PEDIATRICIAN Spring 2003 - AAP-CA
PEDIATRICIAN Spring 2003 - AAP-CA
PEDIATRICIAN Spring 2003 - AAP-CA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
california<br />
<strong>PEDIATRICIAN</strong> <strong>Spring</strong> <strong>2003</strong><br />
AMERI<strong>CA</strong>N A<strong>CA</strong>DEMY OF PEDIATRICS, <strong>CA</strong>LIFORNIA DISTRICT IX<br />
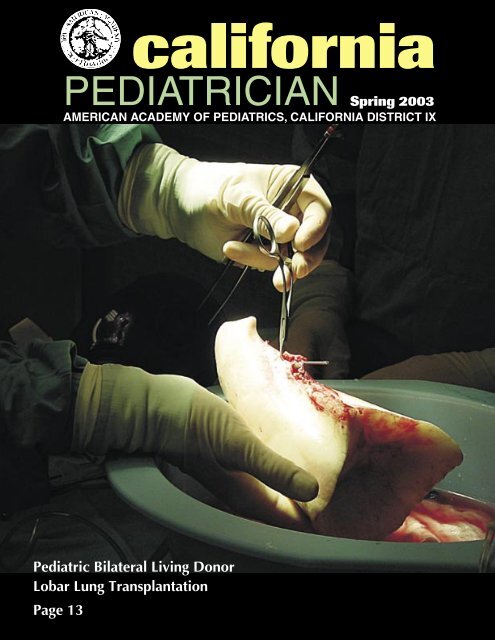
Pediatric Bilateral Living Donor<br />
Lobar Lung Transplantation<br />
Page 13
EDITOR-IN-CHIEF<br />
Jeffrey S. Penso, M.D.<br />
9696 Culver Blvd., #108<br />
Culver City, <strong>CA</strong> 90232<br />
(310) 204-6897<br />
jpenso@ucla.edu<br />
ASSISTANT EDITOR<br />
Marianne Hockenberry<br />
aapmarianne@aol.com<br />
ADVERTISING<br />
Stuart A. Cohen, M.D.<br />
6699 Alvarado Rd., #2200<br />
San Diego, <strong>CA</strong> 92120<br />
(619) 265-3400<br />
scohen98@ipninet.com<br />
DESIGN AND PRODUCTION<br />
Rosalie Blazej<br />
50 Laidley St.<br />
San Francisco, <strong>CA</strong> 94131<br />
(415) 695-0264 FAX (415) 641-5409<br />
rblazej@pacbell.net<br />
DISTRICT EXECUTIVE DIRECTOR<br />
Kris Calvin, MA<br />
853 Ramona Ave.<br />
Albany, <strong>CA</strong> 94706<br />
(510) 559-8383 FAX (510) 559-8464<br />
aapcalifornia@aol.com<br />
Marianne Hockenberry<br />
Associate Director<br />
EDITORIAL BOARD<br />
Chapter 1<br />
Lewis Nerenberg, M.D.<br />
Chapter 2<br />
Joan E. Hodgman, M.D.<br />
Chapter 3<br />
Howard Taras, M.D.<br />
Chapter 4<br />
Stanley Galant, M.D.<br />
CHAPTER OFFICES<br />
Chapter 1 Executive Director<br />
Beverly Busher<br />
900 Fifth Ave. #204<br />
San Rafael, <strong>CA</strong> 94901<br />
(415) 459-4775<br />
aapbev@aol.com<br />
www.aapca1.org<br />
Chapter 2 Executive Director<br />
Kathleen Shematek, MPH<br />
6233 East Allison Circle<br />
Orange, <strong>CA</strong> 92869<br />
(714) 744-8245<br />
aapca2kshematek@socal.rr.com<br />
www.aapca2.org<br />
Chapter 2 Chapter Administrator<br />
Eve Black<br />
P.O. Box 2134<br />
Inglewood, <strong>CA</strong> 90305<br />
(323) 757-1198<br />
aapcach2@aol.com<br />
Chapter 3 Executive Director<br />
Erika Kalter<br />
3020 Children’s Way<br />
MC 5073<br />
San Diego, <strong>CA</strong> 92123<br />
(858) 569-8816<br />
sdpeds@chsd.org<br />
www.aapca3.org<br />
Chapter 4 Executive Director<br />
Debbie Monfea<br />
12377 Lewis Street, #103<br />
Garden Grove, <strong>CA</strong> 92840<br />
(714) 971-0695<br />
ca4aap@sbcglobal.net<br />
www.aapca4.org<br />
Address comments and questions to<br />
Jeffrey S. Penso, M.D.<br />
jpenso@ucla.edu<br />
2 District Report<br />
Burton Willis, M.D. and Kris Calvin, M.A.<br />
3 Childhood Cancer Survivors Report Life Changes<br />
Brad J. Zebrack, Ph.D., M.S.W., and Mark A. Chesler, Ph.D.<br />
Today 75% of children diagnosed with various forms of cancer in the<br />
United States are expected to survive their disease and treatment. But<br />
what of their quality of life expected, enjoyed, or endured?<br />
4 Tandem Mass Spectrometry in Newborn Screening<br />
George C. Cunningham, M.D., M.P.H.<br />
The Department of Health Services keeps us current on neonatal<br />
screening.<br />
5 Culturally Appropriate Communication Is<br />
Good Medical Practice<br />
Allan Lieberthal, M.D., F<strong>AAP</strong><br />
Poor communication results in inferior medical care, and is not in<br />
compliance with federal government standards. Can we improve<br />
compliance?<br />
6 CMA House of Delegates Report<br />
Paul Y. Qaqundah, M.D.<br />
State budget concerns were key but access to the care and employer<br />
mandate proposals were issues we wrestled with in San Francisco.<br />
7 Weighing the Radiation Risks of CT Scans<br />
Nikta Forghani, M.D., Ronald A. Cohen, M.D., Myles B. Abbott,<br />
M.D.<br />
CT scans expose children to high doses of ionizing radiation. What<br />
are the best ways to use CT scans?<br />
8 Adolescent Idiopathic Scoliosis<br />
Robert M. Bernstein, M.D.<br />
What is the natural history of scoliosis, which cases need to be<br />
referred? What are the treatment options?<br />
9 Preventing Ear Infections in Children<br />
Harry Pellman, M.D.<br />
AOM is the most common bacterial infection diagnosed in children.<br />
What is known to reduce the frequency of middle ear problems?<br />
10 A Low-Glycemic Index Diet in the<br />
Treatment of Pediatric Obesity<br />
David S. Ludwig, MD, PhD, et. al.<br />
Obesity is arguably the most prevalent medical problem in the<br />
United States today. Weight loss on current reduced-fat diets is<br />
characteristically modest and transient. Can a novel treatment, the<br />
low-glycemic index diet, be the breakthrough we need?<br />
12 Why California’s MICRA Is Good for the Nation<br />
Ron Bangasser, M.D.<br />
We face a national medical liability crisis. The solution is California’s<br />
MICRA.<br />
13 Ten-Year Experience with Pediatric<br />
Bilateral Living Donor Lobar Lung Transplantation<br />
Marlyn S. Woo, M.D. and Vaughn A. Starnes, M.D.<br />
The medical team had exhausted all conventional medical and surgical<br />
options. What about lung transplantation for this dying patient?<br />
14 The Tao of Pediatrics and Chinese Medicine<br />
Wendy Yu, M.S., L.Ac., Jeffrey I. Gold, Ph.D.,<br />
Michael H. Joseph, M.D.<br />
Health is not just about a disease factor, it’s about the whole<br />
environment.<br />
17 In Memoriam — Joseph H. Davis<br />
A beloved pediatrician is recalled by his son.<br />
18 Chronic Pain in Children: A Multidisciplinary Biopsychosocial<br />
Treatment Approach (Part III)<br />
Michael H. Joseph, M.D. and Jeffrey I. Gold, Ph.D.<br />
we must decrease all ongoing nociceptive pain and support,<br />
encourage, and reinforce the child in working through chronic pain<br />
symptomatology.<br />
21 Twenty-Five-Years of Home Mechanical Ventilation in Children:<br />
The Program at Childrens Hospital Los Angeles<br />
Manisha Witmans, M.D., Sheila S. Kun, R.N., M.S., and<br />
Thomas G. Keens, M.D.<br />
The last 25 years has witnessed enormous improvement in home<br />
mechanical ventilation. Since the inception of the home ventilator<br />
program in 1977, the program at Childrens Hospital Los Angeles<br />
CHLA has grown to include over 375 children.<br />
CONTENTS<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 1
TABLE OF CONTENTS continued<br />
District Report<br />
<strong>AAP</strong>-<strong>CA</strong> Advocacy in Hard Times:<br />
Multiple Strategies to Success<br />
Burton Willis, M.D. and Kris Calvin, M.A.<br />
Despite the flowering trees around the majestic Capitol dome, Sacramento<br />
offers few pretty pictures this year. Take a shot of the full landscape: an<br />
unprecedented $30 billion dollar-plus state deficit looms. Zoom in for a<br />
family portrait? Democrats, Republicans and the Governor’s office seem trapped on<br />
their own limited platforms, with no real solution in sight. Worse yet for pediatrics,<br />
snapshot photos of the health budget show only shrinking dollar signs. This is because<br />
health dollars are largely unprotected in an era of budget “lock-ins” in other areas due<br />
to initiatives or other mandates.<br />
The California District of the American Academy of Pediatrics (<strong>AAP</strong>-<strong>CA</strong>), representing<br />
all four California <strong>AAP</strong> Chapters, has developed a pragmatic, yet hopeful<br />
approach to this state crisis. Strategies include:<br />
• Increased <strong>AAP</strong>-<strong>CA</strong> leadership and participation in coalitions to ensure that<br />
children’s health advocates are heard above the din in the budget debates in<br />
Sacramento. This includes intense advocacy with 70 other groups to oppose<br />
proposed cuts to Medi-Cal physician reimbursment.<br />
• Build on successes. Last year <strong>AAP</strong>-<strong>CA</strong> and our allies were successful in saving<br />
and expanding the Child Health and Disability Prevention (CHDP) state-only<br />
program. If state-only CHDP had been eliminated these children would have<br />
fallen into the ranks of the uninsured and an important source of pediatric revenue<br />
to sustain their care would have been eliminated. This year <strong>AAP</strong>-<strong>CA</strong> has<br />
worked closely with the state to protect the program and improve it. Starting<br />
July 1, <strong>2003</strong> CHDP providers will be able to pre-enroll children into the Medi-<br />
Cal program through the Internet or new Point of Service devices. For more<br />
information go to www.medi-cal.ca.gov/new_chdp.asp.<br />
• “Back-end” involvement in implementation of children’s programs. Programs<br />
are best protected in the budget if they are fully implemented and working well<br />
for both physicians and children. For example, <strong>AAP</strong>-<strong>CA</strong> “Chapter Champions”<br />
are working with the state to ensure that the already enacted Newborn Hearing<br />
Screening Program is fully implemented with appropriate reimbursement.<br />
• Prevent budget problems before they start. This includes careful legislative monitoring<br />
and intervention to ensure that only those bills whose benefits outweigh<br />
their costs are enacted. This requires <strong>AAP</strong>-<strong>CA</strong> to be available to legislators and<br />
their staff as an expert resource on a wide range of issues, including vision<br />
screening, early brain development anticipatory guidance and HMO contracting<br />
issues. We have already had great success this year in this regard.<br />
• Engage legislators and policymakers by utilizing credible pediatrician advocates.<br />
Legislators and other policymakers prefer to hear from you, practicing<br />
pediatricians with first-hand experience with children and families, rather than<br />
from lobbyists and staff. Something as simple as a “form” letter from you to<br />
your legislator on a priority <strong>AAP</strong>-<strong>CA</strong> issue matters. Those of you with a flair for<br />
public comment can make a tremendous difference by testifying for <strong>AAP</strong>-<strong>CA</strong><br />
on a bill or budget item in Sacramento. Building an ongoing trust relationship<br />
with your local legislator in his or her home office is invaluable. If you have<br />
not already completed the brief <strong>AAP</strong>-<strong>CA</strong> Grass Roots Advocacy Survey please<br />
request one from aapcalifornia@aol.com.<br />
Improving the state child health picture in California this year will take more<br />
than just a pretty new frame. <strong>AAP</strong>-<strong>CA</strong> will continue to work towards real change for<br />
pediatricians and the children and families that you serve.<br />
22 Childcare Health Linkages Program: How<br />
Pediatricians Can Collaborate with Local<br />
Childcare Health Consultants<br />
Robin Calo, R.N., M.S., P.N.P. and<br />
Karen Sokal-Gutierrez, M.D., M.P.H.<br />
When you think about the young children in your<br />
practice, who besides their parents takes care of<br />
them? Is a childcare consultant coming to your<br />
neighborhood?<br />
23 Eve Black Honored<br />
24 Annual Las Vegas Seminars —<br />
25 Years of District Education and Support<br />
Rosalie Blazej and Milton Arnold, M.D.<br />
For 25 years, pediatricians have flocked to Las Vegas<br />
to learn and relax.<br />
25 Selling Tobacco Products as a<br />
Public Health Issue<br />
Trisha Roth, M.D.<br />
At the urging of the California Medical Association<br />
and with the help of the Preventing Tobacco Addiction<br />
Foundation, a proposal is on the table to increase the<br />
minimum age for purchasing tobacco to 21.<br />
26 Early Hearing Detection and Intervention<br />
Sudeep Kukreja, M.D.<br />
To be successful, California needs to address several<br />
issues in the Newborn Hearing Screening Program.<br />
29 SED — California Region<br />
Leonard Kutnik, M.D.<br />
One in 10 children suffer from a mental health<br />
illness but only one in five children receive specialty<br />
services. Unfortunately, even this rate of treatment is<br />
not achieved in the Healthy Families Program.<br />
29 California Surgeon General Needed to<br />
Protect Californians<br />
31 Retirement Options for Pediatricians<br />
Joan E. Hodgman, M.D.<br />
Retirement should not be dull or boring. With the<br />
increase in the average life expectancy, more and<br />
more of us can look forward to years of active life<br />
after retirement.<br />
32 Last Word: After the Iraq War<br />
Jeffrey S. Penso, M.D.<br />
Even with victory an implacable worldwide enemy<br />
will remain. While physicians are aware of the<br />
continued threat of bioterrorism, we have yet to<br />
recognize that bioterror will change relationships<br />
between physicians and the community.<br />
33 President-Elect Candidates<br />
33 Contributors<br />
35 Officers and Committees<br />
California Pedatrician does not<br />
assume responsibility for authors’<br />
statements or opinions. Opinions<br />
expressed are not necessarily those<br />
of California Pediatrician or the California<br />
District, American Academy<br />
of Pediatrics.<br />
Vol. 19 No. 1 <strong>Spring</strong> <strong>2003</strong><br />
California Pediatrician [ISSN 0882-3421] is<br />
the official publication of the American Academy<br />
of Pediatrics, California District IX.<br />
Copyright © <strong>2003</strong> American Academy of<br />
Pediatrics, California District IX<br />
2 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Childhood Cancer Survivors Report Life Changes<br />
Brad J. Zebrack, Ph.D., M.S.W., and Mark A. Chesler, Ph.D.<br />
“I used to get really depressed<br />
on the anniversary when I got<br />
sick, August 4. I used to get really<br />
upset; I even wore black to work.<br />
You know, this is the day my life<br />
changed... Like this is really weird,<br />
I see a grave, and that’s the person<br />
that died, on August 4, 1985. She’s<br />
gone. Because you know, my life<br />
had to change, I had cancer and<br />
I can’t go back there, I can’t go in<br />
the past, so it’s like, she’s gone.<br />
(24-year old survivor of childhood<br />
cancer).”<br />
Prior to the 1970s and the advent and use of<br />
multi-modal chemotherapy, survival rates<br />
for children diagnosed with leukemia and<br />
other forms of cancer were dismal. Today,<br />
advances in treatment and the coordination of<br />
pediatric treatment through clinical trials have<br />
greatly increased the long-term life chances<br />
of these young people. Indeed, recent reports<br />
indicate that 75% of children diagnosed with<br />
various forms of cancer in the United States<br />
are expected to survive their disease and treatment.<br />
As we witness increasing lengths of survival<br />
for individuals diagnosed with cancer as<br />
children and a growing number of long-term<br />
survivors there is no indication of their quality<br />
of life expected, enjoyed, or endured. In<br />
1998, the American Cancer Society Task Force<br />
on Children and Cancer reported that “(T)he<br />
progress achieved in attaining 80% survival<br />
among children and adolescents and young<br />
adults with cancer can be justified only if their<br />
physical, emotional, and social quality of life<br />
also are protected.” Thus, success in pediatric<br />
oncology requires researchers and health care<br />
professionals to attend to the psychosocial and<br />
behavioral consequences of treatment and to<br />
the quality of life of these survivors.<br />
Cancer Survivorship<br />
Research literature on cancer survivors consistently<br />
refers to the notion that experiencing<br />
cancer can lead to changes in people’s lives.<br />
While many studies of cancer survivors document<br />
long-term sequelae as having deleterious<br />
effects on psychological well-being and social<br />
functioning, relatively few have investigated<br />
positive adaptation and factors associated with<br />
the potentials for positive life changes which<br />
survivors attribute to cancer.<br />
People often report that they have made<br />
positive changes in themselves and their lives<br />
after a negative event or trauma. Several scholars<br />
have described such changes as part of a<br />
process of cognitive reappraisal in the face<br />
of, or aftermath of, trauma. People thus may<br />
reframe or reinterpret their illness experience<br />
or themselves (e.g., from “victim to victor”),<br />
making new meaning out of their situation.<br />
Seminal work by Taylor indicated that a sizable<br />
proportion of women experienced positive<br />
life changes following their experiences<br />
with breast cancer. Similarly, in a comparison<br />
of adult bone marrow transplant patients to<br />
a matched control group without a history<br />
of cancer, the patients equaled or exceeded<br />
controls in the likelihood of reporting positive<br />
psychosocial changes in life.<br />
Some investigators, however, caution<br />
against such interpretations in that reports of<br />
positive outcomes may be “illusions,” “repressive<br />
denial,” or self-serving distortions that are<br />
more typical of poor mental health rather than<br />
positive adaptation. Our own view, based on<br />
empirical work as well as on our own personal<br />
and clinical experiences, is that cancer and<br />
other trauma should not be viewed as a stressor<br />
with uniformly negative outcomes but rather as<br />
transitional events that create the potential for<br />
both positive and negative change.<br />
Life changes for survivors of<br />
childhood cancer<br />
These issues are beginning to surface in<br />
recent research with survivors of childhood<br />
cancer. There is general agreement that many<br />
adolescent and young adult survivors of childhood<br />
cancer have lasting physical deficits and<br />
that some experience negative psychological<br />
changes as a result of their illness. At the same<br />
time, several scholars argue from empirical<br />
findings that demonstrate that a sizable portion<br />
of this population is coping more positively<br />
than their peers and that they have changed<br />
their psychologic orientations and outlooks<br />
for the better. These positive outcomes are not<br />
necessarily unrealistic or naïve “halo effects”<br />
because often they are accompanied simultaneously<br />
by details of how cancer has had deleterious<br />
effects. Furthermore, these results mirror<br />
findings and interpretations reported in the<br />
literature about gains in “secondary benefits”<br />
such as enhanced relationships with family<br />
members, emotional maturity, and greater life<br />
appreciation.<br />
Young adult survivors’ own words illuminate<br />
the changes they attribute to having had<br />
cancer as children.<br />
“I feel I’ve learned good lessons<br />
from it (my cancer). I realize what’s<br />
important in life and I don’t take<br />
everything for granted. I want to<br />
live life to the fullest.”<br />
“I think I’m stronger. I am very<br />
independent now. I set my mind<br />
to doing something and I do it. I<br />
think a part of me has definitely<br />
been impacted by the fact that<br />
I’ve had cancer. There are a lot<br />
of go-getters out there, but when<br />
you’ve accomplished something<br />
like surviving the cancer and<br />
treatments, when you’ve gotten<br />
through something like that, it just<br />
gives you a determination, a drive,<br />
to achieve well in school and to do<br />
well in life.”<br />
In addition, many long-term survivors of<br />
pediatric malignancies indicate that there is<br />
something inherent to the cancer experience<br />
that makes dealing with the “normal” challenges<br />
of every day life different from a life<br />
without cancer.<br />
“You know, it’s definitely a huge<br />
adjustment getting married, and<br />
having a child, so that’s adjustment<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 3
in and of itself, but I think you<br />
throw a whole other element in<br />
that, you know, like going through<br />
what I went through [cancer],<br />
and you need to try to fit that in<br />
somewhere. And you don’t know<br />
where it fits.”<br />
These statements above are consistent<br />
with what Tedeschi & Calhoun refer to as<br />
“philosophical outcomes” or “new priorities”<br />
in life. They reflect an internal process of<br />
“meaning making,” whereby many of these<br />
survivors (with help from external supports,<br />
no doubt) have reframed or reinterpreted their<br />
initial trauma, placed their current worries or<br />
negative effects in context, and made new and<br />
positive meaning out of their cancer experience.<br />
Complementing recent concern about<br />
evidence of a “post-traumatic stress syndrome”<br />
among childhood cancer survivors, some<br />
survivors may experience “post-traumatic<br />
growth” or a sense of “thriving.” The need for<br />
further research on these issues, and resultant<br />
estimates of the proportion of the childhood<br />
cancer survivor population falling into either<br />
category, is vital.<br />
Implications for intervention<br />
Evaluating reports of positive change and<br />
enhanced quality of life associated with cancer<br />
is important for two reasons: (1) it challenges<br />
us to try to understand the reality and validity<br />
of such reports; and (2) it suggests the need<br />
for psychosocial interventions that not only<br />
prevent or alleviate negative sequelae but also<br />
promote positive outcomes and increase longterm<br />
survivors’ opportunities for expressing<br />
and experiencing cancer as a potentially transformative<br />
experience. Such interventions may<br />
start with the subtle positive messages often<br />
presented at diagnosis (“you will survive this<br />
illness”), then subsesquently include the mobilization<br />
of family and friends’ supports, and<br />
skilled peer (“let me tell you what I learned”)<br />
or professional counseling.<br />
In the current context, where medical<br />
survival from childhood cancer is no longer a<br />
singular or rare phenomenon, the possibilities<br />
of full psychological survival and even growth<br />
have enormous theoretical and practical implications.<br />
The long term impact of experiencing<br />
or recognizing positive change is yet to be fully<br />
explored, but theoretically it has additional<br />
implications for the construction, or re-construction,<br />
of personal and social identity for<br />
adolescent and young adult cancer survivors.<br />
Tandem Mass Spectrometry in<br />
Newborn Screening<br />
George C. Cunningham, M.D., M.P.H.<br />
The state is currently conducting a legislatively mandated demonstration project to<br />
evaluate the most efficient way to add the Tandem Mass Spectrometry (MS/MS)<br />
technology to our newborn screening for metabolic disease. This technology measures<br />
47 different analytes in a blood specimen and can detect over 25 different disorders.<br />
This report is to inform pediatricians generally about the progress and future of this proposed<br />
expansion. Since starting in January 2002, 221,913 newborns have participated in this voluntary<br />
MS/MS screening. The Genetic Disease Branch classified 349 as initially positive and<br />
referred them to metabolic centers for diagnostic evaluation, leading to a definite diagnosis<br />
in 33 newborns. Participation in the pilot is only being offered in 60% of maternity hospitals,<br />
but is accepted by 90% of the mothers when offered. The initial referred rate at this time is<br />
about 8 of every 10,000 newborns screened and approximately 1 in 10 of the referred newborns<br />
have a disorder. The disorders are serious and with a few exceptions can be prevented<br />
or ameliorated by treatment. (See Chart)<br />
The project has demonstrated that the cost of case detection will be $60 to $80,000 per<br />
case, which is offset by the benefits of lives saved and costly hospitalization for treatment<br />
averted. We appreciate the cooperation received from pediatricians in making this project a<br />
success. There are 24 states that are implementing or using MS/MS to expand their programs<br />
at this time. Unfortunately, there are no funds in the current budget to continue this project and<br />
unless funds are added during the budget process, the project will terminate in June <strong>2003</strong>.<br />
Category Description Example Number<br />
Diagnosed<br />
Amino Acid<br />
Disorders<br />
Organic Acid<br />
Disorders<br />
Fatty Acid<br />
Oxidation<br />
Disorders<br />
Caused by the<br />
accumulation of<br />
amino acids in the<br />
blood (e.g. arginine)<br />
Caused by the toxic<br />
buildup of organic<br />
acids in the blood<br />
(e.g., proprionic acid<br />
or methylmalonic<br />
acid).<br />
Caused by a defect<br />
in the conversion of<br />
fats into fatty acids<br />
for use as an energy<br />
source<br />
Arginemia 1<br />
Methylmalonic acidemia<br />
(MMA)<br />
Propionic acidemia (PA) 2<br />
3-methylcrotonyl-CoA<br />
carboxylase deficiency<br />
(3MCC)<br />
Medium chain acyl-CoA<br />
dehydrogenase deficiency<br />
(M<strong>CA</strong>DD)<br />
Short chain acyl-CoA<br />
dehydrogenase deficiency/<br />
Ethyl malonic aciduria<br />
(S<strong>CA</strong>DD/EMA)<br />
Multiple acyl-CoA<br />
dehydrogenase deficiency<br />
(MADD or GA-2)<br />
Total 33<br />
7<br />
1<br />
11<br />
10<br />
1<br />
4 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Culturally Appropriate Communication Is<br />
Good Medical Practice<br />
Allan Lieberthal, M.D., F<strong>AAP</strong><br />
California is the most culturally<br />
diverse state in the country. Fortyseven<br />
percent of the population<br />
is white, 32 % Hispanic, 12 % Asian and<br />
Pacific Islander, 7 % African American, and<br />
1% Native-American. As many as 46% of<br />
the population has Limited English Proficiency<br />
(LEP). Over 100 languages are spoken<br />
including, in addition to English and Spanish,<br />
Tagalog, Armenian, Chinese, Thai, Korean,<br />
Arabic, Vietnamese, Hebrew, Russian, Farsi,<br />
and Hindi. We, as pediatricians, face a constant<br />
challenge to communicate with our patients<br />
and parents effectively. Many of us speak<br />
Spanish or another language, in addition to<br />
English. Some of us are fluent in that language<br />
while others try to get by with limited fluency.<br />
We are used to getting by with interpretation<br />
by children, friends, other parents, or a combination<br />
of the parent’s limited English and what<br />
little we may know of their primary language.<br />
The consequence may be that important information<br />
is miscommunicated or omitted during<br />
the medical encounter.<br />
A recent article in Pediatrics 1 points out<br />
the pitfalls of inadequate interpretation. In a<br />
sample of 13 encounters, six with a hospital<br />
interpreter, six with ad-hoc interpreters and one<br />
with an 11-year-old child interpreting, there<br />
were an average of 31 errors per encounter.<br />
Seventy-seven precent of errors made by the<br />
ad hoc interpreters and the child had clinical<br />
significance. This was significantly more than<br />
the 53% of clinically important errors made by<br />
the hospital interpreters. Errors included omission,<br />
false fluency, substitution, and addition.<br />
Recognizing that poor communication<br />
results in inferior medical care, the federal government<br />
has set standards for Culturally and<br />
Linguistically Appropriate Services (CLAS)<br />
(www.hhs.gov/ocr/lepfinal.htm). Standards<br />
published by the Department of Health and<br />
Human Services (HHS), Office of Civil Rights<br />
(OCR) apply to covered entities that include<br />
“any state or local agency, private institution<br />
or organization, or any public or private individual<br />
that operates, provides or engages in<br />
health, medical or social service programs that<br />
receive or benefit from HHS assistance.” The<br />
federal CLAS standards require covered entities<br />
to identify the language needs of patients<br />
and to provide proficient interpretation in a<br />
timely manner. At the state level, Assembly<br />
Bill 292 (Yee) has been introduced and, if<br />
passed and signed into law, would prohibit the<br />
use of children as interpreters.<br />
There are many approaches to providing<br />
adequate interpreter services. Kaiser-Permanente<br />
in Panorama City has introduced a prototype<br />
program to comply with the standards.<br />
Employees who serve as interpreters must pass<br />
the language proficiency test for interpretation.<br />
These are mostly Spanish speakers. We rarely<br />
have interpreters available for the many other<br />
languages we encounter in our multi-ethnic<br />
practice. In order to meet the needs of all of<br />
our LEP patients, patients are identified as<br />
needing interpretation at the time of making<br />
an appointment and at check-in. A printed<br />
area on the registration papers indicates the<br />
preferred language of the patient and whether<br />
