2007 Cancer Annual_prod5 - St. Joseph Medical Center
2007 Cancer Annual_prod5 - St. Joseph Medical Center
2007 Cancer Annual_prod5 - St. Joseph Medical Center
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
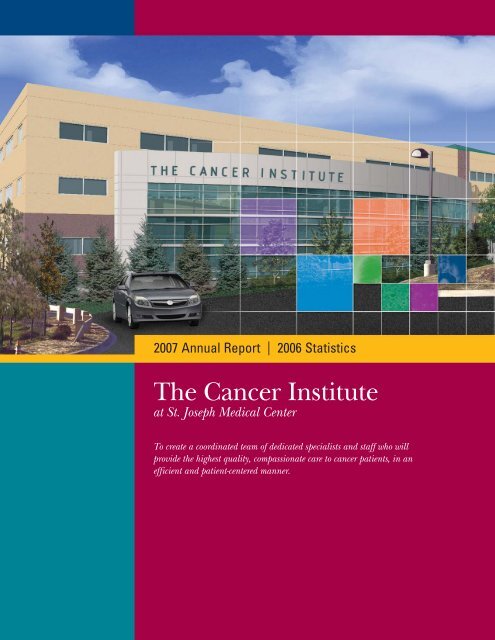
<strong>2007</strong> <strong>Annual</strong> Report | 2006 <strong>St</strong>atistics<br />
The <strong>Cancer</strong> Institute<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong><br />
To create a coordinated team of dedicated specialists and staff who will<br />
provide the highest quality, compassionate care to cancer patients, in an<br />
efficient and patient-centered manner.
A New Day In <strong>Cancer</strong> Treatment<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong><br />
One team. One location.<br />
One comprehensive treatment plan.<br />
Building the Vision<br />
The vision of creating a state-of-the-art, patient-centered cancer<br />
care program is quickly becoming reality as the new <strong>Cancer</strong><br />
Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> approaches completion<br />
in early 2008.<br />
Although other cancer<br />
programs may claim to<br />
provide patient-centered care,<br />
few can match the meticulous<br />
planning, level of expertise<br />
and investment that have gone into creating the patient’s<br />
optimum experience when facing this formidable disease.<br />
At The <strong>Cancer</strong> Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>, the world<br />
revolves around the patient. The patient experience begins with<br />
warm, inviting spaces and welcoming, supportive staff. “Our<br />
vision for The <strong>Cancer</strong> Institute centers around the patients’<br />
needs,” Dr. Mark Krasna, medical director of The <strong>Cancer</strong><br />
Institute says, “and it begins with the architectural design.<br />
From the open reception area to the spacious clinical facilities,<br />
the <strong>Center</strong> creates a welcoming, reassuring first impression.<br />
Even our chemotherapy infusion area – with its own garden<br />
and two-story glass atrium – has an open, pleasant feeling.”<br />
“Not only are the surroundings of the chemotherapy infusion<br />
center beautiful, but the center features infusion chairs<br />
designed specifically for patient comfort. We spent six<br />
months looking at chairs that were available,” Dr. Krasna<br />
says. “None met our needs, so we designed our own. We<br />
hope that our unique <strong>St</strong>. <strong>Joseph</strong>’s chair will someday be<br />
in use throughout cancer programs of Catholic Health<br />
Initiatives, our parent organization.”<br />
However, the physical attributes of the new facility are<br />
just the beginning of the patient experience at The <strong>Cancer</strong><br />
Institute. Treating cancer successfully requires the very highest<br />
level of expert diagnosis, staging, and treatment planning that<br />
brings all the experts together in consultation, supported<br />
by state-of-the-art technology. The <strong>Cancer</strong> Institute is where<br />
renowned cancer experts and cutting-edge technologies<br />
meet old-fashioned personal attention under one roof.<br />
Multidisciplinary Treatment Planning<br />
The multidisciplinary care team includes specialists<br />
for each cancer type, experts in radiation, surgery and<br />
chemotherapy, support services, genetics counseling and<br />
a nurse coordinator who plays a crucial and supportive<br />
role in the patient’s experience.<br />
The team approach is implemented through the weekly<br />
multidisciplinary disease site-specific conference. “When<br />
patients leave at the end of this visit to The <strong>Cancer</strong> Institute,<br />
they will have seen all the specialists at one time,” Dr. Krasna<br />
explains. “The doctors revolve around the patient. The patient<br />
receives a single, customized, comprehensive treatment plan<br />
agreed to by all our experts.<br />
The <strong>Cancer</strong> Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> uses a<br />
multi-modality approach, customized to each patient, to<br />
deliver state-of-the-art cancer care and to provide patients<br />
with unprecedented access to clinical research.<br />
The Breast <strong>Center</strong><br />
The Colorectal Oncology <strong>Center</strong><br />
The Gynecologic Oncology <strong>Center</strong><br />
The Hodes Comprehensive Liver & Pancreas <strong>Center</strong><br />
The Radiation Oncology <strong>Center</strong><br />
The Thoracic Oncology <strong>Center</strong><br />
The Urologic Oncology <strong>Center</strong><br />
2 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
“This way, the patient is assured of getting the care that is<br />
best for him or her,” Dr. Krasna says. “We are fortunate<br />
that <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> recognizes the value of this<br />
approach for cancer patients and was willing to invest in the<br />
resources required to make The <strong>Cancer</strong> Institute a leader in<br />
this unique mission of care.”<br />
No resources have been spared when it comes to providing<br />
and developing the latest treatments either. “Advanced<br />
treatment often involves multi-modality therapies, combining<br />
surgery, radiation and/or chemotherapy,” according to<br />
Dr. Krasna. “This is the case with advanced lung cancer that<br />
involves not only the lung but also the lymph nodes in the<br />
middle of the chest.” Physicians are using an exciting, new<br />
triple modality approach – a hard-hitting combination of<br />
radiation therapy, chemotherapy and surgery – to remove<br />
the tumor. Clinical evidence supports that this combination<br />
can have a big impact on survival.<br />
“By using chemotherapy together with radiation in a certain<br />
timeframe, we can actually downstage the cancer and eradicate<br />
it from the lymph nodes of the center of the chest for many,<br />
though not all, patients,” says Dr. Ziv Gamliel, chief of Thoracic<br />
Surgery at The <strong>Cancer</strong> Institute. “The chemotherapy makes<br />
the tumor more sensitive to the radiation. It is now possible<br />
to treat stage III-A lung cancer patients and have a very high<br />
chance of success by combining the best practices at The<br />
<strong>Cancer</strong> Institute for all three modalities together.”<br />
At The Breast <strong>Center</strong>, patient care also follows the multidisciplinary<br />
model approach for every case. “We sit down with<br />
two to four pathologists in addition to medical oncologists,<br />
radiation oncologists, surgeons, reconstructive surgeons and<br />
other members of the team to discuss the subtleties of each<br />
diagnosis and to make sure the specific cell type or extent<br />
of the disease is accurately reflected before surgery takes<br />
place,” emphasizes Dr. Michael J. Schultz, medical director<br />
of The Breast <strong>Center</strong> at The <strong>Cancer</strong> Institute.<br />
Clinical Trials Reaching the Community<br />
The <strong>Cancer</strong> Institute at <strong>St</strong>. <strong>Joseph</strong> is honored to be the only<br />
