Ocular rosacea Crotoxin for paralysis of extraocular muscles ...
Ocular rosacea Crotoxin for paralysis of extraocular muscles ...
Ocular rosacea Crotoxin for paralysis of extraocular muscles ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
issn 0004-2749<br />
versão impressa<br />
A r q u i v o s b r a s i l e i r o s d e<br />
publicação <strong>of</strong>icial do conselho brasileiro de <strong>of</strong>talmologia<br />
SETEMBRO/OUTUBRO 2012<br />
75 05<br />
<strong>Ocular</strong> <strong>rosacea</strong><br />
<strong>Crotoxin</strong> <strong>for</strong> <strong>paralysis</strong> <strong>of</strong><br />
<strong>extraocular</strong> <strong>muscles</strong><br />
Pseudomonas endophthalmitis<br />
after phaco<br />
Radiation therapy <strong>for</strong> Graves<br />
Prevalence <strong>of</strong> blindness in<br />
Paraguay<br />
indexada nas bases de dados<br />
medline | embase | isi | SciELO
Arquivos Brasileiros de Oftalmologia | set-out 2012 | v.75 n.5 p.301-376
2013<br />
10<br />
AGOSTO<br />
92013<br />
82013<br />
AGOSTO<br />
72013<br />
AGOSTO<br />
AGOSTO<br />
www.<br />
cbo2013<br />
.com.br
Chegou!<br />
®<br />
(alcaftadina solução <strong>of</strong>tálmica 0,25%)<br />
Uso pediátrico: A partir de 2 anos. 1<br />
Rapidez de ação comprovada:<br />
Eficácia demonstrada em 3 minutos 2<br />
Comprovada ação durante todo o dia:<br />
Previne a coceira ocular durante<br />
16 horas 2<br />
Referências Bibliográficas: 1. LASTACAFT In<strong>for</strong>mações na bula. 2. Torkildsen G, Shedden A. The safety and effi cacy <strong>of</strong> alcaftadine 0.25% ophthalmic solution <strong>for</strong> the prevention <strong>of</strong> itching associated<br />
with allergic conjunctivitis. Curr Med Res Opin. 2011;27(3):623-631.<br />
INDICAÇÕES: LASTACAFT ® é indicado para pr<strong>of</strong>i laxia/prevenção do prurido associado com conjuntivites alérgicas. REAÇÕES ADVERSAS: Reação comum (> 1/100 e < 1/10): irritação ocular, ardor e/ou<br />
sensação de pontadas nos olhos à instilação, vermelhidão ocular, prurido ocular, rin<strong>of</strong>aringite, cefaleia e infl uenza. ADVERTÊNCIAS E PRECAUÇÕES: Para não contaminar o colírio evite o contato do conta<br />
gotas com qualquer superfície. Não permita que a ponta do frasco entre em contato direto com os olhos. Mantenha o frasco bem fechado enquanto não estiver sendo utilizado. Gestação e Lactação:<br />
Categoria de risco na gravidez: B. Este medicamento não deve ser utilizado por mulheres grávidas sem orientação médica ou do cirurgião-dentista. Estudos sobre reprodução realizados em ratos<br />
e coelhos não revelaram evidências de alteração na reprodução feminina ou perigos para o feto devidos à alcaftadina. Doses orais em ratos e coelhos de 20 e 80 mg/kg/dia, respectivamente, produziram<br />
níveis de exposição plasmática de aproximadamente 200 e 9000 vezes maior do que a exposição com a dose recomendada para uso ocular em humanos. Entretanto, não <strong>for</strong>am realizados estudos<br />
controlados em mulheres grávidas. Considerando que os estudos em animais nem sempre podem prever a resposta em humanos, este medicamento deve ser utilizado durante a gestação apenas se<br />
<strong>for</strong> claramente necessário. Não se sabe se esta substância é excretada no leite humano. Recomenda-se cautela quando LASTACAFT ® <strong>for</strong> administrado a mulheres durante a amamentação. Pacientes<br />
pediátricos: A efi cácia e segurança de LASTACAFT ® não <strong>for</strong>am estabelecidas em crianças com menos de 2 anos de idade. Pacientes idosos: Não <strong>for</strong>am observadas diferenças na segurança e efi cácia<br />
entre pacientes idosos e adultos mais jovens. Pacientes que utilizam lentes de contato: LASTACAFT ® não deve ser aplicado durante o uso de lentes de contato gelatinosas ou hidr<strong>of</strong>ílicas. Os pacientes<br />
devem ser instruídos a retirar as lentes antes da aplicação do colírio e aguardar pelo menos 10 minutos para recolocá-las após a aplicação de LASTACAFT ® . Os pacientes devem ser advertidos a não utilizar<br />
lentes de contato se seus olhos estiverem avermelhados. LASTACAFT ® não deve ser utilizado para o tratamento de irritação ocular relacionada ao uso de lentes de contato. Pacientes que utilizam mais<br />
de um medicamento <strong>of</strong>tálmico: Quando mais de um medicamento tópico <strong>of</strong>tálmico estiver sendo utilizando pelo paciente, deve ser respeitado o intervalo de pelo menos 5 minutos entre a administração<br />
dos medicamentos. POSOLOGIA: A dose usual é de 1 gota aplicada no(s) olho(s) afetado(s), uma vez ao dia. Para in<strong>for</strong>mações completas para prescrição, consultar a bula do produto ou a Allergan<br />
Produtos Farmacêuticos Ltda. VENDA SOB PRESCRIÇÃO MÉDICA. Reg. ANVISA/MS - 1.0147.0179.<br />
CONTRAINDICAÇÕES: LASTACAFT ® é contraindicado para pacientes que apresentam alergia a qualquer um dos componentes da sua fórmula.<br />
INTERAÇÕES MEDICAMENTOSAS: Não são conhecidas interações entre a alcaftadina e outras substâncias de uso tópico ocular.<br />
VENDA SOB PRESCRIÇÃO MÉDICA.<br />
www.allergan.com.br<br />
BR/0236/2012 ABR/2012
Olho Seco<br />
& Pós-Cirurgia Refrativa1<br />
Ronda Propaganda<br />
Alta capacidade de retenção de água 2,3<br />
- Con<strong>for</strong>to prolongado<br />
Visco-elástico 4<br />
- Impede a visão turva<br />
Muco-adesivo 2,4<br />
- Hidratação prolongada<br />
Melhora as propriedades de adesão intercelular 3,4<br />
Promove rápida cicatrização pós-cirurgias<br />
Ph e osmolaridade semelhantes<br />
às do filme lacrimal normal 2<br />
Mais con<strong>for</strong>to ao paciente<br />
Até<br />
8semanas de<br />
tratamento<br />
após a abertura<br />
Tratamento sintomático do olho seco<br />
Lubrificação e hidratação de lentes de contato 1<br />
Referências Bibliográficas: 1) Bula do produto: Hyabak. Registro MS nº 8042140002. 2) Snibson GR, Greaves JL, Soper ND, Tiffany JM, Wilson CG, Bron AJ. <strong>Ocular</strong> surface residence times <strong>of</strong> artificial tear solutions. Cornea. 1992 Jul;11(4):288-93. 3) Nakamura M, Hikida M. Nakano T, Ito S, Hamano T, Kinoshita S. Characterization <strong>of</strong> water retentive properties <strong>of</strong> hyaluronan. Cornea. 1993<br />
Sep;12(5):433-6. 4) Gomes JA, Amankwah R, Powell-Richards A, Dua HS. Sodium hyaluronate (hyaluronic acid) promotes migration <strong>of</strong> human corneal epithelial cells in vitro. Br J Ophthalmol. 2004 Jun;88(6);821-5.<br />
HYABAK ® . Solução sem conservantes para hidratação e lubrificação dos olhos e lentes de contacto. Frasco ABAK ® . COMPOSIÇÃO: Hialuronato de sódio 0,15g. Cloreto de sódio, trometamol, ácido clorídrico, água para preparações injetáveis q.b.p. 100 mL. NOME E MORADA DO FABRICANTE: Laboratoires Théa, 12 rue Louis Blériot, 63017 CLERMONT-FERRAND CEDEX<br />
2 - França. QUANDO SE DEVE UTILIZAR ESTE DISPOSITIVO: HYABAK ® contém uma solução destinada a ser administrada nos olhos ou nas lentes de contato. Foi concebido: • Para humedecimento e lubrificação dos olhos, em caso de sensações de secura ou de fadiga ocular induzidas por fatores exteriores, tais como, o vento, o fumo, a poluição, as poeiras, o calor seco, o ar<br />
condicionado, uma viagem de avião ou o trabalho prolongado à frente de uma tela de computador. • Nos utilizadores de lentes de contato, permite a lubrificação e a hidratação da lente, com vista a facilitar a colocação e a retirada, e proporcionando um con<strong>for</strong>to imediato na utilização ao longo de todo o dia. Graças ao dispositivo ABAK ® , HYABAK ® permite <strong>for</strong>necer gotas de solução sem<br />
conservantes. Pode, assim, ser utilizado com qualquer tipo de lente de contato. A ausência de conservantes permite igualmente respeitar os tecidos oculares. ADVERTÊNCIAS E PRECAUÇÕES ESPECIAIS DE UTILIZAÇÃO: • Evitar tocar nos olhos com a ponta do frasco. • Não injetar, não engolir. Não utilize o produto caso o invólucro de inviolabilidade esteja danificado. MANTER FORA<br />
DO ALCANCE DAS CRIANÇAS. INTERAÇÕES: É conveniente aguardar 10 minutos entre a administração de dois produtos oculares. COMO UTILIZAR ESTE DISPOSITIVO: POSOLOGIA: 1 gota em cada olho durante o dia, sempre que necessário. Nos utilizadores de lentes: uma gota em cada lente ao colocar e retirar as lentes e também sempre que necessário ao longo do dia. MODO<br />
E VIA DE ADMINISTRAÇÃO: INSTILAÇÃO OCULAR. STERILE A - Para uma utilização correta do produto é necessário ter em conta determinadas precauções: • Lavar cuidadosamente as mãos antes de proceder à aplicação. • Evitar o contato da extremidade do frasco com os olhos ou as pálpebras. Instilar 1 gota de produto no canto do saco lacrimal inferior, puxando ligeiramente a<br />
pálpebra inferior para baixo e dirigindo o olhar para cima. O tempo de aparição de uma gota é mais longo do que com um frasco clássico. Tapar o frasco após a utilização. Ao colocar as lentes de contato: instilar uma gota de HYABAK ® na concavidade da lente. FREQUÊNCIA E MOMENTO EM QUE O PRODUTO DEVE SER ADMINISTRADO: Distribuir as instilações ao longo do dia,<br />
con<strong>for</strong>me necessário. CONSERVAÇÃO DE DISPOSITIVO: NÃO EXCEDER O PRAZO LIMITE DE UTILIZAÇÃO, INDICADO NA EMBALAGEM EXTERIOR. PRECAUÇÕES ESPECIAIS DE CONSERVAÇÃO: Conservar a uma temperatura inferior a 25ºC. Depois de aberto, o frasco não deve ser conservado mais de 8 semanas. Registro MS nº 8042140002.<br />
Produzido em Outubro/2012<br />
UNIÃO QUÍMICA FARMACÊUTICA NACIONAL S/A<br />
Divisão GENOM<br />
Unidade Brasília: Trecho 01 Conjunto 11 Lote 6 a 12<br />
Pólo de Desenvolvimento JK<br />
Santa Maria - Brasília - DF - CEP: 72549-555
Restaura<br />
o con<strong>for</strong>to<br />
ao piscar 1<br />
Pode ser usado<br />
com lentes<br />
de contato 1 15 mL 10 mL<br />
Alívio imediato e prolongado do ardor e da secura ocular 1<br />
Sem riscos de lesões induzidas pelos conservantes 2,3<br />
Nova<br />
Apresentação<br />
Referências Bibliográficas: 1) Bula do Produto: Lacrifilm ® . 2) Noecker R. Ophthalmic preservatives: considerations <strong>for</strong> long-term use in patients with dry eye or glaucoma. Rev Ophthalmol 2001; June: 1-10. 3) Chalmers RL. Hydrogen peroxide in anterior segment physiology: a literature review. Optom Vis<br />
Sci 1989;66:796-803.7.<br />
Lacrifilm ® . (carmelose sódica). Solução Oftálmica Estéril. FORMA FARMACÊUTICA E APRESENTAÇÃO: Solução Oftálmica Estéril 5mg/mL: embalagem contendo frasco de 10 mL ou 15 mL. USO ADULTO. USO OFTÁLMICO. COMPOSIÇÃO: Cada<br />
mL contém: carmelose sódica-5 mg . Veículo: cloreto de sódio, fosfato de sódio, ácido bórico, perborato de sódio, ácido clorídrico e água para injetáveis. INFORMAÇÕES AO PACIENTE. AÇÃO ESPERADA DO MEDICAMENTO: Lacrifilm ® é uma solução<br />
que apresenta composição muito semelhante à composição das lágrimas naturais. Este medicamento é indicado para melhorar a irritação, ardor e secura ocular, que podem ser causados pela exposição ao vento, sol, calor, ar seco, e para melhorar o<br />
descon<strong>for</strong>to que pode estar associado com a utilização de lentes de contato. REAÇÕES ADVERSAS: In<strong>for</strong>me seu médico o aparecimento de reações desagradáveis. TODO MEDICAMENTO DEVE SER MANTIDO FORA DO ALCANCE DAS CRIANÇAS.<br />
CONTRAINDICAÇÕES E PRECAUÇÕES: Lacrifilm ® é contraindicado nos casos de alergia a qualquer componente do medicamento. NÃO USE REMÉDIO SEM O CONHECIMENTO DO SEU MÉDICO, PODE SER PERIGOSO PARA A SAÚDE.<br />
INDICAÇÕES: Lacrifilm ® é indicado para melhorar a irritação, ardor e secura ocular, que podem ser causados pela exposição ao vento, sol, calor, ar seco, e também como protetor contra irritações oculares. É também indicado como lubrificante e reumidificante<br />
durante o uso de lentes de contato. CONTRAINDICAÇÕES: O produto está contraindicado nos casos de alergia a qualquer componente do medicamento. PRECAUÇÕES E ADVERTÊNCIAS: Evite o contato do conta-gotas do frasco com<br />
qualquer superfície para evitar contaminação. Não permitir que a ponta do frasco entre em contato direto com os olhos. Mantenha a tampa do frasco bem fechada após o seu uso. Manter o produto <strong>for</strong>a do alcance das crianças. Armazenar em temperatura<br />
ambiente. Em caso de aparecimento de dor, alterações da visão, ou se ocorrer piora ou persistência da vermelhidão, ou da irritação dos olhos, por mais de 72h após início de uso do produto, descontinuar o tratamento e procurar auxílio médico. Não utilizar<br />
o produto se ocorrer modificação da coloração da solução ou se a solução se tornar turva. Produto de uso exclusivo em adultos. O uso em crianças representa risco à saúde. INTERAÇÕES MEDICAMENTOSAS: Não são conhecidas interações com<br />
outros medicamentos. REAÇÕES ADVERSAS: Não <strong>for</strong>am detectadas reações adversas com o uso do Lacrifilm ® . POSOLOGIA: Aplicar 1 a 2 gotas no(s) olhos(s) afetado(s), tantas vezes quantas <strong>for</strong>em necessárias. SIGA CORRETAMENTE O MODO<br />
DE USAR, NÃO DESAPARECENDO OS SINTOMAS PROCURE ORIENTAÇÃO MÉDICA. Registro MS - 1.0497.1289.<br />
CONTRAINDICAÇÕES: o produto está contraindicado em pacientes com história de hipersensibilidade a qualquer<br />
componente da fórmula. INTERAÇÃO MEDICAMENTOSA: não se conhecem interações medicamentosas.<br />
“LACRIFILM ®<br />
É UM MEDICAMENTO. SEU USO PODE TRAZER RISCOS. PROCURE O MÉDICO E O FARMACÊUTICO. LEIA A BULA.”<br />
Material destinado exclusivamente à classe médica.<br />
Produzido em: Fevereiro/2013 Ronda Propaganda
PUBLICAÇÃO OFICIAL DO<br />
CONSELHO BRASILEIRO<br />
DE OFTALMOLOGIA<br />
CODEN - AQBOAP<br />
PUBLICAÇÃO OFICIAL DO CONSELHO BRASILEIRO DE OFTALMOLOGIA<br />
Publicação ininterrupta desde 1938<br />
ISSN 0004-2749<br />
(Versão impressa)<br />
ISSN 1678-2925<br />
(Versão eletrônica)<br />
Periodicidade: bimestral Arq Bras Oftalmol. São Paulo, v. 75, n. 5, p. 301-376, set./out. 2012<br />
Conselho Administrativo<br />
Marco Antônio Rey de Faria<br />
Harley E. A. Bicas<br />
Roberto Lorens Marback<br />
Rubens Bel<strong>for</strong>t Jr.<br />
Wallace Chamon<br />
Editor-Chefe<br />
Wallace Chamon<br />
Editores Anteriores<br />
Waldemar Bel<strong>for</strong>t Mattos<br />
Rubens Bel<strong>for</strong>t Mattos<br />
Rubens Bel<strong>for</strong>t Jr.<br />
Harley E. A. Bicas<br />
Augusto Paranhos Jr.<br />
Carlos Ramos de Souza Dias<br />
Eduardo Melani Rocha<br />
Eduardo Sone Soriano<br />
Galton Carvalho Vasconcelos<br />
Haroldo Vieira de Moraes Jr.<br />
José Álvaro Pereira Gomes<br />
Editores Associados<br />
Luiz Alberto S. Melo Jr.<br />
Mário Luiz Ribeiro Monteiro<br />
Michel Eid Farah<br />
Norma Allemann<br />
Paulo Schor<br />
Rodrigo Pessoa Cavalcanti Lira<br />
Sérgio Felberg<br />
Suzana Matayoshi<br />
Nacional<br />
Áisa Haidar Lani (Campo Grande-MS)<br />
Ana Luísa Höfling-Lima (São Paulo-SP)<br />
André Augusto Homsi Jorge (Ribeirão Preto-SP)<br />
André Messias (Ribeirão Preto-SP)<br />
Antonio Augusto Velasco e Cruz (Ribeirão Preto-SP)<br />
Arnaldo Furman Bordon (São Paulo-SP)<br />
Ayrton Roberto B. Ramos (Florianópolis-SC)<br />
Breno Barth (Natal-RN)<br />
Carlos Roberto Neufeld (São Paulo-SP)<br />
Carlos Teixeira Brandt (Recife-PE)<br />
Cristina Muccioli (São Paulo-SP)<br />
Denise de Freitas (São Paulo-SP)<br />
Eduardo Cunha de Souza (São Paulo-SP)<br />
Eduardo Ferrari Marback (Salvador-BA)<br />
Enyr Saran Arcieri (Uberlândia-MG)<br />
Érika Hoyama (Londrina-PR)<br />
Fábio Ejzenbaum (São Paulo-SP)<br />
Fábio Henrique C. Casanova (São Paulo-SP)<br />
Fausto Uno (São Paulo-SP)<br />
Flávio Jaime da Rocha (Uberlândia-MG)<br />
Ivan Maynart Tavares (São Paulo-SP)<br />
Jair Giampani Jr. (Cuiabá-MT)<br />
Jayter Silva de Paula (Ribeirão Preto-SP)<br />
João Borges Fortes Filho (Porto Alegre-RS)<br />
João Carlos de Miranda Gonçalves (São Paulo-SP)<br />
João J. Nassaralla Jr. (Goiânia-GO)<br />
João Luiz Lobo Ferreira (Florianópolis-SC)<br />
José Américo Bonatti (São Paulo-SP)<br />
José Augusto Alves Ottaiano (Marília-SP)<br />
Conselho Editorial<br />
José Beniz Neto (Goiânia-GO)<br />
José Paulo Cabral Vasconcellos (Campinas-SP)<br />
Keila Miriam Monteiro de Carvalho (Campinas-SP)<br />
Luís Paves (São Paulo-SP)<br />
Luiz V. Rizzo (São Paulo-SP)<br />
Marcelo Francisco Gaal Vadas (São Paulo-SP)<br />
Marcelo Jordão Lopes da Silva (Ribeirão Preto-SP)<br />
Marcelo Vieira Netto (São Paulo-SP)<br />
Maria Cristina Nishiwaki Dantas (São Paulo-SP)<br />
Maria de Lourdes V. Rodrigues (Ribeirão Preto-SP)<br />
Maria Rosa Bet de Moraes e Silva (Botucatu-SP)<br />
Marinho Jorge Scarpi (São Paulo-SP)<br />
Marlon Moraes Ibrahim (Franca-SP)<br />
Martha Maria Motono Chojniak (São Paulo-SP)<br />
Maurício Maia (Assis-SP)<br />
Mauro Campos (São Paulo-SP)<br />
Mauro Goldchmit (São Paulo-SP)<br />
Mauro Waiswol (São Paulo-SP)<br />
Midori Hentona Osaki (São Paulo-SP)<br />
Milton Ruiz Alves (São Paulo-SP)<br />
Mônica Alves (Campinas-SP)<br />
Mônica Fialho Cronemberger (São Paulo-SP)<br />
Moysés Eduardo Zajdenweber (Rio de Janeiro-RJ)<br />
Newton Kara-José Júnior (São Paulo-SP)<br />
Norma Helen Medina (São Paulo-SP)<br />
Paulo E. Correa Dantas (São Paulo-SP)<br />
Paulo Ricardo de Oliveira (Goiânia-GO)<br />
Procópio Miguel dos Santos (Brasília-DF)<br />
Renato Curi (Rio de Janeiro-RJ)<br />
Roberto L. Marback (Salvador-BA)<br />
Roberto Pedrosa Galvão Fº (Recife-PE)<br />
Roberto Pinto Coelho (Ribeirão Preto-SP)<br />
Rosane da Cruz Ferreira (Porto Alegre-RS)<br />
Rubens Bel<strong>for</strong>t Jr. (São Paulo-SP)<br />
Sérgio Kwitko (Porto Alegre-RS)<br />
Sidney Júlio de Faria e Souza (Ribeirão Preto-SP)<br />
Silvana Artioli Schellini (Botucatu-SP)<br />
Suel Abujamra (São Paulo-SP)<br />
Tomás Fernando S. Mendonça (São Paulo-SP)<br />
Vera Lúcia D. Monte Mascaro (São Paulo-SP)<br />
Walter Yukihiko Takahashi (São Paulo-SP)<br />
Internacional<br />
Alan B. Scott (E.U.A.)<br />
Andrew Lee (E.U.A.)<br />
Baruch D. Kuppermann (E.U.A.)<br />
Bradley Straatsma (E.U.A.)<br />
Careen Lowder (E.U.A.)<br />
Cristian Luco (Chile)<br />
Emílio Dodds (Argentina)<br />
Fernando M. M. Falcão-Reis (Portugal)<br />
Fernando Prieto Díaz (Argentina)<br />
James Augsburger (E.U.A.)<br />
José Carlos Cunha Vaz (Portugal)<br />
José C. Pastor Jimeno (Espanha)<br />
Marcelo Teixeira Nicolela (Canadá)<br />
Maria Amélia Ferreira (Portugal)<br />
Maria Estela Arroyo-Illanes (México)<br />
Miguel N. Burnier Jr. (Canadá)<br />
Pilar Gomez de Liaño (Espanha)<br />
Richard L. Abbott (E.U.A.)<br />
Zélia Maria da Silva Corrêa (E.U.A.)<br />
ABO – Arquivos Brasileiros de Oftalmologia • publicação bimestral do Conselho Brasileiro de Oftalmologia (CBO)<br />
Redação: R. Casa do Ator, 1.117 - 2º andar - Vila Olímpia - São Paulo - SP - CEP 04546-004<br />
Fone: (55 11) 3266-4000 - Fax: (55 11) 3171-0953 - E-mail: abo@cbo.com.br - Home-page: www.scielo.br/abo<br />
Assinaturas - Brasil:<br />
Membros do CBO: Distribuição gratuita.<br />
Não Membros: Assinatura anual: R$ 500,00<br />
Fascículos avulsos: R$ 80,00<br />
Foreign: Annual subscription: US$ 200.00<br />
Single issue: US$ 40.00<br />
Editor: Wallace Chamon<br />
Gerente Comercial: Mauro Nishi<br />
Secretaria Executiva: Claudete N. Moral<br />
Claudia Moral<br />
Revisão Final: Paulo Mitsuru Imamura<br />
Editoria Técnica: Edna Terezinha Rother<br />
Maria Elisa Rangel Braga<br />
Capa: Ipsis<br />
Publicação:<br />
Divulgação:<br />
Tiragem:<br />
Ipsis Gráfica e Editora S.A.<br />
Conselho Brasileiro de Oftalmologia<br />
7.450 exemplares<br />
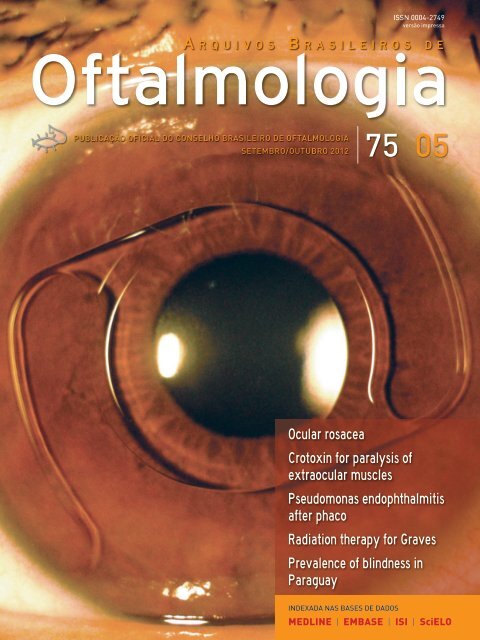
Capa: Fotografia em lâmpada de fenda de paciente fácico com implante de lente intraocular rígida de PMMA de suporte<br />
angular em câmara anterior (Baik<strong>of</strong>f ). Pós-operatório de 15 anos. Autor da Fotografia: Norma Allemann (Pr<strong>of</strong>essora do De par -<br />
tamento de Oftalmologia da UNIFESP).<br />
Cover: Slit-lamp photograph <strong>of</strong> a phakic patient with rigid PMMA, angle-supported, anterior chamber, intraocular lens (Baik<strong>of</strong>f ).<br />
Postoperative follow-up <strong>of</strong> 15 years. Photographer: Norma Allemann (Pr<strong>of</strong>essor <strong>of</strong> the Department <strong>of</strong> Ophthalmology-UNIFESP).
PUBLICAÇÃO OFICIAL DO<br />
CONSELHO BRASILEIRO<br />
DE OFTALMOLOGIA<br />
PUBLICAÇÃO OFICIAL DO CONSELHO BRASILEIRO DE OFTALMOLOGIA<br />
ISSN 0004-2749<br />
(Versão impressa)<br />
ISSN 1678-2925<br />
(Versão eletrônica)<br />
• ABO<br />
Arquivos Brasileiros de Oftalmologia<br />
www.abonet.com.br<br />
www.freemedicaljournals.com<br />
www.scielo.org<br />
• Copernicus<br />
www.copernicusmarketing.com<br />
www.periodicos.capes.gov.br<br />
www.scirus.com<br />
• ISI Web <strong>of</strong> Knowledge (SM)<br />
• MEDLINE<br />
• LILACS<br />
Literatura Latino-americana<br />
em Ciências da Saúde<br />
Diretoria do CBO - 2011-2013<br />
Marco Antônio Rey de Faria (Presidente)<br />
Milton Ruiz Alves (Vice-Presidente)<br />
Carlos Heler Ribeiro Diniz (1º Secretário)<br />
Nilo Holzchuh (Secretário Geral)<br />
Mauro Nishi (Tesoureiro)<br />
Sociedades Filiadas ao Conselho Brasileiro de Oftalmologia<br />
e seus respectivos Presidentes<br />
Centro Brasileiro de Estrabismo<br />
Sociedade Brasileira de Administração em Oftalmologia<br />
Sociedade Brasileira de Catarata e Implantes Intra-<strong>Ocular</strong>es<br />
Sociedade Brasileira de Cirurgia Plástica <strong>Ocular</strong><br />
Sociedade Brasileira de Cirurgia Refrativa<br />
Sociedade Brasileira de Ecografia em Oftalmologia<br />
Sociedade Brasileira de Glaucoma<br />
Sociedade Brasileira de Laser e Cirurgia em Oftalmologia<br />
Sociedade Brasileira de Lentes de Contato, Córnea e Refratometria<br />
Sociedade Brasileira de Oftalmologia Pediátrica<br />
Sociedade Brasileira de Oncologia em Oftalmologia<br />
Sociedade Brasileira de Retina e Vítreo<br />
Sociedade Brasileira de Trauma <strong>Ocular</strong><br />
Sociedade Brasileira de Uveítes<br />
Sociedade Brasileira de Visão Subnormal<br />
Maria de Lourdes Fleury F. Carvalho Tom Back<br />
Flávio Rezende Dias<br />
Armando Stefano Crema<br />
Ricardo Mörschbacher<br />
Renato Ambrósio Júnior<br />
Norma Allemann<br />
Vital Paulino Costa<br />
Caio Vinicius Saito Regatieri<br />
César Lipener<br />
Rosa Maria Graziano<br />
Priscilla Luppi Ballalai Bordon<br />
Walter Yukihiko Takahashi<br />
Nilva Simeren Bueno Moraes<br />
Wilton Feitosa de Araújo<br />
Mayumi Sei<br />
Apoio:
PUBLICAÇÃO OFICIAL DO<br />
CONSELHO BRASILEIRO<br />
DE OFTALMOLOGIA<br />
PUBLICAÇÃO OFICIAL DO CONSELHO BRASILEIRO DE OFTALMOLOGIA ISSN 0004-2749<br />
(Versão impressa)<br />
ISSN 1678-2925<br />
(Versão eletrônica)<br />
Periodicidade: bimestral Arq Bras Oftalmol. São Paulo, v. 75, n. 5, p. 301-376, set./out. 2012<br />
Sumário | Contents<br />
305<br />
306<br />
Editorial | Editorial<br />
Neste fascículo dos ABO<br />
In this issue <strong>of</strong> the ABO<br />
Wallace Chamon<br />
In this issue <strong>of</strong> the ABO<br />
Neste fascículo dos ABO<br />
Wallace Chamon<br />
307<br />
313<br />
316<br />
320<br />
324<br />
333<br />
Artigos Originais | Original Articles<br />
Study <strong>of</strong> crotoxin on the induction <strong>of</strong> <strong>paralysis</strong> in <strong>extraocular</strong> muscle in animal model<br />
Estudo da crotoxina na indução de paralisia da musculatura <strong>extraocular</strong> em modelo animal<br />
Geraldo de Barros Ribeiro, Henderson Celestino de Almeida, David Toledo Velarde, Maria Lygia Vaz de Melo Sá<br />
Alterações retinianas em jovens portadores de anemia falci<strong>for</strong>me (hemoglobinopatias) em hospital universitário<br />
no nordeste do Brasil<br />
Retinal impairment in young individuals with sickle cell anemia (hemoglobin ss disease) in university hospital in northeastern <strong>of</strong> Brazil<br />
Allisson Mário dos Santos, Gustavo Baptista de Almeida Faro, Marcus Vinicius Melo do Amaral, Cristiano de Queiroz Mendonça,<br />
Bruno Campelo Leal, Rosana Cipolotti<br />
Effect <strong>of</strong> aspherical and yellow tinted intraocular lens on blue-on-yellow perimetry<br />
Efeito das lentes intraoculares asféricas e com pigmentação amarela na campimetria azul-amarelo<br />
Rodrigo França de Espíndola, Marcony Rodrigues de Santhiago, Newton Kara-Júnior<br />
Reproducibility <strong>of</strong> peripapillary retinal nerve fiber layer thickness measurements using Spectral Domain OCT<br />
in Brazilian patients<br />
Reprodutibilidade da espessura da camada de fibras nervosas da retina utilizando-se o Spectral Domain OCT em pacientes brasileiros<br />
Daniela Araújo Toscano, Marcos Pereira de Ávila, Maria Regina Catai Chalita<br />
Radiation therapy <strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized controlled trials<br />
Radioterapia para <strong>of</strong>talmopatia de Graves: uma revisão sistemática e meta-análise de ensaios clínicos randomizados e controlados<br />
Gustavo Arruda Viani, André Campiolo Boin, Ligia Issa De Fendi, Ellen Carrara Fonseca, Eduardo Jose Stefano, Jayter Silva de Paula<br />
Cancelamento de cirurgias de catarata em um hospital público de referência<br />
Cancellation <strong>of</strong> cataract surgery in a public hospital<br />
Micheli Patrícia de Fátima Magri, Rodrigo França de Espíndola, Marcony Rodrigues de Santhiago, Elisabeth Frolich Mercadante, Newton Kara Júnior
337<br />
341<br />
344<br />
348<br />
Implantação do exame do reflexo vermelho em crianças da região do Hospital das Clínicas da Faculdade de Medicina<br />
de Botucatu - SP - Brasil<br />
Implementation <strong>of</strong> red reflex exam in children in the area <strong>of</strong> Botucatu Medical School Clinical Hospital - São Paulo, Brazil<br />
Antonio Carlos Lottelli Rodrigues, Rodrigo Bueno Prado, Licério Miguel<br />
Prevalence and causes <strong>of</strong> blindness in an urban area <strong>of</strong> Paraguay<br />
Prevalência e causas de cegueira em uma população urbana do Paraguai<br />
Fernando Yaacov-Peña, David Jure, José Ocampos, Margarita Samudio, João Marcello Furtado, Marissa Carter, Van Charles Lansingh<br />
An outbreak <strong>of</strong> <strong>for</strong>ty five cases <strong>of</strong> Pseudomonas aeruginosa acute endophthalmitis after phacoemulsification<br />
Surto de quarenta e cinco casos de end<strong>of</strong>talmite aguda por Pseudomonas aeruginosa após facoemulsificação<br />
Ricardo Luz Leitão Guerra, Bruno de Paula Freitas, Cintia Maria Felix Medrado Parcero, Otacílio de Oliveira Maia Júnior, Roberto Lorens Marback<br />
Phacoemulsification and foldable acrylic IOL implantation in children with treated retinoblastoma<br />
Facoemulsificação e implante de lente intraocular acrílica dobrável em crianças com retinoblastoma<br />
Marcia Beatriz Tartarella, Gloria Fátima Britez-Colombi, Marcia Motono, Martha Motono Chojniak, Joao Borges Fortes Filho, Rubens Bel<strong>for</strong>t Jr.<br />
352<br />
356<br />
358<br />
361<br />
Relatos de Casos | Case Reports<br />
Síndrome de Waardenburg - aspectos <strong>of</strong>talmológicos e critérios de diagnóstico: relatos de casos<br />
Waardenburg syndrome - ophthalmic findings and criteria <strong>for</strong> diagnosis: case reports<br />
Luciano Sólia Nasser, Lívia Maris Ribeiro Paranaíba, Ana Cláudia Frota, Andreia Gomes, Gisele Versiani, Hercílio Martelli Júnior<br />
Optical coherence tomography image in gelatinous drop-like corneal dystrophy: case report<br />
Tomografia de coerência óptica na distr<strong>of</strong>ia corneana gelatinosa em gotas: relato de caso<br />
Otávio de Azevedo Magalhães, Samuel Rymer, Diane Ruschel Marinho, Sérgio Kwitko, Isabel Habeyche Cardoso, Lúcia Kliemann<br />
Esclerite posterior associada à oclusão da veia central da retina e edema macular cistoide: relato de caso<br />
Posterior scleritis associated with central retinal vein occlusion and cystoid macular edema: case report<br />
Roger Wada Kamei<br />
Buphthalmos development in adult: case report<br />
Buftalmus em adulto: relato de caso<br />
Mônica Alves, Leonardo Tannus Malki, Eduardo Melani Rocha<br />
363<br />
Artigos de Revisão | Review Articles<br />
<strong>Ocular</strong> <strong>rosacea</strong> - a review<br />
Rosácea ocular - revisão<br />
Ana Carolina Cabreira Vieira, Ana Luisa Höfling-Lima, Mark J Mannis<br />
370<br />
Cartas ao Editor | Letters to the Editor<br />
Axonal electrovisiogram or inverse photopic skin electroretinogram?<br />
Eletrovisograma axonal ou eletrorretinograma fotópico inverso de pele?<br />
Katharina Messias, Vinicius Monteiro de Castro, Florian Gekeler, Andre Messias<br />
373 Instruções para os Autores | Instructions to Authors
Editorial | Editorial<br />
Neste fascículo dos ABO<br />
In this issue <strong>of</strong> the ABO<br />
Wallace Chamon<br />
Vários artigos originais e inéditos de grande importância clínica estão publicados nesse fascículo dos ABO,<br />
demonstrando que, cada vez mais, os autores reconhecem a qualidade e abrangência da nossa revista.<br />
A publicação com a maior casuística de end<strong>of</strong>talmite aguda por Pseudomonas aeruginosa do mundo (1) revelou<br />
que 20% dos 45 olhos submetidos à vitrectomia apresentaram acuidade visual pelo menos igual a 20/200.<br />
Apesar da fonte do surto não ter sido identificada, todos os pacientes haviam sido submetidos à cirurgia de<br />
catarata por facoemulsificação em uma mesma instituição em um período determinado de dois dias. Isso induz à<br />
conclusão que a fonte tenha sido intraoperatória e faz com que os leitores questionem os métodos antissépticos<br />
atualmente utilizados nas cirurgias <strong>of</strong>talmológicas.<br />
Mais uma vez o tema da medicina baseada em evidências é abordado nos ABO. A revisão sistemática dos<br />
riscos e benefícios da radioterapia, associada ou não ao uso de glicocorticoides, para o tratamento da <strong>of</strong>talmopatia<br />
de Graves apresentada nesse fascículo é a mais completa já publicada na literatura mundial (2) . Os autores<br />
identificaram 359 artigos científicos sobre o assunto nas diversas fontes de dados e selecionaram os únicos oito<br />
que eram estudos clínicos controlados, aleatorizados e com dados disponíveis. Com a meta-análise dos 439 pacientes<br />
envolvidos neste estudos, os autores concluíram que a radioterapia, especialmente quando associada ao<br />
uso de glicocorticoides, é efetiva na fase ativa da doença e deve ser indicada nos estágios mais iniciais da mesma.<br />
Dois relatos de casos inéditos mundialmente são apresentados nesse fascículo: o primeiro relato de buftalmo<br />
em adulto (3) e a primeira publicação de imagens de tomografia de coerência óptica (OCT) da distr<strong>of</strong>ia corneana<br />
gelatinosa em gotas (4) . O primeiro faz com que os leitores questionem a importância da avaliação elasticidade<br />
escleral em diferentes fases da vida e em diferentes doenças, enquanto o segundo apresenta uma excelente<br />
correlação das imagens de OCT com a anatomia patológica, incluindo a típica birrefringência em luz polarizada<br />
observada nessa distr<strong>of</strong>ia.<br />
A prevalência das causas de cegueira no Paraguai, foi avaliada em um estudo epidemiológico realizado por<br />
instituições paraguaias em colaboração com autores de instituições norte-americanas e da Agência Internacional<br />
para Prevenção da Cegueira (IAPB) (5) . Os autores detectaram uma menor prevalência de deficiência visual em<br />
relação ao único estudo populacional prévio do mesmo país, realizado em 2003 (6) . A importância deste artigo<br />
reside no fato que, apesar de quase 10% das pessoas com cegueira bilateral viverem nas Américas, estudos<br />
<strong>of</strong>talmológicos populacionais, metodologicamente adequados, são infrequentes na América Latina (7) .<br />
Ainda neste fascículo <strong>for</strong>am descritos, pela primeira vez, os efeitos de uma neurotoxina isolada do veneno<br />
de uma cobra sul-americana nos músculos oculares extrínsecos (8) . A crotoxina foi aplicada no músculo reto superior<br />
de coelhos e comparada com a toxina botulínica tipo A. Os autores concluíram que, quando utilizada na<br />
concentração de 1,5 µg, o efeito da crotoxina foi similar ao da toxina botulínica tipo A.<br />
Referências<br />
1. Guerra RLL, Freitas BP, Parcero CMFM, Maia Jr OO, Marback RL. An outbreak <strong>of</strong> <strong>for</strong>ty<br />
five cases <strong>of</strong> Pseudomonas aeruginosa acute endophthalmitis after phacoemulsification.<br />
Arq Bras Oftalmol. 2012;75(5):344-7.<br />
2. Viani GA, Boin AC, de Fendi LI, Fonseca EC, Stefano EJ, de Paula JS. Radiation therapy<br />
<strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized<br />
controlled trials. Arq Bras Oftalmol. 2012;75(5):324-32.<br />
3. Alves M, Malki LT, Rocha EM. Buphthalmos development in adult: case report. Arq Bras<br />
Oftalmol. 2012;75(5):361-2.<br />
4. Magalhães OA, Rymer S, Marinho DR, Kwitko S, Cardoso IH, Kliemann L. Optical coherence<br />
tomography image in gelatinous drop-like corneal dystrophy: case report. Arq<br />
Bras Oftalmol. 2012;75(5):356-7.<br />
5. Yaacov-Peña F, Jure D, Ocampos J, Samudio M, Furtado JM, Carter MJ, Lansingh VC.<br />
Prevalence and causes <strong>of</strong> blindness in an urban area <strong>of</strong> Paraguay. Arq Bras Oftalmol.<br />
2012;75(5):341-3.<br />
6. Duerksen R, Limburg H, Carron JE, Foster A. Cataract blindness in Paraguay results <strong>of</strong><br />
a national survey. Ophthalmic Epidemiol. 2003;10(5):349 -57.<br />
7. Pascolini D, Mariotti SP. Global estimates <strong>of</strong> visual impairment - 2010. Br J Ophthalmol.<br />
2012;96(5):614-8.<br />
8. Ribeiro GB, Almeida HC, Velaverde DT, Sá MLVM. Study <strong>of</strong> crotoxin on the induction <strong>of</strong><br />
para lysis in <strong>extraocular</strong> muscle in animal model. Arq Bras Oftalmol. 2012;75(5):307-12.<br />
Submetido para publicação: 5 de outubro de 2012<br />
Aceito para publicação: 5 de outubro de 2012<br />
1<br />
Médico, Departamento de Oftalmologia, Escola Paulista de Medicina - EPM, Universidade Federal<br />
de São Paulo - UNIFESP - São Paulo (SP), Brasil.<br />
Financiamento: Não houve financiamento para este trabalho.<br />
Divulgação de potenciais conflitos de interesse: W.Chamon, Nenhum.<br />
Arq Bras Oftalmol. 2012;75(5):305<br />
305
Editorial | Editorial<br />
In this issue <strong>of</strong> the ABO<br />
Neste fascículo dos ABO<br />
Wallace Chamon<br />
Several original and unpublished articles <strong>of</strong> great clinical importance are published in this issue <strong>of</strong> the ABO,<br />
showing that, increasingly, the authors recognize the quality and comprehensiveness <strong>of</strong> our journal.<br />
A publication with the highest incidence <strong>of</strong> infectious endophthalmitis by Pseudomonas aeruginosa in the<br />
world (1) revealed that 20% <strong>of</strong> the 45 eyes that underwent vitrectomy presented visual acuity <strong>of</strong> at least 20/200.<br />
Although the source <strong>of</strong> the outbreak has not been identified, all patients had undergone cataract surgery by<br />
phacoemulsification in a single institution in a given period <strong>of</strong> two days. This leads to the conclusion that it was<br />
an intraoperative source and <strong>for</strong>ces readers to question the antiseptic methods currently used in eye surgery.<br />
Again the theme <strong>of</strong> evidence-based medicine is covered in ABO. A systematic review <strong>of</strong> the risks and benefits<br />
<strong>of</strong> radiotherapy, with or without the use <strong>of</strong> glucocorticoids, <strong>for</strong> the treatment <strong>of</strong> Graves’ ophthalmopathy presented<br />
in this issue is the most comprehensive ever published in the world literature (2) . The authors identified 359<br />
scientific articles on the subject in the various data sources and selected the eight ones that were randomized<br />
controlled trials, with data available. With the meta-analysis <strong>of</strong> 439 patients involved in these studies, the authors<br />
concluded that radiotherapy, especially when associated with glucocorticoid treatment, is effective in the active<br />
phase <strong>of</strong> the disease and must be indicated in the earlier stages <strong>of</strong> the same.<br />
Two unpublished case reports are presented in this issue: the first report <strong>of</strong> buphthalmos in adult (3) and the<br />
first publication <strong>of</strong> optical coherence tomography (OCT) images <strong>of</strong> gelatinous drop-like corneal dystrophy (4) . The<br />
first makes readers question the importance <strong>of</strong> assessing scleral elasticity in different stages <strong>of</strong> life and in different<br />
diseases, while the second shows an excellent correlation with the OCT images and pathology, including the<br />
typical birefringence under polarized light observed in this dystrophy.<br />
The prevalence <strong>of</strong> the causes <strong>of</strong> blindness in Paraguay, was evaluated in an epidemiological study conducted<br />
by Paraguayan institutions in collaboration with authors from U.S. institutions and from the International Agency<br />
<strong>for</strong> Prevention <strong>of</strong> Blindness (IAPB) (5) . The authors found a lower prevalence <strong>of</strong> visual impairment in relation the<br />
only previous population-based study from the same country, in 2003 (6) . The importance <strong>of</strong> this paper lies in<br />
the fact that, although almost 10% <strong>of</strong> people with bilateral blindness live in the Americas, methodologically<br />
appropriate, ophthalmic population-based studies are infrequent in Latin America (7) .<br />
Also in this issue, it has been described, <strong>for</strong> the first time, the effects <strong>of</strong> a neurotoxin isolated from the venom<br />
<strong>of</strong> a South American rattlesnake in the external ocular <strong>muscles</strong> (8) . The crotoxin was applied to the superior rectus<br />
muscle <strong>of</strong> rabbits and compared with botulinum toxin type A. The authors concluded that, when used at a<br />
concentration <strong>of</strong> 1.5 µg, the effect <strong>of</strong> the crotoxin was similar to botulinum toxin type A.<br />
ReferENCES<br />
1. Guerra RLL, Freitas BP, Parcero CMFM, Maia Jr OO, Marback RL. An outbreak <strong>of</strong> <strong>for</strong>ty<br />
five cases <strong>of</strong> Pseudomonas aeruginosa acute endophthalmitis after phacoemulsification.<br />
Arq Bras Oftalmol. 2012;75(5):344-7.<br />
2. Viani GA, Boin AC, de Fendi LI, Fonseca EC, Stefano EJ, de Paula JS. Radiation therapy<br />
<strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized<br />
controlled trials. Arq Bras Oftalmol. 2012;75(5):324-32.<br />
3. Alves M, Malki LT, Rocha EM. Buphthalmos development in adult: case report. Arq Bras<br />
Oftalmol. 2012;75(5):361-2.<br />
4. Magalhães OA, Rymer S, Marinho DR, Kwitko S, Cardoso IH, Kliemann L. Optical coherence<br />
tomography image in gelatinous drop-like corneal dystrophy: case report. Arq<br />
Bras Oftalmol. 2012;75(5):356-7.<br />
5. Yaacov-Peña F, Jure D, Ocampos J, Samudio M, Furtado JM, Carter MJ, Lansingh VC.<br />
Prevalence and causes <strong>of</strong> blindness in an urban area <strong>of</strong> Paraguay. Arq Bras Oftalmol.<br />
2012;75(5):341-3.<br />
6. Duerksen R, Limburg H, Carron JE, Foster A. Cataract blindness in Paraguay results <strong>of</strong><br />
a national survey. Ophthalmic Epidemiol. 2003;10(5):349 -57.<br />
7. Pascolini D, Mariotti SP. Global estimates <strong>of</strong> visual impairment - 2010. Br J Ophthalmol.<br />
2012;96(5):614-8.<br />
8. Ribeiro GB, Almeida HC, Velaverde DT, Sá MLVM. Study <strong>of</strong> crotoxin on the induction <strong>of</strong><br />
<strong>paralysis</strong> in <strong>extraocular</strong> muscle in animal model. Arq Bras Oftalmol. 2012;75(5):307-12.<br />
Submitted <strong>for</strong> publication: October 5, 2012<br />
Accepted <strong>for</strong> publication: October 5, 2012<br />
1<br />
Physician, Department <strong>of</strong> Ophthalmology, Escola Paulista de Medicina - EPM, Universidade Federal<br />
de São Paulo - UNIFESP - São Paulo (SP), Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potencial <strong>of</strong> interest: W.Chamon, None.<br />
306 Arq Bras Oftalmol. 2012;75(5):306
Artigo Original | Original Article<br />
Study <strong>of</strong> crotoxin on the induction <strong>of</strong> <strong>paralysis</strong> in <strong>extraocular</strong> muscle in animal model<br />
Estudo da crotoxina na indução de paralisia da musculatura <strong>extraocular</strong> em modelo animal<br />
Geraldo de Barros Ribeiro 1 , Henderson Celestino de Almeida 2 , David Toledo Velarde 3 , Maria Lygia Vaz de Melo Sá 4<br />
ABSTRACT<br />
Purpose: <strong>Crotoxin</strong> is the major toxin <strong>of</strong> the venom <strong>of</strong> the South American rattlesnake<br />
Crotalus durissus terrificus, capable <strong>of</strong> causing a blockade <strong>of</strong> the neurotransmitters at<br />
the neuromuscular junction. The objective <strong>of</strong> this study was to appraise the action<br />
and effectiveness <strong>of</strong> the crotoxin induced <strong>paralysis</strong> <strong>of</strong> the <strong>extraocular</strong> muscle and to<br />
compare its effects with the botulinum toxin type A (BT-A).<br />
Methods: The crotoxin, with LD50 <strong>of</strong> 1.5 μg, was injected into the superior rectus<br />
muscle in ten New Zealand rabbits. The concentration variance was 0.015 up to 150 μg.<br />
Two rabbits received 2 units <strong>of</strong> botulinum toxin type A <strong>for</strong> comparative analysis. The<br />
evaluation <strong>of</strong> the <strong>paralysis</strong> was per<strong>for</strong>med using serial electromyography. After the<br />
functional recovery <strong>of</strong> the <strong>muscles</strong>, which occurred after two months, six rabbits were<br />
sacrificed <strong>for</strong> anatomopathology study.<br />
Results: The animals did not show any evidence <strong>of</strong> systemic toxicity. Transitory ptosis<br />
was observed in almost every animal and remained up to fourteen days. These toxins<br />
caused immediate blockade <strong>of</strong> the electrical potentials. The recovery was gradual in<br />
the average <strong>of</strong> one month with regeneration signs evident on the electromyography.<br />
The <strong>paralysis</strong> effect <strong>of</strong> the crotoxin on the muscle was proportional to its concentration.<br />
The changes with 1.5 μg crotoxin were similar to those produced by the botulinum<br />
toxin type A. The histopathology findings were localized to the site <strong>of</strong> the injection.<br />
No signs <strong>of</strong> muscle fiber’s necrosis were seen in any sample. The alterations induced<br />
by crotoxin were also proportional to the concentration and similar to botulinum<br />
toxin type A in concentration <strong>of</strong> 1.5 μg.<br />
Conclusion: <strong>Crotoxin</strong> was able to induce transitory <strong>paralysis</strong> <strong>of</strong> the superior rectus<br />
muscle. This effect was characterized by reduction <strong>of</strong> action potentials and non-specific<br />
signs <strong>of</strong> fibrillation. <strong>Crotoxin</strong>, in concentration <strong>of</strong> 1.5 μg was able to induce similar<br />
effects as botulinum toxin type A.<br />
Keywords: <strong>Crotoxin</strong>/administration & dosage; Crotalid venoms; Snakes; Botulinum<br />
toxins, type A/administration & dosage; Cobra neurotoxin proteins; Ophthalmople -<br />
gia/chemically induced; Neuromuscular junction; Comparative study<br />
RESUMO<br />
Objetivo: A crotoxina é a principal toxina do veneno da cobra cascavel sul-americana<br />
Crotalus durissus terrificus e causa bloqueio da neurotransmissão na junção neuromuscular.<br />
O objetivo deste estudo foi avaliar a ação e aplicabilidade da crotoxina na indução<br />
de paralisia da musculatura extrínseca ocular, e comparar seus efeitos com os da toxina<br />
botulínica do tipo A (TB-A).<br />
Métodos: A crotoxina, com DL50 de 1,5 μg, foi aplicada no músculo reto superior direito<br />
de dez coelhos da raça neozelandesa, em concentrações que variaram de 0,015 μg a<br />
150 μg. Em dois coelhos, utilizou-se 2 unidades de toxina botulínica do tipo A para análise<br />
comparativa. A avaliação da paralisia foi realizada através de eletromiografia seriada.<br />
Após a recuperação, que ocorreu em dois meses, seis coelhos <strong>for</strong>am sacrificados para<br />
estudo anátomopatológico.<br />
Resultados: Os animais não apresentaram sinais de intoxicação sistêmica. Ptose palpebral<br />
transitória foi observada em quase todos os animais e permaneceu por até 14 dias. As<br />
toxinas causaram um bloqueio imediato da captação dos potenciais elétricos. A recuperação<br />
foi gradativa no período aproximado de um mês, observando-se sinais evidentes<br />
de regeneração no registro eletromiográfico. Os efeitos da crotoxina na paralização do<br />
músculo injetado <strong>for</strong>am proporcionais à concentração. A crotoxina, na concentração<br />
de 1,5 μg, induziu alterações semelhantes às da toxina botulínica do tipo A. Os achados<br />
anátomo-patológicos <strong>for</strong>am localizados somente na região em que se aplicou as toxinas,<br />
não havendo necrose de fibras musculares em nenhuma amostra analisada. As alterações<br />
causadas pela crotoxina também <strong>for</strong>am proporcionais à concentração utilizada e similares<br />
a toxina botulínica do tipo A na concentração de 1,5 μg.<br />
Conclusão: A crotoxina foi capaz de induzir paralisia transitória do músculo reto superior.<br />
Este efeito foi caracterizado pela redução na amplitude dos potenciais de ação e sinais<br />
inespecíficos de fibrilação. Observou-se que a ação da crotoxina, em concentração de 1,5 μg,<br />
proporcionou efeito semelhante ao da toxina botulínica do tipo A.<br />
Descritores: <strong>Crotoxin</strong>a/administração e dosagem; Venenos de crotalídeos; Serpentes;<br />
Toxinas botulínicas tipo A/administração e dosagem; Proteínas neurotóxicas de elapídeos;<br />
Oftalmolplegia/induzido quimicamente; Junção neuromuscular; Estudo comparativo<br />
INTRODUCTION<br />
<strong>Crotoxin</strong> is a b-neurotoxin, isolated from the poison <strong>of</strong> South<br />
American rattlesnake Crotalus durissus terrificus (1) . This toxin is a noncovalent<br />
oligomer, <strong>for</strong>med by two subunits: one acid and the other<br />
basic. The latter has phospholipase A2 activity and is neurotoxic, while<br />
the acid subunit is enzymatically and pharmacologically inactive, but<br />
it highly increases the toxicity <strong>of</strong> the basic subunit (2,3) . The acid subunit<br />
acts as a helper to the basic subunit, giving it specificity and increasing<br />
its stability. <strong>Crotoxin</strong> has molecular weight <strong>of</strong> 23.5KDa. Its basic<br />
subunit has molecular weight <strong>of</strong> 14.3 KDa and isoelectric point 8.9. It<br />
is <strong>for</strong>med by a single polypeptide branch with 123 amino acids. The<br />
acid subunit has molecular weight <strong>of</strong> 9.2 KDa and isoelectric point 3.8,<br />
and it is <strong>for</strong>med by three polypeptides (a,b,¡) linked by seven disulfide<br />
bridges (3-5) . Both crotoxin subunits behave in a synergic manner, but<br />
dissociate when they interact with synaptic membranes. The basic<br />
portion remains attached to the membrane, while the acid portion<br />
is released into solution. The binding <strong>of</strong> the basic portion to synaptic<br />
membranes is not specific, and it can also bind to other membranes,<br />
while the acid portion does not attach. While in association to the<br />
basic portion, the acid subunit enhances its pharmacological action,<br />
Submitted <strong>for</strong> publication: October 11, 2011<br />
Accepted <strong>for</strong> publication: August 12, 2012<br />
Study carried out at Strabismus Clinic at São Geraldo Hospital <strong>of</strong> Universidade Federal de Minas<br />
Gerais - UFMG - Belo Horizonte (MG) - Brazil<br />
1<br />
Physician, Strabismus Service, Universidade Federal de Minas Gerais - UFMG - Belo Horizonte<br />
(MG) - Brazil.<br />
2<br />
Teacher, Universidade Federal de Minas Gerais - UFMG - Belo Horizonte (MG) - Brazil.<br />
3<br />
Biochemist, Hospital Foundation <strong>of</strong> Minas Gerais State - Fhemig - Belo Horizonte (MG) - Brazil.<br />
4<br />
Physician, Institute <strong>of</strong> Clinical Neurophysiology <strong>of</strong> Minas Gerais, Belo Horizonte (MG) - Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: G.B.Ribeiro, inventor in patent UFMG (Universidade<br />
Federal de Minas Gerais) involving the use <strong>of</strong> crotoxin in humans; H.C.Almeida, inventor in patent<br />
UFMG (Universidade Federal de Minas Gerais) involving the use <strong>of</strong> crotoxin in humans; D.T.Velarde,<br />
inventor in patent UFMG (Universidade Federal de Minas Gerais) involving the use <strong>of</strong> crotoxin in<br />
humans; M.L.V.M.Sá, None.<br />
Correspondence address: Geraldo de Barros Ribeiro, Av. Silviano Brandão, 1600 - Belo Horizonte -<br />
MG - 30015-015 - Brazil - E-mail: gbarrosribeiro@gmail.com<br />
Arq Bras Oftalmol. 2012;75(5):307-12<br />
307
Study <strong>of</strong> crotoxin on the induction <strong>of</strong> <strong>paralysis</strong> in <strong>extraocular</strong> muscle in animal model<br />
by significantly reducing the non-specific binding (3-5) . <strong>Crotoxin</strong> blocks<br />
the release <strong>of</strong> neurotransmitter at the presynaptic motor end-plate (6) .<br />
Based on the crotoxin effect as a neuromuscular blocker, we decided<br />
to verify the possibility <strong>of</strong> using it to induce <strong>extraocular</strong> muscle<br />
<strong>paralysis</strong> in rabbits. The objectives <strong>of</strong> this study were: to evaluate the<br />
capacity <strong>of</strong> crotoxin to induce <strong>extraocular</strong> muscle <strong>paralysis</strong> in rabbits,<br />
analyze the duration <strong>of</strong> <strong>extraocular</strong> muscle <strong>paralysis</strong> induced by<br />
crotoxin; observe the duration and possible side effects <strong>of</strong> crotoxin at<br />
different concentrations through electromyography and anatomopathology<br />
exams, and finally compare crotoxin to botulinum toxin<br />
type A (BT-A).<br />
METHODS<br />
All procedures were conducted according to Brazilian Law n o<br />
6.638, May 1979. This law established regulations <strong>for</strong> the scientificdidactic<br />
practices <strong>of</strong> animal vivisection. It <strong>for</strong>esees that research<br />
should be realized always in a manner that does not cause any<br />
suffering to animals involved.<br />
In this study, 12 new-Zealand rabbits were used, with average<br />
weight <strong>of</strong> 2.5 kg. Rabbits were divided in 6 groups, with 2 rabbits<br />
in each group. <strong>Crotoxin</strong> dose initially used was based on the comparison<br />
<strong>of</strong> minimum lethal dose (LD50) <strong>of</strong> crotoxin and botulinum<br />
toxin type A in mice (1) .<br />
<strong>Crotoxin</strong> used had a LD50 <strong>of</strong> 1.5 μg. Toxicity was determined<br />
by minimum lethal dose in 50% <strong>of</strong> injected animals (LD50), using<br />
conventional Swiss mice, with weights from 18 to 22 g.<br />
Based on these calculations, it was decided to use different<br />
concentrations <strong>of</strong> crotoxin. Doses ranged from one hundred times<br />
smaller to one hundred times larger than the estimated DL50 <strong>of</strong><br />
crotoxin.<br />
One group received 2 units <strong>of</strong> botulinum toxin type A (Botox ® ).<br />
<strong>Crotoxin</strong> and botulinum toxin type A were injected into the<br />
right superior rectus muscle <strong>of</strong> each rabbit, with an insulin syringe<br />
(Unijet, Plascalp Produtos Cirúrgicos Ltda., Feira de Santana, BA). The<br />
best place <strong>for</strong> injection was evaluated through electromyography.<br />
Injection was done after instillation <strong>of</strong> 0.5% proximetacaine<br />
chloride anesthesic eye drop (Anestalcon®-Alcon Laboratórios<br />
do Brasil, São Paulo, SP) and under direct visualization <strong>of</strong> the supe -<br />
rior rectus muscle. Needle was introduced transconjunctivally and<br />
inserted into the muscle. Injection was made into superior rectus<br />
muscle 4mm behind to the muscle insertion. Injected volume was<br />
100μl, except in rabbit n o 12, which received a volume <strong>of</strong> 50 μl. Solution<br />
applied in rabbit n o 12 contained a concentration <strong>of</strong> 150 μg in<br />
100μl: that means this rabbit received half the dose <strong>of</strong> rabbit n o 11.<br />
The dose applied in each rabbit was:<br />
Group I > Rabbits 1 and 2 > 0.015 μg crotoxin<br />
Group II > Rabbits 3 and 4 > 0.15 μg crotoxin<br />
Group III > Rabbits 5 and 6 > 1.5 μg crotoxin<br />
Group IV > Rabbits 7 and 8 > 2 U <strong>of</strong> botulinum toxin type A<br />
(BT-A (Botox®)<br />
Group V > Rabbits 9 and 10 > 15 μg crotoxin<br />
Group VI > Rabbits 11 and 12 > 150 μg crotoxin and 75 μg<br />
crotoxin (respectively)<br />
Rabbits were accompanied daily in the first week, watching <strong>for</strong> local<br />
and systemic side effects. Analysis <strong>of</strong> possible systemic side effects<br />
was done through observation <strong>of</strong> animal behavior. Laboratory testing<br />
to evaluate liver and kidney functions were not done. Afterwards,<br />
observation <strong>of</strong> animals was done twice a week until the end <strong>of</strong> the<br />
experiment. The evaluation <strong>of</strong> toxin effects was done through electromyography<br />
exams, and was done 2, 9, 16, 23 and 60 days after the<br />
injections. After the last electromyographic exam, one animal <strong>of</strong> each<br />
group was sacrificed <strong>for</strong> anatomopathology studies.<br />
Electromyographic exams were done in the Institute <strong>of</strong> Clinical<br />
Neurophysiology <strong>of</strong> Minas Gerais, in Belo Horizonte. Animals received<br />
3 drops <strong>of</strong> 0.5% proximetacaine chloride eye drop (Anestalcon ® -<br />
Alcon Laboratórios do Brasil, São Paulo, SP, Brasil) be<strong>for</strong>e the exam.<br />
Electromyograph used was a Neuropack Four Mini Evoked Potential<br />
Measuring System MEB-5304K (Nihon Kohden, Tokio, Japan).<br />
A concentric bipolar electrode was used, with platinum central wire<br />
and stainless steel cannula. Length <strong>of</strong> electrode was 37 mm; needle<br />
had 0.46mm diameter, and a record area <strong>of</strong> 0.07 mm (Teca Corporation,<br />
catalogue number 53156, New York, USA). One hook-and-loop<br />
fastener tape (Teca Corporation, catalogue number GE-V, New York,<br />
USA), soaked in saline solution, was put around the ears <strong>of</strong> the rabbits<br />
<strong>for</strong> grounding the system.<br />
Animals were sacrificed through intracardiac injection <strong>of</strong> 0.75%<br />
bupivacaine hydrochloride (Cristália Produtos Químicos Farmacêuticos<br />
Ltda., Itapira, SP, Brasil) after the last electromyographic exam.<br />
The right orbit <strong>of</strong> odd numbered rabbits, each one representing one<br />
group studied, was carefully exenterated and processed <strong>for</strong> histopathology<br />
exams.<br />
<strong>Crotoxin</strong> used in this research was given by Immunobiological<br />
Division <strong>of</strong> Ezequiel Dias Foundation <strong>of</strong> Belo Horizonte - MG (FUNED).<br />
<strong>Crotoxin</strong> was obtained in its pure <strong>for</strong>m and after lyophilization, was<br />
dissolved in saline buffer and afterwards its toxicity was evaluated<br />
through LD50 testing in mice. Toxicity <strong>of</strong> this solution was determined<br />
through LD50 testing in mice with 18 to 22 grams, intraperitoneally.<br />
Male and female mice were used, in groups <strong>of</strong> 8 animals per<br />
dose, with reading after 48 hours.<br />
RESULTS<br />
Rabbits tolerated well the experiment, not showing any behavior<br />
alteration after the injection <strong>of</strong> both toxins. One day after the toxins<br />
injection, only rabbit 4 did not have blepharoptosis; the other animals<br />
had discrete ptosis, which lasted <strong>for</strong> two days in rabbits 1, 2, 3, 5 and<br />
6, and seven days in rabbits 7, 11 and 12. Rabbit 8 had the longest<br />
duration <strong>of</strong> ptosis: fourteen days. Conjunctival hyperemia on the site<br />
<strong>of</strong> injection was discrete in rabbits 1, 2, 3, 4, 7 and 8, lasting less than<br />
48 hours and moderate in rabbits 5 and 6, gradually improving in seven<br />
days. Rabbit 11 had the strongest reaction: besides conjunctival<br />
reaction, there was corneal edema, which improved after 14 days,<br />
but also produced permanent leukoma in the affected cornea. This<br />
lesion may have no relation to the application, because its location<br />
was distant from the area <strong>of</strong> injection.<br />
Results <strong>of</strong> electromyography<br />
Electromyographic (EMG) exams in superior recti <strong>muscles</strong> <strong>of</strong> all<br />
animals were normal be<strong>for</strong>e the injections, and they were repeated<br />
with 2, 9, 16, 23 and 58 days.<br />
Results are divided in four tables according to days <strong>of</strong> follow-up<br />
(Tables 1 to 4).<br />
At the fifty-eighth day <strong>of</strong> follow-up, the electromyography records<br />
were practically normal in all animals.<br />
Results <strong>of</strong> anatomo-pathology study<br />
The right orbit <strong>of</strong> six rabbits, one from each group, was exenterated<br />
<strong>for</strong> histological study 70 days after the injection <strong>of</strong> crotoxin or<br />
botulinum toxin type A. In all groups, alterations found in the superior<br />
rectus muscle were located 4 to 5mm posterior to the scleral muscle<br />
insertion and observed only at the site <strong>of</strong> injection.<br />
In group I (0.015 μg crotoxin), there was a discrete endomysial<br />
fibrosis on the injected area, the remaining muscle being normal. In<br />
group II (0.15 μg crotoxin), endomysial fibrosis slightly more evident<br />
than in group I. In group III (1.5 μg crotoxin), more evident local<br />
lesions as: discrete chronic inflammation, characterized by discrete<br />
lymphocytic mononuclear histiocytic infiltrate, myophagocytosis and<br />
edema with endomysial fibrosis, fibers with degenerative phenomena<br />
(vacuolated) and signs <strong>of</strong> muscle fibers regeneration (centralization <strong>of</strong><br />
nuclei) (Figure 3).<br />
308 Arq Bras Oftalmol. 2012;75(5):307-12
Ribeiro GB, et al.<br />
Table 1. EMG with two days <strong>of</strong> follow-up<br />
Results <strong>of</strong> electromyographic exams<br />
Group I 0.015 μg crotoxin There were not any observable signs <strong>of</strong> irritability <strong>of</strong> neuromuscular membrane.<br />
Observed contraction potentials had normal amplitude and duration, with no significant alterations in fiber recruitment, which was only incomplete.<br />
Group II 0.15 μg crotoxin Although potentials were under expected limits, the amplitudes were smaller when compared to potentials <strong>of</strong> the smaller dose.<br />
Group III 1.5 μg crotoxin Although the signs <strong>of</strong> membrane irritability were not present, potentials obtained were rare and <strong>of</strong> diminished amplitude. Findings suggested<br />
