Septic shock â Monitoring methods, parameters, end points
Septic shock â Monitoring methods, parameters, end points
Septic shock â Monitoring methods, parameters, end points
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
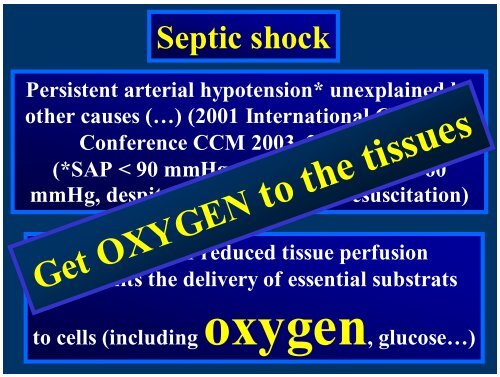
<strong>Septic</strong> <strong>shock</strong><br />
Persistent arterial hypotension* unexplained by<br />
other causes (…) (2001 International Consensus<br />
Conference CCM 2003, 31, 165-172)<br />
(*SAP < 90 mmHg, or 40 %, MAP < 60<br />
mmHg, despite adequate volume resuscitation)<br />
Syndrome of reduced tissue perfusion<br />
that limits the delivery of essential substrats<br />
Get OXYGEN to the tissues<br />
to cells (includingoxygen, glucose…)
<strong>Septic</strong> Shock : Outcome .<br />
Mortality : 35 to 70 %<br />
Annane et al Lancet 2005 , 365 , 63-78<br />
Mortality : 62 % (1990s) to 56 %<br />
in 2000<br />
Excess mortality : 39%<br />
Annane et al AJRCCM 2003 , 168 , 165-72
Severe sepsis/septic <strong>shock</strong><br />
Aims of treatment<br />
Correct . Macrocirculatory failure<br />
. Myocardial failure<br />
. Microcirculatory failure<br />
. Mitochondrial failure<br />
Restaure OXYGEN<br />
availability
Traditional End<strong>points</strong> of Resuscitation<br />
Resuscitation is complete when :<br />
- oxygen debt has been paid<br />
- tissue acidosis eliminated<br />
- aerobic metabolism restored<br />
How does the clinician know that ?<br />
Traditionally when :<br />
- blood pressure is normalized<br />
- heart rate is normalized<br />
- urine output is normalized<br />
correction of uncompensed <strong>shock</strong><br />
However…
Compensated <strong>shock</strong> may persists when<br />
signs of uncompensated <strong>shock</strong> are not<br />
present<br />
Suboptimal tissue perfusion and<br />
• lactate<br />
• SvO 2<br />
• pHi<br />
• … ??<br />
oxygenation
<strong>Septic</strong> Shock<br />
Absolute hypovolemia<br />
Relative hypovolemia<br />
Distributive <strong>shock</strong> :areas<br />
of VD/VC<br />
Cardiac dysfunction<br />
Impaired oxygen availability<br />
Get OXYGEN to the tissues
Initial Resuscitation<br />
MAP ≥ 65 mmHg<br />
CVP 8-12 mmHg ???<br />
UF ≥ 0.5 ml.kg -1 .hr -1<br />
ScvO ≥ 70%<br />
2<br />
SvO ≥ 65%<br />
2<br />
Surviving Sepsis Campaign 2008 Update CCM in press 2008
Task-force on Hemodynamic<br />
Support of Sepsis .<br />
Society of Critical Care Medicine<br />
2004 Update<br />
Crit Care Med 2004<br />
S. Hollenberg<br />
TS. Ahrens<br />
D. Annane<br />
ME. Astiz<br />
DB. Chalfin<br />
JF. Dasta<br />
C. Martin<br />
GM. Sulsa<br />
R. Totaro<br />
JL. Vincent<br />
S. Zanotti<br />
SO. Heard
yes<br />
Maintain<br />
established<br />
goals<br />
MAP at goal ?<br />
Adequate perfusion ?<br />
CVP<br />
PAC<br />
Adequate<br />
filling pressure ?<br />
yes<br />
Vasopressor :<br />
ΝΕ, dopamine<br />
no<br />
Fluid therapy
Surviving Sepsis Campaign –<br />
2008 Update<br />
Insert an arterial catheter (grade 1D)<br />
Use CVP or PAOP during fluid<br />
infusion<br />
