the archdiocese of new york benefits administration resource guide
the archdiocese of new york benefits administration resource guide
the archdiocese of new york benefits administration resource guide
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
THE ARCHDIOCESE OF NEW YORK<br />
BENEFITS ADMINISTRATION<br />
RESOURCE GUIDE<br />
Administration Procedures for Plans Sponsored by <strong>the</strong> Archdiocese <strong>of</strong> New York
THE ARCHDIOCESE OF NEW YORK<br />
MISSION STATEMENT<br />
The beliefs and principles <strong>of</strong> <strong>the</strong> Catholic Faith serve as <strong>the</strong><br />
basis for <strong>the</strong> operation <strong>of</strong> <strong>the</strong> Archdiocese <strong>of</strong> New York and its<br />
constituent members as expressed in <strong>the</strong> following mission<br />
statement.<br />
We, <strong>the</strong> Catholic People <strong>of</strong> God <strong>of</strong> <strong>the</strong> Archdiocese <strong>of</strong> New<br />
York have a mission, given by <strong>the</strong> Lord Himself, to live and<br />
proclaim His gospel message. This mission, entrusted by Jesus,<br />
calls us to be aware <strong>of</strong> <strong>the</strong> local area and <strong>the</strong> world, <strong>the</strong> spiritual<br />
and <strong>the</strong> material, <strong>the</strong> present and <strong>the</strong> future. The same gospel<br />
that challenges us is also our consolation. The same Lord who<br />
commanded, “Go <strong>the</strong>refore and make disciples <strong>of</strong> all nations,”<br />
added, “I am with you always, until <strong>the</strong> end <strong>of</strong> <strong>the</strong> world.”<br />
(Mat<strong>the</strong>w 28:19-20)
THE ARCHDIOCESE OF NEW YORK<br />
BENEFITS ADMINISTRATION RESOURCE GUIDE<br />
TABLE OF CONTENTS<br />
I. Important Information: Page<br />
- Important Notice 1<br />
- New Employee Checklist 2<br />
- Benefits Administrator’s Resource Contacts List 3<br />
- Rules For Member Groups Participating in <strong>the</strong> Archdiocesan Group Insurance Plan 4<br />
- Benefits Eligibility Outline 5<br />
- AONY Division Claim Codes 6<br />
- Change <strong>of</strong> Contact 7<br />
II.<br />
Administration <strong>of</strong> Group Health Benefit Plan:<br />
- HIPAA (Health Insurance Portability & Accountability): Notice <strong>of</strong> Privacy Practices 8<br />
- AONY Authorization For Release <strong>of</strong> Information 9<br />
- United Healthcare Authorization for Use and Disclosure <strong>of</strong> Private Health Information 10<br />
- AONY Group Health Benefits Eligibility 11<br />
- How to Enroll in <strong>the</strong> Group Health Benefit Plan and/or Make Changes to a Member’s<br />
Group AONY Health Benefit Coverage or Change Personal Information 12<br />
- Certification for Disabled Dependent Children over <strong>the</strong> age nineteen (19) 13<br />
- Certification <strong>of</strong> Disability for <strong>the</strong> Disabled Children’s Provision Form 14<br />
III.<br />
Benefits Summaries:<br />
- Summary <strong>of</strong> Benefits: For Clergy, Religious, Seminarians & Lay Employees 15<br />
- Summary <strong>of</strong> Benefits: For Bargaining Lay Faculty 16<br />
- Summary <strong>of</strong> Benefits: For Medicare Supplement for Retired Lay Employees over<br />
age 65, Clergy and Religious Who have Medicare Primary Benefits (MSYRX) 17<br />
IV.<br />
Filing for Claims:<br />
- How to File a Medical Claim (Instructions) 18<br />
- Prescription Benefit Summary 19<br />
- How to File a Claim for Prescription Drugs (Instructions) 20<br />
V. When Group Health Benefit Coverage Ends……..<br />
- Important Notice (Administration Instructions): for completing Benefit Transfer, 21<br />
Termination and Reinstatement Transmittal Form<br />
- Benefit Transfer, Termination and Reinstatement Transmittal Form 22<br />
- Group Health Benefits For Employees Separating From Service 23<br />
- (Sample Letter) Notice to Member Losing Coverage 24<br />
- AONY Notice <strong>of</strong> Group Benefit Continuance Eligibility 25<br />
- Group Health Benefits For Employees Retiring from Service Prior to Age 65 26<br />
- Group Health Benefits For Employees Retiring from Service at Age 65 or Later 27<br />
- Notice <strong>of</strong> Benefit Status due to Separation from Employment 28<br />
Revised July 2009 1
VI. Administration <strong>of</strong> Life & AD&D Page<br />
- Basic Life Insurance Outline 29<br />
- How to File A Claim for Basic Group Life Insurance (Instructions) 30<br />
- Premium Waiver – Basic Group Life Insurance Coverage (Instructions) 31<br />
- Group Life Insurance Benefits For Employees Separating From Service 32<br />
- Portability <strong>of</strong> Group Life Insurance & Supplemental Term Life Insurance Outline 33<br />
- Group Life Insurance Benefits For Employees Separating From Service –<br />
Conversion <strong>of</strong> Basic Group Life & Supplemental Term Life Insurance 34<br />
VII.<br />
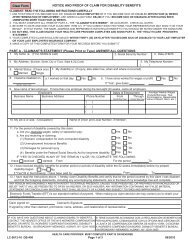
Administration <strong>of</strong> Short Term Disability (New York State Short Term Disability Benefits)<br />
- AONY Short Term Disability Outline 35<br />
- How to File a Claim for New York State Disability Benefits (Instructions) 36<br />
- “Sample Letter” - Notice to Disabled Employee 37<br />
VIII.<br />
Administration <strong>of</strong> Long Term Disability<br />
- Long Term Disability Outline 38<br />
- How to File a Claim for Long Term Disability Benefits (Instructions) 39<br />
IX.<br />
Administration <strong>of</strong> Dental Coverage<br />
- Group Dental Insurance Outline 40<br />
- CIGNA Dental for Clergy and Religious Plan Description 41<br />
- AONY CIGNA Dental PPO for Clergy Enrolled in High Option Plan II 42<br />
- AONY CIGNA Dental PPO for Religious Bro<strong>the</strong>rs and Sisters on Stipend and<br />
Institutions Electing High Option Plan for Religious Plan II 43<br />
- AONY CIGNA Dental PPO for Religious Bro<strong>the</strong>rs and Sisters Plan I 44<br />
- How to File a Dental Claim (Instructions) 45<br />
X. Administration <strong>of</strong> Vision Coverage<br />
- Davis Vision Care for Clergy and Religious Cover Page 46<br />
- AONY Davis Vision PPO Plan for Clergy and Religious Bro<strong>the</strong>rs and Sisters 47<br />
- AONY Benefit Plan Highlights - Group Vision Care Outline 48<br />
- Davis Vision Care for Clergy and Religious Summary 49<br />
- How To File a Vision Care Claim (Clergy and Religious only) 50<br />
XI.<br />
Administration <strong>of</strong> Voluntary Plans<br />
- Description <strong>of</strong> Voluntary Plans 51<br />
- AONY Supplemental Life Insurance 52<br />
- Nor<strong>the</strong>ast Dental Plan <strong>of</strong> America 53<br />
- Important Notice 54<br />
Revised July 2009 2
Section I<br />
Important Information
IMPORTANT NOTICE<br />
The Archdiocese <strong>of</strong> New York reserves <strong>the</strong> right to modify or discontinue any <strong>of</strong> <strong>the</strong><br />
group plans at any time.<br />
The <strong>benefits</strong> described in <strong>the</strong> Resource Guide are subject to <strong>the</strong> terms, conditions,<br />
limitations, and exclusions <strong>of</strong> <strong>the</strong> plan contracts issued by <strong>the</strong> individual insurance<br />
carriers to your group. If a difference exists between <strong>the</strong> information in <strong>the</strong><br />
Resource Guide and <strong>the</strong> actual contract, <strong>the</strong> contract governs.<br />
Participation in any <strong>of</strong> <strong>the</strong> group plans is limited to individuals who o<strong>the</strong>rwise<br />
satisfy <strong>the</strong> specific eligibility requirements for such group plans, and are ei<strong>the</strong>r (i)<br />
employed by <strong>the</strong> Archdiocese <strong>of</strong> New York; or (ii) employed by an institution or<br />
agency properly listed in <strong>the</strong> Official Catholic Directory, which has adopted and<br />
participates in such group plans with <strong>the</strong> consent <strong>of</strong> <strong>the</strong> Archdiocese <strong>of</strong> New York.<br />
Nothing contained in this <strong>guide</strong> should be construed as creating an employment<br />
relationship <strong>of</strong> any kind between <strong>the</strong> Archdiocese <strong>of</strong> New York and any individual,<br />
nor should it be interpreted as affecting any employment relationship between an<br />
employee and his or her actual employer.<br />
-1-
NEW EMPLOYEE CHECKLIST<br />
The following New Employee Checklist was developed as a tool to aid local<br />
administrators when a <strong>new</strong> employee is hired. The list includes benefit plans<br />
available to <strong>new</strong> employees as well as general policies. The checklist also<br />
includes forms and information that should be collected by <strong>the</strong> employer at<br />
<strong>the</strong> time <strong>of</strong> hire.<br />
It is important to note that policies and <strong>benefits</strong> may vary by institution. This<br />
checklist should only be used as a <strong>guide</strong>.<br />
-2-
New Employee Checklist<br />
Below is a list <strong>of</strong> Employee Benefits, Policies and Procedures, which should be discussed with each<br />
<strong>new</strong> employee at <strong>the</strong> time <strong>of</strong> initial orientation (date <strong>of</strong> hire or just before). Not all <strong>benefits</strong> are<br />
applicable to every institution. Simply list “N/A” next to any benefit that does not apply at your<br />
institution, or if <strong>the</strong> <strong>new</strong> employee is not eligible. (If scheduled to work less than 35 hours per week,<br />
an employee may not be eligible for all <strong>benefits</strong>).<br />
Please refer to <strong>the</strong> Summary Plan Description Booklets for each benefit plan for additional<br />
information.<br />
_______Application for Employment<br />
_______W-4 Form<br />
_______I-9 Form + Documentations<br />
_______Health Benefits*<br />
_______Dental Insurance*<br />
_______Basic Life<br />
_______AD&D Insurance*<br />
_______Long Term Disability<br />
_______Pension Form<br />
_______Regular Work Hours<br />
_______Overtime<br />
_______Vacation<br />
_______Absence Policy<br />
_______O<strong>the</strong>r<br />
_______Personal Days<br />
_______Holy Days/Holidays<br />
_______Sign-in Sheet<br />
_______Paycheck – Direct Deposit*<br />
_______I.D. Cards<br />
_______403(b) Savings Plan*<br />
_______ Supplemental Life<br />
_______Job Posting<br />
_______Dress Code<br />
_______Smoking Policy<br />
_______Telephones<br />
_______Code <strong>of</strong> Conduct<br />
_______Problem Resolution<br />
_______Sick Pay<br />
_______Recycling Program<br />
_______Emergency Contact<br />
_____________________________________ _____________________________ _____________<br />
Employee Name (please print) Employee Signature Date<br />
*Keep a copy for your files.<br />
Revised 04/01/06
BENEFITS ADMINISTRATOR<br />
RESOURCE CONTACT LIST<br />
-3-
THE ARCHDIOCESE OF NEW YORK<br />
BENEFITS ADMINISTRATOR’S RESOURCE CONTACTS LIST<br />
VENDOR CONTACT PHONE WEBSITES POLICY<br />
Number<br />
AONY Benefits Office Life & Health Division<br />
212.371.1011 www.archny.org<br />
212.980.1272 Fax<br />
Access & view:<br />
Ella O’Sullivan/Dir. <strong>of</strong> Life & Health (Ext. 3034)<br />
Margaret Gonzalez/Deputy Director (Ext. 3026) -The Archdiocese <strong>of</strong> New<br />
Gloria Glover/Benefits Administrator (Ext. 3018) York’s Notice <strong>of</strong> Privacy<br />
Frances Yee/Benefits Administrator (Ext. 3047) Practice pertaining to<br />
disclosure <strong>of</strong> health<br />
benefit information<br />
REASON<br />
-Oversees health & life<br />
insurance <strong>benefits</strong><br />
management<br />
-Oversees compliancy <strong>of</strong><br />
HIPAA regulations for<br />
disclosure <strong>of</strong> employee PHI<br />
(Personal Health Info)<br />
Employee Benefit<br />
Connections<br />
United Health Care<br />
Ellen Means/Manager<br />
1011 First Avenue – Room 1679<br />
New York, NY 10022<br />
Customer Service<br />
Claims Processing:<br />
United Healthcare<br />
P.O. Box 740800<br />
Atlanta, GA 30374-0800<br />
212.371.1000<br />
Ext. 3060<br />
212.644.0690 Fax<br />
800.736.1264 www.uhc.com<br />
-View copy <strong>of</strong> <strong>the</strong> Benefits<br />
Administrator’s Resource<br />
Guide<br />
ebc@archny.org Administrators can:<br />
-Verify member’s <strong>benefits</strong><br />
-Request enrollment packets<br />
For current provider<br />
directory)<br />
Policy:<br />
#708652<br />
Have members call for:<br />
-Claims Issues<br />
-ID Cards<br />
-Medical Claim Forms<br />
-UHC Directories<br />
-Pre-certification<br />
-Mental Health Info.<br />
CVS Caremark Prescription<br />
Plan<br />
Prescription Drugs Benefits<br />
Revised 07/01/09<br />
Customer Service<br />
Mail Service:<br />
P.O. Box 2110<br />
Pittsburgh, PA 15230-2110<br />
Prescription Reimbursement:<br />
P.O. Box 52196<br />
Phoenix, AZ 85072-2196<br />
800.565.7091<br />
(Pharmacists<br />
may also call for<br />
authorizations<br />
and assistance.)<br />
www.myuhc.com<br />
www.caremark.com<br />
- updated pharmacy info<br />
- online order refills<br />
- Retail info<br />
- Drug history & info<br />
Plan Code:<br />
CRK<br />
Group Code:<br />
CMGRX<br />
Provides member one-step<br />
access to <strong>the</strong>ir personalized<br />
health care information<br />
Have members call for:<br />
-Enrollment verifications<br />
-ID Cards<br />
-Prescription Mail Order<br />
Forms<br />
-Prescription Claim Form<br />
-to get reimbursement at<br />
nonparticipating pharmacy
VENDOR CONTACT PHONE WEBSITES POLICY<br />
Number<br />
Customer Service<br />
888.563.1124<br />
GL-674263<br />
Hartford Life Insurance Co.<br />
Basic Group Life<br />
Life Claims:<br />
Hartford Life Insurance<br />
Companies<br />
P.O. Box 2999<br />
Hartford, CT 06104-2999<br />
877.320.0484 –<br />
Portability,<br />
Conversion &<br />
Claim Status<br />
REASON<br />
-Death Claim Forms<br />
-Assistance with filling out<br />
death claim forms.<br />
-Death Claim Status<br />
Hartford Life Insurance Co.<br />
Premium Waiver <strong>of</strong> Group<br />
Life Benefit for Disabled<br />
Employees<br />
Customer Service 888.563.1124<br />
860-843-4713Fax<br />
GL-674263<br />
-Request form to file Life<br />
Premium Waiver for an<br />
employee who may be absent<br />
from work due to injury or<br />
illness for at least 12 months.<br />
-Assistance with filling out<br />
premium waiver form.<br />
Hartford Life Insurance Co.<br />
Supplemental Life<br />
Enrollment Package<br />
Employee Benefit Connections<br />
Ellen Means/Manager<br />
Johnnell Pankey/Benefits Coordinator<br />
Wendy Calhoun/Benefits Coordinator<br />
212.371.1000<br />
212.644.0690 Fax<br />
(Ext. 3049)<br />
(Ext. 3038)<br />
(Ext. 3048)<br />
GL-674263<br />
-Enrollment package<br />
Hartford Life Insurance Co.<br />
Supplemental Life<br />
(Voluntary Plan)<br />
(Employee payroll<br />
deduction)<br />
Hartford Life Insurance Co.<br />
(Portability & Conversions)<br />
Basic Group Life<br />
Supplemental Life<br />
Hartford Life Insurance Co.<br />
Short Term Disability<br />
Customer Service 888.331.7234 GL-674263 -Assistance with filling out<br />
claim form<br />
Customer Service<br />
Customer Service<br />
Hartford Life Syracuse Benefit<br />
Management Services Center<br />
P.O. Box 4925<br />
Syracuse, NY 13221<br />
Have employee call for:<br />
-Status <strong>of</strong> enrollment<br />
877.320.0484 GL-674263 Have employee call for:<br />
-Status <strong>of</strong> Portability or<br />
Conversion Benefits for Basic<br />
Group Life & Supplemental<br />
Life<br />
800.538.0134 LNY-612197 -Short Term Disability Claim<br />
Form<br />
-Assistance with filling out<br />
claim form<br />
-Status <strong>of</strong> Short Term<br />
Disability Claim<br />
Revised 07/01/09
VENDOR CONTACT PHONE WEBSITES POLICY<br />
Number<br />
Customer Service<br />
Hartford Life Insurance Co.<br />
Long Term Disability<br />
Hartford Life<br />
Syracuse Benefit Management<br />
Services Center<br />
P.O. Box 4871<br />
Syracuse, NY 13221<br />
REASON<br />
800.538.0134 GLT-674263 -Long Term Disability Claim<br />
Form<br />
-Assistance with filling out<br />
claim form<br />
-Status <strong>of</strong> Long Term<br />
Disability Claim<br />
CIGNA Dental Plan<br />
For members <strong>of</strong> Clergy,<br />
Religious & Eligible Lay<br />
Employees<br />
Customer Service 800.244.6224 www.cigna.com 0435433 Have Members <strong>of</strong> Clergy<br />
or Religious call for:<br />
-Dental claim forms<br />
-Status <strong>of</strong> Dental Claim<br />
Davis Vision<br />
For members <strong>of</strong> Clergy,<br />
Religious & Eligible Lay<br />
Employees<br />
Nor<strong>the</strong>ast Dental Plan <strong>of</strong><br />
America<br />
Voluntary Plan<br />
(Employee direct pay to<br />
Nor<strong>the</strong>ast Dental)<br />
Customer Service<br />
Vision Care Processing Unit<br />
P.O. Box 1525<br />
Latham, NY 12110<br />
Customer Service<br />
845 Third Avenue, 20th Fl.<br />
New York, NY 10022<br />
Dentists may also call for<br />
enrollment status and<br />
claims issues.<br />
800.999.5431 www.davisvision.com 7821 Have Members <strong>of</strong> Clergy<br />
or Religious call for:<br />
-Enrollment verification<br />
-Vision claim form<br />
-Claim Status<br />
800.828.2222<br />
212-688-9708 Fax<br />
-Provider Directory<br />
www.dentalsave.com Have employees call for:<br />
-Enrollment package for<br />
employees <strong>of</strong> <strong>the</strong> Archdiocese<br />
<strong>of</strong> New York” (special discount)<br />
Revised 07/01/09
RULES FOR MEMBER GROUPS PARTICIPATING IN THE<br />
ARCHDIOCESE OF NEW YORK<br />
GROUP INSURANCE PLAN<br />
-4-
THE ARCHDIOCESE OF NEW YORK<br />
RULES FOR MEMBER GROUPS PARTICIPATING IN THE ARCHDIOCESAN GROUP BENEFITS PROGRAM<br />
Eligibility for group membership in <strong>the</strong> Archdiocese <strong>of</strong> New York Group Benefits Program (hereinafter referred to as <strong>the</strong><br />
“Benefit Program”) is restricted to agencies, organizations, and institutions (individually and collectively referred to as<br />
“Group[s]”) currently listed in The Official Catholic Directory published by Kennedy and Sons that maintain at least one<br />
location within <strong>the</strong> geographic boundaries <strong>of</strong> <strong>the</strong> Archdiocese <strong>of</strong> New York. The majority <strong>of</strong> a Group’s<br />
employees/members, including an employee’s/member’s spouse and dependent children, (collectively referred to as<br />
“Enrollees”) enrolled in <strong>the</strong> Benefit Program must work and/ or reside within <strong>the</strong> geographic boundaries <strong>of</strong> <strong>the</strong><br />
Archdiocese in order to participate in <strong>the</strong> Benefit Program.<br />
Groups joining <strong>the</strong> Benefit Program must commit to participating in <strong>the</strong> Benefit Program for a minimum <strong>of</strong> two<br />
years.<br />
A) COVERAGE<br />
1. Each Group must include all lines <strong>of</strong> coverage that <strong>the</strong> Group provides for <strong>the</strong>ir eligible Enrollees covered under<br />
<strong>the</strong> Benefit Program unless <strong>the</strong> Enrollee is not eligible for a particular coverage. Each Group must provide<br />
coverage for life, accidental death and dismemberment (“AD&D”), and New York statutory disability<br />
(“NYDBL”) to all eligible Enrollees and <strong>of</strong>fer medical coverage to all eligible Enrollees. The obligatory<br />
coverages are as follows:<br />
i) Clergy Life, AD&D, Medical, Dental, and Vision<br />
ii) Religious Bro<strong>the</strong>rs and Sisters<br />
Medical and Dental *(and Vision for Religious on stipend)<br />
iii) Lay Employees<br />
Life, AD&D, NYDBL, and Medical<br />
*(Dental retired Religious on stipend)<br />
2. Regarding Section A(1) above, <strong>the</strong> Archdiocese will allow any Group insurance arrangements in force prior to<br />
October 1, 2000 for Groups enrolled in <strong>the</strong> Benefit Program as <strong>of</strong> July 1, 2000, but will not permit any additional<br />
deviations. Groups must not <strong>of</strong>fer any o<strong>the</strong>r outside benefit programs that would compete with <strong>the</strong> Benefit<br />
Program. For example, Groups participating in <strong>the</strong> Benefit Program should not <strong>of</strong>fer <strong>the</strong>ir Enrollees medical<br />
coverage options that are not sponsored by <strong>the</strong> Archdiocese.<br />
3. The Benefit Program determines eligibility requirements for enrollment in <strong>the</strong> Benefit Program, and <strong>the</strong> Group<br />
must not vary or restrict eligibility by occupation or class. Except as designated by <strong>the</strong> Benefit Program, <strong>the</strong><br />
eligibility classifications for participation in <strong>the</strong> Benefit Program must be <strong>the</strong> same for all types <strong>of</strong> coverage on<br />
<strong>the</strong> Group level. (Currently, <strong>the</strong> only variance is <strong>the</strong> six-month waiting period for Long Term Disability<br />
coverage.)<br />
4. Groups are responsible for <strong>of</strong>fering medical coverage to eligible <strong>new</strong> hires prior to <strong>the</strong> date that <strong>the</strong> employee<br />
would be eligible for coverage.<br />
Revised 01/2008
5. All clergy and religious orders whose Groups provide medical coverage through <strong>the</strong> Health Benefit Program<br />
must provide coverage for all similarly situated religious and clergy except where like coverage, obtained prior<br />
to <strong>the</strong> eligibility for coverage under <strong>the</strong> Benefit Program, remains in force.*<br />
6. Medicare. Groups must abide by <strong>the</strong> Medicare integration rules that apply to <strong>the</strong> Archdiocese <strong>of</strong> New York.<br />
Medicare is secondary to <strong>the</strong> Archdiocese medical coverage except under <strong>the</strong> following circumstances:<br />
I. Medicare is <strong>the</strong> primary coverage for retired clergy * and retired Enrollees and <strong>the</strong>ir spouses who are age<br />
65 or older.<br />
II.<br />
Medicare is primary for <strong>the</strong> disabled spouses <strong>of</strong> retired Enrollees.<br />
III. Medicare is primary for all religious Bro<strong>the</strong>rs and Sisters who are age 65 and older. * Religious Bro<strong>the</strong>rs<br />
and Sisters age 65 and over who are entitled to Medicare must change <strong>the</strong>ir coverage to a Medicare<br />
Supplement or a Medicare Risk Plan. The employing Group will reimburse <strong>the</strong> Religious Order for <strong>the</strong><br />
Medicare Part B premium.<br />
IV.<br />
Medicare is primary for disabled Enrollees who qualify for Medicare as a result <strong>of</strong> a disabling illness or<br />
injury provided <strong>the</strong> employee has not been on <strong>the</strong> employer’s active payroll for at least six months.<br />
V. If Medicare is <strong>the</strong> primary medical plan for <strong>the</strong> primary insured (employee, clergy, religious) <strong>the</strong><br />
insured cannot be covered under a non-Medicare plan except that lay retirees and retired clergy and<br />
religious with Medicare as primary may enroll in <strong>the</strong> group Medicare supplemental health plan <strong>of</strong>fered<br />
by <strong>the</strong> Archdiocese <strong>of</strong> New York.<br />
7. Any Enrollee who has previously waived medical coverage (for himself/herself and/or his/her dependents) has<br />
<strong>the</strong> right to elect medical coverage each year during <strong>the</strong> open enrollment period. Coverage changes elected<br />
during <strong>the</strong> open enrollment period will take effect on <strong>the</strong> Benefit Program anniversary date, currently January 1.<br />
Normally Enrollees cannot change <strong>the</strong>ir health coverage elections except at open enrollment; however, under<br />
certain circumstances Enrollees can change <strong>the</strong>ir coverage election during <strong>the</strong> Benefit Program year. Enrollees<br />
may elect to join <strong>the</strong> Benefit Program or enroll <strong>the</strong>ir eligible dependents in <strong>the</strong> Benefit Program if <strong>the</strong> Enrollee<br />
experiences a qualifying event, as defined by <strong>the</strong> Benefit Program documents. O<strong>the</strong>r than as previously stated in<br />
this paragraph, mid-year enrollments will not be permitted except for persons <strong>new</strong>ly eligible who enroll within<br />
30 days following <strong>the</strong> date <strong>the</strong>y become eligible for coverage.<br />
8. Long-Term Disability Coverage. Groups providing long-term disability (“LTD”) coverage to <strong>the</strong>ir employed<br />
Enrollees must purchase it through <strong>the</strong> Benefit Program. Employed Enrollees must work a minimum <strong>of</strong> 30 hours<br />
per week (20 hours per week for lay faculty covered by a collective bargaining agreement) and be actively<br />
employed by <strong>the</strong> Group with <strong>the</strong> Archdiocese LTD coverage for <strong>the</strong> previous six months to be eligible for LTD<br />
coverage.<br />
B) GROUP TERMINATION OF COVERAGE<br />
9. If a Group will be terminating coverage under <strong>the</strong> Benefits Program, <strong>the</strong> Group must notify <strong>the</strong> Archdiocese<br />
Benefits Office in writing at least 60 days prior to <strong>the</strong> proposed termination date. All coverage in any part <strong>of</strong> <strong>the</strong><br />
Benefits Program will terminate on <strong>the</strong> same date. Group terminations must be effective on <strong>the</strong> Benefits Program<br />
anniversary date, January 1. Please direct all questions and correspondence regarding Benefits Program<br />
termination to Ella O’Sullivan, Director <strong>of</strong> Life & Health Benefits, Archdiocese <strong>of</strong> New York, 1011 First<br />
Avenue, New York, NY 10022.<br />
10. Groups that terminate <strong>the</strong>ir medical coverage will be billed a terminal premium equal to <strong>the</strong> premium<br />
due for <strong>the</strong> last three months <strong>the</strong> medical coverage was in force with <strong>the</strong> Benefit Program in order to<br />
* Priests or Religious who are not entitled to Medicare coverage should contact Margaret Gonzalez, Deputy Director <strong>of</strong> Life &<br />
Health Benefits, Archdioces <strong>of</strong> New York: phone 212.371.1011, Ext. 3026, Fax 212.980.1272, or e-mail:<br />
Margaret.Gonzalez@archny.org immediately.<br />
Revised 01/2008
provide funds to pay claims submitted after <strong>the</strong> termination date on behalf <strong>of</strong> or by <strong>the</strong> terminating<br />
Group’s Enrollees that were incurred prior to <strong>the</strong> date <strong>of</strong> termination.<br />
11. Groups terminating coverage under <strong>the</strong> Benefit Program will be precluded from rejoining <strong>the</strong> Benefit Program<br />
for a minimum <strong>of</strong> two years from <strong>the</strong> group termination date. Reenrollment will be at <strong>the</strong> discretion <strong>of</strong><br />
Archdiocesan management following a review <strong>of</strong> payment history and claims experience.<br />
C) PREMIUM PAYMENT<br />
12. Basic life, AD&D, and LTD coverage must be provided to eligible employed Enrollees at <strong>the</strong> Group’s expense.<br />
Enrollees must be enrolled for <strong>the</strong>se coverages within 30 days <strong>of</strong> <strong>the</strong> Enrollee’s initial eligibility date. Groups<br />
can charge employed Enrollees <strong>the</strong> maximum allowable contribution for NYDBL. For entities directly reporting<br />
to <strong>the</strong> Archdiocese (including parish corporations and Archdiocesan schools), you must comply with <strong>the</strong><br />
Archdiocese’s schedule <strong>of</strong> employed Enrollee contributions for medical coverage as published annually in <strong>the</strong><br />
open enrollment packages. For all o<strong>the</strong>r Groups, <strong>the</strong> Group must fund at least 70% <strong>of</strong> <strong>the</strong> employed Enrollee and<br />
50% <strong>of</strong> dependent Enrollee medical premiums for full-time employed Enrollees. Groups must submit any<br />
proposed changes in <strong>the</strong> Enrollee contribution levels in writing to <strong>the</strong> Chancellor within 60 days prior to <strong>the</strong><br />
Benefit Program anniversary date, currently January 1.<br />
13. Any employee meeting <strong>the</strong> eligibility requirements for medical coverage is required to contribute towards <strong>the</strong><br />
premiums and must be covered under <strong>the</strong> Benefit Program, unless <strong>the</strong> employee submits a written waiver <strong>of</strong><br />
coverage (form or letter) within 30 days <strong>of</strong> <strong>the</strong> eligibility date. All eligible employees must complete and sign a<br />
Group Health Benefits Election Form to indicate <strong>the</strong>ir payroll deduction election.<br />
14. Premium Payment is due and expected within 30 days <strong>of</strong> <strong>the</strong> premium due date. Groups are responsible for <strong>the</strong><br />
payment <strong>of</strong> <strong>the</strong> full premium to <strong>the</strong> Archdiocese <strong>of</strong> New York.<br />
D) RECORDKEEPING AND ADMINISTRATION<br />
15. Groups providing medical coverage for <strong>the</strong>ir eligible Enrollees must obtain (and retain on file) a completed<br />
Group Enrollment Change form and a Group Health Benefits Election form from each eligible employee. If an<br />
employee has elected to waive medical coverage for a given Benefit Program year, this should be so indicated<br />
on both forms.<br />
16. The Group must comply with all data requests in an accurate and timely manner.<br />
17. All Groups must notify Employee Benefit Connections within 30 days <strong>of</strong> <strong>the</strong> prescribed effective date for a<br />
change in an Enrollee’s coverage status. Some examples are as follows: an Enrollee becomes eligible for<br />
coverage (<strong>new</strong> hire or change in job status), retires, terminates from <strong>the</strong>ir position, experiences a life status<br />
change such as marriage, birth <strong>of</strong> a child, or change in spouse’s employment status that affects medical<br />
coverage. The Group must submit a written memo or change form to Employee Benefit Connections to notify<br />
<strong>the</strong> Benefit Program <strong>of</strong> <strong>the</strong> Enrollee’s status change. The Group administrator must include <strong>the</strong> specific reason<br />
for <strong>the</strong> requested change as part <strong>of</strong> <strong>the</strong> request. Certain Enrollee status changes must also include additional<br />
forms in order for <strong>the</strong> change to be processed. The following changes require a medical enrollment/ change<br />
form: adding a spouse or child, change <strong>of</strong> martial status.<br />
18. Under certain circumstances, an Enrollee may need to be retroactively enrolled or reinstated for medical and/ or<br />
o<strong>the</strong>r coverages. Generally, <strong>the</strong> Archdiocese will allow for an Enrollee to be retroactively enrolled or terminated<br />
within two months following <strong>the</strong> date <strong>of</strong> <strong>the</strong> change in coverage. The Archdiocese will credit Groups for no<br />
more than two months <strong>of</strong> premium for retroactive coverage terminations. Withholding <strong>of</strong> back premium on<br />
<strong>the</strong>se Enrollees will result in <strong>the</strong> same consequences as not paying current premium.<br />
Your Group must abide by <strong>the</strong> coverage and policy rules with respect to eligibility, non-discrimination,<br />
enrollment dates, procedures and vendor contractual requirements. Liabilities arising out <strong>of</strong> <strong>the</strong> Archdiocese’s or<br />
Group’s failure to adhere to <strong>the</strong>se policies will be <strong>the</strong> responsibility <strong>of</strong> <strong>the</strong> erring party. Failure to abide by <strong>the</strong><br />
policies as outlined above can result in termination <strong>of</strong> a Group’s coverage under <strong>the</strong> Benefit Program.<br />
Revised 01/2008
BENEFIT ELIGIBILITY OUTLINE<br />
-5-
B E N E F I T E L I G I B I L I T Y O U T L I N E<br />
BENEFITS ELIGIBILITY EFFECTIVE DATE WAITING<br />
PERIOD<br />
United HealthCare Choice Plus Plan<br />
Customer Service<br />
800.736.1264<br />
Cancer Research Service Center<br />
866.936.6002<br />
(Members must first call to open a dialog<br />
with UHC and <strong>the</strong> Cancer Service Center)<br />
www.myuhc.com<br />
(Member’s personalized information site.<br />
Member needs to create password)<br />
United HealthCare Medicare<br />
Supplement Plan<br />
Customer Service<br />
800.736.1272<br />
Cancer Research Service Center<br />
866.936.6002<br />
(Members must first call to open dialog with<br />
UHC and <strong>the</strong> Cancer Service Center)<br />
www.myuhc.com<br />
(Member’s personalized information site.<br />
Member needs to create password)<br />
• Diocesan and Extern Priests as<br />
approved by <strong>the</strong> Office <strong>of</strong> Priest<br />
Personnel.<br />
• Religious Bro<strong>the</strong>rs & Sisters<br />
• Seminarians<br />
• Aegis <strong>of</strong> Religious Orders for Parish,<br />
and Private Schools<br />
• Non-bargaining Lay Employees<br />
working in Catholic High Schools &<br />
all Bargaining Lay Faculty Members<br />
scheduled to work at least 20 hours.<br />
• Non-bargaining lay employees <strong>of</strong> <strong>the</strong><br />
Archdiocese <strong>of</strong> New York, who<br />
regularly scheduled to work at least 20<br />
hours.<br />
• Employees <strong>of</strong> Child Care Agencies<br />
• Early retired Bargaining Lay Faculty<br />
Members (ages 55 to 64), who<br />
participated in plan prior to<br />
retirement, have 10 years service,<br />
receiving a pension from AONY<br />
and not working for ano<strong>the</strong>r<br />
Archdiocesan institution.<br />
• Retired non-bargaining lay<br />
employees who have worked for <strong>the</strong><br />
Archdiocese at least 10 years and at<br />
least 55 years old, receiving a pension<br />
from AONY and not working for<br />
ano<strong>the</strong>r Archdiocesan institution. Must<br />
have participated in <strong>the</strong> plan prior to<br />
retirement.<br />
•Retired Diocesan & Extern Priests<br />
who are Medicare eligible.<br />
• Religious Bro<strong>the</strong>rs & Sisters who<br />
become eligible and elect Medicare<br />
Parts A & B at age 65.<br />
• Retired non-bargaining lay employees<br />
who elected this coverage prior to<br />
retiring from <strong>the</strong> Archdiocese <strong>of</strong> NY<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- First <strong>of</strong> <strong>the</strong> month after<br />
30 days <strong>of</strong> employment<br />
- Varies by Agency<br />
- Retirement Date<br />
- Retirement Date<br />
- Immediate Coverage<br />
or Date <strong>of</strong> Medicare<br />
(Parts A & B)<br />
- Date <strong>of</strong> Medicare<br />
(Parts A & B)<br />
- Retirement date<br />
- None<br />
- None<br />
- None<br />
- None<br />
- None<br />
- 30 Days<br />
(at least)<br />
- Varies<br />
- None<br />
- None<br />
- None<br />
- None<br />
- None<br />
EMPLOYER’S<br />
COST<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Based on Schedule<br />
- Based on a Schedule<br />
- Varies by Agency<br />
- None (Retiree pays)<br />
- None (Retiree pays)<br />
- Entire Premium<br />
- Entire Premium<br />
- None (Retiree pays)<br />
BASIC DESCRIPTION<br />
Choice Plus plan which provides medical and<br />
hospital <strong>benefits</strong>.<br />
Primarily a self-referral health plan.<br />
Participant is not required to select a<br />
primary care physician.<br />
(See Summary Plan Description for<br />
details)<br />
Medical and hospital plan that supplements Medical<br />
Primary coverage.<br />
Participant is subject to deductibles and coinsurance.<br />
(See Summary Plan Description for<br />
details)<br />
NOTE: This is a summary description <strong>of</strong> <strong>the</strong> plan <strong>benefits</strong> only and is subject to <strong>the</strong> term, conditions, limitations and exclusions set forth in each plan’s <strong>of</strong>ficial plan document. If <strong>the</strong>re are conflicting information contained between this summary and <strong>the</strong> any <strong>of</strong> <strong>the</strong> <strong>of</strong>ficial<br />
plan documents plan documents will preside.<br />
The Archdiocese <strong>of</strong> New York reserves <strong>the</strong> right to amend or revoke its policies at time without notice. Nothing in this summary constitutes a promise or guarantee <strong>of</strong> continuing <strong>benefits</strong><br />
Revised May 2008
BENEFITS ELIGIBILITY EFFECTIVE DATE WAITING<br />
PERIOD<br />
Caremark Prescription Plan<br />
(Must be enrolled in<br />
group medical plan)<br />
(800) 565-7091<br />
www.caremark.com<br />
Hartford Life Insurance Company<br />
Group Life Insurance<br />
Policy #GL-674263<br />
888.563-1124<br />
Conversion & Portability Info:<br />
877.320.0484<br />
Mutual <strong>of</strong> Omaha Company<br />
Accidental Death &<br />
• Active & Retired Diocesan and<br />
Extern Priests as approved by <strong>the</strong><br />
Office <strong>of</strong> Priest Personnel.<br />
• Active and Retired Religious Bro<strong>the</strong>rs<br />
& Sisters<br />
• Seminarians<br />
• Aegis <strong>of</strong> Religious Orders for Parish,<br />
and Private Schools<br />
• Non-bargaining Lay Employees<br />
working in Catholic High Schools &<br />
all Bargaining Lay Faculty Members<br />
scheduled to work at least 20 hours.<br />
• Non-bargaining lay employees <strong>of</strong> <strong>the</strong><br />
Archdiocese <strong>of</strong> New York regularly<br />
scheduled to work at least 20 hours.<br />
• Employees <strong>of</strong> Child Care Agencies<br />
• Early retired Bargaining Lay Faculty<br />
Members (ages 55 to 64), who<br />
participated in plan prior to<br />
retirement, has 10 years service,<br />
receiving a pension from <strong>the</strong><br />
AONY and not working for ano<strong>the</strong>r<br />
Archdiocesan institution.<br />
• Retired non-bargaining lay<br />
employees who have worked for <strong>the</strong><br />
Archdiocese at least 10 years and at<br />
least 55 years old, receiving a pension<br />
from AONY and not working for<br />
ano<strong>the</strong>r Archdiocesan institution.<br />
Must have participated in <strong>the</strong> plan<br />
prior to retirement.<br />
• Members <strong>of</strong> <strong>the</strong> Clergy as approved<br />
for coverage by <strong>the</strong> Office <strong>of</strong> Priest<br />
Personnel.<br />
• Aegis <strong>of</strong> Religious Orders for Parish,<br />
CHSA, & Private Schools.<br />
• Non-bargaining Lay Employees<br />
working in Catholic High Schools &<br />
all Bargaining Lay Faculty Members<br />
scheduled to work at least 20 hours.<br />
• Lay employees who are regularly<br />
scheduled to work 20 hours each<br />
week.<br />
• Lay employees employed by Child<br />
Care Agencies<br />
• Members <strong>of</strong> <strong>the</strong> Clergy as approved<br />
for coverage by <strong>the</strong> Office <strong>of</strong> Priest<br />
Personnel.<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- First <strong>of</strong> <strong>the</strong> month after<br />
30 days <strong>of</strong> employment<br />
- Varies by Agency<br />
- Retirement Date<br />
- Retirement Date<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- First <strong>of</strong> <strong>the</strong> month after<br />
30 days <strong>of</strong> employment.<br />
- Varies by Agency<br />
EMPLOYER’S<br />
COST<br />
BASIC DESCRIPTION<br />
NOTE: This is a summary description <strong>of</strong> <strong>the</strong> plan <strong>benefits</strong> only and is subject to <strong>the</strong> term, conditions, limitations and exclusions set forth in each plan’s <strong>of</strong>ficial plan document. If <strong>the</strong>re are conflicting information contained between this summary and <strong>the</strong> any <strong>of</strong> <strong>the</strong> <strong>of</strong>ficial<br />
plan documents plan documents will preside.<br />
The Archdiocese <strong>of</strong> New York reserves <strong>the</strong> right to amend or revoke its policies at time without notice. Nothing in this summary constitutes a promise or guarantee <strong>of</strong> continuing <strong>benefits</strong><br />
Revised May 2008<br />
- None<br />
- None<br />
- None<br />
- None<br />
- None<br />
- 30 Days<br />
(at least)<br />
- Varies<br />
- None<br />
- None<br />
- None<br />
- None<br />
- None<br />
- 30 days<br />
(at least)<br />
- Varies<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Based on a Schedule<br />
- Based on a Schedule<br />
- Varies by Agency<br />
- None (Retiree pays)<br />
- None (Retiree pays)<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
Prescription drug benefit plan, which enables<br />
participants to purchase prescribed drugs at a retail<br />
pharmacy or through a mail order service.<br />
(Refer to <strong>the</strong> Prescription Drug<br />
Benefit Program booklet for more<br />
details)<br />
(Co-pays subject to change)<br />
Benefits ranges are $10,000 or one times <strong>the</strong> annual<br />
salary ($200,000 max) <strong>of</strong> <strong>the</strong> participant as outlined<br />
in <strong>the</strong> plan booklet.<br />
This benefit plan also provides for waiver <strong>of</strong><br />
premiums due to <strong>the</strong> disability <strong>of</strong> an employee.<br />
Benefit also includes a “living benefit”, which is also<br />
known as an accelerated death benefit, premium<br />
waiver feature, portability and conversion options.<br />
(Refer to <strong>benefits</strong> booklets for fur<strong>the</strong>r details and<br />
requirements)<br />
- Immediate Coverage - None - Entire Premium The principal sum will match <strong>the</strong> group life<br />
plan.
