2004 - 2007 - Cicely Saunders Institute - King's College London
2004 - 2007 - Cicely Saunders Institute - King's College London
2004 - 2007 - Cicely Saunders Institute - King's College London
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
University of <strong>London</strong><br />
Department of Palliative Care, Policy & Rehabilitation<br />
School of Medicine at Guy's, <strong>King's</strong> <strong>College</strong><br />
and St Thomas' Hospitals<br />
<strong>King's</strong> <strong>College</strong> <strong>London</strong><br />
Triennial Report <strong>2004</strong>/5-2006/7
CONTENTS<br />
1 Highlights 2<br />
2 Research 3<br />
2.1 Evaluating & Improving Care 3<br />
2.1.1 Improving Care and Services for People Affected by Cancer 4<br />
2.1.2 Improving Care and Services for People Affected by Neurological Conditions 5<br />
2.1.3 Evaluating and Improving the Cost-efficiency of rehabilitation 6<br />
2.1.4 Improving Care and Services for People Affected by HIV or AIDS 6<br />
2.1.5 Improving Care and Services in Patients with Chronic Heart Failure 7<br />
2.1.6 Improving Care and Services in Primary Palliative Care 7<br />
2.1.7 Improving the Methods to Evaluate Care and Treatments 8<br />
2.2 Symptom Led Research 11<br />
2.2.1 Measuring Symptoms across Five Far Advanced Diseases 11<br />
2.2.2 Symptoms and Care Needs Among People Dying with End-Stage Renal Disease 11<br />
2.2.3 Symptoms in Multiple Sclerosis (MS) 12<br />
2.2.4 ‘Improving Breathlessness’ Programme 12<br />
2.2.5 Managing Symptoms in Complex Neurological Disability 13<br />
2.3 Measuring Outcomes 15<br />
2.3.1 Patient Centred Palliative Outcome Scales 15<br />
2.3.2 Common Language Outcome Measures for Rehabilitation in the UK 16<br />
2.4 Living & Dying in Society 19<br />
2.4.1 A Good Death at Home: Committed to Making it an Achievable Goal 19<br />
2.4.2 Carer Experiences in Long-term Neurological Conditions 20<br />
2.4.3 Ethnicity and Culture 21<br />
2.4.4 Better Palliative Care for Older People 21<br />
3 Policy, Guidelines and Needs Assessments 23<br />
3.1 Guidelines 23<br />
3.2 Needs Assessments 23<br />
3.2.1 Epidemiological Based Needs Assessment 23<br />
3.2.2 Individual Based Needs Assessments 23<br />
4 Clinical Services 24<br />
4.1 Improving Care for People Affected by Multiple Sclerosis (MS): Translation of Study Outcomes to the Clinical Setting 24<br />
4.2 Improving Care for People with Chronic Heart Failure: Translation of Heart Failure Study to Clinical Setting 25<br />
5 Education and Outreach 27<br />
5.1 General Education: Seminars, Masterclasses and Targeted Programmes 27<br />
5.2 MSc, Postgraduate Diploma and Postgraduate Certificate in Palliative Care 28<br />
5.3 Successful MSc Alumni and their Research Study Project Titles 29<br />
5.4 Undergraduate Education 31<br />
6 The <strong>Cicely</strong> <strong>Saunders</strong> <strong>Institute</strong> of Palliative Care 32<br />
7 Research Collaborations, External Committee Work and International Keynote Lectures 33<br />
7.1 Collaborations 33<br />
7.2 Involvement in External Committees <strong>2004</strong>/5 – 2006/7 34<br />
7.3 International and Keynote Lectures 36<br />
8 Publication List 38<br />
9 Research Support 53<br />
10 Developments in Staffing 54<br />
Staff Biographies 55<br />
III
1<br />
Highlights<br />
<strong>2007</strong> is the 10-year anniversary of the founding of<br />
the Department of Palliative Care and Policy, which<br />
has grown in that time from a department comprising<br />
Professor Irene Higginson and two researchers (both on<br />
grant funding) to a large, multi-professional department<br />
with well over 40 staff, plus many honorary and visiting<br />
appointments. Although very saddened by the loss of<br />
Dame <strong>Cicely</strong> <strong>Saunders</strong> in July 2005 we have continued<br />
to drive forward her vision, through research, education,<br />
care and, importantly, the plans to develop an institute<br />
in her name.<br />
Our research is mainly applied and translational<br />
– concerned with discovering solutions to improve the<br />
care, symptom management and support for those<br />
affected by life threatening, progressive or profoundly<br />
disabling conditions. In this regard, palliative care and<br />
rehabilitation have much in common. Both specialities<br />
seek to add quality of life to the time available (whether<br />
in living with a disability or in dying), rather than finding<br />
a ‘cure to a disease’. They seek to cure or reduce the<br />
effects of symptoms, promote dignity and social and<br />
emotional support. Both involve complex ‘interventions’<br />
from a multidisciplinary team of professionals, and the<br />
success of that intervention must usually be judged on<br />
a background of deterioration in the person’s condition.<br />
Thus, the two fields face similar research challenges.<br />
This is reflected in our research activity where there is<br />
the potential to learn from each other, and from other<br />
fields, in the measurement of outcomes, in the design<br />
of evaluations of complex interventions and in the future<br />
in seeking potential solutions to symptoms, methods<br />
and ways to promote dignity and support for carers. As<br />
the remit of palliative care extends beyond cancer to<br />
include people with other long term conditions, there is<br />
an interface to be explored between rehabilitation and<br />
palliative care services to support people who live their<br />
lives with complex disability.<br />
what factors influence whether people are able to<br />
be cared for at home and to die at home, making an<br />
important contribution to end of life strategies in many<br />
countries. We have evolved several new strands of<br />
research, particularly on palliative care in Africa, the<br />
costs and benefits of rehabilitation, and improving<br />
palliative care for older people. During the period of the<br />
report, we have seen 53 MSc, Diploma and Certificate<br />
students graduate, along with 3 successful PhD awards,<br />
while continuing to evolve our undergraduate education<br />
programme.<br />
The following pages outline our research activity across<br />
four main strands - evaluating and improving care;<br />
symptom led research; measuring outcomes; and living<br />
and dying in society. It outlines our influences on policy<br />
and guidelines, educational and clinical activities, and<br />
the plans for the new <strong>Institute</strong> of Palliative Care. Shortly<br />
before her death, Dame <strong>Cicely</strong> <strong>Saunders</strong> was delighted<br />
to see plans for her brainchild developing – to create<br />
the world’s first purpose built <strong>Institute</strong> of Palliative<br />
Care. At the end of the report we list publications,<br />
keynote lectures and supporters, along with a full list of<br />
staff. We are grateful to a wide range of collaborators<br />
and colleagues with whom we work in research,<br />
teaching, care and policy. Special thanks go to those<br />
organisations, statutory and charitable, and individuals<br />
that support our activities. In a climate where in the<br />
UK less than 0.2% of the research spend in cancer<br />
goes to palliative and end of life care, with probably<br />
a lower proportion than this being allocated in noncancer<br />
conditions, their leadership has been vital to our<br />
continued work.<br />
In the period of this report, <strong>2004</strong>/5 to 2006/7, our<br />
research, teaching and policy development have<br />
advanced considerably locally, nationally and<br />
internationally. We have seen the fuller integration of<br />
palliative care and rehabilitation, especially as work<br />
in palliative care grows to consider those people with<br />
longer illness trajectories, with cancer, non-cancer<br />
and multiple conditions. Our results have underpinned<br />
some of the most significant national and international<br />
guidance, including from the National <strong>Institute</strong> of<br />
Clinical Excellence (NICE) in the UK, the State of the<br />
Science Report on End of Life Care in the USA, the UK<br />
Government White Paper on Our Health Our Choice<br />
Our Lives, the House of Commons Health Committee<br />
Report on End of Life Care and several National Service<br />
Frameworks, including that on Long Term Neurological<br />
Conditions in which Professor Lynne Turner-Stokes and<br />
her team played a substantial role.<br />
We have tested and discovered new means to improve<br />
the management of symptoms, such as breathlessness<br />
and spasticity, and have trialled new services for people<br />
with conditions beyond cancer. We have discovered<br />
2
2<br />
Research<br />
Research activity falls into four main programmes<br />
(see figure 2.1). Each programme has a series of interrelated<br />
projects and sub-programmes, with defined<br />
outputs and links to improve practice and care. Across<br />
all strands we are active in influencing policy and<br />
practice, teaching, dissemination and refining the<br />
methods to undertake research. As is clear from the<br />
text, we have a particular expertise in mixed methods,<br />
combining quantitative and qualitative approaches and<br />
in translational and applied research – seeking to make<br />
an early and sustained difference to the care of patients<br />
and families.<br />
2.1 Evaluating & Improving Care<br />
Overview<br />
Palliative care and rehabilitation both suffer from a<br />
lack of evidence about effective models of care and<br />
treatment, partly because research among severely ill<br />
or disabled people is difficult. However, work in our<br />
department has tackled these problems, conducting<br />
research and systematic reviews and developing the<br />
methodologies to evaluate care and services, often<br />
using the MRC framework for the development and<br />
evaluation of complex interventions.<br />
die do so from diseases other than cancer. Therefore<br />
while continuing a strong theme of research in cancer<br />
(cancer patients still remain an important core of<br />
palliative care), we have extended our research into<br />
non-cancer. Little is known about their experiences and<br />
in particular what services and care might help them.<br />
Our work in understanding symptoms found similar<br />
symptoms across five common diseases towards the<br />
end of life (see section 2.2), suggesting that palliative<br />
care may be valuable. But we still needed to answer the<br />
question - what models of care or services might help?<br />
Simply taking palliative care as it is offered for people<br />
with cancer may not be appropriate because of<br />
differences in other existing services, information,<br />
expectations and prognosis, and not knowing when is<br />
the right time to offer services. Therefore, we began a<br />
programme of work to develop and test palliative care<br />
services for people affected by conditions other than<br />
cancer, focusing on some specific conditions, which<br />
might serve as a model for others.<br />
Our 2001-3 report showed how palliative care has<br />
traditionally focussed on people with cancer, with<br />
around 95% of people in hospices and home care<br />
teams having cancer. However, 3 out of 4 people who<br />
