Agenda and supporting papers - Plymouth Hospitals NHS Trust
Agenda and supporting papers - Plymouth Hospitals NHS Trust
Agenda and supporting papers - Plymouth Hospitals NHS Trust
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Trust</strong> Board<br />
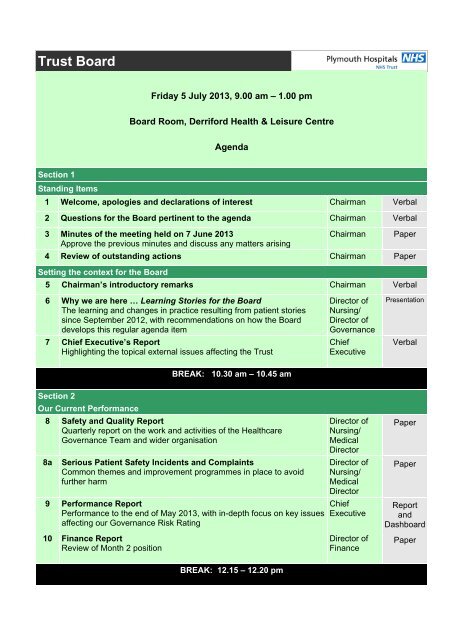
Friday 5 July 2013, 9.00 am – 1.00 pm<br />
Board Room, Derriford Health & Leisure Centre<br />
<strong>Agenda</strong><br />
Section 1<br />
St<strong>and</strong>ing Items<br />
1 Welcome, apologies <strong>and</strong> declarations of interest Chairman Verbal<br />
2 Questions for the Board pertinent to the agenda Chairman Verbal<br />
3 Minutes of the meeting held on 7 June 2013<br />
Approve the previous minutes <strong>and</strong> discuss any matters arising<br />
Chairman<br />
Paper<br />
4 Review of outst<strong>and</strong>ing actions Chairman Paper<br />
Setting the context for the Board<br />
5 Chairman’s introductory remarks Chairman Verbal<br />
6 Why we are here … Learning Stories for the Board<br />
The learning <strong>and</strong> changes in practice resulting from patient stories<br />
since September 2012, with recommendations on how the Board<br />
develops this regular agenda item<br />
7 Chief Executive’s Report<br />
Highlighting the topical external issues affecting the <strong>Trust</strong><br />
Director of<br />
Nursing/<br />
Director of<br />
Governance<br />
Chief<br />
Executive<br />
Presentation<br />
Verbal<br />
BREAK: 10.30 am – 10.45 am<br />
Section 2<br />
Our Current Performance<br />
8 Safety <strong>and</strong> Quality Report<br />
Quarterly report on the work <strong>and</strong> activities of the Healthcare<br />
Governance Team <strong>and</strong> wider organisation<br />
8a<br />
Serious Patient Safety Incidents <strong>and</strong> Complaints<br />
Common themes <strong>and</strong> improvement programmes in place to avoid<br />
further harm<br />
9 Performance Report<br />
Performance to the end of May 2013, with in-depth focus on key issues<br />
affecting our Governance Risk Rating<br />
10 Finance Report<br />
Review of Month 2 position<br />
Director of<br />
Nursing/<br />
Medical<br />
Director<br />
Director of<br />
Nursing/<br />
Medical<br />
Director<br />
Chief<br />
Executive<br />
Director of<br />
Finance<br />
Paper<br />
Paper<br />
Report<br />
<strong>and</strong><br />
Dashboard<br />
Paper<br />
BREAK: 12.15 – 12.20 pm
<strong>Trust</strong> Board<br />
Section 2 (continued)<br />
Our Current Performance<br />
11 Quarterly update on acute hospital st<strong>and</strong>ards for people with<br />
Learning Disabilities<br />
Quarterly review of declaration of compliance<br />
Associate<br />
Director of<br />
Nursing<br />
Paper<br />
12 Equality <strong>and</strong> Diversity update<br />
Integrating <strong>and</strong> embedding equality <strong>and</strong> diversity strategically at Board<br />
level <strong>and</strong> as part of the core business of the <strong>Trust</strong><br />
Section 3<br />
Governance<br />
13 Information Governance<br />
Quarterly update on assurance by the Senior Information Risk Owner<br />
14 <strong>Trust</strong> Seal<br />
Quarterly report in accordance with St<strong>and</strong>ing Orders<br />
Director of<br />
Human<br />
Resources &<br />
OD<br />
Director of<br />
Planning &<br />
Site Services<br />
Board<br />
Secretary<br />
Paper<br />
Paper<br />
Paper<br />
Assuring Committee Chairs’ Reports <strong>and</strong> meeting minutes. The following items will be reviewed<br />
‘in the round’. Issues will be discussed only if not covered as part of the earlier Performance<br />
Review or if Board members require additional assurance to be sought.<br />
15 Safety & Quality Committee<br />
Report of assurances from June meeting <strong>and</strong> review of June minutes<br />
16 Finance, Performance & Investment Committee<br />
Review of May minutes<br />
17 Human Resources & Organisational Development Committee<br />
Report of assurances from the June meeting <strong>and</strong> review of June<br />
minutes<br />
18 Audit Committee<br />
Chair’s Report <strong>and</strong> review of May minutes<br />
Closing items<br />
Committee<br />
Chair<br />
Committee<br />
Chairman<br />
Committee<br />
Chair<br />
Committee<br />
Chair<br />
Paper<br />
Paper<br />
Paper<br />
Paper<br />
19 Any other business Chairman Verbal<br />
20 Date of next meeting<br />
Friday 27 September 2013 at 9.00 am<br />
Chairman<br />
Verbal
Members of <strong>Plymouth</strong> <strong>Hospitals</strong> <strong>NHS</strong> <strong>Trust</strong> Board of Directors have declared the following interests:<br />
Name Position Declared Interest<br />
Richard Crompton Chairman None<br />
Kevin Baber Chief Operating Officer None<br />
Lee Budge Director of Governance None<br />
Greg Dix Director of Nursing None<br />
Ian Douglas Non‐Executive Director Managing Director <strong>and</strong> owner, Blackdown Consulting<br />
Director, Mango Evolution Ltd<br />
Director, Challenge‐X Ltd<br />
Ann James Chief Executive <strong>Trust</strong>ee, Exeter Royal Academy for Deaf Education<br />
Health <strong>and</strong> Medical Champion, Chamber of Commerce<br />
Member, <strong>Plymouth</strong> Council Growth Board<br />
Director, South West Peninsula Academic Health<br />
Science Network<br />
Terence Lewis Non‐Executive Director Honorary Life President, Heartswell South West<br />
Chairman, <strong>Plymouth</strong> Marine Laboratory<br />
Governor, <strong>Plymouth</strong> University<br />
Chairman, <strong>Plymouth</strong> University Peninsula Schools of<br />
Medicine <strong>and</strong> Dentistry Medical School Board<br />
President, <strong>Plymouth</strong> Heartbeat<br />
House of Hope, Nepal – family orphanage<br />
Alex Mayor Medical Director Shareholder in Serco plc<br />
Elizabeth Raikes Non‐Executive Director <strong>Trust</strong>ee, Fortescue Garden <strong>Trust</strong><br />
Hein Scheffer<br />
Director of Human<br />
Resources &<br />
Organisational<br />
Development<br />
Director, Wavelengths 106 (Pty) Ltd<br />
<strong>Trust</strong>ee, Boherwald <strong>Trust</strong><br />
Margaret Schwarz Non‐Executive Director Director, Cornwall Care<br />
Governor of <strong>Plymouth</strong> University (from 1 July 2013)<br />
Joe Teape<br />
Director of Finance &<br />
Strategy<br />
Former Branch Chairman <strong>and</strong> Branch Committee<br />
member of the Healthcare Financial Management<br />
Association<br />
Henry Warren<br />
Denis Wilkins<br />
Associate Non‐Executive<br />
Director<br />
Associate Non‐Executive<br />
Director<br />
Governor <strong>and</strong> member of Finance Committee of<br />
<strong>Plymouth</strong> University<br />
Chairman <strong>and</strong> Director of Tradewind Turbines Ltd<br />
Chairman <strong>and</strong> Director of Fluvial Innovations Ltd<br />
Director of J&S Ltd<br />
Chairman, Council for St John (Ambulance) Cornwall<br />
Governor of <strong>Plymouth</strong> University (from 1 July 2013)<br />
Mike Williams Non‐Executive Director No commercial interests to declare.<br />
Honorary research fellow with South Devon Healthcare<br />
<strong>NHS</strong>FT.<br />
My department at Exeter University has research grants<br />
from South Devon Healthcare <strong>NHS</strong>FT <strong>and</strong> Open<br />
Innovation to conduct research in South Devon Health<br />
<strong>and</strong> Social Care services.
Item 3<br />
<strong>Plymouth</strong> <strong>Hospitals</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Minutes of the <strong>Trust</strong> Board meeting Part 1<br />
9.00 am on Friday 7 June 2013<br />
Board Room, Derriford Health & Leisure Centre<br />
Present:<br />
Apologies:<br />
Richard Crompton, Chairman<br />
Kevin Baber, Chief Operating Officer<br />
Greg Dix, Director of Nursing<br />
Ian Douglas, Non-Executive Director<br />
D<br />
Ann James, Chief Executive<br />
Terence Lewis, Non-Executive Director<br />
Alex Mayor, Medical Director<br />
Elizabeth Raikes, Non-Executive Director<br />
Joe Teape, Director of Finance & Strategy<br />
Henry Warren, Associate Non-Executive Director<br />
R<br />
Denis Wilkins, Associate Non-Executive Director<br />
Mike Williams, Non-Executive Director<br />
Hein Scheffer, Director of Human Resources & Organisational<br />
Development<br />
A<br />
Margaret Schwarz, Vice-Chair<br />
Rob Sneyd, Dean, <strong>Plymouth</strong> University Peninsula Schools of<br />
Medicine & Dentistry<br />
In attendance: Martin Bamber, Deputy Director of Human Resources<br />
Lee Budge, Director of Governance<br />
Gill Hunt, Board Secretary<br />
‘Governors’ in<br />
attendance<br />
F<br />
Brian Jones, Associate Director of Finance<br />
Am<strong>and</strong>a Nash, Head of Communications<br />
Steve Spencer, Comm<strong>and</strong>ing Officer, MDHU<br />
Nick Thomas, Director of Planning & Site Services<br />
Sally Wilson, Chief Financial Accountant<br />
T<br />
Marina Taylor, Public ‘Governor’, <strong>Plymouth</strong> constituency<br />
Action<br />
101/13 Welcome, apologies <strong>and</strong> declarations of interest<br />
The Chairman welcomed members of the public in attendance.<br />
Apologies had been received on behalf of Hein Scheffer, Margaret<br />
Schwarz <strong>and</strong> Rob Sneyd.<br />
Comm<strong>and</strong>er Steve Spencer, MDHU, was attending his last Board<br />
meeting on stepping down from his comm<strong>and</strong> to take up an overseas<br />
posting. The Chairman thanked Comm<strong>and</strong>er Spencer for his<br />
contribution <strong>and</strong> wished him well. The Chairman welcomed Lt<br />
Comm<strong>and</strong>er Tim Jones, who would be taking up his appointment as<br />
MDHU Comm<strong>and</strong>er in July 2013 <strong>and</strong> attended the meeting as an<br />
1
Item 3<br />
observer.<br />
The Chairman required those present to declare any interests they<br />
may have pertaining to the matters listed on the agenda. There were<br />
no declarations of interest.<br />
102/13 Questions to the Board pertinent to the agenda<br />
A member of the public<br />
D<br />
wished to place on record her appreciation of<br />
the care that her husb<strong>and</strong>, currently a patient on Braunton Ward, had<br />
received since his admission one week ago. Her husb<strong>and</strong> had been a<br />
patient on the same ward three years previously <strong>and</strong> it was apparent<br />
to both her <strong>and</strong> her husb<strong>and</strong> that st<strong>and</strong>ards were much improved.<br />
R<br />
Referring to recent local media reporting of the recruitment of<br />
additional nursing staff <strong>and</strong> an increase in the <strong>Trust</strong>’s bed base, a<br />
member of the public queried how, given the <strong>Trust</strong>’s financial position,<br />
this would be funded. Ms James stated that this would be discussed<br />
as part of agenda items 8 <strong>and</strong> 10.<br />
A<br />
The Board Secretary read a written question from shadow ‘governor’<br />
Mrs Vera Mitchell. Mrs Mitchell noted the pressures nationally on<br />
emergency access <strong>and</strong> suggested the Department of Health had a<br />
role to play in influencing the irresponsible lifestyles that contributed to<br />
disease <strong>and</strong> trauma. She asked what the Board would do, in<br />
partnership with stakeholders, to encourage healthy <strong>and</strong> responsible<br />
lifestyles. In response,<br />
F<br />
Dr Mayor stated that there was a clear<br />
commitment from the Board to contribute to the local public health<br />
agenda. He highlighted the smoke-free <strong>Trust</strong> initiative, the <strong>Trust</strong>’s<br />
involvement in the <strong>Plymouth</strong> Alcohol Strategy, <strong>and</strong> its role, through Dr<br />
Paddy English <strong>and</strong> his colleagues, in tackling health problems<br />
associated with obesity.<br />
T<br />
The Board Secretary read a second written question from Mrs<br />
Mitchell. Mrs Mitchell enquired whether the Board would continue its<br />
rigorous support to maintain <strong>and</strong> extend the work of the Infection<br />
Prevention <strong>and</strong> Control team. Mr Dix affirmed that the Board would<br />
do so; in addition to the team’s work with the Peninsula College of<br />
Medicine <strong>and</strong> Dentistry to develop <strong>and</strong> deliver a Master’s programme<br />
in Infection Prevention <strong>and</strong> Control, the <strong>Trust</strong>’s new organisational<br />
structure would facilitate improved practice at service line level.<br />
There were no further questions.<br />
103/13 A Learning Story for the Board<br />
Dr Ian Higginson, Consultant in Emergency Medicine, related his own<br />
experiences in January 2013 during a 28 hour inpatient stay. Dr<br />
Higginson described all aspects of his assessment, diagnosis <strong>and</strong><br />
surgery as highly efficient <strong>and</strong> was of the view that the good nursing<br />
care he had received had facilitated his prompt discharge.<br />
2
Item 3<br />
The Board discussed the learning points <strong>and</strong> matters arising from Dr<br />
Higginson’s experience:<br />
• The Surgical Assessment Unit had been very crowded <strong>and</strong> the<br />
patient experience would be improved by reducing the number<br />
of beds per bay.<br />
• The area was pervaded by the lingering smell of hospital food.<br />
• Rear opening gowns eliminated any sense of patient dignity.<br />
D<br />
• Staff were not aware of two-way claves <strong>and</strong> how to connect<br />
them.<br />
• Ward managers must have control of ward stock lists.<br />
• A patient had been kept in a bed whilst awaiting diagnostics but<br />
could have been discharged <strong>and</strong> called back as an outpatient,<br />
freeing up the bed. The wider issue was medically fit patients<br />
R<br />
detained in beds awaiting diagnostics.<br />
• Delayed discharges waiting for TTAs. Dr Higginson had spent<br />
15% of his entire hospital stay waiting for medications.<br />
• He had been prescribed <strong>and</strong> provided with TTA drugs that he<br />
did not require,<br />
A<br />
resulting in unnecessary costs to the <strong>Trust</strong>.<br />
• The benefits of the Enhanced Recovery programme in<br />
engaging patients in goals for their discharge. This programme<br />
was currently practiced in the <strong>Trust</strong> in surgery but not yet in<br />
medicine.<br />
• The known variations in clinical outcomes according to time<br />
<strong>and</strong> day of admission,<br />
F<br />
recently the subject of national media<br />
reporting.<br />
The Chairman requested an update on the issues arising from Dr<br />
Higginson’s story at the next Board. The next scheduled Board<br />
walkround to the ED <strong>and</strong> SAU would focus on the issues raised. On<br />
behalf of the Board, the TChairman thanked Dr Higginson for attending.<br />
Dr Higginson left the meeting.<br />
104/13 Minutes <strong>and</strong> matters arising from the meeting held on 3 May 2013<br />
DoN/DoG<br />
The minutes of the meeting held on 3 May 2013 were agreed as a<br />
true <strong>and</strong> accurate record. There were no matters arising.<br />
105/13 Review of Action List<br />
95/13 Quality Improvement Strategy<br />
Dr Mayor updated the Board. The points made at the Board on 3 May<br />
had been incorporated into the implementation plan led by the Deputy<br />
Director of Nursing <strong>and</strong> Assistant Medical Director Paul McArdle. The<br />
plan was due to be reviewed at the Senior Management Team<br />
meeting on 24 June <strong>and</strong> by the Safety & Quality Committee in July.<br />
71/13 Review of performance data presented to the Board to ensure<br />
3
Item 3<br />
Board oversight of contributing or underlying issues.<br />
Noted as outst<strong>and</strong>ing.<br />
[Post meeting note: Board Secretary to follow up with Medical<br />
Director <strong>and</strong> NED Mike Williams].<br />
BS<br />
The Board noted the action list.<br />
D<br />
In setting the context for the day, the Chairman referred to recent<br />
media attention on the <strong>Trust</strong> <strong>and</strong> the overriding requirement to focus<br />
on the needs of the patient. For some months now Board members<br />
had stressed the requirement to get the basics of care right <strong>and</strong>, in so<br />
doing, produce a compelling<br />
R<br />
strategy to set the organisation’s future<br />
path. Today the Board would focus on both these important<br />
requirements. It would be asked to approve proposals to improve<br />
emergency target performance, together with an associated bed<br />
programme to increase bed availability <strong>and</strong> aid patient flows, <strong>and</strong> the<br />
Chief Executive would be presenting the Board’s strategy <strong>and</strong> vision<br />
for the <strong>Trust</strong>.<br />
A<br />
106/13 Chairman’s introductory remarks<br />
The new clinical leadership structure was vital to service delivery <strong>and</strong><br />
placed clinicians at the heart of the <strong>Trust</strong>. In return, the Board must<br />
expect this new framework to pay dividends in terms of quality,<br />
performance <strong>and</strong> efficiency. Finance remained a significant challenge<br />
<strong>and</strong> the Board required<br />
F<br />
assurance that this would be effectively<br />
tackled at the pace to effect success.<br />
107/13 Chief Executive’s Report<br />
The Senior<br />
Management Team had had challenging but productive discussions<br />
with the local press <strong>and</strong> had been clear on their commitment to work<br />
with the public <strong>and</strong> with staff as the Board launched its strategic<br />
vision. To support this, details of the new clinical leadership team<br />
would be announced to staff next week; these were key individuals<br />
whose work would support the delivery of the <strong>Trust</strong>’s overarching<br />
strategy, At the Heart of Health in the Peninsula.<br />
Ms James supported the Chairman’s remarks.<br />
T<br />
Ms James gave a presentation to support the strategy launch. The<br />
approach adopted in developing this vision had been open <strong>and</strong><br />
transparent <strong>and</strong> had involved clinicians <strong>and</strong> stakeholders. The<br />
document gave a clear sense of the <strong>Trust</strong>’s future direction <strong>and</strong> set<br />
out the approach to creating new partnerships with patients, staff <strong>and</strong><br />
the health community. Ms James referred to debate concerning the<br />
<strong>Trust</strong>’s future positioning as either a ‘district general hospital’ or a<br />
specialist service provider. It was her view that it should, <strong>and</strong> could,<br />
be both <strong>and</strong> that doing so need not be complex.<br />
The strategy detailed the core services that the <strong>Trust</strong> would continue<br />
4
Item 3<br />
to deliver <strong>and</strong> articulated a firm commitment to continue to develop<br />
specialist services <strong>and</strong> build on existing areas of excellence in cancer,<br />
specialist surgery, major trauma, neonatal care <strong>and</strong> obstetrics.<br />
Feedback from clinical commission groups <strong>and</strong> specialist<br />
commissioners on the document’s tone, style <strong>and</strong> ambition had been<br />
positive.<br />
Ms James highlighted the requirement to sustain partnerships with<br />
commissioners <strong>and</strong><br />
D<br />
local health providers, with the MDHU, with<br />
<strong>Plymouth</strong> University <strong>and</strong> private sector partners, <strong>and</strong> to promote the<br />
growth of clinical research through the Peninsula Academic Health<br />
Science Network. The strategy set out how staff would be engaged in<br />
its delivery <strong>and</strong> how, through strengthening clinical leadership <strong>and</strong><br />
demonstrating responsiveness to patients’ needs, service quality<br />
would improve. In summary,<br />
R<br />
Ms James highlighted the strategy’s<br />
strong patient focus <strong>and</strong> the importance of being confident in our<br />
ambitions - the local population deserved this. She commended the<br />
strategy to the Board.<br />
The Chairman invited discussion. The main points were:<br />
A<br />
• Acknowledgement that the launch provided the opportunity for<br />
the Board’s greater involvement in local partnership working<br />
<strong>and</strong> in influencing key external clinicians. The Board must not<br />
be the recipient of change but drive it. The commitment to<br />
patients <strong>and</strong> to the health community was welcome <strong>and</strong> would<br />
be an important<br />
F<br />
factor in strategy implementation.<br />
• Dr Williams sought to underst<strong>and</strong> the position on local<br />
community-based services. Ms James stated that locally the<br />
pressures on hospitals were recognised, not only in terms of<br />
the dem<strong>and</strong> for urgent care but also in the increased acuity of<br />
patients. There<br />
T<br />
was a will to consider commissioning services<br />
in other ways. The <strong>Trust</strong> could provide different models of care<br />
<strong>and</strong> this was an opportunity to pursue <strong>and</strong> influence the<br />
transformation agenda.<br />
• The requirement to review the strategy in six months in terms<br />
of the broader strategic goals <strong>and</strong> future service provision.<br />
Specifications for National Specialist Commission had just<br />
been released <strong>and</strong> the Senior Management Team would<br />
consider this in the context of strategy refinement.<br />
• Comm<strong>and</strong>er Spencer highlighted the onus on the <strong>Trust</strong> Board<br />
to present a compelling narrative to staff <strong>and</strong> to engage them in<br />
delivery. To aid this, the inclusion of a site plan to bring the<br />
document to life was agreed. Ms James, Mr Teape <strong>and</strong> the<br />
Director of Planning & Site Services would agree the process<br />
<strong>and</strong> timescale to achieve this. Ms James stated that there may<br />
be a requirement for external assistance <strong>and</strong> she would update<br />
CE<br />
5
Item 3<br />
the Board next month.<br />
• The document must link to Annual Business Plan <strong>and</strong> set more<br />
detailed timescales for delivery.<br />
The Board noted the Chief Executive’s Report <strong>and</strong> welcomed the<br />
launch of the strategy document.<br />
108/13<br />
D<br />
Emergency Access Target Recovery <strong>and</strong> Bed Programme<br />
Mr David Brown, Assistant Director of Operations, <strong>and</strong> Ms Sophie<br />
O’Brien, Service Improvement Lead, attended for this item <strong>and</strong> gave a<br />
presentation which described<br />
R<br />
the national context behind current<br />
emergency access performance <strong>and</strong> the local actions being taken to<br />
improve performance to 95%. These actions included changes to the<br />
<strong>Trust</strong>’s bed base.<br />
There was a break between 10.25 am <strong>and</strong> 10.40 am.<br />
Emergency Access Target Recovery<br />
A<br />
The presentation identified three overarching causes for the failure to<br />
deliver the four hour st<strong>and</strong>ard:<br />
• Failure to process patients in a timely way.<br />
• Failure to respond to requests for specialist support in a timely<br />
way.<br />
• Failure to admit patients in a timely way (no bed available).<br />
F<br />
Mr Brown’s report described actions to improve performance against<br />
these three root causes. Mr Baber had communicated to senior<br />
medical staff the new expectations for the ED; this had provoked<br />
some specialties to put forward pathway initiatives to improve flow.<br />
T<br />
The Board discussed the proposed actions. The main points were:<br />
• Assurance was sought, <strong>and</strong> given, that medical staff supported<br />
a nurse-led ED.<br />
• Underst<strong>and</strong>ing the importance of specialist support, the<br />
interface between the ED <strong>and</strong> specialist services <strong>and</strong> the<br />
agreement of internal professional st<strong>and</strong>ards.<br />
• The ongoing debate concerning generalist v specialist <strong>and</strong> the<br />
<strong>Trust</strong>’s ability to contribute to this debate.<br />
• The broader context of workforce planning <strong>and</strong> the <strong>Trust</strong>’s<br />
ability to meet its own needs at a time of national change.<br />
• Mr Baber stated that the health-community Urgent Care Forum<br />
were content with the <strong>Trust</strong>’s plans. He explained the role of<br />
6
Item 3<br />
the Forum in targeting winter funding.<br />
Bed Programme<br />
The aim of the Bed Programme was to deliver the appropriate bed<br />
base for the <strong>Trust</strong>’s patient flow by:<br />
• Ensuring patients were cared for in the most appropriate<br />
setting.<br />
• Preventing the<br />
D<br />
cancellation of surgical patients.<br />
• Operating at a manageable occupancy rate across medicine<br />
<strong>and</strong> surgery to provide personal, high quality, safe care.<br />
The Bed Programme identified the difference between current <strong>and</strong><br />
optimal capacity as 56 beds. It proposed the establishment of:<br />
R<br />
• 20 short stay medical beds driven by the known increase in<br />
patients who stay 0-2 days.<br />
• 26 Healthcare of the Elderly beds on Monkswell ward.<br />
• 10 in-ward escalation beds.<br />
A<br />
The cost of this investment in the current year was £2.246m for the<br />
additional 74.05WTE staff, with a full year effect of £3.388m. In<br />
addition, capital costs associated with relocating services, including a<br />
further relocation of the Preoperative Assessment Unit, totalled £665k.<br />
The main risks associated with delivery were:<br />
F<br />
• Recruitment.<br />
• Internal professional st<strong>and</strong>ards.<br />
Mr Brown drew the Board’s attention to the risks to delivery <strong>and</strong> to<br />
their mitigations set out in the presentation <strong>and</strong> in the accompanying<br />
report. Mr Brown suggested<br />
T<br />
that the most significant risk was the<br />
failure to deploy the enhanced community workforce to support<br />
patients in an alternative environment when winter pressures hit. Dr<br />
Williams stated that there was no reason why the <strong>Trust</strong> should not be<br />
proactive in this regard. Mr Baber agreed, staff could function outside<br />
of the footprint of the hospital; other organisations did so with a<br />
significant positive impact on bed availability.<br />
The Board considered the proposals. In so doing, the main points of<br />
discussion were:<br />
• Uncertainty as to whether 26 beds was sufficient to cope with<br />
the variation in dem<strong>and</strong> <strong>and</strong> whether this number would meet<br />
changing local demographics. Ms O’Brien stated the <strong>Trust</strong><br />
would require thirteen additional beds to cope with future<br />
dem<strong>and</strong> <strong>and</strong> a work stream was reviewing this.<br />
• Mr Wilkins queried the degree of clinical involvement in these<br />
proposals. Mr Baber stated that the Care Group Directors had<br />
7
Item 3<br />
been involved <strong>and</strong> there was service line support. Mr Brown<br />
stated that the proposals had been routed through the relevant<br />
clinical groups to ensure support.<br />
• Dr Williams stated that the Board could not be sure that these<br />
proposals would save money <strong>and</strong> be better for patients.<br />
Success would be dependent on a tight grip on the associated<br />
operational issues. The discharge element, which was<br />
dependent on<br />
D<br />
other parties, was crucial <strong>and</strong> there was limited<br />
assurance that this would be delivered in the short term.<br />
• Mr Teape identified the requirement for a clear audit trail for<br />
admissions/discharges to be shared with commissioners. Mr<br />
Teape <strong>and</strong> Mr Baber would shape this.<br />
R<br />
• Mrs Raikes asked whether this investment would add to the<br />
existing CIP programme. Mr Teape stated that it would not <strong>and</strong><br />
that the costs were included in the £5m ‘investment for quality’<br />
projects discussed at the May Board.<br />
• Successful nurse<br />
A<br />
recruitment was crucial to the plan’s success,<br />
both operationally <strong>and</strong> financially. Mr Dix stated that nurse<br />
recruitment was just keeping pace with internal turnover <strong>and</strong> it<br />
was likely that it would be necessary recruit internationally.<br />
Whilst Ms James agreed in principle, she felt there was more<br />
that could be done in local advertising <strong>and</strong> this should be<br />
pursued.<br />
F<br />
Concluding the Board’s discussions, Ms James stated that the Senior<br />
Management Team must develop range of KPIs for Board level<br />
oversight. Agreement of these proposals would send confirmation to<br />
staff that the Board had listened <strong>and</strong> acted on two of their concerns:<br />
T<br />
• The importance of minimising patient <strong>and</strong> staff moves to meet<br />
operational imperatives.<br />
•<br />
The Board:<br />
The importance of <strong>supporting</strong> staff to deliver the consistently<br />
high levels of care that they would wish.<br />
• Noted the internal actions being taken to support<br />
improvements within the ED pathway <strong>and</strong> improve<br />
hospital-wide support for patients within the ED.<br />
• Noted the community-wide actions required to support<br />
hospital based Emergency Care in the longer term.<br />
• Approved the actions described within the Bed<br />
Programme <strong>and</strong> the associated investment necessary to<br />
8
Item 3<br />
109/13 Performance Report<br />
Finance <strong>and</strong> Efficiency<br />
A contract value of £353.2m had been agreed with commissioners.<br />
The contract would operate on a managed Payment by Results (PbR)<br />
basis which assumed that full PbR would be operated but both parties<br />
would work together to<br />
D<br />
deliver all contractual commitments within the<br />
funding envelope available. Mr Teape drew the Board’s attention to<br />
the variable elements of the contract, including cardiac activity, set out<br />
in his report. Dr Williams asked whether there was confidence that a<br />
PbR contract would enable cardiac to deliver at the required level. Mr<br />
Teape stated that focused support was being given to this team. Two<br />
additional ring fenced<br />
R<br />
beds had been provided as an immediate<br />
measure.<br />
Noting the ISTC provision, locally, of cataract surgery, Dr Williams<br />
asked whether this had been built in to budget assumptions. Mr<br />
Teape confirmed that it had; about £0.5m had been taken out of the<br />
ophthalmology budget<br />
A<br />
<strong>and</strong> the service line had been asked to produce<br />
a capacity plan with sensitively analysis.<br />
Mr Teape stated the intention to include in future reports key contract<br />
issues, including activity variations, as well as contract penalties <strong>and</strong><br />
CQUIN achievements to raise the profile of these issues at Board<br />
level.<br />
F<br />
Operational Performance<br />
Mr Baber stated that May had seen a significant decrease in<br />
cancellations but performance remained unacceptable. The<br />
Chairman queried progress<br />
T<br />
with driving theatre efficiency. Mr Baber<br />
stated that authority had been given to surgeons/anaesthetists to get<br />
lists under way. A Service Line Director for Theatres had been<br />
appointed <strong>and</strong> would drive this.<br />
Cancelled Operations<br />
Accident & Emergency Department 4 hour target<br />
May performance had been 94.75%, with 97.74% to date in June.<br />
Year to date performance was 93.53% <strong>and</strong> the quarter may yet be<br />
recovered.<br />
Follow-up Backlog<br />
Dr Williams was concerned that the follow-up backlog remained static<br />
at 23,000 <strong>and</strong> the Board was not assured that the actions in place<br />
would deliver the required improvement. Dr Mayor stated that he had<br />
asked Assistant Medical Director Paul McArdle to undertake a full risk<br />
assessment on all patients on the follow-up list <strong>and</strong> Mr Baber<br />
explained the approach to appropriately prioritising patients <strong>and</strong> to<br />
remove those with no ongoing clinical need. Comm<strong>and</strong>er Spencer<br />
asked whether there was confidence that the backlog was not<br />
9
Item 3<br />
continuing to build. Mr Baber stated that this was being addressed as<br />
part of the waiting list policy.<br />
Referral to Treatment (exception report)<br />
The report set out actions to address under-performance. The <strong>Trust</strong><br />
would fail this target in Quarter 1 but the planned actions facilitated<br />
the speediest resolution of long patient waits. Mr Baber expected to<br />
reach a sustainable position by October.<br />
D<br />
The Board noted performance ahead of target in April.<br />
The <strong>Trust</strong> failed the target in April <strong>and</strong> performance had further<br />
deteriorated in May.<br />
R<br />
Mr Baber stated that an options paper would be<br />
submitted to commissioners on the <strong>Trust</strong>’s overall capacity; this would<br />
include additional staffing <strong>and</strong> the outsourcing of some activity.<br />
Mrs Raikes queried whether the actions to achieve stroke <strong>and</strong> cancer<br />
performance, reported<br />
A<br />
in February <strong>and</strong> March respectively, remained<br />
relevant as performance had not reached the required targets. Mr<br />
Baber stated that the issue with stroke concerned admittance to the<br />
ASU but beds had been ring fenced, compounded by a peculiarity<br />
around the appropriateness of some of the targets when there were<br />
overriding clinical reasons not to admit to the ASU. Exception reports<br />
on cancer <strong>and</strong> stroke<br />
F<br />
would be included in next month’s report to the<br />
Board.<br />
The Board were pleased to note performance at 85% for April. Mr Dix<br />
stated that the quality of the responses had improved; the next step to<br />
improve quality would<br />
T<br />
be to survey complainants’ satisfaction with the<br />
<strong>Trust</strong>’s process. A recently published report on <strong>NHS</strong> governance of<br />
complaints h<strong>and</strong>ling had been circulated to Board members; this<br />
would inform an internal review of complaints due to be reported in<br />
July.<br />
Fractured Neck of Femur<br />
Diagnostics <strong>and</strong> surveillance<br />
Cancer <strong>and</strong> Stroke<br />
Complaints<br />
COO<br />
Friends <strong>and</strong> Family Test Response<br />
The <strong>Trust</strong> has failed this target in April <strong>and</strong> May. Mr Dix had reviewed<br />
performance by ward in order to focus effort where necessary.<br />
Discretionary Pay<br />
Mrs Raikes queried the high level of discretionary pay reported in<br />
April. Mr Teape acknowledged that the Senior Management Team’s<br />
focus had not yet had the required impact. The Board agreed that a<br />
seminar on underst<strong>and</strong>ing <strong>and</strong> mitigating discretionary pay would be<br />
incorporated in the Board development schedule.<br />
Workforce<br />
Mr Bamber stated that the scoping of a new framework for non-<br />
10
Item 3<br />
medical appraisal was complete <strong>and</strong> he expected to bring a proposal<br />
to the Senior Management Team to review in July. The Board<br />
discussed the inclusion in appraisal documentation of key clinical<br />
competencies by staff grade. Mr Bamber stated that the <strong>Trust</strong> applied<br />
the <strong>Agenda</strong> for Change Knowledge <strong>and</strong> Skills Framework but Mr Dix<br />
acknowledged that the identification of key clinical competencies<br />
across all wards <strong>and</strong> specialties was inconsistent. There was<br />
agreement that the broader issue was for appraisal documentation to<br />
facilitate the alignment of personal objectives with <strong>Trust</strong> objectives.<br />
D<br />
The twelve month average sickness absence rate had reduced to<br />
4.49%. Focus on progress towards achieving the <strong>Trust</strong> target of 3.8%<br />
was being applied through robust management, with additional<br />
training for managers.<br />
R<br />
Monitor’s Governance Risk Rating<br />
The Board noted the RAG rating of red for April. Professor Lewis<br />
queried the underlying reason for failing the cancer screening service<br />
referral <strong>and</strong> Mr Baber would provide this information outside the<br />
meeting.<br />
A<br />
In concluding the Board’s discussions, it was agreed that the Senior<br />
Management Team would review the presentation <strong>and</strong> content of the<br />
performance narrative to ensure that it provided oversight of KPIs<br />
associated with the implementation of the Winter Plan, the Annual<br />
Business Plan <strong>and</strong> the Board-specific KPIs agreed earlier in the year.<br />
F<br />
The Board noted the Performance Report.<br />
110/13 Infection Prevention <strong>and</strong> Control Annual Report 2012/13<br />
Dr Peter Jenks, Director of Infection Prevention <strong>and</strong> Control, <strong>and</strong> Ms<br />
Claire Haill, Lead Nurse<br />
T<br />
Infection Control, attended for this item.<br />
Dr Jenks presented highlights from his report <strong>and</strong> drew the Board’s<br />
attention to key achievements in 2012/13. Overall, he was pleased to<br />
report a significantly improved position since he was last invited to<br />
report to the Board in September 2012. He acknowledged the<br />
contribution of the Chief Executive in this regard, <strong>and</strong> of Julie<br />
Richards, Associate Director of Planning, <strong>and</strong> Stuart Windsor, Facility<br />
Operations Manager in their work with Serco. Looking forward, new<br />
<strong>and</strong> inexperienced staff would be joining the <strong>Trust</strong> in the next few<br />
weeks <strong>and</strong> the infection control team must prepare for their arrival <strong>and</strong><br />
continue to lead on minimising infections associated with medical<br />
devices.<br />
COO<br />
SMT<br />
The Chairman asked how the <strong>Trust</strong> could ensure a consistently<br />
rigorous focus on infection control. Dr Jenks suggested encouraging<br />
a culture keen to demonstrate best practice. Mr Dix agreed; the nurse<br />
preceptorship period was vital in embedding best practice <strong>and</strong><br />
<strong>supporting</strong> relevant training. Noting the number of bed days lost due<br />
11
Item 3<br />
to Norovirus, Professor Lewis queried new developments that may<br />
mitigate this. Dr Jenks stated that early warning to admitting staff of<br />
community-based occurrences was vital.<br />
The Board noted the Infection Control Annual Report.<br />
Dr Jenks <strong>and</strong> Nurse Haill left the meeting.<br />
D<br />
Mr Teape stated that following the Board’s agreement of the budget<br />
strategy, a £13m deficit budget, after planned CIPs of £24m, had been<br />
agreed <strong>and</strong> submitted to the <strong>Trust</strong> Development Authority.<br />
Discussions continued with the TDA to agree additional support during<br />
the year. They would<br />
R<br />
require the production of a robust three year<br />
programme to achieve a sustainable position. He referred the Board<br />
to paragraph 3.14 of his report, which set out the actions <strong>and</strong><br />
timescales to develop this by September 2013.<br />
Against a planned deficit of £941k in month 1, an actual deficit of<br />
£913k had been recorded,<br />
A<br />
£28k better than planned. Mr Teape stated<br />
that improvements to controls were monitored by the Finance,<br />
Performance & Investment Committee (FPIC), alongside mobilisation<br />
of service line implementation from June. A review of CIPs, by<br />
Directorate, was in progress for review by FPIC in June. In reviewing<br />
the report, Dr Williams suggested the inclusion of actual activity <strong>and</strong><br />
the deployment of reserves<br />
F<br />
to meet this. Mr Teape expected the<br />
quality of reporting to improve from next month following changes to<br />
Finance monthly close arrangements.<br />
Ms James updated the Board on discussions with the TDA. Whilst the<br />
<strong>Trust</strong>’s planned deficit was among the highest reported, overall the<br />
<strong>Trust</strong>’s ambition was<br />
T<br />
considered good. There had been no written<br />
response from the TDA following the ‘Board to Board’ in February but<br />
they had accepted the <strong>Trust</strong>’s budget. She expected external support<br />
to commence in the next few weeks.<br />
111/13 Finance Report: Month 1 Financial Results<br />
Mr Warren stated that during his induction he had picked up on a<br />
prevailing attitude amongst staff that financial issues were always,<br />
somehow, satisfactorily resolved <strong>and</strong> suggested that the Board<br />
reflected on this. Mr Teape acknowledged this; staff had been<br />
informed of the financial situation in the current year but there would<br />
doubtless be a level of scepticism that the Senior Management Team<br />
would need to tackle, particularly given the context of media<br />
announcements of spending on additional staff <strong>and</strong> beds.<br />
In concluding the Board’s discussions, the Chairman stated that the<br />
Board expected pace in the development of the financial recovery<br />
plan.<br />
The Board:<br />
12
Item 3<br />
• Noted the financial position of the <strong>Trust</strong> as at 30 April<br />
2013.<br />
• Approved a deficit budget of £13m for 2013/14.<br />
There was a break between 1.05 pm <strong>and</strong> 1.10 pm.<br />
D<br />
Mr Teape’s report set out the proposed capital programme for<br />
2013/14. The programme had been subject to extensive review by<br />
the Investment Panel, the Capital Steering Group <strong>and</strong> the FPIC, all of<br />
which included clinical representation. Mr Teape stated that it would<br />
be unwise to approve<br />
R<br />
individual elements of the programme at the<br />
expense of others <strong>and</strong> recommended that the Board approved the full<br />
plan with the expectation that cash flow would be tightly managed.<br />
The <strong>Trust</strong>’s Scheme of Delegation defined those individual elements<br />
within the overall plan that must come back to the Board for approval.<br />
Progress with the capital plan delivery was reported monthly to the<br />
Board <strong>and</strong> was subject<br />
A<br />
to FPIC oversight.<br />
112/13 Capital Budget Report 2013/14<br />
Mr Budge noted the Medical Equipment Rolling Replacement<br />
Programme budget of £1.7m <strong>and</strong> queried the criteria used to assess<br />
the risks <strong>and</strong> whether the Board could be assured that equipment for<br />
patients would not fail. Dr Mayor explained the risk assessment<br />
employed by the Medical<br />
F<br />
Devices Strategy Group <strong>and</strong> expressed his<br />
confidence in their decision making process.<br />
Mr Teape referred the Board to section 6 of the report which set out<br />
where capital spend would be focused if additional resources were<br />
available. After reviewing the details the Board took the view that it<br />
was not for Board members<br />
T<br />
to second guess others’ best informed<br />
decisions. They should instead seek assurance of the integrity of the<br />
process in bringing forward these recommendations <strong>and</strong> that the<br />
investments proposed were strategically <strong>and</strong> clinically important. Mr<br />
Douglas stated that FPIC had reviewed the proposed programme<br />
twice. There were risks associated with it but there was also<br />
contingency <strong>and</strong> FPIC supported the programme proposed.<br />
Dr Williams queried the degree to which leasing arrangements were<br />
available. Mr Teape stated that FPIC had previously reviewed this but<br />
it would be picked up as part of the longer term procurement strategy.<br />
Echoing earlier discussions, the Board noted that:<br />
• Linking the capital plan with the site development plan to be<br />
developed as part of the strategy implementation would be<br />
welcome.<br />
13
Item 3<br />
• Careful communication of the spending associated with the<br />
plan was important given the mixed messages to staff <strong>and</strong><br />
public that could arise.<br />
The Board:<br />
• Approved a capital programme of £15m consisting of precommitments<br />
of £4.1m <strong>and</strong> additional proposed schemes<br />
of £11.4m on<br />
D<br />
the underst<strong>and</strong>ing that £0.5m of slippage<br />
would be identified as the year progressed.<br />
• Agreed that this approval would be kept under review in<br />
recognition that affordability was dependent on the <strong>Trust</strong>’s<br />
cash position.<br />
R<br />
• Noted the table of reserve bids in the event that additional<br />
funding could be secured.<br />
• Noted that all other schemes would come back to the<br />
Board as Full Business Cases on the basis that they were<br />
loan funded.<br />
A<br />
113/13 Theatre Safety Improvement Plan<br />
This report set out actions to minimise risk to patients following five<br />
Never Events which occurred between November 2012 <strong>and</strong> March<br />
2013. In addition to the immediate actions described, Dr Mayor<br />
explained the remit of the Surgical Safety Improvement Programme to<br />
F<br />
disseminate medium <strong>and</strong> long term interventions to improve patient<br />
safety. Dr Williams queried the initiatives within teamwork<br />
interventions. Dr Mayor cited the introduction of formal theatre<br />
debriefing sessions associated with the WHO checklist <strong>and</strong> Human<br />
T<br />
Factors training.<br />
Mr Dix outlined the key changes resulting from the Theatre Safety<br />
Improvement Plan under the domains of resources, communication,<br />
Five Steps Safe Surgery <strong>and</strong> training <strong>and</strong> education. The report<br />
detailed the changes expecting during the coming month. The <strong>Trust</strong><br />
would be subject to national expert review at the end of June with<br />
recommendations reported in July. Whilst there had been some<br />
overall slippage with the Plan, he was confident that the <strong>Trust</strong>’s new<br />
organisational structure, including the appointment of a service line<br />
lead for Theatres, would bring this back on track.<br />
The Board welcomed the external involvement detailed in the report<br />
<strong>and</strong> requested periodic reports on progress.<br />
The Board noted the report.<br />
14
Item 3<br />
114/13 Quality Account 2012/13<br />
Dr Mayor presented the Quality Account to the Board for approval.<br />
He assured the Board that appropriate consultation had been, <strong>and</strong><br />
continued to be, undertaken <strong>and</strong> that the document supported the<br />
<strong>Trust</strong>’s overall clinical strategy. The Quality Account had been<br />
reviewed by the Safety & Quality Committee prior to submission to the<br />
<strong>Trust</strong> Board.<br />
D<br />
Dr Williams raised the following queries:<br />
• Page 37 – the 42% completion rate for observation charts was<br />
lower than expected. Dr Mayor stated that the methodology<br />
had changed from previous years <strong>and</strong> performance would be<br />
re-audited to ensure improvement.<br />
R<br />
• Page 6 – include the ‘fifth’ <strong>Trust</strong> value for consistency with<br />
other documents.<br />
• Page 7 – over use of acronyms in this public facing document.<br />
115/13<br />
A<br />
Annual Accounts for the year ended 31 March 2013<br />
Mr Teape presented for approval the accounts <strong>and</strong> associated<br />
documentation for the ended 31 March 2013. These had been<br />
completed to the timescale<br />
F<br />
required by the Department of Health <strong>and</strong><br />
to an exacting st<strong>and</strong>ard, by Sally Wilson. Mr Teape wished to place<br />
on record his thanks to Ms Wilson <strong>and</strong> to Brian Jones, also present,<br />
for their hard work.<br />
Subject to these amendments, the Board approved the Quality<br />
Account.<br />
The Audit Committee had reviewed the accounts <strong>and</strong> associated<br />
documentation at their<br />
T<br />
meeting on 31 May <strong>and</strong> recommended them to<br />
the <strong>Trust</strong> Board for approval. In doing so, the Committee had agreed<br />
that the accounts had been prepared on a going concern basis.<br />
Mr Teape drew the Board’s attention to the external auditor’s draft<br />
Audit Findings report, <strong>and</strong> to the qualified Value For Money conclusion<br />
based on the <strong>Trust</strong>’s inability to achieve the original forecast £1m<br />
budget surplus for 2012/13 <strong>and</strong> its failure to set a balanced budget for<br />
2013/14.<br />
There were no questions.<br />
The Board:<br />
• Approved the annual accounts for the year ended 31<br />
March 2013 <strong>and</strong> authorised their signature by the Chief<br />
Executive <strong>and</strong> the Director of Finance.<br />
15
Item 3<br />
• Approved the writing off of losses <strong>and</strong> special payments<br />
made during the year ended 31 March 2013.<br />
• Authorised the Chief Executive to sign the Letter of<br />
Representation.<br />
116/13 Safety & Quality Committee Chair’s Report<br />
D<br />
The Board noted the Chair’s report of the May meeting <strong>and</strong> noted the<br />
minutes of the April <strong>and</strong> May Committee meetings. No further<br />
assurances were sought.<br />
117/13 Finance, Performance & Investment Committee Chairman’s<br />
Report<br />
R<br />
The Board noted the Chairman’s report of the May meeting <strong>and</strong> noted<br />
the minutes of the April Committee meeting. No further assurances<br />
were sought.<br />
118/13 Any Other Business<br />
A<br />
Comm<strong>and</strong>er Steve Spencer wished to record his appreciation of the<br />
Board’s support for MDHU staff <strong>and</strong> its recognition of their<br />
commitment to the wider organisation. During his tenure as CO,<br />
engagement between the <strong>Trust</strong> <strong>and</strong> the MDHU had increased<br />
immeasurably. Comm<strong>and</strong>er Spencer had enjoyed his time with the<br />
<strong>Trust</strong> <strong>and</strong> wished the Board<br />
F<br />
well for the future.<br />
119/13 Date of next meeting<br />
T<br />
There was no other business <strong>and</strong> the meeting concluded at 1.55 pm.<br />
Friday 5 July 2013 at 9.00 am.<br />
Signed<br />
____________________________________<br />
Dated<br />
____________________________________<br />
16
Updated: prior to July Board Item 4<br />
Outst<strong>and</strong>ing Actions<br />
<strong>Plymouth</strong> <strong>Hospitals</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Action List for <strong>Trust</strong> Board Part 1<br />
Date Ref Action Lead Comments<br />
03.05.13 86/13,<br />
page 3<br />
Learning Disabilities Service<br />
Quarterly Declaration of<br />
Compliance: Director of Nursing to<br />
liaise with Deputy Director of<br />
Nursing to ensure evidence of<br />
learning from patient story to May<br />
Board is included in next scheduled<br />
report in July 2013.<br />
DoN/<br />
DDoN<br />
Scheduled for July<br />
2013 <strong>and</strong> included<br />
on agenda.<br />
Associate Director<br />
of Nursing to give<br />
verbal update<br />
when paper<br />
presented.<br />
07.06.13 103/13,<br />
page 3<br />
Learning from Patient Story: Board<br />
to receive update on<br />
implementation of key learning<br />
issues.<br />
[Post meeting note: at Chief<br />
Executive’s request, action<br />
subsequently extended to reflect<br />
learning from all patient stories<br />
since September 2012 to be led by<br />
Director of Nursing/Director of<br />
Governance].<br />
DoN/DoG<br />
Included on July<br />
Board agenda at<br />
item 5.<br />
07.06.13 107/13,<br />
page 6<br />
Inclusion of site plan in strategy.<br />
Chief Executive, Director of Finance<br />
& Strategy <strong>and</strong> Director of Planning<br />
& Site Services to agree process<br />
<strong>and</strong> timescale, including any<br />
requirement for external assistance,<br />
<strong>and</strong> Chief Executive to include<br />
update in her report to the July<br />
Board.<br />
CE<br />
Scheduled for July<br />
2013.<br />
07.06.13 109/13,<br />
page<br />
11<br />
Senior Management Team to<br />
review content <strong>and</strong> narrative of<br />
performance report to include<br />
oversight of KPIs for Winter Plan,<br />
Annual Plan <strong>and</strong> previously agreed<br />
Board-specific KPIs.<br />
SMT<br />
Timescale not set<br />
<strong>and</strong> no lead<br />
nominated.<br />
Completed actions will be shown for one month only. 1
Updated: prior to July Board Item 4<br />
Actions referred by the Board to Board Committees to progress<br />
Date Ref Committee <strong>and</strong> Action Lead Comments<br />
12.04.13 71/13,<br />
page 7<br />
Safety & Quality Committee<br />
Review performance data<br />
presented to the Board to ensure<br />
Board oversight of contributing or<br />
underlying issues.<br />
The action from the April Board<br />
was:<br />
Dr Mayor reminded Board members<br />
that the HSMR <strong>and</strong> the SHMI were<br />
only two performance measures:<br />
they should not be considered in<br />
isolation but as part of a broader<br />
suite of performance metrics.<br />
Professor Lewis queried whether<br />
the underlying data was reviewed<br />
by the Safety & Quality Committee.<br />
[…] Dr Williams stated that the<br />
Committee did not review data<br />
below the level presented to the<br />
Board <strong>and</strong> relied on the Medical<br />
Director to give assurance on<br />
underlying data <strong>and</strong> to identify any<br />
areas requiring a more detailed<br />
analysis. Professor Lewis<br />
suggested that, under these<br />
circumstances, the Committee<br />
should review below the line. The<br />
Board requested Dr Mayor <strong>and</strong> Dr<br />
Williams, who would be chairing the<br />
Safety & Quality Committee from<br />
June, to review data presentation to<br />
ensure that the Board was sighted<br />
of the contributing, or underlying,<br />
issues. It was agreed that the<br />
Safety & Quality Committee would<br />
review the last three months’ data in<br />
depth.<br />
MD/MW<br />
Outst<strong>and</strong>ing.<br />
Board to have<br />
visibility of<br />
outcome via<br />
Chair’s Report <strong>and</strong><br />
meeting minutes.<br />
On 13.06.13<br />
Board Secretary<br />
clarified action<br />
with Medical<br />
Director <strong>and</strong> NED<br />
Mike Williams.<br />
Agreed that they<br />
would discuss on<br />
day of June Safety<br />
& Quality meeting.<br />
Verbal update at<br />
July meeting.<br />
Completed actions will be shown for one month only. 2
Updated: prior to July Board Item 4<br />
Completed Actions<br />
Date Ref Action Lead Comments<br />
12.04.13 70/13,<br />
page 6<br />
Human Resources &<br />
Organisational Development<br />
Committee<br />
South West Pay, Terms &<br />
Conditions Consortium Report:<br />
HR&ODC to agree action plan <strong>and</strong><br />
process for pursuing ‘optimisers’<br />
within identified, prompt, timescales.<br />
DoHR<br />
&OD<br />
Included in<br />
HR&ODC’s Chair’s<br />
Report to the July<br />
Board <strong>and</strong> minutes<br />
of the June<br />
meeting.<br />
Completed.<br />
12.04.13 74/13,<br />
page<br />
12<br />
Human Resources &<br />
Organisational Development<br />
Committee<br />
National Staff Survey 2012: agree<br />
2/3 issues for immediate focus to<br />
secure step change <strong>and</strong> identify<br />
measures to confirm good, credible<br />
progress of delivery.<br />
DoHR<br />
&OD<br />
Included in<br />
HR&ODC’s Chair’s<br />
Report to the July<br />
Board <strong>and</strong> minutes<br />
of the June meeting<br />
2013.<br />
Completed.<br />
03.05.13 95/13,<br />
page<br />
11<br />
Quality Improvement Strategy:<br />
additions to be made, as set out on<br />
page 12 of May <strong>Trust</strong> Board<br />
minutes. Medical Director to give<br />
verbal update at June Board.<br />
MD<br />
Update given at<br />
June Board, as<br />
scheduled.<br />
Completed.<br />
03.05.13 95/13,<br />
page<br />
12<br />
Quality Improvement Strategy: At<br />
request of Chair of HR&ODC,<br />
Deputy Director of Human<br />
Resources to review HR&OD<br />
Strategy to ensure it supports<br />
above. HR&ODC to review at its<br />
June 2013 meeting.<br />
DDofHR<br />
Update included in<br />
HR&ODC’s Chair’s<br />
Report to the July<br />
<strong>Trust</strong> Board.<br />
Completed.<br />
07.06.13 109/13,<br />
page<br />
10<br />
Exception reports on cancer <strong>and</strong><br />
stroke performance to be included<br />
in the Performance Report to the<br />
July Board.<br />
COO<br />
Scheduled for July<br />
2013 <strong>and</strong> included<br />
in Performance<br />
Report narrative.<br />
Completed.<br />
Completed actions will be shown for one month only. 3
Updated: prior to July Board Item 4<br />
07.06.13 109/13,<br />
page<br />
11<br />
Performance Dashboard, p.22.<br />
Chief Operating Officer to identify<br />
underlying reasons for failure in<br />
April of target for <strong>NHS</strong> cancer<br />
screening service referral <strong>and</strong><br />
advise Professor Lewis.<br />
COO<br />
Completed.<br />
Completed actions will be shown for one month only. 4
Item 8<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Safety & Quality Report<br />
Deputy Director of Nursing, Patient Experience Manager, Patient Safety &<br />
Effectiveness Manager<br />
Director of Nursing <strong>and</strong> Medical Director<br />
Director of Nursing <strong>and</strong> Medical Director<br />
Purpose<br />
To provide a quarterly quality report on the work <strong>and</strong> activities of the<br />
Healthcare Governance Team <strong>and</strong> wider organisation.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
This report provides a quarterly update to the <strong>Trust</strong> Board on Quality; it replaces the quarterly<br />
Healthcare Governance report. Healthcare governance activity is reported monthly to the<br />
Safety & Quality Committee. This report provides an overview for the quarter 1 April 2013 to 15<br />
June 2013. The report includes an analysis of trends, hotspots, themes, issues <strong>and</strong> resulting<br />
improvement.<br />
•<br />
Patient Safety & Clinical Effectiveness highlights the following areas of notable performance:<br />
days since last never event; reduction in harm rate evidenced through global trigger tool <strong>and</strong> a<br />
significant reduction in inpatient falls over the past two months. In addition some areas have<br />
been highlighted as areas of concern as follows: an increase in the proportion of patients<br />
harmed measured using the safety thermometer.<br />
Personal experience report details progress against a number of areas including, PALS,<br />
complaints, local inpatient survey programme <strong>and</strong> the ‘friends <strong>and</strong> family test’ (FFT)<br />
The complaints response rate target of 80% has been achieved for 3 consecutive months,<br />
leading to agreement of a stretched target of 90% by October 2013. PALs figures continue to<br />
remain stable <strong>and</strong> have identified issues with access <strong>and</strong> waiting for our patients. Work to<br />
improve REI signage was as a result of information received through PALS. Plans to survey<br />
complainants to Plans to survey complainants once the complaints process is complete are<br />
now in place <strong>and</strong> will commence from July.<br />
314 inpatients were surveyed during April <strong>and</strong> May, using the Meridian system delivered by our<br />
volunteers.<br />
FFT response rates continue to improve although the 15% target has not been achieved to<br />
date, further work to raise awareness with the public is underway with additional posters <strong>and</strong><br />
banners emphasising the importance of feedback from our patients.