Maryland hospital chosen for an unprecedented pilot program<br />
to extend the reach of NCI research and state-of-the-art<br />
treatment into community hospitals across the country. This<br />
exciting initiative expands the offerings of advanced clinical<br />
cancer trials, giving even more treatment options to cancer<br />
patients who come to <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>.<br />
“<strong>St</strong>udies indicate that patients treated in major cancer centers<br />
with access to clinical research may live longer with a greater<br />
chance of cancer cure,” Dr. Krasna says. “The three-year NCI<br />
Community <strong>Cancer</strong> <strong>Center</strong>s Program (NCCCP) expands<br />
clinical trial availability and will increase cancer survival for<br />
parts of our community who do not presently have access to<br />
this type of care. This is our dream: to see multidisciplinary<br />
care in the community and to see clinical trials and research<br />
also done in a community setting.”<br />
The <strong>Cancer</strong> Institute is making that dream a reality by not<br />
only providing advanced, patient-centered cancer care, but<br />
also by offering loving compassionate support for each<br />
patient’s journey through the battle with cancer.<br />
For more information about The <strong>Cancer</strong> Institute at<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> and the multidisciplinary approach<br />
to cancer care or about the NCI Community <strong>Cancer</strong> <strong>Center</strong>s<br />
Program, call <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>, 410-427-2551.<br />
“<br />
A patient may come from three to four hours<br />
away but when they leave at the end of their visit,<br />
they will have seen all the specialists at one time.<br />
The doctors revolve around the patient.<br />
Mark Krasna, M.D.<br />
“<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 3
The <strong>Cancer</strong> Institute<br />
Message from the <strong>Medical</strong> Director & Vice President<br />
Mark Krasna, M.D.<br />
<strong>Medical</strong> Director<br />
The <strong>Cancer</strong> Institute<br />
This has been an exciting year for the<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Cancer</strong> Institute. Since my<br />
arrival here in September of 2006, we<br />
have seen many changes to the face<br />
and mission of The <strong>Cancer</strong> Institute.<br />
The new <strong>Cancer</strong> Institute building has<br />
been completed and now occupies<br />
over 36,000 square feet of <strong>Medical</strong><br />
Building A. This brand new, state-ofthe-art<br />
facility is the first structure one<br />
sees when entering the <strong>St</strong>. <strong>Joseph</strong> campus from Osler Drive.<br />
The magnificent atrium on the building’s facade is comprised<br />
of a two-level glass space which encloses the chemotherapy<br />
infusion areas and the waiting room for our comprehensive<br />
Breast <strong>Center</strong>. The ground floor houses Radiation Oncology<br />
and a dedicated PET/CT scanner for The <strong>Cancer</strong> Institute, as<br />
well as cancer support services. It also includes all of <strong>Cancer</strong><br />
Research, as well as the Tumor Registry. Genetic counseling,<br />
psychosocial services, nurse navigators and a patient<br />
education area are located here as well. A <strong>Cancer</strong> Boutique<br />
and a cafe are scheduled to open in early 2008. The first floor<br />
features the Multidisciplinary Clinics, <strong>Medical</strong> Oncology,<br />
physician offices and <strong>Cancer</strong> Institute executive offices,<br />
in addition to the stunning infusion area. The second floor<br />
is mainly devoted to The Breast <strong>Center</strong> and dedicated Breast<br />
Imaging <strong>Center</strong>.<br />
As exciting as the new construction is, we are just as proud<br />
of the new recruits who have joined us. We are delighted<br />
with our new medical oncologists, Drs. Richard Schraeder and<br />
Rima Couzi, who are working hand-in-hand with the radiation<br />
oncologists and surgeons in The <strong>Cancer</strong> Institute. To add to<br />
the energy, our new cancer surgeons, Drs. Richard Mackey,<br />
Robert Akbari and Linda Martin, have all hit the ground<br />
running and are demonstrating themselves to be excellent<br />
clinicians and cancer team players. Operationalizing our<br />
new Multidisciplinary Clinics, PET/CT and Breast Imaging has<br />
been an exciting undertaking for our new director of <strong>Cancer</strong><br />
Services, Monica Fulton, who brought with her experience<br />
in managing a community cancer center in the Dana Farber<br />
system in Boston. She has met the challenge with vigor and<br />
a sense of mission.<br />
The Multidisciplinary Clinics and prospective case conferences<br />
are the centerpieces of The <strong>Cancer</strong> Institute. These programs<br />
embody the spirit of coordinated care and single out <strong>St</strong>. <strong>Joseph</strong><br />
as an institution where collaboration and team planning are<br />
focused on what is best for our patients. The synergy of the<br />
building and the dedicated staff who work here have come<br />
together to ease cancer patients’ journeys from diagnosis<br />
through treatment during one of the most difficult times in<br />
their lives.<br />
Finally, our Tumor Registry and Research staffs have worked<br />
tirelessly to open more opportunities for our patients to enter<br />
clinical trials. This commitment and dedication have been<br />
recognized by our parent organization, CHI – Catholic Health<br />
Initiatives – who has established a Catholic Health Oncology<br />
Network (CHON) with <strong>St</strong>. <strong>Joseph</strong> at the helm. This work has<br />
also been recognized by Dr. John Niederhuber and the National<br />
<strong>Cancer</strong> Institute (NCI) who have chosen <strong>St</strong>. <strong>Joseph</strong> and four<br />
other hospitals in the CHI system as National Community<br />
<strong>Cancer</strong> <strong>Center</strong> Network Pilot Program participants (NCCCP).<br />
This exciting, new initiative will bring research opportunities<br />
and new research staff to <strong>St</strong>. <strong>Joseph</strong> <strong>Cancer</strong> Institute patients<br />
through the NCI grant.<br />
We hope that this coming year is as successful as the<br />
past one, and that, as our numbers of patients grow,<br />
so will our successful mission of delivering the best,<br />
compassionate multidisciplinary care available in our<br />
Maryland regional community.<br />
Mark Krasna, M.D,<br />
<strong>Medical</strong> Director,<br />
The <strong>Cancer</strong> Institute<br />
Lucy Shamash,<br />
Vice President, Operations<br />
and The <strong>Cancer</strong> Institute<br />
4 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
The <strong>Cancer</strong> Institute<br />
<strong>Cancer</strong> Liason Physician <strong>Annual</strong> Report<br />
Maen Farha, M.D.<br />
<strong>Cancer</strong> Liasion Physician<br />
The <strong>Cancer</strong> Institute<br />
In some ways, <strong>Cancer</strong> Liaison<br />
