Reference Guide - wsib
Reference Guide - wsib
Reference Guide - wsib
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
D E<br />
R M<br />
A TI<br />
T I<br />
S
Acknowledgements<br />
The WSIB would like to acknowledge the significant contributions of the following Health<br />
Professional Associations and workplace representatives who participated in the development of the<br />
Program of Care for Occupational Contact Dermatitis:<br />
• Employers’ Council of Ontario Mr. John Blogg<br />
• Ontario Medical Association Dr. Joel DeKoven<br />
• Ontario Pharmacists’ Association Ms. Susan Halasi<br />
• Ontario Physiotherapy Association Ms. Annette Marcuzzi<br />
• Ontario Podiatric Medical Association Dr. Andrew Klayman<br />
• Registered Practical Nurses Association of Ontario Ms. Ann Marie Hann<br />
• Ontario Professional Firefighters Association Mr. Paul Atkinson<br />
• Ontario Psychological Association Dr. Ian Nicholson<br />
The WSIB would also like to thank Dr. Linn Holness and her team of researchers, Dr. Joan Saary,<br />
Dr. Roohi Qureshi, and Dr. Valerie Palda, at the Department of Occupational and Environmental<br />
Health, St. Michael’s Hospital, University of Toronto, who completed the systematic review of<br />
treatments for contact dermatitis that formed the foundation for this program.<br />
Health Professional Access Line:<br />
1-800-569-7919 or (416) 344-4526<br />
Please call the Health Professional Access Line<br />
if you have any questions about the Program of Care.<br />
Hours: Monday – Friday 9:00 a.m. – 4:00 p.m.<br />
2
Occupational Contact Dermatitis (OCD) POC Algorithm<br />
© (WSIB) Workplace Safety and Insurance Board, 2004 Printed in Canada
Table of Contents<br />
Program of Care Algorithm 3<br />
Introduction 5<br />
Occupational Contact Dermatitis Program of Care 6<br />
Objectives 6<br />
Screening 7<br />
Eligibility Criteria 8<br />
Initial Assessment 8<br />
Treatment 9<br />
Irritant Contact Dermatitis 10<br />
Allergic Contact Dermatitis 12<br />
Reassessment and Follow-up 13<br />
Information for the Worker 13<br />
Discharge from the Program of Care 14<br />
Communication Requirements 14<br />
Program of Care Requirements 14<br />
<strong>Reference</strong>s 17<br />
Appendix A 18<br />
WSIB Contact Dermatitis Formulary 18<br />
Over the Counter Preparations 22<br />
Over the Counter Tar Preparations 23<br />
4
Occupational Contact Dermatitis<br />
Program of Care <strong>Reference</strong> <strong>Guide</strong><br />
for Physicians<br />
Introduction<br />
This reference guide is intended for physicians treating patients who are being investigated for contact<br />
dermatitis or have been diagnosed with contact dermatitis. This guide will inform you about the objectives<br />
of the Program of Care and how to deliver this treatment program to your patients.<br />
The Program of Care for Occupational Contact Dermatitis is an evidence-based health care delivery<br />
plan, based on a systematic review of the scientific literature. Subsequent to implementation, periodic review<br />
of the scientific literature will be necessary to ensure that new scientific evidence is incorporated. Clinical<br />
and program outcome evaluations will be conducted to facilitate improvements to the Program of Care.<br />
All of the interventions searched in the literature were determined to be “recommended” or “not<br />
recommended” for use in the Program of Care based on the quality of available evidence of their efficacy.<br />
The interventions reviewed are categorized as shown in Table 1:<br />
Table 1: Key to evidence grading and strength of recommendations<br />
Grading<br />
A<br />
B<br />
C<br />
D<br />
E<br />
+<br />
Quality of Evidence<br />
Good evidence to support the use of this intervention<br />
Fair evidence to support the use of this intervention<br />
Poor evidence to support the use of this intervention<br />
Fair evidence to support rejection of this intervention<br />
Good evidence to support rejection of this intervention<br />
Recommended based on clinical best practice,<br />
clinical guidelines, and/or expert committees.<br />
Note:<br />
Adherence to these guidelines will not ensure successful treatment in every situation. Further, these<br />
guidelines should not be deemed inclusive of all proper methods of care or exclusive of other methods of care<br />
reasonably directed to obtaining the same results. The ultimate judgement regarding the propriety of any specific<br />
procedure must be made by the physician in light of all the circumstances presented by the individual patient.<br />
The implementation of this care model is not intended to interfere with the rights and obligations of injured<br />
workers, employers, health care professionals or the WSIB.<br />
5
The Occupational Contact Dermatitis Program of Care<br />
Contact dermatitis (CD) has been defined as “an inflammatory skin reaction to direct contact with noxious<br />
agents in our environment” (Lachapelle, 1992). Substances that produce this condition after single or multiple<br />
exposures may be either irritant (ICD) or allergic (ACD) in nature. Occupational contact dermatitis (OCD)<br />
reflects a subcategory of both ICD and ACD in which exposure to a workplace agent causes the dermatitis.<br />
