Summer 2009 - British Columbia Transplant Society
Summer 2009 - British Columbia Transplant Society
Summer 2009 - British Columbia Transplant Society
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
A BC <strong>Transplant</strong> publication<br />
<strong>Summer</strong> <strong>2009</strong><br />
<strong>Transplant</strong> Ti m e s<br />
Innovative<br />
Research<br />
in BC p. 6
On The<br />
In s i d e<br />
DOMINO TRANSPLANT<br />
3 Canadian cities<br />
Domino <strong>Transplant</strong><br />
•<br />
Donation after Cardiac Death<br />
•<br />
Cover: Betterbiomarkers Study<br />
•<br />
BC <strong>Transplant</strong> Research Foundation<br />
•<br />
37 years—one kidney transplant<br />
•<br />
Events<br />
www.transplant.bc.ca<br />
The <strong>Transplant</strong> Times<br />
is published twice a year by the<br />
Communications Department<br />
of BC <strong>Transplant</strong>.<br />
Editor<br />
Allison Colina<br />
Assistant Editor<br />
Ken Donohue<br />
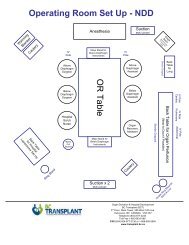
On June 24 th the first multiple province domino kidney transplant<br />
including was performed in Canada. Hospitals in Vancouver,<br />
Edmonton and Toronto simultaneously removed kidneys from living<br />
donors and performed a total of four transplants.<br />
An altruistic living kidney donor (a person willing to donate a kidney<br />
to someone they don’t know) was matched with a patient in need of<br />
a kidney transplant who has a willing but incompatible living donor.<br />
The incompatible donor then donated to another patient in need<br />
of a transplant who had a willing but incompatible donor, and so<br />
the chain continued until the last ‘incompatible’ donor’s kidney was<br />
donated to the person at the top of the deceased donor waiting list.<br />
In this first Canadian wide ‘domino’ transplant, four people received a<br />
transplant—three of those people had an incompatible living donor,<br />
the fourth was at the top of the lengthy deceased donor waitlist. This<br />
strategy can trigger a very long chain of transplants by adding more<br />
incompatible donor-recipient pairs.<br />
Incompatible<br />
pair 1<br />
Incompatible<br />
pair 2<br />
Incompatible<br />
pair 3<br />
Donor Donor Donor<br />
The <strong>Transplant</strong> Times welcomes<br />
submissions and letters.<br />
Altruisitc<br />
living<br />
donor<br />
Recipient<br />
waiting on<br />
deceased<br />
donor list<br />
c/o Editor<br />
West Tower, 3rd Floor<br />
555 West 12th Avenue<br />
Vancouver, BC<br />
V5Z 3X7<br />
(604) 877-2240<br />
1-800-663-6189<br />
e-mail: acolina@bcts.hnet.bc.ca<br />
On The Cover: Sarah Johnston,<br />
heart recipient<br />
Recipient<br />
Recipient<br />
Recipient<br />
In August 2008 Canadian Blood Services (CBS) assumed a National<br />
role in Organ and Tissue Donation—one of the main priorities for<br />
the CBS was to initiate a National Living Donor Paired Exchange<br />
(LDPE) Registry—which launched in February of <strong>2009</strong>. At the time<br />
the Registry launched, Dr. Peter Nickerson, Executive Medical<br />
Director of Organ <strong>Transplant</strong>ation at Canadian Blood Services said,<br />
“The Living Donor Paired Exchange Registry is a major advance for<br />
Page 2 <strong>Transplant</strong> Times <strong>2009</strong>
organ donation<br />
kidney donations and transplants in<br />
this country. Creating a centralized<br />
registry such as this gives us critical<br />
mass, greatly increases the chances<br />
of finding suitable matches, and more<br />
living donors will have their wishes<br />
fulfilled. Canadians in need will now<br />
be able to get compatible kidneys<br />
faster, and that will save lives.”<br />
The cross Canada domino transplant<br />
on June 24 th was the first resulting<br />
from the newly formed Living Donor<br />
Paired Exchange Registry in Canada.<br />
As more transplant programs across<br />
the country begin to participate in<br />
the Registry, the donor pool will grow,<br />
allowing for more large scale kidney<br />
exchanges and domino transplants.<br />
How are pairs entered into the<br />
Living Donor Paired Exchange<br />
Registry?<br />
If the blood tests indicate that the<br />
recipient and donor do not match,<br />
they are considered an incompatible<br />
pair. This means that the donor’s<br />
blood type is not compatible<br />
with the recipient’s blood type.<br />
If the ‘incompatible’ donor is still<br />
interested in donating a kidney, the<br />
pair can be tested to see if they are<br />
healthy enough to participate in<br />
an exchange. If they qualify, their<br />
medical information is entered into<br />
the LDPE Registry.<br />
Who can donate a kidney through<br />
the LDPE Registry?<br />
Any person in general good health<br />
can potentially donate a kidney and<br />
be entered into the LDPE registry. A<br />
person can enter in as a pair with an<br />
incompatible recipient, or a person<br />
can be entered into the Registry<br />
alone with the intention of donating<br />
a kidney to a stranger (altruistic<br />
donor). TT<br />
Donation After<br />
Cardiac Death<br />
By Michael Williams<br />
freelance writer<br />