BENEFITS ELIGIBILITY EFFECTIVE DATE WAITING<br />
PERIOD<br />
Dismemberment Plan<br />
(800) 524-2324<br />
Hartford Life Insurance Company<br />
Short Term Disability<br />
Policy #LNY 612197<br />
(800) 538.0134<br />
Hartford Life Insurance Company<br />
Long Term Disability<br />
Policy #GLT-674263<br />
(800) 538.0134<br />
• Aegis <strong>of</strong> Religious Orders for Parish,<br />
CHSA, & Private Schools.<br />
• Non-bargaining Lay Employees<br />
working in Catholic High Schools &<br />
all Bargaining Lay Faculty Members<br />
scheduled to work at least 20 hours.<br />
• Lay employees who are regularly<br />
scheduled to work 20 hours each<br />
week.<br />
• Lay employees employed by Child<br />
Care Agencies<br />
• All lay employees <strong>of</strong> participating<br />
institutions or divisions, who have<br />
worked at least 4 consecutive weeks<br />
with a covered employer (State<br />
mandated benefit)<br />
• Bargaining lay faculty members<br />
assigned to work 20 hours.<br />
• Non-bargaining lay employees<br />
assigned to work 30 hours.<br />
• Lay employees <strong>of</strong> Child Care agencies<br />
– hours varies by group<br />
- Immediate Coverage<br />
- Immediate Coverage<br />
- First <strong>of</strong> <strong>the</strong> month after<br />
30 days <strong>of</strong> employment.<br />
- Varies by Agency<br />
- Immediate Coverage if<br />
employee changed jobs<br />
from ano<strong>the</strong>r covered<br />
employer.<br />
- First <strong>of</strong> <strong>the</strong> month after 6<br />
months <strong>of</strong> employment.<br />
- First <strong>of</strong> <strong>the</strong> month after 6<br />
months <strong>of</strong> employment<br />
- Varies by Agency<br />
- None<br />
- None<br />
- 30 days<br />
(at least)<br />
- Varies<br />
7 calendar<br />
days <strong>of</strong>f <strong>the</strong><br />
job due to<br />
illness/injury<br />
that is non<br />
job related.<br />
- 180 days <strong>of</strong><br />
disability<br />
- 180 days <strong>of</strong><br />
disability<br />
- 180 days <strong>of</strong><br />
disability<br />
EMPLOYER’S<br />
COST<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium*<br />
*Employee can share<br />
cost <strong>of</strong> premium up to<br />
$0.60 (cents) per<br />
payroll deduction.<br />
- Entire Premium<br />
- Entire Premium<br />
- Entire Premium<br />
BASIC DESCRIPTION<br />
There is dismemberment benefit based on a<br />
schedule.<br />
(Refer to <strong>benefits</strong> booklet for fur<strong>the</strong>r<br />
details and requirements)<br />
Benefits starts on <strong>the</strong> 8th day <strong>of</strong> eligible disability and<br />
pays 50% <strong>of</strong> employee’s base pay up to a maximum<br />
<strong>of</strong> $170.00.<br />
Benefits are paid for a maximum <strong>of</strong> 26 weeks during<br />
52 consecutive weeks or during any one period <strong>of</strong><br />
disability.<br />
Benefit provides 60% <strong>of</strong> monthly earnings to a<br />
maximum <strong>of</strong> $5,000 subject to <strong>of</strong>fsets with o<strong>the</strong>r<br />
disability income such as Social Security disability<br />
and pension.<br />
(Refer to <strong>benefits</strong> booklet for fur<strong>the</strong>r details and<br />
requirements)<br />
Hartford Life Insurance Company<br />
Voluntary Group Supplemental<br />
Life Insurance<br />
(888) 563-1124<br />
Nor<strong>the</strong>ast Dental Plan <strong>of</strong> America<br />
Voluntary Dental Plan<br />
(800) 828-2222<br />
www.ndpa.com<br />
www.dentalsave.com<br />
• Bargaining lay faculty members who<br />
are regularly scheduled to work at<br />
least 20 hours and already enrolled in<br />
<strong>the</strong> basic group life insurance.<br />
• Non-bargaining lay employees who<br />
are regularly scheduled to work at<br />
least 20 hours and already enrolled in<br />
<strong>the</strong> basic group life insurance.<br />
• Lay employees employed by Child<br />
Care Agencies. Eligibility hours<br />
varies among this group. Employees<br />
must already be enrolled in basic<br />
group life insurance.<br />
• All lay employees <strong>of</strong> <strong>the</strong> Archdiocese<br />
<strong>of</strong> New York<br />
- Same as for group basic<br />
life insurance<br />
- Same as for group basic<br />
life insurance.<br />
- Same as for group basic<br />
life insurance.<br />
As soon as membership fee<br />
is received by North-east<br />
Dental. Employee may<br />
enroll over <strong>the</strong> telephone<br />
using his/her credit card.<br />
Same as for<br />
group basic<br />
life ins.<br />
Same as for<br />
group basic<br />
life ins.<br />
Same as for<br />
group basic<br />
life ins.<br />
None<br />
Through payroll deductions, employees have <strong>the</strong><br />
opportunity to purchase additional life insurance,<br />
which provides cash accumulation or cash value.<br />
An eligible employee also has <strong>the</strong> option <strong>of</strong><br />
purchasing supplemental coverage for his/her<br />
spouse and dependent children.<br />
None None Plan <strong>of</strong>fers voluntary dental coverage at<br />
discounted fees for dental services provided by<br />
member dentists.<br />
Employees pay discounted membership fees directly<br />
to Nor<strong>the</strong>ast Dental.<br />
NOTE: This is a summary description <strong>of</strong> <strong>the</strong> plan <strong>benefits</strong> only and is subject to <strong>the</strong> term, conditions, limitations and exclusions set forth in each plan’s <strong>of</strong>ficial plan document. If <strong>the</strong>re are conflicting information contained between this summary and <strong>the</strong> any <strong>of</strong> <strong>the</strong> <strong>of</strong>ficial<br />
plan documents plan documents will preside.<br />
The Archdiocese <strong>of</strong> New York reserves <strong>the</strong> right to amend or revoke its policies at time without notice. Nothing in this summary constitutes a promise or guarantee <strong>of</strong> continuing <strong>benefits</strong><br />
Revised May 2008
DIVISION CLAIM CODES<br />
-6-
ARCHDIOCESE OF NEW YORK<br />
GROUP AND CLAIM DIVISION CODES<br />
MEDICAL PLANS<br />
Group 6000 – Clergy & Seminarians<br />
053 Clergy (Diocesan Clergy and Externs)<br />
055 Seminarians<br />
153 Clergy with Medicare Primary<br />
156 Retired Clergy over age 65 without Medicare Primary<br />
Group 7000 - Religious<br />
050 Religious Bro<strong>the</strong>rs and Sisters – (Religious working in outside institutions - high dental option)<br />
051 Religious Bro<strong>the</strong>rs and Sisters – (Religious working within <strong>the</strong>ir communities with high or low dental option)<br />
154 Religious with Medicare Primary with Rx<br />
Group 4000 - Non-Bargaining Lay Employees<br />
001 Non-Bargaining Lay Faculty – Parish Schools<br />
002 Non-Bargaining Lay Faculty – Private Schools<br />
005 Lay Faculty – Special Education & Religious Vocational Institutions<br />
006 Trustees <strong>of</strong> St. Patrick Ca<strong>the</strong>dral<br />
024 Lay Employees <strong>of</strong> Cemeteries (Non-Bargaining)<br />
025 Incarnation Children’s Center<br />
030A Outside Affiliated Agencies <strong>of</strong> <strong>the</strong> Archdiocese<br />
030B<br />
Employees <strong>of</strong> Dominican Sisters<br />
031 Catholic Charities<br />
032 Lay Employees <strong>of</strong> Private Schools (Non-Bargaining)<br />
033 Chancery, Central Services, and Supporting Departments<br />
034 Parish/Parish School Employees (Non-Bargaining)<br />
035 Office <strong>of</strong> Drug Education (Division <strong>of</strong> <strong>the</strong> Dept. <strong>of</strong> Education)<br />
036 Beacon <strong>of</strong> Hope<br />
037 St. Raymond’s Cemetery – Non-Bargaining<br />
040 Catholic High School Association Non-Bargaining Employees<br />
043 Missionaries receiving stipends – Parish/CHSA<br />
044 Missionaries receiving stipends – Private Schools<br />
106 Trustees <strong>of</strong> St. Patrick’s Ca<strong>the</strong>dral – Grandfa<strong>the</strong>red Retirees with Group Life Benefits<br />
131 Non-Bargaining Lay Retirees over age 65<br />
134 Non-Bargaining Active Lay Employees over age 65 with Medicare Primary – Grandfa<strong>the</strong>red closed group<br />
135 Retired Non-Bargaining Lay Employees under age 65<br />
Group 5000 - Lay Faculty Members Covered by Collective Bargaining<br />
003 Lay Bargaining Faculty – Parish Schools<br />
004 Lay Bargaining Faculty – CHSA Schools<br />
007 Union Officers <strong>of</strong> <strong>the</strong> Federation <strong>of</strong> Catholic Teachers<br />
103 Early Retired Lay Faculty – Parish Schools<br />
104 Early Retired Lay Faculty - CHSA<br />
108 Aged 65+ Spouse <strong>of</strong> Early Retired Lay Faculty Member <strong>of</strong> CHSA<br />
109 Aged 65+ Spouse <strong>of</strong> Early Retired Lay Faculty Member <strong>of</strong> Parish School<br />
Group 2000 - Child Care Agencies<br />
017 Mission <strong>of</strong> <strong>the</strong> Immaculate Virgin, Mt. Loretto – Non-Bargaining Employees<br />
018 St. Cabrini Home<br />
019 St. Dominic’s Home<br />
047 Mission <strong>of</strong> <strong>the</strong> Immaculate Virgin, Mt. Loretto – Bargaining Employees<br />
113 Child Care Agencies Retirees over age 65<br />
114 Child Care Agencies Retirees under age 65<br />
Division Codes.Arch System Revised 07/01/09
Group 3000 - New York State Continuance Coverage<br />
813 Eligible Non-Bargaining Lay Employees and <strong>the</strong>ir dependents<br />
814 Eligible Bargaining Lay Employees and <strong>the</strong>ir dependents<br />
Non-Medical Groups<br />
008 Ferncliff Nursing Home – Dental Only<br />
026 St. Patrick’s Home (Management) – Life Only @ 1xBAE<br />
026 St. Patrick’s Home (Non-Management) – Life Only @ $10,000<br />
027 Rosary Hill Home – LTD Only<br />
028 St. Rose’s Home – LTD Only<br />
038 Dominican Fa<strong>the</strong>rs (Lay Employees) - Life Only @ $10,000<br />
045 St. Vincent De Paul Residence – Dental Only<br />
052 Religious Bro<strong>the</strong>rs and Sisters – No Medical. Dental & Vision Only<br />
Division Codes.Arch System Revised 07/01/09
THE ARCHDIOCESE OF NEW YORK<br />
NOTICE<br />
CHANGE NAME OF CONTACT LISTED ON<br />
MONTHLY INSURANCE BILLING STATEMENT<br />
__________________________________________________________________ _______________<br />
INSTITUTION NAME INSTITUTION #<br />
__________________________________________________________________<br />
STREET ADDRESS<br />
________________________________________________________________________<br />
CITY AND STATE<br />
________________________________________________________________________<br />
TELEPHONE NUMBER<br />
________________________________________________________________________<br />
FAX NUMBER<br />
________________________________________________________________________<br />
CURRENT CONTACT<br />
________________________________________________________________________<br />
NEW CONTACT<br />
_________________<br />
TITLE<br />
_________________<br />
TITLE<br />
__________________________________________________________________<br />
EFFECTIVE DATE OF CHANGE<br />
________________________________________________________________________<br />
SIGNATURE OF PASTOR/PRINCIPAL<br />
________________________________________________________________________<br />
PASTOR/PRINCIPAL PRINT NAME<br />
________________________________________________________________________<br />
SIGNATURE OF LOCAL ADMINISTRATOR<br />
________________________________________________________________________<br />
LOCAL ADMINISTRATOR PRINT NAME<br />
_________________<br />
DATE<br />
_________________<br />
DATE<br />
_________________<br />
DATE<br />
_________________<br />
DATE<br />
SEND FORM TO:<br />
EMPLOYEE BENEFIT CONNECTIONS<br />
1011 FIRST AVENUE – ROOM 1679<br />
NEW YORK, NEW YORK 10022<br />
FAX 212.644.0690<br />
11/2008
HEALTH INSURANCE PORTABILITY & ACCOUNTABILITY ACT<br />
(HIPAA)<br />
NOTICE OF PRIVACY PRATICES<br />
-8-
Revised: January 1, 2006 Effective: April 14, 2003<br />
NOTICE OF PRIVACY PRACTICES<br />
UNDER FEDERAL PRIVACY REGULATIONS YOUR MEDICAL RECORD IS PROTECTED<br />
FROM DISCLOSURE AND YOU ARE GRANTED SPECIFIC RIGHTS TO CONTROL HOW<br />
YOUR HEALTH INFORMATION IS USED. THIS NOTICE OF PRIVACY PRACTICES<br />
DESCRIBES HOW MEDICAL INFORMATION ABOUT YOU MAY BE USED AND DISCLOSED<br />
AND HOW YOU CAN GET ACCESS TO THIS INFORMATION. PLEASE REVIEW IT<br />
CAREFULLY.<br />
We Respect and Protect Your Privacy<br />
Respect for your privacy, especially with regard to Protected Health Information, has long been<br />
highly valued by your employer. We are committed to providing you with quality health care and<br />
services that meet your needs. That commitment includes protecting personal health information we<br />
obtain about you. Your employer, in accordance with applicable federal and state law, is committed<br />
to maintaining <strong>the</strong> privacy <strong>of</strong> your personal health information.<br />
New federal health privacy regulations that were issued as a result <strong>of</strong> <strong>the</strong> Health Insurance Portability<br />
& Accountability Act <strong>of</strong> 1996 (HIPAA) establishes broad individual privacy rights, obligates your<br />
health provider to keep your medical records confidential, and ensures that your employer cannot<br />
have access to your health information for employment purposes. In addition, HIPAA requires all<br />
health care records and o<strong>the</strong>r individually identifiable health information used or disclosed by us in<br />
any form, whe<strong>the</strong>r electronically, on paper, or orally, be kept confidential.<br />
This federal law gives you, <strong>the</strong> plan participant, significant <strong>new</strong> rights to understand and control how<br />
your health information is used. HIPAA imposes penalties if we misuse your personal health<br />
information. As required by HIPAA, we have prepared this Notice <strong>of</strong> Privacy Practices (Notice) to<br />
explain (1) your specific rights to access and control your personal health information, (2) how we are<br />
required to maintain <strong>the</strong> privacy <strong>of</strong> your health information, and (3) <strong>the</strong> limited circumstances in<br />
which we may use and disclose your health information.<br />
Who Will Follow This Notice<br />
This Notice describes <strong>the</strong> Protected Health Information practices <strong>of</strong> (a) your employer, (b) <strong>the</strong> group<br />
health plan it participates in, which is sponsored by <strong>the</strong> Archdiocese <strong>of</strong> New York (<strong>the</strong> “Plan”), and<br />
(c) that <strong>of</strong> any third party that assists in <strong>the</strong> <strong>administration</strong> <strong>of</strong> Plan claims.<br />
Our Pledge Regarding Protected Health Information<br />
We understand that Protected Health Information about you and your health is personal. We are<br />
This Notice is Also Available in Spanish
Revised: January 1, 2006 Effective: April 14, 2003<br />
committed to protecting Protected Health Information about you. We create a record <strong>of</strong> <strong>the</strong> health<br />
care claims reimbursed under <strong>the</strong> Plan for Plan <strong>administration</strong> purposes. This Notice applies to all <strong>of</strong><br />
<strong>the</strong> medical records we maintain. Your personal doctor or health care provider may have different<br />
policies or notices regarding <strong>the</strong> doctor’s use and disclosure <strong>of</strong> your Protected Health Information<br />
created in <strong>the</strong> doctor’s <strong>of</strong>fice or clinic.<br />
Your Rights Regarding Your Protected Health Information<br />
You and your legal representative, if any, have <strong>the</strong> following rights with respect to <strong>the</strong> Protected<br />
Health Information we have about you in our records.<br />
Right to Inspect and Copy. You have <strong>the</strong> right to inspect and copy Protected Health Information<br />
that may be used to make decisions about your Plan <strong>benefits</strong>. To inspect and copy Protected Health<br />
Information that may be used to make decisions about you, you must submit your request in writing.<br />
If you request a copy <strong>of</strong> <strong>the</strong> information, we may charge a fee for <strong>the</strong> costs <strong>of</strong> copying, mailing or<br />
o<strong>the</strong>r supplies associated with your request.<br />
We may deny your request to inspect and copy in certain very limited circumstances. If you are<br />
denied access to Protected Health Information, you may request that <strong>the</strong> denial be reviewed.<br />
Right to Amend. If you feel that Protected Health Information we have about you is incorrect or<br />
incomplete, you may ask us to amend <strong>the</strong> information. You have <strong>the</strong> right to request an amendment<br />
for as long as <strong>the</strong> information is kept by or for <strong>the</strong> Plan. In addition, you must provide a reason that<br />
supports your request. We may deny your request for an amendment if it is not in writing or does not<br />
include a reason to support <strong>the</strong> request. In addition, we may deny your request if you ask us to<br />
amend information that:<br />
• is not part <strong>of</strong> <strong>the</strong> Protected Health Information kept by or for <strong>the</strong> Plan:<br />
• was not created by us, unless <strong>the</strong> person or entity that created <strong>the</strong> information is no<br />
longer available to make <strong>the</strong> amendment;<br />
• is not part <strong>of</strong> <strong>the</strong> information which you would be permitted to inspect and copy; or<br />
• is accurate and complete.<br />
Right to an Accounting <strong>of</strong> Disclosures. You have <strong>the</strong> right to request an “accounting <strong>of</strong><br />
disclosures” <strong>of</strong> your Protected Health Information made to you or our personal representative by <strong>the</strong><br />
Plan in <strong>the</strong> six years prior to <strong>the</strong> date on which <strong>the</strong> accounting is requested, except for disclosures:<br />
• to carry out treatment, payment, or health care operations;<br />
• pursuant to a valid authorization; or<br />
• incident to a permitted or required use or disclosure.<br />
Your request must state a time period, which may not be longer than six years and may not include<br />
dates before April, 2003. Your request should indicate in what form you want <strong>the</strong> list (for example,<br />
paper or electronic). The first list you request within a 12-month period will be free. For additional<br />
lists, we may charge you for <strong>the</strong> costs <strong>of</strong> providing <strong>the</strong> list. We will notify you <strong>of</strong> <strong>the</strong> cost involved<br />
and you may choose to withdraw or modify your request at that time before any costs are incurred.<br />
Right to Request Restrictions. You have <strong>the</strong> right to request a restriction or limitation on <strong>the</strong><br />
Protected Health Information we use or disclose about you for treatment, payment or health care<br />
operations. You also have <strong>the</strong> right to request a limit on <strong>the</strong> Protected Health Information we<br />
disclose about you to someone who is involved in your care or <strong>the</strong> payment for your care, like a<br />
family member or friend. For example, you could ask that we not use or disclose information about<br />
This Notice is Also Available in Spanish
Revised: January 1, 2006 Effective: April 14, 2003<br />
a surgery you had.<br />
We are not required to agree to your request. In your request, you must tell us (1) what information<br />
you want to limit; (2) whe<strong>the</strong>r you want to limit our use, disclosure or both; and (3) to whom you<br />
want <strong>the</strong> limits to apply.<br />
Right to Request Confidential Communications. You have <strong>the</strong> right to request that we<br />
communicate with you about medical matters in a certain way or at a certain location. For example,<br />
you can ask that we only contact you at work or by mail. We will not ask you <strong>the</strong> reason for your<br />
request. We will accommodate all reasonable requests. Your request must specify how or where you<br />
wish to be contacted.<br />
Right to a Paper Copy <strong>of</strong> This Notice. You have <strong>the</strong> right to a paper copy <strong>of</strong> this Notice. You<br />
may ask us to give you a copy <strong>of</strong> this Notice at any time. Even if you have agreed to receive this<br />
Notice electronically, you are still entitled to a paper copy <strong>of</strong> this Notice.<br />
If you wish to make any <strong>of</strong> <strong>the</strong> requests listed above under “Your Rights Regarding Your Protected Health<br />
Information”, you must complete and mail to United Healthcare <strong>the</strong> appropriate form. To obtain <strong>the</strong> form please call<br />
<strong>the</strong> United Healthcare phone number on <strong>the</strong> back <strong>of</strong> your United Healthcare ID card. Forms should be mailed to<br />
<strong>the</strong> address printed on <strong>the</strong> forms. After United Healthcare receives your signed, completed form, United Healthcare<br />
will respond to your request.<br />
You may obtain a copy <strong>of</strong> this Notice from <strong>the</strong> Plan sponsor’s website, www.archny.org<br />
To obtain a paper copy <strong>of</strong> this Notice, call <strong>the</strong> Plan sponsor at (212) 371-1011, Ext. 3034.<br />
Our Responsibilities With Respect to Your Protected Health Information<br />
We are required by law to:<br />
• make sure that Protected Health Information that identifies you is kept private;<br />
• give you this Notice <strong>of</strong> our legal duties and privacy practices with respect to Protected<br />
Health Information about you;<br />
• follow <strong>the</strong> terms <strong>of</strong> <strong>the</strong> Notice that is currently in effect;<br />
• notify you if we cannot accommodate a requested restriction or request;<br />
• accommodate your reasonable requests regarding methods to communicate health<br />
information with you; and<br />
• accommodate your request for an accounting <strong>of</strong> disclosures.<br />
Your Authorization to Use and Disclose Your Protected Health Information<br />
General uses and disclosures <strong>of</strong> Protected Health Information not covered by this Notice or <strong>the</strong> laws<br />
that apply to us will be made only with your written permission. If you provide us permission to use<br />
or disclose Protected Health Information about you, you may revoke that permission, in writing, at<br />
any time. If you revoke your permission, we will no longer use or disclose Protected Health<br />
Information about you for <strong>the</strong> reasons covered by your written authorization. You understand that<br />
we are unable to take back any disclosures we have already made with your permission, and that we<br />
are required to retain our records <strong>of</strong> <strong>the</strong> care that we provided to you.<br />
This Notice is Also Available in Spanish
Revised: January 1, 2006 Effective: April 14, 2003<br />
Limited Circumstances in Which We May Use and Disclose Your Protected Health<br />
Information<br />
The following categories describe <strong>the</strong> limited ways that we use and disclose Protected Health<br />
Information. For each category <strong>of</strong> uses or disclosures we will explain what we mean and present<br />
some examples. Not every use or disclosure in a category will be listed. However, all <strong>of</strong> <strong>the</strong> ways we<br />
are permitted to use and disclose information will fall within one <strong>of</strong> <strong>the</strong> categories.<br />
For Treatment (as described in applicable regulations). We may use or disclose Protected Health<br />
Information about you to facilitate medical treatment or services by providers. We may disclose<br />
Protected Health Information about you to providers, including doctors, nurses, technicians, medical<br />
students, or o<strong>the</strong>r hospital personnel who are involved in taking care <strong>of</strong> you. For example, we might<br />
disclose information about your prior prescriptions to a pharmacist to determine if a pending<br />
prescription is contraindicative with prior prescriptions.<br />
For Payment (as described in applicable regulations). We may use and disclose Protected Health<br />
Information about you to determine eligibility for Plan <strong>benefits</strong>, to facilitate payment for <strong>the</strong><br />
treatment and services you receive from health care providers, to determine benefit responsibility<br />
under <strong>the</strong> Plan, or to coordinate Plan coverage. For example, we may tell your health care provider<br />
about your medical history to determine whe<strong>the</strong>r a particular treatment is experimental,<br />
investigational, or medically necessary or to determine whe<strong>the</strong>r <strong>the</strong> Plan will cover <strong>the</strong> treatment. We<br />
may also share Protected Health Information with a utilization review or precertification service<br />
provider. Likewise, we may share Protected Health Information with ano<strong>the</strong>r entity to assist with <strong>the</strong><br />
adjudication or subrogation <strong>of</strong> health claims or to ano<strong>the</strong>r health plan to coordinate benefit<br />
payments.<br />
For Health Care Operations (as described in applicable regulations). We may use and disclose<br />
Protected Health Information about you for o<strong>the</strong>r Plan operations. These uses and disclosures are<br />
necessary to run <strong>the</strong> Plan. For example, we may use Protected Health Information in connection<br />
with: conducting quality assessment and improvement activities; underwriting, premium rating, and<br />
o<strong>the</strong>r activities relating to Plan coverage; submitting claims for stop-loss (or excess loss) coverage;<br />
conducting or arranging for medical review, legal services, audit services, and fraud and abuse<br />
detection programs; business planning and development such as cost management; and business<br />
management and general Plan administrative activities.<br />
As Required By Law. We will disclose Protected Health Information about you when required to<br />
do so by federal, state or local law. For example, we may disclose Protected Health Information<br />
when required by a court order in a litigation proceeding such as a malpractice action.<br />
To Avert a Serious Threat to Health or Safety. We may use and disclose medical information<br />
about you when necessary to prevent a serious threat to your health and safety or <strong>the</strong> health and<br />
safety <strong>of</strong> <strong>the</strong> public or ano<strong>the</strong>r person. Any disclosure, however, would only be to someone able to<br />
help prevent <strong>the</strong> threat. For example, we may disclose Protected Health Information about you in a<br />
proceeding regarding <strong>the</strong> licensure <strong>of</strong> a physician.<br />
This Notice is Also Available in Spanish
Revised: January 1, 2006 Effective: April 14, 2003<br />
Specific Situations<br />
We may disclose your Protected Health Information under <strong>the</strong> following specific situations:<br />
Disclosure to Health Plan Sponsor. Information maintained by <strong>the</strong> Archdiocese <strong>of</strong> New York<br />
may be disclosed to ano<strong>the</strong>r health plan for purposes <strong>of</strong> facilitating claims payments under that plan.<br />
In addition, Protected Health Information may be disclosed to Archdiocesan personnel solely for<br />
purposes <strong>of</strong> administering <strong>benefits</strong> under <strong>the</strong> Plan.<br />
Disclosure to Business Associate. Business Associate may use and disclose Protected Health<br />
Information for <strong>the</strong> proper management and <strong>administration</strong> <strong>of</strong> <strong>the</strong> Business Associate or to meet its<br />
legal responsibilities. Such Protected Health Information may only be disclosed for such purposes if<br />
<strong>the</strong> disclosures are Required By Law or <strong>the</strong> Business Associate obtains certain reasonable assurances<br />
from <strong>the</strong> person to who <strong>the</strong> information is disclosed.<br />
Organ and Tissue Donation. If you are an organ donor, we may release Protected Health<br />
Information to organizations that handle organ procurement or organ, eye or tissue transplantation<br />
or to an organ donation bank, as necessary to facilitate organ or tissue donation and transplantation.<br />
Military and Veterans. If you are a member <strong>of</strong> <strong>the</strong> armed forces, we may release Protected Health<br />
Information about you as required by military command authorities. We may also release Protected<br />
Health Information about foreign military personnel to <strong>the</strong> appropriate foreign military authority.<br />
Workers’ Compensation. We may release Protected Health Information about you for workers’<br />
compensation or similar programs. These programs provide <strong>benefits</strong> for work-related injuries or<br />
illness.<br />
Public Health Risks. We may disclose Protected Health Information about you for public health<br />
activities. These activities generally include <strong>the</strong> following:<br />
• to prevent or control disease, injury or disability;<br />
• to report births and deaths;<br />
• to report child abuse or neglect;<br />
• to report reactions to medications or problems with products;<br />
• to notify people <strong>of</strong> recalls <strong>of</strong> products <strong>the</strong>y may be using;<br />
• to notify a person who may have been exposed to a disease or may be at risk for<br />
contracting or spreading a disease or condition;<br />
• to notify <strong>the</strong> appropriate government authority if we believe a patient has been <strong>the</strong><br />
victim <strong>of</strong> abuse, neglect or domestic violence. We will only make this disclosure if you<br />
agree or when required or authorized by law.<br />
Health Oversight Activities. We may disclose Protected Health Information to a health oversight<br />
agency for activities authorized by law. These oversight activities include, for example, audits,<br />
investigations, inspections, and licensure. These activities are necessary for <strong>the</strong> government to<br />
monitor <strong>the</strong> health care system, government programs, and compliance with civil rights laws.<br />
Lawsuits and Disputes. If you are involved in a lawsuit or a dispute, we may disclose Protected<br />
Health Information about you in response to a court or administrative order. We may also disclose<br />
Protected Health Information about you in response to a subpoena discovery request, or o<strong>the</strong>r lawful<br />
process by someone else involved in <strong>the</strong> dispute, but only if efforts have been made to tell you about<br />
<strong>the</strong> request or to obtain an order protecting <strong>the</strong> information requested.<br />
This Notice is Also Available in Spanish
Revised: January 1, 2006 Effective: April 14, 2003<br />
Law Enforcement. We may release Protected Health Information if asked to do so by a law<br />
enforcement <strong>of</strong>ficial:<br />
• in response to a court order, subpoena, warrant, summons or similar process;<br />
• to identify or locate a suspect, fugitive, material witness, or missing person;<br />
• about <strong>the</strong> victim <strong>of</strong> a crime if, under certain limited circumstances, we are unable to obtain<br />
<strong>the</strong> person’s agreement; and<br />
• in emergency circumstances to report a crime; <strong>the</strong> location <strong>of</strong> <strong>the</strong> crime or victims;<br />
or <strong>the</strong> identity, description or location <strong>of</strong> <strong>the</strong> person who committed <strong>the</strong> crime.<br />
Coroners, Medical Examiners and Funeral Directors. We may release Protected Health<br />
Information to a coroner or medical examiner. We may also release Protected Health Information<br />
about members <strong>of</strong> <strong>the</strong> Plan to funeral directors as necessary to carry out <strong>the</strong>ir duties.<br />
National Security and Intelligence Activities. We may release Protected Health Information<br />
about you to authorized federal <strong>of</strong>ficials for intelligence, counter intelligence, and o<strong>the</strong>r national<br />
security activities authorized by law.<br />
Inmates. If you are an inmate <strong>of</strong> a correctional institution or under <strong>the</strong> custody <strong>of</strong> a law<br />
enforcement <strong>of</strong>ficial, we may release Protected Health Information about you to <strong>the</strong> correctional<br />
institution or law enforcement <strong>of</strong>ficial. This release would be necessary (1) for <strong>the</strong> institution to<br />
provide you with health care; (2) to protect your health and safety or <strong>the</strong> health and safety <strong>of</strong> o<strong>the</strong>rs;<br />
or (3) for <strong>the</strong> safety and security <strong>of</strong> <strong>the</strong> correctional institution.<br />
Change to This Notice<br />
We reserve <strong>the</strong> right to change this notice. We reserve <strong>the</strong> right to make <strong>the</strong> revised or changed<br />
notice effective for Protected Health Information we already have about you as well as any<br />
information we receive in <strong>the</strong> future. We will post a copy <strong>of</strong> <strong>the</strong> current notice on <strong>the</strong> Plan website.<br />
This notice and future notices will contain on <strong>the</strong> first page, in <strong>the</strong> top right-hand corner, <strong>the</strong><br />
effective date.<br />
This Notice is Also Available in Spanish
Revised: January 1, 2006 Effective: April 14, 2003<br />
More Information or Complaints<br />
If you want more information about your privacy rights, do not understand your privacy<br />
rights, are concerned that your privacy rights have been violated or disagree with a decision<br />
that your employer, <strong>the</strong> Archdiocese <strong>of</strong> New York and/or United Healthcare made about<br />
access to your confidential information, you may contact your employer, <strong>the</strong> Plan sponsor’s<br />
Privacy Office or United Healthcare’s Privacy Office. If you choose, you may also file a<br />
complaint with <strong>the</strong> Secretary <strong>of</strong> <strong>the</strong> U.S. Department <strong>of</strong> Health and Human Services. Any<br />
such complaint would be addressed to:<br />
Secretary <strong>of</strong> <strong>the</strong> U.S. Department <strong>of</strong> Health and Human Services, Region II Office for Civil<br />
Rights U.S. Department <strong>of</strong> Health and Human Services, Jacob Javits Federal Building 26<br />
Federal Plaza - Suite 3302 New York, NY 10278 Telephone number 212-264-3313<br />
Your employer, <strong>the</strong> Archdiocese <strong>of</strong> New York and United Healthcare will not take any action<br />
against you if you file a complaint with <strong>the</strong> Secretary or United Healthcare. The Privacy Office<br />
for <strong>the</strong> Archdiocese <strong>of</strong> New York may be contacted at:<br />
Director <strong>of</strong> Life & Health Benefit Programs, Privacy Officer <strong>of</strong> <strong>the</strong> Archdiocese <strong>of</strong> New<br />
York, 1011 First Avenue New York, New York 10022, Telephone number (212) 371-1011,<br />
Ext. 3034<br />
You may contact United Healthcare’s Privacy Office at:<br />
Privacy Office at United Healthcare, Customer Service-Privacy Unit, P.O. Box 740815,<br />
Atlanta, GA, 30374-0815, Telephone number: (800) 736-1264<br />
All complaints must be submitted in writing.<br />
This Notice is Also Available in Spanish
ARCHDIOCESE OF NEW YORK<br />
AUTHORIZATION FOR RELEASE OF INFORMATION<br />
_____________________________________________________________________________________________________________________<br />
Section A: Must be completed for all authorizations<br />
I hereby authorize <strong>the</strong> use or disclosure <strong>of</strong> my individually identifiable health information as described below. I<br />
understand that this authorization is voluntary. I understand that if <strong>the</strong> organization authorized to receive <strong>the</strong><br />
information is not a health plan or health care provider, <strong>the</strong> released information may no longer be protected by<br />
federal privacy regulations.<br />
Patient/Participant Name _____________________________ SSN: _____________________<br />
Persons/organizations providing <strong>the</strong> information: Person/organizations to receive <strong>the</strong> information:<br />
__________________________________________ ___________________________________________<br />
__________________________________________ ___________________________________________<br />
Specific description <strong>of</strong> information (including date(s)): ______________________________________________<br />
_____________________________________________________________________________________________<br />
_____________________________________________________________________________________________<br />
_____________________________________________________________________________________________<br />
IF THE REQUESTED RECORDS CONTAIN INFORMATION PERTAINING TO PSYCHIATRIC OR<br />
MENTAL HEALTH, DRUG OR ALCOHOL TREATMENT, OR HIV RELATED INFORMATION, YOU MUST<br />
SPECIFICALLY CONSENT TO THE RELEASE OF SUCH INFORMATION BY INITIALING ONE OR<br />
MORE OF THE FOLLOWING:<br />
____ I understand that if my records contain information pertaining to diagnosis and/or treatment for<br />
alcoholism and/or drug abuse or dependency, such information will be released pursuant to this<br />
authorization form.<br />
____ I understand that if my records contain information pertaining to diagnosis and/or treatment regarding<br />
psychiatric and/or mental health issues, such information will be released pursuant to this authorization form.<br />
____ I understand that if my records contain information pertaining to HIV antibody test results and/or AIDS<br />
diagnosis and treatment, such information will be released pursuant to this authorization form.<br />
Restrictions? Yes___ No___ If yes, please describe: _______________________________<br />
_____________________________________________________________________________________________<br />
_____________________________________________________________________________________________<br />
Section B: Must be completed only if a health plan or a health care provider has requested <strong>the</strong> authorization<br />
1. The health plan or health care provider must complete <strong>the</strong> following:<br />
a. What is <strong>the</strong> purpose <strong>of</strong> <strong>the</strong> use or disclosure? ___________________________________________________<br />
_________________________________________________________________________________________<br />
b. Will <strong>the</strong> health plan or health care provider requesting <strong>the</strong> authorization receive financial or in-kind<br />
compensation in exchange for using or disclosing <strong>the</strong> health information described above?<br />
Yes ____ No _____<br />
2. The patient or <strong>the</strong> patient's representative must read and initial <strong>the</strong> following statements:<br />
a. I understand that my health care treatment and payment, my enrollment in <strong>the</strong> health plan and my<br />
eligibility for <strong>benefits</strong> will not be affected if I do not sign this form. Initials: ________<br />
b. I understand that I may see and copy <strong>the</strong> information described on this form if I ask for it, and that I will<br />
get a copy <strong>of</strong> this form after I sign it. Initials: __________<br />
Section C: Must be completed for all authorizations<br />
The patient or <strong>the</strong> patient's representative must read and initial <strong>the</strong> following statements:<br />
- 9 -<br />
NY01/LASKA/855065.1
1. I understand that this authorization will expire (select a. or b.):<br />
a. on __ __/__ __/__ __ __ __ (DD/MM/YYYY) Initials: _________<br />
b. at <strong>the</strong> occurrence <strong>of</strong> <strong>the</strong> following event: __________________________________Initials: _________<br />
2. I understand that I may revoke this authorization at any time by notifying <strong>the</strong> plan in writing, but if I do it won't have<br />
any affect on any actions taken before my revocation was received. Initials: ________<br />
______________________________________________________<br />
Signature <strong>of</strong> individual or individual’s representative<br />
(Form MUST be completed before signing)<br />
____________________________<br />
Date<br />
Printed name <strong>of</strong> individual's representative(if applicable):____________________________________________<br />
Description <strong>of</strong> representative’s authority to act for <strong>the</strong> individual: _____________________________________<br />
*YOU MAY REFUSE TO SIGN THIS AUTHORIZATION*<br />
NY01/LASKA/855065.1
AUTHORIZATION FOR THE USE AND DISCLOSURE OF INFORMATION<br />
This authorization must be dated and signed by <strong>the</strong> individual or by a person authorized by law to give this authorization. File<br />
copy and facsimile transmission are considered equivalent to <strong>the</strong> original (unless applicable state law provides o<strong>the</strong>rwise). If<br />
UnitedHealthcare seeks <strong>the</strong> authorization from an individual for a use or disclosure <strong>of</strong> Protected Health Information (PHI),<br />
UnitedHealthcare must provide <strong>the</strong> individual with a copy <strong>of</strong> <strong>the</strong> signed authorization.<br />
I authorize United HealthCare Insurance Company, and its subsidiaries/affiliates (“UnitedHealthcare”), to use or disclose my medical,<br />
claim, or benefit records, including any individually identifiable health information contained in <strong>the</strong>se records, as described below. I<br />
understand <strong>the</strong>se records may contain information created by o<strong>the</strong>r persons or entities, including physicians and o<strong>the</strong>r health care<br />
providers as well as information regarding <strong>the</strong> use <strong>of</strong> drug and alcohol treatment services, HIV/AIDS treatment, mental health services<br />
[Note: Psycho<strong>the</strong>rapy notes may be used/disclosed only pursuant to a separate authorization pertaining only to psycho<strong>the</strong>rapy notes],<br />
reproductive health services, and treatment for sexually transmitted diseases.<br />
1. Persons/entities authorized to receive <strong>the</strong> information (including address <strong>of</strong> where information should be sent, if applicable):<br />
Name:<br />
Address:<br />
_____________________________________________________________________________________<br />
_____________________________________________________________________________________<br />
2. Type <strong>of</strong> information UnitedHealthcare is authorized to use or disclose:<br />
____________________________________________________________________________________________________<br />
____________________________________________________________________________________________________<br />
3. The information will be used or disclosed for <strong>the</strong> following purposes: At <strong>the</strong> request <strong>of</strong> <strong>the</strong> Individual<br />
4. I understand that I may revoke this authorization at any time by notifying UnitedHealthcare in writing at PO Box 740800, Atlanta,<br />
GA, 30374-0800, except to <strong>the</strong> extent that:<br />
(a) UnitedHealthcare has taken action in reliance on this authorization; or<br />
(b) If authorization was obtained as a condition for obtaining insurance coverage, o<strong>the</strong>r law provides <strong>the</strong> insurer with <strong>the</strong> right to<br />
contest a claim under <strong>the</strong> policy.<br />
5. This authorization expires [on] [upon] ________________[date] or is valid ______________ [event]. Please note: This<br />
authorization may be valid for a maximum time period <strong>of</strong> one year.<br />
I understand that once health information about me has been disclosed by United HealthCare Insurance Company to a third party, <strong>the</strong><br />
health information may no longer be protected by federal privacy laws.<br />
___________________________________________________________________________________________________________<br />
Printed name <strong>of</strong> individual or individual's representative<br />
___________________________________________________________________________________________________________<br />
If representative, relationship to individual and authority to act for individual<br />
_____________________________________________________ _______________________ ______________________<br />
Signature <strong>of</strong> individual Subscriber Id # Date<br />
Form: AUTH MEM 011504 - 10 -
Eligibility<br />
Effective Date<br />
Employee Contribution<br />
Benefit Summary<br />
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefits Eligibility<br />
Employees who are regularly scheduled to work a minimum <strong>of</strong> 20 hours each week.<br />
Eligible dependent spouse.<br />
Unmarried, dependent children (natural or adopted) are eligible until <strong>the</strong> end <strong>of</strong><br />
<strong>the</strong> calendar year in which <strong>the</strong> child turns 19 years old. Dependent children<br />
enrolled as full time college students are eligible unitl <strong>the</strong> end <strong>of</strong> <strong>the</strong> year <strong>the</strong><br />
child turns 25 years old as long as he/she is unmarried and enrolled in an<br />
accredited school on a full time basis.<br />
First <strong>of</strong> <strong>the</strong> month following 30 days <strong>of</strong> employment, provided you have<br />
completed <strong>the</strong> health enrollment form. **(Refer to footnotes)<br />
Fixed schedule based on type <strong>of</strong> coverage elected and regularly scheduled<br />
work hours.<br />
Refer to <strong>the</strong> following section which describes:<br />
*United Healthcare Choice Plus Plans: (In -network providers can be accessed<br />
via 800.736.1264 or www.myuhc.com)<br />
*Medicare Supplement for Retired Lay Employees over age 65, Clergy and Religious<br />
who have Medicare Primary Benefits. (MSYRX)<br />
*Notice <strong>of</strong> Privacy Practice (To be given to all health plan participants)<br />
*Authorization for Use and Disclosure <strong>of</strong> Private Health Information.<br />
(Health plan participants must complete and sign form to authorize local<br />
<strong>benefits</strong> administrator to help resolve health claim issues. Additional form is<br />
required by <strong>the</strong> health plan participant to authorize o<strong>the</strong>r persons to use and<br />
disclosure <strong>of</strong> medical claims information such as family member etc.)<br />
**Effective date is immediate for:<br />
Divs. 001 thru 005 - Bargaining/Non-Bargaining Lay Faculty<br />
Div. 040 - Non-Bargaining Lay Employees <strong>of</strong> CHSA<br />
Divs. 043 & 044 - Aegis <strong>of</strong> Religious Orders for Parish/CHSA & Private schools<br />
Divs. 050 & 051 - Religious Bro<strong>the</strong>rs & Sisters<br />
Div. 053 & 156 - Clergy<br />
Div. 055 - Seminarians<br />
Div. 153 - Clergy with Medicare Primary Coverage<br />
Div. 154 - Active and Retired Religious with Medicare Primary Coverage<br />
**Effective date is first <strong>of</strong> <strong>the</strong> month following 30 days <strong>of</strong> service:<br />
Div. 006 - Trustees <strong>of</strong> St. Patrick's Ca<strong>the</strong>dral<br />
Div. 024 - Non-Bargaining Lay Employees <strong>of</strong> Cemeteries<br />
Div. 030A - Lay Employees <strong>of</strong> Outside Affiliated Agencies<br />
Div. 030B - Employees <strong>of</strong> Dominican Sisters<br />
Div. 031 - Catholic Charities<br />
Div. 032 - Non Bargaining Lay Employees <strong>of</strong> Private Schools<br />
Div. 033 - Central Services<br />
Div. 034 - Non Bargaining Lay Employees <strong>of</strong> Parishes and Parish Schools<br />
Div. 035 - Office <strong>of</strong> Drug Education (ADAPP)<br />
Div. 037 - St. Raymond's Cemetery (Non-Bargaining Employees)<br />
Div. 038 - Lay Employees <strong>of</strong> Dominican Fa<strong>the</strong>rs<br />
Div. 045 - St. Vincent de Paul Residence<br />
Grandfa<strong>the</strong>red closed group Div. 134 - Active Non-Bargaining Lay Employee with Medicare Primary (>age 65 & < 20 ees)<br />
**Effective date is three months for:<br />
Div. 017 - Mission <strong>of</strong> <strong>the</strong> Immaculate Virgin (Non-bargaining)<br />
Div. 018 - Cabrini Home<br />
Div. 019 - St. Dominic's Home<br />
Div. 025 - Incarnation Children Center<br />
Div. 036 - Beacon <strong>of</strong> Hope<br />
Div. 047 - Mission <strong>of</strong> <strong>the</strong> Immaculate Virgin (Bargaining Unit)<br />
11 07/2009
HOW TO ENROLL IN THE GROUP HEALTH BENEFIT PLAN<br />
AND/OR<br />
MAKE CHANGES TO A MEMBERS GROUP HEALTH BENEFIT COVERAGE<br />
OR CHANGE PERSONAL INFORMATION<br />
To enroll a <strong>new</strong> member, or to make changes to an existing member’s benefit<br />
Information:<br />
• The member must manually complete a “Health Benefit Plan Enrollment and<br />
Change Form”<br />
The <strong>new</strong> member should return <strong>the</strong> completed enrollment forms, to <strong>the</strong>ir local <strong>benefits</strong><br />
administrator. The local administrator should retain copies <strong>of</strong> <strong>the</strong> completed forms for <strong>the</strong>ir<br />
records, and forward <strong>the</strong> original forms to:<br />
Employee Benefit Connections<br />
1011 First Avenue – Room 1679<br />
New York, NY 10022<br />
212.371.1000, Ext. 3060 Fax 212.644.0690<br />
Employee Benefit Connections must have <strong>the</strong> completed enrollment information, with all<br />
required documentation within 30 days <strong>of</strong> date <strong>of</strong> eligibility. Incomplete<br />
applications, or applications received more than 30 days after <strong>the</strong> effective date will<br />
NOT be processed. This applies to <strong>new</strong> enrollments, and as well as changes. Failure<br />
to comply can result in loss <strong>of</strong> member’s coverage.<br />
CHANGES TO HEALTH BENEFITS<br />
The member must complete a Health Benefit Plan Enrollment & Change Form,<br />
and attach any required documentation, and submit <strong>the</strong> form and documents to<br />
<strong>the</strong>ir local administrator. The administrator is responsible to review <strong>the</strong> forms and<br />
documents for accuracy and completeness, make copies for <strong>the</strong>ir records, and<br />
mail <strong>the</strong> original forms to Employee Benefit Connections (Address listed on<br />
form) for processing.<br />
TO OBTAIN HEALTH BENEFIT PLAN ENROLLMENT AND CHANGE<br />
FORMS PLEASE CONTACT EMPLOYEE BENEFIT CONNECTIONS AT:<br />
212.371.1000, EXT. 3060<br />
- 12 -<br />
Revised 07/2009
ADDITIONAL INFORMATION CONCERNING CHANGES PERMITTED<br />
OUTSIDE OF INITIAL ELIGIBILITY PERIOD AND OPEN ENROLLMENT<br />
Qualified Life Events:<br />
The following are qualified life events* which would permit employees and <strong>the</strong>ir<br />
eligible dependents to special enroll in <strong>the</strong> group medical plan outside <strong>the</strong> initial<br />
enrollment or open enrollment period:<br />
• Loss <strong>of</strong> o<strong>the</strong>r medical coverage due to loss <strong>of</strong> employment or reduction in hours<br />
• Marriage<br />
• Birth or adoption <strong>of</strong> a child<br />
• Death <strong>of</strong> employee spouse through whom member had medical coverage<br />
O<strong>the</strong>r Changes Permitted:<br />
• Terminate medical coverage for member, member’s spouse/child who is no longer an<br />
eligible dependent under <strong>the</strong> terms <strong>of</strong> <strong>the</strong> group medical plan<br />
• Change <strong>of</strong> home address, martial status<br />
• Change <strong>of</strong> base salary (effects <strong>the</strong> amount <strong>of</strong> Life, AD&D and LTD Insurance)<br />
• Retirement<br />
• Under certain circumstances, when a member <strong>of</strong> <strong>the</strong> Clergy aged 65 & over, is fully<br />
retired and has enrolled in Medicare (Part A and Part B) Coverage, medical coverage<br />
may be changed to a Medicare Supplemental Plan. A photocopy <strong>of</strong> <strong>the</strong> Medicare card<br />
must accompany <strong>the</strong> <strong>new</strong> health enrollment form. **<br />
• Religious Sister who reaches age 65 and eligible for Medicare (Part A and Part B)<br />
Coverage. Secure a copy <strong>of</strong> <strong>the</strong> Medicare I.D. card and attach <strong>the</strong> copy to <strong>the</strong> Health<br />
Benefit Plan Enrollment & Change Form and mail it to Employee Benefit Connections,<br />
1011 First Avenue, Room 1679, New York, New York 10022.<br />
* Documentation will be required to validate life event<br />
** Contact Employee Benefit Connections (212.371.1000, Ext. 3060) for details.<br />
Revised 07/2009
Annual Salary<br />
(Benefit<br />
Administrator Use<br />
Only)<br />
$______________<br />
ARCHDIOCESE OF NEW YORK<br />
HEALTH BENEFIT PLAN ENROLLMENT & CHANGE FORM<br />
Note: Return your completed form to you Local Benefits Administrator within 30 days <strong>of</strong> <strong>the</strong> date <strong>of</strong> enrollment, a life event, date <strong>of</strong> any change(s). Failure to do so may<br />
result in loss <strong>of</strong> coverage.<br />
Effective Date <strong>of</strong><br />
Coverage or<br />
Change<br />
Month/Day/Year<br />
/ /<br />
Please indicate <strong>the</strong> reason you are completing this form:<br />
❑ New Hire ❑ Open Enrollment ❑ Waive Coverage ❑ Marital/ Status Change ❑ Dependent Enrollment<br />
❑ Medicare Enrollment ❑ Retirement ❑ Work Hours Change ❑ Update Salary ❑ Name Change ❑ Address Change<br />