Irritant contact dermatitis (ICD) results from contact with external agents that directly damage the epidermis, in<br />
contrast to allergic contact dermatitis (ACD), in which the damage occurs through the host immune response as<br />
a result of a delayed type (cell-mediated Type IV) hypersensitivity reaction. The most common clinical<br />
expression of this induced inflammation is dermatitis, often called eczema.<br />
Objectives<br />
The objectives of the Program of Care are to:<br />
• enable early identification and appropriate diagnosis of workers with occupational contact<br />
dermatitis<br />
• provide best possible evidence-based quality care to workers with OCD<br />
• facilitate safe, timely and sustainable return to suitable work<br />
• prevent re-exposure to irritating and/or sensitizing agents<br />
• reduce recurrence of symptoms<br />
• help the worker return to the best possible level of overall function and quality of life.<br />
The Program of Care is also intended to improve clinical and return-to-work outcomes through education<br />
of the worker on symptom management, the correct use of medications, and ways to avoid re-exposure in the<br />
workplace, in the home, and at leisure.<br />
6
Screening<br />
The purpose of the screening and initial assessment, completed at the worker’s first contact with the<br />
physician, is to determine the appropriateness of the worker for the Program of Care, to determine<br />
whether any specialist referrals are required, and to begin treatment.<br />
The diagnosis of contact dermatitis should be suspected in workers in high-risk occupations and/or industry<br />
sectors with known workplace agents (e.g. agriculture, health care, manufacturing). Physicians should determine<br />
whether there is a suspected workplace agent (allergen or irritant) that can be identified. Screening should<br />
include determination of the following:<br />
A. Did the skin condition start after the worker started the job?*<br />
OR<br />
Did the skin condition become worse after the worker started the job?*<br />
AND<br />
B. Are symptoms better on weekends or holidays off work?<br />
*NOTE: “started the job” includes changing job duties or locations within the same workplace.<br />
Those patients who answer “yes” to BOTH A and B should be enrolled in the Program of Care.<br />
Referral to a specialist with experience diagnosing and treating occupational contact dermatitis should be<br />
considered when any of the following are suspected:<br />
• all cases of possible ACD<br />
• ICD with allergic features<br />
• chronic ICD<br />
• complicated OCD (e.g., not improving, deteriorating, confounded by another skin disease<br />
such as psoriasis).<br />
Following referral, the specialist will:<br />
• confirm a relationship between contact dermatitis and workplace exposure<br />
• conduct diagnostic tests (e.g. industrial patch testing) to identify a specific allergen.<br />
NOTE: Only a small number of physicians in Ontario are able to conduct patch testing for industrial allergens. Please<br />
call the WSIB Health Professional Access Line to obtain a list of locations where this specialized<br />
testing is performed.<br />
7
Eligibility Criteria<br />
Inclusion Criteria<br />
The Program of Care is appropriate for workers in Ontario:<br />
• with a positive screen for occupational contact dermatitis (either irritant or allergic), and/or a current<br />
diagnosis of occupational contact dermatitis by a dermatologist, occupational medicine physician or<br />
other specialist with experience diagnosing occupational contact dermatitis (uncomplicated ICD may<br />
also be diagnosed by a family physician)<br />
AND<br />
• presenting with a new onset skin disease which is workplace-induced.<br />
Workers may be enrolled in the Program of Care if they are still working (regular or modified duties)<br />
or off work.<br />
Workers who do not meet these criteria should be treated outside the Program of Care.<br />
Exclusion Criteria<br />
The Program of Care is not designed for ill workers with:<br />
• chemical burns<br />
• urticaria<br />
Workers with either of these conditions should be treated outside the Program of Care.<br />
Initial Assessment<br />
In order to make the Program of Care initial assessment visit feasible for primary care physicians, the<br />
clinical experience of committee members was used to select the following essential elements for the initial<br />
assessment of the worker from the much longer list contained in the American Academy of Dermatology<br />
<strong>Guide</strong>lines (www.aad.org). Physicians may include other assessment components as they consider appropriate.<br />
1. History may include the following:<br />
General medical status<br />
Onset of Dermatitis<br />
(1) Location<br />
(2) Symptoms<br />
(3) Description<br />
Progression<br />
(1) Relation between exposure and time interval of dermatitis<br />
(2) Relation between workplace exposure and development of symptoms<br />
Remissions<br />
(1) Response to treatment and rapidity of recurrence after discontinuing medication (if applicable)<br />
Occupational history<br />
(1) Nature of work<br />
(2) How long in current job/job duties<br />