Item 8<br />
Quality Impact Assessment<br />
Paper includes key patient safety, clinical effectiveness <strong>and</strong> patient experience data, providing<br />
assurance regarding high level clinical outcomes, management of adverse events, complaints,<br />
PALS, patient feedback <strong>and</strong> NICE guidance.<br />
Financial Impact Assessment<br />
Potential loss of income if <strong>Trust</strong> fails to meet CQC requirements <strong>and</strong> safety obligations.<br />
Regulatory Impact Assessment<br />
The <strong>Trust</strong> is required to demonstrate compliance with CQC requirements, potential litigation if<br />
incidents <strong>and</strong> complaints are not managed.<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to note the content of the report.<br />
Next Steps<br />
The Safety & Quality Committee will continue to receive monthly reports on healthcare<br />
governance activities. The <strong>Trust</strong> Board will continue to receive detailed quarterly reports,<br />
supplemented by summary reports monthly.<br />
2
Item 8<br />
DETAILED REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Safety & Quality Report<br />
Deputy Director of Nursing, Patient Experience Manager, Patient Safety &<br />
Effectiveness Manager<br />
Director of Nursing<br />
Director of Nursing<br />
1. Purpose<br />
The purpose of this report is to provide the <strong>Trust</strong> Board with an update on Safety <strong>and</strong> Quality<br />
activities within the <strong>Trust</strong>.<br />
2. Background<br />
The <strong>Trust</strong> recognises the importance of continually enhancing its healthcare governance<br />
arrangements for the benefit of our patients. Significant progress has been made in<br />
introducing a revised framework to support the delivery of safe, effective <strong>and</strong> personal care.<br />
The <strong>Trust</strong> has a dedicated Integrated Healthcare Governance Team which seeks to support<br />
clinical teams in the provision of safe, effective <strong>and</strong> personal care.<br />
3. Clinical Effectiveness<br />
3.1 Hospital St<strong>and</strong>ardised Mortality Rate (HSMR)<br />
The Hospital St<strong>and</strong>ardised Mortality Ratio (HSMR) is an indicator of healthcare quality that<br />
measures <strong>and</strong> compares the expected rate of death in the <strong>Trust</strong> with the actual rate of death.<br />
The graph illustrates that the PHNT mean is consistently below the national average of 100<br />
<strong>and</strong> that this position is stable. In addition, there are now 7 consecutive data points below the<br />
mean indicating that the mean could potentially be reset to a lower value. It should be noted<br />
that HSMR is just one quality marker amongst many <strong>and</strong> the drive for improvement must<br />
continue.
Item 8<br />
3.2 Quarterly Summary Hospital-Level Mortality Indicator (SHMI)<br />
SHMI is a hospital-level indicator which reports mortality at trust level across the <strong>NHS</strong> in<br />
Engl<strong>and</strong> using st<strong>and</strong>ard <strong>and</strong> transparent methodology. This indicator is being produced <strong>and</strong><br />
published quarterly by the Health <strong>and</strong> Social Care Information Centre. As with the HSMR<br />
values, the <strong>Trust</strong> has now reported 7 consecutive data points below the mean <strong>and</strong> there is<br />
the option to reset the mean to drive continuous improvement.<br />
4. Patient Safety<br />
4.1 Monthly Incident Reporting Rate<br />
Incident Reporting Rate per 100 Admissions<br />
(May 11 - May 13)<br />
12<br />
Incident Reporting Rate per 100 Admissions<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
6.1<br />
Jul-11<br />
6.7<br />
Aug-11<br />
7<br />
Sep-11<br />
5.8<br />
Oct-11<br />
6.4 6.5<br />
Nov-11<br />
Dec-11<br />
5.6<br />
Jan-12<br />
7.3<br />
Feb-12<br />
6.3<br />
Mar-12<br />
7.5<br />
Apr-12<br />
7.8 8.15 7.95<br />
May-12<br />
Jun-12<br />
Jul-12<br />
8.71<br />
Aug-12<br />
7.92<br />
Sep-12<br />
8.48 8.87 9.69<br />
Oct-12<br />
Nov-12<br />
Dec-12<br />
10.54<br />
9.33 9.4<br />
8.94<br />
Jan-13<br />
Feb-13<br />
Mar-13<br />
Apr-13<br />
Month / Year<br />
Incident Reporting Rate per 100 Admissions UCL LCL Mean<br />
The <strong>Trust</strong> continues to improve the incident reporting rate reflecting an open culture of<br />
reporting <strong>and</strong> learning which is essential in the drive for continuous improvements in patient<br />
safety. The control limits have now been reset to encourage continuing improvement. The<br />
Safe Care Group are currently reviewing the detailed information within this data <strong>and</strong> are<br />
expected to set a revised definition <strong>and</strong> trajectory in order to maintain the focus on patient<br />
safety incidents.<br />
4
Item 8<br />
4.2 Monthly Proportion of Incidents Resulting in Harm<br />
Percentage of Incidents Resulting in Patient Harm<br />
(April 2010 - May 2013)<br />
50%<br />
45%<br />
% of Incidents Resulting in Patient Harm<br />
40%<br />
35%<br />
30%<br />
25%<br />
20%<br />
15%<br />
10%<br />
5%<br />
0%<br />
Apr-10<br />
May-10<br />
Jun-10<br />
Jul-10<br />
Aug-10<br />
Sep-10<br />
Oct-10<br />
Nov-10<br />
Dec-10<br />
Jan-11<br />
Feb-11<br />
Mar-11<br />
Apr-11<br />
May-11<br />
Jun-11<br />
Jul-11<br />
Aug-11<br />
Sep-11<br />
Oct-11<br />
Nov-11<br />
Dec-11<br />
Jan-12<br />
Feb-12<br />
Mar-12<br />
Apr-12<br />
May-12<br />
Jun-12<br />
Jul-12<br />
Aug-12<br />
Sep-12<br />
Oct-12<br />
Nov-12<br />
Dec-12<br />
Jan-13<br />
Feb-13<br />
Mar-13<br />
Apr-13<br />
May-13<br />
Month / Year<br />
% of Incidents Resulting in Harm UCL LCL Mean<br />
This indicates that the current monthly variation is due to natural causes <strong>and</strong> part of a stable<br />
system - the Safe Care Group will review this data <strong>and</strong> investigate potential interventions to<br />
reduce this figure sustainably. Every reported incident is classified based on whether there<br />
was any harm to the patient <strong>and</strong>, if so, the extent of that harm. The previous graph (4.1)<br />
illustrates an increasing reporting rate which, when combined with the above graph, again<br />
suggests that the proportion of incidents resulting in harm to patients is stable in spite of<br />
increasing reporting. Harm is defined as any unintended physical or psychological outcome<br />
for the patient.<br />
4.3 Days Since Last Never Event<br />
300<br />
Number of Days Since Last Never Event<br />
(April 2010 to May 2013)<br />
No of Days Since Last Never Event<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
01/04/2010<br />
01/05/2010<br />
01/06/2010<br />
01/07/2010<br />
01/08/2010<br />
01/09/2010<br />
01/10/2010<br />
01/11/2010<br />
01/12/2010<br />
01/01/2011<br />
01/02/2011<br />
01/03/2011<br />
01/04/2011<br />
01/05/2011<br />
01/06/2011<br />
01/07/2011<br />
01/08/2011<br />
01/09/2011<br />
01/10/2011<br />
01/11/2011<br />
01/12/2011<br />
01/01/2012<br />
01/02/2012<br />
01/03/2012<br />
01/04/2012<br />
01/05/2012<br />
01/06/2012<br />
01/07/2012<br />
01/08/2012<br />
01/09/2012<br />
01/10/2012<br />
01/11/2012<br />
01/12/2012<br />
01/01/2013<br />
01/02/2013<br />
01/03/2013<br />
01/04/2013<br />
01/05/2013<br />
Date<br />
There are no reported Never Events this quarter. The last Never Event was reported on 20 th<br />
March 2013 under the category of Wrong Implant.<br />
5
Item 8<br />
4.4 Monthly Proportion of Patients Harmed (<strong>NHS</strong> Safety Thermometer)<br />
18<br />
<strong>NHS</strong> Safety Thermometer<br />
% of Patients Harmed<br />
Apr 12 ‐ May 13<br />
16<br />
14<br />
% Patients Harmed<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
Apr‐12<br />
May‐12<br />
Jun‐12<br />
Jul‐12<br />
Aug‐12<br />
Sep‐12<br />
Oct‐12<br />
Nov‐12<br />
Dec‐12<br />
Jan‐13<br />
Feb‐13<br />
Mar‐13<br />
Apr‐13<br />
May‐13<br />
% Patients Harmed UCL LCL Mean<br />
Month / Year<br />
The <strong>NHS</strong> Safety Thermometer is a tool for measuring, monitoring <strong>and</strong> analysing the<br />
proportion of patient harm <strong>and</strong> ‘harm-free’ care at a given point in time against four particular<br />
‘types’ of harm. Each month, a snapshot audit is undertaken on every inpatient on a single<br />
day. The audit records the prevalence of 4 different types of harm events:<br />
• Pressure Ulcers<br />
• Catheter Associated Urinary Tract Infections<br />
• DVT <strong>and</strong> PE<br />
• Falls<br />
The audit also records whether the harm event happened prior to or during admission. PHT<br />
is consistently submitting audits for the majority of inpatients <strong>and</strong> is recognised regionally for<br />
this. The graph illustrates that the prevalence of patient harm events remains relatively<br />
stable.<br />
4.5 Monthly Proportion of Patients Harmed (Global Trigger Tool)<br />
GTT: % of Patients Harmed<br />
(Jan 09 - Dec 12)<br />
45%<br />
40%<br />
35%<br />
% of Patients Harmed<br />
30%<br />
25%<br />
20%<br />
15%<br />
10%<br />
5%<br />
0%<br />
Jan-09<br />
Mar-09<br />
May-09<br />
Jul-09<br />
Sep-09<br />
Nov-09<br />
Jan-10<br />
Mar-10<br />
May-10<br />
Jul-10<br />
Sep-10<br />
Nov-10<br />
Jan-11<br />
Mar-11<br />
May-11<br />
Jul-11<br />
Sep-11<br />
Nov-11<br />
Jan-12<br />
Mar-12<br />
May-12<br />
Jul-12<br />
Sep-12<br />
Nov-12<br />
Month / Year<br />
% Patients Harmed Mean UCL<br />
6
Item 8<br />
The <strong>Trust</strong> uses the IHI Global Trigger Tool methodology to conduct retrospective reviews of<br />
patient records using ‘triggers’ to identify possible adverse events. A clinical team review 20<br />
sets of patient notes per month. The graph indicates that from March onwards the majority of<br />
the data points were below the 15% mean. The mean <strong>and</strong> upper control limits have been<br />
recalculated accordingly.<br />
4.6 Hospital Acquired Pressure Ulcers (Datix)<br />
The <strong>Trust</strong> target is a 50% reduction in grade 3 <strong>and</strong> grade 4 hospital acquired pressure ulcers<br />
per month using the P2 measure on National Safety Thermometer<br />
At the Safe Care Group meeting in May 2013 the group reviewed the frequency in<br />
occurrence of hospital acquired pressure ulcers (HAPU) (grade 3 <strong>and</strong> 4) <strong>and</strong> agreed that<br />
hospital acquired pressure ulcers would be monitored monthly by the group. It was also<br />
agreed that the current plan to reduce the numbers of HAPU would be reviewed <strong>and</strong> an<br />
improvement programme implemented to reduce the frequency in line with the CQUIN plan<br />
for 2013/2014.<br />
4.7 Inpatient Falls (Datix)<br />
200<br />
Number of Reported Patient Falls (Datix)<br />
by Month <strong>and</strong> Severity<br />
180<br />
160<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Apr‐11<br />
May‐11<br />
Jun‐11<br />
Jul‐11<br />
Aug‐11<br />
Sep‐11<br />
Oct‐11<br />
Nov‐11<br />
Dec‐11<br />
Jan‐12<br />
Feb‐12<br />
Mar‐12<br />
Apr‐12<br />
May‐12<br />
Jun‐12<br />
Jul‐12<br />
Aug‐12<br />
Sep‐12<br />
Oct‐12<br />
Nov‐12<br />
Dec‐12<br />
Jan‐13<br />
Feb‐13<br />
Mar‐13<br />
Apr‐13<br />
May‐13<br />
None Minor Moderate Severe/Catastrophic Death caused by the incident<br />
7
Item 8<br />
Inpatient falls are currently monitored by the Nursing <strong>and</strong> Midwifery Board. April <strong>and</strong> May<br />
have seen a significant reduction in the number of inpatient falls which is likely to be<br />
attributable to an increase in nursing staffing on the wards. Work continues to further<br />
improve this number. The <strong>Trust</strong> target is to reduce the number of falls to less than 50 per<br />
month.<br />
5 Patient Experience<br />
5.1 Patient Advice <strong>and</strong> Liaison Service (PALS)<br />
PALS team provide an on dem<strong>and</strong> service with the aim of resolving patient issues at an early<br />
stage, to avoid situations developing into formal complaints.<br />
The <strong>Trust</strong> received a total of 847 PALS enquiries for the period 01 Apr 2013 to 17 Jun 2013.<br />
PALS enquiries listed by directorate are detailed below.<br />
8
Item 8<br />
PALS enquiries are broken down in the 5 themes / subjects as detailed below.<br />
• Information, Communication <strong>and</strong> Choice - 277<br />
Communication issues 86<br />
Information provision 40<br />
Staff attitude 21<br />
• Access <strong>and</strong> Waiting - 168<br />
Outpatient delays 55<br />
Inpatient delays / 18ww 47<br />
9
Item 8<br />
REI signage<br />
PALS were contacted by the husb<strong>and</strong> of a patient who is severely visually impaired <strong>and</strong> who<br />
recently attended the REI at Derriford for the first occasion. Following the appointment, the<br />
patient’s husb<strong>and</strong> e-mailed PALS to express concerns regarding the poor signage to the REI<br />
from the car parks at the rear of the hospital site. He suggested a review of the current<br />
signage from the rear of the hospital <strong>and</strong> the route through the building from Level 6 to Level<br />
3 <strong>and</strong> also came up with a number of innovative ideas for the <strong>Trust</strong>’s consideration.<br />
In discussion with the patient <strong>and</strong> her husb<strong>and</strong> <strong>and</strong> the Head of Site <strong>and</strong> Environmental<br />
Services, arrangements are being made to carry out a walk around the site with a view to<br />
determining what can be done to provide a safer/more patient friendly environment. There<br />
are plans to include patient representatives, a member of the RNIB <strong>and</strong> other interested<br />
parties.<br />
Update<br />
Further to the concerns expressed by a patient with severe visual impairment <strong>and</strong> her<br />
husb<strong>and</strong> late in April, a site walk around was conducted at the end of May. The patient<br />
attended with her husb<strong>and</strong> <strong>and</strong> her Guide Dog. Also present were the <strong>Trust</strong> Leads for<br />
Environment <strong>and</strong> Sustainability <strong>and</strong> Hotel Services <strong>and</strong> representatives from the Royal<br />
National Institute for the Blind South Devon <strong>and</strong> Cornwall Institute for the Blind <strong>and</strong> a<br />
member of the PALS team.<br />
The site visit incorporated a review of the bus stop area near the main entrance of the<br />
hospital, the new blue badge parking site that will commence work later this month (adjacent<br />
to the Chest Clinic) <strong>and</strong> signage to <strong>and</strong> from both areas.<br />
Signage within the main building as well as at the REI main base on level 3 was reviewed<br />
<strong>and</strong> reviewed the safety <strong>and</strong> quality of signage to the pedestrian crossings near the main<br />
entrance <strong>and</strong> on level 3. A number of required improvements were noted <strong>and</strong> although the<br />
works are on-going the patient representatives felt the visit was informative <strong>and</strong> were<br />
reassured that the <strong>Trust</strong> is listening <strong>and</strong> acting on what our patients are saying to us. It was a<br />
very positive afternoon which has forged good links with the visually impaired community.<br />
Breaking Bad News<br />
There has been a gradual increase in the number of reports <strong>and</strong> concerns raised by relatives<br />
<strong>and</strong> carers in relation to the approach used when breaking bad news notably the<br />
environment in which these conversations take place. In a number of cases these<br />
conversations were held in corridors or on an open ward. Families feel they have not been<br />
given the time <strong>and</strong> space to absorb sad news. Whilst we appreciate space is at a premium<br />
there is a significant impact on family members many of whom are left with unresolved<br />
questions <strong>and</strong> a sense that the <strong>Trust</strong> does not care or respect their feelings.<br />
Awareness training will be reviewed to ensure it considers the environment when breaking<br />
bad news. Information relating to similar cases will be considered by ward area to identify<br />
any areas where the lack of privacy is a particular issue.<br />
5.2 Complaints<br />
The chart below details the number of complaints received between May 2012 <strong>and</strong> May<br />
2013.<br />
10
Item 8<br />
Continued effort to monitor performance against the complaints response target has<br />
significantly improved the number of complaints responded to within agreed timeframes.<br />
Plans to survey complainants once the complaints process is complete are now in place.<br />
Commencing from July complainants will be sent a satisfaction survey asking them for their<br />
views of the process <strong>and</strong> whether they felt their issues were fully resolved <strong>and</strong> their concerns<br />
addressed.<br />
Following the success achievement of the 80% complaints performance target the Director of<br />
Nursing has agreed a revised target of 90% from 1 st October 2013.<br />
11
Item 8<br />
Complaints received listed by directorate.<br />
Complaints<br />
received broken down in the 5 themes / subjects as detailed below.<br />
12
Item 8<br />
5.3 Learning <strong>and</strong> improving<br />
The following table summarises current themes <strong>and</strong> improvement actions that have been<br />
identified from all Healthcare Governance activity including complaints <strong>and</strong> PALS.<br />
Theme Actions / Improvement Lead Timeframe<br />
Major project aiming to improve overall<br />
healthcare administration functions<br />
including:<br />
Sam Sheridan Mar 2014<br />
• Self Check-In <strong>and</strong> Electronic Outcome<br />
Forms<br />
• Digital dictation<br />
• Review of the clinical office<br />
Clinical<br />
Administration<br />
• Electronic document management<br />
systems<br />
Review • Review of health records<br />
• Ward administration<br />
• Managed mail<br />
• Enhanced telephony<br />
• Appointments, booking <strong>and</strong> prep<br />
• Internal Communication Environment<br />
(ICE) – improved information links with<br />
primary care<br />
Outpatient<br />
Follow Up<br />
Delay<br />
• Issues pertaining to the follow up<br />
backlog <strong>and</strong> subsequent delays in<br />
outpatient appointments at the REI are<br />
managed through Task & Finish Group<br />
chaired by the Assistant Medical<br />
Director. Work is progressing to reduce<br />
the backlog including validation of all<br />
patients <strong>and</strong> appointments<br />
Paul McArdle<br />
Ongoing<br />
Parking –<br />
disabled<br />
spaces<br />
Parking &<br />
signage – REI<br />
• Improved availability for members of<br />
public requiring disabled spaces.<br />
Working Group in place including<br />
members of the public <strong>and</strong> LINK.<br />
• Walk round of the new REI area to<br />
identify future improvements to signage.<br />
Patient representatives, member of<br />
RNIB <strong>and</strong> other interested parties<br />
involved in walk round on 28 May 13.<br />
Action plan agreed.<br />
Andrew Davies Start date<br />
Jun 13<br />
Andres Davies<br />
Liz McGuffog<br />
30 Jun 13<br />
5.4 Patient Feedback<br />
The <strong>Trust</strong> programme for gathering feedback from our inpatients began in October 2010 <strong>and</strong><br />
covers all wards except intensive care, critical care, high dependency <strong>and</strong> paediatric areas,<br />
to date 5824 patients have been surveyed.<br />
Local inpatient ward satisfaction surveys are undertaken using iPads on an ongoing basis by<br />
a number of volunteers. A selection of wards, grouped by Matron is targeted each month on<br />
a rolling programme using the Meridian System. The survey report based on the findings is<br />
available to the matron, sister/manager <strong>and</strong> ward management to review through the<br />
Meridian system. Actions <strong>and</strong> learning are subsequently developed <strong>and</strong> sent to the Patient<br />
Experience<br />
Manager for ongoing management.<br />
13
Item 8<br />
The graphs below illustrate responses provided from the updated Local Adult<br />
Survey between 01 July 2012 – 31 May 2013, when 2903 patients were surveyed.<br />
Inpatient<br />
For the period 01 April 2013 to 31 May 2013 413 patients were surveyed.<br />
Would you recommend <strong>Plymouth</strong> <strong>Hospitals</strong> <strong>NHS</strong> <strong>Trust</strong> to your family <strong>and</strong> friends?<br />
How would you rate the care you are receiving?<br />
Do you think the hospital staff do everything they can to help control your pain?<br />
14
Item 8<br />
Do you feel that staff involve you in decision about your care <strong>and</strong> treatment?<br />
In your opinion how clean is the hospital room or ward you are staying on?<br />
On the ward you are staying on, are you treated with dignity <strong>and</strong> respect?<br />
Plans to introduce a Patient Experience Committee, chaired by the Director of Nursing have<br />
been agreed <strong>and</strong> will include members of the public, clinical <strong>and</strong> management staff. The first<br />
meeting will take place in July 2013. The committee will drive forward the patient experience<br />
strategy <strong>and</strong> develop an annual plan of work. An action plan to address a number of the key<br />
patient experience issues <strong>and</strong> concerns will be produced <strong>and</strong> monitored through the Patient<br />
Experience Committee.<br />
15
Item 8<br />
5.5 Friends <strong>and</strong> Family Test<br />
From 1 st April 2013, all organisations providing <strong>NHS</strong> funded services are required by the<br />
Department of Health to ask the Friends <strong>and</strong> Family question. A similar question is used in<br />
the private sector to give a headline figure that shows overall customer satisfaction, generally<br />
known as the ‘Net Promoter’ score.<br />
The implementation plan agreed in November 2012 is now complete. Further work is now<br />
required to ensure the <strong>Trust</strong> is fully compliant with the Friends <strong>and</strong> Family Test, including<br />
improving performance to achieve the 15% response rate required to achieve the CQUIN<br />
targets. Further roll out to Maternity Services by October 2013 is planned.<br />
Continued efforts throughout May resulted in an increase in response rates from 11.5% to<br />
13.5% for inpatients in May <strong>and</strong> 5.3% to 8.4% for Emergency Department. Further work to<br />
raise awareness for both staff <strong>and</strong> members of the public will include information st<strong>and</strong>s<br />
throughout the remainder of June <strong>and</strong> July, posters <strong>and</strong> banners reminding patients of the<br />
importance of returning their completed questionnaires. Targeted support from the Patient<br />
Services Team will be given to those areas where results are particularly disappointing.<br />
May 2013 Results<br />
Acute Inpatient<br />
Total number of people eligible to respond - 2953<br />
Extremely<br />
Likely<br />
Likely<br />
Neither<br />
Likely nor<br />
Unlikely<br />
Unlikely<br />
Extremely<br />
Unlikely<br />
Don’t Know<br />
Total<br />
Responses<br />
265 112 10 10 5 4 398<br />
Emergency Department<br />
Total number of people eligible to respond – 4511<br />
Extremely<br />
Likely<br />
Likely<br />
Neither<br />
Likely nor<br />
Unlikely<br />
Unlikely<br />
Extremely<br />
Unlikely<br />
Don’t Know<br />
Total<br />
Responses<br />
241 94 23 11 4 4 377<br />
16
Item 8<br />
FFT scores are calculated on a monthly basis using the following equation:<br />
Proportion of respondents who would be extremely likely to recommend (response category:<br />
“extremely likely”)<br />
MINUS<br />
Proportion of respondents who would not recommend (response categories: “neither likely<br />
nor unlikely”, “unlikely” & “extremely unlikely”)<br />
Figures detailing FFT rates for all acute <strong>Trust</strong>s will be published by the Department of Health<br />
at the end of July, thereby providing a benchmark to measure progress against.<br />
6. Patient Opinion<br />
Over the past 12 months 108 comments have been posted, all of which have been<br />
responded to. The top three areas for concern relate to attitude of staffing, communication,<br />
<strong>and</strong> lack of information provided regarding care. In the past three months there has been a<br />
notable increase in the number of compliments posted in the website, 58 of the postings<br />
have been positive feedback. An example of a recent compliment from a gentleman who<br />
was admitted as an emergency is shown below.<br />
As arthritic sufferer, aged 73, I am most grateful for the reception, check, interest <strong>and</strong> respect taken<br />
throughout by all the staff. Given the recent virulent criticisms of the <strong>NHS</strong>, I can only say a massive<br />
"Thank You" to Derriford Hospital. Head of A&E can be proud of their team, <strong>and</strong> I Ieft feeling<br />
comforted <strong>and</strong> re-assured.<br />
7. Ward Audits<br />
The <strong>Trust</strong> programme for audting all wards using the Meridian tool began in December 2011.<br />
This report will now focus on the following Nursing Quality Indicators, the charts below<br />
showing performance in the last year. The next quarter will see considerable changes to<br />
questions as a result of triangulation.<br />
17
Item 8<br />
1. Pressure Ulcers (EoC)<br />
2. Falls (EoC)<br />
3. Hydration & Nutrition (EoC)<br />
4. Observations - completeness <strong>and</strong> escalation (EoC)<br />
5. Cleanliness<br />
7.1 Essence of Care (EoC)<br />
16255 individual patient audits have been completed up to 18 June 2013.<br />
Pressure Ulcers<br />
The essence of care audit assesses the following:<br />
• Compliance with Waterlow assessment<br />
• Compliance with up-to-date EPUAP assessment<br />
Analysis/Action – this assures us that assessments are being undertaken. However, there<br />
are two themes from our RCA’s; inaccurate assessment <strong>and</strong> inaction/wrong action following<br />
assessment. The Safe Care Group will consider a paper in July proposing a revised<br />
approach to measurement (outcome focussed) <strong>and</strong> a re-launch of intentional rounding.<br />
18
Item 8<br />
Falls<br />
The essence of care audit assesses the following:<br />
• Compliance with Morse assessment<br />
• Compliance with up-to-date EPUAP assessment<br />
Analysis/Action - This suggests that assessments of risks of falls are being undertaken on a<br />
reliable basis. However, if does not tell us how these risk assessments have informed the<br />
care plan or if the correct preventative measures have been put in place to reduce the risk of<br />
falls in hospital. The Safe Care Group will consider a paper in July proposing a revised<br />
approach to measurement (outcome focussed) <strong>and</strong> a re-launch of the Falls reduction<br />
package across our wards.<br />
Nutrition & Hydration<br />
The essence of care audit assesses the following:<br />
• Compliance with MUST assessment<br />
• Where needed has a food chart been completed?<br />
Analysis/Action - The newly formed Nutrition task <strong>and</strong> finish will review all feedback<br />
regarding nutrition <strong>and</strong> develop an improvement plan to address patient feedback results,<br />
reduce patient complaints <strong>and</strong> improve use of MUST assessment. The question in the local<br />
inpatient survey will also be revised to ensure that vulnerable patients are being asked the<br />
question; the current results indicate that the wrong patients are being asked if they received<br />
help <strong>and</strong> thus the giving false assurance.<br />
19
Item 8<br />
Observations<br />
The essence of care audit assesses the following:<br />
• Have observations been performed at the required frequency<br />
• Has there been a red trigger in the last 24hrs?<br />
• What is recorded about escalation actions trigger?<br />
Analysis/Action – these results would suggest that Observations are being done when<br />
required <strong>and</strong> that triggers are being escalated. However, a recent spot audit undertaken on<br />
one day suggested concerns about a lack of escalation. That said, different measures were<br />
used during the spot audit <strong>and</strong> as a consequence, a review is underway. <strong>and</strong> a further spot<br />
audit undertaken in July.<br />
7.2 Cleanliness Audits<br />
1951 audits have been completed up to 18 June 2013. The environment audit addresses a<br />
number of cleanliness issues; the key issue being the cleanliness of commodes as part of<br />
infection prevention <strong>and</strong> control. These audits include regular ‘Peer review’.<br />
20
Item 8<br />
Commodes<br />
Analysis/Action – Whilst the position has improved over the past twelve months there<br />
continues to be sporadic failures from both the meridian audit <strong>and</strong> the internal audit process<br />
(latter improved recently). Meridian now sends a real time alert direct to a specified group<br />
when a commode inspection fails; if any ward fails the commodes audit, they are<br />
automatically monitored on a daily basis until the Matron is assured that the issues are<br />
addressed (i.e. as evidenced by consistent non-failure of commode inspections).<br />
21
Item 8a<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Serious Patient Safety Incidents <strong>and</strong> Complaints - Summary Review<br />
June 2012 – May 2013<br />
Patient Safety & Effectiveness Manager, Patient Experience Manager<br />
Medical Director<br />
Medical Director <strong>and</strong> Director of Nursing<br />
Purpose<br />
To provide the Board with a summary of serious incidents, serious <strong>and</strong><br />
significant complaints for June 2012 – May 2013, including common themes<br />
<strong>and</strong> improvement programmes in place to avoid further harm.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
The <strong>Trust</strong> reported 64 serious incidents in the reporting period (June 2012 – May 2013) shown<br />
in Annex 1. These have been categorised by type to provide assurance that themes <strong>and</strong> trends<br />
have been identified <strong>and</strong> that improvement programmes are in place.<br />
During the same period the <strong>Trust</strong> received 36 serious <strong>and</strong> significant complaints, shown as<br />
Annex 2.<br />
Quality Impact Assessment<br />
This report provides assurance that progress is being made in meeting the <strong>Trust</strong>’s objective of<br />
providing safe, effective <strong>and</strong> personal care to patients.<br />
Financial Impact Assessment<br />
Potential loss of income if <strong>Trust</strong> fails to meet CQC requirements <strong>and</strong> safety obligations.<br />
Regulatory Impact Assessment<br />
Applicable to all CQC regulations relating to Safety & Quality.<br />
Key Recommendations<br />
The Board are asked to note the contents of the report.<br />
Next Steps<br />
The <strong>Trust</strong> Board will continue to receive quarterly reports.<br />
•<br />
•
Annex 1<br />
Item 8a<br />
SURGICAL ERROR<br />
• 4 Serious Incidents Reported (+ 3 surgical never<br />
events in March 2013<br />
• Common themes identified during investigation:<br />
• Team working, culture <strong>and</strong> behaviour<br />
• Lack of st<strong>and</strong>ardised process<br />
• Surgical Safety Improvement Programme established<br />
• Accountable Lead: Greg Dix<br />
• Reporting to Safety & Quality Committee<br />
VENOUS THROMBOEMBOLISM<br />
• 2 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
• Failure to act on risk assessment<br />
• Failure to administer prescribed prophylaxis<br />
• VTE Improvement Workstream established<br />
• Accountable Lead: Alex Mayor<br />
• Reporting to Safe Care Group<br />
DELAYED DIAGNOSIS/FAILURE TO ACT ON DIAGNOSTIC RESULTS<br />
• 5 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
• Inadequate system to ensure results reviewed / acted on<br />
• Inadequate failsafe to highlight un‐reviewed reports<br />
• Radiology Improvement Workstream established<br />
• Accountable Lead: Peter Macnaughton<br />
• Reporting to Safe Care Group<br />
UNEXPECTED DEATH OF ADULT<br />
• 2 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
• None‐ remain under investigation<br />
• Completed RCAs to be reviewed by Safe Care<br />
Group to identify learning <strong>and</strong> required actions<br />
Confidential Information Leak, 1<br />
Venous Thromboembolism, 2<br />
Delayed diagnosis or failure to act<br />
on diagnostic results, 5<br />
Unexpected death of adult, 2<br />
Surgical Error (Retained foreign<br />
object or wrong site surgery), 4<br />
Maternity Incident, 2<br />
Ward Closure / Infection Control<br />
Incident, 10<br />
Serious Patient Safety Incidents<br />
Summary Review of Reported SIRIs<br />
June 2012 – May 2013<br />
Serious Incidents Reported by PHNT<br />
Other, 3<br />
WARD CLOSURE/INFECTION CONTROL<br />
• 10 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
•<br />
• Improvement Workstream established:<br />
• Accountable Lead: Peter Jenks<br />
• Reporting to Infection Control Committee<br />
Unexpected death of child, 2<br />
Inpatient fall, 3<br />
Drug Incident (Insulin), 1<br />
Follow Up Appointment Delay, 1<br />
Hospital Acquired Pressure Ulcer<br />
(3/4), 28<br />
INPATIENT FALLS<br />
• 3 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
• Failure to complete risk assessment<br />
• Failure to act on risk assessment<br />
• Safety Improvement workstream established<br />
• Accountable Lead: Kevin Marsh<br />
• Reporting to Nursing <strong>and</strong> Midwifery Board<br />
UNEXPECTED DEATH OF CHILD<br />
• 2 Serious Incident Reported<br />
• Investigation ongoing<br />
• Safe Care Group to review completed investigation<br />
report <strong>and</strong> identify learning <strong>and</strong> necessary actions<br />
HOSPITAL ACQUIRED PRESSURE ULCERS (3/4)<br />
• 28 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
• Failure to complete risk assessment<br />
• Failure to act on completed risk assessment<br />
• Safety Improvement Workstream established<br />
o Accountable Lead: Kevin Marsh<br />
o Reporting to Safe Care Group<br />
DRUG INCIDENT (INSULIN)<br />
• 1 Serious Incidents Reported<br />
• Common themes identified during investigation:<br />
• Failure to follow Hyperkalaemia treatment<br />
guidelines<br />
• Safe Use of Insulin Improvement Workstream<br />
established<br />
• Accountable Lead: Daniel Flanagan<br />
• Reporting to Safe Care Group<br />
FOLLOW UP APPOINTMENT DELAY<br />
• 1 Serious Incidents Reported (Ophthalmology)<br />
• Common themes identified during investigation:<br />
• Waiting lists not prioritised by clinical risk<br />
• Inadequate capacity to meet dem<strong>and</strong><br />
• Follow Up Backlog Improvement Workstream<br />
established<br />
• Accountable Lead: Paul McArdle<br />
• Reporting to Safety & Quality Committee
Annex 2<br />
Item 8a<br />
Summary of Serious <strong>and</strong> Significant Complaints (June 2012 – May 2013)<br />
Serious <strong>and</strong> Significant Complaints by Sub‐type<br />
Adverse outcome of<br />
Operation/Surgery, 3<br />
Weekend Discharge,<br />
1<br />
Aspects of Clinical<br />
treatment, 6<br />
Clinical Review , 1<br />
Communication to<br />
Patient/Relatives, 2<br />
Conflicting Clinical<br />
Decisions, 1<br />
Incorrect diagnosis<br />
(where no<br />
treatment), 7<br />
Breakdown of Complaints by Grading<br />
Number of Serious Complaints = 11<br />
Number of Significant Complaints = 24<br />
Number of Significant Professional Complaints = 1<br />
Breakdown of Complaints by Directorate<br />
Clinical Support Services = 2<br />
Ophthalmology = 1<br />
Emergency Services = 9<br />
Medical Specialties = 3<br />
Orthopaedics & Rheumatology = 2<br />
General<br />
impoliteness/indiffer<br />
ence, 1<br />
Clinical Review, 3<br />
Pain Control, 1<br />
Outpatient delay, 2<br />
Inpatient Delays, 1<br />
Incorrect Diagnosis,<br />
1<br />
Drug error/incident,<br />
3<br />
Slips, Trips <strong>and</strong> Falls,<br />
2<br />
Inappropriate<br />
Discharge, 1<br />
Gastroenterology, Surgery <strong>and</strong> Renal = 10<br />
Oncology & Blood Services = 1<br />
Head & Neck Surgery = 2<br />
Neurosciences = 2<br />
Reproductive Health, Neonatal & Women's<br />
Services = 2<br />
Children & Young People's Health = 1<br />
Anaesthetics, Theatres & Pain = 1
Item 9<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject Performance Report (Month 2)<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Purpose<br />
Advanced Performance Analyst<br />
Deputy Head of Performance<br />
Chief Executive <strong>and</strong> Executive Leads<br />
This paper highlights <strong>and</strong> summarises the key performance issues that have<br />
arisen during May 2013, describes the mitigating actions <strong>and</strong> provides an<br />
assessment of the future projected performance risk.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
• • • •<br />
Executive Summary<br />
This is the integrated performance report for May 2013 <strong>and</strong> formally reports much of the data<br />
that was covered verbally at the June 2013 Board.<br />
As with previous reports, performance against key indicators is mixed with a number of areas of<br />
positive performance for example VTE risk assessment. In some cases such as achievement<br />
of the ED 4 hour target performance has improved markedly on April <strong>and</strong> continues to improve<br />
in June 2013. This is also the case with cancelled operations where performance has<br />
improved significantly in recent weeks.<br />
Of concern is the deterioration of performance against the 6 week diagnostic target <strong>and</strong> this is<br />
largely explained by failure in one area <strong>and</strong> a further verbal update will be given at Board<br />
regarding action to resolve. Exception reports for Stroke, cancer 62 day <strong>and</strong> cancelled<br />
operations are included at annex 2, 3 <strong>and</strong> 4.<br />
Quality Impact Assessment<br />
The safety <strong>and</strong> quality section of the report highlights positive performance against a range of<br />
indicators <strong>and</strong> this will be explored further in the quarterly quality report to this Board.<br />
Financial Impact Assessment<br />
The financial position of the <strong>Trust</strong> is on plan at month 2 although significant actions are required<br />
to ensure the achievement of the cost improvement programme.<br />
The contract position at month 2 is significantly under achieving from a financial perspective as<br />
a result of a lower case mix, lower activity in key areas <strong>and</strong> contract fines. Emergency activity is<br />
already above plan. Whilst the financial impact is mitigated in 2013-14 due to the nature of the<br />
contract signed the recurring impact if this continues is of significant concern <strong>and</strong> action is<br />
required to underst<strong>and</strong> the position in more detail.<br />
Regulatory Impact Assessment<br />
This paper addresses the performance of the <strong>Trust</strong> against its statutory financial <strong>and</strong> performance<br />
duties <strong>and</strong> against <strong>Trust</strong> Development Authority <strong>and</strong> Monitor financial st<strong>and</strong>ards.<br />
•<br />
•<br />
1
Item 9<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Note the monthly position <strong>and</strong> update of the <strong>Trust</strong> on performance for Month 2.<br />
2. Review the summary of performance exception reports for stroke, cancer 62 day <strong>and</strong> cancelled<br />
operations detailed in Annex 1-4.<br />
Next Steps<br />
The Board will be provided with monthly updates on our performance.<br />
2
Item 9<br />
DETAILED REPORT<br />
<strong>Trust</strong> Board June 2013<br />
Subject Performance Report (Month 2)<br />
Prepared by<br />
Approved by<br />
Presented by<br />
1 Introduction<br />
Advanced Performance Analyst<br />
Deputy Head of Performance<br />
Chief Executive <strong>and</strong> Executive Leads<br />
This paper summarises <strong>Trust</strong> performance against the key national <strong>and</strong> local targets up to<br />
end of May 2013. Mitigating actions are described where underperformance is identified.<br />
This report accompanies the detailed Performance Dashboard for May 2013.<br />
2 Safety & Quality<br />
The below diagram provides headlines on current performance across the safety <strong>and</strong><br />
quality domain.<br />
Safe<br />
Care<br />
The <strong>Trust</strong> remains top performer in the South‐West for HSMR <strong>and</strong> benchmarks well for SHMI<br />
Incident reporting rate remains in the national upper quartile demonstrating a positive reporting culture<br />
% of incidents resulting in harm remains above internally set threshold<br />
Effective<br />
Care<br />
The <strong>Trust</strong>'s readmission rate is ~4% better than expected<br />
Despite positive performance against expected levels, the <strong>Trust</strong> does not benchmark well vs other SW <strong>Trust</strong>s<br />
SAFETY<br />
&<br />
QUALITY<br />
Patient<br />
Experience<br />
% of complaints responded to in timeframe remains above target<br />
Zero non‐clinically justified single sex breaches this year<br />
Friends <strong>and</strong> family test response rates are below suggested levels of 15%<br />
Number of cancelled operations <strong>and</strong> associated 28‐day breaches remains high<br />
Infection<br />
Control<br />
Zero cases of hospital apportioned MRSA this year<br />
Number of hospital apportioned C‐Diff cases remains below trajectory<br />
No ward closures for Norovirus<br />
Other<br />
>95% of eligible patients risk assessed for VTE in April <strong>and</strong> May<br />