Physicians (CLPs) are the guardians<br />
of their medical center’s cancer<br />
program. Each cancer program in<br />
the U.S. that is accredited by the<br />
Commission on <strong>Cancer</strong> is required to<br />
have a CLP. It is my honor to be the CLP<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> during<br />
the creation of The <strong>Cancer</strong> Institute.<br />
has been implemented for breast cancer, thoracic malignancies<br />
and gastrointestinal tumors.<br />
The <strong>Cancer</strong> Liaison Program is a grass-root network of 1,600<br />
physicians volunteers (CLPs) whose primary roles are to:<br />
• Serve as the physician champion within the cancer program<br />
• Serve as the liaison between CoC and the cancer program<br />
• Serve as an agent of change within the community<br />
The CoC was founded by the American College of Surgeons<br />
in 1922 and has been inspecting hospital cancer programs and<br />
approving those that meet its stringent standards. The CoC<br />
reviews cancer programs every three years to determine their<br />
compliance with its standards. Twenty-five percent of U.S.<br />
hospitals are CoC approved, but they collectively care for<br />
80 percent of new cancer patients.<br />
MISSION STATEMENT<br />
“The Commission on <strong>Cancer</strong> (CoC) is a consortium<br />
of professional organizations dedicated to improving<br />
survival and quality of life for cancer patients through<br />
standard-setting, prevention, research, education<br />
and the monitoring of quality care.”<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>’s cancer program was reapproved<br />
in 2005 and the CoC will be back next spring to evaluate our<br />
program. We look forward to that with anticipation because<br />
the recent expansion of our cancer program has already<br />
begun to bear fruit and is making a difference in cancer<br />
patients’ care. One of the most impressive initiatives is the<br />
implementation of multidisciplinary prospective Tumor Board.<br />
Specialists from multiple disciplines, including many types of<br />
non-physician providers, confer to plan the treatment of our<br />
cancer patients. The result is always superior to what we can<br />
individually accomplish, since many minds come together to<br />
share expertise and create a treatment plan that is always<br />
rich, intelligent and abundantly detailed for each patient. This<br />
This role has been an enriching and positive experience for<br />
me. In this capacity during the past year, accomplishments<br />
have included:<br />
• Reporting regularly to the <strong>Cancer</strong> Committee including<br />
sharing our NCDB data and comparison to national<br />
benchmarks<br />
• Working closely with tumor registrars and registry to improve<br />
the quality and completeness of our reporting<br />
• Establishing initial relations with the American <strong>Cancer</strong><br />
Society and inviting our ACS Liaison to our <strong>Cancer</strong><br />
Committee meetings<br />
• Establishing initial connection with the <strong>St</strong>ate <strong>Cancer</strong> Control<br />
program and inviting them to present an overview of the<br />
program at our cancer conference<br />
• Attending the annual meeting of the CoC at the clinical<br />
Congress of the American College of Surgeons<br />
What is the value of all that data entry to the NCDB and<br />
the SEER database?<br />
Tumor registrars from the 1,500 or more approved institutions<br />
enter extensive data into that database about each patient<br />
treated at an institution. To date, 20 million patients are in<br />
the database with good solid data on demographics, stage,<br />
treatment and survival. This is a massive amount of data that<br />
can be “farmed” to answer questions that may otherwise be<br />
impossible to answer in a scientific manner. Recent examples<br />
are data analysis that showed that having colon resections<br />
with larger number of lymph nodes in the specimen confers<br />
higher survival rates and that resecting primary tumors in<br />
patients with metastatic breast cancer is associated with<br />
increased survival. Plus, there have been similarly difficult<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 5
The <strong>Cancer</strong> Institute<br />
<strong>Cancer</strong> Liason Physician <strong>Annual</strong> Report (continued)<br />
questions that we have argued about without clear data other<br />
than a few series involving a handful of patients before the<br />
database was created. I believe that this orchard is definitely<br />
ripe for the picking and that the data should be accessed by<br />
all who are interested.<br />
On an institutional level, our data is very useful in that we<br />
can measure our performance against others and we can<br />
measure our compliance with standards set by the CoC. Four<br />
standards are being scrutinized (three for breast cancer and<br />
one for colon) through eQuIPs (Electronic Quality Improvement<br />
Packets). An example is a standard that calls for administering<br />
radiation therapy to patients under 70 years of age after breastconserving<br />
therapy for breast cancer. The challenge is that,<br />
in addition to offering the treatment, the documentation has to<br />
be available to our tumor registrars and that information has to<br />
be entered into the NCDB. I encourage everyone to cooperate<br />
with our registry staff by providing complete information. There<br />
is a strong push in Washington to tie physician and hospital<br />
reimbursement into meeting these standards (P4P).<br />
A year ago, I was asked to perform the CLP role and I accepted<br />
it because, with limited knowledge of its details, I thought it<br />
was a “good” thing to do. As the year passed and I became<br />
more familiar with the role’s details, I began to appreciate<br />
what a worthwhile endeavor this is, and I have found it a very<br />
fulfilling experience. I want to acknowledge the dedication of<br />
the many physicians who, in addition to providing high quality<br />
care, supply the registry with stage and survival data on their<br />
patients; the tumor registry staff who work collecting and<br />
entering the data and the hospital leadership that continues<br />
their strong commitment to our <strong>Cancer</strong> Institute.<br />
What are the CLP and CoC objectives for next year?<br />
The areas of interest for CLPs as determined at the last<br />
meeting of the CoC are: quality improvement, advocacy, ACS<br />
partnership, clinical trials and comprehensive cancer control.<br />
The CoC defined an objective for next year around each focus<br />
area, and here are the objectives:<br />
• Facilitate the utilization of eQuIP to promote quality care<br />
for breast and colorectal cancer<br />
• Work with the American <strong>Cancer</strong> Society <strong>Cancer</strong> Action<br />
Network (ACS-CAN) in the area of legislative and<br />
regulatory advocacy<br />
• Bring ACS staff to the <strong>Cancer</strong> Committee table and facilitate<br />
ACS interaction with the cancer program staff<br />
• Increase enrollment of patients into clinical trials by<br />