Figure 2.1: Map of Department Research Programmes<br />
Multi–professional academic and clinical research team<br />
Evaluating and<br />
improving care<br />
Symptom Led Research Measuring Outcomes Living and Dying in Society<br />
Cancer<br />
Symptoms across diseases<br />
Palliative Care Outcome<br />
Scale (POS)<br />
Place of Death<br />
Neurological<br />
Symptoms in renal disease<br />
Support Team Assessment<br />
Schedule (STAS)<br />
Ageing<br />
HIV/AIDS<br />
Breathlessness<br />
Measures of Complex<br />
Disability<br />
Carers<br />
Rehabilitation<br />
Spasticity<br />
Ethnicity and Culture<br />
Primary care<br />
Pain<br />
Depression<br />
Methodological Development<br />
Policy and Guidance<br />
Teaching<br />
Dissemination<br />
Collaboration<br />
3
2.1.1 Improving Care and Services for People<br />
Affected by Cancer<br />
Gysels and Higginson conducted, for the National<br />
<strong>Institute</strong> of Clinical Excellence (NICE), the first comprehensive<br />
robust appraisal of research evidence in<br />
Supportive and Palliative Care in Cancer. Published in<br />
<strong>2004</strong>, this was the culmination of three years research,<br />
building on earlier systematic reviews within the<br />
department. It combined and appraised findings from<br />
339 studies from across the globe. It showed for the first<br />
time evidence for the effectiveness of some components<br />
of supportive and palliative care, especially for multiprofessional<br />
specialist palliative care teams, information<br />
provision and communication skills training 68 .<br />
Communication, co-ordination and patient<br />
education<br />
In an analysis of effectiveness, 12 studies (15 papers)<br />
showed communication skills training improved the<br />
communication of doctors and nurses, as assessed by<br />
self-report and patients, with effect sizes ranging from<br />
0.15 (modest) to 2 (high) 9 . One further study showed<br />
deterioration in outcomes. In depth analysis found that<br />
to be most effective at changing practice (and not just<br />
skills in artificial situations) training programmes need to<br />
take into account and address attitudes and beliefs 9 .<br />
These findings led the Department of Health in the UK<br />
to support a national roll out of communication skills<br />
training, to commit funding to specialist palliative care<br />
services and provided for the first time a research basis<br />
for supportive and palliative care elements of National<br />
Standards in Cancer Care, which now form part of the<br />
National Health Service Peer Review for cancer.<br />
However, there is also the problem of communicating<br />
between services. Farquhar, Barclay and colleagues<br />
studied in depth the concerns of GPs - of most concern<br />
was tardiness (with delays of up to eight days) especially<br />
at three stages in the patient journeys: (1) in the prediagnostic<br />
and diagnostic stage; (2) in the active<br />
treatment phase; and (3) when oncology withdrew and<br />
the focus of care switched back to the community for<br />
the terminal phase 142 , leading to suggestions in the NICE<br />
guidance about the prompt timing of information and the<br />
use of standardised formats.<br />
Interactive technologies and videotapes appear to be a<br />
promising method for patient education in cancer care.<br />
In an analysis of 1,678 patients, educational technologies<br />
showed improved patient knowledge but no change<br />
in patient satisfaction 320 although the analysis identified<br />
problems of heterogeneity (see figure 2.3).<br />
Figure 2.2 The NICE Research evidence produced by the<br />
team at King’s in <strong>2004</strong>, which is now improving how cancer<br />
care and support is provided<br />
Figure 2.3. Meta-analysis showing that video technologies in patient education improve knowledge but not satisfaction<br />
Source: Gysels and Higginson, Supportive Care in Cancer, <strong>2007</strong>;15:7-20<br />
4
Equivocal results were found in a systematic review of<br />
seven randomised and six non-experimental studies<br />
testing the role of patient held records in improving communication<br />
and information exchange. In particular, the<br />
randomised studies found an absence of effect, but the<br />
non-experimental evaluations shed light on the<br />
conditions for most successful use. Although most<br />
patients in all the studies welcomed the introduction of a<br />
patient held record, there were instances where it was<br />
not suitable for different groups, and a lack of<br />
agreement between patients and health professionals<br />
regarding its function 322 .<br />
Wider effects of the NICE guidance<br />
In some areas of supportive and palliative care our<br />
review found a dearth of robust studies evaluating<br />
services or understanding the longitudinal experience of<br />
cancer, sometimes because of methodological<br />
challenges, in contrast to a relative abundance of crosssectional<br />
studies assessing need 15 . An analysis of<br />
evaluations of palliative day care found qualitative<br />
support for services, but a lack of quantitative studies 137 .<br />
A similar picture was found for hypnotherapy used to<br />
treat symptoms in advanced cancer 160 . An overwhelming<br />
recommendation was that there should be sustained<br />
programmes of research into testing solutions and<br />
longitudinal study. Furthermore the work strongly<br />
advocated that services should be developed only in the<br />
context of robust evaluation. This finding fed into the<br />
National Cancer Research <strong>Institute</strong>’s analysis of<br />
research in Supportive and Palliative Care to begin to<br />
emphasise research to evaluate services and<br />
treatments.<br />
But the Gysels and Higginson review had much wider<br />
effects. It formed the bedrock for the evidence reviews<br />
for the National Service Framework on Long Term<br />
Neurological Conditions, led by Turner-Stokes and<br />
colleagues, which also found evidence to support some<br />
models of rehabilitation and palliative care. In addition, it<br />
underpinned appraisals in other countries, including the<br />
State of the Science Review on End of Life Care,<br />
National <strong>Institute</strong>s of Health, USA.<br />
Survival and quality of life in advanced cancer<br />
In collaboration with colleagues in the USA and Canada,<br />
through a visiting appointment of Dr Antonio Vigano, we<br />
analysed data from two independent cohorts (248<br />
patients in Canada [collected by Professor Eduardo<br />
Bruera and team - Cohort 1] and 756 patients in Ireland<br />
[collected by Professor Irene Higginson and team and<br />
using the outcome measures that we had previously<br />
developed and validated - Cohort 2]. After adjusting for<br />
clinical and demographics variables, using Cox<br />
regression models, physical health related quality of life<br />
indicators - dyspnoea, nausea/emesis and weakness –<br />
were associated with survival, as were liver metastases,<br />
lung tumour and tumour burden. In contrast, emotional<br />
functioning, anxiety, spiritual distress, and lack of insight<br />
were not associated consistently with survival in either<br />
cohort. The study brings into question the prognostic<br />
significance of "positive attitudes", such as hope and<br />
optimism, in patients with advanced cancer, and instead<br />
suggests that physical indicators are more important 34 .<br />
2.1.2 Improving Care and Services for People<br />
Affected by Neurological Conditions<br />
Through collaboration with colleagues in Neurology we<br />
have established the King’s Centre for Palliative Care in<br />
Neurology – a ‘virtual centre’ representing a collaboration<br />
to foster and further research to improve the care of<br />
patients with neurological conditions who need palliative<br />
care and/or rehabilitation.<br />
Developing and testing new palliative care<br />
services for people affected by Multiple Sclerosis<br />
Multiple sclerosis (MS) is a chronic disease affecting the<br />
central nervous system. It affects over 2.5 million people<br />
worldwide, is the commonest cause of neurological<br />
disability in adults under 60 years, and is associated<br />
with a wide spectrum of physical and psychological<br />
symptoms. While the outlook for many is good and<br />
some have a normal life expectancy, around 45% of<br />
people do develop progressive forms, either from the<br />
outset or at later stages, with profound effects not only<br />
for themselves but also their carers.<br />
Developing and testing palliative care for people<br />
affected by MS raises important questions. How should<br />
the service be modelled? What sort of staff does it<br />
need? When is it really needed? Who might benefit<br />
most? Will it replace or supplement existing services?<br />
How might it work with these? Nowhere in the world are<br />
these questions answered.<br />
To investigate this we embarked on a programme,<br />
supported by the UK MS Society, using the MRC<br />
Framework for Evaluating Complex Interventions (see in<br />
Focus 2.1) to develop and test a new palliative care<br />
service for people with MS.<br />
We found that people with the progressive forms of MS<br />
had new concerns about losses and changes (including<br />
financial worries), as a result of the illness. In addition, they<br />
reported ‘having to fight for everything’ as far as access to<br />
care was concerned. This was closely linked to a lack of<br />
coordination and continuity of care, difficulties getting<br />
appropriate information and a poor quality non-specialist<br />
care 319 . While these findings from in depth interviews<br />
made great sense to people affected by MS, Edmonds et<br />
al’s 319 report was the first systematic analysis.<br />
Further interviews and focus groups with healthcare<br />
professionals echoed the patients’ concerns with poor<br />
continuity of care and limited resources. But in addition<br />
doctors and nurses were also bothered by communication<br />
between professionals; unequal provision of and access<br />
to services; patients’ problems with some symptoms,<br />
especially with cognition; bladder and sexual function; and<br />
the needs of patients and their carers around the end of a<br />
person’s life. All these difficulties were compounded<br />
because of the unpredictable course of MS 232 .<br />
This information enabled us to model a new palliative<br />
care service for people affected by MS. This consisted<br />
of a consultant in palliative medicine, a clinical nurse<br />
specialist and a psychosocial worker, some shared with<br />
the existing palliative care service and with close<br />
integration with neurology services. We evaluated this<br />
using our new methods of a fast track versus standard<br />
randomised controlled trial 232 and results are currently<br />
being analysed.<br />
5
As part of the project, resources have been developed<br />
to support people affected by MS and health and social<br />
care professionals, including a referral pathway for care<br />
professionals and a paper and web-based service<br />
directory (see section 4.1).<br />
The palliative care needs of people with<br />
late stage Parkinson’s Disease (PD), Multiple<br />