a blockade <strong>of</strong> conduction between fibers.<br />
Group IV 2 U BT-A There were signs <strong>of</strong> irritability <strong>of</strong> neuromuscular sheaths at rest due to blockade <strong>of</strong> neuromuscular joint conduction. There was no response<br />
<strong>of</strong> fibers and no evidence <strong>of</strong> contraction <strong>of</strong> motor units. The presence <strong>of</strong> fibrillation potentials could indicate a functional denervation.<br />
Group V 15 μg crotoxin No signs <strong>of</strong> membrane irritability, but the rare potentials detected were <strong>of</strong> low amplitude, as if fibers were destroyed or blocked to stimulus<br />
response.<br />
Group VI<br />
150 μg crotoxin<br />
75 μg crotoxin<br />
There was a complete silence in electromyography records.<br />
Table 2. EMG with nine days <strong>of</strong> follow-up<br />
Results <strong>of</strong> electromyographic exams<br />
Group I 0.015 μg crotoxin Action potentials were normal and with no signs <strong>of</strong> irritability (instability <strong>of</strong> membranes).<br />
Group II 0.15 μg crotoxin Similar activity as group I.<br />
Group III 1.5 μg crotoxin Signs <strong>of</strong> irritability were not present, but the detection <strong>of</strong> potentials (that are normal) showed that few motor units had response, such as<br />
happens to group IV.<br />
Group IV 2 U BT-A Signs <strong>of</strong> irritability <strong>of</strong> membrane remain, but with rare normal potentials during contraction.<br />
Group V 15 μg crotoxin Non-specific signs <strong>of</strong> irritability are present, but during contraction there were signs <strong>of</strong> asynchronous recruitment <strong>of</strong> motor units (polyphasic).<br />
Group VI<br />
150 μg crotoxin<br />
75 μg crotoxin<br />
In rabbit 11, which received a volume <strong>of</strong> 100 µl, the main characteristic is the complete absence <strong>of</strong> potentials, with signs <strong>of</strong> non-specific<br />
irritability in rest.<br />
In rabbit 12, which received 50 µl, irritability is lower and, despite the existence <strong>of</strong> functional units, they are rare.<br />
Table 3. EMG with sixteen days <strong>of</strong> follow-up<br />
Results <strong>of</strong> electromyographic exams<br />
Group I 0.015 μg crotoxin Action potentials were normal.<br />
Group II 0.15 μg crotoxin Similar activity as group I.<br />
Group III 1.5 μg crotoxin Normal potentials during contraction, with more intense signs <strong>of</strong> irritability.<br />
Group IV 2 U BT-A Signs <strong>of</strong> neuromuscular irritability were more intense, and potentials with normal amplitude and duration during contraction, associated<br />
to long polyphasic potentials, characterizing asynchronous recruitment process, typical <strong>of</strong> recent reinnervation. Although the pattern <strong>of</strong><br />
recruitment was not normal, there was no rarefaction in response.<br />
Group V 15 μg crotoxin Normal potentials, with signs <strong>of</strong> recent reinnervation.<br />
Group VI<br />
150 μg crotoxin<br />
75 μg crotoxin<br />
Normal potentials during contraction, but the number <strong>of</strong> motor units was reduced.<br />
Table 4. EMG with twenty days <strong>of</strong> follow-up<br />
Results <strong>of</strong> electromyographic exams<br />
Group I 0.015 μg crotoxin Normal potentials and recruitment.<br />
Group II 0.15 μg crotoxin Signs <strong>of</strong> irritability were not present and, during contraction, units were in normal quantity, but there were signs <strong>of</strong> asynchronous recruitment,<br />
typical <strong>of</strong> reinnervation.<br />
Group III 1.5 μg crotoxin Some non-specific signs <strong>of</strong> irritability remained, and present motor units were reduced (figure 1)<br />
Group IV 2 U BT-A Signs <strong>of</strong> irritability were not present, and motor units presented normal amplitude and duration during contraction. The pattern <strong>of</strong> interference<br />
was still incomplete, but there were not long duration polyphasics (asynchrony), which indicated that the process <strong>of</strong> regeneration<br />
was complete (Figure 2).<br />
Group V 15 μg crotoxin Normal potentials during contraction, with intense signs <strong>of</strong> irritability and signs <strong>of</strong> asynchronous recruitment.<br />
Group VI<br />
150 μg crotoxin<br />
75 μg crotoxin<br />
Signs <strong>of</strong> neuromuscular irritability associated with long duration polyphasic potentials, which indicated process <strong>of</strong> asynchronous recruitment,<br />
typical <strong>of</strong> recent reinnervation.<br />
Arq Bras Oftalmol. 2012;75(5):307-12<br />
309
Study <strong>of</strong> crotoxin on the induction <strong>of</strong> <strong>paralysis</strong> in <strong>extraocular</strong> muscle in animal model<br />
In group IV (2 U BT-A), anatomo-pathology alterations were similar<br />
to those found in group III (Figure 4).<br />
In group V (15 μg crotoxin), degenerated fibers (vacuolated), with<br />
loss <strong>of</strong> striation and marked endomysial fibrosis. Muscle fibers with<br />
signs <strong>of</strong> degeneration.<br />
In group VI (150 and 75 μg crotoxin), more marked signs <strong>of</strong> muscle<br />
fiber degeneration, such as myophagocytosis, discrete endomysial<br />
fibrosis and chronic inflammatory infiltrate, and also muscle fibers<br />
with signs <strong>of</strong> degeneration (central nucleus). There was no muscle<br />
necrosis.<br />
DISCUSSION<br />
Most <strong>of</strong> our current knowledge about various human pathologies<br />
was experimentally discovered in animals. It is necessary,<br />
naturally, to take care when extrapolating the analysis <strong>of</strong> results with<br />
animals to human beings.<br />
In our study, the rabbit, despite not having binocularity - vision<br />
axis are not parallel -, was useful <strong>for</strong> presenting <strong>extraocular</strong> <strong>muscles</strong><br />
well developed, especially the superior rectus, and also because it is<br />
an animal <strong>of</strong> easy handling. Using only anesthetic drops, we were able<br />
to per<strong>for</strong>m electromyography <strong>of</strong> the superior rectus muscle to evaluate<br />
the effects <strong>of</strong> the injected toxins and its subsequent recovery.<br />
The injection <strong>of</strong> toxins was well tolerated by rabbits, without<br />
signs <strong>of</strong> prostration or changes in feeding behavior. The main local<br />
side effect observed was ptosis, which occurred in eleven <strong>of</strong> twelve<br />
rabbits, the day after the injection. However, the ptosis was discrete<br />
and improved after two days in rabbits 1, 2, 3, 5 and 6, after seven days<br />
in rabbits 7,11 and 12 and remained <strong>for</strong> two weeks in rabbit 8, which<br />
received 2U <strong>of</strong> BT-A. Ptosis observed in monkeys in the first research<br />
with botulinum toxin lasted up to six weeks (7) . Dosing used <strong>for</strong> this<br />
animal was higher than used in our study. Besides, they injected a<br />
volume up to 500 µl, which easily diffuse to adjacent tissues. Animals<br />
receiving A-bungarotoxin (snake poison) on the same experiment<br />
showed ptosis, which improved after three days (7) .<br />
Conjunctival hyperemia observed after the injection was discrete,<br />
and improved after 48 hours in rabbits 1, 2, 3 and 4 (which were<br />
submitted to lower doses <strong>of</strong> crotoxin), and in rabbits 7 and 8 (which<br />
received 2 units <strong>of</strong> botulinum toxin type A). Rabbits 5 and 6 that had<br />
injections <strong>of</strong> 1.5 μg crotoxin, showed moderate hyperemia, which<br />
gradually improved, in seven days. Scott et al., in 1973 (7) , had also<br />
observed a discrete local reaction in animals submitted to injection<br />
<strong>of</strong> A-bungarotoxin and botulinum toxin, which improved after one<br />
day. A more marked local reaction, with hyperemia and purulent<br />
secretion, was observed in rabbits 9, 10, 11 and 12, but improved<br />
spontaneously, without any topic medication, in approximately one<br />
Figure 1. EMG <strong>of</strong> rabbit 6, twenty-three days after the injection <strong>of</strong> 1.5 μg crotoxin.<br />
Figure 3. Fibers with degenerative phenomena (vacuolated) and signs <strong>of</strong> muscle fibers<br />
regeneration (centralization <strong>of</strong> nuclei) (magnification <strong>of</strong> 400X, stained with hematoxy -<br />
lin-eosin) in group III (1.5 μg crotoxin).<br />
Figure 2. EMG <strong>of</strong> rabbit 7, twenty-three days after the injection <strong>of</strong> 2U botulinum<br />
toxin type A.<br />
Figure 4. Discrete degenerated muscle fibers (vacuolated), edema, endomysial fibrosis<br />
and mononuclear infiltrate (magnification <strong>of</strong> 400 X, stained with hematoxylin-eosin) in<br />
group IV (2 U BT-A).<br />
310 Arq Bras Oftalmol. 2012;75(5):307-12
Ribeiro GB, et al.<br />
week. Rabbit 11, besides conjunctival reaction, had also corneal<br />
leukoma, which persisted until the end <strong>of</strong> the experiment.<br />
There are still some doubts about the mechanism <strong>of</strong> action <strong>of</strong><br />
crotoxin in inducing the neuromuscular blockade. The process <strong>of</strong><br />
transmission <strong>of</strong> in<strong>for</strong>mation in synapses involves several stages. In<br />
a general way, stimulus activate an action potential that leads to<br />
alteration <strong>of</strong> ions flux, due to the opening and/or closing <strong>of</strong> ionic<br />
channels, ending with the release <strong>of</strong> neurotransmitters, which were<br />
stored in synaptic vesicles.<br />
Several proteins located in the plasmatic membrane <strong>of</strong> nervous<br />
terminal or in the membrane <strong>of</strong> synaptic vesicle, or even free in the<br />
neuron cytoplasm, are involved in the process <strong>of</strong> neurotransmitter<br />
release. They act on recycling, translocation, anchorage and fusion<br />
<strong>of</strong> synaptic vesicles to cell membrane. Proteins that are, so far, known<br />
<strong>for</strong> participating in this process, are: syntaxin, synaptosomal-associated<br />
protein 25 (SNAP-25), neurexin, voltage sensitive calcium<br />
channels, PKC, N-ethylmaleimide-sensitive factor (NSF), soluble NSF<br />
attachment proteins (SNAPs) a, b, g, kinase C substrate, myristoylated<br />
alanine-rich (MARCKS) and growth associated protein (GAP-43),<br />
synapsins (Ia, Ib, IIa, IIb and II1a), synaptobrevin, synaptophysin,<br />
synaptotagmin, CaMK I and II, dinamin, rab, GTP-binding proteins<br />
and rabphilin (8,9) .<br />
Botulinum toxin type A targets synaptosomal-associated<br />
protein 25 (SNAP-25), <strong>of</strong> molecular weight 25KDa. Other types <strong>of</strong><br />
botulinum toxin attach themselves to different membrane proteins<br />
or to synaptic vesicle (8,9) .<br />
<strong>Crotoxin</strong> has phospholipase activity A 2<br />
(PLA 2<br />
), necessary <strong>for</strong> its<br />
toxic effect. The substitution <strong>of</strong> Ca 2+ ions, essential to phospolipase<br />
activity, <strong>for</strong> Sr 2+ , inhibits the toxic effect <strong>of</strong> crotoxin (10-12) . According<br />
to these authors, toxins would bind to cell membrane, dependent<br />
on calcium and, afterwards, would be endocyted into synaptic<br />
vesicles. Due to its phospholipase action on the vesicle membrane,<br />
they would irreversibly block vesicular endocytosis. <strong>Crotoxin</strong> also<br />
interferes in calcium and potassium channels, and this could reduce<br />
the acetylcholine release in the neuromuscular junction (13) . It alters<br />
also protein phosphorylation in the neuromuscular junction (14) .<br />
In this study, evaluation <strong>of</strong> <strong>paralysis</strong> or paresis <strong>of</strong> superior rectus<br />
<strong>muscles</strong> after injection <strong>of</strong> crotoxin and BT-A was done through<br />
electromyography. Extrinsic ocular <strong>muscles</strong> <strong>of</strong> rabbits are striated.<br />
This type <strong>of</strong> muscle is functionally <strong>for</strong>med <strong>of</strong> motor units in which<br />
axons <strong>of</strong> individual motor cells innerve several muscle fibers. Motor<br />
units are the smallest functional units <strong>of</strong> the locomotor apparatus.<br />
In<strong>for</strong>mation on the function <strong>of</strong> these units is obtained, mainly, from<br />
the use <strong>of</strong> electromyography. The sum <strong>of</strong> several action potentials<br />
<strong>of</strong> many motor-end plates <strong>for</strong>ms the action potential <strong>of</strong> the muscle,<br />
which originates in the motor-end plates and is initiated from<br />
an afferent nervous impulse to neuromuscular joint. This nervous<br />
impulse is spread all over the muscle fibers, stimulating contraction.<br />
The intensity <strong>of</strong> muscle contraction depends, partially, on the<br />
number <strong>of</strong> motor units that are being activated (recruitment) and,<br />
partially, on the frequency neurons are sending impulses to muscle<br />
fibers. In lesions <strong>of</strong> peripheral nerve, electromyography can be used<br />
in a previous stage than any other method to identify <strong>paralysis</strong> and<br />
record if regeneration is happening accordingly. If peripheral motor<br />
neurons that supply a muscle are completed destroyed, lesion will<br />
be partial, proportional to the number <strong>of</strong> affected cells. In denervated<br />
<strong>muscles</strong>, that lost their nerve supply, there are still some action<br />
potentials that can be observed on electromyography, and these<br />
are called fibrillation potentials, which seem to originate in isolated<br />
muscle fibers that lost their innervations. The origin <strong>of</strong> fibrillation is<br />
not completely understood, but some authors say that it is due to<br />
a “sensitization” <strong>of</strong> the muscle portion <strong>of</strong> the motor-end plate after<br />
denervation. The absence <strong>of</strong> the neurotransmitter can stimulate the<br />
muscle fibers to respond to a very small quantity <strong>of</strong> acetylcholine<br />
present in blood stream.<br />
Electromyographic findings demonstrated that crotoxin caused<br />
a reversible <strong>paralysis</strong> <strong>of</strong> muscular activity, being proportional to the<br />
dose injected, according to other authors (13) . Reduction in action<br />
potentials was observed mainly in crotoxin concentrations greater<br />
than 1.5 μg. Recovery <strong>of</strong> <strong>paralysis</strong> was gradual, and at the end <strong>of</strong><br />
two months <strong>of</strong> follow-up, electromyographic records were almost<br />
normal. BT-A injected also caused a reversible <strong>paralysis</strong>. Action<br />
potentials <strong>of</strong> <strong>muscles</strong> injected with BT-A had its recovery starting<br />
after nine days, and were close to normality after two months. That<br />
shows that <strong>paralysis</strong> induced by known concentrations <strong>of</strong> crotoxin<br />
had similar duration than BT-A.<br />
High concentrations <strong>of</strong> crotoxin have myotoxic effect (3,15) . Mor -<br />
phologic alterations observed in mice, through electron microscopy,<br />
show that, in high doses, crotoxin affects nerve terminals, skeletal<br />
muscle and the axons. These effects were also observed with only the<br />
injection <strong>of</strong> PLA 2<br />
subunit from crotoxin, what was not demonstrated<br />
with the other subunit. First structures that are affected by crotoxin<br />
are: sarcolemma, mitochondria and sarcoplasmic reticulum (16,17) . In<br />
1984, it was evidentiated that the beginning <strong>of</strong> myonecrosis caused<br />
by crotoxin was provoked by a progressive loss <strong>of</strong> sarcolemma integrity,<br />
due to hydrolysis <strong>of</strong> phospholipid component. Regeneration <strong>of</strong><br />
muscle fibers was fast (18) .<br />
In our experiment, one animal from each group was sacrificed<br />
<strong>for</strong> anatomopathology studies. Histological alterations found were<br />
proportional to crotoxin concentration, and located only on the site<br />
<strong>of</strong> injection. There was no muscle fiber necrosis in any specimen.<br />
At lower concentrations (0.015 and 0.15 μg), it was observed only<br />
discrete endomysial fibrosis and, in some regions, mononuclear<br />
infiltrate. At concentration <strong>of</strong> 1.5 μg <strong>of</strong> crotoxin, inflammatory process<br />
was also discrete, however, it was possible to observe signs <strong>of</strong><br />
myophagocytosis, vacuolated fibers (degenerative sign) and fibers<br />
with central nucleus (regeneration sign). These alterations were<br />
similar to those found in rabbits that received BT-A. Some studies<br />
show that the injection <strong>of</strong> botulinum toxin type A causes muscle<br />
alterations, proportional to toxin concentration (19) . Similarly to<br />
studies with crotoxin, histological alterations caused by botulinum<br />
toxin type A were reversible (20) . Changes observed in groups V and<br />
VI, that received crotoxin at concentrations <strong>of</strong> 15 μg and 150 μg,<br />
respectively, were more marked than the changes observed in<br />
other groups, and it is even more evident in the group <strong>of</strong> the<br />
highest concentration. Signs <strong>of</strong> degenerated fibers (vacuolated),<br />
loss <strong>of</strong> striation and endomysial fibrosis were more marked. Signs<br />
<strong>of</strong> regeneration <strong>of</strong> muscle fibers (characterized by the presence <strong>of</strong><br />
central nucleus) were also evident.<br />
CONCLUSIONS<br />
Muscle <strong>paralysis</strong> induced by crotoxin injection could be demonstrated<br />
with the help <strong>of</strong> electromyography. At concentration<br />
<strong>of</strong> 1.5 μg, crotoxin caused similar effects to botulinum toxin type<br />
A, showing only discrete local histological alterations. Based on<br />
these findings, we believe that the pharmacological activity <strong>of</strong> crotoxin<br />
can be useful to treat pathologies that have been receiving<br />
botulinum toxin with success. Clinical studies in human beings are<br />
necessary to corroborate crotoxin applicability in several areas <strong>of</strong><br />
medicine.<br />
REFERENCES<br />
1. Rubsamen K, Breithaupt H, Habermann E. Biochemistry and pharmacology <strong>of</strong> the<br />
crotoxin complex. I. Subfractionation and recombination <strong>of</strong> the crotoxin complex.<br />
Naunyn-Schimiedebergs Arch Pharmak. 1972;270(3):274-88.<br />
2. Horst J, Hendon RA, Frankael-Conrat H. The ative components <strong>of</strong> crotoxin. Biochem<br />
Biophy Res Commun. 1972;46(3):1042-7.<br />
3. Haberman E, Breithaupt H. Mini-review: the crotoxin complex an example <strong>of</strong> biochemical<br />
and pharmacological protein complementation. Toxicon. 1978;16(1):19-30.<br />
4. Bon C, Changeux JP, Jeng TW, Frankael-Conrat H. Post-synaptic effects <strong>of</strong> crotoxin<br />
and <strong>of</strong> its isolated subunits. Eur J Biochem. 1979;99(3):471-81.<br />
5. Tzeng MC, Hseu MJ, Yang JH, Guillory RG. Specific binding <strong>of</strong> three neurotoxins<br />
with phospholipase A2 activity to synaptosomal membranes preparations from the<br />
guinea pig brain. J Protein Chem. 1986;5:221-8.<br />
Arq Bras Oftalmol. 2012;75(5):307-12<br />
311
Study <strong>of</strong> crotoxin on the induction <strong>of</strong> <strong>paralysis</strong> in <strong>extraocular</strong> muscle in animal model<br />
6. De Lima ME, Diniz CR. <strong>Crotoxin</strong> inhibits the release <strong>of</strong> acetylcholine induced by Tityus<br />
serrulatus scorpion venom. Toxicon. 1985;23(4):588.<br />
7. Scott AB, Rosenbaum A, Collins CC. Pharmacologic weakening <strong>of</strong> <strong>extraocular</strong> <strong>muscles</strong>.<br />
Invest Ophthalmol Vis Sci. 1973;12(12):924-7.<br />
8. Bajjalieh SM, Scheller RH. Synaptic vesicle and proteins exocytosis. In: Starne L, Greengard<br />
P, Grillner SE, Hokfelt TG, Ottoson DR. Molecular and cellular mechanisms <strong>of</strong><br />
neurotransmitter release. New York: Raven Press; 1994. p.59-79.<br />
9. C<strong>of</strong>field JA, Considine RV, Simpson LL. The site and mechanism <strong>of</strong> action <strong>of</strong> botulinum<br />
neurotoxin. In: Jankovic J, Halle M, editors. Therapy with botulinum neurotoxin.<br />
New York: Marcel Dekker, 1994. p.3-13.<br />
10. Breithaupt H. Neurotoxic and myotoxic effects <strong>of</strong> crotalus phospholipase A and its<br />
complex with crotapotin. Naunyn-Schmideberg’s Arch Pharmacol. 1976;292(3):271-8.<br />
11. Simpson LL, Lautenslager GT, Kaiser II, Middlebrook JL. Identification <strong>of</strong> the site at<br />
which phospholipase A2 neurotoxins localize to produce their neuromuscular blocking<br />
effects. Toxicon. 1993;31(1):13-26.<br />
12. Montecucco C, Rosseto O. How do presynaptic PLA2 neurotoxins block nerve terminals?<br />
Trends Biochem Sci. 2000;25(6):266-70.<br />
13. Araújo DA, Beirão PS. Effects <strong>of</strong> crotoxin on the action potential kinetics <strong>of</strong> frog<br />
skeletal muscle. Braz J Med Biol Res. 1993;26(10):1111-21.<br />
14. Campos AC. Efeito da crotoxina na fos<strong>for</strong>ilação de proteínas da fração sinaptosomal<br />
de córtex de rato [tese]. Belo Horizonte, Instituto de Ciências Biológicas, Universidade<br />
Federal de Minas Gerais; 2000.<br />
15. Gopalakrishnakone P, Hawgood BJ. Morphological changes in murine nerve,<br />
neuromuscular junction and skeletal muscle induced by the crotoxin complex [proceedings].<br />
J Physiol. 1979;291:5P-6P.<br />
16. Harris JB, Johnson MA, Mac Donell CA. Muscle necrosis induced by some presynaptically<br />
active neurotoxins. In: Eaker D, Wadstrom T, editors. Natural toxins. , Ox<strong>for</strong>d:<br />
Pergamon Press; 1980. p.569-78.<br />
17. Howard BD. Presynaptic polypeptide neurotoxins. Trends Pharmac Sci. 1982;<br />
3:167.<br />
18. Gopalakrishnakone P, Dempster DW, Hawgood BJ, Elder HY. Cellular and mitochondrial<br />
changes induced in the structure <strong>of</strong> murine skeletal muscle by crotoxin, a<br />
neurotoxic phospholipase A2 complex. Toxicon. 1984;22(1):85-98.<br />
19. Borodic GE, Ferrantle R, Pearce LB, Smith K. Histologic assessment <strong>of</strong> dose related<br />
diffusion and muscle fiber response after therapeutic botulinum A toxin injections.<br />
Mov Disord. 1994;9(1):31-39.<br />
20. Porter JD, Strebeck S, Capra NF. Botulinum induced changes in monkey eyelid muscle.<br />
Arch Ophthalmol. 1991;109(3):396-404.<br />
38 o Congresso da<br />
Associação Paranaense de Oftalmologia<br />
14 a 16 de março de 2013<br />
Expo Unimed - Asa 2<br />
Curitiba (PR)<br />
In<strong>for</strong>mações:<br />
Tels.: (41) 3232-4031 ou 3039-8003<br />
Site: www.apo-pr.com.br<br />
312 Arq Bras Oftalmol. 2012;75(5):307-12
Artigo Original | Original Article<br />
Alterações retinianas em jovens portadores de anemia falci<strong>for</strong>me (hemoglobinopatias)<br />
em hospital universitário no nordeste do Brasil<br />
Retinal impairment in young individuals with sickle cell anemia (hemoglobin ss disease)<br />
in university hospital in Northeastern <strong>of</strong> Brazil<br />
Allisson Mário dos Santos 1 , Gustavo Baptista de Almeida Faro 2 , Marcus Vinicius Melo do Amaral 3 , Cristiano de Queiroz Mendonça 4 ,<br />
Bruno Campelo Leal 4 , Rosana Cipolotti 3<br />
RESUMO<br />
Objetivos: Descrever e classificar alterações retinianas encontradas em portadores<br />
de anemia falci<strong>for</strong>me com genótipo SS, bem com comparar métodos diagnósticos<br />
(mapeamento de retina e angi<strong>of</strong>luoresceinografia).<br />
Métodos: Neste estudo transversal <strong>for</strong>am avaliados pacientes portadores de anemia<br />
falci<strong>for</strong>me com idade igual ou superior a sete anos. Esses pacientes <strong>for</strong>am submetidos<br />
a mapeamento de retina e angi<strong>of</strong>luoresceinografia. Os achados do mapeamento de<br />
retina <strong>for</strong>am agrupados em três classes: sem alterações; alterações não proliferativas<br />
e alterações proliferativas. Os resultados à angi<strong>of</strong>luoresceinografia <strong>for</strong>am classificados<br />
de acordo com os estágios de Goldberg, variando de I a V e expressando gradiente<br />
crescente de gravidade.<br />
Resultados: Foram avaliados 61olhos de 31pacientes. A retinopatia falci<strong>for</strong>me foi<br />
encontrada em 38/61 (62,3%) dos olhos examinados. A média de idade do grupo de<br />
portadores de retinopatia foi menor que dos pacientes sem retinopatia (14,4 versus<br />
17,4 anos, p=0,04). Observou-se elevada freqüência de retinopatia não proliferativa,<br />
especialmente as tortuosidades vasculares (27,9%), seguidas por anastomoses arteriovenosas<br />
na periferia da retina (24,6%) e oclusões arteriolares (8,2%). Em um olho<br />
foi observado neovascularização. Em 16,4% dos olhos obteve-se resultado normal no<br />
mapeamento de retina e alterado à angi<strong>of</strong>luoresceinografia.<br />
Conclusões: As alterações retinianas do tipo não proliferativa são frequentes e precoces<br />
nos portadores de anemia falci<strong>for</strong>me do tipo SS, sendo a angi<strong>of</strong>luoresceinografia mais<br />
sensível no diagnóstico quando comparada ao mapeamento de retina.<br />
Descritores: Anemia falci<strong>for</strong>me; Retina/fisiopatologia; Doenças retinianas/diagnóstico;<br />
Angi<strong>of</strong>luoresceinografia/metodos; Oftalmoscopia<br />
ABSTRACT<br />
Purposes: To describe and categorize retinal vascular changes in patients with sickle<br />
cell anemia, as well as to compare diagnostic methods (indirect ophthalmoscopy and<br />
fluorescein angiography).<br />
Methods: Patients with sickle cell anemia over the age <strong>of</strong> seven were examined. Complete<br />
ophthalmologic examination with indirect ophthalmoscopy and angiography was<br />
per<strong>for</strong>med in each patient. The fundoscopy results were grouped in 3 classes: normal; non-<br />
-proliferative retinopathy, which includes vascular tortuosity, black sunburst, salmon- patch<br />
and peripheral closure/anastomoses; and proliferative retinopathy, related to neovascular<br />
proliferation. Angiography results were classified according to Goldberg classifications<br />
from stage I to V.<br />
Results: Retinopathy related to sickle cell anemia was seen in 62.3% (38/61) <strong>of</strong> the eyes<br />
checked. Neovascularization was observed in one eye. The frequency <strong>of</strong> bilateral changes<br />
in angiography was high. Non-proliferative retinopathy was more common, especially<br />
vascular tortuosities (17/61), followed by arteriovenous anastomoses in the retinal periphery<br />
(15/61) and arterial occlusions (5/61). The mean age <strong>of</strong> retinopathy group was 14.4 years<br />
old, significantly lower than the mean age <strong>of</strong> non-retinopathy group, which was 17.4. The<br />
result was normal in16.4% (10/61) <strong>of</strong> the eyes in the fundoscopy exam, while angiography<br />
showed alterations.<br />
Conclusions: All the results pointed to the conclusion that the non-proliferative retinal<br />
vascular changes are frequent and precocious in patients with sickle cell anemia (SS genotype).<br />
Fluorescein angiography is more sensitive in the diagnosis <strong>of</strong> retinopathy when<br />
compared to indirect ophthalmoscopy.<br />
Keywords: Anemia, sickle cell; Retina/physiopathology; Retinal diseases/diagnosis; Fluo -<br />
rescein angiography/methods; Ophthalmoscopy<br />
INTRODUÇÃO<br />
A anemia falci<strong>for</strong>me é a doença hereditária mais prevalente no<br />
Brasil (1) . A hemoglobinopatia ocorre em situação de homozigose do<br />
gene responsável pela produção de uma hemoglobina mutante,<br />
a hemoglobina S, que em seu estado desoxigenado pode s<strong>of</strong>rer polimerização<br />
e originar hemácias falcizadas, responsáveis por anemia<br />
hemolítica crônica e fenômenos vasoclusivos (1-6) .<br />
Embora haja outros genótipos para a doença falci<strong>for</strong>me, acredita-se<br />
que SC, Sβ 0 talassemia, em menor grau, o SS (este o responsável pelo<br />
fenótipo da anemia falci<strong>for</strong>me) resultem em maior risco para complicações<br />
oculares (2,4,5) .<br />
As manifestações oculares da anemia falci<strong>for</strong>me compreendem<br />
alterações orbitárias, conjuntivais, uveais, papilares e, principalmente,<br />
retinianas (7-10) . A retina periférica e a mácula parecem ser os locais<br />
mais suscetíveis à oclusão vascular, onde as lesões são mais evidentes<br />
e destrutivas, podendo ocasionar cegueira (11-13) .<br />
O presente estudo objetiva descrever e classificar alterações<br />
retinianas encontradas em portadores de anemia falci<strong>for</strong>me, bem<br />
Submetido para publicação: 24 de maio de 2012<br />
Aceito para publicação: 17 de agosto de 2012<br />
Trabalho realizado na Universidade Federal de Sergipe em parceria com o Instituto de Olhos Dr.<br />
Cristiano Mendonça, Aracajú - Sergipe.<br />
1<br />
Médico, Departamento de Oftalmologia, Fundação Altino Ventura, Recife (PE), Brasil.<br />
2<br />
Acadêmico de Medicina, Universidade Federal de Sergipe, Aracaju (SE), Brasil.<br />
3<br />
Médico, Universidade Federal de Sergipe, Aracaju (SE), Brasil.<br />
4<br />
Médico, Instituto de Olhos Cristiano Mendonça, Aracaju (SE), Brasil.<br />
Financiamento: Não houve financiamento para este trabalho.<br />
Divulgação de potenciais conflitos de Interesse: A.M.Santos, Nenhum; G.B.A.Faro, Nenhum;<br />
M.V.M.Amaral, Nenhum; C.Q.Mendonça, Nenhum; B.C.Leal, Nenhum; R.Cipolotti, Nenhum.<br />
Endereço de correspondência: Rosana Cipolotti, Av. Beira Mar, 2016, Apto. 402, Aracaju (SE)<br />
49025-040, Brasil - E-mail: rosanaci@yahoo.com<br />
Comitê de ética responsável pela aprovação: Comitê de Ética em Pesquisa Envolvendo Seres<br />
Humanos da Universidade Federal de Sergipe (CEP-UFS) N o .CAAE:0140.0.107.000-07<br />
Arq Bras Oftalmol. 2012;75(5):313-5<br />
313
Alterações retinianas em jovens portadores de anemia falci<strong>for</strong>me (hemoglobinopatias) em hospital universitário no nordeste do Brasil<br />
como comparar os métodos diagnósticos (mapeamento de retina e<br />
angi<strong>of</strong>luoresceinografia).<br />
MÉTODOS<br />
Foram avaliados neste estudo transversal (com dados obtidos<br />
prospectivamente), pacientes portadores de anemia falci<strong>for</strong>me,<br />
confirmada laboratorialmente por eletro<strong>for</strong>ese de hemoglobina em<br />
pH alcalino, com idade igual ou superior a sete anos, em acompanhamento<br />
regular em ambulatório de Hematologia Pediátrica de<br />
Hospital Universitário da região nordeste do Brasil. Os pacientes <strong>for</strong>am<br />
consecutivamente encaminhados para avaliação <strong>of</strong>talmológica,<br />
após assinatura de Termo de Consentimento Livre e Esclarecido pelo<br />
paciente ou seu responsável legal.<br />
O exame <strong>of</strong>talmológico consistiu em medida da acuidade visual<br />
corrigida através dos optotipos de Snellen, tonometria de aplanação<br />
de Goldmann, biomicroscopia com lâmpada de fenda, <strong>of</strong>talmoscopia<br />
binocular indireta, retinografia e angiografia com injeção de<br />
fluoresceína sódica a 20%, sendo esse três últimos após a midríase<br />
medicamentosa com tropicamida a 1%. Todos os pacientes <strong>for</strong>am<br />
submetidos a todos os procedimentos citados.<br />
Os achados fundoscópicos <strong>for</strong>am agrupados em: (1) sem alterações;<br />
(2) retinopatia não-proliferativa: tortuosidade venosa, hemorragias<br />
“salmon patch” (coloração alaranjada advinda da degradação<br />
da hemoglobina) e “blacksunburst” (lesão hiperpigmentada) (2,4,6,13) ,<br />
pontos iridescentes, anastomoses arteriovenosas (5,14) , alterações na<br />
mácula e no nervo óptico (pontos escuros, pequenos e vermelhos) (15,16) ;<br />
(3) retinopatia proliferativa, caracterizada por neovascularização periférica<br />
denominada “seafun” (2,5,6,13) .<br />
Os achados da angi<strong>of</strong>luoresceinografia <strong>for</strong>am descritos através<br />
da classificação de Goldberg (14) em cinco estágios, sendo os dois<br />
primeiros pré-proliferativos e os três restantes proliferativos (4,6,13,15) : (I)<br />
oclusões arteriolares na periferia da retina; (II) anastomoses arteriovenosas<br />
na periferia da retina; (III) proliferações fibrosas e neovasculares;<br />
(IV) hemorragia vítrea; (V) descolamento da retina.<br />
As variáveis categóricas <strong>for</strong>am apresentadas como porcentagens<br />
e a comparação entre os grupos, realizada por meio do teste de Fisher.<br />
As variáveis contínuas <strong>for</strong>am apresentadas por meio de medidas<br />
de tendência central e comparadas pelo teste T ou Mann Whitney,<br />
con siderando-se significativos os valores de p
Santos AM, et al.<br />
Observou-se frequência elevada de alterações bilaterais à an -<br />
gio fluoresceinografia neste estudo. Downes et al. observaram a<br />
possibilidade de reversão para unilateral em cerca de 30% dos casos,<br />
o que indica que esses pacientes devem ser acompanhados clinicamente,<br />
mesmo não havendo indicação de intervenção terapêutica<br />
no momento (12) .<br />
Considerando-se que o paciente se mantém assintomático até<br />
estágios avançados, a identificação precoce de retinopatia proliferativa<br />
permite intervenções terapêuticas curativas. Não parece haver<br />
consenso com relação à idade apropriada para início do tratamento<br />
da retinopatia proliferativa no paciente portador de anemia falci<strong>for</strong>me,<br />
uma vez que existem relatos controversos sobre a eventual resolução<br />
espontânea do quadro (11) , que, no entanto, não foi observada<br />
por outros autores (9) .<br />
O presente estudo apresenta como limitações seu delineamento<br />
transversal e o reduzido tamanho da amostra estudada. Estudos<br />
longitudinais são necessários para ratificar achados aqui presentes e<br />
estabelecer fatores de risco para a retinopatia em pacientes portadores<br />
de anemia falci<strong>for</strong>me.<br />
CONCLUSÃO<br />
Com base nos casos estudados, que as alterações retinianas do<br />
tipo retinopatia não proliferativa, especialmente as tortuosidades vas -<br />
culares, anastomoses arteriovenosas na periferia da retina e oclusões<br />
arteriolares são frequentes e precoces nos portadores de anemia<br />
falci<strong>for</strong>me, sendo a angi<strong>of</strong>luoresceinografia mais sensível no diagnóstico<br />
quando comparada ao mapeamento de retina. Os achados<br />
indicam a necessidade de acompanhamento <strong>of</strong>talmológico, cuja<br />
pe riodicidade deve ser determinada pela extensão e gravidade das<br />
alterações encontradas.<br />
REFERÊNCIAS<br />
1. Paiva e Silva RB, Ramalho AS, Cassorla RM. A anemia falci<strong>for</strong>me como problema<br />
de Saúde Pública no Brasil. Rev Saúde Pública. 1993;27(1):54-8.<br />
2. Freitas LG, Isaac DL, Tannure WT, Lima EV, Abud MB, Tavares RS, et al. Alterações retinianas<br />
apresentadas em pacientes portadores de hemoglobinopatia falci<strong>for</strong>me<br />
atendidos em um Serviço Universitário de Oftalmologia. Arq Bras Oftalmol. 2011;<br />
74(5):335-7.<br />
3. Bunn HF. Pathogenesis and treatment <strong>of</strong> sickle cell disease. N Engl J Med. 1997;<br />
337(11):762-9.<br />
4. Vilela RQ, Bandeira DM, Silva MA. <strong>Ocular</strong> complications in sickle cell disease. Rev<br />
Bras Hematol Hemoter. 2007;29(3):285-7.<br />
5. Gill HS, Lam WC. A screening strategy <strong>for</strong> the detection <strong>of</strong> sickle cell retinopathy in<br />
pediatric patients. Can J Ophthalmol. 2008;43(2):188-91.<br />
6. Bonanomi MT. Alterações oculares na doença falci<strong>for</strong>me. In: Agência Nacional de<br />
Vigilância Sanitária. Manual de diagnóstico e tratamento de doenças falci<strong>for</strong>mes<br />
[Internet]. Brasília: ANVISA; 2002. p.97-105. [citado 2004 Jul 27]. Disponível em:<br />
http://bvsms.saude.gov.br/bvs/publicacoes/anvisa/diagnostico.pdf<br />
7. Osafo-Kwaako A, Kimani K, Ilako D, Akafo S, Ekem I, Rodrigues O, et al. <strong>Ocular</strong><br />
manifestations <strong>of</strong> sickle cell disease at the Korle-bu Hospital Accra, Ghana. Eur J<br />
Oph thalmol. 2010;21(4):484-9.<br />
8. Morel C. [Retinal involvmente in hemoglobinopathy] J Fr Ophtalmol. 2001;<br />
24(9).967-92. French.<br />
9. Bisol T, Fior O, Esteves JF, Friderich JR. Sickle cell hemoglobinopathy genotypes<br />
and retinal manifestations in patients <strong>of</strong> a university hospital. Arq Bras Oftalmol.<br />
2000;63(4):273-6.<br />
10. Fadugbagbe AO, Gurgel RQ, Mendonça CQ, Cipolotti R, Santos AM, Cuevas LE.<br />
<strong>Ocular</strong> manifestations <strong>of</strong> sickle cell disease. Ann Trop Paediatr. 2010;30(1):19-26.<br />
11. Elagouz M, Jyothi S, Gupta B, Sivaprasad S. Sickle cell disease and the eye: old and<br />
new concepts. Surv Ophthalmol. 2010;55(4):359-77.<br />
12. Downes SM, Hambleton IR, Chuang EL, Lois N, Serjeant GR, Bird AC. Incidence and<br />
natural history <strong>of</strong> proliferative sickle cell retinopathy: observations from a cohort<br />
study. Ophthalmology. 2005;112(11):1869-75.<br />
13. Bonanomi MT, Cunha SL, Araújo JT. Funduscopic alterations in SS and SC hemoglobinopathies<br />
- Study <strong>of</strong> a Brazilian population. Ophthalmologica.1988; 197(1):<br />
26-33.<br />
14. Goldberg MF. Classification and pathogenesis <strong>of</strong> proliferative sickle cell retinopathy.<br />
Am J Ophthalmol. 1971;85(4):426-37.<br />
15. Garcia CA, Fernandes MZ, Uchôa UB, Cavalcante BM, Uchôa RA. Achados fundoscópico<br />
sem crianças portadoras de anemia falci<strong>for</strong>me no estado do Rio Grande<br />
do Norte. Arq Bras Oftalmol. 2002;65(5):615-8.<br />
16. Cook WC. A case <strong>of</strong> sickle cell anemia with associated subarachnoid hemorrhage.<br />
J Med. 1930;11:54117.<br />
17. Bonanomi MT, Oliveira AA, Suzuki H. Hemoglobinopatias. In: AbujamraS, Ávila M,<br />
Barsante C. Retina e vítreo. São Paulo: Roca; 2000. p.592-601.<br />
Arq Bras Oftalmol. 2012;75(5):313-5<br />
315
Artigo Original | Original Article<br />
Effect <strong>of</strong> aspherical and yellow tinted intraocular lens on blue-on-yellow perimetry<br />
Efeito das lentes intraoculares asféricas e com pigmentação amarela na campimetria azul-amarelo<br />
Rodrigo França de Espíndola 1 , Marcony Rodrigues de Santhiago 1 , Newton Kara-Júnior 1<br />
ABSTRACT<br />
Purpose: To investigate the possible effect <strong>of</strong> aspherical or yellow tinted intraocular<br />
lens (IOL) on contrast sensitivity and blue-on-yellow perimetry.<br />
Methods: This prospective randomized bilateral double-masked clinical study included<br />
52 patients with visually significant bilateral cataracts divided in two groups;<br />
25 patients (50 eyes) received aspherical intraocular lens in one eye and spherical<br />
intraocular lens in the fellow eye; and 27 patients (54 eyes) received ultraviolet and<br />
blue light filter (yellow tinted) IOL implantation in one eye and acrylic ultraviolet<br />
filter IOL in the fellow eye. The primary outcome measures were contrast sensitivity<br />
and blue-on-yellow perimetry values (mean deviation [MD] and pattern standard<br />
deviation [PSD]) investigated two years after surgery. The results were compared<br />
intra-individually.<br />
Results: There was a statistically significant between-group (aspherical and spherical<br />
intraocular lens) difference in contrast sensitivity under photopic conditions at 12<br />
cycles per degree and under mesopic conditions at all spatial frequencies. There were<br />
no between-group significant differences (yellow tinted and clear intraocular lens)<br />
under photopic or mesopic conditions. There was no statistically significant difference<br />
between all intraocular lens in MD or PSD.<br />
Conclusion: Contrast sensitivity was better under mesopic conditions with aspherical<br />
intraocular lens. Blue-on-yellow perimetry did not appear to be affected by aspherical<br />
or yellow tinted intraocular lens. Further studies with a larger sample should be carried<br />
out to confirm or not that hypotheses.<br />
Keywords: Lenses, intraocular; Cataract extraction; Phacoemulsification; Glaucoma/<br />
diagnosis; Visual field tests/methods; Visual fields; Lens implantation, intraocular; Con -<br />
trast sensitivity<br />
RESUMO<br />
Objetivo: Investigar a possibilidade de efeitos na sensibilidade ao contraste e nos resulta -<br />
dos da campimetria azul-amarelo com implante de uma lente intraocular (LIO) asférica<br />
ou de pigmentação amarela.<br />
Métodos: Trata-se de um estudo prospectivo, randomizado, duplo-mascarado, envolvendo<br />
52 pacientes portadores de catarata senil bilateral, divididos em dois grupos;<br />
25 pacientes (50 olhos) receberam uma LIO asférica em um olho e uma esférica no olho<br />
con tralateral; e 27 pacientes (54 olhos) com implante de uma LIO de pig mentação<br />
amarela e uma LIO convencional no olho contralateral. O principal resultado do<br />
estudo foi a sensibilidade ao contraste e os dados da perimetria azul-amarelo (“mean<br />
deviation” [MD] e “pattern standard deviation” [PSD]). Os resultados <strong>for</strong>am analisados<br />
interindividualmente.<br />
Resultados: Houve diferença estatística entre os grupos (lentes asféricas e esféricas) na<br />
sensibilidade ao contraste em condições fotópicas (12 ciclos por grau) e em condições<br />
mesópicas (todas frequências). Não houve diferença estatística na sensibilidade ao<br />
contraste entre as lentes de pigmentação amarela e convencionais. Não houve diferença<br />
estatística nos valores de MD e PSD entre os grupos.<br />
Conclusão: A sensibilidade ao contraste foi melhor em condições mesópicas com as lentes<br />
asféricas. A campimetria azul-amarelo parece não ser influenciada por LIOs asféricas e<br />
com pigmentação amarela. Mais estudos com uma amostra maior são necessários para<br />
confirmar ou afastar essa hipótese.<br />
Descritores: Lentes intraoculares; Extração de catarata; Facoemulsificação; Glaucoma/<br />
diagnóstico; Testes de campo visual/métodos; Campos visuais; Implante de lente in -<br />
traocular; Sensibilidade de contraste<br />
INTRODUCTION<br />
Short-wavelength automated perimetry (SWAP) or Blue-on-Yellow<br />
(B/Y) perimetry has gained fairly wide acceptance as a clinical test since<br />
its initial use more than 10 years ago. SWAP uses moderately bright<br />
yellow background fields to depress visual sensitivity that is mediated<br />
via long and middle-wavelength-sensitive cones. This selective sensitivity<br />
reduction allows visual sensitivity mediated via short-wavelengthsensitive<br />
cones to be measured in isolation (1) .<br />
Previous studies suggest that visual field defects on B/Y perimetry<br />
occur be<strong>for</strong>e defects on standard automatic white-on-white perimetry<br />
(SAP) and exhibit progression in advance <strong>of</strong> those recorded with whi teon-white<br />
perimetry in both chronic open-angle glaucoma and ocular<br />
hypertension (2-5) . Although, Tafreshi et al., associates compared SAP,<br />
Matrix frequency-doubling technology (FDT) perimetry and SWAP and<br />
detected no significant differences in their diagnostic per<strong>for</strong>mance (6) .<br />
Changes in the absorption characteristics <strong>of</strong> the human lens with<br />
age and lens opacity can influence the results <strong>of</strong> SWAP (7) . Others influences<br />
in B/Y, such as intraocular lenses (IOLs) with ultraviolet filter,<br />
was reported in peer review literature (8) . Another type <strong>of</strong> intraocular lens<br />
(IOL) with aspherical surface, could modify the visual per<strong>for</strong>mance <strong>of</strong><br />
patients implanted with these IOLs in relation to those implanted with<br />
spherical IOLs.<br />
It has been suggested in previous works that aspherical IOLs can<br />
improve contrast sensitivity and reduce the patient’s perception <strong>of</strong> halos<br />
and glare (9) . These theoretical changes can confound the interpretation<br />
<strong>of</strong> the glaucomatous visual field, and it is a great clinical importance to<br />
understand the aspherical IOL´s effect upon such mode <strong>of</strong> perimetry.<br />
The purpose <strong>of</strong> this prospective study was to investigate the<br />
possible effects <strong>of</strong> an aspherical and a blue-light filter (yellow tinted)<br />
IOLs on contrast sensitivity and B/Y perimetry measures.<br />
Submitted <strong>for</strong> publication: March 1, 2012<br />
Accepted <strong>for</strong> publication: August 27, 2012<br />
Study conducted in Ophthalmology Department <strong>of</strong> the University <strong>of</strong> São Paulo, São Paulo, Brazil.<br />
1<br />
Ophthalmology Department, Universidade de São Paulo (USP), São Paulo, Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: R.F.Espíndola, None; M.R.Santhiago, None; N.Kara-<br />
-Júnior, None.<br />
Correspondence address: Rodrigo F. Espíndola. Praça das Hortências, 70 - Itu (SP) - 13301-689 -<br />
Brazil - E-mail: rodrigo166@uol.com.br<br />
316 Arq Bras Oftalmol. 2012;75(5):316-9
Espíndola RF, et al.<br />
METHODS<br />
This study was conducted according to ethical standards <strong>for</strong> clinical<br />
research and was approved by the University Hospital’s research<br />
ethics committee/investigational review board. The observers who<br />
conducted the postoperative visual evaluations did not have access<br />
to the randomization code or in<strong>for</strong>mation about the surgical procedures.<br />
In<strong>for</strong>med consent was obtained, and the study was conducted<br />
in adherence with the tenets <strong>of</strong> the Declaration <strong>of</strong> Helsinki.<br />
All patients involved had bilateral sequential cataract surgery<br />
under similar preoperative conditions using the same phacoemulsification<br />
technique in both eyes. Only one experienced surgeon per -<br />
<strong>for</strong>med all surgeries.<br />
Patients with visually significant bilateral cataract and no history<br />
<strong>of</strong> glaucoma were eligible <strong>for</strong> inclusion in the study. Exclusion criteria<br />
was any ocular disease, such as corneal opacities or irregularity, dry<br />
eye, amblyopia, anisometropia, retinal abnormalities, surgical complications,<br />
IOL tilt, previous or current use <strong>of</strong> medications known to<br />
cause color-vision deficiencies, or incomplete follow-up.<br />
The patients were divided in two groups: first group compromised<br />
25 patients (50 eyes). Each patient received a spherical foldable,<br />
1-piece, hydrophobic acrylic IOL (Akreos Fit, Bausch & Lomb, Inc.) in<br />
one eye and a 1-piece foldable, hydrophobic acrylic IOL (Akreos AO,<br />
Bausch & Lomb, Inc.) with aspherical anterior and posterior surface<br />
in the fellow eye (aberration-free).<br />
The second group enrolled 27 patients (54 eyes) with an ultraviolet<br />
and blue light filter IOL (AcryS<strong>of</strong> Natural SN60AT, Alcon) in one eye<br />
(yellow tinted), and an acrylic ultraviolet filter IOL (AcryS<strong>of</strong> SA60AT,<br />
Alcon) in the fellow eye (non-tinted).<br />
Approximately 30 days after the first surgery, the second eye had<br />
cataract surgery with implantation <strong>of</strong> another IOL model. All patients<br />
and observers were masked about the IOL type implanted.<br />
An envelope system was used to randomly assign all enrolled<br />
patients. Sequenced and sealed envelopes containing the first type<br />
<strong>of</strong> IOL (Akreos AO or Akreos Fit; SN60AT or MA60AC) were prepared<br />
be<strong>for</strong>e surgery. An unscrubbed observer in the operating room opened<br />
the envelopes and assigned each patient.<br />
The individuals met the following inclusion criteria at two years<br />
postoperatively: visual acuity better than 0.3 logMAR in both eyes,<br />
normal intraocular pressures, no evidence <strong>of</strong> posterior capsule opacity,<br />
and no signs <strong>of</strong> glaucoma.<br />
The primary outcome measures <strong>of</strong> the study were contrast sensitivity<br />
and B/Y perimetry values. The contralateral eye was used as<br />
control. Best-corrected visual acuity (BCVA) and distance uncorrected<br />
visual acuity (UCVA) were measured as well as B/Y values. The visual<br />
acuity was measured at 100% contrast using Early Treatment <strong>of</strong><br />
Dia betic Retinopathy Study (ETDRS) charts (Precision Vision) under<br />
pho topic conditions (target luminance 85 candelas [cd]/m 2 ) at 4.0 m.<br />
Contrast sensitivity was measured with VCTS 6000 (Vistech Consultants<br />
Incorporation, Dayton, OH, USA) with best spectacle correction<br />
under photopic (85 cd/m 2 ) and mesopic (3 cd/m 2 ) conditions.<br />
Light conditions were controlled with a luxometer (Gossen-Starlite,<br />
Nürnberg, Germany).<br />
During visual field testing, optimal refractive correction was pla -<br />
ced be<strong>for</strong>e the tested eye, and the fellow eye was occluded with an<br />
opaque eye patch. B/Y perimetry was per<strong>for</strong>med (first in right eye)<br />
using the Humphrey Visual Field Analyzer (Carl Zeiss Meditec, USA).<br />
A full-threshold algorithm (central 24-2 full-threshold strategy) was<br />
used with a blue (440 nm) size V (1.72°) stimulus on a yellow background<br />
(530 nm), with maximum brightness <strong>of</strong> 100 cd/m 2 . The measured<br />
levels were expressed in decibels (dB) <strong>for</strong> all points.<br />
Because the participants did not have previous experience with<br />
any visual field testing, they underwent two initials tests to minimize<br />
the learning curve. These tests were not included in the analysis.<br />
Only visual field tests with reliable results were analyzed. A reliable<br />
test was defined as one with fixation losses <strong>of</strong> less than 25% and<br />
both false-positive and false-negative responses <strong>of</strong> less than 33%.<br />
Statistical analysis was conducted using the s<strong>of</strong>tware SPSS<br />
ver sion 15.0 (SPSS Inc., Chicago, IL, USA). Data were analyzed with<br />
the nonparametric Mann-Whitney U test using a 5% significance<br />
level and 80% power. The normality <strong>of</strong> the quantitative variables was<br />
verified using the Kolmogorov-Smirnov test. The level <strong>of</strong> statistical<br />
significance <strong>for</strong> such comparison was set a p
Effect <strong>of</strong> aspherical and yellow tinted intraocular lens on blue-on-yellow perimetry<br />
Table 2. Pattern standard deviation (PSD) <strong>of</strong> blue-on-yellow<br />
perimetry in eyes implanted with Akreos AO and Akreos Fit<br />
Value<br />
Table 4. Pattern standard deviation (PSD) <strong>of</strong> blue-on-yellow<br />
perimetry in eyes implanted with SN60AT and MA60AC<br />
Value<br />
MA60AC<br />
(dB)<br />
N60AT<br />
(dB)<br />
Mean 3.04 2.52<br />
Minimum 0.00 0.00<br />
Maximum 8.00 5.49<br />
dB= decibels; P=0.42<br />
Akreos AO<br />
(dB)<br />
Akreos Fit<br />
(dB)<br />
Mean 3.30 3.80<br />
Minimum 2.78 3.20<br />
Maximum 4.72 5.10<br />
dB= decibels; P=0.13<br />
Table 3. Mean deviation (MD) <strong>of</strong> blue-on-yellow perimetry in eyes<br />
implanted with SN60AT and MA60AC<br />
Value<br />
MA60AC<br />
(dB)<br />
SN60AT<br />
(dB)<br />
Mean --3.68 --5.62<br />
Minimum -21.70 -22.67<br />
Maximum --6.15 --4.65<br />
dB= decibels; P=0.27<br />
entire refractive system <strong>of</strong> the eye (10) . The selection <strong>of</strong> aspherical IOLs<br />
to compensate <strong>for</strong> corneal aberrations can improve pseudophakic<br />
visual quality (11) .<br />
After cataract removal with IOL implantation, the IOL itself<br />
might confound the findings <strong>of</strong> common diagnostic tests such as<br />
perimetry (12-14) . There are no reports on the effect <strong>of</strong> aspherical IOL<br />
on B/Y perimetry to our knowledge. This contralateral eye study<br />
was conducted to analyze the theoretical benefits <strong>of</strong> aspherical IOL<br />
implantation in improve contrast sensitivity and its consequences in<br />
B/Y parameters. Blue-filter IOLs were also taken into account.<br />
Under mesopic conditions, postoperative VCTS contrast sensitivity<br />
testing showed significant differences between the 2 groups<br />
(aspherical and spherical IOLs) at all spatial frequencies, indicating<br />
that Akreos AO per<strong>for</strong>med better than Akreos Fit in larger pupil sizes.<br />
However, under photopic conditions, the Akreos AO IOL per<strong>for</strong>med<br />
better than Akreos Fit only at 12 cpd. Others studies confirms this<br />
fin dings (9,12) . Despite this improvement in contrast sensitivity, no<br />
chan ges in pattern standard deviation (PSD) or mean deviation (MD)<br />
were found comparing aspherical and spherical IOL.<br />
Benefits <strong>of</strong> blue-filter IOLs that have been suggested include<br />
pro tection against retinal damage due to blue light, with a possible<br />
role in preventing the development or exacerbation <strong>of</strong> age-related<br />
macular degeneration. In addition, by blocking blue light, the optical<br />
chromatic aberration is reduced. Improvement in contrast sensitivity,<br />
reduced glare under photopic and mesopic conditions and reduction<br />
in disturbance <strong>of</strong> blue color vision are also expected. These<br />
changes could confound the interpretation <strong>of</strong> the glaucomatous<br />
visual field (15-20) .<br />
In our study, no statistically difference was found in contrast sensitivity<br />
comparing yellow tinted and clear IOLs. Even with a shorter<br />
follow-up, most previous studies found no detrimental effect <strong>of</strong> blue<br />
light-filtering IOLs on photopic or mesopic contrast sensitivity or on<br />
color vision between eyes with blue light-filtering IOLs and eyes with<br />
UV light-filtering IOLs (21,22) .<br />
Castro et al. (23) , using a blue light spectrum filter (simulating an<br />
AcriS<strong>of</strong> Natural IOL) found statistically significant reductions in MD<br />
and foveal threshold on SWAP, but not in SAP examinations. However,<br />
this study was not conducted <strong>for</strong> patients with cataract (young<br />
patients). Our study did not confirm these results. A previous study by<br />
Jang et al. (24) , had similar findings to the results <strong>of</strong> Castro et al.<br />
Another study on the influence <strong>of</strong> yellow IOL on SWAP, concluded<br />
that yellow IOLs did not affect SWAP results (25) , which is in agreement<br />
with our results. Ueda et al. (26) , also reported that no significant differences<br />
were observed between patients with yellow-tinted and clear<br />
IOLs <strong>for</strong> FDT perimetry results. They suggested that when interpreting<br />
the results <strong>of</strong> perimetry, the effect <strong>of</strong> cataract should be considered<br />
but that <strong>of</strong> IOL color does not need consideration.<br />
Some studies described a better (26,27) or worse (28,29) per<strong>for</strong>mance<br />
<strong>of</strong> blue-light- filtering IOLs. The majority <strong>of</strong> the studies, however, did<br />
not find any statistically significant differences in comparison with<br />
UV-filtering IOL (30-32) .<br />
In this study, no significant difference <strong>for</strong> either MD or PSD was<br />
found between IOLs, although, the Akreos AO group demonstrated<br />
better values (Table 1 and 2). In spite <strong>of</strong> no scientific agreement exists as<br />
to whether removing aberrations from the visual system may result in<br />
a better retinal image, it is also apparent that zero spherical aberration<br />
does not automatically provide best visual per<strong>for</strong>mance.<br />
This study has limitations that included the absence <strong>of</strong> preoperative<br />
B/Y perimetry data, the small number <strong>of</strong> cases, and the absence<br />
<strong>of</strong> concurrent standard automated perimetry. A larger number <strong>of</strong><br />
cases, (proximally 100 cases in each group), could make a difference<br />
in the findings between each group, or confirm the result seen in<br />
this study.<br />
The fact that this study makes a contralateral comparison minimizes<br />
intraindividual factors that could interfere with contrast sensitivity<br />
and the results <strong>of</strong> B/Y perimetry. Different IOLs from the same<br />
manufacturer were used to minimize bias.<br />
CONCLUSION<br />
In summary, aspherical IOL showed better per<strong>for</strong>mance in the<br />
contrast sensitivity test under mesopic conditions compared with<br />
the spherical IOL. Blue-yellow perimetry did not appear to be affected<br />
by aspherical or yellow tinted IOL. Further studies with a larger<br />
sample size are necessary.<br />
REFERENCES<br />
1. Sample PA, Johnson CA, Haegerstrom-Portnoy G, Adams AJ. Optimum parameters<br />
<strong>for</strong> short-wavelength automated perimetry. J Glaucoma. 1996;5(6):375-83. Comment<br />
in: J Glaucoma. 2000;9(1):3-4.<br />
2. Johnson CA. Diagnostic value <strong>of</strong> short-wavelength automated perimetry. Curr Opin<br />
Ophthalmol. 1996;7(2):54-8.<br />
3. Sample PA, Weinreb RN. Progressive color visual field loss in glaucoma. Invest Oph -<br />
thalmol Vis Sci. 1992;33(6):2068-71.<br />
4. Sample PA, Taylor JD, Martinez GA, Lusky M, Weinreb RN. Short-wave-length color<br />
visual fields in glaucoma suspects at risk. Am J Ophthalmol, 1993;115(2):225-33.<br />
5. Wild JM, Moss ID, Whitaker D, O’Neill EC. The statistical interpretation <strong>of</strong> blue-on-yellow<br />
visual field loss. Invest Ophthalmol Vis Sci. 1995;36(7):1398-410.<br />
6. Tafreshi A, Sample PA, Liebmann JM, Girkin CA, Zagwill LM, Weinreb RN, et al. Visual<br />
function-specific perimetry to identify glaucomatous visual loss using three different<br />
definitions <strong>of</strong> visual field abnormality. Invest Ophthalmol Vis Sci. 2009;50(3):1234-40.<br />
7. Carrillo MM, Artes PH, Nicolela MT, LeBlanc RP, Chauhan BC. Effect <strong>of</strong> cataract<br />
extraction on the visual fields <strong>of</strong> patients with glaucoma. Arch Ophthalmol. 2005;<br />
123(7):929-32.<br />
8. Sirtoli MG, Santhiago MR, Parede TR, Espíndola RF, Carvalho RS, Kara-Junior N. Phacoemulsification<br />
versus extracapsular extraction: governmental costs. Clinics. 2010;65(4):<br />
357-61.<br />
9. Guirao A, Redondo M, Artal P. Optical aberrations <strong>of</strong> the human cornea as a function<br />
<strong>of</strong> age. J Opt Soc Am A Opt Image Sci Vis. 2000;17(10):1697-702.<br />
318 Arq Bras Oftalmol. 2012;75(5):316-9