Last November, St. Paul’s<br />
Hospital in Vancouver quietly became<br />
the first in BC to implement a procedure<br />
for organ retrieval that could<br />
considerably increase the number of<br />
life-prolonging transplants.<br />
The procedure, known as donation<br />
after cardio circulatory death,<br />
or DCD, involves the removal of life<br />
support from patients where death is<br />
imminent. With the blessing of family<br />
members, the assisted-breathing device<br />
and other life support is removed<br />
and, after the heart stops beating and<br />
two physicians from the ICU certify<br />
the patient has died, organ retrieval<br />
begins within minutes.<br />
Rigorous protocols had been<br />
put in place at St. Paul’s; experience<br />
from other hospitals worldwide, including<br />
ones in Ontario and Quebec,<br />
thoroughly analysed. The intensivecare<br />
unit (ICU) and the transplant<br />
team— keenly aware of each other’s<br />
very separate, but nonetheless interwoven,<br />
responsibilities —were set.<br />
The implementation date for<br />
the DCD protocols was Nov. 1 and the<br />
preliminary estimate was that three<br />
such procedures would be carried out<br />
in the first year. Within a month, that<br />
number had already been reached.<br />
The following looks at the<br />
re-emergence of DCD and the procedure’s<br />
inherent medical and ethical<br />
dilemmas.<br />
--------<br />
In their book, The Ethics of Organ<br />
<strong>Transplant</strong>s, Arthur Caplan and<br />
Daniel Coelho say in the opening<br />
chapter: “The boundaries of life and<br />
death are not as clear today as in<br />
the past.”<br />
That observation remains<br />
every bit as relevant more than a<br />
decade after the book’s publication.<br />
In 1968—the year of the first heart<br />
transplant in the US and Europe’s<br />
first lung transplant—a special committee<br />
at Harvard University wrote<br />
the definition of brain death—<br />
becoming widely accepted as the<br />
definition of end of life.<br />
Doctors looked for neurological<br />
activity in the brain—essentially<br />
the nervous system. If there<br />
was none, the person was deemed<br />
dead.<br />
If organs met the criteria for<br />
transplantation (assuming that was<br />
the declared wish of the decedent),<br />
they were retrieved.<br />
The concept of brain death<br />
became widely accepted as an<br />
ethical and legal criterion for organ<br />
donation, a practice known as<br />
donation after neurological determination<br />
of death, or DNDD.<br />
However, before the Harvard declaration,<br />
organs were retrieved after<br />
cardiac death, essentially following<br />
the same methods as DCD. The<br />
university’s declaration, later called<br />
the dead-donor rule —seemed, in<br />
hindsight, to have obscured the<br />
concepts surrounding death and<br />
donation.<br />
The debate between<br />
cardiac and brain death began. But<br />
even today the issues are debated<br />
mostly in medical and ethical journals.<br />
Page 3 <strong>Transplant</strong> Times <strong>2009</strong>
donation after cardiac death<br />
In separate interviews, Dr. David<br />
Landsberg, director of renal transplant<br />
at St. Paul’s Hospital in Vancouver,<br />
and Dr. Jeff Zaltzman, his<br />
counterpart at St. Michael’s Hospital<br />
in Toronto, said revisiting DCD as a<br />
means of organ procurement was<br />
driven by the public.<br />
Dr. Landsberg said families<br />
of patients (usually suffering catastrophic<br />
brain injury) were seeking<br />
“an outcome which they felt . . .<br />
gave meaning to that person’s life<br />
and their death.”<br />
The first DCD procedure<br />
in Canada was performed in June,<br />
2006, at the Ottawa Hospital. The<br />
family of a 32-year-old woman,<br />
Sara-Beth Therien, having decided<br />
withdrawal of life support was their<br />
best option, asked doctors to follow<br />
through on her wishes to become a<br />
donor.<br />
At the time, the woman’s<br />
father was quoted as saying DCD<br />
marked “a new era for organ donation<br />
in this wonderful country and<br />
that makes (our daughter) a pioneer.”<br />
Some detractors of DCD<br />
have gone so far as to suggest doctors<br />
caring for patients—usually in<br />
intensive-care—might abandon<br />
efforts to save patients too soon.<br />
Medical personnel stress, though,<br />
that the aim of all doctors is to extend<br />
life—not cut it short as a convenience.<br />
Dr. Landsberg is among<br />
those and says it’s important people<br />
realize the clear-cut and separate<br />
obligations of the attending physician<br />
and the transplant team.<br />
“We’re not involved in any<br />
of the discussions with the family<br />
about life support or its withdrawal.<br />
It’s only when they (the ICU team<br />
and the family) have made the<br />
decision to withdraw life support is<br />
there even a consideration whether<br />
that person is a candidate for DCD.”<br />
He underscores the point that withdrawing<br />
life support is a decision<br />
made in the interests of the patient<br />
and family.<br />
“Regardless of DCD or no<br />