(3) Changes in workplace procedures, chemical exposure, or environment exposure<br />
(4) Protective measures<br />
8
Medical history<br />
(1) History of contact dermatitis: nature, severity, and causative agent(s) if known<br />
(2) Previous treatment including medications<br />
(a) At onset<br />
(b) Self-treatment/over-the-counter treatments, complimentary therapies, herbal medicine<br />
(c) By other physicians<br />
(3) History of atopy – allergies, hayfever, asthma, atopic eczema<br />
2. Physical examination may include the following:<br />
Location – specify site(s)<br />
Involved versus uninvolved skin<br />
(a) Demarcation: Sharp or unclear<br />
(b) Other<br />
Lesion type & characteristics<br />
(a) Acute<br />
(b) Chronic<br />
The detailed findings from the examination and assessment of the worker are recorded on the Program<br />
of Care Screening and Initial Assessment Report. A Program of Care Screening and Initial Assessment<br />
Report should be completed and submitted to the WSIB within 24-48 hours of the initial assessment visit.<br />
Treatment<br />
The activities in the Program of Care are depicted in the algorithm (p. 3). Management will differ<br />
depending on whether the worker has ACD or ICD, and whether the dermatitis is acute, chronic or<br />
complicated.<br />
Although the initial presentation may appear as an uncomplicated case of ICD, complications may<br />
develop at any time during treatment. If complications develop, workers should be referred immediately to<br />
a specialist for appropriate management. It should also be noted that workers with acute ICD will need to<br />
be seen at more frequent intervals (i.e. every 2-4 weeks post-enrolment) until the acute features of the<br />
dermatitis resolve.<br />
Flares may occur at any time during treatment. The treating physician should see patients who<br />
experience flares in their condition as soon as possible, within no more than 2 weeks.<br />
The following is a description of the interventions in the Contact Dermatitis Program of Care.<br />
Interventions for irritant and allergic contact dermatitis are described separately. Within each category,<br />
both treatment interventions and interventions to prevent exacerbation and/or recurrence of symptoms<br />
are described.<br />
The treating physician determines selection of specific interventions.<br />
9
Irritant Contact Dermatitis (ICD)<br />
Treatment<br />
A<br />
Hi-lipid content moisturizers had good evidence of their efficacy in the treatment of ICD. Studies<br />
demonstrated the effect of hi-lipid content moisturizers in accelerating barrier regeneration (Held et al.<br />
2001). Based on the evidence, the moisturizer chosen should have:<br />
- high lipid content<br />
- either physiological lipids (e.g. fatty acids, cholesterol) or non-physiological lipids (e.g. petrolatum)<br />
although the latter were ranked highest in the ability to promote recovery of irritated skin<br />
- few ingredients.<br />
A list of hi-lipid content moisturizers is provided in Appendix A (page 22).<br />
+<br />
Moderate to high-potency topical corticosteroids<br />
Moderate to ultra-high potency topical corticosteroids are widely used in the treatment of ICD, however<br />
there was a lack of scientific evidence of their efficacy. Their use is recommended based on the clinical<br />
opinion of the consensus table members. A list of topical corticosteroids, which are on the WSIB Drug<br />
Formulary for Dermatitis, appears in order of potency in Appendix A (pages 18-21).<br />
The desire to reduce the risks of side effects by using less potent preparations must be balanced with the<br />
desire to gain control of a flare quickly with more potent preparations.<br />
Prevention<br />
A<br />
&<br />
B<br />
A<br />
B<br />
Recommended Interventions:<br />
The following interventions had good or fair evidence of their efficacy in the prevention of symptoms of<br />
ICD:<br />
Hi-lipid content moisturizers<br />
Two good quality studies (Held & Agner, 2001; Loden, 1997) and 4 fair quality studies<br />
(Schiemann-Willers et al, 2002; Ramsing & Agner, 1997; Held et al, 1999 and Zhai et al, 2002) found<br />
that moisturizers with a high lipid content were effective in preventing ICD. Better protection was afforded<br />
by fats with higher linoleic acid content (see Appendix A, page 22).<br />
Barrier creams containing dimethicone<br />
One good quality study (Zhai et al, 2000) found barrier creams containing the active ingredient<br />
dimethicone to be effective in preventing experimentally-induced ICD, and superior to vehicle<br />
treated or untreated control.<br />
Cotton liners under occlusive gloves<br />
One fair quality study (Ramsing & Agner, 1996) found that use of a cotton liner under occlusive<br />
gloves led to better results than the glove alone.<br />
10
Education<br />
B<br />
+<br />
An evidence-based skin care program is recommended both based on the systematic review<br />
(2 fair quality cohort studies; Held et al. 2002; Held et al. 2001), and the clinical experience of<br />
committee members. The educational intervention in the Held (2002) study was delivered in<br />
2 sessions, 14 days apart, and was reinforced 6 weeks later. The components of the education<br />
intervention included the following:<br />
