Tumoral, quasitumoral and pseudotumoral lesions of the ... - Siapec
Tumoral, quasitumoral and pseudotumoral lesions of the ... - Siapec
Tumoral, quasitumoral and pseudotumoral lesions of the ... - Siapec
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
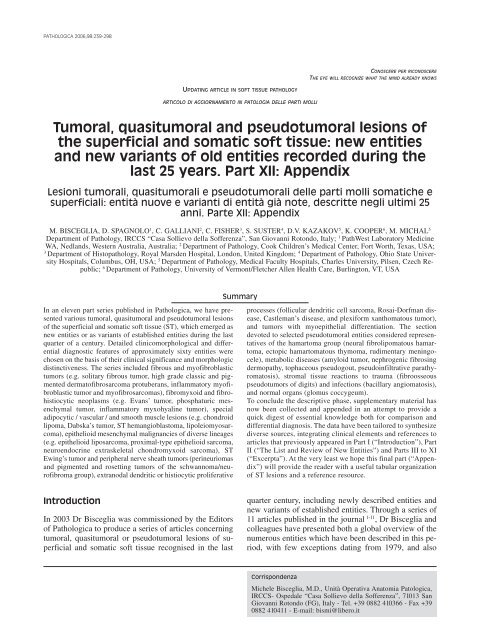
PATHOLOGICA 2006;98:239-298<br />
CONOSCERE PER RICONOSCERE<br />
THE EYE WILL RECOGNIZE WHAT THE MIND ALREADY KNOWS<br />
UPDATING ARTICLE IN SOFT TISSUE PATHOLOGY<br />
ARTICOLO DI AGGIORNAMENTO IN PATOLOGIA DELLE PARTI MOLLI<br />
<strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong><br />
<strong>the</strong> superficial <strong>and</strong> somatic s<strong>of</strong>t tissue: new entities<br />
<strong>and</strong> new variants <strong>of</strong> old entities recorded during <strong>the</strong><br />
last 25 years. Part XII: Appendix<br />
Lesioni tumorali, <strong>quasitumoral</strong>i e <strong>pseudotumoral</strong>i delle parti molli somatiche e<br />
superficiali: entità nuove e varianti di entità già note, descritte negli ultimi 25<br />
anni. Parte XII: Appendix<br />
M. BISCEGLIA, D. SPAGNOLO 1 , C. GALLIANI 2 , C. FISHER 3 , S. SUSTER 4 , D.V. KAZAKOV 5 , K. COOPER 6 , M. MICHAL 5<br />
Department <strong>of</strong> Pathology, IRCCS “Casa Sollievo della S<strong>of</strong>ferenza”, San Giovanni Rotondo, Italy; 1 PathWest Laboratory Medicine<br />
WA, Nedl<strong>and</strong>s, Western Australia, Australia; 2 Department <strong>of</strong> Pathology, Cook Children’s Medical Center, Fort Worth, Texas, USA;<br />
3<br />
Department <strong>of</strong> Histopathology, Royal Marsden Hospital, London, United Kingdom; 4 Department <strong>of</strong> Pathology, Ohio State University<br />
Hospitals, Columbus, OH, USA; 5 Department <strong>of</strong> Pathology, Medical Faculty Hospitals, Charles University, Pilsen, Czech Republic;<br />
6 Department <strong>of</strong> Pathology, University <strong>of</strong> Vermont/Fletcher Allen Health Care, Burlington, VT, USA<br />
Summary<br />
In an eleven part series published in Pathologica, we have presented<br />
various tumoral, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong><br />
<strong>of</strong> <strong>the</strong> superficial <strong>and</strong> somatic s<strong>of</strong>t tissue (ST), which emerged as<br />
new entities or as variants <strong>of</strong> established entities during <strong>the</strong> last<br />
quarter <strong>of</strong> a century. Detailed clinicomorphological <strong>and</strong> differential<br />
diagnostic features <strong>of</strong> approximately sixty entities were<br />
chosen on <strong>the</strong> basis <strong>of</strong> <strong>the</strong>ir clinical significance <strong>and</strong> morphologic<br />
distinctiveness. The series included fibrous <strong>and</strong> my<strong>of</strong>ibroblastic<br />
tumors (e.g. solitary fibrous tumor, high grade classic <strong>and</strong> pigmented<br />
dermat<strong>of</strong>ibrosarcoma protuberans, inflammatory my<strong>of</strong>ibroblastic<br />
tumor <strong>and</strong> my<strong>of</strong>ibrosarcomas), fibromyxoid <strong>and</strong> fibrohistiocytic<br />
neoplasms (e.g. Evans’ tumor, phosphaturic mesenchymal<br />
tumor, inflammatory myxohyaline tumor), special<br />
adipocytic / vascular / <strong>and</strong> smooth muscle <strong>lesions</strong> (e.g. chondroid<br />
lipoma, Dabska’s tumor, ST hemangioblastoma, lipoleiomyosarcoma),<br />
epi<strong>the</strong>lioid mesenchymal malignancies <strong>of</strong> diverse lineages<br />
(e.g. epi<strong>the</strong>lioid liposarcoma, proximal-type epi<strong>the</strong>lioid sarcoma,<br />
neuroendocrine extraskeletal chondromyxoid sarcoma), ST<br />
Ewing’s tumor <strong>and</strong> peripheral nerve sheath tumors (perineuriomas<br />
<strong>and</strong> pigmented <strong>and</strong> rosetting tumors <strong>of</strong> <strong>the</strong> schwannoma/neur<strong>of</strong>ibroma<br />
group), extranodal dendritic or histiocytic proliferative<br />
processes (follicular dendritic cell sarcoma, Rosai-Dorfman disease,<br />
Castleman’s disease, <strong>and</strong> plexiform xanthomatous tumor),<br />
<strong>and</strong> tumors with myoepi<strong>the</strong>lial differentiation. The section<br />
devoted to selected <strong>pseudotumoral</strong> entities considered representatives<br />
<strong>of</strong> <strong>the</strong> hamartoma group (neural fibrolipomatous hamartoma,<br />
ectopic hamartomatous thymoma, rudimentary meningocele),<br />
metabolic diseases (amyloid tumor, nephrogenic fibrosing<br />
dermopathy, tophaceous pseudogout, pseudoinfiltrative parathyromatosis),<br />
stromal tissue reactions to trauma (fibroosseous<br />
pseudotumors <strong>of</strong> digits) <strong>and</strong> infections (bacillary angiomatosis),<br />
<strong>and</strong> normal organs (glomus coccygeum).<br />
To conclude <strong>the</strong> descriptive phase, supplementary material has<br />
now been collected <strong>and</strong> appended in an attempt to provide a<br />
quick digest <strong>of</strong> essential knowledge both for comparison <strong>and</strong><br />
differential diagnosis. The data have been tailored to syn<strong>the</strong>size<br />
diverse sources, integrating clinical elements <strong>and</strong> references to<br />
articles that previously appeared in Part I (“Introduction”), Part<br />
II (“The List <strong>and</strong> Review <strong>of</strong> New Entities”) <strong>and</strong> Parts III to XI<br />
(“Excerpta”). At <strong>the</strong> very least we hope this final part (“Appendix”)<br />
will provide <strong>the</strong> reader with a useful tabular organization<br />
<strong>of</strong> ST <strong>lesions</strong> <strong>and</strong> a reference resource.<br />
Introduction<br />
In 2003 Dr Bisceglia was commissioned by <strong>the</strong> Editors<br />
<strong>of</strong> Pathologica to produce a series <strong>of</strong> articles concerning<br />
tumoral, <strong>quasitumoral</strong> or <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue recognised in <strong>the</strong> last<br />
quarter century, including newly described entities <strong>and</strong><br />
new variants <strong>of</strong> established entities. Through a series <strong>of</strong><br />
11 articles published in <strong>the</strong> journal 1-11 , Dr Bisceglia <strong>and</strong><br />
colleagues have presented both a global overview <strong>of</strong> <strong>the</strong><br />
numerous entities which have been described in this period,<br />
with few exceptions dating from 1979, <strong>and</strong> also<br />
Corrispondenza<br />
Michele Bisceglia, M.D., Unità Operativa Anatomia Patologica,<br />
IRCCS- Ospedale “Casa Sollievo della S<strong>of</strong>ferenza”, 71013 San<br />
Giovanni Rotondo (FG), Italy - Tel. +39 0882 410366 - Fax +39<br />
0882 410411 - E-mail: bismi@libero.it
240<br />
M. BISCEGLIA ET AL.<br />
provided detailed discussion, including any novel data,<br />
<strong>of</strong> selected entities. This information was presented in a<br />
logical <strong>and</strong> algorithmic manner, both in extensive tabular<br />
<strong>and</strong> discursive formats, supported by a comprehensive<br />
but selected, <strong>and</strong> up-to-date bibliography. This allows<br />
<strong>the</strong> reader to navigate through <strong>the</strong> vast amount <strong>of</strong> information<br />
which has accrued in <strong>the</strong> area <strong>of</strong> s<strong>of</strong>t tissue<br />
pathology in <strong>the</strong> last 25 years or so. The intent, <strong>and</strong> its<br />
desired result, is that this treatise should be a valuable resource<br />
not only for pathologists who regularly encounter<br />
s<strong>of</strong>t tissue <strong>lesions</strong> in <strong>the</strong>ir practice, but more importantly<br />
for those who navigate <strong>the</strong> diagnostic s<strong>of</strong>t tissue traps on<br />
a more sporadic basis, for residents <strong>and</strong> fellows in histopathology,<br />
<strong>and</strong> clinicians dealing with s<strong>of</strong>t tissue <strong>lesions</strong>.<br />
A brief summary <strong>of</strong> <strong>the</strong> approach used in this series <strong>of</strong><br />
articles is presented here to facilitate retrospective navigation<br />
through <strong>the</strong> series.<br />
The first article (in Italian) 1 provides an introduction<br />
<strong>and</strong> raison d’être for <strong>the</strong> project, criteria for categorization<br />
<strong>and</strong> a detailed reasoning for inclusion or exclusion<br />
<strong>of</strong> various conditions. It ends with a “master table”<br />
<strong>of</strong> diagnostic categories, presented in 2 broad groupings<br />
<strong>of</strong> “<strong>Tumoral</strong> <strong>and</strong> Quasitumoral Lesions” (18 diagnostic<br />
categories) <strong>and</strong> “Pseudotumoral Lesions” (10<br />
diagnostic categories). This Table forms <strong>the</strong> backbone<br />
for <strong>the</strong> subsequent articles <strong>and</strong> excerpta which exp<strong>and</strong><br />
in detail on many, but not all <strong>lesions</strong> which are included<br />
in each diagnostic category. To compile <strong>the</strong> comprehensive<br />
catalogue <strong>of</strong> <strong>lesions</strong> considered in <strong>the</strong> subsequent<br />
articles in this series, <strong>the</strong> authors have drawn<br />
not only on an exhaustive literature review (which includes<br />
peer-reviewed articles <strong>and</strong> important discussions<br />
appearing as letters to <strong>the</strong> Editor), but also <strong>the</strong><br />
considerable personal experience <strong>of</strong> many <strong>of</strong> <strong>the</strong>m in<br />
<strong>the</strong> field <strong>of</strong> s<strong>of</strong>t tissue pathology. The authors have<br />
wherever possible listed entities according to <strong>the</strong>ir presumed<br />
or accepted histogenesis/differentiation, while a<br />
category is retained for those <strong>of</strong> uncertain histogenesis/differentiation.<br />
The rationale for certain morphological<br />
groupings is provided, for example, those defined<br />
on <strong>the</strong> basis <strong>of</strong> a distinctive extracellular matrix (e.g. fibromyxoid<br />
tumors), or cellular composition (e.g. fibrohistiocytic<br />
or fibromy<strong>of</strong>ibroblastic tumors).<br />
The second article 2 , prefaced with a preamble in Italian,<br />
presents <strong>the</strong> comprehensive list <strong>of</strong> entities (in English)<br />
which fall within each diagnostic category, accompanied<br />
by key references. The latter include important<br />
references <strong>of</strong> a general or review nature in respect<br />
<strong>of</strong> particular diagnostic categories/entities, in addition<br />
to references specific to particular entities <strong>and</strong> <strong>the</strong>ir variants.<br />
While all <strong>of</strong> <strong>the</strong> diagnostic categories <strong>of</strong> <strong>the</strong><br />
2002 WHO classification <strong>of</strong> s<strong>of</strong>t tissue tumors 12 13 are<br />
included in <strong>the</strong> master table, by necessity <strong>and</strong> design,<br />
even within <strong>the</strong> categories <strong>of</strong> tumorous <strong>lesions</strong>, <strong>the</strong>re<br />
has been a deliberate “splitting” so that in contrast to<br />
<strong>the</strong> WHO scheme, some categories appear in <strong>the</strong>ir own<br />
right as major diagnostic categories, e.g. <strong>the</strong> myoepi<strong>the</strong>lial<br />
tumors, malignant mixed mesenchymal tumors<br />
<strong>and</strong> neoplasms <strong>of</strong> perivascular epi<strong>the</strong>lioid cell<br />
origin. It is <strong>the</strong> authors’ intention that <strong>the</strong> “exploded” list<br />
<strong>of</strong> entities with <strong>the</strong>ir pertinent bibliography can provide<br />
<strong>the</strong> casual reader, as well as a pathologist dealing<br />
with a specific s<strong>of</strong>t tissue problem, an intuitive <strong>and</strong> rapid<br />
means <strong>of</strong> assessing <strong>the</strong> breadth <strong>of</strong> differential diagnostic<br />
possibilities <strong>and</strong> <strong>the</strong> state <strong>of</strong> knowledge that<br />
exists at <strong>the</strong> time <strong>of</strong> publication. Selected entities to be<br />
discussed in clinicopathologic detail <strong>and</strong> illustrated in<br />
<strong>the</strong> subsequent articles (“Excerpta”) are highlighted in<br />
<strong>the</strong> list. They were selected for detailed discussion on<br />
<strong>the</strong> basis <strong>of</strong> <strong>the</strong>ir clinical importance <strong>and</strong>/or <strong>the</strong>ir distinct<br />
morphological features.<br />
The third to eleventh articles in <strong>the</strong> series (Excerpta 1<br />
to 9) 3-11 are devoted to presenting <strong>the</strong> clinicopathologic<br />
<strong>and</strong> biologic features <strong>of</strong> specific entities (58 in all) in<br />
detail. The following Table summarizes <strong>the</strong> entities<br />
which are discussed in depth in each Excerpta.
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 241<br />
Series article #/ Ref. # Entities presented in detail Author Pathologica<br />
Excerpta # (initials) fascicle<br />
Part 3 / Excerpta 1 3 1. Dermat<strong>of</strong>ibrosacoma protuberans, classic, <strong>and</strong> pigmented sarcomatous MB GIUGNO<br />
2. Atypical fibroxanthoma, non-pleomorphic spindle-cell, <strong>and</strong> aneurysmal (pigmented) MB (June)<br />
3. Plexiform fibrohistiocytic tumor KC 2004<br />
4. Hemosiderotic fibrohistiocytic lipomatous lesion DVK<br />
5. Nuchal-type fibroma MM<br />
6. Desmoplastic fibroblastoma CF<br />
7. Solitary fibrous tumor SS<br />
8. Pleomorphic hyalinizing angiectatic tumor SS<br />
9. Sclerosing epi<strong>the</strong>lioid fibrosarcoma KC<br />
Part 4 / Excerpta 2 4 1. Dermatomy<strong>of</strong>ibroma MB OTTOBRE<br />
2. Palisaded my<strong>of</strong>ibroblastoma / intranodal hemorrhagic spindle cell tumor with SS (October)<br />
“amianthoid” fibres 2004<br />
3. My<strong>of</strong>ibrosarcoma, low grade <strong>and</strong> high grade CF<br />
4. Angiomy<strong>of</strong>ibroblastoma <strong>of</strong> vulva DVK<br />
5. Lipomatous hemangiopericytoma CF<br />
6. Inflammatory pseudotumor / inflammatory my<strong>of</strong>ibroblastic tumor MB<br />
7. Calcifying fibrous (pseudo)tumor MB<br />
8. Inflammatory myxohyaline tumor / myxoinflammatory fibroblastic sarcoma MM<br />
9. Superficial angiomyxoma <strong>and</strong> juxtarticular myxoma KC<br />
10. Ossifying fibromyxoid tumor CF<br />
11. Low grade fibromyxoid sarcoma & hyalinising spindle cell tumor with giant rosettes KC<br />
Part 5 / Excerpta 3 5 1. Phosphaturic mesenchymal tumor MB DICEMBRE<br />
2. Chondroid lipoma DVK (December)<br />
3. Dendritic fibromyxolipoma SS 2004<br />
4. Epi<strong>the</strong>lioid liposarcoma KC<br />
5. Lipoleiomyosarcoma SS<br />
6. Epi<strong>the</strong>lioid leiomyosarcoma SS<br />
7. Granular cell leiomyosarcoma SS<br />
Part 6 / Excerpta 4 6 1. Acquired elastotic hemangioma DVK FEBBRAIO<br />
2. Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> skin MB (February)<br />
3. Extraneuraxial hemangioblastoma <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> skin MM 2005<br />
4. Dabska’s tumor arising in lymphangioma MB<br />
Part 7 / Excerpta 5 7 1. Psammomatous melanotic Schwannoma KC APRILE<br />
2. Pigmented neur<strong>of</strong>ibroma MM (April)<br />
3. Dendritic cell neur<strong>of</strong>ibroma with pseudorosettes DVK 2005<br />
4. Epi<strong>the</strong>lial sheath neuroma DVK<br />
5. Perineuriomas - intraneural <strong>and</strong> extraneurial forms MB<br />
6. Ewing’s sarcoma <strong>of</strong> <strong>the</strong> skin MB<br />
Part 8 / Excerpta 6 8 1. Extraskeletal myxoid chondrosarcoma with neuroendocrine differentiation CF GIUGNO<br />
2. Proximal epi<strong>the</strong>lioid sarcoma CF (June)<br />
3. Extra-renal malignant rhabdoid tumor CF 2005<br />
4. Follicular dendritic cell sarcoma CF<br />
5. Castleman’s disease <strong>of</strong> <strong>the</strong> subcutis <strong>and</strong> skeletal muscle DVK<br />
6. Rosai-Dorfman disease <strong>of</strong> s<strong>of</strong>t tissue KC<br />
7. Plexiform xanthomatous tumor MM<br />
Part 9 / Excerpta 7 9 1. Hyaline cell-rich chondroid syringoma <strong>and</strong> myoepi<strong>the</strong>lial tumors - mixed tumor <strong>and</strong> MB OTTOBRE<br />
myoepi<strong>the</strong>lioma<br />
(October)<br />
2. Dabska’s parachordoma MM 2005<br />
3. Oncocytoma MB<br />
Part 10 / Excerpta 8 10 1. Ectopic hamartomatous thymoma DVK DICEMBRE<br />
2. Hamartoma <strong>of</strong> <strong>the</strong> scalp with ectopic meningo<strong>the</strong>liomatous elements / rudimentary DVK (December)<br />
meningocele 2005<br />
3. Neural fibrolipomatous hamartoma MB<br />
4. Ischemic fasciitis (atypical decubital fibroplasia) MM<br />
5. Nephrogenic fibrosing dermopathy DVK<br />
6. Bacillary epi<strong>the</strong>lioid angiomatosis KC<br />
Part 11 / Excerpta 9 11 1. Fibro-osseous pseudotumor <strong>of</strong> <strong>the</strong> digits <strong>and</strong> bizarre parosteal osteochondromatous MB GIUGNO<br />
proliferation (Nora’s lesion)<br />
(June)<br />
2. Tophaceous pseudogout (calcium pyrophosphate dihydrate crystals deposition MB 2006<br />
disease – tumoral form)<br />
3. Amyloid tumor <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> breast MB<br />
4. Glomus coccygeum MB<br />
5. Post-implant parathyromatosis MB
242<br />
M. BISCEGLIA ET AL.<br />
In this final APPENDIX (Part XII) to <strong>the</strong> series, 30<br />
“problem-oriented” Tables (with bibliography) are<br />
provided to aid <strong>the</strong> decision making process in everyday<br />
diagnostic practice in s<strong>of</strong>t tissue pathology. These<br />
Tables provide a comprehensive, though admittedly<br />
not exhaustive grouping <strong>of</strong> <strong>lesions</strong> according to<br />
important clues based on cytoarchitectural pattern recognition,<br />
<strong>and</strong> also in consideration <strong>of</strong> particular clinical<br />
circumstances. The Tables should serve not<br />
only as an aide-de-memoir but also as a diagnostic<br />
“check-list” when confronted with a particular diagnostic<br />
problem. To provide maximum benefit from<br />
this problem-oriented tabular approach, we thought<br />
that it would be useful to broaden <strong>the</strong> scope <strong>of</strong> <strong>the</strong> tables<br />
beyond those <strong>lesions</strong> affecting superficial <strong>and</strong><br />
somatic s<strong>of</strong>t tissues, as was our original intent in <strong>the</strong><br />
series, to also include <strong>lesions</strong> affecting o<strong>the</strong>r anatomic<br />
parts/organs, e.g. <strong>the</strong> body cavities. However, genuine<br />
s<strong>of</strong>t tissue visceral organ-based <strong>lesions</strong> have<br />
been excluded from <strong>the</strong> analysis. Updated references<br />
for various entities considered in <strong>the</strong> preceding Excerpta<br />
are provided, in addition to important reviews<br />
<strong>and</strong> references <strong>of</strong> a more generic nature. References<br />
to <strong>the</strong> new entities which had been already quoted in<br />
<strong>the</strong> General List <strong>of</strong> entities (Part II) or were detailed<br />
in <strong>the</strong> Excerpta – with very few exceptions limited to<br />
Table 30 – do not appear in this Appendix, to avoid<br />
repetition. Entities which have been previously described<br />
or referenced are indicated by means <strong>of</strong> various<br />
typographical options.<br />
The Key to navigating <strong>the</strong> Tables is as follows.<br />
• Bolded entities appeared in Excerpta <strong>and</strong> are listed<br />
alphabetically in <strong>the</strong> Index at <strong>the</strong> end <strong>of</strong> this Appendix,<br />
accompanied by key references that have appeared<br />
since <strong>the</strong> publication <strong>of</strong> <strong>the</strong> excerpta.<br />
• Italicized entities were listed in Part II <strong>of</strong> <strong>the</strong> Series<br />
2<br />
with <strong>the</strong>ir annotated bibliography.<br />
• Referenced entities in <strong>the</strong> Tables correspond to recent<br />
articles that appeared after Part II <strong>of</strong> our series<br />
was published 2 , or were not included in <strong>the</strong> previous<br />
List, or are considered to be key <strong>and</strong>/or review<br />
articles.<br />
To keep abreast <strong>of</strong> <strong>the</strong> burgeoning growth in knowledge<br />
<strong>of</strong> s<strong>of</strong>t tissue tumefactive conditions can be<br />
overwhelming, <strong>and</strong> to mine <strong>the</strong> breadth <strong>and</strong> depth <strong>of</strong><br />
<strong>the</strong> data base excerpted from <strong>the</strong> eleven preceding publications<br />
requires an agility that can only be met by<br />
<strong>the</strong> power <strong>of</strong> online search engines. Since <strong>the</strong> publication<br />
<strong>of</strong> <strong>the</strong> series in Pathologica, outst<strong>and</strong>ing contributions<br />
have appeared in <strong>the</strong> world literature 14 15 . In this<br />
Appendix we broaden our previous list <strong>of</strong> entities <strong>and</strong><br />
update <strong>the</strong> bibliography. To complement <strong>the</strong> traditional<br />
morphologic approach used throughout <strong>the</strong> series, <strong>the</strong><br />
reader is referred to <strong>the</strong> January 2006 issue <strong>of</strong> Histopathology,<br />
which is devoted to s<strong>of</strong>t tissue tumors <strong>and</strong><br />
which highlights <strong>the</strong> increasing role <strong>of</strong> new diagnostic<br />
modalities, such as genetic analysis <strong>and</strong> microarray technology<br />
16-18 , in addition to <strong>the</strong> traditional contributions<br />
<strong>of</strong> immunohistochemical <strong>and</strong> ultrastructural examination<br />
19 . Continued refinement in nosology is possible<br />
through advances in <strong>the</strong> expertise <strong>of</strong> <strong>the</strong> investigator<br />
<strong>and</strong> <strong>the</strong> diagnostic tools being applied. Histological<br />
classifications <strong>and</strong> subclassifications that are practically<br />
achieved, reproducible <strong>and</strong> uniquely predictive,<br />
ei<strong>the</strong>r alone or in conjunction with o<strong>the</strong>r patient’s characteristics,<br />
are valuable in <strong>the</strong> design <strong>and</strong> evaluation <strong>of</strong><br />
<strong>the</strong>rapeutic regimens. It is our hope that <strong>the</strong> series with<br />
its comprehensive Appendix will provide <strong>the</strong> reader<br />
with a rapid reference base, maximum availability, <strong>and</strong><br />
practical usefulness.
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 243<br />
“Problem-oriented” tables<br />
With <strong>the</strong> intent to allow one, at a glance, to be pointed in <strong>the</strong> right direction, <strong>and</strong> hopefully provoke a highly satisfying<br />
“Eureka” moment!!<br />
1. Richly collagenized <strong>lesions</strong><br />
A. Tumor-like <strong>lesions</strong><br />
B. <strong>Tumoral</strong> <strong>lesions</strong><br />
2. Myxoid <strong>lesions</strong><br />
A. Myxomatous <strong>lesions</strong><br />
B. Occasionally myxomatous <strong>lesions</strong>, or with myxomatous change<br />
3. Tumors <strong>and</strong> pseudotumors with calcifications, or with chondro-osseous metaplasia<br />
A. Dystrophic <strong>and</strong> psammomatous calcifications<br />
B. Chondroid <strong>and</strong> osseous metaplasia<br />
4. Tumors <strong>and</strong> pseudotumors with inflammatory cell component<br />
A. Lymphoid infiltrate<br />
B. Xanthomatous infiltrate<br />
5. Atypical / bizarre / multinucleated / pleomorphic giant cell-containing tumors <strong>and</strong> pseudotumors<br />
A. Atypical / bizarre / monster cells in benign <strong>lesions</strong><br />
B. Reactive multinucleated, osteoclast-like giant cells in benign tumors <strong>and</strong> pseudotumors<br />
C. Osteoclast-like giant cells in borderline <strong>and</strong> malignant tumors<br />
D. Multinucleated giant cells (intrinsic) in benign tumors<br />
E. Neoplastic giant cells (intrinsic or accompanying) in borderline <strong>and</strong> malignant tumors<br />
F. “Malignant fibrous histiocytoma”-like pattern<br />
6. Tumors <strong>and</strong> pseudotumors with a distinctive architecture / growth pattern<br />
A. Fascicular pattern<br />
B. Storiform pattern<br />
C. Whorled pattern<br />
D. Palisading pattern<br />
E. Amianthoid structures <strong>and</strong> (pseudo-)rosettes<br />
F. Cording / chordoid pattern<br />
G. Endocrinoid pattern<br />
H. Alveolar pattern<br />
I. Pseudogl<strong>and</strong>ular pattern<br />
J. Pseudovascular pattern<br />
K. Retiform pattern<br />
L. Papillary pattern<br />
7. Distinctive vascular patterned <strong>lesions</strong> (non-endo<strong>the</strong>lial)<br />
A. Hemangiopericytoma-like pattern as a constant feature<br />
B. Hemangiopericytoma-like pattern as an occasional feature<br />
C. Perivascular hyalinization prominent<br />
D. Plexiform capillary pattern<br />
E. Glomeruloid capillary pattern<br />
F. Hemorrhagic changes / pattern<br />
G. Aneurysmal changes / pattern<br />
8. Combined, polyphasic, <strong>and</strong> heterologous tumors (o<strong>the</strong>r than collision tumors)<br />
A. Combined (homologous <strong>and</strong> heterologous) tumors<br />
B. Biphasic homologous (bimorphic) tumors<br />
C. Biphasic heterologous tumors – with epi<strong>the</strong>lial elements<br />
D. Pseudo-biphasic tumors<br />
E. Biphasic tumors with skeletal muscle differentiation<br />
9. Histogenetically diverse but morphologically similar tumors <strong>and</strong> pseudotumors with ….<br />
A. Round-cell / epi<strong>the</strong>lioid / plasmacytoid features<br />
B. Clear cell changes<br />
C. (Uni-/multi-)vacuolated cells, (pseudo-)lipoblasts, <strong>and</strong> (pseudo-)physalipherous cells<br />
D. Eosinophilic / oncocytic features<br />
E. Granular cells<br />
F. Rhabdoid / pseudo-rhabdoid features (extra-renal)<br />
G. Ganglion / ganglion-like cells<br />
H. Small round cells<br />
I. Pleomorphic cells
244<br />
M. BISCEGLIA ET AL.<br />
10. Tumors <strong>and</strong> pseudotumors with diagnostic clues<br />
A. Architecturally distinct features<br />
B. Stromal peculiarities<br />
C. Cyto-histologically distinct features<br />
11. Histologically pigmented tumors <strong>and</strong> pseudotumors with ….<br />
A. Melanin<br />
B. Hemosiderin<br />
C. Carbon<br />
12. Clinically alarming benign tumors <strong>and</strong> pseudotumors<br />
A. Multiple, multicentric, recurring benign <strong>lesions</strong><br />
B. Painful s<strong>of</strong>t tissue tumors <strong>and</strong> pseudotumors<br />
13. Pathologically alarming benign tumors <strong>and</strong> pseudotumors<br />
A. Multilobular / mosaic growth pattern<br />
B. Plexiform, infiltrating margins<br />
C. Intravascular growth<br />
D. Hypercellular benign <strong>lesions</strong><br />
14. Histologically benign <strong>lesions</strong> mistaken for malignant<br />
A. Tumor-like <strong>lesions</strong><br />
B. <strong>Tumoral</strong> <strong>lesions</strong><br />
15. Reactive endo<strong>the</strong>lial <strong>lesions</strong> that may histologically mimic malignancy<br />
16. Histologically malignant tumors mistaken for benign <strong>lesions</strong><br />
17. Atypical variants <strong>of</strong> typical tumors<br />
A. Clinically atypical<br />
B. Behaviourally atypical<br />
C. Macroscopically atypical<br />
D. Morphologically atypical (histologic/cytologic)<br />
18. Cystic tumors <strong>and</strong> pseudotumors<br />
A. Primarily cystic<br />
B. Secondarily cystic or with microcystic change<br />
C. With pseudocystic pattern<br />
19. Acral tumors <strong>and</strong> pseudotumors<br />
20. Orbital tumors <strong>and</strong> pseudotumors<br />
21. Paratesticular tumors <strong>and</strong> pseudotumors<br />
A. Benign tumors <strong>and</strong> pseudotumors<br />
B. Malignant tumors<br />
22. Vulvo-vaginal tumors <strong>and</strong> pseudotumors<br />
23. Aerodigestive tract <strong>lesions</strong> (involving <strong>the</strong> orifices)<br />
A. Nasal cavity<br />
B. Oral cavity<br />
C. Anal canal<br />
24. Intranodal primary tumors <strong>and</strong> pseudotumors (o<strong>the</strong>r than hematolymphoid)<br />
25. Mammary stromal spindle cell tumors <strong>and</strong> tumor-like <strong>lesions</strong> <strong>and</strong> mimics<br />
A. Monomorphic spindle cell tumors <strong>of</strong> specialized mammary stroma<br />
B. Monomorphic spindle cell tumors <strong>of</strong> non-specialized mammary stroma<br />
C. Spindle cell myoepi<strong>the</strong>lioma<br />
D. Spindle cell epi<strong>the</strong>lial tumors<br />
26. Infantile-juvenile tumoral <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong><br />
A. Hamartomas – Developmental <strong>lesions</strong><br />
B. Benign tumors <strong>and</strong> pseudotumors<br />
C. Intermediate <strong>and</strong> malignant tumors<br />
27. Lesions as sentinel <strong>of</strong> clinical entities<br />
28. Lesions as sentinel <strong>of</strong> clinical syndromes<br />
29. Embryological rests or normal anatomic structures potentially mistaken for tumors<br />
30. Grade-based categorization <strong>of</strong> s<strong>of</strong>t tissue tumors (<strong>of</strong> relevance to management)
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 245<br />
Table I. Richly collagenized <strong>lesions</strong> 20 .<br />
A. Tumor-like <strong>lesions</strong><br />
• Fibrous papule <strong>of</strong> <strong>the</strong> face (nose) (classic type <strong>and</strong> variants) 21<br />
• Multiple perifollicular fibroma <strong>of</strong> <strong>the</strong> face <strong>and</strong> neck<br />
• Angi<strong>of</strong>ibromas (associated <strong>and</strong> unassociated with tuberous sclerosis complex)<br />
• Collagenoma (connective tissue nevus)<br />
• Rudimentary supernumerary digit<br />
• Acquired digital fibrokeratoma<br />
• Sclerotic fibroma (circumscribed storiform collagenoma)<br />
• Reactive fibrosis<br />
• Hypertrophic scar & keloid<br />
• Knuckle pads<br />
• Diabetic scleredema (upper back)<br />
• Elast<strong>of</strong>ibroma<br />
• Infantile digital fibromatosis<br />
• Gingival fibromatosis<br />
• Juvenile hyaline fibromatosis 22<br />
• Fibrous proliferations in Proteus syndrome<br />
• Intra-articular nodular fasciitis 23<br />
• Calcifying fibrous pseudotumor<br />
• Idiopathic retroperitoneal fibrosis (Ormond’s disease)<br />
24, 25<br />
• Reactive nodular fibrous pseudotumors (<strong>of</strong> <strong>the</strong> gastrointestinal tract <strong>and</strong> mesentery)<br />
• Sclerosing mediastinitis 25a<br />
• Sclerosing extramedullary hematopoietic tumor<br />