championing implementation and recruitment<br />
• Present the state cancer plan to the <strong>Cancer</strong> Committee<br />
and define ways to become involved<br />
6 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
<strong>Cancer</strong> Institute Registry Activity<br />
Data Analysis<br />
2006 Five Most Frequent <strong>Cancer</strong> Sites<br />
The most frequently diagnosed cancer at <strong>St</strong>. <strong>Joseph</strong> in 2006<br />
was Breast, which represented 19.0% of our cases. Prostate was<br />
the second most often diagnosed cancer at <strong>St</strong>. <strong>Joseph</strong> during<br />
this same time period, accounting for 16.1% of our 2006<br />
caseload. Colorectal diagnosis represented 11.8%, followed by<br />
Lung/Bronchus, which comprised 11.0% of the annual cases.<br />
Skin was the fifth most diagnosed cancer at 7.6%.<br />
Breast<br />
Prostate<br />
Colorectal<br />
Lung/Bronchus<br />
11.8%<br />
11.0%<br />
16.1%<br />
19.0%<br />
Skin<br />
7.6%<br />
0 5 10 15 20<br />
Source: <strong>St</strong>. <strong>Joseph</strong> <strong>Cancer</strong> Institute Registry<br />
Follow-Up<br />
Follow-up activity affords the opportunity to collect information<br />
about additional treatment and aids in the identification of those<br />
patients with cancer who have had local recurrence, metastases<br />
or who have been diagnosed with an additional primary cancer.<br />
Follow-up letters to physicians also serve as a reminder to contact<br />
patients they may not have seen in the past year. The <strong>St</strong>. <strong>Joseph</strong><br />
<strong>Cancer</strong> Institute Registry currently has 9,039 cases under active<br />
follow-up, with an average follow-up rate of 94.3%.<br />
<strong>St</strong>. <strong>Joseph</strong> Follow-Up Rate 2006<br />
Total number of cases under active follow-up:<br />
9,039<br />
Total number of cases with current follow-up data:<br />
8,521 (94.3%)<br />
<strong>St</strong>aging<br />
The American College of Surgeons Commission on <strong>Cancer</strong><br />
mandates that all newly diagnosed cancer cases be American<br />
Joint Committee on <strong>Cancer</strong> (AJCC) TNM-staged at initial<br />
diagnosis by the managing physician. The AJCC TNM staging<br />
system is a classification scheme used to assess the extension<br />
and growth of a tumor, involvement of lymph nodes and<br />
metastasis to any distant site at the time of diagnosis. This<br />
staging system was developed to provide consistency in cancer<br />
care and give physicians important information necessary to<br />
choose the most appropriate treatment interventions.<br />
AJCC <strong>St</strong>age at<br />
Diagnosis<br />
ST. JOSEPH<br />
MEDICAL CENTER<br />
2006 FIVE MOST<br />
FREQUENT SITES<br />
Source: <strong>St</strong>. <strong>Joseph</strong> <strong>Cancer</strong><br />
Institute Registry<br />
<strong>St</strong>age 0<br />
<strong>St</strong>age I<br />
<strong>St</strong>age II<br />
<strong>St</strong>age III<br />
<strong>St</strong>age IV<br />
Unknown<br />
Lung/<br />
Breast Prostate Colorectal Bronchus Skin<br />
17.6% 0% 14.8% 0% 37.8%<br />
42.9% 0% 27.3% 32.6% 46.7%<br />
23.9% 80.6% 22.7% 7.1% 6.7%<br />
7.8% 12.9% 25.8% 19.0% 5.5%<br />
3.4% 3.2% 6.3% 27.0% 0%<br />
4.4% 3.2% 3.1% 14.3% 3.3%<br />
<strong>St</strong>age 0 – Carcinoma in situ –<br />
an early form of carcinoma.<br />
<strong>St</strong>age I – Localized to one<br />
part of the body.<br />
<strong>St</strong>age II – Involves regional<br />
lymph nodes.<br />
<strong>St</strong>age III – Locally advanced.<br />
<strong>St</strong>age IV – Metastasized<br />
or spread to other organs<br />
throughout the body.<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 7
10 Most Frequent <strong>Cancer</strong><br />
Sites by Gender<br />
2006 NATIONAL* AND ST. JOSEPH<br />
COMPARATIVE INCIDENCE<br />
*Source: American <strong>Cancer</strong> Society<br />
Female<br />
National*<br />
<strong>St</strong>. <strong>Joseph</strong><br />
Breast 31% 19.0%<br />
Lung 12% 6.6%<br />
Colorectal 11% 6.6%<br />
Corpus Uteri 6% 5.1%<br />
Ovary 3% 1.6%<br />
Non-Hodgkins<br />
Lymphoma 4% 1.0%<br />
Skin 4% 3.5%<br />
Thyroid 3% 0.4%<br />
Pancreas 2% 1.5%<br />
Bladder 2% 2.0%<br />
Male<br />
National*<br />
<strong>St</strong>. <strong>Joseph</strong><br />
Prostate 33% 16.1%<br />
Lung 13% 6.0%<br />
Colorectal 10% 6.9%<br />
Bladder 6% 3.3%<br />
Skin 5% 5.2%<br />
Non-Hodgkins<br />
Lymphoma 4% 0.6%<br />
Kidney 3% 2.4%<br />
Pancreas 2% 1.9%<br />
Leukemia 3% 0.5%<br />
Oral 3% 0.3%<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> 2006 Primary Site Table<br />
Non-<br />
Total<br />
Primary Site Analytic* Analytic** Male Female Cases<br />
Breast 205 29 1 233 234<br />
Prostate 155 19 174 N/A 174<br />
Colorectal 128 17 74 71 145<br />
Lung/Bronchus 124 12 65 71 136<br />
Skin 90 4 56 38 94<br />
Cervix Uteri 55 2 N/A 57 57<br />
Urinary Bladder 46 12 36 22 58<br />
Kidney/Renal/Pelvis &<br />
Other Urinary Organs 33 7 26 14 40<br />
Pancreas 32 4 20 16 36<br />
Corpus Uteri 32 5 N/A 37 37<br />
Unknown/III Defined Sites 28 9 14 23 37<br />
Lymphomas 21 1 8 14 22<br />
Ovary 17 4 N/A 21 21<br />
Brain/Meninges/CNS 14 1 6 9 15<br />
Esophagus 11 5 11 5 16<br />
Liver/Intrahepatic Bile Duct 11 1 9 3 12<br />
Gallbladder/Other Biliary 11 1 5 7 12<br />
<strong>St</strong>omach 10 1 7 4 11<br />
Small Intestine 8 1 4 5 9<br />
Thyroid & Oth. Endocrine 8 1 5 4 9<br />
Hematopoietic/Reticuloendo 6 2 5 3 8<br />
Penis/Testis 6 1 7 N/A 7<br />
Oral Cavity 5 0 3 2 5<br />
Myeloma 5 3 6 2 8<br />
Anus 4 0 2 2 4<br />
Vulva/Vagina 3 1 N/A 4 4<br />
Other Female Genital Site 3 1 N/A 4 4<br />
Larynx/Nasal/Sinuses 2 3 5 0 5<br />
Mesothelioma 2 0 1 1 2<br />
Soft Tissue 2 2 2 2 4<br />
Other Male Genital Site 1 0 1 N/A 1<br />
Retroperitoneum/Peritoneum 0 0 0 0 0<br />
Other Digestive Organs 0 1 0 1 1<br />
Eye & Orbit 0 4 3 1 4<br />
Totals 1078 154 556 676 1232<br />
*ANALYTIC – Any or all of the first course of therapy completed at the reporting facility.<br />
*NON-ANALYTIC – Cases not receiving any first course of therapy at the reporting facility.<br />
8 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
Focus on Non-Small Cell Lung <strong>Cancer</strong><br />
In-Depth Site <strong>St</strong>udy<br />
Ziv Gamliel, M.D., F.A.C.S.<br />
Chief, Thoracic Surgery<br />
With over 185,000 new cases annually,<br />
non-small cell lung cancer remains<br />
the number one cancer killer in the<br />
United <strong>St</strong>ates, claiming more than<br />
150,000 lives each year. While the great<br />
majority of lung cancer patients are<br />
males in their 70s who are current or<br />
former smokers, there is a disturbing<br />
trend of increasing numbers of women<br />
and nonsmokers who are being diagnosed with lung cancer<br />
at younger ages, often in their 40s or 50s.<br />
Survival rates and optimal treatment regimens vary according<br />
to disease stage. Historically, overall cure rates have averaged<br />
roughly 13 percent. However, exciting recent developments<br />
in early detection methods, accurate pretreatment staging,<br />
minimally invasive surgical techniques and aggressive<br />
