Successful Dentures Part II - Removable Prosthodontics
Successful Dentures Part II - Removable Prosthodontics
Successful Dentures Part II - Removable Prosthodontics
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Secrets to <strong>Successful</strong> <strong>Dentures</strong><br />
<strong>Part</strong> <strong>II</strong><br />
Dalhousie Continuing Education<br />
Dr. Mark Vallee BSc MS DDS DP FRCDC<br />
Topics<br />
Conventional Denture Treatment:<br />
Trends in removable prosthodontics.<br />
Anatomy<br />
Maxillo-Mandibular Relationship<br />
Vertical Dimension<br />
Tooth Selection, Arrangement, and Occlusion<br />
Implant Supported Overdentures:<br />
Overdenture abutments<br />
Implant Placement<br />
Locator Abutments<br />
Converting a denture into an overdenture.<br />
Direct Pickup<br />
Trends in <strong>Removable</strong><br />
<strong>Prosthodontics</strong><br />
Conventional Denture Treatment<br />
Patient Demographics<br />
Esthetic Awareness<br />
Implant treatment<br />
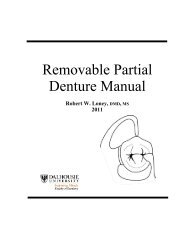
Patient Demographics<br />
Average lifespan of patients:<br />
14<br />
Patient Demographics<br />
60<br />
13<br />
Percent Edentulous<br />
18+ yrs old<br />
50<br />
Percent Edentulous<br />
65+ yrs old<br />
Percent<br />
12<br />
11<br />
40<br />
10<br />
1960 1970 1980 1990<br />
30<br />
1960 1970 1980 1990<br />
Trends in tooth loss
Patient Demographics<br />
Will there be a need for complete dentures in<br />
2020?<br />
Complete dentures patients will increase from<br />
33.6 million adults in 1991 to 37.9 million adults in<br />
2020.<br />
The 10% decline in edentulism experienced each<br />
decade for the past 30 years will be more than<br />
offset by the 71% increase in the adult population<br />
older than 55 years.<br />
Esthetic Awareness<br />
Esthetic Awareness<br />
Implant Treatment<br />
An increase in esthetic awareness has prompted<br />
an increase in patient demand for quality<br />
removable prosthodontic restorative treatment.<br />
Out of 33 million edentulous patients only 2-4% have received<br />
implant treatment<br />
Estimated 60% of patients are NOT given implants as a<br />
treatment option<br />
Implant supported overdentures are now the standard of care for<br />
the edentulous mandible<br />
Anatomy<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
e<br />
d<br />
f<br />
i<br />
a<br />
l<br />
g<br />
k<br />
j<br />
h<br />
c<br />
d<br />
m<br />
b<br />
a. Labial frenum<br />
b. Buccal frenum<br />
c. Labial vestibule<br />
d. Anterior buccal vestibule<br />
e. Posterior buccal vestibule<br />
•Retrozygomatic space<br />
•Coronoid bulge<br />
f. Hamular notch<br />
•Pterygomaxillary notch<br />
g. Fovea palatini<br />
h. Vibrating line<br />
i. Residual alveolar ridge<br />
j. Palatal rugae<br />
k. Incisive papilla<br />
l. Median palatine raphe<br />
m. Maxillary tuberosity
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
e<br />
d<br />
f<br />
i<br />
a<br />
c<br />
k<br />
j<br />
l<br />
g h<br />
d<br />
m<br />
b<br />
a. Labial frenum<br />
•Fold of mucous membrane<br />
•Does not contain muscle<br />
•Labial notch in denture is<br />
narrow<br />
b. Buccal frenum<br />
•Overlies levator anguli oris<br />
•May be moved in an A-P<br />
direction by the actions of the<br />
orbicularis oris and buccinator<br />
e<br />
d<br />
f<br />
i<br />
a<br />
c<br />
k<br />
j<br />
l<br />
g h<br />
d<br />
m<br />
b<br />
c. Labial vestibule<br />
•Reflection contains no muscle<br />
d. Anterior buccal vestibule<br />
•Overlies buccinator muscle<br />
whose fibers are downward and<br />
forward and limit the height and<br />
thickness of the buccal flange<br />
e. Posterior buccal vestibule<br />
•Thickness determined by the<br />
masseter muscle<br />
•Coronoid process of the<br />
mandible encroaches on the<br />
space during lateral excursions<br />
•Labial and buccal flanges of the<br />
denture must contact movable tissues<br />
in order to make a seal<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
e<br />
d<br />
f<br />
i<br />
a<br />
l<br />
g<br />
k<br />
j<br />
h<br />
c<br />
d<br />
m<br />
b<br />
f. Hamular notch<br />
•Pterygomaxillary notch<br />
•Does not contain any<br />
muscles or ligaments to<br />
interfere with the addition<br />
of pressure with a<br />
postdam<br />
g. Fovea palatini<br />
•2 small pits representing<br />
mucous gland openings<br />
•Usually located just<br />
posterior to the vibrating<br />
line<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