Hip fracture <strong>and</strong> stroke targets failed in April <strong>and</strong> May<br />
Follow‐up backlog continues to grow<br />
Safe Care (Section B1 of Performance Dashboard)<br />
2.1 The <strong>Trust</strong> continues as the South-West’s top performer for HSMR <strong>and</strong> performs<br />
approximately 5% better than expected for the SHMI measure. These areas remain<br />
under scrutiny via the Clinical Effectiveness Group.<br />
2.2 The <strong>Trust</strong>’s incident reporting rate of 9.7 incidents per 100 admissions remains within<br />
the national upper quartile <strong>and</strong> demonstrates a positive reporting culture. Conversely,<br />
the data demonstrates a harm rate above the internal threshold set at 28%.<br />
2.3 Surgical safety checklist compliance remains high (98% in May) however the data<br />
shows that particular specialties continue to underperform in this area. A review of the<br />
data is underway to ensure that instances where only a partial checklist is required<br />
are not counting against the service lines inappropriately.<br />
3
Item 9<br />
Effective Care (Section B2 of Performance Dashboard)<br />
2.4 The <strong>Trust</strong>’s readmission rate remains ~3% lower than expected resulting in a<br />
benchmarked South-West position of 12 th from 18 <strong>Trust</strong>s.<br />
Patient Experience (Section B3 of Performance Dashboard)<br />
2.5 The friends <strong>and</strong> family test was introduced to the <strong>Trust</strong> in April <strong>and</strong> has started to<br />
feedback information about patient opinion. Although we are yet to reach the<br />
recommended response rate of 15% for both cohorts (A+E <strong>and</strong> inpatients) the data<br />
shows a gradual improvement in the number of A+E attendees recommending our<br />
service but conversely a reduction in the number of inpatients who would recommend<br />
the <strong>Trust</strong>.<br />
2.6 61 operations were cancelled on the day of admission for non-clinical reasons in May<br />
representing 1.27% of all elective admissions. This is a significant improvement on<br />
April which saw 130 operations cancelled on the day (2.65% of all elective<br />
admissions). The availability of general beds continues to be the most prevalent<br />
reason for cancellation. See Annex 3 for exception report.<br />
Infection Control (Section B4 of Performance Dashboard)<br />
2.7 The <strong>Trust</strong> has reported no cases of hospital apportioned MRSA this year whilst the 4<br />
cases of hospital apportioned C.Difficile are in line with the trust’s trajectory of no<br />
more than 2 cases per month.<br />
2.8 Patient level MRSA screening for elective admissions has reduced to 91% in May,<br />
5% lower than this time last year. This drop in performance has been escalated at the<br />
Matrons meeting <strong>and</strong> individual pockets of poor performance are being addressed.<br />
2.9 The <strong>Trust</strong> has reported no ward closures due to Norovirus in 13/14.<br />
Other Quality <strong>and</strong> Safety Measures (Section B5 of Performance Dashboard)<br />
2.10 The <strong>Trust</strong> continues to achieve the national VTE risk assessment st<strong>and</strong>ard with 95%<br />
of eligible patients being risk assessed. Work continues to focus on those areas<br />
where non-compliant patients are identified whilst qualitative audits are also<br />
underway to ensure the procedure is being carried out effectively.<br />
2.11 The <strong>Trust</strong> has failed to operate on at least 85% of fractured neck of femur patients<br />
within 36hrs of admission in April <strong>and</strong> May. Of the 13 May patients who failed to get to<br />
theatre within the required timeframe, 8 were medically unfit.<br />
2.12 Despite an improvement on April’s performance (59%), the <strong>Trust</strong> has failed to deliver<br />
the stroke target in May with only 67% of stroke patients spending 90% or more of<br />
their stay on the acute stroke unit. See Annex 1 for exception report.<br />
2.13 As at the 31 st May, the follow-up backlog had risen to 24,305 patients, an increase of<br />
767 patients from April.<br />
4
Item 9<br />
3 Access <strong>and</strong> Activity<br />
The below diagram provides headlines on current performance across the access & activity<br />
domain.<br />
A&E<br />
A+E 4hr wait target failed in April <strong>and</strong> May<br />
30‐min ambulance h<strong>and</strong>over target failed in April <strong>and</strong> May<br />
Cancer<br />
Year‐to‐date failure of 62‐day urgent referral <strong>and</strong> screening cancer targets<br />
Remaining seven cancer targets remain on target in‐month <strong>and</strong> YTD<br />
ACCESS<br />
&<br />
ACTIVITY<br />
RTT<br />
April <strong>and</strong> May failure of incomplete pathways <strong>and</strong> admitted pathways 18‐week RTT targets<br />
Decision‐to‐treat <strong>and</strong> non‐admitted RTT backlogs continue to grow<br />
Admitted backlog reduction remains on plan<br />
Diagnostics<br />
173 patients (2.8% of total list) were waiting over 6 weeks for a diagnostic test at end of May<br />
Other<br />
Non‐elective activity remains below plan<br />
Average medical outlier occupancy has reduced in May<br />
Small reduction in medical <strong>and</strong> surgical length of stay in May<br />
Access to rapid access chest pain clinic, GUM <strong>and</strong> primary PCI remain above target<br />
Medical Admissions remain greater than plan<br />
Accident <strong>and</strong> Emergency (Section B1 of Performance Dashboard)<br />
3.1 A&E 4hr wait performance improved significantly in May but fell just short of the 95%<br />
national st<strong>and</strong>ard at 94.8% (402 patients waited longer than 4hrs). Performance<br />
continues to improve throughout June <strong>and</strong> although current trajectory suggests we<br />
can expect an in-month performance in excess of 97%, performance for the quarter is<br />
likely to fall short of the 95% target. This will impact our Monitor governance risk<br />
rating detailed later in this report.<br />
3.2 We continue to report ambulance h<strong>and</strong>over delays of greater than 30 minutes.<br />
Despite this, performance in May did improve significantly with just 36 breaches<br />
reported compared to 64 in April, resulting in a May performance of 1.2%.<br />
Cancer (Section C3 of Performance Dashboard)<br />
3.3 All cancer targets have been met both in-month <strong>and</strong> year-to-date with the exception<br />
of the 62-day urgent referral st<strong>and</strong>ard which failed in April <strong>and</strong> May, <strong>and</strong> the 62-day<br />
screening target which is below target year-to-date after a particularly poor April<br />
performance. There was no common cause relating to the screening target failure<br />
although in 4 cases the patient chose to delay by a number of days whilst considering<br />
treatment options.<br />
5
Item 9<br />
Description<br />
31 days from 'decision to treat' (%)<br />
62 days from urgent GP referral (%)<br />
62 days from screening referral to treat (%)<br />
62 days from consultant upgrade to treat (%)<br />
31 days ‐ DTT to subsequent ‐ surgery (%)<br />
31 days ‐ DTT to subsequent ‐ drugs (%)<br />
31 days ‐ DTT to subsequent ‐ rad'th'py (%)<br />
2 weeks for breast symptom referral (%)<br />
2 weeks from urgent GP referral (%)<br />
Apr May YTD Target RAG<br />
O,A,Q,M 98.2% 99.2% 98.7% 96% Green<br />
O,A,Q,M 81.9% 84.4% 83.1% 85% Red<br />
O,A,Q,M 79.2% 92.7% 85.4% 90% Red<br />
O,Q 100.0% 92.6% 95.7% 85% Green<br />
O,A,Q,M 96.7% 94.4% 95.6% 94% Green<br />
O,A,Q,M 99.1% 99.3% 99.2% 98% Green<br />
O,A,Q,M 98.0% 97.5% 97.8% 94% Green<br />
O,A,Q,M 95.7% 96.1% 95.9% 93% Green<br />
O,A,Q,M 93.2% 95.1% 94.1% 93% Green<br />
The <strong>Trust</strong> reported 20.5 breaches of the 62-day urgent referral st<strong>and</strong>ard in May, of<br />
which 9 were outside of the <strong>Trust</strong>’s control (i.e. due to patient choice or for medical<br />
reasons associated with tertiary referral). Of the remaining 11.5, 9 were due to delays<br />
in diagnostic tests or treatment planning.<br />
Year-to-date performance for the 62-day screening target is still suffering from the 5<br />
breaches reported in April. The trust reported only 1.5 breaches in May.<br />
See Annex 2 for exception report.<br />
Due to recent internal process changes we have seen a significant improvement in<br />
the number of urgent 2 week wait referrals who have been seen within 10 days. The<br />
table below shows the detail of the improvement:<br />
Oct ‐ Dec 2012 Jan‐13 Feb‐13 Mar‐13<br />
Apr‐13<br />
May‐13 Jun‐13<br />
Cancer Site<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Num<br />
Seen<br />
% in 10<br />
days<br />
Gr<strong>and</strong> Total 4174 38.05% 1287 52.21% 1272 45.36% 1331 45.83% 1383 50.98% 1406 61.81% 509 57.96%<br />
Referral to treatment (Section C4 of Performance Dashboard)<br />
3.4 Admitted <strong>and</strong> incomplete pathways 18-week st<strong>and</strong>ards have failed for the second<br />
consecutive month due to a continued <strong>and</strong> planned clearance of the admitted backlog<br />
(backlog reduced by 211 patients to 1215 as at 17 th June).<br />
Detailed specialty level recovery plans have been developed that include recovery<br />
trajectories spanning 13/14. Due to the complex nature of the actions required <strong>and</strong><br />
the size of the backlog, these plans indicate that certain areas will be unable to<br />
recover to a sustainable position until January 2014. As reported at the last Board<br />
this target will be failed during quarter 2 due to the continued <strong>and</strong> planned clearance<br />
of the backlog.<br />
6
Item 9<br />
Diagnostics & surveillance (Section C6 of Performance Dashboard)<br />
3.5 Diagnostic wait performance has deteriorated in May with 2.8% of the total waiting list<br />
(173 patients) waiting longer than 6 weeks for a diagnostic test at the end of May.<br />
Of the 173 breach patients, the majority (79) were waiting for an Echocardiogram. A<br />
number of options are being considered to address the capacity issues identified by a<br />
review of this modality. These options include employing external cardiology<br />
technicians to carry out tests using our facilities although this additional support would<br />
not be available until August. In the meantime, the department are putting on<br />
additional lists to provide extra capacity.<br />
31 patients were waiting for an Endoscopy due to a complex mix of issues ranging<br />
from patient choice to staff availability for specialist paediatric <strong>and</strong> general<br />
anaesthetic cases.<br />
52 patients were waiting for Imaging - 12 MRI scans <strong>and</strong> 14 CT scans were delayed<br />
due to staff availability for specialist cases <strong>and</strong> breakdown of the Alliance scanner<br />
whilst 26 ultrasound delays were due to unusual levels of staff unavailability.<br />
A more detailed report on diagnostic delays is being developed with the service line<br />
<strong>and</strong> will be made available to the Board when complete.<br />
4 Finance & Efficiency –<br />
4.1 A separate report on the <strong>Trust</strong>’s financial position is being presented to the <strong>Trust</strong><br />
Board by the Director of Finance.<br />
4.2 This section of the report will provide the Board with an update on key contract issues<br />
including activity variances as well as full details on contract penalties <strong>and</strong> CQUIN<br />
achievement.<br />
4.3 Contract Position<br />
4.4 If the <strong>Trust</strong> was on a fully variable contract it would, at Month 2 owe commissioners<br />
£1.4m. Key issues to highlight from this high level analysis are the continuing<br />
significant underperformance on elective care, <strong>and</strong> the level of contractual penalties<br />
incurred.<br />
4.5 Elective activity is underperforming at Month 2 by 126 spells (1.2%) under plan <strong>and</strong><br />
£1m under on income. This income underperformance is significant being 8% below<br />
plan. Key specialties with underperformance are cardiac surgery (£189k) where they<br />
are still suffering cancellations. In April, 43 theatre slots were lost, <strong>and</strong> in May 25 slots<br />
were lost. ITU capacity was a key issue, but staffing levels have now been addressed<br />
so performance should improve back to contract level in future. However, if the lost<br />
capacity from the first few months is not recovered through future over-performance<br />
the <strong>Trust</strong> will continue to under-perform for the year. In Neurosurgery the activity is<br />
only slightly under plan but the income variance is £275k under plan due to case mix.<br />
Neurosurgery has capacity gaps that are being addressed through extended days<br />
<strong>and</strong> more formalised weekend working. Plastic Surgery is continuing to underperform<br />
(£221k) with reduced theatre capacity <strong>and</strong> under-utilisation of the plastics trauma<br />
theatre. Waiting lists are beginning to rise slightly. Further work is being done to<br />
underst<strong>and</strong> the picture more fully.<br />
7
Item 9<br />
4.6 Non Elective Activity is overall 455 spells under plan <strong>and</strong> £181k under the income<br />
plan. Within this, Obstetric activity is underperforming (120 spells under for birth<br />
HRGs year to date) as is Neonatology. This underperformance masks the fact that<br />
emergency activity is over performing by 228 (3%) spells <strong>and</strong> £641k income. This<br />
over-performance on emergency activity continues to impact on the <strong>Trust</strong>’s elective<br />
capacity. The <strong>Trust</strong> therefore needs to continue to work with commissioners on<br />
reducing emergency dem<strong>and</strong>, otherwise it will continue to impact upon elective work.<br />
4.7 A&E remains fairly close to plan, though there is a continuing shift towards a more<br />
complex case mix.<br />
4.8 Outpatients are over performing on first outpatients, but this is offset by an<br />
underperformance on outpatient procedures. Further effort is required to work down<br />
the follow up backlog. Wherever possible, this needs to be done by alternatives to<br />
face to face contacts, with minimal resource required. An active discussion with the<br />
CCG is on-going.<br />
4.9 There are further contractual financial penalties in 2013-14 compared with 2012/13.<br />
The <strong>Trust</strong> has incurred £427k of contractual penalties to Month 2. The key figures<br />
within this are for RTT £260k, Diagnostic Waits £47k <strong>and</strong> Cancelled Operations £52k.<br />
RTT is being intentionally breached over the first part of this year, to ensure backlogs<br />
are cleared <strong>and</strong> to put the <strong>Trust</strong> in a sustainable RTT position moving forward. Under<br />
the Managed PbR arrangements, penalties are returned to the <strong>Trust</strong> to invest in<br />
corrective action.<br />
4.10 As the Board will be aware the <strong>Trust</strong>’s contract will operate on a managed payment<br />
by results (PbR) basis. For month 2 this means that the variance to date of £1.4m is<br />
significantly mitigated as only the variable <strong>and</strong> semi variable elements of the contract<br />
have an impact on the <strong>Trust</strong>’s financial position in 2013-14. The variance after return<br />
of fines <strong>and</strong> the managed PbR adjustment is £0.136m with the significant adverse<br />
variance being cardiac surgery offset by stem cell transplant activity.<br />
4.11 Although the financial variance is significantly mitigated due to the contract agreed<br />
the early signs are of concern <strong>and</strong> the overall contract position to date will need<br />
further review <strong>and</strong> close monitoring to ensure that we have a full underst<strong>and</strong>ing of the<br />
issues as well as having mitigating actions in place.<br />
4.12 In respect of CQUIN (Quality payments) measures for the year these are at the final<br />
stages of agreement <strong>and</strong> we expect to be able to start reporting these at the end of<br />
quarter 1.<br />
5 Workforce<br />
Month 2 has seen a small increase in establishment with a similarly small rise in staff<br />
in post. There have also been sharp reductions in discretionary pay <strong>and</strong> sickness<br />
absence.<br />
Key variances are:<br />
Staff in post (Section E1 of Performance Dashboard)<br />
5.1 The budgeted establishment has increased in Month 2 by 7 WTE to 5,754, WTE <strong>and</strong><br />
staff in post has increased in Month 2 by 6 WTE to 5,398.<br />
8
Item 9<br />
Discretionary pay (Section E1 of Performance Dashboard)<br />
5.2 Discretionary pay has reduced by £373k in Month 2 to £1.38m. This is principally due<br />
to a large reduction in nursing bank <strong>and</strong> agency.<br />
Training <strong>and</strong> Appraisals (Section E2 of Performance Dashboard)<br />
5.3 The completion of m<strong>and</strong>atory essential skills training has remained static in Month 2<br />
at 95%. Child protection has also remained static at 97%. Manual h<strong>and</strong>ling <strong>and</strong> basic<br />
life support have both decreased slightly by 1% to 92% <strong>and</strong> 87% respectively.<br />
Appraisal completion rates (for non-medical staff) have remained static in Month 2 at<br />
82%.<br />
Sickness Absence (Section E3 of Performance Dashboard)<br />
5.4 Sickness absence has decreased in Month 2 from 4.34% to 3.63%, with the 12 month<br />
average sickness absence rate also continuing to decrease to 4.44%.<br />
In terms of sickness absence rates within staff groups, the staff groups with combined<br />
short <strong>and</strong> long term absence of more than 4% are Estates (5.42%) <strong>and</strong> Additional<br />
Clinical Services (6.13%).<br />
More robust management of poor attendance is being implemented alongside a<br />
range of prevention <strong>and</strong> wellbeing initiatives.<br />
A number of interventions have been put in place to support the health <strong>and</strong> wellbeing<br />
of staff <strong>and</strong> increase their resilience. The Occupational Health <strong>and</strong> Wellbeing<br />
Department’s Employee Assistance Service provide counselling, mediation, mental<br />
health advice <strong>and</strong> a range of education <strong>and</strong> training including:<br />
• Preventing Stress<br />
• Underst<strong>and</strong>ing Stress<br />
• Promoting Positive Manager Behaviour (which is run for managers)<br />
• Building Resilience (which is available for all staff, as well as a group intervention)<br />
• Self-Care course (to help staff focus on their own individual health <strong>and</strong> wellbeing).<br />
Alongside the implementation of a new Sickness Absence Policy, the contracts of<br />
employment of 17 individuals having been terminated in the past 6 months, following<br />
persistent absence associated with health issues.<br />
6 Compliance with Monitor’s Requirements<br />
Governance Risk Rating (Section F1 of Performance Dashboard)<br />
Continued failure of the A&E 4 hour target <strong>and</strong> 62 day cancer st<strong>and</strong>ards in addition to<br />
the failure of RTT admitted <strong>and</strong> incomplete pathways have resulted in a ‘Red’ rating<br />
for May. We anticipate a final Q1 position of 4.0 (Red), with the same four st<strong>and</strong>ards<br />
failing the quarter.<br />
9
Item 9<br />
Summary of performance exception reports Annex 1<br />
Performance Area Previous report Forecast <strong>and</strong> performance summary Further report?<br />
A&E 4 Hour St<strong>and</strong>ard June 2013 91.7% in April, improved to 94.8% in May. June performance currently above 97% but<br />
unlikely to save the st<strong>and</strong>ard for Q1.<br />
Referral to Treatment<br />
(Admitted patients)<br />
June 2013<br />
Target failed at 88.3% in April <strong>and</strong> May. This is a planned failure to allow clearance of a<br />
large backlog of patients. <strong>Trust</strong>-wide compliance with target expected during Q3 whilst<br />
recovery of certain service-lines will take until year-end.<br />
Cancelled operations June 2013 We previously reported actions being taken to achieve a 0.8% sustainable position.<br />
May performance at 1.27%, a significant improvement on April (2.65%). This is linked to<br />
the bed base proposals as reported to the June Board.<br />
Diagnostics February 2013 Performance has deteriorated in May to 2.8% from 1.6% in April.<br />
We forecast failure of this target in June due to capacity issues for Cardiac<br />
Echocardiogram. Additional capacity not available until July.<br />
Stroke February 2013 We previously said we would achieve the target of 80%.<br />
April <strong>and</strong> May have both failed at 59% <strong>and</strong> 67% respectively.<br />
Cancer<br />
(62 day st<strong>and</strong>ards)<br />
March 2013 We previously said this would be fully achieved by April 2013.<br />
62-day screening target has improved in May but is still failing year-to-date.<br />
62-day urgent referral has failed in April <strong>and</strong> May (81.9% <strong>and</strong> 84.4% respectively)<br />
The attached exception report details two key actions that will allow the <strong>Trust</strong> to achieve<br />
the target from September 2013.<br />
Annex 4<br />
A further detailed<br />
analysis of this area<br />
will be completed for<br />
the next Board<br />
Annex 2<br />
Annex 3<br />
Follow-up backlogs February 2013 Backlog continues to grow with an extra 767 added in May bring total to 24,305. A further detailed<br />
report agreed via<br />
IPAM will come to<br />
Board when complete<br />
10
Item 9<br />
9 Performance Exception Report Annex 2<br />
Stroke patients who spend at least 90% of their time in Hospital on a<br />
Stroke Unit based on Days<br />
Performance summary<br />
Performance from May was 66.7%, an improvement on the April position but still below the<br />
national st<strong>and</strong>ard of 80%.<br />
Update on previous actions<br />
Burrator has been ring-fenced throughout May to be used only for neurosciences. The<br />
intention is that this will lead to an increase in the bed availability for acute stroke patients to<br />
be admitted directly from the emergency department. The impact of this can be seen in the<br />
reduction in the number of patients who were identified as a stroke within the ED but were<br />
not directly admitted to the stroke unit due to bed availability from a volume of 10 patients in<br />
April breaching for this reason to 3 patients in May (2 patients in June so far)<br />
Further planned action<br />
Action Lead Deadline<br />
Continuous review patients who were not assessed in the<br />
emergency as query stroke but who subsequently were<br />
diagnosed with a stroke later in their journey<br />
Establishment of clear patient flows to ensure any<br />
patients admitted to Burrator who are not stroke patients<br />
can be moved in a timely manner.<br />
Review potential for establishment of a high care nursing<br />
area within Burrator to allow for escalated levels of care<br />
for patients who currently are admitted to ICU or MAU lvl<br />
1<br />
David Alao<br />
Davina Finch<br />
Davina Finch<br />
Monthly<br />
review<br />
End July<br />
End July<br />
11
Item 9<br />
Ensure that all patients admitted through ambulatory care<br />
are appropriately recorded as outpatients during their<br />
ambulatory care episode<br />
Review care pathways for patients coded as breaching<br />
due to a short length of stay to identify actions to address<br />
Identification of best performing <strong>Trust</strong>s to compare<br />
working practices <strong>and</strong> additional actions to deliver<br />
sustainable change.<br />
Forecast<br />
Donna Clewer<br />
Edna Piper<br />
Donna<br />
Clewer/Rachel<br />
Bottell<br />
Expected impact of improvements to be achieved by September 2013<br />
Mid July<br />
Mid July<br />
Mid July<br />
12
Item 9<br />
Performance Exception Report Annex 3<br />
62 Day "GP Urgent referral to Treatment"<br />
Performance summary<br />
May Performance was 84.4% <strong>and</strong> 83.1% year to date.<br />
Of the 20.5 breaches in May, 11 were deemed to be influenced by reasons under the control<br />
of the trust. 9 Diagnostic delay breaches, 1 Insufficient Outpatient Capacity <strong>and</strong> 1 Insufficient<br />
Inpatient Capacity.<br />
Update on previous actions<br />
The High level Cancer Action Plan contains 20 specific actions,<br />
9 are flagged as Green, 7 are flagged as Amber <strong>and</strong> 4 as Red.<br />
Red – Plans in place but concerns about delivery<br />
Amber – Plans in place <strong>and</strong> action progressing<br />
Green – Plans complete or in place<br />
Further planned action<br />
Action Lead Deadline<br />
Urology - Implement pre biopsy MRI for high risk patients<br />
Urology - Implement active surveillance for low risk<br />
patients<br />
Lung - One stop shop. Resolve consultant capacity<br />
Paul Hunter-<br />
Campbell/Jemma<br />
Edge<br />
Paul Hunter-<br />
Campbell/Jemma<br />
Edge<br />
Lee Johns/Tim<br />
Howells<br />
July 2013<br />
July 2013<br />
July 2013<br />
13
Item 9<br />
Forecast<br />
Significant progress has been made to implement a new pathway within lung <strong>and</strong> urology.<br />
However due to the patients currently in the system it is unlikely this will be realised until<br />
September. It is anticipated with all the changes small but steady sustainable progress will<br />
be made. However once changes have been embedded it is recognised that continued<br />
progress with all sites is required to ensure all patients where appropriate are treated within<br />
the 62 day st<strong>and</strong>ard.<br />
14
Item 9<br />
Performance Exception Report Annex 4<br />
Cancelled Operations<br />
Background<br />
Performance Summary<br />
During 2012/13 the trust struggled to achieve a low level of Cancelled operations. During<br />
the second half of the year this was principally due to excessive medical outliers occupying<br />
surgical beds. In cardiac high rates were seen <strong>and</strong> the key identified caused was ITU<br />
occupancy. The key performances are highlighted in tables 1-4 below.<br />
Table1. <strong>Trust</strong> cancelled ops<br />
Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13<br />
53 93 61 69 55 75 71 62 70 89 94 108<br />
1.2% 1.7% 1.3% 1.3% 1.1% 1.6% 1.4% 1.2% 1.6% 1.8% 2.0% 2.2%<br />
Table2. Medical outliers<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
33 17 18 10 14 10 22 46 54 64 60 60<br />
Table3. Cancelled elective cardiac cases<br />
Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13 TOTAL<br />
69 83 72 86 83 80 87 84 86 89 78 82 979<br />
5 7 2 7 8 7 9 10 8 11 17 12 103<br />
7.2% 8.4% 2.8% 8.1% 9.6% 8.8% 10.3% 11.9% 9.3% 12.4% 21.8% 14.6%<br />
* Note: Total cardiac activity was 1149 cases including ‘white board’ patients.<br />
10.5%<br />
It is clear that although a trust decision to exp<strong>and</strong> cardiac ICU beds was taken – the reality<br />
was that staff availability <strong>and</strong> agency availability did not meet expectation (increase of<br />
11WTE needed) to allow this.<br />
15
Item 9<br />
Update on previous actions<br />
Current Actions<br />
Key actions taken in April <strong>and</strong> May include:<br />
• ‘Winter ward’ Monkswell remains open – this has significantly improved the start of<br />
lists <strong>and</strong> cancellations in May <strong>and</strong> June.<br />
• Redefinition of list starts to enable theatres to start on time. This has greatly<br />
improved in May <strong>and</strong> June. Theatres now have a ‘green light’ to start first case as<br />
long as trust is not at ‘black’ status. (Subject to HDU <strong>and</strong> level1 patients detailed<br />
planning). This is actively addressing lost time <strong>and</strong> overruns.<br />
• Gradual increase in staff In CICU – although we predict this will take to October to be<br />
fully established.<br />
Table 4. <strong>Trust</strong> cancelled ops<br />
April May June (25 th )<br />
130 61 30<br />
2.6% 1.3% 0.6%<br />
•<br />
Further Planned Action<br />
Action Lead Deadline<br />
Re-Establishment of patient call 3-4 days before surgery<br />
( <strong>Trust</strong> target)<br />
Opening of additional short stay ward in Autumn –<br />
should have 20+ bed impact on reduction of medical<br />
outliers. ( <strong>Trust</strong> target)<br />
Relocation of SAU <strong>and</strong> ring fencing from medicine<br />
(reduce medical outliers)<br />
Re fresh of clinical ownership for list contents (increased<br />
commitment <strong>and</strong> confidence in list make up) <strong>Trust</strong> target.<br />
Increase of Main ITU bed compliment (probably not until<br />
Q3). Both targets.<br />
Modelling of detailed LOS splits in main <strong>and</strong> Cardiac<br />
ITU. (To underst<strong>and</strong> variability on LOS <strong>and</strong> whether<br />
predictable groupings). Both targets.<br />
Forecast<br />
It is expected that the <strong>Trust</strong> target will achieve the 0.8% target going forward. Clearly the<br />
whole occupancy model for both ITU’s into winter will affect the overall result <strong>and</strong> may need<br />
more modelling. It is expected that Cardiac cancellations will improve post October to be in<br />
line with other centres at 8%<br />
16
<strong>Trust</strong> Board Performance Report<br />
Report on performance to the end of May 2013
Contents<br />
EXECUTIVE SUMMARY D FINANCE & EFFICIENCY<br />
A1 Summary performance dashboard D1 Income & Expenditure<br />
D2 Cost Improvement Plan (CIP)<br />
B SAFETY & QUALITY D3 Capital expenditure<br />
B1 Safe care D4 Cash management<br />
B2 Effective care D5 CQUIN & Contract Penalties<br />
B3 Patient experience<br />
B4 Infection control E WORKFORCE<br />
B5 Other safety & quality metrics E1 Staffing numbers<br />
E2 Training & appraisals<br />
C ACCESS & ACTIVITY E3 Sickness absence<br />
C1 Accident & Emergency<br />
C2 Non-Elective Activity F EXTERNAL ASSESSMENTS<br />
C3 Cancer services F1 Monitor's Governance Risk Rating<br />
C4 Referral to treatment (RTT) F2 Monitor's Financial Risk Rating<br />
C5 Elective <strong>and</strong> Outpatient Activity<br />
C6 Other access & activity metrics<br />
Rationale for Inclusion<br />
The following key indicates the source of the metrics included on pages B1 - F2<br />
O - National Operating Framework, A - SHA Acute Performance Framework, CQ - National or locally agreed CQUIN target,<br />
M - Monitor Governance Framework, Q - <strong>NHS</strong> Contract Quality Requirement
OTHER<br />
ACCESS & ACTIVITY<br />
Acting Chief Operating Officer<br />
WORKFORCE<br />
Human Resources Director<br />
SAFETY & QUALITY<br />
Medical Director & Acting Chief Nurse<br />
FINANCE & EFFICIENCY<br />
Acting Director of Finance<br />
A1<br />
Summary performance dashboard - May 2013<br />
Status Ranking Page Metric Status Page<br />
Safe Care<br />
Income & Expenditure<br />
Hospital St<strong>and</strong>ardised Mortality Ratio (HSMR Relative Risk) 83.0 YTD 1/17 (SW YTD) £000s variance from plan (Month) (26)<br />
Summary Hospital-Level Mortality Indicator (SHMI ) 95.5 YTD 6/17 (SW YTD) £000s variance from plan (Year To Date) (54)<br />
D1<br />
% Surgical safety checklist completion 98.0% M2<br />
B1<br />
Cost Improvement Programme<br />
Incidents Reporting Rate (per 100 admissions) 9.70 M2 Full year forecast variance from target (£000s) 1,700<br />
% incidents leading to harm, loss or damage 32% M2 CIPs Delivered (£000s) 6,048<br />
Effective Care<br />
CIPs Forecast as Green Risk (£000s) 10,937 D2<br />
Readmissions (13 Month Avg Relative Risk) 97.0 YTD 12/17 (SW YTD) B2 CIPs Forecast as Amber Risk (£000s) 7,274<br />
Patient Experience<br />
CIPs Forecast as Red Risk (£000s) 1,441<br />
Friends <strong>and</strong> Family Test Response Rate (Inpatient) 13.7% M2<br />
Capital Expenditure<br />
Friends <strong>and</strong> Family Test Response Rate (ED) 8.4% M2 % of capital programme spent 12% D3<br />
Complaints closed within target (%) 85% M2<br />
B3<br />
Cash Management<br />
Non-clinically justified mixed sex breaches (No.) 0 M2 Revised Planned Closing Cash Balance (£'000s) 3,226<br />
Cancelled operations (% of elective FFCEs) 1.96% YTD Actual Closing Cash Balance (£'000s) 8,761<br />
Infection Control<br />
Cleared Balances (£'000s) 9,409<br />
MRSA cases (hospital apportioned) 0 YTD 8 / 17 (SW YTD) BPPC - <strong>NHS</strong> Volume (% within target) 97% D4<br />
B4<br />
C-Diff cases (hospital apportioned) 4 YTD 4 / 17 (SW YTD) BPPC - <strong>NHS</strong> Value (% within target) 98%<br />
Other key safety & quality metrics<br />
BPPC - Non-<strong>NHS</strong> Volume (% within target) 95%<br />
% stroke patients >90% of time on stroke unit 62.6% YTD BPPC - Non-<strong>NHS</strong> Value (% within target) 90%<br />
B5<br />
Follow-up backlog - actual (no.of patients) 24305 YTD<br />
Contract Penalties<br />
Accident & Emergency<br />
Contract Penalties - Year-to-Date (£000's) 427 D5<br />
% of A&E patients waiting 30 mins) 1.7% YTD C1<br />
Discretionary Spend (£000s) 1380<br />
Delayed transfers of care (delayed days as % of occupied days) 1.7% YTD Vacancy % - Nursing 5.52%<br />
Cancer Services<br />
Vacancy % - Medical 7.07% E1<br />
31 days from 'decision to treat' (%) 98.7% YTD 102/168 (Nat Q3) Vacancy % - Admin & Managers 6.60%<br />
62 days from urgent GP referral (%) 83.1% YTD 153/167 (Nat Q3) Vacancy % - Other Staff 6.47%<br />
62 days from screening referral to treat (%) 85.4% YTD 133/145 (Nat Q3)<br />
Training & Appraisals<br />
62 days from consultant upgrade to treat (%) 95.7% YTD 64/154 (Nat Q3) Basic Life Support (% completed) 87%<br />
31 days - DTT to subsequent - surgery (%) 95.6% YTD 140/162 (Nat Q3) C3<br />
Manual H<strong>and</strong>ling (% completed) 92%<br />
31 days - DTT to subsequent - drugs (%) 99.2% YTD 4/152 (Nat Q3) Essential Skills (% completed) 95% E2<br />
31 days - DTT to subsequent - rad'th'py (%) 97.8% YTD 69/78 (Nat Q3) Child Protection (% completed) 97%<br />
2 weeks for breast symptom referral (%) 95.9% YTD 43/143 (Nat Q3) Appraisals (% completed) 82%<br />
2 weeks from urgent GP referral (%) 94.1% YTD 150/170 (Nat Q3)<br />
Referral To Treatment (RTT)<br />
18 weeks - Admitted patients (%) 88.3% M2 160/174 (Nat M12)<br />
18 weeks - Non-admitted patients (%) 95.9% M2 195/207 (Nat M12)<br />
18 weeks - Audiology Direct Access (%) 97.3% M2<br />
C4<br />
% Incomplete pathways within 18 weeks 90.3% M2 187/206 (Nat M12)<br />
Other key access & activity metrics<br />
% patients waiting >6 weeks for diagnostic test 2.8% M2 C6<br />
Sickness Absence<br />
<strong>Trust</strong> Sickness Absence Rate (Average %) 3.63% E3<br />
External Assessments<br />
Monitor's Governance Risk Rating<br />
Monitor's Financial Risk Rating<br />
Red 0% (4.0)<br />
2<br />
F1<br />
F2<br />
3
B1<br />
Safe care<br />
Description<br />
Hospital St<strong>and</strong>ardised Mortality Ratio (HSMR Relative Risk)<br />
Summary Hospital-Level Mortality Indicator (SHMI Relative Risk)<br />
% Surgical safety checklist completion<br />
Incidents Reporting Rate (per 100 admissions)<br />
% incidents leading to harm, loss or damage<br />
Never Events<br />
Overdue safety alerts<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
85 83 83.0 100.0 Green R > 100 G < 100<br />
95 96 95.5 100.0 Green R > 100 G < 100<br />
96.8% 98.0% - 95% Green R < 92% G > 95%<br />
9.8 9.7 - 7.5 Green R < 6.00 G > 7.50<br />
33% 32% - 28% Red R > 28% G < 28%<br />
Q 0 0 0 0 Green R > 0 G < 1<br />
3 3 - 0 Red R > 0 G < 1<br />
120<br />
100<br />
80<br />
60<br />
Mortality (HSMR)<br />
(13 - Month Avg for Feb 12 - Feb 13)<br />
Actual<br />
Lower is better<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
National Average<br />
120<br />
100<br />
80<br />
60<br />
Summary Hospital Mortality Indicator (SHMI)<br />
(13 - Month Avg for Jan 12 - Jan 13)<br />
Lower is better<br />
COMMENTARY<br />
Mortality<br />
The <strong>Trust</strong> continues to perform well in respect of<br />
HSMR (17% better than expected) <strong>and</strong> the SHMI (4%<br />
better than expected). The mortality data presented<br />
is approx 4/5 months in arrears due to the lag time<br />
required for all UK <strong>Trust</strong>s to submit to the National<br />
database <strong>and</strong> results to be analysed. Individual<br />
diagnosis / procedure groups flagged as a concern<br />
are reviewed via the Clinical Effectiveness Group.<br />
40<br />
20<br />
-<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Surgical safety checklist completion<br />
100%<br />
Higher is better<br />
98%<br />
96%<br />
94%<br />
92%<br />
90%<br />
88%<br />
86%<br />
84%<br />
82%<br />
80%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
40<br />
20<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Incident Reporting Rate per 100 admissions<br />
12.0<br />
10.0<br />
Higher is better<br />
8.0<br />
6.0<br />
4.0<br />
2.0<br />
-<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Incident Reporting<br />
Our reporting rate sits firmly within the national<br />
upper quartile with a rate of 9.7 incidents per 100<br />
admissions reported in May 2013. This reporting rate<br />
is significantly above the national average of ~7.5<br />
<strong>and</strong> provides evidence that we have a good culture<br />
of openly reporting incidents.<br />
4
Readmissions Relative Risk<br />
B2<br />
Effective care<br />
Description<br />
Readmissions (13 Month Avg Relative Risk)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
96.4 97.0 97.0 100.0 Green R > 100 G < 100<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
COMMENTARY<br />
Hospital Readmissions (Source : HED)<br />
The readmission relative risk is a statistical<br />
calculation that measures the overall rate of<br />
readmissions within a hospital, compared with a<br />
national benchmark.<br />
The ‘all diagnoses’ readmission rate for <strong>Plymouth</strong><br />
<strong>Hospitals</strong> <strong>NHS</strong> <strong>Trust</strong> for the 13 month period to Jan<br />
2013 was 97.0, a readmission rate 3% better than<br />
expected.<br />
The <strong>Trust</strong>'s Clinical Effectiveness Group continues to<br />
monitor any diagnosis or procedure groups which<br />
flag as a readmission 'alert'.<br />
The latest SW SHA benchmarking position is provided<br />
in the bottom graph.<br />
5
Response Rate<br />
Recommender Score<br />
B3<br />
Patient experience<br />
Description<br />
Friends <strong>and</strong> Family Test Response Rate (ED)<br />
Friends <strong>and</strong> Family Test Response Rate (Inpatient)<br />
Friends <strong>and</strong> Family Test Result (ED)<br />
Friends <strong>and</strong> Family Test Result (Inpatient)<br />
Complaints closed within target (%)<br />
Complaints Backlog (i.e. past their 'reply by' date)<br />
Non-clinically justified mixed sex breaches (No.)<br />
Cancelled operations (% of elective FFCEs)<br />
28 day rebooking breaches (% of cancelled ops)<br />
Friends <strong>and</strong> Family Test<br />
20%<br />
18%<br />
16%<br />
14%<br />
12%<br />
10%<br />
8%<br />
6%<br />
4%<br />
2%<br />
0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Friends <strong>and</strong> Family Test Response Rate (ED)<br />
Friends <strong>and</strong> Family Test Response Rate (Inpatient)<br />
Friends <strong>and</strong> Family Test Result (ED)<br />
Friends <strong>and</strong> Family Test Result (Inpatient)<br />
Reasons for Cancellations<br />
Anaesthetist Sick/Unavailable<br />
Anaesthetist On Leave<br />
Surgeon Sick/Unavailable<br />
Surgeon On Leave<br />
No General Bed Available<br />
No Critical Care Bed Available Post Operatively<br />
Equipment Missing/Failure<br />
No Space On Theatre List/Emerg Took Priority<br />
Theatre List Overran<br />
Lack Of Theatre Staff<br />
Other<br />
Total<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
5.3% 8.4% 5% 15% Red R < 15% G > 15%<br />
11.5% 13.7% 12% 15% Red R < 15% G > 15%<br />
52.1 54.4<br />
66.2 63.1<br />
85% 85% - 80% Green R < 60% G > 80%<br />
11 12<br />
O,A,Q - - - - Green R > 10 G < 0<br />
Q 2.65% 1.27% 1.96% 0.8% Red R > 1.5% G < 0.8%<br />
Q 3.8% 9.8% 5.8% 5.0% Red R > 5% G < 5%<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
COMMENTARY<br />
Complaints closed within target (%)<br />
Friends <strong>and</strong> Family Test<br />
Complaints<br />
Complaints Backlog (i.e. past their 'reply by' date)<br />
From April 2013, all patients will be asked a simple<br />
70 100%<br />
100<br />
question to identify if they would recommend a<br />
60<br />
particular A&E department or ward to their friends<br />
95%<br />
80<br />
<strong>and</strong> family. <strong>Trust</strong>s are expected to reach a minimum<br />
50<br />
15% response rate to ensure an adequate sample<br />
90%<br />
60<br />
size. Recommender scores are also provided.<br />
40<br />
85%<br />
40<br />
30<br />
Complaints<br />
80%<br />
20 The <strong>Trust</strong> responded to 85% of complaints within<br />
20<br />
target during May. The complaints backlog is 12<br />
10<br />
75%<br />
0 overdue cases.<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Apr-13 May-13 Jun-13 Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14 YTD<br />
2<br />
77 27<br />
19 7<br />
2 4<br />
5 6<br />
19 14<br />
3<br />
3 3<br />
130 61<br />
0<br />
Cancelled Operations<br />
3.0%<br />
2.5%<br />
2.0%<br />
1.5%<br />
1.0%<br />
0.5%<br />
0.0%<br />
Lower is better<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD<br />
6<br />
Mixed Sex Accommodation<br />
There were no instances of non-clinically justified<br />
mixed sex accommodation in May.<br />
Cancelled Operations<br />
During May, 61 operations were cancelled on the day<br />
of admission or later due to non-clinical reasons - a<br />
breakdown of the cancellation reasons can be found<br />
in the table below. Of these, 6 were not rebooked<br />
within 28 days as per the national st<strong>and</strong>ard.