interpretation services are needed. If there is no<br />
interpreter available, we are using Language<br />
Line Services (www.languageline.com), a<br />
telephone-based service that can provide interpretation<br />
in over 140 languages. This can be<br />
done in the exam room using a pair of portable<br />
phone extensions, one for the patient/parent<br />
and one for the physician. The process requires<br />
only a small increase in time as compared to<br />
having an interpreter on site.<br />
Shortly after the Language Line Service<br />
was in place, I was seeing one of my Armenian<br />
patients whose mother speaks very limited<br />
English. It appeared to be a routine sick visit.<br />
Through halting English, I understood the<br />
symptoms of a common cold, but felt a little<br />
uneasy because the mother did not appear to<br />
understand my English instructions. I tried the<br />
Language Line and soon found out that I had<br />
totally misunderstood the illness. In fact the<br />
child had a history consistent with cough variant<br />
asthma. Had I been forced to communicate<br />
in English, I am sure the mother would not<br />
have understood my explanation and instructions.<br />
Using the Language Line it was easy<br />
Over 100 languages are spoken including, in addition to English<br />
and Spanish, Tagalog, Armenian, Chinese, Thai, Korean, Arabic,<br />
Vietnamese, Hebrew, Russian, Farsi, and Hindi.<br />
to get a good history and to explain what her<br />
child had since she was hearing it in her own<br />
language. The mother, who I had seen on several<br />
previous occasions without interpretation<br />
services, was effusive in thanking me and telling<br />
me how happy she was with the visit. From<br />
initial skepticism, I became a convert.<br />
Unlike pediatricians in private practice<br />
or in network managed care practices, I do not<br />
have to deal directly with the cost and reimbursement<br />
for interpretation services. This is<br />
especially important for doctors practicing in<br />
poor communities with a high percentage of<br />
ethnic minorities. Use of the Language Line<br />
may cost as much as $15 for a 10 minute visit.<br />
If a practice has a large number of patients<br />
requiring interpretation by a nurse, workflow<br />
may be impaired or additional personnel may<br />
be needed. This should be recognized as an<br />
additional expense and must be reimbursed<br />
appropriately.<br />
Even consistent professional interpreter<br />
service will not bring us to a single standard<br />
of medical care. The reality is that there is a<br />
severe shortage of qualified health professionals<br />
in all minority groups. Until our patients<br />
can receive competent care from clinicians<br />
who share their culture and language, we must<br />
do our best to be sensitive and responsive to<br />
their needs.<br />
REFERENCE<br />
1. Flores G, Laws B, Mayo SJ, et. al. Errors<br />
in medical interpretation and their potential<br />
clinical consequences in pediatric emergencies<br />
Pediatrics <strong>2003</strong>(1):111:6-14<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 5
CMA House of Delegates Report<br />
Paul Y. Qaqundah, M.D.<br />
The 132nd CMA House of Delegates met at the<br />
Hilton Towers in San Francisco on March 22-<br />
25 <strong>2003</strong>. This year, the California <strong>AAP</strong> hosted<br />
its tenth annual breakfast for pediatrician delegates. Your<br />
three specialty representatives, Alan Burkin, Stuart Cohen,<br />
and myself, together with our State Executive Director of<br />
the Academy, Kris Calvin, provided an important opportunity<br />
for county medical society pediatric delegates to dialogue<br />
and coordinate a strategy to influence CMA policy<br />
through the house. Issues discussed included:<br />
1. Extended access to the uninsured, including review of<br />
employer mandate proposals.<br />
2. Medi-Cal physician reimbursement and other state<br />
budget concerns.<br />
3. Options for tapping mental health funds to support<br />
pediatric practice.<br />
4. Coordinated support for resolutions including those<br />
related to reimbursement, obesity, soda sales and junk<br />
foods. Approval of school lunch options, physical<br />
education in schools and Medicaid block grants to<br />
states.<br />
I will highlight the actions of the House on issues that<br />
pertain to pediatrics.<br />
Science and Public Health<br />
The house supported our resolution on childhood obesity<br />
to encourage inclusion of obesity prevention in public<br />
school curricula, support collaborative efforts among<br />
health organizations, promote education, treatment<br />
of obesity, and develop regional centers for comprehensive<br />
treatment of morbid childhood obesity to be<br />
financed through private and public sources.<br />
On our resolution to improve school physical education,<br />
the CMA supported measures that mandate increased<br />
physical activity in schools and explore methods to<br />
protect schools from litigation when school facilities<br />
are made available to communities for after hours<br />
physical activity.<br />
CMA supported <strong>AAP</strong>’s resolution on sale of soda and fast<br />
foods in schools, i.e. to work with health organizations<br />
to strengthen existing standards established by<br />
the “Pupil Nutrition, Health and Achievement Act” of<br />
2001 that all foods provided in public schools (K-12)<br />
meet national government nutritional standards. CMA<br />
urges physicians and local medical societies to work<br />
with local schools to implement these standards.<br />
CMA supported our resolution on Epi-Pen administration<br />
in schools to allow non-CPR certified school personnel<br />
to administer Epi-Pen for anaphylactic reactions<br />
if a CPR certified person is not available. This will<br />
protect schools against litigation.<br />
Emergency contraception. To assist appropriate use of<br />
contraception, CMA supports legislation to prohibit<br />
pharmacists from charging consultation fees when<br />
dispensing emergency contraceptives.<br />
Insurance and physician reimbursement. In 2002 CMA<br />
adopted “Fair Vaccine Payment Resolution” and<br />
requested a report back this year. CMA calls for all<br />
California health plans and Medicare to reimburse<br />
physicians at the average wholesale cost (AWC) of<br />
vaccines plus 10%. CMA also insists on reimbursement<br />
for costs of vaccine administration, at least at the<br />
rate presently paid by Medi-Cal- $9.51.<br />
Child protective services — CMA endorses review of<br />
policies of California Child Protective Services. We<br />
demand that CCPS give substantial weight to recommendations<br />
of treating physicians in the disposition of<br />
any at risk child.<br />
CMA is advocating nationally to fix the absurdities of<br />
HIPAA rules.<br />
The House will work with insurance companies to maintain<br />
a single mailing address for the submission of<br />
claims, the address to be clearly printed on patient<br />
insurance cards. All payers should maintain a single<br />
electronic address and notify physicians of any<br />
changes of addresses.<br />
Newborns who test positive on toxicity screening. CMA<br />
supports immediate entry of the mother into a chemical<br />
dependency treatment program. CMA supports<br />
legislation to increase the number of chemical<br />
dependency treatment and rehabilitation programs<br />
in California.<br />
Jack Levin M.D., CMA’s C.E.O. noted that, “Our<br />
nation remains in a 3 year recession. Our state is broke.<br />
The events of 9/11 made all of that worse. The stress on<br />
health executives from these combined factors have been<br />
horrendous and now we are a nation at war.”<br />
Nevertheless, CMA has fought to protect further<br />
erosion of medical practice by reversing RBRVS cuts<br />
and blocking the impending 4.4% additional cuts in the<br />
<strong>2003</strong> budget. AMA and CMA have saved each physician<br />
involved in Medicare and Medicaid over $15000 in<br />
income. This amounts to the equivalent of CMA dues for<br />
all of a physician’s practice life. When Gov. Davis proposed<br />
$1.6 billion in Medi-Cal cuts the CMA engineered a<br />
complete reversal of those cuts.<br />
CMA has preserved its malpractice rules (MICRA)<br />
despite constant assault by trial lawyers. Thanks to CMA,<br />
California MICRA remains the national gold standard for<br />
malpractice reform. To preserve this, I suggest that you<br />
give generously to <strong>CA</strong>LPAC, the CMA political action<br />
committee.<br />
CMA has additional accomplishments too lengthy<br />
for this report. See www.cmanet.org. President Bush has<br />
stated that it is time to take control of medicine back from<br />
bureaucrats, trial lawyers and HMOs and give it back to<br />
physicians and patients. Don’t believe that anybody will<br />
give you anything. We have to support and join our professional<br />
organizations and take charge of medicine for the<br />
sake of our patients.<br />
6 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Weighing the Radiation Risks of CT Scans<br />
Nikta Forghani, M.D., Ronald A. Cohen, M.D., and Myles B. Abbott, M.D.<br />
Computed tomographic (CT) scanning<br />
is a valuable imaging modality<br />
on which pediatricians increasingly<br />
rely. However, pediatricians may not realize<br />
that CT scans expose children to high amounts<br />
of ionizing radiation that may have detrimental<br />
long-term consequences. Recent data from<br />
studies of survivors exposed to low-dose radiation<br />
from the atomic bombs in Hiroshima and<br />
Nagasaki 1 , and the increased risk of leukemia<br />
in children who have two or more radiologic<br />
procedures 2 , suggest that pediatricians should<br />
be more circumspect when ordering CT scans.<br />
More than two million CT scans are done<br />
on children each year in the United States. 3 The<br />
use of CT imaging in both adults and children<br />
has increased by 700% over the past ten years 3 ,<br />
although it has been estimated that 40% of CT<br />
scans performed on children are unnecessary. 4<br />
This increase is in large part due to the fact that<br />
CT imaging has been more widely recognized<br />
as a superior imaging modality for many clinical<br />
problems. While CT imaging has enormous<br />
diagnostic benefit, its widespread use is a<br />
source of potential harm, especially to pediatric<br />
patients. The National Research Council’s<br />
Factors and Procedures<br />
Yearly exposure at sea level 3<br />
Living in Denver (high altitude) 6<br />
Transcontinental flight 0.25<br />
Committee on the Biological Effects of Ionizing<br />
Radiation on Children has determined<br />
that children under 10 years of age are several<br />
times more sensitive to ionizing radiation than<br />
middle-aged adults. 5 In addition, since children<br />
have a longer life span, their potential longterm<br />
risk of radiation damage is increased.<br />
Furthermore, some of the new advances in<br />
CT technology make the scans faster and<br />
more accurate (and therefore more appealing<br />
in the context of pediatric radiology), but may<br />
come with a price of higher ionizing radiation<br />
exposure.<br />
To appreciate the amount of radiation<br />
in a CT scan, it may be helpful to compare<br />
CT radiation with both a standard chest X-<br />
ray and the background radiation to which<br />
we are all exposed in the environment. The<br />
exposure from an abdominal CT scan is 5 to<br />
10 millisieverts (mSv) 1 , which is 250 to 500<br />
times greater radiation than a standard chest<br />
radiograph (which is .02 mSv). The amount of<br />
background radiation varies in different locations,<br />
but the average background radiation in<br />
the United States (excluding medical sources)<br />
is about 3 mSv per year. The table shows the<br />
Table: Representative Values of Effective Radiation Doses Associated with<br />
Various Environmental Factors and Medical Procedures 7, 8<br />
Chest X-ray 0.02 – 0.05<br />
Skull X-ray<br />
Abdominal X-ray<br />
Intravenous pyelogram<br />
Upper gastrointestinal series<br />
Barium Enema<br />
Head CT<br />
Chest CT<br />
Abdominal CT<br />
Ultrasonography 0<br />
Magnetic Resonance Imaging 0<br />
Effective dose in mSv<br />
0.1– 0.2<br />
0.5 – 1.5<br />
2.5 – 5.0<br />
3.0<br />
3.0 – 7.0<br />
2.0 – 4.0<br />
5.0 – 15.0<br />
5.0 – 15.0<br />
approximate amount of radiation associated<br />
with various environmental factors, medical<br />
procedures involving ionizing radiation, and<br />
medical procedures that do not expose patients<br />
to radiation.<br />
Much of the current concern about the<br />
effects of ionizing radiation on children stems<br />
from recently published research about cancer<br />
risk in atomic bomb survivors. Today, more<br />
than 50 years after their initial exposure,<br />
individuals have been identified who received<br />
radiation doses that are similar to doses<br />
achieved with modern CT scans (8-30 mSv).<br />
The research shows that these individuals have<br />
a small but statistically significant increased<br />
mortality risk from cancer.<br />
Pediatricians and pediatric radiologists<br />
ought to work collaboratively to determine the<br />
best imaging technique for each patient. When<br />
non-radiation modalities (ultrasonography or<br />
MRI) are as diagnostic as CT for the child’s<br />
condition, they should be preferred. However,<br />
CT scans are often the most appropriate imaging<br />
modality. When CT is used, there are ways<br />
to reduce the exposure to radiation:<br />
• Reduce CT settings, which can be<br />
done without significantly compromising<br />
image quality. In one recent trial, ionizing<br />
radiation exposure in children was reduced by<br />
75% while quality was maintained. 6<br />
• Utilize more focused or limited CT<br />
scans to minimize the extent of radiation exposure.<br />
For example, when trying to identify a<br />
hepatic abnormality, CT can focus on the liver<br />
rather than the entire abdomen and pelvis.<br />
• Perform only the minimum number<br />
of CT scans necessary for the diagnosis. There<br />
are very few circumstances when multiple CT<br />
scans are necessary.<br />
• Be judicious in repeating CT scans<br />
to follow a pathologic process. Consider other<br />
imaging modalities to follow the process.<br />
REFERENCES:<br />
1. Pierce DA, Preston DL. Radiation-related<br />
cancer risks at low doses among atomic<br />
bomb survivors. Radiation Research. 2000;<br />
154:178-186.<br />
2. Infante-Rivard C, Mathonnet G, Sinnett D.<br />
Risk of childhood leukemia associated with<br />
CONTINUED ON PAGE 28<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 7
Adolescent Idiopathic Scoliosis<br />
While it is normal for the spine<br />
to have curvatures in the lateral<br />
plane (lordosis in the lumbar and<br />
cervical regions and kyphosis in the thoracic<br />
region), the spine is normally straight when<br />
viewed from the frontal plane. Scoliosis is a lateral<br />
curvature of the spine, and is always abnormal.<br />
The term scoliosis is derived from the<br />
Greek term ‘scolio’ (curved or bent). There are<br />
many causes of scoliosis but the most common<br />
is adolescent idiopathic scoliosis (AIS), which<br />
accounts for a great majority of cases. This is<br />
a structural (stiff) curve with rotation of the<br />
spine that occurs at or near the onset of puberty<br />
without an established cause. A variety of possible<br />
etiological factors have been implicated,<br />
including hormones, genetic predisposition,<br />
muscular imbalance and neurologic abnormalities.<br />
However, no direct link between these factors<br />
and the development of scoliosis have been<br />
established in this population.<br />
The diagnosis of AIS is suspected by the<br />
presence of asymmetry on the Adams forward<br />
bend test. However, some children may have<br />
muscular asymmetry without a true scoliosis.<br />
In addition, care should be taken to account<br />
for any leg-length discrepancy (LLD) as this<br />
can also produce asymmetry of the spine and<br />
a lateral curvature. If scoliosis is suspected,<br />
a standing postero-anterior (PA) radiograph<br />
should be obtained. A curve of 10 degrees or<br />
greater confirms the diagnosis of scoliosis. The<br />
prevalence in the adolescent population (10 to<br />
16 yrs) is approximately 2 to 3%. The female:<br />
male ratio for smaller curves is almost equal,<br />
whereas the female:male ratio for larger curves<br />
is 3.6:1.<br />
The history should include any family<br />
history of scoliosis or other back problems,<br />
prior lower extremity fracture, any neurologic<br />
complaints (including bowel and bladder<br />
function) as well as any history of back pain.<br />
Pain is not normally associated with AIS,<br />
whereas painful scoliosis may be the result of<br />
a herniated disk or tumor. A careful physical<br />
examination should include an evaluation for<br />
LLD and inspection of the back and skin for<br />
any abnormal skin markings, dimples or hairy<br />
patches that may indicate an underlying spinal<br />
cord abnormality. The entire body should be<br />
inspected for the presence of cafe au lait spots<br />
or other manifestations of neurofibromatosis.<br />
Finally, a detailed neurologic examination<br />
including upper and lower extremity motor<br />
Robert M. Bernstein, M.D.<br />
strength, sensation, and reflexes should be<br />
undertaken. Abdominal reflexes (stroking each<br />
side of the umbilicus gently with a blunt object<br />
should result in equal movement of the umbilicus<br />
toward the stimulated side) should also<br />
be checked as asymmetry of this reflex may<br />
indicate intra-spinal pathology.<br />
Pain, asymmetry of abdominal reflexes,<br />
or any abnormal neurologic finding may indicate<br />
an underlying spinal cord abnormality and<br />
should be investigated. The incidence of spinal<br />
cord abnormality (syrinx or chiari malformation)<br />
is extremely low in AIS, and in general,<br />
only a plain radiograph (PA) need be obtained.<br />
PA radiographs are preferred over anteroposterior<br />
radiographs because the radiation<br />
exposure of the breast is minimized. Curves<br />
measuring less than 10 0 should be considered<br />
a normal variant and do not require further<br />
evaluation. In addition, it should be kept in<br />
mind that labeling the child with a diagnosis of<br />
scoliosis may have implications with respect to<br />
future insurability.<br />
The majority of children with AIS will<br />
never require active treatment (less than 10%).<br />
The natural history is related to a number of<br />
factors: the age (maturity) of the patient, the<br />
location of the curve, the curve pattern, and the<br />
size of the curve. Younger patients have more<br />
potential growth and thus have a greater risk<br />
of curve progression. Curves in the thoracic<br />
region are stabilized by the ribs and thus are<br />
less likely to progress than lumbar and thoraco-lumbar<br />
curves. Double curves are more<br />
likely to progress than single curves, and larger<br />
curves are more likely to progress than smaller<br />
ones.<br />
Once the patient reaches skeletal maturity,<br />
curve progression slows dramatically or stops.<br />
Thoracic curves under 30 0 don’t progress after<br />
skeletal maturity. Those curves between 30 0<br />
and 50 0 may progress but do so very slowly.<br />
However, thoracic curves between 50 0 and 75 0<br />
have the greatest risk of progression and may<br />
do so at up to 1 0 per year. The biggest concern<br />
with thoracic curves is the loss of normal<br />
thoracic kyphosis. Loss of kyphosis with progression<br />
of the curve can result in a decrease<br />
in pulmonary function. This loss of function<br />
is measurable when the curve reaches 60 0 to<br />
70 0 , but will not be noticeable to the patient<br />
until the curve reaches over 100 0 . Lumbar<br />
and thoraco-lumbar curves under 30 0 tend not<br />
to progress after maturity. Those greater than<br />
30 0 will progress but the extent of progression<br />
is difficult to predict. They may result in a<br />
significant trunk asymmetry that is cosmetically<br />
displeasing to the patient and family. The<br />
association between curve magnitude and a<br />
decrease in pulmonary function only occurs<br />
with thoracic curves and does not apply to<br />
lumbar and thoraco-lumbar curves.<br />
Treatment may involve simple observation,<br />
bracing, or surgery. While exercises and<br />
electrical stimulation have been utilized in the<br />
past, there is no evidence that these modalities<br />
affect curve progression. In addition, recent<br />
literature has not shown any benefit from<br />
chiropractic manipulation. As the majority<br />
of AIS curves are small and thus have a low<br />
likelihood of progression, most patients will<br />
simply require regular follow-up visits with<br />
radiographs to look for curve progression.<br />
Bracing is instituted in skeletally immature<br />
patients in order to prevent the curve<br />
from achieving a magnitude that will continue<br />
to progress after maturity. Once the brace is<br />
removed, the curve usually returns to its prebrace<br />
magnitude. A brace is recommended<br />
when progression has been documented in<br />
curves under 30 0 , for those curves measuring<br />
30 0 -40 0 on initial presentation, and occasionally<br />
for somewhat larger curves. Curves over<br />
50 0 are likely to progress even after maturity<br />
and thus are generally not brace candidates.<br />
The current surgical treatment for scoliosis<br />
is spinal fusion, usually with instrumentation.<br />
The primary goal of fusion is to<br />
prevent further progression of the curve, and a<br />
secondary goal is to improve cosmetic appearance,<br />
usually by decreasing the size of the<br />
curve using rods, hooks, wires, and/or screws.<br />
Reducing the curve size is only important to<br />
the patient in how it affects their appearance,<br />
and this must be balanced with the risk of<br />
neurologic injury. As a general rule, the curve<br />
can safely be reduced by about 50% its original<br />
size. The indications for surgery vary and are<br />
related to curve magnitude, progression, curve<br />
pattern, and cosmetic appearance. Once a thoracic<br />
curve has reached 50 0 , the risk of progression<br />
after skeletal maturity is high and most of<br />
these patients should undergo fusion. Curves<br />
over 40 0 that progress in spite of bracing are<br />
also fusion candidates. The indications for surgery<br />
in the lumbar and thoraco-lumbar spine<br />
is more controversial. If little trunk imbalance<br />
is present, no intervention may be the best<br />
approach, as fusing into the lumbar spine significantly<br />
affects mobility and may increase the<br />
risk of back pain. However, curves that create<br />
significant trunk imbalance may be candidates<br />
for surgery from a cosmetic standpoint.<br />
The choice between posterior spinal<br />
fusion, anterior spinal fusion, or both is somewhat<br />
surgeon dependant and is also related to<br />
the location of the curve, risk factors for non-<br />
CONTINUED ON PAGE 26<br />
8 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Preventing Ear Infections in Children<br />
Harry Pellman, M.D.<br />
Acute Otitis Media (AOM) is the<br />
most common bacterial infection<br />
diagnosed in children and the most<br />
common reason antibiotics are prescribed in<br />
this age group. Despite these facts, there is still<br />
quite a bit of controversy on how to best make<br />
the diagnosis of AOM and a good strategy for<br />
treating these infections. The American Academy<br />
of Pediatrics is intently working on new<br />
guidelines for the diagnosis and treatment of<br />
acute otitis media (AOM) in children.<br />
There are a variety of strategies known to<br />
reduce the frequency of middle ear problems.<br />
Implementing as many of these strategies as<br />
possible may be like closing the barn door<br />
before the cows get out.<br />
Breast feeding has been clearly shown to<br />
reduce both the incidence of AOM and<br />
otitis media with effusion (OME) in<br />
multiple studies. The protective effect is<br />
related to the duration and exclusivity of<br />
breast feeding and is most prevalent in<br />
infancy.<br />
Avoid environmental tobacco poisoning<br />
(aka cigarette smoking). This type of air<br />
pollution is clearly related to more AOM<br />
and OME.<br />
When bottle feeding, use fully vented bottles.<br />
Fully vented bottles allow air inflow<br />
as the milk exits the bottle and prevents<br />
negative middle ear pressure. Negative<br />
pressure in the middle ear promotes the<br />
entrance of nasopharyngeal contents into<br />
the middle ear chamber. Children using<br />
fully vented bottles have middle ear pressures<br />
that appear to be similar to infants<br />
breast feeding.<br />
Use of pacifiers beyond 18-24 months of age<br />
has been associated with more middle ear<br />
disease. The reason for this association is<br />
not clear. Whether this occurs because<br />
of abnormal pressures generated in the<br />
middle ear, more viral infections associated<br />
with pacifier use, or another mechanism<br />
is unknown.<br />
There are a variety of strategies known to reduce the frequency<br />
of middle ear problems. Implementing as many of these<br />
strategies as possible may be like closing the barn door before<br />
the cows get out.<br />
There is a suggestion that babies that have gastroesophageal<br />
reflux disease (GERD)<br />
have a higher incidence of middle ear<br />
disease. In one study, middle ear fluid<br />
obtained from children having myringotomy<br />
and tube insertion revealed pepsin<br />
and pepsinogen levels 1000 times higher<br />
than serum levels in more than 80% of<br />
children. Ongoing investigations will help<br />
clarify this issue.<br />
Daycare is associated with both an increased<br />
incidence of middle ear disease and the<br />
presence of more resistant bacteria when<br />
infections occur. Of course, daycare<br />
is essential for many working parents.<br />
Training daycare workers to wash hands<br />
frequently and employ hygienic measures<br />
is a Herculean task.<br />
Vaccines will have a dramatic impact on<br />
AOM. Prevnar vaccine provides significant<br />
protection against the seven strains of<br />
streptococcus pneumonia (in the past, the<br />
most common bacteria isolated in AOM)<br />
in the vaccine plus five cross-reacting<br />
strains. The vaccine has only reduced the<br />
overall incidence of AOM about 5-10%.<br />
However, the serotypes of streptococcus<br />
pneumonia present in the vaccine are both<br />
some of the most common bacteria present<br />
in AOM and the most resistant and<br />
difficult to treat bacteria we encounter.<br />
This vaccine has reduced the necessity<br />
for ear tubes about 20%, the frequency<br />
of having multiple episodes of AOM in<br />
an infection-prone child up to 20%, and<br />
changed the bacteriology of AOM so that<br />
non-typable hemophilus influenza bacteria<br />
is now the most common bacteria isolated<br />
in AOM in children vaccinated with<br />
prevnar. Work is presently being done<br />
on a nine-valent pneumococcal vaccine<br />
and a non-typable hemophilus influenza<br />
vaccine. Their impact on reducing AOM<br />
remains to be seen.<br />
Since most episodes of AOM follow viral<br />
respiratory illnesses, it appears that<br />
reducing these illnesses will lessen the<br />
frequency of AOM. Influenza vaccine,<br />
especially the newly released coldadapted<br />
live influenza vaccine, has been<br />
shown to effectively lessen the incidence<br />
of AOM. If a safe, effective RSV vaccine<br />
is ever approved by the FDA, we should<br />
expect a further reduction in AOM episodes.<br />
Xylitol is a natural, non-absorbable sugar most<br />
commonly harvested from birch trees.<br />
Xylitol chewing gum has been used in<br />
Finland for many years to reduce the<br />
incidence of dental caries, an infectious<br />
disease caused by strep mutans. Children<br />
on long term xylitol chewing gum were<br />
found to have as much as 40% fewer<br />
episodes of AOM. However, if used only<br />
during a high risk period, such as a viral<br />
respiratory infection, xylitol may not be<br />
protective. The usefulness of xylitol in<br />
other forms (syrup, lozenges, etc.) is still<br />
being investigated.<br />
There is a suggestion that iron deficiency<br />
anemia may be associated with an<br />
increased risk of AOM.<br />
It sounds like the ideal situation for maximum<br />
middle ear health is an infant exclusively<br />
breast fed for at least six months, living in a<br />
healthful environment without daycare, no<br />
pacifiers, bottles (if used) should be fully<br />
