uasom doctors uasom doctors - University of Alabama at Birmingham
uasom doctors uasom doctors - University of Alabama at Birmingham
uasom doctors uasom doctors - University of Alabama at Birmingham
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
AlumniBulletin<br />
ALABAMA MEDICAL<br />
V O L U M E 3 0 • N U M B E R T W O • S U M M E R 2 0 0 4<br />
UASOM DOCTORS<br />
Serving Our N<strong>at</strong>ion in<br />
Times <strong>of</strong> Need
Dean’s Corner<br />
Dear Colleagues:<br />
This past December we wrapped up the Campaign for UAB. Launched in November 1999, the<br />
Campaign met with unprecedented success in meeting its $250 million goal, which prompted an extension<br />
and a revised goal <strong>of</strong> $350 million.<br />
By the end <strong>of</strong> 2003, the Campaign for UAB raised more than $388 million. The School <strong>of</strong> Medicine<br />
raised more than $260 million—money th<strong>at</strong> will help fund its departments, research programs, endowed<br />
chairs, pr<strong>of</strong>essorships, lectureships, scholarships, and more. Indeed, many <strong>of</strong> you have gone above and<br />
beyond expect<strong>at</strong>ions in giving, and for this I thank you. Your generosity is a direct reflection <strong>of</strong> your belief<br />
in the UASOM: our educ<strong>at</strong>ion, our research, our outreach programs, and our p<strong>at</strong>ient care. Many others<br />
share your belief in our institution. For example, some recent recognitions include:<br />
• The naming <strong>of</strong> 49 UAB physicians in the respected reference book America’s Top Doctors; <strong>University</strong><br />
Hospital was named as one <strong>of</strong> the top medical centers in the same public<strong>at</strong>ion.<br />
• The design<strong>at</strong>ion <strong>of</strong> UAB as a N<strong>at</strong>ional Autoimmunity Center <strong>of</strong> Excellence by the N<strong>at</strong>ional Institutes <strong>of</strong><br />
Health.<br />
Our reput<strong>at</strong>ion as a leader in medicine continues to grow, and the UASOM continues to see its faculty,<br />
researchers, and programs recognized in a variety <strong>of</strong> ways. This recognition would not be possible without<br />
hard work and support on everyone’s part, most notably yours.<br />
While the Campaign for UAB has ended, the need for your support is ongoing. Opportunities to fund<br />
important research, faculty positions, scholarships, and more remain. To learn more about these, please contact<br />
the development <strong>of</strong>fice <strong>at</strong> (205) 934-4469 or visit them online <strong>at</strong> [www.uab.edu/<strong>uasom</strong>/development].<br />
In addition, the <strong>University</strong> <strong>of</strong> <strong>Alabama</strong> Medical Alumni Associ<strong>at</strong>ion needs your continued support in order<br />
to assist UASOM students, residents, and alumni. Please call Elaine Chambless <strong>at</strong> (205) 934-4463 to learn<br />
more about wh<strong>at</strong> you can do to help the Associ<strong>at</strong>ion.<br />
My best to you.<br />
Sincerely,<br />
William B. Deal, M.D.<br />
Vice President for Medicine and Dean<br />
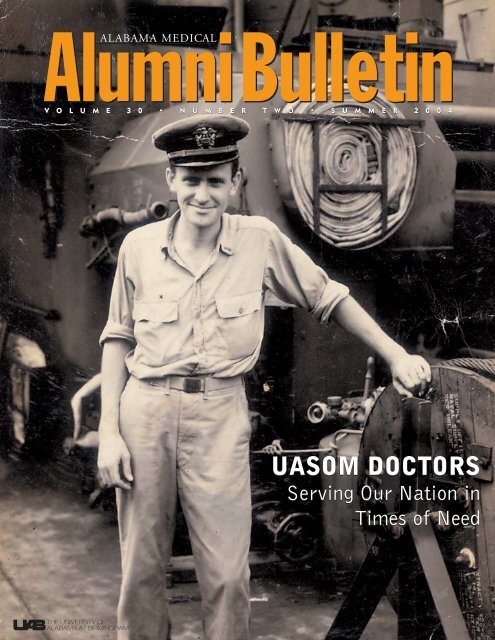
On the Cover: Alumnus Lonnie Funderburg (’50) aboard LST 124 in the South Pacific. Funderburg served as<br />
chief engineer and executive <strong>of</strong>ficer <strong>of</strong> the landing ship during the Second World War.
ALUMNI ASSOCIATION<br />
BOARD OF DIRECTORS<br />
President<br />
Betty W. Vaughan, M.D., ’63 - Dec<strong>at</strong>ur<br />
President-Elect<br />
Albert J. Tully Jr., M.D., ’64 - <strong>Birmingham</strong><br />
Secretary/Treasurer<br />
Alan R. Dimick, M.D., ’58 - <strong>Birmingham</strong><br />
Past President<br />
T. Riley Lumpkin, M.D., ’58 - Tuscaloosa<br />
The Caduceus Club President<br />
Ronald W. Orso, M.D., ’72 - <strong>Birmingham</strong><br />
Vice Presidents<br />
William R. Staggers, M.D., ’89 - Fairhope<br />
J. Noble Anderson Jr., M.D., ’89 - Montgomery<br />
K<strong>at</strong>herine R. Cooper, M.D., ’90 - Alexander City<br />
Bill Beasley, M.D., ’74 - Athens<br />
Ricky L. Irons, M.D., ’82 - Florence<br />
Helen R. Thrasher, M.D., ’63 - <strong>Birmingham</strong><br />
James S. Woodard, M.D., ’85 - Columbus, MS<br />
Betty Ruth Speir, M.D., ’63 - Point Clear<br />
Martha E. Pugh, M.D., ’65 - Houston, TX<br />
Robert M. Dimick, M.D., ’84 - Hermitage, TN<br />
Neil E. Christopher, M.D., ’58 - Guntersville<br />
Jarvis D. Ryals, M.D., ’65 - Pueblo, CO<br />
House Staff Represent<strong>at</strong>ive<br />
Edward R. Anderson III., M.D. - <strong>Birmingham</strong><br />
Senior Class President<br />
Darren Malone - <strong>Birmingham</strong><br />
Vice President and Dean<br />
William B. Deal, M.D. - <strong>Birmingham</strong><br />
Executive Secretary<br />
Elaine O. Chambless - <strong>Birmingham</strong><br />
Administr<strong>at</strong>ive Secretaries<br />
Donna F. Thompson - <strong>Birmingham</strong><br />
Diane A. Woods - <strong>Birmingham</strong><br />
BULLETIN STAFF<br />
Executive Editor<br />
Pam Powell<br />
Managing Editors<br />
Dawn Mesa, M<strong>at</strong>t Windsor<br />
Editor, Alumni Affairs<br />
Elaine O. Chambless<br />
Editors, Development Office<br />
John Lankford, Ph.D.<br />
Meredith Murdock<br />
Editorial Advisory Board<br />
J. Noble Anderson Jr., M.D.<br />
Wayne H. Finley, M.D.<br />
Ronald E. Henderson, M.D.<br />
Paul S. Howard, M.D.<br />
Ronald W. Orso, M.D.<br />
Stephen P. Suggs, M.D.<br />
C. Bruce Alexander, M.D.<br />
Dennis W. Boulware, M.D.<br />
Pam Bounelis, Ph.D.<br />
Amie B. Jackson, M.D.<br />
Sharon A. Spencer, M.D.<br />
Carlton J. Young, M.D.<br />
Executive Art Director<br />
Ron Gamble<br />
Art Director<br />
Jason Bickell<br />
Medical Editor<br />
Julius Linn, M.D.<br />
Production Manager<br />
Lynn Lowrie<br />
Production Assistant<br />
Monica Ssenkoloto<br />
Writers<br />
Sandra Bearden<br />
Elaine O. Chambless<br />
Steve Dupont<br />
Laura Freeman<br />
Doug Gillett<br />
Photographers<br />
Elaine O. Chambless, Steve Wood<br />
Editorial Contributors<br />
UAB Media Rel<strong>at</strong>ions<br />
UABMedical Public<strong>at</strong>ions<br />
UABSynopsis<br />
Charles A. Goldthwaite Jr.<br />
Dawn Mesa<br />
Meredith Murdock<br />
Tim L. Pennycuff<br />
Dale Short<br />
Anita Smith<br />
Russ Willcutt<br />
M<strong>at</strong>t Windsor<br />
AlumniBulletin<br />
ALABAMA MEDICAL<br />
AlumniBulletin<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> School <strong>of</strong> Medicine, <strong>Birmingham</strong>-Huntsville-Tuscaloosa; Telephone: (205) 934-4463;<br />
Fax: (205) 975-7299; Address: MAB, 811 20th Street South, 1530 3RD AVE S, BIRMINGHAM AL 35294-2140;<br />
Executive editor’s e-mail address: ppowell@uab.edu<br />
Table <strong>of</strong> Contents • Summer 2004 Issue<br />
News Briefs ....................................................................................................................... 2<br />
School and university news, faculty news, research and clinical news<br />
Cover Story: A Tradition <strong>of</strong> Service................................................................... 6<br />
UASOM <strong>doctors</strong> recall their war years<br />
Big Changes .................................................................................................................... 10<br />
A fast-paced day in the life <strong>of</strong> a UASOM resident<br />
Making Connections .................................................................................................. 12<br />
Robert Koehler takes the helm in the Department <strong>of</strong> Radiology<br />
Four SPORE .................................................................................................................... 12<br />
UAB’s l<strong>at</strong>est SPORE grant boosts pancre<strong>at</strong>ic-cancer research<br />
The Big Move ................................................................................................................. 13<br />
Sprinting toward completion <strong>at</strong> <strong>University</strong> Hospital’s North Pavilion<br />
Ready for the Future ................................................................................................ 14<br />
Researchers lay the groundwork for a new biodefense labor<strong>at</strong>ory in <strong>Birmingham</strong><br />
Searching for a Diabetes Cure............................................................................ 14<br />
Islet cell transplant<strong>at</strong>ion <strong>of</strong>fers hope <strong>of</strong> life without insulin<br />
In Praise <strong>of</strong> Wine ........................................................................................................ 15<br />
Is the fruit <strong>of</strong> the vine the gre<strong>at</strong> protector?<br />
Physicians’ Forum ....................................................................................................... 16<br />
Indigent care, part II<br />
Student Rounds ........................................................................................................... 18<br />
How new duty-hours rules have changed resident life<br />
From the Development Office .............................................................................20<br />
Kennamer Gift • Programs Worth Supporting • Lanier Gift • Film Premiere<br />
ALUMNI ASSOCIATION NEWS ....................................................................... 24<br />
2004 Annual Alumni Weekend • Class Notes • Alumni News • Prescription Pad<br />
• Alumni Form<br />
Alumni Pr<strong>of</strong>ile: The Schmitt Family, M.D.s ............................................. 30<br />
For these <strong>doctors</strong>, the UASOM runs in the blood<br />
Alumni Pr<strong>of</strong>ile: Tracey Miles, M.D. ................................................................. 31<br />
Making the commitment to family medicine<br />
From the Archives ...................................................................................................... 32<br />
A look <strong>at</strong> the <strong>Alabama</strong> Healthcare Hall <strong>of</strong> Fame<br />
CME Calendar .................................................................................................. Back Cover<br />
Published three times a year by the <strong>University</strong> <strong>of</strong> <strong>Alabama</strong> School <strong>of</strong> Medicine, <strong>Birmingham</strong>, <strong>Alabama</strong>. Produced by UAB’s Public<strong>at</strong>ions<br />
and Periodicals Group, Office <strong>of</strong> Public Rel<strong>at</strong>ions and Marketing, with the cooper<strong>at</strong>ion <strong>of</strong> Medical Public<strong>at</strong>ions, Office <strong>of</strong> the CEO <strong>of</strong><br />
UAB Health Systems.
SCHOOL AND<br />
UNIVERSITY NEWS<br />
REMEMBERING DR. KIRKLIN<br />
John W. Kirklin, M.D., the quiet, supremely efficient<br />
surgeon who shaped both UAB and the field<br />
<strong>of</strong> cardiology, passed away the night <strong>of</strong> April 21.<br />
Born in Muncie, Indiana, Kirklin revolutionized<br />
cardiovascular surgery through his development<br />
and refinement <strong>of</strong> the heart-bypass<br />
machine. In the 1950s, he modified the Gibbon<br />
heart-lung machine and performed the first openheart<br />
oper<strong>at</strong>ions carried out <strong>at</strong> the Mayo Clinic.<br />
“The world <strong>of</strong> medicine lost one <strong>of</strong> its giants<br />
today,” said UAB president Carol Garrison,<br />
Ph.D. “Dr. Kirklin’s dedic<strong>at</strong>ion to continually<br />
find better methods for tre<strong>at</strong>ing p<strong>at</strong>ients resulted<br />
in surgical techniques and health-care tre<strong>at</strong>ments<br />
th<strong>at</strong> saved literally millions <strong>of</strong> lives.”<br />
Kirklin’s efforts led to the development <strong>of</strong> a<br />
computerized intensive-care unit with continuous<br />
monitoring <strong>of</strong> vital functions th<strong>at</strong> became a<br />
model for modern ICUs around the world.<br />
“The contributions th<strong>at</strong> John Kirklin made to<br />
care provided to p<strong>at</strong>ients cannot be measured in<br />
any other terms other than those who are alive as<br />
a result <strong>of</strong> his efforts,” says Albert Pacifico, M.D.,<br />
director <strong>of</strong> cardiovascular surgery <strong>at</strong> UAB. “Those<br />
<strong>of</strong> us who were fortun<strong>at</strong>e enough to have trained<br />
under Dr. Kirklin learned the value <strong>of</strong> continually<br />
striving to improve p<strong>at</strong>ient care.”<br />
In 1966, Kirklin brought star power to UAB<br />
when he arrived as the new chair <strong>of</strong> the<br />
Department <strong>of</strong> Surgery and surgeon in chief for<br />
<strong>University</strong> Hospital, positions he would hold<br />
until 1982. His presence acted as a magnet for<br />
other talented physicians, who followed him to<br />
the young university. Over two decades, he built<br />
one <strong>of</strong> the most prestigious cardiovascular surgical<br />
training programs in the world before retiring<br />
from surgery in 1989.<br />
But Kirklin’s innov<strong>at</strong>ive ideas went beyond<br />
direct p<strong>at</strong>ient care. His organiz<strong>at</strong>ional capabilities<br />
led to the form<strong>at</strong>ion and development <strong>of</strong> the<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> Health Services Found<strong>at</strong>ion,<br />
the practice plan for faculty physicians <strong>at</strong> UAB.<br />
“John Kirklin recognized th<strong>at</strong> a public institution<br />
could not be saddled with the burdens associ<strong>at</strong>ed<br />
with yearly appropri<strong>at</strong>ions from the st<strong>at</strong>e if<br />
it wanted to reach the level <strong>of</strong> excellence he envisioned,”<br />
says Arnold G. Diethelm, M.D., who<br />
joined UAB in 1967 to establish the transplant<strong>at</strong>ion<br />
program and succeeded Kirklin as chairman<br />
from 1982 to 1999. “Bringing together the dispar<strong>at</strong>e<br />
parts <strong>of</strong> this fledgling medical center cre<strong>at</strong>ed<br />
the <strong>at</strong>mosphere necessary to bring world-class<br />
medical care to the city <strong>of</strong> <strong>Birmingham</strong>.”<br />
A hallmark <strong>of</strong> Kirklin’s career was his determin<strong>at</strong>ion<br />
to share inform<strong>at</strong>ion. He authored more than<br />
700 public<strong>at</strong>ions, and his textbook Cardiac Surgery<br />
remains the premier reference work on its subject.<br />
Future issues <strong>of</strong> the Medical Alumni Bulletin<br />
will take a closer look <strong>at</strong> the life, work, and legacy<br />
<strong>of</strong> this groundbreaking physician.<br />
HOIDAL NAMED INTERIM<br />
CEO OF UAB HEALTH SYSTEM<br />
David Hoidal, chief oper<strong>at</strong>ing <strong>of</strong>ficer <strong>of</strong> the<br />
UAB Health System, has been named interim<br />
chief executive <strong>of</strong>ficer, assuming the role following<br />
David Fine’s appointment as CEO <strong>of</strong> St.<br />
Luke’s Episcopal Health System in Houston.<br />
“As a result <strong>of</strong> his four years <strong>at</strong> UAB, and his<br />
many years <strong>of</strong> experience in health-care management,<br />
David Hoidal is very well suited to lead our<br />
management team,” says Carol Garrison, Ph.D.,<br />
UAB president and chair <strong>of</strong> the health system<br />
board.<br />
Hoidal joined UAB in 2000 as executive director<br />
<strong>of</strong> The Kirklin Clinic and president <strong>of</strong> the<br />
Callahan Eye Found<strong>at</strong>ion Hospital <strong>at</strong> UAB. In<br />
2002, he was named chief oper<strong>at</strong>ing <strong>of</strong>ficer for<br />
clinical programs for the health system. Prior to<br />
joining UAB, he served as senior vice president and<br />
COO <strong>of</strong> Tulane <strong>University</strong> Hospital and Clinic.<br />
AMWA HONORS ALABAMA LEGENDS<br />
The American Medical Women’s Associ<strong>at</strong>ion<br />
(AMWA) and the N<strong>at</strong>ional Library <strong>of</strong> Medicine<br />
recently honored seven “local legends” from the<br />
st<strong>at</strong>e <strong>of</strong> <strong>Alabama</strong>, four <strong>of</strong> whom have ties to the<br />
UASOM.<br />
A joint effort between the AMWA and the<br />
Library <strong>of</strong> Medicine, the Changing the Face <strong>of</strong><br />
Medicine: Local Legends program was designed to<br />
celebr<strong>at</strong>e the contribution <strong>of</strong> women physicians<br />
around the country. Members <strong>of</strong> Congress were<br />
asked to nomin<strong>at</strong>e physicians who have made a<br />
“significant impact in the field <strong>of</strong> medicine.”<br />
<strong>Alabama</strong>’s seven nominees were honored <strong>at</strong> a<br />
banquet in San Diego on Feb. 6, 2004. Those with<br />
ties to the UASOM are Sara Finley, M.D., a 1955<br />
gradu<strong>at</strong>e, now retired as pr<strong>of</strong>essor emeritus in the<br />
Department <strong>of</strong> Genetics after a distinguished<br />
career <strong>at</strong> the school; Sandral Hullett, M.D., a resident<br />
in 1979, now CEO <strong>of</strong> Cooper Green<br />
Hospital; Pamela Hudson, M.D., a resident in<br />
1986, now chief oper<strong>at</strong>ing <strong>of</strong>ficer and ethics and<br />
compliance <strong>of</strong>ficer for Crestwood Medical Center<br />
in Huntsville; and Lindy Harrell, M.D., a pr<strong>of</strong>essor<br />
in the Department <strong>of</strong> Neurology.<br />
In another UASOM connection, alumna<br />
Regina Benjamin, M.D. (class <strong>of</strong> 1984) was a<br />
member <strong>of</strong> the selection committee. She is now<br />
the associ<strong>at</strong>e dean for rural health <strong>at</strong> the<br />
<strong>University</strong> <strong>of</strong> South <strong>Alabama</strong> College <strong>of</strong> Medicine<br />
in Mobile.<br />
COLLECTING AMERICA’S TOP DOCTORS<br />
In a sign <strong>of</strong> the depth and breadth <strong>of</strong> experience<br />
<strong>at</strong> the UASOM, 49 physicians from UAB<br />
have been listed in the 2003 reference book<br />
America’s Top Doctors. The <strong>doctors</strong> were nomin<strong>at</strong>ed<br />
by other physicians and screened by a physician-directed<br />
research team.<br />
Top Doctors is a major medical-referral service; it<br />
surveys leading medical specialists and asks them<br />
which <strong>doctors</strong> they would visit if they needed tre<strong>at</strong>ment<br />
in their specialty. Only about 20,000 <strong>doctors</strong>—or<br />
3 percent <strong>of</strong> all physicians in the United<br />
St<strong>at</strong>es—are eventually included in the list. The service<br />
<strong>of</strong>fers d<strong>at</strong>a on each doctor’s credentials, licensing,<br />
and disciplinary review, as well as other inform<strong>at</strong>ion<br />
such as listening and communic<strong>at</strong>ion skills.<br />
The service also lists 620 leading hospitals in<br />
the n<strong>at</strong>ion, including UAB Hospital and<br />
Children’s Hospital.<br />
UAB HOSTS NEUROFIBROMATOSIS<br />
PATIENT SYMPOSIUM<br />
UAB and the N<strong>at</strong>ional Neur<strong>of</strong>ibrom<strong>at</strong>osis<br />
Found<strong>at</strong>ion (NNFF) hosted a symposium for<br />
p<strong>at</strong>ients and families with neur<strong>of</strong>ibrom<strong>at</strong>osis<br />
(NF) on January 17. Neur<strong>of</strong>ibrom<strong>at</strong>osis is the<br />
most common neurological disorder caused by a<br />
single gene mut<strong>at</strong>ion, affecting more than<br />
100,000 Americans. The disease can lead to disfigurement,<br />
blindness, deafness, skeletal abnormalities,<br />
brain and spinal tumors, loss <strong>of</strong> limbs,<br />
and learning disabilities. It is more prevalent than<br />
cystic fibrosis, hereditary muscular dystrophy,<br />
Huntington’s disease, and Tay-Sachs combined.<br />
The symposium was held in the Finley<br />
Conference Center, part <strong>of</strong> the Kaul Human<br />
Genetics Building. Fe<strong>at</strong>ured speakers included<br />
Bruce Korf, M.D., Ph.D., chair <strong>of</strong> the UASOM’s<br />
Department <strong>of</strong> Genetics and chair <strong>of</strong> the medical<br />
advisory board for the NNFF; Ludwine Messiaen,<br />
Ph.D., director <strong>of</strong> the first labor<strong>at</strong>ory to <strong>of</strong>fer<br />
mut<strong>at</strong>ional analysis for NF1, the most common<br />
form <strong>of</strong> NF; and Judy Small, Ph.D., director <strong>of</strong><br />
the clinical trials and technology transfer <strong>of</strong>fice<br />
for the NNFF. The panel conducted a questionand-answer<br />
session with <strong>at</strong>tendees, and tours <strong>of</strong><br />
the clinical and research labor<strong>at</strong>ories <strong>of</strong> the Kaul<br />
Human Genetics Building were <strong>of</strong>fered.<br />
In addition, the NNFF’s board <strong>of</strong> directors<br />
held its semi-annual meeting <strong>at</strong> UAB on the same<br />
day. This group normally meets in New York, but<br />
met in <strong>Birmingham</strong> because <strong>of</strong> Korf.<br />
2
News Briefs<br />
“SOWING THE SEEDS OF HEALTH”<br />
TRAINS HEALTH-CARE PROMOTERS<br />
Nine members <strong>of</strong> the <strong>Birmingham</strong> L<strong>at</strong>ino community<br />
have been trained to serve as resources for<br />
inform<strong>at</strong>ion on health topics and health-care services<br />
to L<strong>at</strong>ino members <strong>of</strong> three area C<strong>at</strong>holic churches,<br />
thanks to a collabor<strong>at</strong>ive endeavor known as Sowing<br />
the Seeds <strong>of</strong> Health. This program is funded by<br />
Mission and Ministry, Inc.; UAB’s Educ<strong>at</strong>ional<br />
Found<strong>at</strong>ion; and St. Vincent’s Found<strong>at</strong>ion.<br />
Sowing the Seeds <strong>of</strong> Health aims to elimin<strong>at</strong>e or<br />
reduce barriers by allowing lay persons in church<br />
communities to help one another by bringing<br />
together resources from UAB and St. Vincent’s.<br />
The program teaches health inform<strong>at</strong>ion and<br />
develops important skills in the volunteer promoters<br />
while providing a solution to many problems<br />
th<strong>at</strong> immigrant communities face, such as<br />
isol<strong>at</strong>ion and dependency.<br />
“The program gives us [trained promoters] an<br />
opportunity to live out our faith by helping others,<br />
and the community has been very receptive,”<br />
says Brenda Bullock, director <strong>of</strong> Hispanic ministry<br />
for the C<strong>at</strong>holic Diocese <strong>of</strong> <strong>Birmingham</strong>.<br />
“They feel like the church is taking an active role<br />
in caring for their needs.”<br />
Promoters have the knowledge and skills needed<br />
to assist community members with health<br />
issues. With training complete, these volunteers<br />
are available after Sunday church services and on a<br />
regular basis to answer questions and promote<br />
health in their communities. Each promoter is<br />
equipped with a resource manual <strong>of</strong> health services<br />
and topics, and is prepared to share this inform<strong>at</strong>ion<br />
through lectures, brochures, announcements,<br />
health fairs, and other appropri<strong>at</strong>e avenues.<br />
Monthly meetings allow the volunteers to share<br />
ideas and address concerns and issues.<br />
“The goal <strong>of</strong> training the Sowing the Seeds <strong>of</strong><br />
Health promoters is to assist the L<strong>at</strong>ino community<br />
in the gre<strong>at</strong>er <strong>Birmingham</strong> area in accessing<br />
health-care services, and to increase awareness<br />
among L<strong>at</strong>inos <strong>of</strong> health and wellness services in<br />
their communities,” says Lisa Reddington,<br />
Hispanic outreach coordin<strong>at</strong>or <strong>at</strong> St. Vincent’s<br />
Hospital, and Sowing’s program director along<br />
with Isabel Scarinci, M.D., assistant pr<strong>of</strong>essor in<br />
the UASOM’s Division <strong>of</strong> Preventive Medicine.<br />
A key component <strong>of</strong> this program is empowering<br />
community members and giving them the<br />
ability to lead and guide others, according to<br />
Scarinci. “The program belongs to the promoters,<br />
we just provide the guidance,” she says.<br />
WEB SITES WIN MEDALS<br />
FOR PUBLIC INFORMATION<br />
P<strong>at</strong>ient-friendly Web sites run by UAB have<br />
won gold and bronze medals from the N<strong>at</strong>ional<br />
Health Inform<strong>at</strong>ion Awards program, organized<br />
by the Health Inform<strong>at</strong>ion Resource Center. Now<br />
in their 10th year, the World Wide Web Health<br />
Awards are designed to establish a seal <strong>of</strong> quality<br />
for consumer health inform<strong>at</strong>ion.<br />
UAB’s “Tone Your Bones” osteoporosis site<br />
[www.toneyourbones.org] won a gold medal in<br />
the Hospital/Healthcare System c<strong>at</strong>egory. The<br />
question-and-answer column “Dear Doctors”<br />
[www.health.uab.edu/deardoc] received a bronze<br />
medal in th<strong>at</strong> c<strong>at</strong>egory.<br />
The “Tone Your Bones” site, which went<br />
online less than a year ago, is a component <strong>of</strong><br />
UAB’s Osteoporosis Prevention and Tre<strong>at</strong>ment<br />
Clinic. The site walks p<strong>at</strong>ients through a virtual<br />
clinic visit and provides up-to-d<strong>at</strong>e inform<strong>at</strong>ion<br />
on ways to prevent, tre<strong>at</strong>, and minimize the<br />
effects <strong>of</strong> osteoporosis.<br />
“Dear Doctors,” published by the UAB Health<br />
System’s Office <strong>of</strong> Medical Public<strong>at</strong>ions since<br />
1985, has received numerous st<strong>at</strong>e and n<strong>at</strong>ional<br />
awards for excellence in providing consumers reliable,<br />
up-to-d<strong>at</strong>e health and fitness inform<strong>at</strong>ion.<br />
Questions are submitted by readers and answers<br />
are provided by Health System physicians and<br />
other health-care pr<strong>of</strong>essionals.<br />
The Health Inform<strong>at</strong>ion Resource Center is a<br />
n<strong>at</strong>ional clearinghouse for consumer-health programs<br />
and m<strong>at</strong>erials.<br />
ALUMNUS TAPPED TO LEAD UNC<br />
HEALTH CARE SYSTEM<br />
William L. Roper, M.D., dean <strong>of</strong> the School <strong>of</strong><br />
Public Health <strong>at</strong> the <strong>University</strong> <strong>of</strong> North Carolina<br />
<strong>at</strong> Chapel Hill (UNCCH), has been named CEO<br />
<strong>of</strong> the <strong>University</strong> <strong>of</strong> North Carolina Health Care<br />
System. The appointment, effective March 15,<br />
2004, was announced January 23 by UNC president<br />
Molly Corbett Broad and r<strong>at</strong>ified by the<br />
UNC Board <strong>of</strong> Governors during a special meeting<br />
in Chapel Hill. Roper, who will serve concurrently<br />
as dean <strong>of</strong> the School <strong>of</strong> Medicine and vice<br />
chancellor for medical affairs <strong>at</strong> UNCCH, succeeds<br />
Jeffrey L. Houpt, who announced last spring<br />
his plans to step down from those posts.<br />
A pedi<strong>at</strong>rician, Roper has been dean <strong>of</strong><br />
UNCCH’s School <strong>of</strong> Public Health since 1997.<br />
He holds dual appointments as pr<strong>of</strong>essor <strong>of</strong> pedi<strong>at</strong>rics<br />
in the School <strong>of</strong> Medicine and pr<strong>of</strong>essor <strong>of</strong><br />
health policy and administr<strong>at</strong>ion in the School <strong>of</strong><br />
Public Health.<br />
Roper, 55, began his career in public health in<br />
his home st<strong>at</strong>e <strong>of</strong> <strong>Alabama</strong>, where he was health<br />
<strong>of</strong>ficer for the Jefferson County Department <strong>of</strong><br />
Health from 1977-83 and assistant st<strong>at</strong>e health<br />
<strong>of</strong>ficer for the <strong>Alabama</strong> Department <strong>of</strong> Public<br />
Health from 1981-83. A gradu<strong>at</strong>e <strong>of</strong> the<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong>, Roper earned his medical<br />
3<br />
degree <strong>at</strong> the <strong>University</strong> <strong>of</strong> <strong>Alabama</strong> School <strong>of</strong><br />
Medicine and his master’s degree in public health<br />
from the UAB School <strong>of</strong> Public Health.<br />
FACULTY NEWS<br />
LINDSEY HONORED AS DISTINGUISHED<br />
FACULTY LECTURER<br />
J. Russell Lindsey, D.V.M., pr<strong>of</strong>essor emeritus<br />
<strong>of</strong> genetics, has been chosen as the recipient <strong>of</strong> the<br />
