequently, the<br />
objective of the MMC focuses less on individual culpability and more on the<br />
identification of systems-based errors to develop systems improvements<br />
to increase patient safety and quality of care (3).<br />
Innovation<br />
To identify issues uncovered during MMC and develop an action plan<br />
to improve our current systems-based practice, we created a Morbidity<br />
and Mortality working group comprised of 10 interested residents, chief<br />
medical residents and multidisciplinary faculty. It is the residents who take<br />
ownership of steering the group with guidance from the chiefs and faculty.<br />
This group provides the residents exposure to systems thinking, supporting<br />
the ACGME core competency of systems-based practice, and encourages<br />
systematic review of our current practice, collaboration with hospital<br />
administration and patient safety officers and hands on development of<br />
methods <strong>for</strong> quality improvement.<br />
1 st Generation Trainer<br />
1 st Generation Certified<br />
2 nd Generation Trainer<br />
2 nd Generation Certified<br />
3 rd Generation Trainer<br />
“Train the Trainer”<br />
Paracentesis MMC Interventions:<br />
• Develop a “train the trainer” program<br />
• Establish a yearly ultrasound use/techniques<br />
workshop led by Radiology faculty including<br />
resident practice with a standardized patient<br />
• Distinguish therapeutic from diagnostic<br />
paracentesis <strong>for</strong> procedure certification<br />
• Evaluate procedure kits to optimize safety<br />
• Implement a validated procedure-specific<br />
checklist<br />
• Increase use of post-procedure order set<br />
• Create a resident simulation case featuring a<br />
patient with a post-paracentesis complication<br />
to assess and teach recognition and<br />
management of post-procedure complications<br />
Discussion<br />
The goal of the Morbidity and Mortality Working Group is to empower<br />
residents to implement systems-based changes to improve patient care.<br />
The participating residents become adept at identifying the systems issues<br />
associated with adverse patient outcomes, and understand the steps<br />
needed to achieve change using a multidisciplinary approach.<br />
References: (1) Kauffmann R, Landman M, Shelton J, et al. The Use of a Multi-disciplinary Morbidity and Mortality Conference to Incorporate ACGME General Competencies. J Surg Educ 2011; 68(4):303-308. (2) ACGME Outcomes Project. General<br />
competencies. http://www.acgme.org/outcome/comp/compmin.asp (3) Rabizadeh S, Gower A, Payton K, et al. Restructuring the Morbidity and Mortality Conference in a Department of Pediatrics to Serve as a Vehicle <strong>for</strong> System Changes. Clin Pediatr<br />
2012;51(11):1079-1086.
<strong>Poster</strong> Number: 33<br />
<strong>Poster</strong> Title: Morbidity and Mortality Conference Working Group—Resident Driven Change<br />
Authors and Affiliate Institutions: Tasha Kouvatsos, Emily Stewart, Gretchen Diemer, Jefferson Medical<br />
College of Thomas Jefferson University<br />
Submitting Author<br />
Tasha Kouvatsos, MD<br />
Chief Resident<br />
Department of Internal Medicine<br />
Jefferson Medical College of Thomas Jefferson University<br />
1011 Chestnut Street<br />
Apartment 502 East<br />
Philadelphia, PA 19107<br />
Telephone: (717) 968-7305<br />
Email: tasha.kouvatsos@gmail.com<br />
Discussion of How the Problem was Identified and Explored: The Morbidity and Mortality Conference (MMC)<br />
has been a requirement <strong>for</strong> all medical training programs by the Accreditation Council <strong>for</strong> Graduate Medical<br />
Education (ACGME) since 1983 (1). Residents graduating from ACGME accredited residency programs must<br />
demonstrate competence in practice based learning and improvement (PBLI) and systems-based practice (SBP) (2).<br />
The New Accreditation System has a specific emphasis on patient safety and quality improvement. Consequently,<br />
the objective of the MMC focuses less on individual culpability and more on the identification of systems-based<br />
errors to develop systems improvements to increase patient safety and quality of care (3). (1) Kauffmann R,<br />
Landman M, Shelton J, et al. The Use of a Multi-disciplinary Morbidity and Mortality Conference to Incorporate<br />
ACGME General Competencies. J Surg Educ. 2011; 68(4):303-308. (2) ACGME Outcomes Project. General<br />
competencies. http://www.acgme.org/outcome/comp/compmin. asp (3) Rabizadeh S, Gower A, Payton K, et al.<br />
Restructuring the Morbidity and Mortality Conference in a Department of Pediatrics to Serve as a Vehicle <strong>for</strong><br />
System Changes. Clin Pediatr (Phila). 2012 Oct 3. [Epub ahead of print].<br />
Description of the Innovation: To identify issues uncovered during MMC and develop an action plan to improve<br />
our current systems-based practice, we created a Morbidity and Mortality working group comprised of residents,<br />
chief medical residents and multidisciplinary faculty. It is the residents who take ownership of steering the group<br />
with guidance from the chiefs and faculty. This group provides the residents exposure to systems thinking,<br />
supporting the ACGME core competency of systems-based practice, and encourages systematic review of our<br />
current practice, collaboration with hospital administration and patient safety officers and hands on development of<br />
methods <strong>for</strong> quality improvement.<br />
Results to Date: The working group meets after each MMC and monthly to discuss the systems issues and create<br />
the plan of action. The residents divide the responsibilities and provide updates to the group via email in between<br />
meetings. All education and systems interventions are presented by the participating residents at the final MMC of<br />
the year and the patient safety officers of the hospital monitor patient outcomes from the interventions. For<br />
example, one MMC highlighted a series of complications from paracentesis. The working group identified several<br />
education and systems issues and then established a multi-level action plan with supervision, education and<br />
procedural components. Interventions included a “train the trainer” program where radiology faculty train senior<br />
housestaff/fellows in appropriate ultrasound technique <strong>for</strong> paracentesis who then supervise the residents per<strong>for</strong>ming<br />
this procedure. Radiology faculty will teach techniques <strong>for</strong> ultrasound-guided procedures using standardized<br />
patients to allow residents to practice in a controlled environment at orientation each year. The residents also<br />
suggested distinguishing therapeutic from diagnostic paracentesis <strong>for</strong> procedure certification. The procedural<br />
solutions include evaluating our procedure kits to optimize safety, implementing a validated procedure-specific<br />
checklist instead of the universal procedure checklist and initiating a policy that requires a post-procedure order set,<br />
prompting recognition of complications and initiation of rescue management earlier.<br />
Discussion/Reflection/Lessons Learned: The goal of the Morbidity and Mortality Working Group is to empower<br />
residents to implement systems-based changes to improve patient care. The participating residents become adept at<br />
identifying the systems issues associated with adverse patient outcomes, and understand the steps needed to achieve<br />
change using a multidisciplinary approach.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 33
The July Transition – Making It Easier<br />
EIP Working Group<br />
Baystate Medical Center / Tufts University School of Medicine<br />
The Problem<br />
• Many residents feel ill prepared <strong>for</strong> the<br />
transition to new responsibilities in July.<br />
• A unique “Fly-up” within our Learner-Manager-<br />
Teacher (LMT) model (Fig. 1) was designed to<br />
allay fears and to develop core skills.<br />
The Innovation<br />
Manager/PGY2 Fears: autonomy on nightfloat,<br />
CICU and wards, code situations.<br />
‣Fly-up focus: independence and autonomy.<br />
•Teacher/PGY3 Fears: knowledge, teaching,<br />
being “in-charge.”<br />
‣Fly-up focus: teaching and leadership .<br />
The “Fly-Up” Solution<br />
Structure:<br />
• The last two weeks of June<br />
(be<strong>for</strong>e interns arrive).<br />
• Alternating one-week rotations address<br />
challenges identified above.<br />
Education:<br />
• “New” Managers/PGY2s and<br />
Teachers/PGY3s rotate through two of their<br />
upcoming rotations with at least one peer and<br />
the additional support of a soon-to-be<br />
graduating resident.<br />
• Daily conferences (Fig. 2) highlight key<br />
transitional topics <strong>for</strong> the two groups.<br />
Figure 1: Baystate LMT Model<br />
M T W Th F<br />
Morning Orientation Illness Scripts Learning Model Case Small Group<br />
Objectives Presentation Teaching<br />
Report<br />
Manager<br />
ACLS Organizing your EMR Tricks and Managing Your Self-Directed<br />
Algorithms<br />
Day<br />
Tips<br />
Attending<br />
Precepting<br />
12-1PM<br />
Teaching Styles Rounding Tips<br />
Giving<br />
One Minute Communication<br />
and Tricks<br />
Feedback<br />
Preceptor<br />
Teacher<br />
1-2PM<br />
SIM Center:<br />
SIM Center:<br />
Code Training<br />
Code Training<br />
Figure 2: Conference Schedule<br />
Results<br />
• The majority of residents rate the rotation<br />
as ‘above average.’<br />
• The majority of residents believe that the<br />
overall experience either ‘got them started’<br />
or helped to ‘consolidate knowledge and<br />
skills.’<br />
• Through resident feedback, we have made<br />
the following changes:<br />
• separate noon conference tracks <strong>for</strong> to-be-<br />
Managers/PGY2s and Teachers/PGY3s.<br />
• Model morning-report session.<br />
• Residents: Fly-up is an invaluable rotation<br />
that helps to alleviate concerns and<br />
improve confidence.<br />
Lessons Learned<br />
• Separate tracks <strong>for</strong> to-be-<br />
Managers/PGY2s and Teachers/PGY3s<br />
allow our program to focus on classspecific<br />
needs.<br />
• Peer support and increased supervision<br />
during the Fly-up experience can allay<br />
fears that accompany the July transition<br />
into more autonomous and leadership<br />
roles.<br />
• The Fly-up is an integral element in our<br />
competency-based curriculum as it<br />
prepares our residents <strong>for</strong> key transitions<br />
and new responsibilities.<br />
Competency-Based<br />
Advancement System<br />
Learner<br />
(direct supervision)<br />
Manager<br />
(indirect supervision)<br />
Teacher<br />
(supervises)<br />
PGY-1<br />
PGY-2<br />
PGY-3
<strong>Poster</strong> Number: 34<br />
<strong>Poster</strong> Title: The July Transition—Making It Easier<br />
Authors and Affiliate Institutions: EIP Working Group, Baystate Medical Center/Tufts University School of<br />
Medicine<br />
Submitting Author<br />
Gina Luciano, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
Baystate Medical Center<br />
759 Chestnut Street—S2570<br />
<strong>Spring</strong>field, MA 01062<br />
Telephone: (413) 794-4143<br />
Email: gina.luciano@baystatehealth.org<br />
Discussion of How the Problem was Identified and Explored: Many residents, including ours, feel ill prepared<br />
<strong>for</strong> July transitions. In response to this need, we designed a unique “Fly-up” opportunity within the context of our<br />
Learner-Manager-Teacher (LMT) model to allay fears and to develop essential skills.<br />
Description of the Innovation: Our “Fly-up” period occurs during the last two weeks of June (be<strong>for</strong>e interns<br />
begin). The experience consists of alternating one-week rotations designed to address challenges identified through<br />
program assessment and to help to-be-Managers and to-be-Teachers gain necessary skills and confidence.<br />
Consistent with the goals of our LMT model, Manager Fly-up is focused on independence and autonomy whereas<br />
education and leadership are emphasized <strong>for</strong> Teacher Fly-up. Prior to this curricular change, Learners transitioning<br />
to Managers were most anxious about nightfloat, CCU and ward rotations. To alleviate this anxiety, upcoming<br />
Managers rotate through two of these rotations (one per week) with at least one peer and the additional support of a<br />
soon-to-be graduating resident. A similar schedule is arranged <strong>for</strong> upcoming Teachers who are most concerned with<br />
being an ICU or ward teaching resident. Our conferences spotlight key transitional topics including managerial<br />
skills, ACLS, and self-directed precepting <strong>for</strong> to-be-Managers and rounding tips, leadership / teaching styles,<br />
communication and giving feedback <strong>for</strong> to-be-Teachers. All residents attend morning report where illness scripts,<br />
learning objectives and small group teaching are the focus.<br />
Results to Date: The majority of residents rate the rotation as ‘above average’ and believe the experience either<br />
‘got them started’ or helped to ‘consolidate knowledge and skills.’ Through resident feedback, we have made the<br />
following changes: separate noon conference tracks <strong>for</strong> to-be-Managers and Teachers as described above and a<br />
‘model morning-report’ session were added. Anecdotally, residents often remark that the Fly-up is an invaluable<br />
rotation that helps to alleviate concerns and improve confidence.<br />
Discussion/Reflection/Lessons Learned: Separate tracks <strong>for</strong> to-be-Managers and Teachers allow our program to<br />
focus on class-specific needs and facilitate open and honest discussion. Peer support and increased supervision<br />
during the Fly-up experience can allay fears that accompany the July transition into more autonomous roles. The<br />
Fly-up is an integral element in our competency-based curriculum as it prepares our residents <strong>for</strong> key transitions<br />
and new responsibilities.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 35
<strong>Poster</strong> Number: 35<br />
<strong>Poster</strong> Title: A Refined Patient Safety and Quality Improvement Curriculum <strong>for</strong> Internal Medicine Residents—<br />
Based on a Six-Year Feedback and Review<br />
Authors and Affiliate Institutions: Srikrishna V Malayala, Daniel Molloy, Mushtaq Bhat, Salim H Memon,<br />
Abdul Samdani, Ridhwan Y Baba, Ramesh Metta, Bishnu Kattel, Tawfiq Zabaneh, Shabnam Rehman, Ammar<br />
Saati, Khalid J Qazi, University at Buffalo (Catholic Health System—Sisters of Charity)<br />
Submitting Author<br />
Srikrishna V. Malayala, MD<br />
PGY 3 Resident<br />
Department of Internal Medicine<br />
University at Buffalo (Catholic Health System—Sisters of Charity)<br />
2157 Main Street<br />
Buffalo, NY 14227<br />
Telephone: (304) 951-3599<br />
Email: varun_msk@yahoo.com<br />
Discussion of How the Problem was Identified and Explored: In September 2007; ACGME Committee on<br />
Innovation called <strong>for</strong> identification of opportunities to enhance quality and safety in teaching institutions by<br />
studying the outcomes of resident involvement in organized institutional quality improvement initiatives. As of<br />
academic year 2012, the Internal Medicine Program of University at Buffalo/ Catholic Health System had a 4 week<br />
rotation titled ‘Per<strong>for</strong>mance Improvement’ which is designed based on the ACGME recommendations. This<br />
rotation was first implemented in 2006 and was scheduled in the second year of training. There were 5 learning<br />
activities in the curriculum: Core measure chart review, Understanding Peer Review Process, rotation with Clinical<br />
Documentation specialist, Clinical Patient Safety Goals and Standards & Adverse Significant Event Reporting.<br />
Description of the Innovation: Aim: To further refine the PSQI curriculum and enhance the resident training in<br />
terms of the ACGME six core competencies. Methods: Residents of the last 3 years were asked to grade the<br />
components of the curriculum on a scale of 1-9 (1-3: unsatisfactory; 4-6: satisfactory and 7-9: superior). Residents<br />
were also asked to submit a subjective evaluation of the rotation.<br />
Results to Date: 1) 36 residents responded to the survey. The evaluations were in the superior category <strong>for</strong> core<br />
measure review (7.26/9); peer review process (7/9); Adverse Event reporting (7.18/9), satisfactory category <strong>for</strong><br />
Patient Safety Goals and Standards (6.94/9). Overall co-ordination of the rotation was graded as satisfactory (6.5/9).<br />
2) Subjectively, majority of residents felt that the rotation should be cut down to 2 weeks. Many felt that some<br />
components of the rotation can be moved to PGY-1 to enhance the training in an early phase. 3) Residents and<br />
faculty suggested a list of additional learning activities based on the available literature and current practice.<br />
Discussion/Reflection/Lessons Learned: Based on the feedback and recommendations, a new PSQI curriculum is<br />
designed which spreads over three years of training entitled Quality 101 (2 weeks in PGY-1), Quality 201 (2 weeks<br />
in PGY-2) and Quality 301. New components of the curriculum will be rotation with department of pharmacy,<br />
Infection Control and Case management. A “PSQI task <strong>for</strong>ce committee” comprising the current residents and<br />
faculty is <strong>for</strong>mulated to submit a periodic feedback of the rotation.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 36
<strong>Poster</strong> Number: 36<br />
<strong>Poster</strong> Title: Preparing Residents <strong>for</strong> Team-Based Patient Care: The Development and Implementation of a<br />
Resident Leadership and Management Training Program<br />
Authors and Affiliate Institutions: Jared Moore, David Wininger, Maria Lucarelli, Michael Velez, Christopher<br />
Hanks, Neil Dunavin, Ohio State University College of Medicine, Wexner Medical Center<br />
Submitting Author<br />
Jared Moore, MD<br />
Assistant Program Director<br />
Department of Internal Medicine<br />
Ohio State University College of Medicine, Wexner Medical Center<br />
2050 Kenny Road<br />
Second Floor Pavilion, Suite 2400<br />
Columbus, OH 43221<br />
Telephone: (614) 685-1923<br />
Email: jared.moore@osumc.edu<br />
Discussion of How the Problem was Identified and Explored: Physicians should be the leaders of the<br />
multidisciplinary healthcare teams that will be required to deliver comprehensive patient care within a complex<br />
medical and social environment. We believe we can help our residents develop the skills needed to do that, so we<br />
enlisted the expertise of both medical center faculty and faculty from the university’s business college in an ef<strong>for</strong>t<br />
to create our Leadership and Management Program.<br />
Description of the Innovation: Our curriculum is divided into three phases: mandatory intern year training,<br />
voluntary second and third year training, and advanced training <strong>for</strong> select residents. The intern curriculum is<br />
divided into four series: awareness, communication, leadership without authority, and developing personal<br />
leadership styles. Individual modules focus on making the sessions applicable to interns and preparing them <strong>for</strong><br />
their transition to resident. Intern modules are scheduled once per rotational block and take place during scheduled<br />
lecture time. Second and third year programming will focus on preparing residents to assume leadership positions<br />
both within and after residency training. The course will cover complex team leadership and management theory,<br />
conflict management, organizational and system strategic planning and leading through change. The advanced<br />
training program will allow residents to work with senior leadership on medical center wide projects.<br />
Results to Date: To date, we have delivered four intern modules with feedback in the <strong>for</strong>m of post-module<br />
surveys. Feedback has been favorable with residents preferring modules that promote resident interaction and<br />
address problems that are most immediately pertinent to them.<br />
Discussion/Reflection/Lessons Learned: We successfully implemented the Leadership and Management Program<br />
because we received support from members of leadership at all levels throughout the medical center. Additionally,<br />
we developed internal and external validity by engaging residents and the business college faculty in the planning<br />
process. While a business school may not be available to all programs, institutional and community leaders could<br />
serve a similar purpose. Buy in <strong>for</strong> the program amongst interns has remained the greatest challenge especially at<br />
the beginning of the intern year. We believe that this program will be successful and sustainable if we can help<br />
residents recognize how a deeper understanding of the principles and skills of leadership and management can<br />
improve patient care.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 37
The Next Step in Collaborative Care:<br />
Medical-Legal Partnerships<br />
Brandon Murguia MD, <strong>APDIM</strong> Presenter<br />
St. Mary’s Medical Center, San Francisco<br />
Introduction<br />
In response to continued health disparities in access to healthcare and<br />
health insurance, rising incidence and cost of chronic illnesses, and a<br />
growing body of evidence demonstrating the influence of social and<br />
environmental factors on health and well-being 1,2 , Medical Legal<br />