DCD, withdrawal of life support is<br />
what’s going to happen. The decision<br />
is made regardless of whether<br />
that person is going to be an organ<br />
donor.<br />
“We [the transplant team],<br />
ethically, legally and morally will not<br />
be involved until the patient has<br />
actually died.”<br />
One concern mentioned<br />
by some detractors of DCD is the<br />
administering of drugs that, while<br />
not of any help to the patient, are<br />
intended to preserve organs. For<br />
example, an anti-clotting medication<br />
could be injected. That decision<br />
must be made by the ICU physician<br />
and not the transplant team.<br />
Dr. Landsberg says such<br />
medications are not administered<br />
until the withdrawal of life support<br />
at St. Paul’s, while Dr. Zaltzman says<br />
St. Michael’s has administered anticlotting<br />
drugs just prior to withdrawal.<br />
Dr. Zaltzman says ICU doctors<br />
might also decide to administer<br />
so-called “comfort measures,”<br />
such as morphine for pain. “These<br />
(measures) have the possibility to<br />
hasten death,” he said, “but they are<br />
exercised for comfort; not with the<br />
idea of DCD.”<br />
He admits, though, that<br />
pre-death medications “add a level<br />
of complexity” to an already complex<br />
subject and those arguments<br />
against the administering of such<br />
medications are not “completely<br />
invalid.”<br />
For now, the success of<br />
DCD is reflected in the numbers. By<br />
the beginning of this year, 45 such<br />
procedures had been performed in<br />
Ontario since the first in mid-2006.<br />
Quebec has had limited experience,<br />
with fewer than 10 performed so<br />
far.<br />
During that three-year<br />
period, DCD organs at one point<br />
accounted for 17 per cent of kidney<br />
“The reality is<br />
that ventilators<br />
are being<br />
turned off. Why<br />
would you not<br />
turn that into<br />
a potentially<br />
positive<br />
situation?”<br />
–Dr. David Landsberg<br />
and liver transplants in Ontario.<br />
The figure could one day reach 20<br />
per cent, says Dr. Zaltzman, but he<br />
feels the figure will likely level out<br />
to somewhere around 12 to 13 per<br />
cent; still an impressive number.<br />
Dr. Landsberg says he<br />
feel strongly the public in general<br />
has faith in the medical system.<br />
“I believe most families trust the<br />
medical system,” he says. “They<br />
believe everyone is working [for]<br />
the patient and not looking ahead<br />
to some potential donor.<br />
“Only when it is no longer<br />
in the best interest of the patient<br />
to be maintained on life support<br />
is consideration given to its withdrawal.”<br />
He accentuates, too, that<br />
withdrawal of life support happens<br />
in hospitals around the world every<br />
day.<br />
“The reality is that ventilators<br />
are being turned off. Why<br />
would you not turn that into a<br />
Page 4 <strong>Transplant</strong> Times <strong>2009</strong>
potentially positive situation? I can’t<br />
believe the public believes doctors<br />
are (withdrawing life support)<br />
so the patient can be a donor. Our<br />
focus is to save peoples’ lives; not<br />
end them.”<br />
He wonders whether the<br />
hard questions surrounding withdrawal<br />
of life support are not more<br />
challenging to the medical community<br />
than the general public.<br />
“When breathing has stopped and<br />
the heart has stopped, most people<br />
accept the fact that person is gone.”<br />
The timing between a<br />
patients’ death and the retrieval of<br />
organs has also become an issue<br />
drawing strong opinion. In the US<br />
and parts of Europe, transplant<br />
teams have begun retrieval of<br />
organs as soon as 75 seconds after<br />
pronouncement of death, although<br />
the generally accepted waiting<br />
period seems to be five minutes.<br />
Advocates of DCD support<br />
this approach, referring to a sometimes<br />
disputed claim that no person<br />
has ever revived after losing a heart<br />
beat for more than 60 seconds.<br />
After much deliberation, St. Michael’s<br />
Hospital decided it would<br />
wait 10 minutes after declaration of<br />
death; St. Paul’s Hospital chose five<br />
minutes.<br />
Both of these waiting<br />
periods are far more conservative<br />
than used in other countries and<br />
Dr. Zaltzman would like to see the<br />
10-minute rule now practised at St.<br />
Michael’s Hospital lowered, saying<br />
there is no “scientific merit” in the<br />
extended wait time.<br />
Dr. Landsberg agrees, saying<br />
the difference between two,<br />
five or even 10 minutes is “splitting<br />
hairs.” TT<br />
clinic<br />
Above from left to right: Kathleen Collin (Pharmacist), Dr. Mina Matsuda-Abedini<br />
(Nephrologist), Kelleigh Graham (16-year-old kidney transplant recipient),<br />
Jessie Ahuja (Registered Nurse Clinician)<br />
New Multi-Organ <strong>Transplant</strong> Clinic at BC<br />
Children’s Hospital Helps Kids and Parents<br />
A<br />
new multi-organ transplant<br />
clinic at BC Children’s<br />
Hospital opened its doors<br />
to pediatric patients and<br />