2003 Distinguished Lecturer Award, the highest<br />
honor bestowed on a faculty member by the academic<br />
health center.<br />
Lindsey, who is intern<strong>at</strong>ionally known for his<br />
research in the field <strong>of</strong> compar<strong>at</strong>ive medicine,<br />
received the award on Oct. 28, 2003 <strong>at</strong> the<br />
Harbert Center. At the ceremony, he presented a<br />
lecture titled “A Celebr<strong>at</strong>ion <strong>of</strong> the Family” and<br />
received a check for $5,000.<br />
This award marks the l<strong>at</strong>est memorable moment<br />
in a long history between Lindsey and UAB. He<br />
joined the faculty 36 years ago as pr<strong>of</strong>essor and chair<br />
<strong>of</strong> the Department <strong>of</strong> Compar<strong>at</strong>ive Medicine. Under<br />
his leadership, the department became one <strong>of</strong> the top<br />
programs in the n<strong>at</strong>ion in the discovery and investig<strong>at</strong>ion<br />
<strong>of</strong> animal models <strong>of</strong> human diseases. He also<br />
established gradu<strong>at</strong>e biomedical research and labor<strong>at</strong>ory-animal<br />
model training programs for veterinarians<br />
and programs in managing animal resources for<br />
the university’s biomedical research community.<br />
A renowned researcher, Lindsey pioneered the<br />
study <strong>of</strong> diseases caused by microscopic organisms<br />
called mycoplasma. His early studies <strong>of</strong> one<br />
species, mycoplasma pulmonis, which causes pneumonia<br />
in mice, led him to engineer an animal<br />
model <strong>of</strong> “walking pneumonia” in humans.<br />
Subsequently he and his research team have engineered<br />
animal models for the study <strong>of</strong> human diseases<br />
including diabetes, Alzheimer’s, prost<strong>at</strong>e cancer,<br />
interstitial cystitis, and various viral infections.<br />
Lindsey has published more than 130 articles<br />
about his work and has received numerous<br />
n<strong>at</strong>ional honors. Among his many pr<strong>of</strong>essional<br />
affili<strong>at</strong>ions, he has served on scientific review<br />
boards <strong>of</strong> the N<strong>at</strong>ional Institutes <strong>of</strong> Health, the<br />
Food and Drug Administr<strong>at</strong>ion, Veterans Affairs,<br />
and the Department <strong>of</strong> Energy. He also represented<br />
the N<strong>at</strong>ional Associ<strong>at</strong>ion <strong>of</strong> St<strong>at</strong>e Universities<br />
and Land Grant Colleges on the board <strong>of</strong> trustees<br />
<strong>of</strong> the Associ<strong>at</strong>ion for Assessment and Accredit<strong>at</strong>ion<br />
<strong>of</strong> Labor<strong>at</strong>ory Animal Care.<br />
Lindsey received his Master’s <strong>of</strong> Science degree<br />
from Auburn <strong>University</strong> and his degree in veterinary<br />
medicine from the <strong>University</strong> <strong>of</strong> Georgia.<br />
Since his retirement from UAB in 2001, he continues<br />
to teach and consult for universities and
News Briefs<br />
research institutions worldwide, including the<br />
UASOM’s Department <strong>of</strong> Anesthesiology.<br />
WHITLEY NATIONAL FINALIST FOR<br />
HUMANISM IN MEDICINE AWARD<br />
Richard Whitley, M.D., pr<strong>of</strong>essor <strong>of</strong> pedi<strong>at</strong>ric<br />
and infectious diseases <strong>at</strong> the UASOM, has been<br />
selected as a distinguished finalist for the 2003<br />
AAMC Humanism in Medicine Award. The annual<br />
award is sponsored by the Associ<strong>at</strong>ion <strong>of</strong><br />
American Medical Colleges (AAMC) through the<br />
support <strong>of</strong> the Pfizer Medical Humanities Initi<strong>at</strong>ive.<br />
Whitley is one <strong>of</strong> 50 honorees from across the<br />
n<strong>at</strong>ion nomin<strong>at</strong>ed by the AAMC Organiz<strong>at</strong>ion <strong>of</strong><br />
Student Represent<strong>at</strong>ives, based on five defining<br />
characteristics <strong>of</strong> humanism in medical educ<strong>at</strong>ion:<br />
positive mentoring skills, involvement in community<br />
service, compassion/sensitivity, collabor<strong>at</strong>ion,<br />
and observance <strong>of</strong> pr<strong>of</strong>essional ethics.<br />
Whitley’s nomin<strong>at</strong>ion is a tribute to his commitment<br />
to training and mentoring young physicians<br />
and having them, in turn, pass on their<br />
knowledge to a new gener<strong>at</strong>ion <strong>of</strong> physicians.<br />
“Like healing, learning happens best when<br />
expertise is joined with caring and partnership,”<br />
says Mike Magee, M.D., vice president <strong>of</strong> medical<br />
rel<strong>at</strong>ions and science policy for Pfizer Inc. and<br />
director <strong>of</strong> the Pfizer Medical Humanities<br />
Initi<strong>at</strong>ive. “The medical students who nomin<strong>at</strong>ed<br />
Dr. Whitley recognized the human qualities th<strong>at</strong><br />
make him both an outstanding teacher and an<br />
outstanding physician. It’s through the stellar<br />
example <strong>of</strong> mentors like Dr. Whitley th<strong>at</strong> the next<br />
gener<strong>at</strong>ion <strong>of</strong> physicians will learn how to practice<br />
compassion, partnership, and understanding in<br />
the practice <strong>of</strong> medicine.”<br />
KOEHLER NAMED RADIOLOGY CHAIR<br />
Robert E. Koehler, M.D., has been appointed<br />
chair <strong>of</strong> the Department <strong>of</strong> Radiology effective<br />
Nov. 1, 2003. Koehler was vice-chair <strong>of</strong> the department<br />
before being named interim chair last year.<br />
In announcing the appointment, William B.<br />
Deal, M.D., dean <strong>of</strong> the School <strong>of</strong> Medicine, said,<br />
“We are pleased th<strong>at</strong> we were able to find such a highly<br />
qualified person within our own faculty to lead this<br />
large department th<strong>at</strong> is so integral to the quality <strong>of</strong><br />
p<strong>at</strong>ient care and research <strong>at</strong> UAB. Bob Koehler’s credentials<br />
and long service to UAB will serve him well.”<br />
Koehler, who joined UAB in 1982, says, “It is<br />
definitely an honor and a challenge to have the<br />
opportunity to lead this distinguished faculty.<br />
The talent and dedic<strong>at</strong>ion <strong>of</strong> our radiology faculty<br />
have brought n<strong>at</strong>ional recognition to UAB,<br />
especially for resident educ<strong>at</strong>ion and skilled, subspecialized<br />
service to p<strong>at</strong>ients. We will now work<br />
to further strengthen those areas and to grow the<br />
department’s research and extramural funding.”<br />
For more on Koehler and his new position, see<br />
the article Making Connections on page 12.<br />
DACHEUX WINS EYE RESEARCH AWARD<br />
Ramon F. Dacheux II, Ph.D., pr<strong>of</strong>essor in the<br />
Department <strong>of</strong> Ophthalmology, has been granted<br />
a $65,000 Senior Scientific Investig<strong>at</strong>or Award by<br />
Research to Prevent Blindness (RPB). RPB Senior<br />
Scientific Awards support n<strong>at</strong>ionally recognized<br />
scientists conducting eye research <strong>at</strong> medical institutions<br />
in the United St<strong>at</strong>es. Dacheux is one <strong>of</strong><br />
122 scientists <strong>at</strong> 50 institutions to be honored<br />
since the award was established in 1987.<br />
Dacheux’s primary research interest is in the role <strong>of</strong><br />
the ganglion cell in the onset <strong>of</strong> glaucoma, the most<br />
common cause <strong>of</strong> blindness worldwide. Dacheux is<br />
examining how different ganglion cell types respond<br />
to changes in intraocular pressure. This inform<strong>at</strong>ion<br />
could lead to a test for early diagnosis <strong>of</strong> glaucoma,<br />
before cell de<strong>at</strong>h and vision loss occur.<br />
RPB is the world’s leading voluntary organiz<strong>at</strong>ion<br />
supporting eye research. Since it was founded<br />
in 1960, RPB has channeled hundreds <strong>of</strong> millions<br />
<strong>of</strong> dollars to medical institutions throughout<br />
the United St<strong>at</strong>es for research into all blinding eye<br />
diseases. To d<strong>at</strong>e, the organiz<strong>at</strong>ion has awarded<br />
grants totaling more than $2 million to UAB.<br />
PIONEERING ENT JACK ODESS DIES<br />
John S. “Jack” Odess, M.D., <strong>of</strong> Chelsea, a pioneer<br />
in developing new services and new medical procedures<br />
for ENT p<strong>at</strong>ients, died Nov. 4, 2003. He is<br />
credited with helping organize the first cleft-pal<strong>at</strong>e<br />
clinic in the United St<strong>at</strong>es and with pioneering the<br />
oper<strong>at</strong>ing microscope. He was 80 years old.<br />
“Dr. Odess was a brilliant and generous man, who<br />
was dedic<strong>at</strong>ed to the health and well-being <strong>of</strong> this community,”<br />
says UAB president Carol Garrison, Ph.D.<br />
Odess was a gradu<strong>at</strong>e <strong>of</strong> Vanderbilt <strong>University</strong><br />
School <strong>of</strong> Medicine. In the 1950s, he returned to<br />
<strong>Birmingham</strong>, where he entered priv<strong>at</strong>e practice<br />
and joined the faculty <strong>of</strong> the UASOM. In 1956,<br />
he helped reestablish the otolaryngology residence<br />
training <strong>at</strong> <strong>University</strong> Hospital. He pioneered the<br />
oper<strong>at</strong>ing microscope and became the first surgeon<br />
in the st<strong>at</strong>e to use it to perform a stapedectomy,<br />
a procedure th<strong>at</strong> restores mobility to the small<br />
bones <strong>of</strong> the inner ear, thereby improving hearing.<br />
He also worked with the Talladega School for<br />
the Deaf and the Junior League Speech and<br />
Hearing Clinic, and was on staff <strong>at</strong> St. Vincent’s<br />
Hospital, Baptist Medical Center–Montclair and<br />
–Princeton, and Children’s Hospital. In addition,<br />
he worked with the Council <strong>of</strong> Accredit<strong>at</strong>ion on<br />
Hearing Conserv<strong>at</strong>ion and assisted in the development<br />
<strong>of</strong> the Occup<strong>at</strong>ional Safety and Health<br />
Administr<strong>at</strong>ion standards to prevent hearing loss<br />
from industrial noise.<br />
Although Odess retired from priv<strong>at</strong>e medical<br />
practice in 1981, he remained active in business and<br />
civic endeavors and the ongoing evolution <strong>of</strong> the<br />
UASOM’s Division <strong>of</strong> Otolaryngology. In 1989, he<br />
provided funding to establish the John S. Odess<br />
Pr<strong>of</strong>essor and Division Director-Otolaryngology/<br />
Head and Neck Surgery Chair in the School<br />
<strong>of</strong> Medicine.<br />
RESEARCH AND CLINICAL NEWS<br />
UAB JOINS CONSORTIUM TO STUDY<br />
RARE DISEASES<br />
Researchers <strong>at</strong> the UAB Civitan Intern<strong>at</strong>ional<br />
Research Center will be part <strong>of</strong> a new multicenter<br />
Rare Diseases Clinical Research Center<br />
(RDCRC) to study three rare syndromes: Rett,<br />
Angelman, and Prader-Willi. The center is funded<br />
by a $6.25 million, five-year grant from the<br />
N<strong>at</strong>ional Institutes <strong>of</strong> Health (NIH).<br />
“The center will help develop an understanding<br />
<strong>of</strong> how these diseases affect individuals<br />
throughout their lives and set the stage for studying<br />
tre<strong>at</strong>ments th<strong>at</strong> may help reduce the effects <strong>of</strong><br />
such diseases,” says Alan K. Percy, M.D., associ<strong>at</strong>e<br />
director <strong>of</strong> the Civitan Center and a leading intern<strong>at</strong>ional<br />
authority on Rett syndrome. The grant is<br />
intended to interface with the UAB General<br />
Clinical Research Center and the Mental<br />
Retard<strong>at</strong>ion and Developmental Disabilities<br />
Research Center.<br />
The principal investig<strong>at</strong>or in the study, Arthur<br />
Beaudet, M.D., chair <strong>of</strong> the Baylor College <strong>of</strong><br />
Medicine’s Department <strong>of</strong> Molecular and Human<br />
Genetics, says the grant will promote clinical<br />
research into disorders th<strong>at</strong> are “<strong>of</strong>ten neglected<br />
because they affect a small percentage <strong>of</strong> the popul<strong>at</strong>ion.”<br />
Beaudet expects th<strong>at</strong> the focus <strong>of</strong> the center<br />
will expand to other disorders in the coming years.<br />
UAB NAMED AUTOIMMUNITY<br />
CENTER OF EXCELLENCE<br />
UAB has received a five-year, $3.6 million NIH<br />
grant to establish an Autoimmunity Center <strong>of</strong><br />
Excellence—one <strong>of</strong> four newly named centers and<br />
one <strong>of</strong> only nine such centers n<strong>at</strong>ionwide. The centers<br />
bring together investig<strong>at</strong>ors representing diverse<br />
disciplines from across the country to conduct basic<br />
research and clinical studies aimed <strong>at</strong> developing<br />
new therapies for autoimmune diseases.<br />
“Autoimmune disorders and diseases comprise<br />
a significant portion <strong>of</strong> the health-care burden in<br />
this country,” says Robert H. Carter, M.D., associ<strong>at</strong>e<br />
pr<strong>of</strong>essor <strong>of</strong> medicine with the Division <strong>of</strong><br />
Clinical Immunology/Rheum<strong>at</strong>ology and director<br />
<strong>of</strong> the UAB center. “NIH cre<strong>at</strong>ed the network<br />
4
News Cover Briefs Story<br />
<strong>of</strong> autoimmunity centers to speed transl<strong>at</strong>ion <strong>of</strong><br />
basic research into new therapies and to further<br />
our understanding <strong>of</strong> human immunology.”<br />
UAB’s long and notable history <strong>of</strong> basic and<br />
clinical study in the field <strong>of</strong> autoimmune research<br />
was a key factor in the NIH’s decision to name it<br />
a center <strong>of</strong> excellence. “UAB received the highest<br />
score among all institutions applying for this<br />
award,” Carter says. “We have gre<strong>at</strong> expertise and<br />
many proven strengths in this area <strong>of</strong> research.”<br />
In addition to its basic research activities, the<br />
center, as part <strong>of</strong> its grant applic<strong>at</strong>ion, has proposed<br />
two clinical studies: one on psori<strong>at</strong>ic arthritis<br />
and one on lupus. “A steering committee <strong>of</strong><br />
leaders representing all the centers will decide<br />
which clinical studies to conduct and which centers<br />
will particip<strong>at</strong>e based on each center’s expertise,”<br />
Carter says. “If one or both <strong>of</strong> UAB’s proposed<br />
clinical studies are selected, the center will<br />
receive additional funding to support these trials.”<br />
“Collabor<strong>at</strong>ive center projects will unite the<br />
expertise <strong>of</strong> investig<strong>at</strong>ors working in diverse areas<br />
<strong>of</strong> human autoimmune disease,” says Larry W.<br />
Moreland, M.D., director <strong>of</strong> clinical activities for<br />
the UAB center. “Taking part in the development<br />
and implement<strong>at</strong>ion <strong>of</strong> these groundbreaking<br />
investig<strong>at</strong>ions will expand our collective knowledge<br />
and place UAB <strong>at</strong> the forefront <strong>of</strong> human<br />
immunological research.”<br />
NIH AWARDS UAB<br />
NEW CENTER ON MINORITY<br />
HEALTH DISPARITIES<br />
Diabetes kills African Americans <strong>at</strong> a r<strong>at</strong>e double<br />
th<strong>at</strong> <strong>of</strong> whites. Colon-cancer mortality is a<br />
third higher, and overall mortality is 50 percent<br />
higher. Now UAB will use a $4.25 million federal<br />
grant to try to help change those st<strong>at</strong>istics through<br />
research, screening and educ<strong>at</strong>ion programs, and<br />
training <strong>of</strong> health-rel<strong>at</strong>ed pr<strong>of</strong>essionals.<br />
The four-year grant comes from the NIH’s<br />
N<strong>at</strong>ional Center on Minority Health and Health<br />
Disparities. It establishes a Regional Deep South<br />
Project Export Center <strong>of</strong> Excellence for Minority<br />
Health (Project Export) to begin developing a<br />
health-disparities center. Selwyn M. Vickers,<br />
M.D., pr<strong>of</strong>essor <strong>of</strong> surgery, is principal investig<strong>at</strong>or<br />
for the program. The grant was developed in<br />
conjunction with co-principal investig<strong>at</strong>ors Mona<br />
Fouad, M.D., Edward Partridge, M.D., and<br />
C<strong>at</strong>arina Kiefe, M.D.<br />
“The health gap between minorities and whites<br />
is a problem th<strong>at</strong> st<strong>at</strong>istics make obvious, and it is<br />
particularly severe in the Black Belt counties <strong>of</strong><br />
<strong>Alabama</strong> with highest concentr<strong>at</strong>ions <strong>of</strong> African<br />
Americans,” Vickers says. “This new center <strong>of</strong><br />
excellence, incorpor<strong>at</strong>ing Project Export, will help<br />
coordin<strong>at</strong>e and build on existing efforts <strong>at</strong> UAB<br />
to comb<strong>at</strong> this problem <strong>of</strong> health disparities in<br />
our st<strong>at</strong>e and region.”<br />
UAB’s center is one <strong>of</strong> seven around the n<strong>at</strong>ion<br />
to receive st<strong>at</strong>us as a comprehensive center <strong>of</strong><br />
excellence and full funding in this fiscal year. The<br />
center aims to build partnerships <strong>at</strong> institutions<br />
enrolling a significant number <strong>of</strong> students from<br />
health-disparity popul<strong>at</strong>ions and will promote<br />
particip<strong>at</strong>ion and training in biomedical and<br />
behavioral research <strong>at</strong> these historically black colleges<br />
and universities.<br />
Vickers noted th<strong>at</strong> Project Export initially will<br />
reach out to the community through screening<br />
and educ<strong>at</strong>ion programs for diabetes and colon<br />
cancer. The diabetes program will be conducted<br />
in Jefferson County in associ<strong>at</strong>ion with the faithbased<br />
Center for Urban Missions, and colon cancer<br />
will be the target <strong>of</strong> programs in Macon<br />
County in partnership with the BND Cancer<br />
Center, a priv<strong>at</strong>e organiz<strong>at</strong>ion.<br />
Project Export will be an integral part <strong>of</strong> the center<br />
and make use <strong>of</strong> UAB’s research and training<br />
expertise in partnership with historically black colleges<br />
and universities in the st<strong>at</strong>e. “There is a need<br />
to recruit and train minorities as health workers,<br />
particularly in the Black Belt,” Vickers says. “A<br />
summer training program is planned in conjunction<br />
with the black colleges in order to prepare students<br />
for careers in allied-health pr<strong>of</strong>essions.”<br />
USING WIRELESS TECHNOLOGY TO<br />
IMPROVE EMERGENCY MEDICAL CARE<br />
Rapid advances in wireless communic<strong>at</strong>ion<br />
technology could provide big benefits in improving<br />
emergency medical response, say UAB<br />
researchers. The l<strong>at</strong>est technology could produce<br />
major improvements in the 911 system and in<br />
how Emergency Medical Services (EMS) teams<br />
handle medical emergencies ranging from heart<br />
<strong>at</strong>tacks to large-scale disasters.<br />
UAB researchers have received a $3.2 million<br />
contract from the N<strong>at</strong>ional Library <strong>of</strong> Medicine, a<br />
branch <strong>of</strong> the NIH, to study the integr<strong>at</strong>ion <strong>of</strong><br />
wireless technology with EMS services. The study,<br />
called Advanced Network Infrastructure for Health<br />
and Disaster Management, is directed by Helmuth<br />
Orthner, Ph.D., pr<strong>of</strong>essor <strong>of</strong> health inform<strong>at</strong>ics in<br />
UAB’s School <strong>of</strong> Health Rel<strong>at</strong>ed Pr<strong>of</strong>essions.<br />
“Our ability to handle medical emergencies is<br />
<strong>at</strong> a revolutionary threshold with the emergence<br />
<strong>of</strong> technologies such as secure, high-speed wireless<br />
communic<strong>at</strong>ions and powerful hand-held computing<br />
and communic<strong>at</strong>ion devices,” says<br />
Orthner. “This study will allow us to test how to<br />
integr<strong>at</strong>e these technologies within the EMS community<br />
in an important new way.”<br />
Orthner says the lessons learned will have value<br />
for EMS teams responding to any kind <strong>of</strong> medical<br />
emergency. He says any changes to the current<br />
system must be capable <strong>of</strong> rapid, failsafe escal<strong>at</strong>ion<br />
so th<strong>at</strong> the system can seamlessly respond to<br />
situ<strong>at</strong>ions ranging from an individual 911 call to<br />
major disasters such as c<strong>at</strong>astrophic we<strong>at</strong>her<br />
events or terrorist <strong>at</strong>tacks.<br />
Co-principal investig<strong>at</strong>ors with Orthner are<br />
Gary Grimes, Ph.D., UAB pr<strong>of</strong>essor <strong>of</strong> engineering,<br />
and Thomas Terndrup, M.D., chair <strong>of</strong> the<br />
Department <strong>of</strong> Emergency Medicine.<br />
SCREEN-SAVER PROVES EFFECTIVE IN<br />
EDUCATING HOSPITAL PHYSICIANS<br />
A training program th<strong>at</strong> uses interactive screensaver<br />
images linked to a Web site to prepare hospital-based<br />
clinicians to respond to bioterrorist<br />
<strong>at</strong>tacks is an effective altern<strong>at</strong>ive to more costly<br />
and more time-consuming educ<strong>at</strong>ional methods,<br />
according to a recent study published in the<br />
American Journal <strong>of</strong> Infection Control. Thomas<br />
Terndrup, M.D., chair <strong>of</strong> the Department <strong>of</strong><br />
Emergency Medicine and director <strong>of</strong> the Center<br />
for Emergency Care and Disaster Preparedness,<br />
led the pilot study to develop and test the new<br />
training program, available on the center’s Web<br />
site <strong>at</strong> [www.uab.edu/cecdp].<br />
“Before the terrorist <strong>at</strong>tacks in September 2001<br />
and subsequent anthrax <strong>at</strong>tacks, few hospitals<br />
considered it a priority to integr<strong>at</strong>e bioterrorist<br />
preparedness into their disaster plans,” Terndrup<br />
says. “Afterward, however, the challenge to educ<strong>at</strong>e<br />
hospital-based clinicians and infection-control<br />
practitioners to recognize and respond to a<br />
bioterrorist event took precedence.”<br />
The pilot study, funded in part by the Agency<br />
for Healthcare Research and Quality, aimed to<br />
streamline hospital preparedness efforts through<br />
the implement<strong>at</strong>ion <strong>of</strong> a screen-saver program as<br />
an educ<strong>at</strong>ional tool for clinicians. “Initi<strong>at</strong>ives to<br />
prepare hospital-based practitioners must fit<br />
among the demands <strong>of</strong> p<strong>at</strong>ient care, administr<strong>at</strong>ive<br />
duties, and continuing educ<strong>at</strong>ion within specialties,”<br />
Terndrup says. “The interactive screensaver<br />
program was designed with these consider<strong>at</strong>ions<br />
in mind.”<br />
The screen-saver program also may direct the<br />
user to access a Web site for additional bioterrorist<br />
inform<strong>at</strong>ion and Web-based learning modules<br />
relevant to the user’s particular specialty. The site,<br />
[www.bioterrorism.uab.edu], currently <strong>of</strong>fers<br />
nine continuing-educ<strong>at</strong>ion courses developed<br />
specifically for the following specialties: emergency<br />
medicine, radiology, p<strong>at</strong>hology, infection<br />
control, pedi<strong>at</strong>rics, family practice, internal medicine,<br />
and derm<strong>at</strong>ology.<br />
5
Cover Story<br />
★★★★★<br />
UASOM DOCTORS<br />
SERVING OUR NATION IN TIMES OF NEED<br />
By Dale Short<br />
ALANDING SHIP IN THE PACIFIC OCEAN,<br />
NEAR GUADALCANAL. A FIELD HOSPITAL IN<br />
THE VIETNAMESE COUNTRYSIDE. A PRISONER-OF-<br />
WAR CAMP IN THE IRAQI DESERT.<br />
FOR DECADES, SCHOOL OF MEDICINE STUDENTS<br />
AND ALUMNI HAVE BEEN CALLED TO SERVE THEIR<br />
COUNTRY IN TIMES OF WAR. BY ITS NATURE, THAT<br />
SERVICE ENTAILS AN INTENSE EMOTIONAL CONFLICT<br />
FOR DOCTORS: WORKING TO SAVE LIVES, AS PART OF<br />
AN ENTERPRISE WHOSE GOAL IS TO TAKE LIVES. BUT<br />
A COMMON THEME, FOR THOSE WILLING TO TALK<br />
ABOUT THEIR EXPERIENCES, IS THAT MILITARY DUTY<br />
HELPED THEM BECOME BETTER PHYSICIANS.<br />
6
Full Speed Ahead:<br />
Lonnie Funderburg, World War II Veteran<br />
Lonnie Funderburg, M.D. (’50), says his World War II service as a naval<br />
<strong>of</strong>ficer was the precursor to his decision to enroll <strong>at</strong> the then-Medical College<br />
<strong>of</strong> <strong>Alabama</strong> in 1946—after initially pursuing a career as a pharmacist. “The<br />
majority <strong>of</strong> the students th<strong>at</strong> year had come out <strong>of</strong> the military,” Funderburg<br />
recalls. “After experiencing life in the service, we had a chance to go to school<br />
full-time on the G.I. Bill, and we felt pretty privileged.<br />
“I was no honors student, but I wasn’t afraid <strong>of</strong> work. I felt I had to prove<br />
to them th<strong>at</strong> I could make the grade, so I bore down pretty hard. We all knew<br />
how important educ<strong>at</strong>ion was, and we felt we had to get busy, making up for<br />
lost time. There was no time to waste, no time to be foolish.”<br />
Funderburg’s damn-the-torpedoes approach has continued throughout his<br />
career. He served an internship in the naval hospital in Philadelphia, conducted<br />
research in narcotic and spinal anesthesia, and worked for 32 years <strong>at</strong> wh<strong>at</strong><br />
is now Baptist Medical Centers. Along the way he found time to study business<br />
<strong>at</strong> Harvard, and to teach anesthesia on mission trips to Nigeria, Haiti,<br />
and Gaza, and English on trips to China.<br />
“I guess I’m sort <strong>of</strong> manic-compulsive,” Funderburg laughs. “I want to get<br />
things done, and I can’t stand to waste an opportunity.” He and his wife,<br />
Mary, who worked as a religious educ<strong>at</strong>or before rearing their two sons and a<br />
daughter, will celebr<strong>at</strong>e 61 years <strong>of</strong> marriage this spring.<br />
“I like to make money, but it’s never been a major factor in wh<strong>at</strong> I choose<br />
to do,” Funderburg says. “If the military and God taught me anything, it’s to<br />
take a crooked stick and make the most you can from it. But God’s been good<br />
to us. I’ve got no complaints.”<br />
(Clockwise from top left) Lonnie Funderburg ashore in New Zealand; Terrell<br />
Spencer <strong>at</strong> his Army Medical Corps st<strong>at</strong>ion in Pleiku, Vietnam; camels paid<br />
frequent visits to Charles Kent Powers Jr.’s field hospital in the Iraqi desert;<br />
Robert Lee Henderson in his school days; medical students <strong>at</strong> the<br />
Tuscaloosa campus during the Second World War; Henderson <strong>at</strong> a camp for<br />
Special Forces advisors in Vietnam; Spencer on a medical tour <strong>of</strong> Army firebases;<br />
wartime medical students in Tuscaloosa; Ronald Orso gradu<strong>at</strong>ed in<br />
the class <strong>of</strong> 1972; Phillip Foshee with his Air Force F-80 fighter; by the time<br />
he gradu<strong>at</strong>ed from medical school in 1962, Foshee had three children;<br />
Henderson tre<strong>at</strong>ing a Montagnard villager in Vietnam.<br />
★★★★★<br />
C<strong>at</strong>ching Up:<br />
Phillip Foshee, Korean War Veteran<br />
Phillip Foshee, M.D. (’62), also found th<strong>at</strong> his military<br />
service—as an Air Force pilot and instructor during the<br />
Korean War—shaped his career choice. When he joined<br />
the Air Force in December 1950, he was facing the draft<br />
while home from college and partway through a degree in<br />
architecture, the pr<strong>of</strong>ession his older brother had chosen.<br />
“My local draft board had just announced they were taking<br />
pretty much everybody in town,” Foshee recalls, “so I<br />
could see it was time for me to sign up.”<br />
For Americans, it was a time <strong>of</strong> shock and crisis in the<br />
burgeoning Korean conflict. Just weeks earlier, a surprise<br />
<strong>at</strong>tack by Chinese and North Korean soldiers had trapped<br />