MEMBER INFORMATION<br />
Last Name_____________________________________________ First Name__________________________________________ MI____ Social Sec. #:__________-_________-___________<br />
Date <strong>of</strong> Birth_____/_____/_____ Gender: ❑ Male ❑ Female Home Address:_________________________________________________________________________ Apt. No.__________<br />
City________________________________________________________ State______ Zip__________ Home Phone__________________________ Work Phone_________________________<br />
Status: ❑ Active ❑ Retired Occupation__________________________________________ Covered by Collective Bargaining Agreement: ❑ Yes ❑ No Date <strong>of</strong> Hire_____/_____/_____<br />
❑ Part Time Employee ❑ Full Time Employee Regular Weekly Work Hours______ Marital Status: ❑ Single ❑ Married Marriage Date: ____/____/_____ ❑ Divorced ❑ Widowed<br />
DEPENDENT INFORMATION<br />
List below your name and <strong>the</strong> name(s) <strong>of</strong> eligible dependent(s) to be covered, your spouse and dependent children. A child will be considered a dependent if: 1) Age 19 to <strong>the</strong> end <strong>of</strong> calendar year) or<br />
2) Age 25 (if full-time college student-to <strong>the</strong> end <strong>of</strong> a calendar month in which child reaches age 25 as long as he/she is unmarried and enrolled in an accredited school on a full time basis.) Obtain <strong>the</strong><br />
Statement <strong>of</strong> Dependent Eligibility Beyond Limiting Age in Plan Due to Mental Retardation or Mental or Physical Handicap Form to apply for extension <strong>of</strong> coverage for a disabled child before <strong>the</strong><br />
child reaches <strong>the</strong> limiting age.<br />
First Name <strong>of</strong> Dependent<br />
(Include Last Name if Different from Yours)<br />
Sex<br />
M/F<br />
Date <strong>of</strong> Birth<br />
Mo./Day/Yr.<br />
Relationship to Employee Social Security Number Full Time<br />
Student?<br />
Yes/No<br />
Disabled?<br />
Yes/No<br />
EMPLOYER INFORMATION<br />
Employer (Institution)_____________________________________________________________________ Institution No.___________ Division Code__________<br />
Employer Street Address ______________________________________________________________________________ City____________________________________________________<br />
State________ Zip Code___________ Phone__________________________<br />
IMPORTANT<br />
FORM CONTINUES ON THE REVERSE SIDE<br />
Page 1 <strong>of</strong> 2<br />
Contact us: ebc@archny.org Web Page: www.archny.org/<strong>benefits</strong> Revised 05/01/08
Select from <strong>the</strong> following coverage options for <strong>the</strong> Plan Year:<br />
MEDICAL PLAN ELECTION<br />
• Type <strong>of</strong> Medical Coverage: ❑ Single ❑ Two Person ❑ Family ❑ Medicare Supplement ❑ Waive Medical Coverage<br />
Payroll contribution Election:<br />
I elect that <strong>the</strong> employee contributions for <strong>the</strong> coverage I have selected be subtracted from my paycheck on <strong>the</strong> following basis:<br />
❑ Pre-Tax ❑ Post-Tax ❑ N/A<br />
OTHER MEDICAL COVERAGE<br />
Are you a dependent/or spouse covered by ano<strong>the</strong>r health plan? ❑ Yes ❑ No.<br />
If “Yes”, please complete this section: Name and address <strong>of</strong> o<strong>the</strong>r insurance carrier: ______________________________________________________ Policy Number_______________________<br />
O<strong>the</strong>r Insurance Carrier Phone #:________________________ Primary Named Insured_____________________________________________ Person(s) Covered: ❑ Self ❑ Spouse ❑ Child(ren)<br />
Policyholder___________________________________________________ Address____________________________________________________________________________________________<br />
Employer___________________________________________________ Address_____________________________________________________________ Phone_____________________________<br />
Association (if applicable)______________________________________ Address____________________________________________________________ Phone_____________________________<br />
Effective Date_______/________/_________ Plan Type: ❑ Hospital ❑ Medical ❑ Major Medical ❑ Extended Medical<br />
MEDICARE INFORMATION<br />
If this election form includes a person with Medicare coverage, complete <strong>the</strong> following (Attach a copy <strong>of</strong> your red, white and blue Medicare card):<br />
Name <strong>of</strong> Medicare Eligible Person Hospital (Part A)<br />
Effective Date<br />
Medical (Part B) Effective<br />
Date<br />
Medicare Identification #<br />
HIB Suffix<br />
VISION CARE - CLERGY AND RELIGIOUS ONLY<br />
Clergy: ❑ Yes ❑ No Coverage Religious: ❑ Yes ❑ No Coverage (Coverage is mandatory for Religious on stipend)<br />
My signature below affirms eligibility for coverage, and authorization to deduct any contribution from my paycheck. All information provided is complete and true to <strong>the</strong> best <strong>of</strong> my knowledge.<br />
Any person who knowingly and with intent to defraud an application <strong>of</strong> health <strong>benefits</strong> or statement <strong>of</strong> claim containing any materially false information or conceals for <strong>the</strong> purpose <strong>of</strong> misleading<br />
information concerning any fact material <strong>the</strong>reto commits a fraudulent act, which subjects such person to civil penalties.<br />
If retired or o<strong>the</strong>rwise not actively at work, I agree to pay <strong>the</strong> applicable premium required or portion <strong>the</strong>re<strong>of</strong> within 30 days <strong>of</strong> <strong>the</strong> premium due date.<br />
Employee/Participant Signature (Required):_________________________________________________________________________________ Date:_________________________________<br />
Employer’s Signature (Required):_________________________________________________________________________________________ Date:_________________________________<br />
Employer Print Name (Required):_________________________________________________________________________________________<br />
Administrators: Mail completed form to – Employee Benefit Connections, 1011 First Avenue, Suite 1679, New York, New York 10022 or Fax form to 212.644.0690<br />
Contact us: ebc@archny.org Web Page: www.archny.org/<strong>benefits</strong> Revised 05/01/08<br />
Page 2 <strong>of</strong> 2
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefit Election Form<br />
Non-Bargaining Full-Time Employees<br />
Effective January 1, _____ to December 31, _____<br />
Name_______________________________________________<br />
Soc. Security Number_________________________<br />
Address_______________________________________ City________________________ State______ Zip________<br />
Institution___________________________________________ Inst. No._______________ Division No.___________<br />
Effective Date____________________ No. <strong>of</strong> Work Hrs./Week______ Payroll File# (If applicable)_____________<br />
Select <strong>the</strong> appropriate member annual contribution option for <strong>the</strong> current benefit plan year:<br />
United Healthcare Plan (PPO)<br />
Single Coverage Two Person Coverage Family Coverage<br />
[ ] $______ [ ] $______ [ ] $_______<br />
Dependent Coverage<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Waiver <strong>of</strong> Medical Coverage<br />
Complete this section if you are waiving employee and/or dependent coverage.<br />
[ ] I elect to waive <strong>the</strong> employee health coverage under this plan.<br />
[ ] I elect to waive <strong>the</strong> dependent health coverage under this plan. (Check this box only if you have eligible dependents that you will not be<br />
covering under this plan).<br />
If you waive medical coverage, you (and/or your eligible dependents) will not be eligible to participate in <strong>the</strong> plan until <strong>the</strong> next benefit plan year,<br />
unless you experience a life status change. Life status changes include marriage, birth or adoption <strong>of</strong> a child, death, or a change in your or your<br />
spouse’s employment status, which affects you or your dependents’ eligibility for medical coverage.<br />
I elect that <strong>the</strong> employee contributions for <strong>the</strong> coverage I have selected be deducted from my paycheck on <strong>the</strong> following basis:<br />
[ ] Pre-tax [ ] After-tax<br />
If you select to have your contributions deducted from your pay on a pre-tax basis, your earnings for <strong>the</strong> purposes <strong>of</strong> computing Social Security<br />
<strong>benefits</strong> could be reduced. If you have concerns regarding this issue, contact your accountant or tax advisor before selecting this option.<br />
I understand that this election is effective during <strong>the</strong> current benefit plan year, unless <strong>the</strong>re is a life status change. Life status change include<br />
marriage, divorce, birth, or adoption <strong>of</strong> a child, death, or change in employment status for my spouse or me, which would affect my dependents’ or<br />
my eligibility for coverage.<br />
I certify that all <strong>of</strong> <strong>the</strong> information contained on this coverage election form and my application is true. I understand <strong>the</strong> elections that I have<br />
indicated above and agree to have any employee contribution(s) deducted from my paycheck.<br />
Signed______________________________________________________________________<br />
Date______________________________________<br />
Member: Return this form to your local administrator<br />
Local Administrator: PLEASE RETAIN THIS FORM IN YOUR FILES FOR PAYROLL DEDUCTIONS<br />
Revised 01/2008
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefit Election Form<br />
Non-Bargaining Part Time Employees<br />
Effective January 1, _____ to December 31, _____<br />
Name_______________________________________________<br />
Soc. Security Number_________________________<br />
Address_______________________________________ City________________________ State______ Zip________<br />
Institution___________________________________________ Inst. No._______________ Division No.___________<br />
Effective Date____________________ No. <strong>of</strong> Work Hrs./Week______ Payroll File# (If applicable)_____________<br />
Select <strong>the</strong> appropriate member annual contribution option for <strong>the</strong> current benefit plan year:<br />
United Healthcare Plan (PPO)<br />
Single Coverage Two Person Coverage Family Coverage<br />
[ ] $__________ [ ] $___________ [ ] $__________<br />
Dependent Coverage<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Waiver <strong>of</strong> Medical Coverage<br />
Complete this section if you are waiving employee and/or dependent coverage.<br />
[ ] I elect to waive <strong>the</strong> employee health coverage under this plan.<br />
[ ] I elect to waive <strong>the</strong> dependent health coverage under this plan. (Check this box only if you have eligible dependents that you will not be<br />
covering under this plan).<br />
If you waive medical coverage, you (and/or your eligible dependents) will not be eligible to participate in <strong>the</strong> plan until <strong>the</strong> next benefit plan year,<br />
unless you experience a life status change. Life status changes include marriage, birth or adoption <strong>of</strong> a child, death, or a change in your or your<br />
spouse’s employment status, which affects you or your dependents’ eligibility for medical coverage.<br />
I elect that <strong>the</strong> employee contributions for <strong>the</strong> coverage I have selected be deducted from my paycheck on <strong>the</strong> following basis:<br />
[ ] Pre-tax [ ] After-tax<br />
If you select to have your contributions deducted from your pay on a pre-tax basis, your earnings for <strong>the</strong> purposes <strong>of</strong> computing Social Security<br />
<strong>benefits</strong> could be reduced. If you have concerns regarding this issue, contact your accountant or tax advisor before selecting this option.<br />
I understand that this election is effective during <strong>the</strong> current benefit plan year, unless <strong>the</strong>re is a life status change. Life status change include<br />
marriage, divorce, birth, or adoption <strong>of</strong> a child, death, or change in employment status for my spouse or me, which would affect my dependents’ or<br />
my eligibility for coverage.<br />
I certify that all <strong>of</strong> <strong>the</strong> information contained on this coverage election form and my application is true. I understand <strong>the</strong> elections that I have<br />
indicated above and agree to have any employee contribution(s) deducted from my paycheck.<br />
Signed______________________________________________________________________ Date______________________________________<br />
Member: Return this form to your local administrator<br />
Local Administrator: PLEASE RETAIN THIS FORM IN YOUR FILES FOR PAYROLL DEDUCTIONS<br />
Revised 01/2008
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefit Election Form<br />
Bargaining Lay Faculty Members<br />
Effective January 1, _____ to December 31, _____<br />
Name_______________________________________________<br />
Soc. Security Number_________________________<br />
Address_______________________________________ City________________________ State______ Zip________<br />
Institution___________________________________________ Inst. No._______________ Division No.___________<br />
Effective Date____________________ No. <strong>of</strong> Work Hrs./Week______ Payroll File# (If applicable)_____________<br />
Select <strong>the</strong> appropriate member annual contribution option for <strong>the</strong> current benefit plan year:<br />
United Healthcare Plan (PPO)<br />
Single Coverage Two Person Coverage Family Coverage<br />
[ ] $_______ [ ] $_______ [ ] $________<br />
Dependent Coverage<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Name___________________________________________ Relationship______________ Date <strong>of</strong> Birth____________<br />
Waiver <strong>of</strong> Medical Coverage<br />
Complete this section if you are waiving employee and/or dependent coverage.<br />
[ ] I elect to waive <strong>the</strong> employee health coverage under this plan.<br />
[ ] I elect to waive <strong>the</strong> dependent health coverage under this plan. (Check this box only if you have eligible dependents that you will not be<br />
covering under this plan).<br />
If you waive medical coverage, you (and/or your eligible dependents) will not be eligible to participate in <strong>the</strong> plan until <strong>the</strong> next benefit plan year,<br />
unless you experience a life status change. Life status changes include marriage, birth or adoption <strong>of</strong> a child, death, or a change in your or your<br />
spouse’s employment status, which affects you or your dependents’ eligibility for medical coverage.<br />
I elect that <strong>the</strong> employee contributions for <strong>the</strong> coverage I have selected be deducted from my paycheck on <strong>the</strong> following basis:<br />
[ ] Pre-tax [ ] After-tax<br />
If you select to have your contributions deducted from your pay on a pre-tax basis, your earnings for <strong>the</strong> purposes <strong>of</strong> computing Social Security<br />
<strong>benefits</strong> could be reduced. If you have concerns regarding this issue, contact your accountant or tax advisor before selecting this option.<br />
I understand that this election is effective during <strong>the</strong> current benefit plan year, unless <strong>the</strong>re is a life status change. Life status change include<br />
marriage, divorce, birth, or adoption <strong>of</strong> a child, death, or change in employment status for my spouse or me, which would affect my dependents’ or<br />
my eligibility for coverage.<br />
I certify that all <strong>of</strong> <strong>the</strong> information contained on this coverage election form and my application is true. I understand <strong>the</strong> elections that I have<br />
indicated above and agree to have any employee contribution(s) deducted from my paycheck.<br />
Signed______________________________________________________________________ Date______________________________________<br />
Member: Return this form to your local administrator<br />
Local Administrator: PLEASE RETAIN THIS FORM IN YOUR FILES FOR PAYROLL DEDUCTIONS<br />
Revised 01/2008
CERTIFICATION FOR DISABLED DEPENDENT CHILDREN OVER THE AGE<br />
OF NINETEEN (19)<br />
Members who are covered under <strong>the</strong> Group Health Benefit and have a covered Dependent<br />
Child(ren) over <strong>the</strong> age <strong>of</strong> 19, who is disabled, must submit a completed Statement <strong>of</strong><br />
Dependent Eligibility Beyond Limiting Age In Plan Due To Mental Retardation or<br />
Mental or Physical Handicap form (refer to sample form on <strong>the</strong> following page).<br />
The Local Administrator should complete and sign <strong>the</strong> Employer’s Statement, before<br />
giving <strong>the</strong> form to <strong>the</strong> employee. Instruct <strong>the</strong> employee to complete <strong>the</strong> Employee Section<br />
<strong>of</strong> <strong>the</strong> form and have <strong>the</strong> dependent child’s physician complete <strong>the</strong> Physician’s Statement.<br />
Upon completion <strong>of</strong> <strong>the</strong> form <strong>the</strong> employee can make a copy for <strong>the</strong>ir confidential file and<br />
mail <strong>the</strong> original form to United Healthcare (address is listed on <strong>the</strong> form).<br />
United Healthcare will review <strong>the</strong> Certification and notify <strong>the</strong> member and <strong>the</strong> Employee<br />
Benefit Connections Department at <strong>the</strong> Archdiocese, if <strong>the</strong> dependent child is approved to<br />
remain as an eligible dependent on <strong>the</strong> group health benefit, and when re-certification is<br />
required.<br />
For additional information, call United Healthcare at 800.736.1264.<br />
- 13 -
STATEMENT OF DEPENDENT ELIGIBILITY BEYOND LIMITING AGE IN PLAN DUE TO<br />
MENTAL RETARDATION OR MENTAL OR PHYSICAL HANDICAP<br />
EMPLOYEE’S STATEMENT<br />
ANSWER ALL QUESTIONS BELOW.<br />
OMITTED INFORMATION WILL CAUSE DELAYS.<br />
Name (Print) First Middle Last Social Security Number<br />
Date <strong>of</strong> birth Male<br />
/ /<br />
Female<br />
Present Street City State Zip Code Marital Single Widowed Phone (with area code)<br />
Address:<br />
Status: Married Divorced ( )<br />
Dependent Information<br />
Name (Print) First Middle Last Social Security Number<br />
/ /<br />
Present Street City State Zip Code Marital Single<br />
Address:<br />
Status: Married<br />
Date <strong>of</strong> birth Male<br />
Female<br />
Relationship to Employee<br />
Name and address <strong>of</strong><br />
dependent’s current employer<br />
If not now employed, give<br />
date last employed<br />
Estimated income <strong>of</strong><br />
dependent from all sources<br />
$_____________ monthly<br />
Percentage <strong>of</strong> support <strong>of</strong><br />
dependent supplied by<br />
employee<br />
_______________%<br />
Is dependent permanently<br />
residing in employer’s<br />
household?<br />
Yes No If No, Explain<br />
Is dependent listed as a dependent in your last Federal Personal Income Tax Return? Yes No If No, Explain<br />
Explanations<br />
I KNOW IT IS A CRIME TO FILL OUT THIS FORM WITH FACTS I KNOW ARE FALSE OR TO<br />
LEAVE OUT FACTS I KNOW ARE IMPORTANT.<br />
Signed (Employee)<br />
Date<br />
PHYSICIAN’S/SURGEON’S STATEMENT<br />
ANY FEE FOR THE COMPLETION OF THIS STATEMENT TO BE PAID BY THE EMPLOYEE.<br />
ANSWER ALL QUESTIONS BELOW. OMITTED INFORMATION WILL CAUSE DELAYS.<br />
Patient’s Name First Middle Last Patient’s Date <strong>of</strong> Birth<br />
Is this dependent presently incapable <strong>of</strong> self-sustaining employment by reason <strong>of</strong>:<br />
Mental Retardation? Physical Handicap? Mental Handicap? O<strong>the</strong>r (explain)<br />
Yes No Yes No Yes No Yes No<br />
Date dependent became<br />
incapable <strong>of</strong> self-sustaining<br />
employment<br />
Diagnosis <strong>of</strong> condition causing incapacity. If mental retardation is present, give degree <strong>of</strong> retardation. Give as much detail as<br />
possible. Please give date and report <strong>of</strong> surgery, X-rays, electrocardiograms, or o<strong>the</strong>r special tests. Use a separate sheet <strong>of</strong><br />
paper if necessary.<br />
Does <strong>the</strong> patient have a job? Yes No<br />
Do you know what <strong>the</strong> patient’s job is? Yes No Do you know what <strong>the</strong> duties <strong>the</strong> patient’s job requires? Yes No<br />
Has this patient been able to do full or part-time work <strong>of</strong> any Will <strong>the</strong> patient be capable <strong>of</strong> self support?<br />
kind? No Yes, From _____________ Date<br />
No Yes, From _____________ Date<br />
The patient is presently (check one) Ambulatory Bed confined House confined Hospital confined<br />
Physician’s/Surgeon’s Name (Print) Address Phone (with area code)<br />
( )<br />
I KNOW IT IS A CRIME TO FILL OUT THIS FORM WITH FACTS I KNOW ARE FALSE OR TO Date<br />
LEAVE OUT FACTS I KNOW ARE IMPORTANT.<br />
Signed<br />
EMPLOYER’S STATEMENT<br />
ANSWER ALL QUESTIONS BELOW.<br />
OMITTED INFORMATION WILL CAUSE DELAYS.<br />
Employee’s Name First Middle Last Certificate No.<br />
Date dependent’s coverage was originally effective<br />
If previously canceled, give date.<br />
Employer Group Branch Sub Division<br />
Title<br />
Date<br />
Signed by<br />
FOR USE BY United Healthcare<br />
Dependent eligibility will continue to Month Day Year<br />
Dependent eligibility declined. Give reason.<br />
Signature<br />
Date
Section III<br />
Benefits Summaries
THE ARCHDIOCESE OF NEW YORK<br />
SUMMARY OF MEDICAL BENEFITS<br />
For Clergy, Religious, Seminarians & Non-Bargaining Lay<br />
Employees<br />
UNITED HEALTHCARE CHOICE PLUS PLAN<br />
-15-
Summary <strong>of</strong> Benefits<br />
UnitedHealthcare Choice Plus<br />
Archdiocese <strong>of</strong> New York<br />
Active Plan for Clergy, Religious, Seminarians, and Lay Employees<br />
Effective January 1, 2006, if you have any questions please call UnitedHealthcare Member<br />
Services at 1-800-736-1264 or register on myuhc.com to get detailed information on your<br />
coverage.<br />
Choice Plus plan gives you <strong>the</strong> freedom to see any Physician or o<strong>the</strong>r health care pr<strong>of</strong>essional<br />
from <strong>the</strong> Network, including specialists, without a referral. With this plan, you will receive <strong>the</strong><br />
highest level <strong>of</strong> <strong>benefits</strong> when you seek care from a network physician, facility or o<strong>the</strong>r health<br />
care pr<strong>of</strong>essional. In addition, you do not have to worry about any claim forms or bills.<br />
You also may choose to seek care outside <strong>the</strong> Network, without a referral. However, you should<br />
know that care received from a non-network physician, facility or o<strong>the</strong>r health care pr<strong>of</strong>essional<br />
means a higher deductible and coinsurance. We recommend that you ask <strong>the</strong> non-network<br />
physician or health care pr<strong>of</strong>essional about <strong>the</strong>ir billed charges before you receive care.<br />
Some <strong>of</strong> <strong>the</strong> Important Benefits <strong>of</strong> Your Plan:<br />
• You have access to a Network <strong>of</strong><br />
physicians, facilities and o<strong>the</strong>r health<br />
care pr<strong>of</strong>essionals, including specialists,<br />
without designating a Primary Physician<br />
or obtaining a referral.<br />
• Benefits are available for <strong>of</strong>fice visits<br />
and hospital care, as well as inpatient<br />
and outpatient surgery.<br />
• United Healthcare’s Nurseline connects<br />
you to registered nurses and a library <strong>of</strong><br />
recorded programs on important health<br />
topics 24 hours a day, 7 days a week,<br />
from anywhere in U.S.<br />
• We <strong>of</strong>fer <strong>the</strong> Language Line Services so<br />
that you can talk with us in 140 different<br />
languages. Just call customer service<br />
and ask for an interpreter.<br />
• Emergencies are covered anywhere in <strong>the</strong><br />
world.<br />
• Care Coordination SM services are available<br />
to help identify and prevent delays in care<br />
for those who might need specialized help.<br />
• The tools and information at myuhc.com<br />
are practical and personalized so you can<br />
get <strong>the</strong> most out <strong>of</strong> your <strong>benefits</strong>. Register<br />
at myuhc.com and connect to current<br />
information about your <strong>benefits</strong> and health<br />
care interests.<br />
• Cancer Resource Services provides<br />
information on comprehensive cancer<br />
treatment services. Benefit from using<br />
one <strong>of</strong> our Centers <strong>of</strong> Excellence by<br />
calling 1-866-936-6002.
Choice Plus Benefits Summary<br />
Types <strong>of</strong> Coverage Network Benefits / Copayment Amounts Non-Network Benefits / Copayment Amounts<br />
This Benefit Summary is intended only to highlight<br />
your Benefits and should not be relied upon to fully<br />
determine coverage. This benefit plan may not cover all<br />
<strong>of</strong> your health care expenses. More complete<br />
descriptions <strong>of</strong> Benefits and <strong>the</strong> terms under which<br />
<strong>the</strong>y are provided are contained in <strong>the</strong> Summary<br />
Plan Description that you will receive upon enrolling<br />
in <strong>the</strong> Plan.<br />
If this Benefit Summary conflicts in any way with <strong>the</strong><br />
Summary Plan Description issued to your employer, <strong>the</strong><br />
Summary Plan Description shall prevail.<br />
Terms that are capitalized in <strong>the</strong> Benefit Summary are<br />
defined in <strong>the</strong> Summary Plan Description.<br />
Network Benefits are payable for Covered Health<br />
Services provided by or under <strong>the</strong> direction <strong>of</strong> your<br />
Network physician.<br />
*Prior Notification is required for certain services.<br />
Annual Deductible: $150 per Covered Person per<br />
calendar year, not to exceed $300 for all Covered Persons<br />
in a family. Cross applies with out <strong>of</strong> network deductible.<br />
Out-<strong>of</strong>-Pocket Maximum: $1,200 per Covered Person<br />
per calendar year, not to exceed $2,400 per family. The<br />
Out-<strong>of</strong>-Pocket Maximum does not include <strong>the</strong> Annual<br />
Deductible. Cross applies with out <strong>of</strong> network out <strong>of</strong><br />
pocket maximum.<br />
Maximum Plan Benefit: No Maximum Plan Benefit.<br />
MEMBER PAYS<br />
1. Ambulance Services - Emergency only Ground Transportation: 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
Air Transportation: 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
2. Dental Services - Accident only (must begin<br />
within 6 months <strong>of</strong> injury)<br />
Annual Deductible: $300 per Covered Person per<br />
calendar year, not to exceed $600 for all Covered Persons<br />
in a family. Cross applies with in network deductible.<br />
Out-<strong>of</strong>-Pocket Maximum: $2,000 per Covered Person<br />
per calendar year, not to exceed $4,000 per family. The<br />
Out-<strong>of</strong>-Pocket Maximum does not include <strong>the</strong> Annual<br />
Deductible. Cross applies with in network out <strong>of</strong> pocket<br />
maximum.<br />
Maximum Plan Benefit: $1,000,000 per Covered<br />
Person.<br />
MEMBER PAYS<br />
Same as Network Benefit<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
3. Durable Medical Equipment (<strong>the</strong> purchase or 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
rental <strong>of</strong> prescribed equipment is covered, including<br />
needed replacement and repairs)<br />
4. Emergency Health Services $50 per visit (copay waived if admitted) True Emergencies - Same as Network Benefit<br />
Non-Emergency Visits - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
*Notification is required if results in an Inpatient Stay.<br />
5. Refractive Eye Examinations No Coverage No Coverage<br />
6. Home Health Care<br />
Network and Non-Network Benefits are limited to<br />
200 per calendar year combined in and out <strong>of</strong><br />
network.<br />
7. Hospice Care<br />
No annual maximum.<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
8. Hospital - Inpatient Stay 10% <strong>of</strong> Eligible Expenses after satisfying deductible *30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
9. Injections Received in a Physician’s Office $25 per visit 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10. Maternity Services Delivery - 10% <strong>of</strong> Eligible Expenses after satisfying<br />
deductible<br />
Prenatal visit – 100% after $25 copay (copay applies to<br />
first prenatal visit only)<br />
Outpatient Diagnostic Services - 10% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible<br />
Mo<strong>the</strong>r’s Hospital Charge - 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
Newborn Nursery Charge - 10% <strong>of</strong> Eligible Expenses<br />
waive deductible<br />
11. Outpatient Surgery, Diagnostic and Therapeutic<br />
Services<br />
Delivery - 30% <strong>of</strong> Eligible Expenses after satisfying<br />
deductible<br />
Prenatal visit – 30% <strong>of</strong> Eligible Expenses after satisfying<br />
deductible<br />
Outpatient Diagnostic Services - 30% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible<br />
Mo<strong>the</strong>r’s Hospital Charge - 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
Newborn Nursery Charge - 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
*Notification is required out <strong>of</strong> network if Inpatient Stay<br />
exceeds 48 hours following a normal vaginal delivery or<br />
96 hours following a cesarean section delivery.<br />
Outpatient Surgery 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Outpatient Diagnostic Services<br />
For lab and radiology/Xray: 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
For mammography testing: 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Outpatient Diagnostic/Therapeutic Services - CT 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Scans, Pet Scans, MRI and Nuclear Medicine<br />
Outpatient Therapeutic Treatments 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible
UnitedHealthcare<br />
Types <strong>of</strong> Coverage Network Benefits / Copayment Amounts Non-Network Benefits / Copayment Amounts<br />
12. Physician’s Office Services<br />
(In network copay does not apply to Preventive<br />
Care visits for children to age 19)<br />
$25 per visit. 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
13. Pr<strong>of</strong>essional Fees for Surgical and Medical<br />
Services<br />
14. Pros<strong>the</strong>tic Devices<br />
(The purchase or rental <strong>of</strong> prescribed equipment is<br />
covered, including needed replacement and repairs)<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
15. Reconstructive Procedures Hospital Inpatient Stay – 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Surgery - 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Diagnostic Therapeutic Services – 10% <strong>of</strong><br />
Eligible Expenses after satisfying deductible.<br />
Outpatient Therapeutic Treatments - 10% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible.<br />
Physician’s Office Services - $25 per visit<br />
16. Rehabilitation Services -Outpatient Therapy<br />
Network and Non-Network Benefits are limited as<br />
follows: 90 visits per year for all types <strong>of</strong> <strong>the</strong>rapy<br />
combined (physical <strong>the</strong>rapy, occupational <strong>the</strong>rapy,<br />
cardiac rehabilitation, and restorative speech<br />
<strong>the</strong>rapy). The visit maximum is combined in and<br />
out <strong>of</strong> network.<br />
17. Skilled Nursing Facility/Inpatient Rehabilitation<br />
Facility Services<br />
Network and Non-Network Benefits are limited to<br />
120 days per calendar year.<br />
*Hospital Inpatient Stay – 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible.<br />
Outpatient Surgery - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Diagnostic Therapeutic Services – 30% <strong>of</strong><br />
Eligible Expenses after satisfying deductible.<br />
Outpatient Therapeutic Treatments - 30% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible.<br />
Physician’s Office Services - 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible.<br />
$25 per visit 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible *30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
18. Transplantation Services *Services rendered via United Resource Network - 100% *30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
for all pr<strong>of</strong>essional and facility related expenses. Includes<br />
travel and lodging benefit up to maximum <strong>of</strong> $10,000.<br />
Services rendered at UHC Hospital which is not part <strong>of</strong><br />
<strong>the</strong> United Resource Network – 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
19. Urgent Care Center Services $50 per visit True Emergency – Same as network benefit<br />
Non-emergency - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible
UnitedHealthcare<br />
Additional Benefits<br />
Mental Health Services – Outpatient (Network and<br />
Non-Network Benefits are limited to 40 visits per<br />
calendar year combined in and out <strong>of</strong> network. Two<br />
group visits reduce 40 visit maximum by one day).<br />
Substance Abuse Services - Outpatient (Network<br />
and Non-Network Benefits are limited to 60 visits per<br />
calendar year combined in and out <strong>of</strong> network. Two<br />
group visits reduce 60 visit maximum by one day).<br />
Mental Health Services – Inpatient and<br />
Intermediate (Network and Non-Network Benefits are<br />
limited to 45 days per calendar year combined in and<br />
out <strong>of</strong> network. Two days <strong>of</strong> residential treatment<br />
coverage reduces visit maximum by one day). Inpatient<br />
Mental Health visits do not apply to out <strong>of</strong> pocket.<br />
Substance Abuse Services – Inpatient and<br />
Intermediate (Network and Non-Network Benefits are<br />
limited to 45 days per calendar year combined in and<br />
out <strong>of</strong> network. Two days <strong>of</strong> residential treatment<br />
coverage reduces visit maximum by one day). Inpatient<br />
Substance Abuse visits do not apply to out <strong>of</strong> pocket.<br />
Spinal Treatment (Limited to 60 visits per calendar<br />
year combined in and out <strong>of</strong> network)<br />
Prescription Drugs – Rx vendor is Caremark<br />
(1-800-565-7091<br />
Pharmacy fills: On <strong>the</strong> third fill <strong>of</strong> a maintenance drug<br />
at <strong>the</strong> retail pharmacy, <strong>the</strong> copay changes to $10/40/70<br />
per 30 day supply.<br />
$25 per individual visit; $25 per group visit.<br />
$25 per individual visit; $25 per group visit.<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
50% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
(does not apply to out <strong>of</strong> pocket)<br />
50% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
(does not apply to out <strong>of</strong> pocket)<br />
*30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
*30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
$25 per visit 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Retail Drug Program –<br />
$5 per 30-day supply for generic drugs<br />
$20 per 30-day supply for preferred drugs<br />
$35 per 30-day supply for non-preferred drugs<br />
Coverage In Network only<br />
Generic Incentive: When you fill a Rx for a brand name<br />
drug that has a generic equivalent you pay <strong>the</strong> brand<br />
name copay plus <strong>the</strong> difference in <strong>the</strong> cost between <strong>the</strong><br />
brand name and its generic equivalent.<br />
Mail Order Program –<br />
$10 per 90-day supply for generic drugs<br />
$40 per 90-day supply for preferred drugs<br />
$70 per 90-day supply for non-preferred drugs<br />
Coverage In Network only
Exclusions<br />
Except as may be specifically provided in Section 1 <strong>of</strong> <strong>the</strong> Summary Plan Description (SPD) or<br />
through a Rider to <strong>the</strong> Plan, <strong>the</strong> following are not covered:<br />
Covered Expenses will not include, and no payment will be made for <strong>the</strong> following expenses incurred,<br />
unless those expenses are considered Medically Necessary.<br />
• Expenses for charges that are not Medically Necessary, except as specified in any notification<br />
requirements shown in this plan.<br />
• To <strong>the</strong> extent that you or any one <strong>of</strong> your Dependents is in any way paid or entitled to payment<br />
for those expenses by or through a public program, o<strong>the</strong>r than Medicaid.<br />
• To <strong>the</strong> extent that payment is unlawful where <strong>the</strong> person resides when <strong>the</strong> expenses are incurred.<br />
• Charges made by a Hospital owned or operated by or which provides care or performs services<br />
for <strong>the</strong> United States Government: (a) unless <strong>the</strong>re is a legal obligation to pay such charges<br />
whe<strong>the</strong>r or not <strong>the</strong>re is insurance; or (b) if such charges are directly related to a military-service<br />
connected Injury or Sickness.<br />
• For or in connection with an Injury or Sickness which is due to war, declared or undeclared.<br />
• Charges which you are not obligated to pay or for which you are not billed or for which you<br />
would not have been billed except that <strong>the</strong>y were covered under this plan.<br />
• Assistance in <strong>the</strong> activities <strong>of</strong> daily living, including but not limited to eating, bathing, dressing,<br />
toileting or o<strong>the</strong>r non-Medically Necessary self-care activities, homemaker services and services<br />
primarily for rest domiciliary or convalescent care.<br />
• Cosmetic surgery and <strong>the</strong>rapies. Cosmetic surgery or <strong>the</strong>rapy is defined as surgery or <strong>the</strong>rapy<br />
performed to improve or alter appearance or self-esteem or to treat psychological<br />
symptomatoloty or psychosocial complaints related to one’s appearance and determined not to<br />
be Medically Necessary. However, reconstructive surgery is covered as provided under Covered<br />
Expenses and for <strong>the</strong> purposes <strong>of</strong> this exclusion <strong>the</strong> term cosmetic surgery or <strong>the</strong>rapy shall not<br />
include reconstructive surgery when such service is incidental to or follows surgery resulting<br />
from trauma, infection or o<strong>the</strong>r disease <strong>of</strong> <strong>the</strong> involved part.<br />
• Macromastia or gynecomastia surgeries; abdominoplasty/panniculectomy; rhinoplasty;<br />
blepharoplasty; orthognathic surgeries; redundant skin surgery; removal <strong>of</strong> skin tags;<br />
acupressure; craniosacral/cranial <strong>the</strong>rapy; dance <strong>the</strong>rapy; movement <strong>the</strong>rapy; applied<br />
kinesiology; rolfing; prolo<strong>the</strong>rapy; extracorporeal shock wave lithotripsy for musculoskeletal<br />
and orthopedic conditions.<br />
• For or in connection with treatment <strong>of</strong> <strong>the</strong> teeth or peridontium unless such expenses are<br />
incurred for: (a) charges made for services or supplies provided for or in connection with an<br />
accidental injury to sound natural teeth, provided a continuous course <strong>of</strong> dental treatment started<br />
within 6 months <strong>of</strong> <strong>the</strong> accident; (b) charges made by a Hospital for Bed and Board or Necessary<br />
Services and Supplies; (c) charges made by a Free-Standing Surgical Facility or <strong>the</strong> outpatient<br />
department <strong>of</strong> a Hospital in connection with surgery, or (d) charges made by a Physician for any<br />
<strong>of</strong> <strong>the</strong> following Surgical Procedures: excision <strong>of</strong> epulis; removal <strong>of</strong> residual root (when<br />
performed by a Dentist o<strong>the</strong>r than <strong>the</strong> one who extracted <strong>the</strong> tooth); intraoral drainage <strong>of</strong> acute<br />
alveolar abscess with cellulitis; alveolectomy; gingvectomy, for gingivitis or periodontitis.<br />
• For medical and surgical services intended for <strong>the</strong> treatment or control <strong>of</strong> obesity, unless<br />
Medically Necessary. However, treatment <strong>of</strong> clinically severe obesity, as defined by <strong>the</strong> body<br />
mass index (BMI) classifications <strong>of</strong> <strong>the</strong> National Heart, Lung and Blood Institute (NHLBI)<br />
<strong>guide</strong>lines to be covered only at approved centers if <strong>the</strong> services are demonstrated, through<br />
existing peer-reviewed, evidence based, scientific literature and scientifically based <strong>guide</strong>lines,<br />
to be safe and effective for treatment <strong>of</strong> this condition. Clinically severe obesity is defined by<br />
<strong>the</strong> NHLBI as a BMMI <strong>of</strong> 40 or greater without comorbidities, or 35-39 with comorbidities. The<br />
following are specifically excluded: (a) medical and surgical services to alter appearance or<br />
physical changes that are <strong>the</strong> result <strong>of</strong> any surgery performed for <strong>the</strong> management <strong>of</strong> obesity or<br />
clinically severe (morbid) obesity; and (b) weight loss programs or treatments, whe<strong>the</strong>r<br />
prescribed or recommended by a Physician or under medical supervision.<br />
• Unless o<strong>the</strong>rwise covered in this plan, for reports, evaluations, physical examinations, or<br />
hospitalizations not required for health reasons including, but not limited to, employment,<br />
insurance or government licenses, and court-ordered, forensic or custodial evaluations.<br />
• Court-ordered treatment or hospitalization, unless such treatment is prescribed by a Physician<br />
and listed as covered in this plan.<br />
• Transsexual surgery including medical or psychological counseling and hormonal <strong>the</strong>rapy in<br />
preparation for, or subsequent to, any such surgery.<br />
• Any medications, drugs, services or supplies for <strong>the</strong> treatment <strong>of</strong> female sexual dysfunction and<br />
male impotence, such as, but not limited to, anorgasmy, and premature ejaculation.<br />
• For Infertility Services, including infertility drugs; surgical or medical treatment programs for<br />
infertility (such as in vitro fertilization, gamete intrafallopian transfer [GIFT], zygote<br />
intrafallopian transfer [ZIFT], or any variations <strong>of</strong> this procedures); and artificial insemination<br />
(including donor fees and any costs associated with <strong>the</strong> collection, washing, preparation, or<br />
storage <strong>of</strong> sperm). Cryopreservation <strong>of</strong> donor sperm or eggs is also excluded form coverage.<br />
• For amniocentesis, ultrasound, or any o<strong>the</strong>r procedures requested solely for gender<br />
determination <strong>of</strong> a fetus, unless Medically Necessary to determine <strong>the</strong> existence <strong>of</strong> a genderlinked<br />
genetic disorder.<br />
• Medical and Hospital care and costs for <strong>the</strong> infant child <strong>of</strong> a Dependent, unless this infant child<br />
is o<strong>the</strong>rwise eligible under this plan.<br />
UnitedHealthcare<br />
• Non-medical counseling or ancillary services, including but not limited to Custodial Services,<br />
education, training, vocational rehabilitation, behavior training, bi<strong>of</strong>eedback, neur<strong>of</strong>eedback,<br />
hypnosis, sleep <strong>the</strong>rapy, employment counseling, back school, return to work services, work<br />
hardening programs, driving safety, and services, training, educational <strong>the</strong>rapy or o<strong>the</strong>r nonmedical<br />
ancillary services for learning disabilities, developmental delays, autism or mental<br />
retardation.<br />
• Therapy or treatment intended primarily to improve or maintain general physical condition or<br />
for <strong>the</strong> purpose <strong>of</strong> enhancing job, school, athletic or recreational performance, including but not<br />
limited to routine, long term or maintenance care which is provided after <strong>the</strong> resolution <strong>of</strong> <strong>the</strong><br />
acute medical problem and when significant <strong>the</strong>rapeutic improvement is not expected.<br />
• Consumable medical supplies o<strong>the</strong>r than ostomy supplies and urinary ca<strong>the</strong>ters. Excluded<br />
supplies include, but are not limited to bandages and o<strong>the</strong>r disposable medical supplies, skin<br />
preparations and test strips, except as specified in <strong>the</strong> “Home Health Services” or “Breast<br />
Reconstruction and Breast Pros<strong>the</strong>ses” sections <strong>of</strong> this plan.<br />
• Private Hospital rooms and/or private duty nursing unless determined by <strong>the</strong> utilization review<br />
Physician to be Medically Necessary.<br />
• Personal or comfort items such as personal care kits provided on admission to a Hospital,<br />
television, telephone, <strong>new</strong>born infant photographs, complimentary meals, birth announcements,<br />
and o<strong>the</strong>r articles which are not for <strong>the</strong> specific treatment or an Injury or Sickness.<br />
• Artificial aids including, but not limited to, corrective orthopedic shoes, arch supports, elastic<br />
stockings, garter belts, corsets, dentures and wigs.<br />
• Hearing aids, including but not limited to semi-implantable hearing devices, audient bone<br />
conductors and Bone Anchored Hearing Aids (BAHAs). A hearing aid is any device that<br />
amplifies sound.<br />
• Aids or devices that assist with nonverbal communications, including but not limited to<br />
communication boards, prerecorded speech devices, laptop computers, desktop computers,<br />
Personal Digital Assistants (PDAs), Braille typewriters, visual alert systems for <strong>the</strong> deaf and<br />
memory books.<br />
• Medical <strong>benefits</strong> for eyeglasses, contact lenses, or examinations for prescription or fitting<br />
<strong>the</strong>re<strong>of</strong>, except that Covered Expenses will include <strong>the</strong> purchase <strong>of</strong> <strong>the</strong> first pair <strong>of</strong> eyeglasses,<br />
lenses, frames, or contact lenses that follows keratoconus or cataract surgery.<br />
• Charges made for or in connection with routine refractions, eye exercises and for surgical<br />
treatment for <strong>the</strong> correction <strong>of</strong> a refractive error, including radial keratotomy, when eyeglasses<br />
or contact lenses may be worn.<br />
• All non injectable prescription drugs, nonprescription drugs, and investigational and<br />
experimental drugs, except as provided in this plan.<br />
• Routine foot care including <strong>the</strong> paring and removing <strong>of</strong> corns and calluses or trimming <strong>of</strong> nails.<br />
However, services associated with foot care for diabetes and peripheral vascular disease are<br />
covered when Medically Necessary.<br />
• Membership cost or fees associated with health clubs, weight loss programs and smoking<br />
cessations programs.<br />
• Genetic screening or pre-implantations genetic screening. General population-based genetic<br />
screening is a testing method performed in <strong>the</strong> absence <strong>of</strong> any symptoms or any significant,<br />
proven risk factors for genetically linked inheritable disease.<br />
• Dental implants for any condition.<br />
• Fees associated with <strong>the</strong> collection or donation <strong>of</strong> blood or blood products, except for<br />
autologous donation in anticipation <strong>of</strong> scheduled services where in <strong>the</strong> utilization review<br />
Physician’s opinion <strong>the</strong> likelihood <strong>of</strong> excess blood loss is such that transfusion is an expected<br />
adjunct to surgery.<br />
• Blood <strong>administration</strong> for <strong>the</strong> purpose <strong>of</strong> general improvement in physical condition.<br />
• Cost <strong>of</strong> biologicals that are immunizations or medications for <strong>the</strong> purpose <strong>of</strong> travel, or to protect<br />
against occupational hazards and risks.<br />
• Cosmetics, dietary supplements and health and beauty aids and nutritional formulae (except as<br />
described in Covered Expenses).<br />
• For or in connection with an Injury or Sickness arising out <strong>of</strong>, or in <strong>the</strong> course <strong>of</strong>, any<br />
employment for wage or pr<strong>of</strong>it.<br />
• Telephone, e-mail, and Internet consultations and telemedicine.<br />
• Massage <strong>the</strong>rapy.<br />
• For charges which would not have been made if <strong>the</strong> person had no health <strong>benefits</strong>.<br />
• To <strong>the</strong> extent that <strong>the</strong>y are more than Reasonable and Customary charges.<br />
• Expenses incurred outside <strong>the</strong> United States or Canada, unless you or your Dependent is a U.S.<br />
or Canadian resident and <strong>the</strong> charges are incurred while traveling on business or for pleasure.<br />
• To <strong>the</strong> extent <strong>of</strong> <strong>the</strong> exclusions imposed by any notification requirement shown in this plan.<br />
• Elective and non-elective abortions.<br />
• Health services received after <strong>the</strong> date your coverage under <strong>the</strong> Plan ends, including health<br />
services for medical conditions arising prior to <strong>the</strong> date your coverage under <strong>the</strong> Plan ends.<br />
This summary <strong>of</strong> Benefits is intended only to highlight your Benefits and should not be relied upon to fully determine coverage. This plan may not cover all your health care<br />
expenses. Please refer to <strong>the</strong> Summary Plan Description for a complete listing <strong>of</strong> services, limitations, exclusions and a description <strong>of</strong> all <strong>the</strong> terms and conditions <strong>of</strong> coverage. If this<br />
description conflicts in any way with <strong>the</strong> Summary Plan Description, <strong>the</strong> Summary Plan Description prevails. Terms that are capitalized in <strong>the</strong> Benefit Summary are defined in <strong>the</strong><br />
Summary Plan Description.<br />
12/15/05 WARNY003 100-3513
THE ARCHDIOCESE OF NEW YORK<br />
SUMMARY OF MEDICAL BENEFITS<br />
For Bargaining Lay Faculty Members<br />
UNITED HEALTHCARE CHOICE PLUS II PLAN<br />
-16 -
Summary <strong>of</strong> Benefits<br />
UnitedHealthcare Choice Plus<br />
Archdiocese <strong>of</strong> New York<br />
Active Plan for Bargaining Lay Faculty<br />
Effective January 1, 2006, if you have any questions please call UnitedHealthcare Member<br />
Services at 1-800-736-1264 or register on myuhc.com to get detailed information on your<br />
coverage.<br />
Choice Plus plan gives you <strong>the</strong> freedom to see any Physician or o<strong>the</strong>r health care pr<strong>of</strong>essional<br />
from <strong>the</strong> Network, including specialists, without a referral. With this plan, you will receive <strong>the</strong><br />
highest level <strong>of</strong> <strong>benefits</strong> when you seek care from a network physician, facility or o<strong>the</strong>r health<br />
care pr<strong>of</strong>essional. In addition, you do not have to worry about any claim forms or bills.<br />
You also may choose to seek care outside <strong>the</strong> Network, without a referral. However, you should<br />
know that care received from a non-network physician, facility or o<strong>the</strong>r health care pr<strong>of</strong>essional<br />
means a higher deductible and coinsurance. We recommend that you ask <strong>the</strong> non-network<br />
physician or health care pr<strong>of</strong>essional about <strong>the</strong>ir billed charges before you receive care.<br />
Some <strong>of</strong> <strong>the</strong> Important Benefits <strong>of</strong> Your Plan:<br />
• You have access to a Network <strong>of</strong><br />
physicians, facilities and o<strong>the</strong>r health<br />
care pr<strong>of</strong>essionals, including specialists,<br />
without designating a Primary Physician<br />
or obtaining a referral.<br />
• Benefits are available for <strong>of</strong>fice visits<br />
and hospital care, as well as inpatient<br />
and outpatient surgery.<br />
• United Healthcare’s Nurseline connects<br />
you to registered nurses and a library <strong>of</strong><br />
recorded programs on important health<br />
topics 24 hours a day, 7 days a week,<br />
from anywhere in U.S.<br />
• We <strong>of</strong>fer <strong>the</strong> Language Line Services so<br />
that you can talk with us in 140 different<br />
languages. Just call customer service<br />
and ask for an interpreter.<br />
• Emergencies are covered anywhere in<br />
<strong>the</strong> world.<br />
• Care Coordination SM services are<br />
available to help identify and prevent<br />
delays in care for those who might need<br />
specialized help.<br />
• The tools and information at myuhc.com<br />
are practical and personalized so you<br />
can get <strong>the</strong> most out <strong>of</strong> your <strong>benefits</strong>.<br />
Register at myuhc.com and connect to<br />
current information about your <strong>benefits</strong><br />
and health care interests.<br />
• Cancer Resource Services provides<br />
information on comprehensive cancer<br />
treatment services. Benefit from using<br />
one <strong>of</strong> our Centers <strong>of</strong> Excellence by<br />
calling 1-866-936-6002.