B. <strong>Tumoral</strong> <strong>lesions</strong><br />
• Nasopharyngeal angi<strong>of</strong>ibroma<br />
• Sclerosing/desmoplastic melanocytic nevi (ordinary acquired melanocytic nevus, Spitz nevus, blue nevus)<br />
• Dermat<strong>of</strong>ibroma variant (keloidal, sclerotic)<br />
• Pleomorphic fibroma<br />
• Nuchal-type fibroma (<strong>of</strong> nuchal <strong>and</strong> extra-nuchal sites)<br />
• Gardner-associated fibroma<br />
• Fibroma <strong>of</strong> tendon sheath<br />
• Giant cell fibroblastoma<br />
• Sclerotic lipoma<br />
• Fibrous spindle cell lipoma<br />
• Sclerosing neur<strong>of</strong>ibroma<br />
• Desmoplastic cutaneous ganglioneuroma<br />
• Atypical fibroxanthoma with prominent sclerosis<br />
• Tenosynovial giant cell tumor – sclerotic variant<br />
• Desmoplastic fibroblastoma (collagenous fibroma)<br />
• Sclerosing perineurioma<br />
• Superficial (fascial) fibromatosis (palmar / plantar / penile types)<br />
• Deep (musculoaponeurotic) fibromatosis (desmoid tumors: extraabdominal / abdominal / intraabdominal types)<br />
• Paratesticular fibroma<br />
• Solitary fibrous tumor 26<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
• Sclerosing epi<strong>the</strong>lioid fibrosarcoma<br />
• Sclerosing primary cutaneous leiomyosarcoma<br />
• “Fibroma-like” epi<strong>the</strong>lioid sarcoma (- desmoplastic variant) 26a<br />
• Sclerosing rhabdomyosarcoma<br />
• Sclerosing paraganglioma 27<br />
• Monophasic synovial sarcoma<br />
• Leiomyomatosis peritonealis disseminata (end-stage)<br />
• Desmoplastic diffuse meso<strong>the</strong>lioma<br />
• Desmoplastic small round cell tumor<br />
• Desmoplastic melanoma 27a<br />
• Lymphoma (occasional)
246<br />
M. BISCEGLIA ET AL.<br />
Table II. Myxoid <strong>lesions</strong> 28 28a .<br />
A. Myxomatous <strong>lesions</strong><br />
• Focal mucinosis (cutaneous <strong>and</strong> subcutaneous) 29<br />
• Polyvynilpyrrolidone granuloma (rare: may occur in <strong>the</strong> skin/subcutis/s<strong>of</strong>t tissue/bone)<br />
• Superficial angiomyxoma (cutaneous <strong>and</strong> subcutaneous myxoma) & juxta-articular myxoma<br />
• Neuro<strong>the</strong>keoma, classic or myxoid type<br />
• Nerve sheath myxoma (“perineurial myxoma” <strong>of</strong> Harkin <strong>and</strong> Reed – “plexiform myxoma”)<br />
• Myxolipoma (myxoid lipoma)<br />
• Angiomyxolipoma<br />
• Dendritic fibromyxolipoma / Myxoid spindle cell lipoma<br />
• Intramuscular myxoma<br />
• Myxopapillary ependymoma<br />
• Superficial acral fibromyxoma<br />
• Aggressive angiomyxoma<br />
• Ossifying fibromyxoid tumor<br />
• Low-grade fibromyxoid sarcoma (Evans’ tumor)<br />
• Superficial low-grade fibromyxoid sarcoma (Evans’ tumor) 30<br />
• Primitive myxoid mesenchymal tumor <strong>of</strong> infancy 31<br />
• Myx<strong>of</strong>ibrosarcoma (low grade myxoid malignant fibrous histiocytoma) 32<br />
• Extraskeletal myxoid chondrosarcoma (chordoid sarcoma)<br />
• Extraskeletal myxoid chondrosarcoma with neuroendocrine differentiation<br />
• Myxoid liposarcoma<br />
• Primary heterotopic chordoma 28 28b , chordoma periphericum 32a<br />
32b 32c<br />
• Parachordoma<br />
• Mixed tumors <strong>of</strong> salivary gl<strong>and</strong>s (recurrence in s<strong>of</strong>t tissue)<br />
• Metastatic myxoid sarcomas to s<strong>of</strong>t tissue <strong>and</strong> skin 33<br />
• Metastatic chordoma<br />
• Metastatic colloid carcinoma<br />
• Pseudomyxoma peritonei<br />
B. Lesions occasionally myxomatous or with myxomatous change<br />
• Trichodiscoma (fibr<strong>of</strong>olliculoma)<br />
• Keloid<br />
• Nodular fasciitis<br />
• Infantile fibromatosis<br />
• Subungual pleomorphic fibroma – myxoid variant<br />
• Proliferative funiculitis<br />
• Fibrous umbilical polyp<br />
• Cutaneous myxoid fibroblastoma<br />
• Giant cell fibroblastoma<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans – myxoid variant<br />
• Myoepi<strong>the</strong>lioma<br />
• Lipoblastoma<br />
• Leiomyoma<br />
• Schwannoma – myxoid variant<br />
• Neur<strong>of</strong>ibroma – myxoid variant<br />
• Dendrocytoma –myxoid variant<br />
• Chondroma – myxoid variant<br />
• Fetal-type rhabdomyoma<br />
• Spindle cell lipoma (occasional)<br />
• Perineurioma – myxoid variant<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans – myxoid variant<br />
• Solitary fibrous tumor – myxoid variant<br />
• Leiomyosarcoma – myxoid variant<br />
• Malignant peripheral nerve sheath tumor<br />
• Rhabdomyosarcoma (mainly botryoid embryonal type)<br />
• Inflammatory acral myxo-hyaline fibroblastic sarcoma<br />
• (Extra-)gastrointestinal stromal tumor 33a<br />
• Fibrous synovial sarcoma<br />
• Clear cell sarcoma – myxoid variant 34<br />
• Lymphoma (occasional)<br />
• Melanoma (primary, <strong>and</strong> metastatic) – myxomatous 35 36 [<strong>and</strong> pseudomyxomatous 36a ] variants
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 247<br />
Table III. Tumors <strong>and</strong> pseudo-tumors with calcifications, or with chondro-osseous<br />
metaplasia.<br />
A. Tumors <strong>and</strong> pseudo-tumors with dystrophic <strong>and</strong> psammomatous calcifications<br />
• Hemangiomas (phleboliths mainly in cavernous <strong>and</strong> spindle cell hemangioma)<br />
• Cutaneous meningioma<br />
• Amyloid tumor (even bone)<br />
• Tophaceous gout (even bone)<br />
• Tophaceous pseudogout (tumoral crystal calcium pyrophosphate dihydrate deposition disease)<br />
• Malakoplakia<br />
• Fat necrosis<br />
• Calcinosis – several types<br />
• Calcifying aponeurotic fibroma<br />
• My<strong>of</strong>ibroma/my<strong>of</strong>ibromatosis<br />
• Calcifying fibrous pseudotumors<br />
• Leiomyoma<br />
• Neuro<strong>the</strong>keoma<br />
• Ancient schwannoma<br />
• Phosphaturic mesenchymal tumor (mixed connective tissue variant)<br />
• Hyalinizing spindle cell tumor with giant rosettes<br />
• Ganglioneuroma<br />
• Psammomatous melanotic schwannoma<br />
• Psammomatous malignant melanoma 37<br />
• Epi<strong>the</strong>lioid sarcoma<br />
• Meso<strong>the</strong>lioma<br />
• Synovial sarcoma<br />
• Differentiating neuroblastoma<br />
• Alveolar s<strong>of</strong>t part sarcoma with psammomatous bodies, <strong>and</strong> calcifications 37a (occasional)<br />
• Any sarcoma with preceding necrosis (may undergo dystrophic calcification)<br />
• Extragonadal (retroperitoneal) burnt-out germ cell tumors<br />
B. S<strong>of</strong>t tissue tumors <strong>and</strong> pseudotumors with chondroid & osseous metaplasia 38<br />
• (Pilomatrixoma)<br />
• Ectopic ossification <strong>of</strong> <strong>the</strong> auricle secondary to frostbite<br />
• Nuchal fibrocartilaginous pseudotumor<br />
• Heterotopic chondro-ossification<br />
• (Chondro-)mesenchymal hamartoma <strong>of</strong> <strong>the</strong> nose 39<br />
• Mesenchymal hamartoma <strong>of</strong> <strong>the</strong> chest wall 40<br />
• Fibrochondroid hamartoma<br />
• Rhabdomyomatous mesenchymal hamartoma <strong>of</strong> <strong>the</strong> skin (occasional)<br />
• Hyperplastic callus in pathologic conditions (e.g. osteogenesis imperfecta, …)<br />
• Tumefactive s<strong>of</strong>t tissue extension <strong>of</strong> Paget’s pseudosarcoma<br />
• Cavernous hemangioma with ossification (occasional)<br />
• Dermat<strong>of</strong>ibroma (ossifying variant)<br />
• Benign fibrous histiocytoma <strong>of</strong> subcutaneous <strong>and</strong> deep s<strong>of</strong>t tissue (occasional)<br />
• Fibromatosis (mainly palmar type)<br />
• Juvenile xanthogranuloma (1 case with ossification)<br />
• My<strong>of</strong>ibromatosis<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma with ossification<br />
• Cutaneous chondroma (solitary form, multiple / familial form)<br />
• Cutaneous osteoma<br />
• Chondro-osteo-lipoma / benign mesenchymoma<br />
• Hyaline cell-rich chondroid syringoma<br />
• Chondroid lipoma<br />
• S<strong>of</strong>t tissue chondroma & periosteal chondroma<br />
• Extra-articular synovial chondromatosis 40a<br />
• Nodular fasciitis, mainly parosteal variant (fasciitis ossificans)<br />
• Myositis & panniculitis ossificans<br />
• Heterotopic mesenteric ossification 41<br />
• Subungual (Dupuytren's) exostosis / turret exostosis (acquired osteochondroma) <strong>of</strong> <strong>the</strong> h<strong>and</strong>s <strong>and</strong> feet<br />
• Fibroosseous pseudotumor <strong>of</strong> <strong>the</strong> digits (florid reactive periostitis <strong>of</strong> <strong>the</strong> tubular bones <strong>of</strong> <strong>the</strong> h<strong>and</strong>s <strong>and</strong><br />
feet)
248<br />
M. BISCEGLIA ET AL.<br />
• Florid reactive periostitis <strong>of</strong> <strong>the</strong> long bones (e.g. tibia 41a )<br />
• Bizarre parosteal osteochondromatous proliferation <strong>of</strong> <strong>the</strong> h<strong>and</strong>s <strong>and</strong> feet (Nora's lesion)<br />
• Bizarre parosteal osteochondromatous proliferation <strong>of</strong> <strong>the</strong> long bones (Nora's lesion)<br />
• Fibrodysplasia ossificans progressiva<br />
• Ossified meningioma<br />
• Ossifying fibromyxoid tumor<br />
• Atypical fibroxanthoma with osteoid production<br />
• Atypical fibroxanthoma with chondroid differentiation<br />
• Mixed tumor <strong>of</strong> <strong>the</strong> skin <strong>and</strong> s<strong>of</strong>t tissue<br />
• Giant cell tumor <strong>of</strong> tendon sheath & giant cell tumor <strong>of</strong> s<strong>of</strong>t tissue<br />
• Phosphaturic mesenchymal tumor (mixed connective tissue variant)<br />
• Hemangiopericytoma<br />
• Schwannoma with bone or cartilage<br />
• Malignant peripheral nerve sheath tumor<br />
• Malignant fibrous histiocytoma<br />
• Epi<strong>the</strong>lioid sarcoma (with chondroid <strong>and</strong> osseous metaplasia)<br />
• Myxoid liposarcoma<br />
• Embryonal rhabdomyosarcoma<br />
• Extraskeletal myxoid chondrosarcoma (chordoid sarcoma)<br />
• Synovial sarcoma<br />
• Extraskeletal s<strong>of</strong>t tissue & synovial chondrosarcoma<br />
• S<strong>of</strong>t tissue mesenchymal chondrosarcoma<br />
• Periosteal chondrosarcoma<br />
• Parosteal, periosteal, high-grade surface osteosarcoma<br />
• S<strong>of</strong>t tissue extraskeletal osteosarcoma<br />
• Primary cutaneous osteosarcoma<br />
• Primary osteogenic sarcoma <strong>of</strong> <strong>the</strong> penis<br />
• Primary osteogenic sarcoma <strong>of</strong> <strong>the</strong> breast<br />
• Malignant mesenchymoma<br />
• Meso<strong>the</strong>lioma (occasional)<br />
• Extraskeletal PNET (with massive osteocartilaginous differentiation)<br />
• Melanoma (osteogenic melanoma) 42<br />
• Metastatic metaplastic breast carcinoma, malignant mixed mullerian tumor, skeletal <strong>and</strong> extraskeletal osteogenic<br />
sarcoma
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 249<br />
Table IV. Tumors <strong>and</strong> pseudotumors with inflammatory cell component.<br />
A. Tumors <strong>and</strong> pseudotumors with lymphoid infiltrate<br />
• Inflammatory fibrous papule <strong>of</strong> <strong>the</strong> face 21<br />
• Lymphangioma<br />
• Amyloid tumor<br />
• Atypical mycobacterial spindle cell pseudotumor<br />
• Pseudoneoplastic (histoid) leprosy<br />
• Malakoplakia<br />
• Bacillary angiomatosis<br />
• Angiolymphoid hyperplasia with eosinophilia<br />
• Kimura’s disease<br />
• Lymphangioma-like Kaposi’s sarcoma<br />
• “Lymphocyte-rich hobnail hemangioendo<strong>the</strong>lioma” (including retiform hemangioendo<strong>the</strong>lioma<br />
<strong>and</strong> Dabska’s tumor)<br />
• Rosai-Dorfman disease, extranodal<br />
24 25<br />
• Reactive nodular fibrous pseudotumors (<strong>of</strong> <strong>the</strong> gastrointestinal tract <strong>and</strong> mesentery)<br />
• Sclerosing mesenteritis, mesenteric panniculitis, mesenteric lipodystrophy, <strong>and</strong> o<strong>the</strong>r inflammatory<br />
43 44<br />
pseudotumors<br />
• Sclerosing retroperitonitis (Ormond’s disease)<br />
• Sclerosing mediastinitis (idiopathic fibroinflammatory <strong>lesions</strong> <strong>of</strong> <strong>the</strong> mediastinum) 25a<br />
• Inflammatory pseudotumor (inflammatory my<strong>of</strong>ibroblastic tumor)<br />
• “Inflammatory fibrosarcoma”<br />
• Inflammatory liposarcoma (lymphocyte-rich well differentiated liposarcoma)<br />
• Inflammatory leiomyosarcoma<br />
• Inflammatory malignant fibrous histiocytoma / undifferentiated pleomorphic sarcoma with prominent<br />
inflammation<br />
• Malignant fibrous histiocytoma – pseudolymphomatous variant<br />
• Angiomatoid fibrous histiocytoma<br />
• Acral inflammatory myxohyaline tumor (myxoinflammatory fibroblastic sarcoma)<br />
• Dedifferentiated liposarcoma – pseudolymphomatous variant 45<br />
• Diffuse-type giant cell tumor<br />
• Meso<strong>the</strong>lioma (lymphohistiocytoid variant)<br />
• Follicular dendritic cell sarcoma<br />
B. Tumors <strong>and</strong> tumor-like <strong>lesions</strong> with xanthomatous infiltrate<br />
• Xanthomatous leprosy<br />
• Atypical mycobacteriosis<br />
• Nodular panniculitis<br />
• Nodular-cystic encapsulated fat necrosis (“encapsulated mobile lipoma”)<br />
• Paraffinoma / oleogranuloma (o<strong>the</strong>r than lung paraffinoma <strong>and</strong> coeliac lipogranulomatous lymphadenitis)<br />
• Lipoma with fat necrosis<br />
• Juvenile xanthogranuloma<br />
• Necrobiotic xanthogranuloma<br />
• Xanthomatous / cholesterolotic benign fibrous histiocytoma<br />
• Xanthoma (tuberous type)<br />
• Plexiform xanthomatous tumor<br />
• Xanthogranulomatous inflammation NOS (<strong>of</strong> any site, including abdomen <strong>and</strong> pelvis)<br />
• Pelvic xanthogranulomatous inflammation <strong>of</strong> infective etiology – overt (e.g. actinomyces) or occult 46<br />
47 48<br />
• Tamm-Horsfall protein deposition (early phases)<br />
• Erdheim-Chester disease with xanthogranulomatous inflammation<br />
• Erdheim-Chester <strong>of</strong> <strong>the</strong> breast 49<br />
• Tenosynovial giant cell tumor both localized <strong>and</strong> diffuse-type<br />
• Schwannoma<br />
• Malignant fibrous histiocytoma – inflammatory type
250<br />
M. BISCEGLIA ET AL.<br />
Table V. Atypical / bizarre / multinucleated / pleomorphic giant cell-containing<br />
tumors <strong>and</strong> pseudotumors.<br />
A. Benign tumors with atypical / bizarre / monster cells<br />
• Pleomorphic fibroma <strong>of</strong> <strong>the</strong> skin<br />
• Subungual pleomorphic fibroma<br />
• Pleomorphic fibroma <strong>of</strong> tendon sheath<br />
• Pleomorphic lipoma<br />
• Pleomorphic leiomyoma<br />
• Atypical decubital fibroplasia <strong>of</strong> debilitated people (ischemic fasciitis)<br />
• Orbital & extraorbital giant cell angi<strong>of</strong>ibro(blast)oma<br />
• Pseudosarcomatous benign fibrous histiocytoma<br />
• Atypical lipoma<br />
• Ancient schwannoma<br />
• Paraganglioma<br />
• Neur<strong>of</strong>ibroma with nuclear atypia<br />
• Symplastic glomus tumor<br />
• Symplastic leiomyoma<br />
• Bizarre angioleiomyoma<br />
• Atrophic striated muscle cells in several conditions<br />
• Regenerating skeletal muscle<br />
• Pseudosarcomatous polyp<br />
• Cellular pseudosarcomatous fibroepi<strong>the</strong>lial stromal polyp <strong>of</strong> <strong>the</strong> lower female genital tract 50<br />
B. Benign tumors <strong>and</strong> pseudotumors with reactive multinucleated, osteoclast-like giant cells<br />
• Suture granulomata<br />
• Textilomas 51 <strong>and</strong> teflonomas 52<br />
• Paraffinoma / oleogranuloma / silicone granuloma<br />
• Amyloid tumor<br />
• Fat necrosis<br />
• <strong>Tumoral</strong> calcinosis<br />
• Tophaceous gout<br />
• Tophaceous pseudogout (nodular deposition <strong>of</strong> calcium pyrophosphate dihydrate crystals)<br />
• Dermat<strong>of</strong>ibroma with osteoclast-like giant cells<br />
• Benign fibrous histiocytoma <strong>of</strong> subcutaneous <strong>and</strong> deep s<strong>of</strong>t tissue<br />
• Fibroma <strong>of</strong> tendon sheath (variant)<br />
• My<strong>of</strong>ibroma / my<strong>of</strong>ibromatosis (rare)<br />
• Fibromatosis (plantar type)<br />
• Giant cell collagenoma<br />
• S<strong>of</strong>t tissue aneurysmal bone cyst<br />
• Giant cell tumor <strong>of</strong> tendon sheath (localized-type) 53<br />
• Chondroma (calcified variant)<br />
• Giant cell tumor <strong>of</strong> <strong>the</strong> skin<br />
• Giant cell tumor <strong>of</strong> s<strong>of</strong>t tissue<br />
• Giant cell tumor <strong>of</strong> mammary stroma<br />
• Calcifying aponeurotic fibroma<br />
• Florid reactive periostitis (fibroosseous pseudotumor <strong>of</strong> <strong>the</strong> digits)<br />
• Extraskeletal chondroma<br />
• Aggressive angiomyxoma (occasional)<br />
C. Borderline & malignant tumors with osteoclast-like giant cells<br />
• Atypical fibroxanthoma with osteoclast-like giant cells<br />
• Plexiform fibrohistiocytic tumor<br />
• Posphaturic mesenchymal tumor (mixed connective tissue variant)<br />
• S<strong>of</strong>t tissue giant cell tumor<br />
• Giant cell tumor <strong>of</strong> tendon sheath (diffuse type)<br />
• Leiomyosarcoma with osteoclastic-like giant cells<br />
• Malignant peripheral nerve sheath tumor with osteoclast-like giant cells<br />
• Extraskeletal osteoclastic(giant cel- rich) osteosarcoma<br />
• Osteoclastic giant cell malignant fibrous histiocytoma<br />
• Undifferentiated pleomorphic sarcoma with osteoclastic giant cells
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 251<br />
• Osteoclastic-rich tumor <strong>of</strong> <strong>the</strong> gastrointestinal tract with features resembling clear cell sarcoma <strong>of</strong> s<strong>of</strong>t parts 53a<br />
• Malignant mesenchymoma with prominent osteoclastic giant cells<br />
• Metastatic osteoclastoma-like or giant cell-rich carcinoma<br />
D. Benign tumors with intrinsic multinucleated giant cells<br />
• Juvenile xanthogranuloma (Touton cells)<br />
• Multinucleated giant cells angiohistiocytoma <strong>of</strong> <strong>the</strong> skin<br />
• Kimura’s disease (polykaryocytes)<br />
• Langerhans’ cell histiocytosis<br />
• Myelolipoma (megakaryocytes)<br />
• Sclerosing extramedullary hematopoietic tumor (megakaryocytes)<br />
• Orbital <strong>and</strong> extra-orbital giant cell angi<strong>of</strong>ibroma (relevant to solitary fibrous tumor group)<br />
• Giant cell fibroblastoma<br />
• Giant cell angioblastoma <strong>of</strong> Nakagawa<br />
E. Borderline <strong>and</strong> malignant tumors with ei<strong>the</strong>r intrinsic or accompanying neoplastic giant cells<br />
• Plexiform fibrohistiocytic tumor<br />
• Pleomorphic hyalinizing angiectatic tumor<br />
• Inflammatory myxohyaline tumor (inflammatory fibroblastic sarcoma)<br />
• Giant cell angi<strong>of</strong>ibroma (<strong>of</strong> orbital <strong>and</strong> extra-orbital sites)<br />
• Malignant fibrous histiocytoma – storiform-pleomorphic type<br />
• Malignant fibrous histiocytoma – giant cell type<br />
• Myxoid malignant fibrous histiocytoma (gr. II)<br />
• Clear cell sarcoma<br />
• Alveolar rhabdmoyosarcoma with pleomorphic giant cells<br />
• Angiomatoid fibrous histiocytoma with pleomorphic giant cells<br />
• Aggressive angiomyxoma<br />
• Alveolar s<strong>of</strong>t part sarcoma<br />
• S<strong>of</strong>t tissue osteosarcoma<br />
• Malignant mesenchymoma<br />
• Melanoma (o<strong>the</strong>r than pleomorphic) 54<br />
• Epi<strong>the</strong>lioid atypical angiomyolipoma<br />
• Any pleomorphic sarcoma (pleomorphic leiomyosarcoma, pleomorphic rhabdomyosarcoma,<br />
plemorphic liposarcoma, undifferendiated high grade pleomorphic sarcoma, <strong>and</strong> o<strong>the</strong>rs)<br />
F. Malignant tumors with “malignant fibrous histiocytoma”-like pattern<br />
• Malignant fibrous histiocytoma<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans with transformation to malignant fibrous histiocytoma<br />
• Dedifferentiated MFH-like areas in liposarcoma<br />
• Inflammatory <strong>and</strong> pleomorphic leiomyosarcoma<br />
• Malignant mesenchymoma with multinucleated osteoclastic-like cells<br />
• Malignant melanoma 55<br />
• Metastatic sarcomatoid/metaplastic carcinoma (e.g. renal cell carcinoma)
252<br />
M. BISCEGLIA ET AL.<br />
Table VI. Tumors/pseudotumors with a distinctive architecture / growth pattern.<br />
A. Tumors <strong>and</strong> pseudotumors with fascicular pattern<br />
• Pseudoneoplastic leprosy (histoid variety)<br />
• Atypical mycobacterial spindle cell pseudotumor<br />
• Fibromatosis<br />
• Dermatomy<strong>of</strong>ibroma<br />
• Myoid fibroma <strong>of</strong> <strong>the</strong> skin<br />
• Cellular schwannnoma<br />
• Leiomyoma (pilar, vascular type, ordinary)<br />
• Myoepi<strong>the</strong>lioma (including storiform, herring-bone)<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans with fibrosarcomatous areas (herring-bone)<br />
• Pigmented dermat<strong>of</strong>ibrosarcoma protuberans (Bednar tumor)<br />
• Bednar tumor with fibrosarcomatous areas (herring-bone)<br />
• Fibrosarcoma (herring-bone)<br />
• Leiomyosarcoma<br />
• My<strong>of</strong>ibrosarcoma 56<br />
• Spindle cell liposarcoma<br />
• Malignant peripheral nerve sheath tumor<br />
• Fibrous monophasic synovial sarcoma<br />
• Fibrous synovial sarcoma (herring bone)<br />
• Leiomyomatous (spindle cell) rhabdomyosarcoma in children<br />
• Spindle cell rhabdomyosarcoma in adults<br />
• (Extra-)gastrointestinal stromal tumor 57 <strong>and</strong> o<strong>the</strong>r intra-abdominal spindle cell <strong>lesions</strong> 58<br />
• Follicular dendritic cell sarcoma<br />
• Cytokeratin-positive fibroblastic reticulum cell neoplasm<br />
• Melanoma 59<br />
B. Tumors with storiform (cartwheel) pattern<br />
• Benign fibrous histiocytoma<br />
• Neur<strong>of</strong>ibroma<br />
• Myoepi<strong>the</strong>lioma<br />
• Cellular perineurioma (storiform perineurial fibroma)<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans (classic type)<br />
• Pigmented dermat<strong>of</strong>ibrosarcoma protuberans (Bednar tumor)<br />
• Malignant fibrous histiocytoma (storiform-pleomorphic)<br />
• Metastatic sarcomatoid renal cell carcinoma<br />
C. Tumors <strong>and</strong> pseudotumors with whorled / curlicue pattern<br />
• Pacinian neuroma<br />
• Benign fibrous histiocytoma (epi<strong>the</strong>lioid type with cellular whorls) (occasional)<br />
• Primary cutaneous <strong>and</strong> metastatic meningioma<br />
• Meningioma-like tumor <strong>of</strong> <strong>the</strong> skin<br />
• Nerve sheath tumor (benign, <strong>and</strong> malignant)<br />
• Nerve sheath myxoma (Pacinian neur<strong>of</strong>ibroma)<br />
• Perineurioma (mainly cellular <strong>and</strong> Pacinian types)<br />
• Myopericytoma-type perivascular myoma 60<br />
• Plexiform fibrohistiocytic tumor<br />
• Spindle cell liposarcoma<br />
• Dedifferentiated liposarcoma (with meningo<strong>the</strong>lial whorls)<br />
• Melanoma 59<br />
D. Tumors <strong>and</strong> pseudotumors with palisading pattern<br />
• Traumatic neuroma<br />
• Palisading cutaneous fibrous histiocytoma<br />
• Dermat<strong>of</strong>ibroma with my<strong>of</strong>ibroblastic differentiation<br />
• Palisaded angioleiomyoma<br />
• Benign nerve sheath tumor<br />
• Palisaded encapsulated neuroma / solitary circumscribed neuroma <strong>of</strong> <strong>the</strong> skin<br />
• Myoepi<strong>the</strong>lioma<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans (occasional)
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 253<br />
• Primary cutaneous <strong>and</strong> metastatic meningioma<br />
• Neuroblastoma-like neurilemmoma<br />
• Leiomyoma<br />
• Leiomyosarcoma<br />
• Epi<strong>the</strong>lioid sarcoma<br />
• Fibrous synovial sarcoma (rare)<br />
• (Extra-)gastrointestinal stromal tumor<br />
• Malignant melanoma<br />
E. Tumors with amianthoid structures <strong>and</strong> (pseudo)rosettes<br />
• Dendritic cell neur<strong>of</strong>ibroma with pseudorosettes<br />
• Myxopapillary ependymoma<br />
• Low-grade fibromyxoid sarcoma<br />
• Hyalinizing spindle cell tumor with giant rosettes<br />
• Intranodal palisaded my<strong>of</strong>ibroblastoma<br />
• S<strong>of</strong>t tissue my<strong>of</strong>ibroblastoma<br />
• Schwannoma<br />
• S<strong>of</strong>t tissue perineurioma<br />
• Peripheral neuroepi<strong>the</strong>lioma (PNET) / Ewing’s sarcoma<br />
• Neuroblastoma<br />
• Malignant peripheral nerve sheath tumor (rare)<br />
• Malignant lymphoma<br />
F. Tumors with cording / chordoid pattern<br />
• Calcifying aponeurotic fibroma<br />
• Chondroid lipoma<br />
• Myoepi<strong>the</strong>lioma<br />
• Mixed tumor<br />
• Parachordoma<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
• Extraskeletal myxoid chondrosarcoma, including <strong>the</strong> neuroendocrine variant<br />
• Round cell liposarcoma (rare)<br />
• Epi<strong>the</strong>lioid variant <strong>of</strong> malignant peripheral nerve sheath tumor<br />
• Metastatic chordoma<br />
• Ossifying fibromyxoid tumor<br />
• Epi<strong>the</strong>lioid sarcoma<br />
G. Tumors with endocrinoid pattern<br />
• Paraganglioma (zellballen)<br />
• Glomus tumor<br />
• Alveolar rhabdomyosarcoma, solid variant<br />
• Paraganglioma-like dermal melanocytic tumors 61<br />
• Metastatic renal cell carcinoma<br />
• Melanoma 59<br />
H. Tumors with alveolar pattern<br />
• Alveolar rhabdomyosarcoma<br />
• Alveolar s<strong>of</strong>t part sarcoma<br />
• Ewing’s sarcoma (pseudoalveolar)<br />
• Metastatic renal cell carcinoma<br />
59, 59a<br />
• Melanoma<br />
I. Tumors with pseudo-gl<strong>and</strong>ular pattern<br />
• Adenomatoid tumor (lace-like or tubular pattern)<br />
• Pseudogl<strong>and</strong>ular schwannoma<br />
• Tenosynovial giant cell tumor – diffuse type (cleft-like “pseudosynovial” spaces)<br />
• Monophasic epi<strong>the</strong>lial synovial sarcoma<br />
• Monophasic epi<strong>the</strong>lial <strong>and</strong> biphasic meso<strong>the</strong>lioma<br />
62, 62a<br />
• PNET with adamantinomatoid pattern<br />
• Melanoma 59
254<br />
M. BISCEGLIA ET AL.<br />
J. Tumors with pseudo-vascular pattern<br />
• Hamartoma <strong>of</strong> <strong>the</strong> scalp with psedoangiosarcomatous features<br />
• Pseudoangiomatous hyperplasia <strong>of</strong> mammary stroma<br />
• Giant cell fibroblastoma<br />
• Spindle cell lipoma – pseudoangiomatous variant<br />
• Angiomy<strong>of</strong>ibroblastoma<br />
• Epi<strong>the</strong>lioid sarcoma<br />
• Rhabdomyosarcoma –sclerosing, pseudovascular variant<br />
• Melanoma 59<br />
K. Tumors with retiform pattern<br />
i. Reticular – Netlike<br />
• Reticular perineurioma<br />
• Extraneurial retiform perineurioma<br />
• Hybrid perineurioma-schwannoma <strong>and</strong> perineurioma-neur<strong>of</strong>ibroma tumors<br />
• Myoepi<strong>the</strong>lioma<br />
ii. Rete Testis-like<br />
• Retiform hemangioendo<strong>the</strong>lioma<br />
• Composite hemangioendo<strong>the</strong>lioma<br />
• Polymorphous hemangioendo<strong>the</strong>lioma<br />
L. Tumors with (pseudo-)papillary pattern<br />
• Lipoma arborescens<br />
• Spindle cell lipoma (occasional)<br />
• Dabska’s tumor<br />
• Tenosynovial giant cell tumor – diffuse type<br />
• Extraspinal ependymoma (myxopapillary type)<br />
• Meso<strong>the</strong>lioma<br />
59, 59a<br />
• Melanoma
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 255<br />
Table VII. Distinctive vascular patterned <strong>lesions</strong> (mainly non-endo<strong>the</strong>lial).<br />
26 63 64<br />
A. Tumors with constant hemangiopericytoma-like pattern<br />
• Nasopharyngeal angi<strong>of</strong>ibroma<br />
• My<strong>of</strong>ibroma <strong>and</strong> my<strong>of</strong>ibromatosis<br />
• Myopericytoma .<br />
• Solitary fibrous tumor<br />
• Hemangiopericytoma<br />
• Extraskeletal mesenchymal chondrosarcoma<br />
• Extrarenal renin-producing juxtaglomerular tumor<br />
• Spindle cell synovial sarcoma<br />
26 63 64<br />
B. Tumors with possible hemangiopericytoma-like pattern<br />
• (Pyogenic granuloma)<br />
• Hemangiopericytoma-like dermat<strong>of</strong>ibroma<br />
• Epi<strong>the</strong>lioid benign fibrous histiocytoma<br />
• Cellular fibrous histiocytoma<br />
• (Kaposi's sarcoma)<br />
• Infantile fibrosarcoma<br />
• Spindle cell lipoma with pseudoangiomaotus pattern<br />
• Malignant fibrous histiocytoma (storiform-pleomorphic)<br />
• Malignant peripheral nerve sheath tumor<br />
• Low grade fibromyxoid sarcoma (sometimes in recurrence)<br />
• Synovial sarcoma<br />
• Phosphaturic mesenchymal tumor<br />
• Leiomyosarcoma<br />
• Liposarcoma (pleomorphic; dedifferentiated)<br />
• Glomus tumor (glomangiopericytoma)<br />
• Paraganglioma<br />
• Thymoma (predominantly spindle cell type / medullary type / type A)<br />
• Low grade endometrial stromal sarcoma - primary retroperitoneal; metastatic<br />
• Malignant meso<strong>the</strong>lioma – fibrous type<br />
• Metastatic sarcomatoid carcinoma (kidney, lung)<br />
• Melanoma – primary, metastatic 59<br />
C. Tumors with prominent perivascular hyalinization<br />
• Orbital & extraorbital giant cell angi<strong>of</strong>ibroma<br />
• Schwannoma<br />
• Cellular angi<strong>of</strong>ibroma (external genital sites)<br />
• Aggressive angiomyxoma<br />
• Solitary fibrous tumor<br />
• Pleomorphic hyalinizing angiectatic tumor<br />
• Hemangiopericytoma<br />
• Extragastrointestinal gastrointestinal stromal tumor (not uncommon)<br />
D. Tumors with plexiform capillary pattern<br />
• Paraganglioma (mainly “branchiomeric type”)<br />
• Hemangioblastoma, extra-neuraxial<br />
• Myxoid liposarcoma 65<br />
• Myxoid malignant fibrous histiocytoma<br />
E. Tumors with glomeruloid capillary pattern<br />
• (Intravascular papillary endo<strong>the</strong>lial hyperplasia - Masson’s phenomenon)<br />
• (Tufted angioma)<br />
• (Glomeruloid hemangioma)<br />
• (Dabska’s tumor) 66<br />
• Malignant angioendo<strong>the</strong>liomatosis (intravascular lymphoma)<br />
• Some neural <strong>and</strong> neuroendocrine neoplasms
256<br />
M. BISCEGLIA ET AL.<br />
F. Lesions with hemorrhagic changes / pattern<br />
• (Organizing hematoma)<br />
• (Pyogenic granuloma)<br />
• (Kaposi’s sarcoma)<br />
• (S<strong>of</strong>t tissue Kaposiform hemangioendo<strong>the</strong>lioma)<br />
• (Capillary hemangioma <strong>of</strong> <strong>the</strong> infantile hemangioendo<strong>the</strong>lioma type)<br />
• Hemorrhagic dermatomy<strong>of</strong>ibroma<br />
• Intranodal hemorrhagic spindle cell tumor with “amianthoid” fibres<br />
• Extraskeletal myxoid chondrosarcoma<br />
• Pleomorphic hyalinizing angiectatic tumor<br />
G. Tumors with aneurysmal changes / pattern<br />
• (Cavernous hemangioma, sinusoidal hemangioma, …)<br />
• Angiomatoid cellular blue nevus 66a<br />
• Aneurysmal bone cyst <strong>of</strong> s<strong>of</strong>t tissue<br />
• Aneurysmal (“angiomatoid”) benign fibrous histiocytoma<br />
• Angiomatoid fibrous histiocytoma (angiomatoid “malignant fibrous histiocytoma”)<br />
• Atypical fibroxanthoma (aneurysmal or pigmented variant)<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans 67<br />
