2004 Summer Meeting - Amsterdam - The Pathological Society of ...
2004 Summer Meeting - Amsterdam - The Pathological Society of ...
2004 Summer Meeting - Amsterdam - The Pathological Society of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
121<br />
<strong>The</strong> correlation between phenotypic expression and tumor<br />
development in colorectal epithelia tumors<br />
T Yao , K Nishiyama , M Tsuneyoshi<br />
Kyushu University, Fukuoka, Japan<br />
<strong>The</strong> purpose <strong>of</strong> this study is to clarify the correlation between the phenotypic<br />
expression and tumor development. Colorectal adenomas and adenocarcinomas<br />
were randomly selected, including 236 tubular (15 low-grade adenoma, highgrade<br />
adenoma 34, invasive carcinoma 187) and 60 villous (low-grade adenoma<br />
15, high-grade adenoma 23, invasive carcinoma 22) tumors. By the<br />
combination <strong>of</strong> expression CD10, MUC2 and human gastric mucin, the lesions<br />
were classified into five types, large intestinal (LI), mixed (Mix), small<br />
intestinal (SI-type), gastric (G-type) and unclassified (UC) types.<br />
Villous tumors revealed higher incidence <strong>of</strong> Mix-type (60% in low-grade<br />
and 83% in high-grade adenomas) than tubular tumor did (13% in low-grade<br />
and 6% in high-grade adenomas). On the other hand, tubular tumors contained<br />
SI-type (35% in high-grade adenoma and 22% in invasive carcinoma),<br />
however, no villous tumors revealed SI-type. In tubular tumors, polypoid<br />
growth carcinomas revealed similar phenotypic expression to tubular<br />
adenomas, but they revealed different phenotypes from non-polypoid ones. In<br />
addition, higher incidence <strong>of</strong> venous invasion was seen in SI-type.<br />
In conclusion, the different carcinogenetic pathway is suggested between<br />
villous and tubular tumors and between polypiod and non-polypiod carcinomas.<br />
Such phenotypic classification is also useful for evaluation <strong>of</strong> the biological<br />
behavior.<br />
122<br />
Audit Of Compliance With Upper GI Cancer Minimum<br />
Datasets<br />
A BISWAS , KP WEST<br />
LEICESTER ROYAL INFIRMARY, LEICESTER, United Kingdom<br />
Minimum datasets assist pathologists in providing clinically useful and relevant<br />
information in surgical pathology reports. <strong>The</strong> purpose <strong>of</strong> this study was to<br />
audit the compliance <strong>of</strong> upper GI cancer reports with the minimum datasets for<br />
oesophageal and gastric cancers.<br />
We included all upper GI cancer resection specimens reported during the period<br />
2001 to 2003 at Leicester. <strong>The</strong>re were 225 cases, comprising gastric<br />
adenocarcinomas (56%), oesophageal adenocarcinomas (20.2%), gastro<br />
oesophageal adenocarcinomas (14.8%), oesophageal squamous cell carcinomas<br />
(7%) and others (2%). In spite <strong>of</strong> the free text style <strong>of</strong> reporting, pathologists<br />
were generally compliant with the relevant minimum datasets. We assessed the<br />
impact <strong>of</strong> using minimum datasets by comparing the present group with a<br />
randomised collection <strong>of</strong> 100 cases from 1998.<br />
Overall, present day surgical pathology reports are more likely to contain<br />
prognostically relevant data like circumferential margin status in lower<br />