I. Basics of Contact Dermatitis<br />
- anatomy and physiology of normal and diseased skin<br />
- description of contact dermatitis and its symptoms<br />
- acute and chronic contact dermatitis<br />
- irritant and allergic contact dermatitis<br />
II. Practical Instructions on Skin Care<br />
- hand washing<br />
- moisturizers<br />
- protective gloves<br />
- cotton gloves<br />
- avoiding irritants/sensitizers in the workplace, at home, and at leisure<br />
- booklet summarizing practical measures<br />
III. Monitoring Daily Behaviour<br />
- card to record behaviours and symptoms<br />
- symptom monitoring<br />
Interventions not recommended for ICD:<br />
+<br />
There was good evidence of the efficacy of barrier creams containing perfluoropolyethers<br />
(compounded extemporaneously); however they are not recommended in the Program of Care<br />
since they are not commercially available in Canada.<br />
E<br />
The use of aluminum chlorohydrate in the prevention of ICD is not recommended due<br />
to good evidence of its lack of efficacy.<br />
11
Allergic Contact Dermatitis (ACD)<br />
Treatment<br />
Recommended Interventions:<br />
The following interventions are recommended in the Program of Care because of good evidence of their<br />
efficacy in the treatment of allergic contact dermatitis.<br />
A<br />
Moderate to high-potency topical steroids<br />
There was good evidence of the efficacy of moderate to high potency topical steroids in the<br />
treatment of ACD, based on the results of two RCTs (Hachem et al, 2002; Queille-Roussel et al, 1990)<br />
and two cohort studies (Hachem et al, 2001; Parneix-Spake et al, 2001). Specific topical steroids in these<br />
studies included: Fluticasone propionate .05%, Clobetasone butyrate .05% and Clobetasol propionate<br />
.05%. Appendix A contains a list of topical corticosteroids listed in the WSIB Drug Formulary for<br />
Dermatitis in order of potency (see pages 18-21).<br />
+<br />
Topical macrolide immunomodulators<br />
NOTE: Topical macrolide immunomodulators are not listed in the WSIB Drug Formulary for<br />
Dermatitis – approval for their use should be obtained from the WSIB for each individual case.<br />
Topical macrolide immunomodulators are a new class of drugs that are being used increasingly for the<br />
treatment of a variety of skin disorders, including contact dermatitis. Currently, there is insufficient evidence<br />
to recommend their use in the Program of Care; it is possible that such evidence could be available in the<br />
next 12-24 months. An update of the scientific review in 12-24 months is indicated to ensure that these<br />
treatments are properly evaluated, and, if necessary, incorporated into the Program of Care. In the interim,<br />
their use should be considered only in exceptional cases in which the patient has failed to respond to topical<br />
corticosteroids.<br />
Prevention<br />
B<br />
There were no good quality studies demonstrating the efficacy of general prevention interventions for ACD.<br />
However, there is fair quality evidence for the prevention of exposure to specific allergens: fair evidence exists<br />
that TSP (Vidmar & Iwane, 1999) and organoclay (Marks et al, 1995) can prevent Rhus dermatitis, and<br />
that DPTA can prevent reactions to nickel, cobalt, and copper (Worl et al, 2001).<br />
+<br />
Education<br />
There was no evidence of the efficacy of an educational program for ACD. The educational program<br />
supported by the evidence for ICD can be used for ACD, but should be augmented to include how to<br />
recognize and avoid causal allergens and cross reactants at work, home, and leisure.<br />
12
Reassessment and Follow-up<br />
The Program of Care begins at the initial assessment visit and continues for a maximum of 6 months.<br />
The duration of the program, frequency, and timing of follow-up visits are detailed on the Algorithm (see<br />
page 3). Workers with acute contact dermatitis will need to be followed more closely. In acute cases, followup<br />
should occur 2-4 weeks following the initial assessment. All workers in the Program of Care will be<br />
reassessed at 6 to 8 weeks, 3 months and 6 months. The maximum length of the program is 6 months.<br />
Follow-up and reassessment will determine if the worker is progressing and if the goals of treatment<br />
are being achieved. This includes symptom monitoring, physical examination, adjustments to medications<br />
as necessary (e.g., tapering down dosage), and health-related quality of life. Referral to a specialist in<br />
occupational contact dermatitis should be considered when the worker is not progressing as expected<br />
or his or her condition is deteriorating.<br />
An additional component of the reassessment should include a review of potential barriers to program<br />
compliance. Factors affecting patient compliance have been broadly categorized as social issues, emotional<br />
issues, educational issues, medication dosing schedules, and medication side effects. Emotional issues may<br />
include self-denial or mood disorders. Social anxiety has been documented in the scientific literature among<br />
individuals with contact dermatitis, particularly when dermatitis is on the face. This may also occur, to a<br />