• Malignant fibrous histiocytoma giant-cell type 67<br />
• S<strong>of</strong>t tissue giant cell tumor<br />
• Pleomorphic hyalinizing angiectatic tumor<br />
• Cutaneous Ewing’s sarcoma<br />
• Paraganglioma (occasional)<br />
• S<strong>of</strong>t tissue telangiectatic osteosarcoma<br />
• Metastatic sarcomatoid carcinoma (mainly from kidney)<br />
• High grade sarcoma <strong>of</strong> various types (e.g. angiomatoid or angiectoid or angiosarcoma-like variant <strong>of</strong> epi<strong>the</strong>lioid<br />
sarcoma 26a, 67a, 67b )
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 257<br />
Table VIII. Combined, polyphasic, <strong>and</strong> heterologous tumors (o<strong>the</strong>r than collision<br />
tumors).<br />
A. Combined (homologous <strong>and</strong> heterologous) tumors<br />
• Combined dermat<strong>of</strong>ibroma (two variants in <strong>the</strong> same lesion)<br />
• Giant cell fibroblastoma / demat<strong>of</strong>ibrosarcoma protuberans<br />
• Giant cell fibroblastoma / Bednar tumor<br />
• Giant cell angi<strong>of</strong>ibroma / dermat<strong>of</strong>ibrosarcoma protuberans<br />
• Bednar tumor / dermal melanocytosis<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans / myx<strong>of</strong>ibrosarcoma<br />
• Lipoma / leiomyoma<br />
• Angiomatosis / glomus cell proliferation<br />
• Acquired tufted angioma / vascular malformation<br />
• Lipoleiomyosarcoma<br />
• Neur<strong>of</strong>ibroma / schwannoma<br />
• Neur<strong>of</strong>ibroma / perineurioma 68<br />
• Schwannoma / perineurioma 69<br />
• Sarcomas (usually angiosarcomas) in malignant peripheral nerve sheath tumor<br />
• Mesenchymoma<br />
• S<strong>of</strong>t tissue ectomesenchymoma (benign <strong>and</strong> malignant Triton tumor, …)<br />
• Angiosarcoma in neur<strong>of</strong>ibroma<br />
• Epi<strong>the</strong>lioid malignancies in schwannomas<br />
59, 59a<br />
• Melanoma with adenoid pattern<br />
• Melanoma with neurosarcomatous transformation<br />
• Melanoma with ganglioneuroblastic differentiation<br />
• Rhabdomyosarcoma in a congenital melanocytic nevus<br />
B. Biphasic homologous (bimorphic) tumors<br />
• Lymphangiomyoma<br />
• Schwannoma (Antoni A & B areas).<br />
• My<strong>of</strong>ibroma <strong>and</strong> my<strong>of</strong>ibromatosis<br />
• Fibrous hamartoma <strong>of</strong> infancy<br />
• Myolipoma (lipoleiomyoma)<br />
• Lip<strong>of</strong>ibromatosis<br />
• Angiolipoma<br />
• Cellular angiolipoma<br />
• Angioleiomyoma<br />
• Neural fibrolipoma (fibrolipomatous hamartoma <strong>of</strong> nerve)<br />
• Lipomatous neur<strong>of</strong>ibroma<br />
• Myelolipoma (adrenal; extraadrenal)<br />
• Fibrohistiocytic lipoma<br />
• Kaposi’s sarcoma<br />
• Plexiform fibrohistiocytic tumor<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans (with myoid differentiation; with nodular sclerotic changes)<br />
• Superficial / cutaneous angiomyxoma with epi<strong>the</strong>lial component<br />
• Low grade fibromyxoid sarcoma<br />
• Hemosiderotic fibrohistiocytic lipomatous tumor<br />
• Intramuscular hemangioma with fatty component (can be viewed as triphasic)<br />
• Spindle cell lipoma in intramuscular lipoma (can be viewed as triphasic) 70<br />
• Angiomyolipoma (can be viewed as triphasic)<br />
• Synovial sarcoma<br />
• Mixed-type liposarcoma (dedifferentiated liposarcoma) 71<br />
• Low-grade dedifferentiated liposarcoma 72<br />
• Mixed-type liposarcoma (combined type: myxoid/round cell <strong>and</strong> pleomorphic liposarcoma)<br />
• Lipoleiomyosarcoma<br />
• Myxoid liposarcoma with nodules <strong>of</strong> round cell liposarcoma<br />
• Lipomatous hemangiopericytoma<br />
• Extraskeletal mesenchymal chondrosarcoma<br />
• Dedifferentiated parosteal osteosarcoma<br />
• Ganglioneuroma (mature Schwannian stroma <strong>and</strong> ganglion cells)<br />
• Ganglioneuroblastoma
258<br />
M. BISCEGLIA ET AL.<br />
• Desmoplastic small round cell tumor (nests <strong>of</strong> undifferentiated tumor cells plus fibrous stroma)<br />
• Merkel cell tumor with squamous cell differentiation, <strong>and</strong>/or gl<strong>and</strong>ular differentiation<br />
C. Biphasic heterologous tumors – with epi<strong>the</strong>lial elements<br />
• Hyaline cell rich-chondroid syringoma<br />
• Mixed tumors<br />
• Myoepi<strong>the</strong>liomas<br />
• Parachordoma<br />
• Lipoma with synovial metaplasia<br />
• Ectopic hamartomatous thymoma<br />
• Superficial angiomyxomas / cutaneous myxomas<br />
• Schwannoma (with gl<strong>and</strong>ular differentiation; with squamous cell elements)<br />
• Malignant peripheral nerve sheath tumor with gl<strong>and</strong>ular <strong>and</strong> neuroendocrine differentiation; with squamous<br />
cell isl<strong>and</strong>s)<br />
• Ectomesenchymoma (benign, <strong>and</strong> malignant)<br />
• Malignant gl<strong>and</strong>ular Triton tumor<br />
• Biphasic synovial sarcoma with gl<strong>and</strong>ular differentiation<br />
• Epi<strong>the</strong>lial synovial sarcoma with squamous cell differentiation<br />
• Pretibial s<strong>of</strong>t tissue adamantinoma<br />
• Merkel cell tumor with leiomyo- or rhabdomyosarcomatous differentiation (see below at “E”)<br />
• Dermal squamomelanocytic tumor 73<br />
• Dermal basomelanocytic tumor 74<br />
D. Pseudo-biphasic tumors<br />
• Tumor growing in normal tissue<br />
i. Intramuscular lipoma<br />
ii. Intramuscular hemangioma<br />
iii. Intramuscular fasciitis<br />
iv. Proliferative myositis<br />
v. Fibromatosis colli<br />
vi. Intraneural leiomyoma<br />
vii. Intraneural glomus tumor<br />
viii. Intraneural synovial sarcoma<br />
ix. Sarcomas infiltrating fat<br />
• Tumor growing in tumor<br />
i. Schwannoma with metastatic carcinoma <strong>of</strong> <strong>the</strong> breast<br />
ii. Meningioma with metastatic carcinoma (various sources)<br />
iii. Malignant transformation in a benign tumor (e.g. angiosarcoma in hemangioma, Dabska tumor in a<br />
lymphangioma, malignant peripheral nerve sheath tumor in a ganglioneuroma, carcinoma arising in ectopic<br />
hamartomatous thymoma, carcinoma arising in a mixed tumor <strong>of</strong> s<strong>of</strong>t tissue, …)<br />
E. Biphasic tumors with skeletal muscle differentiation<br />
• Rhabdomyomatous mesenchymal hamartoma <strong>of</strong> <strong>the</strong> skin<br />
• Leiomyoma <strong>and</strong> leiomyosarcoma<br />
• Dedifferentiated liposarcoma<br />
• Myxoid liposarcoma<br />
• Dedifferentiated chondrosarcoma<br />
• Neuromuscular choristoma (benign Triton tumor / benign ectomesenchymoma)<br />
• Malignant peripheral nerve sheath tumor / Malignant ectomesenchymoma (malignant Triton tumor)<br />
• Benign <strong>and</strong> malignant mesenchymoma<br />
• Ganglioneuroma <strong>and</strong> ganglioneuroblastoma<br />
• Merkel cell tumor<br />
• Metastasis from any tumors (<strong>of</strong> any lineage o<strong>the</strong>r than mesenchymal), possibly containing skeletal muscle<br />
component: germ cell tumors, blastomas, carcinosarcomas, tumors <strong>of</strong> specialized stroma [phyllodes tumors <strong>of</strong><br />
breast, uterine adenosarcoma, Sertoli-Leydig cell tumor <strong>of</strong> <strong>the</strong> ovary], neuroendocrine carcinomas [Merkel<br />
cell tumor <strong>and</strong> o<strong>the</strong>r small cell carcinomas]
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 259<br />
Table IX. Histogenetically diverse but morphologically similar tumors <strong>and</strong><br />
pseudotumors with …<br />
A. Round-cell / epi<strong>the</strong>lioid / plasmacytoid features<br />
• Epi<strong>the</strong>lioid benign fibrous histiocytoma<br />
• Myoepi<strong>the</strong>lioma<br />
• Mixed tumor<br />
• Hyaline cell rich-chondroid syringoma<br />
• Parachordoma<br />
• Epi<strong>the</strong>lioid neur<strong>of</strong>ibroma<br />
• Epi<strong>the</strong>lioid schwannoma<br />
• Cutaneous epi<strong>the</strong>lioid Schwannoma 75<br />
• Epi<strong>the</strong>lioid hemangioma<br />
• Glomus tumor<br />
• Epi<strong>the</strong>lioid leiomyoma<br />
• Epi<strong>the</strong>lioid angioleiomyoma<br />
• Tenosynovial giant cell tumor – diffuse type<br />
• Angiomy<strong>of</strong>ibroblastoma<br />
• Solitary fibrous tumor<br />
• Ossifying fibromyxoid tumor<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
• Epi<strong>the</strong>lioid sarcoma<br />
• Epi<strong>the</strong>lioid sarcoma-like hemangioendo<strong>the</strong>lioma<br />
• Epi<strong>the</strong>lioid leiomyosarcoma<br />
• Epi<strong>the</strong>lioid variant <strong>of</strong> malignant peripheral nerve sheath tumor<br />
• Epi<strong>the</strong>lioid angioleiomyoma<br />
• Epi<strong>the</strong>lioid angiomyolipoma <strong>and</strong> o<strong>the</strong>r PEComas 76-78<br />
• Epi<strong>the</strong>lioid angiosarcoma<br />
• Poorly differentiated fibrosarcoma<br />
• Sclerosing epi<strong>the</strong>lioid fibrosarcoma<br />
• Round cell liposarcoma<br />
• Epi<strong>the</strong>lioid liposarcoma<br />
• Extraskeletal myxoid chondrosarcoma – epi<strong>the</strong>lioid variant<br />
• Alveolar s<strong>of</strong>t part sarcoma<br />
• Proximal-type epi<strong>the</strong>lioid sarcoma<br />
• Extrarenal malignant rhabdoid tumor<br />
• Biphasic & monophasic epi<strong>the</strong>lial synovial sarcoma<br />
• Biphasic & monophasic epi<strong>the</strong>lial meso<strong>the</strong>lioma<br />
• Deciduoid meso<strong>the</strong>lioma 79-81<br />
• Extranodal (epi<strong>the</strong>lioid) histiocytic sarcoma 82<br />
B. Clear cell changes 83<br />
• Fibrous papule <strong>of</strong> <strong>the</strong> nose, clear cell variant 84<br />
• Clear cell dermat<strong>of</strong>ibroma<br />
• Myoepi<strong>the</strong>lioma – clear cell type<br />
• Angioleiomyoma – clear cell variant<br />
• Angiomyolipoma<br />
• Leiomyoma – clear cell variant<br />
• Atypical fibroxanthoma - clear cell type<br />
• PEComas <strong>of</strong> s<strong>of</strong>t tissue 76<br />
• Abdominopelvic PEComa 77<br />
• PEComas <strong>of</strong> <strong>the</strong> skin 78<br />
• Distinctive dermal clear cell mesenchymal neoplasm 85<br />
• Epi<strong>the</strong>lioid leiomyosarcoma<br />
• Epi<strong>the</strong>lioid malignant peripheral nerve sheath tumor<br />
• Sclerosing epi<strong>the</strong>lioid fibrosarcoma<br />
• Alveolar rhabdomyosarcoma – clear cell variant<br />
• Ewing’s sarcoma – clear cell variant 85a<br />
• Clear cell sarcoma<br />
• Ectopic hamartomatous thymoma with cords <strong>of</strong> clear cells<br />
• Alveolar s<strong>of</strong>t part sarcoma (clear cell degenerative variant)<br />
• Balloon cell nevus<br />
• Balloon cell blue nevus<br />
• Balloon cell melanoma<br />
• Paraganglioma-like dermal melanocytic tumor<br />
• Metastasis <strong>of</strong> clear cell tumors from o<strong>the</strong>r organs<br />
• Peripheral T-cell lymphoma “unspecified”
260<br />
M. BISCEGLIA ET AL.<br />
C. (Uni-/multi-)vacuolated (pseudo-)lipoblasts, <strong>and</strong> (pseudo-)physalipherous cells<br />
• Silicone granuloma<br />
• Fat necrosis<br />
• Atrophic fat in malnutrition<br />
• Polyvinylpyrrolidone <strong>pseudotumoral</strong> histiocytic reaction (“mucicarminophilic histiocytosis”)<br />
• Hibernoma<br />
• Rhabdomyoma (secondary vacuoles to loss <strong>of</strong> glycogen)<br />
• Chondroid lipoma<br />
• Pseudolipoma (battered buttock syndrome)<br />
• Spindle cell hemangioma<br />
• Parachordoma<br />
• Paraganglioma<br />
• Adenomatoid tumor (pseudovacuolated cells)<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
• Inflammatory myxohyaline tumor<br />
• Low grade myx<strong>of</strong>ibrosarcoma (myxoid fibrosarcoma or myxoid malignant fibrous histiocytoma gr. I)<br />
• Myxoid malignant fibrous histiocytoma (gr. II)<br />
• Liposarcoma<br />
• Pseudolipoblastic (“signet-ring”) nerve sheath tumor 85b<br />
• Lipoblastic meningioma<br />
• Chordoma - metastatic, primary heterotopic 28 28b , periphericum 32a<br />
• Ewing’s sarcoma<br />
• (Extra-)gastrointestinal stromal tumor 85c<br />
• Large cell lymphoma (signet ring cell type)<br />
59a, 85d-e<br />
• Melanoma (signet ring-cell type - primary, <strong>and</strong> metastatic)<br />
• Metastatic adenocarcinoma<br />
86 87<br />
D. Eosinophilic / oncocytic features<br />
• Silica reaction<br />
• Crystal storing histiocytosis<br />
• Rhabdomyoma – oncocytic type<br />
• Glomus tumor – oncocytic type<br />
• Paraganglioma – oncocytic type<br />
• Oncocytic myoepi<strong>the</strong>lioma<br />
• S<strong>of</strong>t tissue oncocytoma<br />
• Extraskeletal myxoid chondrosarcoma (cellular variant)<br />
• Alveolar s<strong>of</strong>t part sarcoma<br />
• Malignant extrarenal rhabdoid tumor<br />
• Proximal-type epi<strong>the</strong>lioid sarcoma<br />
• Some benign <strong>and</strong> malignant melanocytic tumors<br />
E. Granular cells<br />
• Granular fibrous papule <strong>of</strong> <strong>the</strong> face 21<br />
• Granular histiocytic cell reaction<br />
• Granular stromal cell reaction with various tumors<br />
• Granular cell tumor / granular cell schwannoma<br />
• Congenital gingival granular cell tumor<br />
• Granular cell dermat<strong>of</strong>ibroma<br />
• Atypical fibroxanthoma with granular cells<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans with granular cells<br />
• Primitive polypoid granular cell tumor (<strong>of</strong> <strong>the</strong> skin)<br />
• Primitive nonneural granular cell tumors <strong>of</strong> skin (<strong>the</strong> same as <strong>the</strong> previous one) 88<br />
• Granular cell perineurioma<br />
• Granular cell leiomyoma<br />
• Hibernoma<br />
• Malignant granular cell tumor<br />
• Granular cell leiomyosarcoma<br />
• Granular cell angiosarcoma<br />
• Some benign <strong>and</strong> malignant melanocytic tumors<br />
F. Rhabdoid- / pseudo-rhabdoid features<br />
• Crystal-storing histiocytosis<br />
• Adult rhabdomyoma<br />
• Rhabdomyomatous mesenchymal hamartoma<br />
• Myoepi<strong>the</strong>lioma
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 261<br />
• Leiomyosarcoma with rhabdoid features<br />
• Rhabdomyosarcoma with rhabdoid features<br />
• Synovial sarcoma<br />
• Extraskeletal myxoid chondrosarcoma – rhabdoid variant<br />
• Epi<strong>the</strong>lioid malignant peripheral nerve sheath tumor<br />
• Proximal-type epi<strong>the</strong>lioid sarcoma<br />
• Extrarenal malignant rhabdoid tumor<br />
• Desmoplastic small round cell tumor<br />
• Meso<strong>the</strong>lioma<br />
• [Also carcinoma, lymphoma, meningioma, <strong>and</strong> primary <strong>and</strong> metastatic melanoma 59a, 85c-d can acquire rhabdoid phe<br />
notype]<br />
G. Ganglion / ganglion-like cells<br />
• Ischemic fasciitis (Atypical decubital fibroplasia)<br />
• Ganglion cell choristoma <strong>of</strong> skin<br />
• Cutaneous ganglion cell tumor<br />
• Cutaneous ganglioneuroma<br />
• Desmoplastic cutaneous ganglioneuroma<br />
• Proliferative fasciitis<br />
• Proliferative myositis<br />
• Ganglioneuroma<br />
• Dendritic cell neur<strong>of</strong>ibroma<br />
• Paraganglioma-like dermal melanocytic tumor<br />
• Ectomesenchymoma<br />
• Differentiating neuroblastoma & ganglioneuroblastoma<br />
H. Small round cell tumors 89<br />
• Glomus tumors (benign, borderline, malignant)<br />
• Tenosynovial giant cell tumor<br />
• Primitive neuroectodermal tumor / extraskeletal Ewing’s sarcoma<br />
• Malignant hemangiopericytoma<br />
• Round cell liposarcoma<br />
• Embryonal rhabdomyosarcoma<br />
• Neuroblastoma<br />
• Desmoplastic small round cell tumor<br />
• Extrarenal malignant rhabdoid tumor<br />
• Embryonal <strong>and</strong> alveolar rhabdomyosarcoma<br />
• Extraskeletal mesenchymal chondrosarcoma<br />
• Extraskeletal myxoid chondrosarcoma – cellular variant<br />
• Small cell osteosarcoma<br />
• Malignant lymphoma<br />
• Granulocytic sarcoma / leukaemia<br />
• Extramedullary myeloid cell tumors<br />
59a, 85d<br />
• Malignant melanoma<br />
• Small cell carcinoma (primary: Merkel cell-type, <strong>and</strong> non-Merkel cell type; metastatic: pulmonary, <strong>and</strong><br />
extrapulmonary)<br />
I. Pleomorphic s<strong>of</strong>t tissue tumors<br />
• Benign or intermediate<br />
i. Pleomorphic fibrous papule <strong>of</strong> <strong>the</strong> face 21<br />
ii. Pleomorphic fibroma <strong>of</strong> <strong>the</strong> skin<br />
iii. Subungual pleomorphic fibroma<br />
iv. Subungual myxoid pleomorphic fibroma<br />
v. Pleomorphic hyalinizing angiectatic tumor<br />
vi. Hemosiderotic fibrohistiocytic lipomatous tumor<br />
vii. Atypical fibroxanthoma<br />
• Malignant 90<br />
viii. Storiform-pleomorphic malignant fibrous histiocytoma<br />
ix. Dedifferentiated areas in well-differentiated liposarcoma<br />
x. Pleomorphic liposarcoma 91<br />
xi. Pleomorphic leiomyosarcoma 92<br />
xii. Pleomorphic my<strong>of</strong>ibrosarcoma<br />
xiii. Pleomorphic rhabdomyosarcoma<br />
xiv. Pleomorphic malignant peripheral nerve sheath tumor<br />
xv. Pleomorphic intimal sarcoma 93<br />
xvi. Malignant PEC-oma (may mimic pleomorphic myogenic sarcoma)
262<br />
M. BISCEGLIA ET AL.<br />
Table X. Tumors <strong>and</strong> pseudotumors with diagnostic clues.<br />
A. Architecturally distinct features<br />
• Swiss cheese pattern (oleogranuloma / paraffinoma, silicone granuloma, fat necrosis, chalazion, …)<br />
• Verocay bodies <strong>and</strong> Verocay-like bodies or nuclear palisading (benign <strong>and</strong> malignant nerve sheath tumors,<br />
leiomyoma, leiomyosarcoma, spindle cell synovial sarcoma, extragastrointestinal gastrointestinal stromal tumors)<br />
• Homer-Wright rosettes (neuroblastoma, Ewing’s sarcoma, PNET, Merkel cell carcinoma) <strong>and</strong> perivascular<br />
pseudorosettes (ependymoma)<br />
• Amianthoid fibers, or giant collagen rosettes (palisaded my<strong>of</strong>ibroblastoma, hyalinizing spindle cell<br />
tumor with giant rosettes, dendritic cell neur<strong>of</strong>ibroma with pseudorosettes <strong>and</strong> o<strong>the</strong>r nerve sheath<br />
tumors, solitary fibrous tumor, osteocartilaginous tumors, o<strong>the</strong>rs)<br />
• Nonspecific rosettes (non-Hodgkin lymphoma – occasional; epi<strong>the</strong>lioid osteosarcoma, melanoma)<br />
• “Zellballen” (paraganglioma)<br />
• Cambium layer (botryoid embryonal rhabdomyosarcoma)<br />
• Filigree pattern (Ewing’s sarcoma)<br />
• Light cell/dark cell phenomenon – marble appearance (Ewing’s sarcoma, MPNST)<br />
• Azzopardi’s effect (Merkel cell tumor; o<strong>the</strong>r small cell tumors)<br />
• Zoning phenomenon from fibroblastic center to ossified periphery (myositis ossificans)<br />
• Reverse zoning phenomenon (osteosarcoma)<br />
• Pacinian corpuscle (Pacinian neuroma)<br />
• Wagner-Meissner body (diffuse neur<strong>of</strong>ibroma)<br />
• Pacinian body-like <strong>and</strong> Meissner body-like structures (nerve sheath tumors)<br />
• Onion-bulb structures (hereditary diffuse hypertrophic neuropathies: Charcot-Marie-Tooth disease, Dejerine-Sottas<br />
disease; o<strong>the</strong>r true onion bulb neuropathies: Refsum disease, Krabbe’s disease, Roussy-Levi disease, metachromatic<br />
leukodystrophy, neur<strong>of</strong>ibromatosis type 1, diabetic neuropathy, chronic inflammatory demyelinating<br />
polyradiculoneuropathy; localized hypertrophic inflammatory neuropathy; “localized hypertrophic neuropathy”<br />
as true onion bulb neuropathy)<br />
• Pseudo-onion bulb structures (“localized hypertrophic neuropathy” as intraneural perineurioma;<br />
extraneural/s<strong>of</strong>t tissue perineurioma)<br />
• Cytophagocytosis (cytophagic histiocytic panniculitis/subcutaneous panniculitis-like T-cell lymphoma; inflammatory<br />
malignant fibrous histiocytoma; alveolar rhabdomyosarcoma, melanoma, …)<br />
• Emperipolesis (Rosai-Dorfman disease, inflammatory myxohyaline tumor 94 , inflammatory liposarcoma 95 )<br />
B. Extracellular findings / stromal precipitates<br />
• Schaumann bodies (sarcoid, sarcoid-like granulomatous reactions)<br />
• (Pseudo-)psammomatous calcifications (calcifying fibrous pseudotumor)<br />
• Psammoma bodies (cutaneous meningioma)<br />
• Congophilic green birefringent material (amyloid tumor)<br />
47, 48<br />
• Non-congophilic amorphous material in pelvic <strong>and</strong> retroperitoneal s<strong>of</strong>t tissue (Tamm-Horsfall protein deposition)<br />
• Non-congophilic positively birefringent microcrystals (tumoral pseudogout)<br />
• Non-congophilic, needle-shaped birefringent crystals (tophaceous gout)<br />
• Foreign bodies (even partly intracellular) (silica [soil, glass], talc, starch, condom emulsion, silicone, cactus spine, seaurchin<br />
spine, hairs, wooden splinters, suture material, dacron graft, woollen swab, …) (foreign body reactions<br />
<strong>and</strong> granulomas, <strong>pseudotumoral</strong> granulomatous reactions, textilomas, …)<br />
• Non-congophilic amorphous material in pelvic <strong>and</strong> retroperitoneal s<strong>of</strong>t tissue (Tamm-Horsfall protein deposition) 47,48<br />
• Petaloid globules – chenille bodies (elast<strong>of</strong>ibroma)<br />
• Skeinoid fibres (intestine-based stromal tumor with neural differentiation, <strong>and</strong> rarely extra-gastrointestinal GIST)<br />
• Ferruginous bodies – asbestos bodies (meso<strong>the</strong>lioma)<br />
• Intravascular fibrin thrombi (-angiolipoma)<br />
C. Cytohistologically distinct features<br />
• Cell peculiarities<br />
– Fleurette-like cells (pleomorphic lipoma, giant cell angi<strong>of</strong>ibroma)<br />
– Touton cells (juvenile xanthogranuloma, Erdheim-Chester disease)<br />
– Reed-Sternberg-like cells (inflammatory myxo-hyaline tumor, proliferative myositis, some extranodal s<strong>of</strong>t<br />
tissue large cell lymphomas, …)<br />
– Spider cells (rhabdomyoma)<br />
– Tombstone-cells (epi<strong>the</strong>lioid hemangioma)<br />
– Hobnail-cells (hob-nail hemangiomas – Dabska’s type, retiform; polymorphous hemangioendo<strong>the</strong>lioma, …)<br />
– Vacuolated cells (lipoblast → liposarcoma; lipoblast-like stromal cells → myx<strong>of</strong>ibrosarcoma; lipoblast-like<br />
macrophage → fat necrosis, oleogranulomas; bubbly histiocytes → polyvynilpyrrolidone reaction;<br />
endo<strong>the</strong>lioblast <strong>and</strong> endo<strong>the</strong>liocyte → vascular tumors; …)
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 263<br />
– Strap cells / cross-striated cells (rhabdo-myomatous/-myosarcomatous tumors)<br />
– Longitudinally pseudostriated cells (crystal storing histiocytosis in lymphoproliferative disorders)<br />
• Intracellular findings<br />
i. Melanin (melanocytic tumor; neural tumor; neuroectodermal tumor)<br />
ii. Intracytoplasmic hyaline globules (Kaposi’s sarcoma, glomeruloid hemangioma, Kaposiform<br />
hemangioendo<strong>the</strong>lioma)<br />
iii. Trichrome stain positive intracytoplasmic inclusions (infantile digital fibromatosis; my<strong>of</strong>ibrosarcoma)<br />
iv. Granular material in reactive histiocytes (site <strong>of</strong> previous surgery)<br />
v. Intracytoplasmic small black particles in foamy histiocytes (pros<strong>the</strong>tic heavy metal detritus)<br />
vi. Intracytoplasmic PAS-D resistant bodies (granular cell tumor; extraintestinal Whipple’s disease 96 97 )<br />
vii. Intracellular crystalline PAS-D positive material (alveolar s<strong>of</strong>t part sarcoma)<br />
viii.Intracytoplasmic paracrystalline material (crystal storing histiocytosis in lymphoproliferative disorders)<br />
ix. Michaelis-Gutmann bodies (malakoplakia)<br />
x. Asteroid bodies (sarcoid, sarcoid-like granulomatous reactions, …)<br />
xi. Infectious bacilli (bacillary angiomatosis, mycobacterial disease, atypical mycobacterial disease, Whipple disease)<br />
xii. Cytoplasmic cross-striations (rhabdo-myomatous / -myosarcomatous tumors)<br />
xiii.Cytoplasmic fibrillary pattern (“wrinkled cigarette paper” in Gaucher disease, …)<br />
xiv. Cytoplasmic intranuclear pseudoinclusions (meningioma, nerve sheath tumors, melanocytic tumors, s<strong>of</strong>t tissue<br />
lymphoplasmacytic proliferative disorders [Dutcher bodies], metastatic hepatocellular carcinoma)<br />
xv. Nuclear vacuoles – lochkern (normal fat)<br />
xvi.Nuclear grooves (s<strong>of</strong>t tissue metastatic thyroid papillary carcinoma; metastatic granulosa cell tumor; melanoma)
264<br />
M. BISCEGLIA ET AL.<br />
Table XI. Histologically* pigmented tumors <strong>and</strong> pseudotumors with …<br />
A. Melanin pigment<br />
• Fibrous papule <strong>of</strong> face –pigmented variant 21<br />
• Cutaneous benign fibrous histiocytoma (clinically pigmented)<br />
• Intradermal Spitz nevus<br />
• Dermal dendritic melanocytic proliferations 98 (including deep seated blue nevus)<br />
99 100<br />
• Pigmented pilomatrixoma <strong>and</strong> melanocytic pilomatrixoma<br />
• Pigmented (melanotic) neur<strong>of</strong>ibroma<br />
• Pigmented (melanotic) schwannoma<br />
• Psammomatous melanotic schwannoma<br />
• Cutaneous psammomatous melanotic schwannoma 101<br />
• Pigmented dermat<strong>of</strong>ibrosarcoma protuberans (Bednar tumor)<br />
• Bednar tumor associated with dermal melanocytosis<br />
• Neurocristic cutaneous hamartoma<br />
• Neurocutaneous melanosis (melanoma, melanoblastoma, meningeal melanocytosis)<br />
• Pigmented (melanotic) neuroectodermal tumor <strong>of</strong> infancy<br />
• Ordinary melanoma<br />
• Primary dermal melanoma 102<br />
• Desmoplastic melanoma<br />
• Deep melanoma<br />
• Metastatic melanoma<br />
• Pigmented epi<strong>the</strong>lioid melanocytoma 103 / animal-equine-type melanoma 104 / epi<strong>the</strong>lioid blue nevus (sporadic,<br />
<strong>and</strong> syndromic – associated with Carney’s syndrome 105 )<br />
• Clear cell sarcoma<br />
• Pigmented ganglioneuroblastoma<br />
• Phaeochromocytoma <strong>and</strong> o<strong>the</strong>r extraadrenal paraganglioma 106<br />
• Deep melanoma<br />
• [Melaning-producing non-mesenchymal tumors (pigmented carcinoid, thyroid medullary carcinoma)]<br />
B. Hemosiderin<br />
• Hemorrhage / hematoma / ancient hematoma<br />
• Hemangiomas (mainly cavernous type) <strong>and</strong> phakomatoses<br />
• Synovial hemangioma<br />
• Hemosiderotic dermat<strong>of</strong>ibroma<br />
• Targetoid hemosiderotic hemangioma<br />
• Aneurysmal benign fibrous histiocytoma<br />
• Aneurysmal (pigmented) atypical fibroxanthoma<br />
• Kaposi’s sarcoma<br />
• Pleomorphic hyalinizing angiectatic tumor<br />
• Hemosiderotic fibrohistiocytic lipomatous tumor<br />
• Diffuse-type giant cell tumor (pigmented villonodular synovitis / pigmented villonodular bursitis)<br />
• Angiomatoid fibrous histiocytoma<br />
• Tenosynovial giant cell tumor (localized <strong>and</strong> diffuse type)<br />
• Clear cell sarcoma<br />
C. Purified carbon / charcoal<br />
• Preoperative localization <strong>of</strong> gut biopsy sites<br />
• Preoperative localization <strong>of</strong> nonpalpable tumor <strong>lesions</strong><br />
D. India Ink (rare), Cinnabar, Chrome green, Cobalt blue<br />
• Delayed hypersensitivity reactions to tattoos<br />
E. Heavy metals particles<br />
• Paraarticular histiocytic proliferation induced by cobalt-chromium <strong>and</strong> titanium with intracytoplasmic small black<br />
particles in histiocytes (pros<strong>the</strong>tic heavy metal detritus)<br />
[* Clinically pigmented or ery<strong>the</strong>matous tumors <strong>and</strong> pseudotumors without pigment at histology: Asch<strong>of</strong>f's nodules (rheumatic fever), Farber's lipogranulomatosis, Sweet's<br />
syndrome, panniculitis, juvenile xanthogranuloma, mastocytoma, cutaneous T-cell lymphoma, metastatic cutaneous neuroblastoma]
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 265<br />
Table XII. Clinically alarming benign tumors <strong>and</strong> pseudotumors.<br />
A. Multiple / multicentric, possibly recurring benign <strong>lesions</strong><br />
• Cutaneous sarcoid<br />
• Papular angiokeratoma (a frequent mimicker <strong>of</strong> melanoma)<br />
• Multiple eruptive angi<strong>of</strong>ibromas<br />
• Multiple eruptive dermat<strong>of</strong>ibromas (in HIV <strong>and</strong> immunosuppressed patients)<br />
• Recurrent pyogenic granuloma with satellitosis 107<br />
• Multiple pyogenic granulomas<br />
• Generalized pyogenic granuloma<br />
• Multiple nevus lipomatosus cutaneous superficialis<br />
• Multiple cutaneous pilar leiomyomas<br />
• Multiple cutaneous chondromas<br />
• Multiple miliary osteomas <strong>of</strong> <strong>the</strong> face<br />
• Nodular fasciitis (satellite nodules)<br />
• Infantile fibromatosis (desmoid-type)<br />
• Juvenile hyaline fibromatosis 22<br />
• Juvenile lip<strong>of</strong>ibromatosis<br />
• Infantile digital fibromatosis-recurring<br />
• Multiple juvenile xanthogranuloma<br />
• Multicentric reticulohistiocytosis / multiple reticulohistiocytic granulomata / progressive nodular histiocytoma /<br />
generalized eruptive histiocytoma, xanthoma disseminatum<br />
• Tendinous xanthomas<br />
• Xanthogranulomatous inflammation (e.g. in Erdheim-Chester disease)<br />
• (Recurring) tumoral calcinosis<br />
• (Recurring) tophaceous pseudogout (CPPD crystal deposition disease - tumoral form)<br />
• Infantile my<strong>of</strong>ibromatosis<br />
• Multiple multifocal (adult) rhabdomyomas <strong>of</strong> <strong>the</strong> neck 108<br />
• Multiple intramuscular myxomas<br />
• Myolipoma (<strong>of</strong> s<strong>of</strong>t tissue)<br />
• Inflammatory pseudotumor / inflammatory my<strong>of</strong>ibroblastic tumor<br />
• Infantile hemangiopericytoma<br />
• Multiple glomus tumors<br />
• Glomangiomatosis (may recur)<br />
• Multiple glomangiomyomas<br />
• Infiltrating (aggressive, atypical) glomus tumor<br />
• Recurring glomus tumor<br />
• Plexiform neur<strong>of</strong>ibroma<br />
• Multiple schwannomas (schwannomatosis)<br />
• Multiple cutaneous plexiform schwannomas<br />
• Multiple melanotic schwannomas<br />
• Multiple cellular neuro<strong>the</strong>keomas 109<br />
• Giant cell fibroblastoma (recurring)<br />
• Multiple lipomas<br />
• Multiple spindle cell lipomas (familial <strong>and</strong> non-familial forms)<br />
• Multiple angiolipomas (familial <strong>and</strong> non-familial forms)<br />
• Symmetric lipomatosis<br />
• Diffuse lipomatosis<br />
• Diffuse angiomatosis<br />
• Multiple spindle cell hemangio(endo<strong>the</strong>lio)mas<br />
• Spindle cell hemangiomatosis<br />
• Fibrodysplasia (myositis) ossificans progressiva<br />
• (Recurring) bizarre parosteal osteochondromatous proliferation (Nora’s disease)<br />
• Multiple (multifocal) leiomyomas<br />
• Leiomyomatosis peritonealis disseminata<br />
• Granular cell tumor<br />
• Progressive lymphangioma (benign lymphangioendo<strong>the</strong>lioma)<br />
• Reactive angioendo<strong>the</strong>liomatosis<br />
• (Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma)<br />
• Kaposi’s sarcoma<br />
• Cerebriform fibrous proliferations in Proteus syndrome
266<br />
M. BISCEGLIA ET AL.<br />
• (Some) multiple smooth muscle tumors in immunocompromised patients<br />
• Paraganglioma (multicentric)<br />
24, 25<br />
• Reactive nodular fibrous pseudotumors (<strong>of</strong> <strong>the</strong> gastrointestinal tract <strong>and</strong> mesentery)<br />
43, 44<br />