Espíndola RF, et al.<br />
10. Artal P, Berrio E, Guirao A, Piers P. Contribution <strong>of</strong> the cornea and internal surfaces to<br />
the change <strong>of</strong> ocular aberrations with age. J Opt Soc Am A Opt Image Sci Vis. 2002;<br />
19(1):137-43.<br />
11. Kara-Junior N, Santhiago MR. Lentes asféricas: avaliação da indicação clínica e das<br />
opções de lentes. Rev Bras Oftalmol. 2009;68(4):195-6.<br />
12. Santhiago MR, Netto MV, Barreto J Jr, Gomes BA, Mukai A, Guermandi AP, et al. Wavefront<br />
analysis, contrast sensitivity, and depth <strong>of</strong> focus after cataract surgery with<br />
aspherical intraocular lens implantation. Am J Ophtalmol. 2010;149(3):383-9.<br />
13. Caporossi A, Casprini F, Tosi GM, Baiocchi S. Preliminary results <strong>of</strong> cataract extraction<br />
with implantation <strong>of</strong> a single-piece AcryS<strong>of</strong> intraocular lens. J Cataract Refract Surg.<br />
2002;28(4):652-5.<br />
14. Kim YY, Kim JS, Shin DH, Kim C, Jung HR. Effect <strong>of</strong> cataract extraction on blue-on-yellow<br />
visual field. Am J Ophthalmol. 2001;132(2):217-20.<br />
15. Kook MS, Yang SJ, Kim S, Chung J, Kim ST, Tchah H. Effect <strong>of</strong> cataract extraction on<br />
frequency doubling technology perimetry. Am J Ophthalmol. 2004;138(1):85-90.<br />
16. Moss ID, Wild JM, Whitaker DJ. The influence <strong>of</strong> age-related cataract on blue-on-yellow<br />
perimetry. Invest Ophthalmol Vis Sci. 1995;36(5):764-73.<br />
17. Henderson BA, Grimes KJ. Blue-blocking IOLs: a complete review <strong>of</strong> the literature.<br />
Surv Ophthalmol. 2010;55(3):284-9.<br />
18. Cuthbertson FM, Peirson SN, Wulff K, Foster RG, Downes SM. Blue light-filtering intraocular<br />
lenses: review <strong>of</strong> potential benefits and side effects. J Cataract Refract Surg. 2009;35(7):<br />
1281-97. Comment in: J Cataract Refract Surg. 2009;35(11):2032; author reply 2032.<br />
19. Mainster MA. Violet and blue light blocking intraocular lenses: photoprotection<br />
versus photoreception. Br J Ophthalmol. 2006;90(6):784-92.<br />
20. Rodríguez-Galietero A, Montés-Micó R, Muñoz G, Albarrán-Diego C. Comparison <strong>of</strong><br />
contrast sensitivity and color discrimination after clear and yellow intraocular lens<br />
implantation. J Cataract Refract Surg. 2005;31(9):1736-40.<br />
21. Rodríguez-Galietero A, Montés-Micó R, Muñoz G, Albarrán-Diego C. Blue-light filtering<br />
intraocular lens in patients with diabetes: contrast sensitivity and chromatic<br />
discrimination. J Cataract Refract Surg. 2005;31(11):2088-92.<br />
22. Hayashi K, Hayashi H. Visual function in patients with yellow tinted intraocular lenses<br />
compared with vision in patients with non-tinted intraocular lenses. Br J Ophthalmol.<br />
2006;90(8):1019-23.<br />
23. Castro LC, Souza CE, Soriano ES, Melo LA Jr, Paranhos A Jr. Influence <strong>of</strong> blue light<br />
spectrum filter on short-wavelength and standard automated perimetries. Arq Bras<br />
Oftalmol. 2006;69(5):725-9.<br />
24. Jang SY, Ohn YH, Kim SW. Effect <strong>of</strong> yellow-tinted intraocular lenses on short-wavelength<br />
automated perimetry. Am J Ophthalmol. 2010;150(2):243-7. Comment in: Am<br />
J Ophthalmol. 2011;15(2):380; author reply 380-1.<br />
25. Kara-Júnior N, Jardim JL, de Oliveira Leme E, Dall’Col M, Susanna R Jr. Effect <strong>of</strong> the<br />
AcryS<strong>of</strong> Natural intraocular lens on blue-yellow perimetry. J Cataract Refract Surg.<br />
2006;32(8):1328-30.<br />
26. Ueda T, Ota T, Yukawa E, Hara Y. Frequency doubling technology perimetry after clear<br />
and yellow intraocular lens implantation. Am J Ophthalmol. 2006;142(5):856-8.<br />
27. Yuan Z, Reinach P, Yuan J. Contrast sensitivity and color vision with a yellow intraocular<br />
lens. Am J Ophthalmol. 2004;138(1):138-40.<br />
28. Rodriguez-Galietero A, Montes-Mico R, Munoz G, Albarrán-Diego C. Blue-light filtering<br />
intraocular lens in patients with diabetes: contrast sensitivity and chromatic<br />
discrimination. J Cataract Refract Surg. 2005;31(11):2088-92.<br />
29. Mainster M, Sparrow. How much blue-light should an IOL transmit? Br J Ophthalmol.<br />
2003;87(12):1523-9. Comment in: Br J Ophthalmol. 2004;88(10):1353; author reply<br />
1353.<br />
30. Pierre A, Wittich W, Faubert J, Overbury O. Luminance contrast with clear and yellowtin<br />
ted intraocular lenses. J Cataract Refract Surg. 2007;33(7):1248-52.<br />
31. Landers J, Tan TH, Yen J, Liu H. Comparison <strong>of</strong> visual function following implantation<br />
<strong>of</strong> Acris<strong>of</strong> Natural intraocular lenses with conventional intraocular lenses. Clin Experiment<br />
Ophthalmol. 2007;35(2):152-9.<br />
32. Cionni RJ, Tasi JH. Color perception with AcriS<strong>of</strong> natural and AcriS<strong>of</strong> single-piece<br />
intraocular lenses under photopic and mesopic conditions. J Cataract Refract Surg.<br />
2006;32(2):236-42.<br />
XIX Congresso Norte-Nordeste<br />
de Oftalmologia<br />
21 a 23 de março de 2013<br />
Enotel Resort & SPA Porto de Galinhas<br />
Ipojuca (PE)<br />
In<strong>for</strong>mações:<br />
Tel.: (81) 3033-5147<br />
E-mail: secretaria.cnne2013@snno.com.br<br />
Site: www.snno.com.br<br />
Arq Bras Oftalmol. 2012;75(5):316-9<br />
319
Artigo Original | Original Article<br />
Reproducibility <strong>of</strong> peripapillary retinal nerve fiber layer thickness measurements<br />
using Spectral Domain OCT in Brazilian patients<br />
Reprodutibilidade da espessura da camada de fibras nervosas da retina utilizando-se o<br />
Spectral Domain OCT em pacientes brasileiros<br />
Daniela Araújo Toscano 1 , Marcos Pereira de Ávila 2 , Maria Regina Catai Chalita 1<br />
ABSTRACT<br />
Purpose: To evaluate the reproducibility <strong>of</strong> peripapillary retinal nerve fiber layer<br />
(RNFL) thickness measurements in normal eyes and eyes with glaucoma using<br />
spectral domain optical coherence tomography (SDOCT).<br />
Methods: One eye <strong>of</strong> 79 normal and 72 glaucoma patients was analyzed. All<br />
patients underwent a complete ophthalmological examination, including visual<br />
acuity testing; intraocular pressure, slit-lamp examination, indirect ophthalmoscopy;<br />
and the glaucoma group underwent achromatic perimetry with the 24-2<br />
SITA Fast Humphrey Field Analyzer. All patients’ eyes were scanned using the<br />
spectral domain optical coherence tomography - Spectralis ® and one <strong>of</strong> them<br />
was cho sen randomly. Three con secutive circular B-scan centered at the optic<br />
disc were per<strong>for</strong>med in one visit.<br />
Results: The intraclass correlation coefficient (ICC), coefficient <strong>of</strong> variation and<br />
test-retest variability <strong>for</strong> the mean retinal nerve fiber layer thickness were respectively:<br />
0.94, 2.56% and 4.85 µm <strong>for</strong> the normal group and 0.93, 4.65% and 6.61 µm<br />
<strong>for</strong> the glaucomatous group. The intraclass correlation coefficient <strong>for</strong> retinal nerve<br />
fiber layer thickness in all quadrants were all excellent in both groups, with the<br />
superior quadrant having the highest ICCs (0.964) in glaucomatous eyes and nasal<br />
quadrant measurements having the lowest (0.800), but still excellent in eyes without<br />
glaucoma. The coefficient <strong>of</strong> variation was between 2.56% - 8.74% and between<br />
4.65% - 11.44% in normal and glaucomatous group respectively. The test-retest<br />
variability was between 4.85 µm and 11.51 µm in the normal group and between<br />
6.61 µm and 14.24 µm in the glaucomatous group. The measurements in glaucomatous<br />
eyes were more variable than normal eyes.<br />
Conclusions: Spectral domain optical coherence tomography showed excellent<br />
reproducibility with regard to retinal nerve fiber layer thickness measurements in<br />
normal and glaucomatous eyes.<br />
Keywords: Diagnostic techniques, ophthalmological; Glaucoma/diagnosis; Tomography,<br />
optical coherence/methods; Retinal ganglion cells; Optic nerve/pathology;<br />
Nerve fibers; Reproducibility <strong>of</strong> results<br />
RESUMO<br />
Objetivo: Avaliar a reprodutibilidade da medida da espessura da camada de fibras<br />
nervosas da retina (CFNR) em olhos sem e com glaucoma utilizando-se tomografia de<br />
coerência óptica de domínio espectral (spectral domain OCT - SDOCT).<br />
Métodos: Foram analisados apenas um olho de 79 pacientes normais e 72 com glaucoma.<br />
Todos os pacientes realizaram um exame <strong>of</strong>talmológico completo, incluindo<br />
acuidade visual, pressão intraocular, biomicroscopia, <strong>of</strong>talmoscopia indireta e, para o<br />
grupo com glaucoma, perimetria acromática 24-2 SITA Fast Humphrey Field Ana ly zer.<br />
Foram realizados em todos os olhos e em apenas uma visita, três B-scans circulares<br />
centrados no disco óptico utilizando-se o SDOCT - Spectralis ® .<br />
Resultados: O coeficiente de correlação intraclasse (ICC), coeficiente de variação e va -<br />
riabilidade teste-reteste para a média de espessura da camada de fibras nervosas da<br />
retina <strong>for</strong>am respectivamente: 0,94, 2,56% e 4,85 µm para o grupo sem glaucoma e 0,93,<br />
4,65% e 6,61 µm para o grupo glaucomatoso. O coeficiente de correlação intraclasse<br />
foi excelente em ambos os grupos em todos os quadrantes, com o quadrante superior<br />
sendo o maior (0,964) no grupo glaucomatoso e o nasal sendo o menor (0,800), mas<br />
ainda excelente, em olhos sem glaucoma. O coeficiente de variação foi entre 2,56% -<br />
8,74% e entre 4,65% - 11,44%, nos grupos sem e com glaucoma, respectivamente. A<br />
variabilidade teste-reteste variou de 4,85 µm e 11,51 µm no grupo sem glaucoma; e<br />
entre 6,61 µm e 14.24 µm no com glaucoma. Olhos com glaucoma apresentaram-se<br />
mais variáveis que os sem glaucoma.<br />
Conclusão: A tomografia de coerência óptica “spectral domain” apresentou excelente<br />
reprodutibilidade da espessura da camada de fibras nervosas da retina em pacientes<br />
sem e com glaucoma.<br />
Descritores: Técnicas de diagnóstico <strong>of</strong>talmológico; Glaucoma/diagnostico; Tomografia<br />
de coerência óptica/métodos; Células ganglionares da retina; Nervo óptico/patologia;<br />
Fibras nervosas; Reprodutibilidade dos testes<br />
INTRODUCTION<br />
Glaucoma is an optic neuropathy, multifactorial, characterized<br />
by accelerated death <strong>of</strong> the retinal ganglion cells, subsequent axonal<br />
loss, and visual field impairment (1) .<br />
Detected defects in the retinal nerve fiber layer (RNFL) years<br />
be<strong>for</strong>e arising alterations in the visual field suggests that anatomical<br />
alterations <strong>of</strong> the RNFL can identify progression <strong>of</strong> the glaucoma<br />
be<strong>for</strong>e it causes functional loss in the visual field (2) .<br />
Methods <strong>for</strong> reliably establishing glaucomatous nerve atrophy<br />
are limited. Optical coherence tomography (OCT) is a noninvasive,<br />
high-resolution imaging technique that allows in vivo measurements<br />
<strong>of</strong> RNFL in cross section. High-resolution imaging <strong>of</strong> retinal structure<br />
is clinically relevant <strong>for</strong> the diagnosis <strong>of</strong> glaucoma (3) .<br />
Until recently, the OCT commercially available was the time domain<br />
OCT (TDOCT), which provides an axial resolution <strong>of</strong> 10 μm, and<br />
cross sectional retinal images consisting <strong>of</strong> 512 A-scans can be acquired<br />
Submitted <strong>for</strong> publication: October 4, 2011<br />
Accepted <strong>for</strong> publication: August 31, 2012<br />
Study carried out at Department <strong>of</strong> Ophthalmology, Universidade de Brasília - UnB.<br />
1<br />
Physician, Department <strong>of</strong> Ophthalmology, Universidade de Brasília - UnB - Brasília (DF), Brazil.<br />
2<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Ophthalmology, Universidade Federal de Goiás - UFG - Goiânia (GO),<br />
Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: D.A.Toscano, None; M.P.Ávila, None; M.R.C.Chalita,<br />
None.<br />
Correspondence address: Daniela Araújo Toscano. Av. Ingá, 250, Apto. 302 - João Pessoa (PB)<br />
58038-250 - Brazil - E-mail: danielaatoscano@gmail.com<br />
The study was approved by the Institutional Review Board / Ethics Committee <strong>of</strong> the University <strong>of</strong><br />
Brasília (DF) Brazil (CEP-FM 057/2010).<br />
320 Arq Bras Oftalmol. 2012;75(5):320-3
Toscano DA, et al.<br />
in 1.28 seconds. The main disadvantage <strong>of</strong> TDOCT technology is the<br />
limited resolution and slow acquisition time. With the spectral domain<br />
OCT (SDOCT) or Fourier domain, the echo time delays <strong>of</strong> light<br />
are measured by acquiring the interference spectrum <strong>of</strong> the light<br />
signal and converted to depth in<strong>for</strong>mation by Fourier trans<strong>for</strong>m (4) .<br />
The detection method using a spectrometer allowed a considerable<br />
increase in imaging speed and resolution without compromising<br />
image quality (5) . The increase in imaging speed minimizes motion<br />
artifacts. Resolution is up to 5 times higher, and imaging speed<br />
is 60 times faster than in conventional time domain OCT (4) .<br />
Estimate reproducibility <strong>of</strong> RNFL thickness using OCT is essential<br />
<strong>for</strong> diagnostic precision and in particular, describes the smallest<br />
changes detectable <strong>for</strong> identifying and monitoring the progression<br />
<strong>of</strong> glaucoma as well as indicates therapeutic interventions (6,7) .<br />
Quantifying the reproducibility <strong>of</strong> the RNFL thickness measurements<br />
using Spectralis ® spectral domain OCT is an important step in<br />
evaluating the potential usefulness <strong>of</strong> this device <strong>for</strong> the diagnosis <strong>of</strong><br />
glaucoma and <strong>for</strong> determining glaucomatous progression.<br />
To our knowledge the present study is the first to report on the<br />
reproducibility and test-retest variability <strong>of</strong> RNFL thickness measurements<br />
using Spectralis ® SD-OCT device in Brazilian population.<br />
The purpose <strong>of</strong> this study was to evaluate the reproducibility <strong>of</strong><br />
peripapillary retinal nerve fiber layer (RNFL) thickness measurements<br />
in normal and glaucomatous eyes using spectral domain optical<br />
coherence tomography (Spectralis ® ) in Brazilian population.<br />
METHODS<br />
This prospective observational cross-sectional study was approved<br />
by the Institutional Review Board / Ethics Committee <strong>of</strong> the University<br />
<strong>of</strong> Brasília, Brasília, Brazil. All participants in this study gave their written<br />
in<strong>for</strong>med consent. All normal and glaucoma participants were enrolled<br />
in this study through the glaucoma and cataract service <strong>of</strong> Brasília Center<br />
<strong>of</strong> Vision (CBV, Brasília, Brazil) between August and December 2010.<br />
A total <strong>of</strong> 151 eyes from 79 normal patients and 72 patients with moderate<br />
to advanced glaucoma were analyzed. All subjects underwent a<br />
complete ophthalmological examination, including medical and family<br />
history; visual acuity testing with refraction; intraocular pressure measurements<br />
using Goldmann applanation tonometry (GAT), a complete<br />
slit-lamp examination, including indirect ophthalmoscopy. Patients from<br />
the glaucoma group underwent achromatic perimetry using 24-2 SITA<br />
FAST Humphrey Field Analyzer (Humphrey- Zeiss Systems, Dublin CA).<br />
Inclusion criteria <strong>for</strong> both groups were: age more than or equal to<br />
40 years, spherical refractive error less than or equal to 5 diopters (D),<br />
cylindrical refractive error less or equal to 3D.<br />
Inclusion criteria <strong>for</strong> normal subjects were: best-corrected visual<br />
acuity <strong>of</strong> 20/60 or better; normal slit-lamp examination; intraocular pressure<br />
<strong>of</strong> 21 mmHg or less; normal appearing optic nerve heads; and no<br />
history <strong>of</strong> ocular surgery or laser treatments.<br />
Glaucoma patients were defined on the basis <strong>of</strong> having either:<br />
1. An abnormal Humphrey Field Analyzer, defined as having MD<br />
less than -12dB; Less than 50% <strong>of</strong> the points are depressed<br />
bellow the 5% level and less than 20 points are depressed bellow<br />
the 1% level on the patterns deviation plot; No points in the<br />
central 5 o can have a sensitivity <strong>of</strong> 0 dB; Only one hemifield may<br />
have a point with sensitivity <strong>of</strong> < 15 dB within 5 o <strong>of</strong> fixation (8) and<br />
2. Glaucoma optic disc change defined as a cup-to-disc ratio<br />
greater than or equal to 0.6, cup-to-disc ratio asymmetry between<br />
the eyes greater than or equal to 0.2, disc rim thinning,<br />
notching, localized pallor or nerve fiber layer defect (9) .<br />
All patients from the glaucoma group had primary open-angle glau -<br />
coma or chronic angle-closure glaucoma, being excluded any other kind<br />
<strong>of</strong> glaucoma.<br />
Exclusion criteria <strong>for</strong> both groups included other intraocular diseases,<br />
as well as diseases that affect the visual field, like pituitary lesion, diabetes,<br />
retinal conditions or secondary cause <strong>of</strong> intraocular pressure increase.<br />
Patients were excluded in the glaucoma group if they had unreliable<br />
automated perimetry results: fixation loss, false positives or false<br />
negatives more than 33%. Visual fields were carried out at least twice (9) .<br />
OCT measurements<br />
All patients’ eyes were scanned using the commercially available<br />
SDOCT Spectralis ® HRA (Heidelberg Retina Angiograph) + OCT (Heidelberg<br />
Engineering). This instrument uses a wavelength <strong>of</strong> 820 nm<br />
in the near infrared spectrum in the SLO (scanning laser ophthalmoscopy)<br />
mode. The light source <strong>of</strong> the SDOCT is a super luminescent<br />
diode with a wavelength <strong>of</strong> 870 nm. Infrared images and OCT scans<br />
(40,000 A-Scan/sec) <strong>of</strong> the dual laser scanning systems are acquired<br />
simultaneously (10) . Three consecutive circular B-scan (3.4-mm diameter,<br />
768 A-scans) centered at the optic disc were per<strong>for</strong>med in one<br />
visit by the same operator. The scanning circle was centered manually<br />
on the optic disc first, although the participant was looking at the<br />
internal fixation light. The RNFL borders could be clearly identified<br />
and were marked automatically by the segmentation s<strong>of</strong>tware. Ima -<br />
ges were judged to be <strong>of</strong> sufficient quality on the basis <strong>of</strong> subjecti -<br />
ve operator evaluation. Within each scan session, the instrument<br />
alignment and controls were not changed, unless as part <strong>of</strong> image<br />
acquisition process. The subject was repositioned between the scan<br />
measurements only when necessary. There was no specific attempt<br />
to reposition the subjects between scans done during the same session.<br />
Images were acquired through undilated pupils.<br />
The Spectralis ® reports the average RNFL thickness in the superior,<br />
temporal, inferior, nasal and overall (mean). A RNFL thickness<br />
graph includes the colored normative database range.<br />
Eyes were placed into 1 <strong>of</strong> 3 categories that indicate comparison<br />
versus normative database. Green: within normal limits, with values<br />
inside the 95% normal range. Yellow: borderline, with values outside<br />
95% but within 99% confidence interval <strong>of</strong> normal distribution<br />
(0.01
Reproducibility <strong>of</strong> peripapillary retinal nerve fiber layer thickness measurements using Spectral Domain OCT in Brazilian patients<br />
ICC, COV and TRV <strong>for</strong> both groups are presented in tables 3 and<br />
4, respectively. The lowest ICC was 0.800 in the nasal quadrant <strong>for</strong> the<br />
normal group and 0.827 in the temporal quadrant <strong>for</strong> the glaucomatous<br />
group. The highest ICC was 0.944 <strong>for</strong> the mean RNFL in the normal<br />
group and 0.964 <strong>for</strong> the superior quadrant in the glaucomatous group.<br />
Even the lower 95 % CIs were greater 0.70, indicating excellent reproducibility<br />
<strong>of</strong> all measurements. The overall RNFL had the lowest COV<br />
and the nasal quadrant the highest COV in both groups. TRV showed<br />
the lowest <strong>for</strong> the overall RNFL thickness, 4,85 µm in the normal group<br />
and 6.61 µm in the glaucomatous group. The highest TRV was observed<br />
in the nasal quadrant <strong>for</strong> the normal group (11.51 µm) and in the<br />
inferior quadrant <strong>for</strong> the glaucomatous group (14.24 µm). RNFL measurements<br />
in glaucomatous eyes were more variable than normal eyes.<br />
Table 1: Demographic characteristics<br />
Groups<br />
Number<br />
Male<br />
Gender<br />
Female<br />
Age<br />
Normal group 79 49.37% 50.63% 58 (range 40-86)<br />
Glaucomatous group 72 31.94% 68.06 % 68 (range 44-97)<br />
Table 2. RFNL Thickness in normal and glaucomatous groups<br />
Normal group<br />
Glaucomatous group<br />
Thickness<br />
(µm)<br />
Std deviation<br />
(µm)<br />
Thickness<br />
(µm)<br />
Std deviation<br />
(µm)<br />
Mean 096.25 10.28 73.14 15.37<br />
Temporal 071.55 11.69 62.25 12.63<br />
Superior 117.87 14.48 87.02 25.06<br />
Nasal 069.60 12.18 56.45 14.44<br />
Inferior 125.19 15.01 86.86 25.63<br />
Std= standard<br />
Table 3. Intraclass correlation coefficient, coefficient <strong>of</strong> variation and<br />
test-retest variability in normal eyes<br />
ICC COV (%) TRV (µm)<br />
Mean 0.944 (0.921) 2.56 04.85<br />
Temporal 0.895 (0.852) 5.93 08.41<br />
Superior 0.928 (0.898) 4.09 09.49<br />
Nasal 0.800 (0.726) 8.74 11.51<br />
Inferior 0.931 (0.902) 3.80 09.33<br />
ICC= intraclass correlation coefficient, with lower 95% CI (confidence interval) in parentheses;<br />
COV= coefficient <strong>of</strong> variation; TRV= test-retest variability<br />
Table 4. Intraclass correlation coefficient, coefficient <strong>of</strong> variation and<br />
test-retest variability in glaucomatous eyes<br />
ICC COV (%) TRV (µm)<br />
Mean 0.937 (0.908) 04.65 06.61<br />
Temporal 0.827 (0.757) 08.44 09.95<br />
Superior 0.964 (0.947) 07.23 11.15<br />
Nasal 0.877 (0.824) 11.44 11.78<br />
Inferior 0.855 (0.795) 08.60 14.24<br />
ICC= intraclass correlation coefficient, with lower 95% CI (confidence interval) in parentheses;<br />
COV= coefficient <strong>of</strong> variation; TRV= test-retest variability<br />
DISCUSSION<br />
In glaucoma patients the OCT is an important instrument <strong>for</strong><br />
diagnosis and to follow the progression <strong>of</strong> the disease. Assessing<br />
the reproducibility <strong>of</strong> the RNFL thickness using OCT is <strong>of</strong> paramount<br />
importance <strong>for</strong> its use in clinical practice <strong>of</strong> glaucoma.<br />
This study showed excellent reproducibility <strong>of</strong> RNFL thickness<br />
measurements with Spectralis ® in patients without and with moderate<br />
to advanced glaucoma (generally defined as 0.75 - 1.00). The<br />
lowest ICCs were observed in the nasal quadrant <strong>for</strong> the patients<br />
without glaucoma (0.800) and in the temporal quadrant (0.827) <strong>for</strong><br />
patients with glaucoma. Even the lower 95% CIs were greater 0.70,<br />
indicating excellent reproducibility <strong>of</strong> all measurements.<br />
Comparing two different SD OCTs (Cirrus TM and Spectralis ® ), excellent<br />
repeatability <strong>of</strong> RNFL thickness measurement was observed<br />
in normal participants <strong>for</strong> both devices. Using Spectralis ® in undilated<br />
pupils the average <strong>of</strong> TRV was 4.95, COV 1.7% and ICC 0.971 (11) . In our<br />
study the TRV was 4.85, COV 2.56% and ICC 0.944. These differences<br />
can be explained because the number and the age <strong>of</strong> the participants<br />
in our study were higher.<br />
Many other studies reported the reproducibility <strong>of</strong> RNFL thickness<br />
using different kinds <strong>of</strong> OCT. Blumenthal et al., in 1999 studied 10<br />
eyes with glaucoma and 10 normal eyes and reported, using the<br />
commercially available OCT, that glaucoma patients were found to<br />
be significantly more variable than normal subjects (P=0.03). The<br />
coefficient <strong>of</strong> variation <strong>for</strong> the mean RNFL thickness was significantly<br />
smaller (P=0.02) in normal eyes (6.9%) than in glaucomatous eyes<br />
(11.8%). The coefficient <strong>of</strong> variation was larger in the temporal and<br />
nasal quadrants than in the superior and inferior quadrants, as found<br />
in our study (12) .<br />
Studies with Stratus TM OCT showed good RNFL thickness reproducibility.<br />
Peripapillary RNFL thickness <strong>of</strong> 51 subjects with glaucoma<br />
was measured using the Standard and Fast scan protocols <strong>of</strong> Stratus TM<br />
OCT 3 times on the same day to determine intrasession variability and<br />
on 5 different days within a 2-month period to determine intersession<br />
variability. It was observed the RNFL thickness test-retest variability<br />
intrasession ranged between 5.2 µm and 17.1 µm (mean 5.2 µm) using<br />
standard protocol and between 5 µm and 16.7 µm (mean 5.0 µm) <strong>for</strong><br />
fast protocol, <strong>for</strong> clock hours. The test-retest variability <strong>of</strong> the temporal<br />
quadrant and <strong>of</strong> most temporal clock hours seemed to be less than<br />
that <strong>of</strong> other quadrants or locations, and the Fast scanning protocol,<br />
ICC and COV tended also to be worst <strong>for</strong> the nasal quadrant, similar<br />
to our results. The best ICC was 0.98 <strong>for</strong> both protocols. Intraclass<br />
correlation coefficients were essentially all excellent with the mean<br />
Standard RNFL and Fast RNFL values having the highest <strong>of</strong> 0.98 (13) .<br />
Still assessing the reproducibility <strong>of</strong> the Stratus TM , Budenz et al.,<br />
per<strong>for</strong>med 3 peripapillary circulars scans in 147 subjects normal and<br />
with glaucoma. The ICC was excellent <strong>for</strong> both Standard (mean 0.97)<br />
and Fast (mean 0.95) RNFL measurements. TRV <strong>of</strong> the quadrants measurements<br />
ranged from 3.5 µm to 13.0 µm in normal subjects and<br />
5.2 µm to 13.8 µm in glaucomatous eyes analyzing standard and<br />
fast protocols, and four quadrants (14) . Reproducibility <strong>of</strong> Stratus TM<br />
OCT as also studied in 10 normal subjects that were scanned three<br />
consecutive times with each <strong>of</strong> the following: macular scans, RNFL<br />
scans, and ONH scans be<strong>for</strong>e dilation and three additional times <strong>for</strong><br />
each scan type after dilation. Similarly, all the subjects were scanned<br />
on two additional days within 5 months and the inter and intravisit<br />
reproducibility was calculated. The ICCs <strong>for</strong> the RNFL quadrants<br />
were higher after dilation, ranging between 71% and 84%, with the<br />
exception <strong>of</strong> the superior quadrant (ICC was 79% be<strong>for</strong>e and 75%<br />
after dilation). Stratus TM OCT demonstrated reproducible measurements<br />
<strong>for</strong> NFL thickness, macular thickness, and optic nerve head<br />
parameters (15) .<br />
The reproducibility <strong>of</strong> macula thickness using spectral domain<br />
OCT (Spectralis ® ) was studied in 41 normal eyes. Intravisit reproducibility<br />
was analyzed by per<strong>for</strong>ming 3 scans in the macula. It was<br />
322 Arq Bras Oftalmol. 2012;75(5):320-3
Toscano DA, et al.<br />
observed excellent reproducibility <strong>of</strong> retinal thickness measurements<br />
with mean difference among measurements <strong>of</strong> about 1 µm (6) .<br />
Other SDOCT were also analyzed as RTVue which the RNFL thickness<br />
reproducibility showed the ICC ranged between 0.91 and 0.97 <strong>for</strong><br />
the healthy group (60 eyes) and 0.86 and 0.97 <strong>for</strong> the glaucomatous<br />
group (76 eyes) (7) . Using the SD SLO/OCT OTI the lowest ICC was 0.961<br />
at 3 o’clock in the normal group (98 eyes) and 0.951 at 4 o’clock in the<br />
glaucoma group (79 eyes) (9) .<br />
Bendschneider et al., analyzed the RNFL thickness in 170 healthy<br />
patients using the SDOCT Spectralis ® and observed that the RNFL<br />
thickness was significantly associated with age (1.9 µm decline in<br />
mean total RNFL thickness per age decade), axial length (total RNFL<br />
decrease <strong>of</strong> -4.79 mm per every increasing 1-mm-axial length) and<br />
optic disc area (with a total RNFL increase <strong>of</strong> 6.28 mm <strong>for</strong> every<br />
1-mm 2 -increase in disc area). The total RNFL thickness in the study<br />
population was 97.2 ± 9.7 µm, which is comparable to our study<br />
(96.25 µm ± 10.28) (10) .<br />
Recently, Wu et al., reported the reproducibility <strong>of</strong> Spectralis in<br />
45 normal patients and 33 glaucoma patients. Their ICCs ranged<br />
from 0.977 (temporal) to 0.990 (global and inferior-nasal sector) in<br />
normal eyes, and from 0.983 (temporal) to 0.997 (inferior quadrant)<br />
in glaucomatous eyes. CVs ranged from 1.45% (overall global) to<br />
2.59% (temporal quadrant) <strong>for</strong> normal participants and ranged from<br />
1.74% (overall global) to 3.22% (temporal quadrant) <strong>for</strong> glaucoma<br />
patients (16) . There were some differences between this study and the<br />
present study: they analyzed the RNFL thickness using more than<br />
four quadrants (overall global - 360 degrees), <strong>for</strong> 4 quadrants (superior,<br />
inferior, nasal, and temporal), and then <strong>for</strong> 4 additional sectors:<br />
superior-temporal (TS, 45 to 90 degrees), superior-nasal (NS, 90 to<br />
135 degrees), inferior-nasal (NI, 225 to 270 degrees), and inferior-<br />
-temporal (TI, 270 to 315 degrees); the number <strong>of</strong> participants was<br />
smaller than ours; the subjects had different types <strong>of</strong> glaucoma,<br />
in cluding pseudoexfoliation glaucoma; and they used the TruTrack<br />
image alignment s<strong>of</strong>tware (i.e., the eye tracking system). Probably<br />
because <strong>of</strong> all these facts theirs ICC and COV were better than the<br />
present study, especially because <strong>of</strong> the tracking system.<br />
Evaluating the impact <strong>of</strong> Spectralis ® self-acting eye tracking<br />
system and retest s<strong>of</strong>tware on the reproducibility <strong>of</strong> RNFL thickness<br />
measurements in glaucomatous and healthy eyes it was observed<br />
that the reproducibility can be improved by using the eye tracker,<br />
and this gain was significantly higher in glaucomatous than in healthy<br />
eyes. In healthy subjects, COVs <strong>for</strong> RNFL thickness measurements<br />
without using the system ranged from 3.5% to 7.4% and with the eye<br />
tracker and retest protocol ranged from 1.0% to 2.5%. In glaucoma<br />
patients measurements without the eye tracker ranged from 5.8%<br />
to 10.5% and with the system ranged from 1.6% to 3.8%. The improvement<br />
in reproducibility was significantly higher in glaucomatous<br />
than in healthy eyes (17) . Our study showed COV ranged from 4.65%<br />
to 11.44% in the glaucomatous group similar to the previous study<br />
without using the eye tracker system. Despite not using the eye<br />
tracking system, our study showed an excellent reproducibility <strong>of</strong><br />
RNFL thickness in normal and glaucomatous eyes. It is necessary<br />
to emphasize that the patients included in the present study had<br />
moderate to advanced glaucoma with difficult to fixation on one or<br />
both eyes and it may have contributed to the high COV.<br />
CONCLUSION<br />
The Spectralis ® spectral domain OCT equipped showed excellent<br />
reproducibility with regards to RNFL thickness measurements in normal<br />
and in moderate to advanced glaucoma patients.<br />
REFERENCES<br />
1. Sehi M, Grewal DS, Sheets CW, Greenfield DS. Diagnostic ability <strong>of</strong> Fourier-domain<br />
vs time-domain optical coherence tomography <strong>for</strong> glaucoma detection. Am J Ophthalmol.<br />
2009;148(4):597-605.<br />
2. Sommer A, Miller NR, Pollack I, Maumenee AE, George T. The nerve fiber layer in the<br />
diagnosis <strong>of</strong> glaucoma. Arch Ophthalmol. 1977;95(12):2149-56.<br />
3. Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, et al. Optical coherence<br />
tomography. Science. 1991;254(5035):1178-81.<br />
4. Chen TC, Cense B, Pierce MC, Nassif N, Park BH, Yun SH, et al. Spectral domain optical<br />
coherence tomography: ultra-high speed, ultra-high resolution ophthalmic imaging.<br />
Arch Ophthalmol. 2005;123(12): 1715-20.<br />
5. Nassif N, Cense B, Park B, Pierce M, Yun S, Bouma B, et al. In vivo high-resolution<br />
video-rate spectral-domain optical coherence tomography <strong>of</strong> the human retina and<br />
optic nerve. Opt Express. 2004;12(3):367-76.<br />
6. Menke MN, Dabov S, Knecht P, Sturm V. Reproducibility <strong>of</strong> retinal thickness measurements<br />
in healthy subjects using spectralis optical coherence tomography. Am J<br />
Oph thalmol. 2009;147(3):467-72.<br />
7. Gonzalez-Garcia AO, Vizzeri G, Bowd C, Medeiros FA, Zangwill LM, Weinreb RN. Reproducibility<br />
<strong>of</strong> RTVue retinal nerve fiber layer thickness and optic disc measurements<br />
and agreement with Stratus optical coherence tomography measurements. Am J<br />
Ophthalmol. 2009;147(6):1067-74, 1074 e1.<br />
8. Leung CK, Ye C, Weinreb RN, Cheung CY, Qiu Q, Liu S, et al. Retinal nerve fiber layer<br />
imaging with spectral-domain optical coherence tomography a study on diagnostic<br />
agreement with Heidelberg Retinal Tomograph. Ophthalmology. 2010;117(2):267-74.<br />
9. Lee SH, Kim SH, Kim TW, Park KH, Kim DM. Reproducibility <strong>of</strong> retinal nerve fiber thickness<br />
measurements using the test-retest function <strong>of</strong> spectral OCT/SLO in normal and<br />
glaucomatous eyes. J Glaucoma. 2010;19(9):637-42.<br />
10. Bendschneider D, Tornow RP, Horn FK, Laemmer R, Roessler CW, Juenemann AG, et<br />
al. Retinal Nerve Fiber Layer Thickness in Normals Measured by Spectral Domain OCT.<br />
J Glaucoma. 2010;19(7):475-82.<br />
11. Tan BB, Natividad M, Chua KC. Comparison <strong>of</strong> retinal nerve fiber layer measurement<br />
between 2 spectral domain OCT instruments. J Glaucoma. 2012;21(4):266-73.<br />
12. Blumenthal EZ, Williams JM, Weinreb RN, Girkin CA, Berry CC, Zangwill LM. Reproducibility<br />
<strong>of</strong> nerve fiber layer thickness measurements by use <strong>of</strong> optical coherence<br />
to mography. Ophthalmology. 2000;107(12):2278-82.<br />
13. Budenz DL, Fredette MJ, Feuer WJ, Anderson DR. Reproducibility <strong>of</strong> peripapillary<br />
retinal nerve fiber thickness measurements with stratus OCT in glaucomatous eyes.<br />
Ophthalmology. 2008;115(4):661-6. e4.<br />
14. Budenz DL, Chang RT, Huang X, Knighton RW, Tielsch JM. Reproducibility <strong>of</strong> retinal<br />
nerve fiber thickness measurements using the stratus OCT in normal and glaucomatous<br />
eyes. Invest Ophthalmol Vis Sci. 2005;46(7):2440-3.<br />
15. Paunescu LA, Schuman JS, Price LL, Stark PC, Beaton S, Ishikawa H, et al. Reproducibility<br />
<strong>of</strong> nerve fiber thickness, macular thickness, and optic nerve head measurements<br />
using StratusOCT. Invest Ophthalmol Vis Sci. 2004;45(6):1716-24.<br />
16. Wu H, de Boer JF, Chen TC. Reproducibility <strong>of</strong> retinal nerve fiber layer thickness<br />
mea surements using spectral domain optical coherence tomography. J Glaucoma.<br />
2011;20(8):470-6.<br />
17. Langenegger SJ, Funk J, Toteberg-Harms M. Reproducibility <strong>of</strong> retinal nerve fiber<br />
layer thickness measurements using the eye tracker and the retest function <strong>of</strong><br />
Spectralis SD-OCT in glaucomatous and healthy control eyes. Invest Ophthalmol Vis<br />
Sci. 2011;52(6):3338-44.<br />
Arq Bras Oftalmol. 2012;75(5):320-3<br />
323
Artigo Original | Original Article<br />
Radiation therapy <strong>for</strong> Graves’ ophthalmopathy: a systematic review and<br />
meta-analysis <strong>of</strong> randomized controlled trials<br />
Radioterapia para <strong>of</strong>talmopatia de Graves: uma revisão sistemática e meta-análise de<br />
ensaios clínicos randomizados e controlados<br />
Gustavo Arruda Viani 1 , André Campiolo Boin 2 , Ligia Issa De Fendi 3 , Ellen Carrara Fonseca 3 , Eduardo Jose Stefano 1 , Jayter Silva de Paula 4<br />
ABSTRACT<br />
Purpose: To evaluate the efficacy <strong>of</strong> radiotherapy (RT) with total dose <strong>of</strong> 20 Gy<br />
(RT 20 Gy) in the treatment <strong>of</strong> Graves’ ophthalmopathy.<br />
Methods: A systematic review and meta-analysis <strong>of</strong> randomized controlled trials<br />
was per<strong>for</strong>med comparing RT 20 Gy with or without glucocorticoid to cli nical<br />
treatments <strong>for</strong> Graves’ ophthalmopathy. The MEDLINE, EMBASE, Cochrane Library<br />
databases and recent relevant journals were searched. Relevant reports were<br />
reviewed by two reviewers. Response to radiotherapy was defined as clinical<br />
success according to each trial. We also evaluated the quality <strong>of</strong> life and whether<br />
RT to produce fewer side effects than other treatments.<br />
Results: A total <strong>of</strong> 8 randomized controlled trials (439 patients) were identified.<br />
In the subgroup analysis, the overall response to treatment rates was better <strong>for</strong>:<br />
RT 20 Gy plus glucocorticoid vs glucocorticoids alone, OR=17.5 (CI95% 1.85-250,<br />
p=0.04), RT 20 Gy vs sham RT, OR= 3.15 (CI95%1.59-6.23, p=0.003) and RT 20Gy plus<br />
intravenous glucocorticoid vs RT 20Gy plus oral glucocorticoid, OR=4.15(CI95%<br />
1.34-12.87, p=0.01). There were no differences between RT 20 Gy versus other<br />
fractionations and RT 20 Gy versus glucocorticoid alone. RT 20 Gy with or without<br />
glucocorticoids showed an improvement in diplopia grade, visual acuity, optic<br />
neuropathy, lid width, proptosis and ocular motility. No difference was seen <strong>for</strong><br />
costs, intraocular pressure and quality <strong>of</strong> life.<br />
Conclusion: Our data have shown that RT 20 Gy should be <strong>of</strong>fered as a valid the -<br />
rapeutic option to patients with moderate to severe ophthalmopathy. The effectiveness<br />
<strong>of</strong> orbital radiotherapy can be increased by the synergistic interaction with<br />
glucocorticoids. Moreover, RT 20 Gy is useful to improve a lot <strong>of</strong> ocular symptoms,<br />
excluding intraocular pressure, without any difference in quality <strong>of</strong> life and costs.<br />
Keywords: Graves ophthalmopathy; Exophthalmos; Radiotherapy; Meta-analysis,<br />
Review<br />
RESUMO<br />
Objetivo: Avaliar a eficácia da radioterapia (RT) com dose total de 20 Gy (RT 20 Gy)<br />
no tratamento da <strong>of</strong>talmopatia de Graves.<br />
Métodos: Uma revisão sistemática e meta-análise de ensaios clínicos randomizados<br />
<strong>for</strong>am realizadas comparando RT 20 Gy, com ou sem glicocorticoides a tratamentos<br />
clinicos para a <strong>of</strong>talmopatia de Graves. O MEDLINE, EMBASE, bases de dados da<br />
Biblioteca Cochrane e recentes de revistas relevantes <strong>for</strong>am pesquisados. Relatórios<br />
relevantes <strong>for</strong>am revisados por dois revisores. A resposta à radioterapia foi definida<br />
através do sucesso clinico de acordo a cada ensaio clínico. Nós também avaliamos a<br />
qualidade de vida e se a radioterapia produzia menos efeitos colaterais comparados<br />
a outras intervenções.<br />
Resultados: Um total de 8 ensaios clínicos randomizados (439 pacientes) <strong>for</strong>am iden -<br />
tificados. Na análise de subgrupo, a resposta global para as taxas de tratamento foi<br />
melhor para: RT 20 Gy além de glicocorticoides vs glicocorticoides sozinhos, OR=17,5<br />
(IC95% 1,85-250, p=0,04), RT 20 Gy vs sham RT, OR=3,15 (IC95% 1,59-6,23, p=0,003) e<br />
RT 20 Gy além de glicocorticoides por via intravenosa RT 20 Gy além de glicocorticoides<br />
orais, OR=4,15 (IC95% 1,34-12,87, p=0,01). Não houve diferenças entre RT 20 Gy contra<br />
outros fracionamentos e 20 Gy RT contra glicocorticoides sozinhos. RT 20 Gy, com<br />
ou sem glicocorticoides mostraram uma melhoria no grau de diplopia, acuidade<br />
visual, neuropatia óptica, abertura palpebral, proptose e da motilidade ocular. Não<br />
foi observada diferença para os custos, a pressão intraocular e a qualidade de vida.<br />
Conclusão: Nossos dados mostraram que 20 Gy RT deve ser <strong>of</strong>erecida como uma opção<br />
terapêutica válida para pacientes com moderada a severa <strong>of</strong>talmopatia de Graves. A<br />
eficácia da radioterapia orbital pode ser aumentada pela interação sinérgica com os<br />
glicocorticoides. Além disso, RT 20 Gy é útil para melhorar vários sintomas oculares,<br />
excluindo a pressão intraocular, sem qualquer diferença de qualidade de vida.<br />
Descritores: Oftalmopatia de Graves; Ex<strong>of</strong>talmia; Radioterapia; Meta-análise, Revisão<br />
INTRODUCTION<br />
Graves’ ophthalmopathy is a debilitating disease impairing the<br />
quality <strong>of</strong> life <strong>of</strong> the affected individuals. Despite recent progress in<br />
the understanding <strong>of</strong> its pathogenesis, treatment is <strong>of</strong>ten not sa -<br />
tisfactory. In mild cases, local therapeutic measures (artificial tears<br />
and ointments, sunglasses, nocturnal eyes taping, prisms) can control<br />
symptoms and signs. In severe <strong>for</strong>ms <strong>of</strong> the disease, aggressive<br />
measures are required. The management strategy <strong>for</strong> moderate tosevere<br />
Graves’ ophthalmopathy is controversial. Systemic steroids are<br />
<strong>of</strong>ten effective (1-4) , but relapse is common when they are tapered or<br />
withdrawn (5) . A number <strong>of</strong> retrospective studies have reported the<br />
efficacy <strong>of</strong> orbital irradiation (6,7) but prospective studies have shown<br />
conflicting results (8-10) . Some investigators have suggested that ste -<br />
roids provide excellent improvement in orbital inflammation in the<br />
short term, whereas the effects <strong>of</strong> orbital irradiation take longer to<br />
appear (11) . Studies that have compared combination therapy <strong>of</strong> or -<br />
bi tal irradiation and systemic steroids with steroids alone therapy<br />
have produced conflicting results (12-18) . The accomplishment <strong>of</strong> a<br />
sys tematic review is the best manner <strong>for</strong> describing the state <strong>of</strong> our<br />
knowledge, and hence becomes the best way <strong>of</strong> obtaining high<br />
qua lity scientific evidence. Consequently, this systematic review was<br />
proposed to analyze the results from clinical trials that compared ra -<br />
diotherapy to any other treatment.<br />
Submitted <strong>for</strong> publication: February 6, 2012<br />
Accepted <strong>for</strong> publication: August 27, 2012<br />
Study carried out at Faculty <strong>of</strong> Medicine <strong>of</strong> Marília, Department <strong>of</strong> Radiation Oncology.<br />
1<br />
Physician, Radiation Oncology Department, Escola de Medicina de Marília, Marília (SP), Brazil.<br />
2<br />
Medical Student, Escola de Medicina de Marília, Marília (SP), Brazil.<br />
3<br />
Department <strong>of</strong> Ophthalmology, Escola de Medicina de Marília, Marília (SP), Brazil.<br />
4<br />
Physician, Department <strong>of</strong> Ophthalmology, Escola de Medicina de Ribeirão Preto, Universidade de<br />
São Paulo - USP - Ribeirão Preto (SP), Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: G.A.Viani, None; A.C.Boin, None; L.I.De Fendi, None;<br />
E.C.Fonseca, None; E.J.Stefano, None; J.S.de Paula, None.<br />
Correspondence address: Gustavo Arruda Viani. Rua Coronel José Brás, 205/72 - Marília (SP) -<br />
17501-570 - Brazil - E-mail-gusviani@gmail.com<br />
324 Arq Bras Oftalmol. 2012;75(5):324-32
Viani GA, et al.<br />
METHODS<br />
Types <strong>of</strong> studies<br />
This systematic review properly included randomized controlled<br />
clinical trials. Any trial including only patients with mild Graves<br />
ophthalmopathy (GO), or any trial including patients with moderate-severe<br />
GO were included. The participants <strong>of</strong> studies included<br />
patients with GO diagnosis <strong>for</strong> the first time, not resistant to previous<br />
treatment and with no age limit. The intervention criteria to be included<br />
in this review was any trial in which radiotherapy with total<br />
dose <strong>of</strong> 20 Gy associated or not to glucocorticoid (<strong>of</strong> any kind) was<br />
the primary treatment compared to radiotherapy (RT) with total<br />
dose different <strong>of</strong> 20 Gy, no radiotherapy or any another treatment.<br />
The efficacy <strong>of</strong> radiotherapy was evaluated following measures<br />
after treatment. The lid width was measured as the widest vertical<br />
dimension, proptosis was measured by an exophthalmometer, ocular<br />
motion was measured in degrees or constancy <strong>of</strong> diplopia, intraocular<br />
pressure measured using an applanation tonometer, optic nerve<br />
function was assessed by recording <strong>of</strong> the corrected visual acuity<br />
or fundoscopy. Response to radiotherapy was defined as clinical<br />
suc cess according to each trial. We also evaluated the quality <strong>of</strong> life<br />
and whether RT produced fewer side effects than other treatments.<br />
Medline and manual searches were done (completed independently<br />
and in duplicate) to identify all published (manuscripts and abstracts)<br />
randomized controlled trials (RCTs) that compared radiotherapy <strong>for</strong><br />
GO to any treatment. The Medline search was done between 1966<br />
and 2006 with no language restrictions, using the search terms<br />
“ophthalmopathy,” orbitopathy” and “Graves’ ophthalmopathy,” “radiotherapy”<br />
or “orbital radiotherapy,” and “retro ocular radiotherapy”.<br />
The second search was done through EMBASE and the Cochrane Li -<br />
brary to identify randomized trials published between January 1998<br />
and July 2006, using MeSH headings (ophthalmopathy, orbipathy,<br />
Graves’ ophthalmopathy, orbital radiotherapy, retro ocular radiotherapy<br />
/sc {Secondary}, ex-lode Clinical Trials, clinical trial {publication<br />
type}) and text words (retro ocular radiotherapy radiotherapy, Graves’<br />
ophthalmopathy, trial, and study) without language restrictions. All<br />
the searched abstracts were screened <strong>for</strong> relevance. Manual searches<br />
were done by reviewing articles and abstracts cited in the reference<br />
lists <strong>of</strong> identified RCTs, by reviewing the first author’s article, abstract<br />
file, from reference lists <strong>of</strong> retrieved papers, textbooks and review<br />
articles. Hand searches were carried out in the following journals<br />
between January Ophthalmology; Lancet; Ophthalmology; International<br />
Journal <strong>of</strong> Radiation Oncology, Biology, and Physics; and Journal <strong>of</strong><br />
Clinical endocrinology and metabolism. Reference lists from identified<br />
studies and other relevant publications were scrutinized. Colleagues,<br />
collaborators, and other experts were contacted about ongoing and<br />
unpublished trials. From the titles and abstracts, relevant RCTs were<br />
identified. Two independent reviewers (V.A.G., A.C.B.) then assessed<br />
the RCTs to establish if predetermined inclusion criteria were met.<br />
Study suitableness was assessed using QUOROM criteria (19) . The RCTs<br />
were also independently assessed <strong>for</strong> quality according to predetermined<br />
criteria (method <strong>of</strong> randomization, blinding, statistical methods,<br />
quality <strong>of</strong> life assessment, data completeness, follow-up), and<br />
the data extracted and tabulated. Discrepancies between the two<br />
reviewers were resolved by discussion. The intention was to carry out<br />
a meta-analysis <strong>of</strong> outcomes if there were enough trials <strong>of</strong> sufficient<br />
quality and homogeneity.<br />
Statistics<br />
The efficacy <strong>of</strong> radiotherapy treatment with total dose <strong>of</strong> 20 Gy<br />
was measured through the response to treatment described in each<br />
trial. Responders to treatment were defined as patients who presented<br />
overall response to radiotherapy or other treatment, according<br />
to clinical success defined according to each trial. The data analyses<br />
were made with Review Manager Version 5.1 provided by The Cochrane<br />
Collaboration. All analyses were carried out on an intention<br />
to treat basis; that is, all patients randomly assigned to a treatment<br />
group were included in the analyses according to the assigned treatment,<br />
irrespective <strong>of</strong> whether they received the treatment or were<br />
excluded from analysis by the investigators. For categorical variables,<br />
weighted risk ratios and their 95% confidence interval were calculated<br />
using RevMan 5.1 s<strong>of</strong>tware according to the Peto method (20) .<br />
Results were tested <strong>for</strong> heterogeneity at significance level <strong>of</strong> P
Radiation therapy <strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized controlled trials<br />
RT: radiation therapy; RCT: randomized controlled trial.<br />
Figure 1. Flowchart according to QUOROM statement criteria.<br />
three RCTs, (12,13,16) only one trial (13) showed benefit <strong>for</strong> RT 20 Gy arms.<br />
Diplopia was assessed in five RCTs (9,10,12,14,15) <strong>of</strong> these studies Prummel<br />
et al., (15) and Mourits et al. (9) founded significant differences between<br />
radiotherapy versus sham radiotherapy <strong>for</strong> changes in diplopia, in<br />
the other studies it was not seen. Intraocular pressure was tested in<br />
two RCTs (12,16) , one per<strong>for</strong>med by Ng et al. (16) , and another by Kahaly<br />
et al. (12) , in both studies no benefit was seen in combined orbital<br />
irradiation and systemic steroids or using low dose <strong>of</strong> radiotherapy.<br />
Mar cocci et al. (14) , was the only trial to assess the efficacy <strong>of</strong> radiotherapy<br />
to improve optic neuropathy. In this study combined orbital<br />
irradiation and systemic steroids were associated with significant<br />
difference to improve optic neuropathy.<br />
<strong>Ocular</strong> motility and clinical response was tested in all RCTs (8-10,12-16) .<br />
RT 20 Gy with or without glucocorticoid achieved significant statistical<br />
difference in five <strong>of</strong> the eight trials evaluated <strong>for</strong> clinical response.<br />
<strong>Ocular</strong> motility was improved in six trials (8,9,13-16) comparing RT 20 Gy<br />
with other treatments. Table 2 summarizes the parameters evaluated<br />
and the treatment results. According to the Jadad criteria, we<br />
assessed the quality <strong>of</strong> the randomized and comparative trials with<br />
regard to: a) method <strong>of</strong> randomization, b) treatment allocation, c)<br />
similarity between groups, d) specification <strong>of</strong> eligible criteria, e) blinded<br />
outcome <strong>of</strong> assessor, care provider and patient (22) . Applying these<br />
criteria made clear that the quality <strong>of</strong> the trials was high, as showed<br />
in the table 3 which describes in details the trials design, aim, study<br />
question, results, and conclusions.<br />
Response to treatment<br />
All the studies reported response to treatment as one <strong>of</strong> the out -<br />
comes. The criterions <strong>for</strong> evaluation <strong>of</strong> the response to treatment<br />
were heterogeneous between the trials. Altogether, the analyses<br />
included 8 trials with 439 patients (9, 10, 12-16) . The individual odds ratios<br />
ranged from 0.87 to 17.5 with a pooled odds ratio <strong>for</strong> all <strong>of</strong> the trials<br />
<strong>of</strong> 2.14 with a 95% confidence interval <strong>of</strong> 1.44 to 3.18. The test <strong>for</strong><br />
heterogeneity was not statistically significant with p value 0.14, which<br />
indicates that the pooling <strong>of</strong> the data was valid. The overall odds ratio<br />
suggests that there is difference between RT 20 Gy arms and other<br />
treatments in terms <strong>of</strong> response to treatment rate with p value 0.0002,<br />
as shown in the figure 2.<br />
Radiotherapy versus sham radiotherapy<br />
Three trials (9,10,15) with 190 patients evaluated response to treatment<br />
comparing radiotherapy versus sham radiotherapy. The in -<br />
dividual odds ratios ranged from 1 to 3.5 with a pooled odds ratio<br />
<strong>for</strong> all <strong>of</strong> the trials <strong>of</strong> 3.15 with a 95% confidence interval <strong>of</strong> 1.59 to<br />
6.23. The test <strong>for</strong> heterogeneity was not statistically significant with<br />
p value 0.28, which indicates that the pooling <strong>of</strong> the data was valid.<br />
326 Arq Bras Oftalmol. 2012;75(5):324-32
Viani GA, et al.<br />
Table 1. Characteristics <strong>of</strong> the patients, parameters <strong>of</strong> the treatment, status <strong>of</strong> GO and end points <strong>of</strong> the studies included in this meta-analysis<br />
Trial (year)<br />
Prummel et al.,<br />
(2004)<br />
Marcocci et al.,<br />
(2001)<br />
Kahaly et al.,<br />
(2000)<br />
Patients/<br />
treatment<br />
88<br />
RT: 44<br />
NO RT: 44<br />
82<br />
RT+IVGC:41<br />
RT+ORGC:41<br />
62<br />
A=18 1 Gray/week<br />
20 Gray/20 weeks<br />
B=22 1 Gray/day<br />
10 Gray/2 weeks<br />
C=22 2 Gray/day<br />
20 Gray/2 weeks<br />
Ng et al., (2005) 16<br />
RT+GC:8<br />
GC:8<br />
Bartalena et al.,<br />
(1983)<br />
Gorman et al.,<br />
(2002)<br />
Prummel et al.,<br />
(1993)<br />
Mourits et al.,<br />
(2000)<br />
48<br />
RT+GC36<br />
GC:12<br />
42<br />
RT:21<br />
NO RT:21<br />
56<br />
RT:28<br />
GC:28<br />
60<br />
RT: 30<br />
NO RT: 30<br />
Diagnostic<br />
Signs and symptoms with<br />
enlarged <strong>extraocular</strong> eye <strong>muscles</strong> on<br />
coronal computed tomography scan<br />
<strong>of</strong> the orbits<br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong> on coronal<br />
computed tomography scan <strong>of</strong> the<br />
orbits<br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong> on magnetic<br />
resonance imaging (MRI)<br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong> on<br />
computed tomography or<br />
magnetic resonance imaging (MRI)<br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong><br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong> on<br />
computed tomography<br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong><br />
Signs and symptoms with enlarged<br />
<strong>extraocular</strong> eye <strong>muscles</strong> on coronal<br />
computed tomography scan <strong>of</strong> the<br />
orbits<br />
Status GO/treatment<br />
hypertireoidism<br />
Mild, antithyroid drugs,<br />
TSH supression<br />
Moderate-to-severe<br />
methimazole<br />
<strong>for</strong> 3-4 months be<strong>for</strong>e<br />
radioiodine therapy<br />
Mild to moderate eye<br />
disease, euthyroidism,<br />
antithyroid drugs<br />
Moderate-to-severe<br />
ophthalmopathy,<br />
anti-thyroid drugs,<br />
radioactive iodine,<br />
thyroidectomy<br />
Moderate-to-severe<br />
ophthalmopathy,<br />
anti-thyroid drugs,<br />
radioactive iodine,<br />
thyroidectomy<br />
Mild to moderate<br />
ophthalmopathy<br />
anti-thyroid drugs,<br />
radioactive iodine,<br />
thyroidectomy<br />
Moderate<br />
ophthalmopathy<br />
anti-thyroid drugs,<br />
radioactive iodine,<br />
thyroidectomy<br />
Moderate-to-severe<br />
ophthalmopathy,<br />
anti-thyroid drugs,<br />
radioactive iodine,<br />
thyroidectomy<br />
RT: radiation therapy; NO RT: no radiation therapy; GC: glucocorticoid; IV: intravenous; TSH: thyroid-stimulating hormone.<br />
Equipament<br />
Dose/angle/field<br />
Linear accelerator/<br />
20Gy/3 grade anterior/<br />
5 X 5 cm<br />
Linear accelerator/20Gy10<br />
degrees anterior/<br />
4 X 4 cm<br />
Linear accelerator/20Gy-10<br />
Gy/3 degrees anterior/<br />
5 X 6 cm<br />
Linear accelerator/20Gy-10<br />
Gy/10 degrees anterior/<br />
4 X 4 cm<br />
Cobalt -60/20Gy-10 Gy/10<br />
degrees anterior/<br />
4 X 4 cm<br />
Linear accelerator/20Gy-10<br />
Gy/10 degrees anterior/<br />
4 X 4 cm<br />
Linear accelerator or cobalt<br />
-60/20Gy-10 Gy/10 degrees<br />
anterior/<br />
5 X 5 cm<br />
Linear accelerator/20Gy-10<br />
Gy/10 degrees anterior/<br />
4 X 4 cm<br />
End point<br />
After 12 months, motility in<br />
degrees,<br />
proptosis, lid aperture,<br />
diplopia, quality life, cost<br />
After 12 months, motility in<br />
degrees,<br />
proptosis, lid aperture, optic<br />
neuropathy, diplopia<br />
After 12 months, lid aperture,<br />
proptosis, motility in degrees,<br />
diplopia, intraocular pressure<br />
After 12 months, motility<br />
in degrees,<br />
proptosis, lid aperture<br />
After 12 months,<br />
ophthalmic index,<br />
proptosis, optic neuropathy<br />
After 6 months, motility<br />
in degrees,<br />
proptosis, lid aperture,<br />
clinical activity scores<br />
After 6 months,<br />
eye score and a decrease in<br />
eye-muscle volume<br />
After 6 months,<br />
eyelid aperture, proptosis,<br />
eye movements, subjective<br />
eye score, and clinical-activity<br />
Table 2. <strong>Ocular</strong> parameters and results post treatment evaluated in randomized clinical trails<br />
Trial<br />
Prummel<br />
1993<br />
Marcocci*<br />
2000<br />
Bartalena<br />
1983<br />
Ng<br />
2005<br />
Kahaly<br />
2000<br />
Mourits<br />
2001<br />
Prummel<br />
2004<br />
Gorman<br />
2001<br />
Parameter<br />
Quality <strong>of</strong> life 0 0 0 0 0 0 = 0<br />
Proptosis (mm) = + 0 0 0 0 0 0<br />
Lid width (mm) 0 + 0 0 0 0 0 0<br />
Visual acuity 0 0 0 = = 0 0 0<br />
Diplopia 0 = 0 0 = + + =<br />
Intraocular pressure = = = 0 0 0 0 0<br />
Optic neuropathy 0 + + 0 0 0 0 0<br />
<strong>Ocular</strong> motility + + + + = + + =<br />
Clinical response = + + + = + + =<br />
Cost 0 0 0 0 0 0 = 0<br />
Side effects - - + = - + + +<br />
*= Marcocci trial + was used <strong>for</strong> RT 20 Gy plus iv glucocorticoid and 0 was used <strong>for</strong> RT 20 Gy plus oral glucocorticoid; += significant <strong>for</strong> radiotherapy 20 Gy arms with or without glucocorticoids<br />
