A NEW DAY IN CANCER TREATMENT - St. Joseph Medical Center
A NEW DAY IN CANCER TREATMENT - St. Joseph Medical Center
A NEW DAY IN CANCER TREATMENT - St. Joseph Medical Center
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
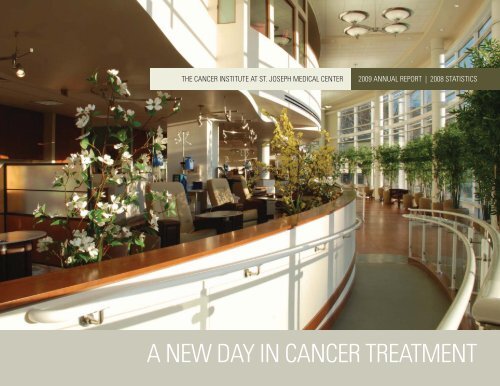
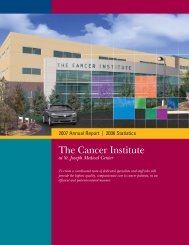
THE <strong>CANCER</strong> <strong>IN</strong>STITUTE AT ST. JOSEPH MEDICAL CENTER2009 ANNUAL REPORT | 2008 STATISTICSA <strong>NEW</strong> <strong>DAY</strong> <strong>IN</strong> <strong>CANCER</strong> <strong>TREATMENT</strong>
WELCOMEFROM THE MEDICAL DIRECTORMARK KRASNA, M.D.The Cancer Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> is made up of fulltime,part-time and private physicians. This team collaborates to providetreatment for the entire spectrum of cancer—from solid organ tohematologic malignancies. The Cancer Institute <strong>Center</strong>s are designedaround specific organ sites to facilitate the best possible care forpatients. Our 33,400 square foot outpatient facility has further facilitatedimprovements in person-centered cancer care delivery, allowing our uniquemultidisciplinary approach to provide all cancer care under one roof.The Cancer Institute truly embodies the concept of patient-centeredmultidisciplinary care. The facility, scheduling and administrativestructure allow patients to be seen at one visit by all the necessaryspecialties pertaining to each individual case, including medical,radiation and surgical oncology. In addition, there is easy access to otherspecialists, such as pulmonologists, gastroenterologists, radiologists,dieticians, genetic counselors, physical therapists and social workerswithout the patient having to move to a different facility or location.Disease-specific multidisciplinary care clinics, prospective weeklydisease-specific conferences and clinical research trials are a regularpart of the comprehensive cancer care provided.The Cancer Institute houses all cancer outpatient services, including:outpatient infusion areas, a dedicated cancer pharmacy and researchpharmacy, dedicated PET/CT unit, outpatient radiation oncology, cancerresearch offices, community outreach, nurse navigators/coordinators,social services, pastoral care and the Tumor Registry.The Comprehensive Breast Oncology <strong>Center</strong>, which opened in October2007, has now exceeded its capacity, resulting in a 4300 square footexpansion for the new Women’s Oncology <strong>Center</strong>. This unit houses theoutpatient evaluation and biopsy programs as well as breast imagingservices, including mammography, ultrasound, dexa scan and X-ray.Likewise, our expanding Gynecologic Oncology program is moving intothis enlarged space, giving our female patients the sense of belongingto one unique Women’s Oncology <strong>Center</strong>. Our Serpick Infusion <strong>Center</strong>has grown beyond all expectations with the resulting need for expansionin this area as well. Additional chemotherapy infusion chairs, designedand patented by Dr. Krasna for the Cancer Institute, as well as additionalmedical oncology and nursing staff will be added by June 2010.This past year saw the beginning of year three of our NationalCommunity Cancer <strong>Center</strong> Program (NCCCP), the only NCI communitycancer program in Maryland. This program has been granted anexpansion for a fourth year due to its success as well as opportunitiesfor additional grant funding from the National Cancer Institute (NCI). Thisyear also marks the beginning of our participation in the National CancerInstitute’s Cancer Genome Project (TCGA). The Cancer Institute is the firstcommunity cancer center in the country to participate in tissue collection,and its team is working with the NCI to define best practices in cancertissue collection, storage and research, to understand the root causesof cancer in the future, and to allow better opportunities to developpersonalized cancer treatments.
This year we also opened our new stereotactic radiosurgery unit in theRadiation Oncology <strong>Center</strong>. The most exciting alternative to surgery fortumors—radiosurgery—is now available to <strong>St</strong>. <strong>Joseph</strong> Cancer Institutepatients with the installation of a hybrid Trilogy linear accelerator witha Clinac IX stereotactic radiosurgery arm. Radiosurgery allows us toperform local treatment of tumors and is similar to surgery without a knife,by delivering a high radiation dose in a very precise volume. Multi-leafcollimators, which are thin metal sliding mechanisms, shape the radiationbeam, so that it can be altered to avoid normal, healthy tissue. Dr. JasonCitron, medical director of the Radiation Oncology <strong>Center</strong>, Dr. Neal Naff,chief of Neurosurgery, Dr. Ziv Gamliel, chief of Thoracic Surgery, andDr. Justin Tortolani of the Orthopedic Institute have participated in treatinginoperable tumors of brain, lung and bone cancers since its installationthis past April. Although the main application for radiosurgery has beenbrain metastases, meningiomas and other benign brain tumors, cerebralarteriovenous malformations and pituitary adenomas, we will expand itsuses in the future and investigate treating inoperable lung cancer, softtissue cancers and liver mestatases.Finally, our Cancer Committee, ably led by Dr. Maen Farha, hasdeveloped admirable quality improvement goals each year which havebeen instrumental in improving patient care. Likewise, they have approveda draft “conditions of participation” at the suggestion of the NCI to betterdefine and recognize appropriate Cancer Institute participation on thepart of physicians across the <strong>Medical</strong> <strong>Center</strong>.The Cancer Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>.CENTER HEADSBreast Oncology <strong>Center</strong> Director s Michael Schultz, M.D.Colorectal Oncology <strong>Center</strong> Director s Howard Berg, M.D.Genitourinary Oncology <strong>Center</strong> Director s Marc Siegelbaum, M.D.Gynecologic Oncology <strong>Center</strong> Director s Neil Rosenshein, M.D.Hepatobiliary Oncology <strong>Center</strong> Director s Mark Fraiman, M.D.<strong>Medical</strong> Oncology s Rima Couzi, M.D.s Richard Schraeder, M.D.Radiation Oncology Director s Jason Citron, M.D.Thoracic Oncology <strong>Center</strong> Director s Ziv Gamliel, M.D.Neuro-Oncology <strong>Center</strong> s Neal Naff, M.D.
