Health Care Collector - Kluwer Law International
Health Care Collector - Kluwer Law International
Health Care Collector - Kluwer Law International
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
PAGE7<br />
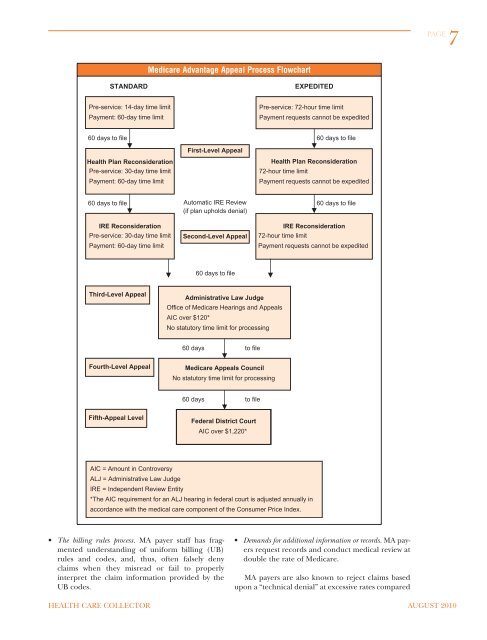
Medicare Advantage Appeal Process Flowchart<br />
STANDARD<br />
EXPEDITED<br />
Pre-service: 14-day time limit<br />
Payment: 60-day time limit<br />
Pre-service: 72-hour time limit<br />
Payment requests cannot be expedited<br />
60 days to file 60 days to file<br />
<strong>Health</strong> Plan Reconsideration<br />
Pre-service: 30-day time limit<br />
Payment: 60-day time limit<br />
First-Level Appeal<br />
<strong>Health</strong> Plan Reconsideration<br />
72-hour time limit<br />
Payment requests cannot be expedited<br />
60 days to file Automatic IRE Review<br />
60 days to file<br />
(if plan upholds denial)<br />
IRE Reconsideration<br />
Pre-service: 30-day time limit<br />
Payment: 60-day time limit<br />
Second-Level Appeal<br />
IRE Reconsideration<br />
72-hour time limit<br />
Payment requests cannot be expedited<br />
60 days to file<br />
Third-Level Appeal<br />
Administrative <strong>Law</strong> Judge<br />
Office of Medicare Hearings and Appeals<br />
AIC over $120*<br />
No statutory time limit for processing<br />
60 days to file<br />
Fourth-Level Appeal<br />
Medicare Appeals Council<br />
No statutory time limit for processing<br />
60 days to file<br />
Fifth-Appeal Level<br />
Federal District Court<br />
AIC over $1,220*<br />
AIC = Amount in Controversy<br />
ALJ = Administrative <strong>Law</strong> Judge<br />
IRE = Independent Review Entity<br />
*The AIC requirement for an ALJ hearing in federal court is adjusted annually in<br />
accordance with the medical care component of the Consumer Price Index.<br />
• The billing rules process. MA payer staff has fragmented<br />
understanding of uniform billing (UB)<br />
rules and codes, and, thus, often falsely deny<br />
claims when they misread or fail to properly<br />
interpret the claim information provided by the<br />
UB codes.<br />
• Demands for additional information or records. MA payers<br />
request records and conduct medical review at<br />
double the rate of Medicare.<br />
MA payers are also known to reject claims based<br />
upon a “technical denial” at excessive rates compared<br />
HEALTH CARE COLLECTOR AUGUST 2010