Concordia PPO Benefit Summary - United Concordia
Concordia PPO Benefit Summary - United Concordia
Concordia PPO Benefit Summary - United Concordia
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
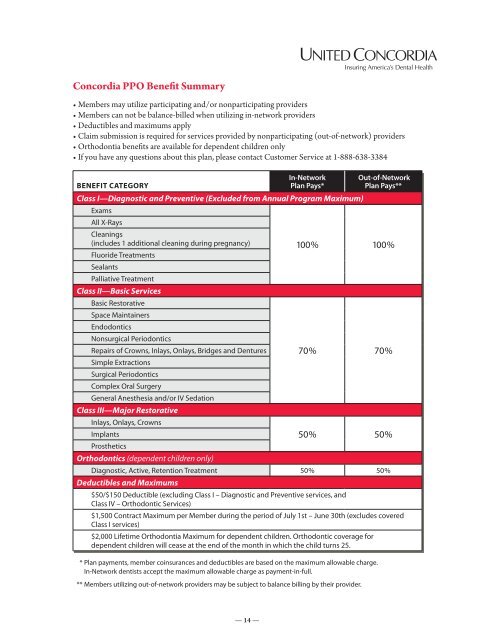
<strong>Concordia</strong> <strong>PPO</strong> <strong>Benefit</strong> <strong>Summary</strong><br />
• Members may utilize participating and/or nonparticipating providers<br />
• Members can not be balance-billed when utilizing in-network providers<br />
• Deductibles and maximums apply<br />
• Claim submission is required for services provided by nonparticipating (out-of-network) providers<br />
• Orthodontia benefits are available for dependent children only<br />
• If you have any questions about this plan, please contact Customer Service at 1-888-638-3384<br />
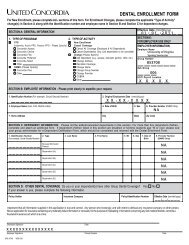
<strong>Benefit</strong> Category<br />
In-Network<br />
Plan Pays*<br />
Class I—Diagnostic and Preventive (Excluded from Annual Program Maximum)<br />
Exams<br />
All X-Rays<br />
Cleanings<br />
(includes 1 additional cleaning during pregnancy)<br />
Fluoride Treatments<br />
Sealants<br />
Palliative Treatment<br />
Class II—Basic Services<br />
Basic Restorative<br />
Space Maintainers<br />
Endodontics<br />
Nonsurgical Periodontics<br />
Repairs of Crowns, Inlays, Onlays, Bridges and Dentures<br />
Simple Extractions<br />
Surgical Periodontics<br />
Complex Oral Surgery<br />
General Anesthesia and/or IV Sedation<br />
Class III—Major Restorative<br />
Inlays, Onlays, Crowns<br />
Implants<br />
Prosthetics<br />
Orthodontics (dependent children only)<br />
* Plan payments, member coinsurances and deductibles are based on the maximum allowable charge.<br />
In-Network dentists accept the maximum allowable charge as payment-in-full.<br />
** Members utilizing out-of-network providers may be subject to balance billing by their provider.<br />
Out-of-Network<br />
Plan Pays**<br />
100% 100%<br />
70% 70%<br />
50% 50%<br />
Diagnostic, Active, Retention Treatment 50% 50%<br />
Deductibles and Maximums<br />
$50/$150 Deductible (excluding Class I – Diagnostic and Preventive services, and<br />
Class IV – Orthodontic Services)<br />
$1,500 Contract Maximum per Member during the period of July 1st – June 30th (excludes covered<br />
Class I services)<br />
$2,000 Lifetime Orthodontia Maximum for dependent children. Orthodontic coverage for<br />
dependent children will cease at the end of the month in which the child turns 25.<br />
— 14 —
EXCLUSIONS – D<strong>PPO</strong> Plan<br />
Schedule of Exclusions and Limitations – <strong>PPO</strong><br />
SCHEDULE OF EXCLUSIONS AND LIMITATIONS<br />
Except as specifically provided in the Certificate, Schedules of <strong>Benefit</strong>s or Riders to the Certificate, no coverage will be<br />
provided for services, supplies or charges:<br />
STMD (07/09)<br />
1. Not specifically listed as a Covered Service on<br />
the Schedule of <strong>Benefit</strong>s and those listed as not<br />
covered on the Schedule of <strong>Benefit</strong>s.<br />
2. Which are necessary due to patient neglect, lack<br />
of cooperation with the treating dentist or failure<br />
to comply with a professionally prescribed<br />
Treatment Plan.<br />
3. Started prior to the Member’s Effective Date or<br />
after the Termination Date of coverage with the<br />
Company, including, but not limited to multi-visit<br />
procedures such as endodontics, crowns,<br />
bridges, inlays, onlays, and dentures.<br />
4. Services or supplies that are not deemed<br />
generally accepted standards of dental<br />
treatment.<br />
5. For hospitalization costs.<br />
6. For prescription or non-prescription drugs,<br />
vitamins, or dietary supplements.<br />
7. Administration of nitrous oxide, general<br />
anesthesia and i.v. sedation, unless specifically<br />