B4<br />
Infection Control<br />
Description<br />
MRSA cases (hospital apportioned)<br />
C-Diff cases (hospital apportioned)<br />
MSSA cases (hospital apportioned)<br />
MRSA Screening -Elective<br />
MRSA Screening -Non Elective<br />
Wards closed due to norovirus<br />
Number of days wards closed due to norovirus<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG<br />
O,A,Q 0 0 0 3 Green<br />
O,A,Q 2 2 4 25 Green<br />
2 5 7<br />
93% 91% 95%<br />
94% 95% 94%<br />
0 0<br />
0 0<br />
RAG Thresholds<br />
See graph below<br />
See graph below<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
MRSA Year To Date Target Upper Threshold<br />
Clostridium Difficile<br />
7<br />
6<br />
40<br />
35<br />
5<br />
30<br />
4<br />
25<br />
20<br />
3<br />
15<br />
2<br />
10<br />
1<br />
5<br />
- - - - - - - - - - -<br />
-<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
6<br />
5<br />
MSSA Cases<br />
Actual cases in month<br />
Ward Closures due to Norovirus<br />
30<br />
Wards closed due to norovirus<br />
25<br />
Number of days wards closed due to norovirus<br />
COMMENTARY<br />
MRSA<br />
The <strong>Trust</strong> reported no cases of hospital apportioned<br />
MRSA bacteraemia in May.<br />
Clostridium Difficile<br />
The <strong>Trust</strong> reported 2 cases of hospital apportioned<br />
Clostridium Difficile in May.<br />
The rate per 100,000 bed days <strong>and</strong> SW benchmark<br />
are currently unavailable whilst the SHA performance<br />
website is migrated to reflect the new CCG structure.<br />
Ward Closures<br />
No ward closures were reported during May due to<br />
Norovirus.<br />
4<br />
20<br />
3<br />
15<br />
2<br />
10<br />
1<br />
5<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
0<br />
0 0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
7
B5<br />
Other safety & quality metrics<br />
Description<br />
% of eligible patients VTE risk assessed<br />
% of hip fracture patients operated on within 36 hrs<br />
% stroke patients >90% of time on stroke unit<br />
Follow-up backlog - actual (no.of patients)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
O,A,CQ 95% 95% 95% 90% Green R < 95% G > 95%<br />
Q 81% 76% 78% 85% Amber R < 70% G > 85%<br />
Q 59% 67% 63% 80% Red R < 75% G > 80%<br />
23,538 24,305<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
VTE Risk Assessment Actual Target<br />
Hip Fractures<br />
120%<br />
90%<br />
COMMENTARY<br />
VTE Risk Assessment<br />
95% of patients admitted in May who required a VTE risk<br />
assessment recieved it on admission.<br />
100%<br />
80%<br />
80%<br />
70%<br />
60%<br />
Hip Fractures<br />
During May 76% of FNOF patients were operated on within<br />
36 hours of admission.<br />
60%<br />
40%<br />
50%<br />
40%<br />
30%<br />
Stroke<br />
During May 67% of stroke patients spent >90% of their stay<br />
on the stroke unit.<br />
20%<br />
0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
20%<br />
10%<br />
0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Follow-Up Backlog<br />
As at the end of May, the follow-up backlog had risen to<br />
24,305 patients.<br />
Stroke Patients<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
Follow-up Backlog<br />
30,000<br />
25,000<br />
20,000<br />
15,000<br />
10,000<br />
5,000<br />
0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
-<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
8
C1<br />
Accident & Emergency<br />
Description<br />
% of A&E patients waiting 30 mins)<br />
Delayed transfers of care (delayed days as % of occupied days)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
O,A,M,Q 91.7% 94.8% 93.3% 95.0% Red R < 95% G > 95%<br />
Q 61 66 64 60 Red R > 60 G < 60<br />
Q 2.2% 1.2% 1.7% 0.0% Red<br />
A,Q 3.0% 3.3% 1.7% 3.5% Green R > 5% G < 3.5%<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
A&E 4 Hour St<strong>and</strong>ard Actual Target<br />
100.0%<br />
98.0%<br />
96.0%<br />
94.0%<br />
92.0%<br />
90.0%<br />
COMMENTARY<br />
A&E Performance<br />
A&E 4 hour wait performance was below target (95%)<br />
at 94.8% in May.<br />
Arrival to Definitive Treatment Time<br />
Median duration was 66 mins for May.<br />
Ambulance H<strong>and</strong>over Times<br />
During May, 1.2% of patients experienced a h<strong>and</strong>over<br />
time of over 30 minutes. The <strong>Trust</strong> is working closely<br />
with SWAST on daily liaison.<br />
Delayed transfers of care<br />
3.3 % of the total occupied bed days in May were<br />
delayed days. Daily escalation <strong>and</strong> meetings with our<br />
wider partners in health <strong>and</strong> social care continue in<br />
order to minimise these delays. Discussing rehab<br />
capacity in <strong>Plymouth</strong> <strong>and</strong> Cornwall with<br />
commissioners.<br />
88.0%<br />
86.0%<br />
91.7%<br />
94.8%<br />
93.3%<br />
84.0%<br />
82.0%<br />
80.0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD<br />
9
C2<br />
Non-Elective Activity<br />
Description<br />
Inpatient activity vs plan (variance in spells)<br />
Inpatient activity vs 12/13 actual (variance in spells)<br />
Marginal Rate Emergency Threshold Adjustment vs plan (000's)<br />
All Admissions<br />
MAU Admissions<br />
From GP<br />
All Admissions<br />
SAU Admissions<br />
From GP<br />
All Admissions<br />
Ambulatory care Admissions<br />
From GP<br />
Surgical inpatient length of stay<br />
Medical inpatient length of stay<br />
Medical Outliers - Average Daily Occupancy Rate<br />
13/ 14 Non-elective Inpatient Activity vs Plan Actual Plan<br />
5,000<br />
4,500<br />
4,000<br />
3,500<br />
3,000<br />
2,500<br />
2,000<br />
1,500<br />
1,000<br />
500<br />
0<br />
3,000<br />
2,500<br />
2,000<br />
1,500<br />
1,000<br />
500<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
All Admissions to SAU, MAU <strong>and</strong> Ambulatory Care<br />
MAU (ALL) SAU (ALL) Ambulatory Care (ALL)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG<br />
-223 -232 -455 0<br />
-144 -320 -463 0<br />
Available from Mnth 4<br />
£0 0<br />
1,453 1,419 2,872<br />
376 384 760<br />
543 619 1,162<br />
298 342 640<br />
242 243 485<br />
193 182 375<br />
6.93 6.85<br />
9.36 9.35<br />
61 54 -<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
£1<br />
£1<br />
£1<br />
£1<br />
£0<br />
£0<br />
£0<br />
3,000<br />
2,500<br />
2,000<br />
1,500<br />
1,000<br />
500<br />
Marginal Rate Emergency Threshold Adjustment<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
GP Admissions to SAU, MAU <strong>and</strong> Ambulatory Care<br />
MAU (GP) SAU (GP) Ambulatory Care (GP)<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Medical Outliers - Average Daily Occupancy Rate<br />
RAG Thresholds<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
COMMENTARY<br />
13/14 Inpatient Activity vs Plan <strong>and</strong> vs 12/13<br />
As at the end of Month 2 we were 455 spells (non-elective inpatient stays) below plan for the year <strong>and</strong> have seen 463 fewer non-elective inpatients than the same period in 12/13. N.B Due to a change in recording practice, 2500 non-elective Obstetrics patients<br />
need to be removed from the 13/14 inpatient plan.<br />
Marginal Rate Emergency Threshold<br />
The National contract <strong>and</strong> PBR rules state that any non-elective inpatients treated above <strong>and</strong> beyond the levels of a nationally set baseline (the levels seen in 08/09) will only attract 30% of the tariff. The amount shown here represents the amount of income lost<br />
each month through non-elective inpatients volumes above <strong>and</strong> beyond the 08/09 levels. N.B Figures will be available from Month 4 onwards<br />
Medical Outliers<br />
These numbers represent the average daily volume of medical patients outlied on surgical wards.<br />
MAU, SAU <strong>and</strong> Ambulatory Care Admissions<br />
These graphs show the overall number of admissions to these three locations <strong>and</strong> the proportion of which are GP admits.<br />
10
C3<br />
Cancer services<br />
Description<br />
31 days from 'decision to treat' (%)<br />
62 days from urgent GP referral (%)<br />
62 days from screening referral to treat (%)<br />
62 days from consultant upgrade to treat (%)<br />
31 days - DTT to subsequent - surgery (%)<br />
31 days - DTT to subsequent - drugs (%)<br />
31 days - DTT to subsequent - rad'th'py (%)<br />
2 weeks for breast symptom referral (%)<br />
2 weeks from urgent GP referral (%)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
O,A,Q,M 98.2% 99.2% 98.7% 96% Green R < 96% G > 96%<br />
O,A,Q,M 81.9% 84.4% 83.1% 85% Red R < 85% G > 85%<br />
O,A,Q,M 79.2% 92.7% 85.4% 90% Red R < 90% G > 90%<br />
O,Q 100.0% 92.6% 95.7% 85% Green R < 85% G > 85%<br />
O,A,Q,M 96.7% 94.4% 95.6% 94% Green R < 94% G > 94%<br />
O,A,Q,M 99.1% 99.3% 99.2% 98% Green R < 98% G > 98%<br />
O,A,Q,M 98.0% 97.5% 97.8% 94% Green R < 94% G > 94%<br />
O,A,Q,M 95.7% 96.1% 95.9% 93% Green R < 93% G > 93%<br />
O,A,Q,M 93.2% 95.1% 94.1% 93% Green R < 93% G > 93%<br />
COMPARISONS WITH THE NATIONAL AVERAGE<br />
Performance Against 62 Day Target Compared with National Average - Analysis of Breaches<br />
Q1 2012/13<br />
Engl<strong>and</strong><br />
Q2 2012/13<br />
Engl<strong>and</strong><br />
Average Last Two<br />
Quarters<br />
Performance in<br />
Month<br />
Variance from<br />
Average<br />
Brain & CNS<br />
86.2%<br />
86.2% 86.2% 100.0%<br />
13.8%<br />
Breast<br />
98.0% 97.8% 97.9% 100.0% 2.1%<br />
Gynaecological 85.3%<br />
85.2% 85.3%<br />
100.0% 14.8%<br />
Haematological (excluding Acute Leukaemia) 83.3% 83.5% 83.4% 100.0% 16.6%<br />
Head & Neck<br />
76.4% 75.8% 76.1%<br />
58.8%<br />
-17.3%<br />
Lower Gastrointestinal 77.3% 79.0% 78.2%<br />
80.0% 1.9%<br />
Lung 83.0% 80.4% 81.7%<br />
66.7%<br />
-15.0%<br />
Other<br />
80.8% 81.3% 81.1% 100.0%<br />
19.0%<br />
Sarcoma<br />
78.3% 83.9%<br />
81.1% 100.0%<br />
18.9%<br />
Skin 97.8%<br />
97.9%<br />
97.9%<br />
97.5%<br />
-0.3%<br />
Upper Gastrointestinal 80.7%<br />
81.0%<br />
80.9%<br />
50.0%<br />
-30.9%<br />
Urological (excluding Testicular)<br />
84.4% 83.0% 83.7%<br />
81.5%<br />
-2.2%<br />
Rare Cancers (Testicular, ACL & Childrens)<br />
93.5%<br />
92.9%<br />
93.2%<br />
100.0%<br />
6.8%<br />
TOTAL 87.3% 87.2% 87.3%<br />
85.1%<br />
-2.2%<br />
BREACHES IN THE MONTH<br />
Total Number % of <strong>Trust</strong><br />
% of Total Total <strong>Trust</strong> % of <strong>Trust</strong><br />
Total Breaches<br />
Treated Treatments<br />
Breaches Breaches Breaches<br />
Brain & CNS<br />
0<br />
0.0%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
Breast<br />
13<br />
10.0%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
Gynaecological<br />
2<br />
1.5%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
Haemotological (excluding Acute Leukaemia)<br />
6<br />
4.6%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
Head & Neck<br />
8.5 (0.5)<br />
6.5%<br />
3.5 (0.5)<br />
17.9%<br />
1.0<br />
8.3%<br />
Lower Gastrointestinal<br />
10<br />
7.7%<br />
2<br />
10.3%<br />
2.0<br />
16.7%<br />
Lung<br />
15<br />
11.5%<br />
5<br />
25.6%<br />
5.0<br />
41.7%<br />
Other<br />
1<br />
0.8%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
Sarcoma<br />
1<br />
0.8%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
Skin<br />
40<br />
30.7%<br />
1<br />
5.1%<br />
0.0<br />
0.0%<br />
Upper Gastrointestinal<br />
6 (1)<br />
4.6%<br />
3<br />
15.4%<br />
1.0<br />
8.3%<br />
Urological (excluding Testicular)<br />
27<br />
20.7%<br />
5<br />
25.6%<br />
3.0<br />
25.0%<br />
Rare Cancers (Testicular, ACL & Childrens) 1<br />
0.8%<br />
0<br />
0.0%<br />
0.0<br />
0.0%<br />
TOTAL<br />
130.5 (1.5) 100.0%<br />
19.5 (0.5)<br />
100%<br />
12.0<br />
100%<br />
COMMENTARY<br />
Cancer St<strong>and</strong>ards<br />
Performance is above target for all cancer st<strong>and</strong>ards with<br />
the exception of:<br />
62 Day GP Urgent Referral (In-Month & Year-to-date)<br />
There were 20.5 breaches in May. 9 of these were outside<br />
of the <strong>Trust</strong>’s control - due to either patient choice or for<br />
medical reasons.<br />
62 days from screening referral to treat (%) (Year-to-date)<br />
This st<strong>and</strong>ard achieved in May but YTD performance is still<br />
below target due to April's poor performance ( 5 breaches<br />
with only 1 out of <strong>Trust</strong> control)<br />
Tertiary Breaches<br />
Pathway improvement being pursued with other acute<br />
trusts.<br />
Comments<br />
11
C4<br />
Referral To Treatment (RTT)<br />
Description<br />
18 weeks - Admitted patients (%)<br />
18 weeks - Non-admitted patients (%)<br />
18 weeks - Audiology Direct Access (%)<br />
% Incomplete pathways within 18 weeks<br />
Backlog - Admitted patients (No.)<br />
Backlog - Non-admitted patients (No.)<br />
Backlog - Decision to Treat (No.)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar - Target RAG RAG Thresholds<br />
O,A,Q,M 88.3% 88.3% 90% Red R < 90% G > 90%<br />
O,A,Q,M 95.6% 95.9% 95% Green R < 95% G > 95%<br />
Q 98.4% 97.3% 95% Green R < 95% G > 95%<br />
O,A,M 89.7% 90.3% 92% Red R < 92% G > 92%<br />
1,426 1,273 420 Green See Graph for Trajectory<br />
285 314 200 Red R > 300 G < 200<br />
576 562 400 Red R > 500 G < 400<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
Admitted Patients Actual Target<br />
Non-admitted Patients<br />
100%<br />
98%<br />
100%<br />
98%<br />
96%<br />
96%<br />
94%<br />
94%<br />
92%<br />
92%<br />
90%<br />
90%<br />
88%<br />
88%<br />
86%<br />
86%<br />
84%<br />
84%<br />
82%<br />
82%<br />
80%<br />
80%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
COMMENTARY<br />
RTT<br />
The <strong>Trust</strong> failed to meet the 18-weeks admitted <strong>and</strong><br />
incomplete pathway RTT st<strong>and</strong>ards in May due to the<br />
planned clearance of the admitted backlog.<br />
RTT Backlogs<br />
As at the end of May, the number of patients waiting<br />
more than 18 weeks for treatment in a non-admitted<br />
setting or awaiting a decision to treat was above<br />
trajectory whilst the admitted backlog was below<br />
planned levels for May.<br />
Audiology Direct Access<br />
100%<br />
98%<br />
96%<br />
94%<br />
92%<br />
90%<br />
88%<br />
86%<br />
84%<br />
82%<br />
80%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Decision to treat<br />
Non-admitted patients<br />
Backlog<br />
Admitted Patients<br />
Admitted Backlog Plan<br />
2500<br />
2000<br />
1500<br />
1000<br />
500<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
12
C5<br />
Elective & Outpatient Activity<br />
Description<br />
Referrals vs plan (variance in referrals ; GP <strong>and</strong> non-GP)<br />
Elective activity vs plan (variance in spells)<br />
Outpatient activity vs plan (variance in attendances)<br />
Length of stay vs 12/13 (variance in days)<br />
Day Case Rates<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD<br />
978 -1039 -61 0<br />
-18 -108 -126 0<br />
937 291 1228 0<br />
0.00 0.12 - 0<br />
78.0% 74.9% -<br />
14,000<br />
12,000<br />
10,000<br />
8,000<br />
6,000<br />
4,000<br />
2,000<br />
0<br />
Referrals vs Plan<br />
13/14 Actual Referrals<br />
13/14 Planned Referrals<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Referrals vs plan<br />
The <strong>Trust</strong> has received 61 fewer referrals than planned as at the end of Month 2.<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
13/14 Elective Actual<br />
Elective Activity vs Plan<br />
13/14 Elective Plan<br />
6,000<br />
5,000<br />
4,000<br />
3,000<br />
2,000<br />
1,000<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
COMMENTARY<br />
Outpatient Actual<br />
Outpatient Activity vs Plan<br />
Outpatient Plan<br />
50,000<br />
45,000<br />
40,000<br />
35,000<br />
30,000<br />
25,000<br />
20,000<br />
15,000<br />
10,000<br />
5,000<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Elective activity vs plan<br />
The <strong>Trust</strong> has admitted 126 fewer elective inpatients than planned as at the end of Month 2.<br />
Outpatient activity vs plan<br />
The <strong>Trust</strong> has seen 1228 more outpatients than planned as at the end of Month 2.<br />
13
C6<br />
Other access & activity metrics<br />
Description<br />
% patients waiting >6 weeks for diagnostic test<br />
% IP/DC planned patients waiting longer that 'treat by' date<br />
Suspended patients as % of total waiting list (%)<br />
Rapid Access Chest Pain - % patients seen within 2 weeks<br />
% pPCI - 150 min call to first balloon inflation<br />
% GUM patients offered to be seen within 48 hrs<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
O,A,Q 1.6% 2.8% - 1% Red R > 1% G < 1%<br />
6.5% 6.9% - 5% Amber R > 15% G < 5%<br />
4.7% 5.0% - 5% Green R > 10% G < 5%<br />
Q 100.0% 100.0% 100% 100% Green R < 98% G > 99%<br />
Q 50.0% 100.0% 81% 75% Green R < 75% G > 75%<br />
Q 100.0% 100.0% 100% 100% Green R < 98% G > 99%<br />
3.0%<br />
2.5%<br />
2.0%<br />
1.5%<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
Diagnostic Waits Actual Target<br />
COMMENTARY<br />
Diagnostic Waits<br />
As at 31st May 2013, 2.8% of patients (173 patients)<br />
on a diagnostic waiting list were waiting over 6 weeks<br />
for their test against a National Operating Framework<br />
target of 1%.<br />
Reperfusion Waiting Times<br />
In-month performance against the new pPCI st<strong>and</strong>ard<br />
in May was 100% (81% year-to-date) against an<br />
annual target of 75%.<br />
GUM Clinic<br />
In May, 100% of those patients attending the GUM<br />
clinic were offered an appointment within 48 hours.<br />
1.0%<br />
Lower is better<br />
0.5%<br />
0.0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
14
£m<br />
D1<br />
0.0<br />
(2,000.0)<br />
(4,000.0)<br />
(6,000.0)<br />
(8,000.0)<br />
Income & Expenditure<br />
OVERALL SUMMARY<br />
Apr-12 May-12 Jun-12 Jul-12 Aug-12 Sep-12 Oct-12 Nov-12 Dec-12 Jan-13 Feb-13 Mar-13<br />
COMMENTARY<br />
At the end of the second month of the new financial year, the <strong>Trust</strong>’s position is some £54k better<br />
than the £2.45 million planned deficit, at an actual position of £2.40 million deficit. Overall, this<br />
represents a £254k underspend against operational budgets <strong>and</strong> a £200k under-delivery of CIP<br />
targets.<br />
Income is £242k behind plan in Month 2 before CIPs as a result of under-performance against cardiac<br />
<strong>and</strong> non-contracted activity within the variable element of the contract <strong>and</strong> low levels of Private<br />
Patient, Education <strong>and</strong> Research income.<br />
Pay is underspent by £668k to Month 2 before CIPs with savings from vacancies exceeding<br />
discretionary pay costs in the majority of areas.<br />
(10,000.0)<br />
(12,000.0)<br />
(14,000.0)<br />
Actual<br />
Plan<br />
Non Pay expenditure is overspent by £154k before CIPs. Drug expenditure remains higher than plan,<br />
with 50% of the excluded drugs overspend being re-imbursed by Commissioners. Medical <strong>and</strong> Surgical<br />
Supplies expenditure is lower than plan reflecting lower than planned activity levels in some high cost<br />
areas.<br />
DETAILED ANALYSIS<br />
PLAN Plan Actual Variance MONTH PERFORMANCE Budget Actual Variance<br />
Variance Variance<br />
DIRECTORATE<br />
Apr-12 (941) (913) (28) Income (34,011) (33,210) 801<br />
in-month YTD<br />
May-12 (2,455) (2,401) (54) Pay expenditure 21,116 20,389 (727) Cardiothoracics 43 (97)<br />
Jun-12 (3,580) Non-pay expenditure 12,580 12,439 (141) Children & Young People's Health 23 52<br />
Jul-12 (4,683) Depreciation <strong>and</strong> interest 1,829 1,869 40 Emergency Services 26 39<br />
Aug-12 (5,869) NET DEFICIT/(SURPLUS) 1,514 1,488 (26) Gastro, Surgery <strong>and</strong> Renal Services 119 184<br />
Sep-12 (7,052) Head & Neck Surgery 60 81<br />
Oct-12 (8,132) YTD PERFORMANCE Budget Actual Variance Medical Specialties 153 222<br />
Nov-12 (9,040) Income (67,945) (66,906) 1,039 Neurosciences 12 30<br />
Dec-12 (9,923) Pay expenditure 41,978 40,859 (1,119) Ophthalmology 50 68<br />
Jan-13 (11,043) Non-pay expenditure 24,764 24,775 10 Oncology & Blood (51) 286<br />
Feb-13 (11,581) Depreciation <strong>and</strong> interest 3,658 3,674 16 Orthopaedics & Rheumatology (11) 126<br />
Mar-13 (13,000) NET DEFICIT/(SURPLUS) 2,455 2,401 (54) Reproductive Health <strong>and</strong> Womens Srvs 97 142<br />
Anaesthetics Pain <strong>and</strong> Critical Care (24) (62)<br />
Pharmacy (37) 9<br />
Health Science & Technology (42) (45)<br />
Clinical Support Services 95 94<br />
Chief Executive (2) 29<br />
Information <strong>and</strong> Planning (15) (54)<br />
Director of Finance (53) (72)<br />
Director of Human Resources (40) (88)<br />
Site Services 126 169<br />
Medical Director (36) (92)<br />
<strong>Trust</strong> Wide (490) (1,077)<br />
All figures are recorded in £000s Research <strong>and</strong> Development (30) 3<br />
TOTAL (26) (54)<br />
15
D2<br />
Cost improvement programme (CIP)<br />
3,500,000<br />
3,000,000<br />
2,500,000<br />
2,000,000<br />
Red<br />
Amber<br />
Green<br />
Delivered<br />
Plan<br />
OVERALL SUMMARY<br />
COMMENTARY<br />
Plans have been developed in order to deliver up to £25.7m of savings. Following the decision by the<br />
Board to allow non-recurring CIPs only in exceptional cases, £1.6 million of Non-Recurring Directorate CIPs<br />
have been removed from the position reported at Month 1. At present, £23.1m of the plans are for<br />
recurring schemes, with a full year effect of £26.8million. The risk assessed value of schemes is currently<br />
£19.7million <strong>and</strong> additional schemes will be required to ensure achievement of the target for the year.<br />
Further work is underway to assess progress with delivery of schemes <strong>and</strong> to review forecasts of delivery<br />
at a more detailed level.<br />
1,500,000<br />
1,000,000<br />
500,000<br />
0<br />
Apr-13 May-13 Jun-13 Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-14 Mar-14<br />
DETAILED ANALYSIS<br />
FORECAST<br />
Plan Delivered Green Amber Red PROGRAMME SUMMARY Target Forecast Variance<br />
Apr-13 1,154,016 1,212,409 Directorate Schemes - Clinical 11,731,000 5,421,149 (6,309,851)<br />
May-13 1,256,484 998,339 0 Directorate Schemes - Corporate 1,346,000 1,101,857 (244,143)<br />
Jun-13 1,228,018 432,257 872,317 291,983 117,933 Outpatient Efficiency 451,000 451,000 0<br />
Jul-13 1,722,667 370,503 866,056 315,529 122,759 Clinical Administration 1,294,000 1,201,860 (92,140)<br />
Aug-13 1,751,560 378,063 898,765 231,954 122,759 Medicines Management 1,300,000 1,299,999 (1)<br />
Sep-13 1,752,583 379,492 898,765 446,239 122,759 Theatre Efficiency 360,000 360,000 0<br />
Oct-13 2,502,879 379,492 1,390,264 984,521 159,093 Beds 0 0 0<br />
Nov-13 2,510,179 379,491 1,149,164 991,910 159,093 Workforce 4,340,000 3,680,498 (659,502)<br />
Dec-13 2,512,768 379,489 1,149,164 999,299 159,093 Medical Job Planning 500,000 500,000 0<br />
Jan-14 2,517,768 379,489 1,149,164 1,007,042 159,093 Non <strong>NHS</strong> Income 1,280,000 1,279,999 (1)<br />
Feb-14 2,567,890 379,489 1,154,289 1,002,042 159,093 Non Pay 2,000,000 2,000,000 0<br />
Mar-14 2,523,189 379,566 1,409,484 1,003,263 159,097 Finance Solutions 1,500,000 2,224,720 724,720<br />
TOTAL 24,000,000<br />
6,048,079 10,937,435 7,273,783 1,440,770 Reserve Slippage 7,000,000 6,178,985 (821,015)<br />
25,700,067<br />
Adjustment for stretch targets (9,102,000) 0 9,102,000<br />
TOTAL 24,000,000 25,700,067 1,700,067<br />
16
D3<br />
16,000<br />
14,000<br />
12,000<br />
10,000<br />
Capital expenditure<br />
OVERALL SUMMARY<br />
Actual<br />
Plan<br />
COMMENTARY<br />
The Capital plan of £15 million was approved at the June meeting of the Board.<br />
Expenditure to date totals £1.8 million, principally on the Stem Cell ward <strong>and</strong> other<br />
projects carried forward from the previous year. The remainder of schemes are<br />
underway or in planning in order to deliver the entirety of the programme by yearend.<br />
8,000<br />
6,000<br />
4,000<br />
2,000<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
DETAILED ANALYSIS<br />
MONTH Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar CAPITAL SCHEME Plan Actual %<br />
Plan 1,262 491 2,027 1,543 1,057 1,591 1,209 1,083 1,143 906 1,060 1,649 Stem Cell Ward upgrade 600 356 59%<br />
Actual 1,262 574 LINAC C replacement 450 18 4%<br />
VARIANCE 0 83 Radiopharmacy 1,000 34 3%<br />
% OF PLAN 100% 117% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 5th Endoscopy Room 40 14 35%<br />
Other Planning Schemes 1,706 70 4%<br />
CUMULATIVE Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Estates Backlog Maintenance 2,958 220 7%<br />
Plan 1,262 1,753 3,780 5,323 6,380 7,971 9,180 10,263 11,406 12,313 13,372 15,022 IM&T systems <strong>and</strong> infrastructure 2,980 698 23%<br />
Actual 1,262 1,836 Rolling Equipment Replacement programme 1,400 0 0%<br />
VARIANCE 0 83 Imaging Replacement Programme<br />
% OF PLAN 100% 105% Directorate equipment/minor works 2,826 403 14%<br />
Transformational Change enabling mesures 522 22 4%<br />
Contingency 540<br />
Donated assets<br />
Over commitment<br />
TOTAL 15,022 1,836 12%<br />
17
D4<br />
Cash Management<br />
Description<br />
Revised Planned Closing Cash Balance (£'000s)<br />
Actual Closing Cash Balance (£'000s)<br />
Cleared Balances (£'000s)<br />
BPPC - <strong>NHS</strong> Volume (% within target)<br />
BPPC - <strong>NHS</strong> Value (% within target)<br />
BPPC - Non-<strong>NHS</strong> Volume (% within target)<br />
BPPC - Non-<strong>NHS</strong> Value (% within target)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
5,362 3,226 3,226<br />
Not applicable<br />
5,846 8,761 8,761<br />
Not applicable<br />
8,416 9,409 9,409<br />
Not applicable<br />
96% 97% 97% 95% Green R < 80% G > 95%<br />
95% 98% 98% 95% Green R < 80% G > 95%<br />
94% 95% 95% 95% Green R < 80% G > 95%<br />
86% 90% 90% 95% Amber R < 80% G > 95%<br />
£000<br />
18,000<br />
16,000<br />
14,000<br />
12,000<br />
10,000<br />
8,000<br />
6,000<br />
4,000<br />
2,000<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
COMMENTARY<br />
The original cash plan anticipated receipt of cash<br />
support in June. The revised cashflow forecast<br />
reflects indications that the support will be provided<br />
in a number of smaller issues when necessary<br />
through the year to avoid cash deficits. The actual<br />
timings <strong>and</strong> values of these payments have yet to be<br />
confirmed.<br />
The cash balance is higher than plan at the end of<br />
May as a result of timing differences in the payment<br />
of Capital <strong>and</strong> Revenue creditors. The forecast<br />
balance at the end of June is close to the revised plan<br />
at £2.2m.<br />
The <strong>Trust</strong>’s Better Payments Practice Code (BPPC)<br />
performance improved against all measures in the<br />
month. Performance at Month 2 against all measures<br />
was at or above the 95% target, with the exception of<br />
Non-<strong>NHS</strong> invoices by value.<br />
0<br />
Mar-13 Apr-13 May-13 Jun-13 Jul-13 Aug-13 Sep-13 Oct-13 Nov-13 Dec-13 Jan-14 Feb-142007/08<br />
Mar-14<br />
Actual Plan Revised Cash Forecast<br />
18
£<br />
D5<br />
Contract Penalties & CQUIN<br />
Description<br />
Never Events<br />
Eliminating Mixed Sex Accommodation<br />
Cancer (62 days)<br />
Cancer (31 days)<br />
Cancer (2 Week Waits)<br />
RTT 18-week st<strong>and</strong>ards<br />
RTT 52-week waiters<br />
Diagnostic Waits<br />
A&E<br />
Ambulance H<strong>and</strong>overs<br />
Cancelled Ops 28-day breaches<br />
Cancelled Ops Multiple Breach Patients<br />
C-Diff<br />
250,000<br />
200,000<br />
150,000<br />
100,000<br />
50,000<br />
-<br />
TOTAL<br />
CONTRACT PENALTIES<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG<br />
- - -<br />
- - -<br />
5,852 4,993 10,845<br />
- - -<br />
- - -<br />
105,239 104,599 209,839<br />
25,000 25,000 50,000<br />
23,925 23,371 47,296<br />
15,401 16,450 31,850<br />
16,800 8,200 25,000<br />
768 25,584 26,351<br />
4,856 20,761 25,616<br />
-<br />
RAG Thresholds<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
Not applicable<br />
197,840 228,957 0 0 0 0 0 0 0 0 0 0 426,797<br />
COMMENTARY<br />
Contract Penalties<br />
As at the end of May, contract penalties have been applied in 9<br />
C-Diff<br />
out of the 13 areas totalling over £426k, over half of which has<br />
Cancelled Ops Multiple Breach Patients been related to RTT - failure against the National 18-week RTT<br />
Cancelled Ops 28-day breaches<br />
st<strong>and</strong>ards <strong>and</strong> reporting of 52+ week waiters.<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Ambulance H<strong>and</strong>overs<br />
A&E<br />
Diagnostic Waits<br />
RTT 52-week waiters<br />
RTT 18-week st<strong>and</strong>ards<br />
Cancer (2 Week Waits)<br />
Cancer (31 days)<br />
Cancer (62 days)<br />
Eliminating Mixed Sex Accommodation<br />
Never Events<br />
19
E1<br />
Staffing numbers<br />
Description<br />
Establishment (WTE)<br />
Contracted Staff in Post (WTE)<br />
Vacancies (WTE)<br />
Discretionary Spend (£000s)<br />
Vacancy % - Nursing<br />
Vacancy % - Medical<br />
Vacancy % - Admin & Managers<br />
Vacancy % - Other Staff<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Current Target RAG RAG Thresholds<br />
5,747 5,754<br />
Not applicable<br />
5,392 5,398<br />
Not applicable<br />
355 356<br />
1,753 1,380 - - Red R > 1300 G < 1000<br />
5.65% 5.52% 5.52% - Amber R > 10% G < 3%<br />
6.90% 7.07% 7.07% - Amber R > 10% G < 5%<br />
6.11% 6.60% 6.60% - Amber R > 10% G < 5%<br />
6.25% 6.47% 6.47% - Amber R > 10% G < 5%<br />
Establishment<br />
Vacancies (WTE) Contracted Staff in Post (WTE)<br />
7,000<br />
6,000<br />
5,000<br />
4,000<br />
3,000<br />
2,000<br />
1,000<br />
-<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
Discretionary Pay Spend<br />
Discretionary Spend (£000s)<br />
2,000<br />
1,800<br />
1,600<br />
1,400<br />
1,200<br />
1,000<br />
800<br />
600<br />
400<br />
200<br />
-<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Vacancy Rates Vacancy % - Nursing Vacancy % - Medical Vacancy % - Admin & Managers Vacancy % - Other Staff<br />
8%<br />
COMMENTARY<br />
Overall Establishment<br />
The budgeted establishment has increased in Month<br />
2 by 7 WTE to 5,754 WTE. Staff in post has increased<br />
in Month 2 by 6 WTE to 5,398.<br />
Discretionary Pay<br />
Discretionary pay has reduced by £373k in Month 2<br />
to £1.38m. This is principally due to a large<br />
reduction in nursing bank <strong>and</strong> agency.<br />
Turnover<br />
Annual turnover for Month 2 is 8.50% in comparison<br />
to 9.35% in the same period in the previous year.<br />
7%<br />
6%<br />
5%<br />
4%<br />
3%<br />
2%<br />
1%<br />
0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
20
E2<br />
Training & appraisals<br />
Description<br />
Basic Life Support (% completed)<br />
Manual H<strong>and</strong>ling (% completed)<br />
Essential Skills (% completed)<br />
Child Protection (% completed)<br />
Appraisals (% completed)<br />
PERFORMANCE INDICATORS<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG RAG Thresholds<br />
88% 87% 87% 95% Amber R < 85% G > 95%<br />
93% 92% 92% 95% Amber R < 85% G > 95%<br />
Q 95% 95% 95% 95% Green R < 85% G > 95%<br />
Q 97% 97% 97% 95% Green R < 85% G > 95%<br />
Q 82% 82% 82% 95% Red R < 85% G > 95%<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
Training Actual Gap from Target<br />
Child Protection Essential Skills Manual H<strong>and</strong>ling Basic Life Support<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
100%<br />
90%<br />
80%<br />
70%<br />
60%<br />
50%<br />
40%<br />
30%<br />
20%<br />
10%<br />
0%<br />
Appraisals<br />
Appraisals<br />
COMMENTARY<br />
M<strong>and</strong>atory Training<br />
The completion of m<strong>and</strong>atory essential skills training<br />
has remained static in Month 2 at 95%. Child<br />
protection has also remained static at 97%. Manual<br />
h<strong>and</strong>ling <strong>and</strong> basic life support have both decreased<br />
slightly by 1% to 92% <strong>and</strong> 87% respectively.<br />
Appraisal<br />
Appraisal completion rates (for non-medical staff)<br />
have remained static in Month 2 at 82%.<br />
21
E3<br />
Sickness absence<br />
PERFORMANCE INDICATORS<br />
Description<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar YTD Target RAG<br />
RAG Thresholds<br />
<strong>Trust</strong> Sickness Absence Rate (Average %)<br />
4.3% 3.6% - 3.5% Amber R > 4.2% G < 3.5%<br />
National Benchmark 18 / 41 32 / 41<br />
Comparator group is all large acute <strong>Trust</strong>s (41)<br />
Add Prof Scientific <strong>and</strong> Technical<br />
4.3% 3.9%<br />
Additional Clinical Services<br />
7.2% 6.1%<br />
Administrative <strong>and</strong> Clerical<br />
4.0% 3.3%<br />
Allied Health Professionals<br />
2.1% 2.8%<br />
Estates <strong>and</strong> Ancillary<br />
6.6% 5.4%<br />
Healthcare Scientists<br />
3.7% 2.5%<br />
Medical <strong>and</strong> Dental<br />
1.4% 1.1%<br />
Nursing <strong>and</strong> Midwifery Registered<br />
4.7% 3.7%<br />
ANALYSIS OF KEY PERFORMANCE INDICATORS<br />
Sickness Absence Rate<br />
Actual Target<br />
5.0%<br />
4.5%<br />
4.0%<br />
3.5%<br />
3.0%<br />
2.5%<br />
2.0%<br />
1.5%<br />
1.0%<br />
0.5%<br />
0.0%<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Sickness Absence<br />
COMMENTARY<br />
Sickness absence has decreased in Month 2 from<br />
4.34% to 3.63%, with the 12 month average sickness<br />
absence rate also continuing to decrease to 4.44%.<br />
In terms of sickness absence rates within staff groups,<br />
the staff groups with combined short <strong>and</strong> long term<br />
absence of more than 4% are Estates (5.42%) <strong>and</strong><br />
Additional Clinical Services (6.13%).<br />
Long <strong>and</strong> Short Term Sickness Absence Rates by Staff Group<br />
Nursing <strong>and</strong> Midwifery Registered<br />
1.82%<br />
1.92%<br />
Medical <strong>and</strong> Dental<br />
0.60%<br />
0.54%<br />
Healthcare Scientists (e.g. clinical scientists <strong>and</strong> biomedical scientists)<br />
1.57%<br />
0.94%<br />
Estates <strong>and</strong> Ancillary<br />
3.33%<br />
2.09%<br />
Allied Health Professionals (e.g. physios, OT, dieticians, radiographers)<br />
Administrative <strong>and</strong> Clerical<br />
1.98%<br />
2.05%<br />
0.85%<br />
1.20%<br />
Additional Clinical Services (e.g. HCAs <strong>and</strong> AHP helpers)<br />
2.85%<br />
3.28%<br />
Add Prof Scientific <strong>and</strong> Technical (e.g. pharmacists, ATOs, ODPs)<br />
1.48%<br />
2.38%<br />
0.00% 1.00% 2.00% 3.00% 4.00% 5.00% 6.00% 7.00%<br />
Sickness Rates - Long Term (28 Days Plus)<br />
Sickness Rates - Short Term (Under 28 Days)<br />
22
F1<br />
Monitor's Governance Risk Rating<br />
Description<br />
Target<br />
Weighting<br />
Quarter 1 Quarter 2<br />
Quarter 3 Quarter 4<br />
Apr May Jun Q1 Jul Aug Sep Q2 Oct Nov Dec Q3 Jan Feb Mar Q4<br />
Clostridium Difficile - Meeting the C Diff Objective<br />
Met 1.0 Met Met<br />
MRSA - Meeting the MRSA Objective<br />
Met 1.0 Met Met<br />
All cancers: 31 day wait<br />
for second or<br />
subsequent treatment<br />
comprising either:<br />
Surgery 94% 96.7% 94.4%<br />
Anti cancer drug treatments 98% 1.0 99.1% 99.3%<br />
Radiotherapy 94% 98.0% 97.5%<br />
All cancers: 62 day wait<br />
for first treatment<br />
comprising either:<br />
From urgent GP referral to<br />
treatment<br />
From <strong>NHS</strong> cancer screening<br />
service referral<br />
85% 81.9% 84.4%<br />
1.0<br />
90% 79.2% 92.7%<br />
All cancers: 31 day wait from diagnosis to first<br />
treatment<br />
96% 0.5 98.2% 99.2%<br />
Cancer: two week wait<br />
from referral to date<br />
first seen comprising<br />
either:<br />
All cancers 93% 93.2% 95.1%<br />
Symptomatic breast patients 93% 95.7% 96.1%<br />
0.5<br />
Total time in A&E (% within 4 hrs)<br />
95% 1.0 91.7% 94.8%<br />
Max 18 week referral to treatment - admitted<br />
90% 1.0 88.3% 88.3%<br />
Max 18 week referral to treatment - non admitted<br />
Max 18 week referral to treatment - incomplete<br />
pathways<br />
Does the <strong>Trust</strong> meet requirements relating to access<br />
to healthcare for people with learning disabilities?<br />
95% 1.0 95.6% 95.9%<br />
92% 1.0 89.7% 90.3%<br />
Met 0.5 - - - Met - - - Met - - - Met - - - Met<br />
Green=
Risk Rating<br />
F2<br />
Monitor's Financial Risk Rating<br />
OVERALL SUMMARY<br />
COMMENTARY<br />
The <strong>Trust</strong>’s Financial Risk Rating remains at 2, in accordance with the plan for the year.<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
OVERALL SCORE Plan Actual Forecast PERFORMANCE VALUES Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
Apr-13 2 2 EBITDA margin 2.6% 1.9%<br />
May-13 2 2 EBITDA % Achieved 100.4% 105.8%<br />
Jun-13 2 Return on assets employed -0.5% -1.2%<br />
Jul-13 2 I&E Surplus Margin -2.7% -3.6%<br />
Aug-13 2 Liquidity Ratio 22 22<br />
Sep-13 2<br />
Oct-13 2<br />
Nov-13 2 SCORING REGIME<br />
Dec-13 2 EBITDA margin<br />
Jan-14 2 EBITDA % Achieved<br />
Feb-14 2 Return on assets employed<br />
Mar-14 2 I&E Surplus Margin<br />
Liquidity Ratio<br />
DETAILED ANALYSIS<br />
Scoring<br />
11=5<br />
100=5<br />
3=5<br />
3=5<br />
60=5<br />
CURRENT SCORE<br />
2<br />
PERFORMANCE SCORES Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar<br />
EBITDA margin 2 2<br />
EBITDA % Achieved 5 5<br />
Return on assets employed 3 2<br />
I&E Surplus Margin 1 2<br />
Liquidity Ratio 4 3<br />
24
Item 10<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 th July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Month 2 Financial Results<br />
Director of Finance<br />
Director of Finance<br />
Director of Finance<br />
Purpose<br />
The purpose of this paper is to provide the Board with a summary of the <strong>Trust</strong>’s<br />
financial performance to the end of May 2013 (Month 2).<br />
This report accompanies the detailed performance dashboard for May 2013 with<br />
the finance section included at D1 to D5.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
At the end of the second month of the new financial year, the <strong>Trust</strong>’s position is some £54k better<br />
than the £2.45 million planned deficit, at an actual position of £2.40 million deficit.<br />
The annual cost improvement target is £24m. There are currently £25.7m of schemes identified.<br />
The risk assessed value of schemes is currently £19.7million which is £4.3million below the target.<br />
The Board will note from this that there remains significant risk in delivering a £24m savings<br />
programme <strong>and</strong> actions are on-going to address this.<br />
•<br />
•<br />
Quality Impact Assessment<br />
Each of the <strong>Trust</strong>’s proposed savings is subject to a formal Quality Impact Assessment, which is<br />
signed off by the Medical Director <strong>and</strong> Director of Nursing <strong>and</strong> monitored by the Programme<br />
Management Office <strong>and</strong> Executive Management Team.<br />
Financial Impact Assessment<br />
This paper updates the Board on the overall financial performance of the <strong>Trust</strong>.<br />
Regulatory Impact Assessment<br />
This paper addresses the performance of the <strong>Trust</strong> against its statutory financial duties <strong>and</strong> against<br />
<strong>Trust</strong> Development Authority <strong>and</strong> Monitor financial st<strong>and</strong>ards.<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Note the financial position of the <strong>Trust</strong> as at 31st May 2013.<br />
2. Endorse <strong>and</strong> discuss the actions set out at 5.3 of the report.<br />
Next Steps<br />
Carry out a review of progress <strong>and</strong> forecast delivery of cost improvement schemes. Implement<br />
improved financial controls. Develop a medium to long term financial recovery plan.