when compared to the other treatment; -= significant <strong>for</strong> another treatment; (=)= no difference between the arms <strong>of</strong> study; 0= no evaluation.<br />
Arq Bras Oftalmol. 2012;75(5):324-32<br />
327
Radiation therapy <strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized controlled trials<br />
Table 3. Description <strong>of</strong> the design, aim, question, results and conclusion <strong>of</strong> the studies included in this meta-analysis<br />
Author Year<br />
Prummel et al.,<br />
2004<br />
Ng et al.,<br />
2005<br />
Prummel et al.,<br />
1993<br />
Marcocci et al.,<br />
2001<br />
Gorman et al.,<br />
2001<br />
Double-blind<br />
randomized trial<br />
Design /aim/<br />
study question Results Conclusions/comments<br />
To compared RT efficacy with sham<br />
irradiation in mild ophthalmopathy<br />
Double-blind<br />
randomized trial<br />
To assess the efficacy and safety<br />
<strong>of</strong> combined orbital irradiation<br />
and systemic steroids in the<br />
management <strong>of</strong> moderate-tosevere<br />
Graves’ ophthalmopathy<br />
Double-blind<br />
randomized trial<br />
Randomized trial<br />
To assess the efficacy and safety <strong>of</strong><br />
orbital radiotherapy combined with<br />
either oral (prednisone; starting<br />
dose, 100 mg/d; withdrawal after 5<br />
months) or iv (methylprednisolone;<br />
15 mg/kg <strong>for</strong> four cycles and then<br />
7.5mg/kg <strong>for</strong> four cycles; each<br />
cycle consisted <strong>of</strong> two infusions<br />
on alternate days at 2-wk intervals)<br />
glucocorticoids<br />
Prospective, randomized, internally<br />
controlled, double-blind clinical trial<br />
To evaluate the efficacy <strong>of</strong><br />
radiotherapy <strong>for</strong> GO<br />
RT was successful in 23 <strong>of</strong> 44 (52%) irradiated patients vs. 12 <strong>of</strong><br />
44 (27%) sham-irradiated patients at 12 months after treatment<br />
(relative risk, 1.9; 95% CI, 1.1 - 3.4; P =0.02). was effective in<br />
improving eye muscle motility and decreasing the severity <strong>of</strong><br />
diplopia. Quality <strong>of</strong> life improved similarly in both groups. In the<br />
radiotherapy group there was less need <strong>for</strong> follow-up treatment;<br />
66% vs. 84% <strong>of</strong> the patients needed further treatment (P=0.049)<br />
Total eye score improved earlier in the SRT group, achieving<br />
statistical significance (P
Viani GA, et al.<br />
OR: odds ratio.<br />
Figure 2. Treatment response comparing radiation therapy 20 Gy to other treatments in the randomized controlled trial.<br />
The overall odds ratio suggests that there is difference between RT<br />
20 Gy arms and no RT 20 Gy arms in terms <strong>of</strong> response to treatment<br />
rate with p value 0.003, as shown in table 4.<br />
Radiotherapy plus glucocorticoid versus glucocorticoid<br />
One randomized study (16) (15 patients) compared the efficacy <strong>of</strong><br />
combined orbital irradiation and systemic steroids in the management<br />
<strong>of</strong> moderate-to-severe Graves’ ophthalmopathy. The odds ratio<br />
<strong>for</strong> this trial was <strong>of</strong> 17.50 with a 95% confidence interval <strong>of</strong> 1.85 to<br />
250. The test <strong>for</strong> heterogeneity was not statistically significant with p<br />
value 0.42, which indicates that the pooling <strong>of</strong> the data was valid. The<br />
overall odds ratio suggests that there is difference between RT 20 Gy<br />
arms and glucocorticoid arms in terms <strong>of</strong> response to treatment rate<br />
with p value 0.04, as demonstrated in the table 4.<br />
Radiotherapy plus IV glucocorticoid versus radiotherapy plus<br />
oral glucocorticoid<br />
One study (14) (82 patients) compared the efficacy radiotherapy<br />
plus IV glucocorticoid versus radiotherapy plus oral glucocorticoid.<br />
The odds ratio <strong>of</strong> this study was 4.15 with 95% confidence interval<br />
<strong>of</strong> 1.34 to 12.87, suggesting that there is difference between<br />
radiotherapy plus IV glucocorticoid versus radiotherapy plus oral<br />
glucocorticoid in terms <strong>of</strong> response to treatment with p value 0.01,<br />
shown in table 4.<br />
Radiotherapy with 20 Gy versus other fractionations<br />
One study (12) (66 patients) compared the efficacy <strong>of</strong> radiotherapy<br />
with a total dose <strong>of</strong> 20 Gy versus others fractionations. The odds ratio<br />
<strong>of</strong> this study was 1.10 with 95% confidence interval <strong>of</strong> 0.39 to 3.10,<br />
suggesting that there is no difference between radiotherapy with a<br />
total dose <strong>of</strong> 20 Gy versus others fractionations <strong>for</strong> response to treatment,<br />
as demonstrated in table 4.<br />
Quality <strong>of</strong> life and costs<br />
One study <strong>of</strong> Prummel et al., (15) (88 patients) evaluated the quality<br />
<strong>of</strong> life and costs and did not evidence differences in quality <strong>of</strong> life<br />
or costs between patients submitted to radiotherapy versus sham<br />
radiotherapy <strong>for</strong> GO.<br />
Radiotherapy versus glucocorticoid<br />
One study (8) (56 patients) compared the efficacy <strong>of</strong> radiotherapy<br />
with a total dose <strong>of</strong> 20 Gy versus glucocorticoid. The odds ratio <strong>of</strong><br />
this study was 0.87 with 95% confidence interval <strong>of</strong> 0.30 to 2.87,<br />
suggesting that there is no difference between radiotherapy with a<br />
total dose <strong>of</strong> 20 Gy versus glucocorticoid <strong>for</strong> response to treatment,<br />
as described in table 4.<br />
Radiotherapy plus IV glucocorticoid versus radiotherapy alone<br />
One study (13) (30 patients) compared the efficacy <strong>of</strong> radiotherapy<br />
plus IV glucocorticoid versus radiotherapy alone. The odds ratio this<br />
study was 3 with 95% confidence interval <strong>of</strong> 0.68 to 13.31, suggesting<br />
that there is no difference between radiotherapy with a total dose <strong>of</strong><br />
20 Gy plus glucocorticoid versus radiotherapy alone <strong>for</strong> response to<br />
treatment, as shown in table 4.<br />
Quality <strong>of</strong> studies<br />
The median <strong>of</strong> the quality scores was <strong>of</strong> 4 points (in a 5-point<br />
scale), with none study scoring 0, 1, 2, or 3. There was complete agreement<br />
in scoring by the two assessors. The quality scores were high,<br />
five trials scored 5 points (8-10,15,16) and three trials scored 4 points in the<br />
Jada scale. This fact occurred because <strong>of</strong> the importance placed on<br />
blinding in the scoring system, and the inherent difficulty in blinding<br />
a treatment such as radiation, as shown in the table 3.<br />
Evaluation <strong>of</strong> publication Bias<br />
The funnel plot <strong>of</strong> the log ORs versus the inverse <strong>of</strong> their variances<br />
<strong>of</strong> the individual studies is displayed in figure 3. The plot <strong>for</strong>med a very<br />
distinct funnel shape with the log ORs evenly distributed around the<br />
meta-analysis OR regardless the study variance. There<strong>for</strong>e, there was<br />
no indication <strong>of</strong> an asymmetry in the study findings by the variance<br />
or size <strong>of</strong> the studies and, thus, little evidence <strong>for</strong> publication bias.<br />
DISCUSSION<br />
External radiotherapy has been used <strong>for</strong> GO <strong>for</strong> around 60 years<br />
and it still represents a mainstay in the management <strong>of</strong> the disease (23) .<br />
The rationale <strong>for</strong> the use <strong>of</strong> radiotherapy <strong>for</strong> GO resides both in its<br />
Arq Bras Oftalmol. 2012;75(5):324-32<br />
329
Radiation therapy <strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized controlled trials<br />
Table 4. Odds ratio calculated according to the response to treatment<br />
<strong>for</strong> the trials included in this meta-analysis<br />
Response to treatment (n=439)<br />
RT 20 Gy vs sham RT (n=190)<br />
Prummel et al., 2004 (15)<br />
Mourits et al., 2000 (9)<br />
Gorman et al., 2001 (10)<br />
RT 20 Gy plus glucocorticoid vs<br />
glucocorticoid (n=15)<br />
Ng et al., 2005 (16)<br />
RT 20 Gy IVGC vs RT ORGC * (n=82)<br />
Marcocci et al., 2001 (14)<br />
RT 20 Gy vs glucocorticoid (n=56)<br />
Prummel et al., 1993 (8)<br />
RT 20 Gy vs Low dose RT (n=66)<br />
Kahaly et al., 2000 (12)<br />
RT 20 Gy plus glucocorticoid vs<br />
RT 20 Gy (n=30)<br />
Marcocci et al., 1991 (13)<br />
Estimated OR (95% CI), p value<br />
3.15 (1.59 - 6.23), p=0.003<br />
2.92 (1.2 - 7.1)<br />
3.50 (1.2 - 10.2)<br />
1.00 (0.26 - 3.87)<br />
17.5 (1.22 - 250), p=0.04<br />
4.15 (1.34 - 12.87), p=0.01<br />
0.87 (0.30 - 2.47), p=0.79<br />
1.10 (0.39 - 3.10), p=0.86<br />
3.00 (0.68 - 13.31), p=0.15<br />
OR= odds ratio; CI= confidence interval; NR= not reported; RT= radiotherapy.<br />
*= iv methylprednisoloneacetate (IVGC) or oral prednisone (ORGC).<br />
SE: size effect; OR: odds ratio.<br />
Figure 3. Funnel plot <strong>for</strong> response to treatment using radiotherapy <strong>for</strong> Graves’ ophthalmopathy.<br />
nonspecific anti-inflammatory effect and in the high radio sensitivity<br />
<strong>of</strong> lymphocytes infiltrating the orbital space (24) . Lymphocytes are generally<br />
suppressed with relatively low doses <strong>of</strong> radiation, and the helper/suppressor<br />
T lymphocyte ratio is also altered by radiotherapy (23) .<br />
In addition, radiotherapy might also reduce glycosaminoglycans<br />
production by orbital fibroblasts (25) . Whether the reported effectiveness<br />
<strong>of</strong> orbital radiotherapy in GO is related either to its nonspecific<br />
anti-inflammatory action, or to specific immunosuppressive effects,<br />
both need to be clarified. Our review <strong>of</strong> papers published between<br />
1983 and 2006 showed that positive results were obtained using RT.<br />
According to most studies, orbital radiotherapy is especially effective<br />
on s<strong>of</strong>t tissue inflammatory changes and recent <strong>extraocular</strong> muscle<br />
involvement, producing improvement in the ocular parameters as<br />
visual acuity, diplopia, proptosis, lid width, ocular motility and optic<br />
neuropathy, but without any benefit on intraocular pressure. It<br />
should be mentioned that all studies were randomized, controlled<br />
and <strong>of</strong> high quality. The latest 5 years have witnessed important discussions<br />
on the role <strong>of</strong> orbital radiotherapy, in particular questioning<br />
its effectiveness and safety (26-32) .<br />
Most authors agree that orbital radiotherapy is a safe procedure.<br />
If the technique <strong>of</strong> radiation is correct, it seems not to increase the<br />
risk <strong>of</strong> cataract and retinopathy, except <strong>for</strong> patients with diabetic and<br />
hypertensive retinopathy (33,34) . The two latter conditions, especially<br />
if associated, should be considered as relative contraindications<br />
to orbital radiotherapy, in particular when signs <strong>of</strong> retinopathy are<br />
present be<strong>for</strong>e irradiation. It is worth noting that, even after a very<br />
long follow-up, orbital radiotherapy does not seem to bear a risk <strong>of</strong><br />
radiation-induced tumors (35-40) . Thus, the safety <strong>of</strong> orbital radiotherapy<br />
is not a major matter <strong>of</strong> argument, but there is a controversy about<br />
its real effectiveness. This debate has been revitalized by a randomized,<br />
placebo-controlled, double-blind study from the Mayo Clinic (10) .<br />
In the original experimental design <strong>of</strong> this study, only one orbit <strong>of</strong><br />
42 patients with moderately severe GO was irradiated, whereas the<br />
contralateral orbit served as an internal control. A detailed analysis <strong>of</strong><br />
objective measures was provided; leading the authors to conclude<br />
that orbital radiotherapy is ineffective and there<strong>for</strong>e, should not be<br />
<strong>of</strong>fered to GO patients (10) . Although Gorman et al. should be congratulated<br />
on the major ef<strong>for</strong>t they made, our point about this study is<br />
that it has some structural errors.<br />
One <strong>of</strong> them was the fact that a lot <strong>of</strong> patients had a longstan<br />
ding ophthalmopathy and had been already treated be<strong>for</strong>e,<br />
apparently not well succeeded, by systemic glucocorticoids (10) . The<br />
second one involves timing <strong>of</strong> therapy, and the therapeutic goals<br />
<strong>of</strong> orbital radiation therapy. The authors in their study included<br />
pa tients between 0.2 and 16 years, with a median <strong>of</strong> 1.3 years with<br />
onset from the eye symptoms. The authors made no attempt to<br />
treat patients in the active progressive phase <strong>of</strong> thyroid eye disease.<br />
This phase disease is characterized by infiltration <strong>of</strong> the extra-ocular<br />
<strong>muscles</strong> with lymphocytes, and it is the prime radiation sensitive<br />
period. Patients who do not respond to glucocorticoids are unlikely<br />
to show any benefit from orbital radiotherapy. In addition, the<br />
obser vation that the untreated orbit did not show any improvement<br />
or worsening during the 6-months period <strong>of</strong> further observation<br />
suggesting that enrolled patients had stable, non progressive,<br />
i.e. inactive (“burnt-out”) eye disease. The third vital error was the<br />
stated goal <strong>of</strong> orbital radiation. In many institutions the stated goal<br />
<strong>of</strong> therapy is to halt or reverse severe progressive thyroid ophthalmopathy.<br />
The author’s therapeutic objectives <strong>of</strong> treating patients<br />
who had chronic fibrotic thyroid ophthalmopathy established<br />
were unclear. This article seemed to evaluate if radiation therapy<br />
reversed such findings as orbital volume in patients with chronic<br />
thyroid ophthalmopathy. Our final concern about this article was<br />
the unusual port design <strong>for</strong> radiation therapy. This design may be<br />
useful as a research data, on the other hand, being human studies<br />
it can be considered as worrisome. Treating with their wedge pair<br />
field design to spare the contralateral eye, the authors increased the<br />
volume <strong>of</strong> normal tissue significantly, including the frontal lobes<br />
and parotid glands, exposed to radiation compared to the standard<br />
opposed lateral fields. Although the risks <strong>of</strong> a secondary malignancy<br />
in the treatment <strong>of</strong> those patients are slight, increasing the volume<br />
would be expected to increase this risk. But the long-term effects<br />
<strong>of</strong> a low dose radiation in a larger volume <strong>of</strong> the frontal lobe may<br />
have subtle effects in the higher brain functions.<br />
What did the other randomized controlled trials tell us about<br />
the efficacy <strong>of</strong> orbital radiotherapy <strong>for</strong> GO? In 1993, a randomized<br />
double-blind trial <strong>of</strong> prednisone vs. orbital radiotherapy in patients<br />
with moderately severe GO (8) demonstrated that the proportion <strong>of</strong><br />
responders in prednisone-treated (14 <strong>of</strong> 28, 50%) and irradiated (13 <strong>of</strong><br />
28, 46%) patients (18%) was similar. That time, there were no doubts<br />
that glucocorticoid was an effective treatment <strong>for</strong> GO. Ho wever, from<br />
this study through non direct comparison RT has star ted to be also<br />
considered effective. In addition, the study above also demonstrated<br />
a decrease in the eye muscle volume, as assessed by the eye muscle<br />
score (8) . In 2000 those data were confirmed <strong>for</strong> a double-blind ran-<br />
330 Arq Bras Oftalmol. 2012;75(5):324-32
Viani GA, et al.<br />
domized study which included 60 patients with moderately severe<br />
GO who were submitted to either orbital radiotherapy or sham-irradiation<br />
(9) . The qualitative treatment outcome was successful in 60%<br />
<strong>of</strong> irradiated patients and in only 31% <strong>of</strong> sham irradiated patients (9) .<br />
Improvement was mainly confined to eye movements; it should also<br />
be noted that 25% <strong>of</strong> irradiated patients were saved from additional<br />
strabismus surgery (9) . In 2004 a new important in<strong>for</strong>mation (15) about<br />
the use <strong>of</strong> orbital radiotherapy was provided <strong>for</strong> GO by Prummel et<br />
al. This double-blind, randomized clinical trial was the first to address<br />
the question <strong>of</strong> whether orbital radiotherapy has a place in the management<br />
<strong>of</strong> nonsevere GO. Based on the evaluation <strong>of</strong> changes in<br />
major and minor criteria prespecified, primary therapeutic outcome<br />
was successful in 52% <strong>of</strong> irradiated patients and in only 27% <strong>of</strong><br />
sham-ir radiated patients (15) , with improvement in the eye muscle<br />
function and diplopia. It should also be noted that the orbital radiotherapy<br />
was not associated with a greater improvement <strong>of</strong> quality <strong>of</strong><br />
life, compared to sham irradiation (15) . This paper also provides valuable<br />
in<strong>for</strong>mation that orbital radiotherapy did not prevent progression<br />
to more severe expressions in about 15% <strong>of</strong> the patients. The reason<br />
why the severe <strong>for</strong>ms <strong>of</strong> GO develop is still un clear nowadays, but it<br />
seems that environmental factors play a decisive role in this progression<br />
(40) . Thus, if the study by Prummel et al. (15) , lends further support<br />
to the concept that orbital radiotherapy is in general an effective<br />
treatment <strong>for</strong> GO, it also suggests that the commonly adopted policy<br />
<strong>of</strong> “wait-and-see” in cases <strong>of</strong> mild GO should be maintained, including<br />
the cost/benefit considerations. At present, most centers utilize linear<br />
accelerators delivering 4-6 megavolts and use a 4 x 4-cm lateral field<br />
slightly angled posteriorly to avoid as much as possible irradiation<br />
to the contralateral lens. The use <strong>of</strong> higher energy sources has not<br />
proven to be particularly advantageous. The most common delivered<br />
dose is 20 grays (Gy) per eye (30) ; this cumulative dose is usually<br />
fractionated in 10 daily doses over a 2-week period to reduce the<br />
cataractogenic effect <strong>of</strong> irradiation (27) . The importance <strong>of</strong> dose was<br />
evaluated by Kahaly et al., (12) , using different radiation doses. It reported<br />
that a therapeutic scheme <strong>of</strong> 1 Gy per week over a 20-week period<br />
was equally effective and possibly better tolerated than the classi cal<br />
2-week scheme. The use <strong>of</strong> higher cumulative doses <strong>of</strong> radiation<br />
(30 Gy vs. 20 Gy) does not produce any increase in the effectiveness<br />
<strong>of</strong> treatment (41) . Irrespective <strong>of</strong> small differences observed using<br />
low-dose vs. high-dose radiotherapy, beneficial effects <strong>of</strong> radiotherapy<br />
were observed in all the three groups <strong>of</strong> patients in 55 to 67% <strong>of</strong><br />
cases. In summary, what is the message to the reader, based on the<br />
present systematic review?<br />
CONCLUSION<br />
Our data has shown that orbital radiotherapy still has an impor -<br />
tant role in the management <strong>of</strong> GO. Although there are a lot <strong>of</strong><br />
avai lable studies in the literature, they have a limited impact owing<br />
to selection bias and lack <strong>of</strong> an appropriate ophthalmological assessment.<br />
In the era <strong>of</strong> evidence-based medicine it cannot be denied<br />
that six <strong>of</strong> eight randomized and controlled studies showed that orbital<br />
radiotherapy is effective on GO, especially on <strong>extraocular</strong> muscle<br />
involvement. Orbital radiotherapy, in burning out eye disease,<br />
can also make eye muscle and/or eyelid corrective surgery possible<br />
in earlier stages. The effectiveness <strong>of</strong> orbital radiotherapy can be increased<br />
by the synergistic interaction with glucocorticoids. Orbital<br />
radiotherapy should still be <strong>of</strong>fered as a valid therapeutic option to<br />
patients with moderate to severe GO. The selection <strong>of</strong> patients is<br />
fundamental, be cause patients with inactive (“burnt-out”) GO are<br />
unlikely to respond to irradiation (as well as to glucocorticoids).<br />
The use <strong>of</strong> orbital radiotherapy in the early stage <strong>of</strong> the disease<br />
(possibly less than 1 year from the onset) is recommended. The real<br />
efficacy <strong>of</strong> orbital radiotherapy should come from well-designed,<br />
multicenter, randomized and controlled studies enrolling a large<br />
number <strong>of</strong> patients.<br />
REFERENCES<br />
1. Brown J, Coburn JW, Wigod RA, Hiss JM Jr, Dowling JT. Adrenal steroid therapy <strong>of</strong><br />
severe infiltrative ophthalmopathy <strong>of</strong> Graves’ disease. Am J Med. 1963;34:786-95.<br />
2. Cortisone in exophthalmos: report on a therapeutic trial <strong>of</strong> cortisone and corticotrophin<br />
(ACTH) in exophthalmos and exophthalmic ophthalmoplegia by a panel<br />
appointed by the Medical Research Council. Lancet. 1955;268(6853):6-9.<br />
3. Bartalena L, Marcocci C, Bogazzi F, Panicucci M, Lepri A, Pinchera A. Use <strong>of</strong> corticosteroids<br />
to prevent progression <strong>of</strong> Graves’ ophthalmopathy after radioiodine therapy<br />
<strong>for</strong> hyperthyroidism. N Engl J Med. 1989;321(20):1349-52. Comment in: N Engl J Med.<br />
1989;321(20):1403-5; N Engl J Med. 1990;322(15):1088-9.<br />
4. Bartalena L, Marcocci C, Bogazzi F, Manetti L, Tanda M, Dell’Unto E, et al. Relation<br />
between therapy <strong>for</strong> hyperthyroidism and the course <strong>of</strong> Graves’ ophthalmopathy. N<br />
Engl J Med. 1998;338(2):73-8. Comment in: N Engl J Med. 1998;338(2):121-2; N Engl<br />
J Med. 1998;338(21):1546-7; ACP J Club. 1998;128(3):71.<br />
5. Trobe JD, Glaser JS, Laflamme P. Dysthyroid optic neuropathy. Clinical pr<strong>of</strong>ile and<br />
rationale <strong>for</strong> management. Arch Ophthalmol. 1978;96(7):1199-209.<br />
6. Marquez SD, Lum BL, McDougall IR, Katkuri S, Levin PS, MacManus M, et al. Long-term<br />
results <strong>of</strong> irradiation <strong>for</strong> patients with progressive Graves’ ophthalmopathy. Int J<br />
Radiat Oncol Biol Phys. 2001;51(3):766-74.<br />
7. Wakelkamp IM, Tan H, Saeed P, Schlingemann RO, Verbraak FD, Blank LE, et al. Orbital<br />
irradiation <strong>for</strong> Graves’ ophthalmopathy: Is it safe? A long-term follow-up study.<br />
Ophthalmology. 2004;111(8):1557-62.<br />
8. Prummel MF, Mourits MP, Blank L, Berghout A, Koornneef L, Wiersinga WM. Randomized<br />
double-blind trial <strong>of</strong> prednisone versus radiotherapy in Graves’ ophthalmopathy.<br />
Lancet. 1993;342(8877):949-54. Comment in: Lancet. 1993;342(8877):941.<br />
9. Mourits MP, van Kempen-Harteveld ML, Garcia MB, Koppeschaar HP, Tick L, Terwee CB.<br />
Radiotherapy <strong>for</strong> Graves’ orbitopathy: randomised placebo-controlled study. Lancet.<br />
2000;355(9214):1505-9.<br />
10. Gorman CA, Garrity JA, Fatourechi V, Bahn RS, Petersen IA, Staf<strong>for</strong>d SL, et al. A prospective,<br />
randomized, double-blind, placebo-controlled study <strong>of</strong> orbital radiotherapy<br />
<strong>for</strong> Graves’ ophthalmopathy. Ophthalmology. 2001;108(9):1523-34.<br />
11. Donaldson SS, Bagshaw MA, Kriss JP. Supervoltage orbital radiotherapy <strong>for</strong> Graves’<br />
ophthalmopathy. J Clin Endocrinol Metab. 1973;37(2):276-85.<br />
12. Kahaly GJ, Rosler H-P, Pitz S, Hommel G Low-versus highdose adiotherapy <strong>for</strong> Graves’<br />
ophthalmopathy: a randomized, single blind trial. J Clin Endocrinol Metab. 2000;<br />
85(1):102-8.<br />
13. Marcocci C, Bartalena L, Bogazzi F, Bruno-Bossio G, Lepri A, Pinchera A. Orbital radiotherapy<br />
combined with high dose systemic glucocorticoids <strong>for</strong> Graves’ ophthalmopathy<br />
is more effective than radiotherapy alone: results <strong>of</strong> a prospective randomized study. J<br />
Endocrinol Invest. 1991;14(10): 853-60.<br />
14. Marcocci C, Bartalena L, Tanda ML, Manetti L, Dell’Unto E, Rocchi R, et al. Comparison<br />
<strong>of</strong> the effectiveness and tolerability <strong>of</strong> intravenous or oral glucocorticoids associated<br />
with orbital radiotherapy in the management <strong>of</strong> severe Graves’ ophthalmopathy:<br />
results <strong>of</strong> a prospective, single-blind, randomized study. J Clin Endocrinol Metab.<br />
2001;86(8):3562-7.<br />
15. Prummel MF, Terwee CB, Gerding MN, Baldeschi L, Mourits MP, Blank L, et al. A randomized<br />
controlled trial <strong>of</strong> orbital radiotherapy versus sham irradiation in patients<br />
with mild Graves’ ophthalmopathy. J Clin Endocrinol Metab. 2004;89(1):15-20.<br />
16. Ng CM, Yuen HK, Choi KL, Chan MK, Yuen KT, Ng YW, et al. Combined orbital irradiation<br />
and systemic steroids compared with systemic steroids alone in the management <strong>of</strong><br />
moderate-to-severe Graves’ ophthalmopathy: a preliminary study. Hong Kong Med J.<br />
2005;11(5):322-30.<br />
17. Bartalena L, Marcocci C, Chiovato L, Laddaga M, Lepri G, Andreani D, et al. Orbital<br />
cobalt irradiation combined with systemic corticosteroid <strong>for</strong> Graves’ ophthalmopathy:<br />
comparison with systemic corticosteroids alone. J Clin Endocrinol Metab. 1983;<br />
56(6):1139-44.<br />
18. Ohtsuka K, Sato A, Kawaguchi S, Hashimoto M, Suzuki Y. Effect <strong>of</strong> steroid pulse therapy<br />
with and without radiotherapy on Graves’ ophthalmopathy. Am J Ophthalmol.<br />
2003;135(3):285-90.<br />
19. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality<br />
<strong>of</strong> reports <strong>of</strong> meta-analyses <strong>of</strong> randomised controlled trials: the QUOROM statement.<br />
Quality <strong>of</strong> Reporting <strong>of</strong> Meta-analyses. Lancet. 1999;354(9193):1896-900. Comment<br />
in: Lancet. 2005;366(9503):2081-2; author reply 2083-6; Lancet. 2000;355(9205):756-7;<br />
Lancet. 1999;354(9193):1834-5.<br />
20. Clarke M, Oxman AD, editors. Analysing and presenting results. Cochrane Reviewers<br />
Handbook, 4.1.6 [updated January 2003], Section 8. In The Cochrane Library. Ox<strong>for</strong>d:<br />
Update S<strong>of</strong>tware; 2003.<br />
21. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):<br />
177-88.<br />
22. Jadad AR, Moore RA, Carroll D. Assessing the quality <strong>of</strong> reports <strong>of</strong> randomized clinical<br />
trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12.<br />
23. Pinchera A, Bartalena L, Chiovato L, Marcocci C. Radiotherapy <strong>of</strong> Graves’ ophthalmopathy.<br />
In: Gorman CA, Waller RR, Dyer JA, editors. The eye and orbit in thyroid disease.<br />
New York: Raven Press; 1984. p.301-16.<br />
24. Bartalena L, Marcocci C, Manetti L, Tanda ML, Dell’Unto E, Rocchi R, et al. A Orbital<br />
radiotherapy <strong>for</strong> Graves’ ophthalmopathy. Thyroid. 1998;8(5):439-41.<br />
Arq Bras Oftalmol. 2012;75(5):324-32<br />
331
Radiation therapy <strong>for</strong> Graves’ ophthalmopathy: a systematic review and meta-analysis <strong>of</strong> randomized controlled trials<br />
25. Kahaly G, Beyer J. Immunosuppressant therapy <strong>of</strong> thyroid eye disease. Klin Wochenschr.<br />
1988;66(21):1049-59.<br />
26. Bartley GB, Gorman CA. The Mayo orbital radiotherapy <strong>for</strong> Graves’ ophthalmopathy<br />
(ORGO) study: lessons learned. Ophthal Plast Reconstr Surg. 2002;18(13):170-2.<br />
27. Kazim M. Radiotherapy <strong>for</strong> Graves orbitopathy: the Columbia University experience.<br />
Ophthal Plast Reconstr Surg. 2002;18(13):173-4.<br />
28. Wiersinga WM. Perspective. Part III. Retrobulbar irradiation in Graves orbitopathy: the<br />
Dutch experience. Ophthal Plast Reconstr Surg. 2002;18(13):175-6.<br />
29. Perros P, Krassas GE. Orbital irradiation <strong>for</strong> thyroid-associated orbitopathy: conventional<br />
dose, low dose or no dose? Clin Endocrinol (Oxf ). 2002;56(6):689-91.<br />
30. Cockerham KP, Kennerdell JS. Does radiotherapy have a role in the management <strong>of</strong><br />
thyroid orbitopathy? View 1. Br J Ophthalmol. 2002;86(1):102-4. Comment in: Br J<br />
Ophthalmol. 2002;86(1):106-7; Br J Ophthalmol. 2002;86(1):104-6.<br />
31. Mourits MP. Does radiotherapy have a role in the management <strong>of</strong> thyroid orbitopathy?<br />
View 2. Br J Ophthalmol. 2002;86(1):104-6. Comment In: Br J Ophthalmol. 2002;<br />
86(1):106-7. Comment on: Br J Ophthalmol. 2002;86(1):102-4.<br />
32. Bartalena L, Marcocci C, Gorman CA, Wiersinga WM, Pinchera A Orbital radiotherapy<br />
<strong>for</strong> Graves’ ophthalmopathy: useful or useless? Safe or dangerous? J Endocrinol<br />
Invest. 2003;26(1):5-18.<br />
33. Miller ML, Goldberg SH, Bullock JD. Radiation retinopathy after standard radiotherapy<br />
<strong>for</strong> thyroid-related ophthalmopathy. Am J Ophthalmol. 1991;112(5):600-1.<br />
34. Kinyoun JL, Kalina RE, Brower SA, Mills RP, Johnson RH. Radiation retinopathy after<br />
orbital irradiation <strong>for</strong> Graves’ ophthalmopathy. Arch Ophthalmol. 1984;102(10):<br />
1473-6.<br />
35. Marcocci C, Bartalena L, Rocchi R, Marino M, Menconi F, Morabito E, et al. A Long-term<br />
safety <strong>of</strong> orbital radiotherapy <strong>for</strong> Graves’ ophthalmopathy. J Clin Endocrinol Metab.<br />
2003;88(8):3561-6.<br />
36. Gorman CA, Garrity JA, Fatourechi V, Bahs RS, Petersen IA, Staf<strong>for</strong>d SL, et al. The aftermath<br />
<strong>of</strong> orbital radiotherapy <strong>for</strong> Graves’ ophthalmopathy. Ophthalmology. 2002;<br />
109(11):2100-7.<br />
37. Marquez SD, Lum BL, McDougall IR, Katkuri S, Levin PS, MacManus PS, et al. Long-term<br />
results <strong>of</strong> irradiation <strong>for</strong> patients with Graves’ ophthalmopathy. Int J Radiat Oncol Biol<br />
Phys. 2001;51(3):766-74.<br />
38. Schaefer U, Hesselmann S, Micke O, Schueller P, Bruns F, Palma C, et al. A long-term<br />
follow-up study after retro-orbital irradiation <strong>for</strong> Graves’ ophthalmopathy. Int J Radiat<br />
Oncol Biol Phys. 2002;52(1):192-7.<br />
39. Bartalena L. Orbital radiation therapy and Graves’ ophthalmopathy. Ophthalmology.<br />
2003;110(3):452-3.<br />
40. Marcocci C, Bartalena L, Bruno-Bossio G, Vanni G, Cartei F, Bogazzi F, et al. A Orbital<br />
radiotherapy in the treatment<strong>of</strong> endocrine ophthalmopathy: when and why? In:<br />
Kahaly G, editor. Endocrine ophthalmopathy: molecular, immunological and clinical<br />
aspects. Basel; Kager; 1993. p.131-41.<br />
41. Petersen IA, Kriss JP, McDougall IR, Donaldson SS. Prognostic factors in the radiotherapy<br />
if Graves’ ophthalmopathy. Int J Radiat Oncol Biol Phys. 1990;19(2):259-64.<br />
332 Arq Bras Oftalmol. 2012;75(5):324-32
Artigo Original | Original Article<br />
Cancelamento de cirurgias de catarata em um hospital público de referência<br />
Cancellation <strong>of</strong> cataract surgery in a public hospital<br />
Micheli Patrícia de Fátima Magri 1 , Rodrigo França de Espíndola 2 , Marcony Rodrigues de Santhiago 2 , Elisabeth Frolich Mercadante 3 , Newton Kara Júnior 2<br />
RESUMO<br />
Objetivo: Analisar a incidência e causas de cancelamento de cirurgias de catarata<br />
em um hospital público de referência.<br />
Métodos: Trata-se de um estudo retrospectivo em que <strong>for</strong>am analisados o número<br />
de cancelamentos de facectomias durante o ano de 2009. Foram analisados sexo,<br />
idade, tipo de procedimento suspenso (facoemulsificação ou extração extracapsular<br />
do cristalino), tipo de anestesia, convênio (Sistema Único de Saúde ou convênio/particular)<br />
e motivo de suspensão da cirurgia (causas clínicas, institucionais ou pessoais).<br />
Resultados: Foram agendadas no período 2.965 cirurgias de catarata, havendo 650<br />
cancelamentos (21,92%). Dentre as principais razões para a suspensão do procedimento<br />
destacaram-se as causas clínicas (86,90%). Os meses de inverno apresentaram<br />
os maiores índices de suspensão de cirurgias de catarata.<br />
Conclusão: A taxa de cancelamento de cirurgia de catarata em serviços públicos<br />
parece ser a mesma que há 10 anos. A principal causa de suspensão deve-se por<br />
condições clínicas (hipertensão, diabetes, falta de exames, etc.).<br />
Descritores: Catarata; Extração de catarata; Facoemulsificação; Cegueira/prevenção<br />
& controle; Hospitais públicos; Procedimentos cirúrgicos eletivos; Eficiência organizacional;<br />
Pacientes desistentes do tratamento<br />
ABSTRACT<br />
Purpose: To report the incidence and causes <strong>of</strong> cataract surgery cancellations in a public<br />
hospital.<br />
Methods: This is a retrospective study, which examined the number <strong>of</strong> cancellations<br />
<strong>of</strong> cataract surgery during 2009. We analyzed the type <strong>of</strong> procedure suspended (phacoemulsification<br />
or extracapsular extraction), type <strong>of</strong> anesthesia, gender, age, covenant<br />
(public/private) and the main reasons <strong>for</strong> suspension <strong>of</strong> the surgeries (clinical causes,<br />
institutional or personal).<br />
Results: We analyzed 2,965 scheduled cataract surgeries, with 650 cancellations (21.92%).<br />
The main reason <strong>for</strong> the suspension <strong>of</strong> the procedure was clinical causes (86.90%). The<br />
winter months had the highest suspension rates <strong>of</strong> cataract surgery.<br />
Conclusion: The cancellation rate <strong>of</strong> cataract surgery in Brazilian public system seems<br />
to be the same as 10 years ago. The main cause <strong>of</strong> the suspension should be in clinical<br />
conditions (hypertension, diabetes, lack <strong>of</strong> exams, etc.).<br />
Keywords: Cataract; Cataract extraction; Phacoemulsification; Blindness/prevention &<br />
control; Hospitals, public; Surgical procedures, elective; Efficiency, organizational; Patient<br />
dropouts<br />
INTRODUÇÃO<br />
A cirurgia da catarata apresenta alta eficiência, favorável custobenefício<br />
no tratamento e na reabilitação visual e <strong>of</strong>erece grande im -<br />
pacto para a sociedade (1-3) .<br />
Nos países em desenvolvimento, o acesso de pacientes necessitados<br />
à cirurgia de catarata é dificultado devido aos fatores so -<br />
cioe co nômicos e culturais, além de obstáculos criados pelo próprio<br />
sistema de saúde, o que impede a realização de mais procedimentos<br />
cirúrgicos (3-6) . Mesmo quando estes obstáculos são superados, algumas<br />
cirurgias de catarata são canceladas, ocasionando um impacto<br />
negativo para o paciente e para a comunidade, além de diminuir a<br />
eficiência do serviço prestado e gerar aumento dos custos (7) .<br />
O cancelamento de cirurgias gera insatisfação e prejuízo aos pa -<br />
cientes em condições clínicas favoráveis para a realização do procedimento<br />
(7) . A taxa de suspensão de cirurgias ambulatoriais varia mui to<br />
de hospital para hospital, dependendo do critério que a define e<br />
como os dados são coletados (8) .<br />
As cirurgias ambulatoriais são fundamentais para qualquer sis -<br />
tema de saúde. A baixa complexidade, a rápida recuperação pós-<br />
-operatória e a segurança do procedimento, fazem com que os<br />
pro cedimentos ambulatoriais estejam cada vez mais em evidência<br />
nas instituições de saúde. Para que isso ocorra é necessário que haja<br />
uma otimização na quantidade de cirurgias realizadas, o que só será<br />
possível se houver reconhecimento de seus benefícios e potencial<br />
econômico, pessoal e material (9) .<br />
Com o crescimento dos custos na área da saúde e as limitações<br />
orçamentárias, tornou-se necessária a adoção de um sistema que<br />
<strong>for</strong>neça in<strong>for</strong>mações capazes de evitar desperdícios, aprimorar os<br />
serviços e impulsionar a melhoria contínua do gerenciamento das<br />
ações (10) .<br />
A utilização máxima da capacidade cirúrgica, em muitos casos,<br />
constitui uma das principais medidas que visam à eficiência do uso<br />
de verbas em uma unidade hospitalar (11) . Uma das estratégias que<br />
podem ser adotadas como ação é a realização de um maior número<br />
de cirurgias, diminuindo o número de cancelamentos de procedimentos<br />
(12) .<br />
O Hospital Regional de Divinolândia (CONDERG) firma-se como<br />
referência regional do Sistema Único de Saúde (SUS) nas especialidades<br />
de <strong>of</strong>talmologia, otorrinolaringologia, ortopedia e cirurgia geral,<br />
além da reabilitação neurológica, sendo referência para 16 cidades<br />
na região de São João da Boa Vista (SP), interior do Estado de São<br />
Paulo. Uma população de aproximadamente 480 mil habitantes são<br />
assistidas pelo CONDERG sendo 97% do atendimento realizado pelo<br />
SUS e o restante por convênios/particular.<br />
Submetido para publicação: 12 de abril de 2012<br />
Aceito para publicação: 28 de agosto de 2012<br />
Trabalho realizado no CONDERG - Hospital Regional de Divinolândia - UNICAMP - em conjunto com<br />
o Hospital das Clínicas da Universidade de São Paulo - HC-FMUSP - e a Faculdade de Medicina<br />
do ABC - FM-ABC.<br />
1<br />
Mestre em Gerontologia. Pontifícia Universidade Católica de São Paulo, São Paulo (SP), Brasil.<br />
2<br />
Médico, Departamento de Oftalmologia, Universidade de São Paulo - USP - São Paulo (SP), Brasil.<br />
3<br />
Pr<strong>of</strong>essor, Pontifícia Universidade Católica de São Paulo - PUCSP - São Paulo (SP), Brasil.<br />
Financiamento: Não houve financiamento para este trabalho.<br />
Divulgação de potenciais conflitos de interesse: M.P.F.Magri, Nenhum; R.F.Espíndola, Nenhum;<br />
M.R.Santhiago, Nenhum; E.F.Mercadante, Nenhum; N.Kara.Júnior, Nenhum.<br />
Endereço para correspondência: Rodrigo França de Espíndola, Praça das Hortências, 70 - Cond.<br />
Portal de Itu - Itu (SP) 13301-689 - Brasil - E-mail: rodrigoespindola@usp.br<br />
Arq Bras Oftalmol. 2012;75(5):333-6<br />
333
Cancelamento de cirurgias de catarata em um hospital público de referência<br />
O objetivo deste estudo é analisar a incidência e as principais<br />
causas de cancelamento de cirurgias de catarata em um hospital referência<br />
do SUS que podem ter contribuído para diminuir a eficiência<br />
do sistema de saúde.<br />
MÉTODOS<br />
Trata-se de um estudo retrospectivo na qual foi avaliado o número<br />
de suspensões de facectomia do centro cirúrgico ambulatorial<br />
de <strong>of</strong>talmologia. Foram incluídos no estudo todos os pacientes com<br />
cirurgias agendadas e canceladas em 2009, de acordo com dados<br />
obtidos em arquivos e prontuários do Hospital Regional de Divinolândia.<br />
A pesquisa foi aprovada pelo Comitê de Ética e Pesquisa<br />
de Enfermagem e Medicina do CONDERG.<br />
A região assistida pelo CONDERG (16 municípios) apresenta uma<br />
população de idosos (>60 anos) de 51.799 pessoas, o que representa<br />
um percentil de 12,70%. Destes 3,70% possuem de 60 a 64 anos,<br />
3.20% de 65 a 69 anos, 2,70% de 70 a 74 anos e 3,10% possuem 75<br />
anos ou mais (Fonte: IBGE, Senso 2000).<br />
Os seguintes dados <strong>for</strong>am coletados nos arquivos do centro cirúrgico:<br />
tipo de procedimento (facoemulsificação [FACO] ou facectomia<br />
extracapsular [FEC]), tipo de anestesia (local, sedação ou geral), sexo,<br />
idade, convênio (SUS ou convênio/particular) e causas de suspensão<br />
da cirurgia.<br />
As cirurgias suspensas <strong>for</strong>am divididas con<strong>for</strong>me demonstrado<br />
abaixo:<br />
A. Causas clínicas: hipertensão arterial, tosse ou resfriado, falta de<br />
exames solicitados na consulta pré-operatória, más condições<br />
clínicas, hipoglicemia ou hiperglicemia - relaciona-se com as<br />
con dições de atendimento nos municípios de origem, devido ao<br />
paciente não comparecer com a(s) doença(s) de base controladas;<br />
B. Causas institucionais: falta de condições da unidade hospitalar<br />
de saúde: material, pessoal, estrutural, falta de horário - relaciona-se<br />
com as condições de atendimento do hospital, que por<br />
alguma justificativa não apresentou as condições necessárias<br />
para a realização do procedimento cirúrgico;<br />
C. Causas pessoais: ingestão de anticoagulante, desistência, falta ou<br />
recusa - relaciona-se com as condições de saúde de cada indivíduo.<br />
Ao final da primeira fase de coleta de dados foi realizado o cálculo<br />
dos indicadores e a análise dos mesmos acima mencionados. Para<br />
tanto, foi utilizado a metodologia descrita no Manual de indicadores<br />
de enfermagem do Controle de Qualidade Hospitalar CQH (2006).<br />
Os dados <strong>for</strong>am tabulados e analisados em três partes: tabulação<br />
dos dados, elaboração de indicadores de qualidade e análise dos<br />
indicadores. Foram analisados os seguintes indicadores:<br />
- Taxa de suspensão de cirurgia<br />
A taxa de suspensão de cirurgias foi calculada através da razão<br />
entre a quantidade de cirurgias suspensas e o total de cirurgias<br />
agendadas em cada mês, sendo o resultado multiplicado por<br />
100 e expresso em números relativos.<br />
- Taxa de aproveitamento das cirurgias<br />
A taxa de aproveitamento das cirurgias foi calculada através da<br />
razão entre a quantidade de cirurgias realizadas e agendadas em<br />
cada mês, sendo o resultado multiplicado por 100 e expresso em<br />
porcentual.<br />
A equipe multidisciplinar do centro cirúrgico incluí 1 enfermeira,<br />
22 técnicos em enfermagem, 4 instrumentadoras, 4 auxiliares de<br />
serviços, 2 anestesistas e equipe médica de residentes, preceptores e<br />
contratados. A grade cirúrgica é pré-definida com um agendamento<br />
de cirurgias eletivas realizadas nas 12 horas disponíveis no centro cirúrgico,<br />
de segunda a sexta-feira, ou através de mutirões que ocorrem<br />
em alguns finais de semana.<br />
A amostragem baseou-se em todos os casos de cancelamento<br />
de cirurgias de catarata durante o ano de 2009. Os dados <strong>for</strong>am analisados<br />
descritivamente e tabulados usando o auxílio do programa<br />
Micros<strong>of</strong>t Excel (versão 2010).<br />
RESULTADOS<br />
Foram agendadas no período analisado 2.965 cirurgias de catarata,<br />
havendo 650 cancelamentos (21,92%). A tabela 1 demonstra<br />
o número de agendamentos, cirurgias realizadas e cancelamentos<br />
durante o período analisado. Todas as cirurgias <strong>for</strong>am financiadas<br />
pelo SUS.<br />
Com relação ao sexo e idade, dos 650 cancelamentos, 353 eram<br />
do sexo feminino (54,30%) e 25,00% encontrava-se na faixa de 60 - 64<br />
anos de idade com uma média de 63 ± 1,21 anos e 297 eram do sexo<br />
masculino (45,70%) e 30,00% encontrava-se na faixa de 60 - 64 anos<br />
de idade com uma média de 64 ± 1,43 anos.<br />
Dos cancelamentos, 640 seriam por FACO (98,40%) e 10 seriam<br />
por FEC (1,60%). Considerando o tipo de anestesia programada,<br />
a grande maioria dos cancelamentos foi com anestesia local (646<br />
pacientes [99,40%]) seguidos por sedação (2 pacientes [0,30%]) e<br />
anestesia geral (2 pacientes [0,30%]).<br />
Analisando-se as causas de cancelamentos de cirurgia de catarata,<br />
a grande maioria foi devido a causas clínicas (86,90%) como<br />
demonstrado na tabela 2. A Tabela 3 mostra a distribuição das causas<br />
de suspensão de facectomias.<br />
O gráfico 1 demonstra as taxas de cancelamento e aproveitamento<br />
de cirurgias durante o ano de 2009. Verifica-se que a taxa<br />
Tabela 1. Distribuição do número de cancelamentos, agendamentos e de cirurgias de catarata realizadas no centro cirúrgico ambulatorial durante 2009<br />
2009 Jan Fev Mar Abr Mai Jun Jul Ago Set Out Nov Dez Total Média<br />
Cancelamentos 044 054 063 037 055 063 071 064 048 064 050 037 0.650 054.10<br />
Agendamentos 202 205 235 241 248 278 276 278 278 296 239 180 2.956 246.30<br />
Cirurgias realizadas 158 151 172 204 193 215 205 214 230 232 189 143 2.306 192.10<br />
Tabela 2. Número de cancelamentos de cirurgias de catarata de acordo com causas clínicas, institucionais e pessoais durante 2009<br />
Causas Jan Fev Mar Abr Mai Jun Jul Ago Set Out Nov Dez Total %<br />
Clínicas 39 45 55 33 52 51 69 62 39 57 35 27 564 86.90<br />
Institucionais 01 02 00 01 01 05 01 01 00 01 10 02 025 003.80<br />
Pessoais 04 07 08 03 02 07 01 01 09 06 05 08 061 009.30<br />
Total 44 54 63 37 55 63 71 64 48 64 50 37 650 100.00<br />
334 Arq Bras Oftalmol. 2012;75(5):333-6
Magri MPF, et al.<br />
Tabela 3. Causas gerais de cancelamento de cirurgia de catarata durante<br />
o ano de 2009<br />
Causas de cancelamento N %<br />
Hipertensão arterial* 369 56,70<br />
Falta de exames 113 17,30<br />
Tosse/resfriado 40 6,10<br />
Más condições clínicas 33 5,07<br />
Hipo/hiperglicemia 29 4,46<br />
Tomou AAS** 21 3,23<br />
Remarcado para cirurgião R4 (com mais experiência) 11 1,60<br />
Recusa do paciente 9 1,38<br />
Faltou tempo 7 1,07<br />
Contra indicado pelo anestesista 4 0,60<br />
Não identificado 4 0,60<br />
Falta de jejum 4 0,60<br />
Falta de médico 3 0,46<br />
Indicação questionada pelo cirurgião 3 0,46<br />
Total 650 100,00<br />
*= pressão arterial ≥ 140 X 90 mmHg; **= acido acetil-salicílico.<br />
Gráfico 1. Distribuição das taxas de cancelamento e de aproveitamento das cirurgias<br />
de catarata durante o ano de 2009.<br />
de aproveitamento cirúrgico variou de 73,20% a 84,70%, com uma<br />
média de 78,95% segundo o agendamento. Através dos indicadores<br />
de suspensões de facectomias, podemos observar que houveram<br />
variações entre 15,30% a 26,30%, com uma média de 20,80%.<br />
DISCUSSÃO<br />
O estudo nacional mais recente que avaliou causas de cancelamento<br />
de cirurgia de catarata no Brasil aconteceu há mais de 10<br />
anos. Lira et al., (11) detectaram uma taxa de suspensão de facectomia<br />
de 19,50%. Arieta et al., (13) em 1992, detectaram 22.80% de cancelamento.<br />
No presente estudo a taxa de cancelamento no ano de 2009<br />
foi de 21,92%, semelhante aos levantamentos anteriores. Nota-se que<br />
esses valores encontram-se praticamente inalterados ao longo dos<br />
anos, apesar dos es<strong>for</strong>ços no sentido de otimizar os centros cirúrgicos<br />
ambulatoriais.<br />
Estudos em outros países mostram taxas de cancelamento muito<br />
inferiores aos do Brasil, variando entre 5 - 12% (14,15) . As principais causas<br />
citadas nestes estudos também <strong>for</strong>am clínicas, como por exemplo<br />
hipertensão arterial, diabetes e resfriado. Alguns autores revelam que<br />
até 80% das causas de cancelamento seriam preveníveis (14) .<br />
Causas relacionadas à condição clínica do paciente (causas pessoais)<br />
levaram à suspensão de 4,50% das cirurgias no último estudo<br />
nacional (11) . Isso demonstra que esse mesmo índice encontrado no<br />
presente estudo (9,30%), demonstrado na tabela 2, está acima dos<br />
encontrados na literatura e que os clientes estão chegando de seus<br />
municípios com nível pressórico muito alto e/ou com falta de exames<br />
laboratoriais solicitados para a realização da cirurgia de catarata.<br />
O resultado da cirurgia e a recuperação da visão traz benefícios<br />
econômicos e sociais para o indivíduo, sua família e comunidade<br />
se gundo os estudos anteriores (13,16) . Desta maneira, todas as partes<br />
envolvidas com o impacto que a baixa visão por catarata acarreta são<br />
beneficiadas quando a saúde ocular é restabelecida.<br />
Para tanto, é necessário conhecer a instituição e o serviço, levantar<br />
dados e analisar os indicadores de qualidade. Elevadas taxas de<br />
cancelamentos refletem diretamente no atendimento prestado à<br />
comunidade. Para melhorarmos a taxa de aproveitamento do centro<br />
cirúrgico ambulatorial (diminuição do número de cancelamentos)<br />
algumas medidas <strong>for</strong>am tomadas:<br />
1. Os dados seriam apresentados ao Departamento Regional de<br />
Saúde de São João da Boa Vista (DRS XIV), um dos 17 departamentos<br />
do Estado de São Paulo, juntamente com os municípios<br />
participantes para propor ações em conjunto e diminuir<br />
estes índices;<br />
2. Criação de um protocolo estabelecendo os parâmetros de<br />
suspensão em relação aos exames pedidos como por exemplo,<br />
glicemia acima de 200 mg/dl, pressão arterial acima de 150 X<br />
90 mmHg e etc.;<br />
3. Criar um espaço para orientações pré-operatória para retirar as<br />
dúvidas e explicar as cirurgias;<br />
4. Realizar uma triagem através da equipe de enfermagem para<br />
re<strong>for</strong>çar as orientações pré-operatórias e verificar os exames<br />
antes do dia agendado para a cirurgia;<br />
5. Priorização do atendimento aos idosos que já tiveram a sua<br />
cirurgia suspensa por algum motivo;<br />
6. Monitorar os indicadores de suspensão de cirurgia mensalmente.<br />
Desta maneira toda a equipe do CONDERG, os municípios e os<br />
clientes estarão interligados com medidas que tentam eliminar as<br />
principais causas de suspensão de cirurgia.<br />
Os meses de abril e dezembro apresentaram menor número de<br />
suspensões, e o mês de julho obteve a maior expressão de suspensão.<br />
Diferentemente, o agendamento possuí o menor índice em dezembro<br />
e o maior em outubro (Tabela 1). Tais dados podem representar<br />
expressivamente os períodos sazonais na qual julho é o mês com um<br />
período mais frio, elevando a pressão arterial, proporcionando assim<br />
os maiores índices de suspensão cirúrgica, o que está de acordo<br />
com a literatura (11) . Em dezembro, com diminuição da produtividade<br />
devido ao período de festividade, houve menos agendamento de<br />
cirurgias.<br />
CONCLUSÃO<br />
A taxa de cancelamento de cirurgia de catarata em serviços<br />
públicos parece ser a mesma que há 10 anos. A principal causa de<br />
suspensão deve-se por condições clínicas (hipertensão, diabetes,<br />
falta de exames, etc.). Não somente o hospital de referência (local da<br />
cirurgia), mas o município de origem dos pacientes devem interagir<br />
para diminuir o número de cancelamentos e assemelhar-se aos padrões<br />
internacionais.<br />
REFERÊNCIAS<br />
1. Batterbury M, Khaw PT, Hands R, Elkington AR. The cataract explosion: the changing<br />
pattern <strong>of</strong> diagnoses <strong>of</strong> patients attending an ophthalmic outpatient department.<br />
Eye (Lond). 1991;5(Pt 3):369-72.<br />
2. Kara-José N, Arieta CE, Temporini ER, Kang KM, Ambrosio LE. Tratamento cirúrgico de<br />
catarata senil: óbices para o paciente. Arq Bras Oftalmol. 1996;59(6):573-7.<br />
Arq Bras Oftalmol. 2012;75(5):333-6<br />
335
Cancelamento de cirurgias de catarata em um hospital público de referência<br />
3. Kara-José N, Temporini ER. Cataract surgery: or why are there some patients excluded.<br />
Rev Panam Salud Publica. 1999;6(4):242-8.<br />
4. Schwab L. Public health, preventive care, and eye care delivery and evaluation. In:<br />
Schwab L, editor. Eye care in developing nations. 3rd ed. San Francisco: The Foundation<br />
<strong>of</strong> the American Academy <strong>of</strong> Ophthalmology; 1999. p.3-17.<br />
5. Rehder JR, Ribeiro LG, Melo Filho PA, Aoki RH. «Projeto Catarata»: uma solução para<br />
saúde pública ocular. Rev Bras Oftalmol. 1990;58(4):271-5.<br />
6. Temporini ER, Kara-José N, Kara-José Jr N. Catarata senil: características e percepções<br />
de pacientes atendidos em projeto comunitário de reabilitação visual. Arq Bras<br />
Oftalmol. 1997;60(1):79-83.<br />
7. Vieira MJ, Furegat AR. Suspensão de cirurgias: atitudes e representações dos enfermeiros.<br />
Rev Esc Enferm USP. 2001:35(2):135-40.<br />
8. Fischer SP. Cost-effective preoperative evaluation and testing. Chest. 1999;115(5 Suppl):<br />
96S-100S.<br />
9. Kara-Junior N, Espindola RF. Evolução e viabilização de um centro cirúrgico ambulatorial<br />
para cirurgias de catarata em larga escala em um hospital universitário. Arq<br />
Bras Oftalmol. 2010;73(6):494-6.<br />
10. Guedes RM. Situando a qualidade na prática médica [Monografia]. Belo Horizonte:;<br />
Universidade Gama Filho; 2005.<br />
11. Lira RP, Nascimento MA, Temporini ER, Kara-José N, Arieta CE. Reasons <strong>of</strong> cataract<br />
surgery cancellation. Rev Saude Publica. 2001;35(5); 487-9.<br />
12. Kara-José N, Delgado AM, Arieta CEL. Exequibilidade da cirurgia de catarata em hospitalescola:<br />
em busca de um modelo econômico. Rev Assoc Med Bras. 1992; 40(3);186-8.<br />
13. Arieta CE, Taiar A, Kara-José N. Utilização e causas de suspensão de intervenções<br />
cirúrgicas oculares em centro cirúrgico ambulatorial universitário. Rev Assoc Med Bras.<br />
1995;41(3):233-5.<br />
14. Bamashmus M, Haider T, Al-Kershy R. Why is cataract surgery canceled? A retrospective<br />
evaluation. Eur J Ophthalmol. 2010;20(1):101-5.<br />
15. Henderson BA, Naveiras M, Butler N, Hertzmark E, Ferrufino-Ponce Z. Incidence and<br />
causes <strong>of</strong> ocular surgery cancellations in an ambulatory surgical center. J Cataract<br />
Refract Surg. 2006;32(1):95-102.<br />
16. Kara-Junior N, Santhiago MR, Parede TR, Espindola RF, Mazurek MG, Germano R, et<br />
al. Influência da correção cirúrgica da catarata na percepção laborativa. Arq Bras<br />
Oftalmol. 2010;73(6):491-3.<br />
XVII Congresso da<br />
Sociedade Brasileira de Uveítes<br />
14 a 16 de março de 2013<br />
In<strong>for</strong>mações:<br />
E-mail: wiltonfeitosa@hotmail.com<br />
336 Arq Bras Oftalmol. 2012;75(5):333-6
Artigo Original | Original Article<br />
Implantação do exame do reflexo vermelho em crianças da região do<br />
Hospital das Clínicas da Faculdade de Medicina de Botucatu - SP - Brasil<br />
Implementation <strong>of</strong> red reflex exam in children in the area <strong>of</strong> Botucatu Medical School Clinical Hospital -<br />
São Paulo, Brazil<br />
Antonio Carlos Lottelli Rodrigues 1 , Rodrigo Bueno Prado 1 , Licério Miguel 2<br />
RESUMO<br />
Objetivo: Descrever a implantação do teste de reflexo vermelho nas 30 cidades<br />
de inserção do Hospital das Clínicas da Faculdade de Medicina de Botucatu,<br />
HC/FMB/UNESP (480.337 habitantes), a criação de um centro para referência<br />
de crianças com reflexo vermelho alterado ou duvidoso, a Triagem do reflexo<br />
vermelho e outro para o tratamento da catarata infantil, o Centro de tratamento<br />
da catarata infantil.<br />
Métodos: O exame do reflexo vermelho foi divulgado em 30 cidades da região de<br />
Botucatu. Foram realizadas palestras aos municípios, convocados pelo Departamento<br />
Regional de Saúde VI do estado de São Paulo (DRS VI). Foram distribuídos 109 “pen<br />
torch ophthalmoscope”, às maternidades e Unidades Básicas de Saúde (UBSs) das<br />
cidades. A Triagem do reflexo vermelho recebeu os casos de reflexo vermelho alterado<br />
ou duvidoso e estabeleceu o diagnóstico <strong>of</strong>talmológico. O Centro de tratamento da<br />
catarata infantil realizou o exame pré-operatório, o tratamento cirúrgico e o acompanhamento<br />
das crianças com catarata.<br />
Resultados: Após um ano de funcionamento a Triagem do reflexo vermelho<br />
aten deu 29 crianças, 17 do sexo masculino e 12 do feminino, com idade média e<br />
desvio padrão (dp) de 10,09 ± 20,35 meses (7 dias - 98 meses). 16 pacientes <strong>for</strong>am<br />
encaminhados com reflexo vermelho alterado, idade média e dp de 13,17 ± 24,14<br />
meses (7 dias - 98 meses), a alteração foi confirmada em todos os casos, 13 deles<br />
apresentavam catarata. Em 13 encaminhamentos com reflexo duvidoso, idade mé -<br />
dia e dp de 6,29 ± 14,46 meses (7 dias - 98 meses), a alteração não se confirmou. A<br />
incidência de alterações do reflexo vermelho encontradas foi de 9,2/10.000 nascidos<br />
vivos e a incidência the catarata foi de 7,9/10.000 nascidos vivos.<br />
Conclusão: Descrevemos a implantação do Teste do reflexo vermelho na Região de<br />
Botucatu, a criação da Triagem do reflexo vermelho e do Centro de tratamento da<br />
catarata infantil e dificuldades encontradas.<br />
Descritores: Catarata/diagnóstico; Catarata/congênita; Oftalmoscópios; Reflexo<br />
pupilar; Vision tests; Criança<br />
ABSTRACT<br />
Purpose: To describe the implantation <strong>of</strong> the red reflex test in 30 cities in the area <strong>of</strong><br />
Botucatu Medical School Clinical Hospital, (480,337 inhabitants) and the creation <strong>of</strong> a<br />
reference Center <strong>for</strong> children with red reflex changes, the Red reflex screening and another<br />
Center <strong>for</strong> treatment <strong>of</strong> childhood cataract.<br />
Methods: The red reflex exam was released in 30 cities <strong>of</strong> the surrounding Botucatu<br />
area, lectures were done in the cities invited to participate by the Regional Department<br />
<strong>of</strong> Health.109 pen torch ophthalmoscopes were distributed to the hospital maternities<br />
and primary care units. The Red reflex screening attended cases <strong>of</strong> altered or doubtful<br />
red reflex and established the diagnosis. The Center <strong>for</strong> treatment <strong>of</strong> childhood cataract<br />
per<strong>for</strong>med the preoperative examination, surgical treatment and follow-up <strong>of</strong> children<br />
with cataracts.<br />
Results: After one year the Red reflex screening attended 29 children, 17 males and<br />
12 females, mean age and pattern deviation (PD) <strong>of</strong> 10.09 ± 20.35 months (7 days - 98<br />
months old). 16 patients were referred with altered red reflex, with a mean age and<br />
pattern deviation <strong>of</strong> 13.17 ± 24.14 months (7 days - 98 months old). The alteration was<br />
confirmed in all <strong>of</strong> these cases. 13 children had cataract. In 13 children with doubtful<br />
exam, with a mean age and PD <strong>of</strong> 6.29 ± 14.46 months (7 days - 54 months old), the<br />
alteration was not confirmed in any <strong>of</strong> these patients. The incidence <strong>of</strong> negative red<br />
reflex found among newborns was 9.2/10,000 and the incidence cataracts in this<br />
same group was 7.9/10,000.<br />
Conclusion: We described the implantation <strong>of</strong> the red reflex exam in the Botucatu area,<br />
and the creation <strong>of</strong> a reference Center <strong>for</strong> eye examination <strong>of</strong> children with changes in<br />
the red reflex, and the creation <strong>of</strong> a reference Center <strong>for</strong> treatment <strong>of</strong> childhood cataract<br />
and difficulties.<br />