Partnership (MLPs) are emerging as a new standard of care <strong>for</strong> lowincome,<br />
vulnerable patient populations across the country. Firstly<br />
developed at Boston Medical Center in 1993, MLPs have rapidly<br />
expanded over the last 10-12 years, and as of 2010, are active at 216<br />
health care sites across the US (in a range of specialties, settings, and<br />
patient populations):<br />
Implementation<br />
Since July 1, 2010 our partnership has focused on achieving the 3 core<br />
components of MLP practice: (1) direct assistance <strong>for</strong> patients, (2)<br />
training <strong>for</strong> health care staff, and (3) combined medical-legal systems<br />
advocacy.<br />
The I-HELP Legal Screening Assessment<br />
Legal need<br />
Examples of legal needs that affect health<br />
Income Supports<br />
Social Security benefits<br />
Disability benefits<br />
Insurance access and benefits<br />
Food stamps<br />
Assistance programs<br />
General income<br />
Housing and Utilities<br />
Sanitary housing conditions<br />
Foreclosure prevention / Eviction protection<br />
Utility access, assistance, and shutoff protection<br />
Access to housing subsidies<br />
Disabled tenant rights<br />
Shelter access<br />
Education/Employment Discrimination<br />
Americans with Disability Act compliance<br />
Family & Medical Leave Act compliance<br />
Worker’s compensation rights<br />
Fair Labor Standards Act<br />
Legal Status<br />
Personal and Family Stability<br />
Immigration status<br />
Criminal record issues<br />
Domestic violence<br />
Sexual abuse<br />
Elder abuse and neglect<br />
Divorce<br />
Capacity/competency<br />
Advance directives<br />
Powers of attorney<br />
Figure 1. Source: National Center <strong>for</strong> Medical-Legal Partnership. MLP Network<br />
[Internet]. Boston (MA): http://www.medical-legalpartnership.org/mlp-network.<br />
An MLP combines the skill sets of medical professionals and lawyers<br />
to treat and teach social determinants of health, 3 including income,<br />
nutrition, housing, energy, employment/education, and personal<br />
stability. In recognizing that these determinants often manifest as<br />
unmet basic needs with legal remedies, which largely go unmet in<br />
low-income communities 4 , MLPs work together to eliminate barriers<br />
to both good health and effective healthcare delivery.<br />
Initial research and evaluation of the MLP model has been promising<br />
in several areas. Several longitudinal studies have shown MLP<br />
training to improve clinical work<strong>for</strong>ce skills, including increased<br />
resident knowledge of social disparities, community resources, and<br />
referral rates. 5-7 Others have demonstrated improved patient health<br />
and well-being, including improved medication adherence, reduced<br />
stress, and improved quality of life. 7-9 And finally, incorporation of<br />
legal services has shown to be financially sustainable (and in many<br />
cases revenue-generating) <strong>for</strong> participating institutions. 10-13<br />
In June of 2010, the Volunteer Legal Services Program (M-BARC)<br />
joined with St. Mary’s Medical Center in San Francisco to found a<br />
medical legal partnership at the Internal Medicine residents’ primary<br />
care clinic, the Sr. Mary Philippa Health Center (SMPHC).<br />
Legal Assistance<br />
Healthcare <br />
Shifting Paradigms in Healthcare and Law<br />
Prevailing Model<br />
• Service is crisis-driven<br />
• Individuals are responsible <strong>for</strong><br />
seeking legal assistance<br />
• Primary pursuit is justice<br />
• Adverse social condi1ons affect <br />
pa1ent health but are difficult to <br />
address <br />
• Healthcare team refers pa1ents to <br />
social worker/case manager <strong>for</strong> <br />
limited assistance <br />
• Advocacy skills are valued, taught and <br />
deployed inconsistently <br />
MLP Model<br />
• Service is preventive, focuses on<br />
early identification of and<br />
response to legal needs<br />
• Healthcare team works with<br />
patients to identify legal needs<br />
and makes referrals <strong>for</strong><br />
assistance<br />
• Aims include improved health<br />
and well-being<br />
• Adverse social condi1ons with legal <br />
remedies are iden1fied and <br />
addressed as part of care <br />
• Healthcare, social work and legal <br />
teams work together to address legal <br />
needs, improve health and change <br />
systems <br />
• Advocacy skills are priori1zed as part <br />
of the standard of care <br />
Figure 3. Referral Process Overview at Sister Mary Philippa Health Clinic.<br />
Results<br />
Since July 1, 2010 the MLP has provided legal assistance to over 140<br />
patients, addressing close to 300 separate legal issues in this time. While<br />
the range of assistance varies widely, the principle areas of legal need<br />
have proved to be housing rights, followed by income supports, family/<br />
personal stability issues, and legal issues (civil, criminal, and<br />
immigration). Over 60% of the patients served are disabled and 35% are<br />
over 60 years old. Remarkably, over 50% have ≥2 unmet legal needs,<br />
consistent with current data on legal disparities in low-income patients<br />
and families.<br />
Legal Needs at Resident Clinic<br />
Housing: 30%<br />
Income Supports: 28%<br />
Family/Personal Stability: 15%<br />
Legal Issues: 14%<br />
Employment: 6%<br />
Other: 7%<br />
Figure 4. Analysis of Legal Needs by Category at Sr. Mary Philippa Clinic from July 2010<br />
through present.<br />
Concurrent ef<strong>for</strong>ts have focused on the development and<br />
implementation of a resident/faculty education module on legal<br />
screening advocacy, accomplished through 1-on-1 attorney-resident<br />
training sessions, creation of advocacy code cards, and monthly case<br />
report conferences analyzing medical-legal barriers, interventions,<br />
and outcomes across our clinic patient population. The results have<br />
been an increase in the total number of referrals by nurses, social<br />
workers, and medical assistants, as well as an increase in the<br />
proportion of referrals from MDs (10 to 25%).<br />
Figure 5. Adapted from C. Kenyon, et al., “Revisiting the Social History <strong>for</strong> Child<br />
Health,” Pediatrics. 120(2007): e734-738. These authors adapted the I-HELP<br />
assessment tool.<br />
Conclusions<br />
MLPs have emerged as a trans<strong>for</strong>mative tool in medicine and law,<br />
empowering physicians and attorneys to directly address adverse social<br />
conditions and work preventively towards improved health and wellbeing.<br />
As oncoming governmental health care re<strong>for</strong>m expands access of<br />
vulnerable patients to medical homes and federal/state health insurance<br />
programs restructure reimbursement models on prevention and patient<br />
outcomes, MLPs may be the innovation necessary to deliver efficient,<br />
cost-effective, and genuinely comprehensive care to our communities.<br />
This year, the SMPHC MLP will undertake a research study that<br />
prospectively evaluates the impact of legal intervention(s) on global<br />
patient health; specifically, (1) objective health status (blood pressure,<br />
A1C, LDL), (2) healthcare utilization (preventive care visits, ER visits,<br />
hospitalizations), and (3) health status intermediates (perceived stress,<br />
subjective social status, and self-rated health).<br />
Bibliography<br />
1. WHO Commission on Social Determinants of Health. Closing the gap in a generation: health<br />
equity through action on the social determinants of health. Available at: http:/whqlibdoc.who.int/<br />
publications/2008/ 9789241563703_eng.pdf. Accessed October 15, 2012.<br />
2. Braveman, P., et al. Broadening the focus: the need to address the social determinants of health.<br />
American Journal of Preventive Medicine. 2011;40(1S1):S4 –S18.<br />
3. Zuckerman B, Sandel M, Lawton E, Morton S. Medical-legal partnerships: trans<strong>for</strong>ming health<br />
care. Lancet. 2008;372:1615–1617.<br />
4. Services Corporation. Documenting the justice gap in America, 2005. LSC.<br />
http://www.lsc.gov/justicegap.pdf. Accessed October 28, 2012.<br />
5. Klein, D., et al. Training in Social Determinants of Health in Primary Care: Does it Change<br />
Resident Behavior? Academic Pediatrics. 2011;11:387-393<br />
6. Cohen et al. Medical-Legal Partnership: Collaborating with Lawyers to Identify and Address<br />
Health Disparities. Journal of General Internal Medicine. 2010; 25(Suppl 2):136–9.<br />
7. Weintraub et al. Pilot Study of Medical-Legal Partnership to Address Social and Legal Needs of<br />
Patients. Journal of Health Care <strong>for</strong> the Poor and Underserved. 21(2010): 157-168.<br />
8. Zevon MA, et al. Medically-related legal needs and quality of life in cancer care: a structural<br />
analysis. Cancer. 2007;109:2600–2606.<br />
9. Fleishman SB, et al. The attorney as the newest member of the cancer treatment team. Journal of<br />
Clinical Oncology. 2006; 24:2123–2126.<br />
10. Teufel, et al. Process and impact evaluation of a legal assistance and health care community<br />
partnership. Health Promotions Practice. 2009(10):378-384.<br />
11. Rodabaugh, et al. A medical-legal partnership as a component of a palliative care model. Journal<br />
of Palliative Medicine. 2010;13(1):15-18.<br />
12. LegalHealth. Financial impact study of LegalHealth services to New York City hospitals .<br />
LegalHealth. Nov 2007. Available at: http://legalhealth.org/docs/lgh_financial_impac_study.pdf.<br />
13. MLP <strong>for</strong> Children. Health Care Recovery Dollars: A Sustainable Strategy <strong>for</strong> Medical-<br />
14. Edward, Paul, et al. Medical-Legal Partnerships: addressing competency needs through lawyers.<br />
Journal of Graduate Medical Education. Dec 2009: 304-309.<br />
Figure 2. Source: National Center <strong>for</strong> Medical-Legal Partnership. MLP Network [Internet].<br />
Boston (MA): http://www.medical-legalpartnership.org/mlp-model.<br />
www.postersession.com
<strong>Poster</strong> Number: 37<br />
<strong>Poster</strong> Title: The Next Step in Collaborative Care: Medical-Legal Partnerships<br />
Authors and Affiliate Institutions: Brandon Murguia, Nooshin Yashar, St. Mary’s Hospital and Medical Center<br />
Submitting Author<br />
Brandon R. Murguia, MD<br />
PGY 2 Resident<br />
Department of Internal Medicine<br />
St. Mary’s Hospital and Medical Center<br />
2250 Hayes Street<br />
Fourth Floor, Medical Education<br />
San Francisco, CA 94117<br />
Telephone: (415) 750-5955<br />
Email: Brandon.Murguia@dignityhealth.org<br />
Discussion of How the Problem was Identified and Explored: In response to continued health disparities in<br />
access to healthcare and health insurance, rising incidence and cost of chronic illnesses, and a growing body of<br />
evidence demonstrating the influence of social and environmental factors on health and well-being, Medical Legal<br />
Partnership (MLPs) are emerging as a new standard of care <strong>for</strong> low-income, vulnerable patient populations across<br />
the country. An MLP is a combined delivery model that brings together medical professionals and attorneys,<br />
integrating legal assistance into the primary care setting to address social determinants of health (including income<br />
and food security, housing, energy, employment/education, and personal stability).<br />
Description of the Innovation: In June of 2011, the Volunteer Legal Services Program (M-BARC) joined with St.<br />
Mary’s Medical Center in San Francisco to found a medical legal partnership at the Internal Medicine residents’<br />
primary clinic, the Sr. Mary Philippa Health Center (SMPHC).<br />
Results to Date: Since then, the MLP has provided legal assistance to over 200 patients, addressing over 150 legal<br />
issues in this time. The principle areas of legal need over this time have proved to be housing rights, disability<br />
income benefits, employment issues, family law, and health insurance issues. Over 60% of the patients served are<br />
disabled and 35% are over 60 years old. Remarkably, over 70% have ≥2 unmet legal needs, consistent with current<br />
data on legal disparities in low-income patients and families. Concurrent ef<strong>for</strong>ts have focused on the development<br />
and implementation of a resident/faculty education module on legal screening advocacy, accomplished through<br />
attorney-resident training sessions and monthly case report conferences analyzing medical-legal barriers,<br />
interventions, and outcomes across our patient population. The results have been an increase in total number of<br />
referrals by healthcare professionals, as well as an increase in the proportion of referrals from MDs (10 to 30%).<br />
Discussion/Reflection/Lessons Learned: MLPs have emerged as a trans<strong>for</strong>mative tool in medicine and law,<br />
empowering physicians and attorneys to directly confront adverse social conditions and work preventively towards<br />
improved health and well-being. This year, our MLP is undertaking a research study that prospectively evaluates<br />
the impact of legal intervention(s) on global patient health; specifically, (1) objective health status (blood pressure,<br />
A1C, LDL), (2) healthcare utilization (preventive care visits, ER visits, hospitalizations), and (3) health status<br />
intermediates (perceived stress, subjective social status, and self-rated health).<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 38
<strong>Poster</strong> Number: 38<br />
<strong>Poster</strong> Title: Improving Resident Documentation: Coding and Billing Practices with a Practical Tutorial<br />
Authors and Affiliate Institutions: Moyna H Ng, Lenox Hill Hospital<br />
Submitting Author<br />
Moyna H. Ng, MD<br />
Associate Program Director<br />
Department of General Internal Medicine<br />
Lenox Hill Hospital<br />
100 East 77th Street<br />
New York, NY 10075<br />
Telephone: (212) 434-4849<br />
Email: mng3@nshs.edu<br />
Discussion of How the Problem was Identified and Explored: While Internal Medicine residents undergo<br />
rigorous clinical training, they rarely participate in any structured learning in medical coding and billing. There is<br />
cursory exposure in the ambulatory care setting. However, in the inpatient setting, residents have minimal<br />
knowledge regarding proper medical coding, billing and adequate supporting documentation. Since these skills are<br />
essential once they become practicing attending physicians, an innovative tutorial was developed and incorporated<br />
into the Medical Consultation rotation targeted at the PGY-3 trainees.<br />
Description of the Innovation: During a two week rotation on Medical Consultation, a PGY-3 resident works<br />
with an academic hospitalist and they are charged with coding and billing each patient encounter on mock billing<br />
cards. The tutorial is divided into four phases. Phase One – the resident codes and bills each patient visit without<br />
any aide. Phase Two – the resident is given a reading packet consisting of two articles on documentation, coding<br />
and billing, a hospitalist progress note template, a hospital pocket pamphlet on coding and billing and a one page<br />
reference guide published by CMS. Phase Three –the resident meets with the academic hospitalist to review each<br />
mock billing card and the corresponding documentation (initial consultation or follow up progress note) <strong>for</strong><br />
appropriate Evaluation & Management coding and level of service billing. Phase Four – the resident continues to<br />
code and bill patient encounters and a final review is per<strong>for</strong>med at the end of the rotation. A pre- and post-rotation<br />
survey based on a Likert scale assessing the resident’s knowledge, confidence and ability to teach documentation,<br />
coding and billing is given on the first and last day of the rotation, respectively.<br />
Results to Date: Results to date reveal a statistically significant trend towards improvement in knowledge,<br />
confidence and ability to teach the fundamentals of medical coding and billing with accurate supportive<br />
documentation. Residents were highly satisfied with this short and effective tutorial.<br />
Discussion/Reflection/Lessons Learned: It also incorporates the Systems Based Practice competency to teach<br />
residents to work effectively in various health care delivery settings. It can be easily imbedded in a variety of two<br />
or four week rotations during academic training with recruitment of a few faculty members.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 39
Ambulatory Clinician‐Education Rotation <strong>for</strong> Primary Care Residents<br />
Kerri Palamara, MD; Valerie E Stone, MD, MPH<br />
Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts<br />
Statement of the Problem <br />
Results <br />
Rotation Components <br />
<br />
<br />
<br />
<br />
ACGME requirements that 1/3 of all residents’ time be spent<br />
in ambulatory setting led to fewer differences in the training<br />
experience of MGH primary care and categorical residents.<br />
Primary care residents expressed a need to better develop<br />
their teaching skills.<br />
Coincidentally, the proportion of MGH’s primary care<br />
residents entering careers in primary care internal medicine<br />
was rising.<br />
This presented an opportunity to innovate and develop<br />
experiences to better prepare primary care residents <strong>for</strong> the<br />
careers they were entering<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
Change in Teaching Abilities<br />
‣Prepare and deliver ambulatory didactic curricular talks –small group, large<br />
group, and case‐based<br />
‣Select useful ambulatory teaching cases and apply them to varied teaching<br />
environments<br />
‣Participate fully in mentored precepting experiences<br />
‣Review Ambulatory Clinician Educator curriculum and apply knowledge to<br />
talk preparation<br />
‣Meet with rotation mentor weekly to discuss progress, plan <strong>for</strong> upcoming<br />
talks, navigate challenges<br />
Findings to Date <br />
Objectives of Innovation <br />
Expose primary care senior residents to the knowledge and<br />
skills necessary <strong>for</strong> competent practice as an ambulatory<br />
clinician educator.<br />
Provide an opportunity and setting <strong>for</strong> direct observation of<br />
teaching skills with specific feedback <strong>for</strong> development.<br />
Description of Innovation <br />
Ambulatory Training Structure at MGH:<br />
‣ Regular continuity clinic sessions scheduled through the<br />
academic year.<br />
‣ 3 months of ambulatory block scheduled in each trimester<br />
‣2 weeks Ambulatory Subspecialty Rotation, 2 weeks<br />
Ambulatory Care Rotation<br />
PC Senior Residents –4 months of ambulatory; 1 month as<br />
designer block, 1 month as Ambulatory Teaching Senior<br />
Four week rotation coordinated by APD.<br />
Scheduled time <strong>for</strong> preparation, teaching, continuity clinic, and<br />
shadowed and mentored precepting.<br />
Ambulatory educational activities in didactic and clinical<br />
settings:<br />
‣ Large and small group didactics<br />
‣ Precepting<br />
‣ Case‐based teaching<br />
0%<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
Create positive<br />
learning<br />
environment<br />
Curriculum<br />
helpful<br />
Modify<br />
teaching to<br />
learners needs<br />
SGT<br />
exercise<br />
useful<br />
Use OMP<br />
Model<br />
LGT<br />
exercise<br />
useful<br />
Prepare<br />
focused<br />
presentation<br />
on essential<br />
teaching points<br />
Prepare AV<br />
materials to<br />
enhance<br />
presentation<br />
Use engaging<br />
delivery style<br />
Encourage<br />
audience<br />
participation<br />
No change Some Improvement Large Improvement<br />
Satisfaction with Curricular Components<br />
Preceptor<br />
shadow ing<br />
useful<br />
Agree<br />
Mentored<br />
precepting<br />
useful<br />
Running<br />
Ambulatory<br />
Intern<br />
Report<br />
useful<br />
Strongly Agree<br />
Morning<br />
report<br />
exercise<br />
useful<br />
<strong>Meeting</strong> w ith<br />
mentor<br />
useful<br />
Apply Feel<br />
facilitation com<strong>for</strong>table<br />
techniques to w ith silence<br />
improve small w hen teaching<br />
group<br />
dynamics<br />
Prep time<br />
adequate<br />
OMP = One Minute Preceptor; LGT = Large group talk SGT = Small Group Talk<br />
Good<br />
addition to<br />
the Primary<br />
Care<br />
Program<br />
All 9 primary care senior residents surveyed – 100% completion.<br />
Varied curricular components were uni<strong>for</strong>mly well received and residents<br />
all reported change in teaching behaviors.<br />
100% strongly agreed that the rotation was a good addition to primary care<br />
program.<br />
Participating supervising faculty increased from 9 to 16 in year 2.<br />
In Year 2, residents asking <strong>for</strong> additional shadowing and precepting<br />
experiences.<br />
Survey comments:<br />
“Great training <strong>for</strong> becoming an ambulatory preceptor/educator and fills<br />
a void in our curriculum.”<br />
“I appreciated trying out different teaching modalities and expanding<br />
skills.”<br />
Key Lessons Learned <br />
Based upon our experience,<br />
‣With dedicated ambulatory clinician educators and faculty supervision,<br />
residency programs can incorporate an Ambulatory Clinician Educator<br />
Rotation <strong>for</strong> residents<br />
‣A four week dedicated teaching rotation is academically valuable, allows<br />
residents to improve upon their teaching skills, and develop greater<br />
confidence in their teaching style.