Item 10<br />
DETAILED REPORT<br />
<strong>Trust</strong> Board 5 th July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Month 2 Financial Results<br />
Director of Finance<br />
Director of Finance<br />
Director of Finance<br />
1. Purpose<br />
1.1 The purpose of this paper is to provide the Board with a summary of the <strong>Trust</strong>’s<br />
financial performance to the end of May 2013 (Month 2).<br />
1.2 This report accompanies the detailed performance dashboard for May 2013 with the<br />
finance section included at D1 to D5.<br />
2. Background<br />
2.1 For 2013-14 the <strong>Trust</strong> has a planned deficit of £13m after assuming savings of £24m.<br />
2.2 The month 2 detailed financial results have been subject to review at the Finance <strong>and</strong><br />
Investment Committee meeting of the 26 th June 2013. Any issues from the Finance<br />
Committee review will be reported to the Board.<br />
3. Overall Position Month 2<br />
3.1 At the end of the second month of the new financial year, the <strong>Trust</strong>’s position is some<br />
£54k better than the £2.45 million planned deficit, at an actual position of £2.40<br />
million deficit. Overall, this represents a £254k underspend against operational<br />
budgets <strong>and</strong> a £200k under-delivery of cost improvement programme (CIP) targets.<br />
3.2 The overall position to date is shown against plan below: -
Item 10<br />
3.3 The Income <strong>and</strong> Expenditure variances to the end of May are shown in Table 1:<br />
Table 1 – Operational Performance Month 2<br />
OPERATIONAL<br />
PERFORMANCE<br />
Budget<br />
M2<br />
Actual<br />
M2<br />
Variance<br />
M2<br />
Budget<br />
YTD<br />
Actual<br />
YTD<br />
Variance<br />
YTD<br />
INCOME<br />
£'000 £'000 £'000 £'000 £'000 £'000<br />
Provision of healthcare<br />
30,053 29,665 (388) 60,038 59,778 (260)<br />
Education, training <strong>and</strong> 2,007 1,950 (57) 4,013 3,910 (103)<br />
research<br />
Other Income 1,545 1,595 50 3,097 3,218 121<br />
Income CIPs 406 0 (406) 797 0 (797)<br />
TOTAL INCOME 30,053 29,665 (388) 67,945 66,906 (1,039)<br />
EXPENDITURE<br />
Pay (21,056) (20,389) 666 (41,526) (40,859) 667<br />
Pay CIP (61) 0 61 (452) 0 452<br />
Non-pay (12,490) (12,439) 51 (24,621) (24,775) (154)<br />
Non-pay CIP (90) 0 90 (144) 0 144<br />
TOTAL EXPENDITURE (33,696) (32,829) 868 (66,742) (65,634) 1,108<br />
NET<br />
315 381 66 1,203 1,273 70<br />
SURPLUS/(DEFICIT)<br />
(Before depreciation<br />
<strong>and</strong> interest)<br />
Depreciation <strong>and</strong> interest (1,829) (1,869) (40) (3,658) (3,674) (16)<br />
NET<br />
(DEFICIT)/SURPLUS<br />
(1,514) (1,488) 26 (2,455) (2,401) 54<br />
CIP MEMO 1,256 998 (258) 2,411 2,211 (200)<br />
3.4 Income is £242k behind plan in Month 2 before CIPs as a result of underperformance<br />
against cardiac <strong>and</strong> non-contracted activity within the variable element<br />
of the contract <strong>and</strong> lower than planned levels of private patient, education <strong>and</strong><br />
research income. In addition, income CIPs are £797k behind plan with the failure to<br />
deliver the planned additional cardiac surgery income <strong>and</strong> delays in receiving<br />
additional private patient income.<br />
3.5 Pay is underspent by £667k to month 2 before CIPs with savings from vacancies<br />
exceeding discretionary pay costs in the majority of areas. Pay CIPs are a further<br />
£452k over-achieved largely as a result of the recognition of pay CIPs from delays<br />
against cost pressures <strong>and</strong> investments held in reserves.<br />
3.6 Non Pay expenditure is overspent by £154k before CIPs with a contribution from nonpay<br />
CIPS <strong>and</strong> delays in spending reserves of £144k, reducing the overall variance to<br />
£10k.<br />
3.7 Overall CIP delivery has fallen behind plan in the month. As in Month 1, a significant<br />
element of CIP delivery reflects delayed commitment of reserves. Further focus on<br />
the implementation of planned schemes will be required to rectify this situation.<br />
Reserves are being tightly managed by the Director of Finance in order to offset<br />
delays in delivery of Cost Improvement Plans.
Item 10<br />
4. Key Issues for the Board<br />
4.1 If the <strong>Trust</strong> was on a fully variable contract it would, at Month 2 owe commissioners<br />
£1.4m due to significant income underperformance on elective care (126 cases but<br />
accounting for £1m), <strong>and</strong> the level of contractual penalties incurred (£0.4m). The key<br />
areas of elective under performance are neurosurgery, cardiac surgery <strong>and</strong> plastic<br />
surgery. A greater underst<strong>and</strong>ing of the elective under performance is required <strong>and</strong><br />
work is on-going to review this.<br />
4.2 Within this net financial under performance emergency activity is over performing by<br />
228 patient spells (3%). This over-performance on emergency activity continues to<br />
impact on the <strong>Trust</strong>’s elective capacity. The <strong>Trust</strong> therefore needs to continue to work<br />
with commissioners on reducing emergency dem<strong>and</strong>, otherwise it will continue to<br />
impact upon elective work.<br />
4.3 The <strong>Trust</strong> has incurred £427k of contractual penalties to Month 2. The key figures<br />
within this are for referral to treatment (RTT) £260k, diagnostic waits £47k <strong>and</strong><br />
cancelled operations £52k. RTT is being intentionally breached over the first part of<br />
this year, to ensure backlogs are cleared <strong>and</strong> to put the <strong>Trust</strong> in a sustainable RTT<br />
position moving forward. Under the Managed PbR arrangements, penalties are<br />
returned to the <strong>Trust</strong> to invest in corrective action.<br />
4.4 As the <strong>Trust</strong> is operating a managed PbR contract in 2013-14 (with only certain items<br />
variable) the variable contract included within the month 2 results (after return of<br />
penalties) is £0.136m under plan. The key area of concern in this month 2 variable<br />
position is the under-performance on cardiac surgery.<br />
4.5 All pay budgets at a summary level are under spent. Discretionary pay has reduced to<br />
£1.38m in the month although this includes the benefit of the reversed accrual from<br />
month 1 of £150,000. After allowing for this one off benefit this is still the lowest<br />
spending since October 2012 although too early to confirm that this improvement can<br />
be sustained.<br />
4.6 The cost improvement programme at month 2 has achieved £2.2m against a target of<br />
£2.4m. However, £1.5m of this sum has been achieved through delayed commitment<br />
of reserves <strong>and</strong> urgent work is on-going via <strong>Trust</strong> Wide programmes <strong>and</strong> Care<br />
Groups to ensure operational delivery. A more detailed CIP update is set out at<br />
section 5 below.<br />
4.7 The cash flow forecast for the year has been updated reflecting indications from the<br />
<strong>Trust</strong> Development Authority that the £13m requested cash support will be provided<br />
in a number of smaller issues when necessary through the year to avoid cash deficits.<br />
The actual timings <strong>and</strong> values of these payments have yet to be confirmed. Current<br />
cash levels remain acceptable without adverse impact on creditor payments.<br />
4.8 In respect of the capital programme there is a £15m plan presently approved. Of this,<br />
£13.7 million of schemes are in planning or underway. £1.3 million has been held<br />
back until later in the year in order to assist with cash issues <strong>and</strong>/or additional<br />
contingencies should they arise. At the present time, the capital programme remains<br />
flexible should the <strong>Trust</strong>’s cash position give cause for concern.<br />
5. Cost Improvement Programme (CIP)<br />
5.1 The agreed CIP target for the year is £24.0m. Against this, plans have been<br />
developed in order to deliver up to £25.7m of savings. Following the decision by the<br />
Board to allow non-recurring CIPs only in exceptional cases, £1.6 million of non-
Item 10<br />
recurring Directorate CIPs have been removed from the position reported at Month 1.<br />
At present, £23.1m of the plans are for recurring schemes, with a full year effect of<br />
£26.8million.<br />
5.2 The risk assessed value of schemes is currently £19.7million set out in the graph<br />
below. The risk assessed value is £4.3million below the target. Further work is<br />
underway with the Programme Management Office to assess progress with delivery<br />
of schemes <strong>and</strong> to review forecasts of delivery at a more detailed level <strong>and</strong> this work<br />
will be completed following the month 3 financial close.<br />
5.3 The Board will note from the above that there remains significant risk in delivering a<br />
£24m savings programme <strong>and</strong> actions on-going include: -<br />
5.3.1 Implementation of new financial controls guidance. A new ‘Financial Controls<br />
Guidance’ document has been issued to all budget holders, giving detailed practical<br />
guidance on the implementation of effective financial controls on recruitment,<br />
discretionary pay <strong>and</strong> non-pay expenditure across the organisation.<br />
5.3.2 Establishment of an Executive Review Panel which meets weekly to give approval to<br />
a number of high cost items including specific recruitment activity, outsourcing <strong>and</strong><br />
additional clinical capacity sessions.<br />
5.3.3 Establishment of Financial Performance Reviews in addition to the overall<br />
performance reviews. These will initially operate at a care group level but will move to<br />
a Service Line level in Month 3 once financial <strong>and</strong> operational data is available to<br />
match the newly established service lines.<br />
5.3.4 Development of a financial recovery plan with the aim of both securing delivery in<br />
2013-14 as well as developing robust plans for 2014-15 <strong>and</strong> 2015-16. At the time of<br />
writing we are in the process of recruiting an external partner to support us with<br />
additional capacity to develop a detailed financial recovery plan. A further update will<br />
be provided to the Board.<br />
6. Conclusion <strong>and</strong> recommendations<br />
6.1 The Board is asked to note the financial position of the <strong>Trust</strong> as at 31 st May 2013.<br />
6.2 The Board is asked to endorse <strong>and</strong> discuss the actions at 5.3
Item 11<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Quarterly update on acute hospital st<strong>and</strong>ards for people with Learning<br />
Disabilities<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Purpose<br />
Associate Director of Nursing/Nurse Consultant Older People<br />
Director of Nursing & Midwifery<br />
Associate Director of Nursing/Nurse Consultant Older People<br />
To report to the Board the outcomes of a recent review Learning Disabilities<br />
Liaison service, including outcomes of recent complaints.<br />
To provide an update on compliance with national st<strong>and</strong>ards.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
People with Learning Disabilities have an equal right to healthcare. It is important, therefore,<br />
that the <strong>Trust</strong> has services, staff <strong>and</strong> support which enable people with Learning Disabilities to<br />
use our services. The <strong>Trust</strong> needs to ensure that our healthcare services provide a high<br />
st<strong>and</strong>ard of care <strong>and</strong> treatment to people with Learning Disabilities – which meet national<br />
requirements <strong>and</strong> st<strong>and</strong>ards. Care <strong>and</strong> treatment of individuals must take into consideration<br />
<strong>and</strong> make reasonable adjustments where necessary, for their complex needs <strong>and</strong> disabilities.<br />
The Learning Disabilities (LD) Liaison service was established three years ago, to provide<br />
support to clinical teams across the <strong>Trust</strong> in the care <strong>and</strong> treatment of people with LD. The<br />
team, its scope of practice <strong>and</strong> ways of working have recently been reviewed. This has<br />
involved external stakeholders <strong>and</strong> has led to the review of the operational protocol <strong>and</strong><br />
development of St<strong>and</strong>ard Operating Procedure for the team. The outcomes of recent<br />
complaints regarding the care of people with Learning Disabilities have also informed the new<br />
SOP. The focus of the Learning Disabilities Liaison team is to work with clinical teams across<br />
the hospital, community settings <strong>and</strong> primary care to facilitate <strong>and</strong> promote high quality of care<br />
to people with Learning Disabilities, as they access <strong>Trust</strong> services.<br />
Progress continues to be made towards the national st<strong>and</strong>ards, as laid out in the Monitor<br />
framework <strong>and</strong> Care Quality Commission; the <strong>Trust</strong> continues to provide high quality care to<br />
people with Learning Disabilities, which is compliant with national st<strong>and</strong>ards.<br />
Quality Impact Assessment<br />
This report provides assurance of compliance with CQC st<strong>and</strong>ards - Outcomes 1, 4, <strong>and</strong> 7.<br />
The <strong>Trust</strong> has a legal duty to ensure equality of service provision <strong>and</strong> to meet requirements from the<br />
Equality Act (2010).<br />
Financial Impact Assessment<br />
No direct impact<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Confirm commitment to the Getting It Right Charter (Annex 1).<br />
2. Note the outcomes of the review of Learning Disabilities Liaison team (Annex 2 & 3).<br />
•
Item 11<br />
3. Review the <strong>Trust</strong>’s continued position <strong>and</strong> satisfy itself that the <strong>Trust</strong> is able to declare<br />
continuing compliance towards the Monitor Compliance framework (Annex 4).<br />
Next Steps<br />
The St<strong>and</strong>ards Operating Procedure will be presented to Personal Care Group for approval; it will<br />
then be published for use across the <strong>Trust</strong> <strong>and</strong> to replace the Joint Working Protocol (current<br />
operational procedure)<br />
The <strong>Trust</strong> Board will continue to receive reports on progress towards the national st<strong>and</strong>ards for<br />
people with Learning Disabilities (quarterly).
Item 11<br />
DETAILED REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Quarterly update on acute hospital st<strong>and</strong>ards for people with Learning<br />
Disabilities<br />
Associate Director of Nursing/Nurse Consultant Older People<br />
Director of Nursing & Midwifery<br />
Associate Director of Nursing<br />
Purpose<br />
People with Learning Disabilities have an equal right to healthcare. It is important, therefore,<br />
that the <strong>Trust</strong> has services, staff <strong>and</strong> support which enable people with Learning Disabilities<br />
to use our services. This report details the work undertaken to review the working of the<br />
Learning Disabilities Liaison team, the scope of practice for this team <strong>and</strong> to improve how<br />
people with Learning Disabilities are supported as they use <strong>Trust</strong> services.<br />
The <strong>Trust</strong> needs to ensure that our healthcare services provide a high st<strong>and</strong>ard of care <strong>and</strong><br />
treatment to people with Learning Disabilities, which takes into consideration <strong>and</strong> makes<br />
reasonable adjustments for their complex needs <strong>and</strong> disabilities. The <strong>Trust</strong> is committed to<br />
<strong>supporting</strong> the Getting It Right Charter - ensuring that we focus on the needs of individuals;<br />
to see the person not the disability (Annex 1).<br />
The <strong>Trust</strong> Board is required to review compliance with the national Monitor framework for<br />
st<strong>and</strong>ards of care for people with Learning Disabilities - this report provides detail of the work<br />
towards compliance (Annex 4)<br />
Background<br />
People with learning disabilities often have specific health needs, in addition to the general<br />
health needs which the rest of the population face throughout life. However, for various<br />
reasons, they often struggle to access the same level of healthcare services – both in terms<br />
of primary <strong>and</strong> secondary care. The range of specific needs people with Learning<br />
Disabilities have included:<br />
• Communication – abilities to read <strong>and</strong> write, verbal communication, sensory needs.<br />
• Memory – ability to tell the time, remember everyday facts, medication compliance.<br />
• Social – ability to forge relationships, deal with people, organise themselves, manage<br />
financial <strong>and</strong> domestic affairs, risk awareness, unemployment.<br />
• Physical needs may be linked to their learning disabilities e.g. immobility, obesity,<br />
swallowing difficulties, incontinence.<br />
• Challenging behaviours in a small number of cases.<br />
• Medical/health conditions often related to learning disabilities e.g. dental care,<br />
diabetes, epilepsy, coronary heart disease, respiratory disease, hypothyroidism,<br />
Gastro-Intestinal conditions <strong>and</strong> cancers, mental health issues.<br />
(Royal College of Nursing 2006 – Meeting the health needs of people with learning disabilities)<br />
The Death by Indifference report by Mencap (2007) highlighted the fact that people with<br />
learning disabilities receive poor care <strong>and</strong> treatment from healthcare services. The report<br />
concluded that:
Item 11<br />
• People with learning disabilities are seen to be a low priority.<br />
• Many healthcare professionals underst<strong>and</strong> little about learning disabilities.<br />
• Many healthcare professionals do not properly consult <strong>and</strong> involve the families <strong>and</strong><br />
carers of people with learning disabilities.<br />
• Many healthcare professionals do not underst<strong>and</strong> the law around capacity <strong>and</strong><br />
consent to treatment.<br />
• Health professionals rely inappropriately on their own estimates of a person’s quality<br />
of life.<br />
• The complaints system within <strong>NHS</strong> services is often ineffectual, time-consuming <strong>and</strong><br />
inaccessible for people with learning disabilities.<br />
(Death by Indifference, Mencap March 2007)<br />
The report claimed that many people with learning disabilities die in hospital due to the<br />
widespread ignorance <strong>and</strong> indifference throughout healthcare services, towards their needs<br />
<strong>and</strong> those of their families <strong>and</strong> carers. Mencap claim that the inequitable service afforded to<br />
those with learning disabilities by hospitals <strong>and</strong> other healthcare services amounts to<br />
institutional discrimination.<br />
Earlier this year, a Confidential Inquiry which reviewed the 247 deaths of people with<br />
Learning Disabilities over a two year period concluded that 42% deaths reviewed were<br />
premature; the reasons for premature deaths being delayed investigations or treatment,<br />
inadequate response to changing needs of individuals <strong>and</strong> inappropriate care for complex<br />
<strong>and</strong> ongoing health needs.<br />
(Confidential Inquiry into the premature deaths of people with Learning Disabilities 2013)<br />
In January 2013, concerns raised through a Coroner’s inquest (heard December 2012; case<br />
two years old), via a Rule 43 letter, were reported to the <strong>Trust</strong> Board. The concerns raised<br />
were in respect of adherence to our own operational policy for managing patients with<br />
Learning Disabilities in hospital; in particular around the support of individuals with consent to<br />
treatments <strong>and</strong> care.<br />
Since then, there have been concerns raised by families of two people with Learning<br />
Disabilities, regarding the lack of consideration of individuals’ complex needs with clinical<br />
decision-making; concerns were raised that staff were not focusing on the needs of<br />
individuals, rather were distracted by their profound disabilities.<br />
As a result of this, a review of the Learning Disabilities Liaison service <strong>and</strong> the <strong>Trust</strong>’s Joint<br />
working protocol (2009) was commenced, at that time by the Acting Director of Nursing.<br />
Following an internal review, a preliminary report was reported to the <strong>Trust</strong> Board in April<br />
(Annex 2).<br />
A Review of the Learning Disabilities Liaison Team with external stakeholders<br />
In order to continue with the good multi-agency working established by the LD Liaison team<br />
<strong>and</strong> to involve (new) local commissioners in the development of the LD Liaison service, a<br />
review involving a range of external stakeholders has been completed. This included:<br />
• Consideration of the outcomes/findings of the internal review of the LD liaison team<br />
structure, working practices/relationships <strong>and</strong> implementation of the Joint operational<br />
protocol.<br />
• Feedback from commissioners, community providers <strong>and</strong> other partners, with respect<br />
to the relationships with the LD liaison team, impact to patients, families <strong>and</strong> other<br />
service providers.
Item 11<br />
• Challenge in respect of the ‘Getting it Right’ Charter.<br />
• Review of numbers of people with Learning Disabilities supported in hospital over the<br />
past three years.<br />
• Joint agreement on the areas of the operational protocol which needed revising.<br />
• Evaluation of the LD Liaison team structure, with discussions regarding further<br />
support/resources needed to extend the service <strong>and</strong> establish seven-day working<br />
• Agreement on further review/feedback processes.<br />
A summary of the feedback <strong>and</strong> agreed actions from this review is presented in Annex 3.<br />
The partnership working, commitment to continuous improvement <strong>and</strong> desire to develop<br />
further the LD liaison team were commended by the commissioners. Working with<br />
community LD services across <strong>Plymouth</strong>, Devon <strong>and</strong> Cornwall services is a challenge - but<br />
there was commitment from both NEW Devon <strong>and</strong> Kernow CCG LD commissioning<br />
managers to facilitate better involvement, breaking down of barriers <strong>and</strong> improvement in<br />
working relationships between primary care, community services <strong>and</strong> secondary care.<br />
Scope of practice of the Learning Disabilities Liaison team<br />
The Learning Disabilities Liaison Service was established in November 2009 to provide<br />
support to clinical teams across the <strong>Trust</strong> in the care <strong>and</strong> treatment of people with LD. The<br />
LD liaison team forms part of the wider Derriford liaison team, <strong>supporting</strong> clinical teams<br />
across the <strong>Trust</strong> in the management of patients with complex needs. Derriford liaison team<br />
includes specialist liaison nurses for mental health, learning disabilities, alcohol <strong>and</strong><br />
vulnerable adult services. The LD liaison team has recently undergone organisational<br />
change: a team leader has been appointed with two other Clinical Nurse Specialists; the<br />
Clinical Nurse Specialist for vulnerable adults in the Emergency Directorate also forms part<br />
of the team <strong>and</strong> supports patients through the urgent care pathway. This newly configured<br />
team has now established an extension to the working hours/days to provide an evening <strong>and</strong><br />
weekend service.<br />
Following the review of service <strong>and</strong> the operational protocol, a St<strong>and</strong>ard Operating<br />
Procedure for the working of the LD liaison team has been developed. The roles of the<br />
Learning Disabilities liaison team are to facilitate the meeting of individual healthcare needs<br />
for people with Learning Disabilities with complex needs <strong>and</strong> support clinical teams to best<br />
meet the needs of individuals. This involves liaising with the community learning disability<br />
teams, community providers, families <strong>and</strong> acute hospital clinical services <strong>and</strong> co-ordinating<br />
support, planning <strong>and</strong> treatment delivery for referrals of people with Learning Disabilities,<br />
who may require help to access acute services. The LD Liaison team will:<br />
• Facilitate <strong>and</strong> co-ordinate of patient care – focusing on needs of the individuals <strong>and</strong><br />
incorporating Hospital Passport information <strong>and</strong> ensuring that reasonable<br />
adjustments are made to take into consideration the individual’s complex needs.<br />
• Ensure appropriate assessments <strong>and</strong> information are made available to inform the<br />
patient care plan.<br />
• Provide assurance that legal requirements are met re clinical decision making, under<br />
Mental Capacity Act.<br />
• Develop effective working relationships – between clinical teams, relatives,<br />
providers/carers involved with the individual, community services.<br />
• Ensure good governance is maintained <strong>and</strong> national st<strong>and</strong>ards are met - with respect<br />
of care planned <strong>and</strong> delivered, communications, patient information <strong>and</strong> involvement.<br />
• Promote staff awareness, education <strong>and</strong> training re need of people with Learning<br />
Disabilities.<br />
• Provide leadership in the developments <strong>and</strong> approach to care for people with LD.
Item 11<br />
The review of the Learning Disabilities liaison team has been very encouraging in terms of<br />
the positive feedback from users, community providers <strong>and</strong> local commissioners. The<br />
structure of the team <strong>and</strong> its scope of practice will be enhanced, once commissioners have<br />
agreed increased resources, to manage the increase in numbers of patients being supported<br />
<strong>and</strong> to accommodate weekend working.<br />
Lessons from recent experiences of people with Learning Disabilities<br />
An internal review has been undertaken of a longst<strong>and</strong>ing complaint made last year. The<br />
parents of the individual felt that they had not been fully involved in the clinical decisionmaking<br />
over a period of some months; they were also concerned that clinicians had focused<br />
on their son’s disabilities rather than his clinical needs.<br />
In an informal complaint, made when the CQC undertook its regular unannounced<br />
inspection, concerns were raised by parents of a lady with Learning Disabilities with regards<br />
to the utilisation of the Liverpool Care Pathway for the Dying. The decision-making <strong>and</strong><br />
involvement of the family were reviewed as part of the investigation into the concerns raised.<br />
Both of these incidents had similarities with the findings of Mencap (2007 <strong>and</strong> 2009) <strong>and</strong> the<br />
CIPOLD (2013) – that people with Learning Disabilities can be disadvantaged in the<br />
processes of clinical decision-making; that clinicians can focus on the person’s disabilities<br />
rather than their clinical needs.<br />
The investigations for both of these incidents identified:<br />
• Good family involvement in all clinical decisions – with regular discussions with<br />
family recorded.<br />
• Compliance with the Mental Capacity Act, with appropriate Best Interest decisions<br />
made regarding plans for treatment.<br />
• No evidence that clinicians focused solely on the person’s disabilities - rather<br />
considered the impact of their long-term condition on any current treatment plans,<br />
clinical interventions <strong>and</strong> prognosis.<br />
• Good teamwork between clinical teams – this allowed regular review of decisions<br />
<strong>and</strong> discussions; so that clinical decisions could be changed according to patient<br />
recovery <strong>and</strong> parent involvement.<br />
However, as with any investigations, there were lessons learned from both incidents. Mostly<br />
for the form of communication clinical teams have with families, terminology used <strong>and</strong> the coordination<br />
of discussions. It was clear in both cases that the Learning Disabilities liaison team<br />
needed to be more active, get involved earlier <strong>and</strong> be more proactive in their support for<br />
individuals <strong>and</strong> their families.<br />
The lessons learned have been incorporated into the revised SOP for the Learning<br />
Disabilities Liaison team<br />
Derriford User Group (DUG)<br />
This is a user/patient group, established in 2011, of people with Learning Disabilities. DUG<br />
is a sub-group of the Health Sub-Group of the Learning Disabilities Board (<strong>Plymouth</strong> City<br />
Council). Members of the group are supported by <strong>Trust</strong> staff <strong>and</strong> with advocacy from People<br />
First from the Highbury <strong>Trust</strong>, to provide feedback on patient experiences, a perspective on<br />
various <strong>Trust</strong> services from people with Learning Disabilities <strong>and</strong> a partnership working for<br />
the LD Liaison team.
Item 11<br />
Over the past two years, members of DUG have been supported to promote initiatives such<br />
as Annual Health Assessments (primary care), development of their own Hospital Passports,<br />
consideration of Organ Donation <strong>and</strong> Staying Healthy campaign. They have also worked<br />
closely with <strong>Trust</strong> staff to contribute to the following:<br />
• Recruitment of staff to the LD Liaison team.<br />
• Signage across the hospital.<br />
• Secret Shopper feedback.<br />
• Webpage for Learning Disabilities on the <strong>Trust</strong>’s website.<br />
• Patient mealtimes <strong>and</strong> menus.<br />
Following discussion with the <strong>Trust</strong> Chairman <strong>and</strong> Chief Executive, at recent DUG meeting,<br />
members of DUG will be supported to continue work towards advising on signage <strong>and</strong> other<br />
aspects of the hospital environment <strong>and</strong> involved in improving the language <strong>and</strong> presentation<br />
of patient letters to people with Learning Disabilities.<br />
There are plans to extend the user group to include people with Learning Disabilities from<br />
both Devon <strong>and</strong> Cornwall local authority areas; also to include DUG in the wider patient/user<br />
feedback planned by the Patient Services team as part of the Patient Experience work.<br />
National St<strong>and</strong>ards for People with Learning Disabilities in Hospital<br />
Progress continues to be made towards the national st<strong>and</strong>ards as laid out in the Monitor<br />
framework <strong>and</strong> Care Quality Commission <strong>and</strong> is reported in Annex 4. The <strong>Trust</strong> continues to<br />
provide high quality care to people with Learning Disabilities:<br />
• Reasonable adjustments are made to care plans/care pathways for people with<br />
Learning Disabilities, through the involvement of LD liaison team <strong>and</strong><br />
communication with community services.<br />
• Clinical teams which care for people with Learning Disabilities on a regular basis,<br />
have active LD Link nurses. These provide leadership <strong>and</strong> support to other<br />
colleagues for the particular care needs for individuals <strong>and</strong> to promote the use of<br />
reasonable adjustments.<br />
• The role <strong>and</strong> scope of the LD liaison team in <strong>supporting</strong> people with complex<br />
needs has recently been reviewed <strong>and</strong> revised. The team provide important<br />
liaison with community services, advice to clinical teams <strong>and</strong> support to<br />
individuals <strong>and</strong> their families.<br />
• Discharges are well planned <strong>and</strong> communicated with community services,<br />
facilitated by the LD liaison team.<br />
• There is regular training <strong>and</strong> education for staff, to raise awareness of the specific<br />
needs of people with LD <strong>and</strong> those who are vulnerable adults.<br />
• Support is provided to carers as they work with clinical teams to meet the needs<br />
of patients in hospital. This is particularly relevant to parents of people with LD,<br />
some of whom have their own health <strong>and</strong> care issues – as they often spend long<br />
periods of time in hospital <strong>supporting</strong> patients.<br />
• Incidents <strong>and</strong> complaints involving patients with LD are flagged, to allow the<br />
involvement of the LD liaison nurses in the investigation <strong>and</strong> resolution of<br />
complaints/incidents.<br />
• The Meridian ‘Essence of Care’ audit system is used to review/audit to st<strong>and</strong>ards<br />
of care for patients identified with LD.
Item 11<br />
Conclusion <strong>and</strong> recommendations<br />
Further progress towards st<strong>and</strong>ards of care in hospital for people with Learning Disabilities<br />
has been made since the last update report. The review of the LD liaison team has been very<br />
useful <strong>and</strong> encouraging; it has enabled a focused revision of the St<strong>and</strong>ard Operating<br />
Procedure for the management of patients with Learning Disabilities in hospital <strong>and</strong> a review<br />
of the team structure. Issues <strong>and</strong> concerns raised through patient experiences have also<br />
been addressed as part of this review <strong>and</strong> revised operational procedure.<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Confirm commitment to the Getting It Right Charter.<br />
2. Note the outcomes of the review of Learning Disabilities Liaison team.<br />
3. Review the <strong>Trust</strong>’s continued position <strong>and</strong> satisfy itself that the <strong>Trust</strong> is able to<br />
declare continuing compliance towards the Monitor Compliance framework.
Item 11<br />
Getting it Right Charter Annex 1<br />
How is it for you? Your feedback?
Item 11<br />
Outcome of Internal review of LD Liaison team service Annex 2<br />
Intervention<br />
Review of the <strong>Trust</strong>’s operational protocol for<br />
people with LD.<br />
Progress (further updates in italic)<br />
Internal review completed – Review with<br />
external stakeholders now also completed<br />
Evaluate weekend working.<br />
Support the LD Liaison team to work in a key<br />
worker/case manager way to ensure the care plan<br />
for people with LD is fully facilitated <strong>and</strong> coordinated<br />
Undertake mortality reviews of any hospital deaths<br />
of people with LD, to review the planning of care,<br />
involvement of patient/carers <strong>and</strong> to review clinical<br />
decision-making processes<br />
Ensure involvement of the LD team in any patient<br />
who is cared for on the Liverpool Care Pathway –<br />
this will be implemented as a strict policy<br />
requirement<br />
Review the care management of people with LD<br />
who have highly complex needs to ensure objective<br />
review <strong>and</strong> learning.<br />
Review the operational leadership to of the team.<br />
Review the team structure<br />
Revise Action plan re National St<strong>and</strong>ards<br />
Complete – interim arrangement for weekend<br />
service is in place whilst Team Leader post is<br />
being recruited.<br />
Discussed with commissioners, need for<br />
additional staff in team to maintain weekend<br />
service - weekend working currently<br />
suspended. Limited value of service, due to<br />
other providers, services etc not available.<br />
Limited planned treatments at weekends<br />
currently<br />
Completed<br />
Meridian template completed – first reviews in<br />
progress.<br />
Process for Mortality reviews by Medical Lead<br />
agreed<br />
Completed<br />
In progress – process of multi-agency<br />
involvement in care management to be agreed<br />
via external review.<br />
Operational policy reviewed – to be presented<br />
to Personal Care Group<br />
Completed – B7 stepping into B6 vacant post,<br />
B7 to national advert. B7 recruited<br />
Complete – for further discussion at external<br />
review (support may be available for further<br />
resource via commissioners) Commissioners<br />
identified need to fund additional post to<br />
extend scope of team <strong>and</strong> also provide admin<br />
support<br />
Completed – pending agreement & adaptation<br />
via external review External stakeholders<br />
pleased with progress <strong>and</strong> plans
Item 11<br />
Outcome of review with external stakeholders Annex 3<br />
Intervention<br />
Update <strong>and</strong> extend use of RAPA - to alert team on<br />
patient movement (admissions, transfers,<br />
discharges)<br />
Update on Progress<br />
LD Liaison Team working with IT managers to<br />
maximise use of RAPA system – extend to<br />
outpatient appointments ;<br />
Community LD team planning to utilise RAPA<br />
to alert patient activity <strong>and</strong> identify need to<br />
support patients<br />
Improve support to those caring for people with<br />
Learning Disabilities - involvement of carers<br />
(family carers <strong>and</strong> formal carers) in hospital care<br />
Carers’ policy utilised as st<strong>and</strong>ard for carers of<br />
people with Learning Disabilities<br />
LD liaison team to facilitate involvement of<br />
carers in hospital care plan<br />
Need to include Carers’ feedback <strong>and</strong><br />
experience<br />
Promote use of Hospital Passport<br />
LD Liaison team to work closely with users,<br />
carers, community services <strong>and</strong> providers re<br />
development of Hospital Passports<br />
Team to ensure Hospital Passports fully<br />
utilised to inform care plan in hospital<br />
Improve patient experience feedback<br />
Local Patient survey now includes inpatients<br />
with Learning Disabilities on regular basis<br />
Derriford User Group (DUG) enhanced <strong>and</strong><br />
involved in range of service planning; further<br />
develop role of DUG in general patient<br />
feedback <strong>and</strong> involvement<br />
Routine Mortality reviews instigated – to review<br />
death in hospital of any patient with Learning<br />
Disabilities<br />
Prioritise LD Liaison team working - to manage<br />
increase in patient numbers (particularly inpatients)<br />
Joint operational protocol currently being<br />
revised; focus on facilitation of complete care<br />
plan, support with clinical decision-making,<br />
involvement in Best Interest Decisions, liaison<br />
with families <strong>and</strong> provider services<br />
Continue with staff awareness training <strong>and</strong><br />
development of LD Link staff<br />
Link staff working well in key<br />
specialities/clinical areas<br />
Continue with delivery of clinical training at<br />
ward/department level<br />
Continue with formal training – to junior<br />
doctors, preceptees, Healthcare Assistants<br />
Support Clinical Educators <strong>and</strong> Clinical Nurse<br />
Specialists
Item 11<br />
Develop formalised care pathway for Children with<br />
Learning Disabilities re transition to adult services;<br />
LD liaison team working with Children’s’<br />
services <strong>and</strong> LD Community team to agree<br />
transition arrangements, pathways, support<br />
Safe Places Scheme<br />
LD Liaison team working with departments – to<br />
raise awareness <strong>and</strong> ensure facilities in place<br />
for Safe Places within hospital<br />
Extend information for people with Learning<br />
Disabilities<br />
Continue with progress on Easy Read<br />
information<br />
Develop further the Web-page, for use by<br />
patients, families, carers <strong>and</strong> staff<br />
Develop LD Liaison team<br />
New Team leader appointed<br />
Agreement with commissioners re need for<br />
more funding for extended service<br />
Weekend working planned once additional<br />
staff funded<br />
Role of team to extend to include people on<br />
transition from children’s services, Autism &<br />
Aspergers - once additional staff funded<br />
Need for administrative support identified -<br />
role defined.<br />
Wider Partnership working to continue<br />
Regular review of service against national<br />
st<strong>and</strong>ards <strong>and</strong> requirements<br />
<strong>Trust</strong> represented at Learning Disabilities<br />
Board; Safeguarding Adults Boards<br />
LD liaison team continue with involvement in<br />
HealthSub Group<br />
Established close working with Patient<br />
advocacy groups, service providers,<br />
Community LD service<br />
Continue with wider network (regional)<br />
Regular report to <strong>Trust</strong> Board<br />
Review of National Confidential Enquiry into<br />
Premature deaths of People with Learning<br />
Disabilities (2013) – to include in update<br />
operational protocol<br />
Review of compliance with CQC st<strong>and</strong>ards on<br />
regular basis
Item 11<br />
Learning Disabilities National St<strong>and</strong>ards Action plan Annex 4<br />
Framework Requirement/Measure Rating Actions<br />
Monitor (2)<br />
St<strong>and</strong>ards with Actions Outst<strong>and</strong>ing<br />
Does the <strong>NHS</strong> <strong>Trust</strong> provide readily available <strong>and</strong><br />
comprehensible information to patients with learning<br />
disabilities about the following criteria?: treatment<br />
options/complaints/procedures/appointments.<br />
(1-4)<br />
PHT = 3<br />
Continue to<br />
develop easy read<br />
information - focus<br />
on specific<br />
treatments in<br />
common use; Easy<br />
Read information<br />
available on <strong>Trust</strong><br />
website.<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
Peer<br />
Review<br />
1.5<br />
Clear, accessible <strong>and</strong> timely information about medication<br />
<strong>and</strong> specific treatments <strong>and</strong> procedures is available to<br />
people with learning disability <strong>and</strong> carers.<br />
(1-3)<br />
PHT - 2<br />
Being developed<br />
with LD Link nurses<br />
for specific<br />
treatments.<br />
Involvement of LD<br />
Liaison team in all<br />
decisions re LCP<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
St<strong>and</strong>ards with ongoing actions to maintain compliance<br />
Monitor (2)<br />
Does the <strong>NHS</strong> <strong>Trust</strong> have protocols in place to encourage<br />
representation of people with learning disabilities <strong>and</strong> their<br />
family carers<br />
(1-4)<br />
PHT = 4<br />
Derriford User<br />
Group (DUG)<br />
involved in local LD<br />
Partnership Board,<br />
Health Sub-group.<br />
DUG involved in<br />
local LD events <strong>and</strong><br />
in regular feedback<br />
to the Liaison team<br />
Representation of<br />
DUG to be<br />
extended<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
Monitor (2)<br />
Does the <strong>NHS</strong> <strong>Trust</strong> have protocols in place to regularly<br />
audit its practices for patients with learning disabilities <strong>and</strong> to<br />
demonstrate the findings in routine public reports?<br />
(1-4)<br />
PHT = 4<br />
Regular reviews of<br />
care for people with<br />
LD – via Essence<br />
of Care (Meridian)<br />
Undertake Mortality<br />
Reviews of people<br />
with LD who have<br />
died in hospital<br />
Review LD Liaison<br />
team complete<br />
Updated LD Liaison<br />
team SOP –
Item 11<br />
Peer<br />
Review<br />
2.2<br />
Peer<br />
Review<br />
6.2<br />
Peer<br />
Review<br />
7.1<br />
Patients with learning disability <strong>and</strong> their carers receive<br />
appropriate information about nutrition <strong>and</strong> hydration during<br />
admission.<br />
Recording of <strong>and</strong> learning from other incidents involving<br />
people with learning disability, including complaints /Patient<br />
advice <strong>and</strong> Liaison Service feedback etc.<br />
Patient safety issues are identified proactively <strong>and</strong> patients<br />
receive a high st<strong>and</strong>ard of fundamental care.<br />
(1-3)<br />
PHT - 3<br />
(1-3)<br />
PHT - 3<br />
(1-3)<br />
PHT - 3<br />
revised with<br />
external<br />
stakeholders<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
Serco have<br />
developed Easy<br />
Read information re<br />
menus - these<br />
have been<br />
reviewed by DUG.<br />
DUG have worked<br />
with Serco to give<br />
feedback on menus<br />
from people with<br />
LD<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
Datix flag in place<br />
to identify incidents<br />
for people with LD.<br />
Incidents reviewed<br />
<strong>and</strong> reported<br />
through<br />
Safeguarding<br />
Steering Group.<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
Meridian Essence<br />
of Care filter in use<br />
– to be reviewed for<br />
all LD patients;<br />
Complaints for<br />
people with LD<br />
highlighted <strong>and</strong><br />
reviewed by LD<br />
team<br />
Review on<br />
Quarterly basis<br />
Ongoing action<br />
Completed Actions<br />
Peer<br />
Review<br />
1.3<br />
All Hospital departments have access to <strong>and</strong> use a wide<br />
range of resources to help in the production of easy read<br />
documents for assessments, care plans etc.<br />
(1-3)<br />
PHT - 3<br />
Resources <strong>and</strong><br />
support available to<br />
specialities re Easy<br />
Read information<br />
Peer<br />
Review<br />
2.4<br />
All hospitals reflect the reasonable adjustments required for<br />
people with learning disability in their Single Equality<br />
Scheme <strong>and</strong> its associated action plan.<br />
(1-3)<br />
PHT - 3<br />
Audit of reasonable<br />
adjustments to care<br />
plans of people<br />
with LD.<br />
Review <strong>and</strong> update<br />
of protocol for<br />
people with LD in
Item 11<br />
Peer<br />
Review<br />
2.5<br />
Peer<br />
Review<br />
2.7<br />
Peer<br />
Review<br />
3.3<br />
Patients with learning disability are discharged home safely. (1-3)<br />
PHT - 3<br />
Training <strong>and</strong> education regarding learning disability, health<br />
inequalities <strong>and</strong> communication is provided to all hospital<br />
staff.<br />
Family carers <strong>and</strong> other care providers are involved as<br />
partners, planning the care of a patient with a learning<br />
disability where possible.<br />
(1-3)<br />
PHT - 3<br />
(1-3)<br />
PHT -3<br />
hospital<br />
Review of roles of<br />
LD Liaison Team<br />
LD Liaison team<br />
involved in<br />
discharge planning.<br />
Readmissions<br />
identified through<br />
RAPA system;<br />
Feedback from<br />
clinical teams in<br />
community –<br />
evidence of good<br />
discharge planning<br />
Wide range of LD<br />
awareness training<br />
achieved;<br />
Safeguarding adult<br />
training now in<br />
induction &<br />
m<strong>and</strong>atory<br />
programme for all<br />
clinical staff.<br />
Link staff supported<br />
by LD Liaison team<br />
<strong>Trust</strong> Carers’ Policy<br />
published.<br />
Recommendations<br />
from Patients<br />
Association Survey<br />
(2012)<br />
implemented<br />
Reviewed the care<br />
management of LD<br />
patient with<br />
complex needs
Item 12<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board<br />
5 th July2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Equality & Diversity Update<br />
Equality & Diversity Leads<br />
Director of HR & OD<br />
Director of HR & OD<br />
Purpose<br />
The purpose of this report is to initiate the work required to integrate <strong>and</strong><br />
embed equality <strong>and</strong> diversity strategically at Board level <strong>and</strong> as part of the<br />
core business of the <strong>Trust</strong>. The report will also inform the Board about the<br />
proposals for the implementation of the Board Inclusion Programme <strong>and</strong><br />
request support with this.<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
•<br />
•<br />
•<br />
Corporate Objectives<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
• • • •<br />
Executive Summary<br />
This report offers detail on the current position of Equality <strong>and</strong> Diversity in the organisation. It<br />
identifies examples of good practice <strong>and</strong> how it can impact on patient <strong>and</strong> staff experiences. It<br />
demonstrates areas where there are obstacles to progress, i.e. where equality processes are<br />
not integrated into core business, as in the case of the equality assessments.<br />
It recommends that Equality <strong>and</strong> Diversity becomes part of core business which in turn<br />
facilitates compliance with the Equality Act 2010 <strong>and</strong> Public Sector Duty. The recently<br />
established Equality <strong>and</strong> Diversity Steering Group (EDSG) requires commitment from the<br />
senior management team to support delivery of the Equality Delivery System (EDS).This<br />
includes proposals for a Board Inclusion Development Programme, supported by the <strong>Plymouth</strong><br />
Way, to further develop a common culture of quality care.<br />
Quality Impact Assessment<br />
Fulfilling our equality obligations will ensure all patients can access consistent quality care<br />
Financial Impact Assessment<br />
Litigation costs<br />
Regulatory Impact Assessment<br />
Compliance with the Equality Act 2010 <strong>and</strong> Public Sector Duty<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Support the principal of equality & diversity becoming part of the <strong>Trust</strong>’s core business.<br />
2. Support proposals for a Board Inclusion Development Programme<br />
3. Support the utilisation of <strong>Trust</strong> surveys, complaints <strong>and</strong> incidents to identify trends <strong>and</strong><br />
the interventions required<br />
4. Support the <strong>Plymouth</strong> Way in embedding the values in the <strong>Trust</strong> <strong>and</strong> allowing the<br />