15,000 Marines, killing 3,000 <strong>of</strong> them and wounding<br />
another 7,000. With ground<br />
troops struggling, America’s air<br />
power seemed the only answer<br />
for turning the tide, and the Air<br />
Force began a massive buildup.<br />
Foshee’s first duty st<strong>at</strong>ion was<br />
San Francisco, where he trained<br />
as a radio oper<strong>at</strong>or on the B-29<br />
bomber. He applied for pilot<br />
school, and gradu<strong>at</strong>ed as a pilot<br />
with a knack for teaching. For<br />
the remaining three years <strong>of</strong> his<br />
stint, he worked as a flight<br />
instructor <strong>at</strong> a training facility<br />
in Greenville, Mississippi.<br />
After his Air Force career, he<br />
joined the <strong>Alabama</strong> Air N<strong>at</strong>ional<br />
Guard and began taking premed<br />
courses in college.<br />
“I had two cousins who were<br />
surgeons,” says Foshee, “and<br />
my f<strong>at</strong>her always wanted to be a physician, but for some<br />
reason I didn’t think I was cut out for it. I’ll never be sure<br />
exactly why I finally chose medicine, but I decided it was<br />
wh<strong>at</strong> the Lord wanted me to do.”<br />
The rel<strong>at</strong>ively l<strong>at</strong>e start was a big hurdle to overcome: “I<br />
was the next-to-oldest guy in my class, and by the time I<br />
gradu<strong>at</strong>ed I had three children. I was afraid I wouldn’t get<br />
a residency.” Th<strong>at</strong> fear turned out to be unfounded, as he<br />
was accepted <strong>at</strong> Mobile General Hospital and l<strong>at</strong>er worked<br />
<strong>at</strong> South Highlands Infirmary in <strong>Birmingham</strong>. For a while<br />
he gravit<strong>at</strong>ed toward surgery, but eventually chose general<br />
practice, serving for 39 years in the town <strong>of</strong> Clanton, where<br />
he has remained since his retirement.<br />
Foshee still does flight physicals for pilots <strong>at</strong> a small<br />
<strong>of</strong>fice in his home and tre<strong>at</strong>s his grandchildren’s occasional<br />
playground injuries. One <strong>of</strong> the pleasures <strong>of</strong> retirement is<br />
meeting multiple gener<strong>at</strong>ions <strong>of</strong> his former p<strong>at</strong>ients as he<br />
goes about his day. “I see them on the street, or in the grocery<br />
store, all the time.”<br />
(Left) Lonnie<br />
Funderburg in his<br />
“dress whites” as<br />
a U.S. Navy <strong>of</strong>ficer.<br />
“About the<br />
only time I wore<br />
those was when I<br />
got married in<br />
1943,” he says.<br />
(Above) Phillip<br />
Foshee was a<br />
flight instructor<br />
with the<br />
<strong>Alabama</strong> Air<br />
N<strong>at</strong>ional Guard<br />
while taking<br />
pre-med classes<br />
<strong>at</strong> college.<br />
7
Cover Story<br />
He’s given up flying and has don<strong>at</strong>ed his home-built Viking airplane<br />
to the Wings <strong>of</strong> Hope humanitarian group in St. Louis. “They’ll use it<br />
in their medical missions around the world,” Foshee says. “I’m just<br />
glad to be able to help.”<br />
Recognizing the Enemy:<br />
Terrell Spencer, Vietnam War Veteran<br />
Like countless other physicians around the country, Terrell Spencer,<br />
M.D. (’68), <strong>at</strong>tended medical school under the constant shadow <strong>of</strong> the<br />
Vietnam War. “Nearly everybody was being called up,” he says. “I<br />
could have been deferred an extra year for more training, but since I<br />
had to go anyway, I decided to go.”<br />
enemy soldier came in wounded, it was my job to tre<strong>at</strong> him, too.<br />
There’s an old saying th<strong>at</strong> war is 29 days <strong>of</strong> boredom followed by one<br />
day <strong>of</strong> sheer terror, and th<strong>at</strong>’s very true.”<br />
Two indelible memories <strong>of</strong> Spencer’s Vietnam service are the .45<br />
autom<strong>at</strong>ic pistol he carried everywhere, but never had to fire, and the<br />
phone call he received in the middle <strong>of</strong> the jungle telling him his first<br />
child had been born.<br />
“The main thing those experiences taught me,” he says, “is how<br />
similar all people are, how many things they have in common.<br />
Under stress, you learn pretty fast which aspects <strong>of</strong> our lives are just<br />
cultural and which ones strike a chord with everybody. The<br />
Vietnamese prisoners had the same fears and wants as everybody<br />
else. You learn to connect with p<strong>at</strong>ients as people, because all those<br />
surface differences just wash away.”<br />
Left to right: During his time in Vietnam, Spencer was awarded the Bronze Star, the Air<br />
Medal, and the Army Commend<strong>at</strong>ion Medal; Henderson prepares for a training<br />
parachute jump with Vietnamese special forces troops; Ronald Orso poses with General<br />
Norman Schwarzkopf in Saudi Arabia during Oper<strong>at</strong>ion Desert Storm.<br />
As a member <strong>of</strong> the Army Medical Corps, Spencer was st<strong>at</strong>ioned<br />
in the rural town <strong>of</strong> Pleiku in Vietnam’s central highlands. “It was<br />
a fairly primitive setup, from which we crafted a very fine medical<br />
group,” he says. “We had some 30 medics, aid st<strong>at</strong>ions, helicopter<br />
services, ambulances. We learned from scr<strong>at</strong>ch, and as a result we<br />
learned quickly.”<br />
A popular misconception, according to Spencer, is th<strong>at</strong> military<br />
<strong>doctors</strong> mainly tre<strong>at</strong> comb<strong>at</strong> wounds. In fact, he says, “Illnesses always<br />
outnumber injuries. You can have whole divisions taken out by diarrhea,<br />
malaria, dengue fever. We saw injuries from field stoves blowing<br />
up, from two-ton truck tires falling on people.<br />
“Then, once every few weeks, there were comb<strong>at</strong> injuries, which we<br />
tried to stabilize in the field and then medevac out. And when an<br />
In the Line <strong>of</strong> Fire:<br />
Robert Lee Henderson, Vietnam War Veteran<br />
Robert Lee Henderson, M.D. (’62), went to Vietnam a few years<br />
before Spencer. After failing to get the field surgery slot he wanted<br />
because too many other <strong>doctors</strong> had already applied, Henderson volunteered<br />
for the Special Forces. He went to jump school <strong>at</strong> Fort<br />
Benning, Georgia, studied special warfare <strong>at</strong> Fort Bragg, North<br />
Carolina, and was assigned to a unit outside Saigon whose job was<br />
transporting medical supplies to hospitals in the hinterland.<br />
“Besides furnishing supplies and protecting soldiers from tropical<br />
diseases,” he says, “we did medical visits to local villages, trying to get<br />
people more on our side by taking care <strong>of</strong> their health problems.”<br />
But some days, the stakes were much higher. Henderson remembers flying<br />
in to tre<strong>at</strong> soldiers <strong>at</strong> an American camp th<strong>at</strong> had been completely overrun<br />
by Vietcong forces, and its two medics killed. “It was nighttime, and<br />
there were .50-caliber tracer rounds coming up alongside the helicopter,”<br />
8
he says. “I thought, ‘Well, I could die right here.’ But<br />
strangely enough, th<strong>at</strong> realiz<strong>at</strong>ion was like a huge weight<br />
being lifted <strong>of</strong>f <strong>of</strong> me. I just said, ‘Okay, let’s go.’ ”<br />
One <strong>of</strong> the clippings in Henderson’s scrapbook is a<br />
United Press Intern<strong>at</strong>ional news story written by a<br />
journalist who was on the last helicopter into the devast<strong>at</strong>ed<br />
camp. “The reporter saw my M1 carbine and<br />
my .45 sidearm and he said, ‘Aren’t you a doctor? Wh<strong>at</strong><br />
kind <strong>of</strong> medicine do you practice with those?’ And<br />
without thinking, I told him, ‘Preventive medicine.’<br />
“The news story didn’t mention my name, but my<br />
mother read the article in the paper and she told me<br />
l<strong>at</strong>er, ‘Th<strong>at</strong> sounded just like something you’d say.’ ”<br />
Like Spencer, Henderson says his time in Vietnam<br />
changed his life. “It’s an experience I wouldn’t have<br />
missed for the world. Before going in the service I was<br />
a hard worker, but I didn’t have a lot <strong>of</strong> confidence or<br />
self-esteem. After three years in Special Forces,<br />
though, I wasn’t afraid <strong>of</strong> anything or anybody. I knew<br />
exactly wh<strong>at</strong> I could do and wh<strong>at</strong> I couldn’t do, and it<br />
stood me in very good stead for my residency.”<br />
Sunrise in Saudi:<br />
Ronald Orso, Oper<strong>at</strong>ion Desert<br />
Storm Veteran<br />
Ronald Orso, M.D. (’72), saw wartime service <strong>at</strong><br />
a much l<strong>at</strong>er stage in his life. Orso was already a 19-<br />
year veteran <strong>of</strong> the N<strong>at</strong>ional Guard when his 109th<br />
Evacu<strong>at</strong>ion Hospital unit was disp<strong>at</strong>ched to the<br />
Desert Storm conflict in early 1991. “It was something<br />
<strong>of</strong> a shock,” he recalls. “In November we were<br />
sent to Fort Benning for training, and we got to<br />
come home for Christmas before being deployed.”<br />
While American troops moved toward Kuwait,<br />
Orso’s group set up their 450-person hospital on the<br />
border between Iraq and Saudi Arabia. As it happened,<br />
the majority <strong>of</strong> their p<strong>at</strong>ients were Iraqi soldiers.<br />
“It was a really pitiful situ<strong>at</strong>ion,” Orso recalls. “Those<br />
guys had been in the middle <strong>of</strong> the desert for months or<br />
years. They were undernourished, they had virtually no<br />
medical facilities, and their hearts were not in wh<strong>at</strong> they<br />
were doing. When they saw we were going to take care<br />
<strong>of</strong> them, not kill them, they were so appreci<strong>at</strong>ive.<br />
“It’s hard to h<strong>at</strong>e somebody who’s wounded.<br />
You n<strong>at</strong>urally feel sorry for them. People would<br />
ask me, ‘How does it feel to take care <strong>of</strong> Iraqis?’<br />
and I would answer, ‘I don’t, I take care <strong>of</strong> human<br />
beings.’ I think it’s a real tribute to our pr<strong>of</strong>ession<br />
th<strong>at</strong> we’re in a war zone with people trying to kill<br />
us and still we’re trying to save their lives. I<br />
believe th<strong>at</strong>’s one thing th<strong>at</strong> sets our culture apart<br />
from some others.”<br />
The few American casualties th<strong>at</strong> Orso did see are<br />
still vivid in his mind.“The only female pilot to die<br />
in th<strong>at</strong> war died in our hospital,” he says. “It was a<br />
very sad time.”<br />
Other memories th<strong>at</strong> linger are an Easter sunrise<br />
service in Saudi Arabia, with a white sheet draped on<br />
a makeshift cross, and the faces <strong>of</strong> wounded Iraqi prisoners<br />
as they were being returned to Baghdad. “They<br />
were afraid th<strong>at</strong> Saddam would kill them if he found<br />
out th<strong>at</strong> the Americans had saved their lives. I’m not<br />
sure wh<strong>at</strong> happened to them. I’ll never know.”<br />
The biggest differences between the Vietnam and<br />
Desert Storm experiences, according to Orso, were<br />
the levels <strong>of</strong> prepar<strong>at</strong>ion and the r<strong>at</strong>e <strong>of</strong> casualties.<br />
“Doctors in Vietnam were overwhelmed with the<br />
massive numbers and the terrible trauma,” he says.<br />
“By contrast, we weren’t short <strong>of</strong> anything. We were<br />
actually overstaffed, which was gre<strong>at</strong>.<br />
“I’m practicing today with two surgeons who were<br />
(Top) Charles Kent Powers Jr. <strong>at</strong> the 800th<br />
M.P. B<strong>at</strong>talion headquarters, Camp Bucca.<br />
(Bottom) “Like many <strong>of</strong> the soldiers, I lost 30<br />
pounds” in the Iraqi sun, Powers says.<br />
in Vietnam, and they’re excellent. Th<strong>at</strong>’s because all<br />
they did, every day, was oper<strong>at</strong>e. Whereas in Saudi<br />
Arabia I would do maybe three or four surgeries a<br />
week. I’m really concerned about the soldiers who<br />
are in Iraq now, because they seem to be having a<br />
much harder time than we did.”<br />
A Hospital in Hell:<br />
Charles Kent Powers Jr.,<br />
Oper<strong>at</strong>ion Iraqi Freedom Veteran<br />
Charles Kent Powers Jr., M.D. (’88), knows about<br />
th<strong>at</strong> firsthand. He recently spent six months serving<br />
in a field hospital for a military police unit th<strong>at</strong> oper<strong>at</strong>es<br />
the main prisoner-<strong>of</strong>-war camp in Iraq, Camp<br />
Bucca in Umm Qasar.<br />
9<br />
“It’s a very austere environment,” Powers says.<br />
“Basically, the Army found a plot <strong>of</strong> desert and<br />
fenced it <strong>of</strong>f. For the troops there are tents with dirt<br />
floors, no air conditioning. The prisoners have a<br />
variety <strong>of</strong> illnesses and injuries th<strong>at</strong> war-time life in<br />
the desert involves—knife and gunshot wounds,<br />
snakebite, scorpion bites, he<strong>at</strong> exhaustion. When I<br />
left <strong>at</strong> the end <strong>of</strong> May, it was 123 degrees during the<br />
day and 100 degrees <strong>at</strong> night.”<br />
Staying focused and encouraged under such grim<br />
conditions was a priority: “Every day you get up and<br />
try to do your best, try to have a positive <strong>at</strong>titude and<br />
set a good example as an <strong>of</strong>ficer,” he says. “You’re serving<br />
with young ‘kids,’ men and women in their early<br />
20s, and you try to keep them cheered up, and encourage<br />
them to complete their mission and continue tre<strong>at</strong>ing<br />
the prisoners with human dignity. I think the<br />
Army was proud <strong>of</strong> the job we did there.”<br />
Powers had a little outside help. “I cannot relay<br />
how much I appreci<strong>at</strong>e the thoughts and prayers <strong>of</strong><br />
those St<strong>at</strong>eside,” he says. “Cards and goodie boxes<br />
lifted our spirits, and God used it as a time to build<br />
me spiritually and physically.”<br />
The first day <strong>at</strong> the camp is still a fresh memory.<br />
“When we got there, the smell told us immedi<strong>at</strong>ely<br />
where we were,” he recalls. “They had been oper<strong>at</strong>ing<br />
about 10 days with no l<strong>at</strong>rines. You could hear a lot <strong>of</strong><br />
yelling and chanting—minor riots broke out on a frequent<br />
basis. There were escape <strong>at</strong>tempts, with flares<br />
going <strong>of</strong>f <strong>at</strong> night and dogs looking for the escapees. I<br />
really missed my wife and seven children.<br />
“One thing I particularly remember is a speed-limit<br />
sign <strong>at</strong> the edge <strong>of</strong> the camp, and on the back <strong>of</strong> it<br />
somebody had written ‘Hell.’ And though the Army is<br />
not generally big on individualism, the sign was not<br />
taken down. The place was like Hell, in a way. It was<br />
hot and miserable and you didn’t know who to trust.”<br />
A Terrible Intensity:<br />
Pictures Th<strong>at</strong> Never Fade<br />
Terrell Spencer says th<strong>at</strong>, regardless <strong>of</strong> the conflict<br />
in which they served, one common thread for all<br />
physicians is the indelible impression war leaves on<br />
the memory:<br />
“Under b<strong>at</strong>tlefield conditions, your senses seem to<br />
be hyper-acute. Everything looks brighter, smells<br />
stronger, is more intense. Your timeline for events<br />
starts to be a single day, because you know you might<br />
be dead by nighttime. You don’t necessarily try to<br />
remember things, but you can’t help it. The impressions<br />
are so strong.<br />
“I’ve found th<strong>at</strong> when I have a p<strong>at</strong>ient who’s in his<br />
80s, and his mind might be wandering, one way to<br />
connect with him is to ask, ‘Wh<strong>at</strong>’s your unit, sir?’ A<br />
man who’s been in the service can tell you his unit and<br />
his serial number, almost every time. Those memories<br />
<strong>of</strong> the military seem to last until the very end.”
Fe<strong>at</strong>ure Stories<br />
BIGChanges<br />
A Day in the Life <strong>of</strong> a Resident Under New Duty-Hours Restrictions<br />
By Anita Smith<br />
It’s a Sunday on the Trauma Service <strong>at</strong> UAB’s<br />
<strong>University</strong> Hospital. Fourth-year surgery resident<br />
Phillip Lackey, M.D., is a chief resident on the<br />
service; he’s on call today, and he’s busy. Arriving<br />
<strong>at</strong> the hospital before 5:30 a.m., Lackey has a junior<br />
resident in tow as he makes rounds <strong>at</strong> trauma<br />
p<strong>at</strong>ients’ bedsides in intensive care and on floor<br />
units. He makes notes and puts in orders for wh<strong>at</strong><br />
needs to be done for these p<strong>at</strong>ients.<br />
ROUNDS IN A RUSH<br />
Shortly before 8 a.m., Lackey walks to a conference<br />
room in an adjoining building, where<br />
Trauma Service Morning Report is about to<br />
begin. This morning, 13 people are particip<strong>at</strong>ing.<br />
Using Morning Report time to review the st<strong>at</strong>us<br />
timetables for various procedures. And they run a<br />
tally <strong>of</strong> available beds.<br />
After Morning Report, Lackey joins an <strong>at</strong>tending<br />
surgeon and a junior resident for more p<strong>at</strong>ient<br />
rounds. Summoned frequently by his pager,<br />
Lackey answers some p<strong>at</strong>ient-care questions by<br />
phone and temporarily interrupts rounds to handle<br />
other needs in person. He receives word th<strong>at</strong><br />
a truck collision victim is being brought in, and<br />
he and an <strong>at</strong>tending surgeon report to the emergency<br />
room to lead the assessment, make sure the<br />
p<strong>at</strong>ient is stabilized, and put in orders for diagnostic<br />
scans <strong>of</strong> his injuries. A few minutes l<strong>at</strong>er,<br />
Lackey interrupts his rounds again to go to the<br />
CT-scan area to reassure the accident victim, who<br />
is having trouble lying still for the scan.<br />
departure time th<strong>at</strong> precisely. “Back then, we went<br />
<strong>of</strong>f-duty whenever our work was done,” he says.<br />
The difference between then and now is the<br />
“80-hour rule,” a hot topic <strong>of</strong> discussion in residency<br />
programs <strong>at</strong> the UASOM and across the<br />
United St<strong>at</strong>es. In effect since July 1, 2003, the<br />
rule specifies th<strong>at</strong> all residents must be limited to<br />
80 hours on duty within a seven-day workweek.<br />
This includes in-house call and encompasses all<br />
overnight-duty hours spent in the hospital,<br />
regardless <strong>of</strong> whether a resident spends some <strong>of</strong><br />
those hours resting. The 80-hour rule covers all<br />
119 specialties and subspecialties in 7,800 residency<br />
programs in the United St<strong>at</strong>es th<strong>at</strong> are<br />
accredited by the Accredit<strong>at</strong>ion Council for<br />
Gradu<strong>at</strong>e Medical Educ<strong>at</strong>ion (ACGME).<br />
<strong>of</strong> every trauma p<strong>at</strong>ient in the hospital, residents<br />
and <strong>at</strong>tending physicians go over wh<strong>at</strong> has been<br />
done for p<strong>at</strong>ients thus far, their progress, and<br />
wh<strong>at</strong> will be done next. They review p<strong>at</strong>ients who<br />
are victims <strong>of</strong> everything from car accidents to<br />
gunshot wounds. They discuss special issues—<br />
such as p<strong>at</strong>ients who have been intub<strong>at</strong>ed and<br />
those dealing with complic<strong>at</strong>ions such as pneumonia<br />
and kidney dysfunction. They identify<br />
Yet in all the uncertainty <strong>of</strong> this busy day,<br />
Lackey is aware <strong>of</strong> something about his own schedule<br />
th<strong>at</strong> he would not have known several months<br />
previously. “I know it’s very likely I’ll be going <strong>of</strong>f<br />
“Our restricted duty hours make it even more important th<strong>at</strong> we as<br />
residents become better <strong>at</strong> communic<strong>at</strong>ing with one another about<br />
such issues as tests and other care we’re ordering for our p<strong>at</strong>ients.…<br />
We need to learn how to have better communic<strong>at</strong>ion.”<br />
— Anne B. Davis<br />
duty and leaving the hospital this evening between<br />
5 and 6 o’clock,” he says. At th<strong>at</strong> point, he will be<br />
expected to hand <strong>of</strong>f in-progress p<strong>at</strong>ient-care work<br />
to other residents. Prior to mid-summer 2003,<br />
Lackey could not have pinpointed his expected<br />
JUDGING THE IMPACT<br />
One <strong>of</strong> those dealing with the effects <strong>of</strong> the<br />
hours change is Dennis W. Boulware, M.D., the<br />
UASOM’s senior associ<strong>at</strong>e dean for educ<strong>at</strong>ion.<br />
“This new rule has somewh<strong>at</strong> polarized the medical<br />
community n<strong>at</strong>ionally,” says Boulware.<br />
“Some gre<strong>at</strong>ly welcomed it. Others think it is<br />
horrible and th<strong>at</strong> it will contribute to the destruction<br />
<strong>of</strong> the tradition <strong>of</strong> medicine. My opinion is<br />
somewh<strong>at</strong> mixed.”<br />
Boulware says years must pass before the full<br />
impact <strong>of</strong> the 80-hour rule will become clear.<br />
However, he has come to some conclusions after<br />
a few months <strong>of</strong> experience with the rule and its<br />
consequences.<br />
Boulware says the rule came into being because<br />
the ACGME was feeling pressure from consumer<br />
groups and Congress, fueled by worries th<strong>at</strong> overtired<br />
residents were contributing to errors in<br />
p<strong>at</strong>ient care.<br />
10
Fe<strong>at</strong>ure Stories<br />
Regarding his own concerns about the potential<br />
neg<strong>at</strong>ive impact <strong>of</strong> the rule, Boulware notes<br />
th<strong>at</strong> by reducing residents’ on-duty hours,<br />
ACGME has cre<strong>at</strong>ed the need for additional<br />
“p<strong>at</strong>ient-care hand<strong>of</strong>fs”—residents having to<br />
hand <strong>of</strong>f p<strong>at</strong>ient-care responsibilities to others.<br />
Boulware fears additional hand<strong>of</strong>fs could contribute<br />
to lack <strong>of</strong> continuity in p<strong>at</strong>ient care and<br />
could result in more confusion in the health-care<br />
system. He says this is ironic, since the ACGME<br />
was trying to use this new rule to contribute to a<br />
smoother system.<br />
“I am concerned, too, about wh<strong>at</strong> this might<br />
mean down the road regarding public trust in a<br />
health-care system already under fire by the public,”<br />
says Boulware.<br />
Regardless <strong>of</strong> one’s opinion about the 80-hour<br />
rule, Boulware says, it’s here to stay—<strong>at</strong> least for<br />
the foreseeable future. “The ACGME planned for<br />
this a long time and it has a reput<strong>at</strong>ion for sticking<br />
to its rules.”<br />
Another prediction th<strong>at</strong> the ACGME will hold<br />
fast comes from Marshall M. Urist, M.D., vice chair<br />
<strong>of</strong> the Department <strong>of</strong> Surgery and co-director <strong>of</strong> the<br />
General Surgery Residency Program. “At least where<br />
surgery is concerned, I think arguments to the<br />
ACGME appealing for exceptions are not going to<br />
go very far,” he says. “Although we do know th<strong>at</strong> it<br />
will be possible to increase residents’ on-duty hours<br />
from 80 to 88 in special cases, we also know such an<br />
increase can be made for educ<strong>at</strong>ional purposes only,<br />
not to accommod<strong>at</strong>e service needs.”<br />
other care we’re ordering for our p<strong>at</strong>ients. This is<br />
good in th<strong>at</strong> we need to learn how to have better<br />
communic<strong>at</strong>ion. Some <strong>of</strong> us tend to be solitary<br />
thinkers, and while solitary thinking can have<br />
good points, it’s also important to learn to be<br />
gre<strong>at</strong> team players. After all, most <strong>of</strong> us will have<br />
partners with whom we will be communic<strong>at</strong>ing<br />
after we go into practice.”<br />
Another positive, says Davis, is the injection <strong>of</strong><br />
some balance into <strong>doctors</strong>’ lives. “Physicians need<br />
to be well-rounded. They don’t need to be trained<br />
as individuals who work all the time. These morerestrictive<br />
duty hours address th<strong>at</strong>.”<br />
Surgery resident Lackey says there is no doubt<br />
th<strong>at</strong> his own family life has benefited from the<br />
new rules. He has more time with his wife and<br />
He is uneasy about the consequences on the<br />
structure <strong>of</strong> residents’ educ<strong>at</strong>ional experiences. At<br />
least until residents become accustomed to the<br />
new rule, Boulware says, senior residents <strong>of</strong>ten<br />
will spend time supplementing wh<strong>at</strong> junior residents<br />
can do for p<strong>at</strong>ients within limited duty<br />
hours. In addition, he notes, the new rule poses<br />
challenges in scheduling certain educ<strong>at</strong>ional experiences<br />
for residents.<br />
Boulware is worried, too, about the long-term<br />
impact the duty-hours changes could have on medical-school<br />
faculty: “Faculty are being impacted in<br />
two ways. Because <strong>of</strong> fewer resident duty hours,<br />
some faculty who once had residents with them<br />
now do not. Also, fewer resident duty hours result<br />
in additional p<strong>at</strong>ient-care responsibilities being<br />
shifted to the faculty. I fear th<strong>at</strong> these impacts could<br />
drive some faculty out <strong>of</strong> medical educ<strong>at</strong>ion into<br />
priv<strong>at</strong>e practice, particularly if they already had<br />
been considering priv<strong>at</strong>e practice as an option.”<br />
Based on his own observ<strong>at</strong>ions, Urist questions<br />
the validity <strong>of</strong> linking sleep-deprived residents to<br />
errors in p<strong>at</strong>ient care. “I have not observed a big<br />
problem with residents making bad decisions<br />
because they were sleep-deprived,” he says.<br />
Urist adds th<strong>at</strong> he had been concerned about<br />
whether the new rule would permit surgery residents<br />
to take part in the diverse surgery experiences<br />
they need, but he says so far th<strong>at</strong> has<br />
worked out well. On the positive side, he says the<br />
80-hour rule will free residents to explore outsidethe-hospital<br />
learning experiences such as independent<br />
reading.<br />
MORE TIME, MORE QUESTIONS<br />
Residents themselves see some positives about<br />
the rule. Anne B. Davis, M.D., a third-year resident<br />
in internal medicine, says, “Our restricted<br />
duty hours make it even more important th<strong>at</strong> we<br />
as residents become better <strong>at</strong> communic<strong>at</strong>ing<br />
with one another about such issues as tests and<br />
11<br />
In order to hand <strong>of</strong>f p<strong>at</strong>ients <strong>at</strong> the end <strong>of</strong><br />
shortened duty hours, residents such as Phillip<br />
Lackey must put an even gre<strong>at</strong>er<br />
emphasis on coordin<strong>at</strong>ion and communic<strong>at</strong>ion.<br />
two children, and he even can make plans for predictable<br />
weekend time <strong>of</strong>f. At the same time, he<br />
worries about the impact th<strong>at</strong> restricted duty<br />
hours might have on continuity <strong>of</strong> p<strong>at</strong>ient care<br />
and on the quality <strong>of</strong> training th<strong>at</strong> residents<br />
receive. He wonders, “Will residents receive less<br />
training because the training is less rigorous? Will<br />
they have the skills they need to have?”<br />
Lackey also ponders possible future implic<strong>at</strong>ions<br />
for residency programs—implic<strong>at</strong>ions th<strong>at</strong><br />
are topics <strong>of</strong> deb<strong>at</strong>e throughout the medical pr<strong>of</strong>ession.<br />
Will the 80-hour rule set the stage for<br />
major changes in the way residents are trained?<br />
Will it in fact help set the stage for residencytraining<br />
periods th<strong>at</strong> will become even longer<br />
than they are today?<br />
As Boulware says, “Only time will tell.”