RESEARCHBarriers to effective use of that database are being tackled. The lagtime between patient diagnosis until data availability will be cutdown from years to a short few weeks with the implementation ofthe Cancer Institute’s Rapid Quality Reporting System (RQRS),which we have begun as part of our NCCCP participation. Interlinkingthe various cancer databases with other health databases will multiplythe amount of available data on patients. Much of the stage dataentered has been based on traditional staging measurements, i.e.,tumor size, lymph node involvement etc., which carry some importance.These, however, are being surpassed by more sophisticated indicators ofthe biologic behavior of tumors. Dr. Carolyn Compton, the new head ofthe American Joint Committee on Cancer, believes they should becomea part of the staging system. Better prediction of a particular tumor’sbehavior will help us reduce the utilization of unnecessary treatmentsand design more personalized treatment regimes. <strong>St</strong>andardizingspecimen handling techniques and maintaining tissue banks that storefresh frozen tissues will be essential to the success of our ambitiouscancer project. This will be aided by the opening of our new <strong>Center</strong> forTranslational Research (CTR) and participating with the TCGA.Accelerating the pace of cancer treatment progress will require us tobe more creative in research, utilize the large amounts of data that havealready been collected, improve the quality and increase the amount ofinformation in our databases, and move more and more into personalizedmedicine. All these efforts are intended to transform many cancers intoa controlled chronic illness and achieve cures for many others.
ACTIVITY<strong>CANCER</strong> <strong>IN</strong>STITUTE REGISTRY ACTIVITYDATA ANALYSIS4The Cancer Registry is an important component of the <strong>St</strong>. <strong>Joseph</strong><strong>Medical</strong> <strong>Center</strong>’s American College of Surgeons Commission on Cancer’s(ACoS-COC) approved cancer program. The Cancer Registry collects andmanages data on all cancer patients diagnosed and/or treated at thehospital since January 1, 1997. Benign and borderline central nervoussystem tumors were included beginning with cases diagnosed January1, 2004 and forward. To date, the Cancer Registry has collected dataon 13,715 cases. Cancer Registry data includes patient demographics,primary tumor site, tumor histology, cancer stage at diagnosis andfirst-course treatment modalities. Patients diagnosed and receivingall or part of their first-course treatment at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>are followed annually and monitored for survival and disease status.Under the direction of the Cancer Committee leadership, three certifiedtumor registrars (CTR) collect, manage, and analyze cancer data inaccordance with the ACoS-COC and the Maryland Cancer Registry (MCR)regulations. This is done with the strictest adherence to guidelinesfor patient confidentiality and in compliance with the Federal HealthInsurance Portability and Accountability Act (HIPPA).Cancer Registry data is an important tool used to assess oncologypatient care outcomes, measure cancer incidence, and provide sourcedocumentation for cancer research efforts. The Cancer Institute’s CancerRegistry data are contributed to a variety of cancer data repositoriesincluding the National Cancer Data Base (NCDB), the Maryland CancerRegistry (MCR), and The <strong>Center</strong>s for Disease Control’s National Programof Cancer Registries (CDC-NPCR). The NCDB is a national cancer datarepository that collects and analyzes data from over 1,400 hospitalsand medical facilities. The NCDB is a joint project of the CommissionAJCC STAGE AT DIAGNOSIS ST. JOSEPH MEDICAL CENTER 2008 FIVE MOST FREQUENT <strong>CANCER</strong> SITESAmericanJoint College ofSurgeons (AJCC)Cancer <strong>St</strong>ageBreast Lung/Bronchus Prostate Colorectal Non-BCC/SCC Skin<strong>St</strong>age 0 23.4% 0.0% 0.0% 11.0% 31.5%<strong>St</strong>age I 35.8% 32.0% 0.0% 23.7% 52.1%<strong>St</strong>age II 25.5% 10.9% 78.8% 23.7% 6.9%<strong>St</strong>age III 9.1% 22.6% 15.8% 28.8% 1.3%<strong>St</strong>age IV 3.6% 25.6% 3.0% 10.2% 0.0%Not <strong>St</strong>aged 2.2% 6.1% 2.4% 0.1% 6.9%Source: <strong>St</strong>. <strong>Joseph</strong> Cancer Institute Registry<strong>St</strong>age 0 – Carcinoma in situ –an early form of carcinoma<strong>St</strong>age I – Localized to onepart of the body<strong>St</strong>age II – Involves regionallymph nodes<strong>St</strong>age III – Locally advanced<strong>St</strong>age IV – Metastasized or spreadto other organs throughoutthe body
“ ...thank you for your extraordinary care and lovingkindness to my Dad during the time he was in your care.During his transfusions, Dad experienced a level of carewhich I have rarely seen. I am most grateful. ” s S.P.on Cancer (CoC) and the American Cancer Society (ACS). The MarylandCancer Registry, under state mandate, began collecting data on allpatients diagnosed with cancer in the <strong>St</strong>ate of Maryland effective July1, 1991. The law was later amended to include the collection of dataon all central nervous system tumors regardless of tumor behavior.The MCR uses the data for analysis of statewide cancer trends and toplan state cancer screening and prevention programs. By collaborativeagreement, the MCR reports state cancer data in aggregate to the CDC-NPCR. The CDC-NPCR in cooperation with the National Cancer Institute(NCI) and the North American Association of Central Cancer Registries2008 FIVE MOST FREQUENT <strong>CANCER</strong> SITESDIAGNOSED AT ST. JOSEPH MEDICAL CENTERBreastLung/BronchusProstateColorectalNon BCC/SCC Skin 6.0%14.4%12.9%9.7%21.8%0 5 10 15 20Source: <strong>St</strong>. <strong>Joseph</strong> Cancer Institute Registry