appropriate challenge of behaviours <strong>and</strong> attitudes<br />
1
Item 12<br />
Next Steps<br />
1. Conversation between the providers of the Board Inclusion Programme <strong>and</strong> the Chair of<br />
the HR&OD Committee<br />
2. Meeting of the Chairman, the Chief Executive, the Director of HR&OD <strong>and</strong> the providers<br />
of the Board Inclusion Programme<br />
3. Board Inclusion Development Programme to commence Quarter 3 13/14.
Item 12<br />
DETAILED REPORT<br />
<strong>Trust</strong> Board 5 th July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Equality & Diversity Update<br />
Equality & Diversity Leads<br />
Director of HR&OD<br />
Director of HR&OD<br />
Purpose<br />
The purpose of this report is to initiate the work required to integrate <strong>and</strong> embed equality <strong>and</strong><br />
diversity strategically at Board level <strong>and</strong> as part of the core business of the <strong>Trust</strong>. The report<br />
will also inform the Board about the proposals for the implementation of the Board Inclusion<br />
Programme <strong>and</strong> request support with this.<br />
Background<br />
Following a period of change within the organisation, the lines of responsibility <strong>and</strong> reporting<br />
for the equality <strong>and</strong> diversity work programme were unclear. The Director of HR & OD has<br />
taken on the role of executive lead for this work <strong>and</strong> the Equality <strong>and</strong> Diversity Steering<br />
Group (EDSG) has been established to replace the previous equality delivery group.<br />
Following the introduction <strong>and</strong> implementation of the Equality Delivery System (EDS), the<br />
<strong>Trust</strong> assessed its performance against the EDS outcomes. This produced equality<br />
objectives as required by the Public Sector Equality Duty.<br />
The EDS is a national framework, developed by the Department of Health, in conjunction<br />
with the Equality <strong>and</strong> Diversity Council. It has 18 outcomes defined under 4 goals. The goals<br />
are:<br />
1. Better health outcomes for all;<br />
2. Improved patient access <strong>and</strong> experience;<br />
3. Empowered, engaged <strong>and</strong> well supported staff; <strong>and</strong><br />
4. Inclusive leadership at all levels.<br />
These grades <strong>and</strong> objectives were agreed <strong>and</strong> published at the beginning of 2012 <strong>and</strong> can<br />
be found in annex 1.<br />
Equality & Diversity<br />
1. Equality & Diversity Steering Group<br />
The EDSG, was established in October 2012 <strong>and</strong> is a sub-committee, reporting to the<br />
HR&OD Committee. The purpose of the group is to develop <strong>and</strong> oversee the equality <strong>and</strong><br />
diversity work programme, including, the <strong>Trust</strong>’s equality objectives <strong>and</strong> the EDS. It will<br />
ensure work is co-ordinated across the <strong>Trust</strong> with the involvement <strong>and</strong> ownership of relevant<br />
stakeholders whilst providing assurance to the Committee that the equality <strong>and</strong> diversity<br />
agenda is placing the patient at the heart of what we do, whilst meeting legislative<br />
requirements, CQC st<strong>and</strong>ards <strong>and</strong> statutory duty.<br />
The group will also support the <strong>Trust</strong> in developing a culture that values staff, improves<br />
patient experience while putting equality, diversity <strong>and</strong> human rights at the heart of all of its<br />
business.<br />
3
Item 12<br />
2. Board Inclusion Development Programme<br />
Following the Board’s review in 2012 <strong>and</strong> though the EDS assessment an area of priority that<br />
was identified, which required action was the positioning of equality strategically at Board<br />
<strong>and</strong> senior management level. Methods to address this were investigated <strong>and</strong> a programme,<br />
provided in conjunction with the <strong>NHS</strong> Leadership Academy was found.<br />
This programme is the Board Inclusion Development Programme provided by Diversity<br />
Practice. The programme is being offered free of charge to the <strong>Trust</strong> but would usually have<br />
a cost of £21000.<br />
Following a small selection process, the Director of HR&OD <strong>and</strong> the Director of Governance<br />
met with Diversity Practice, during April 2013, who is the preferred service provider. They<br />
delivered a detailed presentation on the value of the programme to staff <strong>and</strong> patients <strong>and</strong><br />
made recommendations in terms of the next steps for the <strong>Trust</strong>’s consideration.<br />
The aim of the programme is to support the Board in developing the critical connection<br />
between the organisational culture, Equality, Diversity <strong>and</strong> Inclusion (EDI) <strong>and</strong> the <strong>Trust</strong>’s<br />
core business. It will also identify our current position, identify any gaps <strong>and</strong> what needs to<br />
be done to ensure that the <strong>Trust</strong> delivers an equitable service to all its delivers stakeholders.<br />
It is essential that the programme is aligned to the <strong>Plymouth</strong> Way, the <strong>Trust</strong> Strategy which<br />
incorporates Safety <strong>and</strong> Quality, <strong>and</strong> the Quality Strategy. It will support the objectives of<br />
improving patient experience, staff engagement <strong>and</strong> meeting our financial obligations<br />
The EDSG will support <strong>and</strong> facilitate the programme, providing an advice <strong>and</strong> challenge<br />
function with mutual accountability with the HR&OD Committee <strong>and</strong> will update the <strong>Trust</strong><br />
Board, to give visibility <strong>and</strong> assurance of progress <strong>and</strong> outcomes of the programme.<br />
The EDSG had a meeting in June 2013 which was chaired by the Director of Governance.<br />
The meeting was attended by Diversity Practice, who is the provider of the programme <strong>and</strong><br />
Yvonne Coghill, from the <strong>NHS</strong> Leadership Academy who will support the <strong>Trust</strong> through this<br />
programme. A number of recommendations were made at this meeting which will be<br />
progressed over the coming weeks; these include conversations with the chair of the HR &<br />
OD Committee, Chief Executive <strong>and</strong> the <strong>Trust</strong> Chairman.<br />
3. Good practice<br />
There are areas of good practice across the <strong>Trust</strong> where equality <strong>and</strong> diversity is having a<br />
positive impact on staff <strong>and</strong> patients, these include:<br />
• Project Search – Work rotation opportunities for 19 – 24 year olds with learning<br />
disabilities;<br />
• Flexible Retirement – giving people the option to change the intensity or hours of<br />
their work as they approach retirement which helps the <strong>Trust</strong> retain experienced,<br />
valued employees with a range of skills;<br />
• Valuing people statement in all <strong>Trust</strong> policies;<br />
• Learning Disability Service – liaison nurses providing additional, specialised<br />
support for patient with Learning Disabilities;<br />
• Meal time support for patients as required;<br />
• Bespoke ‘valuing people’ training including dignity in care <strong>and</strong> recommendations<br />
from the Francis report;<br />
• Equality & diversity included in the revised plan for induction; <strong>and</strong><br />
• Equality <strong>and</strong> Diversity Leads are part of the CQC Leads Forum to integrate<br />
equality <strong>and</strong> diversity into the assurance that we collect for each CQC outcome.
Item 12<br />
4. Current risks <strong>and</strong> concerns<br />
The top risks <strong>and</strong> concerns for PHNT have been identified as:<br />
• Equality impact assessment process is not integrated robustly into business<br />
practice. This is a legislative requirement to ascertain how the way we provide our<br />
services affects our patients <strong>and</strong> staff;<br />
• Lack of equality information around complaints <strong>and</strong> incidents;<br />
• Engagement with issues arising from the staff <strong>and</strong> patient surveys;<br />
• Lack of disclosure in workforce data; <strong>and</strong><br />
• Poor quality patient data.<br />
Conclusion<br />
By embedding equality <strong>and</strong> diversity into the day to day business of the organisation, with<br />
clearly defined objectives, we will ensure that we become an employer <strong>and</strong> service provider<br />
of choice.<br />
The Board Inclusion Development Programme, aligned to the <strong>Plymouth</strong> Way <strong>and</strong> Quality<br />
Strategy, will be a first step to developing an improved equality <strong>and</strong> diversity strategy <strong>and</strong><br />
infrastructure, impacting positively on our patients <strong>and</strong> staff.<br />
This will enable us to show, over time, that all our patients have equal access to services<br />
which are open <strong>and</strong> approachable to all. In addition it will let us demonstrate that we deliver<br />
high quality outcomes in partnership with others, are responsible <strong>and</strong> accountable for what<br />
we do, showing to our staff that we value their contributions whilst developing their potential.<br />
Recommendations<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Support the principal of equality & diversity becoming part of the <strong>Trust</strong>’s core<br />
business;<br />
2. Support proposals for Board Inclusion Development Programme;<br />
3. Support the utilisation of <strong>Trust</strong> surveys, complaints <strong>and</strong> incidents to identify trends<br />
<strong>and</strong> the interventions required <strong>and</strong><br />
4. Support the <strong>Plymouth</strong> Way in embedding the values in the <strong>Trust</strong> <strong>and</strong> allowing the<br />
appropriate challenge of behaviours <strong>and</strong> attitudes
Item 12<br />
EDS Grades <strong>and</strong> E & D Objectives Annex 1<br />
<strong>Plymouth</strong> <strong>Hospitals</strong> – Equality Objectives<br />
• To enable the <strong>Trust</strong> to analyse patient outcomes <strong>and</strong> experiences by protected characteristic<br />
<strong>and</strong> as a result, identify <strong>and</strong> initiate improvements as required. To do this we will:<br />
• Improve patient data collection to allow the monitoring of all required protected<br />
characteristics in line with the public sector duty requirements. This will include<br />
improving the facilities to collect patient data on our systems<br />
• Continue to collect <strong>and</strong> exp<strong>and</strong> the collection of equality information on the local patient<br />
surveys.<br />
• Develop <strong>and</strong> deliver a programme of awareness/education to ensure staff have the<br />
knowledge <strong>and</strong> skills to collect this information in appropriate ways<br />
• On-going monitoring <strong>and</strong> analysis of patient/carer feedback, complaints, untoward<br />
incidents <strong>and</strong> patient survey results will be undertaken on a monthly basis, <strong>and</strong><br />
outcomes fed back to the appropriate assurance leads to enable them to develop <strong>and</strong><br />
implement actions as required<br />
• The annual review of the equality objectives will demonstrate an improvement in the<br />
patient data collected, <strong>and</strong> its use.<br />
• To improve the discharge experience for all patients <strong>and</strong> their relatives/carers regardless of<br />
their protected characteristics by ensuring that:<br />
• The discharge process is completed in a timely fashion<br />
• Clear information is provided in an appropriate format about any medications <strong>and</strong> ongoing<br />
care requirements.<br />
• On-going monitoring <strong>and</strong> analysis of patient/carer feedback, untoward incidents,<br />
complaints <strong>and</strong> patient survey results will be undertaken on a monthly basis, <strong>and</strong><br />
outcomes fed back to the appropriate assurance leads to enable them to develop <strong>and</strong><br />
implement actions as required .<br />
• The annual review of the equality objectives with the local interests groups will monitor<br />
the implementation of actions <strong>and</strong> assess the resulting improvements<br />
• Ensure information provided to patients regarding their care/treatment is provided<br />
• Within appropriate timescales<br />
• In an appropriate, underst<strong>and</strong>able format.<br />
• Monitoring <strong>and</strong> analysis of patient/carer feedback, complaints <strong>and</strong> patient survey results<br />
will be undertaken on a monthly basis, <strong>and</strong> outcomes fed back to the appropriate<br />
assurance leads to enable them to develop <strong>and</strong> implement actions as required.<br />
• The annual review of the equality objectives with the local interests groups will monitor<br />
the implementation of actions <strong>and</strong> assess the resulting improvements<br />
• Ensure Equality & Diversity learning <strong>and</strong> development programmes, specifically around<br />
attitudes <strong>and</strong> behaviours, are attended by all staff on an annual basis. Monitor <strong>and</strong> analyse<br />
attendance by staff group via the Oracle Learning Management system (OLM) <strong>and</strong> the<br />
Electronic Staff Record (ESR). Development of an assessment tool needs to be undertaken to<br />
assess the skills <strong>and</strong> competencies of staff gained from the learning <strong>and</strong> how positive<br />
outcomes are produced in the work area.<br />
• Ensure the Board can define <strong>and</strong> position equality & diversity as a strategic opportunity<br />
• To improve access <strong>and</strong> quality in healthcare <strong>and</strong> reduce health inequalities. Monitoring<br />
<strong>and</strong> analysis of patient/carer feedback, complaints <strong>and</strong> patient survey results will be<br />
undertaken on a monthly basis, <strong>and</strong> outcomes fed back to the appropriate assurance<br />
leads to enable them to develop <strong>and</strong> implement actions as required<br />
• To use the <strong>NHS</strong> constitution as an opportunity to ensure comprehensive services to<br />
patients from all protected characteristics. Monitoring <strong>and</strong> analysis of patient/carer<br />
feedback, complaints <strong>and</strong> patient survey results will be undertaken on a monthly basis,<br />
6
Item 12<br />
<strong>and</strong> outcomes fed back to the appropriate assurance leads to enable them to develop<br />
<strong>and</strong> implement actions as required<br />
• To embed equality & diversity into all mainstream business<br />
• Increase leadership competence <strong>and</strong> capability in equality & diversity using the<br />
principles of the <strong>NHS</strong> Leadership Framework <strong>and</strong> EDS Leadership Competency<br />
Framework.<br />
• To underst<strong>and</strong> the impact of equality <strong>and</strong> diversity on staff <strong>and</strong> patients through regular<br />
reports to the <strong>Trust</strong> Board.<br />
7
Item 12<br />
<strong>Plymouth</strong> <strong>Hospitals</strong> <strong>Trust</strong> – EDS Self-Assessment Grades<br />
Goal Outcomes Status<br />
Undeveloped Developing Achieving Excelling<br />
1 Better<br />
health<br />
Outcomes for<br />
all<br />
1.1 Services are commissioned, designed <strong>and</strong> procured to<br />
meet the health needs of local communities. The<br />
health needs of local communities, promote well-being,<br />
<strong>and</strong> reduce health inequalities<br />
1.2 Individual patients needs are assessed <strong>and</strong> resulting<br />
services provided in appropriate <strong>and</strong> effective ways<br />
1.3 Changes across services for individual patients are<br />
discussed with them <strong>and</strong> transitions are made<br />
smoothly<br />
1.4 The safety of patients is prioritised <strong>and</strong> assured. In<br />
particular, patients are free from abuse , harassment,<br />
bullying <strong>and</strong> violence from other patients <strong>and</strong> staff, with<br />
redress being open <strong>and</strong> fair to all<br />
1.5 Public Health, vaccination <strong>and</strong> screening programmes<br />
reach <strong>and</strong> benefit all local communities <strong>and</strong> groups<br />
2 Improved<br />
patient<br />
access <strong>and</strong><br />
experience<br />
2.1 Patients, carers <strong>and</strong> communities can readily access<br />
services <strong>and</strong> should not be denied access on<br />
unreasonable grounds.<br />
2.2 Patients are informed <strong>and</strong> supported to be as involved<br />
as they wish to be in their diagnosis <strong>and</strong> decisions<br />
about their care <strong>and</strong> to exercise choice about<br />
treatments <strong>and</strong> place of treatment<br />
8
Item 12<br />
2.3 Patients <strong>and</strong> carers report positive experiences of their<br />
treatment <strong>and</strong> care outcomes <strong>and</strong> of being listened to<br />
<strong>and</strong> respected <strong>and</strong> how their privacy <strong>and</strong> dignity is<br />
prioritised<br />
2.4 Patients <strong>and</strong> carers complaints about services <strong>and</strong><br />
subsequent claims for redress should be h<strong>and</strong>led<br />
respectfully <strong>and</strong> efficiently<br />
3 Empowered,<br />
engaged <strong>and</strong><br />
well<br />
supported<br />
staff<br />
3.1 Recruitment <strong>and</strong> selection processes are fair, inclusive<br />
<strong>and</strong> transparent so that the workforce becomes as<br />
diverse as it can be within all occupations <strong>and</strong> grades<br />
3.2 Levels of pay <strong>and</strong> related terms <strong>and</strong> conditions are<br />
fairly determined for all posts with staff doing equal<br />
work <strong>and</strong> work rated as of equal value being entitled to<br />
equal pay<br />
3.3 Through support, training, personal development <strong>and</strong><br />
performance appraisal, staff are confident <strong>and</strong><br />
competent to do their work so that services are<br />
commissioned or provided appropriately<br />
3.4 Staff are free from abuse, harassment, bullying <strong>and</strong><br />
violence from both patients <strong>and</strong> their relatives <strong>and</strong><br />
colleagues with redress being fair <strong>and</strong> open to all<br />
3.5 Flexible working options are made available to all staff,<br />
consistent with the needs of the service <strong>and</strong> the way<br />
people lead their lives.<br />
9
Item 12<br />
3.6 The workforce is supported to remain healthy, with a<br />
focus on addressing major health <strong>and</strong> lifestyle issues<br />
that affect individual staff <strong>and</strong> the wider population<br />
4 Inclusive<br />
leadership at<br />
all levels<br />
4.1 Boards <strong>and</strong> senior leaders conduct <strong>and</strong> plan their<br />
business so that equality is advanced <strong>and</strong> good<br />
relations fostered within their organisations <strong>and</strong> beyond<br />
4.2 Middle managers <strong>and</strong> other line managers support <strong>and</strong><br />
motivate their staff to work in culturally competent ways<br />
within a work environment free from discrimination<br />
Excelling – Purple<br />
Achieving - Green<br />
Developing – Amber<br />
Undeveloped – Red<br />
4.3 The organisation uses the competency framework for<br />
Equality <strong>and</strong> Diversity Leadership to recruit, develop<br />
<strong>and</strong> support strategic leaders to advance equality<br />
outcomes<br />
10
Item 13<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 th July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Information Governance<br />
Head of Clinical Systems Governance<br />
Director of Planning <strong>and</strong> Site Services (Senior Information Risk Owner)<br />
Director of Planning <strong>and</strong> Site Services (Senior Information Risk Owner)<br />
Purpose<br />
The Senior Information Risk Owner (SIRO) provides the Board with a quarterly<br />
update on Information Governance; highlighting key progress, risks, incidents <strong>and</strong><br />
management action.<br />
The case note improvement project is being reported to the Safety <strong>and</strong> Quality<br />
Committee at each meeting. The evidence for Care Quality Commission Outcome<br />
21 (Records) was presented to the May 13 Audit Committee.<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
•<br />
•<br />
Corporate Objectives<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
Whilst Information Governance is part of everyone’s role within the <strong>Trust</strong>, work is being carried out by<br />
key teams to improve the overall Information Governance Framework. This is informed by the<br />
Information Governance Toolkit requirements, new incident reporting criteria, Care Quality Commission<br />
& <strong>NHS</strong> Litigation Authority (<strong>NHS</strong>LA) feedback <strong>and</strong> national Data Quality benchmarking on the Secondary<br />
Uses Service (SUS) dashboards.<br />
This report highlights the work carried out by the four steering groups reporting to the Records <strong>and</strong><br />
Information Governance Forum.<br />
Quality Impact Assessment<br />
An effective Information Governance framework is essential to ensure that all members of staff manage<br />
information for the benefit of patients.<br />
Financial Impact Assessment<br />
• Information Governance Breaches can attract financial penalty from the Information<br />
Commissioner.<br />
• Effective corporate document management is essential for NHLSA Assessment <strong>and</strong> will affect<br />
premiums.<br />
• Whilst the primary reason for accurate information is for patient care, this information assists with<br />
running an efficient service.<br />
Regulatory Impact Assessment<br />
• The Information Commissioners Office regulates the use <strong>and</strong> access to personal <strong>and</strong> official<br />
data. The main laws being the Data Protection Act <strong>and</strong> the Freedom of Information Act.<br />
• The Care Quality Commission regulates:<br />
Records st<strong>and</strong>ards under Outcome 21.<br />
Transferring information to other providers under Outcome 6<br />
• The Health & Social Care Information Centre oversee the Secondary Use Service (SUS).<br />
1
Item 13<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to note:<br />
1. Work being overseen by the Records <strong>and</strong> Information Governance forum <strong>and</strong> the Records<br />
Strategy work being reported to the Safety <strong>and</strong> Quality Committee.<br />
2. The Medical Director taking the role of Chief Clinical Information Officer.<br />
3. The recruitment of a dedicated FOI Manager to address the FOI backlog.<br />
Next Steps<br />
1. Follow up action for Outcome 21 issues raised by CARE QUALITY COMMISSION initial<br />
feedback.<br />
2. The “Development <strong>and</strong> Management of <strong>Trust</strong> Wide Documents” Policy is being significantly<br />
changed <strong>and</strong> will be brought to a future Board meeting for ratification.<br />
3. The IG team will submit V11 baseline IG Toolkit by 31 st July 13.<br />
4. The IG team will produce figures for incidents recorded using new categories on Datix for next<br />
Board report.<br />
5. The Caldicott Guardian to update the executive team on the implications of the recent IG report<br />
from Dame Fiona Caldicott known as Caldicott2.<br />
2
Item 13<br />
DETAILED REPORT<br />
<strong>Trust</strong> Board 5 th July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Information Governance<br />
Head of Clinical Systems Governance<br />
Director of Planning <strong>and</strong> Site Services (Senior Information Risk Owner)<br />
Director of Planning <strong>and</strong> Site Services (Senior Information Risk Owner)<br />
Purpose<br />
1. The purpose of the report is to provide an update on Information Governance; highlighting key<br />
progress, risks, incidents <strong>and</strong> management action.<br />
Background<br />
2. Information Governance is overseen by the Records & Information Governance Forum (RIGF)<br />
which is chaired by the SIRO. The following sub groups report into this Forum:<br />
Key Highlights<br />
• Caldicott Information Governance Group (CIGG)<br />
• Data Quality Steering Group (DQSG)<br />
• Health Records Steering Group (HRSG)<br />
• Corporate Records Management Steering Group (CRMSG)<br />
Information Governance<br />
3. The Care Quality Commission’s initial feedback following the last routine investigation highlights<br />
three Information Governance issues under Outcome 21:<br />
Outcome 21 Issues raised by CARE<br />
QUALITY COMMISSION<br />
Physical Security of Casenotes.<br />
• On some wards records were<br />
accessible to patients <strong>and</strong> visitors.<br />
• In some areas case note cupboards<br />
were not locked <strong>and</strong> some had the<br />
key pad access number available on<br />
the cupboard.<br />
• In one ward, the locks were no longer<br />
suitable to lock the cupboard doors.<br />
Electronic check in.<br />
• In some areas information such as<br />
patients' names, addresses <strong>and</strong><br />
dates of birth, was easily visible to<br />
other people in the waiting area.<br />
Initial Management Response<br />
• St<strong>and</strong>ard lockable trollies have been<br />
introduced onto all wards as part of<br />
the Records Management Action<br />
Plan.<br />
• This is being reported to the Safety<br />
<strong>and</strong> Quality Committee by the Interim<br />
Records Strategy Lead.<br />
• Action for the Director of Nursing to<br />
Introduce Audits of the use of these<br />
trollies.<br />
• Audits will be reported to the Health<br />
Records Steering Group.<br />
• The Clinical Admin Programme has<br />
raised these concerns <strong>and</strong> will be<br />
addressing them directly with Intouch<br />
at a contract implementation review<br />
meeting on 27 th June.<br />
• The first priority will be to adapt the<br />
screens to improve confidentiality.<br />
3
Item 13<br />
Telephone conversations.<br />
• On some wards telephone<br />
conversations made by staff about<br />
patients could be clearly heard by<br />
patients <strong>and</strong> visitors in seating areas.<br />
• The Head of Clinical Systems<br />
Governance will review procedures on<br />
wards with Nursing management <strong>and</strong><br />
the Caldicott Guardian.<br />
• The correct procedures will be<br />
communicated to ward staff <strong>and</strong><br />
overseen by the Caldicott Group<br />
4. The Information Governance Toolkit (IGT) is now being overseen by the Health <strong>and</strong> Social Care<br />
Information Centre (HSCIC) which replaced Connecting for Health. The HSCIC released Version<br />
11 in early June13 without any significant change to the 45 requirements. The IG team are<br />
preparing for the Baseline Submission at the end of July 13.<br />
5. In t<strong>and</strong>em with the release of V11 of the IGT, the HSCIC have published new guidance on the<br />
way that <strong>Trust</strong>s should report, manage <strong>and</strong> investigate Information Governance Serious Incidents<br />
Requiring Investigation (SIRIs). From June 13 all Organisations processing health <strong>and</strong> adult<br />
social care personal data are required to use a new online IG Incident Reporting Tool to report IG<br />
SIRIs to the Department of Health, Information Commissioners Office (ICO) <strong>and</strong> other regulators<br />
as appropriate.<br />
6. The algorithm used to decide if an IG incident is a SIRI has altered. The Information Governance<br />
Team is learning the new system. It is recognised that there is no simple definition of a serious<br />
IG incident. What may at first appear to be of minor importance may, on further investigation, be<br />
found to be serious <strong>and</strong> vice versa. <strong>Plymouth</strong> <strong>Hospitals</strong> <strong>Trust</strong> last reported an IG SIRI to the ICO<br />
in January 2012. In the 2012/13 financial year the IG team dealt with 354 IG incidents none of<br />
which were categorised as SIRI’s.<br />
7. The IG Team now record all incidents that they deal with on Datix <strong>and</strong> are currently reviewing the<br />
categories used to reflect the new HSCIC guidance. Figures will be available for the next Board<br />
update. In addition, the team continue to scan the Datix system <strong>and</strong> flag those incidents with an<br />
IG element.<br />
8. Dame Fiona Caldicott has published the report of the recent review of Information Governance.<br />
This is known as Caldicott2. The Caldicott Guardian will present the implications of this review to<br />
the Executive team.<br />
9. The original Caldicott report was written in 1997 when the health services were more paternalistic<br />
<strong>and</strong> much less patient centred, now the public are a lot more concerned about what happens to<br />
their information. Caldicot2 states that a re-balancing of sharing <strong>and</strong> protecting information is<br />
urgently needed in the patients’ <strong>and</strong> service users’ interest.<br />
10. The original Caldicott Principles still st<strong>and</strong> but have been updated with a 7 th principle being<br />
added: “The duty to share information can be as important as the duty to protect patient<br />
confidentiality”. Appropriate sharing of information is seen as important as maintaining<br />
confidentiality.<br />
11. The following Subject Access Requests have been made under the Data Protection Act for 2013<br />
(as at 14/06/2013)<br />
No of requests Disclosed after 40 Cumulative Total<br />
days<br />
January 24 3 24<br />
February 16 5 40<br />
March 13 3 53<br />
April 13 4 66<br />
May 25 None as at 14/06/13 91<br />
4
Item 13<br />
Corporate Documents<br />
12. Accessing <strong>Trust</strong> wide policies <strong>and</strong> procedures will soon be through the new intranet site being<br />
rolled out by the Communications Team. This will replace the current network shared folder. This<br />
is in line with the vision of the Healthnet replacement being the main portal for staff to access<br />
information.<br />
13. The Information Governance (IG) team have continued to target out of date policies. Currently 24<br />
of the 161 policies are out of date. Of this number there is a residual group of 10 policies that<br />
have remained out of date for over 12 months. All of the Ratifying Leads are aware <strong>and</strong> have<br />
been emailed a list of the policies that they are responsible for.<br />
14. The “Development <strong>and</strong> Management of <strong>Trust</strong> Wide Documents” Policy is undergoing a significant<br />
review following feedback from the last <strong>NHS</strong>LA visit <strong>and</strong> on-going learning. The updated policy<br />
will need to be ratified by the <strong>Trust</strong> Board. One key issue that needs to be decided is how local<br />
as opposed to <strong>Trust</strong> wide documents will be governed.<br />
15. The <strong>Trust</strong> has noted that it has become increasingly difficult to sustain compliance within the 20<br />
working day deadline for Freedom of Information requests. The number of requests has now<br />
stabilised, however, the number of questions being asked within each request <strong>and</strong> the case<br />
complexity has increased. We have acted to address this matter by recruiting a fixed-term FOI<br />
Manager with a view to reviewing <strong>and</strong> improving our practices in this regard <strong>and</strong> providing<br />
additional resource <strong>and</strong> focus on this important area<br />
16. Current FOI metrics are as follows:<br />
2009 2010 2011 2012<br />
As at<br />
21/05/13<br />
Open cases that are still within 20 working<br />
day limit<br />
0 0 0 0 22<br />
Open case past the 20 working day limit<br />
(Excluding any previous year open cases)<br />
0 0 0 4 25<br />
Number of cases answered on time 172 138 111 117 49<br />
Number of cases not answered on time 38 64 113 103 37<br />
Data not available 9 32 11 7 2<br />
Total number of Freedom of<br />
Information cases<br />
219 234 235 231 135<br />
Percentage of compliance 79% 68% 50% 53% Pending<br />
Health Records (Casenotes <strong>and</strong> the move to eNotes (electronic notes)<br />
17. Progress on the Records Management Programme <strong>and</strong> Casenote Improvement Programme<br />
continues to be reported to the Safety <strong>and</strong> Quality(S&Q) Committee. The Interim Records<br />
Strategy Lead attended the June 13 meeting to update on the actions.<br />
18. The Director of Planning <strong>and</strong> Site Services <strong>and</strong> Interim Records Strategy Lead met with the<br />
Medical Director on 10 th June 13 to discuss Professional Clinical Leadership for Health Record<br />
keeping <strong>and</strong> the Records Strategy The Medical Director agreed to take on the role of Chief<br />
Clinical Information Officer which is a Board level clinician who leads on electronic health<br />
records. The need for this role was highlighted in the DH Information Strategy; “The power of<br />
information”.<br />
5
Item 13<br />
19. The Medical Director has written to all Service Line Clinical leads instructing them to:<br />
• Ensure that all doctors have access to record keeping training.<br />
• Audit Clinical Record Keeping St<strong>and</strong>ards <strong>and</strong> present to departmental Clinical<br />
Governance meetings.<br />
• To provide assurance to the Safety <strong>and</strong> Quality Committee.<br />
The Medical Director will review these actions through performance meetings.<br />
20. In preparation for the transition to eNotes the Interim Records Strategy Lead is reviewing how<br />
Clinical Letters are stored across the <strong>Trust</strong>. These documents must be captured in order to store<br />
an accurate historic record on the patient’s electronic notes.<br />
21. The Director of Planning <strong>and</strong> Site Services <strong>and</strong> Interim Records Strategy Lead presented to the<br />
Medical Education Committee (MEC) in May 13 to update on the eNotes strategy. This was well<br />
received by the clinicians with offers of support.<br />
Information Security<br />
22. There has beeen a st<strong>and</strong>ardisation of External Storage Devices. All future purchases of USB pen<br />
drives <strong>and</strong> external hard drives will be limited to a product range featuring always-on encryption<br />
which negates the risk of staff purposefully or inadvertently disabling data encryption. The<br />
devices also offer greater compatibility <strong>and</strong> are easier to use.<br />
26. <strong>Plymouth</strong> ICT Shared Service are now deploying the AirWatch Mobile Device Management<br />
solution to <strong>Trust</strong> issued iPads <strong>and</strong> mobile devices. Mobile Device Management is essential to<br />
enable the secure use of consumer devices in business <strong>and</strong> clinical settings. It will also act as an<br />
enabler for any future ‘Bring Your Own Device’ initiative which the <strong>Trust</strong> may wish to explore.<br />
AirWatch is part of the longer term ICT strategy to provide flexibility to choose devices best suited<br />
to the intended task <strong>and</strong> enable mobile access to clinical <strong>and</strong> business applications.<br />
Data Quality of Electronic Patient Records<br />
23. The Data Quality Steering Group benchmarks the quality of the data submitted to the Secondary<br />
Use Service (SUS) using the national SUS Data Quality Dashboard. Patients should be<br />
identified using their <strong>NHS</strong> number; with varying compliance targets based on national<br />
achievement for 3 different categories. The <strong>Trust</strong> continues to achieve these targets in 12/13.<br />
<strong>NHS</strong> Number Categories National Target – Month<br />
12<br />
<strong>Trust</strong> Achievement – Month<br />
12<br />
Admitted Planned Care 99.1% 99.1%<br />
Outpatient 99.3% 99.3%<br />
ED 94.9% 97.1%<br />
24. Similarly, the recording of a patient’s GP Practice must meet national targets, which the <strong>Trust</strong> is<br />
currently exceeding in all areas with the exception of the ED, but the Data Quality team are<br />
implementing a plan to achieve this. The <strong>Trust</strong> is achieving the Outpatient Attendance Outcomes<br />
target, but further improvement will be delivered when the eOutcomes solution is released by the<br />
Clinical Admin Programme.<br />
25. The one outst<strong>and</strong>ing indicator is the population of the Patient Pathway Identifier, when this is<br />
populated on SUS, PHNT have the potential to be top of the Data Quality ratings for all <strong>Trust</strong>s in<br />
the old South West SHA area. This improvement is on the list of priorities for the Software<br />
Development team.<br />
26. A draft Data Quality strategy has been created <strong>and</strong> will be implemented alongside the Clinical<br />
Administration Review. The implementation of the strategy will ensure that the responsibility <strong>and</strong><br />
accountability for data quality is understood <strong>and</strong> built into the new roles. Alongside this,<br />
appropriate administration training will be delivered <strong>and</strong> the Data Quality function will provide ongoing<br />
support <strong>and</strong> performance monitoring of Data Quality indicators.<br />
6
Item 13<br />
Recommendations<br />
27. The Board is asked to note:<br />
Conclusion<br />
• The work being overseen by the Records <strong>and</strong> Information Governance Forum <strong>and</strong> the<br />
records strategy work being reported to the Safety <strong>and</strong> Quality Committee.<br />
• The Medical Director will take over the role as Chief Clinical Information Officer <strong>and</strong> a<br />
dedicated Freedom of Information Manager has been appointed to address the backlog<br />
of Freedom of Information requests.<br />
28. Work is being carried out by all areas holding key Information Governance roles. The CARE<br />
QUALITY COMMISSION report following the recent routine inspection has highlighted immediate<br />
issues to be addressed. Operational Information Governance incident reporting is being<br />
revamped. Metrics for Subject Access <strong>and</strong> Freedom of Information requests are now being<br />
reported. The implications of the Caldicott2 report are being considered. A long term Health<br />
Record Strategy is now in place with a vision to move to eNotes. Clear clinical leadership for<br />
Health Record Keeping has been established.<br />
7
Item 14<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
<strong>Trust</strong> Seal<br />
Board Secretary<br />
Director of Governance<br />
Board Secretary<br />
Purpose<br />
The purpose of this report is to update the Board on the use of the <strong>Trust</strong>’s<br />
Seal.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
In accordance with the <strong>Trust</strong>’s St<strong>and</strong>ing Orders, the <strong>Trust</strong> Board receives regular quarterly<br />
updates on the use of the <strong>Trust</strong>’s Seal. The last report covered the three months ended 27<br />
March 2013. No documents were signed <strong>and</strong> sealed in the period 28 March 2013 to 26 June<br />
2013.<br />
•<br />
Quality Impact Assessment<br />
None.<br />
Financial Impact Assessment<br />
None.<br />
Regulatory Impact Assessment<br />
None but this report demonstrates good governance <strong>and</strong> compliance with St<strong>and</strong>ing Orders.<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to note this report.<br />
Next Steps<br />
Not applicable.
Item 15<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Safety <strong>and</strong> Quality Committee Chair’s Report<br />
Dr Mike D Williams, Safety & Quality Committee Chair<br />
Dr Mike D Williams, Safety & Quality Committee Chair<br />
Dr Mike D Williams, Safety & Quality Committee Chair<br />
Purpose<br />
This report highlights key issues considered at the Safety <strong>and</strong> Quality<br />
Meeting on the 17 June 2013 to provide assurance to the <strong>Trust</strong> Board that<br />
safety <strong>and</strong> quality governance arrangements are in place.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
The main issues discussed at the meeting were:<br />
•<br />
•<br />
1. Theatre Safety<br />
Following the CQC communication about Theatre safety, the committee received<br />
assurance from the Chief Executive <strong>and</strong> Director of Nursing that the Theatre Safety<br />
Improvement Plan had been subject to rigorous external review by the <strong>Trust</strong><br />
Development Authority. Further actions are in h<strong>and</strong> to ensure the implementation of the<br />
plan, particularly around the scheduling of theatre lists.<br />
2. Outpatient backlog<br />
The Committee considered a report detailing the work done to risk assess the outpatient<br />
backlog in ophthalmology. Further actions have now been requested to ensure that a<br />
similar risk assessment is undertaken for other specialties. It is apparent that there is<br />
insufficient capacity in a number of specialties to meet both the current dem<strong>and</strong> <strong>and</strong><br />
eliminate the backlog of patients. The risks associated with this situation need to be<br />
considered by the <strong>Trust</strong> Board in partnership with commissioners.<br />
3. Maternity services<br />
The Committee received assurance from the Royal College of Obstetricians <strong>and</strong><br />
Gynaecologists’ Report on patterns of maternity care in English hospitals.<br />
4. Mortality data<br />
The Committee took assurance from the hospital st<strong>and</strong>ardised mortality ratio, which<br />
provides data about hospital mortality, that the current rate remains at around 20% less<br />
than it could be expected. Similarly, the Committee received assurances from the<br />
hospital mortality indicator, which provides data on deaths up to 30 days following<br />
hospitalisation, that the rate is around 7% less than could be expected. However, the<br />
Committee requested that consideration be given as to how to reduce further the<br />
mortality rate, especially for patients admitted over the weekend.<br />
5. Serious incident W33081/W33105 – action plan report<br />
The Committee considered a range of issues resulting from this report. The general<br />
learning point was made about the necessity for the terms of reference for serious
Item 15<br />
incident investigations to be clearly established <strong>and</strong> timeframes set to ensure issues are<br />
addressed more rapidly than had been in this case.<br />
6. Health Records Action Plan<br />
The Committee received a detailed report about actions being undertaken to meet the<br />
required st<strong>and</strong>ards, which provided limited assurance. It is recognised that the<br />
complexity of some of the issues means that full implementation of the plan will require<br />
further work.<br />
The minutes of the meeting are attached at Annex 1.<br />
Quality Impact Assessment<br />
All issues discussed have potential to negatively impact on the quality of care provided.<br />
Financial Impact Assessment<br />
To be considered, where relevant.<br />
Regulatory Impact Assessment<br />
Relevant to all essential st<strong>and</strong>ards <strong>and</strong> outcomes.<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to:<br />
1. Take assurance that suitable governance arrangements are in place for safety <strong>and</strong> quality<br />
issues addressed by the Committee.<br />
2. Decide how to assess <strong>and</strong> except a degree of risk relating to the outpatient backlog with<br />
commissioners.<br />
Next Steps<br />
The Committee will continue to provide the Board with regular reports on its activities to provide<br />
assurance that we are providing safe, effective <strong>and</strong> personal care to our patients.