e<br />
d<br />
f<br />
i<br />
a<br />
l<br />
g<br />
k<br />
j<br />
h<br />
c<br />
d<br />
m<br />
b<br />
h. Vibrating line<br />
•Imaginary line across palate<br />
•Connects the<br />
pterygomaxillary notches<br />
Posterior Palatal Seal<br />
•Area not a line<br />
•Functions: border seal, prevent food<br />
impaction beneath, improve retention,<br />
compensate for shrinkage of denture<br />
resin<br />
•Pressure on displaceable mucosa that<br />
covers palatal glands<br />
•Anterior border – junction between<br />
hard and soft palate; ‘blow’ line<br />
•Posterior border (vibrating line) –<br />
junction between movable and<br />
immovable soft palate; ‘ah’ line<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Maxilla<br />
e<br />
d<br />
f<br />
i<br />
a<br />
c<br />
k<br />
j<br />
l<br />
g h<br />
d<br />
m<br />
b<br />
Denture bearing areas<br />
i. Residual alveolar ridge<br />
•Crest is primary stress<br />
bearing area<br />
•Fibrous CT least<br />
displaceable and best<br />
able to carry the stress of<br />
mastication<br />
j. Palatal rugae<br />
•Secondary stress<br />
bearing area<br />
e<br />
d<br />
f<br />
i<br />
a<br />
c<br />
k<br />
j<br />
l<br />
g h<br />
d<br />
m<br />
b<br />
k. Incisive papilla<br />
•Guards the incisive<br />
canal<br />
•Pressure will interfere<br />
with the blood and nerve<br />
supply causing a burning<br />
sensation<br />
•Provide relief<br />
l. Median palatine raphe
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
a<br />
d<br />
i<br />
h<br />
e<br />
a. Labial frenum<br />
b. Buccal frenum<br />
c. Lingual frenum<br />
d. Labial vestibule<br />
e. Buccal vestibule<br />
f. Residual alveolar ridge<br />
g. Buccal shelf<br />
h. Retromolar pad<br />
i. Pterygomandibular raphe<br />
j. Mylohyoid ridge<br />
k. Alveololingual sulcus<br />
l. Retromylohyoid space<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
a<br />
d<br />
i<br />
h<br />
e<br />
a. Labial frenum<br />
•Fold of mucous<br />
membrane<br />
•Does not contain muscle<br />
b. Buccal frenum<br />
•Overlies depressor<br />
anguli oris (V<strong>II</strong>)<br />
•Movable by the<br />
buccinator and orbicularis<br />
oris (V<strong>II</strong>) resulting in a<br />
wide notch in the denture<br />
c. Lingual frenum<br />
•Overlies genioglossus<br />
muscle (X<strong>II</strong>)<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
Denture bearing areas<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
a<br />
d<br />
i<br />
h<br />
e<br />
d. Labial vestibule<br />
e. Buccal vestibule<br />
•Entire periphery of denture<br />
must end in soft tissues<br />
•Stability of denture must<br />
come from the maximum use<br />
of all bony foundations where<br />
tissues are firmly and closely<br />
attached to bone<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
a<br />
d<br />
i<br />
h<br />
e<br />
f. Residual alveolar ridge<br />
g. Buccal shelf<br />
•Bounded laterally by the<br />
external oblique ridge and<br />
medially by the crest of the<br />
ridge<br />
•Attachment of buccinator<br />
muscle (V<strong>II</strong>)<br />
•Buccal flange rests upon<br />
buccinator and should extend<br />
as far as the tissues permit<br />
•Masseter muscle (V3) may<br />
crowd buccinator forward<br />
against the denture causing an<br />
indentation at the DB angle<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
a<br />
d<br />
i<br />
h<br />
e<br />
h. Retromolar pad<br />
•Contains:<br />
•Retromolar gland<br />
•Pterygomandibular<br />
raphe<br />
•Buccinator muscle<br />
•Temporal tendon<br />
•Underlying basal bone is<br />
resistant to resorption<br />
•Coverage will provide some<br />
border seal<br />
i. Pterygomandibular raphe<br />
•Extends from the pterygoid<br />
hamulus superiorly to the<br />
alveolar ridge inferiorly under<br />
the retromolar gland<br />
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
a<br />
d<br />
i<br />
h<br />
e<br />
j. Mylohyoid ridge<br />
•Attachment of mylohyoid<br />
muscle (V3) which forms the<br />
muscular floor of the mouth<br />
•Fibers are almost horizontal in<br />
front of the hyoid where they join<br />
those of the opposite side to<br />
form a raphe<br />
•At the level of the hyoid they<br />
pass almost vertically downward<br />
to insert into the hyoid<br />
k. Alveololingual sulcus<br />
•Slopes toward the tongue to<br />
permit action of the mylohyoid<br />
•Length of flange distally<br />
compared to anteriorly is greater<br />
owing to the changed length and<br />