their family members in January<br />
<strong>2009</strong>. The clinic provides access to<br />
specialized health care providers<br />
for over 120 BC children who have<br />
received an organ transplant.<br />
“Previously, care for these patients<br />
was provided in a dispersed manner<br />
at the hospital with kidney transplant<br />
recipients being followed in the renal<br />
clinic, and cardiac, liver and bowel<br />
transplant recipients being followed<br />
in their respective clinics,” said Dr.<br />
Douglas Matsell, division head of<br />
nephrology and the multi-organ<br />
transplant clinic at BC Children’s<br />
Hospital. “Patients are now seen by<br />
a specialist and interdisciplinary<br />
team members on the same visit so<br />
there is an opportunity for urgent<br />
consultations to occur should any<br />
complications be discovered.”<br />
Carmen Carriere, mother of a heart<br />
transplant recipient, worked at<br />
educating the BC Ministry of Health<br />
Services on the challenges faced<br />
by pediatric transplant patients,<br />
and advocating for this cohesive<br />
transplant clinic at BC Children’s<br />
Hospital. “Children who have had<br />
a transplant still face a number<br />
of issues. It’s incredibly important<br />
to have a clinic like the one at BC<br />
Children’s to provide on-going care,”<br />
said Carriere, whose daughter Brynn<br />
McKenna, is a seven-year-old heart<br />
transplant patient.<br />
The clinic addresses the most urgent<br />
needs and ongoing management<br />
of patients who have had a kidney,<br />
heart, liver or bowel transplant. The<br />
multi-organ transplant clinic was<br />
made possible through $288,000 in<br />
annual funding from the Ministry of<br />
Health Services through the PHSA<br />
and BC <strong>Transplant</strong>. In addition to<br />
being followed by their specialized<br />
transplant physician the clinic will<br />
also provide patients with access<br />
to expanded nursing, pharmacist,<br />
social work, dietitian and psychology<br />
support. TT<br />
Page 5 <strong>Transplant</strong> Times <strong>2009</strong>
Biopsies, soon to be a thing of the past?<br />
by Jenny Boon<br />
on the cover<br />
Below: Sarah Johnston with husband Luke Johnston<br />
In 2005, a young BC family<br />
was thrown into crisis. Sarah<br />
Johnston, a wife and mother of<br />
three, was rushed to the Heart<br />
Centre, part of the Providence<br />
Heart + Lung Institute at St. Paul’s<br />
Hospital, with an infection of the<br />
heart known as myocarditis. The<br />
infection was extremely severe, and<br />
did not respond to therapy—doctors<br />
decided to implant a Ventricular<br />
Assist Device (VAD) in Johnston’s<br />
heart. She was put on the transplant<br />
list, and eventually underwent a<br />
successful heart transplant.<br />
As part of her post-transplantation<br />
monitoring, Johnston had to<br />
undergo numerous painful biopsies<br />
in the year after her surgery. A few<br />
weeks after her operation, these<br />
biopsies indicated her body was<br />
rejecting the new heart. Her regime<br />
of immunosuppressant drugs had<br />
to be increased, and more biopsies<br />
were required.<br />
<strong>Transplant</strong>ation is currently the<br />
most common therapy for<br />
patients with end-stage<br />
organ failure. However,<br />
like Johnston, many<br />
t r a n s p l a n t p a t i e n t s<br />
experience rejection<br />
that must be treated<br />
with large doses of toxic<br />
immunosuppressant<br />
drugs.<br />
Given that a single heart<br />
biopsy in Canada costs<br />
somewhere between five<br />
to ten thousand dollars—<br />
and that the average heart<br />
transplant recipient will need<br />
between 14 and 16 of these invasive<br />
procedures in the first year alone—a<br />
group of scientists has joined together<br />
in an innovative research project that<br />
harnesses the power of biomarkers<br />
to find a better way to diagnose<br />
organ rejection before it begins, and<br />
to one day give doctors the tools to<br />
personalize immunosuppressant<br />
therapy for each individual patient.<br />
The Biomarkers in <strong>Transplant</strong>ation<br />
project aims to identify biomarkers<br />
in the blood that will tell a doctor<br />
immediately if a transplanted<br />
organ is being rejected, using a<br />
simple blood test. The project has<br />
two immediate goals: the first is<br />
to decrease the number of times<br />
a transplant patient will have to<br />
undergo painful, expensive biopsies.<br />
The second goal is to reduce health<br />
care costs: the estimated cost savings<br />
of using biomarkers to identify<br />
early organ rejection is estimated<br />
at several million dollars a year in<br />
Canada for heart transplants alone.<br />
By replacing some biopsies with a<br />
blood test, health care costs will be<br />
significantly decreased for heart and<br />
kidney transplant patients across the<br />
board.<br />
Biomarkers in <strong>Transplant</strong>ation<br />
was launched in 2004, when an<br />
investigative team of researchers<br />
began studying advanced genomic<br />