vented, kept on an iron rich diet, fully vaccinated,<br />
properly positioned to lessen GERD,<br />
and chewing xylitol chewing gum when old<br />
enough to do so.<br />
If employing the above strategies fails to<br />
reduce the incidence of ear infections, since<br />
frequent AOM seems to have some kind of<br />
genetic link, the child should consider choosing<br />
different parents!<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 9
A Low-Glycemic Index Diet in the<br />
Treatment of Pediatric Obesity<br />
Leshe E. Spieth, PhD; Jennifer D. Harnish, PhD; Carine M. Lenders, MD, MS; Lauren B. Raezer, PhD;<br />
Mark A. Pereira, PhD; S. Jan Hangen, MS, RD; David S. Ludwig, MD, PhD<br />
This article has been excerpted from one<br />
printed in Archives of Pediatric Adolescent<br />
Medicine, September 2000, pages 47-51.<br />
Reprinted with permission. Copyright 2000,<br />
American Medical Association.<br />
EXCESSIVE BODY weight is arguably<br />
the most prevalent medical problem<br />
in the United States today. Approximately<br />
25% of children and more than 50% of<br />
adults are considered overweight according to<br />
data from the most recent National Health and<br />
Nutrition Examination Survey. 1,2 Overweight<br />
and obesity in childhood contribute to a range<br />
of immediate and long-term problems, including<br />
diabetes mellitus, dyslipidemia, hypertension,<br />
sleep apnea, musculoskeletal problems,<br />
gastrointestinal disease, and psychosocial<br />
difficulties. Overweight children, especially<br />
those older than seven years, are at increased<br />
risk for obesity and cardiovascular disease in<br />
adulthood.<br />
The standard approach to the treatment<br />
of obesity involves the reduction of dietary<br />
fat, the most energy-dense nutrient. The US<br />
Department of Agriculture, the American<br />
Heart Association (Dallas, Tex), and the<br />
American Diabetes Association (Alexandria,<br />
VA) currently recommend reduced-fat diets in<br />
the prevention and treatment of obesity. However,<br />
weight loss on reduced-fat diets is characteristically<br />
modest and transient. Moreover,<br />
prevalence rates of overweight and obesity<br />
have risen dramatically in recent years, despite<br />
decreases in dietary fat as a percentage of total<br />
energy to near recommended levels.<br />
Recently, a low-glycemic index (GI) diet<br />
has been proposed as a novel treatment for<br />
obesity. Glycemic index refers to the relative<br />
rise in blood glucose occurring after consumption<br />
of a food containing a standard amount of<br />
carbohydrate. Most refined grain products and<br />
potatoes have a high GI, whereas nonstarchy<br />
vegetables, legumes, and fruits generally have<br />
a low GI. The glycemic response to a meal<br />
increases with the carbohydrate content and<br />
GI of the component foods, but decreases with<br />
fiber, protein, and fat content. 19-22 Glycemic<br />
index may affect hunger through effects on<br />
pancreatic hormone secretion that, in turn,<br />
alter availability of metabolic fuels after a<br />
meal. Of 16 studies published to date relating<br />
GI to hunger, satiety, or voluntary food<br />
intake, 15 demonstrated beneficial effects of<br />
low-compared with high-GI meals. However,<br />
the effects of GI on body weight have not been<br />
examined.<br />
The purpose of this study was to evaluate<br />
the effects of a low-GI diet in a pediatric outpatient<br />
setting. Specifically, we sought to test the<br />
hypothesis that a low-GI diet would result in<br />
greater weight loss compared with a reducedfat<br />
diet among obese children remaining in<br />
outpatient treatment for at least one month.<br />
Participants and Methods<br />
STUDY DESIGN<br />
During the period between September 1, 1997<br />
and August 31, 1998, children attending the<br />
Optimal Weight for Life Program at Children’s<br />
Hospital, Boston, Massachusetts, for treatment<br />
of obesity were assigned by the program<br />
administrator, based on schedule availability,<br />
to one of two teams, each composed of a subspecialty-trained<br />
pediatrician, a dietitian, and<br />
at times a pediatric nurse<br />
practitioner. One team<br />
prescribed a low-GI diet,<br />
the other a reduced-fat<br />
diet. Except for specific<br />
dietary recommendations,<br />
each team provided similar<br />
diagnostic evaluation and<br />
treatment. To estimate the<br />
effects of dietary treatment<br />
on body fatness, we<br />
retrospectively examined<br />
the changes in body mass<br />
index (BMI [calculated<br />
as weight in kilograms<br />
divided by the square of<br />
height in meters]) and<br />
body weight from the participant’s<br />
initial visit to last<br />
visit before December 31,<br />
1998, according to dietary<br />
treatment assignment.<br />
PARTICIPANTS<br />
A total of 190 patients<br />
(excluding those with<br />
Cushing syndrome, hypothyroidism,<br />
hypothalamic<br />
disease, diabetes mellitus or an obesity-associated<br />
genetic syndrome, or those currently<br />
following a very low-energy diet) were<br />
evaluated during the study period. We further<br />
excluded 83 individuals for lack of follow-up<br />
(< 1 month) and/or incomplete data, leaving a<br />
cohort of 107. Descriptive characteristics of<br />
this cohort are presented in Table 1.<br />
STANDARD TREATMENT COMPONENTS<br />
All patients received a comprehensive medical<br />
evaluation (medical history, physical examination,<br />
and laboratory investigation), dietary<br />
counseling, and lifestyle counseling (recommendations<br />
were based on decreasing physical<br />
inactivity and increasing physical activity).<br />
Counseling sessions included the child and<br />
at least one parent, when possible, according<br />
to established practice. Specific goals were<br />
individualized, with consideration given to the<br />
patient’s developmental level and readiness to<br />
change. Follow-up appointments were generally<br />
recommended to occur on a monthly basis for<br />
the first four months, and then as needed.<br />
10 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
In addition, problem-focused behavior<br />
therapy was provided by the program psychologist<br />
on an individual basis when referred<br />
by a team member. Within these sessions, a<br />
particular nutritional or physical activity goal<br />
was identified as a primary treatment target. A<br />
behavioral program was then developed, using<br />
positive reinforcement for meeting the specified<br />
goal. Specifics of treatment were adapted<br />
according to the patient’s age and developmental<br />
stage.<br />
DIETARY TREATMENTS<br />
One team prescribed a standard balanced,<br />
hypoenergetic reduced-fat diet because of<br />
research demonstrating improvements in<br />
adiposity on this diet when combined with<br />
behavioral modification and exercise. 26, 27 The<br />
diet followed US Department of Agriculture<br />
recommendations for intake of specific food<br />
types, as depicted by the Food Guide Pyramid.<br />
Particular emphasis was placed on limiting<br />
intake of high-fat, high-sugar, and energydense<br />
foods, and increasing intake of grain<br />
products, vegetables, and fruit.<br />
Recommendations were tailored on an<br />
individual basis to incorporate an energy<br />
restriction of approximately 1042 kJ (250<br />
kcal) to 2084 kj (500 kcal) per day compared<br />
with usual energy intake. Specific macronutrient<br />
goals were 55% to 60% carbohydrate, 15%<br />
to 20% protein, and 25% to 30% fat.<br />
The other team prescribed a low-GI diet<br />
because of preliminary research suggesting<br />
a physiologic mechanism relating GI to<br />
body weight regulation. 16,17 The low-GI diet<br />
was designed to obtain the lowest glycemic<br />
response possible while providing adequate<br />
dietary carbohydrates, satisfying all nutritional<br />
recommendations for children, and maintaining<br />
palatability. This diet differed from the<br />
standard diet not just in the GI of the component<br />
carbohydrates foods, but also in the macronutrient<br />
ratio. Emphasis was placed on food<br />
selection, not energy restriction: patients were<br />
instructed to eat to satiety and snack when<br />
hungry. Specifically, patients were told to<br />
combine low-GI carbohydrate, protein, and fat<br />
at every meal and snack. A “Low-GI Pyramid,”<br />
modeled after the Food Guide Pyramid, was<br />
used as a teaching tool. This modified pyramid<br />
placed vegetables, legumes, and fruits at the<br />
base, lean proteins and dairy products on the<br />
second level, whole-grain products on the third<br />
level, and refined grain products, potatoes, and<br />
concentrated sugars at the top. Specific macronutrient<br />
goals were 45% to 50% carbohydrate,<br />
20% to 25% protein, and 30% to 35% fat.<br />
Results<br />
Characteristics of the cohort are described in<br />
Table 1 according to dietary treatment group.<br />
Mean age, length of follow-up, number of<br />
visits, and sex were similar between the two<br />
treatment groups. Baseline BMI and body<br />
weight were slightly greater in the reduced-fat<br />
group compared with the low-GI group, but<br />
the difference was not statistically significant.<br />
Ethnicity differed in the study cohort primarily<br />
owing to different follow-up rates (of the 190<br />
patients before exclusion for lack of follow-up,<br />
white subjects comprised 71% of 118 individuals<br />
assigned to the low-GI group vs. 67% of 72<br />
individuals assigned to the reduced fat group).<br />
The figure depicts the mean change in<br />
BMI from the participant’s first to last clinic<br />
visit according to dietary treatment and baseline<br />
BMI tertile. For each BMI tertile, the low-<br />
GI group had a significantly larger decrease in<br />
BMI than the reduced-fat group. Compared<br />
with the reduced-fat group, a larger percentage<br />
of patients in the low-GI group experienced a<br />
decrease in BMI of at least -3 kg/m2 (11 participants<br />
[17.2%] vs. one participant [2.3%]. As<br />
presented in Table 2, the overall mean change<br />
in BMI for the low-GI group was -1.53 kg/m2,<br />
compared with -0.06 kg/m2 for the reducedfat<br />
group (P
Why California’s MICRA Is Good for the Nation<br />
Ron Bangasser, M.D.<br />
The National Medical<br />
Liability Crisis<br />
It is upsetting to watch physicians walk<br />
off their jobs to protest the cost of medical<br />
liability insurance in New Jersey, Nevada,<br />
Mississippi, West Virginia and Florida. But it<br />
would be far more upsetting if there were no<br />
doctors at all to provide surgery, trauma care,<br />
diagnose illnesses and deliver babies. Some<br />
of these physicians are being charged up to<br />
$200,000 annually for their liability coverage,<br />
and like the proverbial canary in the coalmine,<br />
these physicians are trying to warn us about a<br />
coming national health care crisis.<br />
California faced a similar calamity in the<br />
1970s. Malpractice insurance was soaring with<br />
some physicians expecting 400% premium<br />
increases. Worried that soaring costs would<br />
drive physicians from California and leave<br />
patients without care, then-Gov. Jerry Brown<br />
called a special session of the legislature to<br />
solve the medical liability crisis.<br />
California’s MICRA<br />
The solution then, and now, was the Medical<br />
Injury Compensation Reform Act. Before<br />
MICRA, California malpractice premiums<br />
were among the nation’s highest. But post-<br />
MICRA, rates in California stabilized. Take a<br />
look at the impact on rates beginning in 1986,<br />
the year legal challenges to the law were finally<br />
exhausted. From 1986 to 2000, premiums fell<br />
12% in California, while rising 55% nationally<br />
(inflation adjusted dollars). During that same<br />
period, rates in Florida rose 809%; in Nevada<br />
8375%!<br />
Under our forward-thinking law, injured<br />
patients are entitled to unlimited medical and<br />
economic compensation, which often amount<br />
to millions of dollars to cover true damages,<br />
such as lost wages, medical expenses, rehabilitation,<br />
psychotherapy and long-term care<br />
costs. Physicians support such full compensation<br />
of injured patients. And under MICRA,<br />
patients can also recover an additional quarter<br />
of a million dollars in non-economic or “pain<br />
and suffering” awards. The law also limits<br />
contingency legal fees so that seriously injured<br />
patients get more (and their attorneys correspondingly<br />
less) of the award.<br />
Regardless, the law remains under siege<br />
from trial lawyers. But the number of medical<br />
malpractice suits has remained stable and<br />
From 1986 to 2000, premiums fell 12% in California, while rising<br />
55% nationally (inflation adjusted dollars). During that same<br />
period, rates in Florida rose 809%; in Nevada 8375%!<br />
awards have risen far faster than inflation since<br />
1986, indicating injured patients retain their<br />
access to the courts and fair recovery. And in<br />
California, injured patients are compensated<br />
more quickly than in all states but Minnesota.<br />
The real reason personal injury lawyers hate<br />
MICRA is that it limits the money they make<br />
from patient misfortune. Trial lawyers are not<br />
an endangered species. But physicians, emergency<br />
rooms and safety-net programs for the<br />
uninsured are truly threatened, and everyone’s<br />
access to care is endangered without reform.<br />
Stabilizing insurance premiums is particularly<br />
essential for the poor, who get their health care<br />
from economically fragile medical clinics and<br />
health centers.<br />
It’s MICRA, NOT Proposition 103<br />
The suggestion that Prop 103 forced medical<br />
liability rates down in California is clever<br />
but lacks any foundation in fact. MICRA was<br />
enacted in 1975 but was immediately challenged<br />
in the courts. Until the legal challenges<br />
were resolved and the courts and lawyers<br />
got comfortable with the application of its<br />
various provisions, there were no savings from<br />
MICRA. After the lead case of Fein v. Kaiser<br />
Permanente was decided in 1985 it took several<br />
years for the judgments and settlements to<br />
show a downward trend.<br />
When Prop 103 was passed in 1989,<br />
the California medical liability insurers were<br />
already returning MICRA savings to physicians<br />
in the form of policyholder dividends.<br />
Several had filed for rate reductions but found<br />
the California Department of Insurance reluctant<br />
to even approve rate reductions until the<br />
legal status of PROP 103 was resolved. To<br />
break the logjam, the physician owned companies<br />
met with Commissioner John Garamendi<br />
shortly after he was elected. The commissioner<br />
examined the medical liability rates and found<br />
them appropriate. No rollbacks were required<br />
and the policyholder dividends that the companies<br />
were paying were accepted in lieu of<br />
a rollback refund. Commissioner Garamendi<br />
and his staff did not interfere in any way with<br />
the medical liability rates. Not a single medical<br />
liability rate filing has been denied in California<br />
since Prop 103 was enacted.<br />
In addition to rate reductions voluntarily<br />
undertaken by physician owned medical<br />
liability insurers in California since 1989, the<br />
physician owned companies have voluntarily<br />
returned to California physicians over half a<br />
billion dollars in policyholder dividends in the<br />
1990s in response to savings realized through<br />
application of MICRA. Since Prop 103 does<br />
not affect policyholder dividends, these reductions<br />
cannot be attributed to Prop 103.<br />
MICRA has kept premiums in California<br />
fair and predictable, not Proposition 103. This<br />
is a clever trick by the trial lawyers, but has<br />
no basis in fact. When Prop. 103 was passed<br />
in 1989, the California medical liability insurers<br />
were already returning MICRA savings to<br />
physicians in the form of policyholder dividends.<br />
Before MICRA, California physicians<br />
paid the highest malpractice premiums in the<br />
country. Today they pay a fair share — 11 %<br />
of the total premiums across the country for a<br />
state that has about 12 percent of the national<br />
physician population. Furthermore, using real<br />
dollars, the cost of California premiums has<br />
gone down 51.9% since 1976, compared to a<br />
crisis state like Nevada who has seen the average<br />
premium cost per person go from $4.05 in<br />
CONTINUED ON PAGE 30<br />
12 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Ten-Year Experience<br />
with Pediatric Bilateral<br />
Living Donor Lobar Lung<br />
Transplantation<br />
Marlyn S. Woo, M.D. and Vaughn A. Starnes, M.D.<br />
running out of options<br />
for this kid,” said the voice<br />
“We’re<br />
on the phone. My heart<br />
sank at that statement from an experienced<br />
physician. He had called to discuss his patient<br />
referral that had arrived at our office only a few<br />
days earlier. He had been unable to keep the<br />
ten-year old boy out of the hospital for more<br />
than a few weeks at a time, even though the<br />
child had been on almost continuous intravenous<br />
antibiotic therapy for several months. The<br />
young boy was oxygen-dependent and could<br />
not walk more than a few steps without dyspnea.<br />
He could only speak two to three words<br />
without pausing for breath. The medical team<br />
had exhausted all conventional medical and<br />
surgical options. What about lung transplantation<br />
for this dying patient?<br />
In the past, children with end-stage lung<br />
disease were not likely to survive to receive<br />
cadaveric lung transplantation unless they<br />
were referred as soon as they entered the terminal<br />
stage of their disease. Unlike heart or<br />
liver transplant candidates, cadaveric lungs<br />
available for transplant are allocated based<br />
upon the blood type, size needed, and how<br />
long the candidate has been waiting on the<br />
list. Although lung transplant candidates with<br />
idiopathic pulmonary fibrosis get three months<br />
of time added at their initial listing, cystic<br />
fibrosis and primary pulmonary hypertension<br />
patients with type O or A blood types must<br />
wait over a year (at times, five years!) before<br />
a suitable cadaveric organ becomes available.<br />
This situation puts these fragile children at a<br />
disadvantage compared to the adult lung transplant<br />
candidates (the primary adult diagnosis is<br />
chronic obstructive pulmonary disease), who<br />
comprise the majority of the cadaveric lung<br />
transplant candidates. Thus, it is not surprising<br />
that children are far more likely to die than<br />
adults while awaiting lung transplantation.<br />
The majority of pediatric lung transplant<br />
candidates have cystic fibrosis as their primary<br />
diagnosis. Hence, these patients with purulent<br />
lung disease require double lung transplantation,<br />
which also contributes to their increased<br />
delay in obtaining suitable cadaveric organs. It<br />
was in this milieu that the first human bilateral<br />
living donor lobar lung transplantation was<br />
performed. The patient was a 21-year old girl<br />
with end-stage cystic fibrosis lung disease,<br />
who had been listed for cadaveric lungs for<br />
several months. She had been hospitalized for<br />
several weeks and was not expected to survive<br />
for more than a few weeks. Her parents asked<br />
the transplant surgeon (Starnes) if they could<br />
donate portions of their lungs to save her.<br />
Dr. Starnes had already performed successful<br />
human single lobar lung transplantation. After<br />
clearance with the hospital Ethics Committee<br />
as well as the Institutional Review Board, the<br />
successful surgery took place January 1993 at<br />
USC University Hospital. A few months later<br />
(May 1993), the first successful human pediatric<br />
bilateral lobar lung transplantation took<br />
place at Childrens Hospital Los Angeles. The<br />
pediatric patient was a 13-year-old male who<br />
also had end-stage cystic fibrosis lung disease.<br />
Since those first cases, over 150 living<br />
donor bilateral lobar lung transplants have<br />
been performed throughout the world. While<br />
the majority have occurred in adult and pediatric<br />
cystic fibrosis patients, this procedure has<br />
also been successfully utilized for patients with<br />
primary pulmonary hypertension, non-transplant<br />
bronchiolitis obliterans, primary ciliary<br />
dyskinesis, and severe bronchiectasis. As of<br />
January <strong>2003</strong>, Childrens Hospital Los Angeles<br />
has performed 45 bilateral living donor lobar<br />
lung transplants in children. Although living<br />
donor lobar lung transplant recipients are generally<br />
more ill than our cadaveric candidates,<br />
there has been no significant differences in<br />
length of intubation, post-operative ICU stay,<br />
total length of hospitalization, or in perioperative<br />
mortality between these two groups.<br />
Although both cadaveric and living donor<br />
recipients receive the same triple immunosuppression<br />
therapy, pediatric living donor lobar<br />
lung transplant recipients have better one year<br />
survival and a significantly lower incidence of<br />
chronic rejection/bronchiolitis obliterans syndrome<br />
compared to cadaveric lung transplant<br />
recipients at our institution. So should living<br />
donor lobar lung transplantation be preferentially<br />
performed in all pediatric lung transplant<br />
candidates? There are several obstacles to performing<br />
living donor lobar lung transplantation<br />
in all pediatric candidates.<br />
Living donor lobar lung transplant candidates<br />
must meet the same criteria as those<br />
being considered for cadaveric organs (Table<br />
1). They must be healthy enough to survive<br />
major surgery. Importantly, they must also<br />
have at least two healthy donors acceptable<br />
to the Transplant Team (Table 2). Our Center,<br />
as well as the other United States Transplant<br />
Centers who have performed more than living<br />
donor lobar procedures, do not accept living<br />
donor lobar candidates who have no emotional<br />
attachment to the proposed recipient or family;<br />
solicited or “stranger” volunteers; nor donor<br />
candidates who have been coerced (selling<br />
organs). Interestingly, over half of the living<br />
lobar lung transplants have utilized lobes<br />
donated by healthy adults who are not related<br />
to the recipients.<br />
CONTINUED ON PAGE 20<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 13
The Tao of Pediatrics and<br />
Chinese Medicine<br />
Wendy Yu, M.S., L.Ac., Jeffrey I. Gold, Ph.D., Michael H. Joseph, M.D.<br />
Tao means “the path” and according<br />
to one of the most ancient recorded<br />
texts, the Tao of the universe is<br />
“change.” This is particularly relevant to<br />
today’s model of healthcare as it undergoes a<br />
radical paradigm shift: a shift from diseasecentered<br />
care to patient-centered care. As we<br />
realize that health is not just about a disease<br />
factor, it’s about the whole environment, it<br />
is becoming apparent that the treatment of<br />
modern diseases requires more than the traditional<br />
segmented view of the person.<br />
The ancient Taoists were renowned for<br />
the application of intricate and profound philosophies.<br />
One of the greatest of these applications<br />
is in the field of medicine. The ancient<br />
Chinese felt pictures were superior methods of<br />
conveying information. One of their most profound<br />
symbols is the famous Tai Ji (Yin Yang)<br />
Photography by Robin Dixon<br />
symbol. Aside from the expression that energy<br />
equals matter, this symbol also expresses the<br />
interdependence of every part of a system.<br />
Thus, Taoist theory did not separate a disease<br />
from the environment it thrives in.<br />
When treating a disease, the Chinese<br />
used several strategies typically in combination:<br />
attack the disease directly, strengthen<br />
the host to overcome the disease, and change<br />
the environment to where the disease can no<br />
longer sustain itself. How can we apply these<br />
strategies to pediatrics?<br />
Because the ancient Chinese were an<br />
agricultural society, they were very aware of<br />
the interplay between people and their environment.<br />
Thus they described imbalances of the<br />
body in the same way they perceived imbalances<br />
in the environment. There were disease<br />
factors of cold (impeded circulation, organ or<br />
glandular hypofunction), heat (inflammation),<br />
dampness (fungus, molds, yeasts, endogenous<br />
or exogenous toxins), external wind (viruses,<br />
bacteria), internal wind (tics, tremors, seizures)<br />
and dryness (dehydration). These disease factors<br />
could be combined as well, so you could<br />
have wind combining with heat, which could<br />
be a bacteria or virus associated with sore<br />
throat, high fever, rashes and sweating.<br />
To correct imbalances, the Chinese took<br />
a holistic approach. In the above example, not<br />
only would the microorganisms be addressed,<br />
but the internal environment would be altered<br />
and the host strengthened.<br />
This is where Chinese medicine<br />
becomes an art. The<br />
physician must decide which<br />
part of the strategy to prioritize.<br />
For example, in a strong<br />
child, a physician may decide<br />
to attack the microorganism<br />
directly. In a compromised<br />
child, the physician may want<br />
to deal with the microorganism<br />
indirectly by changing<br />
the terrain of the body.<br />
So what does altering<br />
the terrain mean?<br />
The internal environment<br />
is a result of the interaction<br />
of many factors that<br />
include genetics, diet, emotional<br />
factors, and external<br />
environmental factors (such as xenobiotics, climate,<br />
radiation and other geopathic stressors).<br />
Altering the terrain can involve detoxification<br />
of xenobiotics and endotoxins, resolution of<br />
nutritional deficiencies and regulation of other<br />
physiological processes in the body. To accomplish<br />
this, Chinese medicine utilizes a wide<br />
variety of modalities such as acupuncture,<br />
herbal medicine and dietary therapy.<br />
Before applying these therapies, a thorough<br />
evaluation must be performed. In children<br />
it is difficult to rely on subjective complaints so<br />
the Chinese have developed an intricate diagnostic<br />
system based on observation and palpation.<br />
Facial complexion, eyes, hands, nails,<br />
body morphology, tongue, ears, and mouth are<br />
examined. Qualities in the radial and carotid<br />
pulses, variances in temperature and quality at<br />
specific acupoints on the abdomen and along<br />
the paravertebral muscles are often palpated.<br />
Once the terrain has been assessed, then the<br />
appropriate treatment can be applied.<br />
Acupuncture<br />
Acupuncture is a surprisingly effective modality<br />
for affecting many physiological processes<br />
in the body. According to acupuncture theory,<br />
energy circulates through the body along a<br />
series of pathways called meridians. Most<br />
meridians correspond to different organ systems<br />
and travel through all layers of the body.<br />
Researchers are attempting to explain this<br />
phenomenon in many ways. Measurements<br />
of electrical current, release of enkephalin,<br />
â-endorphin, serotonin, norepinephrine and<br />
CONTINUED ON PAGE 28<br />
14 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
IN MEMORIAM<br />
Joseph H. Davis<br />
March 16, 1914-March 5, <strong>2003</strong><br />
My father passed away last month, less than two<br />
weeks from his 89th birthday. I am sure that a very<br />
large percentage of California pediatricians knew<br />
my dad personally, some of them for longer than<br />
I did! I have been asked to write a memorial, but<br />
since many of his accomplishments are already<br />
widely known, I will mention only a few, and try to<br />
share some personal reflections.<br />
One of life’s ironies is that my father had<br />
moved to Santa Rosa only three months ago. Many<br />
said it was so that he could be closer to me, but,<br />
in truth, it was to be closer to his friend and companion, Helen<br />
Rudee. My mother passed away in 1998. “Doc” had known Helen<br />
since she was a nursing student in one of the courses he taught at<br />
Stanford in the 40s, and they had kept in touch through Stanford<br />
alumni functions. She had been twice widowed and they reconnected<br />
these past several years. My dad said that as a result, he had<br />