Keywords: Cataract/diagnosis; Cataract/congenital; Ophthalmoscopes; Reflex, pupillary;<br />
Child<br />
INTRODUÇÃO<br />
Algumas das importantes afecções oculares que ocorrem no re -<br />
cém-nascido e na criança como a catarata, o retinoblastoma e outras<br />
alterações da córnea ou do polo posterior, podem ser detectadas<br />
usando um teste prático, conhecido como exame do reflexo vermelho<br />
ou teste do reflexo de Bruckner. O exame consiste na visualização<br />
da pupila da criança, usando <strong>of</strong>talmoscópio direto, colocado há cerca<br />
de um braço de distância (1) .<br />
Para ser considerado normal, o examinador deve ver através da<br />
pupila dos dois olhos um reflexo vermelho e simétrico. Qualquer<br />
alteração no reflexo vermelho como manchas escuras, ausência ou<br />
assimetria de reflexo, ou presença de reflexo branco (leucocoria) são<br />
motivos para se suspeitar de doenças oculares, devendo a criança ser<br />
referida para exame especializado com um <strong>of</strong>talmologista (1) .<br />
Tradicionalmente o <strong>of</strong>talmoscópio é usado para o exame do<br />
reflexo vermelho. No entanto, o uso de modelos simplificados como<br />
Submetido para publicação: 28 de março de 2012<br />
Aceito para publicação: 9 de agosto 2012<br />
Trabalho realizado no Departamento de Oftalmologia, Otorrinolaringologia e Cirurgia de Cabeça e<br />
Pescoço - Uni versidade Estadual Paulista “Júlio de Mesquita Filho” - Faculdade de Medicina de<br />
Botucatu, Botucatu (SP), Brasil.<br />
1<br />
Médico, Departamento de Oftalmologia, Otorrinolaringologia e Cirurgia de Cabeça e Pescoço, Fa -<br />
culdade de Medicina de Botucatu, Botucatu (SP), Brasil.<br />
2<br />
Acadêmico de Medicina, Faculdade de Medicina de Botucatu, Botucatu (SP), Brasil.<br />
Financiamento: Fundação de Auxílio à Pesquisa do Estado de São Paulo FAPESP, Secretaria de<br />
Saúde do Estado de São Paulo, Ministério da Saúde, Conselho Nacional de Desenvolvimento<br />
Científico e Tecnológico (CNPQ) (Programa de Pesquisa para o SUS - PPSUS).<br />
Divulgação de potenciais conflitos de interesse: A.C.L.Rodrigues, Nenhum; R.B.Prado, Nenhum;<br />
L.Miguel, Nenhum.<br />
Endereço de correspondências: Antonio Carlos Lottelli Rodrigues. Departamento de Oftalmologia,<br />
Otorrinolaringologia e Cirurgia de Cabeça e Pescoço, UNESP - Distrito de Rubião Jr - Botucatu -<br />
SP - 18618-970 - Brasil - E-mail: eye_acr@fmb.unesp.br<br />
Projeto número 2363/2007, aprovado pelo comitê de ética e pesquisa da Faculdade de Medicina<br />
de Botucatu.<br />
Arq Bras Oftalmol. 2012;75(5):337-40<br />
337
Implantação do exame do reflexo vermelho em crianças da região do Hospital das Clínicas<br />
da Faculdade de Medicina de Botucatu - SP - Brasil<br />
o “pen torch ophthalmoscope” (PTO) (Apramed Indústria e Comércio<br />
de Aparelhos Médicos Ltda.) podem representar uma alternativa<br />
barata e possibilitam o uso por pr<strong>of</strong>issionais de saúde não médicos<br />
treinados na detecção de anormalidades do reflexo vermelho (2) .<br />
A causa mais frequente de alteração do reflexo vermelho na in -<br />
fância é a catarata infantil, doença tratável que apresenta resultado<br />
visual favorável desde que diagnosticada e tratada precocemente (3) .<br />
A catarata infantil é aquela presente ao nascimento (congênita)<br />
ou que se desenvolve até os 12 anos de idade (4) . Sua prevalência<br />
é muito variável sendo de 1 a 4/10.000 nascidos em países desenvolvidos<br />
e 5 a 15/10.000 nascidos em países em desenvolvimento.<br />
A relação inversa entre prevalência e índice de desenvolvimento é<br />
resultado da melhor assistência pré-natal e melhor prognóstico visual<br />
sempre que o diagnóstico e o tratamento adequados são realizados<br />
precocemente. A catarata é responsável por 14% das crianças cegas<br />
do mundo (5) .<br />
No Brasil, as estatísticas são insuficientes e nos últimos anos, por<br />
<strong>for</strong>ça de leis o exame do reflexo vermelho começa a ser realizado nas<br />
maternidades brasileiras. A primeira lei que obriga o teste do reflexo<br />
vermelho na maternidade foi aprovada em 5 de setembro de 2002 no<br />
estado do Rio de Janeiro, desde então várias cidades e estados vêm<br />
criando leis municipais e estaduais obrigando a realização do exame.<br />
No estado de São Paulo, somente em 2007 a Lei Estadual n o 12.551 de<br />
5 de março, tornou obrigatório o exame nas maternidades do estado.<br />
Além da importância de se pesquisar o reflexo vermelho nas ma -<br />
ternidades, sua pesquisa é preconizada pela American Academy <strong>of</strong><br />
Pe diatrics nas consultas pediátricas de rotina com um, dois, quatro,<br />
seis e nove meses, um, dois, três, quatro, cinco, seis, oito, 10 e 12 anos (6) .<br />
O Hospital de Clínicas da Faculdade de Medicina de Botucatu -<br />
UNESP é referência para 30 municípios (480.337 habitantes) na região<br />
centro-oeste do estado de São Paulo. Existiam obstáculos fundamentais<br />
para que o exame fosse realizado e para que o diagnóstico precoce<br />
trouxesse efetivamente benefício às crianças. Muitas maternidades<br />
não dispunham de <strong>of</strong>talmoscópio, os pr<strong>of</strong>issionais envolvidos não<br />
haviam sido capacitados para realização técnica e interpretação do<br />
exame e o serviço de referência dos pacientes não estava estruturado.<br />
Diante do exposto, justificou-se a necessidade da criação de um<br />
projeto com ações que viabilizassem: a concretização do teste do<br />
reflexo-vermelho, a criação de um serviço de referência para exame<br />
<strong>of</strong>talmológico e o tratamento da catarata infantil. O objetivo deste<br />
artigo é descrever: a implementação do teste do reflexo vermelho<br />
nas 30 cidades de inserção do Hospital das Clínicas da Faculdade de<br />
medicina de Botucatu, HC/FMB/UNESP (480.337 habitantes), a criação<br />
de um Centro para referência de crianças com reflexo vermelho<br />
alterado ou duvidoso, a Triagem do reflexo vermelho (TRV) e outro<br />
para o tratamento da catarata infantil, o Centro de tratamento da catarata<br />
infantil (CTCI), as dificuldades encontradas e resultados obtidos<br />
após um ano de funcionamento.<br />
agentes pertencentes aos “Programas de Saúde da Família” (PSF).<br />
Após a palestra realizamos treinamento prático utilizando o PTO. A<br />
palestra e o treinamento prático <strong>for</strong>am repetidos por mais duas vezes<br />
no município de Botucatu, para as cidades que não responderam à<br />
primeira convocação.<br />
Nas palestras <strong>for</strong>am entregues 109 PTO para cada uma das 17 maternidades<br />
e 92 unidades básicas de saúde dos municípios presentes<br />
(Figura 1). Estes instrumentos <strong>for</strong>am montadas ao custo de R$ 200,00,<br />
valor três vezes menor que o de um <strong>of</strong>talmoscópio direto simples<br />
(valores de janeiro de 2008).<br />
Orientamos o encaminhamento dos casos detectados com re fle xo<br />
alterado ou duvidoso a um serviço de triagem criado para receber estas<br />
crianças no HC/FMB/UNESP, a TRV. Esta triagem passou a atender<br />
a partir de julho de 2008, em um dia fixo da semana. Desde então,<br />
toda criança que comparece com diagnóstico de reflexo alterado ou<br />
duvidoso é atendida, sem necessidade de agendamento prévio. As<br />
crianças atendidas no primeiro ano de funcionamento da triagem<br />
<strong>for</strong>am divididas por idade, sexo, motivo do encaminhamento (reflexo<br />
alterado ou duvidoso), se a alteração foi confirmada ou não e o<br />
diagnóstico.<br />
Foi criado um centro especializado no tratamento da catarata<br />
infantil o CTCI composto por ambulatório próprio e centro cirúrgico<br />
especializado. As crianças com catarata infantil triadas pela Triagem<br />
do reflexo vermelho <strong>for</strong>am avaliadas pelo CTCI e divididas em relação<br />
à idade, sexo, lateralidade e necessidade de tratamento clínico ou<br />
cirúrgico. As crianças submetidas à cirurgia <strong>for</strong>am examinadas, sob<br />
anestesia geral, com medida da pressão intraocular (PIO) utilizando<br />
tonômetro de Perkins, ceratometria média utilizando ceratômetro<br />
portátil (Retinomax K plus 2, Righton) e comprimento axial utilizando<br />
biômetro de contato (Microscan Model 100A + , Sonomed).<br />
RESULTADOS<br />
Das 30 cidades convocadas para as reuniões, uma delas, com<br />
1.741 habitantes (0,36% da população da região), não compareceu<br />
para ouvir a palestra, receber o treinamento e o PTO embora tenha<br />
sido reconvocada pela DRS VI por mais duas vezes. Em um ano de funcionamento<br />
a TRV atendeu 29 crianças, 17 do sexo masculino e 12 do<br />
sexo feminino, com idade média e desvio padrão (dp) de 10,09 ± 20,35<br />
meses (7 dias - 96 meses), destas 17 (58,6%) tinham idade igual ou<br />
menor que 3 meses, 16 pacientes <strong>for</strong>am encaminhados com refle xo<br />
vermelho alterado, com idade média e dp de 13,17 ± 24,14 meses (7<br />
MÉTODO<br />
Em parceria com o Departamento Regional de Saúde VI (DRS VI)<br />
do estado de São Paulo, regional em que se insere o HC/FMB/UNESP,<br />
divulgamos o teste do reflexo vermelho através de uma matéria<br />
publicada em jornal regional, duas entrevistas em rádios regionais e<br />
uma entrevista televisiva também regional. Foram confeccionados<br />
e distribuídos pela DRS VI 5.000 folhetos explicativos à população e<br />
aos pr<strong>of</strong>issionais de saúde. Esses folhetos <strong>for</strong>am distribuídos pelos<br />
postos de saúde das cidades. As cidades <strong>for</strong>am divididas em quatro<br />
grupos de acordo com a localidade, para cada grupo foi ministrada<br />
uma palestra abordando a importância da realização do exame e<br />
quais doenças poderiam ser detectadas, com uma breve explicação<br />
sobre cada uma delas. Foi enfatizada a importância de se realizar o<br />
exame não só nas maternidades, mas em toda consulta pediátrica (1) .<br />
Também foi orientado e estimulado a realização do exame com o<br />
PTO por outros pr<strong>of</strong>issionais de saúde não médicos, principalmente<br />
Figura 1. Esquema ilustrativo do funcionamento de um “pen torch ophthalmoscope”<br />
(PTO), à esquerda e foto do aparelho distribuído.<br />
338 Arq Bras Oftalmol. 2012;75(5):337-40
Rodrigues ACL, et al.<br />
dias - 96 meses) e 13 com reflexo duvidoso, com idade média e dp de<br />
6,29 ± 14,46 meses (7 dias - 54 meses). A alteração foi confirmada nos<br />
16 pacientes encaminhadas com reflexo alterado e não se confirmou<br />
em nenhum paciente encaminhado com reflexo duvidoso. Dos 16<br />
pacientes com reflexo alterado uma menina de 4 meses apresentava<br />
leucoma corneano no olho direito, um menino de 28 meses apresentava<br />
descolamento de retina no olho esquerdo e outro de 96<br />
meses apresentava catarata traumática também no olho esquerdo,<br />
13 crianças (81,25%) apresentavam catarata congênita/juvenil, sendo<br />
destas, 6 com catarata bilateral e 7 com catarata unilateral.<br />
Para o cálculo da incidência considerou-se que as crianças com<br />
alterações detectadas nas maternidades deveriam chegar ao serviço<br />
pelo menos até os 3 meses de idade e que o número de nascidos<br />
vivos na região neste período ficou em torno de 7.600 segundo o “Datasus”<br />
do ministério da saúde, considerou-se também que recebemos<br />
sete pacientes com reflexo alterado nesta faixa etária, assim teremos<br />
uma incidência de exame do reflexo vermelho alterado, detectado na<br />
maternidade, de 9,2/10.000 nascidos vivos. Desses, 6 tinham catarata<br />
(7,9/10.000 nascidos vivos) sendo 4 com catarata bilateral (5,3/10.000<br />
nascidos vivos).<br />
A média e dp de idade dos pacientes com catarata congênita/<br />
ju venil foi de 6,50 ± 6,97 meses (0,3 - 22,26 meses), dos pacientes<br />
com catarata congênita/juvenil bilateral foi de 7,74 ± 7,13 meses (1,4<br />
meses - 18,8 meses) e unilaterais 6,37 ± 7,57 meses (0,3 - 22,26 meses).<br />
A média e dp do comprimento axial dos olhos com catarata foi de<br />
18,97 ± 1,94 milímetros (17,20 - 23,12 mm), e a média e dp da ceratometria<br />
média foi de 46,93 ± 3,26 dioptrias (43,00 - 52,75 D) (Gráfico 1).<br />
A média e dp da PIO nestes olhos foi de 9,63 ± 1,89 milímetros de<br />
mercúrio (7 - 12 mmHg).<br />
DISCUSSÃO<br />
O desinteresse de algumas secretarias municipais de saúde é<br />
desestimulante, no entanto a maioria é bastante interessada e<br />
atuan te. O público que compareceu às palestras era composto em<br />
sua maioria por enfermeiros, auxiliares de enfermagem e agentes de<br />
saúde do “Pro grama de Saúde da Família” (PSF), e poucos pediatras.<br />
Este fato inicialmente nos frustrou, no entanto, percebemos que o<br />
esclarecimento das pessoas envolvidas, mesmo que não médicas,<br />
geram cobranças, fazendo com que médicos busquem in<strong>for</strong>mações<br />
sobre o assunto.<br />
Grande parte das crianças encaminhadas (41,37%), tanto como<br />
suspeitas como com reflexo alterado não eram recém-nascidos que<br />
tiveram exame alterado ou duvidoso realizado na maternidade.<br />
Estes encaminhamentos provavelmente decorreram da ação de<br />
pr<strong>of</strong>issionais não médicos e não de pediatras nos atendimentos<br />
Gráfico 1. Gráfico de dispersão dos valores de comprimento axial e ceratometria<br />
média de olhos com catarata infantil em relação à idade e linha de tendência em<br />
es cala logarítmica.<br />
am bulatoriais, pois a frequência destes pr<strong>of</strong>issionais nas palestras foi<br />
pequena e sabemos das dificuldades em mudar hábitos de pr<strong>of</strong>issionais<br />
médicos, principalmente acrescentando “trabalho extra” e não<br />
obrigatório, aos atendimentos ambulatoriais do serviço público. Em<br />
relação ao encaminhamento de recém-nascidos, acreditamos que<br />
tenha sido sim pela ação dos pediatras nas maternidades, obrigados<br />
a realizar o exame por <strong>for</strong>ça da lei n o 12.551 do Estado de São Paulo.<br />
O grande número de pacientes encaminhados com reflexo duvidoso<br />
provavelmente se deveu a dúvidas e dificuldades encontradas<br />
por pr<strong>of</strong>issionais iniciantes na prática do exame. Estas dúvidas e dificuldades<br />
são ainda maiores em crianças recém-nascidas o que pode<br />
ser uma das justificativas para que a média de idade das crianças<br />
encaminhadas com reflexo duvidoso fosse menor que as encaminhadas<br />
com reflexo alterado. Outro fator que pode ter influenciado neste<br />
dado é a obrigatoriedade da realização do exame na maternidade.<br />
Isto é apenas uma tendência já que não encontramos diferença<br />
es tatística entre os dois grupos (p=0,181; teste de Mann-Whitney).<br />
Infelizmente em nosso estudo não pesquisamos em detalhes a<br />
origem dos exames que geraram os encaminhamentos, nem quantos<br />
<strong>for</strong>am feitos por pr<strong>of</strong>issionais médicos ou não médicos.<br />
Não encontramos dados na literatura quanto à incidência de reflexo<br />
vermelho alterado em recém-nascidos, na verdade eles se confundem<br />
com dados de incidência de catarata devido a sua grande<br />
frequência. Em relação à incidência de catarata, no que consideramos<br />
como recém-nascido, foi quase duas vezes maior (7,9/10.000 nascidos<br />
vivos) do que esperávamos para uma região considerada de -<br />
senvol vida e bem assistida em relação à saúde, comparada a média<br />
brasileira e ficando dentro da faixa de países em desenvolvimento (5) .<br />
Te mos que considerar ainda que provavelmente nem todas as crian ças<br />
nascidas <strong>for</strong>am examinadas e que crianças detectadas com reflexo<br />
alterado podem não ter chegado serviço. Não criamos mecanismos<br />
de controle para garantir isto, no entanto estes dados podem servir<br />
de parâmetro para estudos futuros, pois a literatura, principalmente<br />
brasileira é muito pobre em relação a eles. Estas incidências, que consideramos<br />
alta, por outro lado mostra indiretamente o cumprimento<br />
de nossos objetivos de viabilizar o teste do reflexo vermelho na região<br />
e centralizar o encaminhamento destas crianças.<br />
A catarata foi a principal causa de alteração do reflexo vermelho,<br />
corroborando com a literatura (7) . O gráfico da distribuição dos valores<br />
de comprimento axial e média ceratométrica destes pacientes em<br />
relação à idade, possuem linha de tendência logarítmico como era de<br />
se esperar (7-8) .<br />
No Brasil o uso do <strong>of</strong>talmoscópio é competência médica. No entanto,<br />
o exame do reflexo vermelho é um exame tecnicamente fácil<br />
e que pode ser realizado por paramédicos treinados, como acontece<br />
em outros países (2) . Pr<strong>of</strong>issionais não médicos treinados utilizando o<br />
PTO podem auxiliar no diagnóstico de alterações no reflexo vermelho<br />
que se manifestem após o nascimento. Os agentes de saúde dos<br />
PSFs também poderiam exercer um importante papel neste sentido.<br />
Além disso os PTO distribuídos não são <strong>of</strong>talmoscópios, portanto não<br />
existe nenhuma restrição legal ao seu uso.<br />
A Organização Mundial de Saúde (OMS) propõe o “Vision 2020 -<br />
The Right to Sight”, uma iniciativa global para eliminação da cegueira<br />
prevenível até o ano de 2020 (9) . A criação de uma lei federal que<br />
torna obrigatório o exame do reflexo vermelho nas maternidades<br />
brasileiras contribuiria para prevenção da cegueira infantil em nosso<br />
país. Precisamos sim concentrar es<strong>for</strong>ços neste sentido, no entanto<br />
não podemos nos esquecer que as doenças que levam a alterações<br />
do reflexo vermelho podem estar presentes ao nascimento ou se<br />
manifestar posteriormente (10) . Devemos criar nos pediatras o hábito<br />
de examinar os olhos e realizar o exame do reflexo vermelho em toda<br />
consulta de rotina (6) , assim como examina o ouvido e a garganta.<br />
Isso não é ensinado em nossas escolas médicas. O exame do reflexo<br />
vermelho na maternidade é necessário, mas não suficiente.<br />
A TRV continua recebendo crianças com reflexo vermelho alterado<br />
e duvidoso, assim como o CTCI a tratar a catarata infantil, estes<br />
Arq Bras Oftalmol. 2012;75(5):337-40<br />
339
Implantação do exame do reflexo vermelho em crianças da região do Hospital das Clínicas<br />
da Faculdade de Medicina de Botucatu - SP - Brasil<br />
serviços estão se <strong>for</strong>talecendo, aumentaram sua área de abrangência<br />
para toda DRS IV e já começam a receber crianças das DRSs vizinhas. A<br />
criação e <strong>for</strong>talecimento desses centros são de extrema importância<br />
para organização do serviço público de saúde, servindo de base para<br />
a criação de redes de encaminhamento.<br />
CONCLUSÃO<br />
Descrevemos o processo para implementação do projeto que viabilizou<br />
a realização do teste do reflexo vermelho na região de Botucatu.<br />
A sua implementação permitiu a triagem de cerca de 7.600 crianças<br />
tendo sido recebidas 29 para avaliação em Centro de referência<br />
sendo 16 crianças portadoras de doenças oculares e destas, 13 por -<br />
tadoras de catarata congênita/juvenil.<br />
O estudo também mostra que o “Pen torch ophthalmoscope” (PTO)<br />
pode ser uma ferramenta importante na disseminação do exame do<br />
reflexo vermelho e combate da cegueira na infância.<br />
REFERÊNCIAS<br />
1. Red reflex examination in infants. Section on Ophthalmology. American Academy <strong>of</strong><br />
Pediatrics. Pediatrics. 2002;109(5):980-1.<br />
2. Pon JA, Bevin TH, Herbison P, Taylor BJ, Sanderson G. A novel instrument <strong>for</strong> assessing<br />
the retinal red reflex <strong>for</strong> non-ophthalmic health pr<strong>of</strong>essionals. Clin Exp Optom. 2005;<br />
88(3):160-4.<br />
3. Meier P, Sterker I, Tegetmeyer H. [Leucocoria in childhood]. Klin Monbl Augenheilkd.<br />
2006;223(6):521-7. German.<br />
4. Robinson GC, Jan JE, Kinnis C. Congenital ocular blindness in children, 1945 to 1984.<br />
Am J Dis Child. 1987;141(12):1321-4.<br />
5. Foster A, Gilbert C. Cataract in children. Acta Paediatr. 2003;92(12):1376-8. Comment<br />
on: Acta Paediatr. 2003;92(12):1468-73.<br />
6. Recommendations <strong>for</strong> preventive pediatric health care. Committee on Practice and<br />
Ambulatory Medicine. Pediatrics. 1995;96(2 Pt 1):373-4<br />
7. Trivedi RH, Wilson ME. Biometry data from caucasian and african-american cataractous<br />
pediatric eyes. Invest Ophthalmol Vis Sci. 2007;48(10):4671-8.<br />
8. Trivedi RH, Wilson ME. Keratometry in pediatric eyes with cataract. Arch Ophthalmol.<br />
2008;126(1):38-42.<br />
9. VISION 2020: the right to sight. Global initiative <strong>for</strong> the elimination <strong>of</strong> avoidable<br />
blindness [Internet]. Geneva: World Health Organization; revised February 2000.<br />
Fact Sheet 213. [cited 2011 Jan 24]. Available from: https://apps.who.int/inf-fs/en/<br />
fact213.html<br />
10. Committee on Practice and Ambulatory Medicine and Section on Ophthalmology;<br />
American Association <strong>of</strong> Certified Orthoptists; American Association <strong>for</strong> Pediatric<br />
Ophthalmology and Strabismus; American Academy <strong>of</strong> Ophthalmology. Eye examination<br />
in infants, children, and young adults by pediatricians. Pediatrics. 2003;<br />
111(4 Pt 1): 902-7.<br />
XI Congresso Sul-Brasileiro de Oftalmologia<br />
XVII Simpósio de Atualização em Oftalmologia<br />
22 e 23 de março de 2013<br />
Majestic Palace Hotel<br />
Florianópolis (SC)<br />
In<strong>for</strong>mações:<br />
Site: www.<strong>of</strong>talmosul.com.br/2013<br />
340 Arq Bras Oftalmol. 2012;75(5):337-40
Artigo Original | Original Article<br />
Prevalence and causes <strong>of</strong> blindness in an urban area <strong>of</strong> Paraguay<br />
Prevalência e causas de cegueira em uma população urbana do Paraguai<br />
Fernando Yaacov-Peña 1 , David Jure 1 , José Ocampos 1 , Margarita Samudio 2 , João Marcello Furtado 3 , Marissa Carter 4 , Van Charles Lansingh 5<br />
ABSTRACT<br />
Purpose: To determine the prevalence and causes <strong>of</strong> blindness in Piribebuy, Paraguay.<br />
Methods: A population based study was conducted from September to November<br />
2007 in Piribebuy, Paraguay. Based on the city map, seven clusters were randomly<br />
selected, containing 22 to 36 squares (423 to 578 houses) each, where all subjects<br />
≥ 40 years old who agreed to participate were included in the study. Presenting<br />
vision acuity (VA) was obtained <strong>for</strong> each eye, with ‘E’ Snellen charts 6 meters far from<br />
the patient with appropriate light. Eyes with VA ≤20/60 were also tested with the<br />
pinhole. Objective and subjective refraction was per<strong>for</strong>med, followed by examination<br />
<strong>of</strong> anterior segment under the slit-lamp, Goldmann applanation tonometry,<br />
and pupil dilatation with 0.5% tropicamide plus 0.5% phenylephrine, followed by<br />
evaluation <strong>of</strong> the posterior pole. Best corrected visual acuity was used to classify the<br />
patients as follows: blindness was defined as visual acuity <strong>of</strong> the better eye
Prevalence and causes <strong>of</strong> blindness in an urban area <strong>of</strong> Paraguay<br />
The aim <strong>of</strong> the present study is to determine the prevalence and<br />
causes <strong>of</strong> blindness and low vision in Piribebuy, Paraguay, and compare<br />
the findings with available data in the literature.<br />
Methods<br />
The Piribebuy Eye Study is a population-based study per<strong>for</strong>med<br />
in Piribebuy, Paraguay, from September to November 2007, to determine<br />
the prevalence and causes <strong>of</strong> blindness in the area. Piribebuy<br />
is a small town located 72 km east from Asunción. Data from the<br />
last national census described a total <strong>of</strong> 22,807 inhabitants, 2,626 <strong>of</strong><br />
them being 40 years old or above. Demographic and socioeconomic<br />
characteristics from Piribebuy are representative from the entire Cordillera<br />
Department. Also, the distribution <strong>of</strong> the age groups is similar<br />
to the rest <strong>of</strong> the country (7,8) .<br />
To calculate the sample size, based on a previous publication (6)<br />
we estimated a prevalence <strong>of</strong> blindness ranging from 2 to 3.2% in<br />
individuals aged 40 or older, which results in a sample <strong>of</strong> 436 subjects<br />
(95% CI) through the use <strong>of</strong> the Epi Info 2000 s<strong>of</strong>tware.<br />
Based on the Piribebuy city map, seven clusters were randomly<br />
selected, containing 22 to 36 squares (423 to 578 houses) each<br />
(Table 1).<br />
All individuals aged 40+ years old living in these squares were<br />
notified prior to eye exam. The aim <strong>of</strong> the study and the examination<br />
procedure were explained to the subjects, and those who gave verbal<br />
consent were examined.<br />
Eye examination was per<strong>for</strong>med by three third-year residents<br />
in ophthalmology from Fundación Visión, under the supervision <strong>of</strong><br />
an experienced ophthalmologist. In a local ophthalmological clinic,<br />
presented vision acuity (VA) was obtained <strong>for</strong> each eye, with ‘E’<br />
Snellen charts 6 meters far from the patient with appropriate light.<br />
Objective and subjective refraction was per<strong>for</strong>med and also best<br />
corrected visual acuity (BCVA) was obtained, followed by examination<br />
<strong>of</strong> anterior segment under the slit-lamp, Goldmann applanation<br />
tonometry, pupil dilatation with 0.5% tropicamide plus 0.5% phenylephrine<br />
and evaluation <strong>of</strong> the posterior pole with a 90D lens and<br />
with indirect ophthalmoscope and 20D lens. Patients who could not<br />
attend the ophthalmological appointment were submitted to visual<br />
acuity (VA) measurement, refraction, eye examination with a portable<br />
slit-lamp and indirect ophthalmoscope with a 20D lens in their<br />
houses. Best corrected VA was used to classify the patients as follows:<br />
blindness was defined as VA <strong>of</strong> the better eye
Yaacov-Peña F, et al.<br />
recorded if they contributed equally to visual loss, and this likely<br />
biased the findings toward cataract. Patients having dense cataracts<br />
could also have some pathology in the posterior pole such as glaucoma<br />
or diabetic retinopathy that could not be assessed. Also, a<br />
healthier lifestyle (e.g.: eating habits) could also contribute <strong>for</strong> these<br />
findings.<br />
The ProyectoVer, per<strong>for</strong>med with Hispanics living in Arizona, USA,<br />
also found cataract was the main cause <strong>of</strong> visual impairment (best<br />
corrected vision in the better eye worse than 20/40), (12) but the lead<br />
cause <strong>of</strong> blindness (best corrected vision in the better eye ≤20/200)<br />
was glaucoma, while in the present study no blind subjects due to<br />
this disease were found.<br />
Surveys using the rapid assessment <strong>of</strong> avoidable blindness (RAAB)<br />
or the rapid assessment <strong>of</strong> cataract surgical services (RACSS) methodology<br />
examines subjects ≥50 years old, (10,13) while the Los Angeles<br />
Latino Eye Study (LALES) (14) and the Proyecto Ver (12) examined individuals<br />
aged 40 or above. In the present study, only one subject (0.7%)<br />
aged
Artigo Original | Original Article<br />
An outbreak <strong>of</strong> <strong>for</strong>ty five cases <strong>of</strong> Pseudomonas aeruginosa acute endophthalmitis<br />
after phacoemulsification<br />
Surto de quarenta e cinco casos de end<strong>of</strong>talmite aguda por Pseudomonas aeruginosa após facoemulsificação<br />
Ricardo Luz Leitão Guerra 1 , Bruno de Paula Freitas 2 , Cintia Maria Felix Medrado Parcero 2 , Otacílio de Oliveira Maia Júnior 1 , Roberto Lorens Marback 3<br />
ABSTRACT<br />
Purpose: To describe an outbreak <strong>of</strong> Pseudomonas aeruginosa endophthalmitis<br />
post cataract surgery. Clinical findings, treatment and outcome are discussed.<br />
Methods: Clinical charts review <strong>of</strong> <strong>for</strong>ty-five patients treated <strong>for</strong> endophthalmi tis<br />
in a two-day period. The patients underwent primary vitrectomy, anterior chamber<br />
irrigation and intravitreous antibiotic injection. Cultures from vitreous and anterior<br />
chamber samples were per<strong>for</strong>med in all patients.<br />
Results: Forty-five patients (twenty-three men and twenty-two women) were identified.<br />
The average age was 71.2 years (range, 56-83 years). The right eye (62%) was<br />
affected more <strong>of</strong>ten than the left eye (38%). The median interval between surgery<br />
and endophthalmitis onset was 5.5 days (range, 5-6 days). The visual acuity at the<br />
diagnosis was better than 20/40 in one patient (2%), from 20/40 to 20/200 in one<br />
patient (2%), from 20/400 to counting fingers in two patients (4%), hand movements<br />
in eleven patients (24%), and light perception in thirty patients (68%). Pseudomonas<br />
aeruginosa was the isolated agent in twenty-six vitreous samples and in three<br />
anterior chamber samples. Overall, one patient (2%) achieved a final visual acuity<br />
better than 20/40; eight patients (18%) achieved a final visual acuity from 20/40 to<br />
20/200; six patients (13%) achieved a final visual acuity from 20/400 to counting<br />
fingers; eleven patients (25%) achieved a final acuity <strong>of</strong> hand movements; thirteen<br />
patients (29%) achieved a final acuity <strong>of</strong> light perception and six (13%) patients<br />
had no light perception at the last examination. None <strong>of</strong> these eyes underwent<br />
evisceration or enucleation in a three-month follow-up period.<br />
Conclusion: Even with all the safety that cataract surgery has achieved, today,<br />
en dophthalmitis remains a risk and a fearful complication <strong>of</strong> this procedure. In the<br />
present study, it was impossible to identify the source <strong>of</strong> the outbreak.<br />
Keywords: Phacoemulsification/adverse effects; Endophthalmitis/etiology; Pseu -<br />
domonas aeruginosa; Vitrectomy; Pseudomonas, infections; Equipment conta -<br />
mination<br />
RESUMO<br />
Objetivo: Descrever surto de end<strong>of</strong>talmite por Pseudomonas aeruginosa após fa -<br />
cectomia. Os achados clínicos, o tratamento e o resultado são discutidos.<br />
Métodos: Revisão dos prontuários de quarenta e cinco pacientes tratados para end<strong>of</strong>talmite<br />
em um período de dois dias. Todos os pacientes <strong>for</strong>am tratados por vitrectomia<br />
primária, irrigação da câmara anterior e injeção vítrea de antibióticos. Culturas do<br />
vítreo e de amostras de câmara anterior <strong>for</strong>am realizadas em todos os pacientes.<br />
Resultados: Quarenta e cinco pacientes (23 homens e 22 mulheres) <strong>for</strong>am identificados.<br />
A idade média foi 71,2 anos (variação, 56-83 anos). O olho direito (62%) foi mais<br />
afetado do que o esquerdo (38%). O intervalo médio entre a cirurgia e a apresentação<br />
da end<strong>of</strong>talmite foi de 5,5 dias (intervalo de 5-6 dias). A acuidade visual no momento<br />
do diagnóstico foi melhor que 20/40 em um paciente (2%), de 20/40 a 20/200 em um<br />
paciente (2%), de 20/400 para contar dedos em dois pacientes (4%), movimento de mão<br />
em onze pacientes (24%), percepção de luz em trinta pacientes (68%). Pseudomonas<br />
aeruginosa foi o agente isolado em 26 amostras de vítreo e em três amostras da câmara<br />
anterior. No geral, um paciente (2%) obteve acuidade visual final melhor que 20/40,<br />
oito pacientes (18%) obtiveram acuidade visual final de 20/40 a 20/200, seis pacientes<br />
(13%) obtiveram acuidade visual final de 20/400 para contar os dedos; onze pacientes<br />
(25%) obtiveram acuidade visual final de movimento de mão; treze pacientes (29%)<br />
obtiveram acuidade visual final de percepção de luz e seis (13%) pacientes não havia<br />
percepção luminosa no último exame. Nenhum olho foi submetido à evisceração ou<br />
enucleação em três meses de acompanhamento.<br />
Conclusão: Mesmo com toda a segurança da cirurgia de catarata nos dias atuais,<br />
end<strong>of</strong>talmite permanece um risco e uma complicação temível deste procedimento.<br />
No presente estudo não foi possível identificar a fonte do surto.<br />
Descritores: Facoemulsificação/efeitos adversos; End<strong>of</strong>talmite/etiologia; Pseudomonas<br />
aeruginosa; Vitrectomia; Infecções por pseudomonas; Contaminação de<br />
equipamentos<br />
INTRODUCTION<br />
Acute endophthalmitis is the most serious complication <strong>of</strong> cataract<br />
surgery and intraocular lens implantation, with an incidence<br />
<strong>of</strong> 0.07% to 0.12% (1) . Endophthalmitis occurring within 1 to 14 days<br />
postoperatively is classified as acute. The most common cultured<br />
or ganism is Staphylococcus epidermidis, accounting <strong>for</strong> 60% to 80%<br />
<strong>of</strong> cases (1) . Gram-negative bacteria are responsible <strong>for</strong> 6% to 29%<br />
<strong>of</strong> cases, however, the rapid progression <strong>of</strong> infection and their<br />
virulence <strong>of</strong>ten result in a poor visual outcome despite prompt<br />
treatment (2-4) .<br />
The most common ocular infection caused by Pseudomonas aeruginosa<br />
is contact lens-related keratitis, but it may also cause endophthalmitis<br />
(5) . Outbreaks <strong>of</strong> postoperative P. aeruginosa endophthalmitis<br />
have been described in the literature (6-14) . The association with<br />
intrinsic contamination <strong>of</strong> ophthalmic solutions and contaminated<br />
instruments or equipment has been reported (6-13) .<br />
The purpose <strong>of</strong> this study is describing an outbreak <strong>of</strong> Pseudomonas<br />
aeruginosa endophthalmitis after cataract surgery, which occurred<br />
at one ophthalmological center <strong>of</strong> Eunapólis city, Bahia, Brazil.<br />
Clinical findings, treatment and outcome are discussed.<br />
Submitted <strong>for</strong> publication: March 12, 2012<br />
Accepted <strong>for</strong> publication: July 30, 2012<br />
Study carried out at Retina and Vitreous Service, Hospital São Rafael - Fundação Monte Tabor - Salvador<br />
(BA) - Brazil.<br />
1<br />
Physician, Department <strong>of</strong> Ophthalmology, Hospital São Rafael, Fundação Monte Tabor, Salvador<br />
(BA), Brazil.<br />
2<br />
Physician.<br />
3<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Ophthalmology, Hospital São Rafael, Fundação Monte Tabor, Salvador<br />
(BA), Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: R.L.L.Guerra, None; B.P.Freitas, None; C.M.F.M.Parcero,<br />
None; O.O.Maia Jr, None; R.L.Marback, None.<br />
Correspondence address: Otacilio O. Maia Jr. Retina and Vitreous Service, Department <strong>of</strong> Ophthalmology.<br />
Hospital São Rafael - Fundação Monte Tabor. Av. São Rafael, 2142 - Salvador - BA -<br />
41253-190 – Brazil - E-mail: omaiausp@uol.com.br<br />
344 Arq Bras Oftalmol. 2012;75(5):344-7
Guerra RLL, et al.<br />
METHODS<br />
A retrospective study based on medical records analysis <strong>of</strong> <strong>for</strong> tyfive<br />
patients with diagnosis <strong>of</strong> acute endophthalmitis after cataract<br />
surgery per<strong>for</strong>med in two consecutive days at one ophthalmological<br />
center <strong>of</strong> Eunapólis city, Bahia, Brazil, and treated at São Rafael Hos -<br />
pital in a two consecutive day period. All patients underwent pha -<br />
coemulsification and foldable single piece intraocular lens implantation<br />
in the capsular bag. Exclusion criteria were incomplete data or<br />
less than a ninety day follow-up period. No patient was excluded from<br />
the study. The cases occurred in September, 2009.<br />
The study protocol was approved by the Institutional Ethics Review<br />
Board <strong>of</strong> the São Rafael Hospital- Fundação Monte Tabor (CAAE<br />
- 00901112.5.0000.0048), and conducted by the Retina and Vitreous<br />
Service <strong>of</strong> the same institution.<br />
Three vitreoretinal specialists submitted all the patients to oph -<br />
thalmologic examination. The same specialists collected the data.<br />
Data reviewed included demographic in<strong>for</strong>mation, affected eye,<br />
pertinent systemic medical problems, interval between surgery and<br />
onset, signs and symptoms, treatment per<strong>for</strong>med and outcome <strong>of</strong><br />
visual acuity and eye preservation. The ophthalmologic examination<br />
at the ninetieth day after treatment was considered as the last<br />
ophthalmological examination.<br />
All patients were treated <strong>for</strong> endophthalmitis on the day <strong>of</strong> presentation.<br />
Anterior chamber irrigation, administration <strong>of</strong> intravitreous<br />
antibiotics (vancomycin and ceftazidime) and primary vitrectomy<br />
we re per<strong>for</strong>med in all the patients. Secondary vitrectomy (reoperation)<br />
was per<strong>for</strong>med in the cases with poor response to the treatment.<br />
Perioperative images <strong>of</strong> different patients are shown in figure 1.<br />
A<br />
C<br />
E<br />
Figure 1. Perioperative images <strong>of</strong> different patients. A) Appearance<br />
be<strong>for</strong>e the surgery. B) Mechanical removal <strong>of</strong> membrane from the anterior<br />
chamber. C) Mechanical removal <strong>of</strong> membrane from the posterior<br />
chamber. D) Removal <strong>of</strong> opacities from the anterior vitreous and posterior<br />
capsule. E) Vitrectomy in a mild case. F) Vitrectomy in a severe case.<br />
B<br />
D<br />
F<br />
Vitreous and anterior-chamber fluid aspirates were collected in<br />
the operating room using a sterile syringe prior to vitrectomy and<br />
intravitreal antibiotic injection and were sent immediately to the<br />
mi crobiology laboratory (at the same hospital) <strong>for</strong> analysis. A micro -<br />
biologist inoculated the samples on blood agar, chocolate agar, Mac -<br />
conkey agar and Sabouraud agar.<br />
Following the protocol <strong>of</strong> the hospital, susceptibility to amikacin,<br />
ampicillin, ampicillin sulbactam, aztreonam, cephalothin, cefepime,<br />
ce fotaxime, cefoxitin, ceftazidime, gentamicin, imipenem, meropenem,<br />
piperacillin-tazobactam and trimethoprim-sulfa were tested.<br />
RESULTS<br />
Forty-five patients (twenty-three men and twenty-two women)<br />
presenting acute P. aeruginosa endophthalmitis post phacoemulsification<br />
were identified. The average age was 71.2 years (range, 56-83<br />
years). The right eye (62%) was more <strong>of</strong>ten affected than the left<br />
eye (38%). Associated systemic medical findings included arterial<br />
hy pertension (53%) and type 2 diabetes mellitus (11%). The median<br />
interval between surgery and endophthalmitis onset was 5.5 days<br />
(range, 5-6 days).<br />
Visual acuity at diagnosis was better then 20/40 in one patient<br />
(2%), from 20/40 to 20/200 in one patient (2%), from 20/400 to<br />
coun ting fingers in two patients (4%), hand movements in eleven<br />
patients (24%) and light perception in thirty patients (68%). The most<br />
significant findings at the diagnosis were decreased visual acuity<br />
(96%), pain (84%), hyperemia (73%), eyelid edema (42%), headache<br />
(4%), <strong>for</strong>eign body sensation (4%) and fever (2%). Additional clinical<br />
findings at the diagnosis were conjunctival hyperemia (100%), anterior<br />
chamber inflammatory reaction (91%), hypopyon (82%), corneal<br />
edema (76%), pupillary membrane (64%), chemosis (56%), vitreous in<br />
anterior chamber (4%), conjunctival purulent secretion (4%), hyphema<br />
(2%) and shallow anterior chamber (2%) - table 1.<br />
Cultures were positive <strong>for</strong> Pseudomonas in twenty-six patients<br />
(57.8%), three (6.6%) anterior chamber samples and twenty-six<br />
(57.8%) vitreous samples. Nineteen patients (42.2%) had negative<br />
cul tures. Antibiotic resistance test were similar in all cases, sensitive<br />
to amikacin, aztreonam, cefepime, cefotaxime, ceftazidime, gentami -<br />
cin, imipenem, meropenem, piperacillin-tazobactam and trimetho -<br />
Table 1. The most significant findings at the diagnosis<br />
<strong>Ocular</strong> finding Incidence (%)<br />
Hyperemia 100<br />
Decreased visual acuity 096<br />
Anterior chamber reaction 091<br />
Pain 084<br />
Hypopyon 082<br />
Corneal edema 076<br />
Pupillary membrane 064<br />
Chemosis 056<br />
Eyelid edema 042<br />
Vitreous in anterior chambre 004<br />
Purulent secretion 004<br />
Headache 004<br />
Foreing body sensation 004<br />
Fever 002<br />
Hyphema 002<br />
Shallow anterior chamber 002<br />
Arq Bras Oftalmol. 2012;75(5):344-7<br />
345
An outbreak <strong>of</strong> <strong>for</strong>ty five cases <strong>of</strong> Pseudomonas aeruginosa acute endophthalmitis after phacoemulsification<br />
prim-sulfa, and resistant to ampicillin, ampicillin sulbactam, cefoxitin<br />
and cephalothin.<br />
One patient (2%) achieved a final visual acuity better than 20/40;<br />
eight patients (18%) achieved a final visual acuity from 20/40 to<br />
20/200; six patients (13%) achieved a final visual acuity from 20/400<br />
to counting fingers; eleven patients (25%) achieved a final acuity <strong>of</strong><br />
hand movements; thirteen patients (29%) achieved a final acuity<br />
<strong>of</strong> light perception and six patients (13%) were no light perception<br />
at the last follow-up. Five patients were submitted to a secondary<br />
vitrectomy. None <strong>of</strong> the studied eyes underwent evisceration or<br />
enu cleation in a three-month follow-up period. Best corrected visual<br />
acuity be<strong>for</strong>e and after treatment is shown in figure 2.<br />
Discussion<br />
The largest Pseudomonas endophthalmitis outbreak post ca -<br />
taract surgery that we were able to find in the literature involved<br />
twenty eyes <strong>of</strong> twenty patients in a six-week period (14) . In the current<br />
study we had <strong>for</strong>ty-five eyes <strong>of</strong> <strong>for</strong>ty-five patients (twenty-six culture<br />
positive <strong>for</strong> Pseudomonas) in a two consecutive day period. Endophthalmitis<br />
suspect cases cultures turn out to be positive in a range<br />
<strong>of</strong> 24% to 85% according to different studies (15) .<br />
Pseudomonas aeruginosa is one <strong>of</strong> the most common Gramne<br />
gative pathogens associated with nosocomial infections (14) . The<br />
epidemics seem to be related to contaminated intraocular irrigating<br />
solutions (6,7,9,12,14) . Pseudomonas was also identified in povidone-io -<br />
dine solution (14) , at the fluid pathways <strong>of</strong> a phacoemulsifier (9) , water<br />
<strong>of</strong> autoclave (12) and air-conditioning system (14) . Technics as high-re -<br />
solution fluorescent amplified fragment length polymorphism<br />
ana lysis can identify the source <strong>of</strong> the outbreak to help preventing<br />
new ones (16) . It was impossible to identify the source <strong>of</strong> the outbreak<br />
because all the patients were referred from another hospital (500<br />
miles away) and no cultures <strong>of</strong> the phacoemulsification fluids and<br />
oph thalmic solutions were per<strong>for</strong>med.<br />
According to the Endophthalmitis Vitrectomy Study (EVS), the re -<br />
commended treatment <strong>for</strong> endophthalmitis is primary vitrectomy<br />
only <strong>for</strong> cases with light perception, any acuity better than this should<br />
be submitted to intravitreous antibiotic injection after intraocular<br />
fluid aspiration <strong>for</strong> culture (2) . Chen et al., suggests that vitrectomy<br />
(pri mary or secondary) reduces the likelihood <strong>of</strong> evisceration (17) . In<br />
the current study all the patients underwent primary vitrectomy, five<br />
<strong>of</strong> them needed a secondary vitrectomy and no patient underwent<br />
evisceration or enucleation in a three-month follow-up. The EVS protocol<br />
was not followed in this outbreak. The aggressive clinical as pect<br />
at the diagnosis <strong>of</strong> endophthalmitis was crucial <strong>for</strong> the choice <strong>of</strong> the<br />
treatment per<strong>for</strong>med.<br />
Generally the visual prognosis is poor despite <strong>of</strong> the treatment<br />
with intravitreal antibiotics even in cases in which the isolates<br />
Figure 2. Best corrected visual acuity be<strong>for</strong>e and after treatment.<br />
were sensitive (14) . In a nine patient reported outcome, five <strong>of</strong> them<br />
reached final acuity <strong>of</strong> no light perception and no patient reached<br />
acuity better then 20/400 (4) . In the EVS, four <strong>of</strong> the four hundred and<br />
twenty patients had confirmed Pseudomonas endophthalmitis and,<br />
three <strong>of</strong> these, had final acuity worse then 20/400 (2) . In the current<br />
study, nine patients had final acuity 20/200 or better, six patients<br />
between 20/400 and counting fingers, eleven had hand movements,<br />
thirteen had light perception and six no light perception. None <strong>of</strong><br />
these eyes underwent primary or secondary evisceration. Maybe the<br />
better visual outcome in some <strong>of</strong> these cases could be attributed<br />
to the treatment per<strong>for</strong>med (primary vitrectomy, anterior chamber<br />
irrigation and intravitreal antibiotics) in all patients at the diagnosis<br />
despite the visual acuity.<br />
The choice <strong>of</strong> antibiotics <strong>for</strong> injection at the first moment, prior<br />
to culture results, aims to cover gram positive and gram negative<br />
bacteria. The safety and effectiveness <strong>of</strong> vancomycin and ceftazidime<br />
combined has been reported in experimental studies using mice and<br />
confirmed in humans case series (4,18) . To treat ocular Pseudomonas infection<br />
we must take into consideration the increasing prevalence <strong>of</strong><br />
antibiotic-resistant isolates. Reviewing the literature we have found<br />
reports <strong>of</strong> resistance to various antibiotics as cefazolin, ampicillin,<br />
cephalothin, neomycin, chloramphenicol, tetracycline, aminoglycosides,<br />
and fluoroquinolones (14) . In the current study, resistance<br />
to am picillin, ampicillin-sulbactam, cephalothin and cefoxitin was<br />
ob served. The other antibiotics tested (amikacin, aztreonam, cefepime,<br />
cefotaxime, ceftazidime, gentamicin, imipenem, meropenem,<br />
piperacillin-tazobactam and trimethoprim-sulfa) were effective on<br />
the isolated strain <strong>of</strong> Pseudomonas.<br />
CONCLUSION<br />
Even with all the safety cataract surgery has achieved, today,<br />
en dophthalmitis remains a risk and a fearful complication <strong>of</strong> the<br />
procedure. The proper cleaning and sterilization <strong>of</strong> surgical instruments,<br />
surgical quality inputs, and correct prophylaxis are crucial to<br />
prevention. In the present study, it was impossible to identify the<br />
source <strong>of</strong> the outbreak.<br />
Another fact that caught the attention <strong>of</strong> the authors was the<br />
high level <strong>of</strong> preservation <strong>of</strong> the eyeball and some useful vision as<br />
compared to the results <strong>of</strong> other case series found in literature. It<br />
might have been due to the early treatment with primary vitrectomy<br />
and subsequent intravitreal antibiotic injection at the time <strong>of</strong><br />
endophthalmitis diagnosis. Further study is needed to sustain this<br />
hypothesis.<br />
REFERENCES<br />
1. Kresl<strong>of</strong>f MS, Castellarin AA, Zarbin MA. Endophthalmitis. Surv Ophthalmol. 1998;<br />
43(3):193-224.<br />
2. Results <strong>of</strong> the Endophthalmitis Vitrectomy Study. A randomized trial <strong>of</strong> immediate<br />
vitrectomy and <strong>of</strong> intravenous antibiotics <strong>for</strong> the treatment <strong>of</strong> postoperative<br />
bacterial endophthalmitis. Endophthalmitis Vitrectomy Study Group. Arch Ophthalmol.<br />
1995;113(12):1479-96. Comment in: Arch Ophthalmol. 1995;113(12):1555-7;<br />
Arch Ophthalmol. 1996;114(8):1029-30; Arch Ophthalmol. 1996;114(8):1029; author<br />
reply 1028-9, 1030; Arch Ophthalmol. 2002;120(2):231-3; Arch Ophthalmol.<br />
1996;114(8):1025; author reply 1026-7; Arch Ophthalmol. 1996;114(8):1027-8; author<br />
reply 1028-9; Arch Ophthalmol. 2002;120(2):230-1.<br />
3. Aaberg TM Jr, Flynn HW Jr, Schiffman J, Newton J. Nosocomial acute-onset postope -<br />
rative endophthalmitis survey: a 10-year review <strong>of</strong> incidence and outcomes.<br />
Oph thalmology. 1998;105(6):1004-10.<br />
4. Eifrig CW, Scott IU, Flynn HW, Miller D. Endophthalmitis caused by Pseudomonas<br />
aeruginosa. Ophthalmology. 2003;110(9):1714-7.<br />
5. Pinna A, Usai D, Sechi LA, Molicotti P, Zanetti s, Carta A. Detection <strong>of</strong> virulence factors<br />
in Pseudomonas aeruginosa strains isolated from contact lens-associated corneal<br />
ulcers. Cornea. 2008;27(3):320-6.<br />
6. Swaddiwudhipong W, Tangkitchot T, Silarug N. An outbreak <strong>of</strong> Pseudomonas aeruginosa<br />
postoperative endophthalmitis caused by contaminated intraocular irrigating<br />
solution. Trans R Soc Trop Med Hyg. 1995;89(3):288.<br />
7. Centers <strong>for</strong> Disease Control and Prevention (CDC). Outbreaks <strong>of</strong> postoperative bac-<br />
346 Arq Bras Oftalmol. 2012;75(5):344-7
Guerra RLL, et al.<br />
terial endophthalmitis caused by intrinsically contaminated ophthalmic solutions<br />
- Thailand, 1992, and Canada, 1993. MMWR Morb Mortal Wkly Rep. 1996;45(23):<br />
49-4.<br />
8. Arsan AK, Adisen A, Duman S, Aslan B, Koçak I. Acute endophthalmitis outbreak after<br />
cataract surgery. J Cataract Refract Surg. 1996;22(8):1116-20.<br />
9. Zaluski S, Clayman HM, Karsenti G, Bourzeix S, Tournemire A, Faliu B, et al. Pseudomonas<br />
aeruginosa endophthalmitis caused by contamination <strong>of</strong> the internal fluid<br />
pathways <strong>of</strong> a phacoemulsifier. J Cataract Refract Surg. 1999;25(4):540-5.<br />
10. Cruciani M, Malena M, Amalfitano G, Monti P, Bonomi L. Molecular epidemiology in<br />
a cluster <strong>of</strong> cases <strong>of</strong> postoperative Pseudomonas aeruginosa endophthalmitis. Clin<br />
Infect Dis. 1998;26(2):330-3.<br />
11. H<strong>of</strong>fmann KK, Weber DJ, Gergen MF, Rutala WA, Talte G. Pseudomonas aeruginosa-re -<br />
lated postoperative endophthalmitis linked to a contaminated phacoemulsifier. Arch<br />
Ophthalmol. 2002;120(1):90-3.<br />
12. Mateos I, Valencia R, Torres MJ, Cantos A, Conde M, Aznar J. Nosocomial outbreak<br />
<strong>of</strong> Pseudomonas aeruginosa endophthalmitis. Infect Control Hosp Epidemiol. 2006;<br />
27(11):1249 -51.<br />
13. Boks T, van Dissel JT, Teterissa N, Ros F, Mahmut MH, Utama ED, et al. An outbreak<br />
<strong>of</strong> endophthalmitis after extracapsular cataract surgery probably caused by endotoxin<br />
contaminated distilled water used to dissolve acetylcholine. Br J Ophthalmol.<br />
2006;90(9):1094-7.<br />
14. Pinna A, Usai D, Sechi LA, Zanetti S, Jesudasan NC, Thomas PA, et al. An outbreak<br />
<strong>of</strong> post-cataract surgery endophthalmitis caused by Pseudomonas ae ruginosa.<br />
Ophthalmology. 2009;116(12):2321-6. Comment in: Ophthalmology. 2010;117(8):<br />
1657-8; author reply 1658-9.<br />
15. Bispo PJ, Melo GB, d’Azevedo PA, Höfling-Lima AL, Yu MC, Pignatari AC. [Culture proven<br />
bacterial endophthalmitis: a 6-year review]. Arq Bras Oftalmol. 2008;71(5):617-22.<br />
Portuguese.<br />
16. Kenchappa P, Sangwan VS, Ahmed N, Rao KR, Pathengay A, Mathai A, et al. Highre<br />
solution genotyping <strong>of</strong> Pseudomonas aeruginosa strains linked to acute post<br />
cataract surgery endophthalmitis outbreaks in India. Ann Clin Microbiol Antimicrob.<br />
2005;4:19.<br />
17. Chen KJ, Sun MH, Lai CC, Wu WC, Chen TL, Kuo YH, et al. Endophthalmitis caused by<br />
Pseudomonas aeruginosa in Taiwan. Retina. 2011;31(6):1193-8.<br />
18. Yoshizumi MO, Bhavsar AR, Dessouki A, Kashani A. Safety <strong>of</strong> repeated intravitreous<br />
injections <strong>of</strong> antibiotics and dexamethasone. Retina. 1999;19(5):437-41.<br />
4 a Jornada Paulista de Oftalmologia<br />
22 e 23 de março de 2013<br />
Hotel Fonte Colina Verde<br />
São Pedro (SP)<br />
Promoção:<br />
UNESP<br />
UNICAMP<br />
USP - Ribeirão Preto<br />
In<strong>for</strong>mações:<br />
JDE Eventos<br />
Tels.: (11) 5084-9174 / 5082-3030 / 5084-5284<br />
E-mail: diva@jdeeventos.com.br<br />
Site: www.jdeeventos.com.br<br />
Arq Bras Oftalmol. 2012;75(5):344-7<br />
347
Artigo Original | Original Article<br />
Phacoemulsification and foldable acrylic IOL implantation in children with<br />
treated retinoblastoma<br />
Facoemulsificação e implante de lente intraocular acrílica dobrável em crianças com retinoblastoma<br />
Marcia Beatriz Tartarella 1 , Gloria Fátima Britez-Colombi 1 , Marcia Motono 2 , Martha Motono Chojniak 2 , Joao Borges Fortes Filho 3 , Rubens Bel<strong>for</strong>t Jr. 1<br />
ABSTRACT<br />
Purpose: To study the results <strong>of</strong> cataract surgery in children with radiation-induced<br />
cataract after treatment <strong>for</strong> retinoblastoma.<br />
Methods: Retrospective interventional case series. Six consecutive patients diagnosed<br />
with secondary cataracts due to radiation therapy <strong>for</strong> retinoblastoma. Intervention: Pha -<br />
coemulsification and foldable acrylic intraocular lens implantation. Outcomes mea sured:<br />
Visual acuity, binocular indirect ophthalmoscopy and slit-lamp biomicroscopy.<br />
Aspirated lens material and aqueous humor samples were collected during surgery.<br />
Results: Six uniocular children between 3 to 5 years <strong>of</strong> age at time <strong>of</strong> surgery were<br />
studied. The mean time interval between radiotherapy and cataract diagnosis was<br />
22.3 months. The mean follow-up after surgery was 17.2 months (range: 12 to 23<br />
months). All eyes achieved a clear visual axis after surgery allowing monitoring <strong>of</strong><br />
the tumor status. None developed recurrence or retinoblastoma dissemination.<br />
His topathological analysis <strong>of</strong> the aspired material showed no tumoral cells in all<br />
sam ples. All patients improved vision after cataract surgery.<br />
Conclusions: Phacoemulsification with acrylic intraocular lens implantation seems to<br />
be a safe, feasible, and effective method <strong>for</strong> the removal <strong>of</strong> radiation-induced cataracts<br />
in patients with treated retinoblastoma.<br />
Keywords: Retinoblastoma/cirurgia; Retinoblastoma/radiotherapy; Retinal neoplasms/radiotherapy;<br />
Cataract/etiology; Eye enucleation; Radiation injuries; Radiotherapy/adverse;<br />
Lens implantation, intraocular; Humans; Child<br />
RESUMO<br />
Objetivos: Estudar os resultados da cirurgia da catarata induzida pela radioterapia para<br />
o tratamento do retinoblastoma em crianças.<br />
Métodos: Estudo retrospectivo intervencional em série de casos onde seis pacientes consecutivos<br />
apresentaram catarata secundária à terapia por radiação para o retinoblastoma.<br />
Intervenção: Facoemulsificação e implante de lente intraocular acrílica dobrável. Foram<br />
avaliadas: acuidade visual, <strong>of</strong>talmoscopia binocular indireta e biomicroscopia. Material<br />
para análise histológica do cristalino e do humor aquoso foi coletado durante as cirurgias.<br />
Resultados: Seis crianças, entre 3 e 5 anos de idade, com catarata secundária à radiação<br />
para tratamento de retinoblastoma <strong>for</strong>am submetidas à cirurgia de facoemulsificação<br />
com implante de lente intraocular. A média do intervalo de tempo decorrido entre a<br />
radioterapia e o diagnóstico da catarata foi 22,3 meses. O período médio de seguimento<br />
após a cirurgia foi de 17,2 meses (intervalo: 12 a 23 meses). Todos os olhos melhoraram a<br />
visão e mantiveram eixo visual livre permitindo a fundoscopia para monitorar o tumor.<br />
Nenhum paciente evoluiu com recorrência ou disseminação do retinoblastoma. A análise<br />
histopatológica do material colhido resultou em ausência de células tumorais nas amostras.<br />
Conclusões: A cirurgia de facoemulsificação com implante de lente intraocular acrílica<br />
dobrável mostrou ser um procedimento seguro e efetivo para o tratamento da catarata<br />
induzida pela radioterapia em pacientes portadores de retinoblastoma.<br />
Descritores: Retinoblastoma/cirurgia; Retinoblastoma/radioterapia; Neoplasisas da<br />
retina/radioterapia; Catarata/etiologia; Enucleação ocular; Lesões por radiação; Radioterapia/efeitos<br />
adversos; Implante de lente intraocular; Humanos; Criança<br />
INTRODUCTION<br />
Retinoblastoma (RB) is the most common intraocular malignancy<br />
in childhood, occurring in approximately 1 <strong>of</strong> 20,000 live births (1) .<br />
The goals <strong>of</strong> management <strong>of</strong> RB are, first, to preserve life and, second,<br />
to salvage the eye and restore vision if possible (2) . Earlier diagnosis<br />
coupled with new therapeutic modalities such as External Beam Radiotherapy<br />
(EBRT), radioactive plaque and brachytherapy have allowed<br />
successful treatment avoiding enucleation in many cases (1-5) .<br />
About 20% to 87% <strong>of</strong> the patients treated with radiotherapy can<br />
develop a radiation-induced secondary cataract blocking the visual<br />
axis and there<strong>for</strong>e causing severe reduction <strong>of</strong> visual acuity (VA) (6-8) .<br />
Maintenance <strong>of</strong> a clear visual axis is important in order to allow<br />
the examination <strong>of</strong> the eye fundus and to observe the regressed re -<br />
tinoblastoma lesions (9) .<br />
The purpose <strong>of</strong> this study was to evaluate the visual outcome and<br />
ocular complications <strong>of</strong> the cataract surgery by phacoemulsification<br />
and foldable acrylic intraocular lens implantation (IOL) in children<br />
with radiation-induced cataract after treatment <strong>for</strong> RB.<br />
METHODS<br />
Six uniocular patients with secondary cataract due to radiation<br />
therapy <strong>for</strong> RB treatment were submitted to phacoemulsification<br />
and IOL implantation at the Congenital Cataract Section, Department<br />
<strong>of</strong> Ophthalmology, Federal University <strong>of</strong> Sao Paulo SP, Brazil. During<br />
surgery, a sample <strong>of</strong> aqueous humor (0.2 ml) was collected from the<br />
anterior chamber <strong>for</strong> analysis. Aspirated lens material (0.2 ml) was also<br />
sent <strong>for</strong> histopathological analysis.<br />
Table 1 presents the age (in months) <strong>of</strong> patients at RB diagnosis,<br />
the different prescribed treatments, and the time interval between<br />