• Sclerosing mesenteritis, mesenteric panniculitis, mesenteric lipodystrophy, <strong>and</strong> o<strong>the</strong>r inflammatory pseudotumors<br />
• Multiple fibrosclerosis (any combination <strong>of</strong> Ormond’s disease, sclerosing cholangitis, mediastinal fibrosis, Riedel’s<br />
thyroiditis, pseudotumor <strong>of</strong> th orbit, autoimmune pancreatitis)<br />
• Sclerosing mediastinitis (idiopathic fibroinflammatory <strong>lesions</strong> <strong>of</strong> <strong>the</strong> mediastinum) 25a<br />
B. Painful s<strong>of</strong>t tissue tumors <strong>and</strong> pseudotumors<br />
• Traumatic neuroma<br />
• Keloid (sometimes)<br />
• Dercum’s disease (adiposis dolorosa)<br />
• Glomus tumors (see section A, above)<br />
• Angiolipoma<br />
• Angioleiomyoma<br />
• Cutaneous leiomyoma<br />
• Morton’s interdigital neuroma<br />
• Schwannomatosis
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 267<br />
Table XIII. Pathologically alarming benign tumors <strong>and</strong> pseudotumors.<br />
A. Lesions with multilobular / mosaic growth pattern<br />
• <strong>Tumoral</strong> calcinosis<br />
• Lipoblastoma<br />
• Cutaneous myxoma<br />
• Neuro<strong>the</strong>keoma<br />
• Juvenile hemangioma<br />
• Pyogenic granuloma<br />
• Acquired tufted angioma<br />
• Schwannoma<br />
• Extraskeletal chondroma<br />
• Synovial chondromatosis (articular <strong>and</strong> extra-articular variant)<br />
• Giant cell tumor<br />
• Intramuscular myxoma (occasional)<br />
• Ossifying fibromyxoid tumor (not including here <strong>the</strong> atypical & malignant variant)<br />
B. Lesions with plexiform / infiltrating margins<br />
• Proliferative fasciitis<br />
• Cranial fasciitis<br />
• Proliferative myositis<br />
• Fibrous hamartoma <strong>of</strong> infancy<br />
• Fibromatosis (any type, mainly infantile type)<br />
• Plexiform xanthomatous tumor<br />
• Plexiform Schwannoma (cutaneous <strong>and</strong> subcutaneous, <strong>and</strong> deep forms) 109a / Schwannomatosis 109b-d<br />
• Plexiform neur<strong>of</strong>ibroma<br />
• Neuro<strong>the</strong>keoma (classic <strong>and</strong> cellular type)<br />
• Nerve sheath myxoma (“plexiform myxoma”)<br />
• Granular cell tumor (plexiform variant)<br />
• Dendritic fibromyxolipoma<br />
• Intramuscular lipoma (infiltrating lipoma)<br />
• Diffuse lipoblastomatosis (infiltrating lipoblastoma)<br />
• Lipoma arborescens<br />
• Cellular schwannoma (occasional)<br />
• Congenital <strong>and</strong> childhood plexiform (multinodular) cellular schwannoma 110<br />
• Deep-seated plexiform schwannoma 111<br />
• Infiltrating retiform perineurioma 112<br />
• Plexiform fibrohistiocytic tumor<br />
C. Lesions with intravascular growth<br />
• [Intralymphatic granulomas (in Crohn’s disease, granulomatous lymphangitis <strong>of</strong> <strong>the</strong> scrotum <strong>and</strong> penis,<br />
granulomatous cheilitis, Melkerson <strong>and</strong> Rosentahl syndrome)]<br />
• Organizing thrombus<br />
• Pyogenic granuloma – intravascular variant<br />
• Neuro<strong>the</strong>keoma<br />
• Epi<strong>the</strong>lioid hemangioma<br />
• Plasma cell granuloma<br />
• Giant cell fibroblastoma<br />
• Intravenous atypical vascular proliferation<br />
• Intravascular papillary endo<strong>the</strong>lial hyperplasia<br />
• Spindle cell hemangioma<br />
• Epi<strong>the</strong>lioid hemangioma<br />
• Myopericytoma – intravascular variant<br />
• My<strong>of</strong>ibroma (solitary type – adult form)<br />
• Infantile my<strong>of</strong>ibromatosis<br />
• Infantile hemangiopericytoma<br />
• Intravascular glomus tumor<br />
• Intravascular fasciitis<br />
• Angioleiomyoma – intravascular form<br />
• Intravenous leiomyomatosis (conventional <strong>and</strong> unusual variants) 113<br />
• Myointimoma<br />
• Tenosynovial giant cell tumor
268<br />
M. BISCEGLIA ET AL.<br />
D. Benign <strong>lesions</strong> with “hypercellularity”<br />
• Cellular fibrous papule <strong>of</strong> <strong>the</strong> face 21<br />
• Cellular digital fibromas<br />
• Cellular dermat<strong>of</strong>ibroma<br />
• Cellular benign fibrous histiocytoma<br />
• Cellular pseudosarcomatous fibroepi<strong>the</strong>lial stromal polyp<br />
• Cellular infantile capillary hemangioma 114<br />
• Cellular spindle cell hemangio(endo<strong>the</strong>lio)ma<br />
• Cellular angiolipoma<br />
• Cellular schwannoma 115<br />
• Cellular schwannoma with granular cells<br />
• Congenital <strong>and</strong> childhood plexiform (multinodular) cellular schwannoma 110<br />
• Cellular neur<strong>of</strong>ibroma<br />
• Cellular leiomyoma<br />
• Cellular perineurioma<br />
• Cellular neuro<strong>the</strong>keoma<br />
• Infantile fibromatosis (desmoid-type)<br />
• Cellular fibromatosis (palmar type)<br />
• Monophasic cellular variants <strong>of</strong> my<strong>of</strong>ibromatosis 116<br />
• Cellular giant cell fibroblastoma<br />
• Cellular intramuscular myxoma<br />
• Cellular rhabdomyoma <strong>of</strong> fetal type (intermediate variant)<br />
• Cellular tenosynovial giant cell tumor<br />
• Cellular ossifying fibromyxoid tumor<br />
• Cellular blue nevus
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 269<br />
Table XIV. Histologically benign <strong>lesions</strong> (o<strong>the</strong>r than vascular proliferations) mistaken<br />
for malignant.<br />
A. Tumor-like <strong>lesions</strong><br />
• Subcutaneous granuloma annulare (mimicking epi<strong>the</strong>lioid sarcoma, epi<strong>the</strong>lioid angiosarcoma)<br />
• Mitotic granuloma annulare<br />
• Necrobiotic xanthogranuloma<br />
• Malakoplakia<br />
• Nodular fasciitis <strong>and</strong> variants (intravascular, cranial, peri- <strong>and</strong> parosteal, intraarticular fasciitis)<br />
• Ischemic fasciitis (atypical decubital fibroplasia)<br />
• Proliferative fasciitis<br />
• Proliferative myositis<br />
• Desmoid fibromatosis<br />
• Reticulohistiocytoma<br />
• (Juvenile) xanthogranuloma with inconspicuous foam cells <strong>and</strong> giant cells (mimicking melanoma)<br />
• Polyvynilpyrrolidone <strong>pseudotumoral</strong> histiocytic reaction (“mucicarminophilic histiocytosis”)<br />
simulating signet-ring cell carcinoma, <strong>and</strong> myxoid liposarcoma<br />
• Tumefactive fibroinflammatory lesion<br />
• Xanthogranulomatous pseudotumor (several etiologies, mainly infectious)<br />
• Epi<strong>the</strong>lial sheath neuroma<br />
• Reactive angioendotehliomatosis<br />
• Intramuscular hypertrophic scar following sarcoma resection<br />
• Massive localized lymphedema in morbid obesity<br />
• Pseudoneoplastic skeletal muscle regeneration<br />
• Post-implant pseudoneoplastic parathyromatosis<br />
• Hyperplastic callus in pathologic conditions (e.g. osteogenesis imperfecta)<br />
• Tumefactive s<strong>of</strong>t tissue extension <strong>of</strong> Paget’s pseudosarcoma<br />
• Tophaceous pseudogout<br />
• Myositis-, panniculitis-, fasciitis- <strong>and</strong> periostitis ossificans<br />
• Fibrodysplasia ossificans progressiva<br />
• Fibroosseous pseudotumor <strong>of</strong> <strong>the</strong> digits<br />
• Bizarre parosteal osteochondromatous proliferation (Nora's lesion)<br />
• Vulvar hypertrophy with lymphedema<br />
• Cutaneous pseudosarcomatous polyp<br />
• Vaginal pseudosarcomatous fibroepi<strong>the</strong>lial polyp 50<br />
• Pseudotumoral deciduosis<br />
• Extramedullary hematopoiesis (e.g. in breast, in retroorbital site, …)<br />
• Sclerosing extramedullary hematopoietic tumor<br />
B. <strong>Tumoral</strong> <strong>lesions</strong><br />
• Granular cell dermat<strong>of</strong>ibroma<br />
• Benign cellular fibrous histiocytoma<br />
• Atypical (pseudosarcomatous) fibrous histiocytoma <strong>of</strong> <strong>the</strong> skin<br />
• Atypical cellular neuro<strong>the</strong>keoma<br />
• Deeply located benign fibrous histiocytoma<br />
• Intraneural glomus tumor<br />
• Symplastic glomus tumor<br />
• Intraneural leiomyoma<br />
• Granular cell tumor<br />
• Symplastic leiomyoma<br />
• Ancient schwannoma<br />
• Plexiform (multinodular) cellular schwannoma 110<br />
• Intramuscular hemangioma<br />
• Synovial chondromatosis (extra-articular variant)<br />
• Aggressive angiomyxoma
270<br />
M. BISCEGLIA ET AL.<br />
Table XV. Reactive endo<strong>the</strong>lial <strong>lesions</strong> that may histologically mimick malignancy.<br />
• Organizing hematoma<br />
• Ancient hematoma<br />
• Intravascular papillary endo<strong>the</strong>lial hyperplasia<br />
• Acroangiodermatitis<br />
• Glomeruloid hemangioma<br />
• Bacillary angiomatosis<br />
• Acquired progressive lymphangioma / benign lymphangioendo<strong>the</strong>lioma<br />
• Reactive angioendo<strong>the</strong>liomatosis<br />
• Benign atypical vascular <strong>lesions</strong> <strong>of</strong> <strong>the</strong> lip<br />
• Multiple trauma-induced targetoid hemosiderotic hemangioma-like <strong>lesions</strong><br />
• Diffuse dermal angiomatosis <strong>of</strong> <strong>the</strong> breast (response to isotretinoin <strong>the</strong>rapy)<br />
• Acquired vulvar lymphangioma (secondary to Crohn’s disease)<br />
• Pyogenic granuloma-like lesion associated with topical retinoid <strong>the</strong>rapy<br />
• Pseudokaposiform reaction to Monsel’s solution<br />
• Florid vascular proliferation as a needle biopsy effect in <strong>the</strong> breast<br />
• Post-radiation vascular proliferations 117<br />
Table XVI. Histologically malignant tumors mistaken for benign 118 .<br />
• Inflammatory mesenchymal sarcomas (“pseudo-pseudotumors”) (e.g. inflammatory leiomyosarcoma, inflammatory<br />
fibrosarcoma, inflammatory malignant fibrous histiocytoma)<br />
versus my<strong>of</strong>ibroblastic pseudotumors <strong>and</strong> tumefactive fibroinflammatory <strong>lesions</strong><br />
• Low grade fibromyxoid sarcoma<br />
versus myxoid neur<strong>of</strong>ibroma, perineurioma, desmoid fibromatosis, nodular fasciitis<br />
• Low grade myx<strong>of</strong>ibrosarcoma<br />
versus myxoid neur<strong>of</strong>ibroma, perineurioma, intramuscular / juxta-articular myxoma, superficial angiomyxoma<br />
• Low grade my<strong>of</strong>ibroblastic sarcoma<br />
versus desmoid fibromatosis<br />
• Well differentiated lipoma-like liposarcoma 119<br />
versus ordinary lipoma, hibernoma<br />
• Well differentiated sclerosing type liposarcoma<br />
versus pleomorphic lipoma<br />
• Well differentiated inflammatory type liposarcoma 120<br />
versus inflammatory process<br />
• Well differentiated spindle cell (neural-like) liposarcoma 121<br />
versus benign peripheral nerve sheath tumor<br />
• Epi<strong>the</strong>lioid sarcoma<br />
versus pseudogranulomatous inflammatory process (deep granuloma annulare, rheumatoid nodule, deep<br />
rheumatoid nodule, necrobiosis lipoidica, necrobiotic granuloma, fibrous benign tumors 67b )<br />
• Subcutaneous panniculitis-like T cell lymphoma & granulomatous slack skin<br />
versus lupus pr<strong>of</strong>undus vs lymphocytic lobular panniculitis vs. atypical lymphocytic lobular panniculitis<br />
• Histiocytic sarcoma<br />
versus benign histiocytosis<br />
• Non-mesenchymal tumors in special locations (low grade sarcomatoid carcinoma in <strong>the</strong> breast)<br />
versus fibromatosis 122
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 271<br />
Table XVII. Atypical variants <strong>of</strong> typical tumors.<br />
A. By clinical features (<strong>the</strong> so-called “man from Istanbul” 123 )<br />
• Any typical superficial s<strong>of</strong>t tissue tumor in deep location (e.g. deep juvenile xanthogranuloma – subcutaneous,<br />
intramuscular, intraneural <strong>and</strong> visceral forms 124 125 ; retroperitoneal spindle cell lipoma; retroperitoneal<br />
Pacinian neuroma; s<strong>of</strong>t tissue deep <strong>and</strong> visceral 126 127 benign fibrous histiocytoma; deep - subcutaneous<br />
dermat<strong>of</strong>ibrosarcoma protuberans without dermal involvement; …)<br />
• Any typical deep s<strong>of</strong>t tissue tumor in very superficial location (e.g. cutaneous rhabdomyosarcoma; cutaneous –<br />
intradermal liposarcoma; Ewing’s sarcoma <strong>of</strong> <strong>the</strong> skin; adamantinoma <strong>of</strong> <strong>the</strong> pretibial s<strong>of</strong>t tissue; …)<br />
• Any typical tumor in heterotopic/unusual locations (e.g. fibrous hamartoma <strong>of</strong> infancy in h<strong>and</strong>s or feet;<br />
non-midline / non-paraxial paraganglioma; subcutaneous/intravascular/visceral-organ based pyogenic granuloma, …)<br />
• Kimura's disease in non-Orientals<br />
• “Extra-nodal” Castleman’s disease<br />
• “Extra-nodal” Rosai-Dorfman disease<br />
• “Extra-nodal” dendritic cell <strong>and</strong> interdigitating cell sarcomas<br />
• “Extra-abdominal” intra-abdominal desmoplastic round cell tumor (pleura, meninges, …)<br />
• “Extra-orbital” (orbital) giant cell angi<strong>of</strong>ibroma<br />
128, 128a<br />
• “Extra-nasopharyngeal” nasopharyngeal angi<strong>of</strong>ibroma<br />
• “Extra-renal” renin-producing juxtaglomerular tumor<br />
• “Extra-renal” rhabdoid tumor (e.g., s<strong>of</strong>t tissue, skin, vulva, …)<br />
• “Non-acral” acral inflammatory myxohyaline tumor<br />
• “Extra-acral” (acral) calcifying aponeurotic fibroma<br />
• “Non-digital” (long bones) fibroosseus pseudotumors <strong>of</strong> <strong>the</strong> digits<br />
• “Extra-acral” (long bones, skull, maxilla) bizarre osteochondromatous proliferation <strong>of</strong> <strong>the</strong> small tubular<br />
bones <strong>of</strong> <strong>the</strong> h<strong>and</strong>s <strong>and</strong> feet<br />
• “Extra-inguinal” intranodal palisaded my<strong>of</strong>ibroblastoma<br />
• “Non-ossifying” ossifying fibromyxoid tumor<br />
• “Extra-osseus” aneurysmal bone cyst<br />
• “Extra-osseous” adamantinoma <strong>of</strong> <strong>the</strong> pretibial s<strong>of</strong>t tissue<br />
• “Extra-articular” synovial sarcoma (e.g., primary cutaneous, intraabdominal 129 , ...)<br />
• “Extra-articular” (articular) pigmented villonodular synovitis / extraarticular diffuse type giant cell tumor<br />
• “Ectopic” ectopic hamartomatous thymoma<br />
• “Extra-genital” (genital/paragenital) calcifying fibrous pseudotumor<br />
• “Extra-gastrointestinal” gastrointestinal stromal tumor<br />
• “Extra-digital” infantile digital fibromatosis<br />
• “Extra-mammary” mammary-type my<strong>of</strong>ibroblastoma<br />
• “Extra-neuraxial” cerebellar-type hemangioblastoma<br />
• “Extra-uterine” (parasitic) uterine leiomyoma<br />
• “Extra-vulval” (vulval) cellular angi<strong>of</strong>ibroma<br />
• (Vulval) angiomy<strong>of</strong>ibroblastoma in males (scrotum)<br />
• (Vulval) angiomy<strong>of</strong>ibroblastoma-like tumor in males (analogous to cellular angi<strong>of</strong>ibroma)<br />
• Aggressive angiomyxoma (<strong>of</strong> <strong>the</strong> female pelvis) in males<br />
• Nasopharyngeal angi<strong>of</strong>ibroma (<strong>of</strong> <strong>the</strong> males) in females<br />
• Juvenile xanthogranuloma in adults<br />
• Infantile digital fibromatosis in adults<br />
• Infantile my<strong>of</strong>ibromatosis in adults<br />
• Calcifying fibrous pseudotumor <strong>of</strong> childhood in adults<br />
• Kaposiform (infantile) hemangioendo<strong>the</strong>lioma in adults<br />
• Non-infantile (infantile) nasal chondromesenchymal hamartoma 130<br />
• Ectopic meningioma<br />
• Pediatric-type sarcomas in adults (including embryonal & botryoid rhabdomyosarcoma) PNET/EWS, angiomatoid<br />
malignant fibrous histiocytoma, plexiform fibrohistiocytic tumor) 131<br />
• Spindle cell rhabdomyosarcoma in adults 132<br />
• Liposarcoma in children (questioned – debated)<br />
• MPNST in children (questioned – debated)<br />
• “Extra-medullary” myeloid tumors (lymph node, upper respiratory tract, female genital tract, s<strong>of</strong>t tissue, body<br />
cavities …)<br />
• “Extraosseous” plasmacytoma (upper respiratory tract, lymph node, s<strong>of</strong>t tissue, skin, mediastinum, …)<br />
• “Extraneuraxial” (retroperitoneal malignant) meningioma 133<br />
• “Extra-uterine” (retroperitoneal) endometrial stromal sarcoma 134<br />
• Heterotopic (retroperitoneal) germ cell tumor<br />
• “Non-phosphaturic” phosphaturic mesenchymal tumor
272<br />
M. BISCEGLIA ET AL.<br />
B. By clinical behaviour<br />
• Metastasizing benign fibrous histiocytoma 135<br />
• Metastasizing benign uterine leiomyoma 136<br />
• Metastasizing benign meningioma 137<br />
• (Metastasizing benign mixed tumors <strong>of</strong> salivary gl<strong>and</strong>s)<br />
C. By macroscopic features<br />
• “Solid” aneurysmal cyst <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> bone<br />
• “Non-protuberans” (atrophic, plaque-type) dermat<strong>of</strong>ibrosarcoma protuberans<br />
• Encapsulated intradermal dermat<strong>of</strong>ibrosarcoma protuberans<br />
• “Non-ossifying” ossifying fibromyxoid tumor<br />
D. By cytological / histological features<br />
• Cell size / cell type<br />
i. Desmoplastic small round cell tumor, large cell variant<br />
ii. Ewing’s sarcoma, large cell (atypical) variant<br />
iii. Ewing’s sarcoma, pleomorphic/anaplastic variant 137a<br />
iv. Merkel cell tumor, large cell variant<br />
v. Anaplastic large cell lymphoma, small cell variant<br />
vi. Non-pleomorphic spindle-cell atypical fibroxanthoma<br />
vii. Juvenile xanthogranuloma without multinucleated giant cells<br />
viii. Plexiform fibrohistiocytic tumor without multinucleated giant cells<br />
ix. Tenosynovial giant cell tumor without giant cells<br />
• Cell / matrix peculiarities<br />
i. Amelanotic melanoma<br />
ii. Non-lipidized juvenile xanthogranuloma (early phase)<br />
iii. Sclerotic lipoma<br />
iv. Fibrous spindle cell lipoma<br />
v. Extraskeletal myxoid chondrosarcoma without myxoid areas<br />
vi. Ewing’s sarcoma, schlerosing variant 62a<br />
• Cell shape<br />
i. Spindle cell melanoma<br />
ii. Spindle cell lipoma<br />
iii. Spindle cell hemangioendo<strong>the</strong>lioma<br />
iv. Leiomyomatous (spindle cell) rhabdomyosarcoma (both in children <strong>and</strong> in adults)<br />
v.<br />
26a, 67b<br />
Fibroma-like variant <strong>of</strong> epi<strong>the</strong>lioid sarcoma<br />
vi. Ewing’s sarcoma, spindle cell variant 62a<br />
vii. Spindle cell lymphoma 138<br />
viii. Sarcomatoid plasmacytoma<br />
ix. Metastatic spindle cell (fibromatosis-like, sarcomatoid) carcinoma<br />
• Architectural pattern<br />
i. Kaposi’s sarcoma (nodular stage) without erythrocyte extravasation<br />
ii. Solid variant <strong>of</strong> alveolar rhabdomyosarcoma<br />
iii. Solid variant <strong>of</strong> aneurysmal bone cyst<br />
iv.<br />
62 62a<br />
Ewing’s sarcoma with adamantinoma-like pattern<br />
• Immunohistochemistry<br />
i. Sarcoma with partial epi<strong>the</strong>lial differentiation (Ewing’s sarcoma 62, 62a, 139 139a-b , fibroblastic dendritic reticulum<br />
cell sarcoma …)<br />
ii. Any tumor with divergent/aberrant expression (e.g. keratins in melanoma 140 , lymphoma, vascular neoplasms,<br />
smooth muscle neoplasms; neuroendocrine markers in sarcoma [chondrosarcoma with neuroendocrine<br />
differentiation]; …)<br />
iii. Any tumor with loss <strong>of</strong> specific antigen (e.g. S-100 protein <strong>and</strong> HMB-45 negative desmoplastic <strong>and</strong> nondesmo<br />
plastic melanoma 85d , cytokeratin negative sarcomatoid carcinoma)<br />
iv. Non-germ cell tumors expressing germ-cell markers (e.g. PLAP expression in tumors with myogenic<br />
differentiation <strong>and</strong> desmoplastic small round cell tumor, ….) 85e
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 273<br />
Table XVIII. Cystic tumors <strong>and</strong> pseudotumors.<br />
A. Primarily cystic <strong>lesions</strong><br />
• Cutaneous myxoid cyst<br />
• Myxoid cyst <strong>of</strong> tendon sheath (ganglion)<br />
• Nerve sheath ganglion<br />
• Cavernous lymphangioma (cystic hygroma)<br />
• Multicystic meso<strong>the</strong>lioma<br />
• Lymphangioleiomyomatosis<br />
B. Lesions with secondary cystic or microcystic change<br />
• Fat necrosis<br />
• Membranocystic fat necrosis / membranocystic panniculitis / membranous lipodystrophy (primary idiopathic, <strong>and</strong><br />
secondary)<br />
• Nodular-cystic-encapsulated fat necrosis (“mobile encapsulated lipoma”) 141<br />
• Lipoma with fat necrosis (including membranous type)<br />
• Cystic nodular fasciitis<br />
• Myositis ossificans<br />
• Ancient schwannoma<br />
• Perineurioma<br />
• Myxolipoma<br />
• Superficial angiomyxoma & juxtarticular myxoma<br />
• Low grade fibromyxoid sarcoma & hyalinizing spindle cell tumor with giant rosettes<br />
• Ossifying fibromyxoid tumor (occasional)<br />
• Giant cell tumor <strong>of</strong> s<strong>of</strong>t tissue<br />
• Angiomatoid fibrous histiocytoma<br />
• Myx<strong>of</strong>ibrosarcoma<br />
• Myxoid leiomyosarcoma<br />
• Myxoid liposarcoma<br />
• (Extra-)gastrointestinal stromal tumor<br />
• Aggressive angiomyxoma<br />
• Ewing’s sarcoma <strong>of</strong> <strong>the</strong> skin (cystic spiradenoma-like tumor)<br />
• Synovial sarcoma<br />
C. Pseudocystic pattern<br />
• Intravenous leiomyomatosis<br />
• Necrotic sarcomas<br />
Table XIX. Acral tumors <strong>and</strong> pseudotumors.<br />
• Rudimentary supernumerary digit<br />
• Acquired digital fibrokeratoma<br />
• Infantile digital fibromatosis<br />
• Superficial acral fibromyxoma<br />
• Acral myxoinflammatory fibroblastic sarcoma<br />
• Cellular digital fibromas<br />
• Giant cell tumor <strong>of</strong> tendon sheath – localized-type<br />
• Glomus tumors<br />
• Sclerosing perineurioma<br />
• Hybrid schwannoma-perineurioma tumors 68<br />
• Calcifying aponeurotic fibroma<br />
• Chondroma<br />
• Fibroosseous pseudotumor <strong>of</strong> <strong>the</strong> digits<br />
• Lip<strong>of</strong>ibromatous hamartoma <strong>of</strong> <strong>the</strong> nerve (with or without macrodactyly) 141a<br />
• Nora’s lesion<br />
• Fibroma <strong>of</strong> tendon sheath<br />
• Fibromatosis (palmar: Dupuytren’s disease; plantar: Ledderhose’s disease; penile: Peyronie’s disease)<br />
• Congenital & infantile fibrosarcoma<br />
• Clear cell sarcoma<br />
• Epi<strong>the</strong>lioid sarcoma (conventional or “distal” type)
274<br />
M. BISCEGLIA ET AL.<br />
Table XX. Orbital tumors <strong>and</strong> pseudotumors.<br />
• Neuromuscular choristoma / hamartoma<br />
• Infantile my<strong>of</strong>ibromatosis<br />
• Periorbital granuloma annulare<br />
• Nodular fasciitis<br />
• Intravascular papillary endo<strong>the</strong>lial hyperplasia (Masson’s phenomenon)<br />
• Amputation neuroma (following enucleation)<br />
• Amyloid tumor (amyloidoma)<br />
• Inflammatory pseudotumor<br />
• Hemangioma<br />
• Benign fibrous histiocytoma<br />
• Spindle cell lipoma<br />
• Pleomorphic lipoma<br />
• Myolipoma<br />
• Peripheral nerve sheath tumors<br />
• Meningioma (lipoblastic type 142 , …)<br />
• Granular cell tumor<br />
• Giant cell angi<strong>of</strong>ibroma<br />
• Solitary fibrous tumor<br />
• Hemangiopericytoma 143<br />
• Lipomatous hemangiopericytoma (lipomatous solitary fibrous tumor) 144<br />
• Giant cell tumor (benign osteclastoma)<br />
• Synovial sarcoma<br />
• Liposarcoma<br />
• Rhabdomyosarcoma (including sclerosing variant)<br />
• Alveolar s<strong>of</strong>t part sarcoma<br />
• Mesenchymal chondrosarcoma<br />
• Granulocytic sarcoma<br />
• Leukemia / lymphoma<br />
• Metastatic tumors (sarcoma, chordoma, carcinoma, myoepi<strong>the</strong>lioma, carcinoid, …)
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 275<br />
Table XXI. Paratesticular s<strong>of</strong>t tissue tumors <strong>and</strong> pseudotumors.<br />
A. Benign tumors <strong>and</strong> pseudotumors<br />
• (Adrenal rests)<br />
• Extrarenal nephrogenic rests 145<br />
• Angiokeratoma – Fordyce-type, solitary form<br />
• Angiokeratoma – Fordyce type, multiple, iatrogenic form 146<br />
• Smooth muscle hyperplasia <strong>of</strong> testicular adnexa<br />
• Idiopatic scrotal calcinosis<br />
• Mechonium periorchitis<br />
• Sclerosing lipogranuloma<br />
• Fibromatous periorchitis / nodular periorchitis<br />
• Granulomatous lymphangitis <strong>of</strong> <strong>the</strong> scrotum <strong>and</strong> penis<br />
• Granulomatous <strong>and</strong> nongranulomatous epididymitis<br />
• Malakoplakia<br />
• Meso<strong>the</strong>lial hyperplasia<br />
• Perineal nodular induration in cyclists (3rd testicle / accessory testicle)<br />
• Fibroma <strong>of</strong> testicular tunics<br />
• Proliferative funiculitis<br />
• Fibromatosis (<strong>of</strong> spermatic cord)<br />
• Traumatic neuroma (<strong>of</strong> <strong>the</strong> penis)<br />
• Lipoma<br />
• Hibernoma<br />
• Leiomyoma – ordinary (mainly scrotal) & scrotal bizarre leiomyoma<br />
• Myointimoma (penis)<br />
• Rhabdomyoma<br />
• Hemangioma<br />
• Neur<strong>of</strong>ibroma<br />
• Fibrous hamartoma <strong>of</strong> infancy 147<br />
• Granular cell tumor<br />
• Adenomatoid tumor<br />
• Inflammatory my<strong>of</strong>ibroblastic tumor<br />
• Calcifying fibrous pseudotumor<br />
• Angiomyxolipoma<br />
• Angiomy<strong>of</strong>ibroblastoma<br />
• Angiomy<strong>of</strong>ibroblastoma-like tumor in males (analogous to vulval cellular angi<strong>of</strong>ibroma)<br />
• Aggressive angiomyxoma<br />
• Spleno-gonadal fusion<br />
• Solitary fibrous tumor (<strong>of</strong> <strong>the</strong> spermatic cord) 148<br />
B. Malignant tumors<br />
• Melanotic neuroectodermal tumor <strong>of</strong> infancy<br />
• Leiomyosarcoma (paratesticular, <strong>and</strong> penile)<br />
• Fibrosarcoma<br />
• Rhabdomyosarcoma (including <strong>the</strong> spindle cell variant <strong>of</strong> children)<br />
• Liposarcoma (mainly well differentiated)<br />
• Liposarcoma with smooth muscle differentiation)<br />
• Malignant fibrous histiocytoma<br />
• Epi<strong>the</strong>lioid sarcoma (penis)<br />
• Synovial sarcoma (perineum, penis)<br />
• Osteosarcoma (penis)<br />
• Well differentiated papillary meso<strong>the</strong>lioma <strong>of</strong> <strong>the</strong> tunica vaginalis / malignant meso<strong>the</strong>lioma <strong>of</strong> <strong>the</strong> tunica vaginalis 149<br />
• Paratesticular desmoplastic small round cell tumor
276<br />
M. BISCEGLIA ET AL.<br />
Table XXII. Vulvo-vaginal s<strong>of</strong>t tissue tumors <strong>and</strong> pseudotumors 150 .<br />
• Fibromatosis<br />
• Nodular fasciitis<br />
• Fibroepi<strong>the</strong>lial stromal polyp (bl<strong>and</strong> type; pseudosarcomatous) 50<br />
151 152<br />
• Childhood asymmetric labium majus enlargement (aka, prepubertal vulval fibroma)<br />
• Spindle cell lipoma<br />
• Pleomorphic lipoma<br />
• Cellular angi<strong>of</strong>ibroma<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans<br />
• Acquired vulvar lymphangioma (secondary to Crohn’s disease)<br />
• Vulval angiokeratoma (Fordyce type) 153<br />
• Angiomy<strong>of</strong>ibroblastoma<br />
• Angiomy<strong>of</strong>ibrosarcoma (malignant angiomy<strong>of</strong>ibroblastoma)<br />
• Superficial angiomyxoma<br />
• Aggressive angiomyxoma<br />
154 155<br />
• Post-hysterectomy Fallopian tube prolapse<br />
• Myoepi<strong>the</strong>lioma – “true” myoepi<strong>the</strong>lioma<br />
• Adenomyoepi<strong>the</strong>lioma<br />
• “True” mixed tumor <strong>of</strong> <strong>the</strong> vulva<br />
156 157<br />
• So-called “mixed tumor” <strong>of</strong> vagina (spindle cell epi<strong>the</strong>lioma)<br />
• Lipoblastoma-like tumor<br />
• Spindle cell / pleomorphic lipoma<br />
• Atypical lipomatous tumor 158<br />
• Smooth muscle tumors (any type, including <strong>the</strong> clear-cell epi<strong>the</strong>lioid leiomyoma <strong>of</strong> <strong>the</strong> round ligament 158a )<br />
• Genital rhabdomyoma<br />
• Paraganglioma 159<br />
• Perivascular epi<strong>the</strong>lioid cell neoplasms 160<br />
• Epi<strong>the</strong>lioid sarcoma<br />
• Synovial sarcoma<br />
• Extrarenal malignant rhabdoid tumor<br />
• Melanoma & malignant blue nevus<br />
• Melanoma with osteocartilaginous differentiation 161
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 277<br />
Table XXIII. Aerodigestive tract <strong>lesions</strong> (involving <strong>the</strong> orifices).<br />
A. Nasal cavity<br />
• Mycobacterial spindle cell pseudotumor 162<br />
• Amyloid tumor (amyloidoma)<br />
163 164<br />
• Nasal polyps with atypical stromal cells – a pseudosarcomatous lesion<br />
• Congenital nasal hemangiopericytoma / infantile my<strong>of</strong>ibromatosis<br />
• Nasal chondromesenchymal hamartoma in children 39<br />
• Nasal chondromesenchymal hamartoma in children <strong>and</strong> adults 130<br />
• Meningioma<br />
• Nasal glioma – so-called (nasal cerebral heterotopia or sequestered encephalocele)<br />
• Paraganglioma<br />
• Olfactory neuroblastoma<br />
• Sinonasal teratocarcinosarcoma (“mixed olfactory neuroblastoma-craniopharyngioma”) / teratocarcinosarcoma<br />
(olfactory neuroblastoma with gl<strong>and</strong>ular differentiation) 165-167<br />
• Extramedullary plasmacytoma<br />
168 169<br />
• Solitary fibrous tumor<br />
170 171<br />
• Hemangiopericytoma-like tumor (“sinonasal-type hemangiopericytoma”)<br />
• Nasopharyngeal <strong>and</strong> extranasopharyngeal 128,128a angi<strong>of</strong>ibroma<br />
• Smooth muscle tumors 172-174<br />
• Angiomyolipoma 175<br />
• Spindle cell myoepi<strong>the</strong>lioma 176<br />
• Undifferentiated small cell tumor 177<br />
• Alveolar rhabdomyosarcoma (paranasal sinuses)<br />
• Synovial sarcoma<br />
• Malignant melanoma<br />
B. Oral cavity<br />
• Rhabdomyomatous mesenchymal hamartoma 178<br />
• Fibrous hamartoma <strong>of</strong> infancy 179<br />
• Congenital granular cell epulis<br />
• Amyloid tumor (amyloidoma)<br />
• Neuroma<br />
• Schwannoma<br />
• Granular cell tumor<br />
• Rhabdomyoma<br />
• Multifocal rhabdomyoma 180<br />
• Ectomesenchymal chondromyxoid tumor <strong>of</strong> <strong>the</strong> tongue<br />
• Myoepi<strong>the</strong>lioma<br />
• Fibrolipoma<br />
• Ordinary lipoma<br />
• Spindle cell lipoma 181<br />
• Pleomorphic hyalinizing angiectactic tumor 182<br />
• Peripheral myxoma 183<br />
184 185<br />
• Solitary fibrous tumor<br />
• Congenital hemangiopericytoma / infantile my<strong>of</strong>ibromatosis<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma 186<br />
• Leiomyosarcoma<br />
• Liposarcoma<br />
• Embryonal rhabdomyosarcoma<br />
• Malignant fibrous histiocytoma<br />
• Clear cell sarcoma 187<br />
• Lingual alveolar s<strong>of</strong>t part sarcoma 188<br />
• Low-grade malignant Triton tumor 189<br />
• Synovial sarcoma 180<br />
• Ordinary melanoma<br />
• Melanoma with osteocartilaginous differentiation 161<br />
C. Anal canal*<br />
• CD34+ fibroepi<strong>the</strong>lial polyp 191<br />
• Aggressive angiomyxoma<br />
• Schwannoma & neur<strong>of</strong>ibroma<br />
• Leiomyoma 192<br />
• Leiomyosarcoma 192<br />
192a, 192b<br />
• Gastrointestinal stromal tumor
278<br />
M. BISCEGLIA ET AL.<br />
Table XXIV. Intranodal primary tumors & pseudotumors (o<strong>the</strong>r than hematolymphoid).<br />
• Nodular fasciitis (<strong>of</strong> <strong>the</strong> capsule)<br />