direction of the mylohyoid fibers
Anatomy in Relation to Complete<br />
<strong>Dentures</strong><br />
Edentulous Mandible<br />
Panoramic Radiograph<br />
g<br />
b<br />
l<br />
f<br />
j<br />
k<br />
c<br />
i<br />
h<br />
e<br />
l. Retromylohyoid space<br />
•DL extension determined<br />
by styloglossus (X<strong>II</strong>)<br />
•Posterolateral extension<br />
determined by superior<br />
pharyngeal constrictor (X)<br />
and palatoglossus (X)<br />
•Overextension may<br />
cause pain on swallowing<br />
a<br />
d<br />
Mandibular Condyle<br />
Coronoid Process of mandible<br />
Glenoid Fossa<br />
Maxillary Tuberosity<br />
Nasal Septum<br />
Pterygomaxillary Fissure<br />
EAM<br />
Articular Eminence<br />
Anterior Nasal Spine<br />
Hard Palate<br />
Orbit<br />
Zygomatic Arch<br />
Maxillo-Mandibular Relationship<br />
Pharynx<br />
Lip Lines<br />
Earlobe<br />
Mental Foramen<br />
Mandibular Foramen<br />
Shadow of tongue<br />
Styloid Process<br />
Symphysis<br />
Mandibular Canal<br />
External Oblique Ridge<br />
Cervical Vertebrae<br />
Hyoid Bone<br />
Facial Artery Notch<br />
Maxillary Relations<br />
Incisal Display<br />
Dental Midline<br />
Occlusal Plane Orientation<br />
Facebow<br />
Maxillary Relations<br />
Natural Dentition<br />
Incisal edge of central<br />
incisor in relation to<br />
the lip line at rest<br />
Young woman – 3 mm<br />
below lip line at rest<br />
Young man – 2 mm<br />
below lip line at rest<br />
Middle age – 1.5 mm<br />
below lip line at rest<br />
Elderly (>80) – 0 mm<br />
below to 2 mm above<br />
lip line at rest<br />
Incisal Display at Rest<br />
Rest After Wax Adjustment<br />
Maximum Smile After Wax<br />
Adjustment
Maxillary Relations<br />
Dental Midline<br />
Maxillary Relations<br />
Dental Midline<br />
Rest After<br />
Smile After<br />
Maxillary Relations<br />
Dental Midline<br />
Maxillary Relations<br />
Occlusal Plane Orientation<br />
Frontal Plane<br />
Parallel to<br />
interpupillary line<br />
Fox Plane<br />
Maxillary Relations<br />
Occlusal Plane Orientation<br />
Maxillary Relations<br />
Occlusal Plane Orientation<br />
Sagittal Plane<br />
Parallel to Camper’s Line<br />
Inferior border of the ala of<br />
the nose to the superior<br />
border of the tragus of the<br />
ear<br />
Frankfort horizontal plane<br />
Orientation to the external<br />
auditory meatus and<br />
orbitale<br />
Cephalometric landmark<br />
FHP<br />
CL<br />
OP
Mandibular Relations<br />
Vertical Dimension<br />
Centric Relation<br />
Vertical Dimension<br />
Adjust occlusal plane<br />
Parallel to maxillary rim<br />
Clinical assessment of vertical<br />
dimension<br />
Anatomic landmarks<br />
Physiologic rest position<br />
Pre-extraction records<br />
Existing prosthesis<br />
Esthetics<br />
Phonetics<br />
Swallowing<br />
Average occlusal rim<br />
dimensions<br />
Vertical Dimension<br />
Anatomic Landmarks<br />
2/3 up the height of the retromolar pad<br />
Vertical Dimension<br />
Anatomic Landmarks<br />
Level with the lower lip<br />
at rest<br />
Vertical Dimension<br />
Esthetics<br />
Vertical Dimension<br />
Phonetics<br />
‘S’<br />
‘F’<br />
‘Ch’<br />
‘M’
Vertical Dimension<br />
Swallowing<br />
Vertical Dimension<br />
Average Occlusal Rim Dimensions<br />
During swallowing<br />
After swallowing<br />
Maxillary – 22 mm<br />
Mandibular – 18 mm<br />
Tooth Selection<br />
Anterior Tooth Selection<br />
Anterior Tooth Selection<br />
Anterior teeth are<br />
primarily selected to<br />
satisfy esthetic<br />
requirements<br />
Posterior teeth are<br />
primarily selected to<br />
satisfy masticatory<br />
requirements/<br />
occlusion<br />
Anterior Tooth Selection<br />
Guides<br />
Pre-extraction records<br />
Photos, diagnostic<br />
casts, old radiographs<br />
Existing dentures<br />
Patient’s facial<br />
characteristics<br />
Patient’s gender,<br />
personality, age<br />
Arch size and shape<br />
Patient’s preferences<br />
Anterior Tooth Selection<br />
Shape<br />
Square, tapering,<br />
ovoid<br />
Size<br />
Length, width,<br />
circumference<br />
Shade
Anterior Tooth Selection<br />
Shape<br />
Anterior Tooth Selection<br />
Shape<br />
Dentogenics concept<br />
Gender<br />
Male – rugged with square teeth<br />
and bold central incisors<br />
Female – pronounced<br />
curvatures, rounded point angles<br />
Personality<br />
Vigorous or delicate – maxillary<br />
lateral varies more in size, form,<br />
and position<br />
Age<br />
Young – tapered, ovoid, rounded<br />
teeth<br />
