Pain: Facility Assessment Checklists - Primaris
Pain: Facility Assessment Checklists - Primaris
Pain: Facility Assessment Checklists - Primaris
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
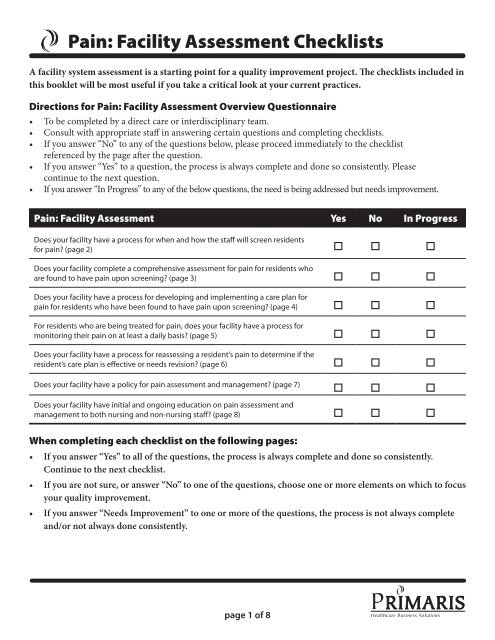
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong><br />
A facility system assessment is a starting point for a quality improvement project. The checklists included in<br />
this booklet will be most useful if you take a critical look at your current practices.<br />
Directions for <strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> Overview Questionnaire<br />
• To be completed by a direct care or interdisciplinary team.<br />
• Consult with appropriate staff in answering certain questions and completing checklists.<br />
• If you answer “No” to any of the questions below, please proceed immediately to the checklist<br />
referenced by the page after the question.<br />
• If you answer “Yes” to a question, the process is always complete and done so consistently. Please<br />
continue to the next question.<br />
• If you answer “In Progress” to any of the below questions, the need is being addressed but needs improvement.<br />
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> Yes No In Progress<br />
Does your facility have a process for when and how the staff will screen residents<br />
for pain? (page 2) o o o<br />
Does your facility complete a comprehensive assessment for pain for residents who<br />
are found to have pain upon screening? (page 3) o o o<br />
Does your facility have a process for developing and implementing a care plan for<br />
pain for residents who have been found to have pain upon screening? (page 4) o o o<br />
For residents who are being treated for pain, does your facility have a process for<br />
monitoring their pain on at least a daily basis? (page 5) o o o<br />
Does your facility have a process for reassessing a resident’s pain to determine if the<br />
resident’s care plan is effective or needs revision? (page 6) o o o<br />
Does your facility have a policy for pain assessment and management? (page 7)<br />
o o o<br />
Does your facility have initial and ongoing education on pain assessment and<br />
management to both nursing and non-nursing staff? (page 8) o o o<br />
When completing each checklist on the following pages:<br />
• If you answer “Yes” to all of the questions, the process is always complete and done so consistently.<br />
Continue to the next checklist.<br />
• If you are not sure, or answer “No” to one of the questions, choose one or more elements on which to focus<br />
your quality improvement.<br />
• If you answer “Needs Improvement” to one or more of the questions, the process is not always complete<br />
and/or not always done consistently.<br />
page of 8
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Screening for <strong>Pain</strong><br />
A screening assessment is a brief assessment or questions that determine if the resident has pain or the potential<br />
for pain. It does not include a thorough assessment about the pain symptoms or reasons for the pain that needs<br />
to be done if the resident is found to have pain upon screening.<br />
Basic questions to use as a screening assessment:<br />
1. Do you have pain now?<br />
2. Do you have pain that recurs?<br />
3. If unable to answer questions 1 and 2,<br />
a) Is there evidence of pain?<br />
b) Are there diagnoses that suggest potential for pain?<br />
4. Are there diagnoses that suggest potential for pain?<br />
Does your facility have a process for screening that addresses all the below listed areas?<br />
Yes<br />
No<br />
Needs<br />
Improvement<br />
Does your facility have a policy and procedure for when and how the staff will<br />
screen residents for pain?<br />
o o o<br />
Does your policy and procedure state that residents should be screened for pain at<br />
the following times:<br />
o o o<br />
• Within 24 hours of admission o o o<br />
• Within 24 hours of readmission o o o<br />
• At each MDS assessment o o o<br />
• With each change in condition o o o<br />
If unable to answer questions 1 and 2, a) Is there evidence of pain? b) Are there<br />
diagnoses that suggest potential for pain?<br />
o o o<br />
Do you have a variety of pain evaluation tools available to allow individualization<br />
(e.g., the Faces, numerical, verbal scales, or the PAINAD tools for the cognitively<br />
impaired)?<br />
o o o<br />
Are residents screened (assessed) using the tool determined to be appropriate for<br />