• Amyloid tumor<br />
• Deciduosis<br />
• Lipomatosis<br />
• Angiomyolipoma<br />
• Lymphangioleiomyomatosis<br />
• Inflammatory pseudotumor<br />
• Mycobacterial spindle cell pseudotumor<br />
• Bacillary angiomatosis<br />
• Rosai-Dorfman disease<br />
• Castleman’s disease (hyaline-vascular type)-related tumors (follicular dendritic cell tumor, Kaposi’s sarcoma)<br />
<strong>and</strong> pseudotumors (angiolipomatous hamartoma)<br />
• Angiomyomatous hamartoma<br />
• Lymphangioma<br />
• Angiolymphatic angiodysplasia<br />
• Vascular transformation <strong>of</strong> sinuses<br />
• Nodular spindle-cell vascular transformation <strong>of</strong> lymph nodes 193<br />
• Nodal angioma (common type – capillary, cavernous, lobular, cellular)<br />
• Epi<strong>the</strong>lioid hemangioma<br />
• Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
• Spindle <strong>and</strong> epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
• Polymorphous hemangioendo<strong>the</strong>lioma<br />
• Angiosarcoma<br />
• Kaposi’s sarcoma<br />
• Leiomyoma<br />
• Palisaded my<strong>of</strong>ibroblastoma<br />
• Plexiform neur<strong>of</strong>ibroma<br />
• Myelolipoma
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 279<br />
Table XXV. Mammary stroma spindle cell tumors <strong>and</strong> tumor-like <strong>lesions</strong>.<br />
A. Monomorphic spindle cell tumors <strong>and</strong> tumor-like <strong>lesions</strong> <strong>of</strong> specialized mammary stroma 194-196<br />
• Pseudoangiomatous stromal hyperplasia<br />
• Benign spindle cell tumor, NOS<br />
• Spindle cell lipoma-like tumor<br />
• Solitary fibrous tumor<br />
• My<strong>of</strong>ibroblastoma<br />
• Combined spindle cell tumor (two <strong>of</strong> <strong>the</strong> above: e.g., my<strong>of</strong>ibroblastoma plus solitary fibrous tumor areas<br />
or spindle cell lipoma-like areas)<br />
• Periductal stromal tumor<br />
• Stromal sarcoma<br />
B. Monomorphic spindle cell tumors <strong>and</strong> tumor-like <strong>lesions</strong> <strong>of</strong> non-specialized mammary stroma<br />
• Nodular fasciitis<br />
• Lipoma<br />
• Muscular hamartoma<br />
• Benign fibrous histiocytoma<br />
• Fibromatosis<br />
• Leiomyoma<br />
• Inflammatory my<strong>of</strong>ibroblastic tumor (benign, low-grade)<br />
• Spindle cell adult type juvenile xanthogranuloma 197<br />
• Angiomyolipoma<br />
• Fibrosarcoma<br />
• My<strong>of</strong>ibrosarcoma<br />
• Leiomyosarcoma<br />
• Peripheral nerve sheath tumor (benign <strong>and</strong> malignant)<br />
• Monophasic fibrous synovial sarcoma<br />
• Hemangiopericytoma<br />
• Mammary NOS-type sarcoma with CD10 expression <strong>and</strong> features <strong>of</strong> myoepi<strong>the</strong>lial differentiation 198<br />
C. Spindle cell myoepi<strong>the</strong>lioma<br />
• Myoepi<strong>the</strong>lioma<br />
D. Spindle cell epi<strong>the</strong>lial tumors<br />
• Metaplastic carcinoma – biphasic <strong>and</strong> monophasic 199<br />
• Monophasic low-grade spindle cell fibromatosis-like carcinoma 122, 199 )<br />
• Monophasic high-grade spindle cell (sarcomatoid) carcinoma (including a subset showing myoepi<strong>the</strong>lial<br />
differentiation) 199a
280<br />
M. BISCEGLIA ET AL.<br />
Table XXVI. Infantile-juvenile tumors <strong>and</strong> pseudotumors.<br />
A. Hamartomas – Developmental <strong>lesions</strong><br />
• Connective tissue nevi<br />
• Palmar cutaneous hamartoma<br />
• Nevus lipomatosus superficialis<br />
• Cutaneous neural heterotopia<br />
• Cutaneous ganglion cell choristoma<br />
• Hamartomatous neuroma combined with heterotopic ganglion cells<br />
• Congenital neural hamartoma (“fascicular schwannoma”)<br />
• Multiple cutaneous neuromuscular choristomas<br />
• Pleomorphic neuromuscular hamartoma <strong>of</strong> <strong>the</strong> subcutis (superficial equivalent <strong>of</strong> deep neuromuscular hamartoma<br />
or benign Triton tumor)<br />
• Congenital neurovascular hamartoma <strong>of</strong> <strong>the</strong> skin<br />
• Fibrous hamartoma <strong>of</strong> infancy<br />
• Congenital smooth muscle hamartoma <strong>of</strong> <strong>the</strong> skin<br />
• Genital smooth muscle hamartoma<br />
• Rhabdomyomatous mesenchymal hamartoma<br />
• Striated muscle hamartoma<br />
• Neuromuscular hamartoma / choristoma (benign Triton tumor)<br />
• Neural fibrolipomatous hamartoma<br />
• Ectopic meningo<strong>the</strong>lial hamartoma <strong>of</strong> <strong>the</strong> scalp<br />
• Sequestrated (rudimentary) meningocele<br />
• Sacro-coccygeal (“myxopapillary”) ependymal rests<br />
• Meningo-glial nodule <strong>of</strong> <strong>the</strong> buttock<br />
• S<strong>of</strong>t tissue gliomatosis in a non-midline location<br />
• Neurocristic cutaneous hamartoma<br />
39 130<br />
• Nasal chondromesenchymal hamartoma<br />
• Mesenchymal hamartoma <strong>of</strong> <strong>the</strong> chest wall 40<br />
• Lipomatous <strong>and</strong> angiomatous lesion associated with occult spinal dysraphism<br />
B. Benign tumors <strong>and</strong> pseudotumors<br />
• Granular (gingival) cell tumor<br />
• Hemangioma<br />
• Lymphangioma<br />
• Infantile fibromatosis, diffuse <strong>and</strong> desmoid type<br />
• Infantile digital fibromatosis<br />
• Infantile my<strong>of</strong>ibromatosis<br />
• Infantile hemangiopericytoma<br />
• Juvenile hyaline fibromatosis 22 / infantile systemic hyalinosis / <strong>and</strong> Winchester syndrome<br />
• Proliferative fasciitis<br />
• Proliferative myositis<br />
• Cranial fasciitis<br />
• Fibrous umbilical polyp (fasciitis-like proliferation <strong>of</strong> infancy) 200<br />
• Umbilical pseudotumors (keloid/hypertrophic scar, umbilical polyp/granuloma with urachal, omphalomesenteric, or<br />
o<strong>the</strong>r remnants)<br />
• Lipoblastoma / lipoblastomatosis<br />
• Lip<strong>of</strong>ibromatosis<br />
• Myositis ossificans progressiva (fibrodysplasia)<br />
• Benign <strong>and</strong> atypical fibrous histiocytoma<br />
• Giant cell fibroblastoma<br />
• Juvenile xanthogranuloma<br />
• Fetal rhabdomyoma<br />
• Fetal rhabdomyoma, cellular-type<br />
• Juvenile rhabdomyoma<br />
• Cellular capillary hemangioma<br />
• Intramuscular hemangioma<br />
• Kaposi-like infantile hemangioendo<strong>the</strong>lioma<br />
• Spindle cell hemangioendo<strong>the</strong>lioma<br />
• Congenital or infantile hemangiopericytoma<br />
• Congenital giant cell angioblastoma<br />
• Nasopharyngeal <strong>and</strong> extra-nasopharyngeal angi<strong>of</strong>ibroma 171a, b<br />
• Congenital <strong>and</strong> childhood plexiform (multinodular) cellular schwannoma 110
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 281<br />
C. Intermediate <strong>and</strong> malignant tumors<br />
• Congenital my<strong>of</strong>ibromatosis (visceral involvement)<br />
• Congenital (infantile) fibrosarcoma<br />
• Kaposi’s sarcoma (HIV-negative, peripartum HHV-8 infection)<br />
• Lymphangioendo<strong>the</strong>liomatosis<br />
• Primitive myxoid mesenchymal tumor 200a<br />
• Pigmented (melanotic) neuroectodermal tumor <strong>of</strong> infancy<br />
(maxilla, m<strong>and</strong>ible, mediastinum, skull, epididymis, s<strong>of</strong>t tissue <strong>of</strong> extremities)<br />
• Inflammatory pseudotumor – Inflammatory my<strong>of</strong>ibroblastic tumor<br />
• Plexiform fibrohistiocytic tumor<br />
• Pediatric dermat<strong>of</strong>ibrosarcoma protuberans (rare; occasionally congenital)<br />
• Pediatric pigmented dermat<strong>of</strong>ibrosarcoma protuberans 200b<br />
• Pediatric leiomyosarcoma<br />
• Endovascular papillary angioendo<strong>the</strong>lioma (Dabska’s tumor)<br />
• Ewing’s sarcoma<br />
• Congenital Ewing’s sarcoma<br />
• Primitive neuroectodermal tumor<br />
• Rhabdomyosarcoma (embryonal, alveolar; rarely congenital)<br />
• Infantile rhabdomy<strong>of</strong>ibrosarcoma<br />
• Synovial sarcoma (even congenital)<br />
• Congenital angiomatoid malignant fibrous histiocytoma<br />
• Congenital synovial sarcoma<br />
• Congenital extraskeletal embryonal chondrosarcoma<br />
• Alveolar s<strong>of</strong>t part sarcoma<br />
• Extrarenal malignant rhabdoid tumor<br />
• Congenital disseminated extrarenal malignant rhabdoid tumor<br />
• Angiomatoid (malignant) fibrous histiocytoma<br />
• Pediatric leiomyosarcoma <strong>of</strong> s<strong>of</strong>t tissue (rare)<br />
• Pediatric epi<strong>the</strong>lioid sarcoma (rare) 201<br />
• Pediatric malignant peripheral nerve sheath tumor (rare) 202<br />
• Pediatric malignant vascular tumors 203<br />
• Liposarcoma (exceptional)<br />
• Pediatric clear cell sarcoma (<strong>of</strong> tendons <strong>and</strong> aponeurosis) 204<br />
• Primitive undifferentiated sarcoma<br />
• Congenital leukemia cutis<br />
• Cutaneous neonatal neuroblastoma<br />
• S<strong>of</strong>t tissue sarcoma as a second malignant neoplasm 205
282<br />
M. BISCEGLIA ET AL.<br />
Table XXVII. Lesions as sentinel <strong>of</strong> clinical entities (see also Table XXVIII).<br />
• Keloid (acne vulgaris; ear-piercing; previous surgical intervention or <strong>the</strong>rmal injuries)<br />
• Membranocystic fat necrosis / membranocystic panniculitis / membranous lipodystrophy (secondary form -<br />
mainly lower leg venous insufficiency in obese women, ery<strong>the</strong>ma nodosum, morphea pr<strong>of</strong>unda,<br />
lupus panniculitis, dermatomyositis, subcutaneous T-cell lymphoma, factitial ulcer, … o<strong>the</strong>rs)<br />
• Nodular panniculitis (Weber-Christian disease; alpha-1-antitrypsin-deficiency; Rothmann-Makai panniculitis;<br />
pancreatic disease)<br />
• Massive localized lymphedema (morbid obesity)<br />
• Polyvinylpyrrolidone granuloma (polymer used as plasma exp<strong>and</strong>er in a previous surgical intervention or as<br />
vehicle for intravenous medications)<br />
• Pseudosclerodermatous panniculitis <strong>of</strong> <strong>the</strong> breast (previous radiation <strong>the</strong>rapy for breast cancer) 206<br />
• Pseudolipoma (“battered buttock syndrome”)<br />
• Folded skin with lipomatous nevus (“Michelin-tire baby”)<br />
• Multiple nevus lipomatous cutaneous superficialis (H<strong>of</strong>fman-Zurhelle disease)<br />
• Granular histiocytic granuloma (local previous site <strong>of</strong> surgery)<br />
• Scleredema (maturity-onset diabetes mellitus)<br />
• Xanthogranulomatous pseudotumor (Erdheim-Chester disease)<br />
• Superficial fibromatoses (association <strong>of</strong> palmar with plantar <strong>and</strong>/or penile forms)<br />
• Multiple desmoids tumors (familial infiltrative fibromatosis)<br />
• My<strong>of</strong>ibroma (my<strong>of</strong>ibromatosis – bone, <strong>and</strong> visceral organ involvement; possible familial occurrence)<br />
• Kimura’s disease (minimal change/membranous glomerulopathy nephrotic syndrome; peripheral blood<br />
eosinophilia; elevated serum IgE)<br />
• Paraffinoma – oleogranuloma (cosmetic purposes [breast <strong>of</strong> females, breast <strong>of</strong> transsexual males, eyelids, lips, male<br />
genitalia – scrotum, penis]; pseudo<strong>the</strong>rapeutic <strong>and</strong> <strong>the</strong>rapeutic procedures (scalp [for baldness], sinonasal surgery<br />
<strong>and</strong> medication, intralesional injection <strong>of</strong> oil based chemo<strong>the</strong>rapeutic agents)<br />
• Gingival pyogenic granuloma (granuloma gravidarum) (pregnancy)<br />
• S<strong>of</strong>t tissue <strong>and</strong> cutaneous deciduosis (pregnancy; occasionally in non-pregnant women) 207<br />
• Leiomyomatosis peritonealis disseminata (excess exogenous or endogenous sex steroids, pregnancy, endometriosis)<br />
• Extramedullary hematopoiesis (anemia <strong>of</strong> various origin, chronic myeloproliferative disorders)<br />
• Extramedullary myeloid tumor (acute or chronic myelogenous leukemia)<br />
• Sclerosing extramedullary hematopoietic tumor (chronic myeloproliferative disorders)<br />
• Extramedullary plasmacytoma (full-blown multiple myeloma)<br />
• Cytophagic histiocytic panniculitis (subcutaneous T-cell lymphoma)<br />
• Angiosarcoma (preexisting lymphedema, previous local irradiation 208 , local lymphedema, …)<br />
• Atypical vascular lesion <strong>of</strong> skin <strong>of</strong> <strong>the</strong> breast (previous irradiation)<br />
• Mucosal, lymph nodal <strong>and</strong>/or visceral Kaposi’s sarcoma (immunosuppression, AIDS)<br />
• Verruga peruana / bacillary angiomatosis (Carrion disease / AIDS)<br />
• Acquired progressive lymphangioma (irradiation, trauma, …)<br />
• Epi<strong>the</strong>lioid hemangioma (multicentricity)<br />
• Multicentric reticulohistiocytosis (paraneoplastic disease)<br />
• Xanthoma – various types (e.g. tendinous xanthoma: disorders <strong>of</strong> lipid metabolism)<br />
• Plexiform xanthomatous tumor (hyperlipidemia)<br />
• Calcinosis circumscripta <strong>and</strong> calcinosis universalis (scleroderma, dermatomyositis, Raynaud disease,<br />
hyperparathyroidism,…)<br />
• Ectopic calcifications (hypercalcemia-associated conditions: milk-alkali-syndrome or Burnett syndrome,<br />
hypervitaminosis D, tumoral bone metastases) <strong>and</strong> calciphylaxis 209 (associated with secondary hyperparathyroidism<br />
/ chronic renal failure)<br />
• (Idiopathic) tumoral calcinosis (unassociated with hypercalcemia: sometimes hyperphosphatemia-associated;<br />
sometimes familial)<br />
• (Secondary) tumoral calcinosis-like lesion (associated with chronic renal failure <strong>and</strong> secondary hyperparathyroidism) 210<br />
• S<strong>of</strong>t tissue calcifications <strong>and</strong> osteomas (Albright hereditary osteodystrophy)<br />
• Cutaneous <strong>and</strong> subcutaneous myxoma (Carney's complex)<br />
• Pretibial myxedema (hyperthyroidism)<br />
• Dermat<strong>of</strong>ibrosarcoma protuberans (familial form)<br />
• Multiple lipomas (familial form)<br />
• Multiple spindle cell lipomas (familial form)<br />
• Multiple angiolipomas (familial form)<br />
• Symmetric lipomatosis <strong>of</strong> <strong>the</strong> head <strong>and</strong> neck (Madelung disease or Launois-Bensaude syndrome)<br />
• Asymmetrical lipomatosis with “buffalo hump” (steroid lipomatosis - Cushing's disease)<br />
• Asymmetrical lipomatosis with wasting face <strong>and</strong> limbs (iatrogenic HIV lipodystrophy)
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 283<br />
• Pelvic lipomatosis (mostly affecting blacks)<br />
• Adiposis dolorosa (Dercum's disease)<br />
• Multiple scwhannoma (schwannomatosis) 109b-d<br />
• Multiple cutaneous chondromas (familial form)<br />
211 212<br />
• Amyloid tumor (plasma cell dyscrasia; chronic inflammatory/autoimmune diseases; chronic hemodyalisis; o<strong>the</strong>rs)<br />
• Pseudoneoplastic parathyromatosis following iatrogenic implantation (hyperparathyroidism)<br />
• Phosphaturic mesenchymal tumor (oncogenic osteomalacia/rickets)<br />
• Idiopathic retroperitoneal fibrosis – Ormond’s disease (association with o<strong>the</strong>r fibrosclerotic disorders, e.g. Riedel<br />
thyroiditis, primary sclerosing cholangitis, sclerosing mediastinitis, inflammatory pseudotumor <strong>of</strong> <strong>the</strong> orbit,<br />
autoimmune pancreatitis)<br />
47 48<br />
• Tamm-Horsfall protein deposition / “retroperitoneal urinary precipitates” (past urine extravasation)<br />
• Hemangiopericytoma & solitary fibrous tumor (hypoglycemia) 213<br />
• (Retroperitoneal) extrarenal juxtaglomerular cell tumor (secondary hyperaldosteronism – hypertension,<br />
hypokalemia)<br />
• Angiomyolipoma & lymphangioleioleiomyomatosis (tuberous sclerosis complex)<br />
• Malignant Triton tumor <strong>and</strong> epi<strong>the</strong>lioid malignant peripheral nerve sheath tumor (neur<strong>of</strong>ibromatosis I)<br />
• Paragangliomas (both head <strong>and</strong> neck <strong>and</strong> retroperitoneal) – ei<strong>the</strong>r alone (PGL1, PGL2, PGL3, PGL4 syndromes) or as<br />
a component <strong>of</strong> a multiple tumor syndrome (von Hippel-Lindau disease, neur<strong>of</strong>ibromatosis type 1, MEN-2b,<br />
Carney's triad, Carney' <strong>and</strong> Stratakis' syndrome 214 or in association with gastrointestinal stromal tumor 214a )<br />
• Gastrointestinal stromal tumor (familial form, <strong>and</strong> syndromic form in association with lentigines <strong>and</strong> mast cell<br />
tumors) 192b<br />
• Multifocal (EBV-associated) smooth muscle tumors (post-transplantation 215 ; congenital immunodeficiencies)<br />
• Multifocal visceral smooth muscle tumors (immunocompromised HIV-patients)<br />
• Myxoid embolus (cardiac myxoma)<br />
• Sarcomatous embolus (great vessel sarcoma) 216
284<br />
M. BISCEGLIA ET AL.<br />
Table XXVIII. Lesions as sentinel <strong>of</strong> clinical syndromes (see also Table XXVII).<br />
• Angi<strong>of</strong>ibroma <strong>of</strong> <strong>the</strong> face (tuberous sclerosis complex)<br />
• Periungual, subungual, <strong>and</strong> gingival angi<strong>of</strong>ibroma (tuberous sclerosis complex; Gardner syndrome)<br />
• Fibr<strong>of</strong>olliculoma (Birt-Hogg-Dube syndrome) 217<br />
• Fibrous papule <strong>of</strong> <strong>the</strong> face (multiple hamartoma syndrome; Cowden’s syndrome)<br />
• Cutaneous myxoma (mainly <strong>of</strong> external ear location) (LAMB / NAME / Carney’s complex)<br />
• Gardner-associated fibroma (Gardner syndrome; familial infiltrative fibromatosis; desmoid fibromatosis)<br />
• Nuchal-type fibroma (diabetes mellitus; Gardner syndrome)<br />
• Desmoid tumor (familial adenomatous polyposis / Gardner syndrome)<br />
• Nasopharyngeal angi<strong>of</strong>ibroma (familial adenomatous polyposis / Gardner syndrome)<br />
• Keloids (Rubinstein-Taybi syndrome; Ehlers-Danlos syndrome)<br />
• Gingival fibromatosis (Zimmermen-Lab<strong>and</strong> syndrome; Ramon syndrome; Klippel-Trenaunay syndrome; Cowden’s<br />
syndrome; prune-belly syndrome)<br />
• Juvenile hyaline fibromatosis <strong>and</strong> infantile systemic hyalinosis (Winchester syndrome)<br />
• Gingival fibromatosis with juvenile hyaline fibromatosis (Murray-Puretic-Drescher syndrome)<br />
• Penile fibromatosis (Cogan syndrome)<br />
• Cerebriform superficial s<strong>of</strong>t tissue fibrous proliferation (Proteus syndrome)<br />
• Multiple lipomas (Proteus syndrome)<br />
• Multiple intramuscular myxoma plus polyostotic fibrous dysplasia (Mazabraud’s syndrome)<br />
• Lymphangioma (Turner syndrome)<br />
• Lipomas <strong>and</strong> hemangiomas (Bannayan-Ruvalcaba-Riley syndrome; Cowden syndrome)<br />
• Multiple lipoma (Bannayan-Zonana syndrome; Frohlich syndrome; Proteus syndrome)<br />
• Kaposiform hemangioendo<strong>the</strong>lioma (Kasabach-Merritt syndrome)<br />
• (Large) cavernous hemangioma (Kasabach-Merritt syndrome)<br />
• Cutaneous <strong>and</strong> gastrointestinal venous malformations (blue rubber bleb nevus syndrome)<br />
• Embryonal rhabdomyosarcomas (Beckwith-Wiedemann syndrome / Exomphalos-macroglossa-gigantism<br />
syndrome)<br />
• S<strong>of</strong>t tissue sarcomas (retinoblastoma syndrome)<br />
• S<strong>of</strong>t tissue sarcomas (Werner syndrome)<br />
• Myogenic sarcomas (Rubinstein-Taybi syndrome)<br />
• Pedal hemangioma (Turner syndrome)<br />
• Hemangiomatosis (Klippel-Trenaunay syndrome)<br />
• Angiomatous <strong>lesions</strong> (Sturge-Weber syndrome; Klippel-Trenaunay syndrome; Parkes-Weber syndrome;<br />
Rendu-Osler-Weber disease)<br />
• Multiple hemangiomas <strong>and</strong> chondromas (Maffucci’s syndrome)<br />
• Spindle cell hemangioma (Maffucci’s syndrome – occasional)<br />
• Angiosarcoma, chondrosarcoma (Maffucci’s syndrome)<br />
• Multiple glomus tumors <strong>and</strong>/or multiple glomus body hamartomas (congenital, familial)<br />
• Glomeruloid hemangioma (POEMS / Crowe-Fukase / PEP / Takatsuki syndrome)<br />
• Hemangioblastoma <strong>of</strong> s<strong>of</strong>t tissue (von Hippel-Lindau syndrome)<br />
• Lymphangioleomyomatosis / s<strong>of</strong>t tissue PEC-oma (tuberous sclerosis complex)<br />
• Major <strong>and</strong>/or minor (2 or more) features <strong>of</strong> tuberous sclerosis complex plus autosomal dominant polycystic<br />
kidney disease (adjacent gene syndrome TSC2/ADPKD1 217a )<br />
• Lymphangiosarcoma (Stewart-Treves syndrome) 218<br />
• Mucosal neuromas (hypertrophied corneal nerves, bumpy lips, nodular tongue in MEN-2b)<br />
• Plexiform neur<strong>of</strong>ibroma <strong>and</strong> multiple neur<strong>of</strong>ibromas (neur<strong>of</strong>ibromatosis type I) 218a<br />
• Bilateral acoustic schwannoma (neur<strong>of</strong>ibromatosis type II)<br />
• Calcinosis circumscripta <strong>and</strong> calcinosis universalis (CREST syndrome; or Thibierge-Weissenbach syndrome [calcinosis,<br />
Raynaud's phenomenon, eophageal dysfunction, sclerodactyly, <strong>and</strong> telangiectasia]; milk-alkali syndrome [Burnett<br />
syndrome]; abnormalities <strong>of</strong> calcium <strong>and</strong> phosphate metabolism)<br />
• Psammomatous melanotic schwannoma (Carney’s complex)<br />
219 220<br />
• Fetal rhabdomyoma (nevoid basal-cell carcinoma syndrome – Gorlin-Goltz syndrome)<br />
219 220<br />
• Ectopic calcifications (nevoid basal-cell carcinoma syndrome – Gorlin-Goltz syndrome)<br />
• Intraabdominal (mesenteric) <strong>and</strong> extrabdominal fibromatosis (Gardner syndrome)<br />
• Idiopathic retroperitoneal fibrosis – Ormond’s syndrome (immune-mediated connective tissue disease complex:<br />
see above at Table 27)<br />
• Malignant peripheral nerve sheath tumors (neur<strong>of</strong>ibromatosis type 1)<br />
• Rhabdomyosarcoma (Costello syndrome)<br />
• Rhabdomyosarcoma, perianal (Nijmegen breakage syndrome)<br />
• Malignant rhabdoid tumor (rhabdoid tumor predisposition syndrome) 221<br />
• Multiple sarcomas (e.g. rhabdomyosarcoma) (Li-Fraumeni syndrome <strong>and</strong> Li-Fraumeni-like syndrome) 222
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 285<br />
Table XXIX. Embryological rests or normal anatomic structures potentially mistaken<br />
for tumors.<br />
A. Normal embryological rests in s<strong>of</strong>t tissue<br />
• Branchial arch-derivatives (may mimic s<strong>of</strong>t tissue chondroma)<br />
• Branchial pouch-derivatives (may mimic metastatic carcinoma, …)<br />
• Supernumerary breast<br />
• Lumbosacral ectopic nephrogenic rest 223 224 (may mimic metastatic or ectopic Wilms’ tumor, monodermal<br />
teratoma, …) associated <strong>and</strong> unassociated with spinal dysraphism<br />
• Sacrococcygeal ependymal rests (resembles ependymal tumors, metastatic papillary carcinoma, …)<br />
• Odontogenic epi<strong>the</strong>lial rests<br />
B. Normal anatomic structures in appropriate locations<br />
• (Dental papilla [resembling myxoma])<br />
• Accessory tragus-elastic cartilage (resembling chondroma)<br />
• Glomus coccygeum (resembling glomus tumor)<br />
225 226<br />
• Organ <strong>of</strong> Zuckerk<strong>and</strong>l hypertrophy (resembling paraganglioma)<br />
227 228<br />
• Carotid body hyperplasia (resembling paraganglioma)<br />
• Chiewitz organ (resembling metastatic carcinoma) 229-231<br />
• Pacinian corpuscle hyperplasia (resembling Pacinian neuroma / Pacinian neur<strong>of</strong>ibroma - Pacinian perineurioma /<br />
onion-bulb neuropathies) 232-233<br />
C. Normal anatomic structures in inappropriate locations<br />
• Dermal thymus (brachio-oculo-facial syndrome) (may mimic thymoma) 234<br />
• Glial heterotopia (may mimic glioma)<br />
• Hamartoma <strong>of</strong> <strong>the</strong> scalp with ectopic meningo<strong>the</strong>lial elements / rudimentary meningocele (may mimic<br />
various neoplasms, e.g. angiosarcoma, meningioma, …)<br />
• Extramedullary hemopoiesis in normal organs (s<strong>of</strong>t tissue, breast, lymph node, brain, …) (may mimic lympho- or<br />
myelo-proliferative processes)<br />
• Extramedullary hemopoiesis in vascular tumors (hemangioblastoma, spindle cell lipoma, pyogenic granuloma,...)<br />
(may mimic lymphoid or myeloid leukemia)<br />
• Subcutaneous splenosis (resembles hematologic proliferations)<br />
• Langerhans’ cell islets in adipose peripancreatic tissue (resembles metastatic carcinoid)<br />
• Discontinuous splenogonadal fusion<br />
• Any o<strong>the</strong>r adult tissue ectopically located in s<strong>of</strong>t tissue (e.g. post-traumatic splenosis in <strong>the</strong> abdomen,<br />
autografted parathyroid in <strong>the</strong> forearm 11/ix-5 , …)
286<br />
M. BISCEGLIA ET AL.<br />
Table XXX. Categorization i-iv <strong>of</strong> s<strong>of</strong>t tissue tumors <strong>and</strong> its relevance to management.<br />
i<br />
ii<br />
iii<br />
iv<br />
Pathologic categorization is defined on <strong>the</strong> basis <strong>of</strong> <strong>the</strong> clinical behaviour <strong>of</strong> each entity.<br />
This clinically-based categorization <strong>of</strong> s<strong>of</strong>t tissue tumors broadly corresponds to that found in specialized st<strong>and</strong>ard<br />
textbooks 235-237 <strong>and</strong> major or specific publications.<br />
The range <strong>of</strong> metastatic rates given within each category/group is an approximation gauged from <strong>the</strong> literature <strong>and</strong> from<br />
<strong>the</strong> authors’ experience, <strong>and</strong> – although it reflects <strong>the</strong> basis for <strong>the</strong> categorization – should be interpreted as approximate<br />
guide only.<br />
Sarcomas are stratified according to a 3-tiered prognostic scheme, intended as a “working formulation” <strong>and</strong> not as a grading<br />
system along <strong>the</strong> lines <strong>of</strong> existing traditional grading schemes such as FNCLCC (see below). This stratification conveys notable<br />
differences in metastatic rate.<br />
• Category I. Clinically benign tumors<br />
Metastatic rate <strong>of</strong> nearly 0%. Local excision is usually curative<br />
Dermat<strong>of</strong>ibroma (including variants – clear cell, epi<strong>the</strong>lioid, sclerosing, myxoid, keloidal, palisading, lipidized, …) & cutaneous benign<br />
fibrous histiocytoma^, fibroma (including variants – sclerotic, pleomorphic, nuchal-type, Gardner-associated type, …), fibroma<br />
<strong>of</strong> tendon sheath, giant cell tumor <strong>of</strong> tendon sheath (localized-type), superficial fibromatosis (prone to recurrence) °, deep<br />
fibromatosis/desmoids tumor (prone to recurrence) °, nasopharyngeal angi<strong>of</strong>ibroma (prone to recurrence)°, desmoplastic fibroblastoma<br />
(collagenous fibroma), mammary-type fibroblastoma, giant cell fibroblastoma (may recur), intranodal palisaded<br />
my<strong>of</strong>ibroblastoma, dermatomy<strong>of</strong>ibroma, my<strong>of</strong>ibroma adult-type, my<strong>of</strong>ibromatosis infantile-type (“infantile hemangiopericytoma”),<br />
intramuscular myxoma (including <strong>the</strong> cellular variant), calcifying fibrous pseudotumor, calcifying aponeurotic fibroma<br />
(prone to recurrence), juxtaarticular myxoma, cutaneous myxoma, superficial angiomyxoma with <strong>and</strong> without epi<strong>the</strong>lial elements<br />
(prone to recurrence) 238 , “aggressive” angiomyxoma <strong>of</strong> <strong>the</strong> pelvis (prone to recurrence) + , vulvovaginal <strong>and</strong> inguinoscrotal<br />
angiomy<strong>of</strong>ibroblastoma § , nasopharyngeal angi<strong>of</strong>ibroma (prone to recurrence; locally aggressive), vulval cellular angi<strong>of</strong>ibroma<br />
(<strong>and</strong> its analogous counterpart “angiomy<strong>of</strong>ibroblastoma-like tumor” in males), localized tenosynovial giant cell tumor,<br />
cutaneous leiomyomas (pilar-type, vascular-type, genital-type) <strong>and</strong> variants (atypical/symplastic, pleomorphic, clear cell, granular<br />
cells, …), leiomyoma <strong>of</strong> deep s<strong>of</strong>t tissue 242 243 , myointimoma (little experience), rhabdomyoma (including variants – fetal type, oncocytic,<br />
genital, …), “usual” glomus tumor (including some variants – glomangioma, glomangiomyoma, glomangiomatosis; intravascular;<br />
oncocytic, …, but excluding “unusual” glomus tumors: see at borderline <strong>and</strong> malignant groups), myopericytoma∞,<br />
glomangiopericytoma, lipoma (including variants: multiple, deep-seated, pleomorphic, spindle cell, fibrohistiocytic, chondroid,<br />
…), lipoblastoma, lip<strong>of</strong>ibromatosis (may recur), hibernoma, myolipoma, angiolipoma (including <strong>the</strong> cellular variant), fibrolipoma,<br />
dendritic fibromyxolipoma, angiomyxolipoma, endo<strong>the</strong>lial neoplasms (capillary hemangioma <strong>and</strong> variants, cavernous hemangioma,<br />
hobnail hemangioma, acquired elastotic hemangioma, epi<strong>the</strong>lioid hemangioma, glomeruloid hemangioma, spindle cell<br />
hemangioma, Kaposiform hemangioendo<strong>the</strong>lioma; angiomatosis; lymphangioma; acquired progressive lymphangioma – benign<br />
lymphangioendo<strong>the</strong>lioma, lymphangiomatosis) 245 246 , s<strong>of</strong>t tissue hemangioblastoma (little experience so far), ordinary schwannoma<br />
(including variants – epi<strong>the</strong>lioid, pseudogl<strong>and</strong>ular, pigmented, neuroblastoma-like, ancient, lipomatous, sclerosing, …, but<br />
excluding <strong>the</strong> psammomatous melanotic type), cellular schwannoma (may recur, does not metastasize) ° 115 247 , neur<strong>of</strong>ibroma<br />
(including typical variants – diffuse, plexiform, dendritic cell, pigmented, sclerosing, lipomatous, …; cellular <strong>and</strong>/or atypical variants<br />
may recur) °, s<strong>of</strong>t tissue perineurioma (7/V-5, 248) (including typical variants – intraneurial, myxoid, reticular, Pacinian, sclerosing,<br />
…- <strong>and</strong> atypical forms ⊃ ), hybrid or composite nerve sheath tumors (neur<strong>of</strong>ibroma/schwannoma, neur<strong>of</strong>ibroma/perineurioma,<br />
schwannoma/perineurioma), usual granular cell tumor (Abrikoss<strong>of</strong> tumor), benign Triton tumor, ganglioneuroma° <strong>and</strong> ganglion<br />
cell tumor, neuro<strong>the</strong>keoma (myxoid-type, cellular-type), s<strong>of</strong>t tissue chondroma, fibrochondroma, myxochondroma, osteoma,<br />
<strong>and</strong> osteochondroma (including variants – multiple, familial), extraarticular synovial chondromatosis, s<strong>of</strong>t tissue oncocytoma<br />
(little experience), hyaline cell-rich chondroid syringoma, ectopic hamartomatous thymoma √ , myelolipoma.<br />
^ Some variants – atypical, cellular, aneurysmal, deepseated – may recur <strong>and</strong> anecdotal metastatic cases 135 are also on record. ° May undergo malignant<br />
change. + 2 metastasizing cases on record 239 240 . § 1 case <strong>of</strong> malignant transformation 241 . ∞ Malignant myopericytomas are also on record 244 .<br />
⊃<br />
Malignant perineuriomas likely correspond to malignant peripheral nerve sheath tumors with perineurial differentiation 249-251 . √ 1 case <strong>of</strong> malignant<br />
transformation 252 .<br />
Note: tumors “prone to recurrence” might be also placed in Group II (see footnote <strong>the</strong>re).