Middle – somewhere between<br />
young/old<br />
Old – square, sharp corners<br />
Ovoid<br />
Pronounced gingivo-incisal<br />
curvature which tends to<br />
disperse light and create a<br />
softened appearance<br />
Square<br />
Tapering<br />
Rounded contours which<br />
taper towards the cervical<br />
ridge<br />
Moderate gingivo-incisal<br />
curvature<br />
Central incisor is dominant and gingivo-incisal curvature is<br />
moderate<br />
Offers maximum light deflection and creates a bold effect<br />
50<br />
Anterior Tooth Selection<br />
Size<br />
Anterior Tooth Selection<br />
Size<br />
Width of 6 anteriors<br />
on a curve<br />
Average 46-56 mm<br />
Wax rim & ruler<br />
•Commissure of lips represents distal surface of canine<br />
Anterior Tooth Selection<br />
Size<br />
Anterior Tooth Selection<br />
Size<br />
Major rugae of palate points to canine position<br />
Exaggerated Smile<br />
Length<br />
High smile – 11%<br />
Reveals total length of<br />
maxillary anterior teeth and a<br />
continuous band of gingiva<br />
Average smile – 69%<br />
Reveals 75-100% of<br />
maxillary anterior teeth and<br />
interproximal gingiva only<br />
Low smile – 20%<br />
Displays less than 75% of<br />
maxillary anterior teeth
Anterior Tooth Selection<br />
Commercial Products<br />
Size & Shape<br />
Anterior Tooth Selection<br />
Determine the facial<br />
outline<br />
Compare form of face<br />
to vertical lines<br />
Square tapering<br />
Determine the size of<br />
the maxillary central<br />
Indicator is<br />
proportioned in a ratio<br />
of 16:1<br />
Width – 9.25 mm<br />
Length – 11 mm<br />
Size & Shape<br />
Length<br />
Width<br />
56<br />
Anterior Tooth Selection<br />
Size & Shape<br />
Take a picture<br />
Insert it into a program<br />
Anterior Tooth Selection<br />
Portrait shade guide<br />
Shade<br />
57<br />
Anterior Tooth Selection<br />
Aim to harmonize<br />
between color of the<br />
skin, hair, & eyes<br />
Guides<br />
Complexion<br />
Hair color<br />
Eye color<br />
Age<br />
Personality & activity<br />
Patient desires<br />
Need to educate patients<br />
Shade<br />
Anterior Tooth Arrangement<br />
Position has been tentatively established during the<br />
clinical refinement of the maxillary occlusal rim<br />
Adequate lip support<br />
Proper phonetics
Anterior Tooth Arrangement<br />
General Arrangement<br />
Considerations<br />
Anterior teeth are set primarily<br />
for esthetics not function<br />
Considering creating<br />
asymmetry after discussion<br />
with patient<br />
Each tooth should appear as<br />
an individual tooth<br />
Gingival 1/3 of maxillary<br />
incisors provide lip support<br />
Incisal 1/3 of maxillary incisors<br />
provides esthetics<br />
Maxillary anterior teeth are set<br />
on the smile line<br />
61<br />
Maxillary Anterior Tooth<br />
Arrangement<br />
Central<br />
Labial surfaces flush with wax rim<br />
contour<br />
Long axis slightly distal to<br />
perpendicular<br />
Incisal edge is at occlusal plane<br />
Lateral<br />
<br />
Long axis at an angle more distal<br />
than central<br />
Incisal edge is slightly above<br />
occlusal plane<br />
Canine<br />
Long axis at a more distal angle<br />
than lateral<br />
Cervical is prominent, incisal<br />
edge looks tucked-in<br />
Incisal edge is at occlusal plane<br />
62<br />
Maxillary Anterior Tooth<br />
Arrangement<br />
Maxillary Anterior Tooth<br />
Arrangement<br />
• Labial surface of the centrals usually 5-7mm anterior to incisal papilla<br />
Maxillary Anterior Tooth<br />
Arrangement<br />
Golden Proportion<br />
Ratio of 1.618:1<br />
Proportion between a<br />
larger part and a smaller<br />
part<br />
Width of the central<br />
incisor is in the golden<br />
proportion to the width of<br />
the lateral incisor<br />
Maxillary Anterior Tooth<br />
Arrangement<br />
Esthetics of natural<br />
teeth<br />
Avoid lampshade<br />
convergence of roots!<br />
65<br />
66
Mandibular Anterior Tooth<br />
Arrangement<br />
Mandibular Anterior Tooth<br />
Arrangement<br />
• Teeth are set over bone<br />
Anterior Tooth Arrangement<br />
Anterior Tooth Arrangement<br />
• 2-3 mm Overjet<br />
• 0 mm Overbite<br />
Tooth Selection<br />
Posterior Tooth Selection<br />
Goals of Complete Denture<br />
Occlusion<br />
Minimize trauma to the<br />
supporting structures<br />
Preserve remaining<br />
structures<br />
Enhance stability of the<br />
dentures<br />
Facilitate esthetics and<br />
speech<br />
Restore mastication<br />
efficiency to a reasonable<br />
level<br />