Making Connections<br />
Koehler Named Chair <strong>of</strong> Radiology Department<br />
By Charles A. Goldthwaite Jr.<br />
Robert Koehler, M.D., may be just beginning<br />
his tenure as chair <strong>of</strong> the Department <strong>of</strong><br />
Radiology, but he’s anything but a novice.<br />
Koehler brings more than 20 years <strong>of</strong> experience<br />
in the department to his current post, having<br />
joined the department in July 1982 as vice chair<br />
and director <strong>of</strong> the program in gastrointestinal<br />
radiology. He held those positions until 2002,<br />
and was named the new department chair last<br />
November after serving as interim chair during a<br />
year-long candid<strong>at</strong>e search.<br />
A Fellow <strong>of</strong> the American College <strong>of</strong> Radiology<br />
and the 2002 recipient <strong>of</strong> the American Board <strong>of</strong><br />
Radiology’s Distinguished Service Award,<br />
Koehler is a n<strong>at</strong>ionally recognized clinician,<br />
scholar, and teacher. At the UASOM, Koehler<br />
received the Department <strong>of</strong> Radiology’s Teacher<br />
<strong>of</strong> the Year Award in 1989 and its Distinguished<br />
Faculty Award in 2003. “Of all the gre<strong>at</strong> things<br />
about my pr<strong>of</strong>ession, I enjoy the interpersonal<br />
elements the most,” Koehler says. “Before I<br />
became chair, I was primarily a doctor and a<br />
teacher, either communic<strong>at</strong>ing with p<strong>at</strong>ients or<br />
training residents. As chair, I’ve become much<br />
more involved in faculty development and getting<br />
people to work effectively together.”<br />
Surprisingly, radiology was not the first area<br />
<strong>of</strong> specialty for Koehler. After receiving his medical<br />
degree from Cornell <strong>University</strong> Medical<br />
College he completed an internship and residency<br />
in internal medicine <strong>at</strong> Washington<br />
<strong>University</strong> School <strong>of</strong> Medicine in St. Louis.<br />
During th<strong>at</strong> time, he developed an affinity for<br />
diagnosis and technology, which was encouraged<br />
by colleagues in radiology. “My mentors <strong>at</strong><br />
Washington <strong>University</strong> felt such an utter enthusiasm<br />
for their work th<strong>at</strong> it was infectious,”<br />
Koehler recalls. “I developed a deeper interest in<br />
radiology and came to see th<strong>at</strong> it was the field<br />
th<strong>at</strong> I wanted to specialize in.”<br />
After serving a two-year stint as an epidemiologist<br />
with the United St<strong>at</strong>es Public Health<br />
Service, Koehler completed a diagnostic radiology<br />
residency and fellowship in gastrointestinal<br />
radiology <strong>at</strong> the <strong>University</strong> <strong>of</strong> California San<br />
“Before I became chair, I was<br />
primarily a doctor and a<br />
teacher, either communic<strong>at</strong>ing<br />
with p<strong>at</strong>ients or training<br />
residents. As chair, I’ve<br />
become much more involved<br />
in faculty development and<br />
getting people to work<br />
effectively together.”<br />
Francisco (UCSF). He spent one year as a clinical<br />
instructor <strong>of</strong> radiology <strong>at</strong> UCSF before<br />
returning to the Washington <strong>University</strong> School<br />
<strong>of</strong> Medicine as an assistant—and l<strong>at</strong>er, an associ<strong>at</strong>e—pr<strong>of</strong>essor<br />
<strong>of</strong> radiology. From there, he<br />
moved to <strong>Birmingham</strong>, serving as the vice chair<br />
Four SPORE<br />
UAB Tops in Cancer Research<br />
By Russ Willcutt<br />
— Robert Koehler<br />
When Selwyn Vickers, M.D., learned th<strong>at</strong> he<br />
had landed a SPORE (Specialized Programs <strong>of</strong><br />
Research Excellence) grant for pancre<strong>at</strong>ic-cancer<br />
research, he was pleased—out <strong>of</strong> 15 applicants,<br />
only UAB, the Mayo Clinic, and M.D.<br />
Anderson had been funded, so there was good<br />
<strong>of</strong> radiology under the leadership <strong>of</strong> Robert<br />
Stanley, M.D.<br />
“When I look back, it is remarkable how much<br />
positive change has occurred since I came to the<br />
university,” Koehler notes. One <strong>of</strong> 11 faculty hires<br />
in the 1982–1983 year, Koehler worked firsthand<br />
with Stanley as the department expanded rapidly<br />
in scope. “The whole fabric <strong>of</strong> radiological care <strong>at</strong><br />
UAB changed markedly in the 1980s, and we<br />
have continued to recruit outstanding people,<br />
increase our level <strong>of</strong> N<strong>at</strong>ional Institutes <strong>of</strong> Health<br />
funding, and expand our residency training.”<br />
As he looks forward to radiology in the 21st<br />
century, Koehler recognizes th<strong>at</strong> there are many<br />
challenges ahead. “Radiologists must constantly<br />
stay in motion, because the dimensions <strong>of</strong> the<br />
field are always changing,” he notes. Many <strong>of</strong><br />
the tools th<strong>at</strong> are standard today did not exist<br />
when Koehler was a resident, a situ<strong>at</strong>ion th<strong>at</strong><br />
will be true for today’s gradu<strong>at</strong>es as well. “When<br />
I was training, the most common indic<strong>at</strong>ion for<br />
abdominal surgery was explor<strong>at</strong>ory laparotomy,<br />
literally cutting open the belly to determine the<br />
problem,” Koehler recalls. “Now, radiology provides<br />
a way to determine the answers, which has<br />
led to less-invasive tre<strong>at</strong>ments and increased<br />
effectiveness when surgery is required.”<br />
Upon embarking on his journey as department<br />
chair, Koehler envisions the Department <strong>of</strong><br />
Radiology as one part <strong>of</strong> an even more integr<strong>at</strong>ed<br />
future. “During the last 20 years <strong>at</strong> the UAB medical<br />
center, I have been impressed daily <strong>at</strong> the gre<strong>at</strong><br />
mutual support and collegiality here,” he says. “We<br />
are blessed with talented faculty and staff who pull<br />
together to improve all aspects <strong>of</strong> care, and it is gre<strong>at</strong><br />
to be part <strong>of</strong> such a community.”<br />
reason to celebr<strong>at</strong>e. Still, the news was bittersweet,<br />
because the $4.5 million awarded was far<br />
less than the $10 to $12 million th<strong>at</strong> had been<br />
requested—a shortfall experienced by all three<br />
institutions due to budgetary constraints <strong>at</strong> the<br />
N<strong>at</strong>ional Institutes <strong>of</strong> Health.<br />
“We’re definitely better <strong>of</strong>f than we were,” says<br />
Vickers, “but pancre<strong>at</strong>ic cancer is a disease th<strong>at</strong><br />
needs as much help as any, and maybe even<br />
more.” Th<strong>at</strong>’s because pancre<strong>at</strong>ic cancer hasn’t<br />
gener<strong>at</strong>ed the same level <strong>of</strong> <strong>at</strong>tention as have others,<br />
such as prost<strong>at</strong>e and breast cancer, resulting in<br />
12
The Big Move<br />
Sprinting Toward Completion<br />
By Emily Delzell, courtesy <strong>of</strong> UAB Synopsis, and Dawn Mesa<br />
“Our first and most<br />
important goal is to cre<strong>at</strong>e<br />
as seamless a transition as<br />
possible in order to continue<br />
providing the same quality<br />
<strong>of</strong> care and services our<br />
p<strong>at</strong>ients now enjoy.”<br />
— Jane Chandler<br />
To ensure a flawless move to the new <strong>University</strong> Hospital, units are carrying out test runs with mock p<strong>at</strong>ients.<br />
As most everyone can <strong>at</strong>test, a lot <strong>of</strong> work goes<br />
into moving a home or <strong>of</strong>fice, even if it’s just a<br />
move across the street. Now imagine moving an<br />
entire hospital across the street—one with many<br />
departments and p<strong>at</strong>ients, and lots <strong>of</strong> equipment,<br />
as well as a bustling emergency room.<br />
Th<strong>at</strong>’s the challenge being faced by UAB’s North<br />
Pavilion Project Oper<strong>at</strong>ions Office, led by coordin<strong>at</strong>or<br />
Jane Chandler, RN, Ph.D. “Our first and most<br />
important goal is to cre<strong>at</strong>e as seamless a transition as<br />
possible in order to continue providing the same<br />
quality <strong>of</strong> care and services our p<strong>at</strong>ients now enjoy,”<br />
notes Chandler, who has organized and implemented<br />
the oper<strong>at</strong>ions planning initi<strong>at</strong>ive and who, along<br />
with many others, is coordin<strong>at</strong>ing the reloc<strong>at</strong>ion<br />
effort. “We also are focused on maintaining continuity<br />
<strong>of</strong> oper<strong>at</strong>ions and minimizing downtime.”<br />
The 885,000-square-foot <strong>University</strong> Hospital<br />
will have 37 oper<strong>at</strong>ing suites, two procedure<br />
rooms, three medical/surgical units, four intensive-care<br />
units—trauma and burn, surgery, neuroscience,<br />
and cardiovascular—and the <strong>University</strong><br />
Emergency Department (UED) spread among<br />
nine p<strong>at</strong>ient-care floors. At 38,000 square feet,<br />
with up to 45 priv<strong>at</strong>e tre<strong>at</strong>ment rooms, the UED<br />
is nearly three times larger than the old space.<br />
The department is loc<strong>at</strong>ed on the first floor,<br />
along with a large public lobby. The second floor<br />
will serve as the main concourse into the <strong>University</strong><br />
Hospital complex from the new visitor parking<br />
deck, with the primary entrance loc<strong>at</strong>ed on Fourth<br />
Avenue South. The new <strong>University</strong> Hospital has 10<br />
elev<strong>at</strong>ors, and visitor elev<strong>at</strong>ors are oriented <strong>at</strong> each<br />
level to either the three-story lobby or the open<br />
light well, which will help with orient<strong>at</strong>ion. A total<br />
<strong>of</strong> six bridges connect the new <strong>University</strong> Hospital<br />
with the Wallace Tumor Institute, Spain Wallace,<br />
the West Pavilion, and other p<strong>at</strong>ient-care areas.<br />
Designed to be p<strong>at</strong>ient- and family-friendly, the<br />
new facility has se<strong>at</strong>ing for more than 900 visitors,<br />
including large, open public accommod<strong>at</strong>ions<br />
centered around the <strong>at</strong>rium and skylight. A healing<br />
garden—a stress-relieving place for p<strong>at</strong>ients<br />
and their families to sit quietly among plants and<br />
seasonal displays <strong>of</strong> colorful flowers—will be<br />
loc<strong>at</strong>ed around the fifth-floor skylight, where it<br />
can be viewed from the floors above.<br />
The Oper<strong>at</strong>ions Planning Committee will be<br />
working with all affected units and services to<br />
finalize the reloc<strong>at</strong>ion plans in the coming<br />
months. The move is currently scheduled to take<br />
place in five stages, with some support services<br />
occupying the building as <strong>of</strong> July. Currently, the<br />
Committee estim<strong>at</strong>es th<strong>at</strong> most clinical areas will<br />
reloc<strong>at</strong>e during the second half <strong>of</strong> August, with all<br />
moves being completed by early fall.<br />
fewer available research dollars. “Nearly everyone<br />
knows somebody who’s had prost<strong>at</strong>e cancer, for<br />
example, and they also know people who’ve survived<br />
it, and those survivors are powerful advoc<strong>at</strong>es,” says<br />
Vickers. “In 2000, something like $190 million was<br />
awarded to fund prost<strong>at</strong>e-cancer research, and about<br />
$380 million for breast cancer—but only $15 million<br />
for pancre<strong>at</strong>ic-cancer research.”<br />
Morbidity r<strong>at</strong>es are especially discouraging: Of<br />
29,700 cases <strong>of</strong> pancre<strong>at</strong>ic cancer reported in a recent<br />
year, there were 29,300 de<strong>at</strong>hs, according to Vickers.<br />
“Th<strong>at</strong> makes it the fourth most deadly cancer, but 10th<br />
Selwyn Vickers leads UAB’s pancre<strong>at</strong>iccancer<br />
research efforts.<br />
in terms <strong>of</strong> incidents reported,” he says.<br />
Th<strong>at</strong>’s why funding to develop screening tests (none<br />
currently exist) and effective tre<strong>at</strong>ments for pancre<strong>at</strong>ic<br />
cancer is so important, and Vickers believes th<strong>at</strong> UAB<br />
is just the place to make a start. “The Cancer Center<br />
has a very good reput<strong>at</strong>ion, and UAB has a history <strong>of</strong><br />
collabor<strong>at</strong>ive effort, so I think th<strong>at</strong> in addition to our<br />
three existing SPORE grants for brain tumor and<br />
breast and ovarian cancer research, those were the<br />
deciding factors in the decision to award us these<br />
funds, and we’ll certainly make the most <strong>of</strong> them …<br />
and hope for more in the future.”<br />
13
READY FOR THE FUTURE Biodefense Prepar<strong>at</strong>ions<br />
By Russ Willcutt<br />
In November 2003, the N<strong>at</strong>ional Institute <strong>of</strong> Allergy<br />
and Infectious Diseases (NIAID) announced plans to<br />
build two n<strong>at</strong>ional and nine regional level-three biocontainment<br />
labor<strong>at</strong>ories and issued a call for proposals. Of<br />
the more than 30 responses th<strong>at</strong> NIAID received, UAB<br />
was among those funded, receiving a $15.9 million grant.<br />
“The grant was structured so th<strong>at</strong> it required a<br />
one-to-three m<strong>at</strong>ch, however, so the university needed<br />
to secure about $5 million in m<strong>at</strong>ching funds,”<br />
says Richard Marchase, Ph.D., senior associ<strong>at</strong>e dean<br />
for biomedical research <strong>at</strong> UAB and principal investig<strong>at</strong>or<br />
on the grant. “About a month l<strong>at</strong>er, in<br />
response to a request by President Garrison and<br />
Chancellor Portera, Governor Riley pledged the<br />
money from the st<strong>at</strong>e, which will allow us to build<br />
this $21 million facility.”<br />
Sites are being evalu<strong>at</strong>ed on and near campus for<br />
the 40,000-square-foot facility, which will be known<br />
as the Southeast Biosafety Labor<strong>at</strong>ory <strong>Alabama</strong><br />
<strong>Birmingham</strong> (SEBLAB). Marchase says it should be<br />
oper<strong>at</strong>ional by early 2007.<br />
“We expect to continue our anthrax-rel<strong>at</strong>ed<br />
research, as well as research to develop diagnostic<br />
screening methods and vaccines for anthrax, West Nile<br />
virus, and the flu,” says Marchase, adding th<strong>at</strong> investig<strong>at</strong>ors<br />
from throughout the region will have access to<br />
the facility. “In writing the proposal, we made the case<br />
th<strong>at</strong> we have an exceptional group <strong>of</strong> investig<strong>at</strong>ors here<br />
<strong>at</strong> UAB, and th<strong>at</strong> we’re one <strong>of</strong> the strongest universities<br />
in the country in terms <strong>of</strong> our potential to understand<br />
and defend ourselves against these deadly agents.”<br />
Those strengths will be bolstered by a consortium<br />
<strong>of</strong> universities known as the Southeastern Regional<br />
Center <strong>of</strong> Excellence for Emerging Infections and<br />
Biodefense (SERCEB). According to Richard<br />
Whitley, M.D., a founding member <strong>of</strong> the N<strong>at</strong>ional<br />
Institutes <strong>of</strong> Health-funded organiz<strong>at</strong>ion, “This is a<br />
founding group <strong>of</strong> six universities—indeed, all academic<br />
medical centers in our region—th<strong>at</strong> will work<br />
together to develop vaccines, drugs, and diagnostic<br />
West Nile virus under the microscope.<br />
tests against emerging infections such as West Nile<br />
virus, among many others. We will also be conducting<br />
research into organisms such as smallpox th<strong>at</strong><br />
could be used in bioterrorist <strong>at</strong>tacks.” UAB’s partners<br />
in this effort are Duke <strong>University</strong>, Emory <strong>University</strong>,<br />
the <strong>University</strong> <strong>of</strong> Florida, the <strong>University</strong> <strong>of</strong> North<br />
Carolina, and Vanderbilt <strong>University</strong>.<br />
Taking the results from research conducted<br />
through the NIAID Collabor<strong>at</strong>ive Antiviral Study<br />
Group (CASG) contract—which was recently refunded<br />
for $34 million over a seven-year period,<br />
with Whitley as principal investig<strong>at</strong>or—scientists <strong>at</strong><br />
UAB, Southern Research Institute, and other<br />
SERCEB member institutions will work to develop<br />
antiviral drugs to comb<strong>at</strong> emerging infections such<br />
as West Nile virus and, eventually, even severe acute<br />
respir<strong>at</strong>ory syndrome (SARS).<br />
“We’re especially interested in the orthopox family,<br />
which includes smallpox and monkeypox,” says<br />
Whitley. “Just to give you an example <strong>of</strong> wh<strong>at</strong> this<br />
collabor<strong>at</strong>ion is allowing us to do here on campus,<br />
we have Earl Kern and Mark Pritchard doing antiviral<br />
drug screening in the Division <strong>of</strong> Infectious<br />
Diseases <strong>at</strong> Children’s, and Ming Luo and Larry<br />
DeLucas <strong>at</strong> the Center for Biophysical Sciences and<br />
Engineering studying the 3-D structure <strong>of</strong> the<br />
enzymes necessary for these viruses to replic<strong>at</strong>e.<br />
David Chaplin examined inn<strong>at</strong>e host immune<br />
responses to biothre<strong>at</strong> organisms, and Jack Secrist,<br />
Tom Voss, and colleagues <strong>at</strong> Southern Research<br />
Institute are synthesizing drugs based on these structures<br />
th<strong>at</strong> will <strong>at</strong>tack smallpox from a completely<br />
different angle, as well as providing animal models<br />
to study the efficacy <strong>of</strong> these drugs. So it’s this huge,<br />
multidisciplinary effort, with the same shared goal.<br />
“Our hope is th<strong>at</strong> SERCEB and SEBLAB will<br />
help unite scientists from all across campus, and the<br />
region, with each contributing their particular<br />
expertise,” says Whitley. “Because, to me, th<strong>at</strong>’s one<br />
<strong>of</strong> the most important characteristics <strong>of</strong> UAB—we<br />
truly are an institution without walls.”<br />
Searching for a Diabetes Cure<br />
ISLET CELL TRANSPLANTATION<br />
By Laura Freeman<br />
As anyone suffering from the complic<strong>at</strong>ions <strong>of</strong> type I diabetes can <strong>at</strong>test, insulin is<br />
far from a cure. Even if p<strong>at</strong>ients manage to avoid blindness and amput<strong>at</strong>ion <strong>of</strong> extremities—for<br />
which they are <strong>at</strong> high risk—they are still more likely to die prem<strong>at</strong>urely<br />
from heart or kidney disease than nondiabetics.<br />
While transplants have been changing the lives <strong>of</strong> p<strong>at</strong>ients with other organ<br />
failures for years, until recently the sensitivity <strong>of</strong> pancre<strong>at</strong>ic islet cells to immunosuppressive<br />
drugs has limited the effort to bring th<strong>at</strong> hope to diabetics.<br />
However, Devin Eckh<strong>of</strong>f, M.D., and his team are working to change th<strong>at</strong> situ<strong>at</strong>ion.<br />
In April, they performed the first islet-cell transplant in <strong>Alabama</strong>, using a<br />
technique pioneered in Canada th<strong>at</strong> employed a less-toxic combin<strong>at</strong>ion <strong>of</strong><br />
immunosuppressive drugs and reversed diabetes in 85 percent <strong>of</strong> p<strong>at</strong>ients. After<br />
two years, the success r<strong>at</strong>e for the <strong>University</strong> <strong>of</strong> Alberta <strong>at</strong> Edmonton program<br />
continues to be an impressive 75 percent.<br />
14<br />
A LIFE WITHOUT INSULIN<br />
“Our ultim<strong>at</strong>e goal is to help p<strong>at</strong>ients live without insulin or immunosuppressive<br />
drugs,” says Eckh<strong>of</strong>f, division director <strong>of</strong> transplant<strong>at</strong>ion surgery. “The transplant<br />
procedure injects islet cells through a c<strong>at</strong>heter. The cells lodge in the liver<br />
and begin producing insulin.”<br />
The team, which includes Carlton Young, M.D., overseeing clinical aspects, and<br />
Juan Contreras, M.D., heading up the lab, hopes to take wh<strong>at</strong> they learn in duplic<strong>at</strong>ing<br />
the Edmonton study and make modific<strong>at</strong>ions in the second stage <strong>of</strong> their program.<br />
“We’ll be working on finding new approaches to improve the survival <strong>of</strong> islet<br />
cells,” adds Eckh<strong>of</strong>f. “We want to transplant more viable cells and learn how to<br />
help more <strong>of</strong> them survive without damage or rejection.”<br />
Since only about half <strong>of</strong> the new islet cells typically make the transition to<br />
become a functioning transplant, living donors are not an option <strong>at</strong> this point;<br />
they would be unable to contribute sufficient numbers <strong>of</strong> islet cells to free a diabetic<br />
from the need for insulin. However, the p<strong>at</strong>ient and donor have to share only<br />
the same blood type, which improves the odds <strong>of</strong> finding a comp<strong>at</strong>ible donor<br />
organ. Close tissue m<strong>at</strong>ching is not necessary and perhaps not even desirable, since<br />
a too-close m<strong>at</strong>ch could make the new islet cells vulnerable to the same type <strong>of</strong><br />
<strong>at</strong>tack th<strong>at</strong> damaged the p<strong>at</strong>ient’s pancreas.
IN PRAISE OF WINE The Gre<strong>at</strong> Protector By Laura Freeman<br />
“To your health!” Th<strong>at</strong> traditional toast, long raised over glasses <strong>of</strong> wine, is<br />
proving to be prophetic.<br />
Recent major studies have shown a consensus th<strong>at</strong> light to moder<strong>at</strong>e consumption<br />
<strong>of</strong> alcohol (one to four drinks daily for men, one to two for women),<br />
particularly red wine, can help prevent coronary-artery disease and heart <strong>at</strong>tacks.<br />
The big question th<strong>at</strong> remains centers on the mechanisms<br />
behind wine’s prevent<strong>at</strong>ive benefits.<br />
UASOM pr<strong>of</strong>essor Francois Booyse, Ph.D., and his<br />
team <strong>of</strong> 17 researchers are working on a study funded by a<br />
$7.6 million, five-year grant from the N<strong>at</strong>ional Heart,<br />
Lung and Blood Institute to find the answer—or in this<br />
case, the answers.<br />
Multiple components in wine appear to work together to<br />
<strong>at</strong>tack heart disease on several fronts simultaneously. In<br />
addition to helping prevent arteriosclerosis and lowering<br />
blood pressure when consumed in moder<strong>at</strong>ion, elements<br />
within wine seem to help reduce thrombic risks th<strong>at</strong> could<br />
lead to a heart <strong>at</strong>tack.<br />
“Our program specifically focuses on studies rel<strong>at</strong>ed to the<br />
effects <strong>of</strong> low to moder<strong>at</strong>e levels <strong>of</strong> alcohol and polyphenols<br />
on the mechanisms <strong>of</strong> fibrinolysis, a normal ongoing process<br />
th<strong>at</strong> results in the removal <strong>of</strong> small blood clots, and vasoreactivity,”<br />
says Booyse. “Both alcohol and various individual<br />
polyphenols inhibit the activity/production <strong>of</strong> a number <strong>of</strong><br />
specific enzymes as well as fibrinogen, all directly involved in<br />
and responsible for reduced coagul<strong>at</strong>ion or clotting. In addition,<br />
alcohol and polyphenols will simultaneously increase the<br />
production <strong>of</strong> various enzymes involved in clot lysis, further<br />
reducing the overall risk <strong>of</strong> clot form<strong>at</strong>ion and heart <strong>at</strong>tacks.”<br />
Alcohol and polyphenols have also been shown to<br />
increase plasma High-Density Lipoprotein (HDL) cholesterol,<br />
which many investig<strong>at</strong>ors believe helps protect the cardiovascular<br />
system through a process known as reverse cholesterol transport.<br />
“Increased plasma HDL will bind more cholesterol and reduce the level <strong>of</strong> the<br />
Why wine? Ferment<strong>at</strong>ion raises the<br />
number <strong>of</strong> beneficial polyphenols—<br />
giving it an edge over grape juice.<br />
lipoprotein-cholesterol pool in the vessel wall and its deleterious effects in vascular<br />
tissue and cells,” notes Booyse.<br />
Would a glass <strong>of</strong> grape juice with breakfast every morning have the same beneficial<br />
effects? Probably not. Although both juice and wine may begin with<br />
grapes from the same vineyard, chemical changes happen along the way.<br />
“Polyphenol composition, content, and <strong>of</strong>ten structure<br />
are modified and altered during ferment<strong>at</strong>ion,” Booyse<br />
explains. “Grape juice contains lower levels and a different<br />
composition <strong>of</strong> polyphenols.”<br />
The long-term goal <strong>of</strong> studying the heart benefits <strong>of</strong> wine is<br />
to gain insights th<strong>at</strong> can be used in developing better drugs<br />
and therapeutic str<strong>at</strong>egies to help both wine drinkers and nondrinkers<br />
avoid heart disease and live longer, healthier lives.<br />
Working with animal models, mouse-derived blood vessels<br />
and hearts, and cultured endothelial cells and cardiomyocytes,<br />
the UAB team draws on the talents and<br />
expertise <strong>of</strong> researchers from multiple disciplines. In addition<br />
to Booyse, who is a pr<strong>of</strong>essor <strong>of</strong> medicine and director<br />
<strong>of</strong> the Molecular Cardiology Research Program, the principal<br />
investig<strong>at</strong>ors and project leaders include Edlue<br />
Tabengwa, MSC, and Hernan E. Grenett, Ph.D., <strong>of</strong> the<br />
Department <strong>of</strong> Medicine; Dale A. Parks, Ph.D., <strong>of</strong> the<br />
Department <strong>of</strong> Anesthesiology; and Victor Darley-Usmar,<br />
Ph.D., <strong>of</strong> the Department <strong>of</strong> P<strong>at</strong>hology. Twelve other<br />
researchers include faculty and co-investig<strong>at</strong>ors from the<br />
departments <strong>of</strong> Genetics, P<strong>at</strong>hobiology, Pharmacology<br />
and Toxicology, and Physiology and Biophysics.<br />
Unlike fine wines, which may require years <strong>of</strong> aging, the first<br />
fruits <strong>of</strong> this study are already being shared. The team is contributing<br />
its insights and conclusions on a continual basis, typically<br />
publishing 10–12 papers and 15–20 abstracts per year.<br />
When the study’s final results are g<strong>at</strong>hered, learning more<br />
about how wine helps to save hearts may teach us something worth celebr<strong>at</strong>ing<br />
with a sip <strong>of</strong> champagne—or better yet, a hearty burgundy or merlot.<br />
IMPROVING IMMUNOSUPPRESSION<br />
UAB transplant immunologist Judith Thomas,<br />
Ph.D., has been working with prim<strong>at</strong>es with diabetes<br />
to improve their tolerance to immunosuppressive<br />
drugs and to reduce their need for insulin.<br />
“We’re hoping to build on her success,” says<br />
Eckh<strong>of</strong>f. “D<strong>at</strong>a from her research is helping the transplant<br />
program select immunosuppressive drugs th<strong>at</strong><br />
are more effective and less damaging to islet cells.”<br />
There is a possibility UAB’s genetic research could<br />
make a contribution down the line. “Perhaps we’ll eventually<br />
be able to modify islet cells from pigs and make<br />
transplants available to more diabetics so they won’t<br />
Fighting a killer: This April, a team led by Devin<br />
Eckh<strong>of</strong>f (se<strong>at</strong>ed), and colleagues Juan Contreras and<br />
Carlton Young, perfomed the first islet cell transplant<br />
procedure in <strong>Alabama</strong>. Their efforts may one day<br />
give type I diabetics a life without insulin injections.<br />
15<br />
have to depend on insulin injections,” Eckh<strong>of</strong>f adds.<br />
Meanwhile, the team is still evalu<strong>at</strong>ing and selecting<br />
p<strong>at</strong>ients for the first stage <strong>of</strong> the study. They will<br />
continue to perform transplants as <strong>of</strong>ten as donor<br />
islets become available.<br />
“For now, our selection criteria include making sure<br />
a transplant could be a net benefit for any p<strong>at</strong>ients we<br />
choose,” says Eckh<strong>of</strong>f. “R<strong>at</strong>her than selecting those<br />
whose diabetes is well controlled with insulin, we’ll be<br />
looking <strong>at</strong> p<strong>at</strong>ients who are having complic<strong>at</strong>ions from<br />
diabetes or difficulty maintaining blood-sugar levels<br />
due to hypoglycemic unawareness or other factors.<br />
“The potential for helping p<strong>at</strong>ients with type II diabetes<br />
is limited, since their problem is insulin resistance<br />
r<strong>at</strong>her than lack <strong>of</strong> insulin. Transplants, however, could<br />
eventually be part <strong>of</strong> an approach to help those whose<br />
islet cells have been exhausted,” he adds.<br />
For Eckh<strong>of</strong>f and other UAB researchers—and the<br />
one million insulin-dependent diabetics in<br />
America—developing a cure to end diabetes would<br />
be sweet success indeed.