never been happier. I too enjoyed having him live closer. We were<br />
beginning a whole new relationship, and I was spending more time<br />
with him than I ever had before.<br />
Doc was born in San Francisco. He was an Eagle Scout, and<br />
graduated a couple of years earlier than normal from Lowel High<br />
School. He was identified as gifted and included in the original<br />
study group by Dr. Louis Terman. This so called group of “termites”<br />
was followed longitudinally over the course of their lives, as were<br />
their offspring, and I recall taking IQ tests on several occasions as a<br />
child to help them determine how the gene pool got diluted. I don’t<br />
mean this as any reflection on my mother’s side of the family; it’s<br />
just that not many people could keep up with my father’s drive and<br />
energy. He has aptly been compared with the Energizer Bunny, but<br />
described himself as hyperactive, and said that were he to have<br />
attended school now, he would have been put on Ritalin. He claimed<br />
that the only reason that he skipped grades was so that certain teachers<br />
wouldn’t have to deal with him any more.<br />
After graduating from Stanford Medical School and then<br />
doing a brief period in practice in San Francisco, he went overseas<br />
with the US Army for four years (while I was age 1-4) during<br />
WWII and served in the Pacific, seeing action in New Guinea and<br />
the Philippines. At the end of the war, he joined Dr. Esther Clark<br />
at the Palo Alto Clinic, where he worked for 52 years. When he<br />
joined, office visits were $3 and house calls $4, and he made LOTS<br />
of house calls. Consequently, he was rarely home, and to have time<br />
with him, my mom, my sisters and I would often ride along with<br />
him in the evening after dinner. When he could no longer work a<br />
full shift as a pediatrician (in his late 70s and with no hip joints)<br />
he created a new job for himself at the clinic as the advice “nurse”<br />
and would work half-day taking the advice calls from patients.<br />
This was so effective, that the internal medicine department hired<br />
some of their retired physicians to do the same.<br />
When he finally left the clinic he continued to volunteer as<br />
a pediatrician in other clinics, the most recent being Samaritan<br />
House in San Mateo (where memorial donations can be made in<br />
his name: www.samaritanhouse.com). He only left there to move<br />
to Santa Rosa, and described himself to his new<br />
neighbors as “semi-retired.”<br />
In addition to the Chapter 1 <strong>AAP</strong> newsletter,<br />
Doc was active in many other of the <strong>AAP</strong> functions.<br />
He became an advocate for adopted children who<br />
were trying to trace their biological roots, and for<br />
parents who were likewise trying to find children<br />
that they had given up for adoption. He worked<br />
with a volunteer organization called “PACER”<br />
(Post Adoption Center for Education and Research;<br />
www.pacer-adoption.org) that is now located in<br />
Carson City, NV and houses a computer database of adopters<br />
and adoptees in the effort to promote reunions. (They are another<br />
group worthy of charitable donations).<br />
His other life-long interest was the Boy Scouts of America.<br />
As mentioned, he became an Eagle Scout as a youth. He claimed<br />
that his experience at scout camp working with the camp physician<br />
was one of the motivating factors in his own decision to become<br />
a doctor (besides having a Jewish mother). When I joined the<br />
scouts, he renewed his interest and involvement. I made it to the<br />
rank of “life” scout at around age 14, and then lost interest and<br />
quit, but my dad stayed on, organized and ran a medical explorer<br />
post and continued right up until the time he left Menlo Park. The<br />
Boy Scouts awarded him the Silver Beaver (their highest award)<br />
for his lifetime achievements in scouting (we always referred to it<br />
as the “eager beaver award”). He was most proud of the number<br />
of graduates from his post that actually went on to careers in the<br />
medical professions.<br />
On Feb. 21, the pediatrics department at Stanford had Dr.<br />
Charles Prober present grand rounds in honor of the career of<br />
Joe Davis. Dr. Prober gave a marvelous talk comparing the history<br />
of antibiotics with the life of Joe Davis (he was a medical<br />
student when Alexander Fleming discovered penicillin). This was<br />
attended by many of his colleagues as well as some friends and<br />
family members. In retrospect, Doc was one of the very few people<br />
privileged to attend their own memorial service. On April 3, the<br />
City of Palo Alto posthumously awarded the Tall Tree Award to<br />
him. This is their highest award for a lifetime contribution of community<br />
service.<br />
Finally, it must be said, that Doc was vital right up to the<br />
very end. His body wore out, but his mind never did. Ultimately,<br />
he died of congestive heart failure after an unsuccessful attempt at<br />
placing an implanted pacemaker. He was ill for less than a week<br />
(that he would admit to, but that’s another story), and was physically<br />
uncomfortable for less than three or four hours. He died the<br />
way he would have wanted to, leaving behind long lists of things<br />
he had been planning to do! He is survived by my sisters, Nancy<br />
Levy and Betsy Faen, and our spouses, as well as six grandchildren<br />
and two great grandchildren. He is missed.<br />
A memorial service for Joe will be held at the Stanford<br />
Chapel on June 5 at 4 p.m.<br />
Leland Davis<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 17
Chronic Pain in Children: A Multidisciplinary<br />
Biopsychosocial Treatment Approach (Part III)<br />
Michael H. Joseph, M.D. and Jeffrey I. Gold, Ph.D.<br />
Having discussed a model of pain<br />
perception and assessment, we<br />
will now complete our three part<br />
series with a discussion about comprehensive<br />
treatment for children with chronic pain. Pain<br />
perception and assessment requires a biopsychosocial<br />
approach to treatment. As clinicians<br />
treating chronic illness, we are all challenged<br />
to stretch treatments beyond acute symptom<br />
management and to embrace a rehabilitation<br />
model of therapy. Simply stated, the child and<br />
family cannot simply wait for the pain to go<br />
away, but rather they must all be active participants<br />
in maintaining the goal of increased daily<br />
life functioning and decreased pain perception.<br />
If our ultimate objective is to retrain the child’s<br />
central nervous system (CNS) to decrease<br />
overall pain perception, we must decrease all<br />
ongoing nociceptive pain and support, encourage,<br />
and reinforce the child in working through<br />
chronic pain symptomatology.<br />
Rehabilitation<br />
The idea of a Cartesian dualistic mind/body<br />
split significantly limits our therapeutic<br />
options. In order to successfully treat and rehabilitate<br />
children with chronic pain, treatment<br />
must always include a combination of biological,<br />
psychological and social interventions.<br />
Once again, an interdisciplinary team approach<br />
to treatment is essential. Those clinicians with<br />
limited experience in an interdisciplinary treatment<br />
approach should study a few necessary<br />
requirements. These requirements include a<br />
shared theoretical pain philosophy, the belief<br />
that all pain is real and that rehabilitation is the<br />
primary goal. Crucial to the success of an interdisciplinary<br />
team approach is mutual respect,<br />
cooperation, communication and consistency.<br />
The more clearly aligned the team is with the<br />
overall rehabilitation objective the greater the<br />
benefit to the child and family.<br />
In the rehabilitation model, the most<br />
important component of care for children with<br />
chronic pain is to maximize their functioning.<br />
Because a child’s primary job is attending<br />
school, clinicians and family members must<br />
be coached to encourage and support as much<br />
school participation as possible. Research<br />
has shown in children with chronic pain and<br />
terminal illness that school reintegration has<br />
therapeutic and rehabilitative qualities (Bouffet,<br />
Zucchinelle, Costanzo, 1997). Clearly,<br />
school represents both academic and social<br />
life, provides an excellent distraction from<br />
over-focus on chronic pain symptoms and<br />
keeps the child on a normal developmental<br />
track. Preventing further setbacks from painrelated<br />
absenteeism can preserve and promote<br />
the child’s level of self-efficacy, provide social<br />
gains, maintain academic and cognitive development<br />
and decrease the stress associated with<br />
missed schooling. School attendance alone has<br />
been shown to be the most significant predictor<br />
of long-term positive outcome for children with<br />
chronic pain. Daily school participation and<br />
overall functioning can often remediate specific<br />
psychological and social deficits or problems,<br />
enhance and maintain communication with<br />
peers and family, facilitate adaptive coping and<br />
problem solving skills and provide symptom<br />
reduction due to distraction and emersion.<br />
With a focus on daily function, a well<br />
designed exercise program can provide additional<br />
advantages. Research has demonstrated<br />
that exercise provides many benefits for children<br />
with chronic pain. To gain the maximum<br />
benefit from exercise our emphasis is always<br />
on non-impact aerobic exercise (walking,<br />
biking and swimming). The overall goal is<br />
to promote increased cardiovascular function<br />
and physical movement, while minimizing the<br />
potential for further injury or harm. The known<br />
benefits from routine sustained cardiovascular<br />
exercise include the release of endorphins,<br />
which can be associated with decreased pain<br />
and improved mood and sleep. Critical to this<br />
goal is to support gradual progress and to avoid<br />
further complications due to rigorous or excessive<br />
exercise. Referral to a physical therapy<br />
program is often warranted. In addition to<br />
customizing and supervising the exercise program,<br />
physical therapists often employ other<br />
beneficial modalities such as massage, thermal<br />
and cryo-therapies and electrical therapies<br />
such and TENS and Interferential therapies.<br />
Sleep hygiene is another area that is obviously<br />
essential for children with chronic pain.<br />
Sleep disturbances (initiation, maintenance,<br />
quality) in children with chronic pain is well<br />
documented and needs to be addressed when<br />
developing a treatment strategy. This goal<br />
is accomplished via medication, relaxation<br />
and good sleep hygiene practices. This goal<br />
requires detailed psychoeducation regarding<br />
sleep hygiene practices, the identification of a<br />
good sleep aid and relaxation training. Usually,<br />
this combination therapy aids the child in initiating<br />
and maintaining good sleep patterns.<br />
Chronic pain therapy offers many challenges<br />
for the child, the family and the treating<br />
team. Patients and families often have<br />
difficulty adopting a rehabilitation philosophy<br />
in lieu of an acute pain management model.<br />
They often search for the underlying etiology<br />
and are overly concerned with the diagnosis<br />
and medication therapy. Families who are<br />
seeking diagnosis and acute treatments are not<br />
as well prepared to accept the chronic nature<br />
of the pain or the rehabilitation philosophy.<br />
In order for the overall treatment to be ultimately<br />
successful the child and the family<br />
must understand and accept the rehabilitation<br />
philosophy above the acute symptom reduction<br />
model. Ultimately, for the program to be<br />
successful, the family “must” work toward<br />
the rehabilitation goals. Often, emotional and<br />
physical demands associated with a longterm<br />
rehabilitation model, places stress on<br />
the family and can create additional distress<br />
on the child. Interestingly, if the family is<br />
resistant to the treatment philosophy or they<br />
experience distress related to the treatment,<br />
often the treating team may also experience<br />
their own resistance and/or distress. In these<br />
circumstances it is vital that the team continue<br />
to provide support, compassion and ongoing<br />
psychoeducation regarding the nature of the<br />
pain and associated distress.<br />
In the initial stages and throughout the<br />
treatment, psychoeducation is essential in<br />
providing the family with an alternative understanding<br />
of pain. Rather than an emphasis<br />
focused on finding the “cause,” discuss pain in<br />
terms of pain mechanisms (i.e., nocioceptive,<br />
anti-nocioceptive, nervous system dysregulation,<br />
hyperalgisa), resulting from a neural<br />
signaling problem versus ongoing tissue<br />
damage. Explain that a goal is to decrease<br />
neural “irritability” and enhance the child’s<br />
own pain inhibitory mechanisms. Discuss<br />
the visceral, somatic, spinal, emotional, cognitive,<br />
and environmental factors that each contributes<br />
to the pain. The family does not need<br />
to become pain specialists, but they require a<br />
framework of information from which they can<br />
base decisions. Once the family and child have<br />
understood and accepted the rehabilitation<br />
model most all interventions and treatments<br />
are designed to keep the patient functioning<br />
and on a path to recovery.<br />
18 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Drawing by a 19-year-old female patient with sickle-cell anemia.<br />
Cognitive and Behavioral<br />
Therapies<br />
All effective biopschosocial treatment plans<br />
include psychological interventions. The<br />
degree of intervention is contingent on many<br />
factors, but mostly the family and the child’s<br />
willingness to participate. Most children can<br />
benefit from relaxation therapy and cognitive<br />
behavioral therapy. These interventions are<br />
effective at targeting stress reduction, sleep<br />
hygiene, school reintegration, peer socialization,<br />
family functioning and empowering the<br />
child to use his/her brain to decrease pain signaling.<br />
Teaching children relaxation exercises<br />
has been demonstrated to be more effective in<br />
the reduction of chronic headaches than medication<br />
alone. These interventions often include<br />
diaphragmatic breathing, progressive muscle<br />
relaxation, guided imagery, biofeedback and<br />
hypnosis. Often when focusing on relaxation<br />
alone other stress, anxiety or depression may<br />
emerge as a result of chronic pain problems,<br />
or family / peer difficulties. Addressing these<br />
issues as they arise in therapy can further<br />
reduce distress, which contributes to overall<br />
pain problems.<br />
In addition to individual therapy, family<br />
therapy (i.e., home-based behavioral programs)<br />
can further enhance the child’s functioning and<br />
decrease the family’s reinforcement of negative<br />
pain behaviors (i.e., asking about pain,<br />
over-focus on pain, doing things for the child<br />
that s/he can do for themselves). Occasionally,<br />
the primary pain reinforcers of the pain are the<br />
parents. Parents often unknowingly facilitate<br />
pain behavior, when they believe they are<br />
assisting the child for his/her best interest. The<br />
goals of family therapy are to further provide<br />
a conceptual framework for understanding<br />
chronic pain, enhance parenting skills that<br />
target increased child self-efficacy, identify and<br />
teach appropriate interventions to address psychological<br />
and behavioral goals, to facilitate<br />
emotion-based communication and promote<br />
problem solving within the family. Ultimately,<br />
the goal of family therapy is to reset the child<br />
and the family’s behaviors surrounding the<br />
newest member of the family — “pain.” By<br />
eliminating or altering the negative pain reinforcers<br />
the family can actively participate in<br />
their child’s rehabilitation. Often parents need<br />
assistance in fine-tuning their parenting skills<br />
that eliminate the reinforcing properties of<br />
negative pain behaviors and promote increased<br />
daily function.<br />
Pharmacological Therapy<br />
The first and best pharmacological intervention<br />
is prevention when possible. Aggressively<br />
treat acute pain in order to prevent dorsal horn<br />
sensitization. Once chronic pain has set in the<br />
goal of pharmacological therapy becomes one<br />
of support. Reducing the symptoms enough so<br />
the patient and family can adopt the rehabilitation<br />
model with less distress.<br />
Few medications have been shown to be<br />
effective. Opioids play a minimal role since<br />
the neuro-physiology of chronic pain diminishes<br />
their effectiveness. On the other hand if<br />
the patient has ongoing nociceptive pain (i.e.<br />
tumor infiltration, or chronic inflammation)<br />
opioids can play a supportive role in therapy.<br />
The use of a long acting preparation with a<br />
shorter acting opioid for breakthrough pain<br />
is the most effective regimen for pain control<br />
and the least likely to produce psychological<br />
addiction or conditioning. Lastly because opioids<br />
may not be effective for chronic pain the<br />
simple upward titration may not result in analgesia<br />
but rather sedation and adverse effects.<br />
Pharmacological therapy can target other<br />
associated symptoms of chronic pain, such<br />
as CNS hypersensitivity. Amitripytiline has<br />
been shown in both adults and children to be<br />
effective in many forms of chronic and recurrent<br />
pain. It is a tricyclic antidepressant and<br />
therefore a norepinephrine and serotonin reuptake<br />
inhibitor. T<strong>CA</strong>’s are thought to increase<br />
antinociceptive tone, consequently decreasing<br />
chronic pain perception. Gabapentin an antiepileptic<br />
medication has also been shown<br />
to decrease the symptoms of chronic pain,<br />
especially neuropathic pain. Its mechanism of<br />
action is less understood, but it appears to work<br />
at the dorsal horn level reducing hypersensitivity.<br />
Medications can also be very useful to<br />
facilitate night sleep (amitriptyline, trazadone),<br />
treat anxiety/depression (SSRI) and to treat<br />
somatic contributors (topical and local anesthetics,<br />
muscle relaxants).<br />
Integrative Therapy<br />
In addition to the above-mentioned interventions<br />
for children, integrative therapies have<br />
been gaining increased exposure and have<br />
undergone greater experimental rigor. While<br />
many of the integrative therapies have been<br />
shown to benefit children with a variety of<br />
pain-related problems, we have listed a few<br />
that we prescribe routinely with good results.<br />
Hypnosis, which works through the creation<br />
of a narrow focus of attention and specific<br />
imagery to reduce distress, to reframe the<br />
experience and help the child dissociate from<br />
the pain, has been shown to be effective in<br />
reducing pain and anxiety during medical procedures<br />
(Zeltzer & Lebaron, 1982), decreasing<br />
chronic headache (Olness, McDonald<br />
& Uden, 1987) and decreasing side effects<br />
from chemotherapy (i.e., nausea). Researchers<br />
and clinicians alike understand that the<br />
underlying principles that guide hypnosis are<br />
based in stress reduction and relaxation. The<br />
CONTINUED ON PAGE 20<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 19
LUNG TRANSPLANTATION CONTINUED<br />
FROM PAGE 13<br />
There are also ethical issues to consider<br />
in the living donors: it is very troubling to<br />
endanger two perfectly healthy individuals<br />
for a chance to prolong the life of another.<br />
However, living donor transplantation is an<br />
accepted option for both kidney and liver failure<br />
patients. And in contrast to the kidney and<br />
liver live donor transplant procedures, there<br />
have been no deaths in the live donors for lobar<br />
lung transplantation.<br />
We conclude that living donor lobar lung<br />
transplantation is an option for selected children<br />
with end-stage lung disease. In certain cases, particularly if the child is not likely to survive<br />
the wait for a cadaveric organ, it may be the surgery of first choice.<br />
REFERENCES<br />
1. Starnes VA. Barr ML. Cohen RG. Lobar transplantation. Indications, technique, and outcome.<br />
Journal of Thoracic & Cardiovascular Surgery. 108(3):403-10; discussion 410-1, 1994 Sep.<br />
2. Woo MS. MacLaughlin EF. Horn MV. Wong PC. Rowland JM. Barr ML. Starnes VA. Living<br />
donor lobar lung transplantation: the pediatric experience. Pediatric Transplantation. 2(3):185-90,<br />
1998 Aug.<br />
3. Starnes VA. Woo MS. MacLaughlin EF. Horn MV. Wong PC. Rowland JM. Durst CL. Wells WJ.<br />
Barr ML. Comparison of outcomes between living donor and cadaveric lung transplantation in<br />
children. Annals of Thoracic Surgery. 68(6):2279-83; discussion 2283-4, 1999 Dec.<br />
4. Woo MS. MacLaughlin EF. Horn MV. Szmuszkovicz JR. Barr ML. Starnes VA. Bronchiolitis<br />
obliterans is not the primary cause of death in pediatric living donor lobar lung transplant recipients.<br />
Journal of Heart & Lung Transplantation. 20(5):491-6, 2001 May.<br />
Table 1 - Criteria for Living Donor Lobar Lung Transplant Candidates<br />
End-stage lung disease that has failed conventional medical/surgical management<br />
No significant kidney/liver disease<br />
No significant cardiac disease/ventricular dysfunction<br />
No active Mycobacterial disease<br />
No active or recent psychiatric disease<br />
Adequate psychosocial support (phone, transportation, housing, etc)<br />
No other significant medical disease which would limit lifespan<br />
No medical compliance problems (patient or caregivers)<br />
HIV negative<br />
No medical condition that would prevent access to removal of lungs (spinal fusion, etc)<br />
Availability of at least two suitable donors (for bilateral lobar)*<br />
* see Table 2<br />
Table 2 - Criteria for Live Lobe Donors<br />
ABO compatible to prospective transplant recipient<br />
Age 18-55 years<br />
No significant past medical history<br />
No recent viral infections (no active EBV, Hepatitis)<br />
Normal pulmonary function tests (FEV1 and FVC > 85% predicted)<br />
Oxygen tension > 80 mmHg on room air<br />
No smoking history for >5 years<br />
Normal chest radiograph<br />
CT scan of chest with no significant pathology (totally normal on proposed donor lobe side)<br />
No previous thoracic surgery on donor side<br />
Normal echocardiogram<br />
Normal coronary angiogram (if indicated)<br />
No coercion or payment for organ donation<br />
Demonstrated close emotional relationship with patient and/or family<br />
CHRONIC PAIN CONTINUED FROM PAGE 19<br />
obvious benefits of relaxation/hypnosis are<br />
exactly competing to the physiological arousal<br />
associated with pain and distress. Similar to<br />
hypnosis, meditation, or the self-focus on a<br />
single word or nothingness while clearing the<br />
mind of all thoughts, has also been show to<br />
be highly effective in reducing pain intensity,<br />
frequency and duration in patients suffering<br />
from migraines.<br />
Massage, defined as either light or deep<br />
tissue and body stroking, has been shown to be<br />
effective in reducing a number of pain symptoms<br />
in children with a variety of pain conditions.<br />
Studies have shown pain reduction in<br />
children with burns, decreased stress hormones<br />
(cortisol and norepinephrine), increased quiet<br />
sleep, increased cytotoxic capacity in children<br />
with juvenile rheumatoid arthritis (Field et. al.,<br />
1997), and the treatment of migraine (Hernandez-Reif<br />
et. al., 1998). The nature of compassionate<br />
touch/massage to children with chronic<br />
pain has demonstrated benefit in immediate<br />
and long-term care.<br />
Acupuncture — the use of needles, heat,<br />
pressure, or other stimulation at points along<br />
the meridian — can be used to to achieve flow<br />
of energy or QI. Acupuncture has been shown<br />
to decrease pain and to increase beta-endorphin<br />
levels and opioid receptors in adolescent<br />
migraine sufferers. Despite its increasing use<br />
as an integrative therapy to treat pain, acupuncture<br />
is rarely considered by pediatricians. In<br />
part this phenomenon is due to perceptions that<br />
it will not be acceptable to pediatric patients or<br />
their family. For further details please review<br />
“The Tao of Pediatrics and Chinese Medicine”<br />
in this issue.<br />
The treatment of chronic pain in pediatric<br />
patients has received little attention to date.<br />
Therefore, there is a lack of empirically based<br />
comprehensive treatments designed to provide<br />
care for these patients. Our clinical experience<br />
embraces the integration of mind and<br />
body as the most effective approach to treating<br />
pediatric chronic pain. This integration<br />
informs a model of assessment and treatment<br />
focused on rehabilitation. Understanding this<br />
model of practice requires frequent evaluation<br />
of the child’s progress, as well as consistent<br />
reinforcement and support of the patient and<br />
family. The comprehensive treatment model<br />
has generated good clinical outcomes for<br />
patients and families who have viewed the<br />
chronic pain clinic as the “last stop.”<br />
“The only source of knowledge is experience.”<br />
— Albert Einstein<br />
20 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Twenty-Five Years of Home Mechanical<br />
Ventilation in Children:<br />
The Program at Childrens Hospital Los Angeles<br />
Manisha Witmans, M.D., Sheila S. Kun, R.N., M.S., and Thomas G. Keens, M.D.<br />
Braun introduced the idea of mechanical<br />
ventilation in 1889 and by the<br />
mid 1940s hospitals were able to<br />
care for adults with respiratory failure with<br />
large ventilators called “iron lungs.” The technology<br />
has continued to evolve from a large,<br />
intrusive hospital based system to a lighter,<br />
portable system that allows families to care for<br />
medically complicated patients at home.<br />
Home mechanical ventilation has<br />
changed tremendously in the last 25 years.<br />
The home mechanical ventilation program at<br />
Childrens Hospital Los Angeles (CHLA) is<br />
an example of what is achievable in children<br />
with chronic respiratory failure who require<br />
mechanical ventilation. Since the inception<br />
of the home ventilator program in 1977, the<br />
CHLA program has grown to include over 375<br />
children who are followed for home mechanical<br />
ventilation. The program children requiring<br />
assisted mechanical ventilation have ventilatory<br />
muscle weakness (45%), chronic lung disease<br />
(hypoplastic lungs and chest wall defects)<br />
(26%) and central hypoventilation syndromes<br />
(29%). The CHLA program is unique in that<br />
there is a large number of small infants with<br />
chronic lung disease.<br />
The need for mechanical ventilation<br />
is likely when there is either an increase in<br />
respiratory load or deficiency in the ventilatory<br />
muscle power or central drive, such that<br />
adequate oxygenation and ventilation cannot<br />
be achieved without assistance. Chronic ventilatory<br />
failure is defined as a medical condition<br />
from which an infant or a child, who is<br />
otherwise medically stable, requires mechanical<br />
ventilation and cannot be weaned from<br />
ventilation, despite repeated attempts. Unlike<br />
adults, infants and children are more prone<br />
to respiratory failure because of decreased<br />
ventilatory muscle strength, diaphragm muscle<br />
fatiguability, and smaller airways prone to atelectasis<br />
and obstruction, and proportionately<br />
increased respiratory loads. Thus, infants and<br />
children require different ventilatory strategies<br />
compared to adults.<br />
The philosophy of home ventilation is<br />
quite different from the intensive care perspective<br />
because the goal is to provide chronic,<br />
not acute, support of ventilation. The ventilator<br />
is adjusted to completely meet the child’s<br />
age-appropriate physiological ventilatory<br />
requirements rather than just providing support<br />
to minimize work of breathing. Using the<br />
ventilatory parameters from the intensive care<br />
setting often underestimates ventilatory needs<br />
for home, as children are more likely to be<br />
active at home. This approach allows the child<br />
to expend energy for activities of daily living,<br />