multi-modality treatment regimens have brought with<br />
them renewed optimism in the fight against lung cancer.<br />
The Thoracic Oncology <strong>Center</strong><br />
Recognizing the importance of providing the community<br />
with the most advanced lung cancer care available, The<br />
<strong>Cancer</strong> Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> established<br />
an outstanding Thoracic Oncology <strong>Center</strong> in 2006.<br />
Dr. Mark J. Krasna, a nationally recognized expert in<br />
Thoracic Oncology, was recruited to serve as The <strong>Cancer</strong><br />
Institute’s medical director. Dr. Ziv Gamliel was recruited<br />
to serve as chief of Thoracic Surgery. They were joined<br />
by Dr. Lope T. Villa, a longstanding member of the<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> staff, to form the surgical<br />
faculty of The Thoracic Oncology <strong>Center</strong>. An additional<br />
thoracic surgeon, Dr. Linda Martin, was recruited in <strong>2007</strong>.<br />
The Radiation Oncology department, under the direction of<br />
Dr. Jason Citron, offers state-of-the-art radiotherapy techniques<br />
to patients with lung cancer. <strong>Medical</strong> Oncology services are<br />
provided by Dr. Richard Schraeder, Jr., and Dr. Rima Couzi,<br />
both recruited in <strong>2007</strong>, as well as Dr. Hecter Silva and<br />
colleagues. Comprehensive Pathology services are provided<br />
by Dr. James Eagan and colleagues. Using state-of-the-art<br />
equipment, expertise in Diagnostic Radiology is provided<br />
by Dr. Fred Yeganeh and in Interventional Radiology by<br />
Dr. Margaret A. Lynch-Nyhan.<br />
Participants in The Thoracic Oncology <strong>Center</strong> from the<br />
division of Pulmonary and Critical Care Medicine include<br />
Dr. Hassan M. Makhzoumi, as well as Dr. John H. Eppler, Jr.,<br />
and colleagues. Participants from the division of<br />
Gastroenterology include Dr. <strong>St</strong>even A. Fleisher, as well as<br />
Dr. Neil D. Goldberg and colleagues. Support is also provided by<br />
Dr. Neal Naff and colleagues from the division of Neurosurgery,<br />
as well as by Dr. Mark H. Fraiman and colleagues from the<br />
division of Hepatobiliary Surgery. Counseling on smoking<br />
cessation is provided by Christine Schutzman.<br />
Multidisciplinary Thoracic Oncology Clinic and<br />
Tumor Conference<br />
Increasingly, the management of thoracic malignancies in<br />
general, and lung cancer in particular, involves the use of<br />
multiple treatment modalities in various combinations. In<br />
the last few years, clinical trials have demonstrated that<br />
patients undergoing surgery for most early stages of lung<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 9
Focus on Non-Small Cell Lung <strong>Cancer</strong><br />
In-Depth Site <strong>St</strong>udy (continued)<br />
cancer can benefit from postoperative adjuvant chemotherapy.<br />
For locally advanced lung cancers, curative surgical resection<br />
has been made possible by pretreatment with neoadjuvant<br />
concurrent chemotherapy and radiation. More than ever<br />
before, the safe and effective delivery of modern lung cancer<br />
care is dependent upon close cooperation and constant<br />
communication between health care providers with many<br />
different areas of expertise. At <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>,<br />
coordination of multidisciplinary lung cancer care in<br />
The Thoracic Oncology <strong>Center</strong> is accomplished in several<br />
different ways.<br />
Table 1<br />
Number and gender distribution of patients<br />
with non-small cell lung cancer evaluated<br />
and/or treated at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>,<br />
by year.<br />
Year Patients Females<br />
2001 67 52.2%<br />
2002 69 59.4%<br />
2003 71 50.7%<br />
2004 77 40.3%<br />
2005 77 55.3%<br />
2006 64 54.7%<br />
New patients seeking lung cancer care at <strong>St</strong>. <strong>Joseph</strong><br />
<strong>Medical</strong> <strong>Center</strong> are encouraged to undergo initial evaluation<br />
in the multidisciplinary Thoracic Oncology Clinic. During a<br />
single clinic visit, the multidisciplinary team revolves around the<br />
patient both figuratively and literally. Lung cancer patients are<br />
evaluated by a thoracic surgeon, medical oncologist, radiation<br />
oncologist, smoking cessation counselor and nurse coordinator.<br />
Patients, together with their loved ones, meet with all the above<br />
health care professionals without even having to move from one<br />
room to another. Not only for local patients, but especially for<br />
patients traveling long distances in order to obtain their care<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>, eliminating the need for multiple<br />
trips to different offices on different days both facilitates and<br />
expedites multidisciplinary evaluation and treatment.<br />
Later on the same day of the multidisciplinary evaluation,<br />
cases are discussed in a multidisciplinary conference during<br />
which biopsy slides are reviewed by participating pathologists,<br />
and radiological imaging studies are reviewed by participating<br />
radiologists. Within hours of a multidisciplinary evaluation,<br />
based upon group consensus at the Tumor Conference, a<br />
comprehensive evaluation and treatment plan is formulated<br />
for each lung cancer patient with input from surgeons, medical<br />
oncologists, radiation oncologists and pulmonologists. The<br />
close cooperation and streamlined communication between all<br />
of the above specialists makes it possible to provide complex,<br />
comprehensive care that is individually tailored to each patient’s<br />
specific circumstances.<br />
Communication between patients and their physicians is of<br />
utmost importance. Such communication can be particularly<br />
confusing and complicated when multiple treating physicians<br />
are involved. The Thoracic Oncology <strong>Center</strong> at <strong>St</strong>. <strong>Joseph</strong><br />
utilizes nurse coordinators to oversee scheduling of tests,<br />
10 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
Table 2<br />
Geographic distribution of patients evaluated and/or treated<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> between 2001 and 2006.<br />
Baltimore County<br />
Baltimore City<br />
Harford County<br />
Carroll County<br />
Other<br />
2.4%<br />
6.1%<br />
9.6%<br />
13.4%<br />
appointments, treatments and surgery for each patient<br />
undergoing multidisciplinary evaluation and treatment.<br />
The nurse coordinators meet the patients at their<br />
multidisciplinary clinic appointment and participate in<br />
the multidisciplinary Thoracic Oncology conference.<br />
After a patient’s case is discussed at the multidisciplinary<br />
conference, their nurse coordinator reinforces the<br />
management plan to them on behalf of all of the physicians<br />
involved. Having a nurse coordinator involved in their care<br />
greatly alleviates patients’ anxiety and increases patients’<br />
confidence as well as their knowledge about their care.<br />