Physicians’ Forum By<br />
Dawn Mesa and Russ Willcutt<br />
I NDIGENT C ARE: A CRISIS IN THE WORKS<br />
With one <strong>of</strong> the lowest per-capita income levels in the United St<strong>at</strong>es, <strong>Alabama</strong> has more than its<br />
fair share <strong>of</strong> indigent residents. They come from many different walks <strong>of</strong> life: homeless, homeowners,<br />
elderly, infants and children, single mothers, families, and both legal and illegal immigrants.<br />
The delivery <strong>of</strong> health care to these largely uninsured popul<strong>at</strong>ions is reaching crisis proportions in<br />
the st<strong>at</strong>e as more and more indigent p<strong>at</strong>ients seek care in our hospitals and clinics. Ultim<strong>at</strong>ely, it is<br />
these institutions th<strong>at</strong> bear the brunt <strong>of</strong> the financial cost for tre<strong>at</strong>ing the indigent—a burden th<strong>at</strong> is<br />
pushing some facilities to the breaking point.<br />
In the second <strong>of</strong> a two-part Physicians’ Forum series, the <strong>Alabama</strong><br />
Medical Alumni Bulletin asked two prominent alumni about their experiences<br />
in tre<strong>at</strong>ing the medically indigent popul<strong>at</strong>ions in two <strong>of</strong> the<br />
largest metropolitan areas in <strong>Alabama</strong>. Wickliffe (Wick) Many, M.D.,<br />
heads up the internal medicine residency program <strong>at</strong> the UASOM in<br />
Montgomery; Iris Fancher, M.D., is a pedi<strong>at</strong>rician who practices <strong>at</strong> the<br />
Bessemer Health Center in metropolitan <strong>Birmingham</strong>.<br />
Wh<strong>at</strong> medical programs are currently in place in your community to assist the indigent popul<strong>at</strong>ion?<br />
Iris Fancher<br />
Iris Fancher (IF): I’m employed with the Jefferson County Department <strong>of</strong> Health, where I am a Public<br />
Health Medical Officer and pedi<strong>at</strong>rician <strong>at</strong> Bessemer Health Center. The health department has a primarycare<br />
program th<strong>at</strong> provides services to all who present, including the indigent and under-insured, as well as<br />
those with insurance. Our fees are based on a sliding scale according to income. It is not unusual for 50 percent<br />
<strong>of</strong> our clientele not to have insurance coverage. Many <strong>of</strong> our p<strong>at</strong>ients are eligible for Medicaid services,<br />
but are unaware <strong>of</strong> their eligibility and never make any <strong>at</strong>tempts to apply for these benefits. There are six health<br />
centers across Jefferson County, staffed by about 16 physicians, pharmacists, and dentists. Each center <strong>of</strong>fers<br />
pedi<strong>at</strong>ric, family planning, m<strong>at</strong>ernity, adult health, pharmacy, and dental services. In addition, we provide<br />
immuniz<strong>at</strong>ion services <strong>at</strong> all our clinics and in Tot Shot Centers <strong>at</strong> specified sites. We also have nutrition consultants<br />
who manage the federal WIC program <strong>at</strong> all our centers.<br />
Wick Many<br />
Wick Many (WM): We have several programs. The first is the county health department, which has some<br />
clinics. There is also a federally funded clinic here—Lister Hill Clinic—and Baptist Health, the parent company<br />
<strong>of</strong> Baptist Medical Center, started an indigent clinic several years ago called Medical Outreach Ministries,<br />
which is staffed mainly by retired physicians. There’s also the UASOM clinic here, staffed entirely by UAB<br />
employees, which takes care <strong>of</strong> both in- and outp<strong>at</strong>ients—we’re really the only facility th<strong>at</strong> takes care <strong>of</strong> both.<br />
We see p<strong>at</strong>ients who present to our hospital, Baptist Medical Center South, with no physician and no insurance,<br />
which is part <strong>of</strong> our mission.<br />
We take care <strong>of</strong> p<strong>at</strong>ients not only from Montgomery County but also from Lowndes, Macon, Bullock, and<br />
other counties traditionally considered part <strong>of</strong> the Black Belt. Our facility also provides space for pedi<strong>at</strong>ric specialty<br />
clinics even though we are an internal-medicine residency program. We have three clinics th<strong>at</strong> deal exclusively<br />
with children. Two are HIV-rel<strong>at</strong>ed; one is an adolescent HIV clinic and the other is a family clinic th<strong>at</strong><br />
provides care for newborns born to HIV-infected mothers. We also have a sickle-cell clinic.<br />
Unfortun<strong>at</strong>ely, we have been too successful. Our adolescent HIV clinic started with only two p<strong>at</strong>ients and<br />
now they’re up to 45. Because <strong>of</strong> the lack <strong>of</strong> resources, lack <strong>of</strong> awareness, and poor public health, HIV in rural<br />
<strong>Alabama</strong> is similar to th<strong>at</strong> seen in underdeveloped n<strong>at</strong>ions. It’s a health-care crisis th<strong>at</strong>’s going to be with us for<br />
quite some time.<br />
Wh<strong>at</strong> has been your experience in tre<strong>at</strong>ing indigent p<strong>at</strong>ients?<br />
IF: I have worked with the health department for about 16 years, and a gre<strong>at</strong> deal has changed since I first<br />
joined. At th<strong>at</strong> time, we would see everyone without regard to his or her ability to pay. Now, because <strong>of</strong><br />
16
Physicians’ Forum<br />
budget cuts, the department is facing a tremendous<br />
challenge.<br />
As a pedi<strong>at</strong>rician, I see p<strong>at</strong>ients from birth to age<br />
19. I will sometimes see some <strong>of</strong> my chronically ill<br />
p<strong>at</strong>ients, such as those with sickle-cell disease or<br />
cerebral palsy, beyond th<strong>at</strong> age. Most <strong>of</strong> these<br />
p<strong>at</strong>ients have Medicaid coverage and they are able<br />
to receive services as needed. We are associ<strong>at</strong>ed with<br />
Children’s Hospital, where we refer our more complex<br />
p<strong>at</strong>ients for specialty care or those requiring<br />
hospitaliz<strong>at</strong>ion.<br />
WM: Working in infectious disease, I see consults<br />
<strong>at</strong> the hospital who may be people who are fully<br />
insured or people who have absolutely no resources<br />
wh<strong>at</strong>soever. As part <strong>of</strong> my responsibilities here with<br />
the UASOM Montgomery, we have a priv<strong>at</strong>e practice<br />
th<strong>at</strong> is part <strong>of</strong> the school, similar to The Kirklin<br />
Clinic in th<strong>at</strong> we do see priv<strong>at</strong>e p<strong>at</strong>ients. Typically,<br />
I see about 30 to 35 consults a month in the hospital,<br />
and anywhere from 10 to 15 <strong>of</strong> those p<strong>at</strong>ients<br />
will be completely indigent. Currently, I’m seeing<br />
three or four in the hospital who have c<strong>at</strong>astrophic<br />
diseases because they didn’t have access to preventive<br />
health care. I have two others in the hospital<br />
right now with newly diagnosed HIV infection.<br />
In wh<strong>at</strong> ways has this impacted you and/or<br />
your practice?<br />
IF: Medicaid coverage changes from day to day, and<br />
many times p<strong>at</strong>ients arrive assuming they have coverage<br />
when they do not. Coverage may be suspended<br />
because the p<strong>at</strong>ients did not reapply for coverage,<br />
because there’s been an address change, or for various<br />
other reasons. Occasionally, a p<strong>at</strong>ient needing<br />
care will leave the clinic because <strong>of</strong> lack <strong>of</strong> coverage.<br />
Sometimes p<strong>at</strong>ients will leave the clinic with a prescription<br />
and not fill it because they have no funds<br />
for medic<strong>at</strong>ion. Whenever we become aware <strong>of</strong><br />
p<strong>at</strong>ients’ inability to pay we implement several cre<strong>at</strong>ive<br />
approaches to provide care. The health centers<br />
and staff also contribute to funds th<strong>at</strong> are administered<br />
through the social workers to help cover medic<strong>at</strong>ion<br />
and some transport<strong>at</strong>ion costs.<br />
WM: It impacts us quite a bit because we have<br />
budget constraints. When you have to write <strong>of</strong>f<br />
large amounts <strong>of</strong> bad debt, the money has to come<br />
from somewhere. We’ve been impacted by the st<strong>at</strong>e<br />
budget cuts and, in a very unusual move, we are<br />
considered a non-st<strong>at</strong>e agency, so our funding was<br />
cut 75 percent.<br />
Unlike <strong>Birmingham</strong>, we do not have a charity<br />
hospital—there’s no Cooper Green here; we are the<br />
area’s Cooper Green. Fortun<strong>at</strong>ely, we do receive<br />
support from the county and from the city. The<br />
amount we’ve received each year has remained the<br />
same, and we’ve been blessed th<strong>at</strong> is hasn’t been cut.<br />
We consider th<strong>at</strong> a success.<br />
Has your p<strong>at</strong>ient base changed in the last five<br />
years, and if so, how?<br />
IF: A few years ago, we began to see an increase in<br />
the number <strong>of</strong> Hispanic p<strong>at</strong>ients presenting to our<br />
clinics. We adjusted by <strong>of</strong>fering Spanish classes to<br />
our staff as well as training in cultural diversity. At<br />
present, most <strong>of</strong> our Hispanic p<strong>at</strong>ient services are<br />
consolid<strong>at</strong>ed <strong>at</strong> two facilities, Central Health<br />
Center and Chris McNair Health Center, where we<br />
have full-time interpreters who assist staff in communic<strong>at</strong>ing<br />
with and providing services to our<br />
Hispanic p<strong>at</strong>ients.<br />
Currently, more p<strong>at</strong>ients are presenting from the<br />
priv<strong>at</strong>e setting for care. Usually there is a loss <strong>of</strong> insurance<br />
coverage or the p<strong>at</strong>ients may be under-insured.<br />
WM: The p<strong>at</strong>ient base has stayed pretty much the<br />
same. Because <strong>of</strong> the fact th<strong>at</strong> there is no hospital in<br />
Lowndes or Macon counties, we continue to serve<br />
both urban and rural communities. P<strong>at</strong>ients come<br />
in from the small rural areas with very little, if any,<br />
preventive health care.<br />
Our main sources <strong>of</strong> p<strong>at</strong>ients are some <strong>of</strong> the<br />
smaller communities near here where there is a very<br />
high r<strong>at</strong>e <strong>of</strong> either uninsured or Medicaid p<strong>at</strong>ients.<br />
How does indigent care affect other physicians<br />
and medical facilities in the area?<br />
IF: I believe the biggest challenge we are facing in<br />
health care is funding, or lack <strong>of</strong> it. I am sure th<strong>at</strong><br />
priv<strong>at</strong>e practitioners see p<strong>at</strong>ients who have no medical<br />
insurance coverage, especially long-term<br />
p<strong>at</strong>ients who for various reasons have lost their<br />
insurance coverage. However, one cannot run a<br />
practice for indigent p<strong>at</strong>ients unless there is some<br />
source <strong>of</strong> funding—and providing hospital care is<br />
almost out <strong>of</strong> the question.<br />
WM: I think it has a big impact on some <strong>of</strong> the surgical<br />
subspecialties. Because we don’t have a charity<br />
hospital here, if you have an indigent p<strong>at</strong>ient who is<br />
involved in a car accident or sustains a gunshot<br />
wound, the physicians still have to tre<strong>at</strong> them, and<br />
still have to deal with their share <strong>of</strong> the costs involved.<br />
It is also somewh<strong>at</strong> <strong>of</strong> a neg<strong>at</strong>ive in recruiting for<br />
our surgical colleagues. It’s an issue because they<br />
can’t compete with communities like <strong>Birmingham</strong>,<br />
for example, as far as reimbursement or compens<strong>at</strong>ion.<br />
This is a spillover effect <strong>of</strong> indigent care.<br />
17<br />
Do you have any ideas or suggestions for<br />
improving indigent care in <strong>Alabama</strong>?<br />
IF: Educ<strong>at</strong>ion <strong>of</strong> the public and funding for public<br />
health are essential to improving health care in our<br />
area. The Jefferson County Department <strong>of</strong> Health<br />
is aggressively pursuing getting the public involved<br />
in learning about healthier lifestyles. If funding is<br />
not available, then programs th<strong>at</strong> are put in place<br />
for specific health-care issues will not be available to<br />
those who need them most due to the cost—specifically,<br />
issues and programs th<strong>at</strong> address weight<br />
management, increased cholesterol, and epidemic<br />
increases in diabetes mellitus type II in pre-teen<br />
and adolescent p<strong>at</strong>ients.<br />
Funding is the central issue as always, but I think<br />
it is also important to build a strong rel<strong>at</strong>ionship<br />
between the county health department and the various<br />
health systems in the area. This rel<strong>at</strong>ionship<br />
should be so interrel<strong>at</strong>ed as to avoid duplic<strong>at</strong>ion <strong>of</strong><br />
services and conserve limited funds. The community<br />
should also have significant input as to the<br />
design and delivery <strong>of</strong> these services.<br />
WM: I can speak medically and I can speak politically.<br />
Medically, I think th<strong>at</strong> we need to do a better<br />
job <strong>of</strong> supporting our health departments in<br />
the sense th<strong>at</strong>—again, this goes back to money—<br />
they are working on shoestring budgets. They<br />
have been cut back so badly th<strong>at</strong> public-health<br />
clinics have basically been annihil<strong>at</strong>ed. They’ve<br />
cut back on important programs, such as those for<br />
hypertension, and it’s a short-sighted move. I<br />
think developing a more coordin<strong>at</strong>ed health-care<br />
policy will be important.<br />
The other thing is th<strong>at</strong>, locally, we have a lot <strong>of</strong><br />
organiz<strong>at</strong>ions th<strong>at</strong> are providing indigent care, but<br />
there’s no “czar <strong>of</strong> health care” in th<strong>at</strong> regard.<br />
Obviously, everyone is doing the best job they<br />
can, but there is some duplic<strong>at</strong>ion <strong>of</strong> resources. It<br />
would be nice to have someone who is in absolute<br />
charge to design<strong>at</strong>e and better coordin<strong>at</strong>e, or <strong>at</strong><br />
least get everyone together to formul<strong>at</strong>e some sort<br />
<strong>of</strong> long-term plan.<br />
Also, our legisl<strong>at</strong>ors are going to need to realize<br />
th<strong>at</strong> health care and educ<strong>at</strong>ion are so intertwined<br />
th<strong>at</strong>, unless they make courageous moves, we’re<br />
going to continue to lag behind.<br />
As physicians, we’ve been blessed and we need to<br />
continue to take the noble approach <strong>of</strong> providing<br />
the best medical care regardless <strong>of</strong> the p<strong>at</strong>ient’s ability<br />
to pay. We’ve got to instill this notion in today’s<br />
medical students from the earliest stages.
Student Rounds: Resident Life<br />
By Dawn Mesa<br />
As previously reported in the Summer 2003 issue <strong>of</strong> the <strong>Alabama</strong><br />
Medical Alumni Bulletin, and in this issue on page 10, the<br />
Accredit<strong>at</strong>ion Council for Gradu<strong>at</strong>e Medical Educ<strong>at</strong>ion (ACGME)<br />
has set new rules regarding the maximum number <strong>of</strong> hours residents<br />
can now work per week.<br />
The rules, which went into effect on July 1, 2003, limit residents to<br />
no more than 80 work hours per week and no more than 30 consecutive<br />
work hours <strong>at</strong> a stretch. In addition, residents must be given<br />
one day out <strong>of</strong> seven free from all clinical and educ<strong>at</strong>ional responsibilities,<br />
they cannot be scheduled for in-house call more than once<br />
every three nights, they should be given <strong>at</strong> least 10 hours for rest<br />
and personal activities between daily duty periods and after in-house<br />
call, and in-house moonlighting counts toward the weekly limit. All<br />
limits are averaged over four weeks.<br />
To see how the new rules are affecting resident life <strong>at</strong> the<br />
UASOM, the <strong>Alabama</strong> Medical Alumni Bulletin asked three current<br />
residents about their experiences in light <strong>of</strong> these changes and their<br />
opinions about wh<strong>at</strong> the changes have meant for UAB’s hardest-hit<br />
specialties: surgery, OB/GYN, and internal medicine. Laurence<br />
Rosenberg, M.D., is a fifth-year general-surgery resident; Erika<br />
O’Donnell, M.D., is a fourth-year OB/GYN resident; and Elizabeth<br />
Turnipseed, M.D., is a first-year internal-medicine resident.<br />
Wh<strong>at</strong> has been the biggest change since the new regul<strong>at</strong>ions went into effect?<br />
Laurence Rosenberg (LR): I think the biggest difference, overall, is th<strong>at</strong> residents aren’t chronically tired all the<br />
time now. Residents are better-rested, they’re able to read and study more. I’m sure there’s not a resident out<br />
there from the previous gener<strong>at</strong>ion who doesn’t have a story about falling asleep <strong>at</strong> the dinner table or while<br />
driving. I know I’ve done th<strong>at</strong> once or twice.<br />
EO: We take a lot less calls, which means less<br />
experience. I think we’re doing a good job maximizing<br />
the calls and experience th<strong>at</strong> we have, but<br />
when I was an intern, I was taking nine calls a<br />
month. When you compare th<strong>at</strong> to interns now<br />
who are taking five or six calls a month, they’re<br />
missing out on a lot <strong>of</strong> experience.<br />
ET: I think, for me and for a lot <strong>of</strong> the interns,<br />
the rule th<strong>at</strong> has affected us most is the 30-hour<br />
post-call rule. I don’t like to walk out <strong>of</strong> the hospital<br />
feeling like things are unfinished, for a variety<br />
<strong>of</strong> reasons. One, you don’t want to put <strong>of</strong>f<br />
wh<strong>at</strong> you’re doing on someone else and, two, it’s<br />
really hard—especially <strong>at</strong> my level in learning—<br />
to really get a sense <strong>of</strong> wh<strong>at</strong>’s going on if you<br />
don’t see something through to fruition.<br />
Wh<strong>at</strong> is the schedule like now for residents<br />
in your field?<br />
LR: General surgery has a “flo<strong>at</strong>” group <strong>of</strong> residents<br />
who take turns in the night rot<strong>at</strong>ion. Each<br />
resident spends a rot<strong>at</strong>ion each year—four to<br />
seven weeks—working from 5 p.m. to 7 a.m.,<br />
Monday till Friday morning; Sunday they then<br />
come in <strong>at</strong> noon and work until 7 a.m. Monday.<br />
They continue th<strong>at</strong> p<strong>at</strong>tern and each level is<br />
assigned to a team—vascular surgery, general surgery,<br />
and so on. There is also a senior-level resident<br />
on call for each team, which allows for easier<br />
access to these residents, who can help out<br />
with certain problems.<br />
EO: The OB/GYN schedule is very manageable.<br />
We didn’t really change anything with our general<br />
service, as far as how many are on it. Things<br />
will change next year when the new hospital<br />
facility opens and we have an extra person to<br />
cover triage.<br />
Erika O’Donnell (EO): I think th<strong>at</strong> some <strong>of</strong> the OB/GYN rot<strong>at</strong>ions had higher time requirements than others<br />
and the 80-hour restriction impacted those services—oncology and antepartum particularly—more than<br />
others. We had to adjust our call schedule and, like surgery, changed our night-flo<strong>at</strong> system. It’s working out<br />
really well now; when we converted initially it was slightly problem<strong>at</strong>ic in terms <strong>of</strong> coverage issues.<br />
Elizabeth Turnipseed (ET): Given th<strong>at</strong> I never worked in the previous environment, I’ve noticed th<strong>at</strong>, in internal<br />
medicine, we can r<strong>at</strong>her easily facilit<strong>at</strong>e the 80-hour workweek. The post-call, 30-hour regul<strong>at</strong>ion is a little<br />
bit more difficult to adhere to and more noticeable. If this system is going to work as it’s intended, it’s got to<br />
involve more shared responsibility.<br />
Wh<strong>at</strong> has been the biggest neg<strong>at</strong>ive since the new regul<strong>at</strong>ions went into effect?<br />
LR: The biggest neg<strong>at</strong>ive th<strong>at</strong> most faculty and people complain about is a perceived lack <strong>of</strong> continuity <strong>of</strong> care.<br />
I don’t necessarily agree with th<strong>at</strong>, though, because prior to the regul<strong>at</strong>ion change, residents weren’t on call<br />
every night—so they weren’t there all the time to take care <strong>of</strong> those p<strong>at</strong>ients regardless.<br />
Erika O’Donnell says the 80-hour workweek has<br />
cre<strong>at</strong>ed a more tight-knit group <strong>of</strong> residents.<br />
18
some nurse clinicians for the different divisions. They help tremendously, and<br />
take care <strong>of</strong> discharges, setting up home health and social services, and answering<br />
p<strong>at</strong>ient phone calls—this does help out a lot.<br />
EO: We cover two hospitals for call: Cooper Green and <strong>University</strong>. The nightflo<strong>at</strong><br />
system is in place <strong>at</strong> <strong>University</strong>, and then we have people <strong>at</strong> Cooper Green<br />
for a particular rot<strong>at</strong>ion who cover most <strong>of</strong> the call during the week, one night a<br />
week, and the general call pool team covers the weekend and Friday. Everyone<br />
takes their turn. The biggest change <strong>at</strong> Cooper Green is th<strong>at</strong> one resident covers<br />
there with an <strong>at</strong>tending present <strong>at</strong> all times, except for Thursdays when there are<br />
two people there. We’ve had to have our third-year on night flo<strong>at</strong> <strong>at</strong> <strong>University</strong><br />
act as a flo<strong>at</strong>er <strong>at</strong> Cooper Green—they’ll help out if it gets busy there.<br />
ET: Our department has increased the number <strong>of</strong> residents th<strong>at</strong> it’s getting<br />
every year. I think we increased by five this past year and th<strong>at</strong> we’ll be increasing<br />
by five for the next several years.<br />
Restricted duty hours give residents more time to rest and c<strong>at</strong>ch up on their<br />
reading, says Laurence Rosenberg. “We’re here to learn and be educ<strong>at</strong>ed—<br />
th<strong>at</strong>’s the point <strong>of</strong> residency.”<br />
ET: Most <strong>of</strong> our ward medicine months have a night-flo<strong>at</strong> system where some<br />
member <strong>of</strong> the team is on every fourth night and night flo<strong>at</strong> comes in to help<br />
them, but the other members get to go home. Ultim<strong>at</strong>ely, you have to spend<br />
every eighth night <strong>at</strong> the hospital, but the team is on call every fourth. The subspecialty<br />
services are a little different. In pulmonary, for instance, there are five<br />
<strong>of</strong> us, but only one member takes call every night. In medicine, <strong>at</strong> least, we<br />
never have call nights more frequently than every fourth night, but then they<br />
range from every fourth night to every eighth night.<br />
On a personal level, how is your situ<strong>at</strong>ion now th<strong>at</strong> these limits are in place?<br />
LR: It affects the junior-level residents a little more than the senior-level residents,<br />
but I am able to read more and I’m not f<strong>at</strong>igued all the time. I can clearly<br />
feel a difference; it allows me to be more communic<strong>at</strong>ive and have a more<br />
positive <strong>at</strong>titude. I think th<strong>at</strong>’s a true benefit from the p<strong>at</strong>ient’s standpoint.<br />
Do you think this system is working out well?<br />
LR: I think it works well. Nothing’s perfect, and every situ<strong>at</strong>ion has problems,<br />
but the old way had problems too. I know th<strong>at</strong>, overall, most people are significantly<br />
happier in terms <strong>of</strong> their ability to complete and toler<strong>at</strong>e five years <strong>of</strong> a<br />
general-surgery residency.<br />
EO: As a chief, I’ve been here going on four years now, and I think th<strong>at</strong> our faculty<br />
and residents have a gre<strong>at</strong> rapport and work together very well. I think the<br />
80-hour workweek has made us a tighter group; we’ve had to rely on each other<br />
for coverage, and it’s brought us even closer together.<br />
ET: There is still some tweaking to be done, but I think for the most part it’s<br />
worked out. From a p<strong>at</strong>ient-care perspective, there were a lot <strong>of</strong> problems with<br />
residents being so grossly overworked. We can’t take our educ<strong>at</strong>ion out on the<br />
p<strong>at</strong>ients th<strong>at</strong> are here for care.<br />
How have the new rules affected hospitals th<strong>at</strong> employ residents?<br />
LR: In the past, it wouldn’t be uncommon for residents to work 110 to 115<br />
hours a week, and if they can now only work 80 hours a week, th<strong>at</strong> time has to<br />
be made up. There was no argument th<strong>at</strong> a lot <strong>of</strong> the time residents are in the<br />
hospital is a waste <strong>of</strong> their time—they’re not being educ<strong>at</strong>ed or doing productive<br />
things to learn. Instead, they’re doing tasks th<strong>at</strong> in other places are done<br />
administr<strong>at</strong>ively but, because residents are the cheapest form <strong>of</strong> labor, the residents<br />
have to do them.<br />
How have the new rules affected your department?<br />
LR: In surgery, either our director—Dr. Kirby Bland—or the hospital has hired<br />
With in-house call limited to every fourth night, Elizabeth Turnipseed and fellow<br />
residents have more time for family and hobbies.<br />
EO: I have a four-and-a-half-month-old daughter, so it’s given me more time<br />
<strong>at</strong> home with my family. I think going home post-call has allowed me to be<br />
rested and get some sleep. I think I’m more efficient the next day because I’m<br />
not so tired and not taking a ton <strong>of</strong> calls a month. Being a chief and looking<br />
for a job this past year, it’s also allowed me the time needed to interview.<br />
ET: It’s definitely been a busy year, but it’s not overwhelming. I do come in<br />
early in the morning, but I leave the hospital in time to go home and see my<br />
family. I think it’s nice to know th<strong>at</strong> there’s a little bit <strong>of</strong> predictability to it.<br />
Looking <strong>at</strong> the residency program in general, there are a lot <strong>of</strong> residents who<br />
are married, who have children, who have hobbies—I think th<strong>at</strong>’s a good indic<strong>at</strong>or<br />
th<strong>at</strong> it’s working.<br />
19
From the Development Office<br />
California Alumnus Funds Endowed Lectureship for Montgomery Program<br />
By Dawn Mesa<br />
S. Rexford Kennamer, M.D., recently made a<br />
generous gift to the School <strong>of</strong> Medicine th<strong>at</strong> provided<br />
for the establishment <strong>of</strong> the S. Rexford<br />
Kennamer, M.D., Endowed Lectureship in Internal<br />
Medicine for the Montgomery Internal Medicine<br />
Residency Program. Kennamer, who has spent the<br />
majority <strong>of</strong> his pr<strong>of</strong>essional life in California, was<br />
raised in Montgomery and is eager to help the cause<br />
<strong>of</strong> medical educ<strong>at</strong>ion in his hometown. The gift will<br />
be used to establish a lectureship th<strong>at</strong> will support<br />
educ<strong>at</strong>ion for residents, fellows, faculty, and priv<strong>at</strong>e<br />
practitioners in the Montgomery area, and to bring<br />
renowned physicians to the area.<br />
Kennamer gradu<strong>at</strong>ed from the two-year program<br />
<strong>of</strong> the Medical College <strong>of</strong> <strong>Alabama</strong> in 1943,<br />
then went on to finish his medical degree <strong>at</strong><br />
Jefferson Medical College in Philadelphia. He<br />
served his internship <strong>at</strong> Jackson Memorial<br />
Hospital in Miami and his residency in internal<br />
medicine <strong>at</strong> Veteran’s Hospital in Dallas before<br />
heading even farther west—to stay. Kennamer<br />
completed a fellowship in cardiology <strong>at</strong> Cedars <strong>of</strong><br />
Lebanon Hospital in Los Angeles and the UCLA<br />
School <strong>of</strong> Medicine. In 1954, he opened a priv<strong>at</strong>e<br />
cardiology practice in Beverly Hills and during the<br />
course <strong>of</strong> his career was the personal physician to<br />
such stars as Gary Cooper, Frank Sin<strong>at</strong>ra, and<br />
Elizabeth Taylor.<br />
Among his career achievements, Kennamer was a<br />
longtime co-investig<strong>at</strong>or in the research lab <strong>at</strong><br />
Cedars-Sinai Medical Center (CSMC); served as<br />
clinical chief <strong>of</strong> cardiology <strong>at</strong> CSMC; was named a<br />
fellow <strong>of</strong> the American College <strong>of</strong> Physicians; and is<br />
founder and president <strong>of</strong> the Western Cardiac<br />
Found<strong>at</strong>ion, which helps fund cardiac research and<br />
biomedical teaching.<br />
Over the years, Kennamer has funded a variety <strong>of</strong><br />
educ<strong>at</strong>ional initi<strong>at</strong>ives, including the Kennamer<br />