“ I would like to mention Lisa, a special positive force...alwayspresents the positive with great assurance and skill. “ s M.L.<strong>CANCER</strong> <strong>IN</strong>STITUTE REGISTRY ACTIVITYDATA ANALYSI<strong>St</strong>hat had first pathological/cytological confirmation of their cancermade by the <strong>St</strong>. <strong>Joseph</strong> Cancer Institute pathology team (patients neverphysically came to the Cancer Institute). The Registry has maintainedannual follow-up rates well above the CoC required rates. The overallfollow-up rate for all patients is 89.44% (CoC required rate is 80%).The follow-up rate for patients diagnosed in the last five years is93.53% (CoC required rate is 90%). The top five cancer sites collectedin 2008 were breast (21.8%), lung (14.4%), prostate (12.9%), colorectal(9.7%) and non BCC/SCC skin (6.0%). This is consistent with theprevious two accession years (2007 and 2006).The <strong>St</strong>. <strong>Joseph</strong> Cancer Institute was awarded full accreditation withcommendation by the American College of Surgeons Commission onCancer in 2009.(NAACCR) produces the official federal cancer incidence statistics.Hospital cancer registry data not only serves as a valuable data sourcefor internal facility-based studies but assists public health professionalsin better ascertaining and alleviating cancer burdens.Cancer Registry data is regularly reviewed for quality by CancerInstitute staff physicians, and the medical staff provides continuousclinical education for the Cancer Registry staff via quality reviewsof registry data. The Cancer Registry staff also stays abreast ofstandardized cancer data collection rules and cancer diagnostics andtherapeutic trends via in-house, local, regional and nationaleducational conferences, as well as webinar conferences.In 2008 the <strong>St</strong>. <strong>Joseph</strong> Cancer Institute Cancer Registry registered1,361 cases treated for cancer at <strong>St</strong>. <strong>Joseph</strong>’s Cancer Institute.Twelve hundred seventy-seven cases (1,277) were either diagnosedand/or received all or part of their first-course treatment at the CancerInstitute. The Cancer Registry also abstracted and reported 92 cases
2008 PRIMARY SITE TABLEPrimary Cancer Site Analytic* Non-Analytic** Male Female TotalCases Cases 2008 CasesBreast 279 11 3 287 290Bronchus/Lung 184 8 90 102 192Prostate 164 15 180 0 180Colorectal 124 10 76 58 134Non BCC/SCC Skin 76 4 54 26 80Pancreas 65 3 33 35 68Bladder 56 3 43 16 59Hematopoietic 35 7 19 23 42Corpus Uteri 33 1 0 34 34Kidney 29 5 22 12 34Unknown Primary 28 3 11 20 31Esophagus 25 4 23 6 29Lymph Nodes 22 2 14 10 24<strong>St</strong>omach 17 2 14 5 19Thyroid Gland 16 0 0 16 16Liver- Intrahep Bile Ducts 12 1 8 5 13Cervix Uteri 11 0 0 11 11Anus & Anal Canal 10 0 3 7 10Ovary 10 0 0 10 10Meninges 10 0 0 10 10Other/unspec PTS of Biliary Tract 7 0 5 2 7Heart, Mediastinum, Pleura 6 0 3 3 6Vulva 5 0 0 5 5Brain 4 1 4 1 5Connective Tissue/Other Soft Tissue 4 1 4 1 5Other Endocrine Gland 4 1 0 5 5Gallbladder 4 0 1 3 4Larynx 4 0 2 2 4Renal Pelvis 3 0 0 3 3Other Urinary Organs 3 0 2 1 3Other CNS 3 0 2 1 3Small Intestine 2 1 2 1 3Parotid 2 0 0 2 2Thymus 2 0 0 2 2Retroperitoneum/peritoneum 2 0 0 2 2Uterus, NOS 2 0 0 2 2Testis 2 0 2 0 2Ureter 2 0 0 2 2Base of Tongue 2 0 2 0 2Other/Unspecf Part of Tongue 0 1 0 1 1Palate 1 0 1 0 1Other Parts Maj Salivary 1 0 0 1 1Nasopharynx 1 0 0 1 1Pyriform Sinus 1 0 1 0 1Other/ILL-Defined Digestive 1 0 1 0 1Vagina 1 0 0 1 1Eye/Adnexa 1 0 0 1 1TOTALS 1,277 84 624 737 1,361*Analytic Cases: Patients either diagnosed or diagnosed and/or received a portion of fi rst-course treatment at <strong>St</strong>. <strong>Joseph</strong> Cancer Institute.**Non-Analytic Cases: Patient received fi rst-course treatment elsewhere and presented to <strong>St</strong>. <strong>Joseph</strong> Cancer Institute disease recurrence or progression .MALEFEMALE10 Most Prevalent Cancers Diagnosed for 2008 by Gender2008 National* and <strong>St</strong>. <strong>Joseph</strong> Comparative IncidenceNationally*Breast 26%Lung/Bronchus 4%Colorectal 10%Corpus Uteri 6%Non-Hodgkin Lymphoma 4%Thyroid 4%Melanoma of Skin 4%Ovary 3%Kidney & Renal Pelvis 3%Leukemia 3%All other sites combined 26%Nationally*Prostate 25%Lung/Bronchus 15%Colorectal 10%Bladder 7%Non-Hodgkin Lymphoma 5%Melanoma of Skin 4%Kidney & Renal Pelvis 4%Oral Cavity 3%Pancreas 3%Leukemia 3%All other sites combined 20%*Source: American Cancer Society<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>Breast 39%Lung 14%Colorectal 8%Corpus Uteri 5%Pancreas 5%Melanoma of Skin 3%Hematopoietic 3%Bladder 2%Thyroid 2%Lymphoma (all) 2%All other sites combined 17%<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>Prostate 29%Lung/Bronchus 15%Colorectal 12%Melanoma of Skin 9%Bladder 7%Pancreas 6%Esophagus 3%Kidney 3%Hematopoietic 2%Unknown Primary 2%All other sites combined 11%