indicated on the Schedule of <strong>Benefit</strong>s.<br />
8. Which are Cosmetic in nature as determined by<br />
the Company, including, but not limited to<br />
bleaching, veneer facings, personalization or<br />
characterization of crowns, bridges and/or<br />
dentures.<br />
9. Elective procedures including but not limited to<br />
the prophylactic extraction of third molars.<br />
10. For the following which are not included as<br />
orthodontic benefits - retreatment of orthodontic<br />
cases, changes in orthodontic treatment<br />
necessitated by patient neglect, or repair of an<br />
orthodontic appliance.<br />
11. For congenital mouth malformations or skeletal<br />
imbalances, including, but not limited to<br />
treatment related to cleft lip or cleft palate,<br />
disharmony of facial bone, or required as the<br />
result of orthognathic surgery including<br />
orthodontic treatment.<br />
12. For dental implants including placement and<br />
restoration of implants unless specifically<br />
covered under a rider to the Certificate.<br />
13. For oral or maxillofacial services including but<br />
not limited to associated hospital, facility,<br />
anesthesia, and radiographic imaging even if the<br />
condition requiring these services involves part<br />
of the body other than the mouth or teeth.<br />
14. Diagnostic services and treatment of jaw joint<br />
problems by any method unless specifically<br />
covered under a Rider to the Certificate. These<br />
jaw joint problems include but are not limited to<br />
— 15 —<br />
such conditions as temporomandibular joint<br />
disorder (TMD) and craniomandibular disorders<br />
or other conditions of the joint linking the jaw<br />
bone and the complex of muscles, nerves and<br />
other tissues related to the joint.<br />
15. For treatment of fractures and dislocations of the<br />
jaw.<br />
16. For treatment of malignancies or neoplasms.<br />
17. Services and/or appliances that alter the vertical<br />
dimension, including but not limited to, full mouth<br />
rehabilitation, splinting, fillings to restore tooth<br />
structure lost from attrition, erosion or abrasion,<br />
appliances or any other method.<br />
18. Replacement of lost, stolen or damaged<br />
prosthetic or orthodontic appliances.<br />
19. For broken appointments.<br />
20. For house or hospital calls for dental services.<br />
21. Replacement of existing crowns, onlays, bridges<br />
and dentures that are or can be made<br />
serviceable.<br />
22. Preventive restorations in the absence of dental<br />
disease.<br />
23. Periodontal splinting of teeth by any method.<br />
24. For duplicate dentures, prosthetic devices or any<br />
other duplicative device.<br />
25. For services determined to be furnished as a<br />
result of a prohibited referral. “Prohibited<br />
referral” means a referral prohibited by<br />
Section 1-302 of the Health Occupations<br />
Article. Prohibited referrals are referrals of a<br />
patient to an entity in which the referring<br />
dentist, or the dentist’s immediate family: (a)<br />
owns a beneficial interest; or (b) has a<br />
compensation arrangement. The dentist’s<br />
immediate family includes the spouse, child,<br />
child’s spouse, parent, spouse’s parent,<br />
sibling, or sibling’s spouse of the dentist, or<br />
that dentist in combination.<br />
26. For which in the absence of insurance the<br />
Member would incur no charge.<br />
27. For plaque control programs, oral hygiene,<br />
and dietary instructions.<br />
28. For any condition caused by or resulting from<br />
declared or undeclared war or act thereof, or<br />
resulting from service in the national guard or<br />
in the armed forces of any country or<br />
international authority.<br />
29. For training and/or appliance to correct or<br />