lesser degree, when the dermatitis is on the hands. Results of the follow-up reassessment may indicate that<br />
referral outside the Program of Care to an appropriate allied health professional is required to address key<br />
issues and barriers to program compliance. Such referrals should be considered on a case-by-case basis.<br />
A Program of Care Reassessment Report should be completed and submitted to the WSIB following<br />
the 6-8 week follow-up, and 3-month follow-up. A Care & Outcomes Summary Report should be submitted<br />
following the 6-month follow-up visit.<br />
Information for the Worker<br />
Occupational Disease Fact Sheet<br />
"Workplace Contact Dermatitis: Facts for Workers in Ontario" is a fact sheet that provides educational<br />
information including: a description of contact dermatitis and its symptoms, how irritant and allergic<br />
contact dermatitis are caused, and how possible cases of occupational contact dermatitis are handled by<br />
physicians. The fact sheet also provides a list of irritants and allergens associated with various jobs.<br />
Additional copies can be downloaded from the WSIB website at www.<strong>wsib</strong>.on.ca<br />
13
Discharge from the Program of Care<br />
Workers should be discharged from the Program of Care when their symptoms have stabilized and no<br />
further clinical intervention is required following the 6-8 week, 3-month, or 6-month follow-up. The<br />
maximum length of the Program of Care is 6 months from the date of enrolment in the program. Workers<br />
should also be discharged from the Program of Care if they develop other serious medical conditions that<br />
affect their ability to attend follow-up visits or to complete the treatment program.<br />
A Care & Outcomes Summary Report should be completed and submitted to the WSIB whenever the<br />
worker leaves the Program of Care for any reason.<br />
Transition to Work<br />
Workers should be moved towards a safe transition to work as early as possible. Measures should be<br />
taken to prevent re-exposure to the workplace agent causing the dermatitis, either by removing the agent<br />
from the workplace, or the use of personal protective equipment, or the removal of the worker from<br />
exposure to the causative agent.<br />
Communication Requirements<br />
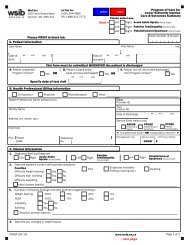
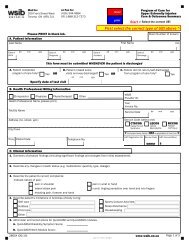
Standard WSIB Reporting Requirements<br />
Following the new onset of symptoms suggestive of contact dermatitis, the worker, employer, and first<br />
physician will complete the appropriate documentation to initiate the WSIB adjudication process. These<br />
forms include:<br />
• Form 6 (Worker’s Report of Injury/Disease) to be completed by the worker<br />
• Form 7 (Employer’s Report of Injury/Disease) to be completed by the employer<br />
• Program of Care Screening & Initial Assessment Report OR Health Professional’s Report<br />
(Form 8/8D).<br />
Program of Care Requirements<br />
Reporting of Health Status and Recovery<br />
Requirements for reporting the worker’s health status, progress, and outcomes include:<br />
Physician-completed assessments and report forms<br />
• Screening & Initial Assessment Report: baseline data collected to enable treatment planning<br />
• Reassessment Report: completed when the worker's needs dictate that he/she moves to another<br />
phase of care<br />
• Care & Outcomes Summary Report: a summary of the worker's achieved recovery, and when<br />
necessary, recommendations.<br />
The duration of the initial assessment and reassessment visits may vary and will be determined<br />
by the treating physician.<br />
14
Communication among workplace parties<br />
Communication is an important element in the success of the Program of Care and the health of<br />
the worker, and may include telephone conversations, written reports and one-on-one discussion with<br />
the ill worker.<br />
The frequency of communication will vary from case to case depending on the circumstances of the<br />
worker and the progress involved. Communication during the recovery and return to work process may<br />
include the following parties:<br />
• the ill worker<br />
• the treating physician and/or specialist<br />
• the employer<br />
• the WSIB service delivery team: adjudicator, nurse case manager, and medical consultant<br />
• other concurrent or future treatment providers.<br />
In order to facilitate return to work planning, it is extremely important that the physician contact the<br />
employer regarding the workers ability to return to work. Communication with the employer should occur<br />
when the screening and initial assessment is completed, when the worker is fit for work with modifications<br />
or limitations, or when the worker may return to regular work with no restrictions.<br />
If the worker is referred to a specialist (e.g. for ACD), it may not be possible to determine the<br />
workplace modifications or limitations upon completion of the screening and initial assessment.<br />
This information will be available following the specialist’s assessment.<br />
NOTE: Communication between the physician and the employer is restricted to discussion of the worker’s functional<br />