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 287<br />
• Category II. Clinically intermediate !!! (borderline) tumors<br />
Metastasis can rarely occur: metastatic rate <strong>of</strong> < 5%.<br />
Prone to recurrence if incompletely excised: attention must be paid to margins.<br />
Adjuvant <strong>the</strong>rapy not warranted.<br />
Tumor may transform or dedifferentiate to group III (below).<br />
Atypical fibroxanthoma (any variant – spindle cell nonpleomorphic, pigmented or aneurysmal, clear cell, granular cell, osteoclastic<br />
giant cell, …), “some” cutaneous <strong>and</strong> subcutaneous “benign” fibrous histiocytomas (histology-dependent – atypical, cellular,<br />
aneurysmal; site-dependent – deep-seated, head & neck area; previous excision – recurring <strong>lesions</strong>) 135 253 , dermat<strong>of</strong>ibrosarcoma<br />
protuberans° (classic-type, Bednar/pigmented type – any site, any age, any variant), hybrid dermat<strong>of</strong>ibrosarcoma protuberans/giant<br />
cell fibroblastoma°, plexiform fibrohistiocytic tumor, giant cell angi<strong>of</strong>ibroma, solitary fibrous tumor° (including<br />
lipomatous hemangiopericytoma), atypical lipomatous tumor°, angiomatoid fibrous histiocytoma (aka, angiomatoid malignant<br />
fibrous histiocytoma), ossifying fibromyxoid tumor°, inflammatory my<strong>of</strong>ibroblastic tumor (“inflammatory pseudotumor”)°,<br />
“inflammatory fibrosarcoma”, pleomorphic hyalinizing angiectatic tumor – hemosiderotic fibrohistiocytic lipomatous tumor<br />
(prone to recurrence) 254 , myxoinflammatory fibroblastic sarcoma, deep-seated or large sized benign appearing smooth<br />
muscle tumors <strong>of</strong> s<strong>of</strong>t tissue 243 243a , well-differentiated liposarcoma (lipoma-like variant, sclerosing variants), “atypical” glomus tumors<br />
(deep-seated only / superficially located & mitotically active only / large-sized only) 255 , endo<strong>the</strong>lial neoplasms (Dabska’s tumor<br />
or papillary intralymphatic angioendo<strong>the</strong>lioma, retiform hemangioendo<strong>the</strong>lioma, composite hemangioendo<strong>the</strong>lioma,<br />
polymorphous hemangioendo<strong>the</strong>lioma, giant cell angioblastoma, Kaposi’s sarcoma) 245 246 , giant cell tumor° (skin, s<strong>of</strong>t tissue,<br />
breast) 256 , phosphaturic mesenchymal tumor° (excluding atypical variants), superficial low-grade fibromyxoid sarcoma (may<br />
recur) 257 , diffuse-type tenosynovial giant cell tumor (“pigmented villonodular synovitis/bursitis”) (prone to recurrence)°, s<strong>of</strong>t tissue<br />
mixed tumor, myoepi<strong>the</strong>lioma, parachordoma.<br />
!!!<br />
“Intermediate” is a term which is also used for tumors which can recur but do not metastasize; <strong>the</strong>se are also (more appropriately) termed locally<br />
aggressive. ° May undergo sarcomatous change.<br />
• Category III (X, Y, Z groups). Clinically malignant tumors<br />
Local excision with critical attention to margins (X, Y, Z).<br />
Consideration given to adjuvant <strong>the</strong>rapy (Y).<br />
Adjuvant <strong>the</strong>rapy usual (Z).<br />
Group III-X. Low-grade malignancy – metastatic rate <strong>of</strong> 5-10%.<br />
Infantile/congenital fibrosarcoma, well-differentiated (fibromatosis-like / Broders gr. I) fibrosarcoma, low-grade fibromyxoid sarcoma<br />
§ (including its variant hyalinising spindle cell tumor with giant rosettes), gr. I malignant fibrous histiocytoma (“low-grade” π<br />
myx<strong>of</strong>ibrosarcoma), angiomatoid (malignant) fibrous histiocytoma, cutaneous leiomyosarcoma, usual / well differentiated solitary<br />
fibrous tumor, low-grade my<strong>of</strong>ibrosarcoma, well-differentiated leiomyosarcoma, leiomyosarcoma in children, well differentiated<br />
liposarcoma with leiomyosarcomatous differentiation (w.d. lipoleiomyosarcoma), spindle cell liposarcoma, “lowgrade”<br />
dedifferentiated liposarcoma 72 , psammomatous melanotic schwannoma, low-grade malignant peripheral nerve<br />
sheath tumor, well-differentiated (gr. I) chondrosarcoma, low-grade angiosarcoma 245 246 .<br />
§<br />
Ungradable according to some.<br />
π<br />
Note: here are two tiered grading systems: one is 2-tiered (low- <strong>and</strong> high-grade) <strong>and</strong> <strong>the</strong> o<strong>the</strong>r is 3-tiered (low-, intermediate-, <strong>and</strong> high-grade).<br />
Group III-Y. Intermediate-grade malignancy – metastatic rate 10-30%<br />
Fibrosarcoma arising in dermat<strong>of</strong>ibrosarcoma protuberans (classic-type, Bednar-type) ψ , moderately differentiated conventional<br />
fibrosarcoma, solitary fibrous tumor (atypical, malignant), “true” well-differentiated malignant hemangiopericytoma 261 , gr.<br />
II myxoid malignant fibrous histiocytoma (“high-grade” π myx<strong>of</strong>ibrosarcoma), storiform malignant fibrous histiocytoma, conventional<br />
myxoid liposarcoma, conventional leiomyosarcoma, myxoid leiomyosarcoma, granular cell leiomyosarcoma (little experience),<br />
spindle cell embryonal rhabdomyosarcoma (“leiomyomatous variant”), moderately differentiated malignant peripheral nerve sheath<br />
tumor, conventionally dedifferentiated liposarcoma, malignant mesenchymoma, epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma ∆ , “lowgrade”<br />
extraskeletal myxoid chondrosarcoma 262 <strong>and</strong> its analogous variant with neuroendocrine differentiation, s<strong>of</strong>t tissue<br />
follicular dendritic cell sarcoma.<br />
ψ<br />
Metastatic rate <strong>of</strong> 10-30% 258-260 . π We have used a 2-tiered grading system for myxoid malignant fibrous histiocytoma (Angerwall’s myx<strong>of</strong>ibrosarcoma).<br />
∆ Classic histologies correlate with <strong>the</strong> lower end <strong>of</strong> metastatic rate <strong>of</strong> <strong>the</strong> category, while atypical features correlate with <strong>the</strong> upper end <strong>of</strong><br />
<strong>the</strong> metastatic prognostic spectrum.
288<br />
M. BISCEGLIA ET AL.<br />
Group III-Z. High-grade malignancy – metastatic rate > 30%.<br />
Poorly differentiated conventional fibrosarcoma, sclerosing epi<strong>the</strong>lioid fibrosarcoma, high grade myxoid/round cell liposarcoma,<br />
epi<strong>the</strong>lioid liposarcoma, pleomorphic liposarcoma ≠ , some mixed-type liposarcoma (myxoid/round cell <strong>and</strong> pleomorphic liposarcoma),<br />
pleomorphic my<strong>of</strong>ibrosarcoma, “true” conventional malignant hemangiopericytoma, poorly differentiated leiomyosarcoma,<br />
pleomorphic leiomyosarcoma, leiomyosarcoma, pleomorphic leiomyosarcoma, leiomyosarcoma with prominent osteoclastic giant<br />
cells, epi<strong>the</strong>lioid leiomyosarcoma ≠ , inflammatory leiomyosarcoma, rhabdomyosarcoma ↑↑↑ ≠ (any type – embryonal, alveolar,<br />
pleomorphic), angiosarcoma ↑↑↑ ≠ (any type – conventional, epi<strong>the</strong>lioid, poorly differentiated) 245 246 , intimal sarcoma, glomangiosarcoma<br />
≠ 255 263 , malignant peripheral nerve sheath tumor (poorly differentiated, epi<strong>the</strong>lioid, pleomorphic) ≠ , malignant granular cell tumor<br />
264<br />
, malignant Triton tumor, conventional epi<strong>the</strong>lioid sarcoma (“distal-type”, classic form ≠ § <strong>and</strong> variants 26a,67a,67b – fibroma-like, angiectoid),<br />
proximal-type epi<strong>the</strong>lioid sarcoma, extra-renal malignant rhabdoid tumor ↑↑↑ ≠ , synovial sarcoma ≠ § , mesenchymal<br />
chondrosarcoma ↑↑↑ , “high-grade” extraskeletal myxoid chondrosarcoma 262 <strong>and</strong> its analogous variant with neuroendocrine differentiation,<br />
extraskeletal osteosarcoma ↑↑↑ ≠ (any type – conventional <strong>and</strong> giant-cell rich), alveolar s<strong>of</strong>t part sarcoma § , clear cell sarcoma<br />
§ , s<strong>of</strong>t tissue PEComas (monotypic epi<strong>the</strong>lioid angiomyolipomas) ≠ , Ewing’s sarcoma / primitive neuroectodermal tumor ↑↑↑ ≠ ,<br />
desmoplastic small round cell tumor ↑↑↑ , high grade malignant fibrous histiocytoma group (pleomorphic malignant fibrous histiocytoma<br />
[undifferentiated pleomorphic sarcoma], osteoclastic giant cell malignant fibrous histiocytoma [undifferentiated pleomorphic<br />
sarcoma with osteoclastic giant cells], inflammatory malignant fibrous histiocytoma / undifferentiated pleomorphic sarcoma with<br />
prominent inflammation).<br />
≠<br />
Primary analogue high grade tumors also described in cutaneous site 2 , for which <strong>the</strong> predicted prognosis should not be applied. ↑↑↑ Definitionally<br />
high grade sarcomas. § May give rise to metastasis after a long duration follow-up, despite <strong>the</strong> absence <strong>of</strong> local recurrence.<br />
Clinical <strong>and</strong> Pathological Parameters influencing Prognosis (“Prognostic Predictors”) 265-272<br />
235-237 243 243a 271<br />
Clinicopathologic features – e.g. anatomical sites (abdominal cavity, retroperitoneum, head-neck worse than<br />
limbs, <strong>and</strong> abdominal <strong>and</strong> chest wall); tumor location (deep s<strong>of</strong>t tissue worse than skin <strong>and</strong> subcutis); tumor size (<strong>the</strong> larger <strong>the</strong><br />
worse); patient’s age (old age generally more adverse than young); clinical setting (secondary sarcomas arising in benign tumors,<br />
immunosuppression-associated tumors, virus-induced tumors, …); o<strong>the</strong>rs …<br />
Grading systems <strong>and</strong> histological grades 265-271 – e.g. grade I, II, III according to <strong>the</strong> French/FNCLCC grading system 266-268 , which<br />
evaluates 3 independent parameters (tumor differentiation, mitosis count, <strong>and</strong> necrosis) each scored 1 to 3: grade I → 2-3; grade<br />
II → 4-5; grade III → 6-8.<br />
Special histological types 269 – e.g. definitionally low grade tumors, definitionally high grade tumors, non-gradable tumors, tumors<br />
with not-yet-established grading parameters.<br />
Clinical stage 272 – e.g. TNM/UICC staging system: stage I (A: low grade, small, superficial, <strong>and</strong> deep; B: low grade, large, superficial);<br />
stage II (A: low grade, large, deep; B: high grade, small, superficial, <strong>and</strong> deep; C: high grade, large, superficial); stage III (hig<br />
grade, large, deep), stage IV (any metastasis).<br />
References<br />
1<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part I: Introduction.<br />
Pathologica 2004;96:9-17.<br />
2<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part II: The List<br />
<strong>and</strong> a Review. Pathologica 2004;96:52-94.<br />
3<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part III: Excerpta<br />
I. I-1: Classic <strong>and</strong> pigmented sarcomatous dermat<strong>of</strong>ibrosarcoma<br />
protuberans. I-2: Non-pleomorphic spindle-cell <strong>and</strong> aneurysmal<br />
(pigmented) atypical fibroxanthoma. I-3: Plexiform fibrohistiocytic<br />
tumor. I-4: Hemosiderotic fibrohistiocytic lipomatous lesion.<br />
I-5: Nuchal-type fibroma. I-6: Desmoplastic fibroblastoma.<br />
I-7: Solitary fibrous tumor. I-8: Pleomorphic hyalinizing angiectatic<br />
tumor. I-9: Sclerosing epi<strong>the</strong>lioid fibrosarcoma. Pathologica<br />
2004;96:121-42.<br />
4<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part IV: Excerpta<br />
II. II-1: Dermatomy<strong>of</strong>ibroma. II-2: Palisaded my<strong>of</strong>ibroblastoma /<br />
Intranodal hemorrhagic spindle cell tumor with “amianthoid”<br />
fibers. II-3: My<strong>of</strong>ibrosarcoma. II-4: Angiomy<strong>of</strong>ibroblastoma <strong>of</strong><br />
vulva. II-5: Lipomatous hemangiopericytoma. II-6: Inflammatory<br />
pseudotumor / inflammatory my<strong>of</strong>ibroblastic tumor. II-7: Calcifying<br />
fibrous (pseudo)tumor. II-8: Acral inflammatory myxohyaline<br />
tumor with Reed-Sternberg-like cells. II-9: Superficial angiomyxoma<br />
& iuxtarticular myxoma. II-10: Ossifying fibromyxoid tumor.<br />
II-11: Low grade fibromyxoid sarcoma & hyalinizing spindle cell<br />
tumor with giant rosettes. Pathologica 2004;96:436-63.<br />
5<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part V: Excerpta<br />
III. III-1: Phosphaturic mesenchymal tumor. III-2: Chondroid<br />
lipoma. III-3: Dendritic fibromyxolipoma. III-4: Epi<strong>the</strong>lioid li-
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 289<br />
posarcoma. III-5: Lipoleiomyosarcoma. III-6: Epi<strong>the</strong>lioid<br />
leiomyosarcoma. III-7: Granular cell leiomyosarcoma. Pathologica<br />
2004;96:481-95.<br />
6<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part VI: Excerpta<br />
IV. IV-1: Acquired elastotic hemangioma. IV-2: Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma<br />
<strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> skin. IV-3: Extraneuraxial<br />
hemangioblastoma <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> skin. IV-4: Tumor <strong>of</strong> Dabska<br />
arising on lymphangioma. Pathologica 2005;97:10-22.<br />
7<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part VII: Excerpta<br />
V. V-1: Epi<strong>the</strong>lioid psammomatous melanotic schwannoma. V-2:<br />
Pigmented neur<strong>of</strong>ibroma. V-3: Dendritic cell neur<strong>of</strong>ibroma with<br />
pseudorosettes. V-4: Epi<strong>the</strong>lial sheath neuroma. V-5: Perineuriomas-intraneurial<br />
<strong>and</strong> extraneurial forms. V-6: Ewing’s sarcoma<br />
<strong>of</strong> <strong>the</strong> skin. Pathologica 2005;97:92-114.<br />
8<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part VIII: Excerpta<br />
VI. VI-1: Extraskeletal myxoid chondrosarcoma with neuroendocrine<br />
differentiation. VI-2: Proximal epi<strong>the</strong>lioid sarcoma. VI-3:<br />
Extra-renal malignant rhabdoid tumour. VI-4: Follicular dendritic<br />
cell sarcoma. VI-5: Castleman’s disease <strong>of</strong> <strong>the</strong> subcutis <strong>and</strong><br />
skeletal muscle. VI-6: Rosai-Dorfman disease <strong>of</strong> s<strong>of</strong>t tissue. VI-7:<br />
Plexiform xanthomatous tumor. Pathologica 2005;97:141-57.<br />
9<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part IX: Excerpta<br />
VII. VII-1 (A,B,C): Myoepi<strong>the</strong>lial tumors - mixed tumor, myoepi<strong>the</strong>lioma,<br />
hyaline cell-rich chondroid syringoma. VII-2: Dabska’s<br />
parachordoma. VII-3: Oncocytoma. Pathologica<br />
2005;97:343-60.<br />
10<br />
Bisceglia M, Fisher C, Suster S, Kazakov DV, Cooper K, Michal<br />
M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong> <strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial<br />
<strong>and</strong> somatic s<strong>of</strong>t tissue: new entities <strong>and</strong> new variants <strong>of</strong><br />
old entities recorded during <strong>the</strong> last 25 years. Part X: Excerpta<br />
VIII. VIII-1: Ectopic hamartomatous thymoma. VIII-2: Hamartoma<br />
<strong>of</strong> <strong>the</strong> scalp with ectopic meningo<strong>the</strong>lial elements / rudimentary<br />
meningocele. VIII-3: Neural fibrolipomatous hamartoma.<br />
VIII-4: Ischemic fasciitis (Atypical decubital fibroplasia).<br />
VIII-5: Nephrogenic fibrosing dermopathy. VIII-6: Bacillary epi<strong>the</strong>lioid<br />
angiomatosis. Pathologica 2005;97:394-406.<br />
11<br />
Bisceglia M, Galliani C, Ben-Dor D, Fisher C, Suster S, Kazakov<br />
DV, Cooper K, Michal M. <strong>Tumoral</strong>, <strong>quasitumoral</strong> <strong>and</strong> <strong>pseudotumoral</strong><br />
<strong>lesions</strong> <strong>of</strong> <strong>the</strong> superficial <strong>and</strong> somatic s<strong>of</strong>t tissue: new entities<br />
<strong>and</strong> new variants <strong>of</strong> old entities recorded during <strong>the</strong> last 25<br />
years. Part XI: Excerpta IX. IX-1: Fibro-osseous pseudotumor <strong>of</strong><br />
<strong>the</strong> digits, <strong>and</strong> bizarre parosteal osteochondromatous proliferation<br />
(Nora’s lesion). IX-2: Tophaceous pseudogout. IX-3: Amyloid<br />
tumor <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> breast. IX-4: Glomus coccygeum. IX-<br />
5: Post-implant parathyromatosis. Pathologica 2006;98:187-208.<br />
12<br />
Fletcher CDM, Unni KK, Mertens F (Eds). Pathology <strong>and</strong> Genetics<br />
<strong>of</strong> Tumors <strong>of</strong> S<strong>of</strong>t Tissue <strong>and</strong> Bone. WHO Classification <strong>of</strong><br />
Tumors. IARC Press: Lyon 2002.<br />
13<br />
Fletcher CD. The evolving classification <strong>of</strong> s<strong>of</strong>t tissue tumours:<br />
an update based on <strong>the</strong> new WHO classification. Histopathology<br />
2006;48:3-12.<br />
14<br />
Guillou L. Entités récentes en pathologie tumorale des tissues<br />
mous. 1 re partie. Ann Pathol 2000;20:38-51.<br />
15<br />
Genevay M, Coindre JM, Guillou L. Entités récentes en pathologie<br />
tumorale des tissues mous. 2 e partie. Ann Pathol 2003;23:135-<br />
48.<br />
16<br />
Several authors. In: Fletcher CDM, ed. Histopathology<br />
2006;48:1-114.<br />
17<br />
Antonescu CR. The role <strong>of</strong> genetic testing in s<strong>of</strong>t tissue sarcoma.<br />
Histopathology 2006;48:13-21.<br />
18<br />
West RB, van de Rijn M. The role <strong>of</strong> microarray technologies in<br />
<strong>the</strong> study <strong>of</strong> s<strong>of</strong>t tissue tumours. Histopathology 2006;48:22-31.<br />
19<br />
Fisher C. The comparative roles <strong>of</strong> electron microscopy <strong>and</strong> immunohistochemistry<br />
in <strong>the</strong> diagnosis <strong>of</strong> s<strong>of</strong>t tissue tumors.<br />
Histopathology 2006;48:32-41.<br />
Table I<br />
20<br />
Nielsen GP, O’Connell JX, Wehrli BM, Rosenberg AE. Collagenrich<br />
tumors <strong>of</strong> s<strong>of</strong>t tissues: an overview. Adv Anat Pathol<br />
2003;10:179-99.<br />
21<br />
Bansal C, Stewart D, Li A, Cockerell CJ. Histologic variants <strong>of</strong><br />
fibrous papule. J Cutan Pathol 2005;32:424-8.<br />
22<br />
Allen PW. Hyaline fibromatosis. Adv Anat Pathol 2001;8:173-8.<br />
23<br />
Hornick JL, Fletcher CD. Intraarticular nodular fasciitis – A rare<br />
lesion: clinicopathologic analysis <strong>of</strong> a series. Am J Surg Pathol<br />
2006;30:237-41.<br />
24<br />
Yantiss RK, Nielsen GP, Lauwers GY, Rosenberg AE. Reactive<br />
nodular fibrous pseudotumor <strong>of</strong> <strong>the</strong> gastrointestinal tract <strong>and</strong><br />
mesentery: a clinicopathologic study <strong>of</strong> five cases. Am J Surg<br />
Pathol 2003;27:532-40.<br />
25<br />
Daum O, Vanecek T, Sima R, Curik R, Zamecnik M, Yamanaka<br />
S, et al. Reactive nodular fibrous pseudotumors <strong>of</strong> <strong>the</strong> gastrointestinal<br />
tract: report <strong>of</strong> 8 cases. Int J Surg Pathol 2004;12:365-74.<br />
25a<br />
Flieder DB, Suster S, Moran CA. Idiopathic fibroinflammatory<br />
(fibrosing/sclerosing) <strong>lesions</strong> <strong>of</strong> <strong>the</strong> mediastinum: a study <strong>of</strong> 30<br />
cases with emphasis on morphologic heterogeneity. Mod Pathol<br />
1999;12:257-64.<br />
26<br />
Gengler C, Guillou L. Solitary fibrous tumour <strong>and</strong> haemangiopericytoma:<br />
evolution <strong>of</strong> a concept. Histopathology<br />
2006;48:63-74.<br />
26a<br />
Miettinen M, Fanburg-Smith JC, Virolainen M, Shmookler BM,<br />
Fetsch JF. Epi<strong>the</strong>lioid sarcoma: an immunohistochemical analysis<br />
<strong>of</strong> 112 classical <strong>and</strong> variant cases <strong>and</strong> a discussion <strong>of</strong> <strong>the</strong> differential<br />
diagnosis. Hum Pathol 1999;30:934-42.<br />
27<br />
Plaza JA, Wakely PE Jr, Moran C, Fletcher CD, Suster S. Sclerosing<br />
paraganglioma: report <strong>of</strong> 19 cases <strong>of</strong> an unusual variant<br />
<strong>of</strong> neuroendocrine tumor that may be mistaken for an aggressive<br />
malignant neoplasm. Am J Surg Pathol 2006;30:7-12.<br />
27a<br />
Busam KJ. Cutaneous desmoplastic melanoma. Adv Anat Pathol<br />
2005;12:92-102.<br />
Table II<br />
28<br />
Allen PW. Myxoid tumors <strong>of</strong> s<strong>of</strong>t tissues. Pathol Annu 1980;15(Pt<br />
1):133-92.<br />
28a<br />
Allen PW. Myxoma is not a single entity: a review <strong>of</strong> <strong>the</strong> concept<br />
<strong>of</strong> myxoma. Ann Diagn Pathol 2000;4:99-123.<br />
28b<br />
Baboiu OE, Taylor WM. Noninvasive sacral chordoma presenting<br />
as a benign s<strong>of</strong>t tissue mass. Ann Diagn Pathol 2006;10:95-9.<br />
29<br />
Rongioletti F, Rebora A. Cutaneous mucinoses: microscopic criteria<br />
for diagnosis. Am J Dermatopathol 2001;23:257-67.<br />
30<br />
Billings SD, Giblen G, Fanburg-Smith JC. Superficial low-grade<br />
fibromyxoid sarcoma (Evans’ tumor). Am J Surg Pathol<br />
2005;29:204-10.<br />
31<br />
Alaggio R, Ninfo V, Rosolen A, C<strong>of</strong>fin CM. Primitive myxoid<br />
mesenchymal tumor <strong>of</strong> infancy. A clinicopathologic report <strong>of</strong> 6<br />
cases. Am J Surg Pathol 2006;30:388-94.<br />
32<br />
Huang HY, Lal P, Qin J, Brennan MF, Antonescu CR. Low-grade<br />
myx<strong>of</strong>ibrosarcoma: a clinicopathologic analysis <strong>of</strong> 49 cases<br />
treated at a single institution with simultaneous assessment <strong>of</strong> <strong>the</strong><br />
efficacy <strong>of</strong> 3-tier <strong>and</strong> 4-tier grading systems. Hum Pathol<br />
2004;35:612-21.<br />
32a<br />
Nielsen GP, Mangham DC, Grimer RJ, Rosenberg AE. Chordoma
290<br />
M. BISCEGLIA ET AL.<br />
periphericum: a case report. Am J Surg Pathol 2001;25:263-7.<br />
32b<br />
Folpe AL, Ag<strong>of</strong>f SN, Willis J, Weiss SW. Parachordoma is immunohistochemically<br />
<strong>and</strong> cytogenetically distinct from axial<br />
chordoma <strong>and</strong> extraskeletal myxoid chondrosarcoma. Am J Surg<br />
Pathol 1999;23:1059-67.<br />
32c<br />
Fisher C. Parachordoma exists - but what is it? Adv Anat Pathol<br />
2000;7:141-8.<br />
33<br />
Bisceglia M. Selected case from <strong>the</strong> Arkadi M. Rywlin international<br />
pathology slide seminar: digital central chondrosarcoma<br />
<strong>of</strong> <strong>the</strong> h<strong>and</strong> with systemic metastases. Adv Anat Pathol<br />
2002;9:309-15.<br />
33a<br />
Suster S, Sorace D, Moran CA. Gastrointestinal stromal tumors<br />
with prominent myxoid matrix. Clinicopathologic, immunohistochemical,<br />
<strong>and</strong> ultrastructural study <strong>of</strong> nine cases <strong>of</strong> a distinctive<br />
morphologic variant <strong>of</strong> myogenic stromal tumor. Am J Surg<br />
Pathol 1995;19:59-70.<br />
34<br />
Kim YC, V<strong>and</strong>ersteen DP, Jung HG. Myxoid clear cell sarcoma.<br />
Am J Dermatopathol 2005;27:51-5.<br />
35<br />
Bhuta S, Mirra JM, Cochran AJ. Myxoid malignant melanoma. A<br />
previously undescribed histologic pattern noted in metastatic <strong>lesions</strong><br />
<strong>and</strong> a report <strong>of</strong> four cases. Am J Surg Pathol 1986;10:203-11.<br />
36<br />
Hitchcock MG, McCalmont TH, White WL. Cutaneous<br />
melanoma with myxoid features: twelve cases with differential diagnosis.<br />
Am J Surg Pathol 1999;23:1506-13.<br />
36a<br />
Urso C. Cutaneous melanoma with pseudomyxoid features. J Cutan<br />
Pathol 2006;33:312-4.<br />
Table III<br />
37<br />
Monteagudo C, Ferr<strong>and</strong>ez A, Gonzalez-Devesa M, Llombart-<br />
Bosch A. Psammomatous malignant melanoma arising in an intradermal<br />
naevus. Histopathology 2001;39:493-7.<br />
37a<br />
Lorigan JG, O’Keeffe FN, Evans HL, Wallace S. The radiologic<br />
manifestations <strong>of</strong> alveolar s<strong>of</strong>t-part sarcoma. AJR Am J<br />
Roentgenol 1989;153:335-9.<br />
38<br />
Reiman HM, Dahlin DC. Cartilage- <strong>and</strong> bone-forming tumors <strong>of</strong><br />
<strong>the</strong> s<strong>of</strong>t tissues. Semin Diagn Pathol 1986;3:288-305.<br />
39<br />
Norman ES, Bergman S, Trupiano JK. Nasal chondromesenchymal<br />
hamartoma: report <strong>of</strong> a case <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Pediatr<br />
Dev Pathol 2004;7:517-20.<br />
40<br />
Ayala AG, Ro JY, Bolio-Solis A, Hern<strong>and</strong>ez-Batres F, Eftekhari<br />
F, Edeiken J. Mesenchymal hamartoma <strong>of</strong> <strong>the</strong> chest wall in infants<br />
<strong>and</strong> children: a clinicopathological study <strong>of</strong> five patients.<br />
Skeletal Radiol 1993;22:569-76.<br />
40a<br />
Ko E, Mortimer E, Fraire AE. Extraarticular synovial chondromatosis:<br />
review <strong>of</strong> epidemiology, imaging studies, microscopy<br />
<strong>and</strong> pathogenesis, with a report <strong>of</strong> an additional case in a child.<br />
Int J Surg Pathol 2004;12:273-80.<br />
41<br />
Patel RM, Weiss SW, Folpe AL. Heterotopic mesenteric ossification:<br />
a distinctive pseudosarcoma commonly associated with intestinal<br />
obstruction. Am J Surg Pathol 2006;30:119-22.<br />
41a<br />
Brien EW, Zahiri CA, Mirra JM. Florid reactive periostitis ossificans<br />
<strong>of</strong> <strong>the</strong> proximal aspect <strong>of</strong> <strong>the</strong> tibia: a lesion that must be distinguished<br />
from osteosarcoma. A case report. J Bone Joint Surg<br />
Am 1999;81:1002-7.<br />
42<br />
Fukunaga M. Osteogenic melanoma. APMIS 2005;113:296-300.<br />
Table IV<br />
43<br />
Emory TS, Monihan JM, Carr NJ, Sobin LH. Sclerosing mesenteritis,<br />
mesenteric panniculitis <strong>and</strong> mesenteric lipodystrophy: a<br />
single entity? Am J Surg Pathol 1997;21:392-8.<br />
44<br />
Dehner LP, C<strong>of</strong>fin CM. Idiopathic fibrosclerotic disorders <strong>and</strong><br />
o<strong>the</strong>r inflammatory pseudotumors. Semin Diagn Pathol<br />
1998;15:161-73.<br />
45<br />
Kuhnen C, Mentzel T, Sciot R, Lehnhardt M, Homann HH, Debiec-Rychter<br />
M. Dedifferentiated liposarcoma with extensive<br />
lymphoid component. Pathol Res Pract 2005;201:347-53.<br />
46<br />
Belville WD, Park JM, Kelly JL, Vaccaro JA. Perineal xanthogranulomatous<br />
pseudotumor due to intermittent ca<strong>the</strong>terization:<br />
a liposarcoma mimic. Case report. Paraplegia 1994;32:624-<br />
6.<br />
47<br />
Truong LD, Ostrowski ML, Wheeler TM. Tamm-Horsfall protein<br />
in bladder tissue. Morphologic spectrum <strong>and</strong> clinical significance.<br />
Am J Surg Pathol 1994;18:615-22.<br />
48<br />
Carr RA, Newman J, Antonakopulos GN, Parkinson MC. Lesions<br />
produced by <strong>the</strong> extravasation <strong>of</strong> urine from <strong>the</strong> upper urinary<br />
tract. Histopathology 1997;30:335-40.<br />
49<br />
Andrade VP, Nemer CC, Prezotti AN, Goulart WS. Erdheim-<br />
Chester disease <strong>of</strong> <strong>the</strong> breast associated with Langerhans-cell<br />
histiocytosis <strong>of</strong> <strong>the</strong> hard palate. Virchows Arch 2004;445:405-9.<br />
Table V<br />
50<br />
Nucci MR, Young RH, Fletcher CD. Cellular pseudosarcomatous<br />
fibroepi<strong>the</strong>lial stromal polyps <strong>of</strong> <strong>the</strong> lower female genital tract:<br />
an underrecognized lesion <strong>of</strong>ten misdiagnosed as sarcoma. Am J<br />
Surg Pathol 2000;24:231-40.<br />
51<br />
Mouhsine E, Halkic N, Gar<strong>of</strong>alo R, Taylor S, Theumann N, Guillou<br />
L, et al. S<strong>of</strong>t-tissue textiloma: a potential diagnostic pitfall.<br />
Can J Surg 2005;48:495-6.<br />
52<br />
Wenig BM, Heffner DK, Oertel YC, Johnson FB. Teflonomas <strong>of</strong><br />
<strong>the</strong> larynx <strong>and</strong> neck. Hum Pathol 1990;21:617-23.<br />
53<br />
Monaghan H, Salter DM, Al-Nafussi A. Giant cell tumour <strong>of</strong> tendon<br />
sheath (localised nodular tenosynovitis): clinicopathological<br />
features <strong>of</strong> 71 cases. J Clin Pathol 2001;54:404-7.<br />
53a<br />
Zambrano E, Reyes-Mugica M, Franchi A, Rosai J. An osteoclast-rich<br />
tumor <strong>of</strong> <strong>the</strong> gastrointestinal tract with features resembling<br />
clear cell sarcoma <strong>of</strong> s<strong>of</strong>t parts: reports <strong>of</strong> 6 cases <strong>of</strong> a GIST<br />
simulator. Int J Surg Pathol 2003;11:75-81.<br />
54<br />
Boyd AS, Wu H, Shyr Y. Monster cells in malignant melanoma.<br />
Am J Dermatopathol 2005;27:208-10.<br />
55<br />
Helm KF. Malignant melanoma masquerading as malignant fibrous<br />
histiocytoma. Am J Dermatopathol 1997;19:473-6.<br />
Table VI<br />
56<br />
Fisher C. My<strong>of</strong>ibroblastic malignancies. Adv Anat Pathol<br />
2004;11:190-201.<br />
57<br />
Miettinen M, Monihan JM, Sarlomo-Rikala M, Kovatich AJ, Carr<br />
NJ, Emory TS, et al. Gastrointestinal stromal tumors/smooth<br />
muscle tumors (GISTs) primary in <strong>the</strong> omentum <strong>and</strong> mesentery:<br />
clinicopathologic <strong>and</strong> immunohistochemical study <strong>of</strong> 26 cases.<br />
Am J Surg Pathol 1999;23:1109-18.<br />
58<br />
Al-Nafussi A, Wong NA. Intra-abdominal spindle cell <strong>lesions</strong>: a<br />
review <strong>and</strong> practical aids to diagnosis. Histopathology<br />
2001;38:387-402.<br />
59<br />
Nakhleh RE, Wick MR, Rocamora A, Swanson PE, Dehner LP.<br />
Morphologic diversity in malignant melanomas. Am J Clin Pathol<br />
1990;93:731-40.<br />
59a<br />
Banerjee SS, Harris M. Morphological <strong>and</strong> immunophenotypic<br />
variations in malignant melanoma.Histopathology 2000;36:387-402.<br />
60<br />
Squillaci S, Cecchetti D, Tallarigo F, Pontieri E, Filardo AV. Myopericytoma-type,<br />
perivascular myoma located in <strong>the</strong> s<strong>of</strong>t tissue<br />
<strong>of</strong> <strong>the</strong> foot: a case report <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Pathologica<br />
2005;97:378-82.<br />
61<br />
Deyrup AT, Alth<strong>of</strong> P, Zhou M, Morgan M, Solomon AR, Bridge<br />
JA, et al. Paraganglioma-like dermal melanocytic tumor: a unique<br />
entity distinct from cellular blue nevus, clear cell sarcoma, <strong>and</strong><br />
cutaneous melanoma. Am J Surg Pathol 2004;28:1579-86.<br />
62<br />
Bridge JA, Fidler ME, Neff JR, Degenhardt J, Wang M, Walker<br />
C, et al. Adamantinoma-like Ewing's sarcoma: genomic confirmation,<br />
phenotypic drift. Am J Surg Pathol 1999;23:159-65.<br />
62a<br />
Folpe AL, Goldblum JR, Rubin BP, Shehata BM, Liu W, Dei Tos<br />
AP, et al. Morphologic <strong>and</strong> immunophenotypic diversity in Ewing<br />
family tumors: a study <strong>of</strong> 66 genetically confirmed cases. Am J<br />
Surg Pathol 2005;29:1025-33.