<strong>Poster</strong> Number: 39<br />
<strong>Poster</strong> Title: Ambulatory Clinician-Educator Rotation <strong>for</strong> Primary Care Residents<br />
Authors and Affiliate Institutions: Kerri Palamara, Valerie Stone, Harvard Medical School Massachusetts<br />
General Hospital<br />
Submitting Author<br />
Kerri L. Palamara, MD<br />
Associate Program Director<br />
Division of General Internal Medicine<br />
Department of Medicine<br />
Harvard Medical School Massachusetts General Hospital<br />
55 Fruit Street<br />
Boston, MA 02114<br />
Telephone: (857) 383-8172<br />
Email: kpalamara@partners.org<br />
Discussion of How the Problem was Identified and Explored: The ACGME requirement that one-third of<br />
residents’ time be spent in the ambulatory setting led to fewer differences in the training experiences of primary<br />
care residents compared to categorical residents at Massachusetts General Hospital. Additionally, the proportion<br />
of MGH’s primary care residents entering careers in primary care internal medicine was rising. This presented an<br />
opportunity to innovate and develop experiences <strong>for</strong> primary care residents to better prepare them <strong>for</strong> primary care<br />
internal medicine careers. Our residents expressed a need to better develop their teaching skills, and there<strong>for</strong>e, the<br />
Ambulatory Teaching Senior Rotation was created.<br />
Description of the Innovation: In this 4 week rotation, primary care senior residents participate in ambulatory<br />
educational activities in both the didactic and clinical settings. The goal of the rotation is to expose primary care<br />
senior residents to the knowledge and skills necessary <strong>for</strong> competent practice as an ambulatory clinician educator.<br />
Activities include large and small group observed teaching, preceptor observation, mentored precepting, career<br />
focused discussions with faculty mentors, observed case-based teaching, and their own continuity clinic 3-4<br />
sessions per week. They are expected to prepare and deliver ambulatory didactic curriculum lectures, select useful<br />
ambulatory teaching cases and apply them to large and small group teaching sessions, and participate fully in<br />
resident precepting sessions.<br />
Results to Date: All nine of the primary care senior residents were anonymously surveyed after they had all<br />
completed the rotation. 100% agreed that the Ambulatory Teaching Senior Rotation was a welcome addition to the<br />
program. 100% reported at least some improvement in their ability to facilitate a small group discussion, encourage<br />
audience participation, prepare a presentation with focused teaching points, modify their teaching to fit the learners’<br />
needs, and use an engaging delivery style. 100% of residents agreed that the opportunities to deliver a small group<br />
talk, PowerPoint talk, be observed precepting, and meet regularly with a faculty mentor throughout the rotation<br />
were useful.<br />
Discussion/Reflection/Lessons Learned: With dedicated ambulatory clinician educators and faculty supervision,<br />
residency programs can incorporate an Ambulatory Clinician Educator Rotation <strong>for</strong> residents. A four week<br />
dedicated ambulatory teaching rotation allows residents to improve upon their teaching skills and develop greater<br />
confidence in their teaching style.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 40
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
16<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
Less Sinking and More Swimming: Resident Primary Care Immersion Blocks<br />
Kerri Palamara, MD; Alaka Ray, MD; Blair Fosburgh, MD; Valerie E Stone, MD, MPH<br />
Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts<br />
<br />
<br />
<br />
<br />
Statement of the Problem <br />
The demand <strong>for</strong> primary care physicians is rising, but fewer trainees are<br />
entering the primary care work<strong>for</strong>ce.<br />
Based on our end‐of‐year resident survey, graduating residents feel<br />
unprepared <strong>for</strong> careers in primary care.<br />
Work hour regulations have led to longer gaps between continuity clinic<br />
sessions and increased inpatient demands.<br />
Without a regular clinic experience, residents are unable to gain an indepth<br />
understanding of resources available to their patients and the<br />
rewards of a primary care career.<br />
Immersion Block Experiences:<br />
Continuity Clinic (3 sessions weekly; 6 total)<br />
1:1 time with preceptor (discuss feedback, high‐risk patients, billing, clinic<br />
procedures)<br />
Shadow preceptor clinic session<br />
1:1 time with practice RN<br />
Shadow clinic‐based Diabetes NP<br />
Panel Management session<br />
1:1 time with EMR specialist<br />
Practice Reorientation<br />
Begin a Practice‐Based Improvement Project<br />
EBM review of a clinic‐generated question<br />
Report back to group on chosen project and EBM review<br />
Objectives of Innovation <br />
Abillity to Use EMR<br />
Findings to Date <br />
Increase resident com<strong>for</strong>t level in care of ambulatory patients<br />
Rein<strong>for</strong>ce principles of team‐based care<br />
Expose residents to positive role models in primary care<br />
Increase resident satisfaction with their continuity clinic<br />
Increase resident preparedness <strong>for</strong> careers in primary care<br />
Description of Innovation <br />
Resident population: All primary care and categorical residents graduating in<br />
2014<br />
Typical ambulatory training structure at MGH:<br />
Regular continuity clinic sessions scheduled through the academic year<br />
3 months of ambulatory block scheduled in each trimester of year –2<br />
weeks ambulatory subspecialty experience, 2 weeks Ambulatory Care<br />
Rotation<br />
Residents in 2 major teaching practices were assigned a Primary Care<br />
Immersion Block (IB) during one regularly scheduled Ambulatory Care<br />
Rotation.<br />
Experiences were focused on Practice‐based Learning & Improvement and<br />
Systems Based Practice competencies.<br />
Voluntary survey data was collected from all participating residents mid‐year<br />
(prior to IB) and at the end of each year of training.<br />
Surveys evaluated their views towards their continuity clinic, primary care,<br />
and the likelihood that they would enter a career in general medicine.<br />
Poor Fair Good Very Good Excellent<br />
IB res Pre IB res Post nonIB res Pre nonIB res Post<br />
Likelihood of Asking MA or RN Help<br />
Very Unlikely Unlikely Unsure Likely Very Likely<br />
IB res Pre IB res Post nonIB res Pre nonIB res Post<br />
How Effective Do You Think You Are At<br />
Providing Primary Care <strong>for</strong> Your Patients<br />
78% of residents agreed that the Primary Care Immersion Block was a useful<br />
educational experience.<br />
Residents in Immersion Block practices felt more supported by their clinic staff<br />
than residents in non‐IB practices, demonstrated by increased likelihood of asking<br />
<strong>for</strong> help from MAs, RNs, and Patient Care Coordinators.<br />
There was a trend towards improved effectiveness at providing primary care <strong>for</strong><br />
their patients in all residents, regardless of whether they were in an Immersion<br />
Block practice or not.<br />
Key Lessons Learned <br />
Based upon our experience, Resident Primary Care Immersion Blocks:<br />
‣ Expose residents to what a career in primary care would look like<br />
‣ Increase resident com<strong>for</strong>t level in their primary care practice<br />
‣ Increase resident satisfaction with their continuity clinic experience<br />
‣ Are generalizable to other institutions looking to improve the resident continuity<br />
clinic experience<br />
‣Additionally, the overall trend amongst all residents toward improved<br />
effectiveness at providing primary care <strong>for</strong> their patients suggests that regular<br />
continuity clinic throughout the year and focused ambulatory care rotations are<br />
sufficient, and Immersion Blocks can only enhance that experience.<br />
Ineffective<br />
Somewhat<br />
Ineffective<br />
Neither Somewhat Effective Effective<br />
Pre<br />
Post
<strong>Poster</strong> Number: 40<br />
<strong>Poster</strong> Title: Less Sinking and More Swimming: Resident Primary Care Immersion Blocks<br />
Authors and Affiliate Institutions: Kerri Palamara, Alaka Ray, Harvard Medical School Massachusetts General<br />
Hospital<br />
Submitting Author<br />
Kerri L. Palamara, MD<br />
Associate Program Director<br />
Division of General Internal Medicine<br />
Department of Medicine<br />
Harvard Medical School Massachusetts General Hospital<br />
15 Parkman Street<br />
WACC 535<br />
Boston, MA 02114<br />
Telephone: (857) 383-8172<br />
Email: kpalamara@partners.org<br />
Discussion of How the Problem was Identified and Explored: The demand <strong>for</strong> primary care physicians is rising<br />
yet fewer trainees are choosing primary care careers. The ACGME work hour regulations complicate this issue due<br />
to longer gaps between continuity clinic sessions and increased inpatient work demands. When residents are not in<br />
clinic regularly, they are unable to gain an in depth understanding of the resources available to them and their<br />
patients.<br />
Description of the Innovation: The objectives were to increase resident com<strong>for</strong>t level in outpatient practice,<br />
rein<strong>for</strong>ce the principles of team-based care and expose residents to what a real career in primary care might look<br />
like. We designed Primary Care Immersion Blocks focused on Practice-based Learning & Improvement and<br />
Systems Based Practice. All residents from the intern class of 2011-12 with clinics in the 2 major teaching practices<br />
were assigned an Immersion Block during one of their regularly scheduled ambulatory blocks. Immersion Block<br />
(IB) experiences include 1:1 time and shadowing with their preceptor and the diabetes nurse practitioner, panel<br />
management time, 1:1 time with the EMR specialist, practice reorientation, time <strong>for</strong> a practice-based improvement<br />
project, and time to review data behind a clinic-generated question (EBM time). Voluntary survey data was<br />
collected from all residents from the intern class of 2011-12 at mid-year and the end of each year of training to<br />
evaluate their views towards continuity clinic, primary care, and the likelihood that they would enter a career in<br />
primary care.<br />
Results to Date: Seventy-six percent of residents surveyed agreed that Immersion Blocks were useful. Residents<br />
in IB practices reported feeling more supported by their clinic staff than residents in non-IB practices. There was a<br />
trend amongst all residents, regardless of IB participation, toward improved effectiveness at providing primary care<br />
<strong>for</strong> their patients.<br />
Discussion/Reflection/Lessons Learned: Resident Ambulatory Immersion Blocks increase resident com<strong>for</strong>t level<br />
in their practice and satisfaction in their continuity clinics. Immersion Blocks are generalizable to other institutions<br />
looking to improve the resident continuity clinic experience.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 41
<strong>Poster</strong> Number: 41<br />
<strong>Poster</strong> Title: Training Residents <strong>for</strong> Independent Inpatient Practice (TRIIP): Ongoing Development of a Novel<br />
Clinical Rotation Using PDCA and Milestones to Improve Education in Hospital Medicine<br />
Authors and Affiliate Institutions: David Paje, Peter Watson, Charles Coffey, Clif<strong>for</strong>d Kaye, James Jeffries,<br />
Gregory Buran, Peter Luyeho, Errol Zimmerman, Henry Ford Hospital; Kelly Caverzagie, University of Nebraska<br />
Medical Center<br />
Submitting Author<br />
David Paje, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
Henry Ford Hospital<br />
2799 West Grand Boulevard, CFP-4<br />
Detroit, MI 48374<br />
Telephone: (313) 916-8144<br />
Email: DPAJE1@hfhs.org<br />
Discussion of How the Problem was Identified and Explored: Evaluation of resident per<strong>for</strong>mance on predefined<br />
competencies while delivering inpatient clinical care has historically been difficult. We developed a novel<br />
clinical rotation incorporating new educational and assessment strategies providing residents intense hospital<br />
medicine training and significant autonomy.<br />
Description of the Innovation: In July 2011, the Training Residents <strong>for</strong> Independent Inpatient Practice (TRIIP)<br />
Rotation was established to prepare PGY-2/3 residents <strong>for</strong> unsupervised hospital medicine practice and allow<br />
faculty to assess their demonstration of high-level integrative skills required of an independently practicing<br />
physician. TRIIP is intended to provide an “academic stress test” and assess progression towards unsupervised<br />
practice. The core of the program is an inpatient preceptor model pairing individual residents with a hospital<br />
medicine faculty cycling through several different roles (primary inpatient provider and medical consultant).<br />
During its implementation, we have utilized a continuous PDCA cycle of resident, faculty and nursing feedback to<br />
enhance the clinical and learning experience.<br />
Results to Date: Over 60 internal medicine residents have been trained. Overall resident assessment of teaching<br />
was 4.15/5 and curriculum 3.80/5. Resident feedback emphasized several strengths (availability of faculty,<br />
increased resident autonomy/independence, improved resident efficiency, and clinical decision making<br />
development) and opportunities <strong>for</strong> improvement (difficult block scheduling, more didactic teaching, variability in<br />
peer resident per<strong>for</strong>mance on small team). This feedback led to further stratification of the rotation into a Level I<br />
(PGY-2 inpatient rounder focus) and Level II (PGY-3 inpatient medical consultant focus) that is linked throughout<br />
the month.<br />
Discussion/Reflection/Lessons Learned: This new rotation met the core goals of increasing resident<br />
independence and per<strong>for</strong>mance on specific clinical activities as judged by faculty, although this experience was<br />
viewed differently depending on the trainee. Without interns or students, residents provide direct clinical care and<br />
are evaluated in a “real-world” clinical environment. The use of “micro-geography” on a geographic clinical unit<br />
allowed residents to work in interdisciplinary teams and <strong>for</strong> direct observation of resident teamwork skills. Faculty<br />
working as one-on-one clinical coaches with a resident allows <strong>for</strong> an in-depth behavioral-based evaluation of the<br />
integrated skills required of the unsupervised physician. Finally, focusing on clinical rotation improvement with<br />
the same rigor as clinical process improvement was an intense faculty development exercise.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 42
<strong>Poster</strong> Number: 42<br />
<strong>Poster</strong> Title: Remediating Residents in Transition: Individualizing the Learner-Manager-Teacher Model<br />
Authors and Affiliate Institutions: Anne Pereira, David Hilden, Sam Ives, Hennepin County Medical Center<br />
Submitting Author<br />
Anne G. Pereira, MD<br />
Associate Professor<br />
Division of Medical Education<br />
Department of Internal Medicine<br />
Hennepin County Medical Center<br />
G5<br />
701 Park Avenue<br />
Minneapolis, MN 55415<br />
Telephone: (612) 873-2691<br />
Email: anne.pereira@hcmed.org<br />
Discussion of How the Problem was Identified and Explored: The educational model <strong>for</strong> PGY-1 to PGY-2<br />
transition places high demand on the new PGY-2 in the inpatient setting: in addition to responsibility <strong>for</strong> an<br />
increased number of patients, PGY-2s must lead interprofessional teams and teach students and interns. Often, this<br />
is the new PGY-2’s first substantial professional leadership role. The majority of our trainees are able to make this<br />
transition with time-limited training in preparation <strong>for</strong> their new role. However, we recognized that the PGY-1s<br />
who struggled to obtain mastery at their level of training were substantially more challenged in this transition.<br />
While faculty could ensure that patients were safe with the struggling new PGY-2’s, their lack of leadership and<br />
peer teaching led to suboptimal experience <strong>for</strong> their interns and students.<br />
Description of the Innovation: Since 2006, we have modified the PGY-1 to PGY-2 transition <strong>for</strong> interns<br />
identified by the clinical competence committee as at risk (typically by February of the PGY-1 year) <strong>for</strong><br />
unsuccessful transition. In the first two months of their PGY-2 year, they work exclusively with our academic<br />
hospitalists to manage patients independently, separate from housestaff teams, in a modified approach to the<br />
Baystate “Learner-Manager-Teacher” model. Goals of remediation are developed collaboratively with the resident,<br />
the program director and the director of the hospitalist division and shared with the teaching hospitalist(s).<br />
Biweekly meetings review progress and identify outstanding goals. Upon completion of the remediation months, if<br />
goals have been met, the resident is integrated into the standard PGY-2 year.<br />
Results to Date: Since 2006, eight of 130 (6%) residents have been required to complete our remedial pathway,<br />
with a range of zero to two residents per year. Five of the eight residents have graduated on time, having made a<br />
successful integration into the standard program. Of the graduates, 4 have been board certified (one delayed<br />
examination), 2 entered subspecialty training programs and 3 are in community practice.<br />
Discussion/Reflection/Lessons Learned: While most trainees are able to successfully transition from intern to<br />
supervising resident, struggling trainees are able to build skills in an individualized academic hospitalist experience.<br />
With this experience, they are able to successfully transition to team leadership and intern/student supervision.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 43