abilities unless the worker’s informed consent is obtained.<br />
15
Once a claim for benefits has been made, the Workplace Safety and Insurance Act gives the WSIB the<br />
authority to review any relevant report from a physician, hospital or health facility, or request a verbal report<br />
from such a person or facility without first obtaining the worker’s informed consent.<br />
Key communications and reporting should occur at certain times during the Program of Care:<br />
Timeframe<br />
Key Communications<br />
After first visit<br />
At 2-4 weeks and 2-week<br />
intervals until resolved<br />
At 6-8 week follow-up<br />
reassessment, at 3 and 6<br />
months, when necessary,<br />
and at discharge<br />
n complete and submit (within 24 to 48 hours) Screening & Initial<br />
Assessment Report to WSIB<br />
n ongoing discussion with worker throughout the Program of Care<br />
n contact employer<br />
n follow-up for workers with acute contact dermatitis<br />
n complete and submit Reassessment Report or Care & Outcomes<br />
Summary Report to WSIB<br />
n ongoing discussion with worker throughout the Program of Care<br />
n contact employer<br />
At any time before<br />
making referrals to allied<br />
health professionals<br />
n contact the WSIB to ensure that the claim is approved<br />
NOTE: This does not apply to referral of patients to specialists for diagnosis.<br />
Timely submission of the Screening & Initial Assessment Report, the Reassessment Report, and the<br />
Care & Outcomes Summary Report is essential. In addition, the WSIB should be contacted when:<br />
• the worker is not progressing as expected<br />
• the worker is referred to another health professional<br />
• medical or other complications arise that warrant further evaluation outside the Program of Care<br />
• any other issue arises.<br />
16
<strong>Reference</strong>s<br />
Hachen JP, De Paepe K, Vanpee E et al. Efficacy of<br />
topical corticosteroids in nickel-induced contact allergy.<br />
Clinical and Experimental model using a contact<br />
allergy patch test combined with TEWL<br />
measurements. Dermatology 2001; 202:314-319.<br />
Held E, Agner T. Effect of Moisturizers on Skin<br />
Susceptibility to Irritants. Acta Derm Venerol<br />
2001; 81: 104-107.<br />
Held E, et al. Prevention of work-related skin problems<br />
in student auxiliary nurses. An intervention study.<br />
Contact Dermatitis 2001; 44: 297-303.<br />
Held E, Lund H, Agner T. Effect of different moisturizers<br />
on SLS-irritated human skin. Contact Dermatitis<br />
2001; 44:229-234.<br />
Held E, Mygind K, Wolff C et al. Prevention of work<br />
related skin problems: an intervention study in wet work<br />
employees. Occup Environ Med 2002; 59: 556-561.<br />
Held E, Sveinsdottir S, Agner T. Effect of long-term use<br />
of moisturizer of skin hydration, barrier function and<br />
susceptibility to irritants. Acta Derm Venerol ( Stockh)<br />
1999; 79: 49-51.<br />
Lachapelle JM. Historical Aspects. In: Rycroft RJG,<br />
Menne T, Frosch PJ, Benezra C. Textbook of Contact<br />
Dermatitis. Springer-Verlag Berlin1992.<br />
Loden M. Barrier recovery and influence of irritant<br />
stimuli in skin treated with a moisturizing cream.<br />
Contact Dermatitis 1997; 36: 256-260.<br />
Marks JG, Belsito DV, Deleo V, et al. North American<br />
Contact Dermatitis group test results 1996-1998. Arcg<br />
Dermatol 2000; 136: 272.<br />
Quielle-Roussel C, Duteil L, Padilla JM et al. Objective<br />
assessment of topical anti-inflammatory drug activity on<br />
experimentally induced nickel contact dermatitis:<br />
comparison between visual scoring, colorimetry, laser<br />
Doppler velocimetry and transepidermal water loss.<br />
Skin Pharmacol 1990; 3: 248-255.<br />
Ramsing D and Agner T. Effect of glove occlusion on<br />
human skin (II). Contact Dermatitis 1996; 34: 258-262.<br />
Ramsing D and Agner T. Preventive and therapeutic<br />
affects of moisturizer. Acta Derm Venerol (Stockh)<br />
1997; 77: 335-337.<br />
Schleimann-Willers S et al. Natural vegetable fats in the<br />
prevention of irritant contact dermatitis. Contact<br />
Dermatitis 2002; 46: 6-12.<br />
Vidmar DA and Iwane MK. Assessment of the ability of<br />
the topical skin protectant (TSP) to protect against<br />
contact dermatitis to urushiol (Rhus) antigen. Am J<br />
Contact Dermatitis 1999; 10(4): 190-197.<br />
Wohrl S et al. A cream containing the chelator DTPA<br />
(diethylenetriaminepenta-acetic acid) can prevent<br />
contact allergic reactions to metals. Contact Dermatitis<br />
2001; 44: 334-228.<br />
Zhai H, Brachman F, Pelosi A et al. A bioengineering<br />
study on the efficacy of a skin protectant lotion in<br />
prevention SLS-induced dermatitis. Skin Research and<br />
Technology 2000; 6: 77-80.<br />
Zhai H, Schmid R, Levin C et al. Prevention and<br />
therapeutic effects of a model emulsion on gloveinduced<br />
irritation and dry skin in man. Occup Environ<br />
Med 2002; 50: 134-138.<br />
17<br />
Parmeix-Spake A, Goustas P, Green R. Eumovate<br />
(clobetasone butyrate) 0.05% cream with its<br />
moisturizing emollient base has better healing properties<br />
than hydrocortisone 1% cream: a study in nickel-induced<br />
contact dermatitis. J Dermatol Treat 2001; 12: 191-197.