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 291<br />
Table VII<br />
63<br />
Nappi O, Ritter JH, Pettinato G, Wick MR. Hemangiopericytoma:<br />
histopathological pattern or clinicopathologic entity?<br />
Semin Diagn Pathol 1995;12:221-32.<br />
64<br />
Gengler C, Guillou L. Solitary fibrous tumor <strong>and</strong> haemangiopericytoma:<br />
evolution <strong>of</strong> a concept. Histopathology 2006;48:63-74.<br />
65<br />
Orvieto E, Furlanetto A, Laurino L, Dei Tos AP. Myxoid <strong>and</strong><br />
round cell liposarcoma: a spectrum <strong>of</strong> myxoid adipocytic neoplasia.<br />
Semin Diagn Pathol 2001;18:267-73.<br />
66<br />
Schwartz RA, Dabski C, Dabska M. The Dabska tumor: a thirty<br />
year retrospect. Dermatology 2000;201:1-5.<br />
66a<br />
Urso C, Tinacci G. Angiomatoid cellular blue nevus: a variant <strong>of</strong><br />
blue nevus with an angioma-like appearance. J Cutan Pathol<br />
2005;32:385-7.<br />
67<br />
Costa MJ, McGlothlen L, Pierce M, Munn R, Vogt PJ. Angiomatoid<br />
features in fibrohistiocytic sarcomas. Immunohistochemical,<br />
ultrastructural, <strong>and</strong> clinical distinction from vascular neoplasms.<br />
Arch Pathol Lab Med 1995;119:1065-71.<br />
67a<br />
von Hochstetter AR, Meyer VE, Grant JW, Honegger HP,<br />
Schreiber A. Epi<strong>the</strong>lioid sarcoma mimicking angiosarcoma: <strong>the</strong><br />
value <strong>of</strong> immunohistochemistry in <strong>the</strong> differential diagnosis. Virchows<br />
Arch A Pathol Anat Histopathol 1991;418:271-8.<br />
67b<br />
Fisher C. Epi<strong>the</strong>lioid sarcoma <strong>of</strong> Enzinger. Adv Anat Pathol<br />
2006;13:114-21.<br />
Table VIII<br />
68<br />
Kazakov DV, Pitha J, Sima R, Vanecek T, Shelekhova K, Mukensnabl<br />
P, et al. Hybrid peripheral nerve sheath tumors: Schwannoma-perineurioma<br />
<strong>and</strong> neur<strong>of</strong>ibroma-perineurioma. A report <strong>of</strong><br />
three cases in extradigital locations. Ann Diagn Pathol<br />
2005;9:16-23.<br />
69<br />
Michal M, Kazakov DV, Belousova I, Bisceglia M, Zamecnik M,<br />
Mukensnabl P. A benign neoplasm with histopathological features<br />
<strong>of</strong> both schwannoma <strong>and</strong> retiform perineurioma (benign<br />
schwannoma-perineurioma): a report <strong>of</strong> six cases <strong>of</strong> a distinctive<br />
s<strong>of</strong>t tissue tumor with a predilection for <strong>the</strong> fingers. Virchows<br />
Arch 2004;445:347-53.<br />
70<br />
Usta U, Turkmen E, Mizrak B, Yildiz D, Guzel Z. Spindle cell<br />
lipoma in an intramuscular lipoma. Pathol Int 2004;54:734-9.<br />
71<br />
Nascimento AG. Dedifferentiated liposarcoma. Semin Diagn<br />
Pathol 2001;18:263-6.<br />
72<br />
Elgar F, Goldblum JR. Well-differentiated liposarcoma <strong>of</strong> <strong>the</strong><br />
retroperitoneum: a clinicopathologic analysis <strong>of</strong> 20 cases, with<br />
particular attention to <strong>the</strong> extent <strong>of</strong> low-grade dedifferentiation.<br />
Mod Pathol 1997;10:113-20.<br />
73<br />
Pool SE, Manieei F, Clark WH Jr, Harrist TJ. Dermal squamomelanocytic<br />
tumor: a unique biphenotypic neoplasm <strong>of</strong> uncertain<br />
biological potential. Hum Pathol 1999;30:525-9.<br />
74<br />
Erickson LA, Myers JL, Mihm MC, Markovic SN, Pittelkow<br />
MR. Malignant basomelanocytic tumor manifesting as metastatic<br />
melanoma. Am J Surg Pathol 2004;28:1393-6.<br />
Table IX<br />
75<br />
Saad AG, Mutema GK, Mutasim DF. Benign cutaneous epi<strong>the</strong>lioid<br />
Schwannoma: case report <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Am J<br />
Dermatopathol 2005;27:45-7.<br />
76<br />
Hornick JL, Fletcher CD. PEComa: what do we know so far?<br />
Histopathology 2006;48:75-82.<br />
77<br />
Bonetti F, Martignoni G, Colato C, Manfrin E, Gambacorta M,<br />
Faleri M, et al. Abdominopelvic sarcoma <strong>of</strong> perivascular epi<strong>the</strong>lioid<br />
cells. Report <strong>of</strong> four cases in young women, one with tuberous<br />
sclerosis. Mod Pathol 2001;14:563-8.<br />
78<br />
Mentzel T, Reisshauer S, Rutten A, Hantschke M, Soares de<br />
Almeida LM, Kutzner H. Cutaneous clear cell myomelanocytic<br />
tumour: a new member <strong>of</strong> <strong>the</strong> growing family <strong>of</strong> perivascular epi<strong>the</strong>lioid<br />
cell tumours (PEComas). Clinicopathological <strong>and</strong> immunohistochemical<br />
analysis <strong>of</strong> seven cases. Histopathology<br />
2005;46:498-504.<br />
79<br />
Nascimento AG, Keeney GL, Fletcher CD. Deciduoid peritoneal<br />
meso<strong>the</strong>lioma. An unusual phenotype affecting young females.<br />
Am J Surg Pathol 1994;18:439-45.<br />
80<br />
Shanks JH, Harris M, Banerjee SS, Eyden BP, Joglekar VM, et al.<br />
Meso<strong>the</strong>liomas with deciduoid morphology: a morphologic spectrum<br />
<strong>and</strong> a variant not confined to young females. Am J Surg<br />
Pathol 2000;24:285-94.<br />
81<br />
Mourra N, de Chaisemartin C, Goubin-Versini I, Parc R, Flejou<br />
JF. Malignant deciduoid meso<strong>the</strong>lioma: a diagnostic challenge.<br />
Arch Pathol Lab Med 2005;129:403-6.<br />
82<br />
Hornick JL, Jaffe ES, Fletcher CD. Extranodal histiocytic sarcoma:<br />
clinicopathologic analysis <strong>of</strong> 14 cases <strong>of</strong> a rare epi<strong>the</strong>lioid<br />
malignancy. Am J Surg Pathol 2004;28:1133-44.<br />
83<br />
d’Amore ES, Ninfo V. Clear cell tumors <strong>of</strong> <strong>the</strong> somatic s<strong>of</strong>t tissues.<br />
Semin Diagn Pathol 1997;14:270-80.<br />
84<br />
Lee AN, Stein SL, Cohen LM. Clear cell fibrous papule with<br />
NKI/C3 expression: clinical <strong>and</strong> histologic features in six cases.<br />
Am J Dermatopathol 2005;27:296-300.<br />
85<br />
Lazar AJ, Fletcher CD. Distinctive dermal clear cell mesenchymal<br />
neoplasm: clinicopathologic analysis <strong>of</strong> five cases. Am J<br />
Dermatopathol 2004;26:273-9.<br />
85a<br />
Llombart-Bosch A, Pellin A, Carda C, Noguera R, Navarro S,<br />
Peydro-Olaya A. S<strong>of</strong>t tissue Ewing sarcoma--peripheral primitive<br />
neuroectodermal tumor with atypical clear cell pattern shows a<br />
new type <strong>of</strong> EWS-FEV fusion transcript. Diagn Mol Pathol<br />
2000;9:137-44.<br />
85b<br />
Plaza JA, Wakely PE Jr, Suster S. Lipoblastic nerve sheath tumors:<br />
report <strong>of</strong> a distinctive variant <strong>of</strong> neural s<strong>of</strong>t tissue neoplasm<br />
with adipocytic differentiation. Am J Surg Pathol<br />
2006;30:337-44.<br />
85c<br />
Suster S, Fletcher CD. Gastrointestinal stromal tumors with<br />
prominent signet-ring cell features. Mod Pathol 1996;9:609-13.<br />
85d<br />
Rutten A, Huschka U, Requena C, Rodriguez-Peralto JL, Requena<br />
L. Primary cutaneous signet-ring cell melanoma: a clinicopathologic<br />
<strong>and</strong> immunohistochemical study <strong>of</strong> two cases. Am J<br />
Dermatopathol 2003;25:418-22.<br />
85e<br />
Magro CM, Crowson AN, Mihm MC. Unusual variants <strong>of</strong> malignant<br />
melanoma. Mod Pathol 2006;19 Suppl 2:S41-70.<br />
85f<br />
Goldsmith JD, Pawel B, Goldblum JR, Pasha TL, Roberts S, Nelson<br />
P, et al. Detection <strong>and</strong> diagnostic utilization <strong>of</strong> placental alkaline<br />
phosphatase in muscular tissue <strong>and</strong> tumors with myogenic<br />
differentiation. Am J Surg Pathol 2002;26:1627-33.<br />
86<br />
Suster S. Tumors <strong>of</strong> <strong>the</strong> skin composed <strong>of</strong> large cells with abundant<br />
eosinophilic cytoplasm. Semin Diagn Pathol 1999;16:162-77.<br />
87<br />
d’Amore ES, Ninfo V. Tumors <strong>of</strong> <strong>the</strong> s<strong>of</strong>t tissues composed <strong>of</strong><br />
large eosinophilic cells. Semin Diagn Pathol 1999;16:178-89.<br />
88<br />
Lazar AJ, Fletcher CD. Primitive nonneural granular cell tumors<br />
<strong>of</strong> skin: clinicopathologic analysis <strong>of</strong> 13 cases. Am J Surg Pathol<br />
2005;29:927-34.<br />
89<br />
d’Amore ES, Ninfo V. S<strong>of</strong>t tissue small round cell tumors: morphological<br />
parameters. Semin Diagn Pathol 1996;13:184-203.<br />
90<br />
Dei Tos AP. Classification <strong>of</strong> pleomorphic sarcomas: where are<br />
we now? Histopathology 2006;48:51-62.<br />
91<br />
Oliveira AM, Nascimento AG. Pleomorphic liposarcoma. Semin<br />
Diagn Pathol 2001;18:274-85.<br />
92<br />
Oda Y, Miyajima K, Kawaguchi K, Tamiya S, Oshiro Y, Hachit<strong>and</strong>a<br />
Y, et al. Pleomorphic leiomyosarcoma: clinicopathologic<br />
<strong>and</strong> immunohistochemical study with special emphasis on its distinction<br />
from ordinary leiomyosarcoma <strong>and</strong> malignant fibrous<br />
histiocytoma. Am J Surg Pathol 2001;25:1030-8.<br />
93<br />
Sebenik M, Ricci A Jr, Di Pasquale B, Mody K, Pytel P, Jee KJ,<br />
et al. Undifferentiated intimal sarcoma <strong>of</strong> large systemic blood<br />
vessels: report <strong>of</strong> 14 cases with immunohistochemical pr<strong>of</strong>ile <strong>and</strong><br />
review <strong>of</strong> <strong>the</strong> literature. Am J Surg Pathol 2005;29:1184-93.
292<br />
M. BISCEGLIA ET AL.<br />
Table X<br />
94<br />
Kinkor Z, Mukensnabl P, Michal M. Inflammatory myxohyaline<br />
tumor with massive emperipolesis. Pathol Res Pract<br />
2002;198:639-42.<br />
95<br />
Argani P, Facchetti F, Inghirami G, Rosai J. Lymphocyte-rich<br />
well-differentiated liposarcoma: report <strong>of</strong> nine cases. Am J Surg<br />
Pathol 1997;21:884-95.<br />
96<br />
Tarroch X, Vives P, Salas A, More J. Subcutaneous nodules in<br />
Whipple’s disease. J Cutan Pathol 2001;28:368-70.<br />
97<br />
Friedmann AC, Perera GK, Jayaprakasam A, Forgacs I, Salisbury<br />
JR, Creamer D. Whipple’s disease presenting with symmetrical<br />
panniculitis. Br J Dermatol 2004;15:907-11.<br />
Table XI<br />
98<br />
Zembowicz A, Mihm MC. Dermal dendritic melanocytic proliferations:<br />
an update. Histopathology 2004;45:433-51.<br />
99<br />
Carlson JA, Healy K, Slominski A, Mihm MC Jr. Melanocytic<br />
matricoma: a report <strong>of</strong> two cases <strong>of</strong> a new entity. Am J Dermatopathol<br />
1999;21:344-9.<br />
100<br />
Williams CM, Bozner P, Oliveri CV, Horenstein MG. Melanocytic<br />
matricoma: case confirmation <strong>of</strong> a recently described entity. J<br />
Cutan Pathol 2003;30:275-8.<br />
101<br />
Claessens N, Heymans O, Arrese JE, Garcia R, Oelbr<strong>and</strong>t B, Pierard<br />
GE. Cutaneous psammomatous melanotic schwannoma: nonrecurrence<br />
with surgical excision. Am J Clin Dermatol<br />
2003;4:799-802.<br />
102<br />
Swetter SM, Ecker PM, Johnson DL, Harvell JD. Primary dermal<br />
melanoma: a distinct subtype <strong>of</strong> melanoma. Arch Dermatol<br />
2004;140:99-103.<br />
103<br />
Zembowicz A, Carney JA, Mihm MC. Pigmented epi<strong>the</strong>lioid<br />
melanocytoma: a low-grade melanocytic tumor with metastatic<br />
potential indistinguishable from animal-type melanoma <strong>and</strong> epi<strong>the</strong>lioid<br />
blue nevus. Am J Surg Pathol 2004;28:31-40.<br />
104<br />
Crowson AN, Magro CM, Mihm MC Jr. Malignant melanoma<br />
with prominent pigment syn<strong>the</strong>sis: “animal type” melanoma – a<br />
clinical <strong>and</strong> histological study <strong>of</strong> six cases with a consideration <strong>of</strong><br />
o<strong>the</strong>r melanocytic neoplasms with prominent pigment syn<strong>the</strong>sis.<br />
Hum Pathol 1999;30:543-50.<br />
105<br />
Carney JA, Ferreiro JA. The epi<strong>the</strong>lioid blue nevus. A multicentric<br />
familial tumor with important associations, including cardiac<br />
myxoma <strong>and</strong> psammomatous melanotic schwannoma.Am J Surg<br />
Pathol 1996;20:259-72.<br />
106<br />
Moran CA, Albores-Saavedra J, Wenig BM, Mena H. Pigmented<br />
extraadrenal paragangliomas. A clinicopathologic <strong>and</strong> immunohistochemical<br />
study <strong>of</strong> five cases. Cancer 1997;79:398-402.<br />
Table XII<br />
107<br />
Blickenstaff RD, Roenigk RK, Peters MS, Goellner JR. Recurrent<br />
pyogenic granuloma with satellitosis. J Am Acad Dermatol<br />
1989;21:1241-4.<br />
108<br />
Blaauwgeers JL, Troost D, Dingemans KP, Taat CW, Van den<br />
Tweel JG. Multifocal rhabdomyoma <strong>of</strong> <strong>the</strong> neck. Report <strong>of</strong> a case<br />
studied by fine-needle aspiration, light <strong>and</strong> electron microscopy,<br />
histochemistry, <strong>and</strong> immunohistochemistry. Am J Surg Pathol<br />
1989;13:791-9.<br />
109<br />
Mahalingam M, Alter JN, Bhawan J. Multiple cellular neuro<strong>the</strong>keomas<br />
– a case report <strong>and</strong> review on <strong>the</strong> role <strong>of</strong> immunohistochemistry<br />
as a histologic adjunct. J Cutan Pathol 2006;33:51-6.<br />
Table XIII<br />
109a<br />
Agaram NP, Prakash S, Antonescu CR. Deep-seated plexiform<br />
schwannoma: a pathologic study <strong>of</strong> 16 cases <strong>and</strong> comparative<br />
analysis with <strong>the</strong> superficial variety. Am J Surg Pathol<br />
2005;29:1042-8.<br />
109b<br />
MacCollin M, Woodfin W, Kronn D, Short MP. Schwannomatosis:<br />
a clinical <strong>and</strong> pathologic study. Neurology 1996;46:1072-9<br />
(Comment in: Neurology 1997;48:787-8).<br />
109c<br />
Jacoby LB, Jones D, Davis K, Kronn D, Short MP, Gusella J, et<br />
al. Molecular analysis <strong>of</strong> <strong>the</strong> NF2 tumor-suppressor gene in<br />
schwannomatosis. Am J Hum Genet 1997;61:1293-302.<br />
109d<br />
Seppala MT, Sainio MA, Haltia MJ, Kinnunen JJ, Setala KH,<br />
Jaaskelainen JE. Multiple schwannomas: schwannomatosis or<br />
neur<strong>of</strong>ibromatosis type 2? J Neurosurg. 1998;89:36-41 (Comment<br />
in: J Neurosurg 1999;91:351-2).<br />
110<br />
Woodruff JM, Scheithauer BW, Kurtkaya-Yapicier O, Raffel C,<br />
Amr SS, LaQuaglia MP, et al. Congenital <strong>and</strong> childhood plexiform<br />
(multinodular) cellular schwannoma: a troublesome mimic<br />
<strong>of</strong> malignant peripheral nerve sheath tumor. Am J Surg Pathol<br />
2003;27:1321-9.<br />
111<br />
Agaram NP, Prakash S, Antonescu CR. Deep-seated plexiform<br />
schwannoma: a pathologic study <strong>of</strong> 16 cases <strong>and</strong> comparative<br />
analysis with <strong>the</strong> superficial variety. Am J Surg Pathol<br />
2005;29:1042-8.<br />
112<br />
Shelekhova K, Kazakov DV, Michal M. Infiltrating retiform perineurioma:<br />
a case report. Ann Diagn Pathol 2005;9:293-4.<br />
113<br />
Clement PB, Young RH, Scully RE. Intravenous leiomyomatosis<br />
<strong>of</strong> <strong>the</strong> uterus. A clinicopathological analysis <strong>of</strong> 16 cases with unusual<br />
histologic features. Am J Surg Pathol 1988;12:932-45.<br />
114<br />
Calonje E, Mentzel T, Fletcher CD. Pseudomalignant perineurial<br />
invasion in cellular (‘infantile’) capillary haemangiomas.<br />
Histopathology 1995;26:159-64.<br />
115<br />
Casadei GP, Scheithauer BW, Hirose T, Manfrini M, Van Houton<br />
C, Wood MB. Cellular schwannoma. A clinicopathologic, DNA<br />
flow cytometric, <strong>and</strong> proliferation marker study <strong>of</strong> 70 patients.<br />
Cancer 1995;75:1109-19.<br />
116<br />
Zelger BW, Calonje E, Sepp N, Fink FM, Zelger BG, Schmid<br />
KW. Monophasic cellular variant <strong>of</strong> infantile my<strong>of</strong>ibromatosis.<br />
An unusual histopathologic pattern in two siblings. Am J Dermatopathol<br />
1995;17:131-8.<br />
Table XV<br />
117<br />
Brenn T, Fletcher CD. Postradiation vascular proliferations: an<br />
increasing problem. Histopathology 2006;48:106-14.<br />
Table XVI<br />
118<br />
Hollowood K, Fletcher CD. S<strong>of</strong>t tissue sarcomas that mimic benign<br />
<strong>lesions</strong>. Semin Diagn Pathol 1995;12:87-97.<br />
119<br />
Laurino L, Furlanetto A, Orvieto E, Dei Tos AP. Well-differentiated<br />
liposarcoma (atypical lipomatous tumors). Semin Diagn<br />
Pathol 2001;18:258-62.<br />
120<br />
Ritter JH, Humphrey PA, Wick MR. Malignant neoplasms capable<br />
<strong>of</strong> simulating inflammatory (my<strong>of</strong>ibroblastic) pseudotumors<br />
<strong>and</strong> tumefactive fibroinflammatory <strong>lesions</strong>: pseudopseudotumors.<br />
Semin Diagn Pathol 1998;15:111-32.<br />
121<br />
Nascimento AG. Spindle cell liposarcoma (Commentary). Adv<br />
Anat Pathol 1995;2:320-5.<br />
122<br />
Sneige N, Yaziji H, M<strong>and</strong>avilli SR, Perez ER, Ordonez NG,<br />
Gown AM, et al. Low-grade (fibromatosis-like) spindle cell carcinoma<br />
<strong>of</strong> <strong>the</strong> breast. Am J Surg Pathol 2001;25:1009-16.<br />
Table XVII<br />
123<br />
Rosai J. Introduction: Dr. Lauren V. Ackerman <strong>and</strong> his man from<br />
Instanbul. Semin Diagn Pathol 2003;20:247-8.<br />
124<br />
Dehner LP. Juvenile xanthogranulomas in <strong>the</strong> first two decades <strong>of</strong><br />
life: a clinicopathologic study <strong>of</strong> 174 cases with cutaneous <strong>and</strong> extracutaneous<br />
manifestations. Am J Surg Pathol 2003;27:579-93.<br />
125<br />
Colby T. Visceral (pulmonary) juvenile xanthogranuloma. AMR<br />
International Slide Seminar # 39 (Case 4). November 2002<br />
(http://www.amr-seminar.org).<br />
126<br />
Kobayashi S, Yamadori I, Ohmori M, Akaeda T. Benign fibrous histiocytoma<br />
<strong>of</strong> <strong>the</strong> renal capsule. Acta Pathol Jpn 1992;42:217-20.<br />
127<br />
Sakakibara N, Seki T, Maru A, Koyanagi T. Benign fibrous histiocytoma<br />
<strong>of</strong> <strong>the</strong> kidney. J Urol 1989;142:1558-9.<br />
128<br />
Schick B, Kind M, Schwarzkopf G, Weber R, Draf W. Early<br />
childhood angi<strong>of</strong>ibroma in an unusual site HNO 1997;45:1022-8.
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 293<br />
128a<br />
Huang RY, Damrose EJ, Blackwell KE, Cohen AN, Calcaterra<br />
TC. Extranasopharyngeal angi<strong>of</strong>ibroma. Int J Pediatr Otorhinolaryngol<br />
2000; 30:56:59-64.<br />
129<br />
Fisher C, Folpe AL, Hashimoto H, Weiss SW. Intra-abdominal<br />
synovial sarcoma: a clinicopathological study. Histopathology<br />
2004;45:245-53.<br />
130<br />
Ozolek JA, Carrau R, Barnes EL, Hunt JL. Nasal chondromesenchymal<br />
hamartoma in older children <strong>and</strong> adults: series <strong>and</strong> immunohistochemical<br />
analysis. Arch Pathol Lab Med<br />
2005;129:1444-50.<br />
131<br />
Montesco MC, Alaggio R, Ninfo V. Pediatric-type sarcomas in<br />
adult patients. Semin Diagn Pathol 2003;20:324-37.<br />
132<br />
Nascimento AF, Fletcher CD. Spindle cell rhabdomyosarcoma in<br />
adults. Am J Surg Pathol 2005;29:1106-13.<br />
133<br />
Huszar M, Fanburg JC, Dickersin GR, Kirshner JJ, Rosenberg<br />
AE. Retroperitoneal malignant meningioma. A light microscopic,<br />
immunohistochemical, <strong>and</strong> ultrastructural study. Am J Surg<br />
Pathol 1996;20:492-9.<br />
134<br />
Morrison C, Ramirez NC, Chan JK, Wakely P Jr. Endometrial<br />
stromal sarcoma <strong>of</strong> <strong>the</strong> retroperitoneum. Ann Diagn Pathol<br />
2002;6:312-8.<br />
135<br />
Bisceglia M, Attino V, Bacchi CE. Metastasizing “benign” fibrous<br />
histiocytoma <strong>of</strong> <strong>the</strong> skin: a report <strong>of</strong> two additional cases<br />
<strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Adv Anat Pathol 2006;13:89-96.<br />
136<br />
Kayser K, Zink S, Schenider T, Dienemann H, Andre S, Kaltner<br />
H, et al. Benign metastasizing leiomyoma <strong>of</strong> <strong>the</strong> uterus: documentation<br />
<strong>of</strong> clinical, immunohistochemicla <strong>and</strong> lectin-histochemical<br />
data <strong>of</strong> ten cases. Vircows Arch 2000;437:284-92.<br />
137<br />
Pramesh CS, Saklani AP, Pantvaidya GH, Heroor AA, Naresh<br />
KN, Sharma S, et al. Benign metastasizing meningioma. Jpn J<br />
Clin Oncol 2003;33:86-8.<br />
137a<br />
Navarro S, Noguera R, Pellin A, Lopez-Guerrero JA, Rosello-<br />
Sastre E, Cremades A, et al. Atypical pleomorphic extraosseous<br />
ewing tumor/peripheral primitive neuroectodermal tumor with<br />
unusual phenotypic/genotypic pr<strong>of</strong>ile. Diagn Mol Pathol<br />
2002;11:9-15.<br />
138<br />
Carbone A, Gloghini A, Libra M, Gasparotto D, Navolanic PM,<br />
Spina M, et al. A spindle cell variant <strong>of</strong> diffuse large B-cell lymphoma<br />
possesses genotypic <strong>and</strong> phenotypic markers characteristic <strong>of</strong> a germinal<br />
center B-cell origin. Mod Pathol 2006;19:299-306.<br />
139<br />
Gu M, Antonescu CR, Guiter G, Huvos AG, Ladanyi M, Zakowski<br />
MF. Cytokeratin immunoreactivity in Ewing's sarcoma: prevalence<br />
in 50 cases confirmed by molecular diagnostic studies. Am J<br />
Surg Pathol 2000;24:410-6.<br />
139a<br />
Collini P, Sampietro G, Bertulli R, Casali PG, Luksch R, Mezzelani<br />
A, et al. Cytokeratin immunoreactivity in 41 cases <strong>of</strong> ES/PNET confirmed<br />
by molecular diagnostic studies. Am J Surg Pathol<br />
2001;25:273-4.<br />
139b<br />
Schuetz AN, Rubin BP, Goldblum JR, Shehata B, Weiss SW, Liu<br />
W, et al. Intercellular junctions in Ewing sarcoma/primitive neuroectodermal<br />
tumor: additional evidence <strong>of</strong> epi<strong>the</strong>lial differentiation.<br />
Mod Pathol 2005;18:1403-10.<br />
140<br />
Zarbo RJ, Gown AM, Nagle RB, Visscher DW, Crissman JD.<br />
Anomalous cytokeratin expression in malignant melanoma: one<strong>and</strong><br />
two-dimensional western blot analysis <strong>and</strong> immunohistochemical<br />
survey <strong>of</strong> 100 melanomas. Mod Pathol 1990;3:494-501.<br />
Table XVIII<br />
141<br />
Hurt MA, Santa Cruz DJ. Nodular-cystic fat necrosis. A reevaluation<br />
<strong>of</strong> <strong>the</strong> so-called mobile encapsulated lipoma. J Am Acad<br />
Dermatol 1989;21:493-8.<br />
141a<br />
Bisceglia M, Vigilante E, Ben-Dor D. Neural lip<strong>of</strong>ibromatous<br />
hamartoma: a report <strong>of</strong> two cases <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature.<br />
Adv Anat Pathol, in press<br />
Table XX<br />
142<br />
Lattes R, Bigotti G. Lipoblastic meningioma: “vacuolated meningioma”.<br />
Hum Pathol 1991;22:164-71.<br />
143<br />
Croxatto JO, Font RL. Hemangiopericytoma <strong>of</strong> <strong>the</strong> orbit: a clinicopathologic<br />
study <strong>of</strong> 30 cases. Hum Pathol 1982;13:210-8.<br />
144<br />
Davies PE, Davis GJ, Dodd T, Selva D. Orbital lipomatous haemangiopericytoma:<br />
an unusual variant. Clin Experiment Ophthalmol<br />
2002;30:281-3.<br />
Table XXI<br />
145<br />
Bennett S, Defoor W, Minevich E. Primary extrarenal nephrogenic<br />
rest. J Urol 2002;168:1529.<br />
146<br />
Bisceglia M, Carosi I, Castelvetere M, Murgo R. Multiple<br />
Fordyce-type angiokeratomas <strong>of</strong> <strong>the</strong> scrotum. A iatrogenic case.<br />
Pathologica 1998;90:46-50.<br />
147<br />
Popek EJ, Montgomery EA, Fourcroy JL. Fibrous hamartoma <strong>of</strong><br />
infancy in <strong>the</strong> genital region: findings in 15 cases. J Urol<br />
1994;152:990-3.<br />
148<br />
Fisher C, Bisceglia M. Solitary fibrous tumour <strong>of</strong> <strong>the</strong> spermatic<br />
cord. Br J Urol 1994;74:798-99.<br />
149<br />
Churg A. Paratesticular meso<strong>the</strong>lial proliferations. Semin Diagn<br />
Pathol 2003;20:272-8.<br />
Table XXII<br />
150<br />
Nucci MR, Fletcher CD. Vulvovaginal s<strong>of</strong>t tissue tumours: update<br />
<strong>and</strong> review. Histopathology 2000;36:97-108.<br />
151<br />
Vargas SO, Kozakewich HP, Boyd TK, Ecklund K, Fishman SJ,<br />
Laufer MR, et al. Childhood asymmetric labium majus enlargement:<br />
mimicking a neoplasm. Am J Surg Pathol 2005;29:1007-16.<br />
152<br />
Iwasa Y, Fletcher CD. Distinctive prepubertal vulval fibroma: a<br />
hi<strong>the</strong>rto unrecognized mesenchymal tumor <strong>of</strong> prepubertal girls:<br />
analysis <strong>of</strong> 11 cases. Am J Surg Pathol 2004;28:1601-8.<br />
153<br />
Novick NL. Angiokeratoma vulvae. J Am Acad Deramtol<br />
1985;12:561-3.<br />
154<br />
Michal M, Rokyta Z, Mejchar B, Pelikán K, Kummel M, Mukensnabl<br />
P. Prolapse <strong>of</strong> Fallopian tube after hysterectomy associated<br />
with exuberant angiomy<strong>of</strong>ibroblastic stroma response. A diagnostic<br />
pitfall. Virchows Arch 2000;437:436-9.<br />
155<br />
Varnholt H, Otis CN, Nucci MR, Johari VP. Fallopian tube prolapse<br />
mimicking aggressive angiomyxoma. Int J Gynecol Pathol<br />
2005;24:292-4.<br />
156<br />
Branton PA, Tavassoli FA. Spindle cell epi<strong>the</strong>lioma, <strong>the</strong> so-called<br />
mixed tumor <strong>of</strong> <strong>the</strong> vagina. A clinicopathologic, immunohistochemical,<br />
<strong>and</strong> ultrastructural analysis <strong>of</strong> 28 cases. Am J Surg<br />
Pathol 1993;17:509-15.<br />
157<br />
Skelton H, Smith KJ. Spindle cell epi<strong>the</strong>lioma <strong>of</strong> <strong>the</strong> vagina<br />
shows immunohistochemical staining supporting its origin from a<br />
primitive/progenitor cell population. Arch Pathol Lab Med<br />
2001;125:547-50.<br />
158<br />
Nucci MR, Fletcher CD. Liposarcoma (atypical lipomatous tumors)<br />
<strong>of</strong> <strong>the</strong> vulva: a clinicopathologic study <strong>of</strong> six cases. Int J<br />
Gynecol Pathol 1998;17:17-23.<br />
158a<br />
Bakotic BW, Cabello-Inchausti B, Willis IH, Suster S. Clear-cell<br />
epi<strong>the</strong>lioid leiomyoma <strong>of</strong> <strong>the</strong> round ligament. Mod Pathol<br />
1999;12:912-8.<br />
159<br />
Hassan A, Bennet A, Bhalla S, Ylagan LR, Mutch D, Dehner LP.<br />
Paraganglioma <strong>of</strong> <strong>the</strong> vagina: report <strong>of</strong> a case, including immunohistochemical<br />
<strong>and</strong> ultrastructural findings. Int J Gynecol<br />
Pathol 2003;22:404-6.<br />
160<br />
Folpe AL, Mentzel T, Lehr HA, Fisher C, Balzer BL, Weiss SW.<br />
Perivascular epi<strong>the</strong>lioid cell neoplasms <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> gynecologic<br />
origin: a clinicopathologic study <strong>of</strong> 26 cases <strong>and</strong> review<br />
<strong>of</strong> <strong>the</strong> literature. Am J Surg Pathol 2005;29:1558-75.<br />
161<br />
Banerjee SS, Coyne JD, Menasce LP, Lobo CJ, Hirsch PJ. Diagnostic<br />
lessons <strong>of</strong> mucosal melanoma with osteocartilaginous differentiation.<br />
Histopathology 1998;33:255-60.<br />
Table XXIII<br />
162<br />
Gunia S, Behrens MH, Stosiek P. Mycobacterial spindle cell
294<br />
M. BISCEGLIA ET AL.<br />
pseudotumor (MSP) <strong>of</strong> <strong>the</strong> nasal septum clinically mimicking Kaposi’s<br />
sarcoma: case report. Rhinology 2005;43:70-1.<br />
163<br />
Kindblom LG, Angervall L. Nasal polyps with atypical stroma<br />
cells: a pseudosarcomatous lesion. A light <strong>and</strong> electron-microscopic<br />
<strong>and</strong> immunohistochemical investigation with implications<br />
on <strong>the</strong> type <strong>and</strong> nature <strong>of</strong> <strong>the</strong> mesenchymal cells. Acta Pathol Microbiol<br />
Immunol Sc<strong>and</strong> 1984;92:65-72.<br />
164<br />
Nakayama M, Wenig BM, Heffner DK. Atypical stromal cells in<br />
inflammatory nasal polyps: immunohistochemical <strong>and</strong> ultrastructural<br />
analysis in defining histogenesis. Laryngoscope<br />
1995;105:127-34.<br />
165<br />
Pai SA, Naresh KN, Masih K, Ramarao C, Borges AM. Teratocarcinosarcoma<br />
<strong>of</strong> <strong>the</strong> paranasal sinuses: a clinicopathologic<br />
<strong>and</strong> immunohistochemical study. Hum Pathol 1998;29:718-22.<br />
166<br />
Kleinschmidt-DeMasters BK, Pflaumer SM, Mulgrew TD, Lillehei<br />
KO. Sinonasal teratocarcinosarcoma (“mixed olfactory neuroblastoma-craniopharyngioma”)<br />
presenting with syndrome <strong>of</strong><br />
inappropriate secretion <strong>of</strong> antidiuretic hormone. Clin Neuropathol<br />
2000;19:63-9.<br />
167<br />
Endo H, Hirose T, Kuwamura KI, Sano T. Case report: Sinonasal<br />
teratocarcinosarcoma. Pathol Int 2001;51:107-12.<br />
168<br />
Hicks DL, Moe KS. Nasal solitary fibrous tumor arising from <strong>the</strong><br />
anterior cranial fossa. Skull Base 2004;14:203-7.<br />
169<br />
Fukunaga M, Ushigome S, Nomura K, Ishikawa E. Solitary fibrous<br />
tumor <strong>of</strong> <strong>the</strong> nasal cavity <strong>and</strong> orbit. Pathol Int 1995;45:952-7.<br />
170<br />
Eichhorn JH, Dickersin GR, Bhan AK, Goodman ML. Sinonasal<br />
hemangiopericytoma. A reassessment with electron microscopy,<br />
immunohistochemistry, <strong>and</strong> long-term follow-up. Am J Surg<br />
Pathol 1990;14:856-66.<br />
171<br />
Thompson LD, Miettinen M, Wenig BM. Sinonasal-type hemangiopericytoma:<br />
a clinicopathologic <strong>and</strong> immunophenotypic<br />
analysis <strong>of</strong> 104 cases showing perivascular myoid differentiation.<br />
Am J Surg Pathol 2003;27:737-49.<br />
172<br />
Huang HY, Antonescu CR. Sinonasal smooth muscle cell tumors:<br />
a clinicopathologic <strong>and</strong> immunohistochemical analysis <strong>of</strong> 12 cases<br />
with emphasis on <strong>the</strong> low-grade end <strong>of</strong> <strong>the</strong> spectrum. Arch<br />
Pathol Lab Med 2003;127:297-304.<br />
173<br />
Bel Haj Salah M, Mekni A, Nouira K, Kharrat S, Bellil K, Bellil<br />
S, et al. Leiomyoma <strong>of</strong> <strong>the</strong> nasal cavity. A case report. Pathologica<br />
2005;97:376-7.<br />
174<br />
Kuruvilla A, Wenig BM, Humphrey DM, Heffner DK.<br />
Leiomyosarcoma <strong>of</strong> <strong>the</strong> sinonasal tract. A clinicopathologic study<br />
<strong>of</strong> nine cases. Arch Otolaryngol Head Neck Surg 1990;116:1278-86.<br />
175<br />
Banerjee SS, Eyden B, Trenholm PW, Sheikh MY, Wakamatsu<br />
K, Ancans J, et al. Monotypic angiomyolipoma <strong>of</strong> <strong>the</strong> nasal cavity:<br />
a heret<strong>of</strong>ore undescribed occurrence. Int J Surg Pathol<br />
2001;9:309-15.<br />
176<br />
Begin LR, Rochon L, Frenkiel S. Spindle cell myoepi<strong>the</strong>lioma <strong>of</strong><br />
<strong>the</strong> nasal cavity. Am J Surg Pathol 1991;15:184-90.<br />
177<br />
Iezzoni JC, Mills SE. “Undifferentiated” small round cell tumors<br />
<strong>of</strong> <strong>the</strong> sinonasal tract: differential diagnosis update. Am J Clin<br />
Pathol 2005;124:S110-21.<br />
178<br />
Magro G, Di Benedetto A, Sanges G, Scalisi F, Alaggio R. Rhabdomyomatous<br />
mesenchymal hamartoma <strong>of</strong> oral cavity: an unusual<br />
location for such a rare lesion. Virchows Arch<br />
2005;446:346-7.<br />
179<br />
Yoshihara T, Oda A, Takahashi Y, Ishii T, Yaku Y. Fibrous hamartoma<br />
<strong>of</strong> <strong>the</strong> tongue: report <strong>of</strong> a case with immunohistochemical<br />
<strong>and</strong> ultrastructural studies. Int J Pediatr Otorhinolaryngol 1995.<br />
180<br />
Schlosnagle DC, Kratochvil FJ, Wea<strong>the</strong>rs DR, McConnel FM,<br />
Campbell WG Jr. Intraoral multifocal adult rhabdomyoma. Report<br />
<strong>of</strong> a case <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Arch Pathol Lab Med<br />