Safety & Quality Committee<br />
Item 15, Annex 1<br />
Monday 17 th June 2013<br />
Maternity Seminar Room, Level 5<br />
Draft Minutes<br />
Chair: Mike Williams (MW) Non-Executive Director – Chairman<br />
Present: Lee Budge (LB) Director of Governance<br />
Greg Dix (GD)<br />
Chief Nurse<br />
Ann James (AJ)<br />
Chief Executive<br />
Alex Mayor (AM)<br />
Medical Director<br />
Margaret Schwarz (MS) Non-Executive Director<br />
Denis Wilkins (DW)<br />
Non-Executive Director<br />
In Attendance: Richard Best (RB) Deputy Director of Operations<br />
Jayne Glynn (JG)<br />
Patient Experience Manager<br />
Debs Hounsome (DH) Acting Officer Comm<strong>and</strong>ing Nursing<br />
Invited members: Kylie Glynn (KG) (Minutes) Healthcare Governance Facilitator<br />
Kevin Marsh (KM) (Item 10) Deputy Chief Nurse<br />
Sue Stock (SS) (Item 11) Head of Midwifery<br />
Anne Bussell (AB) (Item 12) Health Records Advisor<br />
1. Welcome <strong>and</strong> Apologies Action<br />
The Chair welcomed Committee members to the meeting.<br />
The Committee noted apologies from Kevin Baber, Amelia Brooks, Clare Cotter, Sue<br />
Kelley, Paul McArdle <strong>and</strong> Julie Morgan.<br />
Richard Best attended the meeting on behalf of Kevin Baber.<br />
2. Minutes <strong>and</strong> Matters Arising<br />
Minutes of the previous meeting were agreed as a true <strong>and</strong> accurate record.<br />
The Chair asked if the Personal, Safe <strong>and</strong> Effective Care Groups were going to be<br />
merged <strong>and</strong> whether a single report would be presented at future meetings.<br />
LB explained the groups would not be merging imminently as there are significant work<br />
streams being reported through them <strong>and</strong> the detail needs to be discussed at subcommittee<br />
level. When service lines have been agreed the quality governance meeting<br />
structures will be reviewed again. GD highlighted concerns regarding the removal of the<br />
sub-committee care groups as governance frameworks within the directorates <strong>and</strong><br />
service lines is currently very poor therefore, adequate assurance of action could not be<br />
provided.<br />
LB informed the Committee that additional discussions have taken place around<br />
combining the Safe <strong>and</strong> Effective Care Group, which would then be chaired by AM <strong>and</strong><br />
then have a Patient Experience Forum chaired GD. need to be clear about what we need<br />
these groups to do. AJ highlighted the importance of clarifying what the roles of these<br />
groups would be <strong>and</strong> what the Committee would like them to focus on.<br />
AM explained that in the past directorates have depended on the overarching<br />
governance structure <strong>and</strong> the culture must change so that they underst<strong>and</strong> they are<br />
responsible for implementing actions <strong>and</strong> providing assurance. The Chair noted the<br />
Committee can be used to hold relevant leads to account.<br />
S&Q Draft Minutes June 13 Page 1 of 7
Item 15, Annex 1<br />
3. Review of Action Table<br />
Assurance Framework – VTE Risk Assessment<br />
Update on VTE risk assessment figures included within Safe Care report. Action closed.<br />
Safe Care Report – Additional Information<br />
Breakdown of serious, significant <strong>and</strong> moderate incidents included within report. Detail<br />
regarding themes to be included from July 2013.<br />
AB<br />
Follow-up Backlogs – IPAM Report<br />
Update regarding follow-up backlogs presented to the IPAM meeting on 30 th May 2013.<br />
Action closed.<br />
Follow-up Backlogs – Coding System<br />
Meeting with final directorate at the end of the week to discuss the coding systems.<br />
Issues to be dealt with separately by the relevant leads. Action closed.<br />
Review of Consultant Clinical Practice<br />
Relevant paper reviewed <strong>and</strong> disseminated to Non-Executive Directors. Action closed.<br />
4. Messages from the Board <strong>and</strong> Sub-Committees<br />
The Chair informed the Committee that the Board would like clarity on the patient safety<br />
measures that will be used throughout the organisations <strong>and</strong> how these will link to the<br />
overarching quality strategy, improvement plan <strong>and</strong> governance arrangements. Although<br />
these plans will evolve with time the Committee must ensure that governance<br />
arrangements link with improvement. There needs to be assurance that continual<br />
improvements are being made as well as the right boxes being ticked.<br />
AJ explained that GD, AM <strong>and</strong> KM are currently reviewing the structure of the quality<br />
team to ensure it aligns with service improvement. Clear accountability will also be<br />
identified. There needs to be a step change as there are strong reporting mechanisms in<br />
place however processes for implementing timely changes need to be established. The<br />
Chair added that the pressure to demonstrate improvements has increased significantly<br />
since the publication of the Francis report.<br />
The Committee noted that the <strong>Trust</strong> had received a draft report from the CQC visit<br />
conducted in April 2013 <strong>and</strong> the findings were currently being considered.<br />
Implementation of the updated theatre safety action plan has continued to ensure the<br />
concerns that have been raised as a part of the informal feedback are addressed. AJ<br />
explained that a warning notice on surgical safety had been issued to the <strong>Trust</strong> on Friday<br />
14 th June 2013. GD had met with the TDA to explain the detailed action plan in place <strong>and</strong><br />
AJ would be meeting with key staff members to ensure operating list scheduling issues<br />
were resolved rapidly.<br />
5. Weekend Mortality Rates<br />
The Chair highlighted concerns regarding the difference in the mortality rate between<br />
week days <strong>and</strong> weekends within the <strong>Trust</strong>. Data has been presented on page two of item<br />
6, appendix 1. Although this is not uncommon within <strong>Trust</strong>s across the country it is an<br />
issue that should be considered so that improvements can be made.<br />
AM explained that the rates reflect how working systems are currently set-up within the<br />
<strong>Trust</strong> for example, the workforce planning profile focuses on elective services which are<br />
performed during weekdays. This is currently being reviewed to ensure senior<br />
consultants <strong>and</strong> surgeons are in the <strong>Trust</strong> during the weekend. Lack of senior clinical<br />
support is a problem in all areas across the <strong>Trust</strong> <strong>and</strong> is not prevalent within any one<br />
particular department however; this may cause more issues within emergency services.<br />
Work is also ongoing with services in the community <strong>and</strong> peninsula to ensure patients<br />
who are unwell are not transferred to hospital because services in the community are not<br />
currently available at the weekend.<br />
S&Q Draft Minutes June 13 Page 2 of 7
Item 15, Annex 1<br />
RB noted that whilst 7 day working for consultants is currently being considered other<br />
changes can be made to improve the mortality rate at the weekends. For example, if<br />
phlebotomy services coincided with ward rounds there would not be a 24 hour delay in<br />
obtaining results, during which time patients can deteriorate rapidly.<br />
The Chair asked the Committee to consider what changes to drive improvements can be<br />
made within the next 6-12 months. Although this issue cannot be resolved in its entirety<br />
within this timeframe particular elements can be focused on. These can then be included<br />
within the <strong>Trust</strong>’s safety improvement plan.<br />
AM<br />
6. Effective Care Report<br />
The Committee noted the content of the report which focuses on the follow-up backlogs<br />
<strong>and</strong> compliance with NICE Guidance. Capacity for clinical audit within the <strong>Trust</strong> was<br />
highlighted as being particularly small for an organisation of this size. As a result AM <strong>and</strong><br />
GD are discussing how this can be incorporated within the governance quality team.<br />
Follow-up Backlogs<br />
The Chair informed the Committee the Non-Executive Directors were particularly<br />
disappointed with lack of progress in reducing the outpatient follow-up backlog. It would<br />
appear that significant time is being spent trying to complete risk assessments within<br />
each directorate <strong>and</strong> there is not enough focus on resolving the backlog.<br />
RB explained there are significant capacity problems as additional funds to clear the<br />
backlog of patients are not available within the commissioning contract. This is trying to<br />
be done in addition to delivering a normal service. Changes to pathways need to be<br />
made to prevent this from being an ongoing issue in the future. We must ensure the<br />
correct patients are being added to the follow-up waiting lists for the right reason.<br />
The Chair explained risk assessments, as completed within Ophthalmology, need to be<br />
in place within all directorates <strong>and</strong> a review of which patients are being added to the<br />
waiting lists needs to be completed. AJ added that a specific plan for each specialty<br />
needs to be put in place as each backlog will need to be addressed in different ways.<br />
Issues within one area may not be relevant for another.<br />
The Chair noted that Ophthalmology remains the biggest concern particularly given the<br />
risk for some of these patients. RB assured the Committee that patients who have been<br />
identified as high risk are being dealt with as a priority <strong>and</strong> this has been incorporated<br />
within the capacity planning for this specialty.<br />
LB highlighted it was still not clear within the report where the high risk areas lie in other<br />
specialties within the report. AM explained that Paul McArdle is working with directorates<br />
to ensure a breakdown of the risk, as included within appendix 2 for Ophthalmology, is<br />
available for all directorates. Report on progress to be brought to the next meeting<br />
The Chair summarised that there appear to be continual issues in reducing the follow-up<br />
backlog due to the lack of capacity however; high risk patients within all directorates will<br />
be identified so that these can be treated as a priority. In addition, service line leads will<br />
need to develop local action plans to demonstrate how the overall backlog can be<br />
reduced <strong>and</strong> how pathways for adding patients to follow-up waiting lists will be reviewed.<br />
PMc<br />
KB<br />
7. Personal Care Report<br />
GD presented the Personal Care Report to the Committee <strong>and</strong> highlighted the following<br />
key points –<br />
• Publication of results for key performance measures will be reviewed so that the<br />
trend analysis for each measure can be reviewed <strong>and</strong> provide additional assurance<br />
• PALS <strong>and</strong> complaint rates have remained relatively stable during the past five<br />
months except for the spike in the number of complaints received in April 2013<br />
GD/JG<br />
S&Q Draft Minutes June 13 Page 3 of 7
Item 15, Annex 1<br />
• Top three issues raised through PALS remain as communication, inpatient delays<br />
<strong>and</strong> outpatient delays. Although communication remains a top theme there are no<br />
particular areas of concern that could be addressed which would show an<br />
improvement in the overall figures of these issues<br />
• A particular piece of work in relation to communication is being completed with those<br />
who are visually <strong>and</strong> hearing impaired so that feedback can be used to drive<br />
improvements for these care pathways. AJ suggested doing the same with patients<br />
who suffer with learning difficulties<br />
• The FFT response continues to improve <strong>and</strong> run charts will be included within the<br />
report from next month. The <strong>Trust</strong> is currently achieving a response rate of 13.5%.<br />
Some wards have achieved a 40-50% response rate whilst others have only<br />
achieved 4%. Implementation of FFT within good performing areas will be shared to<br />
ensure the response rates are increased.<br />
The Chair noted that a significant number of the PALS <strong>and</strong> complaints received within<br />
the <strong>Trust</strong> relate to the Gastroenterology, Surgery <strong>and</strong> Renal directorate. JG explained the<br />
key issues within this area relate to patient access to treatment for example, a number of<br />
patients are informed they will be reviewed within 4-6 weeks but the waiting list within the<br />
directorate is 12 weeks at that stage. RB noted that there is a strong correlation to the<br />
follow-up backlog as this directorate account for half of the admitted follow-up backlog.<br />
The Committee took assurance from the content of the report <strong>and</strong> asked that actions<br />
were taken to reduce the PALS <strong>and</strong> complaint levels in Surgery.<br />
JG<br />
8. Safe Care Report<br />
AM presented the Safe Care Report to the Committee <strong>and</strong> highlighted the following key<br />
points –<br />
• The HSMR <strong>and</strong> SHMI data demonstrates the <strong>Trust</strong> is maintaining good rates<br />
• In February 2013 VTE cases were identified <strong>and</strong> each patient had received the<br />
appropriate treatment, although 93% of these cases received the appropriate risk<br />
assessment<br />
• The four yearly GTT report shows there has been a continual reduction in harm<br />
caused to patients. Areas identified consistently with top three areas of harm are<br />
wound infections, pressure ulcers <strong>and</strong> hospital acquired pneumonia. All of these are<br />
currently being addressed through ongoing work programmes<br />
The Chair asked whether specific improvement areas from the Regional Patient Safety<br />
Initiative will be incorporate within the overarching quality improvement action plan. AM<br />
explained that service line leads will be expected to lead on particular improvements<br />
however, <strong>Trust</strong> wide issues will be monitored at sub-committee or committee level. GTT<br />
is an indicated of where the efforts of the Trist must be focused.<br />
The Chair highlighted inpatient falls as a particular issue <strong>and</strong> explained that a particular<br />
piece of work regarding intentional rounding was completed at RD&E Hospital <strong>and</strong> this<br />
appeared to have a significant impact on the number of falls. GD added that the<br />
implementation of intentional rounding was re-launched at Taunton hospital as it became<br />
a tick box exercise. Within two years of this re-launch there was a 30% reduction in the<br />
number of inpatient falls. The Chair emphasised the importance of ensuring this is<br />
implemented properly within the <strong>Trust</strong> <strong>and</strong> that there is culture change. For this to<br />
happen within the hospital there needs to be clear leadership. GD <strong>and</strong> DH are working<br />
on getting intentional rounding used within the <strong>Trust</strong> which will reduce falls <strong>and</strong> improve<br />
nursing care.<br />
GD/DH<br />
9. Assurance Framework<br />
LB presented a new Quality Assurance Framework to the Committee <strong>and</strong> asked for their<br />
comments <strong>and</strong> whether any risks were felt to be missing.<br />
The Committee asked that the following comments <strong>and</strong> risks were incorporated within<br />
the framework –<br />
S&Q Draft Minutes June 13 Page 4 of 7<br />
LB
Item 15, Annex 1<br />
• Include additional columns to show what evidence would need be provided to<br />
demonstrate assurance that risks were being adequately managed<br />
• Consider how complexity of resolving issues <strong>and</strong> associated risks can be<br />
incorporated<br />
• Diagnostic reporting to be included as a key risk<br />
• AJ asked that sharing of information reported on Datix <strong>and</strong> STEIS with Executive<br />
Directors is considered for inclusion<br />
Inclusion of medical staffing was discussed however, AM assured the Committee that<br />
this issue was being addressed with service line leads.<br />
The Chair explained that the overall risk assessment <strong>and</strong> assurance framework is due to<br />
be presented to SMT <strong>and</strong> the Board in July 2013 <strong>and</strong> once agreed this will determine the<br />
focus of the Committee.<br />
The Committee agreed to the content of the Assurance Framework subject to the<br />
suggestions listed above.<br />
10. Serious Incident W33081 / W33105 – Action Plan Report<br />
KM presented the serious incident action plan to the Committee following an<br />
independent review of the case. The following key points were highlighted –<br />
• The external investigation looked into the process behind the internal investigation,<br />
access to relevant notes, IT support within the community <strong>and</strong> reporting mechanisms<br />
surrounding Glucose Tolerance Test (GTT) results<br />
• Of the 22 recommendations made, 20 have been implemented <strong>and</strong> the remaining 2<br />
will take some time as they depend on IT support. 12 of the 33 areas in which care is<br />
provided within the Community have poor IT access therefore, if this cannot be<br />
improved the locations will be changed<br />
• Evidence of the recommendations implemented has been provided. The way in<br />
which this has been done will be used for all RCA reports completed within the <strong>Trust</strong><br />
• The first RCA report that was completed focused on the delivery <strong>and</strong> resuscitation of<br />
the infant however, the key issues related to the reporting of GTT results<br />
• GP surgeries were found to be reporting GTT results differently therefore SS worked<br />
to have this st<strong>and</strong>ardised <strong>and</strong> the PCT have confirmed that set parameters are now<br />
in place<br />
• Two b<strong>and</strong> 2 posts within maternity would provide the support required to manage<br />
GTT results within the <strong>Trust</strong> however, recent funding for this roles was removed but<br />
discussions to address this are ongoing<br />
• Considerable learning from the case has been highlighted <strong>and</strong> shared with the<br />
relevant teams<br />
• Terms of reference for investigations, including external, will be put in place to ensure<br />
all staff involved in the case receive the appropriate support<br />
• The case had been referred to the NMC <strong>and</strong> following a review they do not feel there<br />
are any additional issues that need to be followed-up<br />
• Case will be presented to the Child Death Panel <strong>and</strong> the initial RCA report, external<br />
investigation report <strong>and</strong> action plan report will be presented<br />
The Chair asked what the timeframes were surrounding this case. KM explained the<br />
incident occurred approximately two years ago. There were significant delays in finalising<br />
the investigation report <strong>and</strong> issues regarding GTT had not been identified. Lessons about<br />
how the investigation was set up <strong>and</strong> conducted had been learnt. SS added this<br />
investigation was completed outside of the specialty therefore a number of elements had<br />
to undergo an additional review. All incident <strong>and</strong> complaint investigations are now<br />
completed within the directorate by those who are independent of the specific case.<br />
AJ highlighted the importance of clarifying who will be responsible for completing an<br />
investigation, within what timeframe, with the involvement from whom <strong>and</strong> what the brief<br />
is. It is essential these elements are included within the Terms of Reference.<br />
S&Q Draft Minutes June 13 Page 5 of 7
Item 15, Annex 1<br />
The Chair asked SS to ensure timeframes for looking for alternative solutions to the IT<br />
issues is agreed so that progress can be made if the initial recommendations cannot be<br />
implemented. Further update regarding these timeframes <strong>and</strong> evidence of imbedded<br />
actions to be discussed at the Safe Care Group in six months’ time.<br />
SS<br />
11. RCOG Report on Patterns of Maternity Care in English <strong>Hospitals</strong><br />
SS presented the RCOG report to the Committee <strong>and</strong> explained this is the first issue of<br />
the report. Although the first report for all <strong>Trust</strong>s has been anonomised this will be<br />
changed for future reports so that results can be compared <strong>and</strong> used for bench marking.<br />
The following key points were highlighted –<br />
• 11 areas of practice were chosen for the review <strong>and</strong> there were 19 relevant criteria<br />
• The <strong>Trust</strong> was performing above the mean in 17 of these criteria<br />
• Format of data clarified. Both lower <strong>and</strong> higher scores can be positive results<br />
• The key issues related to the disparity in management of a patient on the same care<br />
pathway. These pathways have been refined <strong>and</strong> clear st<strong>and</strong>ards have been put in<br />
place therefore improvements should be reflected within future reports<br />
• Areas of disparity that have been addressed will be audited to ensure the changes<br />
have been imbedded<br />
• The <strong>Trust</strong>’s caesarean section rate is consistently 4-5% lower than the national<br />
average however, research that is now available suggests that if a midwifery lead unit<br />
was available this could be improved even further as patients who deliver in an<br />
obstetric led unit are four times more likely to undergo a caesarean section<br />
AM asked how this information triangulates with other data that is available. SS<br />
explained that when the data is reviewed in line with best practice set by other<br />
organisations it helps clarify how the <strong>Trust</strong> should be performing. For example 2.1% of<br />
patients who deliver at Derriford Hospital suffer a third or fourth degree tear however,<br />
best practice suggests that a rate below 4% could demonstrate that these tears are not<br />
being identified <strong>and</strong> therefore patients are not receiving the adequate treatment.<br />
The Committee noted the content of the report.<br />
12. Health Records Action Plan<br />
AB presented the Health Records Update Report to the Committee <strong>and</strong> highlighted the<br />
following key points –<br />
• Meeting held with AM <strong>and</strong> he has now been identified as the clinical lead for records<br />
• Letter sent to all service line leads explaining their responsibilities including the need<br />
for annual case note training <strong>and</strong> audits<br />
• A new working group has been established to discuss how improvements can be<br />
made to the paper records<br />
• A presentation regarding electronic notes was presented to the MEC <strong>and</strong> a significant<br />
amount of support has been offered. Currently awaiting approval of funding before<br />
this can be progressed any further<br />
• Significant progress has been made in relation to the transportation of notes.<br />
Maternity have not yet identified a space where blue boxes can be delivered <strong>and</strong><br />
stored however, if this not agreed by the end of June 2013 all notes will be delivered<br />
to the level 3 storage room<br />
• MAU looking to use a fixed storage space for notes on the ward as opposed to<br />
lockable trolleys due to space issues. Lynher ward have also opted to store notes in<br />
lockable office<br />
S&Q Draft Minutes June 13 Page 6 of 7
Item 15, Annex 1<br />
• Concerns raised via ‘ask Ann’ regarding departments not tracing notes. This will now<br />
be included as a performance indicator for each directorate to ensure poor<br />
performing directorates are addressed<br />
• Case note training is ongoing <strong>and</strong> 140 members of staff have been trained. The<br />
training has been followed-up by an audit <strong>and</strong> it has demonstrated that the training<br />
has had the impact required<br />
• 50,000 pieces of loose notes have now been filed which is approximately 25% of all<br />
filing that needs to be completed<br />
• A pilot for sending paper to filing service at Bush Park will be piloted by Neurology in<br />
July 2013<br />
LB highlighted that concerns regarding overheard discussions of patient information <strong>and</strong><br />
notes left on the nurses’ station were raised by the CQC. AB explained that issues<br />
regarding discussions on the telephone will be picked up through training being provided<br />
by the information governance team by demonstrating scenarios <strong>and</strong> use of lockable<br />
should improve issues relating to notes left at the nurses’ stations.<br />
The Committee took assurance that progress that had been made <strong>and</strong> recognised the<br />
hard work it had taken to achieve this <strong>and</strong> the challenges that remain.<br />
13. Communication<br />
The Chair listed the following key points for onward communication to the <strong>Trust</strong> Board –<br />
• Updated Theatre Safety Action Plan has continued to be implemented as planned<br />
• Risk assessment for follow-up backlog within Ophthalmology will be completed for all<br />
directorates so that high risk patients can be dealt with as a priority<br />
• The <strong>Trust</strong> continues to maintain a good mortality rate however, the difference in the<br />
rate between week days <strong>and</strong> weekend will be reviewed in further detail<br />
• A number of key learning points from external review regarding investigation<br />
processes will be incorporated within investigation terms of reference<br />
• RCOG report shows Maternity unit within the <strong>Trust</strong> is performing above the mean rate<br />
within 17 of the 19 relevant criteria considered<br />
• Good progress made with implementation of the health records action plan <strong>and</strong><br />
Committee noted particularly difficult implementation points within the plan<br />
14. Review <strong>and</strong> Learning<br />
The Chair informed the Committee that meetings will be held on a bi-monthly from July<br />
2013.<br />
LB suggested that performance reports regarding key issues should be included on the<br />
agenda for review.<br />
Date <strong>and</strong> time of next meeting<br />
Monday 15 th July 2013 – 12:30, Maternity Seminar Room (Lv 5)<br />
S&Q Draft Minutes June 13 Page 7 of 7
Item 16<br />
COMMITTEE MINUTES<br />
Finance, Performance & Investment Committee (FPIC)<br />
Date 22 nd May 2013<br />
Location Room 2 DHLC<br />
Attendees<br />
Ian Douglas, (Chairman)<br />
Keith Chapman, Assistant Director of Operations (ADoO)<br />
David Cooper, Project Accountant (PA)<br />
Annie Cornelius, Senior Matron (SM)<br />
Phil Hughes, Assistant Medical Director (AMD)<br />
Brian Jones, Associate Director of Finance (AsDoF)<br />
David Killoran, Interim Deputy Director of Finance (IDDoF)<br />
Elizabeth Raikes, NED (ER)<br />
Dan Stevens, Deputy Head of Performance (DHoP)<br />
Joe Teape, Director of Finance (DoF)<br />
Nick Thomas, Director of Planning & Site Services (DoPSS)<br />
Henry Warren, Associate NED (HW)<br />
Jenny Waycott, Contract Manager (CM)<br />
Michelle Smith, Executive Office Team Leader (MS) – minutes<br />
Corporate & Committee Affairs<br />
44/13 Welcome <strong>and</strong> apologies<br />
The apologies were noted as above.<br />
Apologies<br />
Kevin Baber, Chief Operating Officer (COO)<br />
Richard Best, Director of Operations (DoO)<br />
David Brown, Assistant Director of Operations<br />
(ADoO)<br />
Lee Budge, Director of Governance (DoG)<br />
Greg Dix, Director of Nursing (DoN)<br />
Ann James, Chief Executive (CE)<br />
Alex Mayor, Medical Director (MD)<br />
The Chairman introduced Henry Warren to the Committee, who had recently joined the <strong>Trust</strong><br />
as an Associate Non-Executive Director.<br />
45/13 Minutes <strong>and</strong> matters arising from the previous meeting<br />
The minutes of the last meeting were agreed as a true <strong>and</strong> accurate record. There were no<br />
matters arising.<br />
46/13 Action update<br />
• Business planning 13/14<br />
Further update to be provided to the <strong>Trust</strong> Board via finance paper but this was likely to<br />
attract some media interest.<br />
• Contract Penalties<br />
No formal response had been received from the Commissioners but as the contract had<br />
been agreed <strong>and</strong> signed <strong>and</strong> both organisations had submitted accounts it would be<br />
assumed that there was no liability.<br />
• Budgetary control policy<br />
Update due next meeting but the DoF updated the Committee on plans to introduce a<br />
comprehensive developmental programme both for the finance team <strong>and</strong> the wider<br />
organisation, encouraging a culture of financial management throughout.<br />
• DV Valuation<br />
The DoF tabled an update from the Financial Management Accountant which outlined<br />
the methods <strong>and</strong> processes used in the valuation of assets. The DoF would provide a<br />
further update on the challenges <strong>and</strong> the effect of annual dividend at the next meeting of<br />
the Committee. The DoF <strong>and</strong> DoPSS would also look at ways of improving the<br />
relationship with the District Valuer.<br />
• Assurance Framework<br />
This item did not feature on the agenda as the framework was currently being updated<br />
by the DoG, but updates noted at the previous Committee meeting would be<br />
incorporated into the new version.<br />
• Best Practice Tariffs<br />
DoF/<br />
DoPSS<br />
1
Although it was agreed at the last meeting of the Committee that a paper would be<br />
received instead a contact update had been presented, with more information on Best<br />
Practice Tariffs to be presented in June.<br />
47/13 Messages from the Board <strong>and</strong> other Committees<br />
There were no messages from the Board or other Committees.<br />
48/13 Review of Investment Panel minutes<br />
The May meeting of the Investment Panel had taken place the previous day so minutes were<br />
not yet available. The DoPSS highlighted the key issues discussed as the capital<br />
programme, the e-prescribing project <strong>and</strong> the replacement gamma cameras. He also<br />
reported that the terms of reference <strong>and</strong> membership of the group had been reviewed in light<br />
of the implementation of the Care Group Structure, <strong>and</strong> the newly appointed Care Group<br />
Directors would be invited to attend future meetings.<br />
Finance & Performance<br />
49/13 Operational Performance Review<br />
The full performance report was not yet available for review but the DHoP tabled the<br />
Monitor Governance Risk Rating scorecard for month 1, <strong>and</strong> highlighted key areas for<br />
discussion:<br />
• The Monitor Governance Risk Rating was 4 (red) for month 1.<br />
• 62 day cancer – both failed in M1 <strong>and</strong> screening target failed in last 7 out of 8<br />
quarters, meaning that Monitor could choose to apply an override.<br />
• A&E 4 hour – failed in M1 due to difficulties with flow.<br />
• C-Difficile – Monitor target set at 25 for the year, although this would again be<br />
straight-lined. The DHoP believed that no cases were reported in M1.<br />
• RTT – Admitted <strong>and</strong> Incomplete pathway targets both failed. The DHoP highlighted<br />
that any failure of the incomplete pathway target would result in the failure of the<br />
entire quarter. Therefore there was an opportunity to focus on treating the longest<br />
waiting patients first which would hopefully bring performance to a sustainable<br />
position for quarter 2.<br />
The ADoO highlighted the reasons for failure including cancellation of elective surgery due<br />
to an increase in non-elective activity <strong>and</strong> also noted the work of the DoO with the cancer<br />
teams to improve performance, particularly in 3 sub-specialties. The Committee discussed<br />
the impact of GP working patterns which could result in a notable increase in pressure on<br />
emergency services, <strong>and</strong> ER felt that this should be noted/diarised so that the<br />
Commissioners could be challenged accordingly.<br />
Item 16<br />
The DoF agreed to discuss with the COO formalising a monthly response from the <strong>Trust</strong> to<br />
the Commissioners <strong>and</strong> for the purpose of audit trail. Also the DoF <strong>and</strong> COO, with the<br />
support of senior performance team, would discuss the development of a plan to address<br />
the RTT issues that would include a clear correlation between waiting lists, activity <strong>and</strong> the<br />
finances required each month to deliver, <strong>and</strong> when it would be expected to achieve. This<br />
plan would be agreed by FPIC before approval by the <strong>Trust</strong> Board<br />
DoF<br />
DoF<br />
50/13 Financial Performance Review<br />
The AsDoF presented the financial update for month 1. Key areas discussed were as<br />
follows:<br />
• Annual <strong>and</strong> income <strong>and</strong> expenditure plans were reviewed <strong>and</strong> the month 1 position<br />
was noted to be slightly better than planned.<br />
• The Committee noted the overspend in month 1 <strong>and</strong> ER expressed concern that<br />
there was no detail on how much of this was planned or unplanned. The DoF <strong>and</strong><br />
IDDoF explained that a meeting had been arranged for later in the week to review<br />
existing arrangements <strong>and</strong> plan a more formalised process, ensuring a greater level<br />
of detail <strong>and</strong> visibility for future meetings.<br />
• The AsDoF updated the Committee on the performance of the variable contract, in<br />
particular Neuro <strong>and</strong> Cardiac Surgery. He outlined the current positions of income,<br />
2
Item 16<br />
pay <strong>and</strong> staffing, highlighting that medical agency/locum spend was still of concern,<br />
in the main due to junior doctor cover issues. The Committee expressed concern<br />
that junior doctor movements/changeover had not been planned for when they were<br />
expected at this point in the year. The DoF agreed to discuss with the MD who was<br />
already undertaking work on this, <strong>and</strong> an update would be requested for the <strong>Trust</strong><br />
Board to include the scale of the problem, the options available <strong>and</strong> the potential<br />
impact on patients if not addressed.<br />
• The Committee also noted the current position of Private Patients, Research <strong>and</strong><br />
Development <strong>and</strong> non-pay expenditure. The DoF noted the agreement with<br />
Commissioners that any over or under spend on drugs would be split 50% with the<br />
<strong>Trust</strong>. This had not been anticipated so the full year impact had not been included<br />
in the plan. The DoF confirmed that he would be<br />
• The Committee discussed the current discretionary spend <strong>and</strong> the actions in place<br />
to reduce it. The DoF reported that there was a reserve of £4m for discretionary pay<br />
but spend from this would only be approved by well managed areas in exceptional<br />
circumstances. Directorates had been asked to map out workforce plans for the<br />
year <strong>and</strong> alongside the controls plan in place, it was expected that spend would<br />
come down.<br />
• The AsDoF presented the month 1 CIP summary, outlining the actual <strong>and</strong> planned<br />
savings, although these had not been risk assessed. It was expected that once risk<br />
assessed, planned savings would be between £19-22m, so further work was<br />
required to reach the target of £24m. Currently £12m of this could be comfortably<br />
achieved. The Committee discussed the importance of finding recurrent savings.<br />
The DoF advised that only one off large items would be accepted as non-recurrent<br />
<strong>and</strong> other savings identified previously such as slipped vacancies would instead be<br />
classed as underspend. The AsDoF reported that the policy was still in the process<br />
of being implemented <strong>and</strong> the forecast would be refreshed once this was in place,<br />
with some CIPs reclassified as underspend.<br />
The Chairman requested that future updates included a split of planned recurrent<br />
<strong>and</strong> non-recurrent savings. The Committee endorsed the approach <strong>and</strong> agreed to<br />
review the CIP savings programme in detail at next month’s meeting.<br />
• The AsDoF concluded his presentation by briefly updating the Committee on the<br />
cash position <strong>and</strong> the Capital Programme. The Committee noted that the Monitor<br />
financial risk rating was 2 <strong>and</strong> was likely to remain so for the year which would<br />
impact on the <strong>Trust</strong>’s Foundation <strong>Trust</strong> application as a minimum of 3 was required.<br />
DoF<br />
DoF<br />
51/13 2013/14 Contract update<br />
The CM updated the Committee on key developments of the existing contract deal with the<br />
Commissioners <strong>and</strong> the planning for 2014/15:<br />
• The agreed contract value was improved on the previous year at £353.2m.<br />
• A managed PbR contract had been agreed, removing almost all significant financial<br />
risk to the <strong>Trust</strong>. Never events, single sex accommodation breaches <strong>and</strong> MRSA<br />
bacteraemias could still attract penalties but these were not felt to be high risk. The<br />
Committee discussed the benefits of a managed PbR contract <strong>and</strong> the other types<br />
of contracts available, <strong>and</strong> the contracting process.<br />
• The CM outlined the variable elements of the contract <strong>and</strong> highlighted successful<br />
investments.<br />
• Major sticking points in negotiations were non-elective activity, follow up backlog,<br />
the definition of admission/consultant to consultant referrals <strong>and</strong> CQUINs. The CM<br />
explained that the <strong>Trust</strong> felt that CQUIN should be paid on the whole contract value<br />
including pass-through. National guidance was being sought <strong>and</strong> if successful this<br />
could mean an additional £1m from commissioners. The Committee noted that the<br />
CQUIN milestones were still to be confirmed.<br />
• Work was underway to forward plan for the 2014/15 contracting process, although<br />
the CM highlighted that there were outside influences beyond the <strong>Trust</strong>’s control<br />
which would need to be accounted for later.<br />
• The implementation of the new Care Group structure would be key as teams would<br />
be able to develop strategic aims, highlight issues <strong>and</strong> work with the contracting<br />
teams to negotiate with commissioners. The Committee discussed engagement<br />
3
Item 16<br />
<strong>and</strong> involvement of clinicians, which had been patchy in the past.<br />
• The Committee recognised the challenge of the whole health community <strong>and</strong> the<br />
need to take cost out of the system <strong>and</strong> ensure that it is sustainable. However the<br />
Chairman highlighted the importance of ensuring the <strong>Trust</strong> negotiates the best deal<br />
possible.<br />
• The CM highlighted the importance of retaining specialist services <strong>and</strong> ensuring<br />
stability through maximum take during 2013/14. The Committee discussed the<br />
involvement of the Specialised Commissioning Group which made up around 30%<br />
of the contract value.<br />
• There were some issues with the system that collected data on activity which<br />
needed to be resolved.<br />
• The Committee noted the contract deal for 2013/14. The Committee requested a<br />
further update at the July Committee on the resolution of outst<strong>and</strong>ing issues, <strong>and</strong><br />
process for planning for the 2014/15 contract.<br />
• HW to meet with the CM to review the contract with the Commissioners <strong>and</strong> also<br />
the Commercial Contract Manager to discuss how the <strong>Trust</strong>’s commercial contracts<br />
could be strengthened.<br />
CM<br />
CM/HW<br />
52/13 Reference Costs<br />
The AsDoF outlined the requirement for the <strong>Trust</strong> to submit an annual return, <strong>and</strong> the<br />
national process introduced which required Committee/Board approval before the return<br />
could be submitted. It was expected that the submission will be ready for review by the<br />
accountants <strong>and</strong> directorate teams in around 2 weeks, with the submission due on 16 th<br />
July.<br />
Due to data collection issues in some areas the <strong>Trust</strong> was currently reporting a low silver<br />
st<strong>and</strong>ard on the MAQ scoring system. However it was expected that the implementation of<br />
the Care Group structure would improve the engagement of clinicians. Also the<br />
introduction of some new IT systems would increase the data available. The <strong>Trust</strong>’s index<br />
was favourable against the national average.<br />
The Committee discussed the disconnect between a favourable reference cost index <strong>and</strong><br />
the financial position <strong>and</strong> the potential reasons for this such as varying marginal rates,<br />
direct access income <strong>and</strong> educational funding arrangements. It was agreed that further<br />
work was required to underst<strong>and</strong> this in more detail <strong>and</strong> the DoF would give thought to<br />
types of assurance available such as internal/external audit <strong>and</strong> peer review.<br />
The Committee agreed to receive the submission by email for virtual approval as it was<br />
unlikely that it would be available for the June Committee meeting.<br />
DoF<br />
AsDoF<br />
Closing Issues<br />
53/13 Any other business<br />
The DoPSS highlighted that, due to concerns regarding the speed of retrieval of ‘prior’<br />
images, the PACS Board had made the decision to defer the go live date of the final phase<br />
of the project by 3 months. There will now be a series of commercial discussions with the<br />
suppliers regarding remediation. A further briefing would be brought back to the committee<br />
as those discussions develop.<br />
54/13 Communication<br />
The Chairman listed items for inclusion in the Chair’s report for the <strong>Trust</strong> Board:<br />
• Peninsula Pathology Partnership<br />
• District Valuation<br />
• Operational Performance – 18 week work due June FPIC/July <strong>Trust</strong> Board<br />
• Finance – CIP performance, comfortable on delivery of £12m against target of<br />
£24m, with a focus on recurrent savings.<br />
• Cover for Junior Doctor gaps<br />
• Contact update 213/14 – update to be brought back in July on progress against Q1<br />
objectives<br />
• Reference Costs – exercise to be undertaken to provide assurance<br />
4
Item 16<br />
• PACS contract – likely deferral of go-live date due to issues with migration of<br />
existing data.<br />
55/13 Next Meeting: 26 th June 2013, 0930 Conference Room DHLC<br />
5
Item 17<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Human Resources & Organisational Development Committee Chair’s<br />
Report<br />
Deputy Director of HR&OD<br />
NED HR&OD Committee Chair<br />
NED HR&OD Committee Chair<br />
Purpose<br />
To summarise the key issues discussed <strong>and</strong> assurances received at the Human<br />
Resources <strong>and</strong> Organisational Development Committee (HR&OD) meeting held<br />
on 14 June 2013.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
• •<br />
Executive Summary<br />
•<br />
The key issues <strong>and</strong> assurances considered by the Committee are outlined below.<br />
HR & OD Strategy<br />
The Committee received an update on the HR&OD Strategy <strong>and</strong> confirmation that it supported the<br />
Quality Improvement Strategy. In light of the new <strong>Trust</strong> Strategy, “In the Heart of Health in the<br />
Peninsula” having been approved at the June <strong>Trust</strong> Board, it was agreed that the HR&OD Strategy<br />
would be further reviewed against this <strong>and</strong> the <strong>Trust</strong>’s corporate objectives. The Committee<br />
received assurance that progress was being made with recruiting to ward vacancies but sought<br />
additional assurance on issues of retention <strong>and</strong> the position regarding medical workforce staffing<br />
levels.<br />
Staff Survey<br />
The Director of HR&OD updated the Committee that the Executive Team had agreed from the Staff<br />
Survey results, three key areas of immediate focus, in addition to directorate actions in response to<br />
the Staff Survey results. These relate to Communication; the <strong>Trust</strong> as a place to work; <strong>and</strong> the <strong>Trust</strong><br />
as a place to be treated. The Committee accepted these were the right areas of focus <strong>and</strong><br />
requested a more detailed update on how this would be achieved at the next meeting.<br />
Francis Report<br />
The Committee received a report on the key HR&OD implications arising from the Francis Report,<br />
<strong>and</strong> the associated workstreams of the <strong>Trust</strong>’s HR&OD Strategy. The Committee received<br />
assurance that the HR&OD Strategy <strong>and</strong> delivery plan had appropriate workstreams in place to<br />
respond to the recommendations. It was also acknowledged that cultural change was key, in<br />
ensuring that patients are placed at the heart of everything we do, particularly during the current<br />
time of financial challenge. The Committee agreed that the key issues were for a culture of<br />
openness to be strengthened, leadership development, correct staffing levels <strong>and</strong> retention, <strong>and</strong><br />
that lessons learnt are effectively shared to embed learning.
Item 17<br />
Terms <strong>and</strong> Conditions of Employment<br />
The Workforce QIPP Programme Manager updated the Committee on the Foundation <strong>Trust</strong><br />
Network Optimisers, <strong>and</strong> how these had been systematically reviewed <strong>and</strong> were being implemented<br />
within the <strong>Trust</strong>.<br />
It was noted that whilst some of the Optimisers did not show significant savings in the current year,<br />
this was because many of the possible actions were already being implemented <strong>and</strong> included in the<br />
<strong>Trust</strong>'s existing Workforce CIP schemes. These are subject to formal monitoring through the<br />
Programme Management Office. Other elements of the Optimisers required work this year to lead<br />
to savings in the next financial year.<br />
The Committee noted that the medical staff Optimisers were being led separately by the Medical<br />
Director, <strong>and</strong> sought assurance at a future meeting on how these were being progressed,<br />
particularly given the scale of possible savings. It was noted that it would be important to consider<br />
any unintended consequences as a result of implementing the optimisers, <strong>and</strong> engaging effectively<br />
with staff <strong>and</strong> the trade unions.<br />
Leadership Development<br />
The Committee was concerned over the potential risk to the delivery of the planned Leadership<br />
Development Programme, due to the financial position of the <strong>Trust</strong>. The Director of HR&OD<br />
confirmed that alternative plans are being considered.<br />
Assurance on the <strong>Trust</strong>’s Leadership Development <strong>and</strong> OD capability was sought, by means of a<br />
Skills Review, which the Director of HR&OD will undertake.<br />
Equality <strong>and</strong> Diversity<br />
The Committee received an update on progress being made over the delivery of the Equality<br />
Delivery System. It was noted that membership of the Equality Delivery Steering Group required<br />
stronger clinical staff representation to help ensure that the EDS objectives are delivered.<br />
The Committee supported the proposed recommendations in relation to the Board Inclusion<br />
Development Programme, which would help ensure equality <strong>and</strong> diversity is better considered in<br />
day to day decision making.<br />
The minutes of the meeting are attached at Annex 1.<br />
Quality Impact Assessment<br />
Implementation of the HR&OD Strategy will have a positive impact on quality of care.<br />
Financial Impact Assessment<br />
Increased productivity will support achievement of CIP savings.<br />
Regulatory Impact Assessment<br />
Compliance with CQC Outcomes 12,13, <strong>and</strong> 14, <strong>and</strong> Equality Objectives.<br />
Key Recommendations<br />
The <strong>Trust</strong> Board is asked to receive this report <strong>and</strong> consider if any further assurances are required.<br />
Next Steps<br />
The Committee will progress its Forward Work Programme <strong>and</strong> the emerging issues to be referred<br />
to other Board Committees will be communicated through this report.
