Management of Complications of Sleeve Gastrectomy: Leak, Gastric ...
Management of Complications of Sleeve Gastrectomy: Leak, Gastric ...
Management of Complications of Sleeve Gastrectomy: Leak, Gastric ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Management</strong> <strong>of</strong> <strong>Complications</strong> <strong>of</strong> <strong>Sleeve</strong><br />
<strong>Gastrectomy</strong>:<br />
<strong>Leak</strong>, <strong>Gastric</strong> Torsion<br />
Bariatric Education 2010<br />
University <strong>of</strong> Minnesota<br />
May 26, 2010<br />
Vivek N. Prachand MD FACS<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Surgery<br />
University <strong>of</strong> Chicago<br />
Chicago, IL<br />
VNP<br />
ASMBS POSITION STATEMENT ON PREVENTION<br />
AND DETECTION OF<br />
GASTROINTESTINAL LEAK AFTER GASTRIC BYPASS<br />
INCLUDING THE ROLE OF IMAGING<br />
AND SURGICAL EXPLORATION<br />
The American Society for Metabolic and Bariatric Surgery<br />
Clinical Issues Committee<br />
Approved by the ASMBS Executive Council, January 2009<br />
http://www.asmbs.org/Newsite07/resources<br />
/leak_management_position.pdf<br />
VNP<br />
Patient History<br />
48yo ♀ BMI 70<br />
DM, HTN, Chol, GERD, OA, prothrombin<br />
gene mutation<br />
Previous lap Nissen fundoplication, CCK<br />
Lives 300 miles away<br />
rIVCF + Laparoscopic Duodenal Switch<br />
• 60F Bougie, 4.8mm w/bovine pericardium<br />
• Stayed lateral to intact Nissen<br />
• Intra-op endoscopy<br />
• 19F Blake drain<br />
VNP<br />
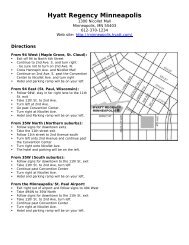
POD#3<br />
• Tachycardia, abdominal pain, oliguria<br />
• Drain “murky”<br />
• Exploratory laparoscopy<br />
• <strong>Leak</strong> adjacent to staple line distal to prior<br />
wrap, oversewn, endoscopy<br />
• abd washout, drains placed, NGT<br />
POD#6-14<br />
• Nausea, vomiting<br />
VNP<br />
POD#14<br />
• Murky fluid from drains<br />
• Exploratory laparoscopy<br />
• Converted to open<br />
• Staple line intact but dehisced from stomach<br />
• 2-layer closure over 56F bougie<br />
• J-tube in biliopancreatic limb<br />
epigastric pain, wound infection<br />
POD#28 D/C on TF’s, PO as tolerated<br />
POD#60 Readmission with rectal bleeding,<br />
epigastric pain, diarrhea<br />
VNP<br />
VNP<br />
1
Patient History<br />
Endoscopic Therapy<br />
• Porcine SIS mesh inserted into fistula, clipped in<br />
place, fibrin glue sprayed<br />
• 15cm, 21mm Polyflex stent placed<br />
• Proximal fixation above GEJ<br />
• Clips used to attempt fixation<br />
• Distal end in antrum<br />
VNP<br />
VNP<br />
Continued epigastric pain<br />
Severe regurgitation<br />
POD#120 Readmission<br />
Stent had migrated proximally, no distal flow<br />
Gastrocolic fistula present<br />
Unable to retrieve stent endoscopically<br />
VNP<br />
VNP<br />
Exploratory Laparotomy<br />
Proximal gastrectomy with fistula resection<br />
and stent retrieval<br />
Partial colectomy with colocolostomy<br />
Jejunal interposition using PB limb<br />
(Esophagojejunostomy, jejunogastrostomy)<br />
Post-op course uneventful<br />
VNP<br />
VNP<br />
2
In Hindsight …<br />
4 years post-op<br />
• 223.7 lb wt loss (79% EBWL, BMI 31)<br />
• DM, ↑chol resolved<br />
• Had ventral hernia repair/panniculectomy<br />
with Plastics Surgery team<br />
BPD instead <strong>of</strong> DS given prior Nissen?<br />
1st drain was helpful, but drains migrate<br />
Bovine pericardial strip contribution to<br />
inflammatory response<br />
Earlier placement <strong>of</strong> enteral access?<br />
What if sleeve was narrower?<br />