1983;107:638-42.<br />
181<br />
Said-Al-Naief N, Zahurullah FR, Sciubba JJ. Oral spindle cell<br />
lipoma. Ann Diagn Pathol 2001;5:207-15.<br />
182<br />
Ide F, Shimoyama T, Horie N. Pleomorphic hyalinizing angiectactic<br />
tumor <strong>of</strong> <strong>the</strong> buccal mucosa. J Oral Pathol Med<br />
2004;33:451-3.<br />
183<br />
Ramaraj PN, Shah SP. Peripheral myxoma <strong>of</strong> maxilla. A case report.<br />
Indian J Dent Res 2003;14:67-9.<br />
184<br />
Lukinmaa PL, Hietanen J, Warfvinge G, Sane J, Tuominen S,<br />
Henriksson V, et al. Solitary fibrous tumour <strong>of</strong> <strong>the</strong> oral cavity:<br />
clinicopathological <strong>and</strong> immunohistochemical characterization<br />
<strong>of</strong> three cases. J Oral Pathol Med 2000;29:186-92.<br />
185<br />
Wu SL, Vang R, Clubb FJ Jr, Connelly JH. Solitary fibrous tumor<br />
<strong>of</strong> <strong>the</strong> tongue: report <strong>of</strong> a case with immunohistochemical <strong>and</strong> ultrastructural<br />
studies. Ann Diagn Pathol 2002;6:168-71.<br />
186<br />
Chi AC, Wea<strong>the</strong>rs DR, Folpe AL, Dunlap DT, Rasenberger K,<br />
Neville BW. Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma <strong>of</strong> <strong>the</strong> oral cavity:<br />
report <strong>of</strong> two cases <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Oral Surg Oral<br />
Med Oral Pathol Oral Radiol Endod 2005;100:717-24.<br />
187<br />
Fisher C. Clear cell sarcoma (<strong>of</strong> tendon sheath) arising in palate.<br />
AMR International Slide Seminar #39 (Case 10). November 2002<br />
(http://www.amr-seminar.org)<br />
188<br />
Fanburg-Smith JC, Miettinen M, Folpe AL, Weiss SW, Childers<br />
EL. Lingual alveolar s<strong>of</strong>t part sarcoma; 14 cases: novel clinical<br />
<strong>and</strong> morphological observations. Histopathology 2004;45:526-37.<br />
189<br />
James JA, Bali NS, Sloan P, Shanks JH. Low-grade malignant<br />
Triton tumor <strong>of</strong> <strong>the</strong> oral cavity: a case report. Oral Surg Oral Med<br />
Oral Pathol Oral Radiol Endod 2003;95:699-704.<br />
190<br />
Massarelli G, T<strong>and</strong>a F, Salis B. Synovial sarcoma <strong>of</strong> <strong>the</strong> s<strong>of</strong>t<br />
palate: report <strong>of</strong> a case. Hum Pathol 1978;9:341-5.<br />
191<br />
Sakai Y, Matsukuma S. CD34+ stromal cells <strong>and</strong> hyalinized vascular<br />
changes in <strong>the</strong> anal fibroepi<strong>the</strong>lial polyps. Histopathology<br />
2002;41:230-5.<br />
192<br />
Miettinen M, Furlong M, Sarlomo-Rikala M, Burke A, Sobin LH,<br />
et al. Gastrointestinal stromal tumors, intramural leiomyomas,<br />
<strong>and</strong> leiomyosarcomas in <strong>the</strong> rectum <strong>and</strong> anus: a clinicopathologic,<br />
immunohistochemical, <strong>and</strong> molecular genetic study <strong>of</strong> 144<br />
cases. Am J Surg Pathol 2001;25:1121-33.<br />
192a<br />
Tworek JA, Goldblum JR, Weiss SW, Greenson JK, Appelman<br />
HD. Stromal tumors <strong>of</strong> <strong>the</strong> anorectum: a clinicopathologic study<br />
<strong>of</strong> 22 cases. Am J Surg Pathol 1999;23:946-54<br />
192b<br />
Rubin BP. Gastrointestinal stromal tumours: an update.<br />
Histopathology 2006;48:83-96.<br />
Table XXV<br />
193<br />
Cook PD, Czerniak B, Chan JK, Mackay B, Ordonez NG, Ayala<br />
AG, et al. Nodular spindle-cell vascular transformation <strong>of</strong> lymph<br />
nodes. A benign process occurring predominantly in retroperitoneal<br />
lymph nodes draining carcinomas that can simulate Kaposi's<br />
sarcoma or metastatic tumor. Am J Surg Pathol<br />
1995;19:1010-20.<br />
194<br />
Bisceglia M, Nirchio V, Carosi I, Cappucci U, Decata A,<br />
Paragone T, et al. Tumor <strong>and</strong> tumor-like benign mesenchymal <strong>lesions</strong><br />
<strong>of</strong> <strong>the</strong> breast. Pathologica 1995;87:20-41.<br />
195<br />
Magro G, Michal M, Bisceglia M. Benign spindle cell tumors <strong>of</strong><br />
<strong>the</strong> mammary stroma: diagnostic criteria, classification, <strong>and</strong> histogenesis.<br />
Pathol Res Pract 2001;197:453-66.<br />
196<br />
Brogi E. Benign <strong>and</strong> malignant spindle cell <strong>lesions</strong> <strong>of</strong> <strong>the</strong> breast.<br />
Semin Diagn Pathol 2004;21:57-64.<br />
197<br />
Shin SJ, Scamman W, Gopalan A, Rosen PP. Mammary presentation<br />
<strong>of</strong> adult-type “juvenile” xanthogranuloma. Am J Surg Pathol<br />
2005;29:827-31.<br />
198<br />
Leibl S, Moinfar F. Mammary NOS-yype sarcoma with CD10 expression:<br />
a rare entity with features <strong>of</strong> myoepi<strong>the</strong>lial differentiation.<br />
Am J Surg Pathol 2006;30:450-6.<br />
199<br />
Kurian KM, Al-Nafussi A. Sarcomatoid/metaplastic carcinoma<br />
<strong>of</strong> <strong>the</strong> breast: a clinicopathological study <strong>of</strong> 12 cases.<br />
Histopathology 2002;40:58-64.<br />
199a<br />
Carter MR, Hornick JL, Lester S, Fletcher CD. Spindle cell (sar-
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 295<br />
comatoid) carcinoma <strong>of</strong> <strong>the</strong> breast: a clinicopathologic <strong>and</strong> immunohistochemical<br />
analysis <strong>of</strong> 29 cases. Am J Surg Pathol<br />
2006;30:300-9<br />
Table XXVI<br />
200<br />
Vargas SO. Fibrous umbilical polyp: a distinct fasciitis-like proliferation<br />
<strong>of</strong> early childhood with a marked male predominance.<br />
Am J Surg Pathol 2001;25:1438-42.<br />
200a<br />
Alaggio R, Ninfo V, Rosolen A, C<strong>of</strong>fin CM. Primitive myxoid<br />
mesenchymal tumor <strong>of</strong> infancy: a clinicopathologic report <strong>of</strong> 6<br />
cases. Am J Surg Pathol 2006;30:388-94<br />
200b<br />
Reis-Filho JS, Milanezi F, Ferro J, Schmitt FC. Pediatric pigmented<br />
dermat<strong>of</strong>ibrosarcoma protuberans (Bednar tumor): case<br />
report <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature with emphasis on <strong>the</strong> differential<br />
diagnosis. Pathol Res Pract 2002;198:621-6.<br />
201<br />
Casanova M, Ferrari A, Collini P, Bisogno G, Alaggio R, Cecchetto<br />
G, et al. Epi<strong>the</strong>lioid sarcoma in children <strong>and</strong> adolescents:<br />
a report from <strong>the</strong> Italian S<strong>of</strong>t Tissue Sarcoma Committee. Cancer<br />
2006;106:708-17.<br />
202<br />
Carli M, Ferrari A, Mattke A, Zanetti I, Casanova M, Bisogno G,<br />
et al. Pediatric malignant peripheral nerve sheath tumor: <strong>the</strong><br />
Italian <strong>and</strong> German s<strong>of</strong>t tissue sarcoma cooperative group. J Clin<br />
Oncol 2005;23:8422-30.<br />
203<br />
Ferrari A, Casanova M, Bisogno G, Cecchetto G, Meazza C, G<strong>and</strong>ola<br />
L, et al. Malignant vascular tumors in children <strong>and</strong> adolescents:<br />
a report from <strong>the</strong> Italian <strong>and</strong> German S<strong>of</strong>t Tissue Sarcoma<br />
Cooperative Group. Med Pediatr Oncol 2002;39:109-14.<br />
204<br />
Ferrari A, Casanova M, Bisogno G, Mattke A, Meazza C, G<strong>and</strong>ola<br />
L, et al. Clear cell sarcoma <strong>of</strong> tendons <strong>and</strong> aponeuroses in<br />
pediatric patients: a report from <strong>the</strong> Italian <strong>and</strong> German S<strong>of</strong>t Tissue<br />
Sarcoma Cooperative Group. Cancer 2002;94:3269-76.<br />
205<br />
Bisogno G, Sotti G, Nowicki Y, Ferrari A, Garaventa A, Zanetti I,<br />
et al. S<strong>of</strong>t tissue sarcoma as a second malignant neoplasm in <strong>the</strong><br />
pediatric age group. Cancer 2004;100:1758-65.<br />
Table XXVII<br />
206<br />
Winkelmann RK, Grado GL, Quimby SR, Connolly SM. Pseudosclerodermatous<br />
panniculitis after irradiation: an unusual<br />
complication <strong>of</strong> megavoltage treatment <strong>of</strong> breast carcinoma.<br />
Mayo Clin Proc 1993;68:122-7.<br />
207<br />
Kondi-Pafiti A, Grapsa D, Kontogianni-Katsarou K, Papadias K,<br />
Kairi-Vassilatou E. Ectopic decidua mimicking metastatic <strong>lesions</strong><br />
– report <strong>of</strong> three cases <strong>and</strong> review <strong>of</strong> <strong>the</strong> literature. Eur J Gynaecol<br />
Oncol 2005;26:459-61.<br />
208<br />
Billings SD, McKenney JK, Folpe AL, Hardacre MC, Weiss SW.<br />
Cutaneous angiosarcoma following breast-conserving surgery<br />
<strong>and</strong> radiation: an analysis <strong>of</strong> 27 cases. Am J Surg Pathol<br />
2004;28:781-8.<br />
209<br />
Essary LR, Wick MR. Cutaneous calciphylaxis. An underrecognized<br />
clinicopathologic entity. Am J Clin Pathol 2000;113:280-7.<br />
210<br />
McGregor DH, Mowry M, Cherian R, McAnaw M, Poole E. Nonfamilial<br />
tumoral calcinosis associated with chronic renal failure<br />
<strong>and</strong> secondary hyperparathyroidism: report <strong>of</strong> two cases with<br />
clinicopathological, immunohistochemical, <strong>and</strong> electron microscopic<br />
findings. Hum Pathol 1995;26:607-13.<br />
211<br />
Bisceglia M, Grossi GB, Panniello G, Bertani T, Cenacchi G,<br />
Pasquinelli G. Amyloidosis. Clinico-pathological picture. Part I:<br />
Nosography. Pathologica 1997;89:329-45.<br />
212<br />
Bisceglia M, Grossi GB, Panniello G, Bertani T, Cenacchi G,<br />
Pasquinelli G. Amyloidosis. Clinico-pathological pr<strong>of</strong>ile. Part II:<br />
Diagnosis. Pathologica 1998;90:57-78.<br />
213<br />
Young RH, Clement PB, McCaughey WT. Solitary fibrous tumors (‘fibrous<br />
meso<strong>the</strong>liomas’) <strong>of</strong> <strong>the</strong> peritoneum. A report <strong>of</strong> three cases <strong>and</strong><br />
a review <strong>of</strong> <strong>the</strong> literature. Arch Pathol Lab Med 1990;114:493-5.<br />
214<br />
Carney JA, Stratakis CA. Familial paraganglioma <strong>and</strong> gastric<br />
stromal sarcoma: a new syndrome distinct from <strong>the</strong> Carney triad.<br />
Am J Med Genet 2002;108:132-9.<br />
214a<br />
Perry CG, Young WF Jr, McWhinney SR, Bei T, Stergiopoulos S,<br />
Knudson RA, et al. Functioning paraganglioma <strong>and</strong> gastrointestinal<br />
stromal tumor <strong>of</strong> <strong>the</strong> jejunum in three women: syndrome<br />
or coincidence. Am J Surg Pathol 2006;30:42-9.<br />
215<br />
Deyrup AT, Lee VK, Hill CE, Cheuk W, Toh HC, Kesavan S, et<br />
al. Epstein-Barr virus-associated smooth muscle tumors are distinctive<br />
mesenchymal tumors reflecting multiple infection events:<br />
a clinicopathologic <strong>and</strong> molecular analysis <strong>of</strong> 29 tumors from 19<br />
patients. Am J Surg Pathol 2006;30:75-82.<br />
215<br />
Burke AP, Virmani R. Cardiac myxoma. A clinicopathologic<br />
study. Am J Clin Pathol 1993;100:671-80.<br />
216<br />
Burke AP, Virmani R. Sarcomas <strong>of</strong> <strong>the</strong> great vessels. A clinicopathologic<br />
study. Cancer 1993;71:1761-73.<br />
Table XXVIII<br />
217<br />
Vincent A, Farley M, Chan E, James WD. Birt-Hogg-Dube syndrome:<br />
a review <strong>of</strong> <strong>the</strong> literature <strong>and</strong> <strong>the</strong> differential diagnosis <strong>of</strong><br />
firm facial papules. J Am Acad Dermatol 2003;49:698-705.<br />
217a<br />
Bisceglia M, Carosi I, Simeone A. Tuberous sclerosis complex<br />
with polycystic kidney dsiease <strong>of</strong> adult type (adjacent gene syndrome<br />
<strong>of</strong> TSC2/ADPKD1 type). Adv Anat Pathol, submitted<br />
218<br />
Stewart NJ, Pritchard DJ, Nascimento AG, Kang YK. Lymphangiosarcoma<br />
following mastectomy. Clin Orthop Relat Res<br />
1995;320:135-41.<br />
218a<br />
Bisceglia M, Attino V, Dimitri L, Armillotta M, Centola A, D’Angelo<br />
V. Le manifestazioni cutanee ed extracutanee della neur<strong>of</strong>ibromatosi.<br />
G Ital Dermatol Venereol 2003;138:86-91.<br />
219<br />
Gorlin RJ. Nevoid basal cell carcinoma (Gorlin) syndrome. Genet<br />
Med 2004;6:530-9.<br />
220<br />
Watson J, Depasquale K, Ghaderi M, Zwillenberg S. Nevoid<br />
basal cell carcinoma syndrome <strong>and</strong> fetal rhabdomyoma: a case<br />
study. Ear Nose Throat J 2004;83:716-8.<br />
221<br />
Lee HY, Yoon CS, Sevenet N, Rajalingam V, Delattre O, Walford<br />
NQ. Rhabdoid tumor <strong>of</strong> <strong>the</strong> kidney is a component <strong>of</strong> <strong>the</strong> rhabdoid<br />
predisposition syndrome. Pediatr Dev Pathol 2002;5:395-9.<br />
222<br />
Olivier M, Goldgar DE, Sodha N, Ohgaki H, Kleihues P, Hainaut<br />
P, et al. Li-Fraumeni <strong>and</strong> related syndromes: correlation between<br />
tumor type, family structure, <strong>and</strong> TP53 genotype. Cancer Res<br />
2003;63:6643-50.<br />
Table XXIX<br />
223<br />
Ibrahim AE, Myles L, Lang DA, Ellison DW. Case <strong>of</strong> <strong>the</strong> month:<br />
June 1998 – 2 year old boy with lumbosacral mass. Brain Pathol<br />
1998;8:817-8.<br />
224<br />
Horenstein MG, Manci EA, Walker AB, Dehner LP. Lumbosacral<br />
ectopic nephrogenic rest unassociated with spinal dysraphism.<br />
Am J Surg Pathol 2004;28:1389-92.<br />
225<br />
Ober WB. Emil Zuckerk<strong>and</strong>l <strong>and</strong> his delightful little organ.<br />
Pathol Annu 1983;18:103-19.<br />
226<br />
Blecha M, Galanopolous C, Dharkar D, Salti G. Massive organ <strong>of</strong><br />
Zuckerk<strong>and</strong>l inducing small bowel obstruction. J Am Coll Surg<br />
2005;201:480-1.<br />
227<br />
Bee D, Howard P. The carotid body: a review <strong>of</strong> its anatomy,<br />
physiology <strong>and</strong> clinical importance. Monaldi Arch Chest Dis<br />
1993;48:48-53.<br />
228<br />
Wang ZY, Bisgard GE. Chronic hypoxia-induced morphological<br />
<strong>and</strong> neurochemical changes in <strong>the</strong> carotid body. Microsc Res<br />
Tech 2002;59:168-77.<br />
229<br />
Pantanowitz L, Balogh K. Significance <strong>of</strong> <strong>the</strong> juxtaoral organ (<strong>of</strong><br />
Chievitz). Head Neck 2003;25:400-5.<br />
230<br />
Ide F, Mishima K, Saito I. Juxtaoral organ <strong>of</strong> Chievitz presenting<br />
clinically as a tumour. J Clin Pathol 2003;56:789-90.<br />
231<br />
Ide F, Mishima K, Saito I. Pacinian corpuscle in <strong>the</strong> juxtaoral organ<br />
<strong>of</strong> Chievitz. J Oral Pathol Med 2004;33:443-4.<br />
232<br />
Fraitag S, Gherardi R, Wechsler J. Hyperplastic pacinian corpuscles:<br />
an uncommonly encountered lesion <strong>of</strong> <strong>the</strong> h<strong>and</strong>. J Cutan
296<br />
M. BISCEGLIA ET AL.<br />
Pathol 1994;21:457-60.<br />
233<br />
Rinaldi P, Andreini A, Ercolani C, Bernardi L, Bernardi S. Digital<br />
pacinian hyperplasia. Report <strong>of</strong> a case associated with foreign<br />
body reaction. Pathologica 2000;92:36-40.<br />
234<br />
Drut R, Galliani C. Thymic tissue in <strong>the</strong> skin: a clue to <strong>the</strong> diagnosis<br />
<strong>of</strong> <strong>the</strong> branchio-oculo-facial syndrome: report <strong>of</strong> two cases.<br />
Int J Surg Pathol 2003;11:25-8.<br />
Table XXX<br />
235<br />
Kempson RL, Fletcher CDM, Evans HL, Hendrickson MR, Sibley<br />
RK. Tumors <strong>of</strong> <strong>the</strong> S<strong>of</strong>t Tissues. Atlas <strong>of</strong> Tumor Pathology. 3 rd<br />
Series. Fascicle 30. Washington DC: AFIP 2001.<br />
236<br />
Weiss SW, Goldblum J. Benign s<strong>of</strong>t tissue tumors <strong>and</strong> pseudotumors<br />
<strong>of</strong> miscellaneous type. Ch. 36. In: Enzinger <strong>and</strong> Weiss’s S<strong>of</strong>t<br />
Tissue Tumors. 4 th Edition. St. Louis: Mosby 2001.<br />
237<br />
Fletcher CDM, Unni KK, Mertens F. World Health Organization<br />
Classification <strong>of</strong> Tumours. Pathology <strong>and</strong> Genetics <strong>of</strong> Tumors <strong>of</strong><br />
S<strong>of</strong>t Tissue <strong>and</strong> Bone. Lyon: IARC Press 2002.<br />
238<br />
Allen PW, Dymock RB, MacCormac LB. Superficial angiomyxomas<br />
with <strong>and</strong> without epi<strong>the</strong>lial components. Report <strong>of</strong> 30 tumors<br />
in 28 patients. Am J Surg Pathol 1988;12:519-30.<br />
239<br />
Siassi RM, Papadopoulos T, Matzel KE. Metastasizing aggressive<br />
angiomyxoma. N Engl J Med 1999;341:1772.<br />
240<br />
Bl<strong>and</strong>amura S, Cruz J, Faure Vergara L, Machado Puerto I, Ninfo<br />
V. Aggressive angiomyxoma: a second case <strong>of</strong> metastasis with<br />
patient’s death. Hum Pathol 2003;34:1072-4.<br />
241<br />
Nielsen GP, Young RH, Dickersin GR, Rosenberg AE. Angiomy<strong>of</strong>ibroblastoma<br />
<strong>of</strong> <strong>the</strong> vulva with sarcomatous transformation<br />
(“angiomy<strong>of</strong>ibrosarcoma”). Am J Surg Pathol 1997;21:1104-8.<br />
242<br />
Billings SD, Folpe AL, Weiss SW. Do leiomyomas <strong>of</strong> deep s<strong>of</strong>t<br />
tissue exist? An analysis <strong>of</strong> highly differentiated smooth muscle<br />
tumors <strong>of</strong> deep s<strong>of</strong>t tissue supporting two distinct subtypes. Am J<br />
Surg Pathol 2001;25:1134-42.<br />
243<br />
Miettinen M, Fetsch JF. Evaluation <strong>of</strong> biological potential <strong>of</strong><br />
smooth muscle tumours. Histopathology 2006;48:97-105.<br />
243a<br />
Hornick JL, Fletcher CD. Criteria for malignancy in nonvisceral<br />
smooth muscle tumors. Ann Diagn Pathol 2003;7:60-6.<br />
244<br />
McMenamin ME, Fletcher CD. Malignant myopericytoma: exp<strong>and</strong>ing<br />
<strong>the</strong> spectrum <strong>of</strong> tumours with myopericytic differentiation.<br />
Histopathology 2002;41:450-60.<br />
245<br />
O’Hara CD, Nascimento AG. Endo<strong>the</strong>lial <strong>lesions</strong> <strong>of</strong> s<strong>of</strong>t tissues:<br />
a review <strong>of</strong> reactive <strong>and</strong> neoplastic entities with emphasis on lowgrade<br />
malignant (“borderline”) vascular tumors. Adv Anat<br />
Pathol 2003;10:69-87.<br />
246<br />
Hunt SJ, Santa Cruz DJ. Vascular tumors <strong>of</strong> <strong>the</strong> skin: a selective<br />
review. Semin Diagn Pathol 2004;21:166-218.<br />
247<br />
White W, Shiu MH, Rosenblum MK, Erl<strong>and</strong>son RA, Woodruff<br />
JM. Cellular schwannoma. A clinicopathologic study <strong>of</strong> 57 patients<br />
<strong>and</strong> 58 tumors. Cancer 1990;66:1266-75.<br />
248<br />
Hornick JL, Fletcher CD. S<strong>of</strong>t tissue perineurioma: clinicopathologic<br />
analysis <strong>of</strong> 81 cases including those with atypical histologic<br />
features. Am J Surg Pathol 2005;29:845-58.<br />
249<br />
Hirose T, Scheithauer BW, Sano T. Perineurial malignant peripheral<br />
nerve sheath tumor (MPNST): a clinicopathologic, immunohistochemical,<br />
<strong>and</strong> ultrastructural study <strong>of</strong> seven cases. Am<br />
J Surg Pathol 1998;22:1368-78.<br />
250<br />
Zamecnik M, Michal M. Malignant peripheral nerve sheath tumor<br />
with perineurial cell differentiation (malignant perineurioma).<br />
Pathol Int 1999;49:69-73.<br />
251<br />
Rosenberg AS, Langee CL, Stevens GL, Morgan MB. Malignant<br />
peripheral nerve sheath tumor with perineurial differentiation:<br />
“malignant perineurioma”. J Cutan Pathol 2002;29:362-7.<br />
252<br />
Michal M, Neubauer L, Fakan F. Carcinoma arising in ectopic<br />
hamartomatous thymoma. An ultrastructural study. Pathol Res<br />
Pract 1996;192:610-8.<br />
253<br />
Guillou L, Gebhard S, Salmeron M, et al. Metastasizing fibrous<br />
histiocytoma <strong>of</strong> <strong>the</strong> skin: a clinicopathologic <strong>and</strong> immunohistochemical<br />
analysis <strong>of</strong> three cases. Mod Pathol 2000;13:654-60.<br />
254<br />
Folpe AL, Weiss SW. Pleomorphic hyalinizing angiectatic tumor:<br />
analysis <strong>of</strong> 41 cases supporting evolution from a distinctive precursor<br />
lesion. Am J Surg Pathol 2004;28:1417-25.<br />
255<br />
Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical<br />
<strong>and</strong> malignant glomus tumors: analysis <strong>of</strong> 52 cases, with a proposal<br />
for <strong>the</strong> reclassification <strong>of</strong> glomus tumors. Am J Surg Pathol<br />
2001;25:1-12.<br />
256<br />
Oliveira AM, Dei Tos AP, Fletcher CD, Nascimento AG. Primary<br />
giant cell tumor <strong>of</strong> s<strong>of</strong>t tissues: a study <strong>of</strong> 22 cases. Am J Surg<br />
Pathol 2000;24:248-56.<br />
257<br />
Billings SD, Giblen G, Fanburg-Smith JC. Superficial low-grade<br />
fibromyxoid sarcoma (Evans tumor): a clinicopathologic analysis<br />
<strong>of</strong> 19 cases with a unique observation in <strong>the</strong> pediatric population.<br />
Am J Surg Pathol 2005;29:204-10.<br />
258<br />
Bisceglia M, Vairo M, Calonje E, Fletcher CD. Pigmented fibrosarcomatous<br />
dermat<strong>of</strong>ibrosarcoma protuberans (Bednar tumor).<br />
3 case reports, analogy with <strong>the</strong> “conventional” type <strong>and</strong><br />
review <strong>of</strong> <strong>the</strong> literature. Pathologica 1997;89:264-73.<br />
259<br />
Mentzel T, Beham A, Katenkamp D, Dei Tos AP, Fletcher CD. Fibrosarcomatous<br />
(“high-grade”) dermat<strong>of</strong>ibrosarcoma protuberans:<br />
clinicopathologic <strong>and</strong> immunohistochemical study <strong>of</strong> a series<br />
<strong>of</strong> 41 cases with emphasis on prognostic significance. Am J<br />
Surg Pathol 1998;22:576-87.<br />
260<br />
Abbott JJ, Oliveira AM, Nascimento AG. The prognostic significance<br />
<strong>of</strong> fibrosarcomatous transformation in dermat<strong>of</strong>ibrosarcoma<br />
protuberans. Am J Surg Pathol 2006;30:436-43.<br />
261<br />
Espat NJ, Lewis JJ, Leung D, Woodruff JM, Antonescu CR, Shia<br />
J, et al. Conventional hemangiopericytoma: modern analysis <strong>of</strong><br />
outcome. Cancer 2002;95:1746-51.<br />
262<br />
Antonescu CR, Argani P, Erl<strong>and</strong>son RA, Healey JH, Ladanyi M,<br />
Huvos AG. Skeletal <strong>and</strong> extraskeletal myxoid chondrosarcoma: a<br />
comparative clinicopathologic, ultrastructural, <strong>and</strong> molecular<br />
study. Cancer 1998;83:1504-21.<br />
263<br />
Suster S. Malignant glomus tumor with systemic metastases.<br />
AMR International Slide Seminar #14 (Case 11). March 1994<br />
(http://www.amr-seminar.org).<br />
264<br />
Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG.<br />
Malignant granular cell tumor <strong>of</strong> s<strong>of</strong>t tissue: diagnostic criteria<br />
<strong>and</strong> clinicopathologic correlation. Am J Surg Pathol<br />
1998;22:779-94.<br />
265<br />
Costa J, Wesley RA, Glatstein E, Rosenberg SA. The grading <strong>of</strong><br />
s<strong>of</strong>t tissue sarcomas. Results <strong>of</strong> a clinicohistopathologic correlation<br />
in a series <strong>of</strong> 163 cases. Cancer 1984;53:530-41.<br />
266<br />
Trojani M, Contesso G, Coindre JM, Rouesse J, Bui NB, de Mascarel<br />
A, et al. S<strong>of</strong>t-tissue sarcomas <strong>of</strong> adults; study <strong>of</strong> pathological<br />
prognostic variables <strong>and</strong> definition <strong>of</strong> a histopathological<br />
grading system. Int J Cancer 1984;33:37-42.<br />
267<br />
Coindre JM, Trojani M, Contesso G, David M, Rouesse J, Bui<br />
NB, et al. Reproducibility <strong>of</strong> a histopathologic grading system for<br />
adult s<strong>of</strong>t tissue sarcoma. Cancer 1986;58:306-9.<br />
268<br />
Guillou L, Coindre JM, Bonichon F, Nguyen BB, Terrier P, Collin<br />
F, et al. Comparative study <strong>of</strong> <strong>the</strong> National Cancer Institute <strong>and</strong><br />
French Federation <strong>of</strong> Cancer Centers Sarcoma Group grading<br />
systems in a population <strong>of</strong> 410 adult patients with s<strong>of</strong>t tissue sarcoma.<br />
J Clin Oncol 1997;15:350-62.<br />
269<br />
Association <strong>of</strong> Directors <strong>of</strong> Anatomic <strong>and</strong> Surgical Pathology.<br />
Recommendations for <strong>the</strong> reporting <strong>of</strong> s<strong>of</strong>t tissue sarcomas. Mod<br />
Pathol 1998;11:1257-61.<br />
270<br />
Oliveira AM, Nascimento AG. Grading in s<strong>of</strong>t tissue tumors:<br />
principles <strong>and</strong> problems. Skeletal Radiol 2001;30:543-59.<br />
271<br />
Deyrup AT, Weiss SW. Grading <strong>of</strong> s<strong>of</strong>t tissue sarcomas: <strong>the</strong> challenge<br />
<strong>of</strong> providing precise information in an imprecise world.<br />
Histopathology 2006;48:42-50.<br />
272<br />
UICC. TNM Classification <strong>of</strong> malignant tumors. 6th Edition.<br />
Hoboken, New Jersey: John Wiley & Sons 2002.
TUMORAL, QUASITUMORAL AND PSEUDOTUMORAL LESIONS OF SOFT TISSUE - APPENDIX 297<br />
Index<br />
This Index lists alphabetically only those entities which appeared in <strong>the</strong> several preceding Excerpta.<br />
In paren<strong>the</strong>sis is <strong>the</strong> reference to <strong>the</strong> particular Excerpta published in Pathologica which describes <strong>the</strong> entity in detail.<br />
Acquired elastotic hemangioma (2005;97:10-22 / IV-1).<br />
Acral inflammatory myxohyaline tumor with Reed-Sternberg-like cells (2004;96:436-63 / II-8)<br />
Amyloid tumor (2006;98:187-208 / IX-3)<br />
Angiomy<strong>of</strong>ibroblastoma <strong>of</strong> vulva (2004;96:436-63 / II-4)<br />
Atypical decubital fibroplasia (2005;97:394-408 / VIII-4)<br />
Atypical fibroxanthoma - non-pleomorphic spindle-cell (2004;96:121-42; I-2)<br />
Atypical fibroxanthoma - aneurysmal (pigmented) variants (2004;96:121-42; I-2)<br />
Bacillary epi<strong>the</strong>lioid angiomatosis (2005;97:394-408 / VIII-6)<br />
Bednar tumor - fibrosarcomatous (2004;96:121-42 / I-1)<br />
Bizarre parosteal osteochondromatous proliferation (2006;98:187-208 / IX-1)<br />
Calcifying fibrous (pseudo)tumor (2004;96:436-63 / II-7)<br />
Calcium pyrophosphate dehydrate crystals deposition disease (tumoral form) (2006;98:187-208 / IX-4)<br />
Castleman’s disease <strong>of</strong> <strong>the</strong> subcutis <strong>and</strong> skeletal muscle (2005;97:141-57 / VI-5)<br />
Chondroid lipoma (2004;96:481-95 / III-2)<br />
CPPD (calcium pyrophosphate dihydrate) crystals deposition disease (2006;98:187-208 / IX-2)<br />
Dabska tumor arising on lymphangioma (2005;97:10-22 / IV-4)<br />
Dabska’s parachordoma (2005;97:343-60 / VII-2)<br />
Dendritic cell neur<strong>of</strong>ibroma with pseudorosettes (2005;97:92-114 / V-3)<br />
Dendritic fibromyxolipoma (2004;96:481-95 / III-3)<br />
Dermat<strong>of</strong>ibrosarcoma protuberans – sarcomatous, classic type (2004;96:121-42 / I-1)<br />
Dermat<strong>of</strong>ibrosarcoma protuberans – sarcomatous, pigmented variant (2004;96:121-42 / I-1)<br />
Dermatomy<strong>of</strong>ibroma (2004;96:436-63 / II-1)<br />
Desmoplastic fibroblastoma (2004;96:121-42 / I-6)<br />
Ectopic hamartomatous thymoma (2005;97:394-408 / VIII-1)<br />
Epi<strong>the</strong>lial sheath neuroma (2005;97:92-114 / V-4)<br />
Epi<strong>the</strong>lioid hemangioendo<strong>the</strong>lioma <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> skin (2005;97:10-22 / IV-2)<br />
Epi<strong>the</strong>lioid leiomyosarcoma (2004;96:481-95 / III-6)<br />
Epi<strong>the</strong>lioid liposarcoma (2004;96:481-95 / III-4)<br />
Epi<strong>the</strong>lioid psammomatous melanotic schwannoma (2005;97:92-114 / V-1)<br />
Ewing’s sarcoma <strong>of</strong> <strong>the</strong> skin (2005;97:92-114 / V-6)<br />
Extraneural perineurioma (2005;97:92-114 / V-5B)<br />
Extraneuraxial hemangioblastoma <strong>of</strong> s<strong>of</strong>t tissue <strong>and</strong> skin (2005;97:10-22 / IV-3)<br />
Extra-renal malignant rhabdoid tumour (2005;97:141-57 / VI-3)<br />
Extraskeletal myxoid chondrosarcoma with neuroendocrine differentiation (2005;97:141-57 / VI-1)<br />
Fibroosseous pseudotumor <strong>of</strong> <strong>the</strong> digits (2006;98:187-208 / IX-1)<br />
Fibrosarcomatous dermat<strong>of</strong>ibrosarcoma protuberans, classic type (2004;96:121-42 / I-1)<br />
Fibrosarcomatous Bednar tumor (dermat<strong>of</strong>ibrosarcoma protuberans, pigmented type) (2004;96:121-42 / I-1)<br />
Florid reactive periostitis <strong>of</strong> <strong>the</strong> tubular bones <strong>of</strong> <strong>the</strong> h<strong>and</strong>s <strong>and</strong> feet (2006;98:187-208 / IX-2)<br />
Follicular dendritic cell sarcoma (2005;97:141-57 / VI-4)<br />
Glomus coccygeum (2006;98:187-208 / IX-4))<br />
Granular cell leiomyosarcoma (2004;96:481-95 / III-7)<br />
Hamartoma <strong>of</strong> <strong>the</strong> scalp with ectopic meningo<strong>the</strong>lial elements (2005;97:394-408 / VIII-2)<br />
Hemosiderotic fibrohistiocytic lipomatous lesion (2004;96:121-42 / I-4)<br />
Hyaline cell-rich chondroid syringoma (2005;97:343-60 / VII-1C)<br />
Hyalinizing spindle cell tumor with giant rosettes (2004;96:436-63 / II-11)<br />
Inflammatory my<strong>of</strong>ibroblastic tumor (2004;96:436-63 / II-6)<br />
Inflammatory pseudotumor (2004;96:436-63 / II-6)<br />
Inflammatory myxo-hyaline tumor (2004;96:436-63 / II-8)<br />
Intranodal hemorrhagic spindle cell tumor with “amianthoid” fibers (2004;96:436-63 / II-2)<br />
Intraneural perineurioma (2005;97:92-114 / V-5A)<br />
Ischemic fasciitis (2005;97:394-408 / VIII-4)
298<br />
M. BISCEGLIA ET AL.<br />
Juxtarticular myxoma (2004;96:436-63 / II-9)<br />
Lipoleiomyosarcoma (2004;96:481-95 / III-5)<br />
Lipomatous hemangiopericytoma (2004;96:436-63 / II-5)<br />
Localized hypertrophic (mono)neuropathy (2005;97:92-114 / V-5A)<br />
Low grade fibromyxoid sarcoma (2004;96:436-63 / II-11)<br />
Mixed tumor (2005;97:343-60 / VII-1A)<br />
Myoepi<strong>the</strong>lioma (2005;97:343-60 / VII-1B)<br />
My<strong>of</strong>ibrosarcoma (2004;96:436-63 / II-3)<br />
Myxoinflammatory fibroblastic sarcoma (2004;96:436-63 / II-8)<br />
Nephrogenic fibrosing dermopathy (2005;97:394-408 / VIII-5)<br />
Neural fibrolipomatous hamartoma (2005;97:394-408 / VIII-3)<br />
Nora’s lesion (2006;98:187-208 / IX-1)<br />
Nuchal-type fibroma (2004;96:121-42 / I-5)<br />
Oncocytoma (2005;97:343-60 / VII-3)<br />
Ossifying fibromyxoid tumor (2004;96:436-63 / II-10)<br />
Palisaded my<strong>of</strong>ibroblastoma (2004;96:436-63 / II-2)<br />
Perineuriomas - intraneural <strong>and</strong> extraneural forms (2005;97:92-114 / V-5)<br />
Pigmented neur<strong>of</strong>ibroma (2005;97:92-114 / V-2)<br />
Phosphaturic mesenchymal tumor (2004;96:481-95 / III-1)<br />
Pleomorphic hyalinizing angiectatic tumor (2004; 96:121-42 / I-8)<br />
Plexiform fibrohistiocytic tumor (2004;96:121-42 / I-3)<br />
Plexiform xanthomatous tumor (2005;97:141-57 / VI-7)<br />
Post-implant parathyromatosis (in heterotopic locations) (2006;98:187-208 / IX-5)<br />
Proximal-type epi<strong>the</strong>lioid sarcoma (2005;97:141-57 / VI-2)<br />
Rosai-Dorfman disease <strong>of</strong> s<strong>of</strong>t tissue (2005;97:141-57 / VI-6)<br />
Rudimentary meningocele (2005;97:394-408 / VIII-2)<br />
Sclerosing epi<strong>the</strong>lioid fibrosarcoma (2004; 96:121-42 / I-9).<br />
S<strong>of</strong>t tissue perineurioma (2005;97:92-114 / V-5B)<br />
Solitary fibrous tumor (2004;96:121-42 / I-7)<br />
Superficial angiomyxoma (2004;96:436-63 / II-9)<br />
Tophaceous pseudogout (2006;98:187-208 / IX-2)<br />
<strong>Tumoral</strong> calcium pyrophosphate dihydrate crystals deposition disease (CPPDCDD) (2006;98:187-208 / IX-2)