Guidelines for the management of community ... - Brit Thoracic
Guidelines for the management of community ... - Brit Thoracic
Guidelines for the management of community ... - Brit Thoracic
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
BTS guidelines<br />
Recommendations<br />
c<br />
c<br />
c<br />
Most patients with low severity CAP can be adequately<br />
treated with oral antibiotics. [C]<br />
Oral <strong>the</strong>rapy with amoxicillin is preferred <strong>for</strong> patients<br />
with low severity CAP who require hospital admission<br />
<strong>for</strong> o<strong>the</strong>r reasons such as unstable comorbid illnesses<br />
or social needs. [D]<br />
When oral <strong>the</strong>rapy is contraindicated, recommended<br />
parenteral choices include intravenous amoxicillin or<br />
benzylpenicillin, or clarithromycin. [D]<br />
8.11 Empirical antibiotic choice <strong>for</strong> adults hospitalised with<br />
moderate severity CAP<br />
The principles <strong>of</strong> antibiotic selection <strong>for</strong> moderate severity CAP<br />
managed in hospital are similar to those <strong>for</strong> its <strong>management</strong> in<br />
<strong>the</strong> <strong>community</strong>. The current guidelines incorporate a stratified<br />
approach based on disease severity (see Section 6). The<br />
predominant pathogen will be S pneumoniae. However, overall<br />
atypical pathogens including Legionella spp account <strong>for</strong> approximately<br />
20% <strong>of</strong> defined infections. There<strong>for</strong>e, in patients who are<br />
admitted with moderate severity disease, oral <strong>the</strong>rapy with a<br />
combined b-lactam/macrolide regimen is recommended.<br />
When oral <strong>the</strong>rapy is inappropriate, parenteral amoxicillin or<br />
penicillin G are <strong>of</strong>fered as alternatives to oral amoxicillin, with<br />
clarithromycin given twice a day as <strong>the</strong> preferred macrolide <strong>for</strong><br />
parenteral <strong>the</strong>rapy.<br />
For patients intolerant <strong>of</strong> penicillin and in whom oral <strong>the</strong>rapy<br />
is inappropriate, intravenous lev<strong>of</strong>loxacin once daily or a<br />
combination <strong>of</strong> intravenous cephalosporin with intravenous<br />
clarithromycin are appropriate alternative choices. Institutions<br />
wishing to avoid <strong>the</strong> use <strong>of</strong> quinolones and cephalosporins in<br />
<strong>the</strong>se patients may wish to consider mono<strong>the</strong>rapy with<br />
intravenous clarithromycin, but must weigh <strong>the</strong> ecological<br />
benefit <strong>of</strong> this strategy against <strong>the</strong> risk <strong>of</strong> undertreating<br />
pneumococcal pneumonia (erythromycin resistance <strong>of</strong> about<br />
9%; see Section 8.3 and fig 9).<br />
Recommendations<br />
c Most patients with moderate severity CAP can be<br />
adequately treated with oral antibiotics. [C]<br />
c Oral <strong>the</strong>rapy with amoxicillin and a macrolide is<br />
preferred <strong>for</strong> patients with moderate severity CAP<br />
who require hospital admission. [D]<br />
– Mono<strong>the</strong>rapy with a macrolide may be suitable <strong>for</strong><br />
patients who have failed to respond to an adequate<br />
course <strong>of</strong> amoxicillin prior to admission. Deciding on<br />
<strong>the</strong> adequacy <strong>of</strong> prior <strong>the</strong>rapy is difficult and is a<br />
matter <strong>of</strong> individual clinical judgement. It is <strong>the</strong>re<strong>for</strong>e<br />
recommended that combination antibiotic <strong>the</strong>rapy<br />
is <strong>the</strong> preferred choice in this situation and that<br />
<strong>the</strong> decision to adopt mono<strong>the</strong>rapy is reviewed on<br />