No recomm<strong>end</strong>ation for PAC<br />
No recomm<strong>end</strong>ation for other devices<br />
No recomm<strong>end</strong>ation to monitor CI<br />
SCC 2008 CCM In Press 2008
Clinical<br />
signs<br />
Skin (color – temperature)<br />
Mental status ,capillary refill<br />
Laboratory<br />
<strong>parameters</strong><br />
Lactate WBC, ph, BE, PO 2<br />
Global<br />
Hemodynamics<br />
and oxygenation<br />
Local circulation<br />
Microcirculation<br />
MAP, PP,SVV,<br />
CI, DO 2, VO 2 , ScvO2<br />
Phi, gastric CO 2, urine flow<br />
Mitochondria
Clinical<br />
signs<br />
Skin (color – temperature)<br />
Mental status ,capillary refill<br />
Laboratory<br />
<strong>parameters</strong><br />
Lactate WBC, ph, BE, PO 2<br />
Global<br />
Hemodynamics<br />
and oxygenation<br />
Local circulation<br />
Microcirculation<br />
MAP, PP,SVV,<br />
CI,DO 2 ,VO 2 ScvO 2<br />
Phi, gastric CO 2, urine flow<br />
Mitochondria
Initial Resuscitation<br />
MAP ≥ 65 mmHg<br />
CVP 8-12 mmHg ???<br />
UF ≥ 0.5 ml.kg -1 .hr -1<br />
ScvO ≥ 70%<br />
2<br />
SvO ≥ 65% ?????<br />
2<br />
Surviving Sepsis Campaign 2008 Update CCM in press 2008
Fluid challenge<br />
Fluid challenge<br />
MAP<br />
(driving force)<br />
Venous return<br />
and ventricular preload<br />
SV<br />
blood flow
RAP (mmHg)<br />
before<br />
volume expansion<br />
20<br />
10<br />
Chest 2002, 121:2000-8<br />
responders<br />
Nonresponders<br />
*<br />
*<br />
0<br />
Calvin Schneider Reuse<br />
Wagner Michard<br />
1981 1988 1990 1998 2000<br />
number of pts 28 18 41 25 40<br />
SB pts (%) 54 33 24 6 0
Influence of Mechanical Ventilation on SAP<br />
Tavernier et al. Anesthesiology 1998; 89:1313-21
Guide to Fluid Therapy in <strong>Septic</strong> Shock<br />
25 patients with septic <strong>shock</strong><br />
Graded volume<br />
expansion : 500 mL increments<br />
Fluid loading: as long as<br />
CI ⇑ ≥15%<br />
Tavernier B et al. Anesthesiology 1998;89:1313-1321
Pulse Pressure Variations<br />
∆PP<br />
PPmax<br />
Michard et al.<br />
Am J Respir Crit Care Med<br />
2000<br />
PPmin
Am J Respir Crit Care Med 2000; 162:134-8<br />
100<br />
Sensitivity (%)<br />
80<br />
60<br />
40<br />
20<br />
ΔPP<br />
SPV<br />
RAP<br />
PAOP<br />
0<br />
0 20 40 60 80 100<br />
100- Specificity(%)
Stroke Volume Variation<br />
SV max<br />
SV min<br />
SV mean<br />
SVV =<br />
SV max + SV min<br />
2
Stroke volume variation as a pre dictor of fluid responsiveness in patients undergoing br ain surgery<br />
Berkenstadt H. Margalit N, Hadani M, Frie dman Z, Segal E, Vila Y, Perel A .<br />
Anesth Analg 2001;92:984-9<br />
1<br />
9.5 % Sensitivity = 79 %<br />
Specificity = 93 %<br />
sensitivity<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
SVV<br />
CVP<br />
0<br />
0 0.5 1<br />
1- specificity
Fluid Responsiveness in Patients with Severe Sepsis<br />
Evaluation of Stroke Volume Variations (SVV) induced by mechanical<br />
ventilation in patients with severe sepsis<br />
Pulsiocath ® and PICCO ® monitor<br />
Marx et al Eur J Anaesth 2004, 21, 132-138.