Choice Plus Benefits Summary<br />
Types <strong>of</strong> Coverage Network Benefits / Copayment Amounts Non-Network Benefits / Copayment Amounts<br />
Annual Deductible: $150 per Covered Person per<br />
calendar year, not to exceed $300 for all Covered Persons<br />
in a family. Cross applies with out <strong>of</strong> network deductible.<br />
Annual Deductible: $300 per Covered Person per<br />
calendar year, not to exceed $600 for all Covered Persons<br />
in a family. Cross applies with in network deductible.<br />
This Benefit Summary is intended only to highlight<br />
your Benefits and should not be relied upon to fully<br />
determine coverage. This benefit plan may not cover all<br />
<strong>of</strong> your health care expenses. More complete<br />
descriptions <strong>of</strong> Benefits and <strong>the</strong> terms under which<br />
<strong>the</strong>y are provided are contained in <strong>the</strong> Summary<br />
Plan Description that you will receive upon enrolling<br />
in <strong>the</strong> Plan.<br />
If this Benefit Summary conflicts in any way with <strong>the</strong><br />
Summary Plan Description issued to your employer, <strong>the</strong><br />
Summary Plan Description shall prevail.<br />
Terms that are capitalized in <strong>the</strong> Benefit Summary are<br />
defined in <strong>the</strong> Summary Plan Description.<br />
Network Benefits are payable for Covered Health<br />
Services provided by or under <strong>the</strong> direction <strong>of</strong> your<br />
Network physician.<br />
*Prior Notification is required for certain services.<br />
Out-<strong>of</strong>-Pocket Maximum: $1,000 per Covered Person<br />
per calendar year, not to exceed $1,000 per family. The<br />
Out-<strong>of</strong>-Pocket Maximum does not include <strong>the</strong> Annual<br />
Deductible. Cross applies with out <strong>of</strong> network out <strong>of</strong><br />
pocket maximum.<br />
Maximum Plan Benefit: No Maximum Plan Benefit.<br />
MEMBER PAYS<br />
1. Ambulance Services - Emergency only Ground Transportation: 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
Air Transportation: 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
Out-<strong>of</strong>-Pocket Maximum: $1,000 per Covered Person<br />
per calendar year, not to exceed $1,000 per family. The<br />
Out-<strong>of</strong>-Pocket Maximum does not include <strong>the</strong> Annual<br />
Deductible. Cross applies with in network out <strong>of</strong> pocket<br />
maximum.<br />
Maximum Plan Benefit: $1,000,000 per Covered Person.<br />
MEMBER PAYS<br />
Same as Network Benefit<br />
2. Dental Services - Accident only (must begin<br />
within 6 months <strong>of</strong> injury)<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
3. Durable Medical Equipment<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
(The purchase or rental <strong>of</strong> prescribed equipment is<br />
covered, including needed replacement and repairs)<br />
4. Emergency Health Services $50 per visit (copay waived if admitted) True Emergencies - Same as Network Benefit<br />
Non-Emergency Visits - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
*Notification is required if results in an Inpatient Stay.<br />
5. Refractive Eye Examinations No Coverage No Coverage<br />
6. Home Health Care<br />
Network and Non-Network Benefits are limited to<br />
200 per calendar year combined in and out <strong>of</strong><br />
network.<br />
7. Hospice Care<br />
No annual maximum.<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
8. Hospital - Inpatient Stay 10% <strong>of</strong> Eligible Expenses after satisfying deductible *30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
9. Injections Received in a Physician’s Office $25 per visit 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10. Maternity Services Delivery - 10% <strong>of</strong> Eligible Expenses after satisfying<br />
deductible<br />
Prenatal visit – 100% after $25 copay (copay applies to<br />
first prenatal visit only)<br />
Outpatient Diagnostic Services - 10% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible<br />
Mo<strong>the</strong>r’s Hospital Charge - 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
Newborn Nursery Charge - 10% <strong>of</strong> Eligible Expenses<br />
waive deductible<br />
Delivery - 30% <strong>of</strong> Eligible Expenses after satisfying<br />
deductible<br />
Prenatal visit – 30% <strong>of</strong> Eligible Expenses after satisfying<br />
deductible<br />
Outpatient Diagnostic Services - 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
Mo<strong>the</strong>r’s Hospital Charge - 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
Newborn Nursery Charge - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible<br />
*Notification is required if Inpatient Stay exceeds 48 hours<br />
following a normal vaginal delivery or 96 hours following<br />
a cesarean section delivery.
UnitedHealthcare<br />
Types <strong>of</strong> Coverage Network Benefits / Copayment Amounts Non-Network Benefits / Copayment Amounts<br />
11. Outpatient Surgery, Diagnostic and Therapeutic<br />
Services<br />
Outpatient Surgery 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Outpatient Diagnostic Services<br />
For lab and radiology/Xray: 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
For mammography testing: 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Outpatient Diagnostic/Therapeutic Services - CT 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Scans, Pet Scans, MRI and Nuclear Medicine<br />
Outpatient Therapeutic Treatments 10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
12. Physician’s Office Services (In network copay<br />
does not apply to Preventive Care visits for children<br />
to age 19)<br />
13. Pr<strong>of</strong>essional Fees for Surgical and Medical<br />
Services<br />
14. Pros<strong>the</strong>tic Devices (<strong>the</strong> purchase or rental <strong>of</strong><br />
prescribed equipment is covered, including needed<br />
replacement and repairs)<br />
$25 per visit. 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
15. Reconstructive Procedures Hospital Inpatient Stay – 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Surgery - 10% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Diagnostic Therapeutic Services – 10% <strong>of</strong><br />
Eligible Expenses after satisfying deductible.<br />
Outpatient Therapeutic Treatments - 10% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible.<br />
Physician’s Office Services - $25 per visit<br />
*Hospital Inpatient Stay – 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Surgery - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible.<br />
Outpatient Diagnostic Therapeutic Services – 30% <strong>of</strong><br />
Eligible Expenses after satisfying deductible.<br />
Outpatient Therapeutic Treatments - 30% <strong>of</strong> Eligible<br />
Expenses after satisfying deductible.<br />
Physician’s Office Services - 30% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible.<br />
16. Rehabilitation Services -Outpatient Therapy<br />
Network and Non-Network Benefits are limited as<br />
follows: 90 visits per year for all types <strong>of</strong> <strong>the</strong>rapy<br />
combined (physical <strong>the</strong>rapy, occupational <strong>the</strong>rapy,<br />
cardiac rehabilitation, and restorative speech<br />
<strong>the</strong>rapy). The visit maximum is combined in and<br />
out <strong>of</strong> network.<br />
17. Skilled Nursing Facility/Inpatient Rehabilitation<br />
Facility Services<br />
Network and Non-Network Benefits are limited to<br />
120 days per calendar year.<br />
$25 per visit 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible *30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
18. Transplantation Services *Services rendered via United Resource Network - 100%<br />
for all pr<strong>of</strong>essional and facility related expenses. Includes<br />
travel and lodging benefit up to maximum <strong>of</strong> $10,000.<br />
*30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Services rendered at UHC Hospital which is not part <strong>of</strong><br />
<strong>the</strong> United Resource Network – 10% <strong>of</strong> Eligible Expenses<br />
after satisfying deductible<br />
19. Urgent Care Center Services $50 per visit True Emergency – Same as network benefit<br />
Non-emergency - 30% <strong>of</strong> Eligible Expenses after<br />
satisfying deductible
UnitedHealthcare<br />
Additional Benefits<br />
Mental Health Services – Outpatient (Network and<br />
Non-Network Benefits are limited to 40 visits per<br />
calendar year combined in and out <strong>of</strong> network. Two<br />
group visits reduce 40 visit maximum by one day).<br />
Substance Abuse Services - Outpatient (Network<br />
and Non-Network Benefits are limited to 60 visits per<br />
calendar year combined in and out <strong>of</strong> network. Two<br />
group visits reduce 60 visit maximum by one day).<br />
Mental Health Services – Inpatient and<br />
Intermediate (Network and Non-Network Benefits are<br />
limited to 45 days per calendar year combined in and<br />
out <strong>of</strong> network. Two days <strong>of</strong> residential treatment<br />
coverage reduces visit maximum by one day). Inpatient<br />
Mental Health visits do not apply to out <strong>of</strong> pocket<br />
maximum.<br />
Substance Abuse Services – Inpatient and<br />
Intermediate (Network and Non-Network Benefits are<br />
limited to 45 days per calendar year combined in and<br />
out <strong>of</strong> network. Two days <strong>of</strong> residential treatment<br />
coverage reduces visit maximum by one day). Inpatient<br />
Substance Abuse visits do not apply to out <strong>of</strong> pocket<br />
maximum.<br />
$25 per individual visit; $25 per group visit.<br />
$25 per individual visit; $25 per group visit.<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
50% <strong>of</strong> Eligible Expenses after satisfying deductible (does<br />
not apply to out <strong>of</strong> pocket maximum)<br />
50% <strong>of</strong> Eligible Expenses after satisfying deductible (does<br />
not apply to out <strong>of</strong> pocket maximum)<br />
*30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
*30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Spinal Treatment (Limited to 60 visits per calendar<br />
year combined in and out <strong>of</strong> network)<br />
$25 per visit 30% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
Prescription Drugs – Rx vendor is Caremark<br />
(1-800-565-7091<br />
Pharmacy fills: On <strong>the</strong> third fill <strong>of</strong> a maintenance drug<br />
at <strong>the</strong> retail pharmacy, <strong>the</strong> copay changes to $10/40/70<br />
per 30 day supply.<br />
Generic Incentive: When you fill a Rx for a brand name<br />
drug that has a generic equivalent you pay <strong>the</strong> brand<br />
name copay plus <strong>the</strong> difference in <strong>the</strong> cost between <strong>the</strong><br />
brand name and its generic equivalent.<br />
Retail Drug Program –<br />
$5 per 30-day supply for generic drugs<br />
$20 per 30-day supply for preferred drugs<br />
$35 per 30-day supply for non-preferred drugs<br />
Mail Order Program –<br />
$10 per 90-day supply for generic drugs<br />
$40 per 90-day supply for preferred drugs<br />
$70 per 90-day supply for non-preferred drugs<br />
Coverage In Network only<br />
Coverage In Network only
Exclusions<br />
UnitedHealthcare<br />
Except as may be specifically provided in Section 1 <strong>of</strong> <strong>the</strong> Summary Plan Description (SPD) or<br />
through a Rider to <strong>the</strong> Plan, <strong>the</strong> following are not covered:<br />
Covered Expenses will not include, and no payment will be made for <strong>the</strong> following expenses incurred,<br />
unless those expenses are considered Medically Necessary.<br />
• Expenses for charges that are not Medically Necessary, except as specified in any notification<br />
requirements shown in this plan.<br />
• To <strong>the</strong> extent that you or any one <strong>of</strong> your Dependents is in any way paid or entitled to payment<br />
for those expenses by or through a public program, o<strong>the</strong>r than Medicaid.<br />
• To <strong>the</strong> extent that payment is unlawful where <strong>the</strong> person resides when <strong>the</strong> expenses are incurred.<br />
• Charges made by a Hospital owned or operated by or which provides care or performs services<br />
for <strong>the</strong> United States Government: (a) unless <strong>the</strong>re is a legal obligation to pay such charges<br />
whe<strong>the</strong>r or not <strong>the</strong>re is insurance; or (b) if such charges are directly related to a military-service<br />
connected Injury or Sickness.<br />
• For or in connection with an Injury or Sickness which is due to war, declared or undeclared.<br />
• Charges which you are not obligated to pay or for which you are not billed or for which you<br />
would not have been billed except that <strong>the</strong>y were covered under this plan.<br />
• Assistance in <strong>the</strong> activities <strong>of</strong> daily living, including but not limited to eating, bathing, dressing,<br />
toileting or o<strong>the</strong>r non-Medically Necessary self-care activities, homemaker services and services<br />
primarily for rest domiciliary or convalescent care.<br />
• Cosmetic surgery and <strong>the</strong>rapies. Cosmetic surgery or <strong>the</strong>rapy is defined as surgery or <strong>the</strong>rapy<br />
performed to improve or alter appearance or self-esteem or to treat psychological<br />
symptomatoloty or psychosocial complaints related to one’s appearance and determined not to<br />
be Medically Necessary. However, reconstructive surgery is covered as provided under Covered<br />
Expenses and for <strong>the</strong> purposes <strong>of</strong> this exclusion <strong>the</strong> term cosmetic surgery or <strong>the</strong>rapy shall not<br />
include reconstructive surgery when such service is incidental to or follows surgery resulting<br />
from trauma, infection or o<strong>the</strong>r disease <strong>of</strong> <strong>the</strong> involved part.<br />
• Macromastia or gynecomastia surgeries; abdominoplasty/panniculectomy; rhinoplasty;<br />
blepharoplasty; orthognathic surgeries; redundant skin surgery; removal <strong>of</strong> skin tags;<br />
acupressure; craniosacral/cranial <strong>the</strong>rapy; dance <strong>the</strong>rapy; movement <strong>the</strong>rapy; applied<br />
kinesiology; rolfing; prolo<strong>the</strong>rapy; and extracorporeal shock wave lithotripsy for<br />
musculoskeletal and orthopedic conditions.<br />
• For or in connection with treatment <strong>of</strong> <strong>the</strong> teeth or peridontium unless such expenses are<br />
incurred for: (a) charges made for services or supplies provided for or in connection with an<br />
accidental injury to sound natural teeth, provided a continuous course <strong>of</strong> dental treatment started<br />
within 6 months <strong>of</strong> <strong>the</strong> accident; (b) charges made by a Hospital for Bed and Board or Necessary<br />
Services and Supplies; (c) charges made by a Free-Standing Surgical Facility or <strong>the</strong> outpatient<br />
department <strong>of</strong> a Hospital in connection with surgery, or (d) charges made by a Physician for any<br />
<strong>of</strong> <strong>the</strong> following Surgical Procedures: excision <strong>of</strong> epulis; removal <strong>of</strong> residual root (when<br />
performed by a Dentist o<strong>the</strong>r than <strong>the</strong> one who extracted <strong>the</strong> tooth); intraoral drainage <strong>of</strong> acute<br />
alveolar abscess with cellulitis; alveolectomy; gingvectomy, for gingivitis or periodontitis.<br />
• For medical and surgical services intended for <strong>the</strong> treatment or control <strong>of</strong> obesity, unless<br />
Medically Necessary. However, treatment <strong>of</strong> clinically severe obesity, as defined by <strong>the</strong> body<br />
mass index (BMI) classifications <strong>of</strong> <strong>the</strong> National Heart, Lung and Blood Institute (NHLBI)<br />
<strong>guide</strong>lines to be covered only at approved centers if <strong>the</strong> services are demonstrated, through<br />
existing peer-reviewed, evidence based, scientific literature and scientifically based <strong>guide</strong>lines,<br />
to be safe and effective for treatment <strong>of</strong> this condition. Clinically severe obesity is defined by<br />
<strong>the</strong> NHLBI as a BMMI <strong>of</strong> 40 or greater without comorbidities, or 35-39 with comorbidities. The<br />
following are specifically excluded: (a) medical and surgical services to alter appearance or<br />
physical changes that are <strong>the</strong> result <strong>of</strong> any surgery performed for <strong>the</strong> management <strong>of</strong> obesity or<br />
clinically severe (morbid) obesity; and (b) weight loss programs or treatments, whe<strong>the</strong>r<br />
prescribed or recommended by a Physician or under medical supervision.<br />
• Unless o<strong>the</strong>rwise covered in this plan, for reports, evaluations, physical examinations, or<br />
hospitalizations not required for health reasons including, but not limited to, employment,<br />
insurance or government licenses, and court-ordered, forensic or custodial evaluations.<br />
• Court-ordered treatment or hospitalization, unless such treatment is prescribed by a Physician<br />
and listed as covered in this plan.<br />
• Transsexual surgery including medical or psychological counseling and hormonal <strong>the</strong>rapy in<br />
preparation for, or subsequent to, any such surgery.<br />
• Any medications, drugs, services or supplies for <strong>the</strong> treatment <strong>of</strong> female sexual dysfunction and<br />
male impotence, such as, but not limited to, anorgasmy, and premature ejaculation.<br />
• For Infertility Services, including infertility drugs; surgical or medical treatment programs for<br />
infertility (such as in vitro fertilization, gamete intrafallopian transfer [GIFT], zygote<br />
intrafallopian transfer [ZIFT], or any variations <strong>of</strong> this procedures); and artificial insemination<br />
(including donor fees and any costs associated with <strong>the</strong> collection, washing, preparation, or<br />
storage <strong>of</strong> sperm). Cryopreservation <strong>of</strong> donor sperm or eggs is also excluded form coverage.<br />
• For amniocentesis, ultrasound, or any o<strong>the</strong>r procedures requested solely for gender<br />
determination <strong>of</strong> a fetus, unless Medically Necessary to determine <strong>the</strong> existence <strong>of</strong> a genderlinked<br />
genetic disorder.<br />
• Medical and Hospital care and costs for <strong>the</strong> infant child <strong>of</strong> a Dependent, unless this infant child<br />
is o<strong>the</strong>rwise eligible under this plan.<br />
• Nonmedical counseling or ancillary services, including but not limited to Custodial Services,<br />
education, training, vocational rehabilitation, behavior training, bi<strong>of</strong>eedback, neur<strong>of</strong>eedback,<br />
hypnosis, sleep <strong>the</strong>rapy, employment counseling, back school, return to work services, work<br />
hardening programs, driving safety, and services, training, educational <strong>the</strong>rapy or o<strong>the</strong>r<br />
nonmedical ancillary services for learning disabilities, developmental delays, autism or mental<br />
retardation.<br />
• Therapy or treatment intended primarily to improve or maintain general physical condition or<br />
for <strong>the</strong> purpose <strong>of</strong> enhancing job, school, athletic or recreational performance, including but not<br />
limited to routine, long term or maintenance care which is provided after <strong>the</strong> resolution <strong>of</strong> <strong>the</strong><br />
acute medical problem and when significant <strong>the</strong>rapeutic improvement is not expected.<br />
• Consumable medical supplies o<strong>the</strong>r than ostomy supplies and urinary ca<strong>the</strong>ters. Excluded<br />
supplies include, but are not limited to bandages and o<strong>the</strong>r disposable medical supplies, skin<br />
preparations and test strips, except as specified in <strong>the</strong> “Home Health Services” or “Breast<br />
Reconstruction and Breast Pros<strong>the</strong>ses” sections <strong>of</strong> this plan.<br />
• Private Hospital rooms and/or private duty nursing unless determined by <strong>the</strong> utilization review<br />
Physician to be Medically Necessary.<br />
• Personal or comfort items such as personal care kits provided on admission to a Hospital,<br />
television, telephone, <strong>new</strong>born infant photographs, complimentary meals, birth announcements,<br />
and o<strong>the</strong>r articles which are not for <strong>the</strong> specific treatment or an Injury or Sickness.<br />
• Artificial aids including, but not limited to, corrective orthopedic shoes, arch supports, elastic<br />
stockings, garter belts, corsets, dentures and wigs.<br />
• Hearing aids, including but not limited to semi-implantable hearing devices, audient bone<br />
conductors and Bone Anchored Hearing Aids (BAHAs). A hearing aid is any device that<br />
amplifies sound.<br />
• Aids or devices that assist with nonverbal communications, including but not limited to<br />
communication boards, prerecorded speech devices, laptop computers, desktop computers,<br />
Personal Digital Assistants (PDAs), Braille typewriters, visual alert systems for <strong>the</strong> deaf and<br />
memory books.<br />
• Medical <strong>benefits</strong> for eyeglasses, contact lenses, or examinations for prescription or fitting<br />
<strong>the</strong>re<strong>of</strong>, except that Covered Expenses will include <strong>the</strong> purchase <strong>of</strong> <strong>the</strong> first pair <strong>of</strong> eyeglasses,<br />
lenses, frames, or contact lenses that follows keratoconus or cataract surgery.<br />
• Charges made for or in connection with routine refractions, eye exercises and for surgical<br />
treatment for <strong>the</strong> correction <strong>of</strong> a refractive error, including radial keratotomy, when eyeglasses<br />
or contact lenses may be worn.<br />
• All non injectable prescription drugs, nonprescription drugs, and investigational and<br />
experimental drugs, except as provided in this plan.<br />
• Routine foot care including <strong>the</strong> paring and removing <strong>of</strong> corns and calluses or trimming <strong>of</strong> nails.<br />
However, services associated with foot care for diabetes and peripheral vascular disease are<br />
covered when Medically Necessary.<br />
• Membership cost or fees associated with health clubs, weight loss programs and smoking<br />
cessations programs.<br />
• Genetic screening or pre-implantations genetic screening. General population-based genetic<br />
screening is a testing method performed in <strong>the</strong> absence <strong>of</strong> any symptoms or any significant,<br />
proven risk factors for genetically linked inheritable disease.<br />
• Dental implants for any condition.<br />
• Fees associated with <strong>the</strong> collection or donation <strong>of</strong> blood or blood products, except for<br />
autologous donation in anticipation <strong>of</strong> scheduled services where in <strong>the</strong> utilization review<br />
Physician’s opinion <strong>the</strong> likelihood <strong>of</strong> excess blood loss is such that transfusion is an expected<br />
adjunct to surgery.<br />
• Blood <strong>administration</strong> for <strong>the</strong> purpose <strong>of</strong> general improvement in physical condition.<br />
• Cost <strong>of</strong> biologicals that are immunizations or medications for <strong>the</strong> purpose <strong>of</strong> travel, or to protect<br />
against occupational hazards and risks.<br />
• Cosmetics, dietary supplements and health and beauty aids and nutritional formulae (except as<br />
described in Covered Expenses).<br />
• For or in connection with an Injury or Sickness arising out <strong>of</strong>, or in <strong>the</strong> course <strong>of</strong>, any<br />
employment for wage or pr<strong>of</strong>it.<br />
• Telephone, e-mail, and Internet consultations and telemedicine.<br />
• Massage <strong>the</strong>rapy.<br />
• For charges which would not have been made if <strong>the</strong> person had no health <strong>benefits</strong>.<br />
• To <strong>the</strong> extent that <strong>the</strong>y are more than Reasonable and Customary charges.<br />
• Expenses incurred outside <strong>the</strong> United States or Canada, unless you or your Dependent is a U.S.<br />
or Canadian resident and <strong>the</strong> charges are incurred while traveling on business or for pleasure.<br />
• To <strong>the</strong> extent <strong>of</strong> <strong>the</strong> exclusions imposed by any notification requirement shown in this plan.<br />
• Elective and non-elective abortions.<br />
• Health services received after <strong>the</strong> date your coverage under <strong>the</strong> Plan ends, including health<br />
services for medical conditions arising prior to <strong>the</strong> date your coverage under <strong>the</strong> Plan ends.<br />
This summary <strong>of</strong> Benefits is intended only to highlight your Benefits and should not be relied upon to fully determine coverage. This plan may not cover all your health care<br />
expenses. Please refer to <strong>the</strong> Summary Plan Description for a complete listing <strong>of</strong> services, limitations, exclusions and a description <strong>of</strong> all <strong>the</strong> terms and conditions <strong>of</strong> coverage. If this<br />
description conflicts in any way with <strong>the</strong> Summary Plan Description, <strong>the</strong> Summary Plan Description prevails. Terms that are capitalized in <strong>the</strong> Benefit Summary are defined in <strong>the</strong><br />
Summary Plan Description.<br />
12/15/05 WARNY004 100-3513
THE ARCHDIOCESE OF NEW YORK<br />
SUMMARY OF MEDICAL BENEFITS<br />
Medicare Supplement For Clergy, Religious and Lay<br />
Employees (over 65), Who Have Medicare Primary<br />
Benefits (MSYRX)<br />
UNITED HEALTHCARE MEDICARE SUPPLEMENT WITH RX<br />
-17 -
Summary <strong>of</strong> Benefits<br />
UnitedHealthcare Medicare plan<br />
Archdiocese <strong>of</strong> New York<br />
Medicare Supplemental Plan for Clergy, Religious, and Lay Employees (MSYRX)<br />
Effective January 1, 2006, if you have any questions please call UnitedHealthcare<br />
Member Services at 1-800-736-1264 or register on myuhc.com to get detailed<br />
information on your coverage.<br />
Your Medicare Supplemental plan provides a maximum freedom for dealing with any health care<br />
situation. This incredibly flexible program lets you make your own health care decisions,<br />
including which doctors and specialists to visit. Benefits are provided for covered health services<br />
received from any physician or o<strong>the</strong>r licensed medical provider. This plan coordinates with<br />
Medicare.<br />
Some Important Benefits <strong>of</strong> your plan:<br />
• Receive care from any licensed medical<br />
physician or o<strong>the</strong>r provider you want.<br />
• Choose to see any licensed specialist you<br />
want without having to get a referral.<br />
• Go to any hospital you want-anywhere,<br />
anytime.<br />
• Emergencies are covered anywhere in <strong>the</strong><br />
world.<br />
• Benefits are available for <strong>of</strong>fice visits and<br />
hospital care, as well as inpatient and<br />
outpatient surgery, when covered health<br />
services are provided.<br />
• We <strong>of</strong>fer <strong>the</strong> Language Line Services so<br />
that you can talk with us in 140 different<br />
languages. Just call customer service and<br />
ask for an interpreter.<br />
• United Healthcare’s Nurseline<br />
connects you to registered nurses and a<br />
library <strong>of</strong> recorded programs on<br />
important health topics 24 hours a day,<br />
7 days a week, from anywhere in U.S.<br />
• Care Coordination SM services are available<br />
to help identify and prevent delays in care<br />
for those who might need specialized help.<br />
• The tools and information at myuhc.com<br />
are practical and personalized so you can<br />
get <strong>the</strong> most out <strong>of</strong> your <strong>benefits</strong>. Register<br />
at myuhc.com and connect to current<br />
information about your <strong>benefits</strong> and health<br />
care interests.<br />
• Cancer Resource Services provides<br />
information on comprehensive cancer<br />
treatment services. Benefit from using<br />
one <strong>of</strong> our Centers <strong>of</strong> Excellence by<br />
calling 1-866-936-6002.
Medicare Supplemental Plan Benefits Summary<br />
Types <strong>of</strong> Coverage<br />
Benefits /Copayment Amounts<br />
This Benefit Summary is intended only to highlight Annual Deductible: $150 per Covered Person per calendar year.<br />
your Benefits and should not be relied upon to fully<br />
determine coverage. This benefit plan may not cover all Out-<strong>of</strong>-Pocket Maximum: $750 per Covered Person per calendar year.<br />
<strong>of</strong> your health care expenses. More complete<br />
descriptions <strong>of</strong> Benefits and <strong>the</strong> terms under which Maximum Plan Benefit: No Maximum Plan Benefit.<br />
<strong>the</strong>y are provided are contained in <strong>the</strong> Summary<br />
Plan Description that you will receive upon enrolling<br />
in <strong>the</strong> Plan.<br />
If this Benefit Summary conflicts in any way with <strong>the</strong><br />
Summary Plan Description issued to your employer, <strong>the</strong><br />
Summary Plan Description shall prevail.<br />
Terms that are capitalized in <strong>the</strong> Benefit Summary are<br />
defined in <strong>the</strong> Summary Plan Description.<br />
MEMBER PAYS<br />
1. Ambulance Services - Emergency only Ground Transportation: 0% <strong>of</strong> Eligible Expenses<br />
Air Transportation: 0% <strong>of</strong> Eligible Expenses<br />
2. Dental Services - Accident only – Treatment must<br />
begin within six months <strong>of</strong> injury.<br />
3. Durable Medical Equipment<br />
The purchase or rental <strong>of</strong> prescribed equipment is<br />
covered including needed replacement and repair.<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
4. Emergency Health Services 0% <strong>of</strong> Eligible Expenses<br />
5. Refractive Eye Examinations No Coverage<br />
6. Home Health Care<br />
Benefits are limited to 200 visits for skilled care<br />
services per calendar year.<br />
7. Hospice Care<br />
No annual maximum<br />
0% <strong>of</strong> Eligible Expenses<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
8. Hospital - Inpatient Stay 0% <strong>of</strong> Eligible Expenses<br />
9. Injections Received in a Physician’s Office 20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
10. Maternity Services No coverage<br />
11. Outpatient Surgery, Diagnostic and Therapeutic<br />
Services<br />
Outpatient Surgery<br />
Outpatient Diagnostic Services<br />
Outpatient Diagnostic/Therapeutic Services - CT<br />
Scans, Pet Scans, MRI and Nuclear Medicine<br />
Outpatient Therapeutic Treatments<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
For lab and radiology/Xray: 20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
For mammography testing: 20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
12. Physician’s Office Services 20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
13. Pr<strong>of</strong>essional Fees for Surgical and Medical<br />
Services<br />
14. Pros<strong>the</strong>tic Devices<br />
The purchase or rental <strong>of</strong> prescribed equipment is<br />
covered including needed replacement and repair.<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
15. Reconstructive Procedures Hospital Inpatient Stay – 20% <strong>of</strong> Eligible Expenses after satisfying deductible.<br />
Outpatient Surgery - 20% <strong>of</strong> Eligible Expenses after satisfying deductible.<br />
Outpatient Diagnostic Therapeutic Services – 20% <strong>of</strong> Eligible Expenses after satisfying deductible.<br />
Outpatient Therapeutic Treatments - 20% <strong>of</strong> Eligible Expenses after satisfying deductible.<br />
Physician’s Office Services - 20% <strong>of</strong> Eligible Expenses after satisfying deductible.