APPENDIX A: WSIB Dermatitis Formulary<br />
Topical Corticosteroids in order of potency<br />
NOTE: The products listed were covered under the WSIB Drug Benefit Program at the time of publication.<br />
Products may be added or removed at any time.<br />
POTENCY GENERIC NAME TRADE NAME DIN<br />
Ultra High Beclomethasone Dipropionate 0.5% Diprolene cream 00688622<br />
(in propylene glycol base) Diprolene ointment 00629367<br />
Clobetasol Propionate 0.5% Clobetasol cream (Prempharm) 02230071<br />
Clobetasol ointment (Prempharm) 02230072<br />
Clobetasol scalp lotion (Prempharm) 02230073<br />
Clobetasol cream (Taro) 02245523<br />
Clobetasol ointment (Taro) 02245524<br />
Clobetasol solution (Taro) 02245522<br />
Dermovate cream 02213265<br />
Dermovate ointment 02213273<br />
Dermovate scalp lotion 02213281<br />
Gen-Clobetasol cream 02024187<br />
Gen-Clobetasol ointment 02026767<br />
Gen-Clobetasol scalp lotion 02216213<br />
Novo-Clobetasol cream 02093162<br />
Novo-Clobetasol ointment 02126192<br />
PMS-Clobetasol cream 02232191<br />
PMS-Clobetasol ointment 02232193<br />
PMS-Clobetasol solution 02232195<br />
Ratio-Clobetasol cream 01910272<br />
Ratio-Clobetasol ointment 01910280<br />
Ratio-Clobetasol lotion 01910299<br />
18
POTENCY GENERIC NAME TRADE NAME DIN<br />
High Amcinonide 0.l% Amcinonide cream 02247098<br />
Amcort cream 02246714<br />
Cyclocort cream 02192284<br />
Cyclocort ointment 02192268<br />
Cyclocort lotion 02192276<br />
Betamethasone Dipropionate 0.05% Diprosone cream 00323071<br />
Diprosone ointment 00344923<br />
Diprosone lotion 00417246<br />
Ratio-Topilene lotion 01927914<br />
Ratio-Topilene cream 00849650<br />
Ratio-Topilene ointment 00849669<br />
Ratio-Topisone ointment 00805009<br />
Ratio-Topisone lotion 00809187<br />
Rolene cream 02122073<br />
Rolene pommade 02122081<br />
Rolene lotion 02122065<br />
Rosone cream 02122049<br />
Rosone pommade 02122057<br />
Taro-sone cream 01925350<br />
Flucinonide 0.05% Lidemol cream 02163152<br />
Lidex cream 02161923<br />
Lidex ointment 02161966<br />
Lyderm cream 00716863<br />
Lyderm gel 02236997<br />
Lydonide cream 02187655<br />
Lydonide ointment 02187663<br />
Lydonide emollient cream 02187671<br />
Tiamol cream 00598933<br />
Topactin cream 00816132<br />
Topactin emollient cream 02240269<br />
Topsyn gel 02161974<br />
Halocinonide 0.l% Halog cream 02011921<br />
Halog ointment 02010283<br />
Halog solution 02010291<br />
19
POTENCY GENERIC NAME TRADE NAME DIN<br />
Medium Beclomethasone Dipropionate 0.025% Propaderm ointment 02089599<br />
Betamethasone Valerate 0.05%, 0.1% Betaderm 0.1% cream 00716626<br />
Betaderm 0.05% cream 00716618<br />
Betaderm 0.l% scalp lotion 00716634<br />
Betaderm 0.1% ointment 00716650<br />
Betaderm 0.05% ointment 00716642<br />
Betamethasone val 0.l% lotion 00726486<br />
Betnovate 0.1% lotion 02100193<br />
Celestoderm -V 0.l% cream 00027901<br />
Celestoderm-V/2 0.05% cream 00027898<br />
Celestoderm-V 0.l% ointment 00028363<br />
Celestoderm-V/2 0.05% ointment 00028355<br />
Ratio-Ectosone 0.1% cream 00535435<br />
Ratio-Ectosone 0.05% mild cream 00535427<br />
Ratio-Ectosone 0.05% mild lotion 00653209<br />
Ratio-Ectosone 0.1% scalp lotion 00653217<br />
Ratio-Ectosone 0.l% lotion 00750050<br />
Valisone scalp 0.l% lotion 00027944<br />
Clobetasone Butyrate 0.05% Eumovate cream 02214415<br />
Eumovate ointment 02214423<br />
Diflucortolone Valerate 0.l% Nerisone oily cream 00587818<br />
Nerisone cream 00587826<br />
Nerisone ointment 00587834<br />
Flumethasone Pivalate 0.03% Fluoderm 0.025% cream 00716790<br />
Fluoderm 0.01% cream 00716782<br />
Fluoderm 0.025% ointment 00716812<br />
Fluocinolone Acetonide 0.01%, 0.025% Synalar 0.025% cream 02162539<br />
Synalar 0.01% lotion 02162504<br />
Synamol 0.01% cream 02163489<br />
Mometasone Furoate 0.1% Elocom cream 00851744<br />
Elocom ointment 00851736<br />
Elocom lotion 00871095<br />
PMS-mometasone cream 02244767<br />
PMS-mometasone ointment 02244769<br />