FOCUS<strong>CANCER</strong>S OF THE COLON, RECTUM AND ANUSHOWARD BERG, M.D. AND ROBERT AKBARI, M.D.8Colorectal CancerYou may be familiar with the pink ribbon for breast cancer awareness,but how about the blue star for colorectal cancer awareness? Colorectalcancer is less commonly publicized than some other common cancersbut is equally important in many ways.The estimated number of new colorectal cancer cases in the U.S. inthe year 2009 is 146,970 (Jemal A, et al. CA Cancer J Clin 59:225-492009). The estimated number of deaths secondary to colorectal cancerin the same year is 49,920. This makes colorectal cancer the third mostcommon solid organ cancer and the third most common cause of solidorgan cancer-related death in the U.S. for both men and women.Colorectal cancer is also one of the most preventable and treatablecancers. A number of physician societies have proposed standardscreening guidelines for colorectal cancer, which are quite similar toone another. Recommendations in common include: yearly Fecal OccultBlood Tests (FOBT) and intermittent colonoscopies usually starting atage 50. By following standard guidelines, colorectal polyps can be foundbefore they turn into cancers and cancers can be caught before theygrow and metastasize to other organs.When a patient is diagnosed with colorectal cancer, there are a myriadof treatment options available and the plan of action is best determinedby using a multidisciplinary approach. The Colorectal Oncology <strong>Center</strong>of the Cancer Institute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> uses such anapproach to efficiently create a treatment plan and enact the planunder the direction of a team of physicians and allied health specialists.There is also an active interest at the Institute in cutting-edge researchprotocols for patients interested in pursuing this option.The colon and rectal surgeons at the Colorectal Oncology <strong>Center</strong> areHoward Berg, M.D., and Robert Akbari, M.D. They are both experiencedin the surgical management of colorectal cancer. They are well-versedin the state-of-the-art techniques for the work-up and surgical treatmentof colorectal cancer. These techniques, among others, include: flexibleendoscopy, endorectal and endoanal ultrasound and laparoscopy. Themajority of colorectal cancer operations they perform are done using aminimally-invasive laparoscopic approach.Other physicians at the Institute who are indispensable to the careof patients with colorectal cancer include the medical oncologistsRichard Schraeder, M.D., Rima Couzi, M.D., John Downs, M.D., andHector Silva, M.D., and the radiation oncologists Jason Citron, M.D.,and <strong>St</strong>ephen Ronson, M.D. Allied health professionals who are veryuseful in the management of these patients include: enterostomaltherapy Sue Currence, B.S.N., R.N, C.W.O.N., genetic counseling NishaIsaac, M.S., C.G.C., nutritional services Asa House, R.D., L.D.N., andsocial services Penny Graf, L.C.S.W.-C. Nurse navigator Diana Smith,R.N., is also available for the close follow-up and the coordinationof services for the patient and family throughout their continuum of
In the <strong>St</strong>. <strong>Joseph</strong> multidisciplinary approach to cancer care,technology provides yet another tool to further enable each clinicalteam to choose the most effective method for treating each patient.Michael Rutstein, M.S., M.B.A. andJerry Bowman, chief radiation therapy technologistoncology care. By using the multidisciplinary expertise available,patients with colorectal cancer have all physical, psychosocial andemotional aspects of their care covered.Rectal CancerThe literature has shown that for higher stage rectal cancers, upfrontcombination chemotherapy and radiation (neoadjuvant treatment) priorto surgical intervention leads to lower locoregional recurrence rates(Sauer R, et al. N Eng J Med 351:1731-40 2004). The best way to discernthe higher stage rectal cancers is through use of endorectal ultrasound,a procedure performed weekly at the Colorectal Oncology <strong>Center</strong> of theCancer Institute. Patients who are candidates for neoadjuvant treatmentare managed in concert by both the radiation and medical oncologists.When rectal cancer is of a lower stage, upfront surgery is the usual nextstep. Depending on the specifics of the cancer and the patient, optionsmay include anything from local excision of the cancer via the transanalroute (transanal excision) to radical excision via a transabdominalapproach (low-anterior resection or abdominoperineal resection).The Colorectal Oncology <strong>Center</strong> surgeons at <strong>St</strong>. <strong>Joseph</strong> do their best toavoid a permanent stoma in their rectal cancer patients. When sphinctersalvage is oncologically safe and technically feasible, they are usuallysuccessful. Because of their experience with low rectal cancer resections,they can often “save sphincters” when other surgeons may not be able to so.After surgical resection of either a colon or a rectal cancer,chemotherapy is often indicated. Chemotherapy has been shown inmany studies to increase overall survival rates with this disease.The medical oncologists of the Cancer Institute have much experiencewith adjuvant chemotherapy for colorectal cancer and are up-to-dateon the latest recommendations. When receiving chemotherapy, thepatients are well attended at the Serpick Infusion <strong>Center</strong>, a beautifulfacility on the 1st level with a great view of the hospital campus.Anal CancerAnal cancer received a lot of national attention recently due to thewell-publicized death of Farrah Fawcett. This tumor is much lesscommon than either colon or rectal cancer. An estimated 5,290patients will be diagnosed with anal cancer in 2009 (Jemal A, et al.CA Cancer J Clin 59:225-49 2009). The estimated number of deathsfrom this ailment in the same year is 710.9