rather than ventilation alone. The strategy<br />
for chronic ventilation is also different from<br />
intensive care units. Smaller, uncuffed tracheostomy<br />
tubes are better alternatives because<br />
they prevent tracheomalacia, iatrogenic tracheal<br />
trauma and allow room for ventilation to<br />
bypass the tracheostomy in the event of tube<br />
obstruction. In addition, they allow children to<br />
speak, as many children on home mechanical<br />
ventilation are able to attend school and other<br />
social events where speaking is necessary.<br />
Ideally, the ventilator parameters are adjusted<br />
to meet the patients’ needs instead of making<br />
the patient adapt to the ventilators mechanical<br />
capabilities.<br />
A variety of modes of ventilation and<br />
types of ventilators are available in the United<br />
States. The choice of ventilator is dependent on<br />
the underlying medical condition and the individual<br />
patient needs. The modes of ventilation<br />
include: non-invasive positive pressure ventilation<br />
with bi-level positive airway pressure,<br />
positive pressure ventilation with a tracheostomy,<br />
negative pressure ventilation and diaphragmatic<br />
pacing. The most common mode of<br />
ventilation is via a tracheostomy and a portable<br />
home ventilator. Compared to older ventilators,<br />
the advantages of the newer ventilators<br />
include: continuous flow, ventilatory strategies<br />
that provide pressure support and/or positive<br />
end-expiratory pressure and have a lightweight<br />
internal battery. Ventilator malfunction is also<br />
surprisingly uncommon. The newer ventilators<br />
are able to provide ventilation for children with<br />
more severe lung disease at home, which has<br />
resulted in improved survival quality of life.<br />
A popular method of providing assisted<br />
ventilation non-invasively is bi-level positive<br />
airway pressure (B-PAP). The interface<br />
consists of a nasal or facemask that delivers<br />
compressed air to splint the airway open<br />
and provide positive inspiratory pressure.<br />
Currently, over 100 children on B-PAP are<br />
followed at CHLA. Children with congenital<br />
hypoventilation, ventilatory muscle weakness<br />
and certain types of chronic lung disease can<br />
be ventilated with B-PAP, especially if the<br />
ventilatory requirements are sleep related. This<br />
type of ventilation does not require a tracheostomy,<br />
has minimal side effects (nasal irritation,<br />
skin breakdown, intolerance of the mask) and<br />
is well tolerated in children.<br />
Children that need mechanical ventilation<br />
have some special requirements related<br />
to ongoing care and follow-up. During acute<br />
illnesses, these children have to be monitored<br />
closely as they may not show signs of respiratory<br />
distress as noticeably as other children.<br />
They may need increased bronchodilator<br />
treatments, more airway clearance treatments,<br />
diuretics, and/or chest physiotherapy. They<br />
often need increased ventilatory support during<br />
respiratory tract infections and hospitalizations.<br />
Two relatively easy monitoring methods<br />
are: pulse oximetry and end tidal Pco 2<br />
monitoring<br />
to ensure adequate oxygenation and<br />
CONTINUED ON PAGE 27<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 21
Childcare Health Linkages Program:<br />
How Pediatricians Can Collaborate with<br />
Local Childcare Health Consultants<br />
Robin Calo, R.N., M.S., P.N.P. and Karen Sokal-Gutierrez, M.D., M.P.H.<br />
When you think about the young<br />
children in your practice, who<br />
besides their parents takes care<br />
of them? Traditionally, pediatric health professionals<br />
have focused on parents and the home<br />
setting to promote the health and safety of<br />
young children. However, a large proportion<br />
of young children spend a significant amount<br />
of time in the care of other adults in out-ofhome<br />
settings. When providing health services<br />
for children and families, pediatricians need to<br />
also consider children’s “extended families,”<br />
including relatives and childcare providers.<br />
Why is childcare important to<br />
children’s health?<br />
Over the past 20 years, as more parents return<br />
to work and school, the proportion of young<br />
children attending childcare has increased by<br />
50%. 1 Currently, over 60% of children under 6<br />
years of age regularly attend child care. 2 This<br />
includes 44% of children under 1 year of age, 3<br />
and 77% of 3-5 year olds. 4 For children under<br />
age 5 in childcare, 41% spend 35 hours or more<br />
per week in childcare. 5<br />
Children are cared for in a variety of<br />
childcare settings including childcare centers<br />
and preschools; family childcare homes; and<br />
by nannies, family members and friends in<br />
their homes and/or the child’s home. Commonly,<br />
families use a combination of childcare<br />
arrangements.<br />
Childcare providers, like parents, deal<br />
with a wide range of child health issues on<br />
a daily basis, including promoting children’s<br />
development, nutrition, preventing injuries,<br />
caring for children with special needs, reducing<br />
the spread of infectious diseases, caring for<br />
mildly-ill children, and emergency preparedness.<br />
California licensing regulations require<br />
that childcare providers have 15 hours of<br />
health and safety training, but the training is<br />
limited and many unlicensed caregivers have<br />
no health training at all.<br />
How can childcare health<br />
consultants assist childcare<br />
programs?<br />
In response to the need for assistance on<br />
child health and safety issues in childcare,<br />
the federal Department of Health and Human<br />
Services Maternal and Child Health Bureau<br />
funded national and state Healthy Childcare<br />
America initiatives and the National Training<br />
Institute to promote health consultation<br />
to childcare programs. Until recently, only<br />
a few counties in California provided health<br />
consultation to childcare. In 2000, however,<br />
First Five California (Proposition 10) funded<br />
the University of California San Francisco-<br />
California Childcare Health Program (UCSF-<br />
CCHP) to create the Childcare Health Linkages<br />
Project (CCHLP) to develop childcare health<br />
consultation programs in 21 counties across<br />
California: Alameda, Colusa, Humboldt, Inyo,<br />
Kern, Lake, Los Angeles, Marin, Mendocino,<br />
Napa, Sacramento, San Benito, San Francisco,<br />
San Luis Obispo, Santa Clara, Shasta, Nevada,<br />
Siskiyou, Sonoma, and Yolo. There are also<br />
childcare health consultation programs operating<br />
without CCHLP funding in Long Beach,<br />
Orange, San Diego, Santa Barbara, and San<br />
Bernadino counties. UCSF-CCHP provides<br />
training and technical assistance for all of the<br />
childcare health consultation programs.<br />
The CCHLP model of childcare health<br />
consultation consists of a network of trained<br />
childcare health consultants and Childcare<br />
Health Advocates who provide health education<br />
and consultation to all types of childcare<br />
programs. All of the childcare health consultants<br />
and Advocates have completed nine days<br />
of specialized training on childcare health<br />
through UCSF-CCHP’s California Training<br />
Institute.<br />
The Childcare Health Consultant is a<br />
licensed health professional, typically a nurse<br />
with pediatric expertise, employed by either<br />
the local public health department or a community<br />
agency such as the childcare resource<br />
and referral agency. The Childcare Health<br />
Consultant serves as a link between the pediatric<br />
medical community, childcare providers<br />
and families. Childcare health consultants<br />
address a wide range of issues including access<br />
to health care, immunizations, infant and child<br />
nutrition, child behavior and development,<br />
infection control, playground and child passenger<br />
safety, special health care needs, and<br />
child abuse. Some of their activities include:<br />
• Making site visits to childcare programs<br />
to conduct health and safety assessments<br />
• Providing linkages and referrals to medical<br />
homes, health insurance, and other<br />
community services<br />
• Coordinating health, dental, hearing, or<br />
vision screenings for children in child<br />
care<br />
• Working with the pediatric provider,<br />
family and childcare provider to develop<br />
care plans for children with special needs<br />
• Conducting trainings on specific health<br />
and safety issues for childcare staff, parents,<br />
and/or children<br />
22 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
The childcare health advocate is usually<br />
a teacher at a childcare program. The health<br />
advocate is the on-site liaison who collaborates<br />
with the childcare health consultant to<br />
promote health and safety in the childcare<br />
environment.<br />
How can pediatricians link with their<br />
local childcare health consultant?<br />
Pediatricians and childcare health consultants<br />
are working toward the same aim: to<br />
promote children’s health and prevent disease<br />
and injury. The following case studies illustrate<br />
successful collaborations between physicians<br />
and childcare health consultants:<br />
In Kern County, childcare health consultants<br />
work with local physicians to develop<br />
individual care plans for children in childcare<br />
with special health care needs (e.g., asthma,<br />
diabetes, and orthopedic conditions). The care<br />
plans instruct childcare providers on the child’s<br />
health conditions; routine care measures,<br />
medications and equipment; how to prevent<br />
complications; and emergency procedures.<br />
The childcare health consultants also help<br />
ensure that caregivers receive the necessary<br />
medications, equipment, and training to implement<br />
the care plans. Since asthma is one of the<br />
most common special health needs, childcare<br />
health consultants have developed trainings<br />
for local childcare providers on how to give<br />
inhaled medications to children with asthma.<br />
This collaboration has helped childcare providers,<br />
parents and physicians feel more confident<br />
that children with special health care needs are<br />
cared for safely in childcare programs.<br />
In Inyo County, childcare health consultants<br />
and advocates help children prepare for<br />
their preschool and kindergarten well-child<br />
medical visits by setting up a practice “visitto-the-doctor.”<br />
Local pediatricians loaned<br />
medical equipment to the staff of the Childcare<br />
Health Linkages Project. The childcare health<br />
consultant and advocates set up a mini-clinic<br />
and checked children’s blood pressures and<br />
reflexes; looked in their eyes, ears, and throats;<br />
listened to their hearts and lungs; and gave the<br />
children a chance to receive a pretend shot and<br />
a fun bandage. Parents and pediatricians stated<br />
that the children were more prepared for their<br />
medical visit, which made it a better experience<br />
for everyone involved.<br />
In other counties, pediatricians have<br />
served as consultants to local childcare health<br />
consultants and childcare providers on children’s<br />
health, development and safety. Pediatricians<br />
have also provided workshops for<br />
childcare program staff, parents and children<br />
on a variety of health topics; participated in<br />
community-based health promotion and injury<br />
prevention programs in childcare; and served<br />
on childcare program boards of directors and<br />
health advisory boards.<br />
Consider exploring new avenues for<br />
promoting children’s development, health and<br />
safety in your community by collaborating<br />
with your local childcare programs. For more<br />
information, contact:<br />
Robin Calo, RN, PNP, Coordinator<br />
California Childcare Linkages Project<br />
University of California San Francisco<br />
California Childcare Health Program<br />
1322 Webster Street, Suite 402<br />
Oakland, <strong>CA</strong> 94612<br />
(510) 839-1195<br />
www.ucsfchildcarehealth.org<br />
NOTES<br />
1. U.S. Department of Education, National<br />
Center for Education Statistics, 1995.<br />
2. U.S. Department of Education, National<br />
Center for Education Statistics, 1999.<br />
3. U.S. Department of Education, National<br />
Center for Education Statistics, Data from<br />
the 1995 National Household Education<br />
Survey, 2000.<br />
4. U.S. Department of Education, National<br />
Center for Education Statistics, Digest of<br />
Education Statistics, 2002.<br />
5. Urban Institute, 1997 National Survey of<br />
Families, 2000.<br />
Eve Black Honored<br />
On February 8, <strong>2003</strong>, at the Annual Joint District Meeting, Eve Black was honored for her<br />
nearly 50 years of hard work and dedication to the children and pediatricians of California. In<br />
addition to a plaque from the California District American Academy of Pediatrics, which was<br />
presented by Burt Willis, M.D., District Chair, Eve received a check for $1,000 to the Gene<br />
Black Summer Career Program. The summer program, which introduces high school juniors<br />
and seniors to careers in the health professions, is named in honor of her husband, Gene Black.<br />
It is administered by the Los Angeles Pediatric Society.<br />
Eve’s work with Chapter 2 and with LAPS has been comprehensive and wide-ranging. As<br />
Chapter Administrator for Chapter 2 and Executive Secretary for LAPS, Eve Black continues in<br />
her role as champion of the children of California and the physicians who look after them.<br />
Burt Willis presents Eve Black with a plaque honoring her many years of service.<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 23
Annual Las Vegas Seminars —<br />
25 Years of District Education<br />
and Support<br />
Rosalie Blazej and Milton Arnold, M.D.<br />
November 20-23, <strong>2003</strong> marks the<br />
25 th anniversary of the American<br />
Academy of Pediatrics California<br />
Chapters 1, 2, 3, and 4’s Annual Las Vegas<br />
Seminars.<br />
Conceived in the late 1970s as the first<br />
joint California Chapters CME meeting, the<br />
seminars offered the practicing pediatrician<br />
a “maximum of learning in a comfortable,<br />
relaxed, and informal atmosphere.” Twentyfive<br />
years later, the seminars have grown from<br />
250 registrants to over 800, but the emphasis<br />
on learning in a venue of relaxation and<br />
world-class accommodations has remained<br />
unchanged. Meeting attendees come from all<br />
over the U.S. and from foreign countries. Over<br />
65% of 2002 registrants came from areas outside<br />
of California.<br />
At each meeting, nationally known<br />
speakers deliver presentations from varied<br />
and wide-ranging pediatric subspecialties.<br />
Speakers for the <strong>2003</strong> Seminar include Angela<br />
Anderson, M.D., Daniel L. Coury, M.D.,<br />
Kathryn Edwards; M.D., Lewis R. First, M.D.,<br />
Francine R. Kaufman, M.D., and Anthony J.<br />
Mancini, M.D.<br />
Not only do the seminars benefit the<br />
individual pediatrician, the meetings have<br />
become the principal source of funding for<br />
the District’s advocacy efforts on behalf of the<br />
children of California. Dr. Milton Arnold, who<br />
was a catalyst in organizing the first meeting,<br />
remains the program chairman and the educational<br />
and financial success of the Las Vegas<br />
Seminars is due in large part to his tireless<br />
work. The seminars are also indebted to Dr.<br />
Anthony Hirsch and Dr. Martin Gershman,<br />
who were among the first to advance and support<br />
the idea of a joint meeting in Las Vegas.<br />
The Venetian Resort and Casino was the<br />
site of the 2002 Las Vegas Seminars and will<br />
again serve as the meeting venue for <strong>2003</strong>.<br />
Over three hundred of the hotel’s exquisite<br />
Luxury and Bella suites have been set aside<br />
for meeting registrants at special seminar rates.<br />
Advance meeting and hotel registration forms<br />
are printed on the inside back cover and are<br />
also available on the Web at www.aapca2.org.<br />
24 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Selling Tobacco Products as a<br />
Public Health Issue<br />
Trisha Roth, M.D.<br />
This year, the California State Legislature<br />
will be acting on a bill to<br />
increase the sale age for tobacco to<br />
21. This proposal causes us to think about the<br />
current state of smoking in California, question<br />
the age-18 law that is a standard nationwide,<br />
look for any signs that this would help reduce<br />
tobacco addiction, and think about the social<br />
mores regarding a person’s age and their relative<br />
ability to take risks with their own lives.<br />
It is clear that California is at the cutting<br />
edge of national and international tobacco<br />
reforms. The state has comprehensive restrictions<br />
on smoking in public places, an 87¢<br />
per-pack tax on tobacco, and an aggressive<br />
anti-tobacco advertising campaign.<br />
For most California adults, the tobacco<br />
culture of the 60s and 70s is clearly waning.<br />
There are few public places, aside from workplace<br />
entryways crowded with smokers, where<br />
adults see other adults smoke. We are also relatively<br />
free of widespread tobacco advertising;<br />
there is no longer a skyscraper high Marlboro<br />
Man on Sunset Boulevard, and there are few if<br />
any tobacco advertisements in our newspapers<br />
and major publications.<br />
Yet this is not a time to grow complacent.<br />
The fact is, while we may think that the battle is<br />
being won, it has actually just moved below our<br />
radar. According to a Surgeon General’s report,<br />
if a person is not addicted by the age of 21 there<br />
is less than a 5% chance that they will ever<br />
become addicted. For this reason, the 18-20<br />
year old population is the new battleground, and<br />
the tobacco companies have shifted their $10<br />
billion advertising campaign to most directly<br />
affect the smoking rates for this age group.<br />
This tobacco industry strategy has<br />
worked. In California the smoking rate for<br />
18-20 year olds has increased more than 35%<br />
over the past eight years. The rate of addiction<br />
for this age group is 40% higher than for those<br />
over 30 years old. This growing rate of smoking<br />
threatens to undo the effects of years of<br />
tobacco reform in California.<br />
In addition, the tobacco industry has<br />
recognized that their advertising to 18-20 yearolds<br />
has a certain “spillover” to younger teens.<br />
By advertising in Sports Illustrated, Spin, Vibe,<br />
and Rolling Stone, they are able to reach the<br />
impressionable minds of 12-17 year olds. To<br />
help the tobacco companies even more, the<br />
current 18-year old sale age for tobacco allows<br />
thousands of high school seniors to legally buy<br />
cigarettes and bring them to the high school<br />
campus. Thus, the powerful combination of<br />
advertising, peer pressure, and ready access is<br />
permitted to take hold — all with sanction by<br />
our current state laws.<br />
Now the California Legislature is recognizing<br />
the problem and trying to do something<br />
about it. At the urging of the California Medical<br />
Association and with the help of the Preventing<br />
Tobacco Addiction Foundation, a proposal<br />
is on the table to increase the minimum age for<br />
purchasing tobacco to 21. This measure, AB<br />
221 by Assemblyman Paul Koretz, may be just<br />
the action necessary to stymie the industry’s<br />
hopes for a resurgence of tobacco addiction<br />
in our state.<br />
The proposal to increase the sale age for<br />
tobacco has grown out of the experience with<br />
age limits for alcohol. In the early 70s, as the<br />
nation reduced the voting age to 18, states<br />
throughout the nation reduced their drinking<br />
ages. This resulted in increased teenage alcoholism,<br />
a spike in drinking for younger teens,<br />
and more drunk driving deaths.<br />
As a result of the unintended consequences<br />
of the younger drinking age, President<br />
Reagan championed the Uniform Drinking<br />
Age Act in 1984, which called on all states to<br />
return their drinking age to 21. This resulted<br />
in a dramatic decline in usage, a reduction in<br />
teenage alcoholism and related deaths, and<br />
more negative teenage attitudes towards drinking.<br />
These positive benefits came even though<br />
there were no significant changes in enforcement<br />
and educational efforts targeted towards<br />
this population.<br />
If the change to 21 for tobacco has similar<br />
effects on usage, it can be expected that teenage<br />
smoking would be reduced by a third. The<br />
Board of Equalization, which collects data<br />
associated with the tobacco tax, has suggested<br />
that the implementation of an age-18 sale law<br />
would reduce smoking among 12-20 year<br />
olds by 30 million packs per year. And these<br />
reductions in smoking are getting at the bud<br />
of nicotine addiction. According to a report by<br />
the Surgeon General, the chance of someone<br />
developing an addiction after the age of 21 is<br />
less than 5%.<br />
A poll completed just before the 2002<br />
General Election showed that 58% of likely<br />
California voters support an increase in the<br />
purchase age for tobacco to 21. This confirms<br />
the results of a June 2002 ABC poll that found<br />
Americans by nearly a 2 to 1 margin favor raising<br />
the minimum legal age to buy cigarettes to<br />
21 in their state. The support in the poll was<br />
found to be strongest among the state’s growing<br />
Latino population, with 68% supporting<br />
the measure and 64% stating “strong support.”<br />
Additionally, two-thirds of the state’s African<br />
American voters support the increase to 21.<br />
According to a Surgeon General’s report, if a person is not<br />
addicted by the age of 21 there is less than a 5% chance that they<br />
will ever become addicted.<br />
Even with this strong support, some will<br />
cling to the old saying “Old enough to fight and<br />
die, old enough to drink and smoke.” Yet if the<br />
drinking age experiment showed this country<br />
anything, it was the necessity for us to collectively<br />
decide the best age at which young<br />
people can responsibly deal with these dangerous<br />
life decisions.<br />
We must not take lightly the need to<br />
protect personal rights, and we should not run<br />
roughshod over the ability of Californians to<br />
make decisions for themselves. Yet the data<br />
clearly suggests that delaying for a few years<br />
access to this heavily marketed product may<br />
avert a lifetime of addiction and premature<br />
death in literally millions of our state’s youngest<br />
citizens. Increasing the sale age for tobacco<br />
is a logical, sensible and timely step for California.<br />
To find out more information, you may<br />
contact the author at TrishaRoth@aol.com<br />
or www.trisharoth.com, Paul Mitchell at<br />
paul@tobacco21.org, or visit the campaign<br />
website at<br />
http://www.tobacco21.org/california.<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 25
Early Hearing Detection and<br />
Intervention<br />
Sudeep Kukreja, M.D., EHDI, Chapter Champion <strong>AAP</strong> Chapter 4<br />
The 2nd Annual Early Hearing Detection<br />
and Intervention (EHDI) Conference<br />
was held in Atlanta, Georgia in<br />
February <strong>2003</strong>. EHDI refers to the process of<br />
screening all newborns for hearing loss and<br />
having all who fail the screening receive diagnostic<br />
evaluation before three months of age.<br />
When necessary, infants are enrolled in early<br />
intervention programs by six months of age.<br />
The conference was hosted by National<br />
Center for Hearing Assessment and Management<br />
(NCHAM) and sponsored by the<br />
U.S. Center for Disease Control and Prevention<br />
(CDC) and the federal Maternal and<br />
Child Health Bureau (MCHB) of the Health<br />
Resources and Services Administration<br />
(HRSA) in partnership with American Academy<br />
of Pediatrics (<strong>AAP</strong>). The purpose of the<br />
conference was to provide a forum to present<br />
the current knowledge regarding Early Hearing<br />
Detection Intervention (EHDI), and to promote<br />
information sharing and idea exchange<br />
between states, private industry, advocacy and<br />
partner groups, education organizations and<br />
regarding the implementation and enhancement<br />
of EHDI programs.<br />
The conference was attended by over 350<br />
delegates, including audiologists, neonatologists,<br />
pediatricians, developmental pediatricians,<br />
public health personnel, nurses, speech<br />
and language pathologists, and parents of hearing-impaired<br />
children. The State of California<br />
was represented by Hallie Morrow, MD MPH,<br />
Medical Consultant to the California Newborn<br />
Hearing Screening Program (NHSP) and three<br />
EHDI chapter champions, Sudeep Kukreja,<br />
M.D., Richard Powers, M.D., Shirley Russ,<br />
M.D. from <strong>AAP</strong> chapters IV, I and II respectively.<br />
There are certain areas in the California<br />
NHSP which require additional attention:<br />
1. Inequities between CCS and non-<br />
CCS approved hospitals regarding<br />
newborn hearing screening:<br />
The legislation regulating newborn hearing<br />
screening in California is applicable<br />
only to babies born in CCS approved<br />
hospitals. The other 30% babies, born in<br />
non-CCS hospitals may remain undiagnosed.<br />
While legislation to cover non-<br />
CCS approved hospitals is an important<br />
long-term goal it is clear that the current<br />
state budget deficit makes this not a feasible<br />
target this year. The chapter leaders<br />
requested information for colleagues<br />
working in non-CCS approved hospitals,<br />
to encourage those hospitals to voluntarily<br />
adopt newborn hearing screening as a<br />
standard of care. Chapter Champions plan<br />
to meet with health plans to discuss reimbursement<br />
for babies who are screened in<br />
non-CCS approved hospitals. Extension<br />
legislation may be reconsidered in future<br />
fiscal years.<br />
2. Shortage of pediatric audiologists:<br />
It is estimated that 1500 infants will be<br />
identified each year in California, at an<br />
age that is well below the former average<br />
of 3-4 years prior to newborn screening.<br />
However, there is a shortage of appropriately<br />
trained audiologists and speech<br />
therapists to evaluate and treat infants<br />
identified in the screening program.<br />
3. Access to pediatric audiologist:<br />
There are delays in evaluation due to<br />
lack of access to otolaryngologists experienced<br />
in evaluation of infants and young<br />
children.<br />
4. Lack of insurance coverage for the costs<br />
of screening incurred by the hospitals:<br />
Often screening costs are included in the<br />
capitated payment for normal newborn<br />
care, without adjustment for the incremental<br />
cost for the required screening.<br />
Improved insurance reimbursement will<br />
be an incentive for voluntary participation<br />
in newborn hearing screening by<br />
non-CCS hospitals. Lack of health insurance<br />
coverage for diagnostic follow up is<br />
also a barrier.<br />
5. Poor communication between pediatricians<br />
and Early Intervention Programs:<br />
There is a need for closer collaboration<br />
between pediatricians and early intervention<br />
services for children with hearing<br />
loss.<br />
6. Lack of a tracking and information<br />
technology system to assure access to<br />
services and follow up for identified<br />
children and confirmatory evaluations,<br />
indicated consultations, and auditory<br />
amplification devices (hearing aids).<br />
Additional Resources:<br />
1. <strong>CA</strong>LIFORNIA<br />
www.dhs.ca.gov.pcfh/cms<br />
(916)327-1400<br />
<strong>AAP</strong> Chapter 1, Chapter Champion<br />
Richard Powers, M.D., dp@rjpowers.org<br />
<strong>AAP</strong> Chapter 2, Chapter Champion<br />
Shirley Russ, M.D., shirlyruss@aol.com<br />
<strong>AAP</strong> Chapter 3, Chapter Champion<br />
Donald Miller, M.D.<br />
dmiller@nchs-health.org<br />
<strong>AAP</strong> Chapter 4, Chapter Champion<br />
Sudeep Kukreja, M.D,<br />
sudeepmd@pol.net<br />
2. OTHER NATIONAL RESOURCES:<br />
National Association of the Deaf<br />
www.nad.org<br />
National Center for Hearing Assessment<br />
and Management<br />
(NCHAM) www.infanthearing.org<br />
SCOLIOSIS CONTINUED FROM PAGE 8<br />
union (large curves, those with neurofibromatosis),<br />
maturity, and curve stiffness. Curves in<br />