each resident?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Assessing <strong>Pain</strong><br />
A comprehensive assessment for pain is done when pain is identified on screening, someone develops<br />
new symptoms of pain, or worsening pain that warrants a thorough assessment for this new complaint or<br />
improvement of the condition causing the pain.<br />
Does your comprehensive pain assessment include all of the below elements?<br />
Yes<br />
No<br />
Needs<br />
Improvement<br />
If pain is identified during screening, does your facility have a process that will lead<br />
to a comprehensive assessment within 24 hours?<br />
o o o<br />
Are the following elements included in your comprehensive assessment? o o o<br />
• Description of the pain o o o<br />
• Location of the pain o o o<br />
• Intensity/severity of the pain using an accepted pain scale o o o<br />
• Frequency of pain o o o<br />
• Current pain o o o<br />
• <strong>Pain</strong> at its least o o o<br />
• <strong>Pain</strong> at its worst o o o<br />
• Aggravating factors (what makes it worse) o o o<br />
• Alleviating factors (what makes it better) o o o<br />
• Effects of the pain on the resident’s life (ADLs, sleep, appetite, physical activity,<br />
emotions, mood, nausea)<br />
o o o<br />
• Current treatment o o o<br />
• Response to current treatment o o o<br />
When a comprehensive assessment is done, are all these elements completed and<br />
recorded on your assessment form and in a timely manner?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Monitoring <strong>Pain</strong><br />
For residents who are being treated for pain, does your facility have a process for monitoring their pain on at<br />
least a daily basis?<br />
Does your facility’s process for monitoring pain include these components?<br />
Yes<br />
No<br />
Needs<br />
Improvement<br />
Do you ask residents to rate their pain using a pain scale identified as appropriate<br />
for the resident?<br />
o o o<br />
Does your facility use an appropriate pain scale to monitor for pain on a daily basis<br />
for those with cognitive impairment (e.g., the <strong>Pain</strong>AD scale)?<br />
o o o<br />
Do you use nonverbal cues to monitor for pain? o o o<br />
Do you record a monitored pain scale score: o o o<br />
• At least every 24 hours? o o o<br />
• Before giving a prn pain medication? o o o<br />
• Approximated 30 minutes after giving a prn pain medication? o o o<br />
• With each complaint of pain? o o o<br />
Do you have a system for tracking in the medical record the results of your<br />
monitoring?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Reassessing <strong>Pain</strong><br />
Does your facility have a process for reassessing a resident’s pain to determine if the resident’s care plan is<br />
effective or needs revision?<br />
Does your facility’s process for reassessing the care plan for pain address all the below areas?<br />
Yes No<br />
Needs<br />
Improvement<br />
Does your facility have a policy and procedure defining when a comprehensive<br />
reassessment of pain will be completed? (A complete reassessment should be<br />
performed for any persistent or worsening pain.)<br />
o o o<br />
Does the reassessment include all the components in the comprehensive<br />
assessment? (See page 4, Monitoring <strong>Pain</strong>)<br />
o o o<br />
Does your staff follow the policy and procedure for reassessing pain when the<br />
resident is complaining of persistent or worsening pain?<br />
o o o<br />
Is the resident reassessed for pain at regular intervals after being assessed initially<br />
as having pain?<br />
o o o<br />
Do you reassess residents who are taking increasing doses of prn medication<br />
(including those who are also on regularly scheduled medications for pain)?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Developing <strong>Pain</strong> Care Plans<br />
Does the plan of care for pain address all the below areas?<br />
Yes<br />
No<br />
Needs<br />
Improvement<br />
If pain is identified in admission, is a plan of care put into place within 48 hours of<br />
admission?<br />
o o o<br />
Does the care plan for any resident identified with pain include a pain control goal<br />
as defined by the resident/caregiver/family member?<br />
o o o<br />
Does the care plan include education of the resident and family related to these<br />
areas of pain management:<br />
o o o<br />
• Goal of therapy o o o<br />
• Side effects (e.g., drowsiness) o o o<br />