control harmful habits, including, but not
deciduous molars and permanent first molars,<br />
or deciduous molars and permanent first<br />
molars that have not, or will not develop.<br />
8. Prefabricated stainless steel crowns - one per<br />
limited to, muscle training therapy<br />
31. Which<br />
tooth per<br />
are<br />
lifetime<br />
not<br />
for<br />
Dentally<br />
age fourteen<br />
Necessary<br />
years and<br />
as<br />
(myofunctional therapy).<br />
younger.<br />
determined by the Company.<br />
30. For any claims submitted to the Company by the<br />
9.<br />
32.<br />
Crown<br />
For prosthetic<br />
lengthening<br />
services<br />
- one<br />
including<br />
per tooth<br />
but<br />
per<br />
not<br />
lifetime.<br />
limited<br />
Member or on behalf of the Member in excess of<br />
to full or partial dentures or fixed bridges, if such<br />
twelve (12) months after the date of service.<br />
10. Periodontal services replace maintenance one or more following teeth missing active<br />
limited to, muscle training therapy<br />
31. Which are not Dentally Necessary as<br />
prior<br />
Failure to furnish the claim within the time<br />
periodontal to the Member's therapy eligibility – two under per twelve the Company. months in<br />
(myofunctional therapy).<br />
determined by the Company.<br />
required does not invalidate or reduce a claim if<br />
addition to routine prophylaxis.<br />
For Group Policies issued and delivered in<br />
30. For it any was claims not reasonably submitted to possible the Company to submit by the the<br />
32. For prosthetic services including but not limited<br />
11. Periodontal Maryland, this scaling exclusion and root does planing not - one apply per<br />
Member<br />
to<br />
claim within or on behalf the required of the Member time, if in the excess claim of is<br />
to full or partial dentures or fixed bridges, if such<br />
two<br />
furnished as soon as reasonably possible and,<br />
prosthetic year period services per area placed of the five mouth.<br />
twelve (12) months after the date of service.<br />
services replace one or more teeth years missing after prior the<br />
Failure except to in furnish the absence the claim of legal within capacity the time of the<br />
12. to Placement Member’s the Member's Effective or eligibility replacement Date under for of services. the single Company. crowns,<br />
required Member, does not not later invalidate than 1 or year reduce from a claim the time if<br />
inlays, onlays, single and abutment buildups<br />
For Group Policies issued and delivered in<br />
it claim was not is otherwise reasonably required. possible to submit the<br />
and post and cores, bridges, full and partial<br />
Maryland, this exclusion does not apply to<br />
claim within the required time, if the claim is<br />
dentures – one within five years of their<br />
furnished as soon as reasonably possible and,<br />
prosthetic<br />
placement.<br />
services placed five years after the<br />
except in the absence of legal capacity of the<br />
Member’s Effective Date for services.<br />
LIMITATIONS Member, - D<strong>PPO</strong> not later than 1 year from the time<br />
13. Denture relining, rebasing or adjustments - are<br />
claim is otherwise required.<br />
included in the denture charges if provided<br />
within six months of insertion by the same<br />
The following services will be subject to limitations as set forth below:<br />
dentist.<br />
1. Full mouth x-rays – one every five years.<br />
14. Subsequent primary posterior denture molars. relining or rebasing –<br />
2. One set(s) of bitewing x-rays per six months<br />
limited to one every three year(s) thereafter.<br />
18. Root canal treatment and retreatment – one<br />
through age thirteen, and one set(s) of<br />