System Atrophy (MSA), and Progressive<br />
Supranuclear Palsy (PSP)<br />
Building on our earlier research we have commenced a<br />
new study, supported by the Department of Health (UK)<br />
to understand the experiences and needs of people<br />
severely affected by PD, MSA and PSP in order to identify<br />
the most effective approaches to enhancing quality of life<br />
and providing flexible personalised support. Patients and<br />
carers are recruited to a longitudinal study, which<br />
measures symptom problems and costs of care.<br />
2.1.3 Evaluating and Improving the Costefficiency<br />
of Rehabilitation<br />
There is now reasonable evidence to support the costeffectiveness<br />
of rehabilitation following brain injury 84 .<br />
But which patients may benefit most?<br />
Routine collection of data in the course of clinical<br />
practice is key to the demonstration of effective and<br />
cost-efficient practice. Within this three-year cycle,<br />
Turner-Stokes et al have analysed a six-year longitudinal<br />
cohort 251 to examine whether our rehabilitation<br />
programme is effective in reducing long term care<br />
needs, such that it could pay for itself through reducing<br />
the cost of on-going care. The programme uses<br />
measures developed in earlier research (see section 2.3).<br />
It is often thought that rehabilitation is not worthwhile for<br />
very severely dependent patients because they will remain<br />
dependent on care to some degree. However, our study<br />
showed that, contrary to expectation, rehabilitation was<br />
in fact most cost-effective for these heavily dependent<br />
patients. Although they required longer periods of<br />
rehabilitation, and thus cost more to treat, the gains<br />
in reduction of care costs were much higher than in the<br />
less dependent group, so the initial cost of rehabilitation<br />
was more quickly offset by savings in on-going care 252 .<br />
Moreover, serial analysis of change in dependency for the<br />
most dependent and long-staying patients confirmed that<br />
they continued to make changes throughout their<br />
admission, and that earlier discharge would have led to<br />
poor outcomes and increased care needs 313 .<br />
The Functional Independence Measure (FIM TM ) is widely<br />
used in the USA and Europe as an outcome measure for<br />
rehabilitation and benchmarking of services and FIMefficiency<br />
(Gain in FIM score / Length of stay) is often<br />
used as a surrogate for cost-efficiency. A further<br />
interesting finding from this study was that the FIM did<br />
not demonstrate the additional cost benefits of rehabilitation<br />
in the highest dependency group that were<br />
revealed by the group’s new measure, the NPDS (see<br />
figure 2.4) 314 .<br />
2.1.4 Improving Care and Services for People<br />
Affected by HIV or AIDS<br />
In the era of antiretroviral therapy (ART), palliative care has<br />
a new and evolving role in supporting treatment, as well as<br />
caring for those for whom treatment is either not available<br />
or cannot prevent disease progression. All of these groups<br />
may require palliative care to address the physical,<br />
spiritual and emotional pain related to the disease and its<br />
treatment. It should be remembered that there are<br />
significant excess risks associated with HIV infection for<br />
several cancers, including Kaposi’s Sarcoma, lymphoma,<br />
vulval and cervical cancer; linking our work in this<br />
programme very directly with our cancer programme.<br />
Harding and Higginson have been collaborating in the<br />
USA, UK and Africa to investigate the palliative care<br />
needs of patients with early as well as advanced disease,<br />
both in resource-rich and resource-poor countries.<br />
Change in FIM score<br />
Change in NPDS score<br />
100<br />
20<br />
80<br />
10<br />
60<br />
0<br />
Change in Total FIM<br />
40<br />
20<br />
0<br />
-20<br />
-40<br />
N= 83<br />
Low<br />
Dependency group<br />
111<br />
Medium<br />
102<br />
High<br />
Change in NPDS score<br />
-10<br />
-20<br />
-30<br />
-40<br />
-50<br />
-60<br />
N= 82<br />
Low<br />
Dependency group<br />
111<br />
Medium<br />
100<br />
High<br />
Figure 2.4 Comparison of the change in FIM (old measure) and NPDS (new more sensitive measure) scores across the three dependency groups.<br />
Box plots show median, inter-quartile range, range and outliers<br />
Source: Turner-Stokes et al, Arch Phys Med Rehab 2006; 87(11) e11.<br />
6
Evaluation of HIV/AIDS services<br />
in the USA and UK<br />
In collaboration with colleagues in the USA, we evaluated<br />
new palliative care services for people with HIV and AIDS.<br />
Analysis of clients needs entering the three services<br />
identified problems of poor mental health 24 , especially<br />
clients with history of drug dependence (in Baltimore) and<br />
more severe physical symptoms (in New York).<br />
Conversely, better mental health was most strongly<br />
correlated with more positive perceptions of interpersonal<br />
relationships and of meaning and purpose in life,<br />
underlining the need to take a holistic approach to care.<br />
Most clients at all programs were socioeconomically<br />
disadvantaged, from ethnic minorities, and had a history<br />
of substance abuse, although significant differences were<br />
noted in the distributions of clients at each program with<br />
regard to these characteristics. A common set of medical<br />
(ambulatory/outpatient care, laboratory testing,<br />
pharmacy) and ancillary (nutritional counselling, transportation)<br />
services were identified by at least 25% of clients<br />
and staff at each program. These findings suggested<br />
there is a need for a mix of "care" and "cure" services to<br />
reflect the erratic disease trajectory experienced by some<br />
clients who move in and out of treatment as well as the<br />
vulnerability and marginalized lives of the clients served<br />
by these programs 23 .<br />
Two systematic literature reviews appraised effectiveness<br />
of 146 and access to 147 palliative care in HIV disease.<br />
Analysing data from 34 studies found that home and<br />
inpatient palliative care significantly improved patient pain<br />
and symptom control, anxiety, insight, and spiritual<br />
wellbeing 146 . Despite this evidence, and the clear<br />
symptom and psychological needs care is often poor and<br />
less than optimal. The results proposed a model of<br />
integrated palliative care from diagnosis to end-of-life,<br />
alongside antiretroviral therapy when initiated.<br />
HIV/AIDS and cancer research in Africa<br />
Supported by the Princess Diana Foundation, Harding<br />
and Higginson researched the nature of palliative care<br />
services in Africa 148 . Here the palliative care services<br />
support patients with both cancer and HIV/AIDS. The<br />
analysis suggested home and community-based<br />
palliative care has been largely successful, but<br />
community capacity and the resources and clinical<br />
supervision necessary to sustain quality care are<br />
lacking. Coverage and referrals must be primary<br />
concerns. Simple lay and professional protocols have<br />
been developed, but opioid availability remains a major<br />
constraint to the success of palliative care programmes<br />
in Africa. Areas of good practice, and areas where<br />
further success may be achieved include: attention to<br />
community needs and capacity; explicit frameworks for<br />
service development and palliative-care integration<br />
throughout the disease course (including antiretroviral<br />
provision); further education and protocols; strengthening<br />
and dissemination of diverse referral and care<br />
systems; increasing advocacy; and funding and<br />
technical skills to build audit and quality assessment.<br />
Building from this Logie and Harding found that although<br />
morphine regulation had achieved its goal of preventing<br />
misuse and leakage from the supply chain, confusion<br />
and complexity in storage and authorisation rules led to<br />
discontinuation of opioid pain management for patients<br />
and also wasted service time in trying to obtain supplies<br />
to which they were entitled. The multi-method study also<br />
identified under-prescribing, as a result of clinician<br />
behaviour and public fear of opioids 158 .<br />
In a new partnership with MEASURE Evaluation (an<br />
evaluation team at the University of North Carolina, USA)<br />
Harding and Higginson have launched a new<br />
programme to evaluate the palliative care for patients<br />
with HIV in Kenya and Uganda. This will be the first<br />
study in the world to evaluate the clinical, social and<br />
psychological outcomes and costs comparing different<br />
models of palliative care in Africa. It is being conducted<br />
in collaboration with Paul McCrone, Health Economist in<br />
the <strong>Institute</strong> of Psychiatry, King’s <strong>College</strong> <strong>London</strong>.<br />
2.1.5 Improving Care and Services in Patients<br />
with Chronic Heart Failure<br />
In advance of developing a new clinical service at Guy’s<br />
and St Thomas’ Hospital, the end of life preferences of<br />
patients and families were explored. Of the 20 patients, all<br />
with New York Heart Association Functional classification<br />
III – IV, and 11 family carers, none had discussed their end<br />
of life preferences with clinicians or were aware of choices<br />
or alternatives in future care, such as availability of<br />
palliative services. The patients and families appeared to<br />
be living with fear and anxiety but were uninformed about<br />
the implications of their diagnoses. Interviews with<br />
clinicians confirmed that they rarely raised such issues<br />
with patients. The results highlighted a need to provide<br />
mechanisms to offer sensitively developed information<br />
and opportunities for discussion about future care issues,<br />
including the end of life and has led to agreed referral<br />
criteria and a preliminary care pathway, which will be<br />
evaluated through future research 337 .<br />
2.1.6 Improving Care and Services in Primary<br />
Palliative Care<br />
Evaluating the National Palliative Care<br />
Education and Support Programme for District<br />
and Community Nurses<br />
The department was commissioned by the Department<br />
of Health (DoH) to evaluate this national palliative care<br />
education and support programme for district and<br />
community nurses which ran from 2001-<strong>2004</strong>. Professor<br />
Julia Addington-Hall led this multi-professional and<br />
multi-site project, with Cathy Shipman as the primary<br />
researcher. It aimed to evaluate the acceptability and<br />
effectiveness of the programme by assessing whether it<br />
had measurable impact on district nurses’ (DNs)<br />
confidence in competency and knowledge, on GPs<br />
perceptions of the adequacy of communication, on the<br />
views of bereaved relatives, on place of death and<br />
referrals to specialist palliative care services.<br />
The educational programmes were provided through all<br />
34 Cancer Networks in England and the range of<br />
educational models and methods of delivery used were<br />
identified and categorised. Both quantitative and<br />
