Testing for Allergy - NCC Pediatrics Residency at Walter Reed
Testing for Allergy - NCC Pediatrics Residency at Walter Reed
Testing for Allergy - NCC Pediatrics Residency at Walter Reed
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
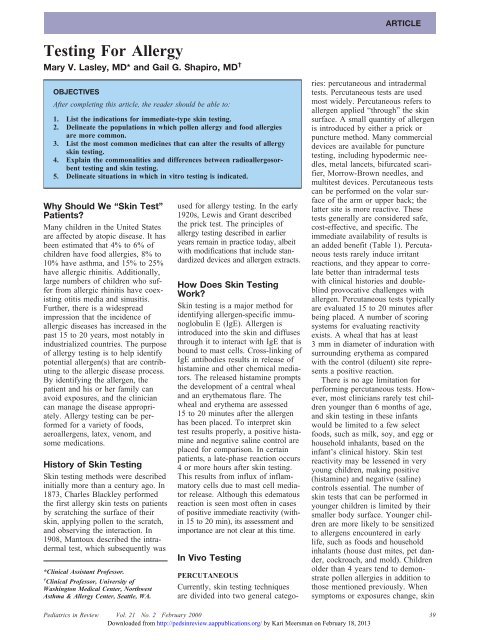
ARTICLE<br />
<strong>Testing</strong> For <strong>Allergy</strong><br />
Mary V. Lasley, MD* and Gail G. Shapiro, MD †<br />
OBJECTIVES<br />
After completing this article, the reader should be able to:<br />
1. List the indic<strong>at</strong>ions <strong>for</strong> immedi<strong>at</strong>e-type skin testing.<br />
2. Deline<strong>at</strong>e the popul<strong>at</strong>ions in which pollen allergy and food allergies<br />
are more common.<br />
3. List the most common medicines th<strong>at</strong> can alter the results of allergy<br />
skin testing.<br />
4. Explain the commonalities and differences between radioallergosorbent<br />
testing and skin testing.<br />
5. Deline<strong>at</strong>e situ<strong>at</strong>ions in which in vitro testing is indic<strong>at</strong>ed.<br />
Why Should We “Skin Test”<br />
P<strong>at</strong>ients?<br />
Many children in the United St<strong>at</strong>es<br />
are affected by <strong>at</strong>opic disease. It has<br />
been estim<strong>at</strong>ed th<strong>at</strong> 4% to 6% of<br />
children have food allergies, 8% to<br />
10% have asthma, and 15% to 25%<br />
have allergic rhinitis. Additionally,<br />
large numbers of children who suffer<br />
from allergic rhinitis have coexisting<br />
otitis media and sinusitis.<br />
Further, there is a widespread<br />
impression th<strong>at</strong> the incidence of<br />
allergic diseases has increased in the<br />
past 15 to 20 years, most notably in<br />
industrialized countries. The purpose<br />
of allergy testing is to help identify<br />
potential allergen(s) th<strong>at</strong> are contributing<br />
to the allergic disease process.<br />
By identifying the allergen, the<br />
p<strong>at</strong>ient and his or her family can<br />
avoid exposures, and the clinician<br />
can manage the disease appropri<strong>at</strong>ely.<br />
<strong>Allergy</strong> testing can be per<strong>for</strong>med<br />
<strong>for</strong> a variety of foods,<br />
aeroallergens, l<strong>at</strong>ex, venom, and<br />
some medic<strong>at</strong>ions.<br />
History of Skin <strong>Testing</strong><br />
Skin testing methods were described<br />
initially more than a century ago. In<br />
1873, Charles Blackley per<strong>for</strong>med<br />
the first allergy skin tests on p<strong>at</strong>ients<br />
by scr<strong>at</strong>ching the surface of their<br />
skin, applying pollen to the scr<strong>at</strong>ch,<br />
and observing the interaction. In<br />
1908, Mantoux described the intradermal<br />
test, which subsequently was<br />
*Clinical Assistant Professor.<br />
† Clinical Professor, University of<br />
Washington Medical Center, Northwest<br />
Asthma & <strong>Allergy</strong> Center, Se<strong>at</strong>tle, WA.<br />
used <strong>for</strong> allergy testing. In the early<br />
1920s, Lewis and Grant described<br />
the prick test. The principles of<br />
allergy testing described in earlier<br />
years remain in practice today, albeit<br />
with modific<strong>at</strong>ions th<strong>at</strong> include standardized<br />
devices and allergen extracts.<br />
How Does Skin <strong>Testing</strong><br />
Work?<br />
Skin testing is a major method <strong>for</strong><br />
identifying allergen-specific immunoglobulin<br />
E (IgE). Allergen is<br />
introduced into the skin and diffuses<br />
through it to interact with IgE th<strong>at</strong> is<br />
bound to mast cells. Cross-linking of<br />
IgE antibodies results in release of<br />
histamine and other chemical medi<strong>at</strong>ors.<br />
The released histamine prompts<br />
the development of a central wheal<br />