UnitedHealthcare<br />
Types <strong>of</strong> Coverage<br />
16. Rehabilitation Services -Outpatient Therapy<br />
90 visits per year for all types <strong>of</strong> <strong>the</strong>rapy combined<br />
(physical <strong>the</strong>rapy, occupational <strong>the</strong>rapy, cardiac<br />
rehabilitation, restorative speech <strong>the</strong>rapy, and<br />
chiropractic care).<br />
17. Skilled Nursing Facility/Inpatient Rehabilitation<br />
Facility Services<br />
Benefits are limited to 120 days per calendar year.<br />
Benefits /Copayment Amounts<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
0% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
18. Transplantation Services 20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
19. Urgent Care Center Services 0% <strong>of</strong> Eligible expenses<br />
Additional Benefits<br />
Mental Health Services – Outpatient<br />
Benefits are limited to 45 visits per calendar year. Two<br />
group visits reduce <strong>the</strong> 45 visit maximum by one day.<br />
Outpatient Mental Health visits do not apply to out <strong>of</strong><br />
pocket maximum.<br />
Mental Health Services - Inpatient and Intermediate<br />
Benefits are limited to 45 visits per calendar year. Two<br />
days <strong>of</strong> residential treatment reduces <strong>the</strong> 45 visit<br />
maximum by one day.<br />
Substance Abuse Services – Outpatient<br />
Benefits are limited to 60 visits per calendar year. Two<br />
group visits reduce <strong>the</strong> 60 visit maximum by one day.<br />
Outpatient Substance Abuse visits do not apply to out<br />
<strong>of</strong> pocket maximum.<br />
Substance Services - Inpatient and Intermediate<br />
Benefits are limited to 45 visits per calendar year. Two<br />
days <strong>of</strong> residential treatment reduces <strong>the</strong> 45 visit<br />
maximum by one day.<br />
Prescription Drugs - Rx vendor is Caremark<br />
(1-800-565-7091<br />
Pharmacy fills: On <strong>the</strong> third fill <strong>of</strong> a maintenance drug<br />
at <strong>the</strong> retail pharmacy, <strong>the</strong> copay changes to $10/40/70<br />
per 30 day supply.<br />
Generic Incentive: When you fill a Rx for a brand name<br />
drug that has a generic equivalent you pay <strong>the</strong> brand<br />
name copay plus <strong>the</strong> difference in <strong>the</strong> cost between <strong>the</strong><br />
brand name and its generic equivalent.<br />
50% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
0% <strong>of</strong> Eligible Expenses<br />
20% <strong>of</strong> Eligible Expenses after satisfying deductible<br />
0% <strong>of</strong> Eligible Expenses<br />
Retail Drug Program –<br />
$5 per 30-day supply for generic drugs<br />
$20 per 30-day supply for preferred drugs<br />
$35 per 30-day supply for non-preferred drugs<br />
Mail Order Program –<br />
$10 per 90-day supply for generic drugs<br />
$40 per 90-day supply for preferred drugs<br />
$70 per 90-day supply for non-preferred drugs
Exclusions<br />
UnitedHealthcare<br />
Except as may be specifically provided in Section 1 <strong>of</strong> <strong>the</strong> Summary Plan Description (SPD) or<br />
through a Rider to <strong>the</strong> Plan, <strong>the</strong> following are not covered:<br />
Covered Expenses will not include, and no payment will be made for <strong>the</strong> following expenses incurred,<br />
unless those expenses are considered Medically Necessary.<br />
• Expenses for charges that are not Medically Necessary, except as specified in any notification<br />
requirements shown in this plan.<br />
• To <strong>the</strong> extent that you or any one <strong>of</strong> your Dependents is in any way paid or entitled to payment<br />
for those expenses by or through a public program, o<strong>the</strong>r than Medicaid.<br />
• To <strong>the</strong> extent that payment is unlawful where <strong>the</strong> person resides when <strong>the</strong> expenses are incurred.<br />
• Charges made by a Hospital owned or operated by or which provides care or performs services<br />
for <strong>the</strong> United States Government: (a) unless <strong>the</strong>re is a legal obligation to pay such charges<br />
whe<strong>the</strong>r or not <strong>the</strong>re is insurance; or (b) if such charges are directly related to a military-service<br />
connected Injury or Sickness.<br />
• For or in connection with an Injury or Sickness which is due to war, declared or undeclared.<br />
• Charges which you are not obligated to pay or for which you are not billed or for which you<br />
would not have been billed except that <strong>the</strong>y were covered under this plan.<br />
• Assistance in <strong>the</strong> activities <strong>of</strong> daily living, including but not limited to eating, bathing, dressing,<br />
toileting or o<strong>the</strong>r non-Medically Necessary self-care activities, homemaker services and services<br />
primarily for rest domiciliary or convalescent care.<br />
• Cosmetic surgery and <strong>the</strong>rapies. Cosmetic surgery or <strong>the</strong>rapy is defined as surgery or <strong>the</strong>rapy<br />
performed to improve or alter appearance or self-esteem or to treat psychological<br />
symptomatoloty or psychosocial complaints related to one’s appearance and determined not to<br />
be Medically Necessary. However, reconstructive surgery is covered as provided under Covered<br />
Expenses and for <strong>the</strong> purposes <strong>of</strong> this exclusion <strong>the</strong> term cosmetic surgery or <strong>the</strong>rapy shall not<br />
include reconstructive surgery when such service is incidental to or follows surgery resulting<br />
from trauma, infection or o<strong>the</strong>r disease <strong>of</strong> <strong>the</strong> involved part.<br />
• Macromastia or gynecomastia surgeries; abdominoplasty/panniculectomy; rhinoplasty;<br />
blepharoplasty; orthognathic surgeries; redundant skin surgery; removal <strong>of</strong> skin tags;<br />
acupressure; craniosacral/cranial <strong>the</strong>rapy; dance <strong>the</strong>rapy; movement <strong>the</strong>rapy; applied<br />
kinesiology; rolfing; prolo<strong>the</strong>rapy; and extracorporeal shock wave lithotripsy for<br />
musculoskeletal and orthopedic conditions.<br />
• For or in connection with treatment <strong>of</strong> <strong>the</strong> teeth or peridontium unless such expenses are<br />
incurred for: (a) charges made for services or supplies provided for or in connection with an<br />
accidental injury to sound natural teeth, provided a continuous course <strong>of</strong> dental treatment started<br />
within 6 months <strong>of</strong> <strong>the</strong> accident; (b) charges made by a Hospital for Bed and Board or<br />
Necessary Services and Supplies; (c) charges made by a Free-Standing Surgical Facility or <strong>the</strong><br />
outpatient department <strong>of</strong> a Hospital in connection with surgery, or (d) charges made by a<br />
Physician for any <strong>of</strong> <strong>the</strong> following Surgical Procedures: excision <strong>of</strong> epulis; removal <strong>of</strong> residual<br />
root (when performed by a Dentist o<strong>the</strong>r than <strong>the</strong> one who extracted <strong>the</strong> tooth); intraoral<br />
drainage <strong>of</strong> acute alveolar abscess with cellulitis; alveolectomy; gingvectomy, for gingivitis or<br />
periodontitis.<br />
• For medical and surgical services intended for <strong>the</strong> treatment or control <strong>of</strong> obesity, unless<br />
Medically Necessary. However, treatment <strong>of</strong> clinically severe obesity, as defined by <strong>the</strong> body<br />
mass index (BMI) classifications <strong>of</strong> <strong>the</strong> National Heart, Lung and Blood Institute (NHLBI)<br />
<strong>guide</strong>lines to be covered only at approved centers if <strong>the</strong> services are demonstrated, through<br />
existing peer-reviewed, evidence based, scientific literature and scientifically based <strong>guide</strong>lines,<br />
to be safe and effective for treatment <strong>of</strong> this condition. Clinically severe obesity is defined by<br />
<strong>the</strong> NHLBI as a BMMI <strong>of</strong> 40 or greater without comorbidities, or 35-39 with comorbidities. The<br />
following are specifically excluded: (a) medical and surgical services to alter appearance or<br />
physical changes that are <strong>the</strong> result <strong>of</strong> any surgery performed for <strong>the</strong> management <strong>of</strong> obesity or<br />
clinically severe (morbid) obesity; and (b) weight loss programs or treatments, whe<strong>the</strong>r<br />
prescribed or recommended by a Physician or under medical supervision.<br />
• Unless o<strong>the</strong>rwise covered in this plan, for reports, evaluations, physical examinations, or<br />
hospitalizations not required for health reasons including, but not limited to, employment,<br />
insurance or government licenses, and court-ordered, forensic or custodial evaluations.<br />
• Court-ordered treatment or hospitalization, unless such treatment is prescribed by a Physician<br />
and listed as covered in this plan.<br />
• Transsexual surgery including medical or psychological counseling and hormonal <strong>the</strong>rapy in<br />
preparation for, or subsequent to, any such surgery.<br />
• Any medications, drugs, services or supplies for <strong>the</strong> treatment <strong>of</strong> female sexual dysfunction and<br />
male impotence, such as, but not limited to, anorgasmy, and premature ejaculation.<br />
• For Infertility Services, including infertility drugs; surgical or medical treatment programs for<br />
infertility (such as in vitro fertilization, gamete intrafallopian transfer [GIFT], zygote<br />
intrafallopian transfer [ZIFT], or any variations <strong>of</strong> this procedures); and artificial insemination<br />
(including donor fees and any costs associated with <strong>the</strong> collection, washing, preparation, or<br />
storage <strong>of</strong> sperm). Cryopreservation <strong>of</strong> donor sperm or eggs is also excluded form coverage.<br />
• For amniocentesis, ultrasound, or any o<strong>the</strong>r procedures requested solely for gender<br />
determination <strong>of</strong> a fetus, unless Medically Necessary to determine <strong>the</strong> existence <strong>of</strong> a genderlinked<br />
genetic disorder.<br />
• Medical and Hospital care and costs for <strong>the</strong> infant child <strong>of</strong> a Dependent, unless this infant child<br />
is o<strong>the</strong>rwise eligible under this plan.<br />
• Non-medical counseling or ancillary services, including but not limited to Custodial Services,<br />
education, training, vocational rehabilitation, behavior training, bi<strong>of</strong>eedback, neur<strong>of</strong>eedback,<br />
hypnosis, sleep <strong>the</strong>rapy, employment counseling, back school, return to work services, work<br />
hardening programs, driving safety, and services, training, educational <strong>the</strong>rapy or o<strong>the</strong>r nonmedical<br />
ancillary services for learning disabilities, developmental delays, autism or mental<br />
retardation.<br />
• Therapy or treatment intended primarily to improve or maintain general physical condition or<br />
for <strong>the</strong> purpose <strong>of</strong> enhancing job, school, athletic or recreational performance, including but not<br />
limited to routine, long term or maintenance care which is provided after <strong>the</strong> resolution <strong>of</strong> <strong>the</strong><br />
acute medical problem and when significant <strong>the</strong>rapeutic improvement is not expected.<br />
• Consumable medical supplies o<strong>the</strong>r than ostomy supplies and urinary ca<strong>the</strong>ters. Excluded<br />
supplies include, but are not limited to bandages and o<strong>the</strong>r disposable medical supplies, skin<br />
preparations and test strips, except as specified in <strong>the</strong> “Home Health Services” or “Breast<br />
Reconstruction and Breast Pros<strong>the</strong>ses” sections <strong>of</strong> this plan.<br />
• Private Hospital rooms and/or private duty nursing unless determined by <strong>the</strong> utilization review<br />
Physician to be Medically Necessary.<br />
• Personal or comfort items such as personal care kits provided on admission to a Hospital,<br />
television, telephone, <strong>new</strong>born infant photographs, complimentary meals, birth announcements,<br />
and o<strong>the</strong>r articles which are not for <strong>the</strong> specific treatment or an Injury or Sickness.<br />
• Artificial aids including, but not limited to, corrective orthopedic shoes, arch supports, elastic<br />
stockings, garter belts, corsets, dentures and wigs.<br />
• Hearing aids, including but not limited to semi-implantable hearing devices, audient bone<br />
conductors and Bone Anchored Hearing Aids (BAHAs). A hearing aid is any device that<br />
amplifies sound.<br />
• Aids or devices that assist with nonverbal communications, including but not limited to<br />
communication boards, prerecorded speech devices, laptop computers, desktop computers,<br />
Personal Digital Assistants (PDAs), Braille typewriters, visual alert systems for <strong>the</strong> deaf and<br />
memory books.<br />
• Medical <strong>benefits</strong> for eyeglasses, contact lenses, or examinations for prescription or fitting<br />
<strong>the</strong>re<strong>of</strong>, except that Covered Expenses will include <strong>the</strong> purchase <strong>of</strong> <strong>the</strong> first pair <strong>of</strong> eyeglasses,<br />
lenses, frames, or contact lenses that follows keratoconus or cataract surgery.<br />
• Charges made for or in connection with routine refractions, eye exercises and for surgical<br />
treatment for <strong>the</strong> correction <strong>of</strong> a refractive error, including radial keratotomy, when eyeglasses<br />
or contact lenses may be worn.<br />
• All non injectable prescription drugs, nonprescription drugs, and investigational and<br />
experimental drugs, except as provided in this plan.<br />
• Routine foot care including <strong>the</strong> paring and removing <strong>of</strong> corns and calluses or trimming <strong>of</strong> nails.<br />
However, services associated with foot care for diabetes and peripheral vascular disease are<br />
covered when Medically Necessary.<br />
• Membership cost or fees associated with health clubs, weight loss programs and smoking<br />
cessations programs.<br />
• Genetic screening or pre-implantations genetic screening. General population-based genetic<br />
screening is a testing method performed in <strong>the</strong> absence <strong>of</strong> any symptoms or any significant,<br />
proven risk factors for genetically linked inheritable disease.<br />
• Dental implants for any condition.<br />
• Fees associated with <strong>the</strong> collection or donation <strong>of</strong> blood or blood products, except for<br />
autologous donation in anticipation <strong>of</strong> scheduled services where in <strong>the</strong> utilization review<br />
Physician’s opinion <strong>the</strong> likelihood <strong>of</strong> excess blood loss is such that transfusion is an expected<br />
adjunct to surgery.<br />
• Blood <strong>administration</strong> for <strong>the</strong> purpose <strong>of</strong> general improvement in physical condition.<br />
• Cost <strong>of</strong> biologicals that are immunizations or medications for <strong>the</strong> purpose <strong>of</strong> travel, or to protect<br />
against occupational hazards and risks.<br />
• Cosmetics, dietary supplements and health and beauty aids and nutritional formulae (except as<br />
described in Covered Expenses).<br />
• For or in connection with an Injury or Sickness arising out <strong>of</strong>, or in <strong>the</strong> course <strong>of</strong>, any<br />
employment for wage or pr<strong>of</strong>it.<br />
• Telephone, e-mail, and Internet consultations and telemedicine.<br />
• Massage <strong>the</strong>rapy.<br />
• For charges which would not have been made if <strong>the</strong> person had no health <strong>benefits</strong>.<br />
• To <strong>the</strong> extent that <strong>the</strong>y are more than Reasonable and Customary charges.<br />
• Expenses incurred outside <strong>the</strong> United States or Canada, unless you or your Dependent is a U.S.<br />
or Canadian resident and <strong>the</strong> charges are incurred while traveling on business or for pleasure.<br />
• To <strong>the</strong> extent <strong>of</strong> <strong>the</strong> exclusions imposed by any notification requirement shown in this plan.<br />
• Elective and non-elective abortions.<br />
• Health services received after <strong>the</strong> date your coverage under <strong>the</strong> Plan ends, including health<br />
services for medical conditions arising prior to <strong>the</strong> date your coverage under <strong>the</strong> Plan ends.<br />
This summary <strong>of</strong> Benefits is intended only to highlight your Benefits and should not be relied upon to fully determine coverage. This plan may not cover all your health care<br />
expenses. Please refer to <strong>the</strong> Summary Plan Description for a complete listing <strong>of</strong> services, limitations, exclusions and a description <strong>of</strong> all <strong>the</strong> terms and conditions <strong>of</strong> coverage. If this<br />
description conflicts in any way with <strong>the</strong> Summary Plan Description, <strong>the</strong> Summary Plan Description prevails. Terms that are capitalized in <strong>the</strong> Benefit Summary are defined in <strong>the</strong><br />
Summary Plan Description.<br />
01/16/07 OARNY005 100-3507
Section IV<br />
Filing for Claims
HOW TO FILE A MEDICAL CLAIM<br />
There are several ways to file a claim for medical <strong>benefits</strong>:<br />
• Direct Claim - Your healthcare provider’s <strong>of</strong>fice can file <strong>the</strong> claim electronically<br />
on your behalf with <strong>the</strong> insurance carrier.<br />
• Paper Claim - You must complete and sign <strong>the</strong> Health Claim Transmittal form,<br />
and mail it to:<br />
United Healthcare<br />
P.O. Box 740800<br />
Atlanta, GA 30374-0800<br />
United Healthcare’s Customer Service Telephone Number 1.800.736.1264<br />
• Invoice - If you receive an invoice from a healthcare provider or healthcare<br />
facility, (laboratory/anes<strong>the</strong>siologist, etc.) that lists an insurance information<br />
section (most times this will be on <strong>the</strong> reverse side <strong>of</strong> <strong>the</strong> invoice), you can<br />
complete <strong>the</strong> insurance information section, and ei<strong>the</strong>r return to <strong>the</strong> service<br />
provider, or send it directly to <strong>the</strong> insurance carrier (follow <strong>the</strong> directions on<br />
invoice). Remember to include <strong>the</strong> group policy number listed on your ID card.<br />
• If <strong>the</strong> invoice is itemized, and lists <strong>the</strong> date(s) <strong>of</strong> service, a diagnosis or diagnostic<br />
code, and a total dollar amount <strong>of</strong> charges you can paper clip (do not staple) <strong>the</strong><br />
invoice to a Health Claim Transmittal form. Complete, sign and mail it to United<br />
Healthcare at <strong>the</strong> address listed above.<br />
Important Note: Keep a copy <strong>of</strong> any claims that you submit to <strong>the</strong> insurance<br />
carrier.<br />
- 18 -<br />
Revised 07/2009
Caremark is our current prescription carrier.<br />
Eligibility<br />
PRESCRIPTION BENEFIT SUMMARY<br />
• Participants and <strong>the</strong>ir dependents must also be enrolled in <strong>the</strong> United Healthcare plan<br />
• Dependent Children covered to age 19, to age 25 full time student or disabled child.<br />
Co-payments<br />
• Generic Drug - Lowest Co-payment<br />
• Preferred Brand Drugs included on Caremark’s Primary Drug list - Moderate Co-payment<br />
• Brand Drugs not included on Caremark’s Primary Drug list - Highest Co-pay<br />
Retail Pharmacy<br />
Participants may purchase a 30-day supply <strong>of</strong> medications from participating retail pharmacies.<br />
(For a list <strong>of</strong> participating pharmacies, please call Customer Service at 800.565.7091 or visit <strong>the</strong><br />
website at www.caremark.com).<br />
Restrictions – After two maintenance fills at a retail pharmacy during a calendar year, <strong>the</strong> third<br />
maintenance fill at a retail pharmacy will be subject to higher Mail Order copayment for a 30 day<br />
supply. (Refer to Health Benefit Summary for details).<br />
Mail order<br />
Participants also have <strong>the</strong> option <strong>of</strong> purchasing up to a 90-day supply <strong>of</strong> medications through<br />
Caremark’s Mail Order Service Pharmacy. Mail order is one <strong>of</strong> <strong>the</strong> most cost effective options.<br />
(Please refer to booklet for fur<strong>the</strong>r details or call Customer Service at 800.565.7091).<br />
NOTES:<br />
• Vacation Supplies<br />
Participants and dependents should contact Customer Service at 800.565.7091 or visit <strong>the</strong> website<br />
at www.caremark.com before going on vacation for <strong>the</strong> nearest out <strong>of</strong> town participating<br />
pharmacy, or to request a vacation supply <strong>of</strong> medications.<br />
Prescriptions purchased through non-participating (out-<strong>of</strong>-network) pharmacies are not covered.<br />
• Prescription Exceptions<br />
Participants requesting coverage for medications not listed in <strong>the</strong> benefit booklet should fax a<br />
letter <strong>of</strong> medical necessity from <strong>the</strong> physician to <strong>the</strong> attention <strong>of</strong> <strong>the</strong> Fatima Faria, Caremark at<br />
401.335.7488.<br />
Refer to Booklet for detailed information regarding covered services.<br />
- 19 -<br />
07/2009
HOW TO FILE A CLAIM FOR PRESCRIPTION DRUGS<br />
In-Network Retail Pharmacy: When a prescription is filled at an in-network pharmacy,<br />
<strong>the</strong> insured must present his/her Caremark ID Card and pay <strong>the</strong> applicable co-pay.<br />
Prescriptions filled at a non-participating pharmacy are not covered. There is no out-<strong>of</strong>network<br />
coverage for this benefit.<br />
Mail Order: When using <strong>the</strong> Mail Order Option, <strong>the</strong> insured must complete <strong>the</strong> Mail<br />
Service Order Form, attach <strong>the</strong> prescription from <strong>the</strong> physician, and enclose a check,<br />
money order, or Credit Card number for <strong>the</strong> co-payment. (An incomplete Mail Service<br />
Order form will be returned and processing will be delayed).<br />
Paper Claim: When a prescription is filled at a non-participating pharmacy and <strong>the</strong><br />
insured has to pay for <strong>the</strong> full cost <strong>of</strong> a covered prescription drug; he/she should file a<br />
paper claim with Caremark. To file a paper claim <strong>the</strong> insured must complete and sign a<br />
Prescription Drug Claim Form, attach <strong>the</strong> original receipt from <strong>the</strong> pharmacy, and send it<br />
directly to:<br />
CVS Caremark, Inc.<br />
Attn: Claims Department<br />
P.O. Box 52196<br />
Phoenix, AZ 85072-2196<br />
Important Note: Keep a copy <strong>of</strong> any claims that you submit to <strong>the</strong> insurance carrier<br />
- 20 -<br />
07/2009
MAIL SERVICE<br />
ORDER FORM<br />
Mail order form to:<br />
Please fold here<br />
Enter ID# if not shown or different from above<br />
CVS CAREMARK<br />
PGH WB STD<br />
PO BOX 2110<br />
PITTSBURGH, PA 15230-2110<br />
Please fold here<br />
Please fold here<br />
Prescription Plan Sponsor or Company Name<br />
DIRECTIONS: Print in BLUE or BLACK ink, using CAPITAL letters. Fill in ovals completely ( ). Complete<br />
both sides <strong>of</strong> form.<br />
To order <strong>new</strong> prescriptions: Mail your prescription(s) with this form. # <strong>of</strong> <strong>new</strong> prescriptions:<br />
To order refills: Order by Web, phone, or write in Rx number(s) below. # <strong>of</strong> refill prescriptions:<br />
FOR FASTEST SERVICE, order refills at www.caremark.com or call <strong>the</strong> number on your prescription<br />
benefit identification card.<br />
SHIPPING ADDRESS IF NOT SHOWN OR DIFFERENT FROM ABOVE:<br />
Last Name First Name MI Suffix (JR, SR)<br />
Street Address<br />
Apt./Suite#<br />
Use this address<br />
for this order only.<br />
City State ZIP Code<br />
Please fold here<br />
Daytime Phone #:<br />
- -<br />
Evening Phone #: - -<br />
* WEB *<br />
REFILL INFORMATION:<br />
To order mail service refills, enter your prescription number(s) here:<br />
1) 2) 3) 4)<br />
5) 6) 7) 8)<br />
* WEB *<br />
Prescriptions sent in one envelope may be shipped toge<strong>the</strong>r unless you request o<strong>the</strong>rwise.<br />
©2008 Caremark. All rights reserved. P12-N
FILL IN FOR UP TO TWO PEOPLE WHO WILL RECEIVE PRESCRIPTIONS WITH THIS ORDER<br />
1st PERSON ORDERING A PRESCRIPTION<br />
N I C K N A M E<br />
Your E-mail:<br />
Gender: M F<br />
Easy open caps Print in Spanish<br />
Suffix<br />
(JR,SR)<br />
Date <strong>of</strong> Birth:<br />
MM-DD-YYYY<br />
Date <strong>new</strong> prescription written:<br />
Last Name First Name MI<br />
Please fold here<br />
Doctor’s Last Name<br />
Doctor’s First Name<br />
Doctor’s Phone #<br />
ALLERGY/HEALTH INFORMATION: COMPLETE ONLY IF CHANGED OR NOT PREVIOUSLY REPORTED<br />
Allergies: None Aspirin Cephalosporin Codeine Erythromycin Peanuts Penicillin<br />
Sulfa<br />
O<strong>the</strong>r:<br />
Conditions: Arthritis Asthma Diabetes Acid Reflux Glaucoma Heart Problem<br />
High Blood Pressure High Cholesterol Migraine Osteoporosis Prostate Issues Thyroid<br />
O<strong>the</strong>r:<br />
2nd PERSON ORDERING A PRESCRIPTION<br />
N I C K N A M E<br />
Your E-mail:<br />
Gender: M F<br />
Easy open caps Print in Spanish<br />
Suffix<br />
(JR,SR)<br />
Date <strong>of</strong> Birth:<br />
MM-DD-YYYY<br />
Date <strong>new</strong> prescription written:<br />
Last Name First Name MI<br />
Please fold here<br />
Please fold here<br />
* WEB *<br />
Doctor’s Last Name<br />
Doctor’s First Name<br />
Doctor’s Phone #<br />
ALLERGY/HEALTH INFORMATION: COMPLETE ONLY IF CHANGED OR NOT PREVIOUSLY REPORTED<br />
Allergies: None Aspirin Cephalosporin Codeine Erythromycin Peanuts Penicillin<br />
Sulfa<br />
O<strong>the</strong>r:<br />
Conditions: Arthritis Asthma Diabetes Acid Reflux Glaucoma Heart Problem<br />
High Blood Pressure High Cholesterol Migraine Osteoporosis Prostate Issues Thyroid<br />
O<strong>the</strong>r:<br />
Special Instructions:<br />
PAYMENT INFORMATION: Select one payment method below.<br />
Electronic Check Processing (Please pre-register at Caremark.com or call Customer Care)<br />
Bill Me Later ® (Subject to credit approval. Please pre-register at Caremark.com or call Customer Care)<br />
Credit/Debit Card (VISA, MasterCard, Discover or American Express)<br />
Charge most recently used credit card<br />
Charge <strong>new</strong>/updated credit/debit card (provide info below)<br />
Exp. Date<br />
MMDD<br />
Check/Money Order: Amount $<br />
.<br />
Make check or money order payable to CVS Caremark and<br />
write your ID# on <strong>the</strong> check/money order. Returned checks<br />
will be subject to a fee <strong>of</strong> up to $40, depending on state<br />
law.<br />
The selected payment method (unless paying by check) will<br />
be charged for future orders, unless a different form <strong>of</strong><br />
payment is provided. It will also be charged for any<br />
outstanding balance due.<br />
Fill in oval if you DO NOT want <strong>the</strong> selected payment<br />
method to be automatically charged for future orders.<br />
PGH-WB-MOF-1208<br />
Credit Card Holder Signature/Date<br />
REGULAR DELIVERY IS FREE<br />
(Allow up to 10 days for delivery)<br />
Fill in oval for faster delivery:<br />
2nd Business Day $17 per order<br />
Next Business Day $23 per order<br />
(Charges subject to change)<br />
Faster delivery options only affect shipping time,<br />
not processing time and can only be sent to a<br />
street address, not a P.O. box.<br />
Please fold here
14423-0808<br />
STANDARD<br />
Important!<br />
STEP 1<br />
Prescription Reimbursement Claim Form<br />
* Always allow up to 30 days from <strong>the</strong> time you send this form until <strong>the</strong> time you receive <strong>the</strong> response to<br />
allow for mail time plus claims processing.<br />
* Keep a copy <strong>of</strong> all documents submitted for your records.<br />
* Do not staple or tape receipts or attachments to this form.<br />
Card Holder/Patient Information<br />
Card Holder Information<br />
Identification Number (refer to your prescription card)<br />
This section must be fully completed to ensure proper reimbursement <strong>of</strong> your claim.<br />
Group No./Group Name<br />
Name (Last Name) (First Name) (MI)<br />
Address<br />
City State Zip<br />
Patient Information–Use a separate claim form for each patient.<br />
Name (Last Name) (First Name) (MI)<br />
Date <strong>of</strong> Birth Male Female<br />
Phone Number<br />
Relationship to Primary member<br />
Member Spouse Child O<strong>the</strong>r ____________<br />
O<strong>the</strong>r Insurance Information<br />
COB (Coordination <strong>of</strong> Benefits)<br />
Are any <strong>of</strong> <strong>the</strong>se medicines being taken for an on-<strong>the</strong>-job injury? ❍ Yes ❍ No<br />
Is <strong>the</strong> medicine covered under any o<strong>the</strong>r group insurance? ❍ Yes ❍ No<br />
If yes, is o<strong>the</strong>r coverage: ❍ Primary ❍ Secondary<br />
If o<strong>the</strong>r coverage is Primary, include <strong>the</strong> explanation <strong>of</strong> <strong>benefits</strong> (EOB) with this form.<br />
Name <strong>of</strong> Insurance Company___________________________ ID #__________________<br />
Important! A signature is REQUIRED<br />
NOTICE<br />
Any person who knowingly and with intent to defraud any insurance company or o<strong>the</strong>r person files an application for<br />
insurance or statement <strong>of</strong> claim containing any materially false information or conceals for <strong>the</strong> purpose <strong>of</strong> misleading<br />
information concerning any fact material <strong>the</strong>reto commits a fraudulent insurance act, which is a crime and subjects<br />
such person to criminal and civil penalties.<br />
I certify that I (or my eligible dependent) have received <strong>the</strong> medicine described herein and that <strong>the</strong> plan participant<br />
named is eligible for prescription <strong>benefits</strong>. I also certify that <strong>the</strong> medicine received is not for treatment <strong>of</strong> an on-<strong>the</strong>job<br />
injury or covered under ano<strong>the</strong>r benefit plan. I certify that I have read and understood this form, and that all <strong>the</strong><br />
information entered on this form is true and correct.<br />
x<br />
Signature <strong>of</strong> Plan Participant<br />
Date<br />
(Over)
STEP 2<br />
Submission Requirements:<br />
You MUST include all orginal receipts in order for your claim to process. Cash register receipts will only be accepted for<br />
diabetic supplies. The minimum information required is:<br />
• Patient Name • Prescription Number • Medicine NDC number<br />
• Date <strong>of</strong> Fill • Metric Quantity • Days Supply<br />
• Total Charge • Pharmacy Name and Address or Pharmacy NABP Number<br />
If Foreign Claim: Country:_______________ Currency:_______________<br />
Amount:_______________<br />
STEP 3<br />
Mailing Instructions:<br />
RXBIN:<br />
XXXXX<br />
RXPCN: CRK<br />
RXGRP: XXXXX<br />
ISSUER: (80840)<br />
The RXBIN # is located on front <strong>of</strong> your<br />
CVS Caremark Prescription ID card. Please see<br />
highlighted area to <strong>the</strong> left for reference. Match<br />
your RXBIN # to <strong>the</strong> addresses below.<br />
ID<br />
Name<br />
RXBIN # 610415 mail to:<br />
CVS Caremark<br />
P.O. Box 52116<br />
Phoenix, Arizona 85072-2116<br />
RXBIN # 004336 mail to:<br />
RXBIN # 610029 mail to:<br />
CVS Caremark<br />
P.O. Box 52136<br />
Phoenix, Arizona 85072-2136<br />
CVS Caremark<br />
P.O. Box 52196<br />
Phoenix, Arizona 85072-2196<br />
RXBIN # 610474 , 610468 , 004245 or 610449 mail to:<br />
CVS Caremark<br />
P.O. Box 52010<br />
Phoenix, Arizona 85072-2010<br />
IMPORTANT REMINDER<br />
To avoid having to submit a paper claim form:<br />
• Always have your card available at time <strong>of</strong> purchase<br />
• Always use pharmacies within your network<br />
• Use medication from your formulary list.<br />
• If problems are encountered at <strong>the</strong> pharmacy, call <strong>the</strong> number on <strong>the</strong> back <strong>of</strong> your card .
Section V<br />
When Group Health<br />
Benefits End
ARCHDIOCESE OF NEW YORK<br />
BENEFITS TRANSFER, TERMINATION AND REINSTATEMENT TRANSMITTAL<br />
This form is designed to provide a simple and fast method <strong>of</strong> reporting terminations, transfers & reinstatements. It should be<br />
submitted within 10 days <strong>of</strong> an employee’s/dependent’s status change date in order to ensure that <strong>the</strong> benefit records reflect <strong>the</strong><br />
most current membership status adjustment on <strong>the</strong> next premium billing. Employers should not wait until paying <strong>the</strong> premiums to<br />
report <strong>the</strong>se status adjustments. Employers must keep copies <strong>of</strong> transmittals for <strong>the</strong>ir records.<br />
Date Last Worked: _________<br />
Benefit End Date: _________<br />
Benefit Start Date: _________<br />
Employee Name:________________________________________ SSN________________________ Division Code________<br />
Dependent Name:_______________________________________ SSN________________________ Division Code________<br />
Dependent Name:_______________________________________ SSN________________________ Division Code________<br />
New Institution Name/Institution Number (If transfer)_______________________________________________________<br />
Transaction Type: _______ Reason: ________ Coverage(s) being transferred, terminated or reinstated: _________<br />
(See codes below) (See codes below) (See codes below)<br />
Reason for Termination: Voluntary Termination Involuntary Termination (IMPORTANT – This Section Must Be Completed)<br />
Priest & Religious transfers only: New Home Address__________________________________________________________<br />
__________________________________________________________<br />
Telephone __________________________________________________________<br />
Preparer’s Signature______________________________________________________________________ Date__________________<br />
Preparer Print Name______________________________________________________________________<br />
Institution Name/ Inst. Number __________________________________ Address__________________________________________<br />
__________________________________________________________ Telephone_____________________________________<br />
Refer all questions concerning this form to Employee Benefit Connections, 212.371.1000, Ext. 3060, Fax 212.644.0690.<br />
TR<br />
TE<br />
TD<br />
TI<br />
RE<br />
RD<br />
RI<br />
Transaction Type<br />
(Code descriptions)<br />
Transfer employee’s & dep. coverage<br />
Terminate employee’s & dependents’<br />
coverage<br />
Terminate all dependents coverage<br />
Terminate single dependent coverage<br />
Reinstate employee’s coverage<br />
Reinstate all dependents coverage<br />
Reinstate single dependent coverage<br />
ET<br />
RW<br />
SE<br />
DV<br />
IC<br />
MD<br />
DE<br />
TOC<br />
LOC<br />
NYS<br />
IT<br />
Reason<br />
(Code descriptions)<br />
Termination <strong>of</strong> Employment<br />
Reduction in Work Hours<br />
Separation<br />
Divorce<br />
Ineligible Child<br />
Medicare<br />
Death<br />
Transferred to O<strong>the</strong>r<br />
Coverage<br />
Loss <strong>of</strong> o<strong>the</strong>r coverage<br />
NYS Continuation<br />
Institution Transfer<br />
Coverage(s) being transferred, termed or<br />
reinstated<br />
(Code descriptions)<br />
HPC Health Plan Coverage<br />
MSP<br />
LB<br />
ADD<br />
DVI<br />
DPPO1<br />
DPPO2<br />
DEN<br />
ALL<br />
LOCAL ADMINISTRATOR, return this form to:<br />
Employee Benefit Connections<br />
1011 First Ave, Suite 1679<br />
New York, NY 10022<br />
Telephone: 212.371.1000, Ext. 3060, Fax: 212.644.0690<br />
Medicare Supplemental Plan<br />
Life Benefit<br />
AD&D<br />
Davis Vision<br />
CIGNA Dental/Opt 1<br />
CIGNA Dental/Opt 2<br />
CIGNA Dental Indemnity<br />
Transfer, Terminate, Reinstate<br />
all <strong>benefits</strong><br />
Contact us: ebc@archny.org<br />
- 22 - Web Page: www.archny.org/<strong>benefits</strong><br />
Revised April 2009
INFORMATION GUIDELINES FOR<br />
GROUP HEALTHBENEFITS FOR<br />
EMPLOYEES SEPARATING FROM SERVICE<br />
NEW YORK STATE CONTINUATION<br />
OF GROUP HEALTH BENEFITS COVERAGE<br />
• Eligible employees, who are separating from <strong>the</strong> Archdiocese and not eligible for early retirement, may continue<br />
<strong>the</strong>ir group health insurance under <strong>the</strong> New York State Continuation Law. The continuation period for an<br />
employee with his/her qualified dependents is 18 months.<br />
• Under <strong>the</strong> Uniformed Services Employment and Reemployment Rights Act (USERRA), if an employee is called<br />
to active duty beyond 30 days, he/she and/or <strong>the</strong>ir covered dependents can elect to continue <strong>the</strong> health <strong>benefits</strong> for<br />
up to 24 months during <strong>the</strong> employee’s military service. This is effective for elections made on or after December<br />
10, 2004.<br />
• All employers must provide employees with notice <strong>of</strong> <strong>the</strong>ir rights, <strong>benefits</strong> and obligations under <strong>the</strong> Uniformed<br />
Services Employment and Reemployment Rights Act (USERRA). The notice requirement can be satisfied by<br />
posting a notice in <strong>the</strong> same location where o<strong>the</strong>r required notices are customarily posted. Please refer to <strong>the</strong><br />
following page for a copy.<br />
• Qualified dependents include <strong>the</strong> spouse, dependent children under age 19 or dependent children who are full time<br />
students under <strong>the</strong> age <strong>of</strong> 25. Children born to or placed for adoption with a covered employee during <strong>the</strong> New<br />
York Continuance period are also considered qualified dependents.<br />
• Covered dependents are eligible for continuation <strong>of</strong> <strong>the</strong>ir group health coverage for 36 months if one <strong>of</strong> <strong>the</strong><br />
following events occurs: <strong>the</strong> employee’s death; change in dependent’s status when child reaches age 19 or no<br />
longer a college student; divorce or legal separation from spouse; when employee becomes entitled to Medicare.<br />
• The spouse <strong>of</strong> <strong>the</strong> employee eligible for Medicare may continue health coverage until he/she becomes eligible for<br />
Medicare.<br />
• Disabled employees are eligible for continuation coverage up to 29 months provided <strong>the</strong> Social Security<br />
Administration determines that such individual was disabled at termination <strong>of</strong> <strong>the</strong> group health insurance or at any<br />
time during <strong>the</strong> first sixty days <strong>of</strong> <strong>the</strong> continuation coverage. Documentation <strong>of</strong> such disability must be provided<br />
to <strong>the</strong> Archdiocese within 60 days <strong>of</strong> Social Security’s determination.<br />
• Continuation coverage is not available to individuals entitled to Medicare or become covered under ano<strong>the</strong>r group<br />
health plan that has no limitations or exclusions with respect to any pre-existing conditions that <strong>the</strong> employee or<br />
his/her dependents may have.<br />
• The employer is to notify Employee Benefit Connections, in writing, within 30 days from <strong>the</strong> date <strong>of</strong><br />
termination by completing a “Benefits Transfer, Termination, and Reinstatement Transmittal”, and submit<br />
<strong>the</strong> completed Form to Employee Benefit Connections. The form must list <strong>the</strong> health insurance termination<br />
date.<br />
• Beginning December 1, 2007, Employee Benefit Connections will, upon notice, administer <strong>the</strong> Group Health<br />
Continuation Benefit, and on behalf <strong>of</strong> <strong>the</strong> employer, will complete and sign Part I <strong>of</strong> <strong>the</strong> Group Health Benefit<br />
Continuation Election Form, and forward to <strong>the</strong> individual losing coverage<br />
• If an employee or a qualified dependent elect <strong>the</strong> continuation coverage, <strong>the</strong> application must be submitted to<br />
Employee Benefit Connections within <strong>the</strong> later <strong>of</strong> 60 days <strong>of</strong> <strong>the</strong> group health coverage termination or 60 days <strong>of</strong><br />
<strong>the</strong> receipt <strong>of</strong> <strong>the</strong> Notice <strong>of</strong> Group Insurance Continuance Eligibility letter. THE FIRST MONTH’S<br />
PREMIUM PAYMENT MUST ACCOMPANY THE GROUP HEALTH CONTINUATION ELECTION<br />
FORM.<br />
- 23 -
★<br />
★<br />
REEMPLOYMENT RIGHTS<br />
YOUR RIGHTS UNDER USERRA<br />
THE UNIFORMED SERVICES EMPLOYMENT<br />
AND REEMPLOYMENT RIGHTS ACT<br />
USERRA protects <strong>the</strong> job rights <strong>of</strong> individuals who voluntarily or involuntarily leave employment positions to undertake<br />
military service or certain types <strong>of</strong> service in <strong>the</strong> National Disaster Medical System. USERRA also prohibits employers<br />
from discriminating against past and present members <strong>of</strong> <strong>the</strong> uniformed services, and applicants to <strong>the</strong> uniformed services.<br />
HEALTH INSURANCE PROTECTION<br />
You have <strong>the</strong> right to be reemployed in your civilian job if you leave that<br />
job to perform service in <strong>the</strong> uniformed service and:<br />
✩<br />
✩<br />
✩<br />
✩<br />
you ensure that your employer receives advance written or verbal<br />
notice <strong>of</strong> your service;<br />
you have five years or less <strong>of</strong> cumulative service in <strong>the</strong> uniformed<br />
services while with that particular employer;<br />
you return to work or apply for reemployment in a timely manner<br />
after conclusion <strong>of</strong> service; and<br />
you have not been separated from service with a disqualifying<br />
discharge or under o<strong>the</strong>r than honorable conditions.<br />
If you are eligible to be reemployed, you must be restored to <strong>the</strong> job and<br />
<strong>benefits</strong> you would have attained if you had not been absent due to<br />
military service or, in some cases, a comparable job.<br />
RIGHT TO BE FREE FROM DISCRIMINATION AND RETALIATION<br />
If you:<br />
✩ are a past or present member <strong>of</strong> <strong>the</strong> uniformed service;<br />
✩ have applied for membership in <strong>the</strong> uniformed service; or<br />
✩ are obligated to serve in <strong>the</strong> uniformed service;<br />
<strong>the</strong>n an employer may not deny you:<br />
✩ initial employment;<br />
✩ reemployment;<br />
✩ retention in employment;<br />
✩ promotion; or<br />
✩ any benefit <strong>of</strong> employment<br />
because <strong>of</strong> this status.<br />
✩<br />
✩<br />
If you leave your job to perform military service, you have <strong>the</strong> right<br />
to elect to continue your existing employer-based health plan<br />
coverage for you and your dependents for up to 24 months while in<br />
<strong>the</strong> military.<br />
Even if you don't elect to continue coverage during your military<br />
service, you have <strong>the</strong> right to be reinstated in your employer's<br />
health plan when you are reemployed, generally without any waiting<br />
periods or exclusions (e.g., pre-existing condition exclusions) except<br />
for service-connected illnesses or injuries.<br />
ENFORCEMENT<br />
✩<br />
✩<br />
✩<br />
✩<br />
The U.S. Department <strong>of</strong> Labor, Veterans Employment and Training<br />
Service (VETS) is authorized to investigate and resolve complaints<br />
<strong>of</strong> USERRA violations.<br />
For assistance in filing a complaint, or for any o<strong>the</strong>r information on<br />
USERRA, contact VETS at 1-866-4-USA-DOL or visit its website at<br />
http://www.dol.gov/vets. An interactive online USERRA Advisor can<br />
be viewed at http://www.dol.gov/elaws/userra.htm.<br />
If you file a complaint with VETS and VETS is unable to resolve it,<br />
you may request that your case be referred to <strong>the</strong> Department<br />
<strong>of</strong> Justice or <strong>the</strong> Office <strong>of</strong> Special Counsel, as applicable, for<br />
representation.<br />
You may also bypass <strong>the</strong> VETS process and bring a civil action<br />
against an employer for violations <strong>of</strong> USERRA.<br />
In addition, an employer may not retaliate against anyone assisting in<br />
<strong>the</strong> enforcement <strong>of</strong> USERRA rights, including testifying or making a<br />
statement in connection with a proceeding under USERRA, even if that<br />
person has no service connection.<br />
The rights listed here may vary depending on <strong>the</strong> circumstances. The text <strong>of</strong> this notice was prepared by VETS, and may be viewed on <strong>the</strong> internet at<br />
this address: http://www.dol.gov/vets/programs/userra/poster.htm. Federal law requires employers to notify employees <strong>of</strong> <strong>the</strong>ir rights under USERRA,<br />
and employers may meet this requirement by displaying <strong>the</strong> text <strong>of</strong> this notice where <strong>the</strong>y customarily place notices for employees.<br />
U.S. Department <strong>of</strong> Labor<br />
1-866-487-2365<br />
U.S. Department <strong>of</strong> Justice<br />
Office <strong>of</strong> Special Counsel 1-800-336-4590<br />
Publication Date—July 2008
(Sample Letter)<br />
NOTICE TO MEMBER LOSING COVERAGE<br />
TO:<br />
FROM :<br />
RE:<br />
DATE:<br />
____________________________________________________________________<br />
(Member’s Name)<br />
____________________________________________________________________<br />
(Employer’s Name)<br />
Continuation <strong>of</strong> Health Coverage<br />
____________________________________________________________________<br />
Enclosed is <strong>the</strong> information you requested regarding <strong>the</strong> continuation <strong>of</strong> your or your qualified<br />
dependent’s group coverage. As your employer, we have included <strong>the</strong> termination date on <strong>the</strong><br />
enclosed Notice <strong>of</strong> Group Health Benefit Continuance Eligibility letter. We have also<br />
completed and signed Part I <strong>of</strong> <strong>the</strong> enclosed Group Health Benefit Continuation Election<br />
Form.<br />
As mentioned in <strong>the</strong> enclosed material, if you or your qualified dependent want to apply for<br />
continuation <strong>of</strong> <strong>the</strong> group health coverage, <strong>the</strong> first month’s premium must be mailed along with<br />
<strong>the</strong> enclosed Group Health Continuation Election Form to:<br />
Employee Benefits Connections<br />
1011 First Avenue – Room 1679<br />
New York, NY 10022<br />
The checks must be made payable to <strong>the</strong> Archdiocese <strong>of</strong> New York. Employee Benefits<br />
Connections will administer <strong>the</strong> record keeping <strong>of</strong> <strong>the</strong> continuation <strong>of</strong> health coverage. If you or<br />
your dependents have any questions regarding enrollment or premium billing issues, please<br />
contact Employee Benefit Connections at (212) 371-1000, Ext. 3060 for assistance.<br />
Enclosure<br />
-24-
ARCHDIOCESE OF NEW YORK<br />
NOTICE OF GROUP INSURANCE CONTINUANCE ELIGIBILITY<br />
This is to inform you that effective ________________________ your health insurance coverage under <strong>the</strong><br />
Archdiocese <strong>of</strong> New York Group Insurance Plan will be discontinued.<br />
Under <strong>the</strong> New York State Continuation Law, you and your covered dependents are eligible for Continuation <strong>of</strong><br />
Health coverage provided your employment terminated or because you are transferred to an ineligible class <strong>of</strong><br />
employee. You and/or your covered dependents can elect to continue coverage under <strong>the</strong> plan for up to 18<br />
months from <strong>the</strong> date your coverage terminated, provided you pay <strong>the</strong> required premiums within <strong>the</strong> balance due<br />
period.<br />
Under <strong>the</strong> Uniformed Services Employment and Reemployment Rights Act, if you are called to active duty<br />
beyond 30 days, you and/or your covered dependents can elect to continue health coverage under <strong>the</strong> plan for up<br />
to 24 months during your military service.<br />
Covered dependents include a child born to or placed for adoption with a covered employee during <strong>the</strong> period <strong>of</strong><br />
New York Continuance. Qualified beneficiaries may elect to change <strong>the</strong>ir coverage upon <strong>the</strong> birth or adoption<br />
<strong>of</strong> a child while under continuance.<br />
Covered dependents are eligible for coverage for up to 36 months if one <strong>of</strong> <strong>the</strong> following events occurs:<br />
‣ <strong>the</strong> Employee’s death,<br />
‣ change in dependent status (for example, child reaches limiting age or is no longer a full-time student),<br />
‣ divorce or legal separation, or<br />
‣ <strong>the</strong> dependent would o<strong>the</strong>rwise lose coverage when <strong>the</strong> employee becomes entitled to Medicare.<br />
When <strong>the</strong> employee becomes eligible for Medicare, <strong>the</strong> spouse may continue coverage until such time he/she<br />
becomes eligible for Medicare or until <strong>the</strong> allowed 36 months <strong>of</strong> coverage lapses, whichever comes first.<br />
Documentation that <strong>the</strong> spouse is not eligible for Medicare is to be sent to Employee Benefit Connections within<br />
31 days <strong>of</strong> <strong>the</strong> date <strong>the</strong> employee becomes Medicare eligible.<br />
Disabled individuals are eligible for up to 29 months <strong>of</strong> continuation coverage provided <strong>the</strong> Social Security<br />
Administration determines that <strong>the</strong> individual was disabled at termination or at any time during <strong>the</strong> first sixty<br />
days <strong>of</strong> continuation coverage. Disabled individuals must provide documentation <strong>of</strong> <strong>the</strong> determination <strong>of</strong><br />
disability to Employee Benefit Connections within 60 days <strong>of</strong> Social Security’s determination.<br />
- 25 -<br />
Revised 01/2008
Continuation coverage is not available to you if you are entitled to Medicare or become covered under ano<strong>the</strong>r<br />
group health plan that has no limitations or exclusions with respect to any pre-existing conditions that you or<br />
your dependents may have.<br />
If you decide to elect this coverage, you must submit your applications within <strong>the</strong> later <strong>of</strong> 60 days <strong>of</strong> your<br />
coverage termination or 60 days <strong>of</strong> your receipt <strong>of</strong> this letter. You must also at that time submit your first<br />