qualitative methods were used in a ‘before and after<br />
design’ to assess the impact of the programme in eight<br />
randomly selected cancer networks on the confidence<br />
and knowledge of DNs, views of GPs and of bereaved<br />
carers. Quantitative methods included using postal questionnaires<br />
and qualitative methods included conducting<br />
face-to-face and telephone interviews and focus groups.<br />
A major success was the nationwide development of<br />
educational programmes across all 34 Cancer Networks<br />
7
which focused on a core curriculum although delivering<br />
this in varying ways dependent on local needs and<br />
resources. The process of establishing and providing<br />
the educational programmes led to improved relationships<br />
between specialist palliative care providers and<br />
primary care practitioners. About one third of members<br />
of DN teams in England were estimated to have been in<br />
contact with one of the network programmes, and there<br />
were small statistically significant improvements<br />
identified in DNs perceptions of confidence in palliative<br />
care competencies and in palliative care knowledge.<br />
Interviews with DNs, programme providers and commissioners<br />
identified ways in which the programmes were<br />
felt to have been successful. Further details of results<br />
can be found in the report to the DoH which can be<br />
accessed via www.kcl.ac.uk/palliative.<br />
Working with Primary Care Trusts (PCTs):<br />
Perspectives on caring for dying people<br />
in <strong>London</strong><br />
A two year research and development project was<br />
completed in March 2005 185 for the King’s Fund. This<br />
project, which worked with five PCTs across <strong>London</strong>,<br />
found variations between how different PCTs organised<br />
their community palliative care services and in the range of<br />
services offered. The three key services providing palliative<br />
care within primary care were GPs, district nurses and<br />
clinical nurse specialists, linked together within a<br />
‘Supportive Triangle.’ Good relationships underpinned this<br />
collaboration, but over-stressed services and communication<br />
breakdowns could threaten it.<br />
Evaluation of a telephone advice and<br />
information line for patients with advanced<br />
disease and their carers<br />
One barrier to effective primary palliative care is the<br />
fundamental lack of awareness of palliative care and<br />
related services among disadvantaged groups within<br />
society, such as people over 65, people from black and<br />
ethnic minority (BME) communities and those living in<br />
socially and materially deprived areas. The usage of<br />
traditional routes to access health information and<br />
advice, such as NHS Direct, is equally low among these<br />
vulnerable groups. On the basis of these findings, a<br />
partnership was established between NHS Direct and<br />
the King’s Fund to launch a pilot project called<br />
COMPASS, a palliative care telephone helpline for<br />
patients, carers and health care professionals.<br />
Longhurst, Koffman and Shipman conducted a process<br />
evaluation of COMPASS, auditing calls, conducting<br />
qualitative interviews with staff, managers and key<br />
stakeholders and follow-up interviews with callers to the<br />
helpline. The results suggested that COMPASS provided<br />
information to previously underserved population groups<br />
such as ethnic minorities, and was a resource for health<br />
professionals 384 .<br />
Scoping exercise on generalist services for<br />
adults at the end of life: research, knowledge,<br />
policy and future research needs<br />
Higginson and Shipman are leading a multi-site international<br />
team that won, in 2006, the NHS Service Delivery &<br />
Organisation R&D Programme (SDO) call to undertake a<br />
scoping exercise on generalist services for adults at the<br />
end of life. The work maps current research, knowledge<br />
and policy to identify specific topics for research to<br />
inform the future commissioning by the SDO programme.<br />
This exercise presented an important opportunity to<br />
identify priorities for research to improve generalist<br />
services for adults at the end of life, which will lead<br />
directly to a call for research by SDO in 2008, and may<br />
influence the support by other research organisations.<br />
2.1.7 Improving the Methods to Evaluate Care<br />
and Treatments<br />
Because of the lack of evaluative studies our work has<br />
focused on refining the methods to evaluate services<br />
and treatments, building on the MRC framework for the<br />
evaluation of complex interventions (see In Focus 2.1),<br />
and applying this in two recent studies. Through this and<br />
other methods we have developed and refined<br />
randomised controlled trial (RCT) methods, seeking to<br />
overcome many of the problems found in previous<br />
palliative care and rehabilitation trials. In addition to<br />
using for the first time in palliative care a delayed<br />
intervention randomised trial (In Focus 2.1). Separately<br />
Harding and colleagues 13 developed methods for, and<br />
conducted, a community based RCT of multi-session<br />
group work for HIV prevention among 50 gay men in the<br />
UK. At eight weeks, those attending the group reported<br />
significant gains over their control in making sexual<br />
choices, physical safety, HIV and STI transmission<br />
knowledge, and sexual negotiation skills. The trial also<br />
demonstrated that high-risk community samples could<br />
be recruited to multi-session interventions, and provided<br />
feasibility data for future evaluations.<br />
Health economic evaluation in palliative care is in its<br />
infancy, and yet there is a desperate need to understand<br />
better the costs of, and choices between, services.<br />
Standard utility measures based on survival, such as<br />
Quality Adjusted Life Years, do not reflect the needs and<br />
concerns in palliative care or rehabilitation. Working with<br />
colleagues at the <strong>London</strong> School of Hygiene and<br />
Tropical Medicine, we found that a new approach, the<br />
Choice Experimentation Method, could be used in<br />
palliative day care to help patients prioritise between<br />
different service elements 138 . In 79 patients attending<br />
four day care centres, the Choice Experimentation<br />
Method found that access to specialist therapies was<br />
three times more important than medical support, and<br />
twice as important as staying all day. More recently,<br />
working with Dr Paul McCrone and colleagues at the<br />
<strong>Institute</strong> of Psychiatry, we have begun to measure costs<br />
of health and social care, the costs incurred by patients<br />
and families, and the cost effectivness of treatments<br />
in some of our studies.<br />
8
In focus 2.1 New methods to evaluate services<br />
Refining the MRC Framework in palliative care<br />
and developing a new approach to randomised<br />
controlled trials<br />
Patients and families in palliative care and rehabilitation<br />
have complex needs, often needing multi-professional<br />
and complex services. Therefore, we looked to follow<br />
the latest developments in health care research and<br />
found valuable the Medical Research Council’s (MRC)<br />
‘Framework for the Development and Evaluation of RCTs<br />
for Complex Interventions to Improve Health’ (MRC,<br />
<strong>London</strong> 2000). This provides investigators with guidance<br />
in recognising the unique challenges that arise in the<br />
evaluation of complex interventions, as well as<br />
suggesting strategies for addressing these issues in the<br />
development of trials.<br />
Complex interventions are built from a number of<br />
components which may act independently and interdependently.<br />
The framework suggests that a series of<br />
phases of investigation take place which may, in reality, be<br />
more iterative (Campbell et al, BMJ 2000;321:694-696)<br />
including: 1) a ‘Pre-clinical’ or theoretical phase; 2) Phase I<br />
or modelling; 3) Phase II or exploratory trial; 4) Phase III or<br />
definitive RCT; and 5) Phase IV or long-term surveillance<br />
(see figure). We believed that this framework would be<br />
especially useful because our earlier systematic reviews<br />
(Higginson et al, JPSM 2003;25:150-168, Harding and<br />
Higginson, Pall Med 2003;17:63-74; see also 2001-3<br />
report) and the results of the NICE guidance on supportive<br />
and palliative care 68 had found a poor understanding of<br />
what services did, wide variation in practice, as well as<br />
poor evaluation designs, which led to failed studies.<br />
We worked with the framework and are using it in two<br />
studies to evaluate palliative care ‘complex interventions’:<br />
(a) A new palliative care service for people<br />
severely affected by MS (see section 2.1.2); and (b) A<br />
Breathlessness Intervention Service (see section 2.2).<br />
The randomised trial; gave good recruitment<br />
and was acceptable in palliative care<br />
Although use of the MRC framework in palliative care<br />
evaluation is in itself innovative, we also have tested a<br />
further new development for palliative care research –<br />
that of using fast-track versus standard (or wait-list/<br />
delayed intervention) designs for their Phase II trials 232 .<br />
This design has been used in studies of behavioural<br />
interventions in education (Flannery et al, Dev Psychol<br />
2003;39:292-308), health education (Morgan et al, Rev<br />
Med 1996;25:346-354) and occasionally in health care<br />
(Fonda et al, Age and Ageing 1995;24:283-286). In the<br />
trial, the ‘fast-track’ group receive the intervention or<br />
service immediately after baseline interview, whereas<br />
the control group also receive the intervention, but only<br />
after a period of delay. As a result, potentially every<br />
participant is offered the intervention, potentially<br />
reducing selection bias and disappointment. In the<br />
health services some delay is often common, and even<br />
in palliative care there are waiting lists for some services<br />
and others that are not widely available.<br />
Theory<br />
Modelling<br />
Exporatory trial<br />
Definitive RCT<br />
Long–term<br />
implementation<br />
Explore relevant<br />
theory and<br />
evidence to ensure<br />
best choice of<br />
intervention<br />
and predict<br />
confounders<br />
Identify<br />
components<br />
of required<br />
intervention and<br />
the underlying<br />
mechanisms,<br />
explore how<br />
intervention might<br />
work in practice<br />
Describe the<br />
components of the<br />
intervention, test<br />
its likely effects<br />
and protocol for<br />
comparitive study,<br />
continue to revise<br />
intervention<br />
Test fully developed<br />
intervention<br />
compared to<br />
alternative/control<br />
in appropriate<br />
comparitive<br />
protocol in study<br />
with appropriate<br />
statistical power<br />
Determine<br />
whether others<br />
can replicate the<br />
results by testing<br />
in multi–centre<br />
studies<br />
Pre–clinical–<br />
Phase 0<br />
Phase 1 Phase II Phase III Phase IV<br />
Continuum of increasing evidence<br />