the lumbar and thoraco-lumbar regions may be<br />
amenable to anterior fusions with instrumentation,<br />
thereby limiting the amount of lumbar<br />
immoblization. Placing instrumentation anteriorly<br />
in the thoracic spine is more controversial<br />
given the proximity of the great vessels, and<br />
its place in the current treatment of scoliosis is<br />
still to be delineated. Both anterior and posterior<br />
spinal fusions are performed when there is<br />
a significant risk of continued growth (called<br />
the “crankshaft” phenomenon), when the<br />
magnitude of the curve or underlying disease<br />
decreases the chance of a successful fusion, or<br />
when the curve is very stiff in order to improve<br />
correction.<br />
Finally, a note about pregnancy and<br />
scoliosis. The effect of pregnancy on curve<br />
progression has been debated for many years.<br />
Recent literature does not indicate a risk of<br />
curve progression with pregnancy, nor does<br />
it seem to affect the patient’s treatment from<br />
an obstetrical standpoint. Thus, patients with<br />
scoliosis may be counseled to not be concerned<br />
about childbearing.<br />
In conclusion, adolescent idiopathic scoliosis<br />
is a lateral curvature of the spine over<br />
10 0 in a patient between the ages of 10 and<br />
16 years with no detectable underlying cause.<br />
A careful history and physical examination<br />
should be performed, and only a single plain<br />
radiograph is necessary to document the scoliosis.<br />
Even with evidence of scoliosis, few<br />
children will require active treatment with a<br />
brace or surgery.<br />
26 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
TWENTY-FIVE YEARS OF HOME MECHANI<strong>CA</strong>L VENTILATION IN CHILDREN CONTINUED FROM PAGE 21<br />
ventilation. We generally keep the end-tidal<br />
Pco 2<br />
at values between 30-35 torr at all times<br />
to provide the children with some respiratory<br />
reserve in the event of an illness. It is imperative<br />
that each child has a general pediatrician<br />
participate in her overall care.<br />
Mechanical ventilation is not always a<br />
life-long therapy. Some of the children may<br />
be weaned from ventilation depending on<br />
the underlying lung disease. The types of<br />
patients that can be weaned include those with<br />
chronic lung disease and some children with<br />
ventilatory muscle weakness. The process of<br />
weaning, also known as “sprinting,” should<br />
be gradual, with brief periods of time breathing<br />
spontaneously off the ventilator. These are<br />
progressively increased as long as the patient<br />
tolerates the changes. The tolerance of the<br />
weaning regimen can be assessed clinically<br />
and objectively by means of oximetry and<br />
carbon dioxide monitoring. These children are<br />
weaned during waking hours first and should<br />
be able to tolerate this regimen before considering<br />
changes in nighttime ventilation.<br />
The goals of home ventilation are: 1) to<br />
ensure medical safety, 2) prevent and minimize<br />
complications, 3) optimize quality of life and<br />
rehabilitation potential, and 4) reintegrate the<br />
child back into the family. The success of a<br />
home ventilator program is dependent on the<br />
dedicated and integrated services provided by<br />
the hospital and the community. Once an infant<br />
or child is deemed to need home mechanical<br />
ventilation, the coordinated effort for transition<br />
from hospital to home is dependent on<br />
multiple factors including: the availability of<br />
ventilators, the education of the parents, and<br />
the availability of home nursing. Criteria for<br />
discharge to home are: medical stability with<br />
stable ventilatory settings, family commitment<br />
to home care, education of parents regarding<br />
technical aspects of care of children with<br />
mechanical ventilation, adequate home care<br />
environment (power, telephone and electricity),<br />
access to emergency services, and vendor<br />
services as well as access to a pediatrician.<br />
Local pulmonary services should be consulted<br />
to help plan the process of implementing ventilatory<br />
support.<br />
In summary, home ventilation has<br />
approached a new era with many changes in<br />
the last 25 years. With the new technology,<br />
children with severe lung disease are able to<br />
live at home and reintegrate into their families<br />
with a reasonably good quality of life. The<br />
transition from hospital to home is possible<br />
with more portable technology and with the<br />
dedication of all those involved in the program,<br />
in the hospital and in the community.<br />
Address Correspondence to:<br />
Thomas G. Keens, M.D.<br />
Division of Pediatric Pulmonology<br />
Childrens Hospital Los Angeles<br />
4650 Sunset Boulevard, Box #83<br />
Los Angeles, California 90027-6062<br />
Phone: 323/669-2101<br />
FAX: 323/664-9758<br />
E-Mail: tkeens@chla.usc.edu<br />
Head to Toe: Orthopaedic Aspects of the Growing Child.<br />
Orthopaedic problems are a common cause of concern for parents and a frequent reason for<br />
visiting the primary care provider. The evaluation and treatment of these problems is rapidly<br />
evolving. This course will focus on orthopaedic problems commonly encountered by primary<br />
care physicians (pediatricians and family practitioners), including congenital abnormalities of the<br />
hip and feet, fractures, sports injuries, and developmental deformities such as lower extremity<br />
bowing and leg length discrepancies. Participants will have the opportunity to actively discuss<br />
these problems with experts in the field.<br />
SATURDAY, October 18, <strong>2003</strong><br />
7:30 am to 4:30 pm<br />
Cedars-Sinai Medical Center<br />
Harvey Morse Auditorium<br />
8701 Gracie Allen Drive<br />
Los Angeles, California<br />
For additional information call the Office of Continuing Medical Education at<br />
(310) 423-5548 or 423-2935; you may also email: stokes@cshs.org<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 27
THE TAO OF PEDIATRICS AND CHINESE MEDICINE CONTINUED FROM PAGE 14<br />
CT S<strong>CA</strong>NS CONTINUED FROM PAGE 7<br />
cortisol levels have all been demonstrated, but<br />
these do not explain many of the physiological<br />
changes these points can induce. There is<br />
other promising research being conducted at the<br />
University of California Irvine by Dr. Zang Hee<br />
Cho, one of the inventors of the MRI. Utilizing<br />
the fMRI, Dr. Cho has demonstrated the effects<br />
of distal acupuncture points on blood flow in the<br />
brain. For example, when a point traditionally<br />
indicated for the treatment of ocular disorders<br />
was stimulated, the fMRI showed an increase in<br />
blood flow in the visual cortex.<br />
Unfortunately, research in acupuncture in<br />
the West is still in its infancy. There have been<br />
relatively limited numbers of Western studies<br />
done in pediatrics. Examples of some of the<br />
research in which acupuncture was shown to<br />
be effective in pediatrics include pain, postoperative<br />
nausea and vomiting, constipation,<br />
drooling, nocturnal enuresis and asthma. However,<br />
the range of conditions spans far beyond<br />
those mentioned due to the inherent energetic<br />
nature of acupuncture.<br />
Modern acupuncture needles are very fine<br />
(generally between 32 and 38 gauge). They are<br />
manufactured in sterile blister packs and are<br />
disposed of immediately after use. Children are<br />
very sensitive to the effects of acupuncture and<br />
needles do not need to be retained very long.<br />
The older the child, the longer the needles are<br />
retained. Generally, the length of the needles<br />
is between 1⁄2 and 1 inch. Many pediatric acupuncturists<br />
use very shallow insertion (5mm),<br />
especially within the Japanese traditions.<br />
Both research and anecdotal reports<br />
indicate that many children find acupuncture<br />
“positive or relaxing.” Most fears were found<br />
to be overcome through communication and<br />
positive reinforcement. Should fear continue<br />
to be an issue, there are several effective noninvasive<br />
techniques available. These include:<br />
• Microcurrent electrostimulation to acupoints<br />
• Shonishin: Japanese pediatric technique<br />
involving a set of tools to be used to<br />
stimulate strategic meridians<br />
• Magnet therapy (800-10000 gauss)<br />
• Laser therapy (1-10 mW)<br />
• External application of herbal preparations,<br />
essential oils or seeds to acupoints<br />
• Massage and acupressure<br />
Herbal Medicine<br />
Herbal medicine can be a gentle and<br />
effective therapeutic modality. In Chinese<br />
Herbology, herbs are very rarely used alone.<br />
Combining herbs allows the practitioner to<br />
customize the formula to the specific needs of<br />
the child.<br />
For example, a commonly used herbal formula<br />
from the later Han dynasty (25-220 CE)<br />
used for influenza is cinnamon twig decoction<br />
(Gui Zhi Tang). This formula includes 5 ingredients:<br />
Cinnamomum cassia, Peony lactiflora,<br />
Zingiber officianal, Ziziphus jujube, and Glycyrrhiza<br />
uralensis (honey-fried). Cinnamomum<br />
has been demonstrated to have antibiotic properties<br />
against such microorganisms as Staphylococcus<br />
aureus, ECHO virus and Salmonella<br />
typhi. It also has antipyretic and vasodilating<br />
properties. Peony lactiflora is anti-inflammatory<br />
and antibiotic in nature (Shigella sonnei,<br />
Staphylococcus aureus, herpes zoster). The<br />
remaining herbs are primarily for mitigating<br />
inflammation, and to protect, soothe, and<br />
strengthen the gastrointestinal tract. They can<br />
help alleviate symptoms such as nausea, sore<br />
throat, and abdominal discomfort. They also<br />
prevent negative interactions between incompatible<br />
herbs or other medications. While the<br />
great majority of research exists in the Chinese<br />
Medicine literature, empirically based research<br />
in the United States is less established.<br />
As the terrain begins to change, an adequately<br />
trained herbalist will modify the ingredients<br />
and dosages. Herbal medicine can also<br />
be used in conjunction with pharmaceuticals<br />
to help support the child and minimize adverse<br />
drug reactions.<br />
Dietary Therapy<br />
According to Chinese Medicine, children<br />
under the age of 6 do not have adequately<br />
developed digestive tracts. It is felt that many<br />
pediatric diseases can be directly attributed to<br />
inadequate dietary habits or the relative inability<br />
of the child to digest his/her foods. This<br />
creates toxic by-products the Chinese termed<br />
dampness. The dampness can be thought of as<br />
the undigested by-products and the heat can<br />
be thought of as the body’s response (possibly<br />
allergies, otitis media, sinus infections). Acupuncture<br />
and herbal medicine are used to correct<br />
imbalances, but if the imbalance is rooted<br />
in the digestive impairment, it may continue to<br />
recur until the diet is addressed.<br />
When used properly, Chinese Medicine<br />
can be a safe and effective adjunctive therapy<br />
for children. Research has shown that children<br />
respond favorably to acupuncture and<br />
herbal medicine. In 1992, NIH formed the<br />
National Commission for Complementary<br />
and Alternative Medicines and was allocated<br />
50 million dollars for research. Currently, the<br />
NC<strong>CA</strong>M is expecting 113.2 million dollars<br />
in funding. Presently, at Childrens Hospital<br />
of Los Angeles, we are beginning a research<br />
program in collaboration with the Magik Pain<br />
Program and the Childrens Center for Cancer<br />
and Blood Diseases examining the integration<br />
of acupuncture for decreasing pain and<br />
fear in children going through painful medical<br />
procedures.<br />
diagnostic irradiation and polymorphisms in<br />
DNA repair genes. Environmental Health<br />
Perspective. 2000; 108:495-498.<br />
3. Radiation and Pediatric Computed Tomography.<br />
National Cancer Institute. Summer<br />
2002. Website: www.cancer.gov/cancerinfo/<br />
causes/radiation-risks-pediatric-CT<br />
4. Frush, D. Pediatric CT: practical approach to<br />
diminish the radiation dose. Pediatric Radiology.<br />
2002; 32:714-717.<br />
5. FDA Public Health Notification: Reducing<br />
Radiation Risk from CT for Pediatric and<br />
Small Adult Patients. Pediatric Radiology.<br />
2002; 32:314-316.<br />
6. Donnelly LF, Emery KH, Brody AS, et al.<br />
Minimizing radiation dose for pediatric<br />
body applications of single-detector helical<br />
CT: strategies at a large children’s hospital.<br />
AJR American Journal of Roentgenology<br />
2001; 176:289-296.<br />
7. Brody A, Guillerman RP. Radiation Risk<br />
from Diagnostic Imaging. Pediatric Annals.<br />
2002;31:643-647.<br />
8. Huda, W. Radiation Dosimetry in Diagnostic<br />
Radiology. AJR American Journal of<br />
Roentgenology 1997; 169:1487-1488.<br />
FOOTNOTES<br />
1 The sievert (Sv) is the current standard international<br />
unit used to describe a human radiation<br />
dose, used preferentially over the more<br />
familiar “rad.” Sv refers to the effective<br />
dose, taking the type of radiation and tissue<br />
involved into consideration, while rad refers<br />
to the absorbed dose.<br />
ERRATA<br />
The text below was missing from Dr. Harvey<br />
Karp’s article Solving the Colic Mystery:<br />
The Fourth Trimester, the Calming Reflex<br />
and the Five “S”s, which appeared in the Fall<br />
2002 issue of California Pediatrician. California<br />
Pediatrician regrets the omission.<br />
The calming reflex and Five “S”s are<br />
presented in detail in Dr. Karp’s new<br />
book and video, “The Happiest Baby<br />
on the Block.” To learn more, visit<br />
www.thehappiestbaby.com.<br />
28 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
SED — California Region<br />
Leonard Kutnik, M.D.<br />
California Surgeon<br />
General Needed to Protect<br />
Californians<br />
The Surgeon General’s Office reports<br />
that one in ten children and adolescents<br />
suffer from a mental health<br />
illness (1), but only one in five of these children<br />
receive specialty mental health services.<br />
Unfortunately, this rate of treatment is not<br />
being achieved in the State’s health insurance<br />
program for children, the Healthy Families<br />
Program. Only one-half of one percent of<br />
enrolled children were referred to a county<br />
mental health department for evaluation and<br />
treatment of a Serious Emotional Disturbance<br />
(SED). Primary care providers (including<br />
pediatricians) are ideally positioned at the<br />
frontline to identify HFP children with mental<br />
health problems. Therefore, greater assistance<br />
is needed from primary care providers (PCPs)<br />
to refer children who present signs and symptoms<br />
of SED to county mental health programs<br />
for evaluation and treatment.<br />
The Healthy Families Program is a state<br />
and federally funded insurance program that<br />
provides health care to low-income children<br />
up to age 19 who do not qualify for Medi-Cal<br />
and do not have private health insurance. The<br />
HFP provides comprehensive mental health<br />
services through participating health plans<br />
and local county mental health departments.<br />
Basic mental health services are provided<br />
by the participating health plans. Evaluation<br />
and treatment of SED are provided by county<br />
mental health departments. Serious emotional<br />
disturbance of a child is defined in the California<br />
Welfare and Institutions Code, Section<br />
5600.3(a)(2) as a mental disorder as identified<br />
in the most recent edition of the Diagnostic and<br />
Statistical Manual of Mental Disorders (other<br />
than a primary substance use disorder or developmental<br />
disorder) which results in behavior<br />
inappropriate to the child’s age according to<br />
expected developmental norms. SED treatment<br />
services provided by county mental<br />
health departments include outpatient services,<br />
inpatient services and prescription drugs.<br />
Most children enrolled in the HFP are<br />
members of health plans that require a primary<br />
care provider (PCP). Because of the<br />
large number of children who are affiliated<br />
with a PCP, the PCP plays a crucial role in<br />
the early detection of mental health problems<br />
and in improving HFP children’s access to<br />
SED services. HFP data indicate that in 2000,<br />
approximately 57% of children enrolled in<br />
the program for 12 consecutive months saw<br />
a PCP. Reports show that most families, and<br />
to a higher degree, ethnic minority families,<br />
are more likely to seek help from primary<br />
care providers as opposed to specialty care<br />
providers. (2) Given the large number (80%)<br />
of HFP subscribers who belong to an ethnic<br />
minority group, these reports further validate<br />
the importance of the PCP in detecting mental<br />
health problems.<br />
PCPs can receive assistance from participating<br />
health plans in referring children<br />
to county mental health departments for SED<br />
The Healthy Families Program provides comprehensive mental<br />
health services through participating health plans and local county<br />
mental health departments.<br />
treatment. The health plans use a variety of<br />
methods to assist physicians in serving HFP<br />
subscribers and to communicate information<br />
about the HFP benefits. Examples of these<br />
methods include periodic newsletters and<br />
bulletins, quick reference guides, periodic luncheon<br />
meetings, electronic mail and website<br />
access. The methods used are specific to individual<br />
health plans. Physicians should call the<br />
health plans they are affiliated with for more<br />
information.<br />
In addition to the assistance the health<br />
plans provide, the California Institute of<br />
Mental Health (CIMH), with funding from<br />
the David and Lucile Packard Foundation, has<br />
developed a provider manual. This manual,<br />
Healthy Families Resources Binder, was<br />
developed through collaboration among counties,<br />
health plans, State staff and CIMH. The<br />
binder provides information about the HFP and<br />
the SED referral process that is practical and<br />
easily accessible. Specific information provided<br />
includes health plan and county mental<br />
health liaison phone numbers, flow charts for<br />
CONTINUED ON PAGE 31<br />
On April 10, <strong>2003</strong>, the Little Hoover Commission<br />
urged policy-makers to fortify California’s<br />
public health system so it can better detect and<br />
respond to a wide range of threats, from emerging<br />
diseases and hospital-acquired infections to<br />
bioterrorism.<br />
The Commission recommended the State<br />
develop expert leadership, establish standards,<br />
increase training, improve communications,<br />
and strengthen laboratory and other capacities<br />
essential to the public health infrastructure.<br />
The report — To Protect and Prevent:<br />
Rebuilding California’s Public Health System<br />
— was issued after 10 months of public meetings,<br />
interviews, and deliberations, during<br />
which an array of experts identified specific<br />
weaknesses and practical improvements to<br />
a system that has gradually eroded over the<br />
last three decades. The Commission initiated<br />
the project after the terrorist attacks of 2001<br />
revealed that the traditional capacities of the<br />
public health system to detect and respond<br />
to epidemics and other disasters had been<br />
neglected as a public attention focused on individual<br />
health care. The Commission concluded<br />
that the improvements are needed to protect all<br />
California from a range of health risks.<br />
The Commission recommended that the<br />
core public health functions be consolidated<br />
into a single state department and that the State<br />
re-establish a volunteer public health board<br />
to provide expert involvement and public<br />
accountability to the government’s efforts.<br />
The State needs to strategically develop<br />
and employ technologies and trained professionals<br />
to make sure the system detects and<br />
assesses health threats, develops the most<br />
effective responses, and communicates with<br />
health care providers and the public. Together,<br />
the reforms would redefine public health as the<br />
third component of California’s public safety<br />
triad — police, fire, and public health.<br />
A fortified public health system would<br />
reduce the risk to all Californians, ensuring<br />
capacities in times of emergency, and reducing<br />
demands on the overall health system.<br />
While the federal and state government<br />
have taken steps since September 11, 2001<br />
to repair the system, the fundamental and<br />
structural problems have not been adequately<br />
addressed in California.<br />
The Little Hoover Commission is a bipartisan<br />
and independent state agency charged<br />
with advising the Governor and Legislature on<br />
ways to improve the efficiency and effectiveness<br />
of state programs. The full Commission<br />
report is available on www.lhc.ca.gov.<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 29
A LOW-GLYCEMIC INDEX DIET IN THE TREATMENT OF PEDIATRIC OBESITY CONTINUED FROM PAGE 11<br />
ing in treatment programs. Much of this weight<br />
is regained within 12 months, with a virtually<br />
complete relapse after five years. Clinical studies<br />
of obesity treatment in children have yielded<br />
mixed results. This situation has prompted calls<br />
from experts and official agencies for the development<br />
of innovative treatment strategies. 33 The<br />
results of this study suggest that a low-GI diet<br />
may be one such approach.<br />
Children receiving the standard reducedfat<br />
diet showed no change in adjusted BMI<br />
during the course of the study, representing<br />
a modest improvement over the increase in<br />
BMI that would be expected with increasing<br />
age. By contrast, children receiving the low-GI<br />
diet showed an adjusted decrease in BMI of<br />
1.15 kg/m 2 . This result is especially interesting<br />
in that the low-GI diet involved no restriction<br />
of total energy or specific macronutrient consumption.<br />
Instead, patients in this treatment<br />
group were encouraged to eat to satiety and<br />
snack when hungry. Furthermore, the magnitude<br />
of the effect seen here may have been<br />
limited by factors inherent to an urban pediatric<br />
obesity clinic, including a heterogeneous<br />
patient population, inadequate insurance coverage<br />
for obesity management, and poverty.<br />
To our knowledge, the vast majority of<br />
pediatric obesity studies to date have tested<br />
different behavioral modification techniques<br />
or multimodality programs (behavioral<br />
therapy, diet, and physical activity together).<br />
Surprisingly few studies involving children<br />
have examined the effects of dietary composition<br />
on weight loss per se, while controlling for<br />
other interventions. In our study, by contrast,<br />
specific dietary prescriptions differed between<br />
groups, whereas dietary counseling methods<br />
(parent and child), behavioral modification<br />
techniques, ancillary recommendations (to<br />
increase physical activity and decrease inactivity),<br />
and treatment intensity did not.<br />
Regarding possible underlying mechanisms,<br />
a low-GI diet may facilitate weight<br />
loss by lowering insulin levels. High-GI<br />
diets stimulate more insulin secretion than<br />
isoenergetic, low-GI diets, as evidenced by<br />
higher postprandial insulin levels and greater<br />
c-peptide secretion. Acutely high insulin<br />
levels would tend to promote uptake of nutrients<br />
into liver, muscle, and adipose tissue;<br />
inhibit hepatic release of glucose; and suppress<br />
lipolysis. After the nutrients of a high-GI<br />
meal have been absorbed from the digestive<br />
tract, the body may have difficulty accessing<br />
stored metabolic fuels, leading to excessive<br />
hunger and overeating. Chronically, hyperinsulinemia<br />
would tend to direct nutrients from<br />
oxidation to storage. Several, though not all,<br />
epidemiological studies have shown that individuals<br />
with the highest fasting or stimulated<br />
insulin levels at baseline gain the most weight<br />
prospectively. Moreover, insulin treatment of<br />
type 2 diabetes, and intensive insulin treatment<br />
of type 1 diabetes predictably results in weight<br />
gain. In animal studies, a high-GI diet was<br />
found to increase fatty acid synthetase activity,<br />
adipocyte size, glucose incorporation into total<br />
lipids, and insulin resistance compared with a<br />
low-GI diet.<br />
Several issues relating to study design<br />
and interpretation should be addressed. First,<br />
participants were not formally randomized<br />
to treatment group. Thus, the presence of<br />
confounding influences, such as selection<br />
bias and provider effects, cannot be excluded.<br />
Second, dietary change was not monitored<br />
following intervention (as, for example, with<br />
diet records). Therefore, the degree to which<br />
noncompliance affected outcome is not known.<br />
Third, mean follow-up time was relatively<br />
short (4.3 months); long-term evaluation of the<br />
dietary treatments is beyond the scope of this<br />
study. Fourth, the target macronutrient composition<br />
of the low-GI diet differed from that of<br />
the reduced-fat diet, in an attempt to obtain the<br />
After the nutrients of a high-GI meal have been absorbed from<br />
the digestive tract, the body may have difficulty accessing stored<br />
metabolic fuels. . .<br />
lowest possible glycemic response. Therefore,<br />
the effects of this diet cannot be attributed<br />
solely to GI. In light of these qualifications, our<br />
findings should be viewed as preliminary.<br />
Nevertheless, we believe that these<br />
findings are relevant because the magnitude<br />
of the observed effect is large and remained<br />
significant after adjustment for a variety of<br />
potentially confounding factors; the low-GI<br />
diet was tested against the current standard of<br />
care; and the data are consistent with a plausible<br />
physiologic mechanism. Moreover, the<br />
study reflects experience of a major, clinical<br />
pediatric obesity program, not a specialized<br />
research protocol employing carefully selected<br />
subjects and costly interventions. Rather, our<br />
study confronted a variety of problems inherent<br />
to the outpatient treatment of childhood<br />
obesity today, including variable motivation<br />
and compliance (eg, some patients enrolled<br />
in our program at the insistence of a parent<br />
or physician, and have little interest in losing<br />
weight), limited resources (ie, inadequate<br />
insurance reimbursement), and a lengthy waiting<br />
period for clinic appointments. Thus, the<br />
findings speak to the clinical effectiveness of<br />
this dietary approach. Finally, this study underscores<br />
the need for a prospective, controlled<br />
clinical trial of a low-GI diet in the treatment<br />
of obesity.<br />
Corresponding author: David S. Ludwig,<br />
MD, PhD, Department of Medicine, Children’s<br />
Hospital, 300 Longwood Ave, Boston, MA<br />
02115 (e-mail: ludwigd@tch.harvard.edu).<br />
For references, see the original article in<br />
JAMA Archives of Pediatric and Adolescent<br />
Medicine, 2000.<br />
WHY <strong>CA</strong>LIFORNIA’S MICRA IS GOOD FOR THE NATION CONTINUED FORM PAGE 12<br />
1976 to $254.22 in 2000 (an increase of 2073%<br />
when adjusted for inflation).<br />
National MICRA<br />
Mindful of the national problem, Senator<br />
Dianne Feinstein (D-California) has courageously<br />
proposed a law modeled on California’s<br />
27-year experience of dealing fairly with<br />
injured patients and protecting access to health<br />
care.<br />
Here it is in dollars and cents: In California<br />
two years ago, an OB/GYN paid on<br />
average $47,500 for malpractice insurance.<br />
In Florida, she paid $173,000. Neurosurgeons<br />
paid $68,436 in Los Angeles County in<br />
2002, but $278,829 in Dade County, Fla., and<br />
$163,000 in suburban Detroit and New York.<br />
In California in 2002, an orthopedic surgeon<br />
paid $22,730, but in Pennsylvania $90,297.<br />
Why should patients care? It’s difficult<br />
to put a value on having doctors there when<br />
you need them. But patients in Nevada drive<br />
hundreds of miles to find obstetricians who<br />
still deliver babies. And for accident and cardiac<br />
victims, it is a matter of life and death if<br />
there is no neurosurgeon or ER doc at the local<br />