Decrease lateral forces to<br />
the residual ridges<br />
Right Working<br />
Left Working
General Concepts of Denture<br />
Occlusion<br />
Occlusal Spectrum<br />
Common Features<br />
Functional anatomy is the main<br />
determinant of denture tooth<br />
position<br />
Simultaneous, bilateral posterior<br />
contact in centric relation<br />
Centralization of centric occlusal<br />
forces over the mandibular<br />
residual ridges<br />
Buccal-lingually<br />
Anterior-posteriorly<br />
Centric Relation<br />
Anatomic<br />
Balanced occlusion<br />
Lingualized<br />
Balanced occlusion<br />
Non-balanced occlusion<br />
Non-anatomic (Monoplane)<br />
Balanced occlusion<br />
Non-balanced occlusion<br />
Neutrocentric<br />
Occlusal Spectrum<br />
Lingualized<br />
(lingual contact)<br />
semianatomic<br />
nonanatomic<br />
(balancing<br />
ramp)<br />
Posterior Tooth Selection<br />
Criteria<br />
Resorbed or flabby ridges<br />
Physical condition of the patient<br />
Patients who clench or brux<br />
Previous denture occlusion<br />
Ridge relationship<br />
Immediate dentures<br />
Opposing arch<br />
anatomic<br />
nonanatomic<br />
Posterior Tooth Selection<br />
Indications<br />
Posterior Tooth Selection<br />
Indications<br />
Anatomic<br />
Non-anatomic<br />
Anatomic<br />
Non-anatomic<br />
Good residual ridges<br />
Well coordinated patient<br />
Previously successful with<br />
anatomic dentures<br />
Class I ridge relationship<br />
Denture opposes natural<br />
dentition<br />
When “Lingualized”<br />
occlusion is desired<br />
Poor residual ridges<br />
Poor neuromuscular control<br />
(Bruxers, CP, etc.)<br />
Previously successful with<br />
monoplane dentures or<br />
severely worn occlusion on<br />
previous denture<br />
Arch discrepancies<br />
Class <strong>II</strong> or <strong>II</strong>I or cross-bite<br />
Good residual ridges<br />
Poor residual ridges<br />
Immediate dentures<br />
Except when opposing natural<br />
dentition<br />
Potential poor follow-up
Posterior Tooth Selection<br />
Indications<br />
Posterior Tooth Selection<br />
Indications<br />
Anatomic<br />
Non-anatomic<br />
Anatomic<br />
Non-anatomic<br />
Well coordinated patient<br />
Poor neuromuscular control<br />
(Bruxers, CP, etc.)<br />
Previously successful with<br />
anatomic dentures<br />
Previously successful with<br />
monoplane dentures or<br />
severely worn occlusion on<br />
previous denture<br />
Posterior Tooth Selection<br />
Indications<br />
Posterior Tooth Selection<br />
Indications<br />
Anatomic<br />
Non-anatomic<br />
Anatomic<br />
Non-anatomic<br />
Class I ridge relationship<br />
Arch discrepancies<br />
› Class <strong>II</strong> or <strong>II</strong>I or cross-bite<br />
Denture opposes natural<br />
dentition<br />
Immediate dentures<br />
› Except when opposing natural<br />
dentition<br />
Anatomic Occlusion<br />
Lingualized Occlusion<br />
Advantages<br />
Definite point of positive<br />
intercuspation may be<br />
developed<br />
Esthetically similar to natural<br />
dentition<br />
Tooth-to-tooth and cusp-tocusp<br />
balanced occlusion can<br />
be achieved<br />
Maintains some shearing<br />
ability after moderate wear<br />
Disadvantages<br />
Difficult to set<br />
Less adaptable to arch<br />
relation discrepancies<br />
Horizontal force<br />
development due to cusp<br />
inclinations<br />
Harmonious balanced<br />
occlusion is lost with denture<br />
base settling<br />
Requires frequent follow-up<br />
and may require more<br />
frequent relines to maintain<br />
proper occlusion<br />
Indications<br />
High esthetic demands<br />
Severe mandibular ridge<br />
atrophy<br />
Displaceable supporting<br />
tissues<br />
Malocclusion<br />
Previous successful denture<br />
with lingualized occlusion<br />
Advantages<br />
Good esthetics<br />
Freedom of non-anatomic<br />
teeth<br />
Potential for bilateral balance<br />
Centralizes vertical forces<br />
Minimizes tipping forces<br />
Facilitates bolus penetration<br />
(mortar and pestle effect)
Non-Anatomic Occlusion<br />
Is ‘Balance’ Necessary?<br />
Advantages<br />
Reduction of horizontal<br />
forces<br />
CR can be developed as an<br />
area instead of a point<br />
Freedom of movement<br />
Can develop solid occlusion<br />
despite arch alignment<br />
discrepancies<br />
Easily adapted to situations<br />
prone to denture base<br />
shifting<br />
Easy to set and adjust teeth<br />
Disadvantages<br />
No vertical component to aid<br />
in shearing during<br />
mastication<br />