Fellowship Program in internal medicine <strong>at</strong> CSMC<br />
and the UCLA Medical Center.<br />
PROGRAMS WORTH SUPPORTING:<br />
Division <strong>of</strong> Infectious Diseases<br />
By Dawn Mesa<br />
The Division <strong>of</strong> Infectious Diseases in the Department <strong>of</strong> Pedi<strong>at</strong>rics does<br />
not focus solely on medicine for children. In fact, collabor<strong>at</strong>ive research programs<br />
currently in place in the division are making a difference in the lives <strong>of</strong><br />
both children and adults.<br />
Directed by Richard Whitley, M.D., the division is one <strong>of</strong> 14 within the<br />
Department <strong>of</strong> Pedi<strong>at</strong>rics. With 21 faculty members, the division has a primary<br />
focus on herpes viruses, but there are several faculty members who delve<br />
into areas outside this arena, such as severe acute respir<strong>at</strong>ory syndrome<br />
(SARS), West Nile virus, and the human immunodeficiency virus (HIV). The<br />
division brings in about $18 million in annual support from the N<strong>at</strong>ional<br />
Institutes <strong>of</strong> Health (NIH), second only to the Division <strong>of</strong> Hem<strong>at</strong>ology/<br />
Oncology division in NIH support <strong>at</strong> UAB.<br />
“Wh<strong>at</strong>’s fun about this division,” says Whitley, “is th<strong>at</strong> our people not only<br />
really like to do research, but they also like to take care <strong>of</strong> p<strong>at</strong>ients as well.<br />
When you look <strong>at</strong> the division’s research interests, we focus our work on herpes<br />
viruses, but we also recognize the need to move into emerging infections<br />
and microbial agents th<strong>at</strong> compromise our n<strong>at</strong>ion’s biodefense—areas which<br />
have now become key components <strong>of</strong> the division.”<br />
With this in mind, Whitley himself is a co-chair <strong>of</strong> the newly formed<br />
Southeast Regional Center <strong>of</strong> Excellence for Emerging Infections and Biodefense<br />
(SERCEB), <strong>of</strong> which UAB is a member institution—as are Duke <strong>University</strong>,<br />
Emory <strong>University</strong>, the <strong>University</strong> <strong>of</strong> Florida, the <strong>University</strong> <strong>of</strong> North Carolina,<br />
and Vanderbilt <strong>University</strong>. The consortium is centered <strong>at</strong> Duke and led by<br />
Barton Haynes, M.D., <strong>of</strong> the Duke Human Vaccine Institute.<br />
The consortium will initially work on developing new vaccines, diagnostics,<br />
and tre<strong>at</strong>ments for orthopox viruses (including smallpox and monkeypox),<br />
bacillus anthracis (anthrax), and yersinia pestis, the bacteria th<strong>at</strong> causes<br />
plague. SERCEB also will develop new vaccines to prevent emerging infections,<br />
including SARS (Dr. Sullender), and innov<strong>at</strong>ive diagnostics (Drs.<br />
Lakeman and Sullender) and new drugs to tre<strong>at</strong> infections for which current<br />
tre<strong>at</strong>ments may not be optimal.<br />
In addition to SERCEB, there is other cutting-edge research taking place<br />
within the division. Much work is being done to study congenital<br />
cytomegalovirus (CMV) infection (Drs. Britt, Boppana, Fowler, and Pass)—<br />
the most common cause <strong>of</strong> congenital infection in the United St<strong>at</strong>es today, one<br />
with a societal cost <strong>of</strong> about a billion dollars a year. Whitley notes, “From the<br />
perspective <strong>of</strong> the N<strong>at</strong>ional Academies <strong>of</strong> Science, they’ve made it their highest<br />
priority to find methods to prevent the infection.”<br />
The division also has made CMV research a high priority—both its molecular<br />
aspects and the mechanics <strong>of</strong> the body’s response to the virus. Work is<br />
being done to develop third- or fourth-gener<strong>at</strong>ion vaccines against the virus<br />
and to prevent hearing loss in children afflicted with the condition.<br />
Additional studies are underway to implement a n<strong>at</strong>ional screening program<br />
for babies <strong>at</strong> risk for hearing impairment due to CMV.<br />
Other important research in the division comes by way <strong>of</strong> the gene therapy<br />
group, which includes Drs. Parker, Cassady, and Markert. In particular,<br />
20
says Whitley, “we are using genetically engineered herpes simplex virus to tre<strong>at</strong><br />
the tumors <strong>of</strong> glioblastoma multiforme—the most lethal form <strong>of</strong> brain cancer—and<br />
understand how the tumor and virus interact, which is leading to the<br />
design <strong>of</strong> new viruses th<strong>at</strong> are more active in the tumor. The ultim<strong>at</strong>e goal is to<br />
have a virus th<strong>at</strong> can be administered intravenously to go directly to the tumor<br />
and ‘shell’ it out.”<br />
Developing new antiviral drugs is another research focus in the division.<br />
Funding has recently been awarded to develop orthopox vaccines th<strong>at</strong> will tre<strong>at</strong><br />
the viruses th<strong>at</strong> are a factor in bioterrorism and emerging infections, such as<br />
smallpox and monkeypox, as led by Drs. Earl Kern and Mark Pritchard. It is<br />
hoped th<strong>at</strong> these vaccines will<br />
“We focus our work<br />
on herpes viruses, but<br />
we also recognize the<br />
need to move into<br />
emerging infections<br />
and microbial agents<br />
th<strong>at</strong> compromise our<br />
n<strong>at</strong>ion’s biodefense.”<br />
— Richard Whitley<br />
be available for use in p<strong>at</strong>ients<br />
in the fall <strong>of</strong> 2004.<br />
Other projects in the division<br />
include the development <strong>of</strong><br />
HIV intervention techniques<br />
for adolescents (Drs. Wilson<br />
and Crain), as well as hospital<br />
models for improved antibiotic<br />
usage and ambul<strong>at</strong>ory care (Dr.<br />
Hutto) so th<strong>at</strong> children won’t<br />
have to be kept in hospitals for<br />
long periods <strong>of</strong> time. Plans are<br />
also in the works to develop a<br />
protocol to tre<strong>at</strong> SARS and West<br />
Nile virus.<br />
“At the end <strong>of</strong> the day,” says<br />
Whitley, “the division is primarily<br />
focused on virology, but we have a lot <strong>of</strong> fun in terms <strong>of</strong> addressing the contemporary<br />
needs <strong>of</strong> the popul<strong>at</strong>ion <strong>at</strong> large, not just the needs <strong>of</strong> children.”<br />
For more inform<strong>at</strong>ion on how you can help the division further its research,<br />
please contact Jennifer Philpot in the Development Office <strong>at</strong> (205) 975-7298,<br />
or see the envelope enclosed in this issue. To learn more about the work being<br />
done in the division, please visit its Web site <strong>at</strong> [main.uab.edu/<strong>uasom</strong>/2/<br />
show.asp?durki=23257].<br />
PROGRAMS WORTH SUPPORTING:<br />
Sparks Clinics Rett Syndrome Clinic<br />
By Doug Gillett<br />
For the first six to 18 months, everything appears normal. Then the girls<br />
start to regress. They lose any progress they made in learning to walk, as well<br />
as wh<strong>at</strong>ever vocabulary they’ve developed. They don’t make eye contact the<br />
way they used to. And they engage in strange, constant hand motions like<br />
wringing their hands or pulling <strong>at</strong> their hair. The worst part is th<strong>at</strong> this<br />
regression is permanent—these girls will grow and develop little over the<br />
remainder <strong>of</strong> their lives.<br />
The disease th<strong>at</strong> has subjected thousands <strong>of</strong> baby girls to this f<strong>at</strong>e, Rett<br />
syndrome, was first diagnosed by an Austrian pedi<strong>at</strong>rician in the 1960s. But<br />
it was only in the early 1980s th<strong>at</strong> the world began taking notice. Since then,<br />
Alan K. Percy, M.D.—director <strong>of</strong> the Sparks Clinics and associ<strong>at</strong>e director<br />
<strong>of</strong> the Civitan Intern<strong>at</strong>ional Research Center—has dedic<strong>at</strong>ed himself to<br />
tracking down the syndrome’s causes and devising tre<strong>at</strong>ment.<br />
21<br />
“We always thought it was a genetic condition, because it only affected<br />
girls,” he says. “The unusual thing about it is th<strong>at</strong> it rarely recurs in the family,<br />
so th<strong>at</strong> made traditional genetic-linkage studies impossible.”<br />
Working with Rett expert Huda Zoghbi, M.D., in Houston, Percy loc<strong>at</strong>ed<br />
a gene with which the syndrome was associ<strong>at</strong>ed, and he says th<strong>at</strong> 80 to 85<br />
percent <strong>of</strong> the girls who meet the clinical criteria for Rett syndrome have<br />
mut<strong>at</strong>ions in th<strong>at</strong> gene. Researchers have identified more than 200 different<br />
mut<strong>at</strong>ions, but eight specific mut<strong>at</strong>ions make up the vast majority <strong>of</strong> those<br />
cases, Percy explains.<br />
“By the n<strong>at</strong>ure <strong>of</strong> this gene, we think we have <strong>at</strong> least a ballpark idea <strong>of</strong> wh<strong>at</strong><br />
the problem is—the connections th<strong>at</strong> nerve cells make with each other, the<br />
synapses, are not formed stably, or they’re not formed <strong>at</strong> all,” he says. “And if<br />
they are formed, they’re not maintained properly, so the brain itself doesn’t<br />
develop the way it would in a normal person.” Estim<strong>at</strong>es once put the incidence<br />
<strong>of</strong> the disease <strong>at</strong> one in 40,000 females, but the frequency increased as<br />
<strong>doctors</strong> got better <strong>at</strong> differenti<strong>at</strong>ing the syndrome from disorders th<strong>at</strong> had similar<br />
symptoms, such as autism and cerebral palsy. Incidence is now estim<strong>at</strong>ed<br />
<strong>at</strong> approxim<strong>at</strong>ely one in 20,000.<br />
continued on next page
continued from previous page<br />
Alan K. Percy has spent decades investig<strong>at</strong>ing<br />
Rett syndrome.<br />
From the Development Office<br />
Percy has a rare-disease grant proposal in the works to<br />
study the n<strong>at</strong>ural history <strong>of</strong> the disorder. “The only way we<br />
can do th<strong>at</strong> is to follow large numbers <strong>of</strong> girls and women<br />
over time to see how they m<strong>at</strong>ure,” he says. “Then we’ll<br />
have some kind <strong>of</strong> composite inform<strong>at</strong>ion. . . . And if we<br />
collect a significant number <strong>of</strong> girls with each <strong>of</strong> those<br />
mut<strong>at</strong>ions, perhaps we can make inferences about wh<strong>at</strong> one<br />
mut<strong>at</strong>ion does versus another.”<br />
UAB’s d<strong>at</strong>abase contains inform<strong>at</strong>ion on more than<br />
150 girls, in addition to more than 300 in the d<strong>at</strong>abase<br />
Percy started during his time <strong>at</strong> the Baylor College <strong>of</strong><br />
Medicine. “The goal <strong>of</strong> this n<strong>at</strong>ural-history study, which<br />
is being conducted between the two loc<strong>at</strong>ions, is to follow<br />
1,000 girls,” he says.<br />
“Our costs are minimized by the fact th<strong>at</strong> the clinic visits<br />
are free—the families simply have to get here,” Percy<br />
explains. “We will see girls up to age 12 twice a year, and over<br />
age 12 once a year. We’re not trying to become the physicians<br />
for these girls—they’ll remain with their own <strong>doctors</strong>, wherever<br />
they are. We just want to have the inform<strong>at</strong>ion.”<br />
These efforts have applic<strong>at</strong>ions beyond research. The work<br />
is proving to be an invaluable resource for families, Percy says,<br />
“because we’ve g<strong>at</strong>hered things from our own experience as<br />
to how to approach various aspects <strong>of</strong> care.”<br />
Families need all the help they can get. Girls with Rett<br />
syndrome are classified as “total-care,” meaning they need<br />
lifelong assistance with everyday concerns such as feeding,<br />
transport<strong>at</strong>ion, and hygiene; they also experience a higher<br />
incidence <strong>of</strong> health problems ranging from constip<strong>at</strong>ion<br />
and gastric reflux to scoliosis so severe it requires surgery.<br />
“We’ve learned a gre<strong>at</strong> deal about th<strong>at</strong>,” Percy says. “So<br />
there are aspects <strong>of</strong> this disorder for which we’ve become<br />
a resource for people all over the country.”<br />
For more inform<strong>at</strong>ion on how you can contribute to<br />
the efforts <strong>of</strong> the Sparks Clinics Rett Syndrome Clinic,<br />
please contact Jennifer Philpot in the Development Office<br />
<strong>at</strong> (205) 975-7298, or see the envelope enclosed in this<br />
issue. In addition, to learn more about the work being<br />
done in the clinic, please visit its Web site <strong>at</strong><br />
[www.circ.uab.edu/Sparks/Rett/index.html].<br />
PROGRAMS WORTH<br />
SUPPORTING:<br />
Division <strong>of</strong> Orthopaedic Surgery<br />
By Russ Willcutt<br />
Knees are necessary. Th<strong>at</strong>’s why research being<br />
conducted in the Division <strong>of</strong> Orthopaedic Surgery<br />
is so important. Not only are they working to<br />
design better artificial-knee mechanisms, they’re<br />
testing those th<strong>at</strong> have been in use for some time,<br />
and then removed, to examine the wear and tear<br />
they’ve undergone—all in an <strong>at</strong>tempt to provide<br />
better future m<strong>at</strong>erials and designs.<br />
“We’re working with the Department <strong>of</strong><br />
Biomedical Engineering both to design new totalknee<br />
replacement mechanisms, along with other<br />
components, and to examine those we’ve retrieved<br />
through replacement procedures—known in the<br />
orthopedic community as ‘device retrieval and analysis,’<br />
” says Jack Lemons, M.S., Ph.D., who is the<br />
director <strong>of</strong> labor<strong>at</strong>ory surgical research for the<br />
22<br />
Far left: Jack Lemons.<br />
Left: The orthopaedic<br />
surgery division’s analysis<br />
<strong>of</strong> wear and tear on<br />
existing artificial knee<br />
mechanisms will help<br />
engineers design<br />
stronger, more durable<br />
joints for elderly p<strong>at</strong>ients.<br />
Division <strong>of</strong> Orthopaedic Surgery in the School <strong>of</strong><br />
Medicine and Prosthodontics and Biom<strong>at</strong>erials in the<br />
School <strong>of</strong> Dentistry. “We receive about 400 devices<br />
each year, and we rely on residents and gradu<strong>at</strong>e students<br />
to perform the majority <strong>of</strong> the analyses.”<br />
The program is mostly funded internally <strong>at</strong> this<br />
point, with additional funds provided by the N<strong>at</strong>ional<br />
Institutes <strong>of</strong> Health (NIH)—but more help is needed.<br />
“While we need stipends for the students and<br />
money to cover the costs <strong>of</strong> m<strong>at</strong>erials, wh<strong>at</strong> we need<br />
more than anything is to be able to purchase new<br />
equipment and to refurbish our labs,” Lemons says.<br />
He adds th<strong>at</strong> he has hopes <strong>of</strong> gaining new labor<strong>at</strong>ory<br />
space in the Shelby Building once it’s completed,<br />
but there is still the m<strong>at</strong>ter <strong>of</strong> the new equipment<br />
th<strong>at</strong> will be needed to continue the division’s<br />
research and achieve successful outcomes.<br />
“To re-outfit our current facilities, we’d need<br />
something along the lines <strong>of</strong> half a million to a million<br />
dollars,” he says. “The various micro- and nanohardness<br />
machines, for instance, can cost anywhere<br />
from $30,000 to $250,000, but the return on th<strong>at</strong><br />
investment can be quite substantial.”<br />
While these devices are sometimes used to aid<br />
trauma victims or younger individuals afflicted<br />
with osteoarthritis, the vast majority <strong>of</strong> the p<strong>at</strong>ients<br />
who will benefit from the division’s research findings<br />
are elderly. “We’re constantly looking to the<br />
NIH and the N<strong>at</strong>ional Science Found<strong>at</strong>ion for<br />
funding,” Lemons says. “But we also feel th<strong>at</strong> there<br />
might be members <strong>of</strong> the community who would<br />
be interested in furthering our efforts, too.”<br />
To learn more about contributing to this worthy<br />
cause, including naming opportunities, contact<br />
Jeannie Horton <strong>at</strong> (205) 325-8660, or see the<br />
envelope enclosed in this issue. In addition, to<br />
learn more about the work being done in the division,<br />
please visit its Web site <strong>at</strong> [main.uab.edu/<br />
<strong>uasom</strong>/2/show.asp?durki=23738].
Lanier Gifts Support<br />
Neurology Research<br />
Family Found<strong>at</strong>ion Aids Efforts to Solve Parkinson’s Disease<br />
By M<strong>at</strong>t Windsor<br />
When Ray L. W<strong>at</strong>ts, M.D., came to the UASOM from Emory <strong>University</strong> last<br />
year, he brought with him decades <strong>of</strong> research into neurological disorders and<br />
an invaluable partner: the Sartain Lanier Family Found<strong>at</strong>ion.<br />
The charitable organiz<strong>at</strong>ion, founded by successful apparel businessman Sartain<br />
Lanier, had a history <strong>of</strong> contributions to Vanderbilt <strong>University</strong> and Atlanta-area<br />
institutions such as Emory. But personal tragedy brought the found<strong>at</strong>ion into contact<br />
with W<strong>at</strong>ts, and the rel<strong>at</strong>ionship has continued to flourish in <strong>Birmingham</strong>.<br />
An expanding neurology department is working on tre<strong>at</strong>ments for Parkinson’s,<br />
Alzheimer’s, and more, says Ray L. W<strong>at</strong>ts.<br />
“My longtime p<strong>at</strong>ient, Vance Lanier [vice chairman <strong>of</strong> the found<strong>at</strong>ion’s board<br />
<strong>of</strong> trustees and Sartain’s son], was a very strong supporter <strong>of</strong> Parkinson’s<br />
research—he had Parkinson’s himself,” W<strong>at</strong>ts explains. “He passed away in<br />
December <strong>of</strong> 2003, but the family and the found<strong>at</strong>ion continue a strong interest<br />
in helping to solve Parkinson’s disease.”<br />
W<strong>at</strong>ts has received gifts <strong>of</strong> $300,000 from the found<strong>at</strong>ion both last year and<br />
in 2004, and those gifts are helping support research efforts in the UAB<br />
Parkinson Disease and Movement Disorders Center. The center, design<strong>at</strong>ed by<br />
the N<strong>at</strong>ional Institutes <strong>of</strong> Health in 2003, <strong>of</strong>fers comprehensive clinical care,<br />
conducts clinical research to evalu<strong>at</strong>e novel tre<strong>at</strong>ment options for the disease,<br />
and educ<strong>at</strong>es health-care pr<strong>of</strong>essionals and the public.<br />
Philanthropic support will also help W<strong>at</strong>ts and colleagues reach two ambitious<br />
goals, he says: “Wh<strong>at</strong> brought me back to UAB was the opportunity to<br />
help build on the excellence already present in the Department <strong>of</strong> Neurology,<br />
and perhaps even more important, the opportunity to work with others <strong>at</strong> UAB<br />
in an effort to build a comprehensive Neurosciences Center <strong>of</strong> Excellence and<br />
position th<strong>at</strong> center to become a n<strong>at</strong>ional and intern<strong>at</strong>ional leader in the coming<br />
five to 10 years.”<br />
To achieve those goals, “we’re going to recruit about 25 additional faculty in Neurology,<br />
half <strong>of</strong> whom will be labor<strong>at</strong>ory research-oriented, and half <strong>of</strong> whom will be<br />
clinical research-oriented,” says W<strong>at</strong>ts. The expansion will double the size <strong>of</strong> the<br />
department; plans call for Neurology to move to the Sparks Building so it will be in<br />
close proximity to investig<strong>at</strong>ors in Psychi<strong>at</strong>ry, Neurop<strong>at</strong>hology, and Neurobiology.<br />
“Th<strong>at</strong>’s wh<strong>at</strong> it will take to get us to a size comparable to the best departments in<br />
the n<strong>at</strong>ion,” he says. “And if we recruit the right people, then with them will come<br />
excellent clinical programs, research programs, and educ<strong>at</strong>ional programs.”<br />
23<br />
Film Premiere Benefits 1917 Clinic<br />
By Dawn Mesa<br />
A bit <strong>of</strong> Tinseltown came to <strong>Birmingham</strong> this past November,<br />
when a Hollywood-style movie premiere <strong>at</strong> the <strong>Alabama</strong> The<strong>at</strong>re<br />
was held to benefit UAB’s AIDS Outp<strong>at</strong>ient (1917) Clinic.<br />
The Trip was produced by two <strong>Alabama</strong> n<strong>at</strong>ives, producer<br />
Houston King and executive producer Tom Blount. “The benefit<br />
was our most successful ever, in a number <strong>of</strong> ways,” says Michael<br />
Saag, M.D., director <strong>of</strong> the clinic. “Financially, we netted more than<br />
$31,000 for the clinic, which is<br />
quite remarkable … and even<br />
more important, the turnout<br />
was quite phenomenal.”<br />
The clinic, which opened in<br />
1988, conducts high-quality<br />
research protocols in both the<br />
clinical science and basic science<br />
arenas, provides educ<strong>at</strong>ion<br />
to health-care providers, and<br />
establishes vital links with the<br />
p<strong>at</strong>ient community and general<br />
popul<strong>at</strong>ion through orchestr<strong>at</strong>ed<br />
outreach programs. The<br />
clinic provides many services to<br />
individuals living with HIV/<br />
AIDS, including an outp<strong>at</strong>ient<br />
tre<strong>at</strong>ment clinic, research clinic,<br />
dental clinic, women’s HIV<br />
clinic, and oncology clinic. The<br />
1917 Clinic also serves as one<br />
<strong>of</strong> 28 federally funded AIDS<br />
Clinical Trials Group sites<br />
involved in the evalu<strong>at</strong>ion <strong>of</strong><br />
experimental therapeutics.<br />
Looking ahead, the clinic is<br />
planning to host additional fundraising<br />
events—though not on<br />
the scale <strong>of</strong> a Hollywood-type<br />
movie premiere. Presently, plans<br />
are under way to host a the<strong>at</strong>er-type event l<strong>at</strong>er this year. In addition,<br />
volunteer opportunities are available for those interested in assisting<br />
in the clinic. For more inform<strong>at</strong>ion on how you can help the 1917<br />
Clinic and its p<strong>at</strong>ients, please contact Rebecca Lark in the<br />
Development Office <strong>at</strong> (205) 975-6149.<br />
While W<strong>at</strong>ts is an intern<strong>at</strong>ionally known leader in Parkinson’s research, his<br />
department’s interests run the gamut <strong>of</strong> neurological problems. “We want to<br />
understand basic normal processes in the brain,” he says, “but our real focus is<br />
on understanding disease mechanisms so th<strong>at</strong> we can develop new and better<br />
tre<strong>at</strong>ments in many different areas: Parkinson’s disease, Alzheimer’s, brain<br />
tumors, stroke, multiple sclerosis—you name it.”<br />
A <strong>Birmingham</strong> n<strong>at</strong>ive, W<strong>at</strong>ts says he relishes his return to the campus where<br />
he earned undergradu<strong>at</strong>e degrees in electrical and biomedical engineering. “I<br />
love UAB, and I love <strong>Alabama</strong>, so it’s gre<strong>at</strong> to be back.”
2004 Alumni Weekend Report<br />
The 31st annual Medical Alumni Weekend, February 27-28, 2004,<br />
fe<strong>at</strong>ured the traditional activities: the Reynolds Historical Lecture,<br />
the Alumni Associ<strong>at</strong>ion Board <strong>of</strong> Directors’ meeting, the Scientific<br />
Program, the annual luncheon and associ<strong>at</strong>ion meeting, the<br />
Constance and James A. Pittman Lecture, and 13 class reunion dinners.<br />
We also fe<strong>at</strong>ured two book signings just before the luncheon:<br />
Martin L. Dalton Jr., M.D., class <strong>of</strong> 1957, brought his new book,<br />
Champ Lyons: Surgeon; and former dean Clifton K. Meador, M.D.,<br />
signed his newest public<strong>at</strong>ion, Med School.<br />
REYNOLDS LECTURE<br />
The 25th annual Reynolds Historical Lecture on Friday evening fe<strong>at</strong>ured James<br />
H. Thrall, M.D., lecturing on “Scientific Reductionism and 21st-Century<br />
Radiology.” The lecture was presented in the Historical Library’s Ireland Room,<br />
loc<strong>at</strong>ed in Lister Hill Library. It was followed by a reception sponsored by the<br />
Reynolds Library and the Caduceus Club <strong>at</strong> the Woodward House.<br />
SCIENTIFIC PROGRAM<br />
S<strong>at</strong>urday morning, President Betty W. Vaughan, M.D., welcomed everyone to<br />
the scientific program, “Medical Issues 2004.” Then she turned the program over<br />
to chair Alan R. Dimick, M.D. There was something for everyone, starting with<br />
the present<strong>at</strong>ion on “Organiz<strong>at</strong>ion and Functions <strong>of</strong> the Jefferson County<br />
Coroner/Medical Examiner’s Office,” by Robert M. Brissie, M.D. Brissie is pr<strong>of</strong>essor<br />
and director <strong>of</strong> the UASOM’s Division <strong>of</strong> Forensic P<strong>at</strong>hology and serves as<br />
chief coroner/medical examiner <strong>of</strong> Jefferson County. Next on the program was<br />
“The Management <strong>of</strong> Menopause” by R. Edward Varner, M.D., pr<strong>of</strong>essor in the<br />
Department <strong>of</strong> Obstetrics and Gynecology. Sarah L. Morgan, M.D., associ<strong>at</strong>e<br />
dean for research compliance and pr<strong>of</strong>essor <strong>of</strong> nutrition science, followed with a<br />
discussion titled “Osteoporosis 2004.” After the c<strong>of</strong>fee break, Ray L. W<strong>at</strong>ts,<br />
M.D., pr<strong>of</strong>essor and chair <strong>of</strong> the Department <strong>of</strong> Neurology, presented “Recent<br />
Advances in the Understanding <strong>of</strong> Parkinson’s Disease.” The program closed with<br />
a fascin<strong>at</strong>ing present<strong>at</strong>ion, “Skin Grafting Between Burned Twins,” by William<br />
D. Hardin, M.D., associ<strong>at</strong>e pr<strong>of</strong>essor <strong>of</strong> surgery and director <strong>of</strong> the Burns and<br />
Trauma Center <strong>at</strong> Children’s Hospital.<br />
ANNUAL LUNCHEON<br />
President Vaughan presided over the annual luncheon, held <strong>at</strong> the <strong>Birmingham</strong><br />
Marriott. The traditional awards were presented as follows:<br />
2004 DISTINGUISHED ALUMNUS<br />
In recognition <strong>of</strong> outstanding contributions in the field <strong>of</strong> medicine and<br />
demonstr<strong>at</strong>ion <strong>of</strong> the high principles <strong>of</strong> the medical pr<strong>of</strong>ession<br />
Norman E. McSwain Jr., M.D., FACS<br />
Norman E. McSwain Jr., M.D., is a n<strong>at</strong>ive <strong>of</strong> Albertville, <strong>Alabama</strong>. He received<br />
his Bachelor <strong>of</strong> Science degree from the <strong>University</strong> <strong>of</strong> the South, Sewanee, Tennessee,<br />
in 1959 and gradu<strong>at</strong>ed from the Medical<br />
College <strong>of</strong> <strong>Alabama</strong> in 1963. He is currently<br />
pr<strong>of</strong>essor <strong>of</strong> surgery in the Department<br />
<strong>of</strong> Surgery <strong>at</strong> Tulane <strong>University</strong> School <strong>of</strong><br />
Medicine in New Orleans, Louisiana, and<br />
has been the visiting clinical pr<strong>of</strong>essor for<br />
NASA <strong>at</strong> the Johnson Space Center in<br />
Houston, Texas, since 2002.<br />
Over the course <strong>of</strong> his career, McSwain<br />
Norman McSwain and his<br />
daughter Merry.<br />
24<br />
has been the trauma director <strong>at</strong> Charity Hospital Level I Trauma Center, Medical<br />
Center <strong>of</strong> Louisiana <strong>at</strong> New Orleans; special assistant, clinical medicine, <strong>at</strong> the<br />
Johnson Space Center; and associ<strong>at</strong>e residency program director and director <strong>of</strong> the<br />
Trauma Program in the Department <strong>of</strong> Surgery <strong>at</strong> Tulane <strong>University</strong> School <strong>of</strong><br />
Medicine. He has been a member <strong>of</strong> the teaching staff in the emergency department<br />
<strong>at</strong> Charity Hospital <strong>of</strong> Louisiana <strong>at</strong> New Orleans and the <strong>at</strong>tending staff <strong>at</strong> Tulane<br />
Medical Center Hospital and Clinic and Charity Hospital. He has also served as<br />
police surgeon <strong>at</strong> the New Orleans Police Department and medical director <strong>of</strong> the<br />
New Orleans Jazz and Heritage Festival.<br />
McSwain is founder, medical director, and editor-in-chief <strong>of</strong> the PreHospital<br />
Trauma Life Support (PHTLS) training program for the N<strong>at</strong>ional Associ<strong>at</strong>ion <strong>of</strong><br />
Emergency Medical Technicians (NAEMT). The program has trained more than<br />
300,000 pre-hospital providers in 37 countries since it started in 1981. He has<br />
served as a member <strong>of</strong> the Prehospital Care Committee <strong>of</strong> the American College<br />
<strong>of</strong> Surgeons (ACS), and as chair and initial member <strong>of</strong> the ad hoc committee to<br />
start the Advanced Trauma Life Support program (ATLS) for the ACS. This program<br />
has trained more than 400,000 physicians since 1980. He also founded the<br />
Emergency Medical Technician Training Program <strong>at</strong> the <strong>University</strong> <strong>of</strong> Kansas<br />
School <strong>of</strong> Medicine and served as chair from 1973–1977.<br />