<strong>the</strong> ‘‘post take’’ round within <strong>the</strong> first 24 h <strong>of</strong><br />
admission. [D]<br />
c When oral <strong>the</strong>rapy is contraindicated, <strong>the</strong> preferred<br />
parenteral choices include intravenous amoxicillin or<br />
benzylpenicillin, toge<strong>the</strong>r with clarithromycin. [D]<br />
c For those intolerant <strong>of</strong> penicillins or macrolides, oral<br />
doxycyline is <strong>the</strong> main alternative agent. Oral lev<strong>of</strong>loxacin<br />
and oral moxifloxacin are o<strong>the</strong>r alternative<br />
choices. [D]<br />
c When oral <strong>the</strong>rapy is contraindicated in those intolerant<br />
<strong>of</strong> penicillins, recommended parenteral choices<br />
include lev<strong>of</strong>loxacin mono<strong>the</strong>rapy or a second-generation<br />
(eg, cefuroxime) or third-generation (eg, cefotaxime<br />
or ceftriaxone) cephalosporin toge<strong>the</strong>r with<br />
clarithromycin. [D]<br />
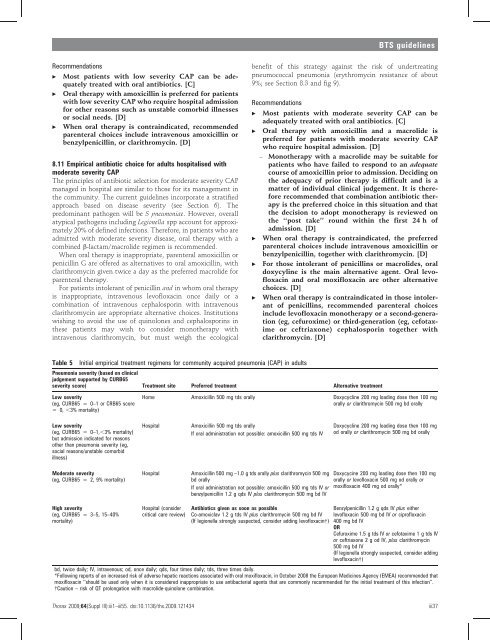
Table 5<br />
Initial empirical treatment regimens <strong>for</strong> <strong>community</strong> acquired pneumonia (CAP) in adults<br />
Pneumonia severity (based on clinical<br />
judgement supported by CURB65<br />
severity score) Treatment site Preferred treatment Alternative treatment<br />
Low severity<br />
(eg, CURB65 = 0–1 or CRB65 score<br />
= 0, ,3% mortality)<br />
Home Amoxicillin 500 mg tds orally Doxycycline 200 mg loading dose <strong>the</strong>n 100 mg<br />
orally or clarithromycin 500 mg bd orally<br />
Low severity<br />
(eg, CURB65 = 0–1,,3% mortality)<br />
but admission indicated <strong>for</strong> reasons<br />
o<strong>the</strong>r than pneumonia severity (eg,<br />
social reasons/unstable comorbid<br />
illness)<br />
Hospital<br />
Amoxicillin 500 mg tds orally<br />
If oral administration not possible: amoxicillin 500 mg tds IV<br />
Doxycycline 200 mg loading dose <strong>the</strong>n 100 mg<br />
od orally or clarithromycin 500 mg bd orally<br />
Moderate severity<br />
(eg, CURB65 = 2, 9% mortality)<br />
Hospital<br />
Amoxicillin 500 mg –1.0 g tds orally plus clarithromycin 500 mg<br />
bd orally<br />
If oral administration not possible: amoxicillin 500 mg tds IV or<br />
benzylpenicillin 1.2 g qds IV plus clarithromycin 500 mg bd IV<br />
Doxycycine 200 mg loading dose <strong>the</strong>n 100 mg<br />
orally or lev<strong>of</strong>loxacin 500 mg od orally or<br />
moxifloxacin 400 mg od orally*<br />
High severity<br />
(eg, CURB65 = 3–5, 15–40%<br />
mortality)<br />
Hospital (consider<br />
critical care review)<br />
Antibiotics given as soon as possible<br />
Co-amoxiclav 1.2 g tds IV plus clarithromycin 500 mg bd IV<br />
(If legionella strongly suspected, consider adding lev<strong>of</strong>loxacin{)<br />
Benzylpenicillin 1.2 g qds IV plus ei<strong>the</strong>r<br />
lev<strong>of</strong>loxacin 500 mg bd IV or cipr<strong>of</strong>loxacin<br />
400 mg bd IV<br />
OR<br />
Cefuroxime 1.5 g tds IV or cefotaxime 1 g tds IV<br />
or ceftriaxone 2 g od IV, plus clarithromycin<br />
500 mg bd IV<br />
(If legionella strongly suspected, consider adding<br />
lev<strong>of</strong>loxacin{)<br />
bd, twice daily; IV, intravenous; od, once daily; qds, four times daily; tds, three times daily.<br />
*Following reports <strong>of</strong> an increased risk <strong>of</strong> adverse hepatic reactions associated with oral moxifloxacin, in October 2008 <strong>the</strong> European Medicines Agency (EMEA) recommended that<br />
moxifloxacin ‘‘should be used only when it is considered inappropriate to use antibacterial agents that are commonly recommended <strong>for</strong> <strong>the</strong> initial treatment <strong>of</strong> this infection’’.<br />
{Caution – risk <strong>of</strong> QT prolongation with macrolide-quinolone combination.<br />
Thorax 2009;64(Suppl III):iii1–iii55. doi:10.1136/thx.2009.121434<br />
iii37