15. Surgical per tooth periodontal lifetime. procedures - one per two<br />
bitewing x-rays per twelve months<br />
for age<br />
year period per area of the mouth.<br />
19. Recementations by the same dentist who<br />
fourteen and older.<br />
16. Sealants initially inserted - one per the crown tooth per or bridge three during year(s)<br />
the<br />
3. Periodic oral evaluation – two per consecutive<br />
through first twelve age months fifteen are on included permanent in the first crown and<br />
or<br />
LIMITATIONS - D<strong>PPO</strong><br />
twelve month period.<br />
second bridge molars.<br />
benefit, then one per twelve months<br />
thereafter; one per twelve months for other<br />
The 4. following Limited services oral evaluation will be subject (problem to limitations focused) – as set forth below: 17. Pulpal therapy - through age five on primary<br />
than the dentist who initially inserted the crown<br />
limited to one per dentist per twelve months.<br />
anterior teeth and through age eleven on<br />
or bridge.<br />
1. 5.<br />
Full Prophylaxis<br />
mouth x-rays –<br />
– two<br />
one per<br />
every twelve<br />
five years.<br />
consecutive<br />
primary posterior molars.<br />
STMD (07/09)<br />
20. Replacement restorations – limited to one per<br />
2. One month set(s) period. of bitewing One (1) x-rays additional per for six Members months<br />
18. Root twelve canal months. treatment and retreatment – one<br />
through under the age care thirteen, of a medical and professional one set(s) during of<br />
per tooth per lifetime.<br />
bitewing pregnancy. x-rays per twelve months for age<br />
21. Contiguous surface posterior restorations not<br />
19. Recementations involving the occlusal by the surface same will dentist be payable who<br />
6.<br />
fourteen Fluoride<br />
and treatment<br />
older.<br />
– two per consecutive<br />
initially as one inserted surface the restoration. crown or bridge during the<br />
3. Periodic twelve month oral evaluation period. – two per consecutive<br />
first twelve months are included in the crown or<br />
7.<br />
twelve Space<br />
month maintainers<br />
period.<br />
22. - only eligible for Members<br />
bridge Posts benefit, are only then covered one per as twelve part of months a post<br />
through age eighteen when used to maintain<br />
thereafter; buildup. one per twelve months for other<br />
4. Limited oral evaluation (problem focused) –<br />
space as a result of prematurely lost<br />
23.<br />
than An<br />
the Alternate<br />
dentist <strong>Benefit</strong><br />
who initially Provision<br />
inserted (ABP)<br />
the crown<br />
limited to one per dentist per twelve months.<br />
will be<br />
deciduous molars and permanent first molars,<br />
or applied<br />
bridge.<br />
if a dental condition can be treated by<br />
5. Prophylaxis or deciduous – two molars per and twelve permanent consecutive<br />
first<br />
20. Replacement means of restorations a professionally – limited to acceptable one per<br />
month molars period. that have One not, (1) or additional will not develop. for Members<br />
twelve procedure months.<br />
which is less costly than the<br />
under the care of a medical professional during<br />
treatment recommended by the dentist. The<br />
8. pregnancy.<br />
Prefabricated stainless steel crowns - one per<br />
21. Contiguous ABP does surface not commit posterior the member restorations the not<br />
less<br />
tooth per lifetime for age fourteen years and<br />
involving costly treatment. the occlusal However, surface if will the member payable<br />
6. Fluoride younger. treatment – two per consecutive<br />
and<br />
as the one dentist surface restoration.<br />
twelve month period.<br />
choose the more expensive<br />
9. Crown lengthening - one per tooth per lifetime.<br />
22. Posts treatment, are only the member covered is as responsible part of a for post<br />