PMS-mometasone lotion 02244768<br />
Triamcinolone Acetonide 0.01%, 025% Aristocort R cream 02194058<br />
Aristocort R ointment 02194031<br />
Kenalog 0.1% ointment 01999761<br />
Triaderm 0.025% cream 00716952<br />
Triaderm 0.01% cream 00716960<br />
Triaderm 0.01% ointment 00716987<br />
20
POTENCY GENERIC NAME TRADE NAME DIN<br />
Low Desonide Desocort 0.05% cream 02048639<br />
Desocort 0.05% ointment 02115522<br />
Desocort 0.05% lotion 02115514<br />
PMS-desonide 0.05% cream 02229315<br />
PMS-desonide 0.05% ointment 02229323<br />
Hydrocortisone Tridesilon 0.05% cream 02154862<br />
Tridesilon 0.05% ointment 02154870<br />
Cortate 0.5% cream 00513288<br />
Cortate 0.5% ointment 00513261<br />
Cortate l% cream 00502200<br />
Cortate l% ointment 00502197<br />
Cortoderm 0.5% ointment 00716685<br />
Cortoderm 1% ointment 00716693<br />
Emocort l% cream 00192597<br />
Emocort l% lotion 00192600<br />
Hydrocortisone 0.5% cream 00551953<br />
Hydrocortisone 1% cream 00551945<br />
Novo-hydrocort 0.5% cream 00461911<br />
Novo-hydrocort 1% cream 00461903<br />
Methylprednisolone Medrol Veriderm 0.25% cream 00031062<br />
21
Over The Counter Preparations<br />
NOTE: Over the counter products are not covered under the WSIB Drug Benefit Program at this time.<br />
CLASS GENERIC NAME TRADE NAME DIN<br />
Barrier Product Dimethicone Marathon Protective Barrier 02238789<br />
Cream 20%<br />
Baza Cleanse and Protect Lotion 2% 02243966<br />
Clean N Moist Spray 1.5% 02144638<br />
Barrier Crème 1.5% 02144522<br />
Therapeutic Lotion (unscented) 3% 02240213<br />
Dimethicone (in lipid base) Moisturel Lotion 3% 01909169<br />
Moisturel Cream l% 01909142<br />
Dimethicone (menthol) Gold Bond Extra Strength 02237563<br />
Lotion 5%<br />
Gold Bond Regular Strength 02237526<br />
Lotion 5%<br />
High Lipid Silicone Barriere Cream 20% 02060841<br />
Content<br />
Moisturizers Petrolatum Prevex Cream 67 (67%) 00635189<br />
Vaseline Petroleum Jelly (100%) 00365351<br />
White Petroleum Jelly USP (100%) 00741515<br />
White Petroleum Jelly BP (100%) 00600679<br />
22
Over the Counter Tar Preparations (containing at least 1% coal tar)<br />
NOTE: The use of these products may be appropriate for patients with atopic dermatitis and OCD.<br />
Over the counter tar preparations are not covered under the WSIB Drug Benefit Program at this time.<br />
COAL TAR ADDITIONAL<br />
STRENGTH INGREDIENTS TRADE NAME DIN<br />
Coal tar 1% Exorex gel 1-Eml –1 (gel emulsion) 02184672<br />
Exorex Formula 1% 00632295<br />
Neutrogena T/gel Extra 02238642<br />
Tersa Tar Mild shampoo 00632295<br />
Zetar Shampoo 02220393<br />
Coal tar 1.25% Psoriasin gel 02240152<br />
Coal tar 1.4% Tegrin Medicated Shampoo 01918990<br />
Coal tar 2% Doak Oil 2 00579955<br />
Exorex gel 2-EML-2 (gel emulsion) 02184680<br />
Salicylic acid 2%, Sulphur 2% Sterex Shampoo 00444448<br />
Coal tar 2.5% Balnetar Liquid 01908855<br />
Coal tar 3% Tersatar Shampoo 3% 00632309<br />
Coal tar 4% Salicylic acid 2% Medi-Dan Shampoo 00888591<br />
Pentrax Gold Shampoo 4 00864706<br />
Coal tar 5% Estar gel-5 01909185<br />
Salicylic acid 2% Tardan Shampoo 00266493<br />
Coal tar 7.5% Menthol 1.5% Denorex Medicated Shampoo-Regular 01942379<br />
Coal tar 8% Salicylic acid 2% P & S Plus Gel 00560448<br />
Salicylic acid 2%, Menthol 1% X-Tar Shampoo 00800694<br />
Coal tar 10% Doak oil Forte 00579971<br />
Targel 10% 00344508<br />
Salicylic acid 3% Targel SA 00510335<br />
Salicylic acid 4% Sebcur-T 00666114<br />
Salicylic acid 3%, Menthol 1% X-Seb T Plus Shampoo 00866601<br />
Salicylic acid 4% X-Seb T Extra Strength Shampoo 00509906<br />
Menthol 1.5% Denorex Medicated Shampoo 02106299<br />
Coal tar 20% Odans LCD 00358495<br />
Coal tar 40.8% Salicylic acid 1% Oxipor Lotion 02230134<br />
Coal tar 100% Tar distillate 100 00579963<br />
Tar Soaps Mazon Medicated Soap 0.5% 01981293<br />
Polytar Soap 00251372<br />
23
Notes<br />
24
© (WSIB) Workplace Safety and Insurance Board, 2003 Printed in Canada<br />
2855A 05/04