Aggressive Pretreatment <strong>St</strong>aging<br />
68.5%<br />
0 5 10 15 ... 60 65<br />
The optimal management of non-small cell lung cancer is<br />
highly dependent upon the stage of the disease. A serious<br />
consequence of incorrect staging is that it can lead to incorrect<br />
treatment. In some cases, standard radiological imaging studies<br />
may fail to identify the true extent of a patient’s disease, which<br />
is how incorrect staging can occur. In our efforts to maintain<br />
an unsurpassed standard of excellence in radiological imaging,<br />
The <strong>Cancer</strong> Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> has<br />
recently acquired a state-of-the-art PET/CT scanner with<br />
which high-speed/high-resolution CT images of a patient<br />
can be obtained simultaneously with PET images. In order<br />
to enhance the diagnostic usefulness of this imaging and in<br />
order to avoid performing a separate contrast-enhanced CT<br />
scan, intravenous contrast is administered during the PET/CT<br />
scan, allowing both scans to be accomplished at once. The<br />
high-quality imaging that results allows detection of very subtle<br />
but critically important metastatic disease that might otherwise<br />
go unrecognized.<br />
In non-small cell lung cancer, involvement of lymph nodes in<br />
the mediastinum has a major negative impact on the likelihood<br />
of accomplishing curative surgery. While CT scans and PET<br />
scans can often identify metastatic involvement of mediastinal<br />
lymph nodes, microscopic involvement of these nodes with<br />
tumor can easily be missed. Mediastinoscopy is a minimally<br />
invasive outpatient surgical technique in which mediastinal<br />
lymph nodes are sampled and microscopic metastatic<br />
disease can be identified. At <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>,<br />
mediastinoscopy is used routinely in non-small cell lung<br />
cancer patients in order to rule out mediastinal lymph node<br />
involvement before surgical resection is undertaken. Often,<br />
patients whose CT scans and PET scans failed to reveal any<br />
metastatic cancer in their mediastinal lymph nodes are<br />
found to have microscopic lymph node involvement using<br />
mediastinoscopy. Knowing about this type of microscopic<br />
metastatic disease is vital before treatment is undertaken,<br />
Never Smoked<br />
10.4%<br />
Table 3<br />
Smoking status of patients with<br />
non-small cell lung cancer evaluated<br />
and/or treated at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong><br />
<strong>Center</strong> between 2001 and 2006.<br />
Previous Smokers<br />
Current Smokers<br />
Unknown 3.1%<br />
30.1%<br />
56.5%<br />
0 10 20 30 40 50<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 11
Focus on Non-Small Cell Lung <strong>Cancer</strong><br />
In-Depth Site <strong>St</strong>udy<br />
(continued)<br />
in order to ensure that the best treatment strategy is applied.<br />
Patients with unrecognized mediastinal lymph node metastases<br />
who undergo major operations to remove their cancer are<br />
unlikely to be cured by their surgery. By identifying microscopic<br />
mediastinal lymph node involvement, mediastinoscopy can<br />
ensure that patients do not undergo major surgery that is<br />
unlikely to result in a cure. Instead, more appropriate treatment<br />
methods with a higher likelihood of success can be offered.<br />
Expanded Minimally Invasive Surgery Capabilities<br />
Patients with non-small cell lung cancer whose tumor has<br />
not yet spread beyond the lung have a significant chance to<br />
be cured by surgical removal of the tumor. While limited<br />
operations such as “wedge” resections can be curative, the<br />
likelihood of remaining free of disease is greater in patients<br />
who undergo complete removal of the entire lobe in which<br />
the cancer is located, using formal anatomic dissection.<br />
Increasingly, during the last 10 years, surgeons have used<br />
minimally invasive surgical techniques aided by slender<br />
telescopes and instruments in order to perform lung operations<br />
through very small incisions. These smaller incisions decrease<br />
the extent and duration of postoperative disability and allow<br />
an earlier return to normal functioning. In contrast, the<br />
standard surgical approach has involved making large incisions<br />
and spreading the ribs apart in order to gain access to the lung.<br />
Due to the added complexity of minimally invasive surgery<br />
techniques, surgeons who lack experience with these techniques<br />
are often restricted in the extent of surgical procedure they<br />
are capable of performing and may be limited to performing<br />
thoracoscopic “wedge” resections for lung cancer. However,<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>, minimally invasive surgery<br />
techniques are now regularly used to perform procedures that<br />
most other centers are only able to offer using large incisions.<br />
The same anatomic dissection and surgical principles that<br />
would be used in open surgical procedures are always applied<br />
to minimally invasive procedures as well. Thoracoscopic<br />
lobectomy is routinely performed at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong><br />
using meticulous individual dissection and ligation of anatomic<br />
structures through three, small thoracoscopy port sites, the<br />
largest of which typically measures less than two inches.<br />
Tri-Modality Therapy for Locally<br />
Advanced Lung <strong>Cancer</strong><br />
The optimal treatment of lung cancer that has not spread to<br />
distant organ sites is surgical removal. Sometimes, however,<br />
the cancer has advanced locally to the point that complete<br />
surgical removal is not technically feasible. This is the case<br />
in stage III lung cancer.<br />
Recently, there has been increasing evidence that “triple<br />
modality” treatment with chemotherapy, radiation therapy<br />
and surgery results in greatly improved cure rates for locally<br />
advanced lung cancer. Due to the logistical complexity of<br />
coordinating patient care between three different specialists,<br />
and due to the technical challenges of performing surgery on<br />
such patients, most hospitals in the United <strong>St</strong>ates do not offer<br />
such sophisticated treatment. Tri-modality treatment of locally<br />
advanced lung cancer has been performed mainly in a limited<br />
number of large university centers. In a warm and caring<br />
Table 4<br />
Comparative stage distribution<br />
of patients with non-small cell<br />
lung cancer<br />
<strong>Cancer</strong> <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> National<br />
<strong>St</strong>age 2001– 2006 1996 – 2003<br />
Localized 41% 16%<br />
Regional 17% 35%<br />
Distant 31% 42%<br />
Unstaged 11% 7%<br />
12 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
community setting, The Thoracic Oncology <strong>Center</strong> at<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> now has the necessary tools and<br />
expertise to provide even the most challenging locally<br />