oesophageal cancers (98% versus 82%), lymphovascular invasion (84% versus<br />
72%) and character <strong>of</strong> invasive margin in gastric cancers (70% versus 53%). A<br />
significant improvement in the prognostic value <strong>of</strong> the reports was readily<br />
apparent with the incorporation <strong>of</strong> minimum datasets in reporting <strong>of</strong> upper GI<br />
cancers.<br />
123<br />
Dysplasia Risk and Subtypes <strong>of</strong> Intestinal Metaplasia in<br />
Barrett’s Mucosa<br />
LJ Neilson , RC Stuart , JJ Going<br />
University <strong>of</strong> Glasgow, Glasgow, United Kingdom<br />
Dysplasia is strongly associated with intestinal metaplasia (IM) but not with<br />
non-intestinal metaplastic mucosal phenotypes (cardiac, fundic) which also<br />
occur in Barrett’s mucosa. This study sought to investigate whether the risk <strong>of</strong><br />
dysplasia in Barrett’s metaplasia varies between IM subtypes (type 1 or<br />
complete IM and the two subtypes <strong>of</strong> incomplete IM defined by the absence<br />
(IIa) or presence (IIb) <strong>of</strong> sulphomucins in columnar cells).<br />
Biopsies from a total <strong>of</strong> 812 oesophageal sites (excluding the OG junction) in<br />
long-segment Barrett’s oesophagus patients were stained with High Iron<br />
Diamine / Alcian Blue pH 2.5 to reveal acidic and sulphated mucins and were<br />
scored for the presence <strong>of</strong> type I IM (with a brush border and negligible<br />
alcianophilia <strong>of</strong> columnar cells), type IIa IM and type IIb IM (as defined<br />
above). Dysplasia was grouped as either absent (no atypia or reactive only)<br />
versus probable and definite dysplasia. <strong>The</strong> table shows observed and (exected)<br />
numbers <strong>of</strong> biopsies by dysplasia category and IM type:<br />
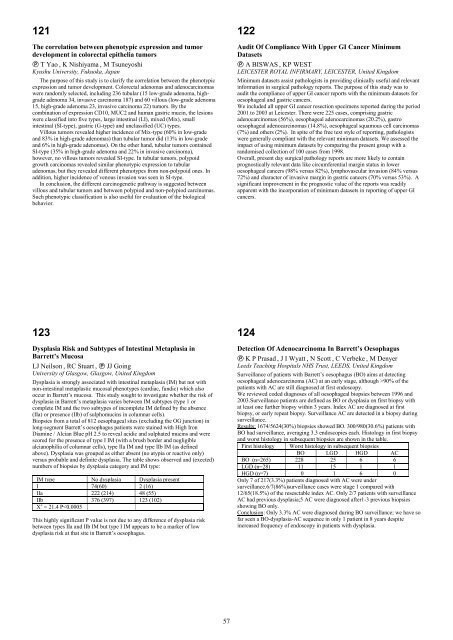
IM type No dysplasia Dysplasia present<br />
I 74(60) 2 (16)<br />
IIa 222 (214) 48 (55)<br />
IIb 376 (397) 123 (102)<br />
2 = 21.4 P90% <strong>of</strong> the<br />
patients with AC are still diagnosed at first endoscopy.<br />
We reviewed coded diagnoses <strong>of</strong> all oesophageal biopsies between 1996 and<br />
2003.Surveillance patients are defined as BO or dysplasia on first biopsy with<br />
at least one further biopsy within 3 years. Index AC are diagnosed at first<br />
biopsy, or early repeat biopsy. Surveillance AC are detected in a biopsy during<br />
surveillance.<br />
Results: 1674/5624(30%) biopsies showed BO. 300/980(30.6%) patients with<br />
BO had surveillance, averaging 3.3 endoscopies each. Histology in first biopsy<br />
and worst histology in subsequent biopsies are shown in the table.<br />
First histology Worst histology in subsequent biopsies<br />
BO LGD HGD AC<br />
BO (n=265) 228 25 6 6<br />
LGD (n=28) 11 15 1 1<br />
HGD (n=7) 0 1 6 0<br />
Only 7 <strong>of</strong> 217(3.3%) patients diagnosed with AC were under<br />
surveillance.6/7(86%)surveillance cases were stage 1 compared with<br />
12/65(18.5%) <strong>of</strong> the resesctable index AC. Only 2/7 patients with surveillance<br />
AC had previous dysplasia;5 AC were diagnosed after1-3 previous biopsies<br />
showing BO only.<br />
Conclusion: Only 3.3% AC were diagnosed during BO surveillance; we have so<br />
far seen a BO-dysplasia-AC sequence in only 1 patient in 8 years despite<br />
increased frequency <strong>of</strong> endoscopy in patients with dysplasia.<br />
57