• Constipation o o o<br />
• Overall treatment plan o o o<br />
For residents with daily pain, does the plan provide for medication on a regular<br />
schedule (e.g., around the clock), not just prn?<br />
o o o<br />
Does the plan provide for medication use by mouth if at all possible? o o o<br />
Does the plan provide for using non-pharmacological approaches to pain<br />
management (e.g., massage, music, aromatherapy, ice or heat, etc.)?<br />
o o o<br />
Does the plan provide for keeping the resident as mobile as possible? o o o<br />
Does the plan address positioning and proper movement to minimize the resident’s<br />
pain?<br />
o o o<br />
Does the plan provide for regular monitoring of resident’s response to pain<br />
medications at least every 24 hours?<br />
o o o<br />
Does the plan outline when the reassessment of resident’s pain and responses to<br />
pain will be completed?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Assessing <strong>Pain</strong> Management Policies<br />
Does your facility’s policy for pain assessment and management include the following components?<br />
Yes<br />
No<br />
Needs<br />
Improvement<br />
Does your facility’s policy include a statement regarding your facility’s commitment<br />
to pain management?<br />
o o o<br />
Does your facility’s policy include screening, assessment, and reassessment of<br />
residents for pain?<br />
o o o<br />
Does your facility’s policy include the goals of the pain assessment and<br />
management program such as:<br />
o o o<br />
• Prompt assessment and diagnosis of pain o o o<br />
• Specification of appropriate pain scale tools for both cognitively intact and<br />
cognitively impaired residents<br />
o o o<br />
• Steps to be taken to monitor treatment effectiveness o o o<br />
• <strong>Pain</strong> treatment techniques based on clinically accepted guidelines, including<br />
non-pharmacological therapies<br />
o o o<br />
• Improving the resident’s well being by increasing comfort and reducing<br />
depression and anxiety<br />
o o o<br />
• Optimize the resident’s ability to perform ADLs and participate in activities o o o<br />
• Monitoring for side effects prevention/treatment related to the use of pain<br />
medication (i.e., constipation, nausea, vomiting, sedation, respiratory depression)<br />
o o o<br />
Does your facility’s policy address who, how, and when pain management program<br />
effectiveness should be monitored and evaluated?<br />
o o o<br />
Does your facility’s policy address a protocol for ongoing monitoring of pain? o o o<br />
Does your facility’s policy address a protocol for communication of reporting of pain<br />
to the designated MDS personnel to ensure correct coding?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________
<strong>Pain</strong>: <strong>Facility</strong> <strong>Assessment</strong> <strong>Checklists</strong> page of 8<br />
<strong>Pain</strong>: Assessing Staff Education and Training<br />
Does your facility’s education program for pain assessment and management include the following<br />
components?<br />
Yes<br />
No<br />
Needs<br />
Improvement<br />
Are new nursing staff assessed for their need for education on pain screening,<br />
assessment, and management?<br />
o o o<br />
Are current staff provided with ongoing education on the principles of pain<br />
management?<br />
o o o<br />
Does education staff provide discipline specific education for pain assessment and<br />
management?<br />
o o o<br />
Is there a designated clinical “expert” available at the facility to answer questions<br />
from all staff about pain assessment and management?<br />
o o o<br />
Does education take into consideration the personal, ethnic, cultural, and religious<br />
beliefs surrounding pain management?<br />
o o o<br />
Is the education provided at the appropriate level for the learner (i.e., CNA vs. RN)? o o o<br />
Does the education include staff training on documentation methods related to<br />
pain (i.e., location, duration, intensity, frequency, aggravating/alleviating factors,<br />
pain scales)?<br />
o o o<br />
Completed by:________________________________________<br />
Date:_______________________________<br />
Document available at www.primaris.org<br />
MO-06-15-PAIN July 2006 This material was prepared by <strong>Primaris</strong>, the Medicare Quality Improvement Organization for Missouri, under contract<br />
with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents<br />
presented do not necessarily reflect CMS policy.