hospital.<br />
California has health care problems, but<br />
this insurance crisis isn’t one of them. That’s<br />
why the rest of the nation needs to take California’s<br />
lead and adopt medical malpractice<br />
reform.<br />
30 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
Retirement should not be dull or<br />
boring. With the increase in the average<br />
life expectancy, more and more<br />
of us can look forward to years of active life<br />
after retirement. If it is not necessary to make<br />
money, the number of choices available is<br />
truly astonishing. Fortunately this is true even<br />
for those with physical limitations. Retired<br />
pediatricians can choose to stay in touch with<br />
their profession. Alternately, this is a time to<br />
pursue some favorite activity which was limited<br />
by time available before retirement. It is<br />
even possible to go back to school and become<br />
educated in an entirely new area. A partial list<br />
of possibilities organized by category follows.<br />
Pediatric Related:<br />
Retirement Options for<br />
Pediatricians<br />
If a retired pediatrician is located in an area<br />
with access to a medical school or training<br />
program, there are opportunities for teaching.<br />
Many programs use practicing or retired pediatricians<br />
as voluntary faculty. This involves<br />
making rounds on wards or supervising students<br />
and residents in clinics for assigned periods.<br />
Selection of a clinic in a particular area in<br />
which the physician can indulge a long standing<br />
interest can be very rewarding. Malpractice<br />
insurance for the faculty is covered by the<br />
medical school or hospital in most instances.<br />
Contact can be made with the Chairman of the<br />
Pediatric Department or the Chief of the Resident<br />
Training Program.<br />
Most medical schools have a mentor program<br />
for students usually starting in the first<br />
or second year. Students are assigned to physicians<br />
in areas of specialty which they choose.<br />
Practicing physicians are particularly desirable<br />
as having different experiences from faculty.<br />
Mentoring can take minimal or more time<br />
depending on the number of students and the<br />
interpersonal chemistry involved. Information<br />
can be obtained from the Student Affairs Office<br />
of the medical school.<br />
Many communities have free clinics for<br />
families without health care coverage. These<br />
can be sponsored by religious organizations,<br />
schools or community organizations. It is possible<br />
to cover a specific time for a specified<br />
period. Malpractice insurance can be a problem<br />
for retired physicians and this should be<br />
investigated before making a commitment.<br />
Joan E. Hodgman, M.D.<br />
American Academy of Pediatrics:<br />
Each Academy Chapter has a number of<br />
committees chaired and manned by volunteer<br />
members. The number and level of activity<br />
depend largely on the interests of the chapter<br />
members. Areas that are particularly active<br />
include legislation, access to care, reimbursement,<br />
membership, violence and accident prevention,<br />
school health and international health.<br />
Participation is actively encouraged and well<br />
received. It is possible for a member with a<br />
special interest to develop a task force to work<br />
on that issue. Each chapter has staff available<br />
to assist with meeting notices, agendas and<br />
minutes. California District IX has an active<br />
State Government Affairs committee with representatives<br />
from each chapter who have been<br />
appointed because of their interest.<br />
Educational:<br />
Schools are encouraging older individuals to<br />
become students again. After retirement is an<br />
optimal time to return to school and study a<br />
subject just for pleasure. Local community colleges<br />
have little or no tuition and a full curriculum<br />
of courses, including cultural subjects such<br />
as music appreciation and art history, courses<br />
in foreign languages, drawing and sculpture are<br />
available, as well as computers. Taking a shop<br />
course is a great opportunity for a woman of<br />
a certain age to learn how to take care of the<br />
upkeep of her house, something she was not<br />
taught in her youth.<br />
Hobbies:<br />
Retirement is a time to seriously indulge a<br />
hobby. Gardening, Bridge, physical activities<br />
such as tennis, swimming and running are all<br />
available at community centers. There are<br />
competitions organized by age group for many<br />
of the activities particularly swimming, tennis<br />
and rowing. Access can be through a community<br />
senior center. Many communities have<br />
amateur performance groups where an individual<br />
can indulge a taste for singing, dancing<br />
or acting. This is also a time to polish skills in<br />
playing a musical instrument or learn to play a<br />
new one. And, one is never too old for golf.<br />
Community Service:<br />
The potential here is mind-boggling. All museums<br />
have docents who are regularly educated<br />
in the specialties of the museum and then<br />
volunteer to conduct tours for members and<br />
guests, including children’s groups. Big Brothers<br />
and Big Sisters are represented in many<br />
communities. Retired pediatricians make<br />
particularly knowledgeable candidates to support<br />
a disadvantaged child. Communities have<br />
appointed committees to advise the officials in<br />
specific areas such as cultural affairs, population<br />
growth, property density among others.<br />
Interest in community affairs could lead to<br />
entering politics as a member of the school<br />
board or city council.<br />
The above suggestions are only the tip of<br />
the iceberg. California Pediatrician would like<br />
to hear from readers with their own experiences<br />
to share. These should be sent to the<br />
author by e-mail, FAX or snail mail.<br />
Joan E. Hodgman, M.D.<br />
494 Stanford Drive, Arcadia, <strong>CA</strong> 91007<br />
(323) 226-3440 FAX<br />
hodgman@hsc.usc.edu<br />
SED CONTINUED FROM PAGE 29<br />
the SED referrals and billing processes and<br />
HFP updates. A copy of the binder can be<br />
obtained at www. cimh.org.<br />
Since PCPs play an important role in providing<br />
and coordinating care for their patients,<br />
PCPs can have a positive impact on access to<br />
appropriate treatment for SED services. Early<br />
detection and treatment of SED can restore<br />
the functioning of children with mental health<br />
disorders. Active teamwork between PCPs in<br />
private health programs and county mental<br />
health coordinators can help to assure the<br />
best outcomes of access to care and improve<br />
the lives of SED children. Toward this end,<br />
pediatricians and other providers who serve<br />
HFP enrollees are encouraged to refer children<br />
who present signs and symptoms of serious<br />
emotional disturbances to county mental health<br />
programs for SED evaluation and treatment.<br />
REFERENCES<br />
1. Burns, et al. (1995) & Shaffer, et al. (1996).<br />
The Surgeon General’s Conference Children’s<br />
Mental Health September 18 & 19,<br />
2000 – The Conference Summary<br />
2. Cooper-Patrick et al. (1999). U.S. Department<br />
of Health & Human Services (2001).<br />
A Supplement to Mental Health: A Report of<br />
the Surgeon General. The Substance Abuse<br />
and Mental Health Services Administration<br />
(SAMAHA) Report.<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>/ 31
I<br />
write in late March, as American forces<br />
entered Iraq. War brings inevitable<br />
destruction and human tragedy, and<br />
the outcome is unclear. Even with victory<br />
an implacable worldwide enemy will remain<br />
and the threat of terrorism at home will continue.<br />
Protection of our civilian population<br />
remains of paramount concern. Physicians<br />
have become acutely aware of the threat of<br />
bioterrorism, a term which includes microbial,<br />
chemical and radiological agents used indiscriminately<br />
against civilian population targets.<br />
Much has been written about the response to<br />
these threats. See www.bt.cdc.gov.<br />
We have yet to recognize that bioterror<br />
will change relationships between physicians<br />
and the community. Despite hardships and<br />
challenges, a sense of crisis can stimulate<br />
positive change. No matter what our political<br />
opinions, physicians will have to elevate our<br />
community leadership and become effective<br />
agents of progress.<br />
There are many key objectives physicians<br />
should seek today. Here are the top ten:<br />
10. Renew the importance of<br />
primary care.<br />
Primary care doctors must maintain consistent<br />
quality while treating a diverse group of<br />
patients. We pediatricians now add the role of<br />
“first responders.” Infectious diseases that were<br />
once relegated to the small print in textbooks-<br />
— the zebras — are now in play. Skin lesions<br />
take on new significance. What was once a<br />
white pimple may now be smallpox. Could<br />
that dark lesion be anthrax? Recall that one of<br />
the initial anthrax cases in 2001 involved an<br />
infant whose pediatrician recognized the lesion<br />
and saved the child’s life.<br />
9. Brush up on toxins.<br />
We hear and read about once exotic substances<br />
like VX, sarin and ricin. Physicians need to<br />
know more about these. Sarin is out there and<br />
has already been used by terrorists in Tokyo.<br />
Ricin, the preferred toxin of Iraqi agents, is a<br />
component of castor beans, which grow wild<br />
in Los Angeles. Even in “normal” times plant<br />
toxins are a potentially deadly risk to California<br />
toddlers.<br />
8. Improve our ties with health<br />
departments.<br />
Physicians’ relations with health departments<br />
LAST WORD<br />
After the Iraq War<br />
Jeffrey S. Penso, M.D., Editor, California Pediatrician<br />
and government agencies have left much to<br />
be desired in recent years. Pronouncements<br />
have appeared from on high and responses<br />
demanded. For example, recent HIPAA regulations<br />
require us to present each patient family<br />
with a multiple page document regarding<br />
privacy — quite a reading chore for a young<br />
mother with a crying, sick child. But recently<br />
relations have improved. County agencies now<br />
send us compelling materials about smallpox<br />
and other infectious diseases. There is suddenly<br />
a new respect for local clinicians. Health agencies<br />
actually request your assistance in disease<br />
detection and smallpox vaccine programs. We<br />
should reply positively to these requests.<br />
7. Become better teachers<br />
“Doctor” is Latin for “teacher” — that is our<br />
first avocation. In a time of crisis when many<br />
people are skeptical and fearful, we remain the<br />
trustworthy source of information for the families<br />
under our care. We have the responsibility<br />
and opportunity to care for physical needs and<br />
to assist communities in coping with crisis.<br />
6. Strengthen appreciation of<br />
vaccines<br />
In recent years, disinformation has poisoned<br />
public understanding about vaccines. Now<br />
our community has learned of new, very lethal<br />
diseases that may be coming to our neighborhoods.<br />
Here, again is our chance to effectively<br />
teach patients about the risks (low) and benefits<br />
(great) of vaccines. We also must bolster<br />
the Vaccines for Children Program, and eliminate<br />
its chronic shortages of prevnar and other<br />
key vaccines.<br />
5. Work with first responders<br />
First responders like firefighters and paramedics<br />
have strong ties to local hospital emergency<br />
centers. These systems, all understaffed,<br />
require additional citizen assistance even in<br />
“normal” emergency situations like earthquakes.<br />
The threat of bioterror should make<br />
us redouble efforts to strengthen response<br />
systems. Trauma centers also need appropriate<br />
funding. Citizens need to be trained in<br />
CPR and in Community Emergency Response<br />
Teams (CERT). We physicians must take the<br />
lead in these efforts.<br />
4. Eliminate legal barriers<br />
The time has come for more physicians to contribute<br />
more time in service to the community.<br />
Those who volunteer should be treated as the<br />
Good Samaritans that they are. Retired physicians<br />
and those starting careers would make<br />
excellent volunteers, but are blocked by persistent<br />
litigation issues. It is time that legislatures<br />
removed these barriers to care as part of real<br />
tort reform.<br />
3. Upgrade public health<br />
It is time to end the disgraceful underfunding<br />
of public health services in California. We need<br />
the ability to detect and monitor all illnesses<br />
that have public health implications. The barrier<br />
of political correctness must also fall. We<br />
have the power to eliminate virtually all cases<br />
of pediatric HIV. It is CDC policy that all pregnant<br />
women should be tested for HIV, unless<br />
they opt out. California does not have this<br />
policy and is out of step with sound national<br />
guidelines. The state should be brought into<br />
compliance. Children’s lives are at stake.<br />
2. Assist veterans<br />
Returning veterans should be honored for<br />
their service. Appreciation should be more<br />
than verbal. They and their families must have<br />
access to quality health care, through expansion<br />
of Healthy Families or other programs.<br />
Veterans have significant skills and positive<br />
work ethic. They would be excellent health<br />
professionals, and should be encouraged to<br />
receive training as nurses, paramedics and doctors.<br />
This would be a solution to the shortages<br />
of these professionals in our communities.<br />
1. Support nation building<br />
America has been the traditional leader in<br />
medical education throughout the planet. We<br />
have assisted higher education in Cairo and<br />
Beirut for over one century. This is, in some<br />
way, in response to the contributions Arab culture<br />
made to western science and medicine one<br />
millennium ago. Can the Middle East return to<br />
its historic tradition of tolerance and knowledge?<br />
Can America again become a beacon of<br />
learning and friendship? This task of course,<br />
will be the most difficult of all. It will require<br />
patience and bravery, and certainly the leadership<br />
of the medical community.<br />
32 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
PRESIDENT-ELECT <strong>CA</strong>NDIDATES<br />
CONTRIBUTORS<br />
Carol D. Berkowitz, MD, F<strong>AAP</strong><br />
Torrance, <strong>CA</strong><br />
Dr. Carol Berkowitz, born in New York, attended<br />
Barnard College, Columbia University College of<br />
Physicians and Surgeons, and did her pediatric training<br />
at Roosevelt Hospital. After a number of years in practice, she joined<br />
the full-time faculty at Harbor-UCLA Medical Center in Torrance, <strong>CA</strong>,<br />
where she is currently Professor and Executive Vice Chair in the Department<br />
of Pediatrics.<br />
Carol’s clinical interests have been in general and emergency pediatrics,<br />
with a focus on child maltreatment. Academically, she has been<br />
active in the area of Women in Pediatrics, having founded the Women in<br />
Medicine Special Interest Group of the Ambulatory Pediatric Association.<br />
She also served as the APA’s President.<br />
Carol currently serves on the <strong>AAP</strong>’s Committee on the Pediatric<br />
Workforce, and its subcommittee, Women in Pediatrics. She spent six<br />
years on the Board of Directors of the American Board of Pediatrics,<br />
serves on the Program Directors Committee of the ABP, and helped<br />
develop the Resident Program on Professionalism in Pediatrics. She<br />
was a pediatric program director for 20 years, and currently serves on<br />
the Accreditation Council on Graduate Medical Education. She was the<br />
Academy’s representative to the Residency Review Committee in Pediatrics,<br />
and was the Chair of the RRC and of the Council of RRC Chairs.<br />
She is currently the <strong>AAP</strong>’s representative to the Council of Medical<br />
Specialty Societies.<br />
She is the author of multiple articles and the editor of Pediatrics:<br />
A Primary Care Approach – a text used by many medical students and<br />
residents in their continuity clinic.<br />
Francis E. Rushton, Jr, MD, F<strong>AAP</strong><br />
Beaufort, SC<br />
Dr. Francis Rushton, throughout his 24 years as a<br />
practicing pediatrician, has successfully balanced a<br />
busy private practice with numerous child advocacy<br />
efforts, academic endeavors, and involvement with the<br />
American Academy of Pediatrics. Currently, Francis is senior partner of<br />
Beaufort (SC) Pediatrics, a member of the <strong>AAP</strong> Committee on Community<br />
Health Services, chapter <strong>CA</strong>TCH facilitator, and Clinical Associate<br />
Professor of Pediatrics at the University of South Carolina’s Institute for<br />
Families in Society. In recent years, he participated on the Academy’s<br />
Nominating Committee, served as president of the South Carolina<br />
Chapter of the <strong>AAP</strong>, led the state legislative committee, and chaired the<br />
Alliance for South Carolina’s Children. Dr. Rushton authored the book,<br />
Family Support in Community Pediatrics, and worked as a visiting<br />
professor at Okinawa Chubu Hospital in Japan for three months. Still<br />
seeking avenues to promote child health issues, he ran for – but lost by<br />
four votes – the SC House of Representatives in 1998.<br />
In 2001, Governor Jim Hodges presented Dr. Rushton with the<br />
Order of the Palmetto, South Carolina’s highest citizen award, for his<br />
commitment to children and pediatricians. In 2002, the Georgetown<br />
University Communities Can! Program recognized Beaufort’s collaborative<br />
early childhood team as one of five outstanding community<br />
programs nationally.<br />
Dr. Rushton attended Phillips Exeter Academy, University of<br />
Florida, Georgetown University, and University of Miami School of<br />
Medicine before completing a pediatric residency in Birmingham, AL<br />
and serving three years with the National Health Service Corps in Tennessee.<br />
He is married to Margaret and has three teenage children.<br />
To vote online, go to the <strong>AAP</strong> members-only channel and choose “Web-<br />
Based National Academy Election” under “What’s New.”<br />
Myles B. Abbott, M.D.<br />
Weighing the Radiation<br />
Risks of CT Scans<br />
Dr. Abbott is a private<br />
pediatrician in Berkeley<br />
and Orinda, California<br />
and a Clinical Professor<br />
of Pediatrics at the University of California<br />
San Francisco School of Medicine.<br />
Milton Arnold, M.D.,<br />
F<strong>AAP</strong><br />
Annual Las Vegas<br />
Seminars —25 Years of<br />
District Education and<br />
Support<br />
Dr. Arnold graduated from<br />
Franklin and Marshall College in 1948<br />
and received his M.D. from Chicago<br />
Medical School in 1952. He completed<br />
his medical education in Los Angeles and<br />
continued to practice and teach in Southern<br />
California. He has been active in<br />
both California Chapter 2, <strong>AAP</strong> and the<br />
Los Angeles Pediatric Society, holding<br />
the chairmanships of many committees.<br />
He is presently the District Chair of the<br />
Committee on Medical Education.<br />
Ron Bangasser, M.D.<br />
Why California’s MICRA is good for<br />
the Nation<br />
Dr. Bangasser is a board-certified family<br />
physician and Director of External<br />
Affairs for the Beaver Medical Group<br />
in Redlands. In March <strong>2003</strong>, he was<br />
elected President of the California Medical<br />
Association. From 2001-2002, he<br />
was Speaker of the California Medical<br />
Association House of Delegates, CMA’s<br />
policy-making body. He currently is a<br />
member of the California Delegation<br />
to the AMA and in June 2001, he was<br />
elected to AMA’s Council on Medical<br />
Service.<br />
Robert Matthew<br />
Bernstein, M.D.<br />
Adolescent Idiopathic<br />
Scoliosis<br />
Robert Matthew Bernstein,<br />
MD is director of<br />
Pediatric Orthopedic Surgery at Cedars-<br />
Sinai Medical Center’s Ahmanson<br />
Pediatric Center. He is Assistant Clinical<br />
Professor of Orthopedics at UCLA<br />
School of Medicine. Dr. Bernstein is a<br />
recognized expert in the areas of scoliosis<br />
and spinal deformity, hip dysplasia,<br />
clubfoot, arthrogryposis, and pediatric<br />
limb deficiencies.<br />
Rosalie Blazej<br />
Annual Las Vegas<br />
Seminars —25 Years of<br />
District Education and<br />
Support<br />
Ms. Blazej received her<br />
degree form Pratt Institute<br />
in 1967. She has been art director of<br />
California Pediatrician for 17 years. She<br />
is also a published writer with wide-ranging<br />
interests, including a keen interest in<br />
science. She lives in San Francisco with<br />
her husband of 35 years, Lucian Blazej.<br />
They have three grown children.<br />
Robin G. Calo, R.N., M.S., P.N.P.<br />
A “Parents’ Instructional Manual”<br />
Robin Calo obtained her M.S. degree and<br />
Pediatric Nurse Practitioner certificate<br />
from the University of California San<br />
Francisco School of Nursing. She is<br />
currently the Project Coordinator for the<br />
California Child Care Health Linkages<br />
Project, a statewide project funded by<br />
FIRST 5 California.<br />
Ronald A. Cohen M.D.,<br />
F<strong>AAP</strong><br />
Weighing the Radiation<br />
Risks of CT Scans<br />
Dr. Cohen is Director of the<br />
Deptartment of Diagnostic<br />
Imaging at Children’s Hospital,<br />
Oakland. After attending Medical<br />
School at the University of California,<br />
Davis, he was a Pediatric Resident at<br />
the University of Arizona, a Radiology<br />
Resident at Stanford University and a<br />
Pediatric Radiology fellow at Cincinnati<br />
Children’s Hospital. His special areas of<br />
interest include special applications of<br />
Computed Tomography and imaging of<br />
child abuse.<br />
Kris Calvin, M.A.<br />
District Report<br />
Ms. Calvin has been<br />
Executive Director of<br />
<strong>AAP</strong>-<strong>CA</strong> for 13 years.<br />
Prior to that, she was<br />
Manager of Maternal<br />
and Child Health Policy at the California<br />
Medical Association. Trained in<br />
health economics and child psychology<br />
and development at Stanford and UC<br />
Berkeley, Ms. Calvin staffs legislative<br />
and policy activities for the District. In<br />
her spare time she is a single mother of<br />
three.<br />
Mark A. Chesler, Ph.D.<br />
Childhood Cancer<br />
Survivors Report Life<br />
Changes<br />
Mark A. Chesler is Professor<br />
of Sociology at<br />
the University of Michigan, Ann Arbor,<br />
Michigan. He has published widely in<br />
the area of childhood cancer and its<br />
impact on the family, voluntary and<br />
self-help organizations, and race and<br />
ethnic relations. He is a past-president<br />
of the Candlelighters Childhood Cancer<br />
Foundation and the International Confederation<br />
of Childhood Cancer Parent<br />
Organizations. He is a member-advocate<br />
and consultant with a variety of other<br />
public agencies and educational organizations.<br />
He is married and has two adult<br />
children.<br />
George C.<br />
Cunningham, M.D.,<br />
M.P.H.<br />
Tandem Mass<br />
Spectrometry in Newborn<br />
Screening<br />
Dr. Cunningham has a<br />
B.S. degree from USF, an M.D. from<br />
the UCLA, and an M.P.H. from the UC<br />
Berkeley. A Board Certified pediatrician,<br />
he has been with the California Department<br />
of Health Services since 1965. He<br />
is currently Principal Investigator of the<br />
Pacific Southwest Regional Genetics<br />
Network. He has been appointed to the<br />
FDA Panel on Molecular and Genetic<br />
Testing, and serves on the Workgroup<br />
on Newborn Screening reporting to the<br />
Secretary’s Advisory Committee on<br />
Genetic Testing.<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong> / 33
Nikta Forghani, M.D.<br />
Weighing the Radiation Risks of CT<br />
Scans<br />
Dr. Forghani is a second year Resident<br />
at Children’s Hospital Oakland and a<br />
graduate of the UC Davis School of<br />
Medicine.<br />
Jeffrey I. Gold, Ph.D.<br />
Chronic Pain<br />
in Children: A<br />
Multidisciplinary<br />
Biopsychosocial<br />
Treatment Approach<br />
(Part III); The Tao of<br />
Pediatrics and Chinese Medicine<br />
Dr. Gold has specialized in the assessment,<br />
treatment, and clinical investigation<br />
of acute and chronic pain in children,<br />
adolescents, and adults with sickle cell<br />
disease and cancer. After graduating with<br />
his doctoral degree in Clinical Psychology<br />
(1999), Dr. Gold completed a post-doctoral<br />
fellowship in the Departments of<br />
Hematology/Oncology and Psychiatry<br />
at Children’s Hospital Oakland. He is<br />
currently a Clinical Assistant Professor<br />
of Pediatrics at USC, Keck School of<br />
Medicine.<br />
Joan E. Hodgman,<br />
M.D.<br />
Retirement Options for<br />
Pediatricians<br />
Dr. Hodgman received<br />
her M.D. at UCSF in<br />
1946 and pediatric<br />
internship at UC Hospital. From 1955<br />
to 1986, Joan was director of the nursery<br />
service at LA County-USC Medical<br />
Center. She has devoted her career to the<br />
American Academy of Pediatrics and has<br />
served <strong>AAP</strong> at local, state and national<br />
positions of leadership. Dr. Hodgman<br />
is a widow and has two daughters, four<br />
grandchildren, and a black labrador.<br />
Michael H. Joseph,<br />
M.D.<br />
Chronic Pain<br />
in Children: A<br />
Multidisciplinary<br />
Biopsychosocial<br />
Treatment Approach<br />
(Part III); The Tao of Pediatrics and<br />
Chinese Medicine<br />
Dr. Joseph is a pediatrician that specializes<br />
in pain management. After receiving<br />
his MD at Creighton University School<br />
of Medicine in 1993 and his pediatric<br />
residency at the UCI Medical Center Dr.<br />
Joseph completed a fellowship in Pediatric<br />
Pain Management and a postdoctoral<br />
research fellowship in Psychoneuroimmunology<br />
at UCLA Medical Center.<br />
Now as an Assistant Clinical Professor<br />
at USC Keck School of Medicine he is<br />
the Director of Pain Services at Childrens<br />
Hospital Los Angeles. At CHLA he has<br />
created a multidisciplinary service that<br />
treats both acute and chronic pain in<br />
children.<br />
Thomas G. Keens, M.D.<br />
Twenty-Five-Years of Home Mechanical<br />
Ventilation in Children: The Program at<br />
Childrens Hospital Los Angeles<br />
Dr. Keens is a Professor of Pediatrics,<br />
Physiology and Biophysics, at the Keck<br />
School of Medicine of the University of<br />
Southern California, and a member of<br />
the Division of Pediatric Pulmonology at<br />
Childrens Hospital Los Angeles.<br />
Sheila S. Kun, R.N., M.S.<br />
Twenty-Five-Years of Home Mechanical<br />
Ventilation in Children: The Program at<br />
Childrens Hospital Los Angeles<br />
Sheila Kun is a Nursing Care Manager<br />
for children on home mechanical ventilation<br />
in the Division of Pediatric Pulmonology,<br />
Childrens Hospital Los Angeles.<br />
Sudeep Kukreja, M.D.<br />
Early Hearing Detection<br />
and Intervention<br />
Dr. Kukreja is a staff<br />
Neonatologist at Children’s<br />
Hospital of Orange<br />
County. He is <strong>AAP</strong>-<strong>CA</strong><br />
Chapter 4 Champion for the Early Hearing<br />
Detection and Intervention Program<br />
as well as Chairman of Chapter 4’s International<br />
Child Health Committee. He is<br />
also currently a member of the advisory<br />
board to the California Department of<br />
Health’s Newborn Hearing Screening<br />
Program and Director of the Newborn<br />
Hearing Screening Program at Children’s<br />
Hospital of Orange County.<br />
Leonard Kutnik, M.D.<br />
SED — California Region<br />
Dr. Kutnik attended medical school<br />
at UCLA and received an MBA from<br />
UC Irvine. He practiced primary care<br />
pediatrics in San Diego for 20 years<br />
and is presently Chief Executive Officer<br />
and Medical Director for Children<br />
First HealthCare Network (CFHN) in<br />
Oakland <strong>CA</strong>. From 1991-1997, he was<br />
District Chair of California District IX,<br />
<strong>AAP</strong> and is now the chair of recently<br />
developed Pediatric Reimbursement<br />
Advisory Team.<br />
Allan Lieberthal, M.D.,<br />
F<strong>AAP</strong><br />
Culturally Appropriate<br />
Communication is Good<br />
Medical Practice<br />
Allan Lieberthal MD,<br />
F<strong>AAP</strong> is Vice-President of<br />
<strong>AAP</strong> California Chapter 2. He practices<br />