Occlusal adjustment impairs<br />
efficiency unless spillways<br />
and cutting edges restored<br />
Patients may complain of<br />
lack of positive<br />
intercuspation position<br />
Somewhat esthetically<br />
limited (don’t look like natural<br />
teeth)<br />
“Bolus in”<br />
“Balance out”<br />
Complete Denture Occlusion<br />
Investigators have not shown one<br />
type of denture occlusion to be:<br />
Superior in function<br />
Safer to oral structures<br />
More acceptable to patients<br />
Neuromuscular control may be<br />
the single most significant factor<br />
in the successful manipulation of<br />
complete dentures under function<br />
Tongue function and denture<br />
wearing experience<br />
Posterior Landmarks<br />
Landmarks for the Arrangement of Posterior Denture<br />
Teeth<br />
Crest of the ridge<br />
Mandibular posterior teeth<br />
are centered over the ridge<br />
Medial/lateral<br />
Retromolar pad<br />
Medial/lateral<br />
Superior/inferior<br />
2/3 height retromolar pad<br />
88<br />
Posterior Landmarks<br />
Mandibular Posterior Tooth<br />
Arrangement<br />
Three landmarks used to determine the plane of occlusion:<br />
Retromolar pad<br />
2/3 height retromolar pad<br />
Incisal edge of the<br />
mandibular central incisor<br />
90
Mandibular Posterior Tooth<br />
Arrangement<br />
Mandibular Posterior Tooth<br />
Arrangement<br />
Horizontal Plane<br />
Pound’s triangle<br />
Lingual aspect of mandibular teeth should be positioned within<br />
a triangle created by drawing 2 lines from the mesial aspect<br />
of the canine to each side of the retromolar pad<br />
Horizontal Plane<br />
Central groove of denture teeth centered over the crest of the<br />
ridge<br />
91<br />
92<br />
Mandibular Posterior Tooth<br />
Arrangement<br />
Mandibular Posterior Tooth<br />
Arrangement<br />
Sagittal Plane<br />
Boucher<br />
Occlusal plane of mandibular arch should be established at ⅔<br />
height of the retromolar pad<br />
Teeth are not set on the ascending area of the mandibular ridge<br />
or the retromolar pad<br />
Otherwise the mandibular denture tends to shift forward<br />
Sagittal Plane<br />
Long axes of the teeth are perpendicular to the occlusal plane<br />
Marginal ridges of adjacent teeth should be at the same level<br />
93<br />
94<br />
Mandibular Posterior Tooth<br />
Arrangement<br />
Mandibular Posterior Tooth<br />
Arrangement<br />
Frontal Plane<br />
Facial view<br />
Buccal and lingual cusps should contact the occlusal plane<br />
analyzer<br />
Frontal Plane<br />
Lingual view<br />
Buccal and lingual cusps should contact the occlusal plane<br />
analyzer<br />
95<br />
96
Maxillary Posterior Tooth<br />
Arrangement<br />
Maxillary Posterior Tooth<br />
Arrangement<br />
Lingual cusps should be<br />
set over central fossa of<br />
mandibular teeth<br />
Teeth should be set up<br />
to, but not on top of, the<br />
tuberosity<br />
Teeth should not extend<br />
beyond the denture base<br />
periphery on the facial<br />
97<br />
98<br />
Implant Supported Overdentures<br />
Conventional <strong>Dentures</strong><br />
Tooth loss increases with age<br />
the number of edentulous people will continue to increase for<br />
several decades because of the increase in mean age.<br />
Complete dentures have been the traditional standard of<br />
care for edentulous patients for more than a century.<br />
Complete denture wearers are usually able to wear an<br />
upper denture without problems, but many struggle with<br />
the complete lower denture because they are loose.<br />
Conventional dentures have a bite force of 25% and 20%<br />
chewing efficiency of natural teeth.<br />
Patient Demographics<br />
Dissatisfied<br />
7.7 %<br />
Moderately<br />
Fully Satisfied<br />
Satisfied<br />
66.7 %<br />
25.6 %<br />
Patient satisfaction also depends upon<br />
expectations and some patients may have very<br />
unrealistic expectations. For this reason it is<br />
important to guide and educate the patient.<br />
Implant Supported Overdentures<br />
Patients are significantly more satisfied with 2-implant<br />
overdentures than with new conventional dentures<br />
regardless of the type of attachment system used<br />
bar, ball, magnet, locator.<br />
Implant overdentures increase the bite force to 60%<br />
of natural teeth.<br />
Patients find implant overdentures significantly more<br />
stable,<br />
their ability to chew various foods are significantly<br />
easier,<br />
they are more comfortable<br />
and speak more easily.