premium payment. Note: Subsequent premiums are due on <strong>the</strong> first <strong>of</strong> each month. If you are submitting<br />
your application later than 45 days from <strong>the</strong> effective date <strong>of</strong> your Continuation <strong>of</strong> Coverage, you must<br />
submit payment for all months due with your application.<br />
Your continuation coverage will terminate when one <strong>of</strong> <strong>the</strong> following occurs:<br />
‣ <strong>the</strong> period <strong>of</strong> continuation coverage has elapsed,<br />
‣ coverage under <strong>the</strong> policy would have o<strong>the</strong>rwise ended,<br />
‣ you do not pay <strong>the</strong> monthly premium within <strong>the</strong> 31-day grace period,<br />
‣ <strong>the</strong> Archdiocese <strong>of</strong> New York terminates and does not replace <strong>the</strong> plan,<br />
‣ (If you lose your disability status) ei<strong>the</strong>r at <strong>the</strong> end <strong>of</strong> <strong>the</strong> original 29-month period or 31 days after Social<br />
Security determines that you are no longer disabled.<br />
The current rates and <strong>the</strong> coverage options are indicated on <strong>the</strong> enclosed enrollment form. The rates are subject<br />
to change at any time and may also change on <strong>the</strong> first <strong>of</strong> a given month if warranted by a plan change. When<br />
<strong>benefits</strong> end, <strong>the</strong>re is no conversion option.<br />
If you elect continuation coverage, please complete <strong>the</strong> attached election form and return it to Employee Benefit<br />
Connections within 60 days. Please keep in mind that if you decline continuation coverage, or if you do not<br />
elect coverage within <strong>the</strong> 60-day notification period, you will no longer be entitled to this benefit. Your checks<br />
must be made payable to <strong>the</strong> Archdiocese <strong>of</strong> New York. You must submit your enrollment form along with<br />
your initial payment to:<br />
Employee Benefit Connections<br />
1011 First Avenue – Room 1679<br />
New York, NY 10022<br />
All subsequent monthly premiums must be submitted to:<br />
Employee Benefit Connections<br />
1011 First Avenue – Room 1679<br />
New York, NY 10022<br />
Please call (212) 371-1000, Ext. 3060 to speak to a representative if you have questions concerning your<br />
premium billing.<br />
Revised 01/2008
Archdiocese <strong>of</strong> New York<br />
Group Health Continuation Election Form<br />
January 1, _____ to December 31, _____<br />
Employee Name:<br />
PART 1: To be completed by Employer<br />
Gender:<br />
Male<br />
Female<br />
Social Security Number:<br />
Hire Date:<br />
Name and Address <strong>of</strong> Employer: Institution #:<br />
Qualified Event: Date <strong>of</strong> Event: Date Coverage Ends:<br />
Applicant (If O<strong>the</strong>r Than Employee) Name:<br />
Relationship to Employee:<br />
Gender:<br />
__ Male<br />
__ Female<br />
Date <strong>of</strong> Birth:<br />
12:00 a.m.<br />
____ Surviving Spouse ____ Former Spouse ____ Dependent Child<br />
UNITED HEALTHCARE PPO PLAN<br />
CONTINUATION MEDICAL COVERAGE TYPE<br />
Coverage Type: [ ] $______ [ ] $_______ [ ] $_______<br />
Single Two Person Family<br />
It is hereby certified that <strong>the</strong> above employee/applicant is eligible for <strong>the</strong> continuation <strong>of</strong> <strong>the</strong> type <strong>of</strong> coverage indicated<br />
above.<br />
Authorized Employer Representative’s Signature:___________________________________________________<br />
Employer’s Name______________________________________________ Date___________________________<br />
PART 2: To be completed by Person making <strong>the</strong> election. Please check <strong>the</strong> appropriate boxes below.<br />
I have read <strong>the</strong> NOTICE FOR CONTINUATION OF COVERAGE and understand that I have <strong>the</strong> option <strong>of</strong> changing my<br />
current coverage.<br />
__ I elect to continue my current medical coverage. (If you checked this section, please continue on <strong>the</strong> reverse side)<br />
__ I do not wish to continue any medical coverage. ________________________________________ Date__________<br />
(Please sign and date here and return to your employer if you checked<br />
this section)<br />
Revised 09/2007
Archdiocese <strong>of</strong> New York<br />
Group Health Continuation Election Form<br />
(Continued)<br />
PART 3: To be completed by Employee’s Spouse if Employee made election. Please check one <strong>of</strong> <strong>the</strong><br />
boxes below.<br />
I have read <strong>the</strong> NOTICE FOR CONTINUATION OF COVERAGE and have reviewed <strong>the</strong> election my<br />
spouse made above.<br />
____ I agree with <strong>the</strong> election made by my spouse.<br />
____ I do not wish to participate with <strong>the</strong> continuation <strong>of</strong> health coverage as elected by my spouse.<br />
Signature <strong>of</strong> Spouse:<br />
Date:<br />
PART 4: To be completed by Person making <strong>the</strong> election to continuation <strong>of</strong> health <strong>benefits</strong> coverage.<br />
Names <strong>of</strong> Persons to be<br />
covered (including<br />
Employee)<br />
Social Security<br />
Number<br />
Gender Date <strong>of</strong><br />
Birth<br />
Relationship to<br />
Employee (Self,<br />
Spouse or<br />
Dependent child)<br />
If covered by ano<strong>the</strong>r plan,<br />
give insurance company<br />
name and address and policy<br />
number.<br />
Name:<br />
PART 5: To be completed by Person making <strong>the</strong> election.<br />
Number and Street Address:<br />
City: State: Zip Code Country:<br />
Telephone Number:<br />
Note: Subsequent premiums are due on <strong>the</strong> first <strong>of</strong> each month. If you are submitting your application<br />
later than 45 days from <strong>the</strong> effective date <strong>of</strong> your Continuation <strong>of</strong> Coverage (shown on Page 1), you must<br />
submit payment for all months due with your application.<br />
Signature <strong>of</strong> Person making <strong>the</strong> election<br />
Date:<br />
Revised 09/2007
GROUP HEALTH BENEFITS FOR EMPLOYEES<br />
RETIRING FROM SERVICE PRIOR TO AGE 65<br />
RETIREE HEALTH BENEFITS PRIOR TO AGE 65<br />
• Eligible employees, who are retiring from <strong>the</strong> Archdiocese prior to age 65 and entitled to receive<br />
pension income, may elect to keep <strong>the</strong>ir group health coverage at full cost up to age 65. At such<br />
time <strong>the</strong> employees may elect <strong>the</strong> United Healthcare Medicare Supplemental Plan.<br />
• The early retirees must have completed 10 years <strong>of</strong> full time employment and be at least 55 years<br />
old (55/10 rule).<br />
• Early retirees will be responsible for paying <strong>the</strong> monthly premiums to <strong>the</strong>ir former employers.<br />
• The retirees should complete Group Health Benefits Election for Retirees form and <strong>the</strong> Health<br />
Benefit Plan Enrollment & Change Form. These forms will be sent to Employee Benefit<br />
Connections to process <strong>the</strong> status code change to <strong>the</strong> appropriate retiree division code:<br />
103 - Bargaining Lay Faculty Members <strong>of</strong> <strong>the</strong> Association <strong>of</strong> Catholic School (Terminate at 65)<br />
104 – Bargaining Lay Faculty Members <strong>of</strong> <strong>the</strong> Catholic High School Association (Terminate at 65)<br />
114 – Non-bargaining lay employees under <strong>the</strong> Child Care Agencies (Prior to age 65)<br />
135 – Non-bargaining lay employee (Prior to age 65)<br />
- 26 -
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefit Election for<br />
Early Retired Lay Bargaining Faculty Members<br />
Effective January 1, _____ through December 31, _____<br />
Name__________________________________________________________ Soc. Security No.______________________<br />
Address_____________________________________________ City______________________ State______ Zip_________<br />
Institution_________________________________________________________ Institution/Division Number __________<br />
Month and Year <strong>of</strong> Retirement____________________________ Home Telephone Number_________________________<br />
Select one <strong>of</strong> <strong>the</strong> following coverage options for <strong>the</strong> remainder <strong>of</strong> <strong>the</strong> current benefit plan year. Only those employees and<br />
dependents, who are presently covered under <strong>the</strong> Archdiocese medical plan on your retirement date, are eligible. Retired Lay<br />
Bargaining Faculty members age 65 and older are not eligible to continue coverage. Please refer to your contract or<br />
consult with your local personnel administrator.<br />
United Healthcare Plan<br />
Monthly Rates: Retiree Only Retiree (Pre-65) + Retiree (Pre-65) Retiree (Pre-65)<br />
(Select One) (Pre-65) One Dependent + One Dependent + Two or More<br />
(Pre-65) (Post-65) Dependents<br />
[ ] $_____ [ ] $_______ [ ] $_______ [ ] $______<br />
Waiver <strong>of</strong> Coverage<br />
[ ] I elect to waive <strong>the</strong> retiree health coverage under this plan.<br />
I understand that I can only change my election when a qualifying life event applies during <strong>the</strong> current benefit plan year.<br />
I understand that this election is effective during <strong>the</strong> current benefit plan year.<br />
I certify that all <strong>of</strong> <strong>the</strong> information contained on this coverage election form and my application is true. I agree to pay <strong>the</strong><br />
monthly premium for <strong>the</strong> plan selected for <strong>the</strong> remainder <strong>of</strong> <strong>the</strong> policy year.<br />
Signed: ____________________________________________________________________<br />
Date:<br />
____________________________________________________________________<br />
Retiree: Return this form to you former local administrato<br />
Local Administrator: RETAIN THIS FORM IN YOUR FILES FOR FUTURE REFERENCE<br />
Revised 09/2007
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefits Election for Retired Lay Employees<br />
Effective January 1, _____ through December 31, _____<br />
Name__________________________________________________________ Soc. Security No.______________________<br />
Address_____________________________________________ City______________________ State______ Zip_________<br />
Institution_________________________________________________________ Institution/Division Number __________<br />
Month and Year <strong>of</strong> Retirement____________________________ Home Telephone Number_________________________<br />
Select one <strong>of</strong> <strong>the</strong> following coverage options for <strong>the</strong> remainder <strong>of</strong> <strong>the</strong> current benefit plan year. Only those employees and<br />
dependents, who are presently covered under <strong>the</strong> Archdiocese medical plan on your retirement date, are eligible.<br />
United Healthcare Plan<br />
Monthly Rates: Single Two Person Single Two Person Two Person Family Coverage<br />
(Select One) 65 & Over 65 & Over Under 65 Under 65 1 under 65 &<br />
1 over 65<br />
[ ] $_____ [ ] $______ [ ] $______ [ ] $______ [ ] $______ [ ] $______<br />
Waiver <strong>of</strong> Coverage<br />
[ ] I elect to waive <strong>the</strong> retiree health coverage under this plan.<br />
I understand that I can only change my election when a qualifying life event applies during <strong>the</strong> current benefit plan year.<br />
I understand that <strong>the</strong> rates are subject to change on <strong>the</strong> first <strong>of</strong> any given month if warranted by <strong>the</strong> plan.<br />
I certify that all <strong>of</strong> <strong>the</strong> information contained on this coverage election form and my application is true. I agree to pay <strong>the</strong><br />
monthly premium for <strong>the</strong> plan option selected for <strong>the</strong> remainder <strong>of</strong> <strong>the</strong> current benefit plan year.<br />
Signed: ____________________________________________________________________<br />
Date:_______________________________________<br />
Retiree: Return this form to your former local administrator<br />
Local Administrator: RETAIN THIS FORM IN YOUR FILES FOR FUTURE REFERENCE<br />
Revised September 11, 2007
GROUP HEALTH BENEFITS FOR EMPLOYEES<br />
RETIRING FROM SERVICE AT AGE 65 OR LATER<br />
RETIREE HEALTH BENEFITS AT AGE 65 OR LATER<br />
• Eligible employees, who are retiring from <strong>the</strong> Archdiocese at age 65 or later, may elect to<br />
apply United Healthcare Medicare Supplemental Plan at full cost <strong>of</strong> <strong>the</strong> premium.<br />
• The retirees should complete <strong>the</strong> Group Health Benefit Election for Retirees form and <strong>the</strong><br />
Health Benefit Plan Enrollment & Change Form. These forms must be sent to Employee<br />
Benefit Connections to process <strong>the</strong> status change to <strong>the</strong> appropriate retiree division code:<br />
108 – Aged 65+ spouses <strong>of</strong> early retired lay bargaining faculty members <strong>of</strong> parish schools<br />
109 – Aged 65+ spouses <strong>of</strong> early retired lay bargaining faculty members <strong>of</strong> CHSA<br />
113 – Non-bargaining lay employees under <strong>the</strong> Child Care Agencies<br />
131 – Non-bargaining lay employees<br />
• In addition, a copy <strong>of</strong> <strong>the</strong> red, white & blue Medicare card must accompany <strong>the</strong>se forms.<br />
• The retirees will be responsible for <strong>the</strong> monthly premium payments to <strong>the</strong>ir former employers.<br />
• Medical <strong>benefits</strong> will be coordinated between Medicare as <strong>the</strong> primary coverage and <strong>the</strong><br />
United Healthcare Medicare Supplemental Plan as secondary coverage.<br />
Note: Bargaining Lay Faculty Members and <strong>the</strong>ir dependents are not eligible to <strong>the</strong> retiree group health<br />
when <strong>the</strong> Early Retired Bargaining Lay Faculty Members turns age 65.<br />
- 27 -
ARCHDIOCESE OF NEW YORK<br />
Group Health Benefits Election for Retired Lay Employees<br />
Effective January 1, _____ through December 31, _____<br />
Name__________________________________________________________ Soc. Security No.______________________<br />
Address_____________________________________________ City______________________ State______ Zip_________<br />
Institution_________________________________________________________ Institution/Division Number __________<br />
Month and Year <strong>of</strong> Retirement____________________________ Home Telephone Number_________________________<br />
Select one <strong>of</strong> <strong>the</strong> following coverage options for <strong>the</strong> remainder <strong>of</strong> <strong>the</strong> current benefit plan year. Only those employees and<br />
dependents, who are presently covered under <strong>the</strong> Archdiocese medical plan on your retirement date, are eligible.<br />
United Healthcare Plan<br />
Monthly Rates: Single Two Person Single Two Person Two Person Family Coverage<br />
(Select One) 65 & Over 65 & Over Under 65 Under 65 1 under 65 &<br />
1 over 65<br />
[ ] $_____ [ ] $______ [ ] $______ [ ] $______ [ ] $______ [ ] $______<br />
Waiver <strong>of</strong> Coverage<br />
[ ] I elect to waive <strong>the</strong> retiree health coverage under this plan.<br />
I certify that all <strong>of</strong> <strong>the</strong> information contained on this coverage election form and my application is true. I agree to pay <strong>the</strong><br />
monthly premium for <strong>the</strong> plan option selected for <strong>the</strong> remainder <strong>of</strong> <strong>the</strong> current benefit plan year.<br />
Signed: ____________________________________________________________________<br />
Date:_______________________________________<br />
Retiree: Return this form to your former local administrator<br />
Local Administrator: RETAIN THIS FORM IN YOUR FILES FOR FUTURE REFERENCE<br />
Revised September 11, 2007
GUIDELINES FOR COMPLETING NOTICE OF BENEFIT STATUS<br />
DUE TO SEPARATION FROM EMPLOYMENT FORM<br />
The following form was developed to aid local administrators when reviewing various <strong>benefits</strong> at<br />
<strong>the</strong> time an employee is terminating employment.<br />
Ideally, we suggest that whenever possible, that <strong>the</strong> local administrator review this list in<br />
advance and prepare any necessary papers and forms, so that at <strong>the</strong> time <strong>of</strong> <strong>the</strong> Exit Interview,<br />
<strong>the</strong>y are prepared and <strong>the</strong> process should proceed with relative ease.<br />
Instructions For Completing Form:<br />
• Complete <strong>the</strong> top <strong>of</strong> <strong>the</strong> form by listing <strong>the</strong> terminating employee’s full legal name, <strong>the</strong> name<br />
<strong>of</strong> <strong>the</strong> institution (employer) and <strong>the</strong> institution-division number.<br />
• Insert <strong>the</strong> employee’s separation date on <strong>the</strong> next line.<br />
• Insert <strong>the</strong> termination date in <strong>the</strong> Group Medical Coverage section. The group medical<br />
benefit will terminate on <strong>the</strong> last date <strong>of</strong> <strong>the</strong> month in which <strong>the</strong> employee terminates<br />
employment.<br />
• Ask <strong>the</strong> terminating employee if <strong>the</strong>y wish to continue <strong>the</strong> group medical coverage for<br />
<strong>the</strong>mselves or <strong>the</strong>ir eligible dependents.<br />
• Employee Benefit Connections will mail <strong>the</strong> Group Health Continuation Election form to <strong>the</strong><br />
employee or eligible dependents, when <strong>the</strong>y receive from <strong>the</strong> institution (employer) <strong>the</strong><br />
BenefitsTransfer, Termination and Reinstatement Transmittal form to terminate group<br />
health <strong>benefits</strong> for an employee or a dependent. Employee Benefit Connections will also<br />
administer <strong>the</strong> continuance <strong>of</strong> <strong>the</strong> medical coverage. The employee will be instructed to<br />
return <strong>the</strong> completed and signed form to Employee Benefit Connections along with <strong>the</strong> first<br />
month’s premium.<br />
• Insert <strong>the</strong> termination date in <strong>the</strong> Group Life Insurance section. The group life insurance will<br />
terminate on <strong>the</strong> employee’s last day <strong>of</strong> employment at 12:00 (midnight).<br />
• In <strong>the</strong> Group Long Term Disability Insurance section, if your institution <strong>of</strong>fers this benefit,<br />
insert <strong>the</strong> termination date for this benefit. The group long term disability insurance will<br />
terminate on <strong>the</strong> employee’s last day <strong>of</strong> employment.<br />
• An authorized employer representative and <strong>the</strong> terminating employee must sign and date <strong>the</strong><br />
Notice <strong>of</strong> Benefits Status Due to Separation From Employment form on pages 1 and 2.<br />
The original copy <strong>of</strong> <strong>the</strong> form should be given to <strong>the</strong> employee and a copy should be retained<br />
in <strong>the</strong> employer’s <strong>of</strong>fice.<br />
- 28 - Revised 07/2009
____________________________________ _____________________________________ ____________<br />
Employee Name (Print) Employer (Institution) Institution-Div. #<br />
NOTICE OF BENEFIT STATUS DUE TO SEPARATION FROM EMPLOYMENT<br />
The following is a summary <strong>of</strong> your benefit coverage status as <strong>of</strong> your separation date:__________________<br />
(insert date)<br />
GROUP MEDICAL COVERAGE<br />
If you and/or your spouse and/or dependent child(ren) are not entitled to Medicare or covered as an employee or continue<br />
under ano<strong>the</strong>r group health plan you have <strong>the</strong> option to continue your group medical coverage(s) for up to eighteen (18)<br />
months. Additionally, <strong>the</strong> eighteen (18) month continuation period may be extended for an additional eleven (11) months (to<br />
<strong>the</strong> maximum <strong>of</strong> twenty-nine (29) months <strong>of</strong> continuation <strong>of</strong> coverage), if it is determined that <strong>the</strong> qualified beneficiary was<br />
disabled at any time during <strong>the</strong> first sixty (60) days <strong>of</strong> continuation <strong>of</strong> coverage. To qualify for <strong>the</strong> extension, <strong>the</strong><br />
determination <strong>of</strong> disability must be an <strong>of</strong>ficial determination made by <strong>the</strong> Social Security Administration and <strong>the</strong> plan<br />
administrator must be notified with <strong>the</strong> determination within sixty (60) days <strong>of</strong> <strong>the</strong> date <strong>of</strong> such determination.<br />
Covered dependents are eligible to continuation <strong>of</strong> group medical coverage for up to 36 months in <strong>the</strong> event <strong>of</strong> <strong>the</strong> employee’s death;<br />
change in dependent status (i.e. no longer a full time student; divorce or legal separation); dependent would o<strong>the</strong>rwise lose coverage when<br />
employee becomes eligible for Medicare. If you or your spouse, and/or dependent children wish to elect continuation <strong>of</strong> coverage, you<br />
must notify your local administrator in writing within 60 days from <strong>the</strong> date you would lose coverage as a result <strong>of</strong> a qualifying event or<br />
60 days from <strong>the</strong> date you receive this notice, whichever is later. In addition, you must pay <strong>the</strong> premiums within 45 days from <strong>the</strong> date <strong>of</strong><br />
election <strong>of</strong> continuation <strong>of</strong> coverage. Subsequent premiums are due on <strong>the</strong> first <strong>of</strong> each month. All premium payment checks should be<br />
made payable to <strong>the</strong> Archdiocese <strong>of</strong> New York and should be sent to:<br />
Employee Benefit Connections<br />
1011 First Ave, Suite 1679<br />
New York, NY 10022<br />
Your current single, family, or employee plus one medical coverage(s) will terminate on __________________________,<br />
unless you elect one <strong>of</strong> <strong>the</strong> following options:<br />
Do you elect continuation <strong>of</strong> your group medical coverage:<br />
Employee: Yes_______ No_________<br />
Spouse: Yes_______ No_________<br />
Dependent Child(ren) Yes_______ No_________<br />
If you have elected yes, you must complete and sign <strong>the</strong> Group Health Continuation Election Form, which will be mailed<br />
under separate cover.<br />
__________________________________________________________________________<br />
Authorized Employer Representative’s Signature<br />
______________________<br />
Date<br />
____________________________________________________________________________<br />
Employee/Member Signature<br />
____________________________________________________________________________<br />
Spouse’s/Dependent’s Signature<br />
____________________<br />
Date<br />
____________________<br />
Date<br />
NOTE: ORIGINAL OF THIS FORM SHOULD BE GIVEN TO EMPLOYEE, MAKE A COPY FOR EMPLOYEE’S FILE.<br />
Separation From Employment 07/2009
____________________________________ _____________________________________ ____________<br />
Employee Name (Print) Employer (Institution) Institution-Div. #<br />
GROUP LIFE INSURANCE<br />
Your current group life insurance with Hartford Life will terminate on your last day <strong>of</strong> employment ____________________.<br />
(insert date)<br />
You may continue your life insurance by electing one <strong>of</strong> <strong>the</strong> following options within 31 days following <strong>the</strong> date your coverage<br />
terminates.<br />
Portability Option:<br />
Terminating employees who have not reached <strong>the</strong> Defined Retirement Age (in accordance with <strong>the</strong> 1983 amendments <strong>of</strong> <strong>the</strong><br />
United States Social Security Act) would be eligible to apply for continuation <strong>of</strong> life insurance under <strong>the</strong> Portability Option at<br />
group rates. If you are age 65 or older when electing portability, coverage would immediately be reduced by 25% <strong>of</strong><br />
<strong>the</strong> amount eligible for portability. Additional coverage terminates at age 75.<br />
Conversion Option:<br />
Conversion is available upon termination <strong>of</strong> coverage subject to plan limitations. Please contact your local administrator for<br />
additional information.<br />
To secure Applications for Portability or Conversion, you may call Hartford Life at (877) 320-0484.<br />
GROUP LONG TERM DISABILITY INSURANCE (if applicable)<br />
Your current LTD insurance will terminate on your last day <strong>of</strong> employment ______________________. There is no<br />
conversion privilege for this benefit.<br />
(insert date)<br />
FLEXIBLE SPENDING ACCOUNT (if applicable)<br />
If you have an accrued amount in your Flexible Spending Account as <strong>of</strong> your date <strong>of</strong> separation, you can be reimbursed for<br />
medical/dependent expenses incurred prior to your separation date. You must submit an FSA claim form and copies <strong>of</strong><br />
supporting documentation directly to Ceridian.<br />
RETIREMENT PLAN<br />
For information concerning pension <strong>benefits</strong>, please send written request to <strong>the</strong> Archdiocese <strong>of</strong> New York, Pension<br />
Department, 1011 First Avenue, New York, NY 10022. All inquiries must include your name, social security number, <strong>the</strong><br />
name and address <strong>of</strong> <strong>the</strong> local employer institution where you were employed (list all institutions if more than one), and<br />
signature <strong>of</strong> <strong>the</strong> employee.<br />
___________________________________________________ ____________________________________________<br />
Authorized Employer Representative Signature Date Employee Signature Date<br />
NOTE: ORIGINAL OF THIS FORM SHOULD BE GIVEN TO EMPLOYEE, MAKE A COPY FOR EMPLOYEE’S FILE.<br />
Separation From Employment 07/2009
Section VI<br />
Administration <strong>of</strong> Life,<br />
Supplemental & AD&D
ARCHDIOCESE OF NEW YORK<br />
Basic Life<br />
Eligibility<br />
Effective Date<br />
Employee<br />
Contribution<br />
Basic Benefit<br />
Employees who are regularly scheduled to work a minimum <strong>of</strong> 20 hours each<br />
week and after you have satisfied <strong>the</strong> waiting period. (Refer to summary plan<br />
description booklet for fur<strong>the</strong>r details).<br />
First <strong>of</strong> <strong>the</strong> month after waiting period (see summary benefit booklet for<br />
additional details).<br />
None<br />
See benefit booklet for life amount<br />
Minimum Benefit $10,000<br />
Maximum Benefit $375,000<br />
Age Reduction<br />
Accidental Death<br />
&<br />
Dismemberment<br />
Benefit (AD&D)<br />
Beneficiary<br />
Portability Option<br />
Conversion<br />
Privilege<br />
Reduced by 35% at age 65 and to 50% <strong>of</strong> <strong>the</strong> basic benefit at age 70. (Refer to<br />
summary plan description booklet for minimum benefit.)<br />
Same amount as basic life benefit for accidental death. Benefits also payable if<br />
you suffer an accidental injury resulting in <strong>the</strong> loss <strong>of</strong> a hand, foot or eye. (Refer<br />
to summary plan booklet for details).<br />
The person or persons you choose to receive any benefit payable upon <strong>the</strong> insured's<br />
death.<br />
This option permits an individual prior to retirement, who has not reached <strong>the</strong><br />
normal retirement age under <strong>the</strong> 1983 United States Social Security Act , to<br />
continue <strong>the</strong> same amount <strong>of</strong> basic life in place on <strong>the</strong> date <strong>of</strong> his/her employment<br />
termination at a group premium rate. (Refer to <strong>the</strong> summary plan description<br />
booklet for details).<br />
This option provides for <strong>the</strong> conversion <strong>of</strong> <strong>the</strong> group life <strong>benefits</strong> to an individual<br />
life policy, if for example, your coverage ends due to termination <strong>of</strong> employment.<br />
The individual can apply for life insurance coverage up to <strong>the</strong> amount in place on<br />
<strong>the</strong> date <strong>of</strong> his/her employment termination. The insurance carrier will determine<br />
<strong>the</strong> premium. (Refer to <strong>the</strong> summary plan booklet for details) .<br />
- 29 - Revised 07/01/09
ARCHDIOCESE OF NEW YORK<br />
Life and Accidental Death & Dismemberment<br />
Enrollment/Beneficiary Designation Form<br />
For Priests & Final Year Seminarians<br />
PLEASE PRINT CLEARLY OR TYPE<br />
Name <strong>of</strong> Insured: _________________________________________________________________<br />
(Last) (First) (MI)<br />
Date <strong>of</strong> Birth: __________________________<br />
(Month) (Day) (Year)<br />
Social Security No.: ______________________<br />
Institution Number: _________________ Plan Code (Division Number): ( ) 053 ( )153 ( )156<br />
Insurance Benefit: $15,000.00<br />
Effective Date: _________________________________<br />
(Month) (Day) (Year)<br />
Beneficiary: Archbishop <strong>of</strong> New York Beneficiary Tax ID Number: 133089351<br />
Beneficiary Address:<br />
Archdiocese <strong>of</strong> New York<br />
1011 First Avenue - Room 1940<br />
New York, New York 10022<br />
I Certify That The Above Information Is Correct<br />
_______________________________________________________________<br />
(Insured’s Signature)<br />
______________<br />
(Date Signed)<br />
Administrator, please return original copy <strong>of</strong> this form to:<br />
Archdiocese <strong>of</strong> New York<br />
Attn: Benefits Office<br />
Life & Health Department<br />
1011 First Avenue – 16 th Floor<br />
New York, New York 10022<br />
Revised 06//2008
ARCHDIOCESE OF NEW YORK<br />
GROUP NON-CONTRIBUTORY BASIC LIFE<br />
ENROLLMENT AND CHANGE FORM<br />
Please print clearly and be sure to sign and date this form. Return your completed form to your employer’s <strong>of</strong>fice.<br />
( ) I want to be covered under <strong>the</strong> group plan <strong>benefits</strong> for which I am eligible. (Initial enrollment)<br />
( ) Update: Change <strong>of</strong> beneficiary<br />
Your Name:_______________________________________________________________________________________<br />
Home Address:_____________________________________________________________________________________<br />
Social Security Number:______________________________________________________________________________<br />
Date <strong>of</strong> Birth:___________________________ Sex: ( ) Male ( ) Female<br />
Marital Status: ( ) Single ( ) Married ( ) Divorced ( ) Widowed<br />
Home Phone:_____________________________________ Work Phone:_____________________________________<br />
Name <strong>of</strong> Employer:___________________________________________________________________________________<br />
Employer’s Address:__________________________________________________________________________________<br />
Occupation:_________________________________________________________________________________________<br />
Institution #:__________ Division #::___________ If this is a transfer, give old institution/Division #:______________<br />
Salary:$______________________ Date <strong>of</strong> Hire:____________________ Effective Date:_____________________<br />
( ) I do not want to be covered for <strong>the</strong> group plan <strong>benefits</strong> for which I am eligible. I understand that I will have to submit<br />
evidence <strong>of</strong> good health satisfactory to <strong>the</strong> insurance carrier if I want this coverage at a later date.<br />
Designation <strong>of</strong> Beneficiary<br />
( ) I designate as my beneficiary(ies):<br />
Name:______________________________________________________________________________________________<br />
Address:____________________________________________________________________________________________<br />
Date <strong>of</strong> Birth:______________________________ Relationship to Employee:____________________________________<br />
Name:______________________________________________________________________________________________<br />
Address:____________________________________________________________________________________________<br />
Date <strong>of</strong> Birth:______________________________ Relationship to Employee:____________________________________<br />
If <strong>the</strong> beneficiary dies before me, I designate as contingent beneficiary:<br />
Name:______________________________________________________________________________________________<br />
Address:____________________________________________________________________________________________<br />
Date <strong>of</strong> Birth:______________________________ Relationship to Employee:____________________________________<br />
♦ If <strong>the</strong>re is more than one beneficiary or more than one contingent beneficiary, <strong>the</strong>y will share <strong>the</strong> death <strong>benefits</strong> equally,<br />
or all will be paid to <strong>the</strong> survivor.<br />
♦ I RESERVE <strong>the</strong> right to change this designation at any time.<br />
Employee’s Signature:______________________________________________ Date:____________________________<br />
ADMINISTRATORS, mail original form to: Employee Benefit Connections, 1011 First Ave., Room 1679, New York, NY 10022<br />
For additional beneficiaries, please attach a separate list and include <strong>the</strong> names, addresses, dates <strong>of</strong> births and relationship to <strong>the</strong> employee<br />
Contact us: ebc@archny.org Web Page: www.archny.org/<strong>benefits</strong> Revised 09/04/07
HOW TO FILE A CLAIM FOR BASIC GROUP LIFE INSURANCE<br />
(Hartford Life Insurance Company – Group Policy Number – GL 674263)<br />
Upon notification <strong>of</strong> death:<br />
• Verify that <strong>the</strong> deceased employee was covered under <strong>the</strong> Basic Group Life<br />
Insurance and <strong>the</strong> amount <strong>of</strong> Basic Life Insurance Benefit in effect at <strong>the</strong> time <strong>of</strong><br />
<strong>the</strong> employee/insured) death.<br />
• Contact Hartford Life Insurance Company at 1-888-563-1124 and request a Pro<strong>of</strong><br />
<strong>of</strong> Death Claim Form.<br />
• Secure a copy <strong>of</strong> <strong>the</strong> initial Group Life Enrollment Form, signed by <strong>the</strong> employee,<br />
and if applicable, <strong>the</strong> latest Change <strong>of</strong> Beneficiary Designation Form. (Copies <strong>of</strong><br />
<strong>the</strong>se forms are usually retained in an employee’s file and <strong>the</strong> original is retained<br />
at <strong>the</strong> Employee Benefit Connections Office).<br />
• Secure a Certified Copy <strong>of</strong> <strong>the</strong> Certificate <strong>of</strong> Death (this is usually obtained from<br />
<strong>the</strong> beneficiary or and immediate family member <strong>of</strong> <strong>the</strong> deceased).<br />
• When <strong>the</strong> current primary beneficiary(s) is established, send <strong>the</strong> Pro<strong>of</strong> <strong>of</strong> Death<br />
Claim Form to <strong>the</strong> beneficiary(s) (if more than one primary beneficiary; send a<br />
claim form to each primary beneficiary listed) to complete, sign and return to <strong>the</strong><br />
local administrator with one Certified Copy <strong>of</strong> <strong>the</strong> Certificate <strong>of</strong> Death. The<br />
completed form(s) can be mailed to:<br />
Hartford Life Insurance Companies<br />
Attn: Life Claims<br />
P.O. Box 2999<br />
Hartford, CT 06104-2999<br />
Suggest that <strong>the</strong> Local Administrator include a cover letter to Hartford Life,<br />
requesting that <strong>the</strong> local administrator is copied on all communications<br />
concerning <strong>the</strong> particular group life insurance claim. If claim is not paid within<br />
15 working days contact Hartford Life to find out <strong>the</strong> status <strong>of</strong> <strong>the</strong> claim.<br />
Follow same procedure for Accidental Death and Dismemberment, except <strong>the</strong><br />
claim* would be filed with:<br />
Mutual Of Omaha<br />
Mutual <strong>of</strong> Omaha Plaza<br />
Omaha, NE 68175<br />
Tel: 1-800-524-2324<br />
* Claim Amount for AD&D is <strong>the</strong> same as Basic Life – refer to AD&D Summary<br />
Booklet for Group policy number for your institution)<br />
Note: Keep a copy <strong>of</strong> all claims filed with <strong>the</strong> insurance carrier.<br />
- 30 -
PREMIUM WAIVER<br />
Basic Group Life Insurance Coverage<br />
Employees under age 65 who are covered under <strong>the</strong> basic group life insurance plan, who<br />
are absent from work due to injury or illness for an extended period <strong>of</strong> time (at least 12<br />
months) would be eligible to apply for a premium waiver for <strong>the</strong>ir basic group life.<br />
A premium waiver is a provision, which allows for <strong>the</strong> continuation <strong>of</strong> life insurance<br />
coverage for <strong>the</strong> employee, without payment <strong>of</strong> premium, while <strong>the</strong> employee is disabled.<br />
To apply for a waiver <strong>of</strong> premium, <strong>the</strong> employer, or <strong>the</strong> employee may contact Hartford<br />
Life Insurance Company at 1.888.563.1124 to request an Application for Premium<br />
Waiver. The Application for Premium Waiver is composed <strong>of</strong> three sections, <strong>the</strong><br />
Employer Section, <strong>the</strong> Employee Section, and <strong>the</strong> Physician’s Statement.<br />
If <strong>the</strong> employee is covered under <strong>the</strong> Hartford Life Group Long Term Disability Plan (LTD) and a<br />
claim for LTD Benefits has been filed with <strong>the</strong> Hartford Life, Hartford Life will automatically<br />
start <strong>the</strong> premiums waiver process. We encourage <strong>the</strong> local <strong>benefits</strong> administrator to contact<br />
Hartford Life directly (1.888.563.1124) to confirm that <strong>the</strong> premium waiver application has been<br />
filled.<br />
For questions about how to complete <strong>the</strong> Premium Waiver Application form, call<br />
Hartford life toll-free number at 1.888.563.1124.<br />
Completed Applications for Premium Waiver should be mailed to:<br />
Hartford Life<br />
Group Life Claims<br />
P.O. Box 2999<br />
Hartford, CT 06104-2999<br />
If approved by Hartford Life, <strong>the</strong> life insurance coverage will continue until <strong>the</strong> employee/member<br />
is no longer disabled or <strong>the</strong> employee is deceased. Hartford will contact <strong>the</strong> disabled employee for<br />
periodic updates. If <strong>the</strong> employee fails to reply, <strong>the</strong> life insurance coverage may be terminated.<br />
(Refer to <strong>the</strong> Hartford Life Group Life Booklet for details).<br />
IMPORTANT:<br />
This benefit is time sensitive. Please be aware that <strong>the</strong> policy requires that <strong>the</strong> Notice and<br />
Pro<strong>of</strong> <strong>of</strong> Loss be submitted to Hartford Life within one year <strong>of</strong> <strong>the</strong> last day <strong>of</strong> work as an<br />
Active Full Time Employee.<br />
- 31 -
GROUP LIFE INSURANCE BENEFITS FOR<br />
EMPLOYEES SEPARATING FROM SERVICE<br />
PORTABILITY OF BASIC GROUP LIFE &<br />
GROUP SUPPLEMENTAL TERM LIFE INSURANCE<br />
• Employees may elect portability <strong>of</strong> <strong>the</strong>ir group life insurance to a group portability policy<br />
when employment terminates for any reason prior to retirement. (Retirement means <strong>the</strong> date<br />
you attain normal retirement age under <strong>the</strong> 1983 United States Social Security Act, and any<br />
amendments <strong>the</strong>reto). Eligible employees may apply for a group portability policy within 31<br />
days from <strong>the</strong> termination date <strong>of</strong> <strong>the</strong> group life insurance. Also, <strong>the</strong> application can be filed<br />
within 45 days from <strong>the</strong> date <strong>the</strong> portability notice is given, if that date is later than 15 days<br />
from <strong>the</strong> date <strong>the</strong> <strong>benefits</strong> terminated. (Refer to booklet for eligibility requirements).<br />
• The enrollment period for <strong>the</strong> portability <strong>of</strong> <strong>the</strong> group life insurance policy ends 90 days from<br />
<strong>the</strong> date <strong>the</strong> employee’s employment is terminated, regardless <strong>of</strong> when <strong>the</strong> portability<br />
application was given to <strong>the</strong> employee.<br />
• Portability insurance for $5,000 or less is not allowed unless <strong>the</strong> insurance applies to<br />
Dependent Child coverage. (Refer to booklet for fur<strong>the</strong>r details).<br />
• The employer must complete and sign part A <strong>of</strong> <strong>the</strong> Application for Group Life Insurance<br />
Under <strong>the</strong> Hartford Group Insurance Trust Form. The employee should get <strong>the</strong> original<br />
copy to be mailed to <strong>the</strong> insurance company. (A photocopy should also be included in <strong>the</strong><br />
employee’s file).<br />
• It is <strong>the</strong> employee’s responsibility to mail <strong>the</strong> form to Hartford Life Insurance Company,<br />
Attention: Portability Administration, P.O. Box 248108, Cleveland, OH 44124-8108. The<br />
employee must submit <strong>the</strong> required premium along with <strong>the</strong> application. The local employer<br />
will advise <strong>the</strong> applicant <strong>of</strong> <strong>the</strong> premium cost. The employee should call (800) 548-5157 for<br />
any assistance. Employer should call (800) 228-6108, extension 2201 for additional<br />
assistance.<br />
February 2008 - 32 -
PORTABILITY OF GROUP LIFE INSURANCE & SUPPLEMENTAL TERM LIFE INSURANCE<br />
Notice <strong>of</strong> Portability<br />
If an individual is not given notice <strong>of</strong> <strong>the</strong> existence <strong>of</strong> <strong>the</strong> Portability privilege within 15 days <strong>of</strong> <strong>the</strong> terminating<br />
event, which results in <strong>the</strong> Portability option he/she will have an additional period in which to exercise Portability<br />
rights. This additional period will end 45 days following <strong>the</strong> date he/she is given notice <strong>of</strong> <strong>the</strong> right to exercise<br />
Portability rights or 90 days following <strong>the</strong> date on which <strong>the</strong> terminating event which results in <strong>the</strong> Portability<br />
option occurs, whichever occurs first.<br />
What if death occurs during <strong>the</strong> Portability election period?<br />
If <strong>the</strong> individual should die within <strong>the</strong> 31-day portability election period, <strong>the</strong> current carrier will, upon receipt <strong>of</strong><br />
acceptable pro<strong>of</strong> <strong>of</strong> death, pay <strong>the</strong> Amount <strong>of</strong> Life Insurance <strong>the</strong> individual was entitled to continue under <strong>the</strong><br />
Portability provision. However, in no event will a benefit be payable under both <strong>of</strong> <strong>the</strong> 31-day conversion privilege<br />
election period and this portability election period.<br />
INSTRUCTIONS:<br />
Employer: Complete Part A <strong>of</strong> <strong>the</strong> application, make a copy to be included in <strong>the</strong> institution’s records and <strong>the</strong>n<br />
give <strong>the</strong> application to <strong>the</strong> employee (or <strong>the</strong> employee’s spouse under <strong>the</strong> Supplemental Term Life Insurance)<br />
whose coverage is terminating. The employer must attach to <strong>the</strong> application <strong>the</strong> most current copy <strong>of</strong> <strong>the</strong><br />
employee’s enrollment form. The amount <strong>of</strong> insurance that <strong>the</strong> employer identified in Part A must match <strong>the</strong><br />
amount <strong>of</strong> insurance elected on <strong>the</strong> enrollment form. If <strong>the</strong> amounts are not <strong>the</strong> same, an explanation must be<br />
attached.<br />
Applicant: If an employee wishes to continue <strong>the</strong> group life insurance <strong>the</strong>y had with <strong>the</strong> employer, he/she must<br />
complete Part B <strong>of</strong> <strong>the</strong> application, make a copy for his/her records and return <strong>the</strong> completed application along with<br />
<strong>the</strong> premium within 31 days <strong>of</strong> termination <strong>of</strong> group coverage to:<br />
Hartford Life<br />
Attention: Portability Administration<br />
P.O. Box 248108<br />
Cleveland, OH 44124-8108<br />
IMPORTANT NOTE: The employee should be advised to take <strong>the</strong> following information into consideration when<br />
deciding whe<strong>the</strong>r to apply for portability <strong>of</strong> coverage. Coverage under <strong>the</strong> group portability policy reduces and<br />
terminates upon reaching certain ages.<br />
Under <strong>the</strong> Supplemental Term Life Insurance, a dependent child or student coverage terminates when such<br />
dependents reach <strong>the</strong> limiting ages <strong>of</strong> 19 (child) or 25 (student). Portability coverage for <strong>the</strong> employee and spouse<br />
will be reduced by 25%. If Portability is elected at age 65 or older <strong>the</strong> Supplemental coverage will immediately be<br />
reduced by 25%. Supplemental Insurance coverage terminates at age 75.<br />
Under <strong>the</strong> Basic Group Life Insurance benefit, only <strong>the</strong> eligible employee has <strong>the</strong> right to exercise <strong>the</strong> portability<br />
and conversion options. See booklets for fur<strong>the</strong>r details<br />
If an employer or applicant has questions about completing <strong>the</strong> application, <strong>the</strong>y should call Hartford Life at<br />
1.877.320.0484.<br />
- 33 - 07/2009
GROUP LIFE INSURANCE BENEFITS FOR<br />
EMPLOYEES SEPARATING FROM SERVICE<br />
CONVERSION OF BASIC GROUP LIFE & SUPPLEMENTAL TERM LIFE INSURANCE<br />
• Employees are eligible to convert <strong>the</strong>ir basic group life insurance & <strong>the</strong>ir group supplemental<br />
term life insurance to individual policies. Eligible employees should apply for conversion<br />
policies within 31 days from <strong>the</strong> termination date <strong>of</strong> <strong>the</strong>ir basic group life insurance and <strong>the</strong>ir<br />
supplemental term life insurance. Also, <strong>the</strong> application can be filed within 45 days from <strong>the</strong><br />
date <strong>the</strong> conversion notice is given, if that date is later than 15 days from <strong>the</strong> date <strong>the</strong> <strong>benefits</strong><br />
terminated.<br />
• Eligibility for application for conversion to individual life insurance coverage ends 91 days<br />
from <strong>the</strong> date <strong>the</strong> basic group life insurance and <strong>the</strong> supplemental term life insurance<br />
terminated, regardless <strong>of</strong> when <strong>the</strong> conversion application was given to <strong>the</strong> employee.<br />
• The employer must complete and sign parts A. Notice <strong>of</strong> Conversion Privilege – Life<br />
Insurance Only Form. The employee should be given <strong>the</strong> original copy <strong>of</strong> <strong>the</strong> form to be<br />
mailed to <strong>the</strong> insurance company. (A photocopy should also be included in <strong>the</strong> employee’s<br />
file).<br />
• The conversion option under <strong>the</strong> Group Supplemental Term Life Insurance is also<br />
available to an eligible employee’s spouse and dependent child.<br />
• It is <strong>the</strong> employee’s responsibility to mail <strong>the</strong> form to The Hartford Life Companies, Attn:<br />
Group Conversion Unit, P.O. 248108, Cleveland, OH 44124-8108. The employee will receive<br />
a cost and benefit quotation for <strong>the</strong> converted coverage from Hartford once <strong>the</strong> form is<br />
received. The employee should call 877.320.0484 for any assistance.<br />
- 34 -
SAMPLE NOTICE<br />
(This information should be sent to <strong>the</strong> employee who is losing group life coverage.)<br />
GROUP LIFE INSURANCE BENEFITS FOR<br />
EMPLOYEES SEPARATION FROM SERVICE<br />
NOTICE OF CONVERSION PRIVILEGE FOR BASIC GROUP LIFE<br />
& SUPPLEMENTAL TERM LIFE INSURANCE<br />
Insurance coverage for you is being terminated as <strong>of</strong> <strong>the</strong> DATE OF GROUP COVERAGE TERMINATION<br />
shown on <strong>the</strong> NOTICE OF BENEFITS STATUS DUE TO SEPARATION FROM EMPLOYMENT<br />
summary. You have <strong>the</strong> right to CONVERT your Group Life coverage without having to submit evidence <strong>of</strong> good<br />
health. Your group insurance booklet contains <strong>the</strong> specific conversion privilege.<br />
BASIC GROUP LIFE INSURANCE may be converted to an individual life insurance plan. Conversion to term<br />
insurance is not available in all states. You may convert any amount up to <strong>the</strong> benefit level you had under <strong>the</strong><br />
group plan. Special restrictions and limits apply when coverage on an entire class <strong>of</strong> employees or members<br />
terminates.<br />
The conversion option for <strong>the</strong> GROUP SUPPLEMENTAL TERM LIFE INSURANCE is also extended to an<br />
eligible employee’s spouse and dependent children.<br />
To receive a cost and benefit quotation for CONVERTED coverage:<br />
• Complete all information requested in Part B <strong>of</strong> <strong>the</strong> enclosed form. Your local employer or local administrator<br />
must complete Part A. Both Parts A & B must be completed and signed before a quote may be given by <strong>the</strong><br />
insurance carrier. Retain a copy <strong>of</strong> <strong>the</strong> Notice <strong>of</strong> Conversion Privilege-Life Only form for your records.<br />
• Mail <strong>the</strong> original copy <strong>of</strong> <strong>the</strong> Notice <strong>of</strong> Conversion Privilege-Life Insurance Only form directly to:<br />
The Hartford Life Companies<br />
Attn: Group Conversion Unit<br />
P.O. Box 248108<br />
Cleveland, OH 44124-8108<br />
Conversions will expire unless <strong>the</strong> completed form is mailed to Hartford within:<br />
a. 31 days from <strong>the</strong> Date <strong>of</strong> Group Coverage Termination, or<br />
b. 15 days from <strong>the</strong> date <strong>the</strong> NO TICE OF CONVERSION PROVILEGE is given to you, whichever is<br />
later. (This will not extend your rights to apply for conversion beyond 91 days after <strong>the</strong> Date <strong>of</strong> Group<br />
Coverage Termination).<br />
If you have any questions on how to complete <strong>the</strong> enclosed form, you may call <strong>the</strong> Conversion Unit at<br />
1.877.320.0484.