general pediatrics and clinical pediatric<br />
pulmonology at Kaiser-Permanente in<br />
Panorama City where he was Chief of<br />
Pediatrics for 13 years. He is also Director<br />
of the Kaiser Permanente Southern<br />
California Cystic Fibrosis Center and<br />
was lead physician in the development<br />
of the Kaiser Permanente Immunization<br />
Tracking System (KITS). He is Clinical<br />
Professor of Pediatrics at the University<br />
of Southern California<br />
David S. Ludwig, M.D., Ph.D.<br />
A Low-Glycemic Index Diet in the<br />
Treatment of Pediatric Obesity<br />
David Ludwig, MD, PhD, is Director of<br />
the Obesity Center at Boston Children’s<br />
Hospital and Assistant Professor of<br />
Pediatrics at Harvard Medical School.<br />
Dr. Ludwig is a graduate of Stanford<br />
University School of Medicine.<br />
Harry Pellman, M.D.<br />
Preventing Ear Infections in Children<br />
Dr. Harry Pellman is in private practice in<br />
Huntington Beach and Fountain Valley,<br />
California. He is Clinical Professor of<br />
Pediatrics at the University of California,<br />
Irvine, College of Medicine. Harry<br />
is also past president of <strong>AAP</strong> California<br />
Chapter 4. Since 1991, Dr. Pellman has<br />
been author of a monthly column, “What<br />
Parents Want to Know About...” in Pediatrics<br />
for Parents.<br />
Jeffrey S. Penso, M.D.<br />
Last Word<br />
Dr. Penso, editor of<br />
California Pediatrician,<br />
is in pediatric<br />
practice in Culver City.<br />
He did his pediatric residency<br />
at UCLA, where<br />
he is now Associate Clinical Professor of<br />
Pediatrics. Dr. Penso was the physician<br />
representative to the Healthy Families<br />
advisory panel, and led the Department<br />
of Health Services Committee on<br />
Outreach to underserved and uninsured<br />
children of California. He enjoys walks<br />
with his wife, Rebecca, and his dog.<br />
Paul Y. Qaqundah,<br />
M.D.<br />
CMA House of<br />
Delegates Report<br />
Dr. Qaqundah is Clinical<br />
Professor of Pediatrics<br />
at University of<br />
California, Irvine. He<br />
was the first president of the <strong>AAP</strong> Orange<br />
County Chapter and was elected Pediatrician<br />
of the Year by the Orange County<br />
Chapter of <strong>AAP</strong> in 1988.<br />
Trisha Roth, M.D.<br />
Selling Tobacco<br />
Products as a Public<br />
Health Issue<br />
Dr. Roth has been a<br />
practicing pediatrician<br />
for the past 30 years.<br />
Her main focuses have been policy on<br />
tobacco, alcohol and other drugs; underage<br />
drinking; verbal abuse; and ADHD.<br />
She is also currently the chair of <strong>AAP</strong>-<br />
<strong>CA</strong> Chapter 2’s committee on Substance<br />
Abuse and in October 2002 was honored<br />
with the SHARE Recovery Award for<br />
work on promoting self-help groups.<br />
Karen Sokal-<br />
Gutierrez, M.D.,<br />
M.P.H.<br />
Childcare Health Linkages<br />
ProgramDr. Sokal-<br />
Gutierrez works at the<br />
University of California,<br />
Berkeley, School of<br />
Public Health in the Health and Medical<br />
Sciences Program and the Center for<br />
Community Wellness; and the University<br />
of California, San Francisco, California<br />
Child Care Health Program. She is the<br />
chair of the <strong>AAP</strong> Chapter 1 Committee<br />
on Early Childhood and Dependent Care,<br />
on the national <strong>AAP</strong> committee on Early<br />
Brain and Child Development and the<br />
Executive Committee of the Section on<br />
Community Pediatrics.<br />
Vaughn A. Starnes, M.D.<br />
Ten-Year Experience<br />
with Pediatric<br />
Bilateral Living<br />
Donor Lobar Lung<br />
Transplantation<br />
Dr. Vaughn Starnes, Director of the<br />
Heart Institute, is one of the world’s<br />
most renowned pediatric cardiothoracic<br />
surgeons. Dr. Starnes is also the Chair<br />
of the Department of Cardiothoracic<br />
Surgery at the Keck School of Medicine<br />
of the University of Southern California.<br />
His major areas of research interest<br />
include heart transplantation, heart/lung<br />
transplantation, congenital heart surgery,<br />
lung tissue growth and development, and<br />
adult acquired heart disease.<br />
Burton F. Willis, M.D.<br />
District Report<br />
Dr. Willis is District Chairperson, California<br />
District, <strong>AAP</strong>. Dr. Willis helped<br />
establish California Chapter 4 and has<br />
served as Secretary, Program<br />
Chair, Vice-President<br />
and President of the<br />
chapter. He was a past<br />
editor of the California<br />
Pediatrician. Dr. Willis<br />
has been practicing primary<br />
care pediatrics in a<br />
multi-specialty group for over 30 years<br />
and is a Clinical Professor of Pediatrics at<br />
the University of California Irvine Medical<br />
Center, Department of Pediatrics<br />
Manisha Witmans, M.D.<br />
Twenty-Five-Years of Home Mechanical<br />
Ventilation in Children: The Program at<br />
Childrens Hospital Los Angeles<br />
Dr. Witmans is a Post-doctoral Fellow in<br />
Pediatric Pulmonology at the Childrens<br />
Hospital Los Angeles.<br />
Marlyn S. Woo, M.D.<br />
Ten-Year Experience<br />
with Pediatric<br />
Bilateral Living<br />
Donor Lobar Lung<br />
Transplantation<br />
Dr. Woo is a pediatric<br />
pulmonologist and the former Director<br />
of the Cystic Fibrosis Center at Childrens<br />
Hospital Los Angeles. She has been a<br />
member of the Childrens Hospital Los<br />
Angeles Cardiothoracic Transplant Team<br />
since its inception in 1992. Currently, Dr.<br />
Woo is an assistant professor of pediatrics<br />
at the Keck School of Medicine at<br />
the University of Southern California.<br />
Wendy Yu, M.S., L.Ac.<br />
The Tao of Pediatrics<br />
and Chinese Medicine<br />
Wendy Yu is an Oriental<br />
medical practitioner in<br />
private practice with<br />
office locations in West<br />
Los Angeles and Pasadena.<br />
She received her bachelor’s degree<br />
from Rutgers University in New Jersey<br />
and her graduate degree from Samra<br />
University of Oriental Medicine in Los<br />
Angeles. She is collaborating in clinical<br />
research with the Magik Pain Program<br />
and the Childrens Center for Cancer and<br />
Blood Diseases at Childrens Hospital of<br />
Los Angeles.<br />
Brad J. Zebrack,<br />
Ph.D., M.S.W.<br />
Childhood Cancer<br />
Survivors Report Life<br />
Changes<br />
Dr. Brad Zebrack is<br />
a research fellow at<br />
the David Geffen School of Medicine<br />
at UCLA, Department of Pediatrics,<br />
where he studies the impact of cancer on<br />
patients, survivors and their families. Dr.<br />
Zebrack obtained his doctorate degree<br />
in Social Work and Medical Sociology<br />
from the University of Michigan in<br />
1999, and has masters degrees in both<br />
social work and public health from the<br />
UC Berkeley.<br />
34 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
OFFICERS<br />
<strong>CA</strong>LIFORNIA DISTRICT<br />
District Chair<br />
Burton F. Willis, M.D.<br />
9900 Talbert, #201<br />
Fountain Valley, <strong>CA</strong> 92708<br />
(714) 965-2531<br />
burtfwill@aol.com<br />
Past District Chair<br />
Lucy Crain, M.D., M.P.H.<br />
400 Parnassus Ave.<br />
UCSF Box 0374<br />
San Francisco, <strong>CA</strong> 94143<br />
(415) 476-4988<br />
lcrain@itsa.ucsf.edu<br />
Alternate District Chair &<br />
Lead Contract Medical Director<br />
Robert Adler, M.D.<br />
4650 Sunset Blvd.,<br />
Mailstop 76<br />
Los Angeles, <strong>CA</strong> 90027<br />
(323) 669-2110<br />
radler@chla.usc.edu<br />
District Resident Coordinator<br />
Theresa Murdock-Vlautin, M.D.<br />
UCSD Medical Center<br />
200 Arbor Dr.<br />
San Diego, <strong>CA</strong> 92103<br />
tmurdockvlautin@ucsd.edu<br />
Representative, Annual<br />
Chapter Forum<br />
Quynh Kieu, M.D.<br />
11100 Warner Ave., #116<br />
Fountain Valley, <strong>CA</strong> 92708<br />
(714) 641-0850<br />
qkieu@projectvietnam.net<br />
Chair, Committee on<br />
State Government Affairs<br />
Robert Black, M.D.<br />
920 Cass St.<br />
Monterey, <strong>CA</strong> 93940<br />
(831) 372-5841<br />
Chair, Program<br />
Committee<br />
Milton Arnold, M.D.<br />
27434 Rainbow Ridge Rd.<br />
Palso Verdes Peninsula,<br />
<strong>CA</strong> 90274<br />
(310) 377-2698<br />
marncalaap@aol.com<br />
Representative, National<br />
Nominating Committee<br />
Paul H. Jewett, M.D.<br />
900 Fifth Ave. #204<br />
San Rafael, <strong>CA</strong> 94901<br />
(925) 837-2634<br />
hpjewett@aol.com<br />
Pediatric Delegate to<br />
CMA House of Delegates<br />
Paul Qaqundah, M.D.<br />
17822 Beach Blvd.,#278<br />
Huntington Beach,<br />
<strong>CA</strong> 92647<br />
(714) 842-1441<br />
pqaqundah@aol.com<br />
President, Children’s<br />
Health Systems<br />
Leonard Kutnik, M.D.<br />
1835 Alcatraz Ave.<br />
Berkeley, <strong>CA</strong> 94703<br />
(510) 428-3472 (wk)<br />
leonardak@aol.com<br />
Subspecialty Liasion<br />
Joan Hodgman, M.D.<br />
494 Stanford Drive<br />
Arcadia, <strong>CA</strong> 91007<br />
(323) 226-3406 (wk)<br />
Hodgman@hsc.usc.edu<br />
District <strong>CA</strong>TCH Representative<br />
Arnold Gold, M.D.<br />
800 Third St.<br />
Marysville, <strong>CA</strong> 95901<br />
(530) 749-3326<br />
algold@pol.net<br />
District School Health Group Chair<br />
Sidney Smith, M.D.<br />
601 Cascada Way<br />
Los Angeles, <strong>CA</strong> 90049<br />
(310) 472-8034<br />
sidsmith@ucla.edu<br />
District Young Physician<br />
Representative (YPS)<br />
Elaine Ong, M.D.<br />
25800 Industrial Blvd., Apt G362<br />
Hayward, <strong>CA</strong> 94545<br />
(510) 784-6953 (hm)<br />
District Treasurer<br />
Myles Abbott, M.D.<br />
2999 Regent St., #325<br />
Berkeley, <strong>CA</strong> 94705<br />
(925) 254-9203 (wk)<br />
mabbottmd@aol.com<br />
CHAPTER 1<br />
OFFICERS<br />
President<br />
George J. Monteverdi<br />
900 Fifth Ave. #204<br />
San Rafael, <strong>CA</strong> 94901<br />
(707) 253-8511<br />
ggmale@napanet.net<br />
Vice President<br />
Mika Hiramatsu, M.D.<br />
20101 B Lake Chabot Rd.<br />
Castro Valley, <strong>CA</strong> 94546<br />
(510) 581-1446 x126<br />
cho.dr.mhi@cho.org<br />
Secretary<br />
Yasuko Fukuda, M.D.<br />
3905 Sacramento St., #301<br />
San Francisco <strong>CA</strong> 94118<br />
(415) 752-8038<br />
Treasurer<br />
Eileen Aicardi, M.D.<br />
3641 California St.<br />
San Francisco, <strong>CA</strong> 94118<br />
(415) 668-0888<br />
eaicardi@pacbell.net<br />
Past President<br />
Paul H. Jewett, M.D.<br />
900 Fifth Ave. #204<br />
San Rafael, <strong>CA</strong> 94901<br />
(925) 837-2634<br />
hpjewett@aol.com<br />
<strong>CA</strong>TCH Facilitators<br />
Arnold Gold, M.D.<br />
(530) 749-3326<br />
Aparna Kota, M.D.<br />
(415) 202-4593<br />
CHAPTER 2<br />
OFFICERS<br />
President<br />
Elliot Weinstein, M.D.<br />
9645 Monte Vista Ave., #301<br />
Montclair, <strong>CA</strong> 91763<br />
(909) 621-0973<br />
Elst@cyberg8t.com<br />
Vice President<br />
Allan S. Lieberthal, M.D.<br />
13652 Cantara St.<br />
Panorama City, <strong>CA</strong> 91402<br />
(818) 375-2412<br />
Allan.S.Lieberthal@kp.org<br />
Secretary<br />
Luis Montes, M.D.<br />
Childrens Hospital Los Angeles<br />
4650 Sunset Blvd.<br />
Los Angeles, <strong>CA</strong> 90027<br />
(323) 669-2231<br />
lmontes@chla.usc.edu<br />
Treasurer<br />
Howard Reinstein, M.D.<br />
5400 Balboa Blvd., Suite 103<br />
Encino, <strong>CA</strong> 91316<br />
(818) 784-5437<br />
RhineHow@aol.com<br />
Past President<br />
Steven A. Feig, M.D.<br />
3756 Santa Rosalia Dr., #600<br />
Los Angeles, <strong>CA</strong> 90008<br />
(323) 299-3200<br />
Pedsdoc2@aol.com<br />
Program Chairman<br />
Milton I. Arnold, M.D.<br />
27434 Rainbow Ridge Rd.<br />
Palso Verdes Peninsula,<br />
<strong>CA</strong> 90274<br />
(310) 377-2698<br />
marncalaap@aol.com<br />
<strong>CA</strong>TCH Facilitator<br />
Elisa Nicholas, M.D.<br />
Miller Children’s Hospital<br />
2801 Atlantic Ave., Box 1428<br />
Long Beach, <strong>CA</strong> 90806<br />
(310) 933-0430<br />
enicholas@memorialcare.org<br />
CHAPTER 3<br />
OFFICERS<br />
President<br />
Gene Nathan, M.D.<br />
10862 Calle Verde<br />
La Mesa, <strong>CA</strong> 91941<br />
(619) 660-5400<br />
gnathan@chsd.org<br />
Vice President<br />
Amethyst Cureg, M.D.<br />
3851 Rosecrans St. (MSP511H)<br />
P.O. Box 85222<br />
San Diego, <strong>CA</strong> 92186<br />
(619) 692-8819<br />
amethyst.cureg@sdcounty.ca.gov<br />
Secretary/Treasurer<br />
Donald T. Miller, M.D., MPH<br />
408 Cassidy Street<br />
Oceanside, <strong>CA</strong> 92054<br />
(760) 757-4566<br />
dmiller@nchs-health.org<br />
Past President<br />
Stuart A. Cohen, M.D.<br />
6699 Alvarado Road, #2200<br />
San Diego, <strong>CA</strong> 92120<br />
(619) 265-3400<br />
schoen98@ipninet.com<br />
<strong>CA</strong>TCH Facilitator<br />
Paul Parker, M.D.<br />
408 Cassidy Street<br />
Oceanside, <strong>CA</strong> 92054<br />
(760) 757-4566<br />
CHAPTER 4<br />
OFFICERS<br />
President<br />
Quynh Kieu, M.D.<br />
11100 Warner Ave., #116<br />
Fountain Valley, <strong>CA</strong> 92708<br />
(714) 641-0850<br />
qkieu@projectvietnam.net<br />
Vice President<br />
Marc Lerner, M.D.<br />
University of California, Irvine<br />
Gottschalk Medical Plaza<br />
#1 Medical Plaza Dr.<br />
Irvine, <strong>CA</strong> 92697<br />
(949) 824-8600<br />
malerner@uci.edu<br />
Secretary/Treasurer<br />
Maria Tupas, M.D.<br />
CHOC<br />
455 S. Main St.<br />
Orange, <strong>CA</strong> 92868<br />
(714) 516-4238<br />
mtupas@choc.org<br />
Past President<br />
Harry Pellman, M.D.<br />
9900Talbert #201<br />
Fountain Valley, <strong>CA</strong> 92708<br />
(714) 965-2531<br />
hpellman@earthlink.net<br />
CHOC Representative<br />
James D. Korb, M.D.<br />
CHOC<br />
455 S. Main St.<br />
Orange, <strong>CA</strong> 92668<br />
(714) 532-8338<br />
<strong>CA</strong>TCH Facilitators<br />
Paul Qaqundah, M.D.<br />
17822 Beach Blvd., #278<br />
Huntington Beach, <strong>CA</strong> 92647<br />
(714) 842-1441<br />
Mohan Kumaratne, M.D.<br />
17692 Beach Blvd., #200<br />
Huntington Beach, <strong>CA</strong> 92647<br />
(714) 847-6975<br />
UCI Representative<br />
Feizal Waffarn, M.D.<br />
Department of Pediatrics<br />
UCI Medical Center<br />
101 City Drive South<br />
Orange, <strong>CA</strong> 92868<br />
(714) 456-8470<br />
<strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong> / 35
COUNCIL ON<br />
CHILD HEALTH<br />
CHAPTER 1<br />
Behavioral/Developmental<br />
J. Lane Tanner, M.D.<br />
Renee Wachtel, M.D.<br />
Child Abuse<br />
James Crawford, M.D.<br />
Kevin Coulter, M.D.<br />
Children with Disabilities<br />
Donald Mangravite, M.D.<br />
Felice W. Parisi, M.D.<br />
Community Health<br />
Aparna Kota, M.D.<br />
Early Childhood<br />
Adoption/Dependent Care<br />
Karen Sokal-Gutierrez, M.D.<br />
Environmental Health<br />
Brian Linde, M.D.<br />
Mark D. Miller, M.D.<br />
Infectious Disease<br />
Dean Blumberg, M.D.<br />
Medical Informatics<br />
Mark M. Simonian, M.D.<br />
Nominating Committee<br />
Myles Abbott, M.D.<br />
School Health<br />
Diane Dooley, M.D.<br />
Renee Wachtel, M.D.<br />
Substance Abuse<br />
Seth Ammerman, M.D.<br />
Martin J. Joye, M.D.<br />
Young Physicians<br />
Nelson Branco, M.D.<br />
Shannon Udovic-Constant, M.D.<br />
Youth<br />
Tonya Chaffee, M.D.<br />
CHAPTER 2<br />
Injury Prevention<br />
Mary Anne Limbos, M.D.<br />
AIDS<br />
Audra A. DeVeikis, M.D.<br />
Bioethics<br />
Joan Hodgman, M.D.<br />
Child Abuse<br />
Jess Diamond, M.D.<br />
Children with<br />
Disabilities/CCS<br />
Robert Jacobs, M.D.<br />
Committee on Breastfeeding<br />
Touraj Shafai, M.D.<br />
Environmental Health<br />
Harvey Karp, M.D.<br />
Fetus and Newborn<br />
George Franco, M.D.<br />
Foster Care and Adoptions<br />
Kerry English, M.D.<br />
Hospital Care<br />
Harold N. Amer, M.D.<br />
Infectious Disease<br />
Wilbert Mason, M.D.<br />
Mental Health<br />
Eleanore U. Meyer, M.D.<br />
Pediatric Emergency<br />
Medicine<br />
James Seidel, M.D.,Ph.D.<br />
School Health<br />
Sidney Smith, M.D.<br />
Substance Abuse<br />
Trisha Roth, M.D.<br />
Youth/Adolescence<br />
Curren W. Warf, M.D.<br />
CHAPTER 3<br />
Access to Care<br />
Bronwen Anders, M.D.<br />
Adoption/Foster Care<br />
Gene Nathan, M.D.<br />
Breastfeeding Coordinator<br />
Nancy Wight, M.D.<br />
Child Abuse<br />
Cynthia Kuelbs, M.D.<br />
Children with Disabilities<br />
Howard Wolfinger, M.D.<br />
Day Care<br />
Laurel Leslie, M.D.<br />
Emergency Medicine<br />
Jim Harley, M.D.<br />
Fetus & Newborn<br />
David Golembeski, M.D.<br />
Hospital Care<br />
Erin Stucky, M.D.<br />
Infectious Disease<br />
John Bradley, M.D.<br />
Injury Prevention<br />
Tom Page, M.D. &<br />
Sylvia Micik, M.D.<br />
Mental Health<br />
Martin Stein, M.D.<br />
Healthy Tomorrows<br />
Laura Clapper, M.D.<br />
School Health<br />
Gene Nathan, M.D.<br />
Sports Medicine<br />
Henry Chambers, M.D.<br />
CHAPTER 4<br />
Injury, Violence, and<br />
Poison Prevention<br />
Phyllis Agran, M.D.<br />
Alberto Gedissman, M.D.<br />
Breastfeeding Coordinator<br />
Harry Pellman, M.D.<br />
Child Care<br />
Maria Tupas, M.D.<br />
Children with Special Needs<br />
Arleen Downing, M.D.<br />
Anju Khanijou, M.D.<br />
International Health<br />
Quynh Kieu, M.D.<br />
Mohan Kumaratne, M.D.<br />
Sudeep Kukreja, M.D.<br />
Practice Management<br />
Mohan Kumaratne, M.D.<br />
Victoria Jackson, M.D.<br />
School Health and Nutrition<br />
Chris Koutures, M.D.<br />
Paul Qaqundah, M.D.<br />
COUNCIL ON<br />
PEDIATRIC PRACTICE<br />
CHAPTER 1<br />
<strong>CA</strong>TCH<br />
Aparna Kota, M.D.<br />
Medical Education<br />
Gena Lewis, M.D.<br />
Membership<br />
Devi Ananda, M.D.<br />
Newsletter<br />
Mika Hiramatsu, M.D.<br />
Mark Simonian, M.D.<br />
Public Relations<br />
Mike Harris, M.D.<br />
CHAPTER 2<br />
Electronics Communications<br />
Committee<br />
Oved Fattal, MD, Chair<br />
Legislation<br />
Jeffrey S. Penso, M.D.<br />
Membership<br />
Sheila Phillips, M.D.<br />
Nominating<br />
Lawrence Ross, M.D.<br />
Pediatric Practice<br />
Jeffrey S.Penso, M.D.<br />
Program<br />
Milton Arnold, M.D.<br />
Public Relations<br />
Howard Reinstein, M.D.<br />
Publications<br />
Elliot Weinstein, M.D.<br />
Resident Section<br />
Martha Rivera, M.D.<br />
CHAPTER 3<br />
Federal Access Coordinator<br />
Gene Nathan, M.D.<br />
Future of Pediatric<br />
Education<br />
Laurel Leslie, M.D.<br />
Kaiser Permanente Rep.<br />
Joe McQuaide, M.D.<br />
Legislation<br />
Norman Gollub, M.D. &<br />
Cynthia Kuelbs, M.D.<br />
Membership<br />
Donald Miller, M.D.<br />
Managed Care<br />
Norman Gollub, M.D.<br />
North County Rep<br />
Donald Miller, M.D.<br />
Programs<br />
Allen Schwartz, M.D.<br />
Public Relations<br />
Stuart Cohen, M.D.<br />
CHAPTER 4<br />
Continuing Medical Education<br />
Harry Pellman, M.D.<br />
Legislation<br />
Quynh Kieu, M.D.<br />
Management<br />
Burton Willis, M.D.<br />
Membership<br />
Marc Lerner, M.D.<br />
Nominating Committee<br />
Alberto Gedissman, M.D.<br />
Maria Minon, M.D.<br />
Harry Pellman, M.D.<br />
Public Policy/Advocacy<br />
Quynh Kieu, M.D.<br />
Pediatric Research in<br />
Office Setting<br />
Harry Pellman, M.D.<br />
Valery Brouwer, M.D.<br />
Practice Management<br />
Mohan Kumaratne, M.D.<br />
Victoria Jackson<br />
Would you like to be on the mailing list?<br />
California Pediatrician is the official publication of California<br />
District IX, American Academy of Pediatrics. If you would like<br />
to be on the regular mailing list for California Pediatrician, please<br />
complete the following form.<br />
Name. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Address . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Mail this form to: DISTRICT EXECUTIVE DIRECTOR<br />
Kris Calvin, 853 Ramona Ave., Albany, <strong>CA</strong> 94706<br />
36 / <strong>CA</strong>LIFORNIA <strong>PEDIATRICIAN</strong> — SPRING <strong>2003</strong>
ANGELA ANDERSON, M.D.<br />
Associate Professor of Pediatrics, Brown University<br />
Medical School; Attending Physician and Toxicologist,<br />
Hasbro Children’s Hospital, Providence, Rhode Island.<br />
DANIEL L. COURY, M.D., F.A.A.P.<br />
Chief, Section of Behavioral – Developmental-<br />
Pediatrics, Columbus Children’s Hospital, The Ohio<br />
State University, Columbus, Ohio.<br />
KATHRYN EDWARDS, M.D., F.A.A.P.<br />
Professor of Pediatrics, Vice Chair for Clinical Research,<br />
Department of Pediatrics, Vanderbilt University,<br />
Nashville, Tennessee.<br />
LEWIS R. FIRST, M.D., F.A.A.P.<br />
Professor and Chair, Department of Pediatrics,<br />
University College of Vermont, Burlington, Vermont.<br />
FRANCINE R. KAUFMAN, M.D., F.A.A.P.<br />
Professor of Pediatrics, Keck School of Medicine of<br />
University of Southern California; Chief, Center for<br />
Diabetes and Endocrinology, Childrens Hospital of Los<br />
Angeles, California.<br />
ANTHONY J. MANCINI, M.D., F.A.A.D., F.A.A.P.<br />
Assistant Professor of Pediatrics and Dermatology,<br />
Northwestern University Medical School, Chicago,<br />
Illinois.<br />
<br />
Pediatric Update <strong>AAP</strong>, California Chapters 1, 2, 3, 4 Venetian Hotel, November 20-23, <strong>2003</strong><br />
Please remit to Venetian Hotel, 3355 Las Vegas Blvd, South, Las Vegas, NV 89109 Phone 877-2VENICE.<br />
Name. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Address . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
City . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . State . . . . . . . . . Zip. . . . . . . . . .<br />
Phone # ( ) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Accommodations Requested: ____ Luxury ($189) ____ Bella ($239) Number in Party . . . . . . .<br />
Arrival Date/Time . . . . . . . . . . . . . . . . . . . . . . . . Departure Date/Time . . . . . . . . . . . . . . . . . . . . .<br />
Hotel Accommodations: 300 suites of the Venetian Hotel will be available to registrants. Special rates are<br />
$189 per day for Luxury (1 king), $239 for Bella (2 queens), subject to tax. Charge for extra person: $35<br />
a day. Children under 12 are free. Note: Special rates will be available only until October 20, <strong>2003</strong> or<br />
until all 300 blocked suites are taken. Once these are taken, regular hotel rates will apply. Chapter 2<br />
disclaims any responsibility for hotel arrangements.<br />
WE RECOMMEND YOU MAKE RESERVATIONS FAR IN ADVANCE OF THE MEETING.<br />
Your credit card is acceptable in payment. MasterCard VISA American Express (circle one)<br />
#. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Exp. Date. . . . . . . . . . . . . . . . . Signature . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Please make checks payable and send to: Venetian Hotel, 3355 Las Vegas Blvd. South, Las Vegas,<br />
Nevada 89109. Phone 877-2VENICE.<br />
<br />
Pediatric Update <strong>AAP</strong>, California Chapters 1, 2, 3, 4 Venetian Hotel, November 20-23, <strong>2003</strong><br />
Please remit this part to <strong>AAP</strong>, PO Box 2134, Inglewood <strong>CA</strong> 90305 Return policy: Refunds will be<br />
made in full if meeting reservation cancellation is received prior to Oct. 20, <strong>2003</strong>.<br />
Name. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Date. . . . . . . . . . . . .<br />
Address . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
City . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . State. . . . . . . . . . . . Zip. . . . . . . . . . . . . .<br />
Phone ( ). . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Fax ( ) . . . . . . . . . . . . . . . . . . . . . .<br />
Email. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Tuition Fee: (tuition does not include luncheon seminar costs) Before Oct. 15 After Oct. 15<br />
Physicians: Members of <strong>AAP</strong> California Chapters 1, 2, 3, & 4 . . . . $550. . . . . $575 . . . . . . $______<br />
All other <strong>AAP</strong> Members & Physician Non-members . . . . . . . . . . . $600 . . . . $625 . . . . . . $______<br />
Pediatric Residents . . . . Hospital: . . . . . . . . . . . . . . . . . . . . . . . . . . $325 . . . . $350 . . . . . . $______<br />
Allied Health Personnel Category: . . . . . . . . . . . . . . . . . . . . . . . . . $325 . . . . $350 . . . . . . $______<br />
Physicians Emeritus with California Chapters 1, 2, 3, 4 . . . . . . . . . $100. . . . . $125 . . . . . . $______<br />
Luncheon Seminars: $35 each. You may select one for each day. Please give a second and third<br />
choice. Attendance is limited. Preference assignment will depend on order of receipt of registration.<br />
Fri. Seminar: 1, 2, 3, 4, 5, 6 (enter number in box) Pref: 1o 2o 3o $35 . . . $______<br />
Sat. Seminar: 1, 2, 3, 4, 5, 6 (enter number in box) Pref: 1o 2o 3o $35 . . . $______<br />
Your credit card is acceptable in payment. MasterCard VISA (circle one)<br />
Total<br />
$______<br />
#. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Exp. Date. . . . . . . . . . . . . . . . . Signature . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Please make checks payable to: <strong>AAP</strong>, Chapter 2 and return to: P.O. Box 2134, Inglewood, <strong>CA</strong> 90305.<br />
Phone: 310/540-6240 or 323/757-1198 for more information.
<strong>CA</strong>LENDAR<br />
May 14, <strong>2003</strong><br />
Los Angeles<br />
Pediatric Society<br />
Annual <strong>Spring</strong> Meeting and Parmelee<br />
Lecture<br />
Sportsmen’s Lodge, Studio City,<br />
California,<br />
Call (310) 540-6240 or (323) 757-1198<br />
or email aapcach2@aol.com<br />
www.lapedsoc.org<br />
May 24-26, <strong>2003</strong><br />
California Chapter 1, <strong>AAP</strong><br />
Annual <strong>Spring</strong> Meeting<br />
Pediatric Symposium and<br />
Legislative Update<br />
Hyatt Regency Hotel, Monterey,<br />
California<br />
Call (415) 459-4775<br />
www.aapca1.org<br />
June 29-July 5, <strong>2003</strong><br />
University Childrens Medical Group and<br />
California Chapter 2, <strong>AAP</strong><br />
Pediatrics in the Islands …<br />
Clinical Pearls<br />
Hyatt Regency Maui Resort, Hawaii<br />
Call (323) 669-2305 or (800) 354-3263<br />
(800) 3-KID-CME www.ucmg.org<br />
September 18-21, <strong>2003</strong><br />
Los Angeles Pediatric Society<br />
60th Annual Brennemann<br />
Memorial Lectures<br />
Bahia Hotel, Mission<br />
Bay, San Diego,<br />
California<br />
Call (310) 540-6240 or<br />
(323) 757-1198<br />
or email aapcach2@aol.com<br />
www.lapedsoc.org<br />
October 10-12, <strong>2003</strong><br />
California Chapter 4, <strong>AAP</strong><br />
Current Advances in Pediatrics<br />
Irvine Marriott Hotel<br />
Irvine, California<br />
Call (714) 971-0695<br />
or email ca4aap@sbcglobal.net<br />
October 11-17, <strong>2003</strong><br />
University Childrens Medical Group and<br />
California Chapter 2, <strong>AAP</strong><br />
Aloha Update: Pediatrics®<br />
Hyatt Regency Kauai Resort & Spa,<br />
Kauai, Hawaii<br />
Call (323) 669-2305 or (800) 354-3263<br />
(800) 3-KID-CME www.ucmg.org<br />
November 20-23, <strong>2003</strong><br />
California Chapters 1, 2, 3, 4, <strong>AAP</strong><br />
Pediatric Update, 25th Annual<br />
Las Vegas Seminars<br />
Venetian Hotel, Las Vegas Nevada<br />
Call (323) 757-1198 or email<br />
aapcach2@aol.com www.aapca2.org<br />
December 6, <strong>2003</strong><br />
California Chapter 1<br />
Pediatric Infectious Disease Symposium<br />
San Francisco, California<br />
Call (415) 459-4775<br />
January 14, 2004<br />
California Chapter 2, <strong>AAP</strong><br />
Is There Life After Residency?<br />
Courtyard by Marriot,<br />
Marina Del Rey, California<br />
Call (310) 540-6240 or (323) 757-1198<br />
or email aapcach2@aol.com<br />
www.aapca2.org<br />
February 14-20, 2004<br />
University Childrens Medical Group and<br />
California Chaper 2, <strong>AAP</strong><br />
Pediatric Potpuri®<br />
Hawaii<br />
Call (323) 669-2305, (800) 354-3263, or<br />
(800) 3-KID-CME www.ucmg.org<br />
March 4-7, 2004<br />
California Chapter 2, <strong>AAP</strong>, cosponsored<br />
by the Los Angeles Pediatric Society and<br />
Southwestern Pediatric Society<br />
Combined Southern California Pediatric<br />
Postgraduate Meeting—<br />
Clinical Pediatrics<br />
Hilton Palm <strong>Spring</strong>s Reosrt,<br />
Palm <strong>Spring</strong>s, California<br />
Call (310) 540-6240 or (323) 757-1198<br />
or email aapcach2@aol.com<br />
www.aapca2.org<br />
April 15-18, 2004<br />
California Chapter 2, <strong>AAP</strong><br />
Advances in Pediatrics, 15th Annual<br />
Las Vegas Postgraduate Meeting<br />
Flamingo Hotel, Las Vegas, Nevada<br />
Call (310) 540-6240 or (323) 757-1198<br />
or email aapcach2@aol.com<br />
www.aapca2.org<br />
July 3-9, 2004<br />
University Childrens<br />
Medical Group and<br />
California Chapter 2,<br />
<strong>AAP</strong><br />
Pediatrics in the<br />
Islands...Clinical Pearls<br />
Hawaii<br />
Call (323) 669-2305 or (800) 354-3263<br />
(800) 3-KID-CME www.ucmg.org<br />
American Academy of Pediatrics<br />
California District<br />
853 Ramona Ave.<br />
Albany, <strong>CA</strong> 94706<br />
Address Service Requested<br />
PRSRT STD<br />
U.S. POSTAGE<br />
PAID<br />
Tucson, AZ<br />
Permit No. 271