A multidisciplinary approach is the standard approach formost cancers. The team of experts at the Cancer Instituteat <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> meet weekly and discusstreatment options prospectively.<strong>CANCER</strong>S OF THE COLON, RECTUM AND ANUS10Anal cancer is very distinct from colorectal cancer in many ways,including: risk factors, progression of disease and treatment. It is oneof the few solid organ tumors that is potentially curable without surgery.The combination of chemotherapy and radiation is very effective intreating this malignancy, often to the point where there is no moreevidence of disease. The standard treatment algorithm currently usedwas actually first described back in 1974 (Nigro ND, et al. Dis ColonRectum 17:354-8 1974). When chemotherapy and radiation are notenough, “salvage” surgery can be curative.A multidisciplinary approach is necessary for the cure of anal cancer.The team of experts at the Colorectal Oncology <strong>Center</strong> of the CancerInstitute at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>, including surgeons, radiationoncologists, medical oncologists and gastroenterologists, is veryexperienced with the treatment of this rare tumor. From upfront stagingwith ultrasound and PET/CT, to tailoring a regimen of chemotherapy andradiation for each particular patient, to surgical removal if needed, allfacets of workup and treatment are addressed at the <strong>Center</strong>.Focus on Laparoscopyhospitalization after the operation and cosmesis. The concern manycancer surgeons had regarding these techniques is whether they areoncologically sound. In other words, does laparoscopy have the samepotential for cure of a given cancer in comparison to traditional surgery?In the realm of colon cancer surgery, this question was definitivelyaddressed by the COST trial in 2004 (N Engl J Med 350:2050-9 2004).This well-publicized study found that recurrence rates for colon cancerwere similar when colectomy was performed by either laparoscopicor traditional techniques. Not long thereafter, the American Societyof Colon and Rectal Surgeons released a statement enumeratingFigure 1ST. JOSEPH MEDICAL CENTERCOLORECTAL PRIMARY TUMORS BY SITEFIVE YEAR (2004-2008)Total Colon = 519 (75%)Rectum = 141 (20%)Anal = 32 (4%)Left Colon19027%TransverseColon8%Other3%Anal4%In recent years, minimally-invasive approaches to common surgicalconditions have received a lot of public attention. The techniques oflaparoscopy, in particular, have been applied to almost any operationthat can be performed in the traditional “open” fashion. The obviousbenefits of laparoscopy include: less postoperative pain, shorterRight Colon25838%Rectum14120%
“ For Jen, R.N.—I met her during my lung biopsy at <strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>. She did more to teach me about my cancer and itstreatment during my pre-biopsy prep than anyone had yet done. It is because of her that I made the decision to seek all of mycancer treatment at the Cancer Institute. ” s J.G.Figure 2HISTOLOGY OF TUMOR<strong>St</strong>hat laparoscopic colectomy for colon cancer is a safe alternative totraditional “open” technique when performed by a surgeon who isexperienced with this technique.The colon and rectal surgeons at the Colorectal Oncology <strong>Center</strong>,Drs. Berg and Akbari, are well-versed in the minimally-invasive/laparoscopic approach to colorectal cancer. In fact, the great majorityof the operations they perform for colorectal cancer are performed usingeither “straight” laparoscopy or a laparoscopically-assisted approach.Both surgeons, in fact, have been instructors in courses to teach othersurgeons these techniques.Our Own ResultsThe Cancer Institute takes pride in tracking and analyzing its owndata. Focusing on cancers of the colon, rectum and anus, the primarysites of these cancers from the years 2004-2008 can be seen inFigure 1. As can be seen, as with the national data mentioned earlier,colon cancer was the most prevalent, followed by rectal and anal.The histology of these tumors was overwhelmingly adenocarcinoma,the most common histology of colon and rectal cancers (Figure 2).Anal cancers have squamous histology. The most common malignancycategorized under the “other” category was the carcinoid (low-gradeneuroendocrine) histology. In regards to the age of patients with acolorectal cancer at diagnosis, the apex of the distribution curve wasin the mid 70s (Figure 3).HISTOLOGY DISTRIBUTION PERCENTAGEFigure 3NUMBER OF CASES100%90%80%70%60%50%40%30%20%10%0%35302520151050COLON RECTUM ANALST. JOSEPH <strong>CANCER</strong> <strong>IN</strong>STITUTEFIVE-YEAR COLORECTAL <strong>CANCER</strong> AGE DISTRIBUTIONAge at DiagnosisPoly. (Age at Diagnosis)Average Age = 69Median Age = 71Maximum = 95Minimum = 25AGE AT DIAGNOSISOtherRareCloagenicCarcinoidBasiloidSquamousAdenocarcinoma25 30 35 40 45 50 55 60 65 70 75 80 85 9011