VNP<br />
VNP<br />
Disclaimers<br />
Who is a leak “expert”?<br />
Evidence base is suspect<br />
• <strong>Leak</strong>s are rare (but serious)<br />
• Few data comparing leak vs. no leak<br />
• Heterogeneity <strong>of</strong> technique, skill<br />
• Heterogeneity <strong>of</strong> patients<br />
“Truthiness”<br />
"truth that comes<br />
from the gut, not<br />
books"<br />
“The battles are won<br />
and lost in the OR”<br />
“… some are more<br />
equal than others”<br />
Continuity <strong>of</strong> care<br />
Is the Pre-test<br />
Probability Increased?<br />
“Index <strong>of</strong> Suspicion”<br />
“Pre”-Evaluation<br />
VNP<br />
VNP<br />
Evaluation <strong>of</strong> <strong>Leak</strong>s: Clinical Findings<br />
Appearance<br />
• Apprehension, feeling <strong>of</strong> doom<br />
• “don’t look right”<br />
Tachycardia<br />
Hamilton EC et al Surg Endosc 2003<br />
• >100 bpm vs. >120 bpm<br />
• Sensitivity 60-80%, specificity, PPV ?<br />
Fever<br />
Respiratory Distress<br />
Oliguria<br />
Do Not Forget<br />
Abdominal pain<br />
Pulmonary Embolism!<br />
Leukocytosis<br />
Drain amylase >400 IU/L Maher JW et al JACS 2009<br />
VNP<br />
Now What?<br />
Sin <strong>of</strong> Omission > Sin <strong>of</strong> Commission<br />
Testing should not be used as a stall tactic<br />
How sick is the patient?<br />
VNP<br />
3
Radiographic Evaluation<br />
UGI<br />
• Operator-dependent<br />
• Weight limit?<br />
• Routine vs. selective<br />
• Sensitivity 22-75%<br />
CT<br />
• Less operator-dependent<br />
• Weight limit<br />
• May identify presence<br />
(not source) <strong>of</strong> leak,<br />
abscess, obstruction<br />
• PE protocol CT<br />
VNP<br />
Source<br />
control<br />
Drainage<br />
Nutrition<br />
delivery<br />
Abdominal<br />
Lavage<br />
Goals <strong>of</strong> Treatment<br />
Non-Op<br />
(Perc Drain)<br />
NPO<br />
(saliva)<br />
++<br />
TPN<br />
None<br />
Endoscopic<br />
(Stent)<br />
++<br />
Additional IR<br />
procedure<br />
PO<br />
“Immediate”<br />
None<br />
NO RCT’s, , COMPARATIVE DATA MINIMAL<br />
Operative<br />
++<br />
+++<br />
+++<br />
Enteral<br />
+++<br />
VNP<br />
Surgical Exploration as Diagnostic Tool<br />
Up to 30% <strong>of</strong> patients with leaks will have<br />
both “normal” UGI and “normal” CT<br />
Laparoscopy as a game-changer<br />
Intraoperative endoscopy vs. alternative<br />
interrogation methods<br />
Allows potentially definitive therapy and<br />
access for enteral feeding<br />
Negative exploration is NOT a complication!<br />
<strong>Sleeve</strong> <strong>Gastrectomy</strong> <strong>Leak</strong>s<br />
Where?<br />
• Proximal (80%)<br />
• Thin tissue<br />
• Blood supply<br />
• Distal obstruction<br />
• Distal (20%)<br />
• Thick tissue<br />
VNP<br />
VNP<br />
Endoscopic Stents<br />
Off-label use (esophageal)<br />
Small series<br />
Migration<br />
Reflux<br />
Removal<br />
Operative Treatment:<br />
Laparoscopy vs. Open<br />
Laparoscopy<br />
• Visualization superior<br />
• Good access for washout/lavage<br />
• Can patient tolerate pneumoperitoneum?<br />
• Changes in abdominal compliance<br />
• Sepsis, ileus<br />
• Personnel availability<br />
• Port-site closure<br />
Fukumoto R SOARD 2007<br />
Eubanks S JACS 2008<br />
VNP<br />
VNP<br />
4
Conclusions<br />
Meticulous technique/prevention<br />
Index <strong>of</strong> suspicion<br />
How sick is the patient<br />
Testing should not be a stall tactic<br />
Goals <strong>of</strong> therapy<br />
Negative exploration is not a complication<br />
VNP<br />
5