Global End-diastolic Volume<br />
Michard et al Chest 2003;124,1900-19O8
Response to Fluid Loading According<br />
Responsivness<br />
(%)<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
to GEDV<br />
< 500 < 550 < 600 < 645 > 645 > 700 > 750 > 800 > 850 > 900 > 950<br />
Intérêt de la thermodilution transpulmonaire pour guider le remplissage vasculaire au cours du choc<br />
septique<br />
Michard F, Alaya S, Richard C, Teboul JL. SRLF 2002
Cardiac Output<br />
High ? Low ?<br />
Adequate<br />
CI?<br />
SvO2 , ScvO2<br />
lactates<br />
pH i<br />
Clinical examination<br />
Inadequate
PiCCO Plus
SCHEMA D’INSTALLATION du PiCCO<br />
CVC<br />
standard<br />
injection du<br />
bolus<br />
robinet 3 voies<br />
standard<br />
Moniteur<br />
de<br />
surveillance<br />
12<br />
13<br />
0<br />
86<br />
70<br />
Pièce en T réf : P 4046<br />
détecteur de bolus T°c ambiante<br />
se trouvant dans le set de<br />
Pression PV 8015.<br />
Prise<br />
auxiliair<br />
PAS<br />
Câble auxiliaire de<br />
renvoi de courbe de P.A.<br />
Cathéter Artériel<br />
de<br />
Thermodilution<br />
Capteur de pression Pulsion<br />
set réf : PV 8015
PRINCIPE DU PULSE CONTOUR – 2<br />
Mesure en continu de la pression artérielle<br />
P [mm Hg]<br />
Intégration Automatique de la Calibration à l’Aire<br />
sous la Courbe de Pression Artérielle<br />
= Paramètres Mesurés en Continu, Beat to Beat<br />
t [s]
Stroke Volume Variation<br />
SV max<br />
SV min<br />
SV mean<br />
SVV =<br />
SV max + SV min<br />
2
Global End-diastolic Volume<br />
By Thermodilution
Fluid challenge<br />
500 ml (7 ml/kg)<br />
(either colloid or crystalloid<br />
20 – 30 min
Fluid challenge<br />
French Consensus Conference 2005<br />
Respiratory variation under MV<br />
Parameter<br />
threshold<br />
ΔSAP<br />
Δdown<br />
ΔPP<br />
SVV<br />
10 mmHg or 9%<br />
5 mmHg<br />
12-13 %<br />
9-10%<br />
CVP<br />
< 5 mmHg
32 patients randomized : dopamine (Until<br />
25 µg/kg/min)<br />
or norepi ( Until 5 µg/kg/min)<br />
Objectif : PAM > 80 mmHg 6 h<br />
Dopa (n=16)<br />
Norepi (n=16)<br />
success (n=5)<br />
échec (n=11)<br />
success (n=15)<br />
failure (n=1)<br />
10 to 25 µg/kg/min<br />
25 µg/kg/min<br />
1.5±1.21.2 µg/kg/min<br />
5 µg/kg/min<br />
increase in urine output<br />
decrease in lactate<br />
increase in urine output<br />
decrease in lactate<br />
10 success with Dopa + Norepi (25 µg/kg/min +1.7±1.8 1.8 µg/kg/min)<br />
increase in urine output<br />
and decrease in lactate<br />
Chest 1993, 103:1826-<br />
31
Resistance to Dopamine<br />
110 patients<br />
MAP < 70 mmHg with 20 μg/kg/min<br />
60%<br />
40%<br />
P < 0.001<br />
Dopa S<br />
Dopa R<br />
Levy et al CCM 2005, 33.