advanced lung cancer cases with tri-modality treatment that<br />
is second-to-none.<br />
One example of stage III lung cancer that can benefit from<br />
triple modality treatment is disease that has spread locally to<br />
regional lymph nodes in the mediastinum. Another example<br />
of locally advanced lung cancer involves cancer arising at the<br />
top of the lung that has invaded the nerves and/or blood<br />
vessels of the arm. In these situations, surgical removal without<br />
any other treatment is very unlikely to be curative and the<br />
cancer usually recurs. Combined treatment with chemotherapy<br />
and radiation therapy is effective at decreasing the extent of the<br />
cancer and is better than surgery alone. Even with combined<br />
chemotherapy and radiation therapy, cure rates have remained<br />
rather low.<br />
However, locally advanced lung cancer that responds well<br />
to combined chemotherapy and radiation therapy can often<br />
be completely removed. The response of lung cancer to<br />
combined chemotherapy and radiation therapy is better in<br />
patients receiving relatively high doses of radiation therapy.<br />
Because radiation therapy results in inflammation and scar<br />
tissue formation, performing lung surgery on patients who have<br />
undergone such treatment is much more difficult than usual.<br />
The risk of complications can also be higher. For well over ten<br />
years, Drs. Krasna, Gamliel and Martin have been operating<br />
on lung cancer patients who have undergone combined<br />
chemotherapy and high-dose radiation therapy with enviably<br />
low complication rates, thus making it possible to implement the<br />
high standard of tri-modality treatment offered at The Thoracic<br />
Oncology <strong>Center</strong>.<br />
Improved Palliation Capabilities<br />
The goal of lung cancer treatment must not be limited<br />
to achieving a cure. For many patients whose lung cancer is<br />
not curable, relief of symptoms is essential. These patients<br />
may become short of breath for a variety of reasons. Most<br />
commonly, their shortness of breath is due to buildup of<br />
fluid in the chest cavity or due to airway obstruction by<br />
tumor. Obtaining rapid relief of their shortness of breath<br />
using minimally invasive methods can allow these patients<br />
to stay out of the hospital and regain quality of life.<br />
When advanced lung cancer results in fluid buildup in the<br />
chest cavity, the lung has less space for inflation. One-time<br />
drainage of the fluid provides only temporary relief, since the<br />
fluid will rapidly reaccumulate. One method for preventing<br />
fluid reaccumulation is to instill sterile powdered talc onto<br />
the lung using minimally invasive thoracoscopy through a tiny<br />
incision. The resulting inflammation causes the formation of<br />
adhesions between the lung and the rib cage, called pleurodesis,<br />
effectively obliterating the space where fluid might accumulate.<br />
In certain cases where the lung cannot reexpand due to a<br />
restricting rind of tumor, convenient long-term drainage can<br />
be achieved using an indwelling tunneled catheter. Patients<br />
are able to drain the fluid from their chest cavity at home by<br />
themselves as often as necessary, using convenient prepackaged<br />
sterile supplies. Often, after a couple of months of intermittent<br />
drainage at home, the fluid stops reaccumulating.<br />
Table 5<br />
Number of patients with<br />
non-small cell lung cancer<br />
undergoing mediastinoscopy,<br />
surgical resection, neoadjuvant<br />
(preoperative) therapy and<br />
adjuvant (postoperative) therapy<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>,<br />
by year.<br />
Year Mediastinoscopy Neoadjuvant Surgical Resection Adjuvant<br />
2001 0 1 23 1<br />
2002 5 0 24 4<br />
2003 2 0 31 1<br />
2004 1 1 32 0<br />
2005 9 1 28 3<br />
2006 7 2 28 2<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 13
Focus on Non-Small Cell Lung <strong>Cancer</strong><br />
In-Depth Site <strong>St</strong>udy<br />
(continued)<br />
Table 6<br />
Comparative overall three-year survival rates for patients<br />
with non-small cell lung cancer, by stage.<br />
<strong>Cancer</strong> <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> National<br />
<strong>St</strong>age 2001– 2006 1988 – 2003<br />
Localized 62.1% 58.0%<br />
Regional 18.6% 20.8%<br />
Distant 3.8% 4.5%<br />
Unstaged 11.6% 14.3%<br />
Patients with advanced lung cancer may develop airway<br />
obstruction due to their tumor. Such airway obstruction<br />
can often be relieved with conventional radiation therapy,<br />
but this treatment method may require several weeks to<br />
produce results and not all patients are suitable candidates.<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> now offers bronchoscopic tumor<br />
ablation and airway stenting. Using the Nd:YAG laser through<br />
a fiberoptic video bronchoscope, thoracic surgeons are able<br />
to essentially vaporize a tumor blocking a patient’s airway.<br />
In cases where a tumor is causing external compression of<br />
the airway, an expandable stent can be deployed into the<br />
airway in order to keep it open. These interventions typically<br />
produce instantaneous results and can usually be performed<br />
on an outpatient basis.<br />
Availability of Clinical Trials<br />
The nature of cancer treatment is continually evolving.<br />
Rather than follow others, The Thoracic Oncology <strong>Center</strong> at<br />
<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> is striving to lead the fight against<br />
lung cancer. As an accredited center with the South West<br />
Oncology Group (SWOG) and with the Radiation Therapy<br />
Oncology Group (RTOG), we can now offer many of our<br />
patients the opportunity to participate in exciting clinical trials<br />
that will help to establish the standard of care for tomorrow.<br />
Future Directions<br />
The future of lung cancer care is exciting. The Thoracic<br />
Oncology <strong>Center</strong> at <strong>St</strong>. <strong>Joseph</strong> is poised to achieve prominence<br />
as a leader in many aspects of lung cancer care. Already in<br />
<strong>2007</strong>, aggressive pretreatment staging including routine use<br />
of mediastinoscopy has improved our ability to make optimal<br />
treatment decisions for our patients. Our patients with early<br />
stages of lung cancer have been undergoing thoracoscopic<br />
lobectomy and enjoying faster than ever recuperation. Patients<br />
with regionally advanced lung cancer have been undergoing<br />
tri-modality therapy, including high-dose radiotherapy and<br />
surgery, with low complication rates and excellent results.<br />
Aggressive management of obstructing airway tumors using<br />
lasers and stents has helped patients to regain quality of life.<br />
As The Thoracic Oncology <strong>Center</strong> establishes itself as a local<br />
and regional leader in lung cancer care, we will need to share<br />
and compare our results with other centers. Toward this end,<br />
we are planning to undertake full participation in the Society<br />