“ Please accept my words of gratitude towards your goodness, patience, and love that you bestowon all of us, and mainly to me, the recipient of your great qualities. You make our treatment so easy andso comfortable that I forget where I am and pretend I am in a spa. ” s D.F.<strong>CANCER</strong>S OF THE COLON, RECTUM AND ANUSThe five-year survival rates for patients with colon cancer treated atThe American College of Surgeons has described important quality<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong> from 1998-2001 are similar to data from themeasures in the treatment of colorectal cancers. These include timelyNational Cancer Database (Figure 4). Not surprisingly, patients withadministration of chemotherapy and radiation when appropriate andlower stage disease fared better than those with higher stage tumors.an adequate lymph node harvest. The Cancer Institute has analyzed itsFortunately, with the availability of hepatobiliary surgeonsdata and compared to regional and national data as available in theMarc Fraiman, M.D., and Richard Mackey, M.D., stage 4 patients withNational Cancer Data Base (NCDB). For the most recent year analyzed12908580isolated liver disease may have a chance at cure.Figure 4 PRIMARY COLON <strong>CANCER</strong> FIVE-YEAR SURVIVAL<strong>St</strong>. <strong>Joseph</strong> Cancer Institute (n=131)National Cancer Database (n=1,342)in this regard, 2006, radiation was administered appropriately 60% ofthe time, chemotherapy was administered appropriately 87.5% of thetime, and an adequate lymph node harvest was achieved 59.6% of thetime. At first glance these numerics may not seem impressive. However,when comparing to regional and national data from the NCDB for thesame year, these data are fairly comparable. We will review the 2007outcome data once it is made available and identify opportunities forimprovement in the care of patients with colon and rectal cancer.SURVIVAL PERCENTAGE7570656055504540.5 yr 1 yr 1.5 yrs 2 yrs 2.5 yrs 3 yrs 3.5 yrs 4 yrs 4.5 yrs 5 yrsThe FutureThe future of treatment for cancer of the colon, rectum and anus isundoubtedly challenging and yet hopeful. By using a multidisciplinaryteam approach, the Colorectal Oncology <strong>Center</strong> is well-positionedto deliver state-of-the-art treatment in an efficient and coordinatedfashion. Patients receive the personal, friendly care associated witha community hospital as well as the expertise and cutting-edgetechnology associated with an NCI Community Cancer <strong>Center</strong> Program.
SERVICESOur Nurse Navigators/Coordinators.SUPPORT SERVICESCancer Institutes NCCCP Program <strong>St</strong>atuss Nurse Navigators/Coordinators:Comprehensive Support forPatients and Familiess Clinical Researchs Ostomy/Wound Cares Nutrition Counselings Psychosocial Support forPatients and Familiess Chemotherapy Classs Genetic Counselings Tumor Registrys Pain Managements Lymphedema Servicess Financial Counselings End of Treatment Classs Oncology Certified Nurses<strong>Medical</strong> Oncologys Serpick Infusion <strong>Center</strong>s Inpatient Unit 7 Wests Biotherapys Management of Red Cell,Leukocyte and Platelet Disorderss Chemotherapys Targeted TherapySurgical Oncologys Robotic prostatectomys Hepatic resections Whipple proceduress Endobrachial therapiess Video-assisted thoracicsurgery (VATS)s Minimally invasivehepatic/pancreatic surgerys Intrahepatic microspheresRadiation Oncologys <strong>St</strong>ereotactic radiosurgery (SRS)s Varian trilogy systems CT Simulators Prostate Brachytherapys High Dose Rate Brachytherapys Mammosite HDRs IMRTs IGRTs Respiratory GatingSpiritual Cares Spiritual Counselings Advanced Directives Counselings Caregivers Support GroupCommunity Participations Susan G. Komen Race for the Cures SOS (Survivors Offering Support)s Great Prostate Cancer Challenges Hopewell Runs Relay for Life: AmericanCancer Societys Cancer Coalition:Baltimore County/Baltimore City Health Departments Smoke Free Marylands Look Good, Feel Better ©s Cancer Survivor Celebrations Pancreatic Cancer ActionNetwork: Purple <strong>St</strong>rides Red Devilss Sister’s Networks Esperanza <strong>Center</strong>s Maryland Regional CommunityNetwork Programs LUNGS (Learning, Understanding,Navigating, Growing,Survivorship)s Lungevity WalkCommunity Outreachs Screenings for Colorectal,Prostate, Skin, Breast, andHead/Neck/Oral Cancerss Ostomy Support Groups Community Cancer Education:Lectures and Health Fairss Bereavement Support Group13PO<strong>IN</strong>TS OF CONTACTHospital Information 410-337-1000Advanced Directives Counseling410-337-1109Breast Oncology <strong>Center</strong> 410-427-5510Cancer Institute 410-427-5585Clinical Research 410-427-4569Comfort Care Boutique 410-337-7117Community Outreach 410-427-2548Customer Service – Billing 410-337-1020Doctors Directory 410-337-1337Genetics Counselor 410-337-1697Inpatient Oncology (7 West)410-337-1390Serpick Infusion <strong>Center</strong> 410-337-1841Multidisciplinary Clinic 410-427-5585Nurse Navigators/CoordinatorsBreast 410-427-5509GI-GU-GYN 410-427-2354Lung & Esophagus 410-427-2321410-427-2225Nutrition Counseling/Education410-337-1246Ostomy/Wound Care 410-427-1845PET/CT 410-427-2516Pathology 410-337-1717Physical/Occupational Therapy410-337-1330Radiation Oncology 410-427-2525Radiology 410-337-1441Social Work(Inpatient) 410-337-1550(Outpatient) 410-427-2124Spiritual Counseling 410-337-1109Tumor Registry 410-337-1968