(study of genes), proteomic (study<br />
of proteins), and bioinformatic<br />
(information science) tools to<br />
better understand variations in<br />
acute or chronic tissue rejection in<br />
heart, liver, and kidney transplant<br />
patients. The study involves many<br />
of Canada’s foremost experts in<br />
clinical transplantation, immunology,<br />
pathology, biochemistry, statistics<br />
and computer science, who are<br />
using the most advanced genomic,<br />
proteomic and bioinformatic tools<br />
to develop inexpensive, noninvasive<br />
and accurate diagnostic and<br />
prognostic tests for organ rejection<br />
and immunosuppressive therapy<br />
responsiveness.<br />
After four years of study, the team<br />
has now identified sets of genes and<br />
proteins in the blood that diagnose<br />
acute rejection in the first few weeks<br />
after transplantation and chronic<br />
rejection beyond one year after<br />
transplantation. Team members<br />
have also identified a set of blood<br />
biomarkers that can predict organ<br />
rejection; this set could be used<br />
to allow doctors to adjust drug<br />
therapies to prevent graft injury and<br />
avoid toxicity.<br />
Biomarkers in <strong>Transplant</strong>ation is now<br />
entering its second phase, a Canadawide<br />
study of transplant patients<br />
that will allow scientists to test these<br />
biomarker panels in a more diverse<br />
group of patients with heart and<br />
Page 6 <strong>Transplant</strong> Times <strong>2009</strong>
kidney transplants. This next phase of<br />
the study will run for two years, and<br />
will hopefully culminate with Health<br />
Canada and the US FDA approving<br />
the test for use in clinical care.<br />
On May 26, <strong>2009</strong>, Johnston joined<br />
members of the Biomarkers in<br />
<strong>Transplant</strong>ation team for the official<br />
launch of the second phase of the<br />
Biomarkers in <strong>Transplant</strong>ation Project,<br />
which took place at the PROOF<br />
Centre for Excellence 2 nd Annual<br />
Meeting in Vancouver. The event—<br />
which attracted significant media<br />
coverage – was an opportunity for<br />
Johnston to share her story, and also<br />
thank the doctors and researchers for<br />
their work.<br />
“It’s exciting for me to be here for<br />
the launch of the Better Biomarkers<br />
in <strong>Transplant</strong>ation project, especially<br />
since I’ve been through so many<br />
biopsies. The thought that other<br />
people will only need a blood test,<br />
rather than going through the pain<br />
of multiple biopsies, is inspiring.<br />
I’m so thankful to the doctors and<br />
researchers at St. Paul’s—they saved<br />
my life and continue to work and<br />
study to improve other people’s lives.<br />
My husband, my three kids and I are<br />
so grateful for this new heart and the<br />
life it has given me. My hope is that<br />
future transplant recipients will have<br />
a chance at an easier road to recovery<br />
after their surgery, and I think this<br />
project will help achieve that.”<br />
The Biomarkers in <strong>Transplant</strong>ation<br />
initiative is currently supported<br />
by the Prevention of Organ Failure<br />
Centre of Excellence (PROOF Centre;<br />
a Networks of Centres of Excellence<br />
program), Genome <strong>British</strong> <strong>Columbia</strong>,<br />
Astellas Pharma, St. Paul’s Hospital<br />
Foundation, BC <strong>Transplant</strong> and the<br />
University of <strong>British</strong> <strong>Columbia</strong>. For<br />
more information on the project, visit<br />
www.allomark.ubc.ca TT<br />
jesse pratt memorial ride<br />
Over 130 people<br />
took part in a<br />
memorial ride on<br />
Sunday, May 24 th<br />
at the Mountain View Harley<br />
Davidson in Chilliwack,<br />
organized by Grant Pratt and<br />
his family, to honour his<br />
young son’s memory and<br />
to raise awareness about<br />
organ donation.<br />
Eighteen year old Jesse<br />
Pratt’s life came to a tragic<br />
end last May after a terrible<br />
motorcycle accident on<br />
the Trans-Canada highway.<br />
Jesse was living his dream,<br />
riding a brand new Harley<br />
Davidson Fat Boy on his way<br />
to Hell’s Gate with his father.<br />
Jesse’s generous spirit in<br />
life continued with the altruistic gift of organ donation after his death. Six<br />
individuals received a new lease on life as a result of his donation.<br />
Jesse’s family set up a Facebook site in his memory, and on it they state, “Jesse<br />
was the most amazing guy anyone could ever know. He had the biggest heart<br />
and always put others before himself, no matter what the issue.”<br />
The 1 st Jesse Pratt Memorial Ride will now be an annual event to remember<br />
Jesse for the remarkable young man he was. Money raised from the ride<br />
totaled over $2,100, which the family has kindly donated to the BC <strong>Transplant</strong><br />
Research Foundation. TT<br />
Page 7 <strong>Transplant</strong> Times <strong>2009</strong>
RESEARCH FOUNDATION<br />
T h e B C<br />
Tr a n s p l a n t<br />
R e s e a r c h<br />
Foundation<br />
recently<br />
w e l c o m e d<br />
Pamela Scott<br />