of Thoracic Surgeons clinical database. We are expecting to<br />
14 | ST. JOSEPH MEDICAL CENTER sjmcmd.org
treat ever increasing numbers of patients from outside<br />
Baltimore City, Baltimore County and Harford County<br />
and have already seen a dramatic increase in the number<br />
of patients traveling to our center from over two hours away.<br />
In order to allow these patients to receive all of their care<br />
at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>, we are seeking a commitment<br />
from the American <strong>Cancer</strong> Society to establish a Hope Lodge<br />
that will provide nearby free accommodations for patients<br />
undergoing treatment and/or their family members. We<br />
are also exploring new treatment strategies to offer patients<br />
with malignant pleural effusions, including intrapleural<br />
hyperthermic chemotherapy.<br />
As our Thoracic Oncology <strong>Center</strong> evolves and expands, striving<br />
for ever increasing excellence, we must never lose sight of our<br />
other core values: reverence, integrity and compassion. For<br />
while our patients will always continue to seek us out for our<br />
excellence, it is our adherence to these other core values that<br />
truly sets <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> apart from the rest.<br />
<strong>2007</strong> <strong>Cancer</strong> Committee Members<br />
Arthur Serpick, M.D.<br />
Chairman<br />
Lucy Shamash, R.N., M.A.<br />
V. P. <strong>Cancer</strong> Institute<br />
Howard Berg, M.D.<br />
Colon and Rectal Surgery<br />
Elaine Que Lim, M.D.<br />
Obstetrics and Gynecology<br />
Richard Schraeder, M.D.<br />
<strong>Medical</strong> Oncology<br />
Michael Schultz, M.D.<br />
Breast Surgery<br />
Sue Currence, R.N.,<br />
B.S.N., C.E.T.N.<br />
Wound Ostomy<br />
Continence Nursing<br />
Monica Fulton, R.N.,<br />
B.S.N., M.B.A.<br />
The <strong>Cancer</strong> Institute<br />
Danielle McQuigg, R.N., O.C.N.<br />
<strong>Cancer</strong> Navigator<br />
Marcia Medina<br />
Performance Improvement<br />
Carol Smith<br />
<strong>Cancer</strong> Institute Registry<br />
Paul Chang, M.D.<br />
<strong>Medical</strong> Oncology<br />
Hector Silva, M.D.<br />
<strong>Medical</strong> Oncology<br />
Pat Johnson, R.N., O.C.N.<br />
Research<br />
Pam Trombero<br />
Clinical Research Associate<br />
Jason Citron, M.D.<br />
Radiation Oncology<br />
Rima Couzi, M.D.<br />
<strong>Medical</strong> Oncology<br />
Mark Fraiman, M.D.<br />
Hepatobiliary Surgery<br />
Maen Farha, M.D.<br />
General Surgery<br />
Mark Krasna, M.D.<br />
Thoracic Surgery/<strong>Medical</strong><br />
Director of The <strong>Cancer</strong><br />
Institute<br />
Nassif Soueid, M.D.<br />
Plastic and Reconstructive<br />
Surgery<br />
Alma Nyhan, M.D.<br />
Diagnostic Radiology<br />
Fowzia Taqi, M.D.<br />
Pathology<br />
Nancy Conner, R.N.,<br />
NACC Certified<br />
Spiritual Care<br />
Brian Cornblatt, Ph.D.<br />
Research<br />
Sharon Katrinak, M.B.A., R.C.H.<br />
Inpatient Pharmacy<br />
Coordinator<br />
Kathleen Kelly<br />
<strong>Cancer</strong> Institute Registry<br />
Ann Kennedy, R.N., B.S.N.<br />
Supportive Care Coordinator<br />
Sherry McCarter, L.S.C.W.<br />
Social Services<br />
Pat Wallace<br />
<strong>Cancer</strong> Institute Registry<br />
Gloria Webster, R.N.<br />
Community Outreach<br />
Bernadette White, R.N., M.S.<br />
Community Outreach<br />
<strong>2007</strong> THE CANCER INSTITUTE ANNUAL REPORT | 15
The <strong>Cancer</strong> Institute Services<br />
Oncologic Surgery<br />
• General<br />
• Abdominal<br />
• Thoracic<br />
• Head and Neck<br />
• Neurologic<br />
• Urologic<br />
• Gynecologic<br />
• Liver and Pancreas<br />
•Breast<br />
• Colorectal<br />
<strong>Medical</strong> Oncology<br />
• Serpick Infusion<br />
<strong>Center</strong><br />
• Inpatient Unit 5 East<br />
• Biotherapy<br />
• Management of Red<br />
Cell, Leukocyte and<br />
Platelet Disorders<br />
• Clinical Research<br />
• Ostomy/Wound Care<br />
• Pain Management<br />
• Nurse Navigator:<br />
Comprehensive<br />
Support for Patients<br />
with <strong>Cancer</strong><br />
• Supportive Care:<br />
Comprehensive<br />
Support for Patients<br />
with a Life-Threatening<br />
Illness<br />
• Nutrition Counseling<br />
7601 Osler Drive<br />
Towson, MD 21204-7582<br />
sjmcmd.org<br />
• Psychosocial Support<br />
for Patients and<br />
Families<br />
• Chemotherapy Class<br />
• Lymphedema Services<br />
• Genetic Counseling<br />
Services<br />
Radiation Oncology<br />
• Clinac IX & Varian<br />
2100 Accelerators<br />
• CT Simulator<br />
• Prostate Brachytherapy<br />
• High Dose Rate<br />
Brachytherapy<br />
• IMRT<br />
• IGRT<br />
• Mammosite HDR<br />
• Respiratory Gating<br />
• Cone-Beam CT<br />
Spiritual Care<br />
• Spiritual Counseling<br />
• Advanced Directives<br />
Counseling<br />
• Caregivers Support<br />
Group<br />
Community Outreach<br />
• Screenings for<br />
Prostate, Skin, Breast<br />
and Head/Neck/Oral<br />
<strong>Cancer</strong>s<br />
sjmcmd.org<br />
• Ostomy Support<br />
Group<br />
• Community <strong>Cancer</strong><br />
Education: Lectures<br />
and Health Fairs<br />
• Smoking Cessation:<br />
Inpatient, Outpatient<br />
and Community<br />
• Bereavement Support<br />
Group<br />
Community<br />
Participation<br />
• Susan G. Komen<br />
Race for the Cure<br />
• SOS (Survivors<br />
Offering Support)<br />
• Making <strong>St</strong>rides Against<br />
Prostate <strong>Cancer</strong><br />
• Hopewell Run<br />
• Relay for Life:<br />
American <strong>Cancer</strong><br />
Society<br />
• <strong>Cancer</strong> Coalition:<br />
Baltimore County<br />
Health Department<br />
• Smoke Free Maryland<br />
• Look Good, Feel<br />
Better ©<br />
• <strong>Cancer</strong> Survivor<br />
Celebration<br />
Non-Profit Org.<br />
US Postage<br />
PAID<br />
Baltimore, MD<br />
Permit #4944<br />
Important Phone Numbers<br />
Hospital Information<br />
410-337-1000<br />
Advanced Directives Counseling<br />
410-337-1109<br />
Clinical Research<br />
410-337-4543<br />
Community Outreach<br />
410-337-1479<br />
Customer Service–Billing<br />
410-337-1020<br />
Doctors Directory<br />
410-337-1337<br />
Home Care/Hospice<br />
410-931-0990<br />
Inpatient Oncology (5 East)<br />
410-337-1390<br />
Serpick Infusion <strong>Center</strong><br />
410-337-1841<br />
Nuclear Medicine<br />
410-337-1328<br />
Nurse Navigator<br />
410-427-2319<br />
Nutrition Counseling/Education<br />
410-337-1246<br />
<strong>Cancer</strong> Institute Registry<br />
410-337-1968<br />
Ostomy/Wound Care<br />
410-337-1845<br />
Pain Management Coordinator<br />
410-337-1185<br />
Palliative Care<br />
410-337-1535<br />
Pathology<br />
410-337-1717<br />
Physical/Occupational Therapy<br />
410-337-1330<br />
Radiation Oncology<br />
410-427-2525<br />
Radiology<br />
410-337-1441<br />
Smoking Cessation<br />
410-337-1555<br />
Social Work and Integrated<br />
Care Management<br />
410-337-1550<br />
Spiritual Counseling<br />
410-337-1109<br />
Surgical Services<br />
410-337-1066<br />
TDD Access<br />
410-337-1671<br />
© <strong>2007</strong> <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>