65 85
Lactate<br />
Increasing MAP ?<br />
65 85<br />
DO2<br />
VO2<br />
A Bourgoin et al<br />
CCM 2005,33,780-786
UF<br />
Increasing MAP ?<br />
65<br />
Creatinine<br />
85<br />
Cr Cl<br />
A Bourgoin et al<br />
CCM 2005,33,780-786
MAP :<br />
65 mmHg
<strong>Septic</strong> <strong>shock</strong>. Inotropic Therapy<br />
. Dobutamine is the first<br />
choice for patients with low CO<br />
(< 2.5 l/min/m2)<br />
<br />
after fluid resuscitation<br />
after an adequate MAP<br />
(Level<br />
. Dobutamine<br />
E)<br />
may cause hypotension<br />
and /or tachycardia in some patients:<br />
especially those with low filling<br />
pressure<br />
Task Force of the SCCM. Crit. Care Med 2004,32,1928-1948
Global OXYGEN<br />
availability<br />
ScvO 2<br />
SvO 2
SvO 2 ScvO 2<br />
AP<br />
TaO2<br />
(IC Hb SaO2)<br />
VO 2<br />
EO 2
Rivers et al NEJM, 2001, 345, 1368-1377<br />
« Early Goal-directed Therapy »<br />
263 patients :<br />
. Severe sepsis<br />
. <strong>Septic</strong> <strong>shock</strong><br />
ECG, SpO 2 , UF<br />
Art cath , CVC<br />
Standard treatment<br />
n = 133<br />
CVP 8 -12 mmHg<br />
MAP > 65 mmHg<br />
UF > 0.5 ml/kg/h<br />
For 6 hours<br />
Protocol<br />
n = 130<br />
idem + ScvO 2 > 70%<br />
SaO 2 > 93%<br />
HT> 30 %
ADDING DOBUTAMINE TO<br />
NOREPINEPHRINE ?<br />
Open circles :Pco2 gap <<br />
8 mmHg<br />
Solid circles : Pco2 gap ><br />
8 mmHg<br />
Levy et al CCM 1997 , 25 ,<br />
1649 .
ADDING DOBUTAMINE TO NOREPINEPHRINE ?<br />
Open circles :<br />
Pco2 gap < 8 mmHg<br />
Solid circles :<br />
Pco2 gap > 8 mmHg<br />
Levy et al CCM 1997, 25 ,1649 .
Macrocirculation and MOF<br />
The density of<br />
perfused small<br />
(< 20 µm) vessels<br />
is reduced in<br />
septic patients<br />
(OPS)<br />
De Backer et al AJRCCM 2002, 166, 98-104
MicrocirculationAlteration and Outcome<br />
Sakr et al CCM 2004 , 32 , 1825-1831
Initial Resuscitation<br />
MAP ≥ 65 mmHg<br />
CVP 8-12 mmHg ???<br />
dPP , SVV 5-7%<br />
UF ≥ 0.5 ml.kg -1 .hr -1<br />
ScvO ≥ 70%<br />
2<br />
SvO ≥ 65% ?????<br />
2
Clinical<br />
signs<br />
Skin (color – temperature)<br />
Mental status ,capillary refill<br />
Laboratory<br />
<strong>parameters</strong><br />
Lactate WBC, ph, BE, PO 2<br />
Global<br />
Hemodynamics<br />
and oxygenation<br />
Local circulation<br />
Microcirculation<br />
MAP, PP,SVV,<br />
CI,DO 2 ,VO 2 ScvO 2<br />
Phi, gastric CO 2, urine flow<br />
Mitochondria
O 2
ATP is life