as Executive<br />
Pamela Scott<br />
D i re c tor, a<br />
newly created<br />
position for the Foundation.<br />
Pamela Scott began her career<br />
in Pittsburgh after completing<br />
her Masters degree in Public<br />
Administration and International<br />
Affairs at the University of Pittsburgh.<br />
Scott continued on at the University,<br />
working as a Community Relations<br />
Specialist, bridging the medical<br />
department with members of the<br />
public to help identify research<br />
subjects. Through her experience<br />
working with the University,<br />
Scott developed a familiarity with<br />
research, and today is still inspired<br />
by researchers.<br />
Throughout her distinguished career,<br />
Scott has been closely tied to the<br />
non-profit sector. While working in<br />
Illinois, Scott was appointed to the<br />
State Public Advocacy Committee. In<br />
that role she lobbied to have organ<br />
donor decals placed on the driver’s<br />
license. Through her work with the<br />
Governors office the legislation<br />
passed—a major success. Scott<br />
has committed a large amount<br />
of time to her volunteer career<br />
within the non-profit community,<br />
serving as a member and executive<br />
leader on numerous boards. For the<br />
past 10 years she has worked with<br />
Foundations in Connecticut as a<br />
fundraiser, with a wonderful history<br />
of success—she has a love of seeking<br />
funds.<br />
With over 20 years experience<br />
working in government relations and<br />
fundraising, Scott brings a wealth of<br />
information and leadership to the<br />
BC <strong>Transplant</strong> Research Foundation.<br />
As the Executive Director, Scott will<br />
focus on the development of a long<br />
term funding strategy and the ability<br />
to support more research projects.<br />
HONOR your loved one.<br />
Flowers wilt<br />
Balloons loose air<br />
A donation to the BC <strong>Transplant</strong><br />
Research Foundation will have<br />
ever-lasting benefits for the<br />
health of transplant patients.<br />
www.transplant.bc.ca/BCTRF.htm<br />
Brighten the spirit of your loved<br />
one while they stay in hospital—<br />
consider making a donation<br />
to the BC <strong>Transplant</strong> Research<br />
Foundation. Your friend or loved<br />
one will receive a card letting<br />
them know you made a donation<br />
in their name. Research inspires<br />
better health for the future. Visit<br />
the website and make a donation<br />
today!<br />
he BC <strong>Transplant</strong> Research<br />
Foundation’s (BCTRF) mission<br />
is to promote peer reviewed<br />
research into solutions which<br />
will benefit <strong>British</strong> <strong>Columbia</strong>ns<br />
whose lives are threatened by organ<br />
failure.<br />
All of the research funded through<br />
the BCTRF is peer-reviewed. Before<br />
a research proposal receives funds<br />
a panel of experts from across N.<br />
America reviews the proposal. The<br />
Michael Smith Foundation facilitates<br />
the BCTRF peer review process. The<br />
BCTRF funds research through two<br />
processes:<br />
1. Venture Grants— h e l p i n g<br />
to support new, high-risk/highreward<br />
research ideas identified<br />
by investigators across BC. This will<br />
fund new areas of research (e.g.,<br />
new hypotheses, new techniques,<br />
and new ideas) that are in a pilot/<br />
feasibility stage.<br />
2. Peer Reviewed Research—Fund<br />
new research by providing ‘seed’<br />
money to researchers, which allows<br />
them to secure remaining funds from<br />
larger donors.<br />
In order to fund research and further<br />
improve the lives of transplant<br />
patients in BC, the Foundation needs<br />
to secure monetary donations. As<br />
Executive Director of the BCTRF,<br />
Pamela Scott will be developing<br />
relationships and creating a plan to<br />
increase fundraising activities for the<br />
Foundation. TT<br />
Page 8 <strong>Transplant</strong> Times <strong>2009</strong>
the only child in the dialysis room.<br />
I waited to recover from the<br />
kidney removal surgery before the<br />
transplant could take place (the kidneys<br />
are no longer removed before<br />
a transplant unless they are cancerous<br />
or infected).<br />
The big day was April 28,<br />
1972. My dad, lying on a stretcher<br />
waiting for surgery to have his kidney<br />
removed, smiled and squeezed<br />
my hand as we passed in the hall—<br />
not knowing if I’d even survive the<br />
surgery.<br />
It was an all day surgery,<br />
but I pulled through. I managed to<br />
escape falling into a coma in Recovery.<br />
A small fridge was brought<br />
to my room and I was allowed to<br />
eat whatever I wanted! I had to gain<br />
weight. I asked for Bologna sandwiches,<br />
hotdogs, ice cream and<br />
Jeannie’s cake (it’s a famous bakery<br />
in Winnipeg)! I wanted everything<br />
I hadn’t been allowed to eat on the<br />
restrictive pre transplant diet.<br />
After four months living in<br />
a hospital room, I went home. I was<br />
even able to finish grade 3.<br />
The kidney has been working<br />
great ever since.<br />
The transplant brought<br />