<strong>Poster</strong> Number: 43<br />
<strong>Poster</strong> Title: Training Homework: Does a Structured Reading and Testing Program Improve Per<strong>for</strong>mance on the<br />
ABIM In-Training Exam?<br />
Authors and Affiliate Institutions: Seth Politano, Eric Hseih, Keck School of Medicine at the University of<br />
Southern Cali<strong>for</strong>nia<br />
Submitting Author<br />
Seth Politano, DO<br />
Associate Program Director<br />
Department of Geriatric, Hospitalist, Palliative, and General Internal Medicine<br />
Keck School of Medicine at the University of Southern Cali<strong>for</strong>nia<br />
1200 North State Street<br />
IRD 637<br />
Los Angeles, CA 90089<br />
Telephone: (323) 226-6571<br />
Email: politano@usc.edu<br />
Discussion of How the Problem was Identified and Explored: Internal Medicine residency programs use the<br />
American Board of Internal Medicine (ABIM) In-Training examination (ITE) to assess the per<strong>for</strong>mance of their<br />
trainees. Both Program Directors and Residents use the in<strong>for</strong>mation from the examination to target deficient areas<br />
of medical knowledge. In addition, programs can gauge the results of the ITE to target residents that have a high<br />
likelihood of not passing the initial internal medicine certification examination (i.e. the “boards”). Our Internal<br />
Medicine Program has noticed that residents were not progressing in their knowledge levels after advancing each<br />
year as demonstrated by results on the in-training examination. There<strong>for</strong>e, our program initiated a structured<br />
curriculum/reading program to target weak areas. Our goal was to see if this learning program did indeed improve<br />
per<strong>for</strong>mance on the ITE, with an eventual goal towards improvement on the boards.<br />
Description of the Innovation: Study modules were created by the authors in each of the content areas specified<br />
by the ABIM (i.e. Cardiology, Neurology, Geriatrics, etc.). The packets are based on specific content area as set<br />
<strong>for</strong>th by the ABIM using the Medical Knowledge Self-Assessment program (MKSAP), Medstudy, and internet<br />
resources as a guide. Each packet contains open-ended questions <strong>for</strong> residents to study. At the end of the month,<br />
the resident was required to take a written quiz based on content in the packet and required a score of at least 70%<br />
to pass the module. Data was collected regarding who had completed a module, and results were compiled until the<br />
ITE in October 2011.<br />
Results to Date: There was a significant increase in ITE scores in those subjects in which residents completed the<br />
learning module and quiz compared to those in which no module and quiz was completed.<br />
Discussion/Reflection/Lessons Learned: Our core curriculum reading program increases per<strong>for</strong>mance on the<br />
ABIM ITE. Perhaps by requiring residents to read monthly, and assessing the knowledge gained by administering<br />
a quiz, we are simply en<strong>for</strong>cing good study habits. The use of the program will hopefully increase board pass rates,<br />
and a similar structured learning program can be used by other training program to improve medical knowledge.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 44
<strong>Poster</strong> Number: 44<br />
<strong>Poster</strong> Title: “Intern Boot Camp:” Case-Based Interactive Curriculum <strong>for</strong> the New Intern<br />
Authors and Affiliate Institutions: Patrick A Rendon, Mark E Garcia, Marc T Montanaro, University of New<br />
Mexico School of Medicine<br />
Submitting Author<br />
Patrick A. Rendon, MD<br />
Chief Resident<br />
Department of Internal Medicine<br />
University of New Mexico School of Medicine<br />
2211 Lomas Boulevard, NE<br />
Albuquerque, NM 87120<br />
Telephone: (505) 264-3217<br />
Email: prendon@salud.unm.edu<br />
Discussion of How the Problem was Identified and Explored: New interns starting in July have often gone<br />
several months without any clinical duties or patient care, often leaving them underprepared <strong>for</strong> the rigors of their<br />
internship. The controversial so-called “July effect” has been extensively documented in the past and provides an<br />
excellent opportunity <strong>for</strong> systems improvement and education.<br />
Description of the Innovation: In the Department of Internal Medicine at the University of New Mexico, the<br />
Chief Residents have developed a curriculum <strong>for</strong> interns the first 2 months of their internship called “Intern Boot<br />
Camp”. This hour-long weekly curriculum focuses on the day-to-day skills necessary <strong>for</strong> a functioning intern and<br />
is run in small group sessions led by upper level residents and fellows with assistance from the Chief Residents.<br />
Cases were developed by the Chief Residents and fellows to educate interns in the following areas: Cross-cover,<br />
EKGs, Chest X-rays, common complications on wards, common medicine admissions, sepsis, and empiric<br />
antibiotics.<br />
Results to Date: The interns were surveyed regarding these sessions using a 1-7 Likert scale rating their abilities in<br />
these areas be<strong>for</strong>e and after the session and we found a net gain on average of 1.5 points (preliminary data) on the<br />
scale. The greatest level of improvement was found in the area of crosscovering (preliminary data). Although not<br />
<strong>for</strong>mally surveyed, anecdotally the upper level residents who ran the small groups also found these sessions to be of<br />
high educational value.<br />
Discussion/Reflection/Lessons Learned: In summary, this innovative resident-led case-based small group<br />
curriculum <strong>for</strong> the starting intern helps improve interns’ skills in diagnosis and management of common problems<br />
encountered early in their internship. This may be an area <strong>for</strong> further inquiry into patient safety effects of this<br />
curriculum and the “July Effect.”<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 45
<strong>Poster</strong> Number: 45<br />
<strong>Poster</strong> Title: Hospital Practice Profiles: Improving Training by Linking Patient Outcomes to Resident Practice<br />
Authors and Affiliate Institutions: Julius Yang, Anjala Tess, C Christopher Smith, Sarah Moravick, Eileen E<br />
Reynolds, Harvard Medical School Beth Israel Deaconess Medical Center<br />
Submitting Author<br />
Eileen E. Reynolds, MD<br />
Program Director<br />
Department of Internal Medicine<br />
Harvard Medical School Beth Israel Deaconess Medical Center<br />
330 Brookline Avenue<br />
Boston, MA 02215<br />
Telephone: (617) 632-8264<br />
Email: ereynold@bidmc.harvard.edu<br />
Discussion of How the Problem was Identified and Explored: Study Aim: To design, implement, and assess the<br />
potential utility of trainee-specific “hospital practice profiles” in a structured self-assessment and improvement<br />
program to promote resident competency in the domains of patient care, problem-based learning improvement, and<br />
systems-based care.<br />
Description of the Innovation: Methods: Hospital practice profiles were created <strong>for</strong> each PGY-1 intern in the<br />
Department of Medicine, based on each intern’s authored discharge summaries. Each profile contains data<br />
including patient names, principal diagnosis, attending MD, discharge floor and division, PCP MD and practice,<br />
insurance, principal diagnosis at discharge, discharge date, discharge hour, length of stay, number of medications at<br />
discharge, 30-day readmission outcomes, and patient satisfaction survey results. A faculty member met with<br />
interns in small groups (approximately 6-8 interns) to introduce the data available in the profiles, then assigned<br />
three structured reviews <strong>for</strong> each intern to per<strong>for</strong>m based on his/her own data: a 30-day readmission review, a<br />
chronic disease management review, and a patient experience review. The small group re-convened with the<br />
faculty member one week later to share discussion and findings based on their reviews. A post-intervention survey<br />
was administered at the end of the second meeting to assess educational impact.<br />
Results to Date: Results: 54/58 (93%) interns completed the survey. For each of the following statements, the<br />
proportion of respondents who either agreed or strongly agreed were as follows: “I learned something about my<br />
practice that I didn’t previously know/understand”: (50/54, 93%); “I generated questions about my practice that I<br />
didn’t previously have”: (48/54, 89%); “I learned something about the health care system that I didn’t previously<br />
know/understand”: (45/54, 83%); “I generated questions about the health care system that I didn’t previously<br />
have”: (50/54, 93%); “I anticipate that my future practice will change as a result of this experience”: (44/54, 81%);<br />
“I found this experience valuable, would recommend to future interns”: (53/54, 98%); “I found this experience<br />
valuable, would recommend I should repeat this in subsequent years of training”(50/54, 93%).<br />
Discussion/Reflection/Lessons Learned: Conclusions: A structured self-reflection program based on reported<br />
patient outcomes, including patient experience survey data, can promote self-assessed learning in the domains of<br />
patient care, problem-based learning improvement, and systems-based practice.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 46
Educational Competition to Improve Resident Experience<br />
Heather Sand, Varaz Bozoghlanian, Lloyd Rucker<br />
University of Cali<strong>for</strong>nia, Irvine, Department of Medicine<br />
Introduction<br />
Internal medicine is the largest, most diverse specialty in the United States. 1<br />
At our acute care academic medical center, residents provide care <strong>for</strong> diverse<br />
patients with challenging diagnoses and management. Residents are<br />
expected to assume personal responsibility <strong>for</strong> the care of individual patients<br />
in order to develop the skills, knowledge, and attitudes necessary <strong>for</strong><br />
proficiency as an internist. 2 However, great teaching cases are often not<br />
widely discussed across teams in the hub-bub of busy days restricted by duty<br />
hours and limited teaching interactions across teams. We wanted to identify<br />
great cases with important learning points, but residents often were<br />
reluctant to bring these cases <strong>for</strong>ward, and morning case conferences could<br />
not accommodate all the cases. We sought to create an entertaining and<br />
thoughtful conference to incentivize residents to present their great cases:<br />
Best Case of the Block.<br />
Innovation<br />
The “Best Case of the Block” contest challenges each of our six ward teams to<br />
identify and present their best case of the current ward block.<br />
Teams<br />
Select<br />
Cases<br />
Teams<br />
Present<br />
Cases<br />
Vote<br />
FIGURE 1. Process of preparing and hosting Best Case of the Block.<br />
Prize<br />
In the days leading up to competition, teams select their best case (Figure 1).<br />
Teams prepare a 5-minute presentation, often using handouts, slides, and<br />
skits. The day be<strong>for</strong>e competition, each team must submit their slides and a<br />
brief <strong>for</strong>m outlining in<strong>for</strong>mation such as the diagnosis and teaching points.<br />
The competition is held during a thirty minute morning report at the end of<br />
the rotation. Students, residents, and faculty vote <strong>for</strong> the best case with<br />
points based equally in 3 categories: uniqueness of the case, importance of<br />
the learning issue, and quality and innovation of the presentation (Figure 2).<br />
The team’s attending must be present <strong>for</strong> a team to win in order to allow <strong>for</strong><br />
additional case discussion as needed. The team with the highest overall score<br />
wins Best Case of the Block. The residency program pays <strong>for</strong> a team lunch <strong>for</strong><br />
the team with the best overall presentation.<br />
Team<br />
Uniqueness &<br />
Interest of<br />
Diagnosis<br />
Importance of<br />
Learning Issues<br />
Quality & Style of<br />
Presentation<br />
Total Score<br />
A 12 3 4 5 12 3 4 5 12 3 4 5<br />
B 12 3 4 5 12 3 4 5 12 3 4 5<br />
C 12 3 4 5 12 3 4 5 12 3 4 5<br />
D 12 3 4 5 12 3 4 5 12 3 4 5<br />
E 12 3 4 5 12 3 4 5 12 3 4 5<br />
G 12 3 4 5 12 3 4 5 12 3 4 5<br />
FIGURE 2. Score sheet to be completed by voting medical students, residents, attending phyicians.<br />
Results<br />
To date, 16 competitions have showcased 89 cases. Cases have covered a breadth<br />
of medicine specialties and pathologies (Figure 3). Teaching points have also<br />
varied from clinically rare pathology to how to approach diagnostic data.<br />
Cardiology<br />
• HOCM<br />
• HACEK Endocarditis with<br />
septic emboli<br />
• Methamphetamine<br />
cardiomyopathy &<br />
withdrawal<br />
• Syncope 2/2 metastatic<br />
pericardial effusion with<br />
impending tamponade<br />
Pulmonology<br />
• Aspergillus necrotizing<br />
pneumonia<br />
• Bilateral PE<br />
• Hiccups secondary to<br />
lung cancer<br />
• Active TB<br />
• TACO vs. TRALI<br />
• Portopulmonary HTN<br />
Gastroenterology<br />
• Metastatic liver<br />
adenocarcinoma with<br />
cavernous sinus<br />
involvement<br />
• Biloma following<br />
cholecystectomy<br />
• Lynch syndrome<br />
• Ischemic pancreatitis<br />
• Autoimmune<br />
pancreatitis and necrotic<br />
mucocele presenting as<br />
"Rectal mass”<br />
Endocrinology<br />
• Myxedema coma<br />
• Hashimoto's thyroiditis &<br />
Pernicious anemia<br />
• Cushing's syndrome<br />
• Polyglandular autoimmune<br />
syndrome<br />
• Stage IV insulinoma &<br />
concomitant skin cancer<br />
• Nesidioblastosis (noninsulinoma<br />
hyperinsulinemic hypoglycemic<br />
syndrome)<br />
Nephrology<br />
• Nephrotic syndrome from<br />
minimal change disease<br />
• RPGN<br />
• Severe hyponatremia,<br />
ulcerated Torus palatinus<br />
• Severe hyponatremia,<br />
tea/toast diet<br />
• AKI from multiple myeloma vs<br />
septic ATN & rhabdomyolysis<br />
Hematology‐Oncology<br />
• Spur/Burr cell anemia<br />
• Anemia & malnourishment<br />
• Acquired autoimmune<br />
hemolytic anemia<br />
• DRESS<br />
• Immune reconstitution<br />
syndrome with<br />
thrombocytopenia<br />
• Hodgkin's lymphoma<br />
FIGURE 3. Examples of diagnoses presented at Best Case of the Block.<br />
Infectious Disease<br />
• Dengue hemorrhagic fever<br />
• Capnocytophagia infection<br />
with gangrene<br />
• Disseminated histoplasmosis<br />
• Disseminated cryptococcus<br />
• Disseminated gonoccus<br />
• AIDS with PCP pneumonia<br />
and candidal esophagitis<br />
• TB Meningitis<br />
Neurology<br />
• Paraplegia from B12<br />
deficiency with NO inhalation<br />
• Neurological changes from<br />
migrated PICC<br />
• Hemineglect from MCA CVA<br />
• Necrosis of craniotomy seal and<br />
aseptic meningitis from GBM<br />
vaccine<br />
Rheumatology<br />
• Polymyalgia rheumatica<br />
• Scleroderma with pulmonary<br />
adenocarcinoma<br />
• Pseudogout & epiploic<br />
appendigitis<br />
• Lupus flare, ischemic<br />
Raynaud’s crisis and arterial<br />
occlusion from APS<br />
• Pseudoporphyria cutanea tarda<br />
• Fitz‐Hugh‐Curtis syndrome<br />
Participants were surveyed to assess their perceptions of the competition.<br />
Survey results showed an average quality and learning score of 4 on a Likert<br />
Scale, suggesting that students and residents agree that the competition is an<br />
important learning experience and should be continued (Table I).<br />
Average Score<br />
Best Case is an important learning experience and should be continued. 4<br />
Best Case has increased my medical knowledge. 4<br />
I apply the teams’ lessons learned to the care of my patients. 3<br />
Thinking about my cases as the potential Best Case has increased my<br />
4<br />
focus on potential learning opportunities.<br />
TABLE I. Survey of medical students and residents (n=33) regarding Best Case of the Block.<br />
Scores are on a Likert Scale, 1-5, 1 = Strongly Disagree, 5 = Strongly Agree.<br />
Discussion<br />
The “Best Case of the Block” competition successfully engages students and<br />
residents, increases their exposure to educational cases, and increases their<br />
focus on potential learning opportunities throughout the inpatient rotation.<br />
As exhibited by the participant feedback, the implementation of the “Best<br />
Case of the Block” challenge has improved the learning experience of our<br />
medical students and residents.<br />
Since implementation, some challenges were noted. For instance, residents<br />
may find it difficult to identify extraordinary cases. However, participants<br />
are encouraged that voting is based on three categories, not only the rarity of<br />
the diagnosis. Voting methods have also been a concern. Voting rules are<br />
strict and overseen by the chief resident. Rules include that all voters must<br />
be present at the beginning of morning report, the attending physician must<br />
be present, and each participant may only cast one ballot.<br />
The UC Irvine Internal Medicine Residency Program intends to continue the<br />
competition each rotation, and to maintain a record of the cases. The authors<br />
are considering a “Best Case of the Year” competition <strong>for</strong> the future.<br />
Acknowledgements<br />
The authors thank the students, residents and hospitalists at UC Irvine <strong>for</strong> their creative<br />
participation in competitions, and <strong>APDIM</strong> <strong>for</strong> the opportunity to share this programmatic<br />
innovation.<br />
References<br />
1 “Facts About Departments of Internal Medicine.” <strong>Alliance</strong> <strong>for</strong> Academic Internal Medicine,<br />
n.d. http://www.im.org/About/FactsaboutDepartments/Pages/default.aspx.<br />
2. “ACGME Program Requirements <strong>for</strong> Graduate Medical Education in Internal Medicine,”<br />
July 1, 2009.<br />
http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/140_intern<br />
al_medicine_07012009.pdf.<br />
For more in<strong>for</strong>mation, please contact Lloyd Rucker at lrucker@uci.edu.