Figure 2.5 The Medical Research Council Framework for the development and evaluation of complex interventions<br />
Source: MRC.ac.uk<br />
9
Our trials using this design have achieved substantially<br />
better uptake and recruitment than previous palliative<br />
care randomised trials 232 . While many factors may have<br />
contributed to our improved recruitment, to date we<br />
have found the use of the MRC framework and the ‘fasttrack’<br />
versus ‘current best practice’ design acceptable<br />
to staff, patients, families, patient representative<br />
organisations, funders and research ethics committees.<br />
In both studies we have found that attention is needed to<br />
decide the ‘correct’ period of control before the intervention<br />
is offered. This had to be different in our two<br />
studies - because we had to base it on how stable the<br />
patients were and how quickly we expected the service<br />
to have an effect. We have also found that using the<br />
MRC Framework was more costly than traditional<br />
designs, in the short term, because of the need to<br />
undertake phase I and II work 232 . However, in the long<br />
term, if the trial is successful it represents a good<br />
investment in research, especially as traditional designs<br />
have often failed.<br />
Almost all studies within the department employ mixed<br />
method approaches - where quantitative and qualitative<br />
methods are used together, one informing the other. We<br />
are further developing the ways that these methods are<br />
integrated and work to give a rounded picture of the<br />
issues faced by patients and families, whose problems<br />
are usually complex and multi-dimensional, requiring a<br />
multi-professional and multi-method approach, especially<br />
to capture less tangible aspects such as quality of life,<br />
quality of care, dignity and caregiver needs.<br />
10
2.2<br />
Symptom Led Research<br />
Our research into symptoms assessed both the range of<br />
symptoms in different conditions, and the management<br />
of individual symptoms, which can be common across<br />
several conditions.<br />
2.2.1 Measuring Symptoms Across Five Far<br />
Advanced Diseases<br />
Research by Solano, Gomes and Higginson 250 , and<br />
supported by <strong>Cicely</strong> <strong>Saunders</strong> International, established<br />
that patients’ symptoms, especially pain, fatigue and<br />
breathlessness, are as common and as high in four nonmalignant<br />
diseases as in cancer. This evidence has been<br />
instrumental in advocating the expansion of palliative<br />
care beyond cancer, so that patients with other<br />
advanced and progressive diseases such as chronic<br />
heart disease, AIDS, COPD and end stage renal failure<br />
can benefit. It also produced symptom profiles for these<br />
groups of patients, which can be used as a preliminary<br />
basis to model services.<br />
The comparative grid (see table 2.1) showed that the<br />
prevalence of the 11 symptoms is widely but homogeneously<br />
spread across the five diseases, thus there<br />
appears to be a common pathway towards death for<br />
malignant and non-malignant diseases.<br />
2.2.2 Symptoms and Care Needs Among<br />
People Dying with End-Stage Renal Disease<br />
In collaboration with the Renal Units at King’s <strong>College</strong><br />
Hospital, Guy’s Hospital, and Canterbury Hospital this<br />
innovative study, led by Murtagh and Higginson, is at the<br />
forefront of research into the palliative care needs of<br />
patients with end-stage renal disease who are managed<br />
conservatively, without dialysis. Nephrology services are<br />
recognising that this steadily increasing group of<br />
patients have unmet palliative care needs. There is<br />
however little evidence to underpin service development.<br />
This study is beginning to address this gap, supported<br />
by the Guys and St Thomas’ Charity.<br />
A systematic review of symptom prevalence in renal<br />
disease found no studies among patients who are<br />
conservatively managed 331 , as well as a lack of longitudinal<br />
studies. The similarity of symptoms between endstage<br />
renal disease and cancer were confirmed in a pilot<br />
survey 247 . This led to the development of a longitudinal<br />
study, which is due to report in <strong>2007</strong>/8.<br />
However, our first cross-sectional data on the epidemiology<br />
of symptoms shows levels of symptom prevalence<br />
and overall symptom burden that are comparable to<br />
those experienced by patients with cancer and other noncancer<br />
diseases (see figure 2.6). Opioid use for analgesia<br />
in these patients is especially challenging, and as a result,<br />
evidence-based detailed clinical recommendations have<br />
been prepared 388 . Qualitative data on the impact of<br />
symptoms, information and care preferences of this very<br />
elderly population is currently being analysed.<br />
Symptoms<br />
Cancer<br />
AIDS<br />
Heart Disease<br />
COPD<br />
Renal Disease<br />
Pain<br />
35–96%<br />
63–80%<br />
41–77%<br />
34–77%<br />
47–50%<br />
Fatigue<br />
32–90%<br />
54–85%<br />
69–82%<br />
68–80%<br />
73–87%<br />
Breathlessness<br />
10–70%<br />
11–62%<br />
60–88%<br />
90–95%<br />
11–62%<br />
Anorexia<br />
30–92%<br />
51%<br />
21–41%<br />
35–67%<br />
25–64%<br />
Confusion<br />
6-93%<br />
30–65%<br />
18–32%<br />
18–33%<br />
–<br />
Anxiety<br />
13–79%<br />
8–34%<br />
49%<br />
51–75%<br />
39–70%<br />
Depression<br />
3–77%<br />
10–82%<br />
9–36%<br />
37–71%<br />
5–60%<br />
Insomnia<br />
9–69%<br />
74%<br />
36–48%<br />
55–65%<br />
31–71%<br />
Nausea<br />
6–68%<br />
43–49%<br />
17–48%<br />
–<br />
30–43%<br />
Constipation<br />
23–65%<br />
34–35%<br />
38–42%<br />
27–44%<br />
29–70%<br />
Diarrhoea<br />
3–29%<br />
30–90%<br />
12%<br />
–<br />
21%<br />
Table 2.1 Prevalence of Symptoms in Five Advanced Diseases; results of a systematic review<br />
Source: Solano et al, JPSM 2006;30(1):58-69<br />
_<br />
11
2.2.3 Symptoms in Multiple Sclerosis (MS)<br />
As part of the development and evaluation of palliative<br />
care services for people affected by MS (see 2.1.2) we<br />
found that people severely affected by MS had an<br />
average of nine (median = 8.5, mode = 12) symptoms.<br />
As for other conditions, pain and fatigue/lack of energy<br />
were found in over 50% of the 52 study participants, but<br />
four other symptoms were equally common - problems<br />
using legs, problems using arms, spasms, and feeling<br />
sleepy. Higher levels of disability were correlated with<br />
greater symptom severity for nine symptoms (Spearman<br />
rho 0.28-0.56, p < 0.05), suggesting that there was a<br />
weak to modest link between increasing disability and<br />
more severe symptoms 231 .<br />
2.2.4 ‘Improving Breathlessness’ Programme<br />
A five-year integrated programme on breathlessness<br />
commenced in September <strong>2004</strong>. Primarily supported by<br />
<strong>Cicely</strong> <strong>Saunders</strong> International and led by Higginson,<br />
Gysels and Booth, it builds on work within King’s and<br />
Cambridge, with specific projects winning external<br />
funding. Individual projects are testing treatments and<br />
new models of care and are providing a better understanding<br />
of the experience of breathlessness among<br />
patients and their carers over time. Their results are<br />
being combined to discover multi-professional multidimensional<br />
means to alleviate breathlessness.<br />
Improving the experience of breathlessness<br />
in different conditions<br />
Exploring the experience of breathlessness in 27<br />
patients with chronic heart failure, Edmonds and<br />
colleagues identified three dominant experiences of<br />
breathlessness, "everyday", "worsening" and "uncontrollable",<br />
predominantly focused on physical functioning.<br />
Worsening breathlessness was a symptom that patients<br />
were unable to manage and prompted a hospital<br />
admission, whereas uncontrollable breathlessness was<br />
experienced as a symptom that even health care<br />
professionals struggled to control 140 . However, it is not<br />
known whether heart failure patients' descriptions of<br />
breathlessness are different to those of cancer patients.<br />
Therefore, Gysels, Bausewein, Malik and Higginson are<br />
embarking on an integrated series of studies to further<br />
explore the experiences of breathlessness among<br />
patients with different conditions (lung cancer, COPD,<br />
cardiac failure, MND) and in different care settings.<br />
Gysels has completed interviews with patients and<br />
carers in all groups, and Bausewein is investigating for<br />
her PhD, the experience of breathlessness over time and<br />
the effectiveness of a hand-held fan in the home. Here a<br />
pragmatic trial is embedded as part of the longitudinal<br />
component where patients are randomised either to the<br />
use of a handheld fan or a wristband. As an initial phase,<br />
we have completed a systematic literature review to<br />
identify the appropriate measures for the trial 317 . For her<br />
Fatigue<br />
Itching<br />
Drowsiness<br />
Feeling anxious<br />
Dyspnoea<br />
Swelling arms or legs<br />
Pain<br />
Muscle cramps<br />
Dry mouth<br />
Restless legs<br />
Lack of appetite<br />
Dry skin<br />
Difficulty concentrating<br />
Difficulty sleeping<br />
Constipation<br />
Dizziness<br />
Muscle soreness<br />
Nausea<br />
0% 20% 40% 60% 80% 100%<br />
quite a lot / very much<br />
a little / somewhat<br />
none<br />
missing data<br />
Figure 2.6 Symptom prevalence at first symptom assessment in patients (N=65) with conservatively managed end-stage renal disease<br />
Source: Murtagh et al, Journal of Pain & Palliative Care Pharmacotherapy, <strong>2007</strong> In press<br />
12
PhD, Malik is exploring the experiences of caregivers,<br />
and how patient symptoms and care affects them, with<br />
a particular focus on sleep.<br />
Evaluation of a new breathlessness intervention<br />
service in Cambridge<br />
One specific new intervention for Breathlessness is<br />
being tested with Addenbrooke’s NHS Trust, Cambridge,<br />
UK. The Breathlessness Intervention Service (BIS) is a<br />
service for patients with intractable breathlessness<br />
(regardless of their diagnostic group) and their carers,<br />
located within the Palliative Care Team. The evaluation<br />
follows the MRC’s framework for the evaluation of<br />
complex interventions, see section 2.1.7.<br />
pilot pragmatic fast-track (delayed intervention)<br />
randomised controlled trial of the service with COPD<br />
patients (see In Focus 2.1). The trial uses a mixed<br />
methodology including clinical outcomes, quantitative<br />
measures and qualitative elements to explore the impact<br />
of the intervention (patient experience) and its outcome<br />
on patients’ quality of life. Uniquely among evaluations<br />
of breathlessness services to date, carer outcomes and<br />
the views of staff and referring agencies are also being<br />
collected. The pilot trial is providing the opportunity to:<br />
(1) examine the acceptability of a fast-track RCT<br />
methodology with breathless patients in a palliative care<br />
setting; (2) test the protocol and randomisation strategy;<br />