the<br />
7. Space maintainers - only eligible for Members<br />
additional charges beyond those allowed for<br />
10. Periodontal maintenance following active<br />
buildup.<br />
through age eighteen when used to maintain<br />
the ABP.<br />
space periodontal as a therapy result – two of per prematurely twelve months lost<br />
in<br />
23. An Alternate <strong>Benefit</strong> Provision (ABP) will be<br />
deciduous addition to molars routine and prophylaxis. permanent first molars,<br />
applied if a dental condition can be treated by<br />
11.<br />
or Periodontal<br />
deciduous scaling<br />
molars and<br />
and root<br />
permanent planing - one<br />
first<br />
per<br />
means of a professionally acceptable<br />
molars two year<br />
that period<br />
have not, per area<br />
or will of<br />
not the<br />
develop.<br />
mouth.<br />
procedure which is less costly than the<br />
treatment recommended by the dentist. The<br />
8. 12.<br />
Prefabricated Placement or<br />
stainless replacement<br />
steel crowns of single<br />
- one crowns,<br />
per<br />
ABP does not commit the member to the less<br />
tooth inlays,<br />
per onlays,<br />
lifetime single<br />
for age and<br />
fourteen abutment<br />
years buildups<br />
and<br />
costly treatment. However, if the member and<br />
younger.<br />
and post and cores, bridges, full and partial<br />
the dentist choose the more expensive<br />
9. Crown dentures lengthening – one - within one per five tooth years per lifetime.<br />
of their<br />
treatment, the member is responsible for the<br />
placement.<br />
additional charges beyond those allowed for<br />
10. Periodontal maintenance following active<br />
the ABP.<br />
13. periodontal Denture relining, therapy rebasing – two per or twelve adjustments months - are in<br />
STMD (07/09) addition included to routine the prophylaxis.<br />
denture charges if provided<br />
within six months of insertion by the same<br />
11. Periodontal dentist. scaling and root planing - one per<br />
two year period per area of the mouth.<br />
14. Subsequent denture relining or rebasing –<br />
12. Placement<br />
STMD (07/09)<br />
limited to one or replacement every three year(s) of single thereafter. crowns,<br />
inlays, onlays, single and abutment buildups<br />
— 16 —<br />
15. and Surgical post and periodontal cores, procedures bridges, full - and one partial<br />
per two
<strong>United</strong> <strong>Concordia</strong><br />
Rider to Schedule of <strong>Benefit</strong>s and<br />
Schedule of Exclusions and Limitations<br />
Implantology<br />
This Rider is effective on July 1, 2009 and is attached to and made a part of the Schedule of<br />
<strong>Benefit</strong>s and Schedule of Exclusions and Limitations.<br />
SCHEDULE OF BENEFITS<br />
The Company will pay implantology benefits for eligible Members for the following Covered<br />
Services equal to 50% of the Maximum Allowable Charge.<br />
Implantology Services<br />
Surgical Services<br />
D6010 surgical placement of implant body: endosteal implant<br />
D6040 surgical placement: eposteal implant<br />
D6050 surgical placement: transosteal implant<br />
D6100 implant removal, by report<br />
Supporting Structures<br />
D6055 dental implant supported connecting bar<br />
D6056 prefabricated abutment – includes placement<br />
D6057 custom abutment – includes placement<br />
Implant/Abutment Supported Removable Dentures<br />
D6053 implant/abutment supported removable denture for completely edentulous arch<br />
D6054 implant/abutment supported removable denture for partially edentulous arch<br />
Implant/Abutment Supported Fixed Dentures (Hybrid Prosthesis)<br />
D6078 implant/abutment supported fixed denture for completely edentulous arch<br />