Implant Supported Overdentures<br />
Studies of several populations have shown that ratings of<br />
quality of life are significantly higher for patients who<br />
receive 2-implant mandibular overdentures opposing<br />
complete maxillary conventional dentures than for those<br />
with conventional dentures.<br />
People who receive mandibular 2-implant overdentures<br />
modify their diets which improves their nutritional state.<br />
Such improvements may have a strong positive impact on<br />
general health, particularly for senior adults who are<br />
vulnerable to malnutrition.<br />
2-implant overdenture are becoming the first choice of<br />
treatment for the edentulous mandible.<br />
Overdenture Attachments<br />
Ball attachments<br />
Ball and rubber o-rings and/or metal housings<br />
Used to be the attachment of choice<br />
Wear quickly, not as retentive<br />
Overdenture Attachments<br />
Overdenture Attachments<br />
Bar Attachments<br />
1-3 bars with 1-3 clips<br />
Retentive at first, get loose or break over time.<br />
Hard to adjust and fix<br />
Not as popular anymore<br />
Locator<br />
Lowest vertical height of 3.17mm.<br />
Self aligning<br />
Durable<br />
Up to 40° angle correction<br />
Retention flexibility<br />
Overdenture Attachments<br />
Fixed Full-arch Restorations<br />
Can also have a bar with locators cast or tapped into the framework.<br />
Usually have 3 - 4 locators incorporated.<br />
Framework can be gold (cast) or titanium (milled).<br />
Framework must be passively attached to the implants.<br />
Returns the bite-force of the edentulous to approximately 80% of natural<br />
teeth.<br />
Implant supported and retained.<br />
Returns the bite-force of the edentulous pt close to natural teeth<br />
Must have enough space for restoration, minimum of 10mm.<br />
Framework can be gold (cast), titanium or zirconia (milled).<br />
Prosthesis can be metal-ceramic, or metal-acrylic.<br />
Framework must be passive.<br />
Patient must be able to clean underneath framework<br />
Implant supported and retained.
External-hex and Internal-hex<br />
External-hex Implants<br />
More common in the past<br />
Good for multiple unit restorations<br />
Rely more on the screw for retention of<br />
single unit restorations.<br />
Internal-hex Implants<br />
More common now<br />
Good for single tooth restorations<br />
Can use for multiple unit restorations -<br />
cement retained or need specific<br />
abutments.<br />
Rely more on the connection for<br />
retention of single unit restorations.<br />
Overdenture Attachments<br />
Md Implants usually placed in position of:<br />
2 implants - 33, 43<br />
4 implants - 32, 34, 42, 44<br />
Mx Implants usually placed in position of:<br />
4 implants - 13, 23, 16, 26<br />
6 implants - 13, 23, 15, 25, 17, 27<br />
Tissue supported, implant retained.<br />
Implant Placement<br />
Implant Placement<br />
Parallel to each other<br />
Perpendicular to the occlusal<br />
plane<br />
Same occlusal height<br />
Equal distance from the<br />
midline<br />
Center of the ridge Bu-‐Li<br />
Too far apart:<br />
Increased ant-‐post rocking<br />
22 mm<br />
17 mm<br />
One implant is more distal<br />
Primary rotation point or<br />
fulcrum when the patient<br />
occludes posteriorly<br />
Increase complications<br />
Wear of the attachment<br />
Abutment loosening<br />
Crestal bone loss<br />
Implant failure<br />
Prosthesis fracture<br />
Surgical Guides<br />
A necessity.<br />
Allows the clinician to<br />
have control over the<br />
prosthetic outcome.<br />
Should be<br />
made/designed by the<br />
DDS not the lab.<br />
Duplicate the denture or<br />
wax set-up in orthodontic<br />
resin<br />
Drill holes for placement<br />
Slot from foramen to<br />
foramen, end at the<br />
incisal edge<br />
Panoramic Radiograph
Panoramic Radiograph<br />
Panoramic Radiograph<br />
Panoramic Radiograph<br />
Panoramic Radiograph<br />
Panoramic Radiograph<br />
Locator Abutments<br />
Diameter of Locator<br />
retention top – 3.85<br />
mm.<br />
Available in a variety<br />
of cuff heights and for<br />
most implant types<br />
and sizes.<br />
1.5 mm of the top<br />
should be<br />
supragingival to be<br />
able to retain the<br />
overdenture.<br />
Recommended torque<br />
is 20-25 Ncm.<br />
Height mm 1 2 3 4 5<br />
height mm<br />
Ø mm
Locator Selection<br />
Locator Abutment Delivery<br />
Select the correct Locator Abutment based on the<br />
level of tissue indicated when using the Abutment<br />
Depth Gauge.<br />
Appropriate abutment height keeps the top 1.5<br />
mm extended above the soft tissue.<br />
Seat the Locator Abutment using the Locator<br />
Abutment Driver, part of the Core Tool.<br />
For final tightening, use the Torque Wrench Bit<br />
together with a Torque Wrench, or insert a driver<br />
into the Abutment Driver.<br />
The recommended seating torque is 20-25 Ncm.<br />
Next steps<br />
Make a new denture start to finish<br />
Initial impression<br />
Final impression with your choice of implant<br />
impression<br />
Wax Rim adjustment<br />
Wax try-in<br />
Delivery<br />
Convert an existing denture into an overdenture<br />
With a reline impression (indirect approach)<br />
Direct pickup of Locator housings with a chairside<br />
reline.<br />
Implant Impressions<br />
Open Tray Impression<br />
Coping<br />
Locator Pickup<br />
Impression Coping<br />
Closed Tray Impression<br />
Coping<br />
Fixture Level Impression<br />
Abutment Level impression<br />
Firmly attach the Locator Abutment Pick-ups to<br />
the Locator Abutments.<br />
Verify to ensure a perfect fit.<br />
The copings should have stable friction retention.