and (3) assess the acceptability and suitability of the<br />
Booth and Higginson, after winning support from the<br />
Gatsby Charitable Foundation, conducted Phase I (the<br />
modelling phase) consisted of a qualitative study of<br />
service users and audit of breathlessness management<br />
locally. This built on a Pre-Clinical (theoretical) phase –<br />
which showed that lung cancer and COPD patients<br />
found breathlessness a frightening, disabling and<br />
restricting condition. Carers also reported severe anxiety<br />
and helplessness and felt powerless. Existing services<br />
were highly valued, but were described as inconsistent<br />
and sporadic 212 .<br />
In Phase I the BIS service was commenced and<br />
Farquhar conducted qualitative interviews with patients<br />
(n=10) and carers (n=9) using it, GPs (as referrers, n=4),<br />
respiratory nurses (as referrers, n=2) and BIS staff<br />
themselves (n=2). Patients and carers valued BIS;<br />
positive aspects included: its positive, educational<br />
approach which emphasised what was possible (not<br />
what lost); non-pharmacological strategies which were<br />
described as helpful and new; and the open access to<br />
advice and flexibility of BIS, which was especially helpful<br />
when patients were frightened. However, some aspects<br />
required development, including carers’ need for more<br />
support and information; the problem of the historical<br />
location of BIS within oncology; and the need for prior<br />
information about BIS before patients were seen by the<br />
service. In addition, referrers valued the educational role<br />
and second opinion that BIS provided 212 .<br />
various outcome measures for both patients and carers<br />
before a formal Phase III trial of all patients referred to<br />
the service (regardless of diagnostic group) commences.<br />
2.2.5 Managing Symptoms in Complex Neurological<br />
Disability<br />
The Regional Rehabilitation Unit at Northwick Park<br />
provides in-patient rehabilitation for younger adults with<br />
complex neurological disabilities whose needs for<br />
rehabilitation are beyond the scope of their local<br />
services. The prompt management of symptoms such<br />
as pain, depression and spasticity is key to the success<br />
of rehabilitation in this group.<br />
We have developed a series of integrated care<br />
pathways (ICPs) which not only guide clinical<br />
management, but also support systematic on-going<br />
data collection to evaluate the success of our interventions.<br />
As a first step we have focused on the<br />
development and evaluation of tools for the<br />
assessment of symptoms in patients with cognitive /<br />
communication problems who have difficulty with<br />
reporting their symptoms through the normal methods.<br />
In this period, the ICPs have provided the following:<br />
The results from phase I led to modification of BIS and in<br />
Phase II (exploratory trial phase) we are conducting a<br />
13
ICP for assessment and management<br />
of hemiplegic shoulder pain:<br />
• The ShoulderQ, which we have developed to assess<br />
shoulder pain in this context, was shown to provide a<br />
specific and sensitive assessment of response to<br />
treatment 252 .<br />
• The Scale of Pain Intensity (SPIN) was developed as<br />
a simple and accessible tool for assessing pain in<br />
people who are unable to complete the ShoulderQ.<br />
Preliminary evaluation suggests that it has potential<br />
for use in this context, and further evaluation is now<br />
underway 234 . (see In Focus 2.2)<br />
ICP for assessment and management of<br />
depression:<br />
• National clinical guidelines on the assessment and<br />
management of depression in patients following<br />
stroke and acquired brain injury have been modelled<br />
on the ICP 189 .<br />
ICP for the management of spasticity<br />
• Our on-going evaluation of the functional benefits of<br />
botulinum toxin in the management of spasticity was<br />
a significant factor in the successful achievement of<br />
a UK licence for its use in the management of upper<br />
limb spasticity 5 .<br />
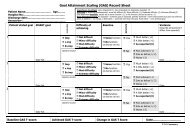
• Our first successful use of goal attainment scaling<br />
(GAS) to measure meaningful change in this context<br />
is now being taken up in other studies 209 .<br />
• The Depression Intensity Scale Circles (DISCs) is an<br />
equivalent scale to the SPIN. Evaluation using the ICP<br />
showed it to provide a valid and reliable assessment<br />
of depression in the context of brain injury<br />
(see In Focus) 164 .<br />
In focus 2.2<br />
Assessment Of Pain & Depression<br />
Assessing symptoms in people with cognitive<br />
and communication problems:<br />
A novel approach to a difficult problem<br />
Assessing symptoms is essential for the successful<br />
management of medical conditions. However, people<br />
with cognitive or communication problems, for example<br />
due to acquired brain injury, confusion or other severe<br />
illness, may have difficulty in using traditional measures.<br />
As visual cues may help communication, we have<br />
developed and evaluated a pictorial measure that can<br />
help patients report on their symptoms.<br />
This work has been carried out in the context of<br />
developing Integrated Care Pathways (ICPs) for the<br />
management of depression and pain respectively, in<br />
which regular symptom assessment plays an integral part.<br />
The Depression Intensity Scale Circles (DISCs)<br />
The concept of increasing depression is represented by<br />
a sequence of five dark grey circles increasing in size.<br />
The mode of administration is adapted to suit the<br />
individual’s cognitive and communicative abilities. Their<br />
ability to make reliable ‘yes/no’ responses is established<br />
using a screening questionnaire, the AbilityQ, and is<br />
followed by a verbal explanation of the scale reinforced<br />
by gesture or pictures as appropriate.<br />
The DISCs has been shown to have acceptable<br />
convergent validity, reliability and responsiveness as a<br />
simple graded tool for the screening and assessment of<br />
depression in patients with complex disabilities following<br />
acquired brain injury and is now one of the<br />
recommended tools for assessing depression in the<br />
Royal <strong>College</strong> of Physicians guidelines for depression<br />
following brain injury 164 .<br />
The Scale of Pain Intensity (SPIN)<br />
The SPIN uses the same idea as the DISCs, except that<br />
the circles are coloured red to convey the concept of<br />
pain. To reinforce its meaning, the colour red is also<br />
used on separate body drawings to indicate the region<br />
of the body where pain may be a problem.<br />
A preliminary study to validate<br />
the SPIN in a general<br />
population with pain has<br />
found that it could quantify<br />
pain as well as the current<br />
preferred tool, a 0-10 numeric<br />
rating scale. Subsequent<br />
observation of verbal and<br />
non-verbal interaction<br />
between speech and<br />
language therapists and<br />
patients with severe<br />
dysphasia, together with the<br />
experience of clinicians in<br />
using the SPIN, has informed<br />
its administration 280;234 . This<br />
tool is now an integral part of<br />
the multidisciplinary ICP for<br />
managing shoulder pain in<br />
stroke patients in daily use on<br />
our regional rehabilitation unit.<br />
Figure 2.7 The Depression<br />
Intensity Scale Circles (DISCs)<br />
Most severe<br />
Depression<br />
No Depression<br />
14<br />
14
2.3<br />
Measuring Outcomes<br />
Palliative care and rehabilitation are relatively new fields,<br />
and evaluations have been weakened by inappropriate<br />
or insensitive measures of benefit, such as the outcome<br />
of care and quality of life. To evaluate or set standards of<br />
care, or to assess need, we need appropriate tools to<br />
measure quality of life, outcomes and evidence about<br />
the most cost-effective models.<br />
The department has led the development of measures in<br />
palliative care, principally: the Palliative Outcome Scale<br />
(POS) and the earlier Support Team Assessment<br />
Schedule (STAS), with a programme building on 20 years<br />
experience in outcome measurement and assessment.<br />
Outcome measurement is also important in rehabilitation.<br />
Since 1995, Professor Turner-Stokes has<br />
spearheaded a drive to develop common language<br />
outcome measurement for brain injury rehabilitation in<br />
the UK. A common strand for much of the recent work is<br />
the development of outcome measures with which to<br />
assess the effectiveness of rehabilitation interventions,<br />
and exploration of the relationship between different<br />
measures in current use in the UK.<br />
2.3.1 Patient Centred Palliative Outcome Scales<br />
Support Team Assessment Schedule (STAS)<br />
The Support Team Assessment Schedule (STAS) was<br />
developed by Higginson when based at University<br />
<strong>College</strong> <strong>London</strong>. The psychometric testing was presented<br />
in her PhD thesis. It is a unique tool that assesses the<br />
clinical outcomes and intermediate outcomes of palliative<br />
care. Before STAS was developed there was no standard<br />
reliable, valid and responsive measure to assess palliative<br />
care: most existing measures had floor effects and did not<br />
reflect palliative care goals. STAS can be used in studies<br />
to compare palliative care services or in clinical audit. It<br />
has nine core or up to 20 optional items covering physical,<br />
psychosocial, spiritual, communication, planning, family<br />
concerns and service aspects. Although POS has<br />
replaced some aspects of STAS, there are elements of the<br />
original STAS, e.g. communication, insight, and professional<br />
education, which remain solely part of STAS. It is<br />
still used in many studies. This results in many services<br />
continuing to use STAS, with over 118 users in 17<br />
countries. Further details are in Clinical Audit in Palliative<br />
Care (ed. Higginson I) published by Radcliffe Medical<br />
Press. You can download a copy of STAS from the<br />
Questionnaires & tools section of www.kcl.ac.uk/palliative.<br />
Palliative Outcome Scale (POS)<br />
The POS was devised following a systematic review of<br />
outcome measures used in palliative care. This<br />
concluded that there was a paucity of clinical questionnaires<br />
that could adequately reflect the holistic nature of<br />
palliative care (Hearn and Higginson, Pall Med<br />
1997;11:71-72). The POS was, therefore, designed to<br />
overcome some of the limitations associated with<br />
existing outcome measurement scales in palliative care.<br />
It evolved using a literature review of measures, work by<br />
a multi-professional project group with individuals who<br />
worked in different palliative care settings and a patient<br />
representative. The POS was then piloted in hospice,<br />
Total Registered (so far) 457<br />
Europe<br />
UK 288<br />
Italy 5<br />
Czech Republic 2<br />
Portugal 2<br />
Switzerland 2<br />
Spain 2<br />
Greece 1<br />
France 1<br />
Poland 2<br />
Sweden 2<br />
North America<br />
USA 91<br />
Canada 15<br />
Mexico 1<br />