new opportunities—I was a part<br />
of one of the first groups to attend<br />
Kidney Camp, it was held in BC with<br />
kids from all across Canada. I also<br />
rode on a float for organ transplant<br />
kids the year the Grey Cup was in<br />
Winnipeg.<br />
In 1980 I found out I had a<br />
cancerous tumor. The cancer treatyears<br />
later<br />
by Teresa Zahirney37<br />
I received a live donor kidney<br />
transplant in Winnipeg in 1972.<br />
From the time I was 5 years<br />
old, I remember being on a high<br />
protein, no salt diet, but that wasn’t<br />
enough. It was just before Valentine’s<br />
Day in 1972 when I was hospitalized<br />
with chronic renal failure—I<br />
was 7 years old. I was started on<br />
peritoneal dialysis and was too sick<br />
to leave the hospital. The hospital<br />
room would become my home for<br />
the next three months.<br />
I celebrated my 8 th birthday<br />
in the hospital. They allowed my<br />
sister, brother, and a cousin to come<br />
in. I wasn’t allowed to have even a<br />
sliver of my own cake. The staff at<br />
my dad’s school had brought me<br />
so many gifts, filling a drawer in my<br />
dresser. Each day I was allowed to<br />
open one.<br />
I was allowed to go home<br />
on Sunday afternoons if my blood<br />
pressure was okay—I usually ended<br />
up asleep on the living room couch.<br />
I needed a new kidney to survive.<br />
Family members were<br />
tested for suitability as a kidney donor.<br />
There were many discussions<br />
as to where the transplant would<br />
take place—Boston? Toronto? Living<br />
kidney donation was brand new<br />
in Winnipeg at that time.<br />
It was decided that a team<br />
of doctors from Winnipeg would<br />
do the transplant. My dad was the<br />
best match. First was the surgery<br />
to remove my two kidneys, then<br />
hemodialysis—the machines back<br />
then were big and scary for an<br />
eight year old. I remember being<br />
ments were successful, and since<br />
then, aside from regular 3 month<br />
check ups at the transplant clinic,<br />
my life is fairly normal. I went to<br />
the University of Manitoba and<br />
graduated with a Bachelor of<br />
Education in 1987. I now reside in a<br />
small town—Yahk, BC.<br />
Living over 30 years with<br />
a transplant—I have met a lot of<br />
young people over the years that<br />
have gone through the transplant<br />
experience. Some are doing well.<br />
Some didn’t make it.<br />
I chose to write this for<br />
the summer issue for one special<br />
reason—to say thank you to my<br />
dad for giving me a second chance<br />
to live. Thank you for giving me<br />
life, for allowing me to grow, make<br />
mistakes along the way, for loving<br />
me and making me the person I am<br />
today. TT<br />
Who are the living<br />
donors in BC?<br />
Sibling 34%<br />
Unrelated (friends,etc.) 16%<br />
Parent 16%<br />
Spouse 16%<br />
Offspring 12%<br />
Related 6%<br />
Page 9 <strong>Transplant</strong> Times <strong>2009</strong>
Canadian <strong>Transplant</strong> Association<br />
The Canadian <strong>Transplant</strong> Associatin (CTA) encourages and<br />
motivates transplant recipients to maintain a healthy lifestyle<br />
by supporting athletic and other awareness events<br />
WORLD TRANSPLANT GAMES<br />
The 17th World <strong>Transplant</strong> Games (the Olympics of the<br />
transplant world) will take place Aug. 22-30th on the<br />
Gold Coast in Australia. The Canadian team is 148 strong<br />
and consists of 48 athletes (22 juniors/ 26 adults) and 100<br />
supporters. Six <strong>British</strong> <strong>Columbia</strong>ns are attending: Angela<br />
Burghard (kidney), Aron Cleugh (kidney/pancreas),<br />
Dick Lingham (liver), Marvin Meissner (kidney), Robbie<br />
Thorton (heart) and Margaret Benson (double lung).<br />
They hope to make BC proud and come home with a few<br />
medals.<br />
NATIONAL TRANSPLANT GAMES 2010<br />
The 5th Canadian <strong>Transplant</strong> Games will take place in<br />
Quebec City, August 9-14th, 2010<br />
Check out the Canadian <strong>Transplant</strong> Association’s website:<br />
www.organ-donation-works.org<br />
HALLOWEEN DANCE<br />
Save the date! Friday, Oct.23rd is the BC CTA’s annual<br />
Halloween dance. Party begins at 7:30pm. There will be<br />
a raffle, door prizes, spot dances, best costume contests<br />
and more. Come join the fun and at the same time help<br />
promote organ donation, transplantation and healthy,<br />
active living for recipients. For more information or if<br />
you would like to volunteer contact Margaret Benson at<br />
winniethepooh@telus.net<br />
SUN RUN<br />
The Gift of Life Organ Donation Works Sun Run team<br />
had another successful run on April 19th <strong>2009</strong>. Thirtyfive<br />
friends and family registered for the team which<br />
included 11 recipients and one living donor. One team<br />
member, Cheryl Nilsson (double lung recipient) received<br />
local and national coverage on Global TV. Look for our<br />
team again next year and come join the fun. Registration<br />
begins in January and the Run is always the first Sunday<br />