<strong>Poster</strong> Number: 46<br />
<strong>Poster</strong> Title: Best Cases Create Best Case Scenario: Educational Competition to Improve Resident Experience<br />
Authors and Affiliate Institutions: Heather Sand, Varaz Bozoghlanian, Lloyd Rucker, University of Cali<strong>for</strong>nia,<br />
Irvine, School of Medicine<br />
Submitting Author<br />
Lloyd Rucker, MD<br />
Vice Chair and Program Director<br />
Division of General Internal Medicine<br />
Department of Medicine<br />
University of Cali<strong>for</strong>nia, Irvine, School of Medicine<br />
101 City Drive South<br />
Route One, City Tower, Suite 400<br />
Orange, CA 92868<br />
Telephone: (714) 456-5691<br />
Email: lrucker@uci.edu<br />
Discussion of How the Problem was Identified and Explored: Internal medicine residents at our acute care<br />
academic medical center provide care <strong>for</strong> diverse patients with challenging diagnoses and management. However,<br />
great teaching cases are often not widely discussed across teams in the hub-bub of busy days restricted by duty<br />
hours and limited teaching interactions across teams. We wanted to identify great cases with important learning<br />
points, but residents often were reluctant to bring these cases <strong>for</strong>ward, and morning case conferences could not<br />
accommodate all the cases. We sought to create an entertaining and thoughtful conference to incentivize residents<br />
to present their great cases.<br />
Description of the Innovation: The “Best Case of the Block” contest challenges each of our six ward teams to<br />
identify and present their best case of the current ward block. Teams prepare a 5-minute presentation of their best<br />
case, often using handouts, slides, and skits. The competition is held during a thirty minute morning report at the<br />
end of the rotation. Students, residents, and faculty vote <strong>for</strong> the best case with points based equally in 3 categories:<br />
uniqueness of the case, importance of the learning issue, and quality and innovation of the presentation. The<br />
residency program pays <strong>for</strong> a team lunch <strong>for</strong> the team with the best overall presentation.<br />
Results to Date: To date, eight competitions have showcased 48 cases. Cases have covered a breadth of medicine<br />
specialties and pathologies including endocrinology with nesidioblastosis, infectious disease with dengue<br />
hemorrhagic fever, and dermatology with pseudo porphyria cutanea tarda. Teaching points have also varied from<br />
clinically rare pathology to how to approach diagnostic data. Participants were surveyed to assess their perceptions<br />
of the competition. Survey results showed an average quality and learning score of 4/5 on a Likert Scale, suggesting<br />
that students and residents agree that the competition is an important learning experience and should be continued.<br />
Discussion/Reflection/Lessons Learned: The “Best Case of the Block” competition successfully engages students<br />
and residents, increases their exposure to educational cases, and increases their focus on potential learning<br />
opportunities throughout the inpatient rotation. As exhibited by the participant feedback, the implementation of the<br />
“Best Case of the Block” challenge has improved the learning experience of our medical students and residents.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 47
A Longitudinal, Experiential Curriculum<br />
Lloyd Rucker, Bindu Swaroop, Kanwalpreet Hundal<br />
University of Cali<strong>for</strong>nia, Irvine, Department of Medicine<br />
Introduction<br />
Results<br />
Discussion<br />
Cost consciousness is central to high quality, safe medical care. Cost control<br />
is one of the highest priorities <strong>for</strong> health care in the US, and cost awareness<br />
must become fundamental to medical education. Ironically, caring <strong>for</strong><br />
patients in teaching hospitals has always been a very expensive proposition.<br />
Residents and faculty tend to practice expensive care. In recognition of the<br />
need to change this and to train residents in the importance of quality and<br />
cost, the ACP has introduced the “High Value, Cost Conscious Care<br />
Curriculum.” This curriculum consists of “10 interactive one hour modules<br />
based upon actual patients and their hospital bills” and designed to “ help<br />
residents develop habits of using high value care by using a 5-step<br />
framework.” We sought to incorporate this curriculum into a more<br />
comprehensive and experiential curriculum on medical economics and cost<br />
consciousness designed <strong>for</strong> internal medicine residents in our universitybased<br />
IM residency program.<br />
Innovation<br />
In the PGY1 year, our internal medicine residents engage in a seminar<br />
series on process improvement. This series introduces awareness of cost<br />
and also enhances the residents’ critical thinking on the topic of cost. In the<br />
PGY2 year, the longitudinal curriculum continues with faculty member-led<br />
small group seminars on medical economics including health care systems,<br />
the history of cost-control ef<strong>for</strong>ts in the US including the HMO movement,<br />
the role of the medical-industrial complex, and the potential impact of<br />
changes introduced by the Af<strong>for</strong>dable Care Act. These seminars address the<br />
massive cost of medical care in the US ($2.7 trillion per year or 18% of<br />
GDP) and the affect of that massive expenditure on health outcomes and<br />
the health of the economy.<br />
Each resident then chooses an aspect of medical care where he or she has<br />
personally noted opportunities <strong>for</strong> saving resources such as test ordering,<br />
procedures, algorithms of care, or medication use. Using the medical<br />
literature, the resident then develops quality guidelines <strong>for</strong> cost-conscious<br />
test ordering, medications or other aspects of medical care. He or she then<br />
evaluates up to 50 consecutive current patients to see how ordering<br />
patterns meet the recommendations from the literature. The residents<br />
present the results of this survey, first to a small group of colleagues and 2<br />
or 3 faculty members and then to a large conference of residents and<br />
hospitalists. Be<strong>for</strong>e each conference, a faculty member presents one of the<br />
interactive seminars from the “High Value, Cost Conscious Care<br />
Curriculum”. The department of medicine then uses the data from the<br />
presentations to implement changes. At times, the data are further<br />
presented to relevant groups such as the ICU faculty or radiology<br />
department.<br />
32 residents have participated to date. All have completed their initial cost<br />
evaluation projects. 18 residents have presented to the joint residenthospitalist<br />
conference. The conferences have been integrated into the core<br />
educational conferences of the residency program. Residents have<br />
enthusiastically embraced the curriculum and several have gone beyond the<br />
basic requirements to introduce educational programs based upon their<br />
findings.<br />
PPI<br />
CBC<br />
CXR<br />
CT<br />
Additional<br />
Topics<br />
By conservative criteria, 34% of medicine ward patients were<br />
placed on PPIs inappropriately. An intervention based on these<br />
findings cut down PPI use by 75%.<br />
Many patients get daily CBCs. One resident developed strict<br />
criteria <strong>for</strong> CBCs and found that only 1/3 were indicated.<br />
Furthermore, of those indicated, most were ordered with a<br />
differential that was not indicated.<br />
Patients in our MICU were undergoing an average of 1.4 CXRs per<br />
day. One patient had 35 CXRs in a 15 day period. These findings<br />
were presented to our intensivist faculty and critical care fellows.<br />
A follow‐up project is planned to assess the impact of this<br />
presentation.<br />
Only 4 of 48 patients presenting with syncope had<br />
documentation of abnormal neurologic exams. All of those with<br />
abnormal exams had abnormal CTs. However, of the 44 with<br />
normal exams, only 4 (12%) had abnormal head CT scans. Of<br />
those 4 patients, none of the abnormal head CTs explained the<br />
syncope. ThisprojecthasledtoajointIM–EDtask<strong>for</strong>cePI<br />
project to create diagnostic protocols <strong>for</strong> syncope.<br />
Iatrogenic Anemia<br />
Constipation Meds<br />
Mg and Phos Replacement<br />
Inpatient Lipid Screening<br />
Transfusion Indications<br />
Repeated Cardiac ECHOs<br />
IV Antiemetics<br />
Telemetry Indications & Utilization<br />
Admission CXRs<br />
Coagulation Test Ordering<br />
BMP Ordering<br />
PE Screening<br />
Our educational institutions are in the midst of massive change and challenge.<br />
The rapid pace of change is impacting graduate medical education in ways that<br />
we cannot entirely predict. These changes include measures introduced by the<br />
Af<strong>for</strong>dable Care Act, concerns about Medicare and Medicaid re<strong>for</strong>m (including<br />
quality of care measures and readmission paybacks), the recent imposition of<br />
the sequester, and challenges to the funding of graduate medical education<br />
(GME). Furthermore, we must also pile onto these changes recent re<strong>for</strong>ms in<br />
GME including the Next Accreditation System and the duty hours regulations.<br />
Our hospitals and medical schools are anticipating these re<strong>for</strong>ms through new<br />
programs and, in many cases, cutbacks. All of these challenges impact our<br />
residents and our training programs in ways that residents feel immediately,<br />
not just as some hypothetical construct that will affect their future careers. So<br />
that residents can understand and function in this evolving healthcare<br />
environment, it is imperative that GME training programs implement<br />
meaningful instruction in medical economics. “Parsimonious” utilization of<br />
scarce resources is a core element in that education.<br />
As part of a comprehensive curriculum in medical economics, we implemented<br />
a requirement that our residents per<strong>for</strong>m cost awareness projects. Our<br />
residents choose their own projects based upon their observations in the<br />
context of providing care. We believe this project selection method is key to the<br />
learning process. The residents’ own concerns about the magnitude of<br />
overutilization are often significantly trumped by overutilization that is actually<br />
much greater than they had expected.<br />
All of these projects are presented to residents and faculty. Some have had<br />
major impact such as the 75% decrease in inappropriate PPI ordering. Others<br />
are in process. One resident, moved by the dramatic excess ordering of blood<br />
transfusions, is in the process of preparing to teach about transfusion<br />
indications and protocols through preparation of an online educational module<br />
<strong>for</strong> residents and a live presentation <strong>for</strong> hospitalist faculty.<br />
Residents can embrace enthusiasm <strong>for</strong> quality and safety in the context of cost<br />
conscious care. Residency programs can implement projects that rein<strong>for</strong>ce<br />
theseconcerns.Intheprocess,wecanhavemeasurableimpactsthatactuallydo<br />
enhance the care we provide <strong>for</strong> patients through our GME programs and<br />
residents.<br />
Acknowledgements<br />
The authors thank the residents and hospitalists at UC Irvine <strong>for</strong> their creative participation in<br />
in the educational sessions and cost consciousness research projects and <strong>APDIM</strong> <strong>for</strong> the<br />
opportunity to share this programmatic innovation.<br />
Reference<br />
www.acponline.org/curriculum.html<br />
For more in<strong>for</strong>mation, please contact Lloyd Rucker at lrucker@uci.edu.
<strong>Poster</strong> Number: 47<br />
<strong>Poster</strong> Title: Cost Awareness Curriculum <strong>for</strong> Residents<br />
Authors and Affiliate Institutions: Lloyd Rucker, Kanwalpreet Hundal, University of Cali<strong>for</strong>nia, Irvine, School<br />
of Medicine; Bindu Swaroop, Long Beach Veterans Administration Hospital<br />
Submitting Author<br />
Lloyd Rucker, MD<br />
Vice Chair and Program Director<br />
Division of General Internal Medicine<br />
Department of Medicine<br />
University of Cali<strong>for</strong>nia, Irvine, School of Medicine<br />
101 City Drive South<br />
Route One, City Tower, Suite 400<br />
Orange, CA 92868<br />
Telephone: (714) 456-5691<br />
Email: lrucker@uci.edu<br />
Discussion of How the Problem was Identified and Explored: Cost-consciousness is central to high quality, safe<br />
medical care. Cost control is one of the highest priorities <strong>for</strong> health care in the US. Cost awareness must become<br />
fundamental to medical education. In recognition, the AAIM-ACP has introduced the “High Value, Cost Conscious<br />
Care Curriculum”. We sought to incorporate this curriculum into a more comprehensive and experiential<br />
curriculum on medical economics and cost consciousness.<br />
Description of the Innovation: The longitudinal curriculum begins with faculty-led small group seminars on<br />
medical economics including the Patient Protection Af<strong>for</strong>dable Care Act. Each resident then chooses an aspect of<br />
care such as PPI prophylaxis or a test such as head CT <strong>for</strong> syncope. The resident develops quality guidelines <strong>for</strong><br />
cost-conscious test or medication ordering. He or she then evaluates the care of 50 current patients. The resident<br />
presents the results of this survey, first to colleagues in a small group setting and then to a conference of residents<br />
and hospitalists. Be<strong>for</strong>e each conference, a faculty member presents elements of the “High Value, Cost Conscious<br />
Care Curriculum”. The department then sets priorities <strong>for</strong> emphasizing areas of cost-saving potential and advertises<br />
these to faculty and residents.<br />
Results to Date: Twenty-two PGY2 residents have participated to date. All have completed their initial cost<br />
evaluation projects. Residents have presented 3 projects to the hospitalist-resident conference; the rest are<br />
scheduled throughout the year. An initial intervention project led to a 50% decrease in inappropriate PPI<br />
prophylaxis. Another has led to creation of a task <strong>for</strong>ce on syncope guidelines. Others have discovered dramatic<br />
excesses in ordering of constipation prophylaxis, lipid testing, chest x-rays, urinalyses, head CT, PT/PTT/INR, CT<br />
Angiography, echo cardiograms, CBCs, and telemetry. Residents have rated this experience very highly and<br />
uni<strong>for</strong>mly support its continuation. Faculty members and hospital administrators have noted residents’ enthusiasm<br />
<strong>for</strong> and ownership of these projects.<br />
Discussion/Reflection/Lessons Learned: Residents have taken enthusiastic ownership of their projects and<br />
become advocates <strong>for</strong> change. The curriculum incorporates many <strong>for</strong>mal interactions over a 12-month period of<br />
time. Early results show that an integrated, longitudinal curriculum which includes educational seminars, residentled<br />
projects, faculty involvement, and discussion of the “High Value, Cost Conscious Care Curriculum” can be<br />
agents <strong>for</strong> positive, cost-conscious change.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 48
Creation of Mini‐Lectures to Improve Resident Teaching<br />
Bindu Swaroop, Lloyd Rucker, Kanwalpreet Hundal<br />
University of Cali<strong>for</strong>nia, Irvine, Department of Medicine<br />
Introduction<br />
Internal medicine is a vast and complex field. Residents often feel<br />
overwhelmed with the amount of material they are expected to learn and<br />
eventually teach to others. Busy residents who want to teach often do<br />
not have time to prepare topics. To meet this need, residents in our<br />
program created a learner-centered, centralized database of core, highvalue<br />
and evidence-based inpatient topic mini lectures.<br />
Skill Mark “x” if accomplished Comments<br />
Choose an appropriate and relevant topic<br />
Appropriately concise and relevant to the topic<br />
Practical<br />
Limited and appropriate number of key points<br />
Where appropriate, specialists review lectures and ensure they<br />
correspond to the guidelines and practices of the medical center. Of the<br />
41 lectures, seven have been revised to meet current guidelines.<br />
Innovation<br />
Each of our residents in their 1 st year of training are taught to create<br />
mini-lectures during a doctoring skills rotation. They then put those<br />
lessons into place in their 2 nd year when they create their official minilecture.<br />
Visual aids and handouts memorable<br />
FIGURE 2. Evaluation <strong>for</strong>m filled out by committee members.<br />
Results<br />
Over a six week time period, lectures have been viewed 264 times<br />
representing an average of 44 views per week.<br />
Mini‐Lecture Topic<br />
# of views<br />
Intern Pearls/Orientation 19<br />
ECG <strong>for</strong> Interns 15<br />
Electrolyte Replacement 12<br />
To date, residents have developed and revised <strong>for</strong>ty one mini-lectures.<br />
Lecture topics range from IV fluid management to acute<br />
decompensated heart failure, and also include core measures such as<br />
VTE prophylaxis.<br />
Community Acquired Pneumonia 8<br />
TABLE 2. Most viewed mini-lecture topics.<br />
To ensure durability and accuracy, residents update the lectures<br />
annually during a required teaching rotation.<br />
Discussion<br />
FIGURE 1. Process <strong>for</strong> creating a mini-lecture.<br />
Resident leaders and faculty mentors provide a set of guidelines to<br />
follow including a ten minute time limit, inclusion of clinical vignettes,<br />
and use of an objectives and summary slide. Residents use the “notes”<br />
section of each slide to provide in<strong>for</strong>mation on how to deliver the talk.<br />
Each resident then presents his or her lecture to 2-3 attending<br />
physicians and 2 senior residents. Additional feedback is provided and<br />
the final version of the lecture is added to a website created specifically<br />
to host the lectures.<br />
Figure 3. Screenshot of the mini-lecture website.<br />
Both residents and attendings have demonstrated enthusiasm and<br />
support <strong>for</strong> the core curriculum website. The mini-lectures have<br />
provided a tangible evidence-based <strong>for</strong>mat to efficiently and effectively<br />
present key inpatient medicine topics during inpatient rounds. The<br />
residents themselves have driven the curriculum and have chosen the<br />
topics they feel are most relevant and useful to their colleagues. They<br />
are revised annually to ensure they follow the most recent and<br />
evidenced based guidelines. The result has been the creation of a great<br />
educational resource that is managed, updated, owned, and<br />
disseminated by the residents themselves.<br />
Acknowledgements<br />
The authors thank the residents and hospitalists at UC Irvine and VA Long<br />
Beach <strong>for</strong> their participation in creation and revision of the mini-lectures.<br />
For more in<strong>for</strong>mation, please contact Lloyd Rucker at lrucker@uci.edu.