and an erythem<strong>at</strong>ous flare. The<br />
wheal and erythema are assessed<br />
15 to 20 minutes after the allergen<br />
has been placed. To interpret skin<br />
test results properly, a positive histamine<br />
and neg<strong>at</strong>ive saline control are<br />
placed <strong>for</strong> comparison. In certain<br />
p<strong>at</strong>ients, a l<strong>at</strong>e-phase reaction occurs<br />
4 or more hours after skin testing.<br />
This results from influx of inflamm<strong>at</strong>ory<br />
cells due to mast cell medi<strong>at</strong>or<br />
release. Although this edem<strong>at</strong>ous<br />
reaction is seen most often in cases<br />
of positive immedi<strong>at</strong>e reactivity (within<br />
15 to 20 min), its assessment and<br />
importance are not clear <strong>at</strong> this time.<br />
In Vivo <strong>Testing</strong><br />
PERCUTANEOUS<br />
Currently, skin testing techniques<br />
are divided into two general c<strong>at</strong>egories:<br />
percutaneous and intradermal<br />
tests. Percutaneous tests are used<br />
most widely. Percutaneous refers to<br />
allergen applied “through” the skin<br />
surface. A small quantity of allergen<br />
is introduced by either a prick or<br />
puncture method. Many commercial<br />
devices are available <strong>for</strong> puncture<br />
testing, including hypodermic needles,<br />
metal lancets, bifurc<strong>at</strong>ed scarifier,<br />
Morrow-Brown needles, and<br />
multitest devices. Percutaneous tests<br />
can be per<strong>for</strong>med on the volar surface<br />
of the arm or upper back; the<br />
l<strong>at</strong>ter site is more reactive. These<br />
tests generally are considered safe,<br />
cost-effective, and specific. The<br />
immedi<strong>at</strong>e availability of results is<br />
an added benefit (Table 1). Percutaneous<br />
tests rarely induce irritant<br />
reactions, and they appear to correl<strong>at</strong>e<br />
better than intradermal tests<br />
with clinical histories and doubleblind<br />
provoc<strong>at</strong>ive challenges with<br />
allergen. Percutaneous tests typically<br />
are evalu<strong>at</strong>ed 15 to 20 minutes after<br />
being placed. A number of scoring<br />
systems <strong>for</strong> evalu<strong>at</strong>ing reactivity<br />
exists. A wheal th<strong>at</strong> has <strong>at</strong> least<br />
3 mm in diameter of indur<strong>at</strong>ion with<br />
surrounding erythema as compared<br />
with the control (diluent) site represents<br />
a positive reaction.<br />
There is no age limit<strong>at</strong>ion <strong>for</strong><br />
per<strong>for</strong>ming percutaneous tests. However,<br />
most clinicians rarely test children<br />
younger than 6 months of age,<br />
and skin testing in these infants<br />
would be limited to a few select<br />
foods, such as milk, soy, and egg or<br />
household inhalants, based on the<br />
infant’s clinical history. Skin test<br />
reactivity may be lessened in very<br />
young children, making positive<br />
(histamine) and neg<strong>at</strong>ive (saline)<br />
controls essential. The number of<br />
skin tests th<strong>at</strong> can be per<strong>for</strong>med in<br />
younger children is limited by their<br />
smaller body surface. Younger children<br />
are more likely to be sensitized<br />
to allergens encountered in early<br />
life, such as foods and household<br />
inhalants (house dust mites, pet dander,<br />
cockroach, and mold). Children<br />
older than 4 years tend to demonstr<strong>at</strong>e<br />
pollen allergies in addition to<br />
those mentioned previously. When<br />
symptoms or exposures change, skin<br />
<strong>Pedi<strong>at</strong>rics</strong> in Review Vol. 21 No. 2 February 2000 39<br />
Downloaded from http://pedsinreview.aappublic<strong>at</strong>ions.org/ by Kari Meersman on February 18, 2013