of National Organ and Tissue Donor Awareness Week<br />
(NOTDAW)<br />
For more information, or to join the CTA visit<br />
www.organ-donation-works.org<br />
or contact Margaret at winniethepooh@telus.net<br />
yess<br />
Kidney Disease Patients & Supporters<br />
In association with the Kidney Foundation<br />
of Canada BC Branch<br />
Dear Renal Patients and Supporters,<br />
My name is Ada and I have been a kidney patient for over 23<br />
years. Currently, I am a volunteer with The Kidney Foundation<br />
of Canada (BC Branch) working to establish a support<br />
group for kidney patients in Metro Vancouver called “yess”.<br />
The magic of a support group is that participants will receive<br />
mutual support from each other and by attending educational<br />
seminars, fun social activities, and by sharing their feelings.<br />
Some of you may cope with the disease quite well on<br />
your own and may not need further support; or you<br />
may be a renal health provider, or a patient’s friend or<br />
a family member. But, if you agree with me that “yess”<br />
can help to reduce stress or fear and uplift the spirit<br />
of kidney patients, then please join us to help others.<br />
A formal social gathering will be planned for September<br />
to meet all who are interested. At this gathering, we can<br />
express our mutual concerns, and set our goals - such as how<br />
to help each other, how to promote organ donation and<br />
how to plan the future of “yess”. Meanwhile, you are most<br />
welcome to contact me any time by email or by phone to add<br />
your comments and suggestions for this support group.<br />
Please pass along this message to your f r iends<br />
or other individuals who may be interested in “yess”.<br />
Thank you very much for your support. Please contact me<br />
for further details.<br />
Ada Cheung - coordinator of “yess”<br />
Tel: 604-351-0880<br />
Email: yess<strong>2009</strong>@live.ca<br />
Page 10 <strong>Transplant</strong> Times <strong>2009</strong>
T-Shirts $15<br />
Order a t-shirt today!<br />
Please contact BC <strong>Transplant</strong> by email:<br />
info@transplant.bc.ca or by tel: 604-877-2240<br />
T-shirts are $15 each and available in all sizes:<br />
xs, s, m, l, xl<br />
October 25 th <strong>2009</strong><br />
Join BC <strong>Transplant</strong> and people all over the world in the<br />
“World’s Biggest Walk” to raise global awareness for<br />
organ donation and transplantation. In cities all over the<br />
world people will walk 5KM at noon.<br />
Register Today at www.transplant.bc.ca<br />
October 25th<br />
Locarno Beach, Vancouver<br />
12 PM<br />
front<br />
The Children’s Organ<br />
<strong>Transplant</strong> <strong>Society</strong> of BC<br />
and<br />
The Heart <strong>Transplant</strong><br />
Home <strong>Society</strong><br />
present<br />
4th Annual Golf Tournament<br />
Date: September 12, <strong>2009</strong><br />
Where: Country Meadows Golf Club, Richmond BC<br />
Sponsorship opportunities available<br />
back<br />
The golf tournament begins at 1pm with a shot gun<br />
start. To participate in the golf tournament & help raise<br />
much needed funds for transplant children in BC and<br />
accommodation for heart transplant patients please<br />
contact:<br />
Debbie: 604-271-7719 dbielech@cotsbc.org<br />
Ron Bayne 778-237-5311 ronbayne@hotmail.com<br />
Page 11 <strong>Transplant</strong> Times <strong>2009</strong>
Just the Facts<br />
Number on the Organ Donor Registry 718,972<br />
Special Thanks<br />
Number of people waiting for a transplant 307<br />
Number of transplants to date in <strong>2009</strong> 120<br />
Kidney (deceased donor) 39<br />
Kidney (living donor) 44<br />
Pancreas-Kidney 1<br />
Pancreas Islet 4<br />
Pancreas 4<br />
Liver (deceased donor) 16<br />
Liver (living donor) -<br />
Heart 5<br />
Single-Lung 6<br />
Double-Lung 1<br />
Number of recipients followed in BC 2863<br />
Don’t keep us in the dark<br />
Have you moved?<br />
Name__________________________________________________<br />
New Address____________________________________________<br />
_______________________________________________________<br />
The following individuals and<br />
organizations have made a<br />
significant impact on organ<br />
donor awareness through<br />
volunteer work, and/or<br />
fundraising activities<br />
City of Langley<br />
Township of Langley<br />
City of Vernon<br />
BC Children’s Hospital<br />
BC Women’s Hospital<br />
Sunny Hill Hospital<br />
BC Child & Family Research<br />
Institute<br />
Chris & Gillian Stringer<br />
Joscelyn McCarthy<br />
Serge Vaillancourt<br />
Pratt Family<br />
Mountainview Harley Davidson<br />
No, I don’t want to receive future copies of the <strong>Transplant</strong> Times<br />
Name________________________________________________________<br />
Address_______________________________________________________<br />
555 W. 12th Ave • Vancouver, BC • V5Z 3X7 • 1-800 663-6189<br />
If you would like to receive future copies of the<br />
<strong>Transplant</strong> Times electronically, via e-mail, please respond to<br />
info@transplant.bc.ca<br />
Page 12 <strong>Transplant</strong> Times <strong>2009</strong>