Rest of the World<br />
Australia 8<br />
South Africa 6<br />
New Zealand 4<br />
Argentina 3<br />
Brazil 3<br />
Peoples Republic of China 3<br />
Singapore 2<br />
Hong Kong 2<br />
Taiwan 1<br />
Thailand 1<br />
Puerto Rico 1<br />
Malawi 1<br />
Botswana 1<br />
Republic of Korea 1<br />
Uganda 1<br />
Japan 1<br />
Nigeria 1<br />
Independent Validations/Translations of POS<br />
UK – Stevens et al, Support Cancer Care 2005;13:1027-34<br />
Italian<br />
German – Bausewein et al JPSM 2005;30:51-62<br />
Urdu<br />
Spanish – Serra-Prat et al Med Clin (Barc) <strong>2004</strong>;123:406-12<br />
Portuguese<br />
Table 2.2 Palliative Care Outcome Scale (POS)<br />
home, hospital and other community settings. The<br />
questionnaire covers physical symptoms, psychological<br />
symptoms, spiritual considerations, practical concerns,<br />
emotional concerns and psychosocial needs.<br />
Importantly, it also has an open question so<br />
respondents can identify their most important concern.<br />
There are two main versions of the POS questionnaire,<br />
one for patients to complete, the other for staff. Bringing<br />
together these two complementary perspectives allows<br />
15
the POS to identify patient's problems and enables staff<br />
to provide individualised care. It is a flexible tool, the<br />
usage of which can be determined by the needs of local<br />
services. A version completed by the family/caregiver<br />
has also been developed.<br />
The POS showed acceptable validity when used in a<br />
variety of settings, such as home care, hospice inpatient<br />
and day care, and hospital inpatient care, as well as<br />
outpatient and community services. It has also been<br />
shown to be a credible, clinical, research and audit tool,<br />
which is acceptable to both patients and staff and quick<br />
(five minutes) to complete (Hearn and Higginson Quality<br />
in Healthcare 1999;8:219-277). The POS can be used<br />
routinely to guide clinical practice and monitor service<br />
interventions. Moreover, the POS is a valuable audit tool<br />
that can help meet the current statutory requirements on<br />
clinical governance. You can download free copies of<br />
the POS questionnaires from the Questionnaires & tools<br />
section of our website (www.kcl.ac.uk/palliative). A<br />
user's guide to the POS with further details on the<br />
origins of the POS, as well as suggestions for its<br />
implementation in clinical practice and analysis of data<br />
is also available. Table 2.2 shows details of current users<br />
of POS, and external validations which independently<br />
confirm the value of POS assessment and<br />
measurement. A next step with the POS is to test: its<br />
utility in identifying patients who would benefit from<br />
referral to palliative care and potential to assess<br />
complexity and costs using a similar approach to<br />
rehabilitation measures (see 2.3.3); culturally appropriate<br />
formats; and additional modules assessing symptoms or<br />
other aspects in more detail.<br />
Comparison of quality of life scales in<br />
palliative care<br />
Using data collected on 140 patients to evaluate<br />
palliative day care we further explored the factors within<br />
the Palliative Outcome Scale (POS) and other measures<br />
of hope and quality of life. Using these different tools, we<br />
were able to identify a relative factorial structure of all<br />
scales combined. Four components appeared to be<br />
reflected in the different measures – self sufficiency,<br />
positivity, symptoms and spiritual needs. The results<br />
suggest ways in which items within the POS might be<br />
further improved, and suggests that the POS could form<br />
the basis of a measure in the future containing 11 (rather<br />
than 10) items which would explain the variability of<br />
needs within patients and might be useful for identifying<br />
individuals for referral to palliative care 16 .<br />
The German translation of POS<br />
The German version of the POS was translated forward<br />
and backward according to EORTC recommendations<br />
for translation procedures and then validated in palliative<br />
care (hospital support team, hospice, home care) and a<br />
pain clinic. The German POS version was well accepted<br />
by patients and staff, and appears to be valid. The study<br />
identified some areas where the scale would benefit<br />
from expansion to more closely capture staff and patient<br />
concerns 132 .<br />
The APCA African POS<br />
This collaboration between the African Palliative Care<br />
Association (APCA), KCL and National Hospice and<br />
Palliative Care Organisation (NHPCO) (USA), along with<br />
partner agencies in 11 sites across South Africa, has<br />
developed and begun the validation of an African<br />
Palliative Outcome Scale (POS) for use across the<br />
region. This important collaboration will enable future<br />
evaluative efforts to be conducted using a valid outcome<br />
tool, something missing to date. Work is currently<br />
underway to develop an African POS for children.<br />
Funded by the BIG Lottery in the UK, The Encompass<br />
Project (Ensuring Core Outcomes and Measuring<br />
Palliation in Sub-Saharan Africa) unites five sites across<br />
ENCOMPASS<br />
Ensuring Core Outcomes and Measuring<br />
Palliation in Sub-Saharan Africa<br />
South Africa and Uganda: The Hospice Association of<br />
the Western Cape, Philanjalo Hospice in Tugela Ferry,<br />
South Coast Hospice, The N’Doro project at Chris Hani<br />
Baragwanath Hospital in SOWETO, and Hospice Africa<br />
Uganda. The project aims to complete validation of the<br />
African APCA POS and to work with the partners above<br />
to act as “model” audit centres, conducting a full audit<br />
cycle during the second year. This project has achieved<br />
a number of successes: the recruitment and training of a<br />
cadre of African palliative care nurses; the generation of<br />
a large original dataset; and has laid the foundation for<br />
audit in these new services. Harding, Selman and<br />
Higginson are now planning the analysis of the data, so<br />
it can be fed back to services, and the utility of this new<br />
version of POS can be tested.<br />
2.3.2 Common Language Outcome Measures<br />
for Rehabilitation in the UK<br />
In the last triennial report we described the tools we<br />
have developed to measure outcomes from rehabilitation<br />
and provide a common language with which to<br />
compare different populations, programmes and<br />
practices. These include the Northwick Park<br />
Dependency and Care needs assessment (NPDS/<br />
NPCNA) and the UK Functional Assessment Measure<br />
(UK FIM+FAM). A recent survey has demonstrated that<br />
these are now widely taken up and used in clinical<br />
practice in rehab units across the UK 248 .<br />
The NPDA/NPCNA provides a generic measure of care<br />
needs in the community and thus the cost of continuing<br />
care provided by health and social services. Work is<br />
ongoing to develop hospital versions of these scales (the<br />
NPDS-H and NPRNA) which could ultimately be used to<br />
determine the nursing staff required for a rehabilitation<br />
16
ENCOMPASS partners – palliative care research nurses in Sub-Saharan Africa<br />
ward, adjusted in relation to case-mix 363;364 ; and also to<br />
develop an equivalent scale for assessment of needs for<br />
therapy input – the Northwick Park Therapy Dependency<br />
Assessment (NPTDA) 276 .<br />
In her capacity as national lead for the development<br />
of Healthcare Resource Groups for Rehabilitation,<br />
Professor Turner-Stokes is currently working in<br />
collaboration with the Department of Health through<br />
The Information Centre, Connecting for Health and<br />
the Payment by Results Team to develop suitable<br />
tools for banding cost tariffs for rehabilitation when<br />
Payment by Results is introduced for rehabilitation<br />
services.<br />
The NPDS and NPTDA have been put forward as the<br />
tools likely to be used for costing rehabilitation<br />
inputs for patients with complex rehabilitation needs.<br />
A much simpler tool, the Rehabilitation Complexity<br />
Scale (RCS) has been developed for use at the less<br />
specialised end of the service spectrum.<br />
See figure 2.8.<br />
Measuring function outcome from focal interventions<br />
such as the use of botulinum toxin for<br />
upper limb spasticity<br />
Intramuscular injection of botulinum toxin is increasingly<br />
recognised as a safe and effective intervention for<br />
reducing spasticity in the arm and hand due to stroke or<br />
other brain injury. However, whilst there is good<br />
evidence for its effect on muscle tone, it is harder to<br />
demonstrate that this translates into actual benefit for<br />
patients. Focal changes that arise form the localised<br />
injection of one or two muscles may be lost against a<br />
background of unchanging items in the commonly used<br />
disability measures.<br />
Pooling data on stroke patients in two randomised<br />
controlled trials of intra-muscular botulinum toxin (BTX),<br />
Wade, Turner-Stokes and colleagues showed that it was<br />
possible to demonstrate a relationship between changes in<br />
spasticity and functional gain. However, functional benefits<br />
were often not observed until 6-8 weeks after relieving<br />
spasticity, due to the time needed to practice functional<br />
skills. These functional gains may therefore be missed in<br />
trials which use a single time-point for assessment of<br />
outcome based on maximal effect on spasticity 5 .<br />
A second reason for failure to demonstrate functional<br />
gain is because measurement tools evaluate the wrong<br />
(NPDS = Northwick Park nursing Dependency Scale, NPTDA = Northwick Park Therapy Dependency Assessment; RCS = Rehabilitation Complexity Scale)<br />
Complexity of need<br />
Costing tools<br />
NPDS<br />
NPTDA<br />
RCS<br />
Complex Specialised<br />
Rehabilitation (CSR) –<br />
tertiary services<br />
}<br />
District Specialised<br />
Rehabilitation (DSR)<br />
Areas covered<br />
by proposed<br />
HRGS<br />
Local General<br />
Rehabilitation (LGR)<br />
Patients requiring rehabilitation<br />
Figure 2.8 Current proposals for use of costing tools to develop banded cost tariffs for rehabilitation services under payment by results:<br />
Source: Turner-Stokes et al, Clinical Medicine, <strong>2007</strong>, in press<br />
17
tasks. Some patients, especially early in the recovery<br />
phase, may expect to regain voluntary control of their<br />
arm and hand following relief of spasticity, but for more<br />
severe and longer-standing paralysis, the goals for<br />
intervention tend to be ‘passive function’ such as<br />
improving the ease of caring for the person – for<br />
example making it easier to maintain hygiene or to put<br />
the arm through a sleeve while dressing. A systematic<br />
review of the literature revealed no suitable tools<br />
currently available for measuring both passive and active<br />
functions of the upper limb that would properly assess<br />
the functional benefits of managing upper limb<br />
spasticity, so we have developed a new tool called the<br />
ArMA, which is now undergoing evaluation.<br />
Patient-centred outcomes in rehabilitation - the<br />