OUTREACHSURVIVORS OFFER<strong>IN</strong>G SUPPORT (SOS)“ What a team you have here! Kudos to each and everyoneof your staff! They all seem to support each other, helpeach other and keep a joyful spirit through it all. ”EDLA COLEMANs S.J.C.14Survivors Offering Support(SOS) is a resourcefulnetwork of women whohave battled breast cancerand are making a differenceby offering their supportand knowledge to newlydiagnosedpatients. SOSis funded by the MarylandAffiliate of Susan G. KomenRace for the Cure andEdla Coleman, SOS Coordinator<strong>St</strong>. <strong>Joseph</strong> <strong>Medical</strong> <strong>Center</strong>.The Cancer Institute at <strong>St</strong>. <strong>Joseph</strong> is proud to offer this valuableprogram under the leadership of Edla Coleman, a breast cancer survivorwho knows the emotional impact that this diagnosis creates.“We help women through the initial shock and then continue to providethem with vital support,” she explains. “There’s a big emotional gapwith breast cancer. Your family tries to help, your friends try to help, butthey don’t really know what to say.”SOS mentors are expertly trained volunteers who not only know whatto say, but will meet in person, help patients communicate with theirphysicians, provide computer resources, and are available by phonewhenever needed. This psychosocial and emotional support isintegrated into <strong>St</strong>. <strong>Joseph</strong>’s standard of care.The program was founded by survivor Denise O’Neill, who wasrecognized with the 2007 Daily Record Healthcare Heroes Award forCommunity Outreach. “At first, the emotional response to a breastcancer diagnosis is total devastation, but a little later you begin tounderstand there are gifts to this experience, and SOS is here tosupport women through the journey,” says Coleman.The on-site mentors are available to meet real time with patientsas they are diagnosed or in emotionally stressful times whena survivor’s support is required. The mentors provide psychosocialsupport and work hand in hand with the nurse navigators and/ordoctors. Any patient issues, such as early signs of lymphedema orneeded social services, are communicated back to the nurse navigator,social worker and/or doctor. SOS is linked to the hospital and not astand-alone survivor support program.s Breast cancer survivor volunteers from <strong>St</strong>. <strong>Joseph</strong> are matched inage, stage and demographics with newly diagnosed patients.Volunteers are available on-site at the Cancer Institute.s Survivor shares with the new patient insight into her personal breastcancer experience and provides information and emotional supportover the course of diagnosis and treatment. Volunteers are trained
Pam Trombero, B.S., C.C.R.P., LUNGS coordinator with Sylvia Levine,esophageal cancer survivor and LUNGS mentor.LUNGSmentors who can make the breast cancer journey less confusingand solitary. They provide an invaluable support system.s SOS mentors are trained extensively on topics like breast cancerdiagnosis, surgery and treatments, mentoring do’s and don’ts androle playing. Mentors are required to attend additional trainingthrough the Mentor Education Lecture Series.s A volunteer can elect to follow a single patient or severaldepending on her desire and availability. Mentoring is flexible andinvolves regular phone conversations with the patient as well aspersonal visits.s Each mentor is asked to provide two physicians’ releasesindicating she is emotionally ready to participate as a mentor inthe SOS program.s SOS volunteer meetings are also held to provide feedback, sharelearnings and new information about breast cancer, and recognizethe efforts of the volunteers.To become a mentor or to make a patient referral, please contact EdlaColeman at 410-427-2513 or email edlacoleman@catholichealth.net.Learning, Understanding, Navigating, and Growing SurvivorshipLUNGS, which stands for Learning, Understanding, Navigating, andGrowing Survivorship, was created in 2007 to address an unmet need inthe community—to support patients being treated for lung and esophagealcancers. With grants from the Dorothy Friedman Caplan Guild and theAmerican Cancer Society, the Cancer Institute has trained mentors to providesupport based on personal experience. Mentors and patients are able toshare the feelings, emotions and fears cancer patients sometimes have.The LUNGS program also focuses on education and guidance promoting ahealthy lifestyle and preventative care. The program offers free lecturesfocused on the challenges of cancer, common medical problems andstrategies for coping with the psychological effects of cancer.The LUNGS program at the Cancer Institute is distinct in acknowledging thesignificance of diverse quality-of-life issues and is able to provide cancersurvivors and their families with emotional and social support—crucial tocancer survivors. Patients are encouraged to embrace life, each other andthe future. Whether a patient is living with cancer, has been cured, or hasrecurred, LUNGS mentors understand cancer survivors’ questions and needsbecause they have lived the experience and have survived.To become a mentor or to make a patient referral, please contactPam Trombero at 410-427-4543.15