radiotherapy and the diagnosis <strong>of</strong> cataract. All patients had bilateral<br />
RB, and all <strong>of</strong> them had one eye previously enucleated. All eyes had<br />
Submitted <strong>for</strong> publication: April 4, 2012<br />
Accepted <strong>for</strong> publication: August 22, 2012<br />
Study carried out at Department <strong>of</strong> Ophthalmology, Universidade Federal de São Paulo - UNIFESP - São<br />
Paulo (SP), Brazil.<br />
1<br />
Physician, Department <strong>of</strong> Ophthalmology, Universidade Federal de São Paulo - UNIFESP - São<br />
Paulo (SP), Brazil.<br />
2<br />
Physician, <strong>Ocular</strong> Oncology Department, Hospital A C Camargo, São Paulo (SP), Brazil.<br />
3<br />
Physician, Department <strong>of</strong> Ophthalmology, Universidade Federal do Rio Grande do Sul - UFRS -<br />
Porto Alegre (RS), Brazil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: M.B.Tartarella, None; G.F.Britez-Colombi, None;<br />
M.Motono, None; M.M.Chojniak, None; J.B.Fortes Filho, None; R.Bel<strong>for</strong>t Jr, None.<br />
Correspondence address: João Borges Fortes Filho. School <strong>of</strong> Medicine, Department <strong>of</strong> Ophthalmology.<br />
Hospital de Clinicas de Porto Alegre, Federal University <strong>of</strong> Rio Grande do Sul. Rua Ramiro<br />
Barcelos, 2350 - Porto Alegre (RS) 90035-903 - Brazil - E-mail: jb<strong>for</strong>tes@cursohbo.com.br<br />
348 Arq Bras Oftalmol. 2012;75(5):348-51
Tartarella MB, et al.<br />
inactive tumors when they presented <strong>for</strong> cataract surgery. Lens opa -<br />
cities hindered fundus examination in all patients.<br />
Visual acuity was measured with Snellen acuity cards, Teller Acuity<br />
Cards or Lea Hyvarigen Acuity Cards depending on patient collaboration.<br />
Final best corrected visual acuity (BCVA) was obtained at the<br />
last followup visit.<br />
Calculation <strong>of</strong> the IOL power was based on previous studies <strong>of</strong><br />
axial length growth in pseudophakic eyes <strong>of</strong> children with lamellar<br />
cataract, as follows: children aged 3 to 4 years had a 10% reduction<br />
<strong>of</strong> the calculated IOL power. Children between 4 and 6 years had an<br />
addition <strong>of</strong> 0.75% on the preoperative axial length in order to calculate<br />
the final IOL diopter (10) .<br />
The same surgeon (MBT) operated on all cases using the same<br />
technique. A clear corneal tunnel incision was per<strong>for</strong>med and a lateral<br />
paracentesis was used to allow the introduction <strong>of</strong> any additional instrument<br />
during phacoemulsification. Viscoelastic substance (Viscoat ® )<br />
was used to fill the anterior chamber. An anterior continuous circular<br />
capsulorhexis followed by hydrodissection and hydrodeliniation were<br />
per<strong>for</strong>med. Phacoemulsification or phacoaspiration <strong>of</strong> the lens was<br />
per<strong>for</strong>med followed by a meticulous aspiration <strong>of</strong> lens material. A<br />
foldable acrylic IOL (AcryS<strong>of</strong> ® ) was implanted within the capsular bag.<br />
Next step included aspiration <strong>of</strong> the viscoelastic substance from the<br />
anterior chamber and injection <strong>of</strong> a miotic drug (Miostat ® ). One or two<br />
single sutures (mononylon 10-0) were used to achieve a safe closure <strong>of</strong><br />
the corneal incision. Subconjuntival dexamethasone (0.5 mg/1 ml) and<br />
gentamicin (40 mg/1 ml) were injected at the end <strong>of</strong> surgery. Topical<br />
antibiotics and corticosteroids were applied <strong>for</strong> the first two weeks<br />
after surgery and tapered during 2 months <strong>of</strong> follow-up.<br />
Visual acuity, binocular indirect ophthalmoscopy and slit lamp<br />
examination were assessed on all postoperative visits.<br />
RESULTS<br />
Patients were between 3 and 5 years-old (mean 4.9 years-old) at<br />
the time <strong>of</strong> cataract surgery. Three eyes presented nuclear cataract<br />
and three eyes presented posterior sub-capsular cataract. Mean time<br />
between radiotherapy and cataract diagnosis was 22.3 months. All<br />
patients included in this study showed initial VA worse than 20/200.<br />
All children improved VA after surgery (Table 2). Mean postoperative<br />
follow-up was 17.2 months (12 to 23 months).<br />
A posterior paracentral capsule opacification (PCO) was observed<br />
during surgery in three eyes (patients #2, #4 and #5) but the capsule<br />
was left intact. No patient needed a Neodimium YAG laser posterior<br />
capsulotomy.<br />
Patient #4 presented an inflammatory membrane anterior to the<br />
IOL that disappeared within two weeks after surgery.<br />
One eye (patient #3) developed a paracentral mild PCO during<br />
the follow-up. This PCO did not affect VA or eye fundus examination<br />
(Figure 2).<br />
Five eyes received a three-piece acrylic hydrophobic foldable IOL<br />
(MA60AC, Alcon AcryS<strong>of</strong> ® ) and one eye received a single-piece IOL<br />
(SA30AL Alcon AcryS<strong>of</strong> ® ).<br />
Intraocular lens power ranged from +21 to +29 (mean +25.5 D).<br />
Refraction was obtained and glasses with protective polycarbonate<br />
multifocal lenses were prescribed <strong>for</strong> all patients.<br />
Slit lamp examination postoperatively showed severe dry eye<br />
with fluorescein staining in two eyes.<br />
All eyes achieved a clear visual axis after cataract surgery, allowing<br />
monitoring tumoral status (Figure 1, patient #6). None had recurrence<br />
or spread <strong>of</strong> the tumor during the follow-up time <strong>of</strong> this study. Histopathological<br />
analysis <strong>of</strong> aqueous humor and aspirated lens material<br />
showed no tumoral cells in the samples <strong>of</strong> all patients.<br />
DISCUSSION<br />
Retinoblastoma is the most frequent intraocular tumor in child hood (1)<br />
and early detection and treatment is essential. Erwenne and Franco (11)<br />
found that advanced age and delayed diagnosis increase the chance<br />
<strong>for</strong> <strong>extraocular</strong> disease that mandates significantly more aggressive<br />
treatment.<br />
Time range between the appearance <strong>of</strong> first RB signs and the<br />
initial treatment as well as the management <strong>of</strong> RB influence the outcomes<br />
(4) .<br />
In the past, standard treatments <strong>for</strong> RB consisted <strong>of</strong> enucleation<br />
and EBRT. Systemic chemotherapy was generally reserved <strong>for</strong><br />
patients with invasion <strong>of</strong> the optic nerve, choroid, orbit or with metastatic<br />
disease (1) . Nowadays, chemoreduction has been widely used<br />
to avoid EBRT (1,5) . Other management options in children include ra-<br />
Table 2. Visual acuity be<strong>for</strong>e and after cataract surgery<br />
Patient<br />
Age at surgery<br />
(years)<br />
VA be<strong>for</strong>e<br />
cataract surgery<br />
Follow-up<br />
(months)<br />
Final<br />
BCVA<br />
1 3 20/570 23 20/400<br />
2 5 20/200 12 20/30<br />
3 4 CF 2 m 19 20/70<br />
4 4 CF 50 cm 13 20/200<br />
5 5 LP 16 20/60<br />
6 5 LP 20 20/40<br />
VA= visual acuity; Final BCVA= best corrected VA at last follow-up; CF= counting fingers<br />
vision; LP= light perception vision.<br />
Table 1. Retinoblastoma diagnosis, therapy and time interval between<br />
radiotherapy and cataract development<br />
Patient Age* TTT Cryo Photo Brachy Chemo RXT Cataract †<br />
1 10 + + + 0 + + 14<br />
2 04 0 0 + 0 0 + 40<br />
3 02 + + + 0 + + 25<br />
4 02 + + + + 0 + 14<br />
5 22 + 0 + 0 + + 14<br />
6 20 + 0 0 + 0 + 24<br />
*= age in months at retinoblastoma diagnosis; TTT= transpupillary thermotherapy; Cryo=<br />
cryotherapy; Photo= phototherapy; Brachy= brachytherapy; Chemo= chemotherapy;<br />
RXT= radiotherapy; += therapy yes; 0= therapy no; † = time interval between radiotherapy<br />
and radiation-induced cataract (in months).<br />
Figure 1. Patient # 6 - Eye fundus with inactive retinoblastoma: tumor status 20 months<br />
after cataract surgery and IOL implantation.<br />
Arq Bras Oftalmol. 2012;75(5):348-51<br />
349
Phacoemulsification and foldable acrylic IOL implantation in children with treated retinoblastoma<br />
Figure 2. Patient #3 - posterior capsule opacification.<br />
diation therapy, photocoagulation, cryotherapy, and chemotherapy.<br />
Focal treatment modalities, as radioactive plaques, have promising<br />
prospects (4,9) .<br />
Radiotherapy has been a useful modality in the treatment <strong>of</strong> RB,<br />
but lens irradiation may cause cataract induction, usually occurring 2<br />
to 12 years after treatment (12) . In our study we found a mean latency<br />
period <strong>of</strong> 22.3 months from radiotherapy to cataract diagnosis.<br />
Treatment <strong>of</strong> radiation-induced cataracts is similar to treatment<br />
<strong>for</strong> pediatric cataracts. The implantation <strong>of</strong> an IOL by itself may not<br />
increase the risk <strong>of</strong> recurrence <strong>of</strong> RB or systemic metastasis and could<br />
be considered <strong>for</strong> providing optimal visual rehabilitation after cataract<br />
surgery. All patients in this series improved VA, although other<br />
factors as tumor size and location, age <strong>of</strong> the patient and amblyopia<br />
may influence the final visual results.<br />
Samples <strong>of</strong> aqueous humor and aspirated lens material were<br />
easily obtained during cataract surgery. Hadjistilianou et al., analyzed<br />
aqueous humor proteins in patients with RB and reported an increase<br />
in protein content in eyes with RB (13) . In order to investigate malignant<br />
cells, the samples were collected and a histopathological analysis was<br />
per<strong>for</strong>med. The results <strong>of</strong> our study showed the absence <strong>of</strong> malignant<br />
cells in the samples.<br />
The role <strong>of</strong> posterior capsulotomy in spreading tumor cells is yet<br />
unknown but Brooks et al. (3) , recommended avoiding posterior capsulotomy<br />
to prevent an eventual seeding <strong>of</strong> the tumor. Although posterior<br />
capsulorrhexis in children is advisable, we preferred to main tain<br />
the posterior capsule in order to respect the anatomical barrier between<br />
anterior and posterior eye segments. All children were older than 3<br />
years-age at the time <strong>of</strong> surgery and might be able to collaborate to<br />
per<strong>for</strong>m Neodimiun- YAG laser posterior capsulotomy if necessary.<br />
Miller et al. (14) , described good results after pars plana lensectomy<br />
and IOL implantation in radiation-induced cataracts in children with RB.<br />
Same authors (15) reported a series <strong>of</strong> eleven eyes that underwent<br />
a primary IOL implantation after RB treatment. They concluded that<br />
IOL implantation seemed to be a safe method <strong>for</strong> aphakia correction.<br />
The authors advised penetrating the anterior chamber through a<br />
clear corneal incision to avoid direct contact with conjunctival blood<br />
vessels, scleral tissues, and vitreous management in order to reduce<br />
the risk <strong>of</strong> spreading tumoral cells (15) .<br />
Besides tumoral spread or recurrences, the complications expected<br />
in the removal <strong>of</strong> radiation-induced cataracts are similar to<br />
pediatric cataract surgery (3,9,16-17) . In this case series no complications<br />
related to the RB occurred. All eyes studied did not develop tumor<br />
recurrence or dissemination during the follow-up period. Attention<br />
to dry eye signs and symptoms is a must in those irradiated eyes.<br />
Artificial tear drops and ointments were prescribed to two patients<br />
diagnosed with dry eye.<br />
In three eyes a partial PCO was detected at the end <strong>of</strong> surgery, but<br />
posterior capsulotomy was not per<strong>for</strong>med due to the risk <strong>of</strong> tumor<br />
dissemination. Despite the capsular opacification, indirect ophthalmoscopy<br />
was feasible and VA improved after surgery. Maintenance<br />
<strong>of</strong> a clear visual axis was obtained, allowing adequate view <strong>of</strong> the<br />
posterior pole in order to monitor the regressed tumoral lesions.<br />
Intraocular lenses choice was important, IOL material and model<br />
are related to biocompatibility in adults (18,19) and children (20-22) . This<br />
study showed good results with acrylic hydrophobic IOLs.<br />
Refractive results were within the expected calculated diopters.<br />
Future changes in refraction may occur in these growing eyes. IOL<br />
power calculation was based on previous data on axial lengths in<br />
children with cataracts (10) . There are no studies <strong>of</strong> ocular growth in<br />
eyes with RB and cataracts. Predictive IOL power calculation and axial<br />
growth in eyes with RB need further investigation.<br />
Hoehn et al. (23) , showed the effectiveness <strong>of</strong> cataract surgery to<br />
improve quality <strong>of</strong> life in affected children. The children in our study<br />
were all uniocular patients and achieved an improvement <strong>of</strong> vision<br />
that could lead to better ambulation and better integration in the<br />
community and school.<br />
CONCLUSION<br />
No tumor spread or recurrences were observed in this series and<br />
improvement <strong>of</strong> VA was obtained in all patients. We conclude that<br />
although the long term risk-benefit is still unknown, phacoemulsification<br />
and foldable acrylic IOL implantation in eyes with previously<br />
treated RB seems to be a feasible, safe and effective treatment <strong>for</strong><br />
radiation-induced cataracts, but the number <strong>of</strong> included patients is<br />
too low in order to establish an outcome complication pr<strong>of</strong>ile.<br />
REFERENCES<br />
1. Brichard B, De Bruycker JJ, De Potter P, Neven B, Vermylen C, Cornu G. Combined chemotherapy<br />
and local treatment in the management <strong>of</strong> intraocular retinoblastoma.<br />
Med Pediatr Oncol. 2002;38(6):411-5.<br />
2. Honavar SG, Singh AD, Shields CL, Meadows AT, Demirce H, Cater J, et al. Postenucleation<br />
adjuvant therapy in high-risk retinoblastoma. Arch Ophthalmol. 2002;<br />
120(7):923-31.<br />
3. Brooks HL Jr, Meyer D, Shields JA, Balas AG, Nelson LB, Fontanesi J. Removal <strong>of</strong><br />
radiation-induced cataracts in patients treated <strong>for</strong> retinoblastoma. Arch Ophthalmol.<br />
1990;108(12):1701-8.<br />
4. Balmer A, Munier F, Zografos L. Nouvelles stratégies dans le traitement du rétinoblastome.<br />
J Fr Ophtalmol. 2002;25:187-93.<br />
5. Shields CL, Honavar SG, Meadows AT, Shields JA, Demirci H, Singh A, et al. Chemoreduction<br />
plus focal therapy <strong>for</strong> retinoblastoma: factors predictive <strong>of</strong> need <strong>for</strong> treatment<br />
with external beam radiotherapy or enucleation. Am J Ophthalmol. 2002;133(5):657-64.<br />
Comment in: Am J Ophthalmol. 2002;134(4):633; author reply 633-4.<br />
6. Anteby I, Ramu N, Gradstein L, Miskin H, Pe’er J, Benezra D. <strong>Ocular</strong> and orbital complications<br />
following the treatment <strong>of</strong> retinoblastoma. Eur J Ophthalmol. 1998;8(2):<br />
106-11.<br />
7. Blach LE, McCormick B, Abramson DH. External beam radiation therapy and retinoblastoma:<br />
long-term results in the comparison <strong>of</strong> two techniques. Int J Radiat Oncol<br />
Biol Phys. 1996;35(1):45-51.<br />
8. Fontanesi J, Pratt CB, Kun LE, Hustu HO, C<strong>of</strong>fey D, Meyer D. Treatment outcome and<br />
dose-response relationship in patients younger than 1 year treated <strong>for</strong> retinoblastoma<br />
with primary irradiation. Med Pediatr Oncol. 1996;26(5):297-304.<br />
9. Honavar SG, Shields CL, Shields JA, Demirci H, d Naduvilath TJ. Intraocular surge ry<br />
after treatment <strong>of</strong> retinoblastoma. Arch Ophthalmol. 2001;119:1613-21.<br />
10. Tartarella MB. Estudo do comprimento axial em olhos de crianças portadoras de<br />
catarata lamelar bilateral [Tese]. São Paulo: Universidade Federal de São Paulo; 1998.<br />
11. Erwenne CM, Franco EL. Age and lateness <strong>of</strong> referral as determinants <strong>of</strong> <strong>extraocular</strong><br />
retinoblastoma. Ophthalmic Pediatr Genet. 1989;10(3):179-84.<br />
12. Egbert PR, Donaldson SS, Moazed K, Rosenthal AR. Visual results and ocular<br />
complications following radiotherapy <strong>for</strong> retinoblastoma. Arch Ophthalmol. 1978;<br />
96(10):1826-30.<br />
13. Hadjistilianou T, Giglioni S, Micheli L, Vannoni D, Brogi E, Cevenini G, et al. Analysis <strong>of</strong><br />
aqueous humour proteins in patients with retinoblastoma. Clin Experiment Ophthalmol.<br />
2012;40(1):e8-e15.<br />
14. Miller DM, Murray TG, Cicciarelli NL, Capo H, Markoe AM. Pars plana lensectomy and<br />
intraocular lens implantation in pediatric radiation-induced cataracts in retinoblastoma.<br />
Ophthalmology. 2005;112(9):1620-4.<br />
350 Arq Bras Oftalmol. 2012;75(5):348-51
Tartarella MB, et al.<br />
15. Portellos M, Buckley EG. Cataract surgery and intraocular lens implantation in patients<br />
with retinoblastoma. Arch Ophthalmol. 1998;116(4):449-52.<br />
16. Sinha R, Titiyal JS, Sharma N, Vajpayee RB. Management <strong>of</strong> radiotherapy-induced<br />
cataracts in eyes with retinoblastoma. J Cataract Refract Surg. 2004;30(5):1145-6.<br />
17. Osman IM, Abouzeid H, Balmer A, Gaillard MC, Othenin-Girard P, Pica A, et al. Modern<br />
cataract surgery <strong>for</strong> radiation-induced cataracts in retinoblastoma. Br J Ophthalmol.<br />
2011;95(2):227-30.<br />
18. Hollick EJ, Spalton DJ, Ursell PG, Pande MV, Barman SA, Boyce JF, et al. The effect <strong>of</strong><br />
polymethylmethacrylate, silicone, and polyacrylic intraocular lenses on posterior capsular<br />
opacification 3 years after cataract surgery. Ophthalmology. 1999;106(1):49-55.<br />
19. Sundelin K, Friberg-Riad Ylva, Östberg A, Sjöstrand J. Posterior capsule opacification<br />
with AcryS<strong>of</strong>® and poly(methylmethecrylate) intraocular lenses - comparative study<br />
with a 3-year follow-up. J Cataract Refract Surg. 2001;27(10):1586-90.<br />
20. Verçosa IMC, Tartarella MB. Catarata na criança. Fortaleza, CE: Celigráfica, 2008. 319p.<br />
21. Hosal BM, Biglan AW. Risk factors <strong>for</strong> secondary membrane <strong>for</strong>mation after removal<br />
<strong>of</strong> pediatric cataract. J Cataract Refract Surg. 2002;28(2):302-9.<br />
22. Wilson ME, Elliot L, Johnson B, Peterseim MM, Rah S, Werner L, et al. AcryS<strong>of</strong> acrylic<br />
intraocular lenses implantation in children: clinical indications <strong>of</strong> biocompatibility. J<br />
AAPOS. 2001;5(6):377-80.<br />
23. Hoehn ME, Irshad F, Kerr NC, Wilson MW. Outcomes after cataract extraction in<br />
young children with radiation-induced cataracts and retinoblastoma. J AAPOS. 2010;<br />
14(3):232-4.<br />
V Jornada de Oftalmologia<br />
do Hospital São Rafael<br />
1 e 2 de março de 2013<br />
Hospital São Rafael<br />
Salvador (BA)<br />
In<strong>for</strong>mações:<br />
E-mail: dimagnavitaeventos@yahoo.com.br<br />
Site: www.ceosr.com.br/jornada<br />
Arq Bras Oftalmol. 2012;75(5):348-51<br />
351
Relatos de Casos | Case Reports<br />
Síndrome de Waardenburg - aspectos <strong>of</strong>talmológicos e critérios de diagnóstico:<br />
relatos de casos<br />
Waardenburg syndrome - ophthalmic findings and criteria <strong>for</strong> diagnosis: case reports<br />
Luciano Sólia Nasser 1 , Lívia Maris Ribeiro Paranaíba 1 , Ana Cláudia Frota 2 , Andreia Gomes 3 , Gisele Versiani 4 , Hercílio Martelli Júnior 1<br />
RESUMO<br />
Objetivo: Descrever as características clínicas e imaginológicas de duas famílias com<br />
a síndrome de Waardenburg, sendo uma do tipo I e outra do tipo II, enfatizando as<br />
manifestações <strong>of</strong>talmológicas, bem como o padrão de herança genética.<br />
Método: Realizou-se um estudo clínico envolvendo as duas famílias afetadas pela sín -<br />
dro me de Waardenburg, sendo, através dos heredogramas, determinado o padrão de<br />
herança genética presente. Também <strong>for</strong>am realizadas análises <strong>of</strong>talmológicas abordando<br />
a me dida da acuidade visual, a presença de distopia cantorum (telecanto), a avaliação da<br />
coloração da íris e o mapeamento de retina, além de exames otológicos e dermatológicos.<br />
Resultados: O heredograma da família afetada pela síndrome de Waardenburg tipo I<br />
revelou um modo autossômico dominante de transmissão. A condição estava presente<br />
em 85,71% dos pacientes. A distopia cantorum foi a alteração mais frequente, seguida<br />
pela mecha branca na pele da fronte, hipopigmentação da íris e da retina e surdez<br />
neurossensorial. A família com síndrome de Waardenburg tipo II apresentou 33,33%<br />
dos familiares com a alteração. Nenhum membro apresentou distopia cantorum e<br />
hipopigmentação de íris. Três pacientes apresentaram surdez neurossensorial (12,5%),<br />
associada ao topete branco e manchas acrômicas confluentes pelo corpo.<br />
Conclusão: O presente estudo mostra a importância do <strong>of</strong>talmologista no auxílio do<br />
diagnóstico desta rara condição genética, uma vez que inclui alterações <strong>of</strong>talmológicas<br />
como telecanto, hipopigmentação da íris e retina. A distopia cantorum é o principal<br />
critério diagnóstico para diferenciar o tipo I do II e deve ser feita por <strong>of</strong>talmologista<br />
treinado. As famílias encontram-se em acompanhamento multipr<strong>of</strong>issional, tendo<br />
recebido orientações genéticas e os cuidados referentes à proteção ocular.<br />
Descritores: Síndrome de Waardenburg; Doenças da íris; Doenças retinianas; Acon -<br />
selhamento genético; Surdez; Pálpebras/anormalidades; Nariz/anormalidades; Relatos<br />
de casos<br />
ABSTRACT<br />
Purpose: To describe the clinical and imaginological features <strong>of</strong> two families with Waardenburg<br />
syndrome: type I and II, with emphasis on ophthalmic manifestations, as well as<br />
the pattern <strong>of</strong> genetic inheritance.<br />
Methods: We conducted a clinical study involving two families affected by Waardenburg<br />
syndrome, and through the pedigree, determined the present pattern <strong>of</strong> genetic inheritance.<br />
Analyses were per<strong>for</strong>med including the measurement <strong>of</strong> visual acuity, the presence <strong>of</strong><br />
dystopia cantorum (telecanthus), evaluation <strong>of</strong> iris color and retinal mapping, as well as<br />
dermatological and otological examinations.<br />
Results: The pedigree <strong>of</strong> the family affected by the Waardenburg syndrome type I showed<br />
an autosomal dominant mode <strong>of</strong> transmission. The syndrome was present at 85.71% <strong>of</strong><br />
patients. The dystopia cantorum was the most frequent feature, followed by the white<br />
streak on the skin <strong>of</strong> the <strong>for</strong>ehead, hypopigmentation <strong>of</strong> the iris and retina and deafness.<br />
The Waardenburg syndrome family type II had 33.33% <strong>of</strong> family members affected by<br />
the syndrome. No member had dystopia cantorum and hypopigmentation <strong>of</strong> the iris.<br />
Three patients had sensorineural hearing loss (12.5%), associated with white <strong>for</strong>elock and<br />
achromatic spots confluent by the body.<br />
Conclusion: This study shows the importance <strong>of</strong> the ophthalmologist in aiding the<br />
diagnosis <strong>of</strong> this rare genetic condition, since it includes ocular disorders such as telecanthus,<br />
hypopigmentation <strong>of</strong> the iris and retina. The cantorum dystopia is the main<br />
diagnostic criterion to differentiate type I and II syndrome and should be done by a trained<br />
ophthalmologist. The families are in medical monitoring, receiving genetic guidelines<br />
and care related to eye protection.<br />
Keywords: Waardenburg’s syndrome; Iris diseases; Retinal diseases; Genetic counseling;<br />
Deafness; Eyelids/abnormalities; Nose/abnormalities; Case reports<br />
INTRODUÇÃO<br />
Síndrome de Waardenburg (SW; MIM #193500) é uma alteração<br />
do sistema melanocítico-pigmetário resultante de uma desordem na<br />
diferenciação, sobrevivência e migração dos melanócitos derivados<br />
da crista cristal no período embriogênico (1) . A SW apresenta distribuição<br />
universal, sem predileção por raça e gênero e sua prevalência<br />
estimada é de 1:42.000 nativivos na população geral (2) .<br />
Análise histológica das estruturas afetadas na SW mostra ausência<br />
de melanócitos teciduais como na região frontal do cabelo<br />
(topete branco), pele, íris e estria vascular da cóclea (surdez neurosensorial)<br />
(3) . Além destas alterações de pigmentação, pode ocorrer a<br />
distopia cantorum ou telecanto, um deslocamento lateral dos cantos<br />
internos dos olhos (2) . Características menos frequentes associadas<br />
são, a presença de manchas acrômicas da pele, a confluência dos<br />
supercílios (sinófris) e uma base larga do nariz (4) . Diante desta diversidade<br />
clínica, <strong>for</strong>am propostos os critérios diagnósticos maiores para<br />
a SW: perda auditiva neurossensorial, alterações na pigmentação da<br />
íris, hipopigmentação do cabelo (topete branco ou cabelos grisalhos<br />
surgidos antes dos 30 anos de idade) e distopia cantorum, além de<br />
critérios menores: sinófris, hipopigmentação da pele e uma base larga<br />
do nariz (4-8) . Para ter a confirmação da SW o paciente deve apresentar<br />
dois critérios maiores e um menor (4) .<br />
Submetido para publicação: 26 de julho de 2012<br />
Aceito para publicação: 6 de outubro de 2012<br />
Trabalho realizado na Universidade Estadual de Montes Claros, Unimontes, Montes Claros, Minas<br />
Gerais, Brasil.<br />
1<br />
Programa de Pós-graduação em Ciências da Saúde, Universidade Estadual de Montes Claros,<br />
Unimontes, Montes Claros, Minas Gerais, Brasil.<br />
2<br />
Estudante de Medicina, Universidade Estadual de Montes Claros, Unimontes, Montes Claros,<br />
Minas Gerais, Brasil.<br />
3<br />
Estudante de Odontologia, Universidade Estadual de Montes Claros, Unimontes, Montes Claros,<br />
Minas Gerais, Brasil.<br />
4<br />
Departamento de Fonoaudiologia do Hospital Universitário Clemente de Faria da Universidade<br />
Estadual de Montes Claros, Unimontes, Minas Gerais, Brasil.<br />
Financiamento: Não houve financiamento para este trabalho.<br />
Divulgação de potenciais conflitos de interesse: L.S.Nasser, Nenhum; L.M.R. Paranaíba, Nenhum;<br />
A.C.Frota, Nenhum; A.Gomes, Nenhum; G.Versiani, Nenhum; H.Martelli.Jr., Nenhum.<br />
Endereço para correspondência: Luciano Sólia Násser. Rua Walter F. Barreto, 57 - Montes Claros<br />
(MG) 39401-347 - Brasil - E-mail: solianasser@gmail.com<br />
Comitê de Ética: Unimontes 2781/2011.<br />
352 Arq Bras Oftalmol. 2012;75(5):352-5
Nasser LS, et al.<br />
De acordo com a combinação dessas alterações clínicas, a SW<br />
é classificada em 4 tipos, SW1, SW2, SW3 e SW4. O tipo I (SW1; MIM<br />
#193500) é a <strong>for</strong>ma clássica com distopia cantorum, o tipo II (SW2;<br />
MIM #193510) caracterizado pela presença de tecidos com distúrbios<br />
de pigmentação e surdez, porém, sem a presença de distopia cantorum,<br />
o tipo III (síndrome de Klein-Waardenburg; MIM #148820) é<br />
similar ao tipo I com anormalidades musculoesqueléticas adicionais;<br />
enquanto o tipo IV (síndrome de Shah-Waardenburg ou doença de<br />
Waardenburg- Hirschsprung, MIM #277580) é caracterizada pela presença<br />
de megacolon congênito (4) . A tabela 1 mostra os critérios de<br />
diagnóstico para a SW.<br />
O objetivo do presente estudo foi descrever as características<br />
clínicas e imaginológicas em 2 famílias brasileiras com a SW (tipo I e<br />
tipo II), enfatizando as manifestações <strong>of</strong>talmológicas.<br />
MÉTODOS<br />
Família 1<br />
Paciente de 2 anos, masculino, procedente de Montes Claros,<br />
Mi nas Gerais, acompanhado de seus pais, apresentava surdez total<br />
bilateral desde o nascimento. Foi avaliado no departamento de <strong>of</strong>talmologia<br />
da Universidade Estadual de Montes Claros, Unimontes,<br />
Minas Gerais, Brasil, por apresentar queixa principal de fot<strong>of</strong>obia e os<br />
olhos extremamente claros. Ao exame clínico, observou-se uma mecha<br />
branca na região cutânea da fronte, uma mancha hipocrômica no<br />
braço direito, íris extremamente azuis e telecanto (Figura 1). Diante<br />
da clínica observada, o diagnóstico presuntivo foi de SW. Iniciou-se<br />
um estudo envolvendo toda a família do paciente, composta por 15<br />
membros nas últimas quatro gerações, para determinar o padrão de<br />
herança e a expressividade da doença (Figura 2).<br />
Os pacientes afetados tinham idade entre 2 e 55 anos (média de<br />
18,27 anos). A avaliação clínica incluiu anamnese e exame físico completo.<br />
O estudo <strong>of</strong>talmológico abordou a medida da acuidade visual,<br />
a presença de distopia cantorum (telecanto), a análise da coloração da<br />
íris e o mapeamento de retina com retinografia colorida (Figura 3). A<br />
medida da distopia cantorum foi obtida através do cálculo do índice W,<br />
resultante de uma análise envolvendo a medida de três pontos anatômicos<br />
entre os dois olhos, con<strong>for</strong>me a figura 4. A distopia está presente<br />
quando o índice W resulta em valor maior ou igual a 1,95 mm (4) .<br />
Exames otológicos envolveram otoscopia, impedanciometria e<br />
audiometria computadorizada. Análise de imagens, incluindo fotografias<br />
do telecanto, hipopigmentação da íris e retina (retinografia<br />
colorida), além de alterações na pigmentação do cabelo e pele <strong>for</strong>am<br />
realizadas.<br />
Família 2<br />
Paciente de 53 anos, feminino, procedente de Capitão Enéas, Minas<br />
Gerais, foi avaliada no mesmo Serviço da família 1, pois apresentava<br />
pterígio bilateral com crises de inflamação recorrente. A paciente<br />
apresentava uma mecha branca na região frontal, manchas acrômicas<br />
em membros inferiores e surdez moderada (Figura 1). Por meio de uma<br />
avaliação auditiva e uma audiometria, detectou-se a presença de surdez<br />
neurossensorial. Como a paciente não apresentava distopia cantorum,<br />
confirmou-se o diagnóstico de SW tipo II. Iniciou-se um estudo<br />
envolvendo toda a família da paciente, composta por 24 membros,<br />
nas últimas quatro gerações, para determinar o padrão de herança e a<br />
expressividade da doença (Figura 5).<br />
Os pacientes afetados tinham idade entre 4 e 53 anos (média<br />
de 25,3 anos). A avaliação clínica incluiu anamnese e exame físico.<br />
O estudo <strong>of</strong>talmológico abordou a medida da acuidade visual, presença<br />
de distopia cantorum (telecanto), análise da coloração da íris<br />
e mapea mento de retina. Exames otológicos envolveram otoscopia,<br />
impedanciometria e audiometria computadorizada. Análise de imagens,<br />
incluindo fotografias do telecanto e alterações na pigmentação<br />
do cabelo e pele <strong>for</strong>am realizadas.<br />
O estudo foi submetido e aprovado pelo Comitê de Ética Institucional.<br />
Consentimento in<strong>for</strong>mado, livre e esclarecido foi obtido de<br />
cada paciente ou seu responsável legal, antes da inclusão no estudo.<br />
Tabela 1. Critérios diagnósticos para a síndrome de Waardenburg<br />
tipos I e II<br />
Critérios maiores<br />
1-Distopia cantorum<br />
2-Alterações na pigmentação da íris<br />
3-Hipopigmentação do cabelo (topete<br />
branco ou cabelos grisalhos surgidos<br />
antes dos 30 anos de idade)<br />
Critérios menores<br />
1-Hipopigmentação da pele<br />
2-Confluência dos supercílios (sinófris)<br />
3-Base alta e alargada do nariz<br />
4- Perda auditiva neurossensorial 4-Hipoplasia das asas do nariz<br />
SW tipo I = Dois critérios maiores<br />
SW tipo II = Dois critérios maiores, exceto a distopia cantorum<br />
Read, Newton (4) . Waardenburg syndrome: syndrome <strong>of</strong> the month.<br />
A<br />
C<br />
Figura 1. Pacientes com síndrome de Waardenburg tipo I (A e B): notam-se iris extrememente<br />
azuladas, dystopia cantorum, sinófris e base alargada do nariz. Pacientes com<br />
SW tipo II (C e D): notam-se manchas acrômicas espalhadas pelo corpo e topete branco.<br />
Figura 2. Heredograma da família com síndrome de Waardenburg tipo I.<br />
B<br />
D<br />
Arq Bras Oftalmol. 2012;75(5):352-5<br />
353
Síndrome de Waardenburg - aspectos <strong>of</strong>talmológicos e critérios de diagnóstico: relatos de casos<br />
RESULTADOS<br />
Família 1<br />
O exame clínico das últimas quatro gerações da família revelou<br />
que dos 15 membros (4 homens e 11 mulheres), 11 (73,33%) apresentaram<br />
ca racterísticas da SW. Desses 11 pacientes, a distribuição por<br />
sexo foi de 3 (27,27%) masculino e 8 (72,72%) do feminino. Não havia<br />
história de consanguinidade na família. O heredograma da família revelou<br />
um padrão de transmissão autossômico dominante com penetrância<br />
incompleta e expressividade variável (Figura 2). Dez membros<br />
apresentaram dystopia cantorum. Desses 10, 2 apresentaram surdez<br />
neurossensorial, 6 hipopigmentação da íris confirmada por uma significativa<br />
hipoplasia do epitélio pigmentado observado no exame de<br />
biomicroscopia e 6 topete branco, caracterizando o tipo I da SW por<br />
possuírem dois critérios maiores, segundo Read, Newton (4) . Sinófris<br />
foi observado em 4 pacientes afetados pela síndrome. O probando<br />
foi submetido à cirurgia para implante coclear bilateral aos 2 anos e<br />
já responde a comandos verbais e fala com dicção compreensível.<br />
Todos os pacientes portadores de hipopigmentação da íris receberam<br />
óculos solares com filtro contra UV-A e UV-B, além da correção<br />
óptica, quando necessário.<br />
Figura 3. Retinografia do probando com síndrome de Waardenburg tipo I. Ob -<br />
ser va-se a intensa rarefação do epitélio pigmentado da retina.<br />
Família 2<br />
Nesta família, composta por 24 descendentes distribuídos em<br />
quatro gerações, características da SW estiveram presentes em 33,33%<br />
(6 homens e 2 mulheres) (Figura 1). A primeira geração foi considerada<br />
pelos relatos dos membros das gerações seguintes. Desses 8,<br />
a distribuição por sexo foi de 2 (25%) masculino e 6 (75%) feminino.<br />
Não havia história de consanguinidade na família. O heredograma da<br />
família revelou um padrão autossômico dominante (Figura 5). Ne nhum<br />
membro apresentou distopia cantorum. Três pacientes apresentaram<br />
surdez neurossensorial associada a topete branco e manchas acrômicas<br />
confluentes pelo corpo, caracterizando o tipo II da SW por possuírem<br />
dois critérios maiores e ausência de distopia, segundo alguns<br />
autores (5) . A probanda foi submetida a implante de prótese auditiva<br />
com recuperação dos limiares auditivos normais e à exérese do pterígio<br />
no olho esquerdo.<br />
Figura 4. Medidas oculares para o diagnóstico da distopia cantorum. Distância entre<br />
os cantos mediais (a), distância interpupilar (b), distância entre os cantos laterais (c).<br />
Cálculo: X= (a - 0,2119c - 3.909)/c;<br />
Y= (a - 0,2479b - 3.909)/b;<br />
Índice W= X+Y+ a/b.<br />
Partington MW (1964). Waardenburg`s syndrome and heterochromia iridum in a deaf<br />
school population (13) .<br />
Figura 5. Heredograma da família com síndrome de Waardenburg tipo II.<br />
DISCUSSÃO<br />
A SW é uma doença de distribuição universal, sem predileção para<br />
raça e gênero (4) . A prevalência estimada do tipo I foi de 1:42.000 na<br />
população geral e 1:143 (1,43%) em portadores de surdez congênita (4) .<br />
A SW apresenta um padrão de herança autossômica dominante com<br />
penetrância incompleta e expressividade variável, especialmente nos<br />
tipos I e II (9) . A expressiva heterogeneidade clinica da SW é atribuída a<br />
uma rede complexa de interação entre seis genes identificados até o<br />
momento: o gene PAX3, principal responsável pela SW tipo I e III, os<br />
genes MITF, SOX10 e SNAI2 na SW tipo II e os genes EDN3 e EDNRB na<br />
SW tipo IV. Todos esses seis genes estão envolvidos dentro de uma rede<br />
de interações que determinam falhas na embriogênese das células derivadas<br />
da crista neural e caracterizam a diversidade fenotípica da SW (1) .<br />
No presente estudo, relatou-se duas famílias, ambas do norte do<br />
estado de Minas Gerais. A primeira apresentou o padrão clínico tipo<br />
I, e segunda família, tipo II. A distopia cantorum é a característica mais<br />
comum da SW tipo I, podendo ter uma incidência de 99% nesse<br />
sub grupo (4) . Este deslocamento lateral do canto interno dos olhos se<br />
tornou o recurso diagnóstico mais confiável para classificação do tipo<br />
I, devido a sua elevada frequência (1) . Já a hipertricose medial das sobrancelhas<br />
(sinófris) é mais frequente no tipo I (85%) do que no tipo II<br />
(25%) (5) . A família com SW tipo I apresentou 78,57% dos seus membros<br />
com distopia cantorum e 28,57% deles com sin<strong>of</strong>ris. A segunda família,<br />
<strong>for</strong>mada por indivíduos com a SW tipo II, apresentou um padrão de<br />
transmissão autossômica dominante com penetrência incompleta e<br />
expressividade variável. Nenhum membro desta família apresentou<br />
distopia cantorum e hipopigmentação da íris.<br />
354 Arq Bras Oftalmol. 2012;75(5):352-5
Nasser LS, et al.<br />
A heterocromia de íris pode ser completa ou parcial (5) . Na parcial,<br />
existe a presença de cores diferentes em um mesmo olho. Alguns<br />
autores encontraram heterocromia parcial em 4,2% dos indivíduos<br />
com SW tipo I e em 27,5% dos indivíduos com SW tipo II (5) . Ohno et al.,<br />
descreveram a presença de heterocromia de íris completa ou parcial<br />
em 30% dos indivíduos com SW tipo I e II (10) . Iris extremamente azul bilateralmente<br />
pode fazer parte do quadro ocular em 10% de todos os<br />
pacientes com diagnóstico de SW e esta coloração é devido à intensa<br />
hipoplasia do seu epitélio pigmentado (1) . No presente estudo, hipopigmentação<br />
da íris esteve presente em 42,85% na família com SW<br />
tipo I. Uma característica desta alteração é que a hipopigmentação da<br />
íris se apresentou simetricamente entre os dois olhos e no probando<br />
com SW tipo I <strong>for</strong>am observadas íris extremamente azuladas (Figura<br />
1). Neste paciente foi observada uma significativa rarefação e mobilização<br />
do epitélio pigmentado da retina nos dois olhos, alteração<br />
descrita na literatura e que geralmente correspondente ao mesmo<br />
território alterado na íris (10) .<br />
A perda auditiva na SW é neurossensorial, de caráter congênito,<br />
não progressivo, podendo ser uni ou bilateral e variar em níveis de intensidade<br />
(4) . Outros autores, encontraram uma penetrância de perda<br />
auditiva neurossensorial na SW tipo I de 69% e de 87% na SW tipo II (11) .<br />
A hipoacusia decorre de uma degeneração cocleossacular e ausência<br />
completa de pigmentação na estria vascular da cóclea culminando<br />
em uma atr<strong>of</strong>ia do órgão de Corti (3,12) . No presente estudo a surdez<br />
neurossensorial esteve presente em 14,28% dos indivíduos com SW<br />
tipo I e em 12,50% na família com SW tipo II.<br />
Em relação à mecha branca frontal, esta pode estar presente<br />
desde o nascimento ou surgir na primeira infância, como também<br />
pode desaparecer com a idade adulta (4) . Pingault et al., relatam que a<br />
alteração da cor dos cabelos está presente em pelo menos um terço<br />
dos tipos I e II (1) . No presente estudo o topete branco esteve presente<br />
em 50% na família com SW tipo I e 29,16% na SW tipo II.<br />
A expressividade da SW varia amplamente na literatura, sendo<br />
apresentada de <strong>for</strong>ma diferente em cada família acometida. Na<br />
avaliação das famílias apresentadas neste estudo <strong>for</strong>am encontradas<br />
características clínicas diferentes na <strong>for</strong>ma de apresentação e nas<br />
suas prevalências. Por exemplo, a penetrância de distopia cantorum<br />
e hipopigmentação da íris <strong>for</strong>am expressivas na família com SW tipo<br />
I (78,57 e 50%, respectivamente), mas a perda auditiva foi limitada<br />
(14,28%) e observada apenas em dois indivíduos (III-6 e IV-7) dos 14<br />
membros da família. Na família com SW tipo II, não <strong>for</strong>am observadas<br />
alterações <strong>of</strong>talmológicas, apenas surdez e manchas hipocrômicas<br />
no cabelo e na pele.<br />
A presença de alterações <strong>of</strong>talmológicas na SW tipo I exige uma<br />
abordagem <strong>of</strong>talmológica direcionada a todos os membros da família<br />
baseada na prevenção de doenças oculares e na reabilitação visual<br />
destes pacientes com deficiência de pigmentação em dois tecidos de<br />
suma importância na fisiologia visual, a íris e a retina. Todos os pacientes<br />
<strong>for</strong>am submetidos a exame refracional e receberam a prescrição da<br />
correção. Nos casos de emetropia, <strong>for</strong>am indicados óculos solares com<br />
filtros contra os raios ultravioletas.<br />
CONCLUSÃO<br />
O presente estudo mostra a importância do <strong>of</strong>talmologista no<br />
auxílio do diagnóstico deste raro quadro sistêmico, uma vez que inclui<br />
alterações <strong>of</strong>talmológicas como distopia cantorum, hipopigmentação<br />
da íris e da retina. A distopia cantorum é o principal critério diagnóstico<br />
para diferenciar o tipo I do II e deve ser feita por <strong>of</strong>talmologista treinado.<br />
Aconselhamento genético e cuidados para proteger um olho com<br />
deficiência de pigmentação na íris e na retina <strong>for</strong>am <strong>of</strong>erecidos aos<br />
pacientes. Investigações envolvendo amostras maiores, com enfoque<br />
em bases genéticas e moleculares são necessárias para elucidar as consequências<br />
destas alterações clínicas e melhorar nossa compreensão<br />
sobre os mecanismos envolvidos nesta patologia, a fim de podermos<br />
<strong>of</strong>erecer um aconselhamento genético criterioso e um tratamento<br />
mais completo aos pacientes.<br />
REFERÊNCIAS<br />
1. Pingault V, Ente D, Dastoto-Le Moal F, Goossens M, Marlin S, Bondurand N. Review<br />
and update <strong>of</strong> mutations causing Waardenburg syndrome. Human Mutat. 2010;31(4):<br />
391-406.<br />
2. Waardenburg PJ. A new syndrome combining developmental anomalies <strong>of</strong> the<br />
eyelids, eyebrowns and nose root with pigmentary defects <strong>of</strong> the iris and head hair<br />
and with congenital deafness. Am J Hum Genet. 1951;3(3):195-253.<br />
3. Nakashima S, Sando I,Takahashi H, Hashida Y. Temporal bone histopathologic findings<br />
<strong>of</strong> the Waardenburg`s syndrome: a case report. Laryngoscope. 1992;102(5):563-67.<br />
4. Read AP, Newton VE. Waardenburg syndrome. J Med Genet. 1997;34(8):656-65.<br />
5. Liu XZ, Newton VE, Read AP. Waardenburg syndrome type 2: phenotypic findings and<br />
diagnostic criteria. Am J Med Genet. 1995;55(1):95-100.<br />
6. Farrer LA, Grundfast KM, Amos J, Arnos KS, Asher JH Jr, Beithton P, et al. Waardenburg<br />
syndrome (WS) tipe 1 is caused by defects at multiple loci, one <strong>of</strong> which is near ALPP<br />
on chromosome 2: first report <strong>of</strong> the WS Consortium. Am J Hum Genet. 1992;50(5):<br />
902-13.<br />
7. Hageman MJ, Delleman JW. Heterogeneity in Waardenburg syndrome. Am J Hum<br />
Genet. 1977;29(5):468-85.<br />
8. Fraser Gr. The cause <strong>of</strong> pr<strong>of</strong>ound deafness in childhood. Baltimore: John Hopkins<br />
University Press; 1976<br />
9. Arias S. Genetic heterogeneity in the Waardenburg syndrome. Birth Defects Orig Artic<br />
Ser. 1971;7(4):87-101.<br />
10. Ohno N, Kiyosawa M, Wang WF, Takase H, Mochizuki M. Clinical findings in Japanese<br />
patients with Waardenburg syndrome type 2. Jpn J Ophthalmol. 2003;47(1):77-84.<br />
11. Newton VE, Read AP. Waardenburg Syndrome. Audiol Med. 2003;1(1):77-88.<br />
12. Steel KP, Barkway C. Another role <strong>for</strong> melanocytes: their importance <strong>for</strong> normal stria vas -<br />
cularis development in the mammalian inner ear. Development. 1989;107(3):453-63.<br />
13. Partington MW. Waardenburg`s syndrome and heterochromia iridum in a deaf school<br />
population. Can Med Assoc J. 1964;90:1008-17.<br />
Arq Bras Oftalmol. 2012;75(5):352-5<br />
355
Relato de Caso | Case Report<br />
Optical coherence tomography image in gelatinous drop-like corneal dystrophy:<br />
case report<br />
Tomografia de coerência óptica na distr<strong>of</strong>ia corneana gelatinosa em gotas: relato de caso<br />
Otávio de Azevedo Magalhães¹, Samuel Rymer 2 , Diane Ruschel Marinho 2 , Sérgio Kwitko 2 , Isabel Habeyche Cardoso 3 , Lúcia Kliemann 4<br />
ABSTRACT<br />
Gelatinous drop-like corneal dystrophy is a rare disorder with few cases described<br />
in the present literature. The following report will show how difficult it is to<br />
diagnose this disease in early stages. Modern image exams, such as optical co -<br />
he rence tomography helps to diagnose and can be crucial to establish the best<br />
treatment. We will present the histopathological changes and clinical features in<br />
this unusual dystrophy.<br />
Keywords: Corneal dystrophies, hereditary/diagnosis; Tomography, optical coheren -<br />
ce/methods; Corneal opacity; Case report; Humans; Child<br />
RESUMO<br />
A distr<strong>of</strong>ia corneana gelatinosa em gotas é uma desordem rara e pouco descrita em<br />
nossa literatura. O caso apresentado demonstra a dificuldade de realizar o diagnóstico<br />
nas fases mais iniciais da doença. O uso de modernos exames de imagem, como a<br />
to mografia de coerência óptica de segmento anterior, auxilia no diagnóstico e pode<br />
ser crucial para definir a melhor conduta terapêutica. Apre sentaremos as alterações<br />
histopatológicas e as características clínicas desta incomum distr<strong>of</strong>ia.<br />
Descritores: Distr<strong>of</strong>ias hereditárias da córnea/diagnóstico; Tomografia de coerência<br />
óptica/métodos; Opacidade da córnea; Relato de caso; Humanos; Criança<br />
INTRODUCTION<br />
Gelatinous drop-like corneal dystrophy is a rare disorder also<br />
known as primary familial amyloidosis <strong>of</strong> the cornea (1) . It usually<br />
occurs in the first decade <strong>of</strong> life and its clinical appearance can simulate<br />
other diseases such as band keratopathy (2) . Symptoms include<br />
photophobia, tearing and poor vision. Bilateral corneal opacification<br />
increases with age. Microscopic findings include subepithelial deposits<br />
that resemble a mulberry shape without any inflammatory<br />
component. The genetic inheritance pattern is not well established (3) ,<br />
but it is believed to be autosomal recessive. Bowman’s membrane<br />
can be absent at the histopathological analysis and characteristic<br />
ap ple-green birefringence is viewed in polarized light (4) .<br />
CASE REPORT<br />
A five-year-old girl was referred to our Cornea and External Disea -<br />
se Department because <strong>of</strong> bilateral corneal opacity and low vision.<br />
Her past medical history was negative <strong>for</strong> any systemic disease, trauma<br />
or prenatal disorders. Similar findings were found in her 8-year-old<br />
brother, who had the same biomicroscopic characteristic but milder<br />
symptoms. Her best corrected visual acuity was counting fingers at<br />
1 meter in both eyes. Slit lamp examination revealed a total lack <strong>of</strong><br />
transparency, epithelial edema with bubbles and a thin layer <strong>of</strong> calcification<br />
(Figure 1). The main initial diagnostic hypothesis was congenital<br />
hereditary endothelial dystrophy (CHED) and a penetrating<br />
keratoplasty (PK) was indicated in the right eye. Histopathological<br />
analysis revealed amyloid nodules in the subepithelial layer and in the<br />
anterior portion <strong>of</strong> the corneal stroma that stained with Congo Red<br />
(Figure 2) and <strong>for</strong>med apple-green birefringence when combined<br />
with polarized light (Figure 3). Bowman’s membrane was absent, there<br />
was no significant posterior stromal edema and Descemet´s membrane<br />
was normal. Histopathological findings were consistent with<br />
the diagnosis <strong>of</strong> gelatinous drop-like corneal dystrophy and showed<br />
that our first hypothesis <strong>of</strong> CHED was mistaken. Optical Coherence<br />
Tomography (OCT - Optovue Fourier-Domain System ® ) was per<strong>for</strong>med<br />
in the opposite eye that had the same clinical appearance. This exam<br />
showed increased anterior reflectivity with nodules measuring about<br />
327 microns in thickness. Total central corneal width was 1070 microns.<br />
There were no significant changes in the posterior stroma and<br />
Descemet’s membrane (Figure 4).<br />
DISCUSSION<br />
There are few descriptions <strong>of</strong> this type <strong>of</strong> dystrophy and no reports<br />
<strong>of</strong> anterior OCT images. Had we per<strong>for</strong>med a corneal OCT exam<br />
be<strong>for</strong>e PK <strong>of</strong> the right eye, we could have made a different surgical<br />
approach since the OCT showed only anterior stromal alterations.<br />
Submitted <strong>for</strong> publication: June 12, 2012<br />
Accepted <strong>for</strong> publication: July 27, 2012<br />
Study carried out at the Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Gran de<br />
do Sul.<br />
1<br />
Physician, Setor de Córnea e Doenças Externas, Serviço de Oftalmologia, Hospital de Clínicas de<br />
Porto Alegre, Universidade Federal do Rio Grande do Sul - UFRS - Porto Alegre (RS), Brasil.<br />
2<br />
Physician, Serviço de Oftalmologia, Hospital de Clínicas de Porto Alegre, Universidade Federal do<br />
Rio Grande do Sul - UFRS - Porto Alegre (RS), Brasil.<br />
3<br />
Physician, Porto Alegre (RS), Brasil.<br />
4<br />
Physician, Serviço de Patologia, Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio<br />
Grande do Sul - UFRS - Porto Alegre (RS), Brasil.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: O.A.Magalhães, employee <strong>of</strong> Hospital Nossa Senhora<br />
da Conceição; S.Rymer, None; D.R.Marinho, employee <strong>of</strong> Hospital de Clínicas de Porto Alegre;<br />
S.Kwitko, None; I.H.Cardoso, None; L.Kliemann,<br />
Correspondence address: Otávio de Azevedo Magalhães. Rua Mostardeiro, 333/401 - Porto Alegre<br />
(RS) - 90430-001 - Brazil - E-mail: otaviomaga@yahoo.com.br<br />
356 Arq Bras Oftalmol. 2012;75(5):356-7
Magalhães OA, et al.<br />
Figure 1. Gelatinous drop-like dystrophy biomicroscopic findings - grayish, mulberry-like<br />
and protruding subepithelial deposits.<br />
Figure 3. Apple-green birefringence when viewed with polarized light.<br />
Figure 2. Red Congo stain showing anterior amyloid nodular deposits.<br />
Figure 4. OCT image showing hypereflective nodular <strong>for</strong>mation in the anterior corneal<br />
layer.<br />
During the diagnostic investigation, it is essential to use this kind <strong>of</strong><br />
technology. That way, invasive procedures with high rates <strong>of</strong> rejection<br />
can be avoided. Anterior lamellar procedures or phototherapeutic<br />
keratectomy (PTK) (5) can be better options <strong>for</strong> this disease.<br />
REFERENCES<br />
1. Nakaizumi K. A rare case <strong>of</strong> corneal distrophy. Acta Soc Ophthal Jpn. 1914;18:949-50.<br />
2. Kanai A, Kaufman HE. Electron microscopic studies <strong>of</strong> primary band-shaped keratopathy<br />
and gelatinous drop-like corneal dystrophy in two brothers. Ann Ophthalmol.<br />
1982;14(6):535-9.<br />
3. Kawasaki S, Kinoshita S. Clinical and basic aspects <strong>of</strong> gelatinous drop-like corneal<br />
dys trophy. Dev Ophthalmol. 2011;48:97-115.<br />
4. Garner A. Amyloidosis <strong>of</strong> the cornea. Br J Ophthalmol. 1969;53(2):73-81.<br />
5. Ito M, Takahashi J, Sakimoto T, Sawa M. [Histological study <strong>of</strong> gelatinous drop-like<br />
dys trophy following excimer laser phototherapeutic keratectomy]. Nihon Ganka<br />
Gakkai Zasshi. 2000;104(1):44-50. Japanese.<br />
Arq Bras Oftalmol. 2012;75(5):356-7<br />
357
Relato de Caso | Case Report<br />
Esclerite posterior associada à oclusão da veia central da retina<br />
e edema macular cistoide: relato de caso<br />
Posterior scleritis associated with central retinal vein occlusion and cystoid macular edema: case report<br />
Roger Wada Kamei 1<br />
RESUMO<br />
Apresentamos um caso de esclerite posterior associada à oclusão da veia central<br />
da retina e edema macular cistoide. Com esse caso, observamos como a doença<br />
pode ser agressiva e como a acuidade visual pode ser comprometida. No entanto,<br />
o tratamento correto pode melhorar as alterações oculares com melhora visual.<br />
Aler tamos também para os cuidados que devem ser tomados em relação ao uso<br />
de altas doses de corticosteroides.<br />
Descritores: Esclerite/quimioterapia; Oclusão da veia retiniana; Edema macular;<br />
Uveítes; Angi<strong>of</strong>luoresceinografia; Metilprednisolona/uso terapêutico; Relato de caso;<br />
Humanos; Idoso; Feminino<br />
ABSTRACT<br />
A case <strong>of</strong> posterior scleritis associated with central retinal vein occlusion and cystoid<br />
macular edema is reported. With this case, we noticed how the disease can be aggressive<br />
and how the visual acuity can be compromised. However, the correct treatment can<br />
improve the ocular changes with visual improvement. We also alert to the care with the<br />
use <strong>of</strong> high doses <strong>of</strong> corticosteroids.<br />
Keywords: Scleritis/drug therapy; Retinal vein occlusion; Macular edema; Uveitis;<br />
Fluo rescein angiography; Methylprednisolone/therapeutic use; Case report; Humans;<br />
Aged; Female<br />
INTRODUÇÃO<br />
A esclerite posterior é uma <strong>for</strong>ma rara de esclerite que, apesar<br />
da sua grande morbidade, apresenta uma grande dificuldade no seu<br />
diagnóstico. Definida como um processo inflamatório da esclera posterior<br />
até a ora serrata com sintomas que, frequentemente, simulam<br />
outras condições, sendo uma doença pouco diagnosticada (1-3) .<br />
Como em outras <strong>for</strong>mas de esclerites, a dor é um sintoma importante<br />
e a visão pode ser gravemente afetada. Além do quadro<br />
clínico, a ecografia B mostra-se de grande utilidade para confirmar o<br />
diagnóstico, achados ecográficos são muito comuns e fundamentais<br />
para o acompanhamento desses casos (1,2) , principalmente quando<br />
não há sinais fundoscópicos.<br />
Em geral acomete mais mulheres (60 a 70%) que homens, entre<br />
40 e 59 anos, sendo bilateral em 5% dos casos e com recorrências<br />
frequentes. Podendo estar associada à esclerite anterior em 43,5%,<br />
principalmente na <strong>for</strong>ma difusa (4-6) .<br />
A esclerite posterior pode ser idiopática ou estar associada a uma<br />
doença sistêmica em até 40% dos casos. Causas infecciosas podem<br />
estar presentes, como herpes zoster, herpes simples, tuberculose e<br />
sí filis. Porém, a artrite reumatóide é descrita como sendo a associação<br />
mais comum. Outras vasculites sistêmicas como granulomatose de<br />
Wegener também podem ser uma causa (7,8) .<br />
O tratamento depende do diagnóstico correto e, em casos mais<br />
graves e não responsivos ao tratamento convencional com drogas<br />
anti-inflamatórias, pode ser necessário o uso de drogas imunossupressoras<br />
para o controle do quadro ocular (9,10) .<br />
Uma abordagem multidisciplinar desses casos, muitas vezes, é<br />
necessária. Sendo uma avaliação clínica geral e uma investigação<br />
laboratorial precoce de extrema importância. O encaminhamento<br />
para o reumatologista é aconselhável para cooperação no diagnóstico<br />
e tratamento.<br />
O processo inflamatório escleral pode ser potencialmente devastador.<br />
O não reconhecimento e não tratamento dessa condição pode<br />
comprometer a visão de maneira rápida e irreversível.<br />
RELATO DE CASO<br />
A.M.B., sexo feminino, 71 anos. Iniciou quadro de baixa acuidade<br />
visual (AV), hiperemia e dor no olho direito (OD) há dois meses, desde<br />
então, com diagnóstico e tratamento de conjuntivite. Referia ser<br />
“pré-diabética” controlada com dieta, sem uso de medicação hipoglicemiante.<br />
Negava hipertensão arterial sistêmica e trauma.<br />
A AV era de movimentos de mãos frente os olhos em OD e de<br />
20/25 em OE. À biomicroscopia, o OD apresentava quadro de esclerite<br />
anterior difusa, com grande congestão dos vasos episclerais superficiais<br />
e pr<strong>of</strong>undos, ausência de reação de câmara anterior (RCA),<br />
pressão intraocular normal e pseud<strong>of</strong>acia sem complicações. O olho<br />
esquerdo (OE) mostrava-se sem alterações.<br />
A fundoscopia do OD (Figura 1) mostrava um descolamento<br />
se roso da retina com descolamento periférico da coroide e ausência<br />
de roturas retinianas. O vítreo estava claro com raras células<br />
in flamatórias. Havia um edema do disco óptico importante com<br />
si nais compatíveis com oclusão da veia central da retina (OVCR)<br />
com he morragias retinianas superficiais, dilatação e ingurgitamento<br />
ve noso significativo, alguns exsudatos algodonosos e mácula sem<br />
edema. OE normal.<br />
Submetido para publicação: 21 de março de 2012<br />
Aceito para publicação: 9 de outubro de 2012<br />
Trabalho realizado no Instituto Penido Burnier.<br />
1<br />
Médico, Setor de Retina e Vítreo, Uveítes e AIDS, Instituto Penido Burnier, Campinas (SP), Brasil.<br />
Financiamento: Não houve financiamento para este trabalho.<br />
Divulgação de potenciais conflitos de interesse: R.Kamei, Nenhum.<br />
Endereço para correspondência: Roger Kamei. Rua Coelho Neto, 15 - Apto. 54 - Campinas (SP) -<br />
13023-020 - Brasil - E-mail: rwkamei@gmail.com<br />
358 Arq Bras Oftalmol. 2012;75(5):358-60
Kamei RW<br />
O ultrassom mostrava um vítreo pouco acometido e sem trações<br />
vitreorretinianas anormais, descolamento de coroide periférico, descolamento<br />
seroso da retina e edema do disco óptico perceptível ao<br />
exame. A coroide apresentava um espessamento importante e difuso<br />
sem, no entanto, apresentar acúmulo de líquido no espaço subtenoniano.<br />
Não foi observado o característico “sinal do T invertido”. O<br />
exame também afastou a presença de massas e demais alterações<br />
da parede ocular.<br />
A angi<strong>of</strong>luoresceinografia (AGF) mostrava o grande comprometimento<br />
vascular retiniano e ausência de edema macular (Figura 2).<br />
Neste momento, <strong>for</strong>am solicitados exames laboratoriais infecciosos<br />
e reumatológicos, assim como uma avaliação clínica para liberação<br />
para pulsoterapia com metilprednisolona endovenosa por três<br />
dias consecutivos. Os exames laboratoriais mostraram negatividade<br />
para toda a investigação sorológica e as condições clínicas da paciente<br />
permitiram a realização da pulsoterapia. O tratamento foi realizado<br />
