Summer 2009 - British Columbia Transplant Society
Summer 2009 - British Columbia Transplant Society
Summer 2009 - British Columbia Transplant Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
organ donation<br />
kidney donations and transplants in<br />
this country. Creating a centralized<br />
registry such as this gives us critical<br />
mass, greatly increases the chances<br />
of finding suitable matches, and more<br />
living donors will have their wishes<br />
fulfilled. Canadians in need will now<br />
be able to get compatible kidneys<br />
faster, and that will save lives.”<br />
The cross Canada domino transplant<br />
on June 24 th was the first resulting<br />
from the newly formed Living Donor<br />
Paired Exchange Registry in Canada.<br />
As more transplant programs across<br />
the country begin to participate in<br />
the Registry, the donor pool will grow,<br />
allowing for more large scale kidney<br />
exchanges and domino transplants.<br />
How are pairs entered into the<br />
Living Donor Paired Exchange<br />
Registry?<br />
If the blood tests indicate that the<br />
recipient and donor do not match,<br />
they are considered an incompatible<br />
pair. This means that the donor’s<br />
blood type is not compatible<br />
with the recipient’s blood type.<br />
If the ‘incompatible’ donor is still<br />
interested in donating a kidney, the<br />
pair can be tested to see if they are<br />
healthy enough to participate in<br />
an exchange. If they qualify, their<br />
medical information is entered into<br />
the LDPE Registry.<br />
Who can donate a kidney through<br />
the LDPE Registry?<br />
Any person in general good health<br />
can potentially donate a kidney and<br />
be entered into the LDPE registry. A<br />
person can enter in as a pair with an<br />
incompatible recipient, or a person<br />
can be entered into the Registry<br />
alone with the intention of donating<br />
a kidney to a stranger (altruistic<br />
donor). TT<br />
Donation After<br />
Cardiac Death<br />
By Michael Williams<br />
freelance writer<br />
Last November, St. Paul’s<br />
Hospital in Vancouver quietly became<br />
the first in BC to implement a procedure<br />
for organ retrieval that could<br />
considerably increase the number of<br />
life-prolonging transplants.<br />
The procedure, known as donation<br />
after cardio circulatory death,<br />
or DCD, involves the removal of life<br />
support from patients where death is<br />
imminent. With the blessing of family<br />
members, the assisted-breathing device<br />
and other life support is removed<br />
and, after the heart stops beating and<br />
two physicians from the ICU certify<br />
the patient has died, organ retrieval<br />
begins within minutes.<br />
Rigorous protocols had been<br />
put in place at St. Paul’s; experience<br />
from other hospitals worldwide, including<br />
ones in Ontario and Quebec,<br />
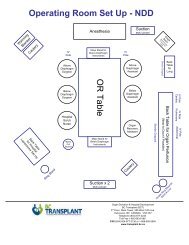
thoroughly analysed. The intensivecare<br />
unit (ICU) and the transplant<br />
team— keenly aware of each other’s<br />
very separate, but nonetheless interwoven,<br />
responsibilities —were set.<br />
The implementation date for<br />
the DCD protocols was Nov. 1 and the<br />
preliminary estimate was that three<br />
such procedures would be carried out<br />
in the first year. Within a month, that<br />
number had already been reached.<br />
The following looks at the<br />
re-emergence of DCD and the procedure’s<br />
inherent medical and ethical<br />
dilemmas.<br />
--------<br />
In their book, The Ethics of Organ<br />
<strong>Transplant</strong>s, Arthur Caplan and<br />
Daniel Coelho say in the opening<br />
chapter: “The boundaries of life and<br />
death are not as clear today as in<br />
the past.”<br />
That observation remains<br />
every bit as relevant more than a<br />
decade after the book’s publication.<br />
In 1968—the year of the first heart<br />
transplant in the US and Europe’s<br />
first lung transplant—a special committee<br />
at Harvard University wrote<br />
the definition of brain death—<br />
becoming widely accepted as the<br />
definition of end of life.<br />
Doctors looked for neurological<br />
activity in the brain—essentially<br />
the nervous system. If there<br />
was none, the person was deemed<br />
dead.<br />
If organs met the criteria for<br />
transplantation (assuming that was<br />
the declared wish of the decedent),<br />
they were retrieved.<br />
The concept of brain death<br />
became widely accepted as an<br />
ethical and legal criterion for organ<br />
donation, a practice known as<br />
donation after neurological determination<br />
of death, or DNDD.<br />
However, before the Harvard declaration,<br />
organs were retrieved after<br />
cardiac death, essentially following<br />
the same methods as DCD. The<br />
university’s declaration, later called<br />
the dead-donor rule —seemed, in<br />
hindsight, to have obscured the<br />
concepts surrounding death and<br />
donation.<br />
The debate between<br />
cardiac and brain death began. But<br />
even today the issues are debated<br />
mostly in medical and ethical journals.<br />
Page 3 <strong>Transplant</strong> Times <strong>2009</strong>