Section VII<br />
Administration <strong>of</strong><br />
Short Term Disability<br />
(New York State Short<br />
Term Disability Benefits)
ARCHDIOCESE OF NEW YORK<br />
Short Term Disability<br />
Eligibility<br />
Effective<br />
Date.<br />
Employee<br />
Contribution<br />
Basic Benefit<br />
Waiting<br />
Period<br />
Definition <strong>of</strong><br />
Disability<br />
Benefit<br />
Duration<br />
Employees who have worked at least four<br />
consecutive weeks.<br />
First <strong>of</strong> <strong>the</strong> month following 30 days <strong>of</strong> employment<br />
None<br />
50% <strong>of</strong> employee's average weekly wage up to a<br />
maximum <strong>of</strong> $170.00.<br />
Seven calendar days <strong>of</strong> disability due to <strong>of</strong>f <strong>the</strong> job<br />
illness or injury for which no <strong>benefits</strong> are payable.<br />
Benefits are payable on <strong>the</strong> eighth consecutive day <strong>of</strong><br />
disability.<br />
Employee is prevented from performing work because<br />
<strong>of</strong> <strong>of</strong>f <strong>the</strong> job illness or injury. Disability connected<br />
with pregnancy is included.<br />
Benefits are paid for a maximum <strong>of</strong> 26 weeks during<br />
52 consecutive weeks or during any one period <strong>of</strong><br />
disability.<br />
Time Limit 20 days after <strong>the</strong> first day <strong>of</strong> disability (to avoid any<br />
for a Filing penalties ).<br />
Claim<br />
- 35 -
HOW TO FILE A CLAIM FOR NEW YORK STATE DISABILITY BENEFITS<br />
(Hartford Life Insurance Company -Policy Number LNY 612197)<br />
• Upon notification that an employee is unable to work for eight consecutive days due to a non<br />
job-related illness or injury, <strong>the</strong> local administrator should send a, Notice And Pro<strong>of</strong> Of Claim<br />
For Disability Benefits Form (DB-450) to <strong>the</strong> disabled employee, with a cover letter requesting<br />
that <strong>the</strong> employee to complete:<br />
- Part A - <strong>the</strong> Claimants Statement, and have <strong>the</strong>ir doctor complete<br />
- Part B - Health Care Provider’s Section<br />
The form should be returned to <strong>the</strong> employer, to complete <strong>the</strong> Employer’s Statement.<br />
• The employer should make a copy for <strong>the</strong>ir files, and mail <strong>the</strong> original disability form to:<br />
The Hartford<br />
Syracuse Benefit Management Services Office<br />
P.O. Box 4925<br />
Syracuse, NY 13221-4925<br />
• Should <strong>the</strong> employee express any concerns about <strong>the</strong> confidentiality relating to <strong>the</strong>ir disability,<br />
<strong>the</strong> employer should complete and sign <strong>the</strong> Employer’s Statement section, make a copy for <strong>the</strong><br />
institution’s or agency’s records and give <strong>the</strong> form to <strong>the</strong> employee to have his or her physician<br />
complete and sign Part B–HealthCare Provider’s Statement section. The employee must<br />
complete and sign Part A-Claimant’s Statement, before submitting <strong>the</strong> claim form directly to<br />
<strong>the</strong> Hartford<br />
• If <strong>the</strong> employee is eligible for salary continuance, (sick pay), from <strong>the</strong> employer, for part or all<br />
<strong>the</strong> time that <strong>the</strong>y are absent from work, <strong>the</strong> employer would be reimbursed for salary<br />
continuance at <strong>the</strong> state disability rate. If <strong>the</strong> employee is not eligible for sick pay, disability<br />
<strong>benefits</strong> will be paid directly to <strong>the</strong> employee, during <strong>the</strong> disability period.<br />
• The employer will receive statement(s) from <strong>the</strong> Hartford confirming <strong>the</strong> time period, and <strong>the</strong><br />
amount <strong>of</strong> <strong>benefits</strong> <strong>the</strong> employee was paid during a disability period.<br />
• Contact <strong>the</strong> Hartford DBL Customer Service Center at 1 800-538-0134 if you have any<br />
claims inquiries.<br />
• Review Part B, 7d. date claimant will be able to return to work.<br />
Note: See NYS DBL Claim Form (DB 450), and Sample Cover Memo to employee.<br />
- 36 -
(Sample Letter)<br />
NOTICE TO DISABLED EMPLOYEE<br />
To:<br />
Address:<br />
Re:<br />
Date:<br />
_______________________________________________________________<br />
_______________________________________________________________<br />
Short Term Disability Benefits Claim Forms<br />
________________________________________________________________<br />
Enclosed is a Notice and Pro<strong>of</strong> <strong>of</strong> Claim for Disability form as you requested. In order to have this<br />
claim properly processed, <strong>the</strong> following is required:<br />
1. You must complete Part A – Claimant’s Statement.<br />
2. Your employer must complete and sign <strong>the</strong> Employer’s Statement section <strong>of</strong> this form.<br />
3. Your attending physician must complete and sign Part B- Health Care Provider’s section.<br />
The general time limit for filing a claim is twenty (20) days after <strong>the</strong> first day <strong>of</strong> disability. Therefore,<br />
<strong>the</strong> completed form should be filed as soon as possible with:<br />
The Hartford<br />
Syracuse Benefit Management Services Office<br />
P.O. Box 4925<br />
Syracuse, NY 13221-4925<br />
Our policy number under <strong>the</strong> current carrier is LNY 612197.<br />
Just to summarize this coverage, New York State Short Term Disability pays 50% <strong>of</strong> <strong>the</strong> average<br />
weekly wage up to a maximum <strong>of</strong> $170.00. Benefits are payable on <strong>the</strong> eighth day <strong>of</strong> disability after<br />
<strong>the</strong> waiting period <strong>of</strong> seven calendar days.<br />
Should you have any claim inquiries concerning your claim, please call <strong>the</strong> Hartford’s claims<br />
department at (800) 538-0134<br />
Sincerely,<br />
Enclosure<br />
[Employer/Benefits Administrator Name]<br />
- 37 -
NOTICE AND PROOF OF CLAIM FOR DISABILITY BENEFITS<br />
CLAIMANT: READ THE FOLLOWING INSTRUCTIONS CAREFULLY<br />
1. USE THIS FORM IF YOU BECOME SICK OR DISABLED WHILE EMPLOYED OR IF YOU BECOME SICK OR DISABLED WITHIN FOUR (4) WEEKS AFTER<br />
TERMINATION OF EMPLOYMENT. USE GREEN CLAIM FORM DB-300 IF YOU BECOME SICK OR DISABLED AFTER HAVING BEEN UNEMPLOYED<br />
MORE THAN FOUR (4) WEEKS.<br />
2. YOU MUST COMPLETE ALL ITEMS OF PART A - THE "CLAIMANT'S STATEMENT". BE ACCURATE. CHECK ALL DATES.<br />
3. BE SURE TO DATE AND SIGN YOUR CLAIM (SEE ITEM 12). IF YOU CANNOT SIGN THIS CLAIM FORM, YOUR REPRESENTATIVE MAY SIGN IT IN YOUR<br />
BEHALF. IN THAT EVENT, THE NAME, ADDRESS AND REPRESENTATIVE'S RELATIONSHIP TO YOU SHOULD BE NOTED UNDER THE SIGNATURE.<br />
4. DO NOT MAIL THIS CLAIM UNLESS YOUR HEALTH CARE PROVIDER COMPLETES AND SIGNS PART B - THE "HEALTH CARE PROVIDER'S<br />
STATEMENT.<br />
5. YOUR COMPLETED CLAIM SHOULD BE MAILED WITHIN THIRTY (30) DAYS AFTER YOU BECOME SICK OR DISABLED TO YOUR LAST EMPLOYER<br />
OR YOUR LAST EMPLOYER'S INSURANCE COMPANY.<br />
6. MAKE A COPY OF THIS COMPLETED FORM FOR YOUR RECORDS BEFORE YOU SUBMIT IT.<br />
PART A - CLAIMANT'S STATEMENT (Please Print or Type) ANSWER ALL QUESTIONS<br />
1. My name is: (First, Middle & Last) 2. Social Security Number: 3. Date <strong>of</strong> Birth:<br />
4. My Address: ( Number, Street, City or Town, State & Zip Code)<br />
5. My Telephone Number<br />
( )<br />
6. Martial Status: (Check one) 7. My disability is: (if injury, also state how, when and where it occurred)<br />
Married Single<br />
8. I became disabled on:<br />
Month/ Day/ Year<br />
a. I worked on that day: Yes No<br />
b. I have since worked for wages or pr<strong>of</strong>it: Yes No<br />
If "Yes", give dates:<br />
9. Give name <strong>of</strong> last employer. If more than one employer during <strong>the</strong> last eight (8) weeks, name all employers.<br />
Employer's Dates <strong>of</strong> Employment Average Weekly Wages<br />
Business Name Business Address Phone Number From Through (Include Bonuses, Tips,<br />
Month/Day/Year Month/ Day/Year<br />
( )<br />
Commissions, Reasonable<br />
Value <strong>of</strong> Board, Rent, etc.)<br />
( )<br />
( )<br />
10. My job is or was: (Occupation) Name <strong>of</strong> Union and Local Number, if member:<br />
11. For <strong>the</strong> period <strong>of</strong> disability covered by this claim:<br />
a. Are you receiving wages, salary or separation pay:<br />
Yes No<br />
b. Are you receiving or claiming:<br />
(1) Workers' compensation for work-connected disability<br />
Yes No<br />
(2) Unemployment Insurance Benefits<br />
Yes No<br />
(3) Damages for personal injury<br />
Yes No<br />
(4) Benefits under <strong>the</strong> Federal Social Security Act for long-term disability Yes No<br />
IF "YES" IS CHECKED IN ANY OF THE ITEMS IN 10a OR 10b, COMPLETE THE FOLLOWING<br />
I have received claimed From For <strong>the</strong> period<br />
To<br />
12. I have received disability <strong>benefits</strong> for ano<strong>the</strong>r period or periods <strong>of</strong> disability within <strong>the</strong> 52 weeks immediately before my present<br />
disability began: Yes No<br />
If "Yes" fill in <strong>the</strong> following: I have been paid by:<br />
From<br />
To<br />
13. I have read <strong>the</strong> instructions above. I hereby claim Disability Benefits and certify that for <strong>the</strong> period covered by this claim I was<br />
disabled and that <strong>the</strong> foregoing statements, including any accompanying statements, are to <strong>the</strong> best <strong>of</strong> my knowledge true and<br />
complete.<br />
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR<br />
BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR SELF-INSURER, ANY INFORMATION CONTAINING ANY FALSE MATERIAL STATEMENT<br />
OR CONCEALS ANY MATERIAL FACT SHALL BE GUILTY OF A CRIME AND SUBJECT TO FINES AND IMPRISONMENT.<br />
Claim signed on:<br />
Claimant's Signature:<br />
If signed by o<strong>the</strong>r than claimant, print below: name, address, and relationship <strong>of</strong> representative:<br />
IF YOU HAVE ANY QUESTIONS ABOUT CLAIMING DISABILITY BENEFITS,<br />
CONTACT THE NEAREST OFFICE OF THE NYS WORKERS' COMPENSATION<br />
BOARD, OR WRITE TO: WORKERS' COMPENSATION BOARD, DISABILITY<br />
BENEFITS BUREAU, 100 BROADWAY-MENANDS, ALBANY, NY 12241-0005<br />
SI TIENE DUDAS RELACIONADAS CON LA RECLAMACIÓN DE BENEFICIOS<br />
POR INCAPACIDAD, COMUNIQUESE CON LA OFICINA MAS CERCANA DE<br />
LA JUNTA DE COMPENSACIÓN OBRERA DE NUEVA YORK, O ESCRIBA A:<br />
WORKER'S COMPENSATION BOARD, DISABILITY BENEFITS BUREAU, 100<br />
BROADWAY- MENANDS, ALBANY, NY 12241-0005<br />
HEALTH CARE PROVIDER MUST COMPLETE PART B ON REVERSE<br />
LC-5012-14 DB-450 02/04 Page 1 <strong>of</strong> 3 02/2009
NOTICE AND PROOF OF CLAIM FOR DISABILITY BENEFITS<br />
IMPORTANT: USE THIS FORM ONLY WHEN THE CLAIMANT BECOMES SICK OR DISABLED WHILE EMPLOYED OR BECOMES SICK<br />
OR DISABLED WITHIN FOUR (4) WEEKS AFTER TERMINATION OF EMPLOYMENT. OTHERWISE USE GREEN CLAIM FORM DB-300.<br />
PART B - HEALTH CARE PROVIDER'S STATEMENT (Please Print or Type)<br />
THE HEALTH CARE PROVIDER'S STATEMENT MUST BE FILLED IN COMPLETELY AND THE FORM MAILED TO THE INSURANCE<br />
CARRIER OR SELF-INSURED EMPLOYER, OR RETURNED TO THE CLAIMANT WITHIN SEVEN DAYS OF THE RECEIPT OF THE FORM.<br />
For item 7d, give approximate date. Make some estimate. If disability is caused by or arising in connection with pregnancy,<br />
enter estimated delivery date under "Remarks". (Even if considerable question exists, estimate date. Avoid using terms<br />
such as unknown or undetermined).<br />
1. Claimant's Name: 2. Date <strong>of</strong> Birth: 3. Sex:<br />
Male<br />
Female<br />
4. Diagnosis/Analysis: Diagnosis Code:<br />
a. Claimant's Symptoms:<br />
b. Objective Findings:<br />
5. Claimant Hospitalized? Yes No<br />
From<br />
To<br />
6. Operation Indicated? Yes No<br />
a. Type b. Date<br />
7. Enter Dates for <strong>the</strong> Following:<br />
a. Date <strong>of</strong> your first treatment for this disability:<br />
b. Date <strong>of</strong> your most recent treatment for this disability:<br />
c. Date claimant was unable to work because <strong>of</strong> this disability:<br />
d. Date claimant will be able to perform usual work:<br />
e. If disability is pregnancy related, please estimate delivery date:<br />
8. In your opinion, is this disability <strong>the</strong> result <strong>of</strong> injury arising out <strong>of</strong> and in <strong>the</strong> course <strong>of</strong> employment or occupational disease?<br />
Yes No If "Yes", has form C-4 been filed with <strong>the</strong> Workers' Compensation Board? Yes No<br />
Remarks: (attach additional sheet, if necessary)<br />
I affirm that I am a: Chiropractor Physician Psychologist<br />
Dentist Podiatrist Nurse-Midwife<br />
License Number:<br />
Licensed in <strong>the</strong> State <strong>of</strong>:<br />
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR<br />
BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR SELF-INSURER, ANY INFORMATION CONTAINING ANY FALSE MATERIAL<br />
STATEMENT OR CONCEALS ANY MATERIAL FACT SHALL BE GUILTY OF A CRIME AND SUBJECT TO FINES AND IMPRISONMENT.<br />
Health Care Provider's Signature:<br />
Date:<br />
Health Care Provider's Name: (Please Print)<br />
Telephone Number:<br />
( )<br />
Office Address:<br />
(Number, Street , City or Town, State & Zip)<br />
HIPAA NOTICE - In order to adjudicate a workers' compensation claim, WCL13-a (4) (a) and 12 NYCRR 325-1.3 require health care<br />
providers to regularly file medical reports <strong>of</strong> treatment with <strong>the</strong> Board and <strong>the</strong> carrier or employer. Pursuant to 45 CFR 164.512 <strong>the</strong>se<br />
legally required medical reports are exempt from HIPAA's restrictions on disclosure <strong>of</strong> health information.<br />
LC-5012-14 DB-450 02/04 Page 2 <strong>of</strong> 3 02/2009
NOTICE AND PROOF OF CLAIM FOR DISABILITY BENEFITS<br />
PART C - EMPLOYER'S STATEMENT<br />
Employee's full name: (As shown on Social Security Card)<br />
Social Security Number:<br />
Employee's Address: (Street, City, State & Zip Code)<br />
Date <strong>of</strong> Birth:<br />
Date <strong>of</strong> employment:<br />
If Part Time, give particulars:<br />
Full Time<br />
Part Time<br />
Check days normally worked:<br />
Sun. Mon. Tues. Wed. Thurs. Fri. Sat.<br />
Is employee a Union member? If "Yes," is employee entitled to Union Benefits Occupation:<br />
Yes No Yes No<br />
Date employee last worked: Date employee returned to work: Were wages continued during disability?<br />
Yes No<br />
Were wages Sick pay?<br />
Yes No From: To:<br />
Were wages Vacation pay?<br />
Yes No From<br />
To<br />
Is reimbursement requested?<br />
Yes No<br />
Is disability due to job?<br />
Yes No<br />
EARNINGS 8 WEEKS PRIOR TO DISABILITY<br />
(Including <strong>the</strong> week in which <strong>the</strong> disability began)<br />
No. Days<br />
Month Day Year Worked Amount<br />
If "Yes," has a compensation claim been filed?<br />
Yes No<br />
Indicate Weekly Value <strong>of</strong> Board, Lodging and Tips:<br />
Is this employee currently covered by Social Security?<br />
Yes No<br />
If "No," state grounds for exemption:<br />
Total<br />
Is employee enrolled in a Hartford Long Term Disability Plan?<br />
Yes No If "Yes," effective date<br />
Based on <strong>the</strong> employer/employee premium contributions made over <strong>the</strong> last 3 years, what percentage <strong>of</strong> <strong>the</strong> Weekly<br />
Disability % LTD % benefit is considered taxable? (See section 7 <strong>of</strong> IRS Publication 15-A for<br />
information on determining <strong>the</strong> taxable percentage.) If blank, we will assume <strong>the</strong> benefit is 100% taxable.<br />
Employer's Name:<br />
Employer's Identification Number:<br />
Address: (Street, City, State & Zip Code) Telephone Number:<br />
( )<br />
Signed by: Date: Title:<br />
THE WORKERS' COMPENSATION BOARD EMPLOYS AND SERVES PEOPLE WITH DISABILITIES WITHOUT DISCRIMINATION<br />
LC-5012-14 DB-450 (02/04) Page 3 <strong>of</strong> 3 02/2009
Section VIII<br />
Administration <strong>of</strong><br />
Long Term Disability
ARCHDIOCESE OF NEW YORK<br />
Benefit Plan Highlights<br />
Long Term Disability<br />
Eligibility<br />
Effective Date<br />
Employee<br />
Contribution<br />
Employees who are regularly scheduled to work a minimum <strong>of</strong> 30 hours each<br />
week for a participating Employer. (20 hours for bargaining lay faculty members.<br />
Eligibility varies for employees working for Cemeteries and Child Care Agencies).<br />
Refer to <strong>benefits</strong> booklet for details.<br />
First <strong>of</strong> <strong>the</strong> month following six months <strong>of</strong> employment.<br />
None. Employer pays full cost <strong>of</strong> premium<br />
Basic Monthly 60% <strong>of</strong> your regular monthly salary not to exceed a maximum <strong>of</strong> $5,000.<br />
Benefit<br />
Minimum<br />
Monthly Benefit<br />
Benefit Offsets<br />
Elimination<br />
Period<br />
Definition <strong>of</strong><br />
Disability<br />
Pre-existing<br />
Condition<br />
Limitation<br />
Benefit Duration<br />
Accidental<br />
Dismemberment<br />
and Loss <strong>of</strong> Sight<br />
Survivor Benefit<br />
The greater <strong>of</strong> $100 or 10% <strong>of</strong> <strong>the</strong> gross monthly benefit.<br />
Benefits can be reduced by any o<strong>the</strong>r income as stated in <strong>the</strong> booklet such as<br />
Social Security Disability, Workers' Compensation and Retirement Benefits as<br />
<strong>of</strong>fsets.<br />
180 days <strong>of</strong> continuous disability.<br />
During <strong>the</strong> elimination period and for <strong>the</strong> next 24 months an employee is<br />
prevented from performing one or more <strong>of</strong> <strong>the</strong> essential duties <strong>of</strong> his/her own<br />
occupation and as a result <strong>the</strong>ir current monthly earnings are no more than 80% <strong>of</strong><br />
<strong>the</strong> indexed pre-disability earnings. After that, <strong>the</strong> employee must be so prevented<br />
from performing one or more <strong>of</strong> <strong>the</strong> essential duties <strong>of</strong> any occupation. (Failure to<br />
pass a physical examination required to maintain a license to perform <strong>the</strong> duties<br />
<strong>of</strong> <strong>the</strong> employee's occupation does not alone mean that <strong>the</strong> employee is disabled.)<br />
Benefits will not be payable for disabilities caused or contributed to by preexisting<br />
conditions until <strong>the</strong> employee has been continuously covered under<br />
he plan for 12 months. A pre-existing condition is an illness or injury for which<br />
you received medical treatment, consultation, care or services, or had taken<br />
prescribed drugs or medicines in <strong>the</strong> three months prior to your coverage<br />
effective date.<br />
For employees disabled prior to age 60, <strong>benefits</strong> are payable to age 65 but not for<br />
less than 60 months. Reduced benefit duration for employees disabled after age<br />
60. (Refer to booklet)<br />
Benefits payable for accidental injury for specified losses. (Refer to booklet for<br />
details).<br />
Limited <strong>benefits</strong> payable to eligible survivor upon employee's death.<br />
- 38 -
HOW TO FILE A CLAIM FOR LONG TERM DISABILITY BENEFITS<br />
(Group Policy Number GLT-674263)<br />
A claim for Long Term Disability (LTD) Benefits should be filed:<br />
• when an eligible employee is absent from work due to illness or injury and<br />
• <strong>the</strong> eligible employee has filed for, and is receiving State Disability Benefits for at<br />
least four months and<br />
• based on evidence <strong>of</strong> disability, it is not anticipated that <strong>the</strong> eligible employee will be<br />
able to return to work before <strong>the</strong> six-month elimination period is exhausted.<br />
Procedure:<br />
• Contact <strong>the</strong> Hartford Life Insurance Company at: 1 800-538-0134 to advise <strong>the</strong><br />
carrier <strong>of</strong> <strong>the</strong> anticipation <strong>of</strong> filing a Long Term Disability (LTD) claim for (name <strong>of</strong><br />
employee), and request for an Application For Long Term Disability Income<br />
Benefits, and also ask any related questions.<br />
• Send both <strong>the</strong> Application For Long Term Disability Income Benefits and <strong>the</strong><br />
Authorization to Obtain and Release Information forms to <strong>the</strong> employee to complete,<br />
sign and have <strong>the</strong>ir physician complete <strong>the</strong> Attending Physician’s Statement, and<br />
return all <strong>the</strong> completed forms to <strong>the</strong> Local Administrator (employer).<br />
• The Employer must complete <strong>the</strong> Employer’s Statement and provide required<br />
attachments (see section K <strong>of</strong> form).<br />
• All <strong>of</strong> <strong>the</strong> forms are <strong>the</strong>n submitted to:<br />
Hartford Life Insurance Company<br />
Syracuse Benefits Management Service Center<br />
P.O. Box 4925<br />
Syracuse, NY 13221-4923<br />
• If your institution uses Hartford Life as <strong>the</strong>ir carrier for New York State Short Term<br />
Disability, Hartford will automatically send <strong>the</strong> disabled employee an application to<br />
apply for <strong>the</strong> Long Term Disability Benefits. If not, you will need to contact Hartford<br />
directly for <strong>the</strong> forms: Hartford Life changes forms, and Claim Filing Centers on a<br />
periodic basis, and this is why it is necessary to contact Hartford Life directly<br />
whenever a claim for LTD is anticipated, and forms will be required to file <strong>the</strong> claim.<br />
• Long Term Disability Benefits Plan ends on <strong>the</strong> employee’s date <strong>of</strong> termination <strong>of</strong><br />
employment, or <strong>the</strong> date <strong>the</strong> employee begins to receive Long Term Disability<br />
Benefits, which ever occurs first. The employing Institution no longer needs to pay<br />
for <strong>the</strong> monthly LTD premium for <strong>the</strong> disabled individual once <strong>the</strong> disabled individual<br />
begins to receive <strong>the</strong> monthly LTD benefit.<br />
• There is no Portability or Conversion option available for this insurance.<br />
- 39 -
Section IX<br />
Administration <strong>of</strong><br />
Dental Coverage
ARCHDIOCESE OF NEW YORK<br />
Benefit Highlights<br />
Group Dental Insurance<br />
Eligibility<br />
Effective Date<br />
Premium Cost<br />
Types <strong>of</strong> Dental<br />
Coverage<br />
Member <strong>of</strong> <strong>the</strong> Clergy, or Religious Bro<strong>the</strong>r or Sister<br />
Date assigned to Institution<br />
Premium paid in full by Institution<br />
Dental PPO (Preferred Provider Organization)<br />
*Option I - Non-stipend Religious Bro<strong>the</strong>r & Sisters are eligible<br />
Maximum Annual Benefit - $750<br />
*Option II - Members <strong>of</strong> <strong>the</strong> Clergy, Religious Bro<strong>the</strong>rs & Sisters<br />
on stipend. Maximum Annual Benefit - $1,500<br />
Basic Benefit *Preventive, Restorative Services<br />
Coverage (Orthodontia services are not provided under Option I)<br />
*In-Network and Out-<strong>of</strong>-Network Benefits<br />
(Refer to Dental Schedule <strong>of</strong> Benefits for Details)<br />
- 40 -
CIGNA Dental for Religious and Clergy<br />
The Archdiocese <strong>of</strong>fers <strong>the</strong> PPO Dental program through CIGNA. Plan participants can<br />
receive dental services at reduced fees from CIGNA PPO network dentists. In view <strong>of</strong><br />
<strong>the</strong> $1,500 calendar year maximum, <strong>the</strong> reduced fees allow members to receive a higher<br />
level <strong>of</strong> benefit from <strong>the</strong> plan. Additionally <strong>the</strong> patient’s out-<strong>of</strong>-pocket cost is reduced,<br />
because <strong>the</strong> patient pays <strong>the</strong> member coinsurance on a reduced fee.<br />
• This dental plan for <strong>the</strong> Clergy under Option Plan II provides <strong>the</strong> following <strong>benefits</strong>:<br />
- The PPO network feature allows you to use a network or non-network dentist at<br />
any time.<br />
- Orthodontia services and appliances are covered at 50%. The maximum benefit is<br />
$1,500 per lifetime.<br />
• The Religious on stipend should have Option Plan II, which provides <strong>the</strong> same<br />
<strong>benefits</strong> as <strong>the</strong> Clergy dental plan. Religious who are not on stipend may also be<br />
enrolled in this plan provided <strong>the</strong>ir administrator selects this benefit for <strong>the</strong>m. The<br />
maximum benefit is $1,500 per calendar year. There is a $1,500 per lifetime benefit<br />
for orthodontia.<br />
• Option Plan I, a less costly option, is also available as an option for institutions<br />
covering religious not on stipend. Plan I provides less coverage than Plan II, since it<br />
has a higher deductible and lower coinsurance levels than Plan II. The maximum<br />
benefit is $750 per calendar year. Option Plan I does not provide any coverage for<br />
orthodontia.<br />
- 41 -
ARCHDIOCESE OF NEW YORK<br />
CIGNA Dental PPO for Clergy Enrolled in High Option Plan II<br />
Benefit (1) In-Network (2) Out-<strong>of</strong>-Network<br />
Deductible (per calendar year $ 50 per individual, waived for D&P (3)<br />
Coinsurance:<br />
Class I – Diagnostic & Preventive (D&P) Services<br />
100% 100%<br />
- Oral Exams (2 per calendar year)<br />
- Cleanings (2 per calendar year)<br />
- Full mouth x-rays (complete every 3 calendar years)<br />
- Bitewing x-rays (2 per calendar year)<br />
- Panoramic x-ray (1 every three calendar years)<br />
- Space maintainers (limited to non-orthodontic treatment)<br />
- Emergency care to relieve pain<br />
Class II – Basic Restorative Services<br />
80% 80%<br />
- Fillings, root canal <strong>the</strong>rapy osseous surgery, periodontal<br />
scaling and root planing, denture adjustments & repairs,<br />
anes<strong>the</strong>tics and oral surgery<br />
Class III – Major Restorative Services<br />
60% 60%<br />
- Crowns, dentures & bridgework<br />
Class IV – Orthodontia Services<br />
60% 60%<br />
(Treatment & Appliances)<br />
Maximum Plan Benefit $1,500 per calendar year (3)<br />
Lifetime Orthodontia Maximum $1,500 per lifetime (3)<br />
1. Missing Teeth Limit – The amount payable is 50% <strong>of</strong> <strong>the</strong> amount o<strong>the</strong>rwise payable for replacement <strong>of</strong> teeth that are<br />
missing when a person becomes insured under <strong>the</strong> Archdiocese CIGNA dental plan. This limitation no longer applies after<br />
<strong>the</strong> person has been insured under <strong>the</strong> CIGNA dental plan for 24 months.<br />
2. To locate a network dentist in your area or to find out if a particular dentist is in <strong>the</strong> CIGNA PPO Dental network, call<br />
800.244.6224, or access <strong>the</strong>ir website, cigna.com/dental.<br />
3. All deductibles, plan maximums and service specific maximums (dollar and occurrence) cross accumulate in and out-<strong>of</strong>network.<br />
The annual plan maximum does not apply to <strong>the</strong> orthodontia <strong>benefits</strong>, but <strong>the</strong> plan deductible applies.<br />
- 42 -
ARCHDIOCESE OF NEW YORK<br />
CIGNA Dental PPO for Religious Bro<strong>the</strong>rs and Sisters on Stipend<br />
and Institutions Electing High Option Plan for Religious<br />
Plan II<br />
Benefit (1) In-Network (2) Out-<strong>of</strong>-Network<br />
Deductible (per calendar year $100 per individual, waived for D&P (3)<br />
Coinsurance:<br />
Class I – Diagnostic & Preventive (D&P) Services<br />
100% 100%<br />
- Oral Exams (2 per calendar year)<br />
- Cleanings (2 per calendar year)<br />
- Full mouth x-rays (complete every 3 calendar years)<br />
- Bitewing x-rays (2 per calendar year)<br />
- Panoramic x-ray (1 every three calendae years)<br />
- Space maintainers (limited to non-orthodontic treatment)<br />
- Emergency care to relieve pain<br />
Class II – Basic Restorative Services<br />
80% 80%<br />
- Fillings, root canal <strong>the</strong>rapy osseous surgery, periodontal<br />
scaling and root planing, denture adjustments & repairs,<br />
anes<strong>the</strong>tics and oral surgery<br />
Class III – Major Restorative Services<br />
60% 60%<br />
- Crowns, dentures & bridgework<br />
Class IV – Orthodontia Services<br />
60% 60%<br />
(Treatment & Appliances)<br />
Maximum Plan Benefit $1,500 per calendar year (3)<br />
Lifetime Orthodontia Maximum $1,500 per lifetime (3)<br />
1. Missing Teeth Limit – The amount payable is 50% <strong>of</strong> <strong>the</strong> amount o<strong>the</strong>rwise payable for replacement <strong>of</strong> teeth that are<br />
missing when a person becomes insured under <strong>the</strong> Archdiocese CIGNA dental plan. This limitation no longer applies after<br />
<strong>the</strong> person has been insured under <strong>the</strong> CIGNA dental plan for 24 months.<br />
2. To locate a network dentist in your area or to find out if a particular dentist is in <strong>the</strong> CIGNA PPO Dental network, call<br />
800.244.6224 or access <strong>the</strong>ir website, cigna.com/dental.<br />
3. All deductibles, plan maximums and service specific maximums (dollar and occurrence) cross accumulate in and out-<strong>of</strong>network.<br />
The annual plan maximum does not apply to <strong>the</strong> orthodontia <strong>benefits</strong>, but <strong>the</strong> plan deductible applies.<br />
- 43 -
ARCHDIOCESE OF NEW YORK<br />
CIGNA Dental PPO for Religious Bro<strong>the</strong>rs and Sisters<br />
Plan I<br />
Benefit (1) In-Network (2) Out-<strong>of</strong>-Network<br />
Deductible (per calendar year $100 per individual, waived for D&P (3)<br />
Coinsurance:<br />
Class I – Diagnostic & Preventive (D&P) Services<br />
80% 70%<br />
- Oral Exams (2 per calendar year)<br />
- Cleanings (2 per calendar year)<br />
- Full mouth x-rays (complete every 3 calendar years)<br />
- Bitewing x-rays (2 per calendar year)<br />
- Panoramic x-ray (1 every three calendae years)<br />
- Space maintainers (limited to non-orthodontic treatment)<br />
- Emergency care to relieve pain<br />
Class II – Basic Restorative Services<br />
70% 60%<br />
- Fillings, root canal <strong>the</strong>rapy osseous surgery, periodontal<br />
scaling and root planing, denture adjustments & repairs,<br />
anes<strong>the</strong>tics and oral surgery<br />
Class III – Major Restorative Services<br />
50% 40%<br />
- Crowns, dentures & bridgework<br />
Class IV – Orthodontia Services<br />
(Treatment & Appliances)<br />
Not covered<br />
Not covered<br />
Maximum Plan Benefit $750 per calendar year (3)<br />
1. Missing Teeth Limit – The amount payable is 50% <strong>of</strong> <strong>the</strong> amount o<strong>the</strong>rwise payable for replacement <strong>of</strong> teeth that are<br />
missing when a person becomes insured under <strong>the</strong> Archdiocese CIGNA dental plan. This limitation no longer applies after<br />
<strong>the</strong> person has been insured under <strong>the</strong> CIGNA dental plan for 24 months.<br />
2. To locate a network dentist in your area or to find out if a particular dentist is in <strong>the</strong> CIGNA PPO Dental network, call<br />
800.244.6224, or access <strong>the</strong>ir website, cigna.com/dental.<br />
3. All deductibles, plan maximums and service specific maximums (dollar and occurrence) cross accumulate in and out-<strong>of</strong>network.<br />
The annual plan maximum does not apply to <strong>the</strong> orthodontia <strong>benefits</strong>, but <strong>the</strong> plan deductible applies.<br />
- 44 -
HOW TO FILE A DENTAL CLAIM<br />
There are several ways to file a claim with <strong>the</strong> dental insurance carrier.<br />
• Direct Claim – The participant’s dental <strong>of</strong>fice can file <strong>the</strong> claim electronically on his/her<br />
behalf with <strong>the</strong> dental insurance carrier.<br />
• Paper Claim – The dentist may also complete CIGNA’s ADA Dental Claim Form.<br />
Signatures <strong>of</strong> both <strong>the</strong> benefit participant and <strong>the</strong> dentist are required. The claim form<br />
should be mailed to:<br />
CIGNA HealthCare Service Center<br />
P.O. Box 188037<br />
Chattanooga, TN 37422-8037<br />
CIGNA Customer Service Telephone Number: 1.800.244.6224<br />
• Invoice – If a participant receives an invoice from a dental provider that lists an insurance<br />
information section, (most times this will be on <strong>the</strong> reverse side <strong>of</strong> <strong>the</strong> invoice), complete <strong>the</strong><br />
insurance information section, and ei<strong>the</strong>r return to <strong>the</strong> service provider, or send it directly to<br />
<strong>the</strong> insurance carrier (follow <strong>the</strong> directions on <strong>the</strong> invoice).<br />
If <strong>the</strong> invoice is itemized, and lists <strong>the</strong> date(s) <strong>of</strong> service, a diagnosis or diagnostic code, and a<br />
total dollar amount <strong>of</strong> charges, you can attach <strong>the</strong> invoice to a Dental Claim Form, complete <strong>the</strong><br />
Employee Section and mail it to CIGNA at <strong>the</strong> address listed above.<br />
Important Note: Keep a copy <strong>of</strong> any claims that you submit to <strong>the</strong> insurance carrier<br />
- 45 -
Section X<br />
Administration <strong>of</strong><br />
Vision Coverage
DAVIS VISION CARE<br />
VISION CARE BENEFIT PLAN<br />
- 46 -
Davis Vision for Religious and Clergy<br />
The Archdiocese sponsors <strong>the</strong> managed vision benefit available to <strong>the</strong> Diocesan Clergy<br />
and Religious through Davis Vision. The plan provides network and non-network<br />
<strong>benefits</strong> for routine eye exams, contact lenses, lenses and frames. Network <strong>benefits</strong> are<br />
subject to copays. Services and appliances received from non-network dentists will be<br />
reimbursed based upon a fee schedule.<br />
Clergy and Religious on stipend, who are covered under <strong>the</strong> Archdiocese plan for<br />
medical <strong>benefits</strong>, are also eligible to enroll in this vision plan. Each participating<br />
institution may elect to provide <strong>the</strong> vision coverage for <strong>the</strong>ir non-stipend Religious.<br />
- 47-
ARCHDIOCESE OF NEW YORK<br />
Benefit Highlights<br />
Group Vision Care<br />
Eligibility<br />
Effective Date<br />
Participant Cost<br />
Type <strong>of</strong> Dental<br />
Coverage<br />
Basic Benefit<br />
Coverage<br />
Members <strong>of</strong> <strong>the</strong> Clergy, or Religious Bro<strong>the</strong>r or Sister<br />
Date assigned to Institution<br />
Non-contributory<br />
Vision PPO Coverage (Preferred Provider Organization)<br />
*Eye Examination<br />
*O<strong>the</strong>r In-Network and Out-<strong>of</strong>-Network Benefits<br />
(Refer to Vision Schedule <strong>of</strong> Benefits for Details)<br />
- 48 -
ARCHDIOCESE OF NEW YORK<br />
Davis Vision PPO Plan for Clergy and Religious Bro<strong>the</strong>rs and Sisters (1)<br />
Benefit<br />
In-Network<br />
Copay<br />
Out-<strong>of</strong>-Network<br />
Allowance<br />
Eye Examination (Once every 12 months $10 $60<br />
Eyeglass Lenses (Once every 12 months)<br />
Single<br />
Bifocal<br />
Trifocal<br />
$15 $45<br />
$60<br />
$75<br />
Eyeglass Frames (Once every 24 months) $10 $75<br />
Contact Lenses (In lieu <strong>of</strong> eyeglasses, once<br />
every 12 months) (2)<br />
$25 $125<br />
1. The Vision Plan is automatically provided for Clergy and Religious Bro<strong>the</strong>rs & Sisters on stipend who are<br />
enrolled in an Archdiocese group medical plan. The plan is also available to non-stipend Religious if <strong>the</strong>ir<br />
congregation or employer elects <strong>the</strong> benefit on <strong>the</strong>ir behalf.<br />
2. The Contact Lens <strong>benefits</strong> are quoted for elective contact lenses. Medically necessary contact lenses purchased<br />
from a network provider will be covered in full (prior approval required)<br />
- 49 -
HOW TO FILE A VISION CARE CLAIM (Clergy and Religious only)<br />
The two most common ways to file a claim for vision care are a direct claim or a paper<br />
claim.<br />
Direct Claim - The insured is responsible for all applicable co-pays. The participating<br />
in-network eye care provider will submit <strong>the</strong> claim directly to Davis Vision on <strong>the</strong><br />
insured’s behalf.<br />
Paper Claim - If <strong>the</strong> insured uses an out -<strong>of</strong>- network provider, he/she should complete<br />
and sign a Davis Vision Direct Reimbursement Claim Form. The insured should have <strong>the</strong><br />
vision care provider complete and sign <strong>the</strong> “Provider Information” Section and send <strong>the</strong><br />
claim to:<br />
Vision Care Processing Unit<br />
P.O. Box 1525<br />
Latham, NY 12110<br />
Invoice – If <strong>the</strong> insured receives an invoice from an eye care facility, and <strong>the</strong> reverse side<br />
<strong>of</strong> <strong>the</strong> bill has a section to list insurance information, he/she can complete <strong>the</strong><br />
information, and submit it directly to Vision Care Processing Unit at <strong>the</strong> address above or<br />
return it to <strong>the</strong> facility (following <strong>the</strong> directions on invoice). If <strong>the</strong>re is an itemized bill<br />
with <strong>the</strong> date(s) <strong>of</strong> service listed, <strong>the</strong> insured should complete <strong>the</strong> Member/Employee and<br />
Patient Information sections, attach a copy <strong>of</strong> <strong>the</strong> invoice and submit it to Vision Care<br />
Processing Unit at <strong>the</strong> address listed above. (address is also listed on <strong>the</strong> claim form).<br />
The insured (patient) is responsible for all charges above <strong>the</strong> reimbursable scheduled<br />
amount(s)<br />
Important Note: The insured should keep a copy <strong>of</strong> any claims that you submit for<br />
payment<br />
- 50 -
Direct Reimbursement Claim Form<br />
Important Information:<br />
1. Use this form to request reimbursement for services received from providers who do not participate in <strong>the</strong> Davis Vision network.<br />
2. Expenses for both examinations and eyewear can be claimed on this form. Only services listed on this form will be considered for<br />
reimbursement.<br />
3. Make sure that all sections are completed, that you and <strong>the</strong> providers(s) have signed <strong>the</strong> form, and that all services, charges, and<br />
service dates have been entered. If <strong>the</strong> form is incomplete, additional information may be required. This may result in a delay <strong>of</strong><br />
payment for eligible <strong>benefits</strong>.<br />
4. Please submit claim reimbursement for each patient on a separate claim form.<br />
5. Please note that <strong>the</strong> member’s (or employee’s or authorized person’s) signature is required on this form.<br />
6. Mail completed claim form to: Vision Care Processing Unit, P.O. Box 1525, Latham, NY 12110.<br />
7. The completion and submission <strong>of</strong> this form does not guarantee eligibility for <strong>benefits</strong>. Please verify your coverage with your <strong>benefits</strong> <strong>of</strong>fice<br />
or call 1-800-999-5431 or visit www.davisvision.com. The patient is responsible for <strong>the</strong> costs <strong>of</strong> all treatment and materials provided.<br />
8. FOR PATIENTS RESIDING IN TN ONLY: Tennessee state law stipulates that it is a crime to knowingly provide false, incomplete or<br />
misleading information to an insurance company for <strong>the</strong> purpose <strong>of</strong> defrauding <strong>the</strong> company. Penalties include imprisonment, fines and<br />
denial <strong>of</strong> insurance <strong>benefits</strong>.<br />
Member/Employee Information * Your Member Identification No. is <strong>the</strong> number by which <strong>the</strong> company that sponsors your vision care <strong>benefits</strong> identifies you.<br />
(PLEASE PRINT CLEARLY)<br />
Member Name: _____________________________________________________________ Member Identification No*.:______________________<br />
First Middle Initial Last<br />
Mailing Address: _____________________________________________________________________________________________________________<br />
Street City State Zip<br />
Business Phone: ________________________________________________ Home Phone: _______________________________________________<br />
Patient Information<br />
Patient Name:<br />
Area Code<br />
________________________________________________________<br />
First Middle Initial Last<br />
Relationship: Member Spouse Child DOB: ______________ If student aged 19 or over, attach written pro<strong>of</strong> <strong>of</strong> attendance at school (if required)<br />
Are you and your spouses <strong>benefits</strong> both provided by <strong>the</strong> same agency? Yes No<br />
Area Code<br />
FOR INTERNAL USE ONLY<br />
Auth #: ________________________________<br />
Paid Denied Pended <br />
Provider Information<br />
Examiner<br />
Name: ________________________________________________________<br />
Address: _______________________________________________________<br />
Dispenser<br />
Name:________________________________________________________<br />
Address:______________________________________________________<br />
City: __________________________ State: ____ Zip: ________________ City: __________________________ State: ____ Zip: ______________<br />
Federal Tax I.D. Number: ________________________________________ Federal Tax I.D. Number: ________________________________________<br />
Phone Number:__________________________________________________<br />