NCI COMMUNITY <strong>CANCER</strong> CENTER PROGRAMACCOMPLI16NCCCP YEAR TWO ACCOMPLISHMENTSClinical Trialss MPACT (Maryland Program for Advancing ClinicalTrials): To promote awareness about the importanceof clinical trials and the need for diverse andunderserved community participation in research~ December 13, 2008 Coppin <strong>St</strong>ate College~ April 25, 2009 Bel Alton Community <strong>Center</strong>in Southern Marylands AWARE For All Day sponsored by CISCRP(<strong>Center</strong> for Information and <strong>St</strong>udy on ClinicalResearch Participation): To educate the public,patients, media, and policy makers on clinicaltrials in order to promote greater understandingand awareness of clinical research participationand its effect on public health~ May 29, 2009s Development of physician scorecard to tracknumber of referrals by physicianDisparities/Advocacys NCI Community Network Program with (MRCNP)University of Maryland collaborations Baltimore City Tobacco Grant with Esperanza<strong>Center</strong>~ “Tobacco’s Toll; Personal <strong>St</strong>ories” DVD~ ACS South Atlantic Div. Tools African American Men’s Health Conference~ Collaboration with ACS and <strong>St</strong>. Agnes Hospital~ 515 attendees and 264 screeningss Community Advisory Council~ Serves as a primary forum for discussingprogram priorities and to establish andmaintain strong community collaborationss Hired additional community outreach coordinators Advocacy in Annapolis~ Testified before Senate hearing in supportof Maryland Cancer Treatment Program foruninsured patientsSurvivorship/Palliative Cares Patient/Family Focus group held to provide anopportunity for patients and family to discussneeds and concerns throughout their cancerexperiences Hired part-time Survivorship Nurses Developed Survivorship monthly calendarof eventss Developed disease-site-specific resourcess Opened new BoutiqueQuality of Cares Prospective multidisciplinary case presentation~ New GYN and GU conferencess Genetic counselor is seeing increases in patientreferral numbers and sourcess Disease-specific nurse navigators~ New GI-GU-GYN nurse hireds Developed Monthly Quality and FinancialScorecards Developed and refined Nurse NavigatorTracking ToolIT/Biospecimenss TCGA (The Cancer Genome Atlas) and OBBR(Office of Biospecimen and Biorepository)s Analysis and assessment of CaBig and VarianNCCCP YEAR THREE GOALSs ASCO treatment summaries and care planss End of Treatment classs Health literacy study with University of Marylands Psychosocial Screenings Art program for infusion patientss Patient Binder - My Personal Treatment Journals Expand Survivorship Wellness Programs~ Explore Grant Opportunitiess Building Health Communities<strong>St</strong>aff participation in Sister’s Network “Gift of Life”Block Walk.
HMENTSNCCCP YEAR THREE: 1ST QUARTERDisparitiess Participated in African American HeritageFestival and sponsored Super Colon Exhibit;923 people toured exhibits Dr. Schultz spoke to Christian Life AfricanAmerican Church, 130 womens Breast Cancer Screening, 68 women screeneds Skin Cancer Screening, 64 screeneds Head Neck and Oral Screening, 25 screeneds Attended <strong>Center</strong> to Reduce Health DisparitiesConference in Rockvilles Formalized Health Literacy <strong>St</strong>udy withUniversity of Maryland School of PharmacyHealth Literacy and Health Information SeekingBehaviors of Cancer Patients in AmbulatoryHealth Care Settingss Collaborated with American Cancer SocietyACS Blue Suit Weekends Great Prostate Cancer Run and ProstateScreening, screened 50 mens Sister’s Network “Gift of Life” Block Walks Lead on planning Pancreatic Cancer eventPANCANs Participated on NCCCP planning team for AfricanAmerican Cultural Webinars <strong>St</strong>. <strong>Joseph</strong> Chairing Baltimore County CancerCoalition 2009-2010s Dr. Siegelbaum spoke at <strong>St</strong>. <strong>St</strong>ephens AfricanAmerican Church on prostate cancerClinical Trialss Opened 3 new studiess Attended ENACCT Training Optimizing YourTrial Recruitment and Retention Practicess Research Nurse and Outreach Coordinatorattended ENACCT trainings Completed 1st phase of Patient Survey <strong>St</strong>udy,53.8% response rateQuality of Cares Pilot Patient Education Binderss Added new Radiation Oncologists Conditions of participation approved atAugust Cancer Committee/ Updated CancerCommittee Charters Dr. Schraeder spoke at Nursing Grand RoundsTargeted Therapies 8/19/09s Dr. Berg interview with WJZ TV onColorectal Cancer, Julys End of Treatment Class initiated in Julys End of Treatment Summary andCare Plan implementeds Genetic Counseling metricss Breast Accreditation plannings First RQRS submission (patient outcome data)s Five year strategic plan for Oncology Servicesdevelopeds Dr. Schraeder and Dr. Akbari spoke atBaltimore County Cancer Coalition on Prostateand Colorectal Cancer<strong>St</strong>aff at Hopewell Walk.Survivorship and Palliative Cares Presented Nursing Grand Rounds “Survivorshipin Cancer Care”s Presented Nursing Grand Rounds “ Palliativeand Nursing Care”s Blankets of Courage provided to infusion patientss Nurse attending End of Life Seminar Sponsoredby Maryland Nurses Associations New Social Worker started in Julys Nurse Tracking Tool metricss Developed and Implemented PsychosocialScreening Process for new patientsITs VARIAN electronic medical record approveds ACCESS data base piloted for Thoracic usedfor weekly multidisciplinary conferencess Data Manager worked with five SummerResearch Scholars
THE <strong>CANCER</strong> <strong>IN</strong>STITUTE AT ST. JOSEPH MEDICAL CENTERONE TEAM. ONE PLAN. ONE PLACE.“ I am writing you to thank you and your staff for the caring and expertcare you gave during my treatments from July 2008 through October 2008.Each and every member of your staff was kind, considerate and extremelyknowledgeable. They taught me what to expect and how to deal with it.They were always available to answer my questions and those of my family.Something good comes from every experience and meeting you and having you treatme was amazing... I appreciate you more than I can say. I look forward to stoppingin and visiting as a former patient! ” s I.B.Non-Profit Org.US PostagePAIDBaltimore, MDPermit #49447601 Osler DriveTowson, MD 21204-7582stjosephcancer.com