Converting a denture into an<br />
overdenture.<br />
Identify the positions<br />
of the Locator<br />
Abutments in the<br />
denture base.<br />
Relieve the denture<br />
base to obtain<br />
adequate space for<br />
the impression<br />
material and the<br />
Locator Abutment<br />
Pick-up.<br />
Converting a denture into an<br />
overdenture.<br />
Make an impression<br />
using an elastic<br />
impression material<br />
Make a reline if<br />
needed.<br />
Converting a denture into an<br />
overdenture.<br />
Firmly place the<br />
Locator Abutment<br />
Replica in the<br />
impression copings,<br />
which, if indicated, are<br />
then repositioned in<br />
the impression<br />
Converting a denture into an<br />
overdenture.<br />
Fabricate a working<br />
model with the Locator<br />
Abutment Replica and<br />
high-quality stone<br />
material.<br />
Complete the relining<br />
and convert the<br />
existing denture into a<br />
Locator attachment<br />
retained overdenture<br />
Converting a denture into an<br />
overdenture.<br />
Replace the processing insert with the required<br />
retentive insert.<br />
Remove the Locator Insert by using the Insert<br />
Removal Tool portion of the Locator Core Tool.<br />
Press a new Locator Insert over the Insert Seating<br />
Tool, and press the Locator Insert into the housing<br />
Converting a denture into an<br />
overdenture.<br />
Five types of Locator<br />
Inserts are available to<br />
obtain the required<br />
retention for the<br />
prosthesis.<br />
The inserts come with<br />
different retentive<br />
holding force levels:<br />
Clear 5 Pounds<br />
Pink 3 Pounds<br />
Blue 1.5 Pounds<br />
Green 3-4 Pounds*<br />
Red 1.5 Pounds*<br />
(*for angled implants)
Direct Pickup<br />
Direct Pickup<br />
Choose, insert, and tighten correct Locator<br />
abutments<br />
Place processing ring and locator housing<br />
with black processing insert on the abutments.<br />
Identify position and relieve denture base, create vent<br />
for excess acrylic.<br />
Apply acrylic and seat denture, allow for adequate<br />
curing.<br />
Trim and polish, remove processing ring, and replace<br />
insert with appropriate retentive insert.<br />
Locator Core Tool<br />
Locator Core Tool Use<br />
Gap<br />
Loosen the Insert Removal Tool<br />
a full 3 turns counter clockwise.<br />
You will see a visible gap.<br />
To remove an insert from the titanium metal housing;<br />
simply insert the tip into the insert assembly and push<br />
straight in to the bottom of the nylon insert.<br />
Then tilt the tool so that the sharp edge of the tip will<br />
grab hold of the insert and pull it out of the cap.<br />
Insert Removal Tool Insert Seating Tool Abutment Driver<br />
To discard the insert from the new tip on the Locator Core Tool;<br />
point the tool down and away from you and tighten the<br />
Insert Removal Tool clockwise back onto the Locator Core Tool.<br />
This will activate the removal pin and dislodge the insert from<br />
the tip end of the Insert Removal Tool.<br />
Separate the Insert Removal Tool section from<br />
the Locator Core Tool and use the Insert Seating Tool<br />
end of the remaining two sections to place a<br />
new insert into the empty titanium metal housing.<br />
1. Loosen Insert Removal Tool 2. Remove the Insert<br />
Gap
3. Discard the Insert<br />
4. Remove the Insert Removal<br />
Tool<br />
5. Place a New Insert<br />
Questions?<br />
Insert Seating Tool end