em regime de internação hospitalar e monitorização clínica.<br />
Com a medicação endovenosa, obteve-se resolução total do des -<br />
colamento da coroide e parcial do descolamento seroso da retina.<br />
Sendo programada a manutenção do tratamento com prednisona<br />
oral 1 mg/kg/dia, porém os índices glicêmicos da paciente se elevaram<br />
para valores acima de 300 mg/dL. Assim, permaneceu internada<br />
para controle da glicemia por 20 dias, tendo alta com uso de insulina<br />
diária três vezes ao dia e hipoglicemiantes orais, mantendo glicemia<br />
de 200 mg/dl e 20 mg de predinisona por dia. Neste momento, OD<br />
estava com a retina totalmente colada, mantendo o edema do disco<br />
óptico e melhora parcial dos sinais da OVCR, porém com AV de 20/200.<br />
Com a realização da tomografia de coerência óptica (OCT) e<br />
nova AGF, notou-se um edema macular de 1.075 µm na área central<br />
(Figu ra 4), também evidenciado pelo exame angiográfico.<br />
Devido às condições clínicas da paciente, optou-se pelo tratamento<br />
do edema macular com aplicação de corticosteroide intraocular<br />
de acetato de triancinolona. Após a realização de duas injeções com<br />
intervalo de 40 dias, o edema macular apresentou completa resolução<br />
(245 µm) e a AV melhorou para 20/25. Ao final, a retina estava totalmente<br />
colada, sem edema do disco óptico e sinais de OVCR (Figura 3).<br />
CONCLUSÃO<br />
Com esse relato, podemos perceber como a esclerite posterior<br />
pode ser agressiva e exigir um tratamento intenso a base de corticosteroide.<br />
No entanto, essa condição pode ser erroneamente diagnosticada<br />
e levar a sérias complicações decorrentes da inflamação ocular.<br />
Em relação ao tratamento com corticosteroides, nota-se um gran -<br />
de cuidado principalmente em pacientes idosos e com comorbidades.<br />
Atenção especial deve ser dada à diabetes melito e hipertensão<br />
arterial sistêmica. Nesses casos, pode-se pensar em outras opções<br />
de tratamento, como a aplicação intra e peri-ocular e imunossupres-<br />
Figura 1. Retinografia colorida do OD inicial.<br />
Figura 3. Retinografia colorida do OD após tratamento.<br />
OCT inicial<br />
Após primeira injeção<br />
Após segunda injeção<br />
Figura 2. Angi<strong>of</strong>luoresceinografia do OD.<br />
Figura 4. Evolução do edema macular pelo OCT durante o tratamento.<br />
Arq Bras Oftalmol. 2012;75(5):358-60<br />
359
Esclerite posterior associada à oclusão da veia central da retina e edema macular cistoide: relato de caso<br />
sores sistêmicos. Dessa <strong>for</strong>ma, uma abordagem multidisciplinar com<br />
um reumatologista e um clínico geral é de extrema importância para<br />
o manejo da medicação e acompanhamento desses casos.<br />
Apesar do quadro agressivo que a esclerite posterior pode proporcionar,<br />
o correto tratamento com altas doses de corticosteroides<br />
pode apresentar grande melhora e até resolução das alterações<br />
oculares.<br />
Percebe-se, assim, a importância do diagnóstico precoce e pron to<br />
tratamento da esclerite posterior. Sendo uma condição grave, onde<br />
medicações sistêmicas e uma abordagem multidiscipli nar podem ser<br />
necessárias para uma melhor resposta do quadro inflamatório ocular.<br />
REFERÊNCIAS<br />
1. McCluskey PJ, Watson PG, Lightman S, Haybittle J, Restori M, Branley M. Posterior<br />
scleritis: clinical features, systemic associations, and outcome in a large series <strong>of</strong> pa -<br />
tients. Ophthalmology. 1999;106(12):2380-6.<br />
2. Benson WE. Posterior scleritis. Surv Ophthalmol. 1988;32(5):297-316.<br />
3. Machado DO, Curi AL, Bessa TF, Campos WR, Oréfice F. Esclerite posterior: características<br />
clínicas, associação sistêmica, tratamento e evolução de 23 pacientes. Arq Bras<br />
Oftalmol. 2009;72(3):321-6.<br />
4. Parra AG, Miyazaki FH, Ribeiro RM, Gehlen ML, Skare, T. Análise de 29 casos de<br />
esclerite. Experiência de um serviço de Reumato-Oftalmologia. Arq Bras Oftalmol.<br />
2010;73(3):250-3.<br />
5. Machado DO, Curi AL, Fernandes RS, Bessa TF, Campos WR, Oréfice F. Esclerite: características<br />
clínicas, associação sistêmica, tratamento e evolução de 100 pacientes. Arq<br />
Bras Oftalmol. 2009;72(2):231-5.<br />
6. La Maza MS, Molina N, Gonzalez-Gonzalez LA, Doctor PP, Tauber J, Foster CS. Clinical<br />
characteristics <strong>of</strong> a large cohort <strong>of</strong> patients with scleritis and episcleritis. Ophthalmology<br />
2012;119(1):43-50. Comment in: Ophthalmology. 2012;119(8):1715-1715.e.1.<br />
7. Raiji VR, Palestine AG, Parver DL. Scleritis and systemic disease association in a com -<br />
munity-based referral practice. Am J Ophthalmol. 2009;148(6):946-50.<br />
8. Akpek EK, Thorne JE, Qazi FA, Do DV, Jabs DA. Evaluation <strong>of</strong> patients with scleritis <strong>for</strong><br />
systemic disease. Ophthalmology. 2004;111(3):501-6. Comment in: Ophthalmology.<br />
2007;114(6):1232.<br />
9. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and<br />
treatment results. Am J Ophthalmol. 2000;130(4):469-76.<br />
10. Doctor P, Sultan A, Syed S, Christen W, Bhat P, Foster CS. Infliximab <strong>for</strong> the treatment<br />
<strong>of</strong> refractory scleritis. Br J Ophthalmol. 2010;94(5):579-83.<br />
Mais in<strong>for</strong>mações em: http://www.<strong>of</strong>talmo.epm.br/simasp2013<br />
360 Arq Bras Oftalmol. 2012;75(5):358-60
Relato de Caso | Case Report<br />
Buphthalmos development in adult: case report<br />
Buftalmus em adulto: relato de caso<br />
Mônica Alves 1 , Leonardo Tannus Malki 1 , Eduardo Melani Rocha 1<br />
ABSTRACT<br />
To report a case <strong>of</strong> extensive globe enlargement due to secondary glaucoma in<br />
a young adult suffering from ocular surface disorders related to hypohidrotic<br />
ectodermal dysplasia. To the best <strong>of</strong> our knowledge, this is the first report <strong>of</strong> bu -<br />
phthalmos in the adulthood.<br />
Keywords: Hydrophthalmos; Ectodermal dysplasia 1, anhidrotic; Dry eye syndromes;<br />
Case report; Humans; Male; Adult<br />
RESUMO<br />
Relato de caso do aumento extenso do globo ocular decorrente de glaucoma secundário<br />
e disfunção de superfície ocular em um paciente adulto jovem portador de displasia<br />
ectodérmica anidrótica. Primeiro relato de caso de buftalmo em adulto.<br />
Descritores: Hidr<strong>of</strong>talmos; Displasia ectodérmica anidrótica tipo 1; Síndromes do olho<br />
seco; Relato de caso; Humanos; Masculino; Adulto<br />
INTRODUCTION<br />
The growth <strong>of</strong> the human eye occurs more extensively in the postnatal<br />
period and is limited to the initial five years (1) . Anomalous growth<br />
is called buphthalmos and is related to high intraocular pressure in the<br />
initial months <strong>of</strong> life (2) .<br />
Gordon et al., in a cross-sectional study including premature, fullterm<br />
newborns and patients from 2 months to 36 years old, showed<br />
the progressive changes during the first years <strong>of</strong> life. According to their<br />
results, the main increase in axial length occurs until the age <strong>of</strong> 4, then<br />
slows to 0.4 mm/year and after 5 years <strong>of</strong> age, it grows approximately<br />
only 1 mm to its final length in adulthood. No significant increase in<br />
human eye length is expected after 10-15 years <strong>of</strong> age (1,3) .<br />
The term buphthalmos is used to describe a visible enlargement<br />
<strong>of</strong> the globe at birth or soon thereafter, mostly due to congenital glaucoma.<br />
The name buphthalmos comes from the Greek meaning “oxeyed“<br />
and its first <strong>for</strong>mal mention is uncertain and could have been<br />
used to highlight clinical diagnoses made by the simple inspection a<br />
large globe. Historically, it was just after the 19 th century with the invention<br />
<strong>of</strong> the ophthalmoscope and the tonometer that the etiology<br />
<strong>of</strong> the buphthalmos was related to glaucoma and its distinction <strong>of</strong><br />
the normally sized protuding globe and other <strong>for</strong>ms eye enlargement<br />
were consistently made (2) .<br />
We report a case <strong>of</strong> extensive globe enlargement due to secondary<br />
glaucoma in a young adult suffering from ocular surface disorders<br />
related to hypohidrotic ectodermal dysplasia. To the best <strong>of</strong> our knowledge,<br />
this is the first report <strong>of</strong> buphthalmos in adulthood.<br />
CASE PRESENTATION<br />
A 17-year-old caucasian male patient was referred <strong>for</strong> evaluation<br />
<strong>of</strong> painful ocular surface disorders and uncontrolled and progressive<br />
secondary glaucoma. He had been diagnosed with hypohidrotic<br />
ectodermal dysplasia in childhood, based on sparse, fine hair, brow<br />
and eyelashes hypotrichosis, poor tolerance to heat due to low ability<br />
to sweat. At birth his eyes were normal and he developed normal<br />
visual acuity. However, he had a long-term history <strong>of</strong> ocular irritation<br />
and frequent use <strong>of</strong> topical corticosteroids, antibiotics, lubricants and<br />
subsequently antiglaucoma medications.<br />
At an ophthalmological evaluation he presented poor visual<br />
acuity and dry eye, indicated by tear film instability, low Schirmer test<br />
measurements, corneal opacities and peripheral neovacularization<br />
and punctate keratitis in both eyes (4) . In addition, the patient presented<br />
a 3 mm epithelial defect in his left eye (OS) and subcapsular cataract<br />
OU. The average intraocular pressure (IOP) was 46 mmHg in the<br />
right eye (5) and 30 mmHg in OS, with advanced disc cup in both eyes<br />
despite maximum topical antiglaucoma therapy. A trabeculectomy<br />
was per<strong>for</strong>med in OD, with severe wound healing problems during<br />
the follow-up (Figure 1A).<br />
After six years <strong>of</strong> follow-up, the ocular surface disorders were<br />
properly controlled with preservative free lubricants and autologous<br />
serum applications. The extensive and prolonged use <strong>of</strong> preserved<br />
antiglaucoma eyedrops contributed to ocular irritation, reducing<br />
tolerance and compliance to treatment. Once the high IOP persisted<br />
in OS, we observed an enlargement <strong>of</strong> the globe, from 31mm in 2003<br />
to more than 36 mm <strong>of</strong> axial length in 2010 (Figures 1B and D). The<br />
OS evolved to no light perception which, combined with patient<br />
dissatisfaction with the facial aspect, eventually led to OS evisceration<br />
and a prosthesis adaptation.<br />
DISCUSSION<br />
Ectodermal dysplasia (ED) is a congenital syndrome characterized<br />
in general terms by sparse hair, severe oligodontia, missing or<br />
scanty eye brows, lashes and reduced sweating. It is considered a<br />
Submitted <strong>for</strong> publication: March 29, 2012<br />
Accepted <strong>for</strong> publication: June 25, 2012<br />
Study carried out at Department <strong>of</strong> Ophthalmology, Otorrinolaringology and Head & Neck Surgery,<br />
Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo - USP.<br />
1<br />
Physician, Department <strong>of</strong> Ophthalmology, Otorrinolaringology and Head & Neck Surgery, Faculdade<br />
de Medicina de Ribeirão Preto, Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil.<br />
Funding: This study was supported by FAPESP.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: M.Alves, None; L.T.Malki, None; E.M.Rocha, None.<br />
Correspondence address: Mônica Alves. Department <strong>of</strong> Ophthalmology, Otorrinolaringology and<br />
Head & Neck Surgery. Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo. Av.<br />
Bandeirantes, 3900 - Ribeirão Preto (SP) - 14049-900 - Brazil - E-mail: monicalves@fmrp.usp.br<br />
Arq Bras Oftalmol. 2012;75(5):361-2<br />
361
Buphthalmos development in adult: case report<br />
A<br />
B<br />
<strong>Ocular</strong> surface manifestations <strong>of</strong> ED include reduction <strong>of</strong><br />
eyebrows and lashes, lid keratinization, recurrent epithelial defect,<br />
trichiasis, superficial and deep corneal vascularization, limbal deficiency,<br />
meibomian glands dysfunction and dry eye (8,9) .<br />
Our patient has suffered from ocular surface dysfunction related<br />
to ED and developed glaucoma and cataracts secondary to chronic<br />
corticosteroid use. We hypothesize that there was a close relation<br />
between ED, high IOP and OS globe length growth in this case. The<br />
absence <strong>of</strong> buphthalmos in OD, in which effective IOP control was<br />
obtained following trabeculectomy, is an additional evidence <strong>of</strong> the<br />
association <strong>of</strong> globe length growth and increased IOP in ED patients.<br />
The present work describes a case <strong>of</strong> ED with challenging management<br />
problems that culminated with a unique event <strong>of</strong> buphthalmos<br />
in adulthood.<br />
C<br />
Figure 1. A) External appearance at first examination, loss <strong>of</strong> eye brow and lashes, depressed<br />
nasal bridge, epithelial corneal defect in the right eye and buphthalmos at left.<br />
B) External appearance after 6 years, showing the progression <strong>of</strong> the buphthalmos <strong>of</strong><br />
the left globe. C and D) A-scan ultrasound images <strong>of</strong> both eyes showing an axial length<br />
<strong>of</strong> approximately 25 mm <strong>of</strong> the right eye and more than 36 mm <strong>of</strong> the left.<br />
large and complex group <strong>of</strong> genetic disorders defined by the abnormal<br />
development <strong>of</strong> two or more structures <strong>of</strong> the ectodermal layer.<br />
Nearly 200 different conditions have been described as ED, however,<br />
to the best <strong>of</strong> our knowledge, no previous association with glaucoma<br />
or uncontrollable eye growth has been reported (6,7) .<br />
D<br />
REFERENCES<br />
1. Gordon RA, Donzis PB. Refractive development <strong>of</strong> the human eye. Arch Ophthalmol<br />
1985;103:785-9.<br />
2. Mark HH. Buphthalmos: early glaucoma history. Acta ophthalmologica 2011;89:591-4.<br />
3. Sorsby A, Benjamin B, Sheridan M, Stone J, Leary GA. Refraction and its components<br />
during the growth <strong>of</strong> the eye from the age <strong>of</strong> three. Memo Med Res Counc 1961;<br />
301(Special):1-67.<br />
4. Chen HB, Yamabayashi S, Ou B, Tanaka Y, Ohno S, Tsukahara S. Structure and composition<br />
<strong>of</strong> rat precorneal tear film. A study by an in vivo cry<strong>of</strong>ixation. Invest Ophthalmol<br />
Vis Sci 1997;38:381-7.<br />
5. Macsai MS, Agarwal S. Staphylococcal endophthalmitis following cataract extraction<br />
in a patient with Darier’s disease. Cornea 1998;17:335-7.<br />
6. Itin PH, Fistarol SK. Ectodermal dysplasias. Am J Med Genet C Semin Med Genet 2004;<br />
131C:45-51.<br />
7. Mikkola ML. Molecular aspects <strong>of</strong> hypohidrotic ectodermal dysplasia. Am J Med Ge -<br />
net A 2009;149A:2031-6.<br />
8. Kaercher T. <strong>Ocular</strong> symptoms and signs in patients with ectodermal dysplasia syndromes.<br />
Graefes Arch Clin Exp Ophthalmol 2004;242:495-500.<br />
9. Alves M, Dias AC, Rocha EM. Dry eye in childhood: epidemiological and clinical as -<br />
pects. Ocul Surf 2008;6:44-51.<br />
362 Arq Bras Oftalmol. 2012;75(5):361-2
Artigo de Revisão | Review Article<br />
<strong>Ocular</strong> <strong>rosacea</strong> - a review<br />
Rosácea ocular - revisão<br />
Ana Carolina Cabreira Vieira 1 , Ana Luisa Höfling-Lima 1 , Mark J Mannis 2<br />
ABSTRACT<br />
Rosacea is a prevalent chronic cutaneous disorder with variable presentation and<br />
severity. Although considered a skin disease, <strong>rosacea</strong> may evolve the eyes in 58-72%<br />
<strong>of</strong> the patients, causing eyelid and ocular surface inflammation. About one third <strong>of</strong><br />
the patients develop potentially sight-threatening corneal involvement. Untreated<br />
<strong>rosacea</strong> may cause varying degrees <strong>of</strong> ocular morbidity. The importance <strong>of</strong> early<br />
diagnosis and adequate treatment cannot be overemphasized. There is not yet a<br />
diagnostic test <strong>for</strong> <strong>rosacea</strong>. The diagnosis <strong>of</strong> ocular <strong>rosacea</strong> relies on observation<br />
<strong>of</strong> clinical features, which can be challenging in up to 90% <strong>of</strong> patients in whom<br />
accompanying roseatic skin changes may be subtle or inexistent. In this review,<br />
we describe the pathophysiologic mechanisms proposed in the literature, clinical<br />
features, diagnosis and management <strong>of</strong> ocular <strong>rosacea</strong>, as well as discuss the need<br />
<strong>for</strong> a diagnostic test <strong>for</strong> the disease.<br />
Keywords: Rosacea/diagnosis; Eye manifestations; Eye diseases; Rosacea/drug therapy;<br />
Doxycycline; Visual acuity<br />
RESUMO<br />
A rosácea é uma condição cutânea crônica, que possui apresentações clínicas variáveis.<br />
Apesar de considerada uma doença dermatológica, os olhos podem ser acometidos em<br />
58-72% dos casos, causando inflamação palpebral e da superfície ocular. Aproximadamente<br />
um terço dos pacientes desenvolve acometimento corneano, podendo causar<br />
baixa visual significativa. Diagnóstico precoce e tratamento adequado são de extrema<br />
importância, devido à significativa morbidade ocular que a doença pode causar. Não<br />
há, até o momento, um teste diagnóstico para rosácea. O diagnóstico da rosácea ocular<br />
depende da observação das manifestações clínicas, o que pode ser bastante desafiador<br />
em até 90% dos pacientes, em que os achados cutâneos são discretos ou inexistentes.<br />
Nesta revisão, descrevemos os mecanismos fisiopatológicos propostos na literatura,<br />
manifestações clínicas, diagnóstico e tratamento da rosácea ocular, assim como abordamos<br />
a necessidade de um teste diagnóstico.<br />
Descritores: Rosácea/diagnóstico; Manifestações oculares; Oftalmopatias; Rosácea/qui -<br />
mioterapia; Doxiciclina; Acuidade visual<br />
INTRODUCTION<br />
Rosacea is a widely prevalent chronic cutaneous disorder with<br />
variable presentation and severity. It primarily affects blood vessels<br />
and pilosebaceous units <strong>of</strong> the central facial skin (cheeks, chin,<br />
nose, and central <strong>for</strong>ehead), causing transient or persistent erythema,<br />
telangiectasias, papules, pustules, and phymatous changes<br />
(Fi gu re 1) (1) .<br />
Although considered a skin disease, <strong>rosacea</strong> may evolve the eyes<br />
in up to 58-72% <strong>of</strong> the patients, causing eyelid and ocular surface<br />
inflammation (1,2) . About one third <strong>of</strong> the patients develop corneal<br />
involvement, which may be sight-threatening (1,3) .<br />
Rosacea, albeit common, is <strong>of</strong>ten overlooked by general practitioners<br />
and ophthalmologists (4) . Mild <strong>rosacea</strong> patients may not seek<br />
medical help and may not be diagnosed in clinical practice. <strong>Ocular</strong><br />
<strong>rosacea</strong>, in particular, is frequently underdiagnosed. Its symptoms<br />
and signs can be quite non-specific, and in up to 90% <strong>of</strong> patients,<br />
accompanying roseatic skin changes may be very subtle. More<br />
importantly, in 20% <strong>of</strong> the cases, ocular signs may even precede characteristic<br />
skin involvement (3) . Patients <strong>of</strong>ten do not mention ocular<br />
symptoms in a dermatology clinic, unless directly asked about them.<br />
Conversely, skin manifestations are uncommonly examined during<br />
ophthalmology consults. As a result, a certain number <strong>of</strong> cases remain<br />
undetected (3) .<br />
Chronic, untreated <strong>rosacea</strong> may cause varying degrees <strong>of</strong> ocular<br />
morbidity, facial disfigurement, emotional distress, and social impairment<br />
(5,6) . The importance <strong>of</strong> early diagnosis and adequate treatment<br />
cannot be overemphasized due to the negative impact this disorder may<br />
have on the quality <strong>of</strong> life <strong>of</strong> patients and the potential sight-threatening<br />
complications <strong>of</strong> this disease.<br />
Epidemiology<br />
Rosacea affects over 16 million Americans (7) , and a Swedish survey<br />
revealed a prevalence as high as 10% (8) . A recent large observational<br />
study on the epidemiology <strong>of</strong> <strong>rosacea</strong> in the United Kingdom revealed<br />
an incidence rate <strong>of</strong> 1.65/1,000 person-years as diagnosed by general<br />
practitioners (9) . Women are more commonly diagnosed with <strong>rosacea</strong><br />
than men, and they tend to be diagnosed earlier. A possible explanation<br />
<strong>for</strong> this is that women may seek medical care more <strong>of</strong>ten and earlier than<br />
men. On the other hand, men are more prone to phymatous changes (9,10) .<br />
Rhinophyma is most commonly seen in men over 40 years <strong>of</strong> age, in<br />
more advanced stages <strong>of</strong> the disease (11,12) .<br />
<strong>Ocular</strong> <strong>rosacea</strong> affects both genders equally (9) . The incidence <strong>of</strong><br />
ocular <strong>rosacea</strong> varies among ophthalmologic and dermatologic studies,<br />
ranging from 6-72%, being more prevalent in ophthalmology<br />
clinics (2,3,13) .<br />
Rosacea may be found in early childhood as well as in the elderly,<br />
but it most commonly affects middle-aged adults (14) . Spoendlin et<br />
al., found that 80% <strong>of</strong> <strong>rosacea</strong> patients in the UK were at or above 30<br />
years <strong>of</strong> age, with a peak in the incidence rate between the ages <strong>of</strong><br />
40 and 59 years (9) . Pediatric <strong>rosacea</strong> is thought to be rare, but may be<br />
underreported since the dermatologic features are <strong>of</strong>ten absent or<br />
difficult to identify (15-17) .<br />
Submitted <strong>for</strong> publication: August 7, 2012<br />
Accepted <strong>for</strong> publication: August 23, 2012<br />
Study carried out at Universidade Federal de São Paulo - UNIFESP - São Paulo (SP), Brazil.<br />
1<br />
Physician, Department <strong>of</strong> Ophthalmology, Universidade Federal de São Paulo - UNIFESP - São<br />
Paulo (SP), Brazil.<br />
2<br />
Physician, Department <strong>of</strong> Ophthalmology, University <strong>of</strong> Cali<strong>for</strong>nia, Davis, CA, USA.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: A.C.C.Vieira, None; A.L.Höfling-Lima, employee <strong>of</strong><br />
Federal Governement <strong>of</strong> Brazil; M.J.Mannis, None.<br />
Correspondence address: Ana Carolina Cabreira Vieira, Rua Visconde de Silva, 52/503 - Rio de<br />
Janeiro - RJ - 22271-092 - Brazil - E-mail: anacarolinavieira31@gmail.com<br />
Arq Bras Oftalmol. 2012;75(5):363-9<br />
363
<strong>Ocular</strong> <strong>rosacea</strong> - a review<br />
Figure 1. Cutaneous manifestations <strong>of</strong> <strong>rosacea</strong> with characteristic involvement <strong>of</strong> central<br />
facial skin (cheeks, nose, and central <strong>for</strong>ehead).<br />
Fair-skinned patients <strong>of</strong> European descent are more commonly<br />
affected by <strong>rosacea</strong>; however, any ethnicity can be afflicted with the<br />
disease. It has been suggested that skin pigmentation may obscure<br />
identification <strong>of</strong> the characteristic findings, contributing to underdiagnosis<br />
in dark skinned patients (18) .<br />
Etiology and pathophysiology<br />
The precise etiology and pathophysiologic mechanisms <strong>of</strong> cutaneous<br />
and ocular <strong>rosacea</strong> remain unknown, although different theories<br />
have been proposed. Several studies confirm the inflammatory<br />
nature <strong>of</strong> the disease. An elevated concentration <strong>of</strong> interleukin-1a<br />
and b and a greater activity <strong>of</strong> gelatinase B (metalloproteinase -9) and<br />
colagenase-2 (MMP-8) have been found in tear fluids <strong>of</strong> patients with<br />
ocular <strong>rosacea</strong> (19-22) . Doxycycline, used in the treatment <strong>of</strong> cutaneous<br />
and ocular <strong>rosacea</strong>, decreases both MMP-8 and MMP-9 activity (21,22) .<br />
Tumor necrosis factor (TNF-alfa) was also elevated in <strong>rosacea</strong> (23) .<br />
Significant overexpression <strong>of</strong> ICAM-1 (intercellular adhesion molecule<br />
1) and HLA-DR, inflammatory markers, was observed in conjunctival<br />
epithelial cells <strong>of</strong> patients with <strong>rosacea</strong> (24) .<br />
Recently, studies have shown that disease exacerbation is stimulated<br />
by normal external environmental factors, leading to unique<br />
activation <strong>of</strong> pro-inflammatory systems as well as innate immune<br />
responses (23,25,26) . Molecular studies propose that the enhanced<br />
sensitivity <strong>of</strong> patients with <strong>rosacea</strong> may be caused by abnormal<br />
recognition <strong>of</strong> common environmental stimuli. Factors that trigger<br />
the innate immune system lead to an increase in the expression <strong>of</strong><br />
certain cytokines and anti-microbial molecules in the skin (25,27) . Cathelicidin,<br />
one <strong>of</strong> these antimicrobial peptides, has both vasoactive<br />
and pro-inflammatory actions and is implicated in the pathogenesis<br />
<strong>of</strong> this disorder. Based on the observation <strong>of</strong> a single molecule that<br />
presents both vasoactive and pro-inflammatory actions, researchers<br />
decided to study the behavior <strong>of</strong> such molecule in <strong>rosacea</strong>. As hypothesized,<br />
these peptides were found in greater levels in the skin <strong>of</strong><br />
individuals with <strong>rosacea</strong> than in normal facial skin (25,27,28) . Moreover,<br />
the cathelicidin peptides found in <strong>rosacea</strong> patients were not only<br />
more abundant but were different from those found in normal individuals<br />
(25) . These <strong>for</strong>ms <strong>of</strong> cathelicidin peptides are known <strong>for</strong> its role<br />
in natural host defense against infections and in promoting leukocyte<br />
chemotaxis, angiogenesis, and extracellular matrix component<br />
expression (27) . Supporting this theory, gene array studies found that<br />
mRNA expression levels <strong>of</strong> cathelicidin were found to be significantly<br />
increased in all subtypes <strong>of</strong> <strong>rosacea</strong> (29) . Additionally, local proteases<br />
(serine protease KLK5) that control the production <strong>of</strong> cathelicidin in<br />
epidermis were also abnormally expressed in <strong>rosacea</strong> patients (25,27) .<br />
To further test their hypothesis, researchers injected abnormal<br />
cathelicidin or protease that produce these peptides in the skin<br />
<strong>of</strong> mice and observed similar inflammatory features <strong>of</strong> the disease<br />
found in humans (27) . Observation <strong>of</strong> higher amounts <strong>of</strong> receptors <strong>of</strong><br />
the recognition system, Toll-like receptor 2 (TLR2), in the epidermis<br />
<strong>of</strong> patients with <strong>rosacea</strong> explained the overreaction <strong>of</strong> these patients<br />
to environmental stimuli, since enhanced action <strong>of</strong> TLR2 in keratinocytes<br />
leads to an increase in serine protease KLK5 and cathelicidin<br />
production (23,25) . Interestingly, tetracyclines, which improve signs and<br />
symptoms <strong>of</strong> <strong>rosacea</strong>, are known to inhibit expression and activity <strong>of</strong><br />
several matrix metalloproteinases (21) , as well as a class <strong>of</strong> proteases<br />
that activate cathelicidin, sustaining this theory (26,27) . Furthermore, a<br />
recent study found elevated concentrations <strong>of</strong> 5 molecules involved<br />
in the innate immune response (interleukin-1b, interleukin-16, stem<br />
cell factor, monocyte chemotactic protein (MCP)-1, and monokine<br />
induced by g-interferon) in cutaneous biopsy specimens taken from<br />
ocular <strong>rosacea</strong> patients, supporting the concept that ocular <strong>rosacea</strong><br />
is a disorder <strong>of</strong> innate immunity (30) .<br />
Vascular dilation and incompetence contribute to the signs and<br />
symptoms <strong>of</strong> <strong>rosacea</strong>. The characteristic facial flushing, persistent<br />
erythema and telangiectasia may be caused by altered cutaneous<br />
neurovascular homeostasis. Studies have demonstrated increased<br />
blood flow in the face and larger and more numerous vessels in the<br />
face than in other areas <strong>of</strong> the body (31) . Significantly dilated blood<br />
and lymphatic vessels were reported in all subtypes <strong>of</strong> <strong>rosacea</strong> (29) .<br />
Studies further demonstrated an up-regulation <strong>of</strong> genes involved<br />
in vasoregulation and neurogenic inflammation and suggested that<br />
dysregulation <strong>of</strong> mediators and receptors implicated in neurovascular<br />
and neuroimmune communication may be crucial at early stages<br />
<strong>of</strong> <strong>rosacea</strong> (26,29,32) . Improvement <strong>of</strong> erythema and flushing in <strong>rosacea</strong><br />
by topical administration <strong>of</strong> a-adrenergic receptor agonists, oxymetazoline<br />
and xylometazoline, helps support this theory (25,33,34) .<br />
Cathelicidin causes endothelial changes (26) . Angiogenesis induced<br />
by cathelicidin is mediated by an increase in vascular endothelial<br />
growth factor (VEGF) in epidermal keratinocytes, and could represent<br />
an explanation <strong>for</strong> these vascular events in <strong>rosacea</strong> (25) . An increase in<br />
expression <strong>of</strong> VEGF and its receptors was demonstrated in the skin <strong>of</strong><br />
patients with <strong>rosacea</strong> (35,36) .<br />
Group IIA phospholipase A 2<br />
, an antimicrobial protein capable <strong>of</strong><br />
killing Gram-positive bacteria, is secreted into the tears by lacrimal<br />
glands and plays a role in innate host defense. A decreased concentration<br />
<strong>of</strong> group IIA phospholipase A 2<br />
was found in tears <strong>of</strong> patients<br />
with ocular <strong>rosacea</strong> (37) .<br />
Microbial organisms such as Helicobacter pylori, Demodex folliculorum,<br />
Demodex brevis and Staphylococcus epidermidis have been<br />
appointed as other possible causative factors in exacerbation <strong>of</strong> the<br />
disease; however this remains a controversy (23,26,31,38-43) . The prevalence<br />
<strong>of</strong> H. pylori infection was found higher in patients with <strong>rosacea</strong> when<br />
compared to the general population, and its eradication has been<br />
shown to influence the clinical outcome <strong>of</strong> this disease (31,39,44-46) . However,<br />
other studies have not found such difference (41,47-49) . Demodex,<br />
a microscopic mite found in hair follicles and sebaceous glands, is<br />
the most common ectoparasite in humans. Studies support its role<br />
in the activation <strong>of</strong> immune mechanisms in certain subtypes <strong>of</strong><br />
<strong>rosacea</strong>, especially papulopustular <strong>rosacea</strong> (32) . The Demodex count<br />
was shown significantly higher in patients with facial <strong>rosacea</strong>, and<br />
a study demonstrated a strong correlation between positive serum<br />
immunoreactivity and ocular Demodex infestation in facial <strong>rosacea</strong><br />
and lid margin inflammation (41,50,51) . Another proposed mechanism<br />
364 Arq Bras Oftalmol. 2012;75(5):363-9
Vieira ACC, et al.<br />
is that Demodex mites may act as vectors <strong>for</strong> other microorganisms<br />
such as Bacillus olenorium, which may be responsible <strong>for</strong> initiation <strong>of</strong><br />
inflammatory response in <strong>rosacea</strong>, through production <strong>of</strong> antigenic<br />
proteins and stimulation <strong>of</strong> Toll-like receptor 2 (TLR2) (23,25,38,42,50) .<br />
Diagnosis<br />
The diagnosis <strong>of</strong> <strong>rosacea</strong> is clinical and relies on observation <strong>of</strong><br />
skin manifestations. In cases in which these are only very subtle, the<br />
diagnosis can become very challenging and the disease may remain<br />
undiagnosed. In addition, manifestations <strong>of</strong> ocular <strong>rosacea</strong> are by no<br />
means specific to the disorder alone and other ophthalmologic diseases<br />
may present with similar findings, making the diagnosis even<br />
more difficult and the search <strong>for</strong> a diagnostic test quite important.<br />
Lack <strong>of</strong> diagnostic test<br />
Un<strong>for</strong>tunately, there is not yet a diagnostic test available <strong>for</strong> either<br />
cutaneous or ocular <strong>rosacea</strong> (15) . No serologic or histologic markers<br />
have been described to date. A diagnostic marker may enable earlier<br />
diagnosis and treatment, as well as contribute with an etiologic explanation<br />
<strong>for</strong> this troublesome disorder. Our group has been working<br />
on the glycomic pr<strong>of</strong>ile <strong>of</strong> tears and saliva <strong>of</strong> roseatic patients, as an<br />
initial step in the long pathway towards the search <strong>for</strong> a biomarker <strong>for</strong><br />
the disease. We have previously shown a high abundance <strong>of</strong> O-linked<br />
oligosaccharides in the tears <strong>of</strong> patients with <strong>rosacea</strong> (52) . More recently,<br />
we published our results on glycomic analysis <strong>of</strong> tears and saliva,<br />
and previous results were confirmed in both fluids with N-glycans<br />
dramatically decreased in roseatic tear and saliva samples (53) . Furthermore,<br />
we described highly novel glycans that may be potential<br />
biomarkers <strong>for</strong> <strong>rosacea</strong> (53) .<br />
Classification and grading <strong>of</strong> <strong>rosacea</strong><br />
To aid in diagnosis, in 2002, an expert committee <strong>of</strong> the American<br />
National Rosacea Society published a standard classification system<br />
<strong>for</strong> <strong>rosacea</strong> (54) . As well as serving as a diagnostic tool, this classification<br />
facilitates communication among dermatologists, researchers and<br />
other specialists (54,55) . This important publication describes primary<br />
and secondary features <strong>of</strong> <strong>rosacea</strong> and defines 4 subtypes (erythematotelangiectatic,<br />
papulopustular, phymatous and ocular <strong>rosacea</strong>)<br />
and 1 variant (granulomatous <strong>rosacea</strong>) <strong>of</strong> the disease (54) . The primary<br />
Table 1. Primary and secondary features <strong>of</strong> <strong>rosacea</strong>. Adapted from<br />
the Standard Classification <strong>of</strong> Rosacea, proposed by the National<br />
Rosacea Society Expert Committee, 2002 (54)<br />
Primary features<br />
Flushing (transient erythema)<br />
Nontransient erythema<br />
Papules and pustules<br />
Telangiectasia<br />
Secondary features<br />
Burning or stinging sensations<br />
Elevated plaques<br />
Dry appearance<br />
Edema<br />
<strong>Ocular</strong> manifestations<br />
Peripheral location<br />
Phymatous changes<br />
Description<br />
Frequent blushing or flushing<br />
Persistent redness <strong>of</strong> the facial skin<br />
Red papules with or without pustules. Nodules<br />
may also occur<br />
Telangiectases are common but not necessary<br />
<strong>for</strong> a <strong>rosacea</strong> diagnosis<br />
Description<br />
Dry appearance <strong>of</strong> central facial skin<br />
Facial edema<br />
and secondary features are listed in table 1. The presence <strong>of</strong> one or<br />
more <strong>of</strong> the primary signs with an axial facial distribution is indicative<br />
<strong>of</strong> <strong>rosacea</strong>. One or more <strong>of</strong> the secondary features may or may not<br />
be present.<br />
Later, in 2004, the National Rosacea Society Expert Committee<br />
published a grading system to assess the severity <strong>of</strong> disease. Primary<br />
features were graded on a scale from 0 to 3 whether they were absent,<br />
mild, moderate, or severe, and most secondary features were<br />
graded as absent or present (56) .<br />
Diagnosis <strong>of</strong> ocular <strong>rosacea</strong><br />
The diagnosis <strong>of</strong> ocular <strong>rosacea</strong> relies on observation <strong>of</strong> one or<br />
more <strong>of</strong> the following signs and symptoms: watery or bloodshot<br />
appearance (interpalpebral conjunctival hyperemia), <strong>for</strong>eign body<br />
sensation, burning or stinging, dryness, itching, light sensitivity,<br />
blurred vision, telangiectases <strong>of</strong> the conjunctiva and lid margin, lid<br />
and periocular erythema. Anterior blepharitis, meibomian gland dysfunction<br />
and irregularity <strong>of</strong> the eyelid margins may also be present (54) .<br />
Diagnosis <strong>of</strong> pediatric <strong>rosacea</strong><br />
The clinical features <strong>of</strong> pediatric <strong>rosacea</strong> are similar to those observed<br />
in adults (16) . However, in children, the dermatologic findings<br />
are <strong>of</strong>ten absent, making the diagnosis even more challenging and<br />
the identification <strong>of</strong> ocular manifestations especially important (15,17,57) .<br />
A study revealed ocular symptoms to precede skin features in 55%<br />
<strong>of</strong> children (58) . Ophthalmologists should maintain high suspicion in<br />
children with ocular surface disease, with or without cutaneous features,<br />
to avoid misdiagnosis and complications (59) . A positive family<br />
history <strong>of</strong> cutaneous <strong>rosacea</strong> and previous episodes <strong>of</strong> chalazia may<br />
be helpful in establishing the diagnosis (17) .<br />
Clinical findings<br />
Rosacea<br />
Symptoms may show periods <strong>of</strong> exacerbation and remission;<br />
however, the disease usually progresses over time. Some factors are<br />
known to worsen symptoms <strong>of</strong> <strong>rosacea</strong> and are referred to as trigger<br />
factors. Some examples <strong>of</strong> triggers are sun exposure, spicy foods,<br />
alcohol consumption, extreme temperatures, physical exercise, menopause<br />
and emotional distress such as anger and embarrassment.<br />
These factors tend to be specific to each individual. A recent large<br />
epidemiologic study revealed that alcohol consumption is associated<br />
with only a small increase in risk <strong>of</strong> developing <strong>rosacea</strong>, whereas<br />
smoking may actually substantially reduce such risk (9) .<br />
Figure 2. Eyelid margin <strong>of</strong> a patient with ocular <strong>rosacea</strong> showing meibomian gland<br />
dysfunction and telangiectases.<br />
Arq Bras Oftalmol. 2012;75(5):363-9<br />
365
<strong>Ocular</strong> <strong>rosacea</strong> - a review<br />
<strong>Ocular</strong> <strong>rosacea</strong><br />
Patients with ocular <strong>rosacea</strong> may complain <strong>of</strong> <strong>for</strong>eign body sensation,<br />
dryness, itching, photophobia and tearing (10,60) . Decreased visual<br />
acuity may result when corneal involvement is present.<br />
<strong>Ocular</strong> manifestations are usually bilateral and, as previously<br />
mentioned, can be non-specific (15) . The severity <strong>of</strong> ocular <strong>rosacea</strong><br />
symptoms is <strong>of</strong>ten not related to the severity <strong>of</strong> cutaneous manifestations<br />
(15,31,51,60,61) . One study found a significant relationship between<br />
ocular involvement and the severity <strong>of</strong> telangiectasia (62) .<br />
Eyelids and tear film<br />
Blepharitis and meibomian gland dysfunction are common<br />
findings (3,15) . Slit-lamp examination <strong>of</strong> the eyelid margins reveals<br />
telangiectases (Figure 2), dilated meibomian glands, excessive seborrheic<br />
secretion and collarettes around the eyelashes (15) . Excessive<br />
meibomian secretion may lead to a soapy aspect <strong>of</strong> the inferior tear<br />
meniscus. Debris in the tear film may also be present. Recurrent<br />
hordeolum/chalazion and tear film insufficiency are commonly<br />
observed as a consequence <strong>of</strong> meibomian gland dysfunction (9,15) .<br />
Dry eyes, with abnormal Schirmer test, were reported in 56-62.5%<br />
<strong>of</strong> patients with ocular <strong>rosacea</strong> (24,51,63) . Diminished tear break-up time<br />
(TBUT) has also been reported in a large majority <strong>of</strong> patients with<br />
ocular <strong>rosacea</strong> (24,51,60) .<br />
Facial edema is an uncommon manifestation (64) . Periorbital edema<br />
has been reported in the literature and in one particular case,<br />
eyelid edema was severe enough to cause visual impairment (65,66) .<br />
Conjunctiva<br />
Chronic conjunctivitis characterized by interpalpebral bulbar<br />
conjunctival hyperemia may be present (13,15) , as well as a chronic papillary<br />
reaction (3) . Cicatricial conjunctivitis involving the lower lid was<br />
described by Akpek et al. as one <strong>of</strong> the most common ocular surface<br />
findings in <strong>rosacea</strong> (67) . Chronic cicatrizing conjunctivitis affecting<br />
mainly the upper eyelids, mimicking the classic findings in trachoma,<br />
has also been reported (68) . Pinguecula and conjunctival fibrosis have<br />
been reported in up to 20% <strong>of</strong> patients with ocular <strong>rosacea</strong> (69,70) . Starr<br />
and McDonald described a characteristic “arcade” <strong>of</strong> dilated vessels in<br />
the superficial limbal plexus, usually present in the inferior quadrants<br />
and not extending into the cornea (1) .<br />
Symblepharon <strong>for</strong>mation following surgical excision <strong>of</strong> a pyogenic<br />
granuloma in a patient with ocular <strong>rosacea</strong> has been reported (71) .<br />
Cornea<br />
Corneal manifestations may occur in up to 33% <strong>of</strong> patients with<br />
<strong>rosacea</strong> (1,3) . The inferior cornea is usually affected (15) . Corneal involvement<br />
typically starts with superficial punctate keratitis on the lower<br />
third <strong>of</strong> the cornea. Peripheral neovascularization associated with<br />
subepithelial marginal triangular infiltrates along the advancing<br />
vascular border can also occur (Figure 3) (1) . If left untreated, these<br />
infiltrates may progress centrally and lead to stromal ulceration and<br />
even per<strong>for</strong>ation (15,72,73) .<br />
Recurrent corneal epithelial erosions have been reported in patients<br />
with ocular <strong>rosacea</strong> (67,74,75) . Other uncommon corneal findings<br />
include pseudodendritic ulcer and pseudokeratoconus, presenting<br />
with inferior corneal thinning and high astigmatism (76-78) . Secondary<br />
infectious keratitis has been reported (79,80) .<br />
Decreased visual acuity may result from epithelial ulceration,<br />
surface irregularities and corneal scarring.<br />
Other ocular findings<br />
Other ocular findings include iritis, episcleritis and scleritis (5,15) . We<br />
have previously published a case <strong>of</strong> spontaneous scleral per<strong>for</strong>ation<br />
in a patient with <strong>rosacea</strong> (Figure 4) (81) .<br />
Pediatric <strong>rosacea</strong><br />
The most common ocular signs in pediatric <strong>rosacea</strong> include<br />
meibomian gland dysfunction, telangiectasia, recurrent chalazia,<br />
conjunctival hyperemia, superficial punctate epitheliopathy involving<br />
the inferior cornea, as well as corneal infiltrates, pannus and<br />
neovascularization (16,58) . Phlyctenular keratoconjunctivitis has also<br />
been associated with ocular <strong>rosacea</strong> in children (17) . Corneal scarring<br />
and opacification are possible complications <strong>of</strong> more advanced<br />
disease (17) . Donaldson et al., found that 90% <strong>of</strong> the children in their<br />
series had some degree <strong>of</strong> corneal involvement at the time <strong>of</strong> presentation<br />
(17) .<br />
Differential diagnosis <strong>of</strong> ocular <strong>rosacea</strong><br />
The differential diagnosis <strong>of</strong> ocular <strong>rosacea</strong> may include staphylococcal<br />
and seborrheic blepharokeratoconjunctivitis, and sebaceous<br />
gland carcinoma. Given that there is currently no diagnostic test<br />
<strong>for</strong> <strong>rosacea</strong>, distinguishing ocular <strong>rosacea</strong> from staphylococcal and<br />
seborrheic blepharoconjunctivitis in patients in which ocular signs<br />
precede skin findings may be difficult. Sebaceous gland carcinoma<br />
Figure 3. Corneal involvement in a patient with ocular <strong>rosacea</strong>: peripheral neovascularization<br />
associated with subepithelial marginal infiltrates along the advancing vascular border.<br />
Figure 4. Scleral per<strong>for</strong>ation in a patient with ocular <strong>rosacea</strong>.<br />
366 Arq Bras Oftalmol. 2012;75(5):363-9
Vieira ACC, et al.<br />
is <strong>of</strong>ten misdiagnosed as chalazion and early recognition is <strong>of</strong>ten<br />
challenging. For this reason, recurrent chalazia should be excised<br />
and sent to histopathology.<br />
Treatment<br />
Rosacea treatment should be initiated as early as possible in order<br />
to slow progression <strong>of</strong> inflammation and decrease development <strong>of</strong><br />
irreversible fibrosis and ocular morbidity. The severity <strong>of</strong> the clinical<br />
findings and subtypes will help guide therapy. It is important to note<br />
that it is not uncommon <strong>for</strong> patients to present with an overlap <strong>of</strong><br />
signs, showing features <strong>of</strong> more than one subtype <strong>of</strong> the disease (82) .<br />
Clinicians should there<strong>for</strong>e identify the clinical features <strong>of</strong> the individual<br />
patient in order to guide the treatment, rather than try to<br />
fit the patient into one specific category. Treatment <strong>of</strong> eye-related<br />
symptoms alone may not be effective unless the underlying <strong>rosacea</strong><br />
is diagnosed and adequately treated.<br />
General measures<br />
Initial management includes identification and avoidance <strong>of</strong><br />
trig ger factors (10) . These factors are usually specific to each individual.<br />
Broad-spectrum sunscreen should be used daily <strong>for</strong> photoprotection<br />
(11) . Appropriate use <strong>of</strong> concealing makeup may help<br />
disguise upsetting facial features (83) . Patients should be in<strong>for</strong>med<br />
about the need and importance <strong>of</strong> regular eye exams (4) .<br />
Medical treatment<br />
Cutaneous <strong>rosacea</strong><br />
There are several treatment options available <strong>for</strong> <strong>rosacea</strong> but it is<br />
unclear which are the most effective. Early stages <strong>of</strong> <strong>rosacea</strong> may be<br />
controlled with topical regimens. Medications such as topical metronidazole<br />
(0.75% and 1% <strong>for</strong>mulations) and azelaic acid (15% gel<br />
or 20% cream) are approved <strong>for</strong> the treatment <strong>of</strong> mild to moderate<br />
papulopustular <strong>rosacea</strong>, showing similar results (15,61,82,84-88) . Sodium<br />
sulfacetamide 10%/sulfur 5% preparations have also been used<br />
with satisfactory results; however, its association with metronidazole<br />
cream showed superior efficacy(89). Other topical treatments<br />
used “<strong>of</strong>f-label” include clindamycin, erythromycin, pimecrolimus,<br />
tacrolimus and tretinoin (61,86,89) .<br />
When topical treatment alone is not sufficient, systemic therapy<br />
should be initiated. Oral tetracyclines (500 mg b.i.d.) and<br />
do xycycline (40-100 mg daily from 8-16 weeks) have been shown<br />
to safely improve the signs and symptoms <strong>of</strong> <strong>rosacea</strong> (84) . In 2006,<br />
the FDA approved a daily <strong>for</strong>mulation <strong>of</strong> 40 mg doxycycline mo -<br />
nohydrate (Oracea®, Galderma) <strong>for</strong> the treatment <strong>of</strong> <strong>rosacea</strong>, although<br />
other approved <strong>for</strong>mulations <strong>of</strong> doxycycline are available.<br />
In unresponsive cases and when tetracyclines are contra-indicated<br />
or not tolerated, oral azithromycin (500 mg/day <strong>for</strong> 2 weeks) has<br />
been considered a good option (2,90,91) . Oral isotretinoin (0.3 to 1.0<br />
mg/kg/day) is recommended in more severe intractable cases. The<br />
biggest disadvantage <strong>of</strong> this drug is the risk <strong>of</strong> teratogenicity and,<br />
there<strong>for</strong>e, all female patients in childbearing age should use proper<br />
contraception (92) .<br />
Diffuse and persistent erythema in erythematotelangiectatic<br />
<strong>rosacea</strong> has been successfully treated with topical oxymetazoline<br />
0.05% and xylometazoline 0.05%, alpha-adrenergic receptor agonists<br />
with strong vasoconstrictive properties (33,34) . It is important<br />
to note that these medications are not yet FDA-approved <strong>for</strong> the<br />
treatment <strong>of</strong> <strong>rosacea</strong>, but have been published in case reports.<br />
Another α-agonist currently in study showing promising results <strong>for</strong><br />
the treatment <strong>of</strong> facial erythema is brimonidine tartrate, a highly<br />
selective α2-adrenoreceptor agonist (82,93) . Vascular laser therapy<br />
and intense pulsed light can be used <strong>for</strong> treatment <strong>of</strong> resistant<br />
skin telangiectasias and persistent erythema (15,61,93,94) .<br />
<strong>Ocular</strong> <strong>rosacea</strong><br />
Management <strong>of</strong> mild ocular <strong>rosacea</strong> requires local measures such<br />
as warm compresses, lid hygiene with neutral baby shampoo and<br />
instillation <strong>of</strong> lubricating drops (2,83) . Thicker lubricating agents, such<br />
as gels and ointments, may be prescribed <strong>for</strong> more symptomatic<br />
dry eyes to promote longer-lasting relief. Topical cyclosporine 0.05%<br />
helps increase tear production and quality (95) . Antibiotic ointments<br />
prescribed daily, at bedtime, decreases eyelid flora and helps s<strong>of</strong>ten<br />
collarettes (61) .<br />
Moderate ocular <strong>rosacea</strong> may require systemic therapy (96) . Oral<br />
tetracycline and doxycycline have been used to successfully treat<br />
ocular <strong>rosacea</strong> as an adjunct therapy to topical treatment (60,61,83,97) .<br />
As in the management <strong>of</strong> skin <strong>rosacea</strong>, tetracyclines may be initially<br />
administered 500 mg b.i.d. <strong>for</strong> 2-3 weeks, and then tapered according<br />
to clinical response. Doxycycline possesses anti-angiogenic and anti-<br />
-inflammatory properties as well as fewer side effects than first generation<br />
tetracyclines. Doxycycline may be prescribed in a regimen<br />
<strong>of</strong> 100 mg once or twice daily <strong>for</strong> 6 to 12 weeks. Many patients may<br />
present flare-ups once the medication is discontinued and may there<strong>for</strong>e<br />
require long-term maintenance therapy. However, long-term<br />
use <strong>of</strong> the drug at this dosage has side effects that may compromise<br />
regular treatment, such as gastrointestinal intolerance. As previously<br />
mentioned, the FDA approved a 40 mg doxycycline <strong>for</strong>mulation<br />
(Oracea®, Galderma) <strong>for</strong> the treatment <strong>of</strong> <strong>rosacea</strong>. It contains 30 mg<br />
immediate-release and 10 mg delayed-release doxycycline that<br />
should be administered once daily (98) . Significant improvement <strong>of</strong><br />
ocular <strong>rosacea</strong> was obtained with regular use <strong>of</strong> controlled-release<br />
doxycycline 40 mg, with no side effects leading to discontinuation<br />
<strong>of</strong> therapy (85,99) . Azithromycin improved eye symptoms and was considered<br />
a good alternative therapy <strong>for</strong> ocular <strong>rosacea</strong>, when other<br />
drugs are not tolerated (2) . Long-term oral consumption <strong>of</strong> omega<br />
3 fatty acids has been shown to improve the quality <strong>of</strong> meibomian<br />
gland secretion (15) .<br />
In cases where persistent ocular surface inflammation, episcleritis,<br />
scleritis, iritis and sterile keratitis are present, topical corticosteroids<br />
or cyclosporine may prove beneficial (15,61,85,95,100) . Topical cyclosporine<br />
0.05%, used twice daily, was also beneficial in reducing inflammation<br />
in posterior blepharitis (15) . Long-term use <strong>of</strong> steroids should be avoided<br />
due to the potential side effects, such as glaucoma and cataracts,<br />
in which case the use <strong>of</strong> topical cyclosporine is preferable (15) .<br />
In cases <strong>of</strong> secondary infectious keratitis, antimicrobial agents<br />
should be initiated promptly and topical steroids avoided or used<br />
with care, along with specific antimicrobial therapy (15,79) .<br />
Pediatric ocular <strong>rosacea</strong><br />
Initial treatment should include local measures such as warm<br />
compresses and eyelid hygiene with neutral baby shampoo. This<br />
routine may be difficult to maintain in children; however, the importance<br />
<strong>of</strong> these measures should be rein<strong>for</strong>ced to the parents. Topical<br />
erythromycin ointment may also be used on the eyelid margins (58) .<br />
Low-dose corticosteroid drops may be necessary to control ocular<br />
surface inflammation and treat keratitis, peripheral corneal vascularization<br />
and scarring (17) .<br />
As in adults, those patients with resistant disease should be prescribed<br />
oral therapy. Systemic treatment <strong>of</strong> ocular childhood <strong>rosacea</strong><br />
is very similar to that in adults, although one important difference<br />
is that tetracyclines are contra-indicated in children younger than<br />
7 years <strong>of</strong> age (58) . Tetracycline and doxycycline, commonly used <strong>for</strong><br />
therapy in adults, may result in depressed bone growth and dental<br />
staining in this age range (17) . In these cases, erythromycin (20 mg/kg/<br />
day) is preferable (16,17,101) . Doxycycline (100 mg once or twice daily) is<br />
considered a good therapeutic option <strong>for</strong> older children, since it is<br />
usually better tolerated than tetracycline. Long-term treatment with<br />
systemic erythromycin and doxycycline proved beneficial in children<br />
with ocular <strong>rosacea</strong> (16) . Azithromycin improved eye symptoms and<br />
Arq Bras Oftalmol. 2012;75(5):363-9<br />
367
<strong>Ocular</strong> <strong>rosacea</strong> - a review<br />
may also be considered in young children, where tetracyclines cannot<br />
be prescribed (2) .<br />
Surgical treatment<br />
Punctal occlusion may be beneficial in the management <strong>of</strong> moderate<br />
to severe dry eyes. Persistent chalazia may require surgical<br />
management and specimen should be sent to pathology.<br />
Corneal thinning and per<strong>for</strong>ations in ocular <strong>rosacea</strong> patients<br />
have been managed using simple corneal sutures, tissue adhesive,<br />
amniotic membrane transplantation, and conjunctival flaps (73,102-104) .<br />
Lamellar or full-thickness keratoplasty are other options when surgical<br />
intervention becomes necessary, in cases <strong>of</strong> corneal per<strong>for</strong>ation or<br />
opacification (15) . Gracner and Gracner chose to per<strong>for</strong>m a keratoplasty<br />
to successfully treat an extensive cornealscleral per<strong>for</strong>ation (72) .<br />
Conclusion and future perspectives<br />
Rosacea is a prevalent disorder that may be disfiguring and cause<br />
significant social impairment, as well as various degrees <strong>of</strong> ocular<br />
morbidity, if not diagnosed and managed appropriately. <strong>Ocular</strong><br />
<strong>rosacea</strong> is <strong>of</strong>ten left undiagnosed and no specific diagnostic test is<br />
available to date. For this reason, diagnosis relies on a high level <strong>of</strong><br />
suspicion and clinical observation <strong>of</strong> characteristic skin manifestations<br />
(54) . This becomes very challenging in up to 20% <strong>of</strong> the patients,<br />
when ocular symptoms and signs precede cutaneous features (3) . In<br />
these cases, a diagnostic test would be <strong>of</strong> great importance. Future<br />
studies may provide a biomarker and an etiologic explanation <strong>for</strong> this<br />
troublesome disorder.<br />
REFERENCES<br />
1. Starr PA, McDonald A. Oculocutaneous aspects <strong>of</strong> <strong>rosacea</strong>. Proc R Soc Med. 1969;<br />
62(1):9-11.<br />
2. Bakar O, Demircay Z, Toker E, Cakir S. <strong>Ocular</strong> signs, symptoms and tear function tests<br />
<strong>of</strong> papulopustular <strong>rosacea</strong> patients receiving azithromycin. J Eur Acad Dermatol<br />
Venereol. 2009;23(5):544-9.<br />
3. Ghanem VC, Mehra N, Wong S, Mannis MJ. The prevalence <strong>of</strong> ocular signs in acne<br />
<strong>rosacea</strong>: comparing patients from ophthalmology and dermatology clinics. Cornea.<br />
2003;22(3):230-3.<br />
4. Blount BW, Pelletier AL. Rosacea: a common, yet commonly overlooked, condition.<br />
Am Fam Physician. 2002;66(3):435-40. Summary <strong>for</strong> patients in: Am Fam Physician.<br />
2002;66(3):442.<br />
5. Alvarenga LS, Mannis MJ. Rosacea ocular. Surf Ocul. 2005;3(1):41-58.<br />
6. Cohen AF, Tiemstra JD. Diagnosis and treatment <strong>of</strong> <strong>rosacea</strong>. J Am Board Fam Pract.<br />
2002;15(3): 214-7.<br />
7. National Rosacea Society. 16 million Americans have <strong>rosacea</strong> and most <strong>of</strong> them don’t<br />
know itInternet]. Barrington, Illinois; NRS; 2012. Available from: http://www.<strong>rosacea</strong>.org<br />
8. Berg M, Lidén S. An epidemiological study <strong>of</strong> <strong>rosacea</strong>. Acta Derm Venereol. 1989;<br />
69(5):419-23.<br />
9. Spoendlin J, Voegel JJ, Jick SS, Meier CR. A study on the epidemiology <strong>of</strong> <strong>rosacea</strong> in<br />
the U.K. Br J Dermatol. 2012;167(3):598-605.<br />
10. Baldwin HE. Diagnosis and treatment <strong>of</strong> <strong>rosacea</strong>: state <strong>of</strong> the art. J Drugs Dermatol.<br />