Phone Number: ________________________________________________<br />
Provider Signature: _____________________________________________<br />
Member/Employee Certification<br />
Provider Signature: ____________________________________________<br />
Service Date <strong>of</strong> Service Amount<br />
1. Eye Examination $<br />
2. Frames $<br />
3. Single Vision Lenses (not plano) $<br />
4. Bifocal Lenses $<br />
5. Trifocal Lenses $<br />
6. Contact Lenses $<br />
7. Cataract S.V. Lenses $<br />
8. Cataract Bifocal Lenses $<br />
9. Medically Necessary Contact Lenses $<br />
Total $<br />
I certify that <strong>the</strong> information on this form is correct and authorize <strong>the</strong> Provider to release appropriate information necessary to process this claim to plan provisions. Additionally,<br />
I have read and understand item 8, under Important Information, above.<br />
Required<br />
_____________________________________________________________ ___________________<br />
Member/Employee or authorized person’s signature<br />
Date<br />
SC00015A 1/2/04
Section XI<br />
Administration <strong>of</strong><br />
Voluntary Plans
VOLUNTARY PLANS<br />
The Archdiocese <strong>of</strong>fers an opportunity for <strong>the</strong> lay employees to enroll in several voluntary plans. They<br />
are:<br />
♦<br />
♦<br />
Hartford Supplemental Life Insurance<br />
Nor<strong>the</strong>ast Dental Plan <strong>of</strong> America<br />
The Hartford Supplemental Life Insurance plan will be administered through Hartford. Eligible<br />
employees should contact <strong>the</strong>ir local employer for additional eligibility information. Premiums are paid<br />
through payroll deductions.<br />
Employees also have <strong>the</strong> option <strong>of</strong> participating in <strong>the</strong> Nor<strong>the</strong>ast Dental Plan <strong>of</strong> America at a discounted<br />
membership fee. This insurance carrier will administer <strong>the</strong> voluntary dental plan. All premiums and fees<br />
will be billed directly to <strong>the</strong> employees.<br />
Hartford Supplemental Life Insurance<br />
This is an opportunity for <strong>the</strong> employees to secure additional life insurance that has cash accumulation or<br />
cash value built into <strong>the</strong> coverage. An employee must work at least 20 hours to be eligible to participate.<br />
The premiums are entirely paid by <strong>the</strong> employee through payroll deduction. The employees should call<br />
(800) 228-6108 and ask for Laura Gibbons at extension 2201 for fur<strong>the</strong>r information. The employees<br />
should contact <strong>the</strong>ir local administrator; <strong>the</strong> Benefits Department at 212.371.1000, Ext. 3026 or <strong>the</strong><br />
Employee Benefits Connections Department at 212.371.1000, Ext. 3060 to obtain a copy <strong>of</strong> <strong>the</strong><br />
application form. The completed form should be returned to <strong>the</strong> Employee Benefit Connections, 1011<br />
First Avenue, Room 1679, New York, NY 10022.<br />
Nor<strong>the</strong>ast Dental Plan <strong>of</strong> America<br />
This plan is composed <strong>of</strong> a preferred provider network <strong>of</strong> participating dentists in New York, New Jersey<br />
and Connecticut. The Nor<strong>the</strong>ast Dental Plan <strong>of</strong> America allows <strong>the</strong> employees to obtain dental services at<br />
discounted service fees from network dentists. In order to be eligible for <strong>the</strong>se discounts <strong>the</strong> employees<br />
must pay an annual fee directly to <strong>the</strong> company. This is not an insurance plan and <strong>the</strong>re is no minimum<br />
participation requirement among eligible employees. There are no payroll deduction requirements. At<br />
present <strong>the</strong> annual fees are:<br />
Single Employee $ 60.00<br />
Two Person $120.00<br />
Family $140.00<br />
To participate in this plan, an employee should call Nor<strong>the</strong>ast at ei<strong>the</strong>r (800) 828-2222 or<br />
(212) 688-5555 and request an enrollment package for an employee <strong>of</strong> <strong>the</strong> Archdiocese <strong>of</strong> New York.<br />
- 51 - 11/08
ARCHDIOCESE OF NEW YORK<br />
SUPPLEMENTAL LIFE INSURANCE - Policy #GL-674263<br />
Eligibility<br />
Options<br />
Employee must be enrolled in basic group life insurance sponsored by <strong>the</strong> Archdiocese <strong>of</strong> New York and<br />
assigned to work 20 hours or more weekly.<br />
Employee may purchase additonal life insurance in $10,000 increments on his/her life to <strong>the</strong> lesser <strong>of</strong> 5x<br />
<strong>of</strong> his/her basic annual salary to <strong>the</strong> lesser <strong>of</strong> $500,000. A participant may purchase amount up $150,000<br />
(guarantee issue) without completing a Personal Health Statement.<br />
Employee may also purchase additional life insurance on <strong>the</strong> life <strong>of</strong> his/her spouse in $5,000 increments<br />
to a maximum <strong>of</strong> $100,000 (not to exceed 50% <strong>of</strong> employee's supplemental life benefit). The<br />
employee may purchase <strong>the</strong> spouse's supplement insurance up to $50,000 (guarantee issue) without<br />
completing a Personal Health Statement for <strong>the</strong> spouse.<br />
Employee may also purchase additional life insurance on <strong>the</strong> life <strong>of</strong> his/her dependent child (up to age<br />
19 ) in increments <strong>of</strong> $2,000 to <strong>the</strong> maximum <strong>of</strong> $10,000. (Employee must purchase same amount for<br />
each child).<br />
Evidence <strong>of</strong><br />
Insurability<br />
Beneficiary<br />
Designations<br />
Premium<br />
Payments<br />
Suicide<br />
Exclusion<br />
Clause<br />
Accelerated<br />
Death Benefit<br />
Conversion<br />
A Personal Health Statement will be required for purchase amounts exceeding $150,000 on <strong>the</strong> life <strong>of</strong><br />
employee and $50,000 on <strong>the</strong> life <strong>of</strong> dependent spouse. This form is also required for late entrants<br />
(employees who did not elect enrollment during eligibility period-usually 31 days from <strong>the</strong> date <strong>of</strong> hire or<br />
change in family status).<br />
The names and relationships <strong>of</strong> employee's primary and secondary beneficiaries must be provided. The<br />
employee must be <strong>the</strong> beneficiary for <strong>the</strong> spouse and dependent child coverages<br />
Premiums wil be paid through payroll deductions. This benefit also has <strong>the</strong> Premium Waiver feature in<br />
<strong>the</strong> event <strong>the</strong> employee becomes disabled prior to age 60. Premium waiver continues until employee no<br />
longer disabled or normal retirement age. Premium Waiver for spouse & dependent child is available<br />
only if employee qualifies for waiver .<br />
Payment <strong>of</strong> full face amount will be incontestable if death is caused by suicide within two years <strong>of</strong> <strong>the</strong><br />
effective date <strong>of</strong> coverage.<br />
Yes. Up to 80% <strong>of</strong> Life amount with minimum <strong>of</strong> $10,000 to maximum <strong>of</strong> $500,000. Must have a life<br />
expectancy <strong>of</strong> 12 months or less. Also available for spouse up to 80%<strong>of</strong> Life amount to max <strong>of</strong><br />
$50,000.<br />
Participant may convert benefit to individual coverage within 31 days <strong>of</strong> a qualifying event up to <strong>the</strong> same<br />
amount <strong>of</strong> coverage that was in place prior to qualifying event. Available to spouse & dependent child.<br />
Portability<br />
Participant may port 50%, 75% or 100%<strong>of</strong> amount <strong>of</strong> insurance being termed due to a qualifying event<br />
without evidence <strong>of</strong> insurability. Employee port amount not to exceed $250,000. Also available to<br />
spouse up to $50,000 and dependent child up to $10,000.<br />
Rates per<br />
$1,000 Age Employee Spouse Dependent Child<br />
Supplemental Term Life Insurance<br />
FOR EMPLOYEE TO COMPLETE<br />
Employee Name (last name, first, middle initial)<br />
GROUP PLAN #: GL-674263<br />
Employer Name: Archdiocese <strong>of</strong> New York<br />
Location Name:<br />
Employee Address (street, city, state, zip code) Social Security Number Date <strong>of</strong> Birth<br />
Annual Earnings Date <strong>of</strong> Employment Marital Status Sex<br />
Single Divorced Male<br />
Married Widowed Female<br />
BENEFIT SELECTION<br />
Choose any amount from $10,000 to $500,000 for yourself (in increments <strong>of</strong> $10,000) not to exceed five times your<br />
annual salary. For amounts over <strong>the</strong> Guarantee Issue Amount ($150,000) a Health Statement is required.<br />
______ x Basic Annual Earnings<br />
O<strong>the</strong>r $ ______________<br />
Choose any amount for your spouse from $5,000 to $100,000 (in increments <strong>of</strong> $5,000). Not to exceed 50% <strong>of</strong><br />
Employee Supplemental Life Benefit. For amounts over <strong>the</strong> Guarantee Issue Amount ($50,000) a Health<br />
Statement is required.<br />
Amount $ _______________ Name <strong>of</strong> Spouse: _______________________ Birth Date: ___________<br />
Select an amount from $2,000 to $10,000 (in increments <strong>of</strong> $2,000) for each dependent child. Each child in a<br />
family must be insured for <strong>the</strong> same amount.<br />
Amount per Child $ _______________<br />
Names <strong>of</strong> Child(ren) Birth Dates Relationship<br />
Name <strong>of</strong> Primary Beneficiary: _______________________________<br />
Secondary Beneficiary: _____________________________________<br />
Relationship: __________________<br />
Relationship: __________________<br />
I hereby apply for <strong>the</strong> coverages I have indicated above on behalf <strong>of</strong> myself and all dependents listed.<br />
I authorize my Employer to make <strong>the</strong> appropriate deductions from my salary or wages to pay for <strong>the</strong> cost.<br />
I understand that <strong>the</strong> coverages available to me are in accordance with <strong>the</strong> provisions <strong>of</strong> <strong>the</strong> contract.<br />
Employee Signature<br />
Date<br />
IMPORTANT: INTERNAL OFFICE AND WAIVER INFORMATION REQUIRED ON BACK OF FORM
INTERNAL USE ONLY<br />
Institution Name:<br />
Institution Number:<br />
Street Address:<br />
City: State: Zip:<br />
Claim Division Number:<br />
Insurance Effective Date:<br />
Covered by Collective Bargaining Agreement? Yes No<br />
WAIVER OF SUPPLEMENTAL LIFE INSURANCE<br />
Employee Name ___________________________________________________<br />
(Please Print)<br />
I have been given an opportunity to apply for Supplemental Life Insurance as <strong>of</strong>fered by my<br />
Employer and have decided not to take advantage <strong>of</strong> this <strong>of</strong>fer for myself and all eligible<br />
dependents.<br />
Should I desire to apply for this insurance in <strong>the</strong> future, I realize that satisfactory evidence<br />
<strong>of</strong> insurability must be furnished to <strong>the</strong> Insurance Company at my expense. I understand<br />
that <strong>the</strong> Insurance Company reserves <strong>the</strong> right to reject such future application.<br />
Employee Signature<br />
Date<br />
Suicide Exclusion<br />
This plan includes a Suicide Exclusion for employees and dependents. It applies to<br />
coverage amounts which became effective within two years <strong>of</strong> <strong>the</strong> date <strong>of</strong> death.
SAMPLE FORM<br />
This is a Sample for not to be used for an actual enrollment.<br />
Contact Hartford Life at 1.800.331.7234 for a valid enrollment form
PERSONAL HEALTH APPLICATION<br />
Thank you for choosing The Hartford. All sections <strong>of</strong> this form must be completed and received by The Hartford within 30 days<br />
<strong>of</strong> <strong>the</strong> signature date.<br />
Employers: Please completely fill out Section 1 and Section 2 on this page and forward <strong>the</strong> entire form to <strong>the</strong> employee. Refer to<br />
your Policy and employee records for this information. These records are your property and are not on file with The Hartford. An<br />
incomplete form will result in a delay in processing your employee’s request for insurance.<br />
Section 1: Employer Details (to be completed by Employer)<br />
Employer Name:<br />
PLEASE PRINT CLEARLY<br />
Policy Number:<br />
Division (if applicable):<br />
Employer Mailing Address (Street, City, State, Zip Code):<br />
Benefits Contact Name (First, Last):<br />
Benefits Contact Email Address: Benefits Contact Phone: ( ) -<br />
Section 2: Employee Details (to be completed by Employer)<br />
Employee Name (First, MI, Last):<br />
PLEASE PRINT CLEARLY<br />
Base Annual Earnings*: Social Security Number: - - Date <strong>of</strong> Hire (mm/dd/yyyy): / /<br />
* Base annual earnings as described in <strong>the</strong> contract with The Hartford.<br />
Coverage Details<br />
• Check <strong>the</strong> applicable box(es) in each row to reflect <strong>the</strong> applicant’s current coverage and <strong>new</strong> election.<br />
• Enter <strong>the</strong> amount <strong>of</strong> any existing coverage (including Guarantee Issue (GI)**) in Current Coverage. Please include <strong>the</strong> current<br />
amount <strong>of</strong> Basic Life coverage even if <strong>the</strong> applicant is not requesting Basic Life coverage at this time.<br />
• Enter <strong>the</strong> amount <strong>of</strong> Additional Coverage Requested that requires medical underwriting.<br />
• Enter <strong>the</strong> Total Coverage Amount that will be in force if <strong>the</strong> additional coverage requested is approved.<br />
• If <strong>the</strong> applicant is enrolling after his/her initial eligibility period and does not have current coverage <strong>the</strong>y will be responsible for<br />
all fees incurred during <strong>the</strong> medical underwriting process.<br />
Current Coverage<br />
(including GI Amount)<br />
Additional Coverage<br />
Requested<br />
Total Coverage Amount<br />
Life Insurance Coverage Enter all amounts as dollars. Include Basic Life Current Coverage Amount<br />
even if not requesting this coverage type.<br />
Employee Basic Life $ $ $<br />
Employee Supplemental or Voluntary Life $ $ $<br />
Spouse Basic Life $ $<br />
$<br />
Spouse Supplemental or Voluntary Life $ $ $<br />
Disability Insurance Coverage<br />
Long Term Disability<br />
Enter all amounts as dollars or as percentage <strong>of</strong> Base Annual Earnings<br />
** Guarantee Issue (GI) is <strong>the</strong> maximum amount <strong>of</strong> coverage, as defined in <strong>the</strong> contract with The Hartford, which does not require<br />
evidence <strong>of</strong> good health.<br />
Is <strong>the</strong> employee electing an amount greater than<br />
$15,000 for a child? Yes No<br />
Number <strong>of</strong> Children: Amount Requested Per Child: $<br />
Employees: Please complete pages 2 thru 5. It should take you about 10 minutes to complete this form.<br />
The Hartford® is The Hartford Financial Services Group, Inc. and its subsidiaries, including issuing companies Hartford Life Insurance Company and Hartford Life and Accident<br />
Insurance Company. Policies in New York are underwritten by Hartford Life Insurance Company.<br />
PA-9199<br />
(Rev. 3/07) 1 <strong>of</strong> 5
Applicant Section: Please answer all questions on this page completely and accurately and certify your answers on page 4.<br />
Leaving information blank will result in delays and may result in your file being closed.<br />
Section 3: Employee Information (Complete even if employee is not applying for coverage) PLEASE PRINT CLEARLY<br />
First Name: Last Name: Social Security # : - -<br />
Home Mailing Address (Street, Apt. #):<br />
City:<br />
State: Zip Code: Employer:<br />
Daytime Phone: ( ) Evening Phone: ( ) Height: ___Ft. ___In. Weight:________ lbs.<br />
Gender:<br />
Date <strong>of</strong> Birth: / /<br />
M F<br />
Email Address:<br />
Section 4: Spouse Information (Complete only if applying for this coverage)<br />
PLEASE PRINT CLEARLY<br />
First Name: Last Name: Social Security # : - -<br />
Daytime Phone: ( ) Evening Phone: ( ) Height: ___Ft. ___In. Weight:________ lbs.<br />
Gender:<br />
Date <strong>of</strong> Birth: / /<br />
M F<br />
Email Address:<br />
Section 5 – Medical Information (to be completed only by applicants required to provide evidence <strong>of</strong> good health)<br />
If you or anyone proposed for coverage can answer Yes to any <strong>of</strong> <strong>the</strong> Questions below, check <strong>the</strong> appropriate box and provide additional<br />
details in Section 6. If you are a resident <strong>of</strong> one <strong>of</strong> <strong>the</strong> following states: Connecticut, Florida, Kentucky, Maine, Maryland, Minnesota,<br />
New York, North Carolina, Vermont, or Wisconsin <strong>the</strong>n please go to <strong>the</strong> State Variable Question section on page 3 and answer or review <strong>the</strong><br />
appropriate question for your state. After you have read that information, proceed with completing this section.<br />
1. Within <strong>the</strong> past 5 years, with <strong>the</strong> exception <strong>of</strong> a past pregnancy, have you lost time from work for more than<br />
10 work days for <strong>the</strong> same physical, mental, or emotional condition, disability, injury, or sickness?<br />
Employee Spouse<br />
2. Within <strong>the</strong> past 5 years, have you used any controlled substances, with <strong>the</strong> exception <strong>of</strong> those prescribed by<br />
your physician, received medical advice or sought treatment for drug or alcohol abuse, or been charged with Employee Spouse<br />
operating a motor vehicle under <strong>the</strong> influence <strong>of</strong> drugs or alcohol?<br />
3. Are you currently undergoing any diagnostic testing for symptoms without a final diagnosis or resolution? Employee Spouse<br />
4. Are you currently pregnant? If yes, what was your pre-pregnancy weight?_________ lbs. Employee Spouse<br />
5. During <strong>the</strong> past 5 years have you been diagnosed with or treated by a member <strong>of</strong> <strong>the</strong> medical pr<strong>of</strong>ession for<br />
Acquired Immune Deficiency Syndrome (AIDS), AIDS-Related Complex (ARC), or any o<strong>the</strong>r immune Employee Spouse<br />
deficiency disorder?<br />
6. During <strong>the</strong> past 5 years have you been diagnosed with, treated for, treated with, or had any symptoms due to any <strong>of</strong> <strong>the</strong> following<br />
conditions or treatments listed below? Please check all that apply:<br />
Employee Spouse Employee Spouse<br />
Heart-Related Surgery or Heart Attack<br />
Crohn’s Disease<br />
Stroke<br />
Kidney Failure/Dialysis<br />
Heart Disease (excluding high blood<br />
pressure & heart murmur)<br />
Hepatitis (excluding Hepatitis A)<br />
Blocked Arteries (including<br />
arteriosclerosis, a<strong>the</strong>rosclerosis, aneurysm,<br />
Diabetes<br />
or deep vein blood clot)<br />
Chronic Obstructive Pulmonary Disorder<br />
(COPD)<br />
Knee Disorder, Injury, or Surgery<br />
Emphysema<br />
Back or Neck Disorder, Injury, or Surgery<br />
Adjustment Disorder<br />
Joint/Ligament Disorder, Injury, or Surgery<br />
Bipolar Disorder<br />
Osteoporosis or Osteopenia<br />
Depression (single episode)<br />
Multiple Sclerosis (MS)<br />
Depression (multiple episodes)<br />
Amyotrophic Lateral Sclerosis (ALS)<br />
Psychotic/Personality Disorders<br />
Muscular Dystrophy<br />
O<strong>the</strong>r Mental/Nervous/Psychiatric<br />
Disorders (including Anxiety)<br />
Arthritis<br />
Cancer (excluding Basal Cell Carcinoma)<br />
Fibromyalgia<br />
Cirrhosis<br />
Chronic Fatigue Syndrome<br />
Ulcerative Colitis<br />
Sleep Apnea<br />
The Hartford® is The Hartford Financial Services Group, Inc. and its subsidiaries, including issuing companies Hartford Life Insurance Company and Hartford Life and Accident<br />
Insurance Company. Policies in New York are underwritten by Hartford Life Insurance Company.<br />
PA-9199<br />
(Rev. 3/07) 2 <strong>of</strong> 5
Employee: First Name_____________________________________ Last Name_____________________________________________<br />
Section 5 Continued: State Variable Questions<br />
For residents <strong>of</strong> Connecticut, Florida, Kentucky, Maine, Maryland, Minnesota, New York, North Carolina, Vermont, and Wisconsin review<br />
or answer, where applicable, <strong>the</strong> question listed below instead <strong>of</strong> <strong>the</strong> corresponding question listed in <strong>the</strong> Medical Information section on<br />
page 2. Any “Yes” responses can be explained in <strong>the</strong> Additional Details section <strong>of</strong> this form. Once you have reviewed/answered <strong>the</strong>se<br />
questions, please return to Section 5 and proceed with completing <strong>the</strong> rest <strong>of</strong> <strong>the</strong> form.<br />
Information to be Reviewed<br />
Florida, Kentucky, and Maryland Residents- Please review this question prior to answering Question 6 in <strong>the</strong> Medical Information<br />
Section on Page 2:<br />
Question 6: During <strong>the</strong> past 5 years have you been diagnosed with, treated for, or treated with any <strong>of</strong> <strong>the</strong> following conditions or treatments<br />
listed below? Please check all <strong>of</strong> <strong>the</strong> conditions on page 2 that apply.<br />
Maine Residents- Please review this statement prior to answering <strong>the</strong> medical questions in Section 5 on Page 2:<br />
You are not required to disclose whe<strong>the</strong>r you have been tested for HIV, if you have not developed symptoms <strong>of</strong> <strong>the</strong> disease AIDS or<br />
ARC, in your answer to any <strong>of</strong> <strong>the</strong> questions in <strong>the</strong> Medical Information section.<br />
Minnesota Residents- Please review this statement prior to answering <strong>the</strong> medical questions in Section 5 on Page 2:<br />
You need not disclose an HIV (aids virus) test which was administered: (1) to a criminal <strong>of</strong>fender or criminal victim as a result <strong>of</strong> a crime<br />
that was reported to <strong>the</strong> police; (2) to a patient who received <strong>the</strong> services <strong>of</strong> emergency medical services personnel at a hospital or medical<br />
care facility; (3) to emergency medical personnel who were tested as a result <strong>of</strong> performing emergency medical services.<br />
Please review this question prior to answering Question 6 in <strong>the</strong> Medical Information Section on Page 2:<br />
Question 6: During <strong>the</strong> past 5 years have you been diagnosed by a physician with, treated for, or treated with any <strong>of</strong> <strong>the</strong> following<br />
conditions or treatments listed below? Please check all <strong>of</strong> <strong>the</strong> conditions on page 2 that apply.<br />
Questions to be Answered<br />
Connecticut and Minnesota Residents: Do not answer Question 2 in <strong>the</strong> Medical Information section. Answer <strong>the</strong> following<br />
question below.<br />
Question 2: Within <strong>the</strong> past 5 years, have you used any controlled substances, with <strong>the</strong> exception <strong>of</strong> those prescribed by your physician,<br />
received medical advice or sought treatment for drug or alcohol abuse, or been convicted <strong>of</strong> operating a motor vehicle under <strong>the</strong> influence <strong>of</strong><br />
drugs or alcohol? Employee Spouse<br />
Florida residents: Do not answer Question 5 in <strong>the</strong> Medical Information section. Answer <strong>the</strong> following question below.<br />
Question 5: Have you ever tested positive for exposure to <strong>the</strong> HIV infection or been diagnosed as having ARC or AIDS caused by <strong>the</strong> HIV<br />
infection or o<strong>the</strong>r sickness or condition derived from such infection or had unexplained weight loss or enlarged lymph nodes?<br />
Employee<br />
Spouse<br />
New York Residents: Do not answer Question 5 in <strong>the</strong> Medical Information section. Answer <strong>the</strong> following question below.<br />
Question 5: During <strong>the</strong> past 5 years have you been diagnosed with or treated by a member <strong>of</strong> <strong>the</strong> medical pr<strong>of</strong>ession for Acquired Immune<br />
Deficiency Syndrome (AIDS), AIDS-Related Complex (ARC), or any o<strong>the</strong>r immune deficiency disorder excluding HIV?<br />
Employee<br />
Spouse<br />
North Carolina Residents: Do not answer Question 5 in <strong>the</strong> Medical Information section. Answer <strong>the</strong> following question below.<br />
Question 5: Have you ever been diagnosed or treated by a member <strong>of</strong> <strong>the</strong> medical pr<strong>of</strong>ession for Acquired Immune Deficiency Syndrome<br />
(AIDS) or AIDS Related Complex (ARC) or any o<strong>the</strong>r immune deficiency disorder? AIDS Related Complex (ARC) is a condition with<br />
signs and symptoms which may include generalized lymphadenopathy (swollen lymph nodes), loss <strong>of</strong> appetite, weight loss, fever, oral<br />
thrush, skin rashes, unexplained infections, dementia, depression, or o<strong>the</strong>r psychoneurotic disorders with no known cause. “Disorder <strong>of</strong> <strong>the</strong><br />
Immune System” includes <strong>the</strong> hyperimmune conditions, disorders <strong>of</strong> gammaglobulin syn<strong>the</strong>sis (hypogammaglobulinemia), <strong>of</strong> white blood<br />
cell production and maturation, and <strong>the</strong> immune-deficiency disorders both congenital and acquired. Also included in disorders <strong>of</strong> immunity<br />
are lupus erythamatosus, Grave’s Disease, rheumatoid arthritis, primary biliary cirrhosis, and o<strong>the</strong>rs.<br />
Employee<br />
Spouse<br />
Vermont Residents: Do not answer Questions 3 or 5 in <strong>the</strong> Medical Information section. Answer <strong>the</strong> following questions below.<br />
Question 3: Are you currently undergoing any diagnostic testing (excluding prior HIV related testing) for symptoms without a final<br />
diagnosis or resolution? Employee Spouse<br />
Question 5: Have you been diagnosed as having or been treated for Acquired Immune Deficiency Syndrome (AIDS) or AIDS Related<br />
Complex (ARC) by a licensed medical physician?<br />
Employee<br />
Spouse<br />
Wisconsin Residents: Do not answer Question 3 in <strong>the</strong> Medical Information section. Answer <strong>the</strong> following question below.<br />
Question 3: Are you currently undergoing any diagnostic testing, excluding AIDS or HIV tests, for symptoms without a final diagnosis or<br />
resolution? Employee Spouse<br />
Please proceed with completing <strong>the</strong> rest <strong>of</strong> <strong>the</strong> medical questions on Page 2 once you have completed/reviewed this page.<br />
The Hartford® is The Hartford Financial Services Group, Inc. and its subsidiaries, including issuing companies Hartford Life Insurance Company and Hartford Life and Accident<br />
Insurance Company. Policies in New York are underwritten by Hartford Life Insurance Company.<br />
PA-9199<br />
(Rev. 3/07) 3 <strong>of</strong> 5
Employee: First Name_____________________________________ Last Name_____________________________________________<br />
Section 6: Additional Details: If you or anyone proposed for coverage checked any box related to Questions 1 – 6, please provide<br />
details in <strong>the</strong> space below. If you need more space, please attach, sign and date an additional sheet. The Hartford may contact you for<br />
additional or missing information.<br />
Question #<br />
or Condition<br />
Applicant Name<br />
Medications/<br />
Treatment<br />
Date <strong>of</strong><br />
Diagnosis<br />
Date <strong>of</strong> Last<br />
Symptom<br />
Current Status<br />
<strong>of</strong> Condition<br />
Physician’s Name, Address, and<br />
Phone #<br />
Section 7: Health Question Certification Statement (To be completed by all applicants)<br />
By checking this box: Employee Spouse<br />
I hereby certify that I have reviewed each <strong>of</strong> <strong>the</strong> above questions and conditions.<br />
I also certify that I have checked all <strong>of</strong> <strong>the</strong> questions and conditions that apply to my health history.<br />
Section 8: Authorization (To be reviewed by all applicants)<br />
New York Residents: I understand <strong>the</strong> Medical Information Bureau, Inc. will release records or information only to The Hartford. I<br />
authorize The Hartford to give information about me to: its reinsurer(s); <strong>the</strong> Medical Information Bureau, Inc.; any o<strong>the</strong>r insurance company<br />
to whom I may apply for Life or Health Insurance; or o<strong>the</strong>r persons or organizations handling a claim, underwriting coverage applied for or<br />
administering coverage issued as a result <strong>of</strong> this application; or as required by law.<br />
I understand that upon written request I may revoke this authorization except to <strong>the</strong> extent that action has already been taken in reliance on<br />
this authorization. This authorization expires 24 months from <strong>the</strong> date <strong>of</strong> this application. I understand that a photocopy <strong>of</strong> this form is as<br />
valid as <strong>the</strong> original and that I have a right to receive a copy <strong>of</strong> this form upon request.<br />
Residents <strong>of</strong> All States Except New York: I understand <strong>the</strong> Medical Information Bureau, Inc. will release records or information only to<br />
The Hartford. I authorize The Hartford to give information about me to: its reinsurer(s); <strong>the</strong> Medical Information Bureau, Inc.; any o<strong>the</strong>r<br />
insurance company to whom I may apply for Life or Health Insurance; or o<strong>the</strong>r persons or organizations handling a claim, underwriting<br />
coverage applied for or administering coverage issued as a result <strong>of</strong> this application; or as required by law.<br />
I understand that upon written request I may revoke this authorization except to <strong>the</strong> extent that action has already been taken in reliance on<br />
this authorization. This authorization expires 24 months from <strong>the</strong> effective date <strong>of</strong> my coverage or, if no coverage has been issued, one (1)<br />
year from <strong>the</strong> date <strong>of</strong> this application. I understand that a photocopy <strong>of</strong> this form is as valid as <strong>the</strong> original and that I have a right to receive<br />
a copy <strong>of</strong> this form upon request.<br />
Additional Language for Maine Residents: This authorization excludes disclosure <strong>of</strong> <strong>the</strong> result <strong>of</strong> a test for HIV if <strong>the</strong> applicant has not<br />
developed symptoms <strong>of</strong> <strong>the</strong> disease AIDS. Such test results shall not be discovered or published. Nothing in this caveat will prohibit this<br />
authorization from including <strong>the</strong> fact that <strong>the</strong> applicant has AIDS or ARC. I understand that my failure to sign this authorization may<br />
impair <strong>the</strong> ability <strong>of</strong> The Hartford to process this application or evaluate claims and may be a basis for denying this application or a claim<br />
for <strong>benefits</strong>.<br />
Additional Language for Minnesota Residents: This authorization excludes <strong>the</strong> release <strong>of</strong> information about HIV (AIDS Virus) tests<br />
which were administered (1) to a criminal <strong>of</strong>fender or criminal victim as a result <strong>of</strong> a crime that was reported to <strong>the</strong> police; (2) to a patient<br />
who received <strong>the</strong> services <strong>of</strong> Emergency Medical Services personnel at a hospital or medical care facility; or (3) to emergency medical<br />
personnel who were tested as a result <strong>of</strong> performing emergency medical services. The term “Emergency Medical Personnel” includes<br />
individuals employed to provide pre-hospital emergency services; crime lab personnel, correctional guards, including security guards at <strong>the</strong><br />
Minnesota security hospital, who experience a significant exposure to an inmate who is transported to a facility for emergency medical care;<br />
and o<strong>the</strong>r persons who render emergency care or assistance at <strong>the</strong> scene <strong>of</strong> an emergency, or while an injured person is being transported to<br />
receive medical care and would qualify for immunity under <strong>the</strong> Good Samaritan Law.<br />
The Hartford® is The Hartford Financial Services Group, Inc. and its subsidiaries, including issuing companies Hartford Life Insurance Company and Hartford Life and Accident<br />
Insurance Company. Policies in New York are underwritten by Hartford Life Insurance Company.<br />
PA-9199<br />
(Rev. 3/07) 4 <strong>of</strong> 5
Employee: First Name___________________________________<br />
Last Name____________________________________________<br />
Section 9: Certification (To be reviewed by all applicants)<br />
Residents <strong>of</strong> All States: I hereby certify (“represent” for Kansas residents) that all statements and answers contained herein, are full,<br />
complete, and true to <strong>the</strong> best <strong>of</strong> my knowledge and belief.<br />
Residents <strong>of</strong> All States Except New York: I also understand that any misrepresentation contained herein or relied upon by <strong>the</strong> company<br />
may be used to contest <strong>the</strong> validity <strong>of</strong> <strong>the</strong> coverage, within <strong>the</strong> contestable period if such misrepresentation materially affects acceptance <strong>of</strong><br />
<strong>the</strong> risk. This information may be used by The Hartford for plan <strong>administration</strong> purposes to decide if <strong>the</strong> person(s) is/are eligible for<br />
coverage.<br />
I understand that coverage will not become effective until The Hartford grants it’s underwriting approval. I do not receive temporary or<br />
conditional insurance coverage just because I submit an application and pay <strong>the</strong> first premium.<br />
I agree that this document and all its contents shall form a part <strong>of</strong> my request for group <strong>benefits</strong>.<br />
Section 10: Fraud Statement (To be completed by all applicants)<br />
Residents <strong>of</strong> All States Except California, Pennsylvania, and New York: Any person who knowingly presents a false or fraudulent claim<br />
for payment <strong>of</strong> a loss or benefit or knowingly presents false information in an application for insurance is guilty <strong>of</strong> a crime and may be<br />
subject to fines and confinement in prison.<br />
California Residents: For your protection, California law requires <strong>the</strong> following to appear on this form: any person who knowingly<br />
presents a false or fraudulent claim for <strong>the</strong> payment <strong>of</strong> a loss is guilty <strong>of</strong> a crime and may be subject to fines and confinement in state prison.<br />
Pennsylvania Residents: Any person who knowingly and with intent to defraud any insurance company or o<strong>the</strong>r person files an application<br />
for insurance or statement <strong>of</strong> claim containing any materially false information or conceals for <strong>the</strong> purpose <strong>of</strong> misleading, information<br />
concerning any fact material <strong>the</strong>reto commits a fraudulent insurance act, which is a crime and subjects a person to criminal and civil<br />
penalties.<br />
New York Residents: Any person who knowingly and with intent to defraud any insurance company or o<strong>the</strong>r person files an application<br />
for insurance or statement <strong>of</strong> claim containing any materially false information, or conceals for <strong>the</strong> purpose <strong>of</strong> misleading, information<br />
concerning any fact material <strong>the</strong>reto, commits a fraudulent insurance act, which is a crime, and shall also be subject to a civil penalty not to<br />
exceed five thousand dollars and <strong>the</strong> stated value <strong>of</strong> <strong>the</strong> claim for each such violation.<br />
Notice: To <strong>the</strong> best <strong>of</strong> <strong>the</strong>ir knowledge, an Applicant is required to notify The Hartford in writing <strong>of</strong> any changes in any applicant’s medical<br />
condition between <strong>the</strong> date <strong>the</strong> Applicant signs this form and <strong>the</strong> date <strong>the</strong> coverage is approved.<br />
___________________________________<br />
Employee’s Signature<br />
or Legal Representative/ Relationship to<br />
Employee (Required)<br />
____/____/____<br />
Date Signed<br />
____________________________________<br />
Spouse’s Signature<br />
or Legal Representative/Relationship to Spouse<br />
(Required only if applying for coverage)<br />
____/____/____<br />
Date Signed<br />
Please return <strong>the</strong> completed Employer and Employee sections to:<br />
The Hartford, Medical Underwriting<br />
P.O. Box 2999<br />
Hartford, CT 06104-2999<br />
After submitting this application, you can check your status on line at www.TheHartfordAtWork.com.<br />
If you have any questions or concerns, please call The Hartford Customer Service Department toll-free at<br />
1-800-331-7234, Monday through Friday, 8:00 a.m. to 6:00 p.m., Eastern Time, or email us at medical.uw@hartfordlife.com.<br />
The Hartford® is The Hartford Financial Services Group, Inc. and its subsidiaries, including issuing companies Hartford Life Insurance Company and Hartford Life and Accident<br />
Insurance Company. Policies in New York are underwritten by Hartford Life Insurance Company.<br />
PA-9199<br />
(Rev. 3/07) 5 <strong>of</strong> 5
NORTHEAST DENTAL PLAN OF AMERICA<br />
Enroll by Phone (via Credit Card) & Receive Immediate Benefits<br />
(800) 828-2222 or Fax us (212) 688-9708<br />
845 Third Avenue – 20 th Floor - New York, NY 10022<br />
SPECIAL APPLICATION FOR EMPLOYEES OF THE<br />
ARCHDIOCESE OF NEW YORK<br />
• Membership cards will be mailed to you within 5 to 10 business days.<br />
• Your membership is valid for 12 months. Re<strong>new</strong>al notices are mailed<br />
approximately 45 days prior to your re<strong>new</strong>al date.<br />
• Most current NDPA information can be obtained via our Web Site at<br />
www.dentalsave.com.<br />
Please Check Annual Membership Fee:<br />
___Single $60.00 ___Couple $120.00 ___Family $140.00<br />
(any 2 household members) (3 or more household members)<br />
LAST NAME_________________________ FIRST NAME_________________ M.I. __<br />
ADDRESS_____________________________________________________________________<br />
CITY_______________________________ STATE__________________ ZIP______________<br />
HOME PHONE (____) ________________ DAY/WORK (____) _________________________<br />
SOCIAL SECURITY #________________ E-MAIL ___________________________________<br />
O<strong>the</strong>r Household Members<br />
Name________________________________ Relationship_______________________________<br />
Name________________________________ Relationship_______________________________<br />
Name________________________________ Relationship_______________________________<br />
Name________________________________ Relationship______________________________<br />
The Dentist I have selected from <strong>the</strong> Directory <strong>of</strong> Dentists is:<br />
Name_________________________________________________________________________<br />
Address___________________________ City____________________ State________________<br />
Enclosed is my payment for: $ ____________<br />
I am paying by: ___ Check<br />
___ Money Order ___ Discover ___ Master Card ___ Amex ___Visa<br />
Card Number: ___________________________________ Expiration Date: ________________________<br />
===============================================================<br />
For Office Use Only: Rep/574 ____________ Check # ____________<br />
- 53 -
IMPORTANT NOTICE<br />
The Archdiocese <strong>of</strong> New York reserves <strong>the</strong> right to modify or discontinue any<br />
<strong>of</strong> <strong>the</strong> group plans at any time.<br />
The <strong>benefits</strong> described in <strong>the</strong> Resource Guide are subject to <strong>the</strong> terms,<br />
conditions, limitations, and exclusions <strong>of</strong> <strong>the</strong> plan contracts issued by <strong>the</strong><br />
individual insurance carriers to your group. If a difference exists between <strong>the</strong><br />
information in <strong>the</strong> Resource Guide and <strong>the</strong> actual contract, <strong>the</strong> contract<br />
governs.<br />
Participation in any <strong>of</strong> <strong>the</strong> group plans is limited to individuals who o<strong>the</strong>rwise<br />
satisfy <strong>the</strong> specific eligibility requirements for such group plans, and are<br />
ei<strong>the</strong>r (i) employed by <strong>the</strong> Archdiocese <strong>of</strong> New York; or (ii) employed by an<br />
institution or agency properly listed in <strong>the</strong> Official Catholic Directory, which<br />
has adopted and participates in such group plans with <strong>the</strong> consent <strong>of</strong> <strong>the</strong><br />
Archdiocese <strong>of</strong> New York.<br />
Nothing contained in this <strong>guide</strong> should be construed as creating an<br />
employment relationship <strong>of</strong> any kind between <strong>the</strong> Archdiocese <strong>of</strong> New York<br />
and any individual, nor should it be interpreted as affecting any employment<br />
relationship between an employee and his or her actual employer.<br />
- 54 -