<strong>Poster</strong> Number: 48<br />
<strong>Poster</strong> Title: A Resident-Driven Mini-Lecture Curriculum <strong>for</strong> Inpatient Internal Medicine<br />
Authors and Affiliate Institutions: Bindu Swaroop, Long Beach VA Medical Center; Kanwalpreet Hundal,<br />
Lloyd Rucker, University of Cali<strong>for</strong>nia, Irvine, School of Medicine<br />
Submitting Author<br />
Bindu K. Swaroop, MD<br />
Assistant Clinical Professor<br />
Department of Internal Medicine<br />
University of Cali<strong>for</strong>nia, Irvine, School of Medicine<br />
5901 East Seventh Street<br />
Mail Code 111<br />
Long Beach, CA 90822<br />
Telephone: (714) 655-8494<br />
Email: bkswaroop@yahoo.com<br />
Discussion of How the Problem was Identified and Explored: Internal medicine is a vast and complex field.<br />
Residents often feel overwhelmed with the amount of material they are expected to learn and eventually teach to<br />
others. Busy residents who want to teach often do not have time to prepare topics. To meet this need, residents in<br />
our program created a learner-centered, centralized database of core, high-value and evidence based inpatient topic<br />
mini-lectures.<br />
Description of the Innovation: Each of our residents in their second year of training chooses a core medicine<br />
topic relevant to the inpatient medicine service and creates a PowerPoint “mini-lecture” as part of a core teaching<br />
skills rotation. Resident leaders and faculty mentors provide a set of guidelines to follow including a ten minute<br />
duration, inclusion of clinical vignettes, and use of an objectives and summary slide. Residents use the “notes”<br />
section of each slide to provide in<strong>for</strong>mation on how to deliver the talk. Each resident then presents his or her lecture<br />
to 2-3 attending physicians and 2 senior residents. Additional feedback is provided and the final version of the<br />
lecture is added to a website created to host the lectures.<br />
Results to Date: Residents have developed thirty-five mini-lectures. Topics range from IV fluid management to<br />
acute decompensated heart failure and also include core measures such as VTE prophylaxis. Learners and teachers<br />
often and widely use the lectures to teach. Where appropriate, specialists review lectures and ensure they<br />
correspond to the guidelines and practices of the medical center. To ensure durability and accuracy, residents<br />
update the lectures annually during a required teaching rotation.<br />
Discussion/Reflection/Lessons Learned: Both residents and attendings have demonstrated enthusiasm and<br />
support <strong>for</strong> the core curriculum website. The mini-lectures have provided a tangible evidence-based <strong>for</strong>mat to<br />
efficiently and effectively present key inpatient medicine topics during inpatient rounds. The residents themselves<br />
have driven the curriculum and have chosen the topics they feel are most relevant and useful to their colleagues.<br />
The result has been the creation of a great educational resource that is managed, updated, owned and disseminated<br />
by the residents themselves.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 49
<strong>Poster</strong> Number: 49<br />
<strong>Poster</strong> Title: The Last Lecture? Uniting Resident Preferences and Principles of Adult Learning to Improve the<br />
Noon Conference Lecture Series<br />
Authors and Affiliate Institutions: Adam Sawatsky, Katie Berlacher, Rosanne Granieri, University of Pittsburgh<br />
School of Medicine<br />
Submitting Author<br />
Adam Sawatsky, MD<br />
Instructor<br />
Division of General Internal Medicine<br />
Department of Internal Medicine<br />
University of Pittsburgh School of Medicine<br />
Montefiore Hospital, Suite W933<br />
200 Lothrop Street<br />
Pittsburgh, PA 15213<br />
Telephone: (507) 993-5198<br />
Email: sawatskyap@upmc.edu<br />
Discussion of How the Problem was Identified and Explored: The lecture remains a central means <strong>for</strong><br />
delivering the knowledge content of the residency core curriculum to internal medicine residents, fulfilling the<br />
Accreditation Council <strong>for</strong> Graduate Medical Education requirement <strong>for</strong> “regularly scheduled didactic sessions.”<br />
However, there is little evidence in the literature regarding the effectiveness of lectures at improving long-term<br />
knowledge of residents.<br />
Description of the Innovation: We conducted a targeted needs assessment using focus groups of residents and<br />
faculty, exploring motivations <strong>for</strong> attending or not attending noon conferences, learning preferences within the<br />
noon conference, improvements that could be made to the noon conference, and feelings about increasing active<br />
participation in noon conference. Using that in<strong>for</strong>mation, we designed an active learning <strong>for</strong>mat that could be<br />
easily applied to the noon conference. The <strong>for</strong>mat focused on 3-5 main learning points, centered on cases and<br />
clinical questions, with opportunity <strong>for</strong> small group discussion and commitment to answers. We piloted the <strong>for</strong>mat<br />
using two general medicine faculty to study feasibility and measure initial satisfaction to ensure we were meeting<br />
residents’ needs. We have begun to implement it on a larger scale with subspecialists.<br />
Results to Date: Our needs assessment revealed important themes regarding resident preferences on motivations,<br />
content, delivery and engagement within noon conference, along with faculty opinions about barriers to change.<br />
Our pilot survey revealed 87.1% of the 202 attendees at 8 separate lectures felt the new <strong>for</strong>mat improved overall<br />
learning as compared to lecture, with similar results <strong>for</strong> satisfaction, clarity, relevance, usefulness and engagement.<br />
There was no perceived increase in stressfulness or decrement in residents’ ability to eat lunch and take a break in<br />
their day.<br />
Discussion/Reflection/Lessons Learned: The lecture is the cornerstone of resident education, yet it is not<br />
congruent with principles of adult learning or the educational goal of developing residents who can interact and<br />
apply the knowledge to patient care. The data from our focus groups can guide attempts to design new innovations<br />
on teaching in noon conference. We demonstrate one way this has been accomplished at our institution that can<br />
serve as a model.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 50
<strong>Poster</strong> Number: 50<br />
<strong>Poster</strong> Title: It’s All in the Execution: Description of a Duty Hours Monitoring Process<br />
Authors and Affiliate Institutions: Michael P Stevens, Stephanie Call, Virginia Commonwealth University<br />
Medical College of Virginia<br />
Submitting Author<br />
Michael P. Stevens, MD<br />
Associate Program Director<br />
Department of Internal Medicine<br />
Virginia Commonwealth University Medical College of Virginia<br />
1300 East Marshall Street<br />
PO Box 980019<br />
Richmond, VA 23298<br />
Telephone: (804) 828-2121<br />
Email: mstevens@mcvh-vcu.edu<br />
Discussion of How the Problem was Identified and Explored: The ACGME has mandated a number of duty<br />
hours (DH) related rules. At our large, urban program with 111 residents we have traditionally struggled with<br />
monitoring DH in real time.<br />
Description of the Innovation: One Associate Program Director (APD) was tasked with both monitoring and<br />
addressing DH issues. Utilizing the New Innovations software plat<strong>for</strong>m, we rolled out a new DH logging<br />
compliance mandate, wherein residents who have not logged their DH within a 7 day period of time receive a<br />
professionalism letter in their permanent program file. Thereafter, a new DH violation assessment process was<br />
deployed wherein twice weekly the APD charged with DH monitoring reviewed summary violation data as well as<br />
logging compliance and then worked with the medicine chief residents to address issues in real time. Data on DH<br />
logging compliance as well as overall compliance with each DH rule were tracked throughout a 12 month period.<br />
Violation rates were calculated by dividing the total number of violations <strong>for</strong> a given rule by the total number of<br />
opportunities to violate.<br />
Results to Date: Over the 12 month period from 7/2011 to 6/2012, our compliance with DH logging was 95.4%.<br />
Our violation rates per DH rule were 1) 8 hour rule: 0.5% (203/39,677); 2) 16 hour rule: 0.6% (117/18,227); 3) 24<br />
hour rule: 0.01% (3/21,450); 4) 80 hour rule: 0.1% (23/39,677).<br />
Discussion/Reflection/Lessons Learned: Our DH monitoring and intervention process led to sustained, low<br />
violation rates across all DH violation types, despite our status as a busy urban program with 111 housestaff. We<br />
believe our process would benefit other medicine residency programs.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 51
Standardizing Resident Handoffs in Times of ACGME Duty-Hour Regulations<br />
Vishnu Laalitha Surapaneni, M.B.B.S.,MPH<br />
University Hospitals Case Medical Center<br />
INTRODUCTION<br />
METHODOLOGY<br />
RESULTS<br />
DISCUSSION<br />
•Patient handoffs refer to the transfer of patient in<strong>for</strong>mation and<br />
responsibility from one care provider to the next. (Abraham<br />
2011)<br />
•In 2003, ACGME approved new resident duty-hour regulations<br />
that limited resident workweeks to 80 hours or fewer and limited<br />
continuous duty to 24hours. This caused transfers of care <strong>for</strong> a<br />
hypothetical patient to increase by a mean of 11% during a<br />
Monday-Friday hospitalization. A member of the primary team<br />
was present in the hospital <strong>for</strong> only 47% of a patient's hospital<br />
stay. (Horowitz 2006) The ACGME work-hour regulations<br />
effective July 2011, limiting continuous duty to 16hours <strong>for</strong> PGY-<br />
1s, have further decreased the time spent by residents at the<br />
hospital. Although these regulations are implemented to decrease<br />
fatigue related errors, they also make handoffs a more frequent<br />
and critical part of patient care.<br />
•However, handoffs are inherently error-prone processes.<br />
In 2010, the Joint Commission sentinel event data analysis<br />
showed that 80% of the 4800 sentinel events were due to<br />
improper communication. In a study by Petersen (1994), patients<br />
who suffered preventable errors were 3.5 times more likely to be<br />
cared <strong>for</strong> by a covering physician. Handoffs have also been<br />
implicated in 20% to 24% of malpractice claims in various<br />
health-care settings. (Kachalia 2007)<br />
•Despite these well-identified threats to patient safety, there are<br />
several deficiencies to the way handoffs are practiced currently.<br />
Sign-out skills are not routinely taught in medical schools or<br />
residency programs. (Horowitz 2006) Residents are expected to<br />
learn these skills “on the job”. Residents involved in giving and<br />
receiving patient handoffs often lack training, experience or<br />
supervision.<br />
•To minimize handoff failures, the Joint Commission has<br />
mandated that all US hospitals standardize in<strong>for</strong>mation transfer<br />
practices. However, there are currently no universally adopted<br />
standards <strong>for</strong> handoff communication, either written or verbal.<br />
The templates used <strong>for</strong> handoffs are unique to each institution,<br />
with up to 19 different templates published in scientific journals.<br />
(Cohen 2009)<br />
•The handoff template in the electronic medical record at our<br />
institution is titled HOT and has 6 text boxes that allow <strong>for</strong> freetexting<br />
in<strong>for</strong>mation. There are no guidelines on what patient<br />
in<strong>for</strong>mation should be included in each of these 6 sections.<br />
OBJECTIVES<br />
Objective 1: Refine the existing handoff template in the<br />
electronic medical record to develop a standardized handoff<br />
template <strong>for</strong> our institution.<br />
Objective 2: To pilot and evaluate the efficacy of the new<br />
standardized handoff template.<br />
Study Design:<br />
This is a multi-method qualitative and quantitative, crosssectional<br />
study conducted to improve the existing template <strong>for</strong><br />
patient handoffs.<br />
Study Subjects:<br />
The subjects were first year residents of the Internal Medicine<br />
residency program at our academic teaching hospital.<br />
Data Collection:<br />
To design a standardized handoff template, several data<br />
sources were used.<br />
•Firstly, evidence-based recommendations <strong>for</strong> ideal handoff<br />
templates were reviewed through extensive literature search in<br />
MEDLINE database using search terms such as “sign-out”,<br />
“handoff”, “patient safety” and “resident”. The patient<br />
in<strong>for</strong>mation categories identified as essential in these studies,<br />
that are currently absent in the electronic handoff template<br />
were isolated.<br />
•Secondly, a focus group of Internal Medicine residents was<br />
held to discuss their level of satisfaction with the current<br />
handoff template. This focus group guided the development of<br />
an online survey that was disseminated electronically via<br />
email Through this survey, residents identified the essential<br />
categories in the existing template and made recommendations<br />
<strong>for</strong> new patient in<strong>for</strong>mation categories.<br />
•Lastly, additional categories were also identified through<br />
direct observation of nursing shift reports and<br />
interdepartmental handoffs between anesthesia and surgery.<br />
These were compared with directly observed handoffs between<br />
Internal Medicine residents.<br />
The categories thus identified from various sources were<br />
incorporated to create a standardized handoff template.<br />
Evaluation:<br />
A crucial step in creating the new standardized template was to<br />
first determine the efficacy of the current handoff template by<br />
measuring handoff errors. Two sources were used to collect<br />
data on adverse events caused by handoffs.<br />
•First, data was collected from night-floats each night, in order<br />
to identify essential patient in<strong>for</strong>mation that was not<br />
communicated by the primary team during handoff.<br />
•Second, data was also collected from the primary team each<br />
morning on how many errors had occurred overnight due<br />
to handoffs. Errors included all categories from near-misses<br />
and adverse events to sentinel events.<br />
Data Collection:<br />
Literature Review:<br />
362 references were identified via literature review from<br />
MEDLINE database. Using pre-defined inclusion and<br />
exclusion criteria, 91 references were studied. Categories such<br />
as “severity of patient illness”, “events over past 24 hours”,<br />
“current clinical condition” and “read-back” were incorporated<br />
into the new handoff template.<br />
Online Survey:<br />
Of the 46 residents surveyed, 65% found administrative data<br />
an essential part of the current template, and 80% voted <strong>for</strong> a<br />
well constructed diagnostic one-liner. Residents wanted to<br />
incorporate the following into the new standardized template;<br />
“Events over the past 24hours”, “Abnormal baseline physical<br />
exam findings” and “Events to anticipate overnight”.<br />
Nursing and Interdepartmental Sign-out:<br />
Additional categories that were identified were “New<br />
symptoms that developed during the day”, “Unstable vitals<br />
during the day” and “Read-back time”.<br />
Using data from the above sources, the following standardized<br />
version of the handoff template was designed.<br />
Evaluation:<br />
Night-Floats:<br />
On average, night-float interns covered 68 patients, and<br />
received an average of 47 pages per night. The most common<br />
reasons <strong>for</strong> the pages were pain (85%), unstable vitals (78%),<br />
patient developing new symptoms (70%) and critical lab<br />
values (60%). 15% of the time, night-float residents felt that<br />
they did not have enough in<strong>for</strong>mation from the primary team<br />
to manage ituations overnight.<br />
Primary Team:<br />
Survey of the primary team interns revealed that night-float<br />
interns made 3 hand-off errors <strong>for</strong> 134 patient days.<br />
Results of this study indicated that each intern handed off an<br />
average of 5 patients per night. 60% of all patients admitted to<br />
the General Medicine services were handed off more than once<br />
each night. Night-float residents often felt that the primary<br />
team did not handoff adequate and pertinent patient<br />
in<strong>for</strong>mation in order to deliver optimal patient care overnight.<br />
The standardized handoff template was designed to ensure<br />
transfer of updated and pertinent patient data. The new<br />
template allows <strong>for</strong> less free-texting and standardizes the<br />
<strong>for</strong>mat of the “diagnostic one-liner” thereby decreasing the<br />
chances of patient data omission. The section “Events since<br />
7AM today” uses the patient safety technique of <strong>for</strong>cing<br />
functions. This <strong>for</strong>ces residents to think through all new<br />
outstanding clinical events <strong>for</strong> the day resulting in a more<br />
updated sign-out.<br />
Be<strong>for</strong>e implementing the standardized template, however, we<br />
quantified the efficacy of the current template by analyzing<br />
handoff errors. In our resident focus group, we had identified<br />
dissatisfaction with and safety concerns about the template.<br />
Thus, we hypothesized that the use of the current template<br />
results in several handoff errors per night.<br />
The data showed that despite the confusion expressed by nightfloats<br />
about the plan <strong>for</strong> the night, only 3 handoff errors<br />
occurred <strong>for</strong> 134 patient days. Thus, the second phase of the<br />
project, which was to implement the new handoff template,<br />
was temporarily held.<br />
Our results could be explained in the following ways. Since the<br />
data was collected at the end of the academic year, interns may<br />
have become better trained to deal with unexpected events<br />
overnight. There could have been a bias of underreporting as<br />
this data was collected by self-reporting. Participants might not<br />
have recorded handoff errors if they did not result in adverse<br />
patient outcomes.<br />
The next step is to repeat the study in the beginning of the next<br />
academic year to eliminate the factor of resident training. The<br />
study will also collect data by directly-observing handoffs, so<br />
as to eliminate the factor of underreporting. We hypothesize<br />
that several handoff errors will occur with the current template<br />
and implementing the standardized template will result in less<br />
handoff errors and more resident satisfaction.<br />
ACKNOWLEDGEMENTS<br />
Dr.A.Krikorian, M.D.<br />
Dr.K.Armitage, M.D.<br />
Chief residents- Dr R.Mehta, Dr.P.Oppelt,Dr.G.Prithviraj and<br />
Dr.J.Weingart<br />
Intern class 2011-12<br />
All residents of the Internal Medicine program at UHCMC
<strong>Poster</strong> Number: 51<br />
<strong>Poster</strong> Title: Optimizing Resident Handoffs<br />
Authors and Affiliate Institutions: Vishnu Laalitha Surapaneni, Armand Krikorian, Keith Armitage, University<br />
Hospitals Case Medical Center<br />
Submitting Author<br />
Vishnu Laalitha Surapaneni, MD<br />
Faculty<br />
Department of Internal Medicine<br />
Case Western Reserve University School of Medicine<br />
11100 Euclid Avenue<br />
Cleveland, OH 44106<br />
Telephone: (216) 844-3833<br />
Email: VishnuLaalitha.Surapaneni@UHhospitals.org<br />
Discussion of How the Problem was Identified and Explored: To minimize handoff failures, the Joint<br />
Commission has mandated that all US hospitals standardize in<strong>for</strong>mation transfer practices. However, there are<br />
currently no universally adopted standards <strong>for</strong> handoff communication, either written or verbal. The templates used<br />
<strong>for</strong> handoffs are unique to each institution, with up to 19 different templates published. (Cohen 2009) The<br />
handoff template in the EMR at our institution has 6 text boxes that allow <strong>for</strong> free-texting in<strong>for</strong>mation. There are no<br />
guidelines on what patient in<strong>for</strong>mation should be included in each of these 6 sections. We reviewed evidencebased<br />
recommendations <strong>for</strong> ideal handoff templates through literature search in MEDLINE. Then a focus group of<br />
IM residents was held to discuss their level of satisfaction with the current handoff template. Based upon their<br />