Item 17, Annex 1<br />
MINUTES OF THE HR & OD COMMITTEE<br />
HELD ON FRIDAY 14 TH JUNE 2013 1000-1200<br />
BOARD ROOM, DHLC<br />
Attendees<br />
Chair Elizabeth Raikes Non-Executive Director (ER) Chair<br />
Martin Bamber Deputy Director of HR (MB)<br />
Carolyn Bruce- Shadow Governor<br />
(CBS)<br />
Spencer<br />
Hiu Lam Director of Medical Education (HL)<br />
Kevin Marsh Deputy Director of Nursing (KM)<br />
Anna Orrock Care Group General Manager (CSS) (AO)<br />
Sharon Russell OD Manager (SR)<br />
Hein Scheffer Director of HR & OD (HS)<br />
Nick Varney Workforce QIPP Programme (NV)<br />
Manager<br />
Sophia Wrigley Chair, HMSC (SW)<br />
Mike Williams Non-Executive Director (MW)<br />
In Attendance: Leah Brooks Equality & Diversity Lead (Service) (LB)<br />
Jayne Middleman OD Facilitator (JM)<br />
Gillian Pothecary Minutes (GP)<br />
No. Item Action Timescale<br />
28/2013 Welcome <strong>and</strong> Apologies<br />
Apologies were received <strong>and</strong> noted from:<br />
Ann James, Chief Executive<br />
Greg Dix, Director of Nursing<br />
Alex Mayor, Medical Director<br />
Lee Budge, Director of Governance<br />
Am<strong>and</strong>a Nash, Head of Communications<br />
Laura Cottey, Junior Doctor Representative<br />
Nick Thomas, Director of Site Services <strong>and</strong> Planning<br />
Martyn West, LNC Chairman<br />
• ER commented in relation to attendance, that the Board<br />
had reviewed governance <strong>and</strong> committee structures <strong>and</strong> it<br />
is intended that the HR&OD Committee will focus on the 4<br />
core workforce corporate objectives. The Terms of<br />
Reference will be reviewed at the next meeting.<br />
• Congratulations were noted in relation to the Celebration<br />
Awards, <strong>and</strong> ER thanked the Awards Steering Group for<br />
all their hard work to organise what was a very successful<br />
event.<br />
1
Item 17, Annex 1<br />
29/2013 Minutes <strong>and</strong> Matters Arising from the Previous Meeting<br />
The notes of the meeting held on 10 th April 2013 were agreed as<br />
an accurate record.<br />
SV 16/8/2013<br />
HS highlighted that the rolling action table would in future be fully<br />
completed with comments on progress.<br />
30/2013 HR&OD Strategy<br />
The Committee received an update on the HR&OD Strategy <strong>and</strong><br />
confirmation that, following a review, it supported the Quality<br />
Improvement Strategy. It was agreed that the HR&OD Strategy<br />
would be further reviewed against the new <strong>Trust</strong> Strategy, “In the<br />
Heart of Health in the Peninsula” <strong>and</strong> the <strong>Trust</strong>’s corporate<br />
objectives.<br />
MB 16/8/2013<br />
HS provided an update on actions since the last meeting. Key<br />
points included:<br />
Recruitment <strong>and</strong> ward staffing<br />
• As of 30 March 2013, the total clinical <strong>and</strong> non-clinical<br />
nurse vacancies are 179.18 WTE, including an additional<br />
36 WTE for the staffing of Monkswell. 130.15 WTE of<br />
these vacancies are currently at post-interview stage.<br />
• Steady progress was being made on recruitment,<br />
particularly for HCA’s, but it was noted that retention was<br />
also critical.<br />
• MW highlighted the need to also focus on reviewing plans<br />
to ensure adequate medical staffing levels. HS agreed,<br />
<strong>and</strong> confirmed he had arranged to meet with Yvonne<br />
Linley-Shaw, Medical Workforce Business Partner, to<br />
discuss this issue.<br />
• It was acknowledged that there is a risk when opening<br />
additional beds that medical staffing is not reviewed<br />
robustly in addition to nursing staffing levels. HL agreed,<br />
<strong>and</strong> stated that the junior doctor workforce should be<br />
reviewed within each service line. HL added that Alex<br />
Mayor, Medical Director, <strong>and</strong> Emma Rayment, Business<br />
Manager, are leading a project on junior doctor staffing<br />
levels.<br />
M<strong>and</strong>atory Training <strong>and</strong> Appraisal<br />
• It was noted that a paper on the content <strong>and</strong> delivery of<br />
m<strong>and</strong>atory training would be discussed at the next<br />
HR&OD Committee meeting. The paper would also<br />
highlight proposed changes to m<strong>and</strong>atory training<br />
reporting, where for example, historically, Junior Doctors<br />
are not included in the m<strong>and</strong>atory training figures reported.<br />
• HL stated that reports were produced in relation to JD<br />
2
Item 17, Annex 1<br />
m<strong>and</strong>atory training data, <strong>and</strong> that it should therefore be<br />
possible to incorporate them in the dashboard.<br />
Appraisal<br />
• Feedback from the <strong>Plymouth</strong> Way sessions on appraisal,<br />
show that some staff question the value <strong>and</strong> impact of the<br />
current appraisal experience. Issues raised included the<br />
time available to undertake appraisals <strong>and</strong> their impact.<br />
HS reported on the current work on a new electronic<br />
appraisal process, which can be linked with the KSF <strong>and</strong><br />
development plans, <strong>and</strong> a stronger link to organisational<br />
objectives.<br />
• AO requested any new appraisal process was subject to<br />
consultation with a different staff groups.<br />
• MW added that it is also very important to reflect in the<br />
appraisal process the <strong>Trust</strong>’s strategy <strong>and</strong> objectives. This<br />
will help to embed the new culture <strong>and</strong> strategy.<br />
Leadership Development<br />
• HS stated that due to the financial position of the <strong>Trust</strong>,<br />
there was a real risk that the planned Leadership<br />
Development Programme might be deferred <strong>and</strong><br />
alternative plans are being considered.<br />
• ER asked when the OD <strong>and</strong> leadership development skills<br />
audit feedback would be available. HS agreed this would<br />
be ready for the August meeting.<br />
Staff Survey <strong>and</strong> Temperature Check<br />
• The Director of HR&OD confirmed that the Executive<br />
Team had agreed from the Staff Survey results, three key<br />
areas of focus, in addition to directorate actions in<br />
response to the Staff Survey results. These relate to<br />
Communication; the <strong>Trust</strong> as a place to work; <strong>and</strong> the<br />
<strong>Trust</strong> as a place to be treated. The Committee accepted<br />
these were the right areas of focus <strong>and</strong> requested a more<br />
detailed update on progress at the next meeting.<br />
HS<br />
SR<br />
16/8/2013<br />
16/8/2013<br />
• The local temperature check staff surveys are continuing,<br />
<strong>and</strong> feedback on a monthly basis will be provided to staff.<br />
KM enquired if more analysis on the results could be<br />
undertaken. For example, in relation to how staff feel about<br />
family members being treated at PHNT, <strong>and</strong> a breakdown<br />
of the results to staff groups <strong>and</strong> departments. SR said<br />
she would confirm the level of breakdown possible from<br />
the results <strong>and</strong> discuss this with KM.<br />
Sickness Absence<br />
• The new sickness absence policy has now been<br />
implemented, additional training is being provided to<br />
managers, <strong>and</strong> a wide range of well-being <strong>and</strong> ill health<br />
prevention initiatives were also being made available to<br />
3<br />
SR<br />
16/8/2013
Item 17, Annex 1<br />
31/2013 Francis Report<br />
• MB presented a paper on the key HR&OD implications<br />
arising from the Francis Report, <strong>and</strong> the associated<br />
workstreams of the <strong>Trust</strong>’s HR&OD Strategy. It was noted<br />
that the HR&OD Strategy covered the key workforce<br />
aspects of the Francis Report. The Committee<br />
acknowledged that cultural change <strong>and</strong> leadership<br />
development were crucial.<br />
• MB highlighted that the Whistleblowing Policy has been<br />
reviewed <strong>and</strong> renamed as the “Raising Concerns Policy’.<br />
Summary guidance would also be shortly shared with staff<br />
in support of the new policy.<br />
• MW discussed research around effective teams <strong>and</strong> the<br />
impact of team working on the quality of care <strong>and</strong> patient<br />
outcomes.<br />
32/2013 Terms <strong>and</strong> Conditions Review<br />
• NV presented a report on the Foundation <strong>Trust</strong> Network<br />
Optimisers <strong>and</strong> how each optimiser had been reviewed<br />
<strong>and</strong> was being implemented.<br />
• It was noted that some of the Optimisers were already<br />
included in the existing Workforce CIP schemes <strong>and</strong><br />
savings were not shown against these again in the report<br />
tabled, to avoid double counting of savings.<br />
• Due to the significant potential savings from medical<br />
workforce optimisers which were being led separately by<br />
the Medical Director, it was agreed that a report on<br />
progress with the medical optimisers should be presented<br />
by David Edwards to the Committee at a future meeting.<br />
DE 16/8/2013<br />
• KM asked that all workforce optimisers are carefully<br />
considered to avoid any unintended consequences, such<br />
as staff reverting to agencies to work additional hours, as<br />
has happened amongst the nursing staff group in the past.<br />
• ER asked how the proposed changes are being<br />
communicated with staff. MB confirmed that these would<br />
continue to be subject to Staff Side engagement through<br />
the JSNC, <strong>and</strong> wider communication with staff through<br />
team brief <strong>and</strong> Vital Signs. HS added that the CEO had led<br />
a series of presentations to staff across the <strong>Trust</strong> in the<br />
past few months about the Optimisers <strong>and</strong> SWPC, with<br />
questions raised in the sessions shared with staff.<br />
33/2013 Equality <strong>and</strong> Diversity Update<br />
• JM <strong>and</strong> LB provided the Committee with an update on<br />
progress in delivering the <strong>Trust</strong>’s EDS objectives <strong>and</strong> a<br />
4
Item 17, Annex 1<br />
recent meeting with Diversity Practice.<br />
• JM stated that an area that was highlighted as requiring<br />
action during the EDS assessment <strong>and</strong> the setting of<br />
equality objectives, was that of the positioning of equality<br />
strategically at Board <strong>and</strong> senior management level.<br />
• The Committee supported the recommendation in relation<br />
to the Board Inclusion Development Programme.<br />
• It was noted that the membership of the Equality <strong>and</strong><br />
Diversity Steering Group would need to be reviewed with<br />
stronger clinical representation required.<br />
• In response to a question from ER about the reported lack<br />
of equality information on patient complaints, LB<br />
responded that the process for collection of ethnicity<br />
information was currently not robust enough.<br />
34/2013 Health <strong>and</strong> Safety Committee<br />
• The Committee was unclear as to why the Health <strong>and</strong><br />
Safety Committee minutes were presented at the HR&OD<br />
Committee meeting. HS explained that there had been<br />
some previous discussion over which Committee these<br />
minutes should report in to, <strong>and</strong> agreed to discuss with<br />
Executive Director colleagues <strong>and</strong> clarify.<br />
HS 16/8/2013<br />
35/2013 Communication<br />
ER confirmed the key issues that would be included in feedback<br />
to the <strong>Trust</strong> Board included:<br />
• Recruitment<br />
• Training<br />
• The Francis Report<br />
• Equality <strong>and</strong> Diversity<br />
In terms of learning, it was agreed it had been a productive<br />
meeting, which had covered a number of important issues. ER<br />
asked that moving forward we are clearer on the purpose of<br />
reports submitted to the Committee.<br />
36/2013 Any Other Business<br />
The meeting closed at 11:30hrs<br />
39/2013 Date <strong>and</strong> Time of Next Meeting<br />
The next meeting will be held Friday 16 th August 1000-1200 in the<br />
Board Room DHLC.<br />
5
Item 18<br />
SUMMARY REPORT<br />
<strong>Trust</strong> Board 5 July 2013<br />
Subject<br />
Prepared by<br />
Approved by<br />
Presented by<br />
Audit Committee Chair’s Report<br />
Board Secretary<br />
Margaret Schwarz, NED Chair<br />
Margaret Schwarz, NED Chair<br />
Purpose<br />
This paper provides a summary of assurances received <strong>and</strong> issues or<br />
concerns that the Audit Committee feels should be brought to the attention<br />
of the <strong>Trust</strong> Board, or to other Board Committees, resulting from the Audit<br />
Committee meeting on 31 May 2013.<br />
Corporate Objectives<br />
Decision<br />
Approval<br />
Information<br />
Assurance<br />
Quality Care Inspired People Healthy Organisation Innovate & Collaborate<br />
•<br />
Executive Summary<br />
The Committee received internal management, Internal Audit <strong>and</strong> External Audit reports.<br />
CQC Outcome Review<br />
In accordance with its forward work plan, at each meeting the Committee tests the<br />
adequacy of assurance <strong>and</strong> the process for testing compliance of a CQC outcome. The<br />
Committee assessed Outcome 21 Records, an issue of longst<strong>and</strong>ing concern. The review<br />
had been scheduled as a result of known focus by the Care Quality Commission. The<br />
Director of Planning & Site Services reported on evidence of compliance, gaps in assurance<br />
or areas where evidence of compliance could be strengthened <strong>and</strong> the actions in place to<br />
address these issues. Three issues identified by a CQC inspection in 2012 remain a<br />
concern:<br />
• Security of case notes on wards.<br />
• Updating case notes in a timely manner.<br />
• Treatment Escalation Plans not being completed consistently in respect of DNAR.<br />
The Committee received limited assurance that the planned actions would achieve<br />
compliance <strong>and</strong> no assurance on the timescale for achieving compliance. Health<br />
records was again raised as a concern in verbal feedback from the CQC following a recent<br />
inspection <strong>and</strong> the Committee noted that their written report of their findings was imminent.<br />
The Safety & Quality Committee would continue to oversee this issue.<br />
Bevan Brittan Risk update<br />
This covered key points from the Francis Report, focusing on the requirement for <strong>NHS</strong> trusts<br />
to consider the Report’s recommendations <strong>and</strong> to decide how, <strong>and</strong> to what extent, to apply<br />
them to their respective organisations. Key advice for the Board was to avoid complacency<br />
through over-reliance on positive feedback from patient surveys. More generally, in terms<br />
of the Board’s responsibility to ensure the provision of safe patient care, the advice was for<br />
the Board to be mindful of the pressure in the wider health system <strong>and</strong> to ensure that its<br />
decisions were based on reliable data.<br />
Annual Reports<br />
The Committee reviewed three annual reports for the year 2012/13; Counter Fraud, Internal<br />
•<br />
1
Item 18<br />
Audit <strong>and</strong> the Committee’s own review of its activities.<br />
Annual Accounts 2012/13<br />
With regard to financial reporting for the year ended 31 March 2013, the Committee<br />
received good assurance on the systems <strong>and</strong> processes to finalise these by the<br />
requisite deadline.<br />
• Draft accounts had been submitted to the DoH by the 22 April 2013 deadline,<br />
supported by good quality working <strong>papers</strong> with no material errors.<br />
• The Head of Internal Audit Opinion was, once again, one of ‘significant assurance’.<br />
The Committee’s attention was drawn to weaknesses in controls, identified as health<br />
records management, data protection <strong>and</strong> financial control.<br />
• External Audit’s draft Audit Findings Report set out their expectation to issue an<br />
‘except for’ qualified Value for Money conclusion based on the failure to achieve the<br />
original planned surplus budget <strong>and</strong> the failure to set a balanced budget for 2013/14.<br />
Their audit did not identify any significant control weaknesses that they wished to<br />
bring to the Committee’s attention.<br />
• The Committee scrutinised <strong>and</strong> approved the draft Letter of Representation <strong>and</strong> the<br />
schedule of losses <strong>and</strong> special payments.<br />
• The Committee scrutinised the accounts for the year ended 31 March 2013 <strong>and</strong><br />
agreed that these had been properly prepared on a going concern basis <strong>and</strong><br />
recommended them to the Board for approval.<br />
Management of External Assessments<br />
The Committee received good assurance of the process to respond to recommendations<br />
<strong>and</strong> requirements arising from external assessments. The number of external assessments<br />
has now increased to 101; the management of the register is shifting to a more pro-active<br />
approach to drive the discipline required to ensure that action plans are developed,<br />
implemented, monitored <strong>and</strong> followed up.<br />
PACS Replacement<br />
Further to Internal Audit’s concerns at the previous Audit Committee meeting, the Director of<br />
Planning & Site Services was asked to update the <strong>Trust</strong> Board in April. At the May Audit<br />
meeting Internal Audit again expressed their concerns on the risks to this project. The<br />
Director of Planning & Site Services confirmed that the go-live date had been deferred for<br />
three months with a consequential financial exposure, assessed at a maximum of £60k, to<br />
the <strong>Trust</strong>. The complicated contractual arrangements were compounded by the nonidentification,<br />
at that time, of a commercial negotiator for the <strong>Trust</strong>. The Finance,<br />
Performance & Investment Committee will keep this issue under review.<br />
The minutes of the meeting are attached at Annex 1.<br />
Quality Impact Assessment<br />
None directly.<br />
Financial Impact Assessment<br />
None directly.<br />
Regulatory Impact Assessment<br />
The Audit Committee scrutinises the risks <strong>and</strong> controls affecting all aspects of the <strong>Trust</strong>’s<br />
business <strong>and</strong> is central to the organisation’s governance.<br />
Key Recommendations<br />
The Board is asked to note this report.
Item 18<br />
Next Steps<br />
The Audit Committee will progress its Forward Work Programme <strong>and</strong> the emerging issues to be<br />
referred to other Board Committees will be communicated through this report.
Item 18, Annex 1<br />
<strong>Plymouth</strong> <strong>Hospitals</strong> <strong>NHS</strong> <strong>Trust</strong><br />
Draft minutes of the Audit Committee meeting<br />
12.30 pm on Friday 31 May 2013<br />
Conference Room, Derriford Health & Leisure Centre<br />
Present:<br />
Margaret Schwarz, Non-Executive Director, Committee Chair<br />
Ian Douglas, Non-Executive Director<br />
Terence Lewis, Non-Executive Director<br />
Elizabeth Raikes, Non-Executive Director<br />
D<br />
Henry Warren, Associate Non-Executive Director<br />
Denis Wilkins, Associate Non-Executive Director<br />
Mike Williams, Non-Executive Director<br />
In<br />
attendance:<br />
Apologies:<br />
R<br />
Peter Barber, Audit Lead, Grant Thornton<br />
Kevin Baber, Chief Operating Officer<br />
Martin Bamber, Deputy Director of Human Resources<br />
David Bray, Audit Manager, Grant Thornton<br />
Lee Budge, Director of Governance<br />
Greg Dix, Director of Nursing<br />
Mark Glover, Audit Manager, Audit South West<br />
Gill Hunt, Board Secretary<br />
A<br />
Alex Mayor, Medical Director<br />
Jenny McCall, Director of Audit, Audit South West<br />
Joe Teape, Director of Finance<br />
Nick Thomas, Director of Planning & Site Services<br />
Sally Wilson, Chief Financial Accountant<br />
F<br />
Richard Best, Director of Operations<br />
Ann James, Chief Executive<br />
Hein Scheffer, Director of Human Resources & Organisational<br />
Development<br />
Tracy Wheeler, Local Counter Fraud Specialist<br />
T<br />
40/13 Welcome, apologies <strong>and</strong> declarations of interest<br />
Action<br />
Mrs Schwarz noted the apologies listed above <strong>and</strong> required those<br />
present to declare any interests they had pertaining to the matters<br />
listed on the agenda. There were no declarations of interest.<br />
41/13 Minutes <strong>and</strong> matters arising<br />
The minutes of the meeting held on 10 April 2013 were agreed as a<br />
true <strong>and</strong> accurate record subject to the following amendment:<br />
Combined Cost Improvement Programme, Business Planning <strong>and</strong><br />
Budgetary Control Review<br />
Page 5, final bulleted point to read “[…] of an experienced Deputy<br />
Director of Finance.”<br />
1
Item 18, Annex 1<br />
Matters arising<br />
4/13 <strong>and</strong> 19/13 Counter Fraud Work Plan<br />
The Committee noted that any consequences for SFIs arising from the<br />
risk based approach to this work in 2013/14 had been covered by the<br />
Director of Finance’s paper on financial controls presented to the May<br />
<strong>Trust</strong> Board.<br />
42/13 Review of Action List<br />
D<br />
The Committee noted that there were no outst<strong>and</strong>ing actions.<br />
In order to facilitate the attendance of visitors to the meeting, the Chair<br />
took <strong>papers</strong> in a different order to that set out on the agenda.<br />
R<br />
43/13 Bevan Brittan Risk Update<br />
Mr Simon Lindsay, partner, Bevan Brittan, attended to give a risk<br />
update to the Committee.<br />
Mr Lindsay gave a<br />
A<br />
presentation on key points from the Francis<br />
Report, focusing on the requirement for <strong>NHS</strong> trusts to consider the<br />
Report’s recommendations <strong>and</strong> to decide how <strong>and</strong> to what extent to<br />
apply them to their respective organisations. He explored in depth<br />
three themes:<br />
F<br />
• Constitution <strong>and</strong> st<strong>and</strong>ards.<br />
• C<strong>and</strong>our <strong>and</strong> complaints.<br />
• Nursing care.<br />
Mr Lindsay summarised the Government’s response to the Report<br />
focusing on:<br />
T<br />
• Clear, enforced st<strong>and</strong>ards.<br />
• Professional regulation.<br />
• Patient centred leadership.<br />
• Provision of accurate, useful information.<br />
Mr Lindsay stated that it was incumbent on <strong>NHS</strong> <strong>Trust</strong> Boards not to<br />
delay their responses <strong>and</strong>, in formulating them, to avoid complacency<br />
through over-reliance on positive feedback from patient surveys.<br />
Dr Williams stated that a significant number of the Report’s<br />
recommendations did not apply to hospital trusts <strong>and</strong>, in the absence<br />
of guidance on this point, how should Boards respond? Mr Lindsay<br />
stated that this was a matter for individual trusts to address; however,<br />
to not respond to recommendations which did apply to their<br />
organisation would be unacceptable. Drawing on his experience of<br />
other organisations’ approach to this issue, Mr Budge stated that a<br />
robust way forward would be for provider organisations to identify <strong>and</strong><br />
2
Item 18, Annex 1<br />
evidence those recommendations which were believed to apply <strong>and</strong> to<br />
respond appropriately. He confirmed that <strong>Trust</strong>s were co-operating<br />
<strong>and</strong> sharing their individual approaches, which was helpful for all.<br />
Mr Lindsay briefed the Committee on two inquest case studies <strong>and</strong><br />
the key issues arising from these. The Committee discussed these, in<br />
broad terms. In the context of operational <strong>and</strong> staffing pressures, Mr<br />
Wilkins queried the point at which a service may be withdrawn in the<br />
interests of patient safety<br />
D<br />
<strong>and</strong> the legal position of doing so. Mr<br />
Lindsay stated that there was no guidance or definitive answer to this<br />
difficult question <strong>and</strong> it would depend on the circumstances. However,<br />
conscientious monitoring <strong>and</strong> an ability to audit actions <strong>and</strong> evidence<br />
careful decision-making would be crucial. The broader point was the<br />
pressure in the system going forward <strong>and</strong> <strong>Trust</strong> Boards must be<br />
cognizant of this.<br />
R<br />
44/13 Review of CQC Outcome 21: Records<br />
A<br />
In setting the context for this review, Mrs Schwarz stated that health<br />
records had been an issue of longst<strong>and</strong>ing concern to the Audit<br />
Committee <strong>and</strong> to the<br />
F<br />
Safety & Quality Committee, which was<br />
currently overseeing progress with compliance. The review being<br />
undertaken today had been scheduled as a result of known focus by<br />
the Care Quality Commission (CCQ) <strong>and</strong> as part of the Committee’s<br />
rolling programme to review the process to test assurance of<br />
outcomes declaring compliance. The current status of this outcome<br />
was compliance but with<br />
T<br />
moderate concern.<br />
Mrs Schwarz thanked Mr Lindsay for attending <strong>and</strong> he left the<br />
meeting.<br />
Penny Taylor, Head of Clinical Systems Governance, attended for this<br />
item.<br />
Mr Thomas stated that that this st<strong>and</strong>ard was very broad <strong>and</strong> covered<br />
more than health records. An inspection in 2012 by the CQC <strong>and</strong> a<br />
subsequent mock inspection in March 2013 had identified concerns<br />
with the security of case notes on wards, updating notes in a timely<br />
manner <strong>and</strong> with Treatment Escalation Plans (TEP) not being<br />
completed consistently in respect of DNAR. Dr Williams asked Mr<br />
Thomas how confident he was that the actions in place would ensure<br />
compliance. If the CQC inspected today, would they find the <strong>Trust</strong><br />
compliant? Assurance could not be given on this point <strong>and</strong> Mr Budge<br />
stated that the CQC had been asked if they were able to identify other<br />
similar organisations who exhibited best practice. Mrs Raikes asked<br />
when the <strong>Trust</strong> would be compliant. Mr Budge stated that when the<br />
CQC submitted the formal report of their inspection it was likely that<br />
the <strong>Trust</strong> would be given between thirty <strong>and</strong> sixty days to comply.<br />
Some of the issues were not unique to the <strong>Trust</strong> <strong>and</strong> whilst they were<br />
features of working in a busy environment, they also concerned<br />
culture, which took longer to shape. Overall, the actions would take<br />
3
Item 18, Annex 1<br />
time to embed <strong>and</strong> Mr Budge would ensure that the Head of<br />
Assurance undertook a further review.<br />
Mrs Schwarz queried progress with DNAR recording. Dr Mayor stated<br />
that it was challenging to ensure this conversation was undertaken<br />
sensitively <strong>and</strong> comprehensively. Dr Williams acknowledged this<br />
could be an issue in MAU but it must be comprehensively resolved in<br />
the subsequent patient pathway. Dr Mayor was meeting with junior<br />
doctors to ensure that<br />
D<br />
patient notes were clearly annotated when the<br />
conversation had not been had. Mr Budge suggested that the Safety<br />
& Quality Committee set a timescale for a further audit <strong>and</strong> then track<br />
progress. Dr Mayor stated that TEP was an issue for the wider health<br />
community to address <strong>and</strong> that, overall, the solution lay outside the<br />
<strong>Trust</strong>. Mr Baber suggested seeking <strong>and</strong> adopting best practice from<br />
other trusts who had complied with this st<strong>and</strong>ard.<br />
R<br />
There were no further questions.<br />
The Committee noted the assessment of compliance with moderate<br />
concern <strong>and</strong> the limited assurance provided by the actions identified.<br />
The Board would receive updates via the Safety & Quality Committee.<br />
A<br />
Penny Taylor left the meeting.<br />
45/13 Counter Fraud Annual Report 2012/13<br />
46/13<br />
The Committee noted<br />
F<br />
this document. There were no questions.<br />
Internal Audit Annual Report 2012/13<br />
Mr Glover gave an overview of the report <strong>and</strong> is contents. The<br />
Committee discussed two issues of concern, the delay to the PACS<br />
project implementation<br />
T<br />
<strong>and</strong> the deferral of the Joint Advisory Group on<br />
Gastrointestinal Endoscopy (JAG) accreditation inspection.<br />
PACS<br />
Mr Thomas updated the Committee on developments at the PACS<br />
Project Board which had taken place the previous day. On the<br />
Committee’s recommendation it had been decided to defer the<br />
scheduled go-live date for three months <strong>and</strong> to extend the existing<br />
provider’s contract for the same timescale as there was insufficient<br />
assurance on the speed at which historical images could be<br />
accessed. The maximum financial exposure to the <strong>Trust</strong> would be<br />
c£60k plus costs associated with extending the life of the Project<br />
Board.<br />
Dr Williams queried the degree of confidence Mr Thomas had that a<br />
delay of three months would be sufficient to solve the problem. Mr<br />
Thomas explained the size <strong>and</strong> complex nature of the project <strong>and</strong><br />
contractual arrangements, which involved dealing with sub-contractors<br />
under Connecting for Health (C4H). The situation was aggravated by<br />
4
Item 18, Annex 1<br />
existing terms <strong>and</strong> conditions negotiated under C4H. At this stage Mr<br />
Thomas was not clear about the <strong>Trust</strong>’s contractual position <strong>and</strong><br />
recompense arrangements. The financial benefits of the new system<br />
would not now be realised as early as had been anticipated. Dr<br />
Williams asked who was responsible for the commercial negotiations.<br />
Mr Thomas stated that the SMT had not yet had this discussion.<br />
Professor Lewis asked whether Mr Thomas intended to overlap the<br />
two PACS systems.<br />
D<br />
Mr Thomas stated that it had been intended to<br />
pursue a soft roll out but the <strong>Trust</strong> was aware that other organisations<br />
had experienced problems with implementation. The <strong>Trust</strong> would roll<br />
out to other users prior to Radiology. Professor Lewis sought, <strong>and</strong><br />
received, assurance that contingency plans were in place. Updates<br />
on this issue would be reported to the Board via the Finance,<br />
Performance & Investment RCommittee (FPIC).<br />
Dr Williams queried progress in resolving this issue. Mr Baber stated<br />
that the JAG review was scheduled for September <strong>and</strong> he would be<br />
meeting with the relevant Care Group Director <strong>and</strong> service line<br />
manager to receive an<br />
A<br />
update on progress. Dr Williams queried the<br />
risks to the <strong>Trust</strong> of failing to achieve accreditation. Dr Mayor stated<br />
that should this be the case, the risk would be the loss of the<br />
screening service. Due to the size of the facility, meeting EMSA was<br />
challenging <strong>and</strong> he suggested that there appeared to have been an<br />
underestimate that the size of the facility required to match increased<br />
dem<strong>and</strong> for the service.<br />
F<br />
Endoscopy Suite Review<br />
The Committee considered the executive summaries of Internal Audit<br />
reports issued since the previous meeting:<br />
Tenders & Quotes<br />
Mrs Schwarz queried<br />
T<br />
whether FPIC would overview progress with this<br />
report’s recommendations. Mr Teape stated that they formed part of<br />
the wider approach to controls on non-pay in the programmes being<br />
led by the Head of Procurement, Andy McMinn. Mr McMinn would<br />
appraise FPIC of progress.<br />
Recruitment Processes<br />
For the avoidance of doubt, Mr Glover stated that the report covered<br />
only non-medical recruitment, which was in accordance with the<br />
original briefing. Professor Lewis asked why medical recruitment had<br />
not been covered. Mrs Schwarz stated that the purpose of the audit<br />
had been to establish whether recruitment processes were sufficiently<br />
slick to respond at a time when the <strong>Trust</strong> was urgently seeking to<br />
recruit additional nurses. In responding to Professor Lewis’s question,<br />
Mr Bamber stated that the learning from this report had been applied it<br />
to medical recruitment. The Committee noted that the CQC, having<br />
focused on recruitment, had not expressed concerns during their<br />
recent inspection.<br />
5
Item 18, Annex 1<br />
Payroll & Expenses<br />
No comments were made.<br />
Serco Hygiene Compliance Reporting<br />
Noting the report’s conclusion that Internal Audit could not provide full<br />
assurance that (a) Serco were fully compliant with the hygiene<br />
requirements of the <strong>Trust</strong> <strong>and</strong> (b) Serco inspections were reported<br />
accurately, Mrs Schwarz queried who was responsible for leading<br />
delivery of the recommendations.<br />
D<br />
Mr Thomas stated that this was the<br />
Facility Operations Manager but he could not confirm whether the<br />
report’s recommendations had been implemented.<br />
Dr Williams noted that the report stated that Serco were compliant<br />
with the requirements of the National Specification for Cleanliness in<br />
the <strong>NHS</strong>. However, Internal<br />
R<br />
Audit’s conclusions were at odds with this<br />
assertion. The results of audits undertaken between April 2011 <strong>and</strong><br />
March 2012 were set out in the report but these were inconsistent <strong>and</strong><br />
historic. It was therefore difficult to form a view given the conflicting<br />
statements presented. Mrs Raikes was concerned that there was<br />
insufficient traction on resolving this important issue <strong>and</strong> whilst<br />
Internal Audit’s attention<br />
A<br />
had identified the anomaly, she had limited<br />
assurance of delivery. Noting that a combined audit tool was likely to<br />
be rolled out in June 2013, Mrs Schwarz stated that the Committee’s<br />
concerns would be addressed as part of Internal Audit’s follow-up<br />
process.<br />
F<br />
Mr Budge briefed the Committee on the reasons why this report had<br />
been commissioned <strong>and</strong> stated his intention to provide a copy to the<br />
individual who had raised the matter in the first instance.<br />
Neonatal Transport Contract Review<br />
Hygiene Inspection<br />
Whilst there were no comments<br />
T<br />
on the report, Mr Glover passed on to<br />
the Committee feedback from the Audit team member who had<br />
undertaken the inspection. In her experience staff had been<br />
responsive, well-engaged <strong>and</strong> keen to ensure high st<strong>and</strong>ards of<br />
cleanliness across all wards. Mr Dix would convey these sentiments<br />
at the appropriate forum.<br />
Head of Internal Audit Opinion (HOIAO)<br />
Ms McCall referred the Committee to pages 7 to 16 of the Annual<br />
Report <strong>and</strong> specifically to page 8, which detailed Internal Audit’s<br />
overall opinion of ‘significant assurance’ that there was a generally<br />
sound system of internal control within the <strong>Trust</strong> <strong>and</strong> to the basis for<br />
forming that opinion. Ms McCall drew the Committee’s attention to<br />
the identified weaknesses in controls, which were detailed as health<br />
records management, data protection <strong>and</strong> financial control. Ms<br />
McCall referred the Committee to the two Third Party Assurance<br />
Reports confirming the opinion of effective controls for the Electronic<br />
Staff Record <strong>and</strong> Shared Business Services.<br />
6
Item 18, Annex 1<br />
Five of the seven Non-Executive Directors present had been<br />
appointed since the close of the previous financial year <strong>and</strong> in seeking<br />
to develop a more informed underst<strong>and</strong>ing of the respective roles of<br />
internal <strong>and</strong> external audit, including the processes <strong>and</strong> evidence<br />
used by both audit functions to determine their respective end of year<br />
opinions, a broad discussion developed. Non-Executive Directors<br />
used this as an opportunity to triangulate their own knowledge <strong>and</strong><br />
observations of the <strong>Trust</strong>’s performance with the arguments presented<br />
to them by internal <strong>and</strong><br />
D<br />
external audit <strong>and</strong> to share their perspective,<br />
as Board Directors with corporate responsibility, of audit’s findings. In<br />
general terms the discussion covered:<br />
• Underst<strong>and</strong>ing the roles of internal <strong>and</strong> external audit <strong>and</strong> their<br />
respective focus on process/controls <strong>and</strong> on outcomes.<br />
R<br />
• The requirement of the <strong>Trust</strong> Board, via the Audit Committee,<br />
to have earlier visibility of the inconsistent application of<br />
controls when this could lead to serious risks, for example<br />
controls around discretionary pay. Professor Lewis sought<br />
clarification on the costs included within discretionary pay. Mr<br />
Teape stated<br />
A<br />
that service lines had been asked to prepare<br />
workforce plans which included substantive <strong>and</strong> discretionary<br />
pay for the full year. Temporary <strong>and</strong> agency staff, overtime <strong>and</strong><br />
waiting list initiative payments all contributed to discretionary<br />
pay costs. Professor Lewis highlighted the importance of<br />
ensuring that workforce <strong>and</strong> activity were aligned.<br />
F<br />
• The longer term intention to devolve autonomy to service lines<br />
within the current imperative to apply strict financial controls to<br />
ensure that the <strong>Trust</strong>’s overall financial position did not<br />
deteriorate further. After the last Audit Committee meeting<br />
Non-Executive Directors had received copies of the <strong>Trust</strong>-<br />
T<br />
commissioned PWC report on financial controls. Mr Teape<br />
placed PWC’s work into context for the Committee. Their<br />
recommendations had been incorporated into an action plan,<br />
the implementation of which would be overseen by FPIC.<br />
• Underst<strong>and</strong>ing why the known problems of bed capacity had<br />
not emerged as part of internal <strong>and</strong> external audits’ focus. Mr<br />
Barber stated that this was covered in the review of resources<br />
<strong>and</strong> his firm had commented on this. For the last three years<br />
the focus of his firm’s Value for Money (VFM) conclusion had<br />
shifted from generic to financial resilience. In 2010/11 his firm<br />
qualified its conclusion. An improvement was noted in 2011/12<br />
<strong>and</strong> the <strong>Trust</strong> delivered in a challenging environment <strong>and</strong><br />
therefore their opinion had not been qualified in 2011/12. The<br />
position had deteriorated in 2012/13 in the area of financial<br />
resilience <strong>and</strong> the evidence for this was set out in his firm’s<br />
report.<br />
7
Item 18, Annex 1<br />
The Committee noted Internal Audit’s Annual Report <strong>and</strong> the HOIAO.<br />
47/13 Audit Committee Annual Report 2012/13<br />
The Committee reviewed <strong>and</strong> approved this Annual Report.<br />
48/13 External Audit: Financial Resilience Report (draft)<br />
D<br />
Mr Barber presented this report which summarised the financial<br />
resilience element of his firm’s VFM conclusion on their audit work for<br />
2012/13. The report RAG-rated the <strong>Trust</strong>’s arrangements on:<br />
• Key indicators of financial performance.<br />
• Strategic financial planning.<br />
• Financial governance.<br />
• Financial controls.<br />
R<br />
Mr Barber drew the Committee’s attention to the Executive Summary<br />
<strong>and</strong> to high level risk assessments of red for key indicators of financial<br />
performance <strong>and</strong> strategic financial planning <strong>and</strong> to amber for<br />
financial governance<br />
A<br />
<strong>and</strong> financial control. These ratings contributed<br />
to a qualified VFM conclusion.<br />
Mr Douglas drew Mr Barber’s attention to page 7 of the report <strong>and</strong><br />
stated that there was, in fact, clinical representation on all the Board’s<br />
Committees.<br />
F<br />
Dr Williams suggested that the <strong>Trust</strong>’s financial challenges resulted<br />
from whole system problems. Did Mr Barber’s firm audit other health<br />
organisations, thereby facilitating an holistic view? Mr Barber stated<br />
that his firm audited other <strong>NHS</strong> organisations <strong>and</strong> would submit to the<br />
Department of Health on overall performance report, although within<br />
this individual organisations Twould not be named. In this context his<br />
firm played a role in taking forward topical debates nationally.<br />
Professor Lewis queried whether Mr Barber’s firm had a conflict of<br />
interest. Mr Barber stated that there was not because his firm audited<br />
individual organisations <strong>and</strong> was not involved in contract negotiations.<br />
Mr Warren sought to clarify a definition of ‘Value for Money’. Mr Bray<br />
explained that the Audit Commission, in their Code of Audit Practice,<br />
set out the relevant criteria. This Code, followed by all auditors for<br />
consistency, was approved by Parliament every five years.<br />
The Committee noted the draft report.<br />
49/13 External Audit: Audit Findings Report (draft)<br />
Mr Barber stated that this report had been issued on 29 May <strong>and</strong> his<br />
firm’s deadline to comment on the financial statements fell on 10<br />
8
Item 18, Annex 1<br />
June. However, work was well ahead <strong>and</strong> had not identified any<br />
areas of concern. There had been a small number of trivial errors.<br />
Mr Barber wished to record his thanks to Mr Teape, Mrs Wilson <strong>and</strong> to<br />
their team, who had produced comprehensive working <strong>papers</strong> <strong>and</strong><br />
with whom they had worked to produce a very positive outcome. This<br />
outcome confirmed his audit planning assumptions that the <strong>Trust</strong> was<br />
a low risk organisation.<br />
D<br />
Mr Barber stated that he was satisfied that the <strong>Trust</strong> had in place<br />
arrangements to secure economy, efficiency <strong>and</strong> effectiveness, with<br />
the exception of Financial Resilience. For this reason it was intended<br />
to issue a qualified ‘except for’ conclusion on the <strong>Trust</strong>’s<br />
arrangements for securing economy, efficiency <strong>and</strong> effectiveness in its<br />
use of resources. His<br />
R<br />
firm had been proposing to issue an ‘emphasis<br />
of matter’ conclusion in recognition of the <strong>Trust</strong> Board setting a deficit<br />
budget for 2013/14. However, confirmation had been received from<br />
the <strong>Trust</strong> Development Authority of their willingness to underwrite the<br />
deficit <strong>and</strong> there was now no longer any requirement to issue an<br />
‘emphasis of matter’ conclusion.<br />
A<br />
Mr Barber confirmed that his firm would report on the outcome of their<br />
external assurance work on the <strong>Trust</strong>’s Quality Account prior to<br />
issuing their opinion on the financial statements <strong>and</strong> issuing their VFM<br />
conclusion for the year.<br />
50/13<br />
F<br />
Annual Accounts for the year ended 31 March 2013<br />
The Committee noted the draft report.<br />
Mr Teape presented the Annual Accounts (Annex 1) to the Committee<br />
for scrutiny, together with a statement of comprehensive income for<br />
2012/13, showing movement from 2011/12 (Annex 2), a Going<br />
Concern Review (Annex 3) <strong>and</strong> draft Letter of Representation.<br />
T<br />
Mr Douglas queried whether there had been any significant changes<br />
to format, style or content this year <strong>and</strong> Mrs Wilson confirmed that<br />
there had not. Since circulating the accounts there had been some<br />
minor amendments to the narrative but these were not of a material<br />
nature.<br />
Mr Warren queried whether the financial statements aligned with the<br />
management accounts. Mr Teape <strong>and</strong> Mrs Wilson confirmed that this<br />
was the case. Mr Warren sought, <strong>and</strong> received, clarification of the<br />
information set out in section 9.4 of the accounts. Mr Teape stated<br />
that the <strong>Trust</strong> did not make payments outside contractual terms.<br />
The Committee reviewed <strong>and</strong> approved the Annual Governance<br />
Statement set out on pages 3 to 10 of the accounts.<br />
There were no other queries on the financial statements.<br />
9
Item 18, Annex 1<br />
Going Concern Review<br />
Mr Teape reminded the Committee of its responsibility to obtain<br />
assurance that the accounts had been prepared on a going concern<br />
basis. Referring to page 5 of Annex 3, Dr Williams sought to<br />
underst<strong>and</strong> the statement that “Income for the year has been agreed<br />
with Commissioners on a managed PbR basis.” Mr Teape stated that<br />
there was a joint commitment across the health community to ensure<br />
the <strong>Trust</strong> would deliver<br />
D<br />
the contract value. The contract had been<br />
‘split’ into three themes: block, variables <strong>and</strong> a risk-share element.<br />
The contract had been signed <strong>and</strong> there was good assurance of its<br />
integrity.<br />
Mr Baber would circulate to NEDs the summary briefing recently<br />
issued by commissioners<br />
R<br />
to GPs.<br />
Professor Lewis sought assurance that the <strong>Trust</strong> would be<br />
appropriately recompensed for winter pressures this year. Mr Baber<br />
stated that the <strong>Trust</strong> was involved in discussions <strong>and</strong> there may be<br />
some additional funding to support additional activity <strong>and</strong> there was<br />
optimism that this would<br />
A<br />
be forthcoming.<br />
Mr Warren strongly argued that the <strong>Trust</strong> was a going concern given<br />
its unique purpose <strong>and</strong> funding arrangements <strong>and</strong> Committee<br />
members welcomed his perspective.<br />
COO<br />
The Committee endorsed<br />
F<br />
the assessment of the <strong>Trust</strong> as a going<br />
concern <strong>and</strong> recommended to the <strong>Trust</strong> Board the approval of the<br />
assessment as the basis for preparation of the <strong>Trust</strong>’s financial<br />
statements.<br />
Letter of Representation<br />
The Committee reviewed<br />
T<br />
this <strong>and</strong> recommended to the <strong>Trust</strong> Board<br />
that they approve it <strong>and</strong> that they authorise the Chief Executive <strong>and</strong><br />
Director of Finance to sign it.<br />
51/13 Losses <strong>and</strong> Special Payments for the year ended 31 March 2013<br />
The Committee reviewed the schedule <strong>and</strong> noted that the total, £298k,<br />
was lower than 2011/2012 <strong>and</strong> that the total number of bad debts<br />
written off had reduced. The Committee remained concerned,<br />
however, by the increase, both in terms of incidence <strong>and</strong> payments<br />
made, in respect of the loss of patients’ property.<br />
The Committee noted the report <strong>and</strong> recommended to the <strong>Trust</strong> Board<br />
that they approve the formal write-off.<br />
52/13 Management of External Assessments<br />
Mr Budge presented the half yearly review of progress in responding<br />
to recommendations <strong>and</strong> requirements arising from external<br />
10
Item 18, Annex 1<br />
assessments. Mr Budge explained the process by which issues of<br />
concern arising from external assessments were elevated, via the<br />
Assurance Framework, to the <strong>Trust</strong> Board.<br />
There were no questions <strong>and</strong> the Committee noted the report.<br />
53/13 Safety <strong>and</strong> Quality Committee<br />
Minutes of the April 2013<br />
D<br />
meeting were noted by the Committee.<br />
54/13 Finance, Performance & Investment Committee<br />
Minutes of the April 2013 meeting <strong>and</strong> minutes of the ‘commercial-inconfidence’<br />
section of the April 2013 meeting were noted by the<br />
Committee.<br />
R<br />
55/13 Human Resources & Organisational Development Committee<br />
Minutes of the April 2013 meeting were noted by the Committee.<br />
56/13 Audit Chair’s Report<br />
A<br />
to the Board<br />
It was agreed that this would cover:<br />
• CQC Outcome 21 review.<br />
• Bevan Brittan risk update.<br />
F<br />
• Approval of the accounts <strong>and</strong> associated documentation review<br />
<strong>and</strong> recommendations to the Board.<br />
57/13 Review <strong>and</strong> Learning<br />
As agreed at the May meeting, this item featured a discussion to<br />
extract learning from<br />
T<br />
a topical issue <strong>and</strong> on this occasion it was the<br />
Committee’s relationship with Internal Audit. Prior to the meeting<br />
there had been a Board session to agree Internal Audit’s work plan for<br />
2013/14. The Committee reflected on the following questions:<br />
• Does the Audit Committee underst<strong>and</strong> its relationship with<br />
Internal Audit?<br />
• How are we assured that reports are thorough?<br />
• Is the Audit Committee sufficiently proactive?<br />
• Could we use what they tell us more efficiently?<br />
• How can we improve triangulation?<br />
The Committee agreed that its underst<strong>and</strong>ing of its relationship with<br />
Internal Audit had improved as a result of the pre-meeting session <strong>and</strong><br />
particularly through questioning during the meeting. The Committee<br />
gained assurance on thoroughness through challenge <strong>and</strong> audit<br />
scope <strong>and</strong> agreed that there was a requirement for significant<br />
management attention at the start of the process. It would be helpful<br />
11
Item 18, Annex 1<br />
if Internal Audit more proactively highlighted their upcoming work to<br />
the Committee.<br />
Dr Williams asked whether the Committee’s focus was prepared for<br />
the change to service line reporting. Whilst it was agreed that this<br />
was the long term goal, the new structure was not yet sufficiently<br />
developed to support this. However, just as Directorates had the<br />
opportunity to request Internal Audit support, so would service lines.<br />
In the meantime, audit<br />
D<br />
activity would focus at care group level, with<br />
more in-depth activity at service line level, when necessary.<br />
It was agreed that at the next meeting Review <strong>and</strong> Learning activity<br />
would focus on nurse staffing levels.<br />
R<br />
There was no other business <strong>and</strong> the meeting closed at 3.30 pm.<br />
58/13 Any Other Business<br />
59/13 Date of next meeting<br />
A<br />
12.30 – 3.30 pm Friday 9 August 2013.<br />
F<br />
T<br />
12