McSwain is certified with the American Board <strong>of</strong> Surgery (1972); N<strong>at</strong>ional<br />
Registry <strong>of</strong> Emergency Medical Technicians–Ambulance (1978); and N<strong>at</strong>ional<br />
Registry <strong>of</strong> Emergency Medical Technicians–Paramedic (1980).<br />
He has physician certific<strong>at</strong>es in diving medicine from the Intern<strong>at</strong>ional Society <strong>of</strong><br />
Aqu<strong>at</strong>ic Medicine in Los Angeles, California, and hyperbaric medicine from St.<br />
Luke’s Hospital in Milwaukee, Wisconsin. He also has a divemaster certific<strong>at</strong>e from<br />
the N<strong>at</strong>ional Associ<strong>at</strong>ion <strong>of</strong> Underw<strong>at</strong>er Instructors and an enriched air (nitrox) diver<br />
certific<strong>at</strong>e from Technical Diving Intern<strong>at</strong>ional in Coral Star, Bahamas. He was a<br />
founding member <strong>of</strong> the board <strong>of</strong> directors and director <strong>of</strong> Continuing Medical<br />
Educ<strong>at</strong>ion for the Intern<strong>at</strong>ional Society <strong>of</strong> Aqu<strong>at</strong>ic Medicine from 1975–1995.<br />
A prolific writer, McSwain has authored 26 books and 105 book chapters since<br />
1976, contributed to 331 public<strong>at</strong>ions since 1968, and made more than 700 present<strong>at</strong>ions<br />
since 1972. His significant pr<strong>of</strong>essional honors include the<br />
Commend<strong>at</strong>ion Medal, United St<strong>at</strong>es Air Force (1965); NAEMT President’s<br />
Leadership Award (1980, 1984, 2000); U.S. Naval Forces Central Command<br />
Cit<strong>at</strong>ion for Outstanding Performance as General Surgeon, Medical Tre<strong>at</strong>ment<br />
Facility, USNS Comfort (T-AH 20), during Oper<strong>at</strong>ion Desert Storm (1991);<br />
Surgeons Award for Service to Safety, American College <strong>of</strong> Surgeons, American<br />
Associ<strong>at</strong>ion for the Surgery <strong>of</strong> Trauma, N<strong>at</strong>ional Safety Council (1998); and the<br />
NAEMT’s Rocco V. Morando Lifetime Achievement Award (2002). In 2003, he<br />
was named the Scudder Or<strong>at</strong>or by the American College <strong>of</strong> Surgeons.<br />
McSwain served as a captain in the United St<strong>at</strong>es Naval Reserve on active duty<br />
from 1965–1967; he served in the Medical Corps <strong>of</strong> the Reserve from 1984–1995.<br />
2004 HETTIE BUTLER TERRY COMMUNITY SERVICE AWARD<br />
For outstanding commitment to community service<br />
James H. Alford Jr., M.D.<br />
James H. Alford Jr., M.D., is a n<strong>at</strong>ive <strong>of</strong><br />
Albertville, <strong>Alabama</strong>. He gradu<strong>at</strong>ed from<br />
Albertville High School in 1955 and earned<br />
a Bachelor <strong>of</strong> Science degree from the<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> in 1959. He gradu<strong>at</strong>ed<br />
from the Medical College <strong>of</strong> <strong>Alabama</strong> in<br />
1963 and remained there to complete his<br />
internship and residency in obstetrics and<br />
Susan and James Alford.<br />
gynecology in 1968. He is a fellow <strong>of</strong> the<br />
American College <strong>of</strong> Obstetrics and Gynecology, and is a member <strong>of</strong> several other<br />
medical organiz<strong>at</strong>ions, including the Medical Associ<strong>at</strong>ion <strong>of</strong> the St<strong>at</strong>e <strong>of</strong> <strong>Alabama</strong><br />
and the American Society <strong>of</strong> Addiction Medicine.<br />
Alford is an active member <strong>of</strong> the <strong>Alabama</strong> Physicians Health Program and has
served on the <strong>Alabama</strong> Impaired Physicians Committee for the past four years. He<br />
also serves on the boards <strong>of</strong> Recovery Ministries <strong>of</strong> the Episcopal Church and the<br />
Council on Substance Abuse. For the past two years he has been active as a speaker<br />
for the <strong>Alabama</strong> Campaign to Prevent Teen Pregnancy.<br />
Since 1992, he has been a member <strong>of</strong> Intern<strong>at</strong>ional Doctors in Alcoholics<br />
Anonymous (IDAA). Founded in 1949, this organiz<strong>at</strong>ion has 4,500 doctor<strong>at</strong>e-level<br />
members <strong>of</strong> health-care pr<strong>of</strong>essions who are recovering from addiction. IDAA is dedic<strong>at</strong>ed<br />
to promoting recovery from addiction and its consequences for its members<br />
and their families. Jim has served on the Steering Committee for the past four years;<br />
last year he was the chair <strong>of</strong> the group’s annual meeting, which was held in Mobile,<br />
<strong>Alabama</strong>, with more than 650 members and their families in <strong>at</strong>tendance.<br />
Jim is the f<strong>at</strong>her <strong>of</strong> three children: Vivian, Bradley, and Gregory. He and his wife,<br />
Susan, live in Montgomery, where he has practiced medicine since 1968. They have<br />
one grandson, Huston, and are anticip<strong>at</strong>ing the birth <strong>of</strong> a second grandchild this fall.<br />
2004 GARBER GALBRAITH MEDICAL-POLITICAL SERVICE AWARD<br />
For outstanding service to the medical pr<strong>of</strong>ession<br />
George C. Smith Sr., M.D., FAAFP<br />
George C. Smith Sr., M.D., is a boardcertified<br />
family physician from Lineville,<br />
<strong>Alabama</strong>. He received his Bachelor <strong>of</strong> Science<br />
degree in pharmacy from Howard College<br />
and gradu<strong>at</strong>ed from the Medical College <strong>of</strong><br />
<strong>Alabama</strong> in 1965. After an internship <strong>at</strong><br />
Lloyd Noland Hospital he opened his practice<br />
in Lineville in 1966, and still practices<br />
Wanda and George Smith.<br />
family medicine there with three partners. But his avoc<strong>at</strong>ion is c<strong>at</strong>tle farming; he<br />
and his wife, Wanda, live on their c<strong>at</strong>tle farm in Lineville. They have five sons.<br />
Currently, Smith is a clinical assistant pr<strong>of</strong>essor in the Department <strong>of</strong> Behavioral<br />
Community Medicine <strong>at</strong> the College <strong>of</strong> Community Health Services <strong>of</strong> the<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong>. He is active in serving as a preceptor for medical students,<br />
residents, and nurse practitioners. He also has been active in organized medicine<br />
most <strong>of</strong> his career, as president <strong>of</strong> the <strong>Alabama</strong> Chapter <strong>of</strong> the American Academy<br />
<strong>of</strong> Family Physicians, as a member <strong>of</strong> the board <strong>of</strong> directors <strong>of</strong> <strong>Alabama</strong> Quality<br />
Assurance Found<strong>at</strong>ion, and as a member <strong>of</strong> the task force on health-care reform.<br />
He serves as an altern<strong>at</strong>e deleg<strong>at</strong>e <strong>of</strong> the American Medical Associ<strong>at</strong>ion.<br />
Smith was elected to the Board <strong>of</strong> Censors <strong>of</strong> the Medical Associ<strong>at</strong>ion <strong>of</strong> the<br />
St<strong>at</strong>e <strong>of</strong> <strong>Alabama</strong> in 1994. He has served as chair <strong>of</strong> the Board <strong>of</strong> Censors, St<strong>at</strong>e<br />
Board <strong>of</strong> Medical Examiners, and St<strong>at</strong>e Committee <strong>of</strong> Public Health since 2000.<br />
to all first-year students <strong>at</strong> Harvard Medical School. His book based on this course,<br />
Human Genetics: A Problem-Based Approach (published by Blackwell Science), is<br />
currently in its second edition, and has been transl<strong>at</strong>ed into Italian and Korean.<br />
Korf is also co-editor <strong>of</strong> the fourth edition <strong>of</strong> Emery and Rimoin’s Principles and<br />
Practice <strong>of</strong> Medical Genetics. He is president <strong>of</strong> the Associ<strong>at</strong>ion <strong>of</strong> Pr<strong>of</strong>essors <strong>of</strong><br />
Human and Medical Genetics, and just completed a term as vice president for clinical<br />
genetics <strong>of</strong> the American College <strong>of</strong> Medical Genetics. He also serves as a member<br />
<strong>of</strong> the Liaison Committee on Medical Educ<strong>at</strong>ion, which accredits U.S. and<br />
Canadian medical-educ<strong>at</strong>ion programs. His research interests focus on the n<strong>at</strong>ural<br />
history and tre<strong>at</strong>ment <strong>of</strong> neur<strong>of</strong>ibrom<strong>at</strong>osis type 1.<br />
SATURDAY EVENING REUNIONS<br />
The reunion classes <strong>of</strong> 1949, 1954, 1959, 1964, 1969, 1974, 1979, 1984, 1989,<br />
1994, and the classes <strong>of</strong> 1947, 1956, and 1958 g<strong>at</strong>hered on S<strong>at</strong>urday evening for a<br />
reception <strong>at</strong> the Marriott for all the classes, sponsored by the Medical Alumni<br />
Associ<strong>at</strong>ion. After an hour <strong>of</strong> fellowship, each class went to a separ<strong>at</strong>e class dinner.<br />
Special thanks go to alumni Tom Caldwell, M.D., Bob Lauderdale, M.D., John<br />
Rochester, M.D., Walter Pittman, M.D., Richard Lytle, M.D., George Adams,<br />
M.D., Jimmy Chambers, M.D., Karl Egerman, M.D., Bill Staggers, M.D., Kevin<br />
A large and voluble crowd made up <strong>of</strong> several decades <strong>of</strong> medical school<br />
alumni filled the Marriott for the S<strong>at</strong>urday evening reunions.<br />
Hornsby, M.D., Bill Beasley, M.D., Alan Dimick, M.D., Frank Waldo, M.D., and<br />
Bob Adams, M.D., for all their help with reunions. Jimmy Chambers and Karl<br />
Egerman raised the bar for everyone else—they worked the phones for their 1974<br />
class, and were rewarded with record <strong>at</strong>tendance!<br />
The class reunions are a highlight <strong>of</strong> the Alumni Weekend each year. If you have<br />
a reunion coming up in 2005 (if your class ends in a “5” or “0”) and would like to<br />
help, please call Elaine Chambless <strong>at</strong> the Medical Alumni Office <strong>at</strong> (205) 934-4463.<br />
CONSTANCE S. AND JAMES A. PITTMAN LECTURE<br />
The Pittman lecture fe<strong>at</strong>ured Bruce R. Korf, M.D., Ph.D., with a present<strong>at</strong>ion<br />
titled “Medicine in Transform<strong>at</strong>ion: Integr<strong>at</strong>ion <strong>of</strong> Genetics into<br />
Medical Practice”<br />
Bruce R. Korf, M.D., Ph.D.<br />
Bruce R. Korf, M.D., Ph.D., received his medical<br />
degree from Cornell <strong>University</strong> Medical College and<br />
his doctor<strong>at</strong>e in genetics and cell biology from<br />
Rockefeller <strong>University</strong>. He then completed training in<br />
pedi<strong>at</strong>rics, pedi<strong>at</strong>ric neurology, and genetics <strong>at</strong><br />
Children’s Hospital in Boston, Massachusetts. He<br />
served as clinical director in the Division <strong>of</strong> Genetics <strong>at</strong><br />
Children’s Hospital from 1986 to 1999 and as the medical<br />
director <strong>of</strong> the Harvard-Partners Center for<br />
Genetics and Genomics from 1999–2002. Currently he is the Wayne H. and Sara<br />
Crews Finley Pr<strong>of</strong>essor <strong>of</strong> Genetics and chair <strong>of</strong> the Department <strong>of</strong> Genetics <strong>at</strong> the<br />
UASOM. In his previous appointment <strong>at</strong> Harvard Medical School, he served as codirector<br />
<strong>of</strong> the course Genetics, Developmental and Reproductive Biology, taught<br />
HERE’S TO SIXTY YEARS<br />
The class th<strong>at</strong> m<strong>at</strong>ricul<strong>at</strong>ed in 1943 held a 60-year reunion on December<br />
5-6, 2003. One <strong>of</strong> their weekend activities was a luncheon <strong>at</strong> the Medical<br />
Alumni Building fe<strong>at</strong>uring Kirby Bland, M.D. (’68), chair <strong>of</strong> the<br />
Department <strong>of</strong> Surgery <strong>at</strong> the UASOM, as the speaker. Dewey White,<br />
M.D., organized the host committee, which included Jack Alexander,<br />
M.D., Robert M. Bryan, M.D., John Harris, M.D., William Kessler,<br />
M.D., and Wiley Livingston, M.D.<br />
25
medical alumni bulletin<br />
CLASS NOTES<br />
1955<br />
GEORGE ELLIS RUDD received the Delta Chi<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> Jefferson J. Coleman Alumni<br />
Award for personal and pr<strong>of</strong>essional achievement in<br />
August 2003. Rudd is retired from family practice<br />
and lives in Pinson, <strong>Alabama</strong>.<br />
1955 and 1960<br />
SARA CREWS FINLEY AND WAYNE HOUSE<br />
FINLEY were honored with the Lifetime Achievement<br />
Award <strong>at</strong> the Health Care Heroes Awards<br />
Luncheon on Nov. 4, 2003 <strong>at</strong> The Club in<br />
<strong>Birmingham</strong>. They worked together for more than<br />
35 years as geneticists and established the first medical<br />
genetics program in the southeastern United<br />
St<strong>at</strong>es <strong>at</strong> the UASOM in 1962. The Finleys’ program<br />
was one <strong>of</strong> the first to be accredited by the<br />
American Board <strong>of</strong> Medical Genetics in the early<br />
1980s. Since retiring, they have continued <strong>at</strong> UAB<br />
as pr<strong>of</strong>essors emeriti and each serves on numerous<br />
advisory boards and committees. Sara also was<br />
nomin<strong>at</strong>ed by represent<strong>at</strong>ive Spencer Bachus <strong>at</strong> the<br />
American Medical Women’s Associ<strong>at</strong>ion’s (AMWA)<br />
Vision and Voice <strong>of</strong> Women in Medicine banquet.<br />
Changing the Face <strong>of</strong> Medicine: Local Legends, a collabor<strong>at</strong>ion<br />
between AMWA and the N<strong>at</strong>ional<br />
Library <strong>of</strong> Medicine, was cre<strong>at</strong>ed in an effort to<br />
highlight the contribution <strong>of</strong> women physicians<br />
around the country. Members <strong>of</strong> Congress were<br />
invited to nomin<strong>at</strong>e women physicians from their<br />
st<strong>at</strong>e who have made a significant impact in the field<br />
<strong>of</strong> medicine.<br />
1961<br />
FLEMON CARDEN JOHNSTON JR. became<br />
president <strong>of</strong> the American Academy <strong>of</strong> Pedi<strong>at</strong>rics<br />
(AAP) <strong>at</strong> the 2003 AAP N<strong>at</strong>ional Conference and<br />
Exhibition in New Orleans on November 3. He has<br />
served as the president <strong>of</strong> the <strong>Alabama</strong> chapter <strong>of</strong><br />
the AAP, chair <strong>of</strong> the AAP’s Annual Chapter Forum<br />
Committee, chair <strong>of</strong> the AAP Section on Pedi<strong>at</strong>ric<br />
Emergency Medicine, and member <strong>of</strong> the AAP<br />
board <strong>of</strong> directors. He has also served as president <strong>of</strong><br />
the Jefferson County Medical Society and the<br />
Council <strong>of</strong> Medical Specialty Societies. Johnston<br />
has contributed more than 600 health segments for<br />
the television news program Kids M.D., seen on<br />
more than 40 st<strong>at</strong>ions. He lives in <strong>Birmingham</strong> and<br />
currently practices emergency medicine <strong>at</strong><br />
Children’s Hospital.<br />
1964<br />
WILLIAM E. DISMUKES has been named<br />
Laure<strong>at</strong>e <strong>of</strong> the <strong>Alabama</strong> Chapter <strong>of</strong> the American<br />
College <strong>of</strong> Physicians (ACP). This high honor recognizes<br />
senior physicians with “acknowledged excellence<br />
and peer approval in the field <strong>of</strong> internal medicine.”<br />
Dismukes received the award in recognition<br />
<strong>of</strong> his exceptional career as a clinical educ<strong>at</strong>or and<br />
investig<strong>at</strong>or. He has been a fellow <strong>of</strong> the ACP since<br />
1972, a master <strong>of</strong> the college since 1996, a governor<br />
<strong>of</strong> the <strong>Alabama</strong> chapter <strong>of</strong> the ACP-ASIM from<br />
1999–2003, a member <strong>of</strong> the Executive Committee<br />
<strong>of</strong> the ACP-ASIM Board <strong>of</strong> Governors, and a member<br />
<strong>of</strong> the Board <strong>of</strong> Trustees ACP Found<strong>at</strong>ion. He<br />
has been with the UAB faculty for 33 years, is pr<strong>of</strong>essor<br />
<strong>of</strong> medicine and microbiology and vice chair<br />
<strong>of</strong> the Department <strong>of</strong> Medicine, and was selected as<br />
one <strong>of</strong> the Top Ten Teachers in th<strong>at</strong> department from<br />
1995 to 2002. He also served as director <strong>of</strong> the clerkship<br />
in medicine from 1972 to 1981 and was director<br />
<strong>of</strong> the Department <strong>of</strong> Medicine’s residency training<br />
program from 1981 to 2002. Dismukes lives in<br />
<strong>Birmingham</strong> and specializes in infectious diseases.<br />
1970<br />
RICHARD C. DALE has been recognized by the<br />
<strong>Alabama</strong> Quality Assurance Found<strong>at</strong>ion as one <strong>of</strong><br />
<strong>Alabama</strong>’s outstanding Medicare providers for<br />
p<strong>at</strong>ients receiving mammograms. To achieve this<br />
recognition, claims d<strong>at</strong>a from the Centers for<br />
Medicare and Medicaid Services had to suggest th<strong>at</strong><br />
90 percent or more <strong>of</strong> the female Medicare p<strong>at</strong>ients<br />
seen by Dale between July 1999 and June 2001 had<br />
<strong>at</strong> least one mammogram. He is one <strong>of</strong> only 117<br />
physicians in <strong>Alabama</strong> to be recognized for this<br />
mammography indic<strong>at</strong>or, which is identified by<br />
expert panels as a health-care issue critical to the<br />
care <strong>of</strong> female p<strong>at</strong>ients. Dale lives in <strong>Birmingham</strong><br />
and specializes in internal medicine.<br />
26<br />
1972<br />
PINK L. FOLMAR JR. has been named Laure<strong>at</strong>e<br />
<strong>of</strong> the <strong>Alabama</strong> Chapter <strong>of</strong> the American College <strong>of</strong><br />
Physicians. This high honor recognizes senior physicians<br />
with “acknowledged excellence and peer<br />
approval in the field <strong>of</strong> internal medicine.” Folmar<br />
received the award in recognition <strong>of</strong> extensive service<br />
to organized medicine in the st<strong>at</strong>e. He has practiced<br />
internal medicine <strong>at</strong> the Simon-Williamson<br />
Clinic in <strong>Birmingham</strong> for 27 years. Folmar was<br />
president <strong>of</strong> the 35-physician clinic from<br />
1986–1989 and is a member <strong>of</strong> Baptist Princeton<br />
Medical Center’s teaching faculty, where he currently<br />
serves on the Baptist Regional Board <strong>of</strong> Trustees.<br />
He has been a member <strong>of</strong> the School <strong>of</strong> Medicine<br />
Dean’s Advisory Council, president <strong>of</strong> the Medical<br />
Associ<strong>at</strong>ion <strong>of</strong> the St<strong>at</strong>e <strong>of</strong> <strong>Alabama</strong> (MASA), a<br />
MASA and Jefferson County Medical Society<br />
(JCMS) Board <strong>of</strong> Censors member, JCMS president,<br />
and chair <strong>of</strong> the county Board <strong>of</strong> Health.<br />
Folmar lives in <strong>Birmingham</strong> and specializes in internal<br />
medicine.<br />
1973<br />
THOMAS F. DODSON is currently serving a second<br />
year as secretary-treasurer <strong>of</strong> the Georgia Surgical<br />
Society. He was selected to the steering committee <strong>of</strong><br />
the Eastern Surgical Society in 2003 and selected by<br />
his peers to be included in Best Docs in America for<br />
2003-2004. He continues as program director and<br />
vice chair for educ<strong>at</strong>ion in the Department <strong>of</strong><br />
Surgery <strong>at</strong> Emory <strong>University</strong>. Dodson lives in<br />
Atlanta, Georgia, and specializes in vascular surgery.<br />
1973<br />
ROBERT EDWARD MORRIS was appointed as<br />
chief <strong>of</strong> staff <strong>of</strong> Callahan Eye Found<strong>at</strong>ion Hospital<br />
by the board <strong>of</strong> directors <strong>of</strong> The Eye Found<strong>at</strong>ion,<br />
Inc. He assumed his duties in April 2003 and is the<br />
first chief <strong>of</strong> staff for the hospital, which joined the<br />
UAB Health System in July 1997. Morris is an<br />
associ<strong>at</strong>e pr<strong>of</strong>essor in the Department <strong>of</strong><br />
Ophthalmology, the immedi<strong>at</strong>e past president <strong>of</strong><br />
the CEFH Medical Staff, president <strong>of</strong> the Helen<br />
Keller Found<strong>at</strong>ion for Research and Educ<strong>at</strong>ion,<br />
president <strong>of</strong> the Intern<strong>at</strong>ional Society for Ocular<br />
Trauma, and a member <strong>of</strong> the board <strong>of</strong> directors for<br />
the United St<strong>at</strong>es Eye Injury Registry. He lives in<br />
<strong>Birmingham</strong>.<br />
1973<br />
EDWARD E. PARTRIDGE has stepped down as the<br />
director <strong>of</strong> the Division <strong>of</strong> Gynecologic Oncology<br />
after 13 years to devote more time to communitybased<br />
research and service, particularly ongoing programs<br />
for the underserved in cancer care, prevention,<br />
and control. He will continue to see p<strong>at</strong>ients and<br />
continue as vice chair <strong>of</strong> UAB’s Department <strong>of</strong><br />
Obstetrics and Gynecology, and associ<strong>at</strong>e director<br />
for cancer prevention and control in the UAB<br />
Comprehensive Cancer Center. He lives in<br />
<strong>Birmingham</strong> and specializes in gynecologic oncology.<br />
1974<br />
GEORGE MARSHALL ADAMS retired March<br />
31, 2004, after 30 years <strong>of</strong> family practice to enjoy<br />
Italy and various avoc<strong>at</strong>ions and diversions. He lives<br />
in Tampa, Florida.<br />
1978<br />
MELINDA G. ROWE accepted the position <strong>of</strong><br />
commissioner <strong>of</strong> health for the Lexington-Fayette<br />
County Health Department in Lexington, Kentucky,<br />
on Nov. 1, 2003. She has served as health director
<strong>of</strong> the East Health District in Savannah, Georgia,<br />
for the past two years and was previously the director<br />
<strong>of</strong> health for the Louisville/Jefferson County<br />
Health Department in Louisville, Kentucky, from<br />
1995 to 2001. Rowe specializes in pedi<strong>at</strong>rics and<br />
public health.<br />
1979<br />
MICHAEL PAUL PRUITT was recently elected<br />
vice president <strong>of</strong> the Jacksonville Psychi<strong>at</strong>ric<br />
Society. He lives in Neptune Beach, Florida, and<br />
specializes in psychi<strong>at</strong>ry.<br />
1980<br />
LEIGH FINCHER gradu<strong>at</strong>ed from the <strong>University</strong><br />
<strong>of</strong> Arkansas School <strong>of</strong> Law, magna cum laude, J.D.,<br />
in June 2003, and was awarded a health-law scholarship.<br />
Her interest is in health-care policy as it<br />
affects the doctor-p<strong>at</strong>ient rel<strong>at</strong>ionship. She lives in<br />
Fayetteville, Arkansas, and specialized in emergency<br />
medicine.<br />
1987 (Resident) 1988 (Fellow)<br />
RONALD D. ALVAREZ has succeeded Edward<br />
E. Partridge, M.D. (class <strong>of</strong> 1973), as director <strong>of</strong><br />
the Division <strong>of</strong> Gynecologic Oncology in UAB’s<br />
Department <strong>of</strong> Obstetrics and Gynecology. Alvarez<br />
lives in <strong>Birmingham</strong> and specializes in OB/GYN.<br />
1993<br />
RICHARD “CLARK” CROSS was appointed as<br />
assistant pr<strong>of</strong>essor in UAB’s Department <strong>of</strong><br />
Anesthesiology by Alfred Habeeb Pr<strong>of</strong>essor and Chair<br />
David H. Chestnut (class <strong>of</strong> 1978). Cross is a diplom<strong>at</strong>e<br />
<strong>of</strong> the N<strong>at</strong>ional Board <strong>of</strong> Medical Examiners<br />
and the American Board <strong>of</strong> Anesthesiology. He lives<br />
in <strong>Birmingham</strong> and specializes in anesthesiology.<br />
1993<br />
LETA LOU HERRING was recently appointed as<br />
assistant pr<strong>of</strong>essor in Prime Care by Nancy F.<br />
Dunlap, M.D., Ph.D., chief <strong>of</strong> staff <strong>of</strong> The Kirklin<br />
Clinic and medical director <strong>of</strong> TKC Primary Care<br />
Services and Clinics. Herring is board-certified in<br />
internal medicine and advanced cardiac, pedi<strong>at</strong>ric,<br />
and trauma life support. She is a resident <strong>of</strong><br />
<strong>Birmingham</strong> and specializes in internal medicine.<br />
1993<br />
JENNIFER R. ROOT has been South Carolina’s<br />
deleg<strong>at</strong>e to the American Medical Associ<strong>at</strong>ion<br />
Young Physicians Section (AMA-YPS) for the past<br />
two years and was elected this past summer to the<br />
board <strong>of</strong> trustees <strong>of</strong> the South Carolina Medical<br />
Associ<strong>at</strong>ion. She recently <strong>at</strong>tended the annual<br />
meeting <strong>of</strong> the American Society <strong>of</strong> Anesthesiologists<br />
as a deleg<strong>at</strong>e from South Carolina. She resides in<br />
Columbia, South Carolina, and specializes in<br />
anesthesiology.<br />
1995<br />
STEVEN PRESLEY is on the faculty <strong>at</strong> Baptist<br />
Health System in the Internal Medicine and<br />
Transitional Year Residency Program. He lives in<br />
<strong>Birmingham</strong> and has a small primary-care practice in<br />
addition to his faculty and teaching responsibilities.<br />
1995 (Resident)<br />
JEFFREY D. KERBY was appointed as associ<strong>at</strong>e<br />
pr<strong>of</strong>essor in UAB’s Department <strong>of</strong> Surgery in July<br />
2003 by Kirby I. Bland, M.D., pr<strong>of</strong>essor and chair <strong>of</strong><br />
the department; and Loring W. Rue III, M.D., pr<strong>of</strong>essor<br />
and chief <strong>of</strong> the section <strong>of</strong> Trauma/Burns and<br />
Surgical Critical Care. Kerby was appointed chief resident<br />
during his residency, completed a research fellowship<br />
<strong>at</strong> UAB, and was awarded a Ph.D. in biochemistry<br />
and molecular genetics. A lieutenant<br />
colonel in the U.S. Air Force, he provided direct surgical<br />
support to U.S. forces during Oper<strong>at</strong>ion<br />
Enduring Freedom, for which he was awarded the<br />
Air Force Joint Service Achievement Medal.<br />
1996<br />
LAWRENCE S. “LANCE” PRINCE was recently<br />
appointed as assistant pr<strong>of</strong>essor in UAB’s Department<br />
<strong>of</strong> Pedi<strong>at</strong>rics by Sergio Stagno, M.D., pr<strong>of</strong>essor and<br />
department chair. Prince is a resident <strong>of</strong> Vestavia<br />
Hills, <strong>Alabama</strong>, and specializes in pedi<strong>at</strong>rics.<br />
1997<br />
RANDALL SCOTT DAVIS was recently appointed<br />
as assistant pr<strong>of</strong>essor <strong>of</strong> medicine with a secondary<br />
appointment in the Division <strong>of</strong> Hem<strong>at</strong>ology<br />
and Oncology by Max D. Cooper, M.D., pr<strong>of</strong>essor<br />
and director <strong>of</strong> Development and Clinical<br />
Immunology. Davis was the recipient <strong>of</strong> the<br />
UASOM Walter B. Frommeyer Jr. Fellowship in<br />
Investig<strong>at</strong>ive Medicine Physician Scientist Award<br />
in 2000; he was honored with the J. Claude<br />
Bennett Award for Excellence in Research in 2001<br />
and 2002. Also in 2002, he received the UAB<br />
Division <strong>of</strong> Hem<strong>at</strong>ology/Oncology Award for Best<br />
Research Fellow. He is a resident <strong>of</strong> <strong>Birmingham</strong><br />
and specializes in internal medicine.<br />
1998<br />
SARAH MARIE BOYCE was recently appointed<br />
as assistant pr<strong>of</strong>essor in UAB’s Department <strong>of</strong><br />
Derm<strong>at</strong>ology and director <strong>of</strong> cosmetic derm<strong>at</strong>ologic<br />
surgery by Pr<strong>of</strong>essor and Chair Craig A. Elmets,<br />
27<br />
M.D. Boyce gradu<strong>at</strong>ed cum laude from the<br />
UASOM and received the Samuel Clements Little<br />
Neurology Award. She was the recipient <strong>of</strong> a fouryear<br />
Missouri Delta Medical Center scholarship, a<br />
Russell Medical scholarship, and a Southern<br />
Medical Associ<strong>at</strong>ion scholarship. She is a resident<br />
<strong>of</strong> <strong>Birmingham</strong> and specializes in derm<strong>at</strong>ology.<br />
1999<br />
REBECCA W. MILLER was appointed as assistant<br />
pr<strong>of</strong>essor <strong>of</strong> medicine by Pr<strong>of</strong>essor Robert M.<br />
Centor, M.D., director <strong>of</strong> the Division <strong>of</strong> General<br />
Internal Medicine and associ<strong>at</strong>e dean for Primary<br />
Care. Miller lives in <strong>Birmingham</strong> and specializes in<br />
internal medicine.<br />
1999<br />
DIAMOND VROCHER III was appointed assistant<br />
pr<strong>of</strong>essor <strong>of</strong> medicine by Thomas Terndrup,<br />
M.D., chair <strong>of</strong> UAB’s Department <strong>of</strong> Emergency<br />
Medicine. Vrocher received the Dean’s Award for<br />
Medical Student Excellence in Emergency<br />
Medicine, presented by the Society for Academic<br />
Emergency Medicine, in 1999. His clinical interests<br />
center on acute tre<strong>at</strong>ment <strong>of</strong> stroke and hypertension<br />
in emergency p<strong>at</strong>ients, and his current research<br />
focuses on emergency management <strong>of</strong> neurovascular<br />
emergencies. He lives in <strong>Birmingham</strong>.<br />
2001/2003<br />
PEILY SOONG AND AMANDA L. DUNCAN<br />
were married in May 2003. Amanda (class <strong>of</strong><br />
2003) is currently a pedi<strong>at</strong>rics resident <strong>at</strong> UAB.<br />
Peily (class <strong>of</strong> 2001) will be practicing <strong>at</strong> Pedi<strong>at</strong>rics<br />
East after he completes his pedi<strong>at</strong>ric residency<br />
training <strong>at</strong> UAB.<br />
CORRECTION<br />
JON D. HOLMES, class <strong>of</strong> 1997, specializes in<br />
oral and maxill<strong>of</strong>acial surgery.