feedback a survey tool <strong>for</strong> all residents was created. Additional categories were identified through direct<br />
observation of nursing shift reports and interdepartmental handoffs between anesthesia and surgery. These were<br />
compared with directly observed handoffs between IM residents.<br />
Description of the Innovation: Data was collected from night-floats each night, in order to identify essential<br />
patient in<strong>for</strong>mation that was not communicated by the primary team during handoff. Data was also collected from<br />
the primary team each morning on how many errors had occurred overnight due to handoffs. Errors included all<br />
categories from near misses and adverse events to sentinel events.<br />
Results to Date: On average, night-float interns covered 68 patients, and received an average of 47 pages per<br />
night. The most common reasons <strong>for</strong> the pages were pain (85%), unstable vitals (78%), patient developing new<br />
symptoms (70%) and critical lab values (60%). 15% of the time, night-float residents felt that they did not have<br />
enough in<strong>for</strong>mation from the primary team to manage situations overnight.<br />
Discussion/Reflection/Lessons Learned: Results of this study indicated that each intern handed off an average of<br />
5 patients per night. 60% of all patients admitted to the IM services were handed off > once each night. Night-float<br />
residents often felt that the primary team did not handoff adequate patient in<strong>for</strong>mation in order to deliver optimal<br />
patient care overnight. A standardized handoff template was designed to ensure transfer of updated and pertinent<br />
patient data. The new template allows <strong>for</strong> less free-texting and standardizes the <strong>for</strong>mat of the “diagnostic one-liner”<br />
thereby decreasing the chances of patient data omission.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 52
<strong>Poster</strong> Number: 52<br />
<strong>Poster</strong> Title: Raising Resident Awareness of Their Role in Quality and Safety Through Patient Safety Discussions<br />
Authors and Affiliate Institutions: Tabassum Salam, Jessica A White, Christiana Care Health System<br />
Submitting Author<br />
Tabassum Salam, MD<br />
Associate Residency Program Director<br />
Department of Internal Medicine<br />
Christiana Care Health System<br />
4755 Ogletown-Stanton Road<br />
Suite 2E70, Ammon Building<br />
Newark, DE 19718<br />
Telephone: (302) 733-6384<br />
Email: tsalam@christianacare.org<br />
Discussion of How the Problem was Identified and Explored: It is generally recognized that physicians need<br />
enhanced awareness and exposure to topics in Quality and Safety. Yet, training in Quality and Safety within<br />
residency and fellowship programs is generally insufficient. A baseline study of knowledge, skills and attitudes of<br />
resident physicians, medical students and faculty [N=24] in our community-hospital based Internal Medicine<br />
residency program was undertaken. It revealed that the majority of respondents [62%] had an interest in Quality<br />
and Safety. 54% felt that knowledge about Quality and Safety would impact their current roles. The majority [62%]<br />
felt disquieted about being involved in care that harms or potentially harms. 81% of respondents preferred the<br />
integration of interactive learning into their daily educational structure.<br />
Description of the Innovation: A Patient Safety Discussion was instituted every day at Residents’ Morning<br />
Report. Quality, safety and systems issues were identified by the residents and medical students, and teaching<br />
faculty would catalog these cases. Once a month, an Administrative Fellow in Quality and Patient Safety would<br />
present focused follow-up and Safety Pearls on these cases at Morning Report in order to ‘close the loop’ <strong>for</strong> the<br />
residents.<br />
Results to Date: A survey was administered to residents 4 months after the introduction of the Patient Safety<br />
Discussion [PSD]. Of the respondents [N=9], 78% felt that the Patient Safety Discussion increased their awareness<br />
of systems-thinking, and that the PSD promoted a non-punitive environment to regularly discuss errors. Two-thirds<br />
of the responding residents felt that the PSD integrated Quality and Safety concepts into daily practice, and that the<br />
presentation of the Safety Pearls was an effective learning experience. 89% of the respondents wanted the PSD to<br />
continue.<br />
Discussion/Reflection/Lessons Learned: A relatively succinct educational experience like the Patient Safety<br />
Discussion positively impacted residents’ perception and learning of Quality and Safety. A key to its success was<br />
the integration of this teaching tool into a daily pre-existing <strong>for</strong>um such as Residents’ Morning Report.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 53
<strong>Poster</strong> Number: 53<br />
<strong>Poster</strong> Title: Resident-Led Decision Support Huddles to Improve Risk Factors <strong>for</strong> Patients with Diabetes<br />
Authors and Affiliate Institutions: David Sweet, Lynn Clough, Summa Health System/NEOUCOM; Tho Luong,<br />
Summa Akron City Hospital<br />
Submitting Author<br />
David B. Sweet, MD<br />
Professor<br />
Division of Clinical Sciences<br />
Department of Internal Medicine<br />
Summa Health System/NEOUCOM<br />
55 Arch Street<br />
Suite 1A<br />
Akron, OH 44304<br />
Telephone: (330) 375-3741<br />
Email: sweetd@summahealth.org<br />
Discussion of How the Problem was Identified and Explored: Our residency clinic has conducted an ongoing<br />
quality improvement project to improve risk factor control <strong>for</strong> patients with Diabetes Mellitus (DM). Decision<br />
support has included prospective EHR entries by staff including recent A1c, LDL and blood pressure (BP) results<br />
and prompts to encourage treatment intensification.<br />
Description of the Innovation: Decision support was expanded during the fourth quarter of 2011 with residents<br />
conducting pre-clinic huddles lasting
Hands‐on Quality Improvement: A Curriculum <strong>for</strong> Team‐based Resident‐Led Projects<br />
Training Residents in Quality Improvement Using Small Groups and Resident‐Initiated Projects<br />
Hailey Vincent, MD 1,2 , Lindsey Tricinella, DO 1,2 , Michael McNeal, MD 1,2 , Curtis Mirkes, DO 1,2 ,<br />
Colleen Colbert, PhD 1,2 , Sunita Varghees, MD, PhD 1,2, Tresa McNeal, MD 1,2<br />
Scott & White Healthcare 1 and Texas A&M Health Science Center College of Medicine 2 , Temple, Texas<br />
Background: Quality improvement is an important<br />
part of healthcare that allows identification of<br />
problems, self‐evaluation, planned intervention,<br />
and implementation of solutions. The ACGME<br />
requires that all residency programs include quality<br />
improvement methods within their curriculum. The<br />
Internal Medicine Residency Program at Scott and<br />
White Healthcare/ Texas A&M Health Science<br />
Center College of Medicine has pioneered a unique<br />
curriculum that allows residents to evaluate their<br />
work environment and use quality improvement<br />
methods to solve “real world” problems. While a<br />
quality improvement curriculum is required, it can<br />
be difficult to implement a standardized curriculum<br />
that provides opportunities <strong>for</strong> all residents to have<br />
hands‐on experience. It can be more challenging to<br />
promote actual implementation of solutions within<br />
a healthcare system.<br />
Innovation: Working in groups of 6‐8 residents,<br />
with representation from each post‐graduate year,<br />
residents identify a problem they have<br />
encountered, be it direct patient care or a systembased<br />
issue. A program director, associate program<br />
director, or a chief resident facilitates a guided<br />
discussion and introduces quality improvement<br />
terminology and concepts.<br />
Each group per<strong>for</strong>ms a root cause analysis<br />
and value stream map of the current and<br />
future process <strong>for</strong> their chosen project.<br />
Residents are responsible <strong>for</strong> meeting with<br />
stakeholders, implementing improvement<br />
measures, and evaluating outcomes. At the<br />
completion of the project, small groups<br />
present their projects to a panel of senior<br />
leadership in quality improvement. All<br />
residents attend the presentation, gaining<br />
additional insight into other methods and<br />
areas of quality improvement. The top<br />
scoring team receives a monetary reward.<br />
Results: Six projects were completed in 2011‐<br />
2012, the first year of this curriculum. Two of<br />
these projects are being continued and one of<br />
the projects has spurred further inquiry. In<br />
addition, residents have the opportunity to<br />
submit and present these projects at national<br />
meetings.<br />
Discussion: By working with “real‐world”<br />
problems, identified by the residents<br />
themselves, residents gain knowledge and<br />
experience in quality improvement methods.<br />
The small group setting allows each resident<br />
to play a role in a focused project. All<br />
residents participate in critically evaluating<br />
other projects, developing leadership skills in<br />
quality improvement. Working with the Scott<br />
& White Healthcare system, the residentbased<br />
projects often initiate a change that<br />
improves the patient care in our system.<br />
Annual QI Curriculum Timeline<br />
Aug ‐ Didactic curriculum is presented<br />
Sept –Oct – Groups brainstorm project ideas<br />
and choose a project<br />
Nov – Groups per<strong>for</strong>m root cause analysis<br />
involving stakeholders<br />
Dec –Apr ‐ Groups implement change<br />
involving stakeholders and determine<br />
effectiveness of the solution. Groups may try<br />
several different solutions.<br />
May – Groups present projects in a dedicated<br />
noon conference event
<strong>Poster</strong> Number: 54<br />
<strong>Poster</strong> Title: Hands-On Quality Improvement: A Curriculum <strong>for</strong> Team-Based, Resident-Led Projects Training<br />
Residents in Quality Improvement Using Small Groups and Resident-Initiated Projects<br />
Authors and Affiliate Institutions: Hailey Vincent, Lindsey Tricinella, Micheal McNeal, Tresa McNeal, Curtis<br />
Mirkes, Texas A&M University College of Medicine<br />
Submitting Author<br />
Hailey Vincent, MD<br />
Resident<br />
Department of Internal Medicine<br />
Texas A&M University College of Medicine<br />
2401 South 31st Street<br />
Temple, TX 76508<br />
Telephone: (254) 724-2111<br />
Email: hvincent@sw.org<br />
Discussion of How the Problem was Identified and Explored: Quality Improvement is an important part of<br />
healthcare that allows identification of problems, self-evaluation, planned intervention, and implementation of<br />
solutions. The ACGME requires that all residency programs include quality improvement methods into their<br />
curriculum. The Internal Medicine Residency Program at Scott and White Healthcare/ Texas A&M Health Science<br />
Center College of Medicine has pioneered a unique curriculum that allows residents to evaluate their work<br />
environment and use quality improvement methods to solve “real world” problems. While a quality improvement<br />
curriculum is required, it can be difficult to implement a standardized curriculum that provides opportunities <strong>for</strong> all<br />
residents to have hands-on experience. It can be more challenging to promote actual implementation of solutions<br />
within a healthcare system.<br />
Description of the Innovation: Working in groups of 6-8 residents, with representation from each post-graduate<br />
year, residents identify a problem they have encountered, be it direct patient care or a system-based issue. A<br />
program director, associate program director, or a chief resident facilitates a guided discussion and introduces<br />
quality improvement terminology and concepts. The group per<strong>for</strong>ms a root cause analysis and value stream map of<br />
the current and future process <strong>for</strong> their chosen project. Residents are responsible <strong>for</strong> meeting with stakeholders,<br />
implementing improvement measures, and evaluating outcomes. At the completion of the project, small groups<br />
present their projects to a panel of senior leadership in quality improvement. All residents attend the presentation<br />
gaining additional insight into other methods and areas of quality improvement. The top scoring team receives a<br />
monetary reward.<br />
Results to Date: Six projects were completed in 2011-2012, the first year of this curriculum. Two of these<br />
projects are being perpetuated and one of the projects has spurred further inquiry. In addition, residents have the<br />
opportunity to submit and present these projects as scholarly activity at national meetings.<br />
Discussion/Reflection/Lessons Learned: Results: By working with “real-world” problems, identified by the<br />
residents themselves, residents gain knowledge and experience in quality improvement methods. The small group<br />
setting allows each resident to play a role in a focused project. All residents participate in critically evaluating other<br />
projects, developing leadership skills in quality improvement. Working with the Scott & White Healthcare system,<br />
the resident-based projects often initiate a change that improves the patient care in our system.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 55
<strong>Poster</strong> Number: 55<br />
<strong>Poster</strong> Title: Outcomes from a Three-Year QI Residency Education Program<br />
Authors and Affiliate Institutions: David Meyers, Robert Holland, Mary Thompson, Michelle Kipp, Chris<br />
Hildebrand, Amy Smith, Bennett Vogelman, University of Wisconsin School of Medicine and Public Health<br />
Submitting Author<br />
Bennett S. Vogelman, MD<br />
Vice Chair <strong>for</strong> Education; Director, Internal Medicine Residency Program<br />
Department of Internal Medicine<br />
University of Wisconsin School of Medicine and Public Health<br />
1685 Highland Avenue<br />
Room 5116 MFCB<br />
Madison, WI 53705-2281<br />
Telephone: (608) 263-7352<br />
Email: bsv@medicine.wisc.edu<br />
Discussion of How the Problem was Identified and Explored: We saw the infusion of QI curricula into medical<br />
education as an opportunity to teach QI skills alongside resident-led self-assessment and per<strong>for</strong>mance improvement<br />
exercises.<br />
Description of the Innovation: To explore this synergy, we developed a three-year process during which residents<br />
learn the principles of QI and how to integrate them into their practice. This curriculum results in two end points:<br />
patient care outcomes and resident QI project implementation. The graduating classes of 2010 (n=22) and 2011<br />
(n=21) audited over 400 charts annually (2547 records) <strong>for</strong> 20-22 preventive and disease-specific core measures in<br />
their continuity clinics. After comparing their results to peers and national standards, each resident committed to<br />
change in weak areas. During a one-month rotation as PG3s, residents apply KSABs acquired in prior M&M and<br />
a two-week QI experience to develop their own QI proposals. They are coached in skills related to problem<br />
identification, <strong>for</strong>mal process assessment, intervention design, overcoming barriers, securing stakeholder buy-in<br />
and implementation. We emphasize the importance of a thorough process analysis using interprofessional<br />
collaboration. During presentations to multidisciplinary audiences, residents discuss proposed interventions and<br />
elicit feedback. Resident projects are integrated into existing hospital QI committees or coached by designated<br />
faculty to facilitate implementation.<br />
Results to Date: Both classes showed improvement from PG1 to PG3 year in their average compliance with the<br />
core measures (paired t test: class of 2010, p=0.001; 2011, p=0.006). Immunization rates; cancer, lipid, ETOH,<br />
tobacco and DM screening; HTN control; and diabetes measures improved in one or both classes. Compliance<br />
rates were lowest (10-80%) <strong>for</strong> tobacco cessation, ACE/ARB <strong>for</strong> microalbuminuria, HbgA1C90%), DM foot and<br />
eye care (>85%) and screening <strong>for</strong> cancer, HTN, DM, ETOH, tobacco and lipids (>94%). These longitudinal data<br />
show similar results to residency-wide cross-sectional data from 2003-2007. Residents completed 71 projects in<br />
five years and 58% were implemented.<br />
Discussion/Reflection/Lessons Learned: The chart review, reflection, and commitment-to-change process is an<br />
effective tool <strong>for</strong> self-assessment, learning and improving patient care in continuity clinics. By graduation, residents<br />
have demonstrated the ability to complete key steps in a QI project and many have seen their actions meaningfully<br />
impact patient care.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 56
Background<br />
“If you listen carefully to the patient, they will tell you the diagnosis.”<br />
‐Sir William Osler<br />
Ekaterina Vypritskaya, MD, FACP, Saba A Hasan, MD, FACP<br />
Capital Health Regional Medical Center, Trenton, NJ<br />
Description of the Innovation<br />
Results to Date<br />
In the era of endemic over‐testing, when billions of<br />
care dollars are spent on unnecessary or<br />
inefficiently delivered services, it is our<br />
responsibility to prepare the next generation of<br />
physicians to change their habits of practicing<br />
medicine.<br />
1. Implement the Awareness of High Value, Cost‐Conscious Initiative by ACP<br />
‐Curriculum of 6 lectures by core faculty was incorporated in our noon<br />
conference schedule.<br />
‐ Analyze cases of overuse/misuse of resources in real time; analysis leads to<br />
didactic sessions with emphasis on evidence‐based medicine principles and<br />
current guidelines.<br />
‐ Incorporate analysis of clinical reasoning during teaching rounds (discussing<br />
pretest probability, thinking ahead whether results of test would change<br />
management)<br />
2. Challenge the common replacement of careful history and physical exam<br />
with imaging and laboratory tests<br />
‐ Include didactic sessions on Physical Exam into noon conference schedule<br />
‐Per<strong>for</strong>m bedside workshops on physical exam <strong>for</strong> small groups of residents<br />
(5‐6 people) run by subspecialists (complete neurological exam per<strong>for</strong>med by<br />
neurologist; JVD assessment, heart auscultation by cardiologist)<br />
3. Respond to patient demands to overuse medications or per<strong>for</strong>m<br />
unnecessary tests<br />
‐Conduct simulation sessions with role play <strong>for</strong>mat. (For example: Patient with<br />
sore throat and Centor Score 1 requests antibiotics. Residents practice<br />
educating patient about the nature of viral disease and harm of antibiotics.)<br />
4. Avoid “One size fits all” approach<br />
‐ Conduct didactic sessions with Social Service and Case Management regarding<br />
the basics of health insurance and coverage.<br />
‐Employ multidisciplinary rounds to customize care and craft safe discharge<br />
plans <strong>for</strong> uninsured and underinsured patients.<br />
5. Emphasize preventive care as effective tool <strong>for</strong> assuring good public health<br />
and <strong>for</strong> saving money on medical costs<br />
‐ Conduct didactic sessions on updates in immunization and screening<br />
‐ Address importance of discontinuation of screening <strong>for</strong> patients with limited<br />
life expectancies.<br />
‐ Include patient’s values into clinical decision making.<br />
‐ Implement curriculum in “Cultural awareness”<br />
‐ Conduct simulation sessions on difficult cultural and bio‐ethical cases<br />
Residents have understood principle of High<br />
Value Cost‐Conscious Care. Now they bring <strong>for</strong><br />
discussions cases where physical exam was<br />
underused or/and over‐testing took place.<br />
They seem to be excited to apply these<br />
principles to patient care.<br />
Significance<br />
Incorporation of these curriculum elements in<br />
many aspects of training will promote the<br />
habit of practicing evidence‐based,<br />
comprehensive, patient‐centered medicine.<br />
References<br />
Cynthia D. Smith, MD; and on behalf of the<br />
<strong>Alliance</strong> <strong>for</strong> Academic Internal Medicine–<br />
American College of Physicians High Value,<br />
Cost‐Conscious Care Curriculum Development<br />
Committee; “Teaching High‐Value, Cost‐<br />
Conscious Care to Residents: The <strong>Alliance</strong> <strong>for</strong><br />
Academic Internal Medicine–American College<br />
of Physicians Curriculum.” Annals of Internal<br />
Medicine. 21 August 2012, Vol 157, No 4.