D6079 implant/abutment supported fixed denture for partially edentulous arch<br />
Single Crowns, Abutment Supported<br />
D6058 abutment supported porcelain/ceramic crown<br />
D6059 abutment supported porcelain fused to metal crown (high noble metal)<br />
D6060 abutment supported porcelain fused to metal crown (predominantly base metal)<br />
D6061 abutment supported porcelain fused to metal crown (noble metal)<br />
D6062 abutment supported cast metal crown (high noble metal)<br />
D6063 abutment supported cast metal crown (predominantly base metal)<br />
D6064 abutment supported cast metal crown (noble metal)<br />
D6094 abutment supported crown – (titanium)<br />
Single Crowns, Implant Supported<br />
D6065 implant supported porcelain/ceramic crown<br />
D6066 implant supported porcelain fused to metal crown (titanium, titanium alloy, high noble metal)<br />
D6067 implant supported metal crown (titanium, titanium alloy, high noble metal)<br />
Fixed Partial Denture, Abutment Supported<br />
D6068 abutment supported retainer for porcelain/ceramic FPD<br />
D6069 abutment supported retainer for porcelain fused to metal FPD (high noble metal)<br />
D6070 abutment supported retainer for porcelain fused to metal FPD (predominantly base metal)<br />
D6071 abutment supported retainer for porcelain fused to metal FPD (noble metal)<br />
D6072 abutment supported retainer for cast metal FPD (high noble metal)<br />
D6073 abutment supported retainer for cast metal FPD (predominantly base metal)<br />
D6074 abutment supported retainer for cast metal FPD (noble metal)<br />
D6194 abutment supported retainer crown for FPD – (titanium)<br />
R-Implant (03/07)<br />
Current Dental Terminology © American Dental Association.<br />
— 17 —
Fixed Partial Denture, Implant Supported<br />
D6075 implant supported retainer for ceramic FPD<br />
D6076 implant supported retainer for porcelain fused to metal FPD (titanium, titanium alloy, or<br />
high noble metal)<br />
D6077 implant supported retainer for cast metal FPD (titanium, titanium alloy, or high noble<br />
metal)<br />
Other Repair Procedures<br />
D7950 osseous, osteoperiosteal, or cartilage graft of the mandible or maxilla – autogenous or<br />
nonautogenous, by report<br />
D7951 sinus augmentation with bone or bone substitutes<br />
D7953 bone replacement graft for ridge preservation – per site<br />
Deductible(s)<br />
The annual Deductibles indicated on the Schedule of <strong>Benefit</strong>s will be applied to implantology<br />
services.<br />
Maximum(s)<br />
The annual Maximum indicated on the Schedule of <strong>Benefit</strong>s will be applied to implantology<br />
services.<br />
Waiting Period(s)<br />
No Waiting Period will be applied to implantology services.<br />
SCHEDULE OF EXCLUSIONS AND LIMITATIONS<br />
The Schedule of Exclusions and Limitations is amended as follows:<br />
Exclusions<br />
Any exclusions relating to implantology services are deleted.<br />
The following exclusion is added to the Schedule of Exclusions and Limitations:<br />
Limitations<br />
Implantology services are excluded if such services replace one (1) or more teeth<br />
missing prior to Member’s eligibility under the Group Policy.<br />
The following limitation does not apply to the above listed implantology procedures:<br />
An alternate benefit provision (ABP) will be applied if a covered dental condition can be<br />
treated by means of a professionally acceptable procedure which is less costly than the<br />
treatment recommended by the dentist.<br />
The following limitations are added to the Schedule of Exclusions and Limitations:<br />
Implantology services are limited to one (1) per tooth per lifetime.<br />
Implantology services are limited to Member’s age eighteen (18) and older.<br />
R-Implant (03/07)<br />
Current Dental Terminology © American Dental Association.<br />
— 18 —