94. Hypospadias - Global HELP
94. Hypospadias - Global HELP
94. Hypospadias - Global HELP
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
552 <strong>Hypospadias</strong><br />
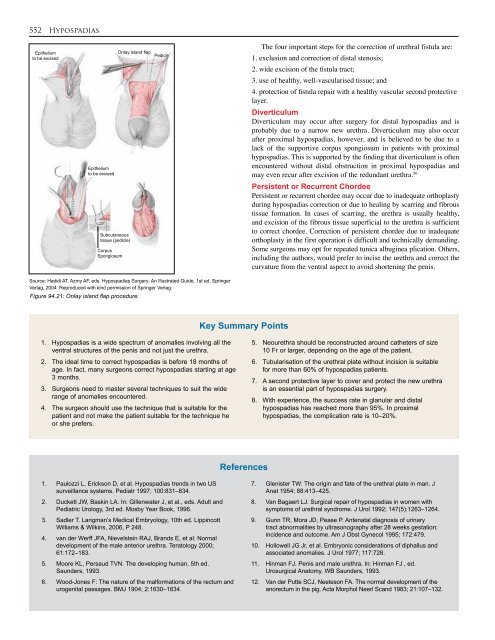
Epithelium<br />
to be excised<br />
Onlay island flap<br />
Pedicle<br />
The four important steps for the correction of urethral fistula are:<br />
1. exclusion and correction of distal stenosis;<br />
2. wide excision of the fistula tract;<br />
3. use of healthy, well-vascularised tissue; and<br />
4. protection of fistula repair with a healthy vascular second protective<br />
layer.<br />
Diverticulum<br />
Diverticulum may occur after surgery for distal hypospadias and is<br />
probably due to a narrow new urethra. Diverticulum may also occur<br />
after proximal hypospadias, however, and is believed to be due to a<br />
lack of the supportive corpus spongiosum in patients with proximal<br />
hypospadias. This is supported by the finding that diverticulum is often<br />
encountered without distal obstruction in proximal hypospadias and<br />
may even recur after excision of the redundant urethra. 56<br />
Persistent or Recurrent Chordee<br />
Persistent or recurrent chordee may occur due to inadequate orthoplasty<br />
during hypospadias correction or due to healing by scarring and fibrous<br />
tissue formation. In cases of scarring, the urethra is usually healthy,<br />
and excision of the fibrous tissue superficial to the urethra is sufficient<br />
to correct chordee. Correction of persistent chordee due to inadequate<br />
orthoplasty in the first operation is difficult and technically demanding.<br />
Some surgeons may opt for repeated tunica albuginea plication. Others,<br />
including the authors, would prefer to incise the urethra and correct the<br />
curvature from the ventral aspect to avoid shortening the penis.<br />
Epithelium<br />
to be excised<br />
Subcutaneous<br />
tissue (pedicle)<br />
Corpus<br />
Spongiosum<br />
Source: Hadidi AT, Azmy AF, eds. <strong>Hypospadias</strong> Surgery: An Illustrated Guide, 1st ed. Springer<br />
Verlag, 2004. Reproduced with kind permission of Springer Verlag.<br />
Figure <strong>94.</strong>21: Onlay island flap procedure.<br />
Key Summary Points<br />
1. <strong>Hypospadias</strong> is a wide spectrum of anomalies involving all the<br />
ventral structures of the penis and not just the urethra.<br />
2. The ideal time to correct hypospadias is before 18 months of<br />
age. In fact, many surgeons correct hypospadias starting at age<br />
3 months.<br />
3. Surgeons need to master several techniques to suit the wide<br />
range of anomalies encountered.<br />
4. The surgeon should use the technique that is suitable for the<br />
patient and not make the patient suitable for the technique he<br />
or she prefers.<br />
5. Neourethra should be reconstructed around catheters of size<br />
10 Fr or larger, depending on the age of the patient.<br />
6. Tubularisation of the urethral plate without incision is suitable<br />
for more than 60% of hypospadias patients.<br />
7. A second protective layer to cover and protect the new urethra<br />
is an essential part of hypospadias surgery.<br />
8. With experience, the success rate in glanular and distal<br />
hypospadias has reached more than 95%. In proximal<br />
hypospadias, the complication rate is 10–20%.<br />
References<br />
1. Paulozzi L, Erickson D, et al. <strong>Hypospadias</strong> trends in two US<br />
surveillance systems. Pediatr 1997; 100:831–834.<br />
2. Duckett JW, Baskin LA. In: Gillenwater J, et al., eds. Adult and<br />
Pediatric Urology, 3rd ed. Mosby Year Book, 1996.<br />
3. Sadler T. Langman’s Medical Embryology, 10th ed. Lippincott<br />
Williams & Wilkins, 2006, P 248.<br />
4. van der Werff JFA, Nievelstein RAJ, Brands E, et al: Normal<br />
development of the male anterior urethra. Teratology 2000;<br />
61:172–183.<br />
5. Moore KL, Persaud TVN. The developing human, 5th ed.<br />
Saunders, 1993.<br />
6. Wood-Jones F: The nature of the malformations of the rectum and<br />
urogenital passages. BMJ 1904; 2:1630–1634.<br />
7. Glenister TW: The origin and fate of the urethral plate in man. J<br />
Anat 1954; 88:413–425.<br />
8. Van Bagaert LJ. Surgical repair of hypospadias in women with<br />
symptoms of urethral syndrome. J Urol 1992; 147(5):1263–1264.<br />
9. Gunn TR, Mora JD, Pease P. Antenatal diagnosis of urinary<br />
tract abnormalities by ultrasonography after 28 weeks gestation:<br />
incidence and outcome. Am J Obst Gynecol 1995; 172:479.<br />
10. Hollowell JG Jr, et al. Embryonic considerations of diphallus and<br />
associated anomalies. J Urol 1977; 117:728.<br />
11. Hinman FJ. Penis and male urethra. In: Hinman FJ , ed.<br />
Urosurgical Anatomy. WB Saunders, 1993.<br />
12. Van der Putte SCJ, Neeteson FA. The normal development of the<br />
anorectum in the pig. Acta Morphol Neerl Scand 1983; 21:107–132.


![Clubfoot: Ponseti Management [Vietnamese] - Global HELP](https://img.yumpu.com/51276842/1/184x260/clubfoot-ponseti-management-vietnamese-global-help.jpg?quality=85)



![Steenbeek Brace For Clubfoot [2nd Edition] - Global HELP](https://img.yumpu.com/46612972/1/190x245/steenbeek-brace-for-clubfoot-2nd-edition-global-help.jpg?quality=85)


![Basics Of Wound Care [Indonesia] - Global HELP](https://img.yumpu.com/41566370/1/190x245/basics-of-wound-care-indonesia-global-help.jpg?quality=85)