2012;11(6):725-30.<br />
11. Buechner SA. Rosacea: an update. Dermatology. 2005;210(2):100-8.<br />
12. Wollina U. Rosacea and rhinophyma in the elderly. Clin Dermatol. 2011;29(1):61-8. Review.<br />
13. Wise G. <strong>Ocular</strong> <strong>rosacea</strong>. Am J Ophthalmol. 1943;26:591-609.<br />
14. Hong E, Fischer G. Childhood ocular <strong>rosacea</strong>: Considerations <strong>for</strong> diagnosis and treatment.<br />
Australas J Dermatol. 2009;50(4):272-5.<br />
15. Oltz M, Check J. Rosacea and its ocular manifestations. Optometry. 2011;82(2):92-103.<br />
16. Çetinkaya A, Okova YA. Pediatric ocular acne <strong>rosacea</strong>: long term treatment with<br />
systemic antibiotics. Am J Ophthalmol. 2006;142(5):816-21.<br />
17. Donaldson KE, Karp CL, Dunbar MT. Evaluation and treatment <strong>of</strong> children with ocular<br />
<strong>rosacea</strong>. Cornea. 2007;26(1):42-6.<br />
18. Browning DJ, Rosenwasser G, Lugo M. <strong>Ocular</strong> <strong>rosacea</strong> in blacks. Am J Ophthalmol.<br />
1986;101(4):441-4.<br />
19. Afonso AA, Sobrin L, Monroy DC, Selzer M, Lokeshwar B, Pflugfelder SC. Tear fluid<br />
gelatinase B activity correlates with IL-1alfa concentration and fluorescein clearance<br />
in ocular <strong>rosacea</strong>. Invest Ophthalmol Vis Sci. 1999;40(11):2506-12.<br />
20. Barton K, Monroy CD, Nava A, Pflugfelder SC. Inflammatory cytokines in tears <strong>of</strong><br />
patients with ocular <strong>rosacea</strong>. Ophthalmology. 1997;104(11):1868-74.<br />
21. Sobrin L, Liu Z, Monroy DC, Solomon A, Slezer MG, Lokeshwar BL, et al. Regulation <strong>of</strong><br />
MMP-9 activity in human tear fuid and corneal epithelial culture supernatant. Invest<br />
Ophthalmol Vis Sci. 2000;41(7):1703-9.<br />
22. Määttä M, Kari O, Tervahartiala T, Peltonen S, Kari M, Saari M, et al. Tear fluid levels <strong>of</strong><br />
MMP-8 are elevated in ocular <strong>rosacea</strong> - treatment effect <strong>of</strong> oral doxycycline. Graefe’s<br />
Arch Clin Exp Ophthalmol. 2006;244(8):957-62.<br />
23. Yamasaki K, Kanada K, Macleod D, Borkowski AW, Morizane, S, Nakatsuji T, et al. TLR2<br />
expression is increased in <strong>rosacea</strong> and stimulates enhanced serine protease production<br />
by keratinocytes. J Invest Dermatol. 2011;131(3):688-97.<br />
24. Pisella PJ, Brignole F, Debbasch C, Lozato A, Creuzot-Garcher C, Bara J, et al. Flow cytometric<br />
analysis <strong>of</strong> conjunctival epithelium in ocular <strong>rosacea</strong> and keratoconjunctivitis<br />
sicca. Ophthalmology. 2000;107(10):1841-9.<br />
25. Yamasaki K, Gallo RL. The molecular pathology <strong>of</strong> <strong>rosacea</strong>. J Dermatol Sci. 2009;<br />
55(2):77-81.<br />
26. Del Rosso JQ. Advances in understanding and managing <strong>rosacea</strong>: Part 1. connecting<br />
the dots between pathophysiological mechanisms and common clinical features<br />
<strong>of</strong> <strong>rosacea</strong> with emphasis on vascular changes and facial erythema. J Clin Aesthet<br />
Dermatol. 2012;5(3):16-25.<br />
27. Yamasaki K, Di Nardo A, Bardan A, Mrakami M, Ohtake T, Coda A, et al. Increased serine<br />
protease activity and cathelicidin promotes skin inflammation in <strong>rosacea</strong>. Nat Med.<br />
2007;13(8):975–80. Comment in: Nat Med. 2007;13(8):904-6.<br />
28. Meyer-H<strong>of</strong>fert U, Schroder JM. Epidermal proteases in the pathogenesis <strong>of</strong> <strong>rosacea</strong>.<br />
J Investig Dermatol Symp Proc. 2011;15(1):16-23.<br />
29. Schwab VD, Sulk M, Seeliger S, Nowak P, Aubert SM, Mess C, et al. Neurovascular and<br />
neuroimmune aspects in the pathophysiology <strong>of</strong> <strong>rosacea</strong>. J Investig Dermatol Symp<br />
Proc. 2011;15(1):53-62.<br />
30. Wladis EJ, Iglesias BV, Adam AP, Gosselin EJ. Molecular biologic assessment <strong>of</strong> cutaneous<br />
specimens <strong>of</strong> ocular <strong>rosacea</strong>. Ophthal Plast Reconstr Surg. 2012;28(4):246-50.<br />
31. Craw<strong>for</strong>d GH, Pelle M, James WD. Rosacea: I. Etiology, pathogenesis, and subtype<br />
classification. J Am Acad Dermatol. 2004;51(3):327-41; quiz 324-4. Comment in: J<br />
Am Acad Dermatol. 2005;53(6):1104-5. Comment on: J Am Acad Dermatol. 2002;<br />
46(4):584-7.<br />
32. Steinh<strong>of</strong>f M,Buddenkotte J, Aubert J, Sulk M, Novak P, Schwab VD, et al. Clinical, cellular,<br />
and molecular aspects in the pathophysiology <strong>of</strong> <strong>rosacea</strong>. J Investig Dermatol<br />
Symp Proc. 2011;15(1):2-11.<br />
33. Shanler SD, Ondo AL. Successful treatment <strong>of</strong> the erythema and flushing <strong>of</strong> <strong>rosacea</strong><br />
using a topically applied selective 1-adrenergic receptor agonist, oxymetazoline.<br />
Arch Dermatol. 2007;143(11):1369-71.<br />
34. Kim JH, Oh YS, Ji JH, Bak H, Ahn SK. Rosacea (erythematotelangiectatic type) effectively<br />
improved by topical xylometazoline. J Dermatol. 2011;38(5):510-3.<br />
35. Gomaa AH, Yaar M, Eyada MM, Bhawan J. Lymphangiogenesis and angiogenesis in<br />
non-phymatous <strong>rosacea</strong>. J Cutan Pathol. 2007;34(10):748-53.<br />
36. Smith JR, Lanier VB, Braziel RM, Falknhagen KM, White C, Rosenbaum JT. Expression<br />
<strong>of</strong> vascular endothelial growth factor and its receptors in <strong>rosacea</strong>. Br J Ophthalmol.<br />
2007;91(2):226-9.<br />
37. Kari O, Aho V, Peltonen S, Saari JM, Kari M, Maatta M, et al. Group IIA phospholipase<br />
A(2) concentration <strong>of</strong> tears in patients with ocular <strong>rosacea</strong>. Acta Ophthalmol Scand.<br />
2005;83(4):483-6.<br />
38. Lacey N, Delney S, Kavanagh K, Powell FC. Mite-related bacterial antigens stimulate<br />
inflammatory cells in <strong>rosacea</strong>. Br J Dermatol. 2007;157(3):474-81.<br />
39. Szlachic A, Silwowski Z, Karczewska E, Bielanski W, Pytko-Polonczk J, Konturek SJ.<br />
Helicobacter pylori and its eradication in <strong>rosacea</strong>. J Physiol Pharmacol. 1999;50(5):<br />
777-86.<br />
40. Diaz C, O´Callaghan CJ, Khan A, Allchyshyn A. Rosacea: a cutaneous marker <strong>of</strong><br />
Helicobacter pylori infection? Results <strong>of</strong> a pilot study. Acta Derm Venereol. 2003;<br />
83(4):282-6.<br />
41. Lazaridou E, Giannopoulou c, Fotiadou C, Vakirlis E, TRIGONI a, Ioannides D. The<br />
potential role <strong>of</strong> microorganisms in the development <strong>of</strong> <strong>rosacea</strong>. J Dtsch Dermatol<br />
Ges. 2011;9(1):21-5. German.<br />
42. O’Reilly N, Menezes N, Kavanagh K. Positive correlation between serum immunoreactivity<br />
to Demodex-associated Bacillus proteins and Erythematotelangiectic<br />
Rosacea. Br J Dermatol. 2012. [Epub ahead <strong>of</strong> print].<br />
43. Whitfeld M, Gunasingam N, Leow LJ, Shirato K, Preda V. Staphylococcus epidermidis:<br />
a possible role in the pustules <strong>of</strong> <strong>rosacea</strong>. J Am Acad Dermatol. 2011;64(1):49-52.<br />
44. Utaş S. Ozbakir S, Turasan A, Utas C. Helicobacter pylori eradication treatment reduces<br />
the severity <strong>of</strong> <strong>rosacea</strong>. J Am Acad Dermatol. 1999;40(3):433-5. Comment in: J Am<br />
Acad Dermatol. 2000;42(3):535-6; J Am Acad Dermatol. 2000;42(3):537-9; J Am Acad<br />
Dermatol. 2000;42(3):536-7.<br />
45. Szlachcic A. The link between Helicobacter pylori infection and <strong>rosacea</strong>. J Eur Acad<br />
Dermatol Venereol. 2002;16(4):328-33.<br />
46. Dakovic Z, Vesic S, Vukovic J, Milenkovic S, Jankovic Terzic K, Dukic S, et al. <strong>Ocular</strong><br />
<strong>rosacea</strong> and treatment <strong>of</strong> symptomatic Helicobacter pylori infection: a case series.<br />
Acta Dermatovenerol Alp Panonica Adriat. 2007;16(2):83-6.<br />
47. Herr H, Você CH. Relationship between Helicobacter pylori and <strong>rosacea</strong>: it may be a<br />
myth. J Korean Med Sci. 2000;15(5):551-4.<br />
48. Schneider MA, Skinner Jr RB, Rosenberg EW, Noah PW, Smith L, Zwarum A. Serological determination<br />
<strong>of</strong> Helicobacter pylori in <strong>rosacea</strong> patients and controls Clin Res. 1992;40:831A.<br />
49. Bam<strong>for</strong>d JT, Tiden RL, Blankush JL, Gangeness DE. Effect <strong>of</strong> treatment <strong>of</strong> Helicobacter<br />
pylori Infection on <strong>rosacea</strong>. Arch Dermatol. 1995;135(6):659-63.<br />
50. Li J, O´Reilly N, Sheha H, Katz R, Raju VK Kavanagh K, Tseng SC. Correlation between<br />
ocular Demodex infestation and serum immunoreactivity to Bacillus proteins in<br />
patients with facial <strong>rosacea</strong>. Ophthalmology. 2010;117(5):870-7.<br />
368 Arq Bras Oftalmol. 2012;75(5):363-9
Vieira ACC, et al.<br />
51. Lazaridou E, Fotiadou C, Ziakas NG, Giannopoulou C, Apalla Z, Ioannides D. Clinical<br />
and laboratory study <strong>of</strong> ocular <strong>rosacea</strong> in northern Greece. J Eur Acad Dermatol<br />
Venereol. 2011;25(12):1428-31.<br />
52. An HJ, Ninonuevo M, Aquilan J, Liu H, Lebrilla CB, Alvarenga LS, et al. Glycomics<br />
analyses <strong>of</strong> tear fluid <strong>for</strong> the diagnostic detection <strong>of</strong> ocular <strong>rosacea</strong>. J Proteome Res.<br />
2005;4)(6:1981-7.<br />
53. Vieira AC, Um HJ, Ozcan S, Kim JH, Lebrilla CB, Mannis MJ. Glycomic analysis <strong>of</strong> tear<br />
and saliva in ocular <strong>rosacea</strong> atients: the search <strong>for</strong> a biomarker. In: XXXIII International<br />
Congress <strong>of</strong> Ophthalmologry. Berlim, Germany, 16-20 feb 2012.<br />
54. Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification<br />
<strong>of</strong> <strong>rosacea</strong>: Report <strong>of</strong> the National Rosacea Society Expert Committee on the classification<br />
and staging <strong>of</strong> <strong>rosacea</strong>. J Am Acad Dermatol. 2002;46(4):584-7.Comment in:<br />
J Am Acad Dermatol. 2004;51(3):327-41; quiz 342-4.<br />
55. R O. The nosology <strong>of</strong> <strong>rosacea</strong>. Cutis. 2004;74(3 Suppl):5-8, 32-4.<br />
56. Wilkin J, Dahl M, Detmar M, Drake L, Liang MH, Odom R, Powell F; National Rosacea<br />
Society Expert Committee. Standard grading system <strong>for</strong> <strong>rosacea</strong>: report <strong>of</strong> the National<br />
Rosacea Society Expert Committee on the Classification and Staging <strong>of</strong> Rosacea. J<br />
Am Acad Dermatol 2004;50(6):907-12. Comment in: J Am Acad Dermatol. 2006;52(pt<br />
1):539-40.<br />
57. Miguel AI, Salgado MB, Lisboa MS, Henriques F, Paiva MC, Castela GP. Pediatric ocular<br />
<strong>rosacea</strong>: 2 cases. Eur J Ophthalmol. 2012;22(4):664-6.<br />
58. Chamaillard M, Mortemousque B, Boralevi F, Marques da Costa C, Aitali F, Taieb A, et al.<br />
Cutaneous and ocular signs <strong>of</strong> childhood <strong>rosacea</strong>. Arch Dermatol. 2008;144(2):167-71.<br />
59. Mavrakanas N, Schutz SJ, Dosso AA. Pediatric ocular <strong>rosacea</strong>. J Pediatr Ophthalmol<br />
Strabismus. 2010;47(2):117-20.<br />
60. Quarterman MJ, Johnson DW, Abele DC, Lesher JL Jr, Casco DS, Davis LS. <strong>Ocular</strong><br />
<strong>rosacea</strong>. Signs, symptoms, and tear studies be<strong>for</strong>e and after treatment with doxycycline.<br />
Arch Dermatol. 1997;133(1):49-54. Comment in: Arch Dermatol. 1997;<br />
133(1):89-90.<br />
61. Odom R, Dahi M, Dover J, Draelos Z, Drake L, Macsal M, Powell F, Thiboutot D, Webster<br />
GF, Wilkin J; National Rosacea Society Expert Committee on the Classification<br />
and Staging <strong>of</strong> Rosacea. Standard management options <strong>for</strong> <strong>rosacea</strong>, part 2: options<br />
according to <strong>rosacea</strong> subtype. Cutis. 2009;84(2):97-104.<br />
62. Keshtcar-Jafari A, Akhyani M, Ehsani AH, Ghiasi M, Lajevardi V, Baradran O, et al. Correlation<br />
<strong>of</strong> the severity <strong>of</strong> cutaneous <strong>rosacea</strong> with ocular <strong>rosacea</strong>. Indian J Dermatol<br />
Venereol Leprol. 2009;75(4):405-6.<br />
63. Gudmundsen KJ O´Donnell BF, Powell FC. Schirmer testing <strong>for</strong> dry eyes in patients<br />
with <strong>rosacea</strong>. J Am Acad Dermatol. 1992;26(2 Pt 1):211-4.<br />
64. Chen DM, Crosby DL. Periorbital edema as an initial presentation <strong>of</strong> <strong>rosacea</strong>. J Am<br />
Acad Dermatol. 1997;37(2 Pt 2):346-8.<br />
65. O’Donnell BF, Foulds IS. Visual impairment secondary to <strong>rosacea</strong> Br J Dermatol.<br />
1992;127(3):300-1.<br />
66. Morales-Burgos A, Alvarez Del manzano G, Sánchez JL, Cruz CL. Persistent eyelid<br />
swelling in a patient with <strong>rosacea</strong>. P R Health Sci J. 2009;28(1):80-2.<br />
67. Akpek EK, Merchant A, Pinar V, Foster CS. <strong>Ocular</strong> <strong>rosacea</strong>: patient characteristics and<br />
follow-up. Ophthalmology. 1997;104(11):1863-7.<br />
68. Ravage ZB, Beck AP, Macsai MS, Ching SS. <strong>Ocular</strong> <strong>rosacea</strong> can mimic trachoma: a case<br />
<strong>of</strong> cicatrizing conjunctivitis. Cornea. 2004;23(6):630-1.<br />
69. Lima KB, Sousa LB, Santos NC, Barros J de N, Antonio D. [Cost-benefit analysis <strong>of</strong><br />
ocular examination <strong>of</strong> patients with <strong>rosacea</strong>]. Arq Bras Oftalmol. 2005;68(1):37-43.<br />
Portuguese.<br />
70. Faraj HG, Hoan.g-Xuan T Chronic cicatrizing conjunctivitis. Curr Opin Ophthalmol.<br />
2001;12(4):250-7.<br />
71. Rahman MQ, Lim Y, Roberts F, Ramaesh K. Fibrosing blepharo-conjunctivitis following<br />
pyogenic granuloma in ocular acne <strong>rosacea</strong>. Ocul Immunol Inflamm. 2012;18(5):346-8.<br />
72. Gracner B, Pahor D, Gracner T. [Repair <strong>of</strong> an extensive corneoscleral per<strong>for</strong>ation<br />
in a case <strong>of</strong> ocular <strong>rosacea</strong> with a keratoplasty]. Klin Monbl Augenheilkd. 2006;<br />
223(10):841-3. German.<br />
73. Al Arfaj K, Al Zamil W. Spontaneous corneal per<strong>for</strong>ation in ocular <strong>rosacea</strong>. Middle East<br />
Afr J Ophthalmol. 2010;17(2):186-8.<br />
74. Jenkins MS, Brown SI, Lempert SL, Weinberg RJ. <strong>Ocular</strong> <strong>rosacea</strong>. Am J Ophthalmol.<br />
1979;88(3 Pt 2):618-22.<br />
75. Ramamurthi S, Rahman MQ, Dutton GN, Ramaesh K. Pathogenesis, clinical features<br />
and management <strong>of</strong> recurrent corneal erosions. Eye (Lond). 2006;20(6):635-44. Comment<br />
in: Eye (Lond). 2007;21(3):439-40. Eye (Lond). 2007;21(8):1128.<br />
76. Lee WB, Darlington JK, Mannis MJ, Schwab IR. Dendritic keratopathy in ocular <strong>rosacea</strong>.<br />
Cornea. 2005;24(5):632-3.<br />
77. Dursun D, Piniella AM, Pflugfelder SC. Pseudokeratoconus caused by <strong>rosacea</strong>. Cornea.<br />
2001;20(6):668-9.<br />
78. Jain V, Shome D, Natarajan S. Pseudodendritic keratitis in ocular <strong>rosacea</strong> causing a<br />
diagnostic dilemma. Indian J Ophthalmol. 2007;55(6):480-1.<br />
79. Jain V, Shome D, Sajnani M, Natarajan S. Fungal keratitis associated with ocular <strong>rosacea</strong>.<br />
Int Ophthalmol. 2010;30(3):239-44.<br />
80. Robertson DM, Cavanagh HD. Pseudomonas aeruginosa keratitis in an atopic silicone<br />
hydrogel lens wearer with <strong>rosacea</strong>. Eye Contact Lens. 2005;31(6):254-6.<br />
81. Vieira AC, Mannis MJ. Spontaneous scleral per<strong>for</strong>ation in ocular <strong>rosacea</strong>. Vision Pan-<br />
-Amer. 2009;8(1):149-51.<br />
82. Del Rosso JQ. Advances in understanding and managing <strong>rosacea</strong>: Part 2. The central<br />
role, evaluation, and medical management <strong>of</strong> diffuse and persistent facial erythema<br />
<strong>of</strong> <strong>rosacea</strong>. J Clin Aesthet Dermatol. 2012;5(3):26-36.<br />
83. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad<br />
Dermatol Venereol. 2005;19(3):273-85.<br />
84. van Zuuren EJ, Kramer SF, Carter BR, Graber MA, Fedorowicz Z. Effective and<br />
evidence-based management strategies <strong>for</strong> <strong>rosacea</strong>: summary <strong>of</strong> a Cochrane systematic<br />
review. Br J Dermatol. 2011;165(4):760-81. Comment in: Br J Dermatol. 2011;<br />
165(4):707-8.<br />
85. van Zuuren EJ, Karmer S, Carter B, Graber MA, Fedorowicz Z. Interventions <strong>for</strong> Rosacea.<br />
Cochrane Database Syst Rev. 2011;16(3):CD003262.<br />
86. Gooderham M. Rosacea and its topical management. Skin Therapy Lett. 2009;14(2):1-3.<br />
87. Wolf JE Jr, Kerrouche N, Arsonnaud S. Efficacy and safety <strong>of</strong> once-daily metronidazole<br />
1% gel compared with twice-daily azelaic acid 15% gel in the treatment <strong>of</strong> <strong>rosacea</strong>.<br />
Cutis. 2006;77(4 Suppl):3-11.<br />
88. Barnhorst DA Jr, Foster JA, Chern KC, Meisler DM. The efficacy <strong>of</strong> topical metronidazole<br />
in the treatment <strong>of</strong> ocular <strong>rosacea</strong>. Ophthalmology.. 1996;103(11):1880-3.<br />
89. Pelle MT, Craw<strong>for</strong>d GH, James WD. Rosacea: II. Therapy. J Am Acad Dermatol.<br />
2004;51(4):499-512; quiz 513-4.<br />
90. Kim JH, Oh Y, Choi EH. Oral azithromycin <strong>for</strong> treatment <strong>of</strong> intractable <strong>rosacea</strong>. J Korean<br />
Med Sci. 2011;26(5):694-6.<br />
91. Modi S, Harling M, Rosen T. Azithromycin as an alternative <strong>rosacea</strong> therapy when<br />
tetracyclines prove problematic. J Drugs Dermatol. 2008;7(9):898-9.<br />
92. Park H, Dell Rosso JQ. Use <strong>of</strong> oral isotretinoin in the management <strong>of</strong> <strong>rosacea</strong>. J Clin<br />
Aesthet Dermatol. 2011;4(9):54-61.<br />
93. Fowler J, Jarrat M, Moore A, Meadows K, Pollack A, Steinholf M, Liu Y, Leoni M; Brimonidine<br />
Phase II study Group. Once-daily topical brimonidine tartrate gel 0.5% is a novel<br />
treatment <strong>of</strong> moderate to severe facial erythema <strong>of</strong> <strong>rosacea</strong>: results <strong>of</strong> two multicenter,<br />
randomized and vehicle-controlled studies. Br J Dermatol. 2012;166(3):633-41.<br />
94. Odom R, Dahl M, Dover J, Draelos Z, Drake L, Macsai M, Powell F, Thiboutot D, Webster<br />
GF, Wilkin J; National Rosacea society Expert Committee on the Classification and<br />
Staging <strong>of</strong> Roasacea. Standard management options <strong>for</strong> <strong>rosacea</strong>, Part 1: overview<br />
and broad spectrum <strong>of</strong> care. Cutis. 2009;84(1):43-7.<br />
95. Schechter BA, Katz RS, Friedman LS. Efficacy <strong>of</strong> topical cyclosporine <strong>for</strong> the treatment<br />
<strong>of</strong> ocular <strong>rosacea</strong>. Adv Ther. 2009;26(6):651-9.<br />
96. Goldgar C, Keahey DJ, Houchins J. Treatment options <strong>for</strong> acne <strong>rosacea</strong>. Am Fam Phys.<br />
2009;80(5):461-8.<br />
97. Stone DU, Chodosh J. Oral tetracyclines <strong>for</strong> ocular <strong>rosacea</strong>: an evidence-based review<br />
<strong>of</strong> the literature. Cornea. 2004;23(1):106-9.<br />
98. Valentin S, Morales A, Sánchez JL, Rivera A. Safety and efficacy <strong>of</strong> doxycycline in the<br />
treatment <strong>of</strong> <strong>rosacea</strong>. Clin Cosmet Investig Dermatol. 2009;2:129-40.<br />
99. Pfeffer I, Borelli C, Zierhut M, Schaller M. Treatment <strong>of</strong> ocular <strong>rosacea</strong> with 40 mg<br />
doxycycline in a slow release <strong>for</strong>m. J Dtsch Dermatol Ges. 2011;9(11):904-7.<br />
100. Donnenfeld E, Plufgfelder SC. Topical ophthalmic cyclosporine: pharmacology and<br />
clinical uses. Surv Ophthalmol. 2009;54(3):321-38. Comment in: Surv Ophthalmol.<br />
2010;55(2):189; author reply 189,<br />
101. Hong E, Fischer G. Childhood ocular <strong>rosacea</strong>: considerations <strong>for</strong> diagnosis and treatment.<br />
Australas J Dermatol. 2009;50(4):272-5.<br />
102. Jain AK, Sukhija J. Amniotic membrane transplantation in ocular <strong>rosacea</strong>. Ann<br />
Ophthalmol (Skokie). 2007;39(1):71-3.<br />
103. Sandinha T, Zaher SS, Roberts F, Devlin HC, Dhillon B, Ramaesh K. Superior <strong>for</strong>niceal<br />
conjunctival advancement pedicles (SFCAP) in the management <strong>of</strong> acute and impending<br />
corneal per<strong>for</strong>ations. Eye (Lond). 2006;20(1):84-9. Comment in: Eye (Lond).<br />
2007;21(2):283-4; Eye (Lond). 2006; 20(12):1468.<br />
104. Bodaghi B, Levy C, Votan P, Hoang-Xuan T. [Value <strong>of</strong> cyanoacrylate tissue adhesives in<br />
peripheral corneal ulcers <strong>of</strong> inflammatory origin]. J Fr Ophtalmol. 1996;19(2):127-32.<br />
French.<br />
Arq Bras Oftalmol. 2012;75(5):363-9<br />
369
Cartas ao Editor | Letters to the Editor<br />
Axonal electrovisiogram or inverse photopic skin electroretinogram?<br />
Eletrovisograma axonal ou eletrorretinograma fotópico inverso de pele?<br />
Katharina Messias 1 , Vinicius Monteiro de Castro 1 , Florian Gekeler 2 , Andre Messias 1<br />
Dear Editor,<br />
We would like to discuss the very interesting article “Axonal electrovisiogram<br />
as an electrophysiological test to evaluate optic nerve<br />
and inner retina electrical potentials: findings in normal subjects”,<br />
published in the 74(1) issue <strong>of</strong> Arquivos Brasileiros de Oftalmologia (1) .<br />
In this work, authors recorded electrophysiological potentials using<br />
the Axonal electrovisiogram (AxEvg) paradigm, which is a method<br />
developed by Sabadel et al. (2) , to record pre-chiasmatic electric potentials,<br />
in normal subjects.<br />
The study is well designed and is nicely reported in the article,<br />
but some major concerns must be made about the origin <strong>of</strong> these<br />
electrical responses.<br />
In this experiment an interference <strong>of</strong> retinal electric potentials<br />
- the electroretinogram (ERG) - cannot be ruled out, since AxEvg is<br />
recorded with electrodes placed very closely to the eye, in a similar<br />
configuration used <strong>for</strong> skin ERG (sERG) (3,4) .<br />
Interestingly, the difference between electrode placement <strong>for</strong><br />
AxEvg and sERG is that the electrode placed closest to the eye is the<br />
negative pole, which might explain the wave<strong>for</strong>m configuration<br />
found in AxEvg recordings. Figure 1 shows electrode placements <strong>for</strong><br />
AxEvg and sERG.<br />
In matter <strong>of</strong> fact, placing the negative pole as the closest electrode<br />
to the eye, regardless <strong>of</strong> the position <strong>of</strong> the positive pole (placed<br />
on ear lobe in case <strong>of</strong> AxEvg or placed below the eye in case <strong>of</strong> sERG),<br />
and stimulating the retina with a strong light flash (2.5 cd.s/m 2 ) using<br />
a Ganzfeld bowl, one cannot avoid the hypothesis <strong>of</strong> the electrical<br />
response to be generated by the retina and presenting as an ERG<br />
with inverse polarity.<br />
Interestingly, the wave<strong>for</strong>m shown by Cella et al. (1) , presents the<br />
same characteristics <strong>of</strong> a photopic ERG response, but recorded with<br />
inverse polarity, with P1 being the a-wave and N1 the b-wave.<br />
To investigate the origin <strong>of</strong> these electrical potentials we per<strong>for</strong>med<br />
recordings using the same electrode configuration and<br />
stimulus parameters used by Cella et al. in a patient with optic chiasm<br />
dissection after a tuberculum sellae meningioma surgery 1 year<br />
earlier (no light perceptions in both eyes ever since). To pro<strong>of</strong> the<br />
retinal origin <strong>of</strong> the AxEvg the electrodes in left eye were placed as<br />
mentioned by Cella at al., whereas, the electrodes in right eye were<br />
placed at the conjunctiva (DTL electrodes were used as negative<br />
pole) and at the earlobe (positive pole) (demonstrated in Figure 1).<br />
Two single flash stimulus intensities were used to pro<strong>of</strong> relationship<br />
between stimulus intensity and amplitude. Finally, 30 Hz flicker was<br />
per<strong>for</strong>med.<br />
Figure 1. Electrode placement <strong>for</strong> AxEvg and sERG. (Left) AxEvg: ground electrode is placed on patient´s <strong>for</strong>ehead, negative electrode at the outer<br />
eye canthus and positive electrode at ipsilateral earlobe. (Right) sERG: ground electrode is placed at earlobe, negative electrode is placed at outer<br />
eye canthus and the positive electrode is placed below the eye.<br />
Submitted <strong>for</strong> publication: September 2, 2012<br />
Accepted <strong>for</strong> publication: September 30, 2012<br />
1<br />
Department <strong>of</strong> Ophthalmology, Otorhinolaryngology and Head and Neck Surgery, School <strong>of</strong> Medicine<br />
<strong>of</strong> Ribeirão Preto - Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil.<br />
2<br />
Center <strong>for</strong> Ophthalmology, University <strong>of</strong> Tübingen, Schleichstraße 12-16, D-72076 Tübingen,<br />
Germany.<br />
Funding: No specific financial support was available <strong>for</strong> this study.<br />
Disclosure <strong>of</strong> potential conflicts <strong>of</strong> interest: K.Messias, None; V.M.de castro, None; F.Gekeler, None;<br />
A.Messias, None.<br />
370 Arq Bras Oftalmol. 2012;75(5):370-1
Messias K, et al.<br />
Figure 2. Potentials recorded from patient with dissected chiasm using AxEvg (red line) and inverted sERG techniques (blue line). (Top) 2.5 cd.s/m 2 stimulus; (Middle) 3 cd.s/m 2<br />
stimulus; (Bottom) 30 Hz Flicker stimulus.<br />
Interestingly, we can observe the same potential configuration, in<br />
both eyes even though we per<strong>for</strong>med the AxEvg in the left eye and<br />
a modified sERG in the right eye. Latencies <strong>for</strong> P1 and N1 are corresponding<br />
in both eyes (see Figure 2). Because <strong>of</strong> the greater spatial<br />
proximity <strong>of</strong> the DTL electrode to the retina, amplitudes in the right<br />
eye are higher when compared to left eye. As the patient does not<br />
posses any functional optic nerve at neither <strong>of</strong> both sides, the only<br />
explicable origin <strong>of</strong> the measured potentials must be the retina. As<br />
we placed the negative electrode in contact with the eye rather than<br />
the positive, as it is use in ERG recording, we have a negative potential<br />
configuration. Note the corresponding latencies <strong>of</strong> the inverted ERG<br />
in figure 2. Furthermore, we can observe stimulus intensity correlation<br />
<strong>of</strong> the recorded potential, which speaks strongly in favor <strong>for</strong><br />
electroretinographic origin <strong>of</strong> the measured potential.<br />
In conclusion, this data shows that the recorded electrical potentials<br />
using electrode placement proposed by Sabadel et al. (2) , <strong>for</strong> assessment<br />
<strong>of</strong> pre-chiasmatical potentials or evaluation <strong>of</strong> optic nerve<br />
function, and carried out by Cella et al. (1) , originate in the retina and<br />
are not optic nerve potentials. Future users should be aware <strong>of</strong> the<br />
electrical potentials generation to better understand its applications.<br />
The normative data shown by Cella et al., is still very valuable, since<br />
sERG can be very useful, especially <strong>for</strong> retinal function evaluation in<br />
children.<br />
With kind regards,<br />
Katharina Messias<br />
Vinicius de Castro<br />
Florian Gekeler<br />
André Messias<br />
References<br />
1. Cella W, Dantas AM, Lima AV, Avila MP. Axonal electrovisiogram as an electrophysiological<br />
test to evaluate optic nerve and inner retina electrical potentials: findings in<br />
normal subjects. Arq Bras Oftalmol. 2011;74(1):37-43.<br />
2. Sabadel A, Dalens H, Sole P. [Axonal electrovisiogram. Recording technic-clinical<br />
value]. Bull Soc Ophtalmol Fr. 1983;83(5):739-44. French.<br />
3. Giltrow-Tyler JF, Crews SJ, Drasdo N. Electroretinography with noncorneal and corneal<br />
electrodes. Invest Ophthalmol Vis Sci. 1978;17(11):1124-27.<br />
4. McCulloch DL, Van Boemel GB, Borchert MS. Comparisons <strong>of</strong> contact lens, foil, fiber<br />
and skin electrodes <strong>for</strong> patterns electroretinograms. Doc Ophthalmol. 1997;94(4):<br />
327-40.<br />
Arq Bras Oftalmol. 2012;75(5):370-1<br />
371
Instruções para Autores | Instructions to Authors<br />
O ARQUIVOS BRASILEIROS DE OFTALMOLOGIA (ABO, ISSN 0004-<br />
2749 - versão impressa e ISSN 1678-2925 - versão eletrônica), publicação<br />
bimestral <strong>of</strong>icial do Conselho Brasileiro de Oftalmologia, obje -<br />
tiva divulgar estudos científicos em Oftalmologia, Ciências Visuais e<br />
Saúde Pública, fomentando a pesquisa, o aperfeiçoamento e a atualização<br />
dos pr<strong>of</strong>issionais relacionados à área.<br />
Metodologia<br />
São aceitos manuscritos originais, em português, inglês ou<br />
espanhol que, de acordo com a metodologia empregada, deverão<br />
ser caracterizados em uma das seguintes modalidades:<br />
Estudos Clínicos<br />
Estudos descritivos ou analíticos que envolvam análises em<br />
seres humanos ou avaliem a literatura pertinente a seres humanos.<br />
Estudos Epidemiológicos<br />
Estudos analíticos que envolvam resultados populacionais.<br />
Estudos de Experimentação Laboratorial<br />
Estudos descritivos ou analíticos que envolvam modelos ani -<br />
mais ou outras técnicas biológicas, físicas ou químicas.<br />
Estudos Teóricos<br />
Estudos descritivos que se refiram à descrição e análise teórica<br />
de novas hipóteses propostas com base no conhecimento existente<br />
na literatura.<br />
Tipos de Manuscritos<br />
A <strong>for</strong>ma do manuscrito enviado deve enquadrar-se em uma das<br />
categorias a seguir. Os limites para cada tipo de manuscrito estão<br />
entre parênteses ao final das descrições das categorias. A contagem<br />
de palavras do manuscrito refere-se do início da introdução ao final<br />
da discussão, portanto, não participam da contagem a página de<br />
rosto, abstract, resumo, referências, agradecimentos, tabelas e figu -<br />
ras incluindo legendas.<br />
Editoriais<br />
Os editoriais são feitos a convite e devem ser referentes a<br />
assuntos de interesse atual, preferencialmente relacionados a arti -<br />
gos publicados no mesmo fascículo do ABO (limites máximos: 1.000<br />
palavras, título, 2 figuras ou tabelas no total e 10 referências).<br />
Artigos Originais<br />
Artigos originais apresentam experimentos completos com<br />
resultados nunca publicados (limites máximos: 3.000 palavras, tí -<br />
tulo, resumo estruturado, 7 figuras ou tabelas no total e 30 referências).<br />
A avaliação dos manuscritos enviados seguirá as prioridades<br />
abaixo:<br />
1. In<strong>for</strong>mação nova e relevante comprovada em estudo com<br />
metodologia adequada.<br />
2. Repetição de in<strong>for</strong>mação existente na literatura ainda não<br />
comprovada regionalmente baseada em estudo com metodologia<br />
adequada.<br />
3. Repetição de in<strong>for</strong>mação existente na literatura e já compro vada<br />
regionalmente, desde que baseada em estudo com me todologia<br />
adequada.<br />
* Não serão aceitos manuscritos com conclusões especulativas, não<br />
comprovadas pelos resultados ou baseadas em estudo com metodologia<br />
inadequada.<br />
Relatos de Casos ou Série de Casos<br />
Relatos de casos ou série de casos serão considerados para<br />
publicação se descreverem achados com raridade e originalidade<br />
ainda não comprovadas internacionalmente, ou quando o relato<br />
apresentar respostas clínicas ou cirúrgicas que auxiliem na elu -<br />
cidação fisiopatológica de alguma doença (limites máximos: 1.000<br />
pa lavras, título, resumo não estruturado, 4 figuras ou tabelas no<br />
total e 10 referências).<br />
Cartas ao Editor<br />
As cartas ao editor serão consideradas para publicação se incluírem<br />
comentários pertinentes a manuscritos publicados anteriormente<br />
no ABO ou, excepcionalmente, resultados de estudos origi -<br />
nais com conteúdo insuficiente para serem enviados como Artigo<br />
Original. Elas devem introduzir nova in<strong>for</strong>mação ou nova interpre -<br />
tação de in<strong>for</strong>mação já existente. Quando seu conteúdo fizer referência<br />
a algum artigo publicado no ABO, este deve estar citado no<br />
primeiro parágrafo e constar das referências. Nestes casos, as cartas<br />
estarão associadas ao artigo em questão, e o direito de réplica dos<br />
autores será garantido na mesma edição. Não serão publicadas cartas<br />
de congratulações (limites máximos: 700 palavras, título, 2 figuras<br />
ou tabelas no total e 5 referências).<br />
Manuscritos de Revisão<br />
Manuscritos de revisão seguem a linha editorial da revista e são<br />
aceitos apenas por convite do editor. Sugestões de assuntos para<br />
artigos de revisão podem ser feitas diretamente ao editor, mas os<br />
manuscritos não podem ser enviados sem um convite prévio (limi-<br />
tes máximos: 4.000 palavras, título, resumo não estruturado, 8 figuras<br />
ou tabelas no total e 100 referências).<br />
Processo Editorial<br />
Para que o manuscrito ingresse no processo editorial, é fundamental<br />
que todas as regras tenham sido cumpridas. A secretaria<br />
editorial comunicará inadequações no envio do manuscrito. Após<br />
a notificação, o autor correspondente terá o prazo de 30 dias para<br />
adequação do seu manuscrito. Se o prazo não <strong>for</strong> cumprido, o ma -<br />
nuscrito será excluído.<br />
Os manuscritos enviados ao ABO são avaliados inicialmente<br />
pelos editores quanto à adequação do seu conteúdo à linha edito -<br />
rial do periódico. Após essa avaliação, todos os manuscritos são<br />
encaminhados para análise e avaliação por pares, sendo o anonima -<br />
to dos avaliadores garantido em todo o processo de julgamento. O<br />
anonimato dos autores não é implementado.<br />
Após a avaliação editorial inicial, os comentários dos avaliado -<br />
res podem ser encaminhados aos autores como orientação para as<br />
mo dificações que devam ser realizadas no texto. Após a implemen<br />
ta ção das modificações sugeridas pelos avaliadores, o manuscrito<br />
re visado deverá ser encaminhado, acompanhado de carta<br />
(enviada como documento suplementar) indicando pon tual mente<br />
todas as modificações realizadas no manuscrito ou os motivos<br />
pelos quais as modificações sugeridas não <strong>for</strong>am efetuadas. Manuscritos<br />
que não vierem acompanhados da carta indicando as<br />
modificações ficarão retidos aguardando o recebimento da mesma.<br />
O prazo para envio da nova versão do manuscrito é de 90 dias<br />
após a comunicação da necessidade de modificações, sendo<br />
ex cluído após esse prazo. A publicação dependerá da aprovação<br />
final dos editores.<br />
Os trabalhos devem destinar-se exclusivamente ao Arquivos<br />
Brasileiros de Oftalmologia, não sendo permitido envio simultâneo<br />
a outro periódico, nem sua reprodução total ou parcial, ou<br />
tradução para publicação em outro idioma, sem autorização dos<br />
editores.<br />
Arq Bras Oftalmol. 2012;75(5):373-6<br />
373
Autoria<br />
Os critérios para autoria de manuscritos em periódicos médi -<br />
cos está bem estabelecido. O crédito de autoria deve ser baseado<br />
em indivíduos que tenham contribuído de maneira concreta nas<br />
seguintes três fases do manuscrito:<br />
I. Concepção e delineamento do estudo, coleta dos dados ou<br />
análise e interpretação dos dados.<br />
II. Redação do manuscrito ou revisão crítica do manuscrito com<br />
relação ao seu conteúdo intelectual.<br />
III. Aprovação final da versão do manuscrito a ser publicada.<br />
O ABO requer que os autores garantam que todos os autores<br />
preenchem os critérios acima e que nenhuma pessoa que preencha<br />
esses critérios seja preterida da autoria. Apenas a posição de chefia<br />
de qualquer indivíduo não atribui a este o papel de autor, o ABO não<br />
aceita a participação de autores honorários.<br />
É necessário que o autor correspondente preencha e envie o<br />
<strong>for</strong>mulário de Declaração de Contribuição dos Autores como docu -<br />
mento suplementar.<br />
Preparação do Artigo<br />
Os artigos devem ser enviados exclusivamente de <strong>for</strong>ma eletrônica,<br />
pela Internet, na interface apropriada do ABO. As normas que se<br />
seguem <strong>for</strong>am baseadas no <strong>for</strong>mato proposto pelo Inter na tional<br />
Com mittee <strong>of</strong> Medical Journal Editors (ICMJE) e publicadas no artigo:<br />
Uni<strong>for</strong>m Requirements <strong>for</strong> Manuscripts Submitted to Bio medical Journals.<br />
O respeito às instruções é condição obrigatória para que o tra -<br />
balho seja considerado para análise.<br />
O texto deve ser enviado em <strong>for</strong>mato digital, sendo aceitos<br />
apenas os <strong>for</strong>matos .doc. ou .rtf. O corpo do texto deve ser digitado<br />
em espaço duplo, fonte tamanho 12, com páginas numeradas em<br />
al garismos arábicos, iniciando-se cada seção em uma nova pági na.<br />
As seções devem se apresentar na sequência: Página de Rosto,<br />
Abstract e Keywords, Resumo e Descritores, Introdução, Métodos,<br />
Resultados, Discussão Agradecimentos (eventuais), Referências, Tabelas<br />
(opcionais) e Figuras (opcionais) com legenda.<br />
1. Página de Rosto. Deve conter: a) título em inglês (máximo<br />
de 135 caracteres, incluindo espaços); b) título em português ou<br />
es panhol (máximo de 135 caracteres, incluindo espaços); c) tí tulo<br />
resumido para cabeçalho (máximo 60 caracteres, incluindo os<br />
es paços); d) nome científico de cada autor; e) titulação de cada<br />
autor (área de atuação pr<strong>of</strong>issional*, cidade, estado, país e, quando<br />
houver, depar tamento, escola, Universidade); f ) nome, endereço,<br />
telefone e e-mail do autor correspondente; g) fontes de auxilio<br />
à pesquisa (se hou ver); h) número do projeto e instituição responsável<br />
pelo parecer do Co mitê de Ética em Pesquisa; i) declaração dos<br />
conflitos de in teresses de todos os autores; j) número do registro<br />
dos ensaios clí nicos em uma base de acesso público.<br />
*Médico, estatístico, enfermeiro, ortoptista, fisioterapeuta, estudante etc.<br />
Aprovação do Comitê de Ética em Pesquisa. Todos os estudos<br />
que envolvam coleta de dados primários ou relatos clínico-cirúrgicos,<br />
sejam retrospectivos, transversais ou prospectivos, de vem<br />
indicar, na página de rosto, o número do projeto e nome da Instituição<br />
que <strong>for</strong>neceu o parecer do Comitê de Ética em Pes quisa.<br />
As pesquisas em seres humanos devem seguir a Declaração de<br />
Helsinque, enquanto as pesquisas envolvendo animais devem<br />
seguir os princí pios propostos pela Association <strong>for</strong> Research in Vision<br />
and Oph thal mo logy (ARVO).<br />
É necessário que o autor correspondente envie, como documento<br />
suplementar, a aprovação do Comitê de Ética em Pesquisa ou seu<br />
parecer dispensando da avaliação do projeto pelo Comitê. Não cabe<br />
ao autor a decisão sobre a necessidade de avaliação pelo Comitê de<br />
Ética em Pesquisa.<br />
Declaração de Conflito de Interesses. A página de rosto deve<br />
conter a declaração de conflitos de interesse de todos os autores<br />
(mesmo que esta seja inexistente). Para maiores in<strong>for</strong>mações sobre<br />
os potenciais conflitos de interesse acesse: Chamon W, Melo LA Jr,<br />
Paranhos A Jr. Declaração de conflito de interesse em apresentações<br />
e publicações científicas. Arq Bras Oftalmol. 2010;73(2):107-9.<br />
É necessário que todos os autores enviem os Formulários para Declaração<br />
de Conflitos de Interesse como documentos suplementares.<br />
Ensaios Clínicos. Todos os Ensaios Clínicos devem indicar, na pá gina<br />
de rosto, número de registro em uma base internacional de re gis -<br />
tro que permita o acesso livre a consulta (exemplos: U.S. Na tional<br />
Ins ti tutes <strong>of</strong> Health, Australian and New Zealand Clinical Trials<br />
Registry, Inter national Standard Randomised Controlled Trial Num ber<br />
- ISRCTN, University Hos pital Medical In<strong>for</strong>mation Net work Clinical Trials<br />
Registry - UMIN CTR, Ne derlands Trial Register).<br />
2. Abstract e Keywords. Resumo estruturado (Purpose, Methods,<br />
Re sults, Conclusions) com, no máximo, 300 palavras. Resumo não<br />
estruturado com, no máximo, 150 palavras. Citar cinco descritores<br />
em inglês, listados pela National Library <strong>of</strong> Medicine (MeSH - Medical<br />
Subject Headings).<br />
3. Resumo e Descritores. Resumo estruturado (Objetivos, Méto -<br />
dos, Resultados, Conclusões) com, no máximo 300 palavras. Resumo<br />
não estruturado com, no máximo, 150 palavras. Citar cinco descritores,<br />
em português listados pela BIREME (DeCS - Descritores<br />
em Ciências da Saúde).<br />
4. Introdução, Métodos, Resultados e Discussão. As citações no<br />
texto devem ser numeradas sequencialmente, em números arábi -<br />
cos sobrescritos e entre parênteses. É desaconselhada a citação<br />
no minal dos autores.<br />
5. Agradecimentos. Colaborações de pessoas que mereçam<br />
re conhecimento, mas que não justificam suas inclusões como<br />
auto res, devem ser citadas nessa seção. Estatísticos e editores médicos<br />
po dem preencher os critérios de autoria e, neste caso, de vem<br />
ser reconhecidos como tal. Quando não preencherem os critérios<br />
de autoria, eles deverão, obrigatoriamente, ser citados nesta<br />
seção. Não são aceitos escritores não identificados no manus -<br />
crito, portanto, escritores pr<strong>of</strong>issionais devem ser reconhecidos<br />
nes ta seção.<br />
6. Referências. A citação (referência) dos autores no texto deve<br />
ser numérica e sequencial, na mesma ordem que <strong>for</strong>am citadas<br />
e identificadas por algarismos arábicos sobrescritos. A apresen tação<br />
deve estar baseada no <strong>for</strong>mato proposto pelo International<br />
Com mittee <strong>of</strong> Medical Journal Editors (ICMJE), con<strong>for</strong>me os exem -<br />
plos que se seguem.<br />
Os títulos de periódicos devem ser abreviados de acordo com o<br />
estilo apresentado pela List <strong>of</strong> Journal Indexed in Index Medicus, da<br />
National Library <strong>of</strong> Medicine.<br />
Para todas as referências, cite todos os autores, até seis. Nos traba -<br />
lhos com sete ou mais autores, cite apenas os seis primeiros,<br />
seguidos da expressão et al.<br />
Exemplos de referências:<br />
Artigos de Periódicos<br />
Costa VP, Vasconcellos JP, Comegno PEC, José NK. O uso da mitomicina<br />
C em cirurgia combinada. Arq Bras Oftalmol. 1999; 62(5):577-80.<br />
Livros<br />
Bicas HEA. Oftalmologia: fundamentos. São Paulo: Contexto; 1991.<br />
374 Arq Bras Oftalmol. 2012;75(5):373-6
Capítulos de livros<br />
Gómez de Liaño F, Gómez de Liaño P, Gómez de Liaño R. Exploración<br />
del niño estrábico. In: Horta-Barbosa P, editor. Estrabismo. Rio de<br />
Ja neiro: Cultura Médica; 1997. p. 47-72.<br />
Anais<br />
Höfling-Lima AL, Bel<strong>for</strong>t R Jr. Infecção herpética do recém-nascido.<br />
In: IV Congresso Brasileiro de Prevenção da Cegueira; 1980 Jul 28-30,<br />
Belo Horizonte, Brasil. Anais. Belo Horizonte; 1980. v.2. p. 205-12.<br />
Teses<br />
Schor P. Idealização, desenho, construção e teste de um cera tô -<br />
metro cirúrgico quantitativo [tese]. São Paulo: Universidade Federal<br />
de São Paulo; 1997.<br />
Documentos Eletrônicos<br />
Monteiro MLR, Scapolan HB. Constrição campimétrica causada por<br />
vigabatrin. Arq Bras Oftalmol. [periódico na Internet]. 2000 [citado<br />
2005 Jan 31]; 63(5): [cerca de 4 p.]. Disponível em:http://www.scielo.<br />
br/scielo.php?script=sci_arttext&pid=S0004-274920000005000<br />
12&lng=pt&nrm=iso<br />
7. Tabelas. A numeração das tabelas deve ser sequencial, em algarismos<br />
arábicos, na ordem em que <strong>for</strong>am citadas no texto. Todas<br />
as tabelas devem ter título e cabeçalho para todas as colunas<br />
e se rem apresentadas em <strong>for</strong>matação simples, sem linhas verticais<br />
ou preen chimentos de fundo. No rodapé da tabela deve constar<br />
legenda para todas as abreviaturas (mesmo que definidas previamente<br />
no texto) e testes estatísticos utilizados, além da fonte<br />
bi bliográfica quando extraída de outro trabalho. Todas as tabelas<br />
devem estar contidas no documento principal do manuscrito após<br />
as referências bibliográficas, além de serem enviadas como documento<br />
suplementar.<br />
8. Figuras (gráficos, fotografias, ilustrações, quadros). A nu -<br />
meração das figuras deve ser sequencial, em algarismos arábi -<br />
cos, na ordem em que <strong>for</strong>am citadas no texto. O ABO publicará as<br />
figuras em preto e branco sem custos para os autores. Os manus -<br />
critos com figuras coloridas apenas serão publicados após o<br />
pagamento da respectiva taxa de publicação de R$ 500,00 por<br />
manuscrito.<br />
Os gráficos devem ser, preferencialmente, em tons de cinza, com<br />
fundo branco e sem recursos que simulem 3 dimensões ou pr<strong>of</strong>undidade.<br />
Gráficos do tipo torta são dispensáveis e devem ser substituídos<br />
por tabelas ou as in<strong>for</strong>mações serem descritas no texto.<br />
Fotografias e ilustrações devem ter resolução mínima de 300 DPI<br />
para o tamanho final da publicação (cerca de 2.500 x 3.300 pixels,<br />
para página inteira). A qualidade das imagens é considerada na<br />
avaliação do manuscrito.<br />
Todas as figuras devem estar contidas no documento principal do<br />
manuscrito após as tabelas (se houver) ou após as referências bibliográficas,<br />
além de serem enviadas como documento suplementar.<br />
No documento principal, cada figura deve vir acompanhada de sua<br />
respectiva legenda em espaço duplo e numerada em algarismo<br />
arábico.<br />
Os arquivos suplementares enviados podem ter as seguintes extensões:<br />
JPG, BMP, TIF, GIF, EPS, PSD, WMF, EMF ou PDF, e devem<br />
ser nomeados con<strong>for</strong>me a identificação das figuras, por exemplo:<br />
“grafico_1.jpg” ou “figura_1A.bmp”.<br />
9. Abreviaturas e Siglas. Quando presentes, devem ser precedidas<br />
do nome correspondente completo ao qual se referem, quando<br />
ci tadas pela primeira vez, e nas legendas das tabelas e figuras<br />
(mesmo que tenham citadas abreviadas anteriormente no texto).<br />
Não devem ser usadas no título e no resumo.<br />
10. Unidades: Valores de grandezas físicas devem ser referidos de<br />
acordo com os padrões do Sistema Internacional de Unidades.<br />
11. Linguagem. A clareza do texto deve ser adequada a uma<br />
pu blicação científica. Opte por sentenças curtas na <strong>for</strong>ma direta e<br />
ati va. Quando o uso de uma palavra estrangeira <strong>for</strong> absolutamente<br />
ne cessário, ela deve aparecer com <strong>for</strong>matação itálica. Agentes<br />
te ra pêuticos devem ser indicados pelos seus nomes genéricos<br />
seguidos, entre parênteses, pelo nome comercial, fabricante, cidade,<br />
es tado e país de origem. Todos os instrumentos ou apare -<br />
lhos de fabricação utilizados devem ser citados com o seu nome<br />
comercial, fabricante, cidade, estado e país de origem. É necessária<br />
a colocação do símbolo (sobrescrito) de marca registrada ® ou <br />
em todos os nomes de instrumentos ou apresentações comerciais<br />
de drogas. Em situações de dúvidas em relação a estilo, terminologia,<br />
medidas e assuntos correlatos, o AMA Manual <strong>of</strong> Style 10th<br />
edition deverá ser consultado.<br />
12. Documentos Originais. Os autores correspondentes devem ter<br />
sob sua guarda os documentos originais como a carta de aprovação<br />
do comitê de ética institucional para estudos com humanos ou<br />
animais; o termo de consentimento in<strong>for</strong>mado assinado por todos<br />
os pacientes envolvidos, a declaração de concordância com o conteúdo<br />
completo do trabalho assinada por todos os autores e declaração<br />
de conflito de interesse de todos os autores, além dos re gistros<br />
dos dados colhidos para os resultados do trabalho.<br />
13. Correções e Retratações. Erros podem ser percebidos após a<br />
publicação de um manuscrito que requeiram a publicação de<br />
uma correção. No entanto, alguns erros, apontados por qualquer<br />
leitor, podem invalidar os resultados ou a autoria do manuscrito.<br />
Se al guma dúvida concreta a respeito da honestidade ou fidedignidade<br />
de um manuscrito enviado para publicação <strong>for</strong> levantada,<br />
é obri gação do editor excluir a possibilidade de fraude. Nestas<br />
si tuações o editor comunicará as instituições envolvidas e as agências<br />
financiadoras a respeito da suspeita e aguardará a decisão<br />
final desses órgãos. Se houver a confirmação de uma publicação<br />
frau dulenta no ABO, o editor seguirá os protocolos sugeridos pela<br />
In ter na tional Committee <strong>of</strong> Medical Journal Editors (ICMJE) e pelo<br />
Com mittee on Publication Ethics (COPE).<br />
Lista de Pendências<br />
Antes de iniciar o envio do seu manuscrito o autor deve confir -<br />
mar que todos os itens abaixo estão disponíveis:<br />
□ Manuscrito <strong>for</strong>matado de acordo com as instruções aos autores.<br />
□ Limites de palavras, tabelas, figuras e referências adequados<br />
para o tipo de manuscrito.<br />
□ Todas as figuras e tabelas inseridas no documento principal<br />
do manuscrito.<br />
□ Todas as figuras e tabelas na sua <strong>for</strong>ma digital para serem<br />
enviadas separadamente como documentos suplementares.<br />
□ Formulário de Declaração da Participação dos Autores<br />
preen chido e salvo digitalmente, para ser enviado como<br />
do cumento suplementar.<br />
□ Formulários de Declarações de Conflitos de Interesses de<br />
todos os autores preenchidos e salvos digitalmente, para<br />
serem enviados como documentos suplementares.<br />
□ Número do registro na base de dados que contem o proto -<br />
colo do ensaio clínico constando na folha de rosto.<br />
□ Versão digital do parecer do Comitê de Ética em Pesquisa<br />
com a aprovação do projeto, para ser enviado como documento<br />
suplementar.<br />
Arq Bras Oftalmol. 2012;75(5):373-6<br />
375
Lista de Sítios da Internet<br />
Interface de envio de artigos do ABO<br />
http://www.scielo.br/ABO<br />
Formulário de Declaração de Contribuição dos Autores<br />
http://www.cbo.com.br/site/files/Formulario Contribuicao dos Autores.pdf<br />
International Committee <strong>of</strong> Medical Journal Editors (ICMJE)<br />
http://www.icmje.org/<br />
Uni<strong>for</strong>m requirements <strong>for</strong> manuscripts submitted<br />
to biomedical journals<br />
http://www.icmje.org/urm_full.pdf<br />
Declaração de Helsinque<br />
http://www.wma.net/en/30publications/10policies/b3/index.html<br />
Princípios da Association <strong>for</strong> Research in<br />
Vision and Ophthal mo logy (ARVO)<br />
http://www.arvo.org/eweb/dynamicpage.aspx?site=arvo2&<br />
webcode=AnimalsResearch<br />
Chamon W, Melo LA Jr, Paranhos A Jr. Declaração de conflito de<br />
interesse em apresentações e publicações científicas.<br />
Arq Bras Oftalmol. 2010;73(2):107-9.<br />
http://www.scielo.br/pdf/abo/v73n2/v73n2a01.pdf<br />
Princípios de Autoria segundo ICMJE<br />
http://www.icmje.org/ethical_1author.html<br />
Formulários para Declaração de Conflitos de Interesse<br />
http://www.icmje.org/coi_disclosure.pdf<br />
U.S. National Institutes <strong>of</strong> Health<br />
http://www.clinicaltrials.gov<br />
Australian and New Zealand Clinical Trials Registry<br />
http://www.anzctr.org.au<br />
International Standard Randomised Controlled<br />
Trial Number - ISRCTN<br />
http://isrctn.org/<br />
University Hospital Medical In<strong>for</strong>mation Network<br />
Clinical Trials Registry - UMIN CTR<br />
http://www.umin.ac.jp/ctr/index/htm<br />
Nederlands Trial Register<br />
http://www.trialregister.nl/trialreg/index.asp<br />
MeSH - Medical Subject Headings<br />
http://www.ncbi.nlm.nih.gov/sites/entrez?db=mesh&term=<br />
DeCS - Descritores em Ciências da Saúde<br />
http://decs.bvs.br/<br />
Formatação proposta pela International Committee<br />
<strong>of</strong> Medical Journal Editors (ICMJE)<br />
http://www.nlm.nih.gov/bsd/uni<strong>for</strong>m_requirements.html<br />
List <strong>of</strong> Journal Indexed in Index Medicus<br />
http://www.ncbi.nlm.nih.gov/journals<br />
AMA Manual <strong>of</strong> Style 10th edition<br />
http://www.amamanual<strong>of</strong>style.com/<br />
Protocolos da International Committee <strong>of</strong><br />
Medical Journal Editors (ICMJE)<br />
http://www.icmje.org/publishing_2corrections.html<br />
Protocolos da Committee on Publication Ethics (COPE)<br />
http://publicationethics.org/flowcharts<br />
Editada por<br />
Ipsis Gráfica e Editora S.A.<br />
Rua Vereador José Nanci, 151 - Parque Jaçatuba<br />
CEP 09290-415 - Santo André - SP<br />
Fone: (0xx11) 2172-0511 - Fax (0xx11) 2273-1557<br />
Diretor-Presidente: Fernando Steven Ullmann;<br />
Diretora Comercial: Helen Suzana Perlmann; Diretora de Arte: Elza Rudolf;<br />
Editoração Eletrônica, CTP e Impressão: Ipsis Gráfica e Editora S.A.<br />
Periodicidade: Bimestral; Tiragem: 7.450 exemplares<br />
Publicidade<br />
conselho brasileiro de<br />
<strong>of</strong>talmologia<br />
R. Casa do Ator, 1.117 - 2º andar - Vila Olímpia -<br />
São Paulo - SP - CEP 04546-004<br />
Contato: Fabrício Lacerda<br />
Fone: (5511) 3266-4000 - Fax: (5511) 3171-0953<br />
E-mail: assessoria@cbo.com.br<br />
376 Arq Bras Oftalmol. 2012;75(5):373-6
AGORA A LINHA<br />
1-DAY ACUVUE® MOIST®<br />
GANHOU UM<br />
REFORÇO<br />
LANÇAMENTO<br />
LENTES<br />
PARA PACIENTES COM<br />
ASTIGMATISMO<br />
PRIMEIRA LENTE DE USO ÚNICO<br />
PARA ASTIGMATISMO DO BRASIL<br />
© Johnson & Johnson do Brasil Indústria E Comércio de Produtos Para Saúde Ltda - SETEMBRO/2012<br />
CONFORTO E PRATICIDADE<br />
DE UMA NOVA LENTE A CADA DIA.<br />
ACESSE O WEBSITE EXCLUSIVO PARA OFTALMOLOGISTAS: www.jnjvisioncare.com.br<br />
PARA MAIS INFORMAÇÕES, LIGUE PARA 0800 7288281 OU ENVIE E-MAIL PARA <strong>of</strong>talmologista@conbr.jnj.com<br />
1-DAY ACUVUE® MOIST® para ASTIGMATISMO.<br />
© Johnson & Johnson do Brasil Indústria e Comércio de Produtos para Saúde Ltda. Veiculado em setembro de 2012.<br />
Sen<strong>of</strong>ilcon A -<br />
1 ACUVUE® OASYS® com HYDRACLEAR® PLUS: Reg.ANVISA 80148620045,<br />
2 ACUVUE® OASYS® para ASTIGMATISMO com HYDRACLEAR® PLUS: Reg.ANVISA 80148620054, Galyfilcon A<br />
-<br />
3 ACUVUE®<br />
ADVANCE® com HYDRACLEAR®: Reg.ANVISA 80148620026,<br />
Etafilcon A -<br />
4 ACUVUE® 2: Reg.ANVISA 80148620019, 5 1-DAY-ACUVUE® MOIST®: Reg.ANVISA 80148620052,<br />
6 1-DAY ACUVUE® MOIST para ASTIGMATISMO: Reg.<br />
ANVISA 80148620064, 7 ACUVUE® 2 COLOURS: Reg.ANVISA 80148620013,<br />
8 ACUVUE® CLEAR: Reg.ANVISA 80148620021 e 9 5,6<br />
ACUVUE® BIFOCAL: Reg.ANVISA 80148620016. Caixas com 30<br />
, 6 1,2,3,4,7,8,9 ou 2<br />
7<br />
lentes de contato<br />
(LC). Indicações: LC Esféricas<br />
1,3,4,5,7,8 : Miopia, hipermetropia (presbiopia em regime de monovisão) afácica ou não afácica. LC Esféricas Coloridas 8 : Miopia, hipermetropia (presbiopia em regime de monovisão) afácica ou não<br />
afácica. LC Bifocais 9 : Presbiopia afácica ou não afácica associada ou não a miopia ou hipermetropia. LC Tóricas 2,6 : Astigmatismo afácico ou não afácico associado ou não a miopia ou hipermetropia. Antes de utilizar LC consulte<br />
um Oftalmologista. Contra-Indicações:<br />
Qualquer inflamação, infecção, doença ocular, lesão ou anormalidade que afete a córnea, conjuntiva ou pálpebras. Qualquer doença sistêmica que venha a afetar os olhos ou ser agravada<br />
pelo uso de LC; reações alérgicas das superfícies oculares ou anexas Qualquer infecção ativa da córnea; olhos vermelhos ou irritados. Precauções e Advertências:<br />
Problemas oculares, incluindo úlceras de córnea, podem se<br />
desenvolver rapidamente e causar perda da visão. Em caso de descon<strong>for</strong>to visual, lacrimejamento excessivo, visão alterada, vermelhidão nos olhos ou outros problemas, retirar imediatamente as LC e contatar o Oftalmologista.<br />
Usuários de LC devem consultar seu Oftalmologista regularmente. Não usar o produto se a embalagem estéril de plástico estiver aberta ou danificada. Reações Adversas:<br />
Ardor, coceira ou sensação de pontada nos olhos.<br />
Descon<strong>for</strong>to quando a LC <strong>for</strong> colocada pela primeira vez. Sensação de que há algo no olho (corpo estranho, área raspada). Lacrimejamento excessivo, secreções oculares incomuns ou vermelhidão dos olhos. Acuidade visual<br />
deficiente, visão embaçada, arco-íris ou halos ao redor de objetos, fot<strong>of</strong>obia, ou olho seco, podem ocorrer caso as LC sejam usadas continuamente ou por tempo excessivamente longo. Se o usuário relatar algum problema,<br />
1,2,4,7,8,9 deve RETIRAR IMEDIATAMENTE AS LENTES e contatar o 1,2,3,4,6,7,8<br />
– Períodos inferiores a um dia uso enquanto acordado. Descartáveis diárias de<br />
5,6 – uso único.<br />
Oftalmologista. Posologia: Uso prolongado<br />
– Um a 7 dias/6 noites de uso contínuo, inclusive durante o sono. Uso diário<br />
VENDA SOB PRESCRIÇÃO MÉDICA<br />
REFRACIONAL (LC com grau) e<br />
VENDA SOB PRESCRIÇÃO MÉDICA (LC plana). Johnson & Johnson Industrial Ltda. Rod. Pres.<br />
Dutra, Km 154 - S. J. dos Campos, SP. CNPJ: 59.748.988/0001-14. Resp. Téc.: Evelise S. Godoy – CRQ No. 04345341. Mais in<strong>for</strong>mações sobre uso e cuidados de manutenção e segurança, fale com seu Oftalmologista, ligue para<br />
Central de Relacionamento com o Consumidor: 0800-7274040, acesse www.acuvue.com.br ou consulte o Guia de Instruções ao Usuário. A PERSISTIREM OS SINTOMAS, O MÉDICO DEVERÁ SER CONSULTADO.
TM<br />
Nova Lente Pronta Essilor Stylis 1,74<br />
Essilor Stylis 1,74 e Crizal Forte UV são marcas registradas da Essilor International.<br />
TAMANHO DOS OLHOS<br />
DISTORCIDOS COM LENTES<br />
PADRÃO PARA MÍOPES<br />
A lente mais fina e mais transparente do mercado para atender às<br />
necessidades de estética e con<strong>for</strong>to dos seus pacientes míopes.<br />
Proporcione máximo con<strong>for</strong>to visual garantindo elegância para usuários de óculos com alta miopia, combinando a mais<br />
avançada tecnologia antirreflexo Crizal Forte UV, com a lente em resina de alto índice mais fina e mais transparente do<br />
mercado - Essilor Stylis 1,74.<br />
• Compatível com todos os tipos de armações.<br />
• Disponível em lentes prontas: -10,00 a -4,00 cil -2,00 e de -10,25 a -12,00 somente dioptrias esféricas.<br />
• Garantia Crizal de resistência a arranhões, de até 24 meses.**<br />
* Índice de referência desenvolvido pelo departamento de Pesquisas e Desenvolvimento da Essilor International certificando a proteção UV global de uma lente. O índice FPS-O = 25 significa que os olhos estão 25<br />
vezes mais bem protegidos com as lentes Crizal UV do que sem lente alguma. FPS-O = 25 para as lentes Crizal UV nos materiais Essilor Stylis, Essilor Airwear, Xperio, Transitions e FPS-O = 10 no material Orma<br />
transparente. Medições realizadas consideram apenas a per<strong>for</strong>mance da lente."<br />
** Mediante cadastro no site www.essilor.com.br/garantiacrizal<br />
Essilor Stylis 1,74<br />
TM<br />
*<br />
www.crizal.com.br | SAC 0800 727 2007