<strong>Poster</strong> Number: 56<br />
<strong>Poster</strong> Title: “If You Listen Carefully to the Patient, They Will Tell You the Diagnosis.” -Sir William Osler<br />
Authors and Affiliate Institutions: Ekaterina A Vypritskaya, Saba A Hasan, Capital Health Regional Medical<br />
Center<br />
Submitting Author<br />
Ekaterina A. Vypritskaya, MD<br />
Faculty<br />
Department of Internal Medicine<br />
Capital Health Regional Medical Center<br />
750 Brunswick Avenue<br />
Trenton, NJ 08648<br />
Telephone: (609) 394-6031<br />
Email: evypritskaya@capitalhealth.org<br />
Discussion of How the Problem was Identified and Explored: In the era of endemic over-testing, when billions<br />
of care dollars are spent on unnecessary or inefficiently delivered services, it is our responsibility to prepare the<br />
new generation of physicians to change habits of practicing medicine.<br />
Description of the Innovation: 1. Implement the Awareness of High Value, Cost-Conscious Initiative by ACP.<br />
Curriculum of 6 lectures by core faculty was incorporated in our noon conference schedule. - Analyze cases of<br />
overuse/misuse of resources in real time; analysis leads to didactic sessions with emphasis on evidence-based<br />
medicine principles and current guidelines. - Incorporate analysis of clinical reasoning during teaching rounds<br />
(discussing pretest probability, thinking ahead whether results of test would change management) 2. Challenge the<br />
common replacement of careful history and physical exam with imaging and laboratory tests. - Include didactic<br />
sessions on Physical Exam into noon conference schedule - Per<strong>for</strong>m bedside workshops on physical exam <strong>for</strong><br />
small groups of residents (5-6 people) run by subspecialists (complete neurological exam per<strong>for</strong>med by neurologist;<br />
JVD assessment, heart auscultation by cardiologist). 3. Respond to patient demands to overuse medications or<br />
per<strong>for</strong>m unnecessary tests. - Conduct simulation sessions with role play <strong>for</strong>mat. (For example: Patient with sore<br />
throat and Centor Score 1 requests antibiotics. Residents practice educating patient about the nature of viral disease<br />
and harm of antibiotics.) 4. Avoid “One size fits all” approach. - Conduct didactic sessions with Social Service<br />
and Case Management regarding the basics of health insurance and coverage. - Employ multidisciplinary rounds<br />
to customize care and craft safe discharge plans <strong>for</strong> uninsured and underinsured patients. 5. Emphasize preventive<br />
care as effective tool <strong>for</strong> assuring good public health and <strong>for</strong> saving money on medical costs. - Conduct didactic<br />
sessions on updates in immunization and screening - Address importance of discontinuation of screening <strong>for</strong><br />
patients with limited life expectancies. 6.Include patient’s values into clinical decision making. - Implement<br />
curriculum in “Cultural awareness” - Conduct simulation sessions on difficult cultural and bio-ethical cases.<br />
Results to Date: Residents have understood principle of High Value Cost-Conscious Care. Now they bring <strong>for</strong><br />
discussions cases where physical exam was underused or/and over-testing took place. They seem to be exited to<br />
apply these principles to daily patient care.<br />
Discussion/Reflection/Lessons Learned: Incorporation of these curriculum elements in many aspects of training<br />
will promote habit of practicing evidence-based, comprehensive, patient-centered medicine.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 57
A Novel Assessment System Created by Mapping Milestones to Entrustable Professional Activities<br />
Eric J. Warm MD, Bradley R. Mathis MD, Carl Fichtenbaum MD, Caroline Mueller MD, Savita Pai MD, Jonathan Tolentino MD, Tiffiny Diers MD, Lauren Ashbrook MD, Justin Held MD, Cheryl Lee MD, David Lee MD, Sharice Wood MD<br />
ABSTRACT<br />
Tracking<br />
Formative<br />
Summative<br />
Background: The ACGME’s Next Accreditation System<br />
Curricular Milestones<br />
Entrustable Professional Activities<br />
Sub-Competency<br />
NAS Reporting Milestones<br />
(NAS) requires measurement and reporting of outcomes<br />
through educational milestones.<br />
Aim: Describe a mapping process between curricular and<br />
NAS milestones and Entrustable Professional Activities<br />
Different educational milestones in each<br />
rotation. Examples:<br />
(EPAs)<br />
Different directly observed skills <strong>for</strong> every<br />
rotation. Examples:<br />
(EPAs) to assess trainee progression towards competence.<br />
PC F2: With minimal supervision, manage patients<br />
Titrate cardiac medications<br />
with common and complex clinical disorders.<br />
Setting: Internal medicine residency in an urban tertiary<br />
Titrate insulin based on glucose readings<br />
referral medical center.<br />
PC B4: Routinely identify subtle or unusual physical<br />
Manage pancreatitis<br />
Participants: Internal medicine residents and faculty.<br />
findings that may influence clinical decision making.<br />
Adjust short and long acting narcotics <strong>for</strong> sickle cell<br />
Program Description: Curricular milestones were mapped<br />
PC E1: Make appropriate clinical decisions based<br />
patients<br />
to more than 350 EPAs that constitute the University of<br />
upon the results of common diagnostic testing.<br />
Manage parathyroid abnormalities in the renal patient<br />
Cincinnati residency curriculum. Assessments based on<br />
PC F10: Customize care in the context of the patient’s<br />
Deliver appropriate goal-directed therapy <strong>for</strong> severe<br />
a 5-point entrustment scale assigned by evaluators <strong>for</strong> a<br />
preferences and overall health.<br />
sepsis<br />
given set of EPAs are also directly assigned to mapped<br />
curricular milestones. Curricular milestone mapping<br />
decisions were based on the following question: would<br />
the likely intent of the evaluator in assessing a trainee on<br />
a given EPA also be to assess the mapped milestones?<br />
EPAs were then aggregated based on subject matter<br />
and mapped to the appropriate sub-competencies. The<br />
aggregate entrustment score <strong>for</strong> those EPAs determines the<br />
NAS reporting milestones achievement level.<br />
Program Evaluation: Assessing EPAs and associated<br />
mapped curricular milestones creates the ability to track<br />
curricular milestone progression across rotations and<br />
over time. By combining these data sets, the competency<br />
committee can attest to specific clinical skills (end-ofrotation<br />
<strong>for</strong>mative assessment of specific EPAs), monitor<br />
progression of curricular milestone attainment (figure 1),<br />
and develop summative assessments relative to peers and<br />
the entrustment scale (figure 2, NAS map).<br />
• Curricular milestones are mapped to EPAs by asking the question: would the likely intent of the<br />
evaluator in assessing a trainee on a given EPA also be to assess the mapped milestones?<br />
• Data from the mapping generates the figures below that the resident and program director can<br />
track over time<br />
• In this example, multiple EPAs that demonstrate development of management plans are aggregated and mapped to the patient care<br />
subcompetency ‘Develops and achieves comprehensive management plan <strong>for</strong> each patient’ (PC2)<br />
• To determine the NAS reporting level, the aggregate 5 point entrustment score is multiplied by 9/5, and then rounded down to the<br />
nearest 0.5, which corresponds to the 9 check boxes under the 5 columns of the NAS reporting tool<br />
Figure 1a. Curricular Milestone Interpersonal<br />
Figure 1b. Curricular Milestone Patient Care C1:<br />
Figure 1c. Curricular Milestone Patient Care A4:<br />
Discussion: Curricular milestones can be mapped<br />
and Communication Skills A1: Provide timely and<br />
Synthesize all available data, including interview,<br />
Demonstrate sufficient knowledge to diagnose and<br />
to EPAs to create a <strong>for</strong>mative assessment system <strong>for</strong><br />
residents . EPAs can be aggregated and mapped to the<br />
subcompetencies and the NAS reporting milestones <strong>for</strong><br />
comprehensive verbal and written communication<br />
to patients/advocates.<br />
physical examination, and preliminary laboratory<br />
data, to define each patient’s central clinical<br />
problem.<br />
treat undifferentited and emergent conditions.<br />
Figure 2a. Communication Skills Radar Plot<br />
Figure 2b. Patient Care Radar Plot<br />
Figure 2c. Systems Based Practice Radar Plot<br />
summative reporting. Further study is needed to determine<br />
if this system predicts progression towards competence.<br />
This represents 25 assessments from 18 evaluators in<br />
the first three quarters of the year <strong>for</strong> a single PGY-1.<br />
This represents 140 assessments from 16 evaluators in<br />
the first three quarters of the year <strong>for</strong> a single PGY-1.<br />
This represents 140 assessments from 12 evaluators in<br />
the first three quarters of the year <strong>for</strong> a single PGY-3.<br />
This represents 202 assessments from 12 evaluators<br />
after eight months of the PGY-3 year.<br />
This represents 488 assessments from 12 evaluators<br />
after eight months of the PGY-3 year.<br />
This represents 139 assessments from 12 evaluators<br />
after eight months of the PGY-3 year.<br />
Entrustment Scale:<br />
1. Resident cannot per<strong>for</strong>m this skill even with assistance.<br />
2. Resident should per<strong>for</strong>m this skill under direct supervision.<br />
3. Resident can per<strong>for</strong>m this skill under indirect supervision.<br />
4. Resident can per<strong>for</strong>m this skill independently.<br />
5. Resident can act as instructor or supervisor <strong>for</strong> this skill (aspirational).<br />
• These graphs show progression over time <strong>for</strong> residents (blue lines with circles) compared to the peer average (grey lines with<br />
diamonds) and an idealized reference (yellow lines).<br />
• The PGY-1 in Figure 1a improved after feedback; the PGY-1 in Figure 1b is on track; and the PGY-3 in Figure 1c has achieved<br />
an entrustment level of “resident can per<strong>for</strong>m this skill independently.”<br />
• Graphs like these can be obtained <strong>for</strong> all 142 curricular milestones.<br />
• Figures were derived using MedHub’s data system (MedHub, Inc., PO Box 4148, Ann Arbor, Michigan 48106).<br />
• These figures are snapshots of a single PGY-3 resident’s curricular milestone data (blue lines) compared to his/her peers (green<br />
shaded area).<br />
• Each of the letter designations around the circles represents a single milestone within that core competency. Levels 1–5<br />
represent the five levels of the entrustment scale.<br />
• The residency competency committee uses this in<strong>for</strong>mation to quickly determine who is on track and who needs closer scrutiny.<br />
• Figures like these can be obtained <strong>for</strong> all 142 curricular milestones.<br />
• Figures were derived using MedHub’s data system (MedHub, Inc., PO Box 4148, Ann Arbor, Michigan 48106).
<strong>Poster</strong> Number: 57<br />
<strong>Poster</strong> Title: A Novel Assessment System Created by Mapping Milestones to Entrustable Professional Activities<br />
Authors and Affiliate Institutions: Eric J Warm, Bradley R Mathis, Carl Fichtenbaum, Caroline Mueller, Savita<br />
Pai, Jonathan Tolentino, Tiffiny Diers, Lauren Ashbrook, Justin D Held, Cheryl Lee, David Lee, Sharice Wood,<br />
University of Cincinnati College of Medicine<br />
Submitting Author<br />
Eric J. Warm, MD<br />
Program Director<br />
Division of General Internal Medicine<br />
Department of Internal Medicine<br />
University of Cincinnati College of Medicine<br />
231 Albert Sabin Way<br />
Mail Location 0557<br />
Cincinnati, OH 45267-0557<br />
Telephone: (513) 558-2590<br />
Email: warmej@ucmail.uc.edu<br />
Discussion of How the Problem was Identified and Explored: The ACGME has mandated programs in the Next<br />
Accreditation System (NAS) to submit composite milestone data on residents every 6 months. Program directors<br />
have found milestones difficult to use <strong>for</strong> <strong>for</strong>mative resident assessment and have turned to the Entrustable<br />
Professional Activity (EPA -- a professional activity the public expects physicians are capable of doing) as a more<br />
practical tool to measure per<strong>for</strong>mance. Our aim was to create an assessment system <strong>for</strong> reporting high value<br />
milestone-based in<strong>for</strong>mation <strong>for</strong> each resident.<br />
Description of the Innovation: We rewrote our entire curriculum using the EPA as the basic element. For each<br />
rotation, we created both content and process EPAs. Content EPAs describe observable skills that differ <strong>for</strong> each<br />
rotation depending on the specific skills learned (<strong>for</strong> example, titrate insulin, manage a ventilator). Process EPAs<br />
describe observable skills conserved across rotations (<strong>for</strong> example, demonstrate shared decision making). Faculty,<br />
peers and staff assess resident per<strong>for</strong>mance on these EPAs using a 5 point entrustment score (1: cannot do EPA, 2:<br />
can do EPA with ongoing proactive supervision, 3: can do EPA with distance supervision, 4: can do EPA<br />
independently, 5: can teach EPA). We mapped each EPA to the 142 curricular milestones asking the question:<br />
Would the likely intent of the evaluator in assessing a trainee on a given EPA also assess the milestone in question?<br />
We then created an in<strong>for</strong>mation system to collect, sort and report this data over time.<br />
Results to Date: Our curriculum and assessment system now consists of approximately 350 EPAs mapped to the<br />
142 curricular milestones. Faculty and residents have responded favorably to using EPAs as <strong>for</strong>mative feedback.<br />
Milestone data derived from setting entrustment scores <strong>for</strong> each mapped EPA provide a summative assessment of<br />
per<strong>for</strong>mance over time, thereby tracking resident progress towards independent practice (entrustment score of 4).<br />
After mapping the entire residency curriculum we discovered important gaps and developed specific experiences to<br />
fill them.<br />
Discussion/Reflection/Lessons Learned: An assessment system consisting of EPAs mapped to curricular<br />
milestones can be used in <strong>for</strong>mative assessment as well as summative reporting. These maps could be easily<br />
extended to the newer NAS milestones <strong>for</strong> ACGME reporting.<br />
<strong>2013</strong> <strong>APDIM</strong> <strong>Spring</strong> <strong>Meeting</strong> <strong>Poster</strong> Abstract Summaries Page 58