Alumni Associ<strong>at</strong>ion News<br />
ALUM BABES<br />
LAURA NORELL, class <strong>of</strong> 1991, announces the birth <strong>of</strong> her second<br />
daughter, Alice, born Nov. 12, 2003. Alice joins her sister, Eva, who is<br />
two-and-a-half years old. Norrell is the medical director <strong>of</strong> St. Luke’s<br />
Women’s Center and department chair <strong>of</strong> OB/GYN <strong>at</strong> St. Luke’s Hospital<br />
in San Francisco, California.<br />
JOHN DAVID WHEELER II, class <strong>of</strong> 1992, and his wife, Alison,<br />
announce the birth <strong>of</strong> twins Anna Wallace Wheeler and John David<br />
Wheeler III on Dec. 9, 2003. John specializes in obstetrics and gynecology<br />
in Huntsville, <strong>Alabama</strong>.<br />
JENNIFER R. ROOT, class <strong>of</strong> 1993, and husband Forest Evans Jr.,<br />
M.D., announce the birth <strong>of</strong> their first child, a baby boy; Finley Lloyd<br />
Evans was born Jan. 14, 2004. Jennifer specializes in anesthesiology and<br />
lives in Columbia, South Carolina.<br />
V. SEENU REDDY, class <strong>of</strong> 1995, and wife Meera announce the birth <strong>of</strong><br />
their first child, Amelia K<strong>at</strong>heryn, born Sept. 21, 2003. Reddy recently<br />
became board-certified in general surgery and is a senior fellow in the<br />
Department <strong>of</strong> Cardiothoracic Surgery <strong>at</strong> Emory <strong>University</strong>. He lives in<br />
Dec<strong>at</strong>ur, Georgia, and specializes in cardiothoracic surgery.<br />
FRANK SCHEFANO III, class <strong>of</strong> 1998, and his wife, Mary Dell,<br />
announce the birth <strong>of</strong> their daughter, Abby Della Schefano, born Sept.<br />
12, 2003. She joins her sister, Anna Maria Schefano, who is seven. Frank<br />
is the director <strong>of</strong> the Department <strong>of</strong> Anesthesiology <strong>at</strong> Arkansas Methodist<br />
Medical Center in Paragould, Arkansas.<br />
LESLIE HARRIS JR., class <strong>of</strong> 1999, and wife K<strong>at</strong>rina announce the birth<br />
<strong>of</strong> their son Nicholas Harris, born Dec. 25, 2003. He joins sister Nyla<br />
Harris, born Feb. 26, 2001. Leslie is currently clinical instructor <strong>of</strong> medicine<br />
and director <strong>of</strong> the Ambul<strong>at</strong>ory Care Clinic <strong>at</strong> the UAB Montgomery<br />
Internal Medicine Residency Program. He lives in Montgomery, <strong>Alabama</strong>.<br />
ANGELA H. REDMOND, class <strong>of</strong> 1999, and her husband, John, announce<br />
the birth <strong>of</strong> their son Alex Michael Redmond, born Jan. 16, 2004. Angela<br />
specializes in pedi<strong>at</strong>rics, and she lives in Cullman, <strong>Alabama</strong>.<br />
JOANNE CHEN MYERS, class <strong>of</strong> 2000, and her husband, Warren,<br />
announce the birth <strong>of</strong> daughter Hayden Elizabeth Myers, born Jan. 24,<br />
2004. Joanne joined OB/GYN <strong>of</strong> West <strong>Alabama</strong> in Tuscaloosa this June.<br />
LISA J. RUSCHAK, class <strong>of</strong> 2000, and her husband, Scott, announce<br />
the birth <strong>of</strong> their son Zachary Joseph Ruschak, born Feb. 17, 2004. Lisa<br />
specializes in family practice and lives in Greeley, Colorado.<br />
ELIZABETH (BETH) TURNER FALKENBERG, class <strong>of</strong> 2000, and her<br />
husband, Mark, announce the birth <strong>of</strong> their son, Luke William<br />
Falkenberg, born March 16, 2004. Beth lives in <strong>Birmingham</strong> and specializes<br />
in radi<strong>at</strong>ion oncology.<br />
IN MEMORIAM<br />
CLYDE DAVIS MCLALLEN, 1943 gradu<strong>at</strong>e <strong>of</strong> the two-year school, died<br />
Jan. 5, 2004. A n<strong>at</strong>ive <strong>of</strong> Anniston, <strong>Alabama</strong>, he moved to <strong>Birmingham</strong>,<br />
where he specialized in internal medicine.<br />
JAMES MACON BURNETT, class <strong>of</strong> 1946, died Jan. 7, 2004. He<br />
served in the U.S. Army from 1943 until 1946 and in the U.S. Air Force<br />
from 1951 to 1952. He lived in <strong>Birmingham</strong> and had a family practice<br />
until his retirement in 1988.<br />
LAMAR MCWHORTER CAMPBELL, class <strong>of</strong> 1955, died Jan. 26,<br />
2004. He was a member <strong>of</strong> the Jefferson County Medical Society, the<br />
<strong>Alabama</strong> Medical Associ<strong>at</strong>ion, the American Medical Associ<strong>at</strong>ion, and the<br />
<strong>Birmingham</strong> Surgical Society. He was a diplom<strong>at</strong>e <strong>of</strong> the American Board<br />
<strong>of</strong> Ophthalmology with certific<strong>at</strong>ion in 1963, a past president <strong>of</strong> the<br />
<strong>Birmingham</strong> Clinical Club, an instructor <strong>at</strong> the <strong>University</strong> <strong>of</strong> <strong>Alabama</strong>,<br />
and a chief <strong>of</strong> the Division <strong>of</strong> Ophthalmology <strong>at</strong> the Baptist Medical<br />
Center. He lived in Ashville, <strong>Alabama</strong>, and specialized in ophthalmology.<br />
WILLIAM SAMUEL MITCHELL, class <strong>of</strong> 1955, died Feb. 15, 2004. He<br />
was a general practitioner for 42 years and lived in Calera, <strong>Alabama</strong>.<br />
CHARLES HAROLD SMITH, class <strong>of</strong> 1955, died June 28, 2003. He<br />
lived in Montgomery, <strong>Alabama</strong>, and specialized in psychi<strong>at</strong>ry.<br />
ANDREW JACKSON GAY JR., class <strong>of</strong> 1955, died on Jan. 18, 2004.<br />
He lived in Belfast, Maine, and specialized in ophthalmology.<br />
OLIVER CHARLES MITCHELL, class <strong>of</strong> 1959, died Oct. 31, 2003. He<br />
lived in Houston, Texas, and specialized in neurological surgery.<br />
WILLIAM “BILL” LLOYD MITCHELL, class <strong>of</strong> 1963, died in June<br />
2003. He was a fellow <strong>of</strong> the American College <strong>of</strong> Obstetricians and<br />
Gynecologists. Mitchell resided and practiced OB/GYN in Enterprise,<br />
<strong>Alabama</strong>, for 35 years. He also was a genealogist, computer programmer,<br />
historian, pilot, and accomplished artist.<br />
RICHARD DAVIS “DICK” HARP, class <strong>of</strong> 1964, died Dec. 30, 2003, in<br />
Panama City, Florida. A n<strong>at</strong>ive <strong>of</strong> <strong>Birmingham</strong>, he was a member <strong>of</strong><br />
numerous organiz<strong>at</strong>ions, including the Medical Associ<strong>at</strong>ion <strong>of</strong> the St<strong>at</strong>e <strong>of</strong><br />
<strong>Alabama</strong>, the American Medical Associ<strong>at</strong>ion, the American College <strong>of</strong><br />
Radiology, and the American Academy <strong>of</strong> Radiology. He served on the<br />
board <strong>of</strong> trustees for Walker Baptist Medical Center in Jasper, <strong>Alabama</strong>; as<br />
president <strong>of</strong> the UASOM from 1983–84; and as founder and senior partner<br />
<strong>of</strong> Radiology Associ<strong>at</strong>es <strong>of</strong> North <strong>Alabama</strong>, P.C. He was a recipient <strong>of</strong><br />
the Paul Harris Fellow Award from Rotary Intern<strong>at</strong>ional for outstanding<br />
achievement and community service. He specialized in radiology.<br />
JAMES EUGENE THOMAS, class <strong>of</strong> 1976, died Dec. 15, 2003. Born<br />
in <strong>Birmingham</strong>, Thomas moved to Troy, <strong>Alabama</strong>, where he opened a<br />
medical practice in 1979. He retired in 2002.<br />
28
Alumni Associ<strong>at</strong>ion News<br />
N<strong>at</strong>ion’s Pedi<strong>at</strong>ricians Select<br />
UASOM Alumnus as New Leader<br />
The n<strong>at</strong>ion’s pedi<strong>at</strong>ricians have chosen a new leader, and he’s one <strong>of</strong><br />
our own. Carden Johnston, M.D., FAAP, was elected as the vice president<br />
<strong>of</strong> the American Academy <strong>of</strong> Pedi<strong>at</strong>rics (AAP) <strong>at</strong> the organiz<strong>at</strong>ion’s<br />
annual meeting in June 2002. He took <strong>of</strong>fice as the president-elect in<br />
October 2002 and recently began serving as president for 2003–2004.<br />
The AAP is the n<strong>at</strong>ion’s largest pedi<strong>at</strong>ric organiz<strong>at</strong>ion, with more<br />
than 58,000 primary care pedi<strong>at</strong>ricians, pedi<strong>at</strong>ric medical specialists,<br />
and pedi<strong>at</strong>ric surgical specialists.<br />
In taking the <strong>of</strong>fice <strong>of</strong> president, Johnston has identified two issues he<br />
believes are essential to securing optimal child health and well being.<br />
“My first priority is financial access to health care for all grandchildren,”<br />
he says. “As a grandparent myself, I know firsthand how important<br />
grandchildren are to their grandparents. To th<strong>at</strong> extent, I believe pedi<strong>at</strong>ricians<br />
and grandparents are n<strong>at</strong>ural allies.” With this in mind, Johnston<br />
plans to work with the AARP on several child-rel<strong>at</strong>ed health projects.<br />
Johnston’s other issue <strong>of</strong> primary importance as he takes <strong>of</strong>fice is<br />
obesity prevention in children. Today’s children are heavier than<br />
ever—a trend th<strong>at</strong> shows no sign <strong>of</strong> slowing down any time soon.<br />
Johnston says, “By tracking body-mass indexes in children, we have an<br />
opportunity for early detection <strong>of</strong> those who are becoming overweight<br />
or obese. Prevention is the cornerstone <strong>of</strong> pedi<strong>at</strong>ric care, and I believe<br />
we can advance our advocacy efforts by exporting obesity-prevention<br />
str<strong>at</strong>egies into our other prevention activities. This is crucial not only<br />
for our children today but also for our adults tomorrow; adult disease,<br />
after all, begins in childhood.”<br />
Johnston currently practices <strong>at</strong> Children’s Hospital and has served as<br />
past president <strong>of</strong> the <strong>Alabama</strong> chapter <strong>of</strong> the AAP, chair <strong>of</strong> their Annual<br />
Chapter Forum Committee, chair <strong>of</strong> their Section on Pedi<strong>at</strong>ric<br />
Emergency Medicine, and a member <strong>of</strong> the AAP Board <strong>of</strong> Directors.<br />
WHY BELONG TO THE MEDICAL<br />
ALUMNI ASSOCIATION?<br />
By Paul S. Howard, M.D.<br />
It was February 1975. I was expecting a letter any day from the<br />
UASOM Admissions Committee. Henry H<strong>of</strong>fman had assured me<br />
th<strong>at</strong> my acceptance was imminent; nonetheless, I was anxious, uncertain,<br />
and frankly scared <strong>of</strong> wh<strong>at</strong> the next four years might entail. I had<br />
no idea wh<strong>at</strong> a doctor-in-training did, nor was I certain th<strong>at</strong> I had<br />
made the correct decision in applying to medical school. Yet even with my personal misgivings,<br />
the notion <strong>of</strong> becoming a doctor made my parents so very proud th<strong>at</strong> I knew it was my destiny.<br />
The next four years would be the most intense and s<strong>at</strong>isfying <strong>of</strong> my young life. Not only did<br />
we all learn to be <strong>doctors</strong>, we were also required to make irrevocable decisions regarding future<br />
training. These decisions shaped our future and were considered without enough inform<strong>at</strong>ion. I<br />
suppose most <strong>of</strong> us chose well. Regardless, we as a group had achieved gre<strong>at</strong>ly. We would then<br />
stumble forward into our careers forever known as the “class <strong>of</strong> 1979.”<br />
I still see, talk with, and enjoy the company <strong>of</strong> many <strong>of</strong> my medical school classm<strong>at</strong>es.<br />
Although we rarely speak <strong>of</strong> it, we are all proud <strong>of</strong> our school. Whenever a UAB doctor is<br />
quoted in the n<strong>at</strong>ional press or UAB is touted as an important place, we all suppress a grin<br />
and find ourselves walking a little taller. Many <strong>of</strong> us remember when today’s famous surgeon<br />
or internist was a young faculty member or even our junior resident. Whether we will<br />
admit it or not, we take collective pride in our medical school, our achievements, and the<br />
achievements <strong>of</strong> all alumni.<br />
The ultim<strong>at</strong>e mission <strong>of</strong> the <strong>Alabama</strong> Medical Alumni Associ<strong>at</strong>ion is to be a voice for its membership.<br />
We remain proud <strong>of</strong> who we are and where we come from. I like to think <strong>of</strong> UAB as an<br />
institution not <strong>of</strong> bricks and mortar but one built on the history <strong>of</strong> its medical alumni. Our collective<br />
memories and experiences are the found<strong>at</strong>ion <strong>of</strong> a gre<strong>at</strong> school. Tinsley, Champ, and<br />
Garber still reside in the clinics, labs, and oper<strong>at</strong>ing rooms where we were cre<strong>at</strong>ed. Their legacy<br />
must be nurtured and protected for the students and residents <strong>of</strong> today. We, the medical alumni,<br />
are the ones to keep the traditions alive; it should be our charge to be the collective memory<br />
<strong>of</strong> those who preceded us. Our mission is to remind the leaders <strong>of</strong> today where we have been and<br />
on whose shoulders we have all ridden.<br />
Is there a better reason to belong to the Medical Alumni Associ<strong>at</strong>ion? I think not.<br />
Alumni, Let Us Hear From You<br />
Please take a few minutes to share with us any personal or pr<strong>of</strong>essional news for<br />
public<strong>at</strong>ion in a future issue <strong>of</strong> the <strong>Alabama</strong> Medical Alumni Bulletin.<br />
Name ______________________________________________ Today’s d<strong>at</strong>e __________ Year gradu<strong>at</strong>ed ________ Specialty _______________________<br />
Home address ________________________________________________________________________________________________________________<br />
Business address ______________________________________________________________________________________________________________<br />
Phone (H) _____________________ (W) ____________________ E-mail _________________________________________ Fax _________________<br />
Spouse’s name ____________________________________ Children (if recent, include d<strong>at</strong>e <strong>of</strong> birth) __________________________________________<br />
Personal/pr<strong>of</strong>essional upd<strong>at</strong>e (List names/d<strong>at</strong>es <strong>of</strong> recent public<strong>at</strong>ions, awards, honors.)<br />
____________________________________________________________________________________________________________________________<br />
____________________________________________________________________________________________________________________________<br />
____________________________________________________________________________________________________________________________<br />
____________________________________________________________________________________________________________________________<br />
Please return this form to: Elaine Chambless - Director <strong>of</strong> Alumni Affairs<br />
The <strong>University</strong> <strong>of</strong> <strong>Alabama</strong> Medical Alumni Associ<strong>at</strong>ion - MAB • 811 20th Street South • 1530 3RD AVE S • BIRMINGHAM AL 35294-2140<br />
29
Alumni Pr<strong>of</strong>ile<br />
Alumni Pr<strong>of</strong>ile: The Schmitt Family, M.D.s<br />
By Sandra Bearden<br />
medicine. “But a lot <strong>of</strong> his golfing buddies were<br />
<strong>doctors</strong>, and several took an interest in my future<br />
career,” Kim says. “One <strong>of</strong> them gave me discarded<br />
medical journals to read when I was only 12 or<br />
13. I didn’t know wh<strong>at</strong> the heck I was looking <strong>at</strong>,<br />
but the gesture was encouraging. Another friend<br />
<strong>of</strong> my dad’s arranged for me to go into an oper<strong>at</strong>ing<br />
room to observe surgery when I was in high<br />
school. Th<strong>at</strong> was a gre<strong>at</strong> experience for me.”<br />
“My parents were<br />
gre<strong>at</strong> believers in<br />
educ<strong>at</strong>ion as a key to<br />
prepar<strong>at</strong>ion for life.”<br />
— Kim Schmitt<br />
Kim and Lee Schmitt.<br />
If Kim Schmitt had chosen tap-dancing, would her younger<br />
brothers have followed in her footsteps as fledgling Fred Astaires?<br />
The world will never know. Kim opted for a medical career,<br />
and th<strong>at</strong> influenced brothers Adam and Lee Schmitt to become<br />
physicians, too. All three are gradu<strong>at</strong>es <strong>of</strong> the <strong>University</strong> <strong>of</strong><br />
<strong>Alabama</strong> in Tuscaloosa and the UASOM. All three—Kim (’81),<br />
Adam (’90), and Lee (’90)—completed residencies <strong>at</strong> <strong>University</strong><br />
Hospital. And all three practice medicine in the <strong>Birmingham</strong> area.<br />
There the similarities end. They’re siblings, but not clones.<br />
Kim Schmitt, M.D., practices otolaryngology as well as head and<br />
neck surgery <strong>at</strong> Medical Center East. Adam Schmitt, M.D., is an<br />
emergency physician <strong>at</strong> Shelby County Medical Center. And Lee<br />
Schmitt, M.D., is a general surgeon <strong>at</strong> Medical Center East.<br />
Although the three all chose medical careers, medicine is a<br />
family business only in their gener<strong>at</strong>ion. As the eldest, Kim led<br />
the other two in th<strong>at</strong> direction.<br />
“As far back as I can remember, I wanted either to be a doctor<br />
or a tap-dancer,” she laughs. “My parents [Vernon Neil Schmitt<br />
<strong>of</strong> Leeds and the l<strong>at</strong>e Jean Schmitt] were gre<strong>at</strong> believers in educ<strong>at</strong>ion<br />
as a key to prepar<strong>at</strong>ion for life. So the tap-dancing idea didn’t<br />
go over very well.<br />
“I knew I was going to have a career, even though I was born<br />
in 1955, when women didn’t prepare for careers. But my mother<br />
was forward-thinking in this regard. And it happened th<strong>at</strong> my<br />
pedi<strong>at</strong>rician was Dr. Vera Stewart. So I had a role model, and in<br />
my early years I thought all <strong>doctors</strong> were female.”<br />
The Schmitts’ f<strong>at</strong>her, who went to college on the GI Bill while<br />
his wife worked to help support the family, practiced law, not<br />
Kim’s enthusiasm for medicine caught hold<br />
with Adam, the middle child, and Lee, the<br />
youngest, both several years younger than she. By<br />
the time they were ready to start thinking <strong>of</strong><br />
careers, she was enrolled <strong>at</strong> the UASOM.<br />
“I think I deliber<strong>at</strong>ely tried to influence Adam,” she says. “Why<br />
one does this, I don’t know. But I really was enthralled with medicine<br />
and thought Adam would be a good doctor. I didn’t try so<br />
hard to influence Lee. I thought he had his mind set on law.”<br />
He did. “I majored in English and was planning to enter law<br />
school,” says Lee Schmitt. “But I used to visit Kim’s Southside<br />
apartment when she was in med school, look <strong>at</strong> her books, and<br />
learn about her work. Somewhere along the way, I switched to premed,<br />
took the required science courses, and entered the UASOM.”<br />
In deciding on a specialty, Lee wanted to “do something th<strong>at</strong><br />
would permit me to work with my hands,” and completed a residency<br />
in general surgery <strong>at</strong> UASOM. Although he still does general<br />
surgery, much <strong>of</strong> his practice in the past year has been in<br />
laparoscopic weight-loss surgery.<br />
Although she also has a clinical practice, Kim Schmitt became<br />
interested in head and neck surgery during her surgical residency,<br />
and also does a good deal <strong>of</strong> nasal and sinus surgery. “It’s delic<strong>at</strong>e<br />
surgery, and having small hands helps,” she says.<br />
Adam Schmitt, like most emergency-department physicians,<br />
keeps a frenetic pace and contributes interesting ED experiences<br />
to the convers<strong>at</strong>ions <strong>at</strong> family get-togethers. “But there’s less shop<br />
talk than you might think,” Lee comments.<br />
While his children chose medicine, Vernon Schmitt may still<br />
have an <strong>at</strong>torney in the family. Lee’s son Payton is still too young<br />
to decide, but Kim’s 16-year-old daughter, Alexandra, an honor<br />
student <strong>at</strong> Altamont School, has set her sights on law school.<br />
30
Alumni Pr<strong>of</strong>ile<br />
Alumni Pr<strong>of</strong>ile: Tracey Miles, M.D.<br />
By Steve Dupont<br />
Tracey Miles admits there are times she questions her career p<strong>at</strong>h.<br />
“Sometimes when I’m still working <strong>at</strong> nine o’clock <strong>at</strong> night, I think, ‘If I were<br />
a radiologist or a p<strong>at</strong>hologist, I’d be home right now,’” she says with a hint <strong>of</strong><br />
irony. But Miles opted to forgo those more lucr<strong>at</strong>ive specialties. Instead she<br />
chose family medicine—and the depth <strong>of</strong> her commitment is in proportion<br />
to the needs <strong>of</strong> her p<strong>at</strong>ients.<br />
Since beginning her post-residency work <strong>at</strong> Tuscaloosa’s Maude Wh<strong>at</strong>ley<br />
Health Center in 1998, Miles has performed a sort <strong>of</strong> clinical balancing act,<br />
weighing tre<strong>at</strong>ment options against economic realities. “I’m very mindful <strong>of</strong><br />
staying abreast <strong>of</strong> the l<strong>at</strong>est tre<strong>at</strong>ments,” she says. “But usually it’s a m<strong>at</strong>ter <strong>of</strong><br />
wh<strong>at</strong> my p<strong>at</strong>ients can afford.” And in many cases, th<strong>at</strong>’s not much. Upwards<br />
<strong>of</strong> half her p<strong>at</strong>ients lack health insurance, and many live on fixed incomes. A<br />
case in point is the victim <strong>of</strong> two strokes who faced a decision between buying<br />
aspirin or food. Needless to say, he chose the l<strong>at</strong>ter—and, as a result,<br />
increased his risk <strong>of</strong> suffering another stroke.<br />
Having grown up in Fort Mitchell, <strong>Alabama</strong>, a humble community in its own<br />
right, Miles knows firsthand how difficult it can be to escape the cycle <strong>of</strong> indigence.<br />
“Out <strong>of</strong> all my friends, I was the only one who didn’t get pregnant in high<br />
school,” Miles recalls. “And I was the only one to go to college.” It is an achievement<br />
she <strong>at</strong>tributes to the strong values reinforced <strong>at</strong> home. Despite the fact th<strong>at</strong><br />
neither <strong>of</strong> her parents gradu<strong>at</strong>ed from high school, they were strong believers in<br />
the value <strong>of</strong> educ<strong>at</strong>ion. However, Miles’ own ambition was likely a prevailing<br />
factor as well. After all, when asked when she decided to become a doctor, she<br />
says, “I remember it very clearly. I was<br />
11 years old.” Her inspir<strong>at</strong>ion? A<br />
family pedi<strong>at</strong>rician who tre<strong>at</strong>ed her<br />
numerous times during a year <strong>of</strong> nagging<br />
health problems.<br />
After receiving her high school<br />
diploma, Miles headed to Macon,<br />
Georgia, where she used a full scholarship<br />
to study biology <strong>at</strong> Mercer<br />
<strong>University</strong>. Then it was on to the<br />
UASOM, where she began her medical<br />
training on another generous scholarship,<br />
this one compliments <strong>of</strong> the<br />
N<strong>at</strong>ional Health Service Corps. There<br />
was just one string <strong>at</strong>tached—an oblig<strong>at</strong>ion<br />
to work in an “underserved<br />
community” after gradu<strong>at</strong>ing in 1995.<br />
As it turned out, her residency in<br />
family practice <strong>at</strong> DCH Regional<br />
“I’m very mindful <strong>of</strong><br />
staying abreast <strong>of</strong> the<br />
l<strong>at</strong>est tre<strong>at</strong>ments. But<br />
usually it’s a m<strong>at</strong>ter<br />
<strong>of</strong> wh<strong>at</strong> my p<strong>at</strong>ients<br />
can afford.… Wh<strong>at</strong><br />
keeps me going is<br />
th<strong>at</strong> I really know I’m<br />
making a difference.”<br />
— Tracey Miles<br />
Medical Center in Tuscaloosa would prepare her especially well for the challenge<br />
ahead. Then, as now, she had to combine her medical knowledge with<br />
diplomacy and resourcefulness to help p<strong>at</strong>ients coping with the effects <strong>of</strong> diabetes,<br />
high blood pressure, heart disease, and stroke. “We’re kind <strong>of</strong> in the<br />
‘stroke belt’ here,” Miles says; she believes this is the result <strong>of</strong> cultural and<br />
socioeconomic factors, namely poor diet and lack <strong>of</strong> preventive care. Poor prioritizing<br />
is also a factor for many <strong>of</strong> the p<strong>at</strong>ients she sees on a daily basis. “I<br />
do have some p<strong>at</strong>ients who say they can’t afford care and then pull out their<br />
cell phones,” she notes.<br />
Clearly, Miles’ role in the clinic goes far beyond medicine. On any given day<br />
she’s there for her p<strong>at</strong>ients, not only as a doctor but as a social worker, a nutritionist,<br />
a financial counselor, and, most important, as a friend. “Wh<strong>at</strong> keeps<br />
me going,” Miles says, “is th<strong>at</strong> I really know I’m making a difference.”<br />
31
From the Archives: <strong>Alabama</strong> Healthcare Hall <strong>of</strong> Fame By Tim L. Pennycuff<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> School <strong>of</strong> Medicine alumni,<br />
faculty, and administr<strong>at</strong>ors are fe<strong>at</strong>ured prominently<br />
in the recently installed <strong>Alabama</strong> Healthcare<br />
Hall <strong>of</strong> Fame display on the UAB campus. The display,<br />
unveiled last year in <strong>University</strong> Hospital’s West<br />
Pavilion adjacent to the p<strong>at</strong>ient-discharge area, is<br />
domin<strong>at</strong>ed by a mosaic <strong>of</strong> photographs <strong>of</strong> the<br />
numerous individuals who have been inducted into<br />
the Hall <strong>of</strong> Fame since it was founded in 1997. The<br />
organiz<strong>at</strong>ion honors those who have worked in the<br />
fields <strong>of</strong> medicine, dentistry, nursing, optometry,<br />
pharmacy, public health, and allied health.<br />
Pictures in the display include former UAB presidents<br />
Joseph F. Volker, D.D.S., Ph.D.; S.<br />
Richardson Hill Jr., M.D.; and Charles A.<br />
McCallum Jr., D.M.D., M.D.; and former UASOM<br />
faculty members J. Garber Galbraith, M.D.; Tinsley<br />
R. Harrison, M.D.; Howard L. Holley, M.D.; John<br />
W. Kirklin, M.D.; Roy R. Kracke, M.D.; Champ<br />
Lyons, M.D.; and James S. McLester, M.D. Others<br />
fe<strong>at</strong>ured include alumni and faculty from the<br />
UASOM’s earlier incarn<strong>at</strong>ions—as the Medical<br />
College <strong>of</strong> <strong>Alabama</strong>—in Mobile, Tuscaloosa, and<br />
<strong>Birmingham</strong>. Also included are photographs <strong>of</strong> campus<br />
landmarks such as the Hillman and Jefferson<br />
Hospitals, and scenes <strong>of</strong> clinical, surgical, and labor<strong>at</strong>ory<br />
work <strong>at</strong> various periods over the past decades.<br />
The West Pavilion display could not possibly<br />
accommod<strong>at</strong>e photographs <strong>of</strong> all 76 individuals who<br />
have thus far been inducted into the Hall <strong>of</strong> Fame<br />
but the display does include a complete list <strong>of</strong> each<br />
induction class honored by the organiz<strong>at</strong>ion.<br />
UASOM alumni to be so honored include William<br />
H. Cooner, M.D.; Sara C. Finley, M.D.; Wayne H.<br />
Finley, Ph.D., M.D.; Carl A. Grote Sr., M.D.;<br />
Charles A. LeMaistre, M.D.; Ira L. Myers, M.D.;<br />
and Martha C. Myers, M.D. Also honored are<br />
numerous current and former members <strong>of</strong> the faculty,<br />
including Alston Callahan, M.D.; Jerome<br />
Cochran, M.D.; Max D. Cooper, M.D.; Arnold G.<br />
Diethelm, M.D.; Seale Harris, M.D.; Basil I.<br />
Hirschowitz, M.D.; Sandral Hullett, M.D.; Josiah<br />
C. Nott, M.D.; and James A. Pittman Jr., M.D.<br />
Additional inform<strong>at</strong>ion, including biographical<br />
summaries <strong>of</strong> all inductees and procedures for nomin<strong>at</strong>ion,<br />
can be found on the organiz<strong>at</strong>ion’s Web site<br />
<strong>at</strong> [www.healthcareh<strong>of</strong>.org].<br />
Members <strong>of</strong> the <strong>Alabama</strong> Healthcare Hall <strong>of</strong> Fame<br />
Committee selected all <strong>of</strong> the images in the display.<br />
Of the almost 60 photographs used, more than 80<br />
percent came from UAB Archives, which has a photographic<br />
collection numbering more than 50,000<br />
images. The <strong>of</strong>ficial archival repository for the<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> <strong>at</strong> <strong>Birmingham</strong>, the UAB<br />
Archives collects and preserves m<strong>at</strong>erial about UAB,<br />
its schools, departments, and <strong>of</strong>fices, and its faculty,<br />
staff, and students. The Archives also include m<strong>at</strong>erials<br />
th<strong>at</strong> document the history <strong>of</strong> the health sciences in<br />
<strong>Alabama</strong> and the South, with a considerable amount<br />
<strong>of</strong> historical inform<strong>at</strong>ion about the UASOM, from its<br />
founding in Mobile in 1859 until the present.<br />
(Clockwise from top left) John W. Kirklin, M.D.;<br />
the Healthcare Hall <strong>of</strong> Fame display, loc<strong>at</strong>ed in<br />
<strong>University</strong> Hospital’s West Pavilion; Hillman<br />
Hospital, circa 1905; Buford Word, M.D., S.<br />
Richardson Hill Jr., M.D., and Charles A.<br />
McCallum Jr., D.M.D., M.D., with the instruments<br />
<strong>of</strong> J. Marion Sims <strong>at</strong> their don<strong>at</strong>ion to the<br />
Reynolds Historical Library, 1965; Jefferson<br />
Hospital, circa 1958; James S. McLester, M.D.,<br />
with Hillman Hospital residents and interns,<br />
1933–1934; (left) Tinsley R. Harrison, M.D.;<br />
(right) Roy R. Kracke, M.D.<br />
32
UASOM ANNUAL FUND<br />
“While interviewing for residency positions and touring another<br />
university’s facilities, a fellow applicant observed from my name<br />
tag th<strong>at</strong> I was from UAB. He had visited the campus a few<br />
years earlier. ‘UAB … I was very impressed by the facilities<br />
they had down there,’ he said. ‘Wh<strong>at</strong> a gre<strong>at</strong> hospital!’ I<br />
agreed with him and proceeded to tell him about the new<br />
st<strong>at</strong>e-<strong>of</strong>-the-art hospital being built and the newly<br />
approved Women and Infants Facility. The student was<br />
extremely impressed, as was everyone I met on the interview<br />
trail who had contact with UAB or a UASOMtrained<br />
physician.<br />
“These experiences impacted my decision about where to do<br />
my residency. Why leave such a good thing? My classm<strong>at</strong>es have<br />
faced a similar scenario. Many <strong>of</strong> us will be here next year, because<br />
the UASOM is the most impressive institution we have seen, and<br />
it is only getting better.”<br />
JAMIE WORTHEN<br />
MS-IV Class <strong>of</strong> 2004 President<br />
Every dollar you give to the <strong>University</strong> <strong>of</strong> <strong>Alabama</strong> School <strong>of</strong> Medicine<br />
Annual Fund helps the school educ<strong>at</strong>e the next gener<strong>at</strong>ion <strong>of</strong> physicians.<br />
Make an investment th<strong>at</strong> will last for gener<strong>at</strong>ions.<br />
Your gift, regardless <strong>of</strong> the amount, will make a difference. Please<br />
take the time now to write a check payable to the School <strong>of</strong> Medicine<br />
Annual Fund and return it in the <strong>at</strong>tached envelope. All gifts are<br />
tax-deductible.<br />
For online gifts, go to [www.uab.edu/supportmedicine].<br />
For more inform<strong>at</strong>ion, contact Meredith Murdock <strong>at</strong> (205) 934-4469.
CONTINUING MEDICAL EDUCATION SCHEDULE<br />
This is a sampling <strong>of</strong> the dozens <strong>of</strong> live and online CME courses scheduled for the next several months. For a complete<br />
listing, contact the UASOM Division <strong>of</strong> Continuing Medical Educ<strong>at</strong>ion <strong>at</strong> (205) 934-2687 or (800) UAB-MIST, or visit their<br />
Web site <strong>at</strong> [www-cme.erep.uab.edu/home.asp].<br />
Live CME Courses<br />
August 2-7, 2004<br />
“24th N<strong>at</strong>ional Symposium for Healthcare Executives”; sponsored<br />
by the Division <strong>of</strong> Continuing Medical Educ<strong>at</strong>ion and the Center<br />
for Health Services Administr<strong>at</strong>ion; 24.5 CME credits.<br />
August 5-8, 2004<br />
“Southeast Trauma Symposium”; sponsored by the Division <strong>of</strong><br />
Continuing Medical Educ<strong>at</strong>ion and supported by an unrestricted<br />
educ<strong>at</strong>ional grant from Smith & Nephew; 17 CME credits.<br />
October 11, 2004<br />
“UAB Emergency Medicine Program”; sponsored by the Division<br />
<strong>of</strong> Continuing Medical Educ<strong>at</strong>ion and the UAB Department <strong>of</strong><br />
Emergency Medicine; supported by unrestricted educ<strong>at</strong>ional<br />
grants from Aventis, BMS, Elan, GlaxoSmithKline, Guilford,<br />
Millenium, Pfizer, and Ortho McNeil; 3 CME credits.<br />
October 17, 2004<br />
“SMDM 26th Annual Meeting: Public Health Decision Making”;<br />
sponsored by the Division <strong>of</strong> Continuing Medical Educ<strong>at</strong>ion and<br />
the Society for Medical Decision Making; 22.5 CME credits.<br />
Online CME Courses<br />
“Diabetic Complic<strong>at</strong>ions in the Elderly”; sponsored by the<br />
Division <strong>of</strong> Continuing Medical Educ<strong>at</strong>ion; 1 CME credit.<br />
“Highlights in Hyperlipidemia Tre<strong>at</strong>ment”; sponsored by the<br />
Division <strong>of</strong> Continuing Medical Educ<strong>at</strong>ion; 1 CME credit.<br />
“Evalu<strong>at</strong>ing a Clinical Approach to West Nile Virus”; sponsored by<br />
the Division <strong>of</strong> Continuing Medical Educ<strong>at</strong>ion; 0.25 CME credit.<br />
AlumniBulletin<br />
ALABAMA MEDICAL<br />
AlumniBulletin<br />
<strong>University</strong> <strong>of</strong> <strong>Alabama</strong> Medical Alumni Associ<strong>at</strong>ion<br />
MAB • 811 20th Street South<br />
1530 3RD AVE S<br />
BIRMINGHAM AL 35294-2140<br />
Non-Pr<strong>of</strong>it Org.<br />
U.S. Postage<br />
PAID<br />
Permit No. 1256<br />
<strong>Birmingham</strong>, AL