use of Goal Attainment Scaling (GAS)<br />
Goal attainment scaling (GAS) was first introduced in the<br />
1960s as a tool for evaluating individualised outcomes in<br />
complex interventions in patients with learning disabilities,<br />
but it has only relatively recently gained popularity<br />
outside in other fields. One of the major challenges for<br />
outcome measurement in rehabilitation is the wide<br />
variety of different goals that patients may have for their<br />
rehabilitation programme. GAS absorbs much of this<br />
variation within the process of goal setting, making it a<br />
potentially valuable tool for this context. Moreover, a<br />
patient-centred instrument that specifically evaluates the<br />
outcomes that are important to the patient and their<br />
family provides an important perspective that is not<br />
included in most standardised measures of outcome.<br />
In our preliminary application of GAS as a measure for<br />
assessing focal changes during the management of<br />
upper limb spasticity (see above) Ashford and Turner-<br />
Stokes found that GAS provided a useful measure of<br />
functional gains in response to treatment, and was more<br />
sensitive than global measures such as the Barthel<br />
Index 208 . Further work is underway to address the<br />
benefits of GAS over currently applied standardised<br />
outcome measures in our wider rehabilitation<br />
programme.<br />
18
2.4<br />
Living & Dying<br />
in Society<br />
2.4.1 A Good Death at Home: Committed<br />
to Making it an Achievable Goal<br />
Most people in many countries of the world do not die<br />
where they wish. The latest data for England & Wales<br />
shows that nearly 300,000 people died in NHS hospitals<br />
and less than 94,000 at home. This project, now funded<br />
by <strong>Cicely</strong> <strong>Saunders</strong> International, aims to improve the<br />
evidence base on how best to support patients and<br />
families to achieve a good death at home if they wish.<br />
Over the last 12 years, Higginson inaugurated a series of<br />
studies scrutinising variations in place of death, the<br />
preferences of patients, families and general public, the<br />
effect of services and the reality for specific groups of<br />
people (e.g. children and young people, the elderly).<br />
Through international collaborations including with the<br />
US, Italy and Ireland, our team investigated differences<br />
and commonalities across countries. We found, for<br />
example, that death demographics and the place where<br />
people die are similar in <strong>London</strong> and New York 220 . In<br />
<strong>London</strong>, however, older people are much less likely to<br />
die at home, whereas in New York they die at home<br />
more often than their younger counterparts.<br />
Percent of Cancer Deaths at Home Ages 40+, 1995-1998<br />
.3%<br />
<strong>London</strong><br />
New York City<br />
.25<br />
.2%<br />
.15<br />
.1%<br />
.05<br />
0%<br />
40 42 44 46 480<br />
50 52 54 56 58 60 62 64 66 68 70 72 74 76 78 80 82 84 86 88 90 92 94<br />
Age<br />
Figure 2.9 Proportions of cancer deaths at home, 1995-1998 by age in <strong>London</strong> and New York<br />
Source: Higginson and Decker, 2006, European Journal of Public Health 2006:doi:10.1093/eurpub/ckl243<br />
Factors related to illness<br />
Individual factors<br />
Environmental factors<br />
Non–solid tumours<br />
Long length of disease<br />
Low functional status<br />
HOSPITAL<br />
HOME<br />
HOME<br />
Demographic variables<br />
Good social conditions<br />
Ethnic minorities<br />
Personal variables<br />
Patient’s preferences<br />
HOME<br />
HOSPITAL<br />
HOME<br />
Healthcare input<br />
Use of home care<br />
HOME<br />
Intensity of home care HOME<br />
Availability of inpatient beds HOSPITAL<br />
Previous admission to hospital HOSPITAL<br />
Rural environment<br />
HOME<br />
Areas with greater hospital<br />
provision<br />
HOSPITAL<br />
Social support<br />
Living with relatives<br />
Extended family support<br />
Being married<br />
Caregiver’s preferences<br />
HOME<br />
HOME<br />
HOME<br />
HOME<br />
Place of death<br />
Macrosocial factors<br />
Historical trends<br />
HOME<br />
Figure 2.10 Model of variations in place of death<br />
Source: Gomes and Higginson, BMJ, 2006, 332:515-521<br />
19
In the attempt to find out what needs to be in place for<br />
patients to die at home, Gomes and Higginson analysed<br />
58 studies, involving 1.5 million patients in 13 countries.<br />
They identified strong evidence for the effect of a<br />
complicated network of 17 factors associated with death<br />
at home 226 . The findings, depicted in an evidence-based<br />
model (figure 2.10), were welcomed by many policy<br />
makers and professionals committed to planning and<br />
providing care that meets patients’ wishes.<br />
The team has taken this research further to understand<br />
and monitor changes in where people die over time. We<br />
unveiled a longstanding dying trend away from home in<br />
England & Wales from 1974 to 2003, that has sustained<br />
for cancer and non-cancer, both genders and all people<br />
aged 45 and over. Concerned by the implications of a<br />
continuation of this trend into the future, a series of<br />
national long-term projections are being prepared<br />
accounting for different scenarios. The data from this<br />
study will be of great value to plan for future palliative<br />
care. Gomes and Higginson then plan to research ways<br />
to improve the quality of palliative care at home to<br />
discover more cost-effective models of home care so<br />
that more people feel supported and can benefit from it.<br />
Figure 2.11 Distribution of ABI carer participants<br />
within UK Strategic Health Authorities<br />
Numbers of carers<br />
10<br />
5<br />
1<br />
2.4.2 Carer Experiences in Long-term Neurological<br />
Conditions<br />
The health and happiness of family carers who look after<br />
people with long-term neurological conditions can be<br />
put at risk because many of those cared for have<br />
multiple problems affecting their functioning in all<br />
aspects of daily life and need round-the-clock care.<br />
The Government’s National Service Framework (NSF) for<br />
Long-Term Conditions (2005) set out specific initiatives<br />
to transform the way that health and social care services<br />
support these family carers. To inform its implementation,<br />
Jackson and Turner-Stokes have conducted a<br />
Department of Health funded programme of research<br />
into carer experiences in neurological conditions.<br />
In collaboration with researchers from the Social Policy<br />
Research Unit at York University, the <strong>Institute</strong> of<br />
Psychiatry and voluntary organisations, they completed<br />
a national survey of the needs and experiences of carers<br />
of adults with acquired brain injury (ABI) (figure 2.11).<br />
This comprised:<br />
• Systematic literature reviews of the sociological,<br />
medical and psychological literature.<br />
• A national questionnaire study, which compared and<br />
contrasted the experiences of carers looking after a<br />
relative of working age with ABI against a group of<br />
carers of people with dementia studied previously.<br />
Results showed that high levels of burden, a diminished<br />
quality-of-life and poor health were common in both<br />
carer groups (figure 2.12). ABI carers fared worse than<br />
dementia carers, probably because more of them lived<br />
with the person cared for and because they spent more<br />
hours caring per week.<br />
Figure 2.12 WHOQoL-BREF quality of life scores compared for ABI carers, dementia carers and a normative sample<br />
100<br />
90<br />
80<br />
Mean Quality of Life Scores<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Physical Psycological Social Environmental<br />
ABI carers (n+222) Dementia carers (n=132) Normative sample (n=396)<br />
20
The problem behaviours shown by the person cared for<br />
had different effects on carer well-being. Looking after<br />
someone with aggressive problems was more of an<br />
issue for ABI carers, whereas passive/low mood<br />
problems caused more difficulty for dementia carers.<br />
Having to cope with a relative displaying violent/<br />
aggressive behaviour was of particular concern for<br />
carers with young children or other dependent relatives.<br />
As one mother told us…<br />
“Constantly tired, haven’t got any available time to play<br />
or do things with the children. Our relationship as<br />
husband and wife has suffered because he cannot<br />
understand there are others in the house and he can’t<br />
have everything done immediately and starts screaming<br />
and yelling at me and the children which is getting us all<br />
down. Because of memory problems I have to do<br />
everything over and over again. I can’t leave the children<br />
with him and can’t leave him either.”<br />
Support for carers with multiple caring roles<br />
in the context of long-term neurological<br />
conditions<br />
As a result of this work, a further Department of Health<br />
grant has been awarded for a follow-on study to<br />
investigate the experiences of carers according to their<br />
differential family circumstances, and the conditionspecific<br />
problems they have to cope with, in a range of<br />
other long-term neurological conditions. The aims of this<br />
study are to:<br />
• Investigate the support needs of people caring for an<br />
adult with a long-term neurological condition,<br />
especially those with other family dependents<br />
(i.e. with multiple caring roles).<br />
• Identify differences in support needs between caring<br />
for people with ‘hidden’ (cognitive, behavioural,<br />
emotional) versus ‘visible’ (physical) disabilities.<br />
• Investigate carers’ changing needs during the first 1-2<br />
years after onset.<br />
• Estimate costs and identify predictors of both current<br />
informal care & support and potential support.<br />
Findings will inform a good practice guide, which will be<br />
disseminated through major service providers in the<br />
NHS and voluntary sector to assist in the planning of<br />
appropriate support services for these carers, and to<br />
evaluate the cost implications of service provision.<br />
2.4.3 Ethnicity and Culture<br />
One question raised about patients common preference<br />
for home care and home death, is whether this varies by<br />
culture. We explored this as part of a wider study<br />
assessing the effects of advanced disease, particularly<br />
cancer, among the local black Caribbean and white<br />
populations. Bereaved relatives reported that 34% of<br />
black Caribbean patients and 27% of white patients had<br />
expressed a firm preference for location of death, and of<br />
these in both groups more than 80% wanted to die at<br />
home. Thus, at least in this group, home preference was<br />
similar. However, fewer respondents representing<br />
Caribbeans rather than white patients stated that they<br />
(x 2 = 8.9, p= 0.01) nor the patients (x 2 = 8.6, p = 0.03)<br />
where given sufficient choice about the actual location<br />
of death, suggesting that further training and support is<br />
needed to elicit the preferences of, and to meet the<br />
needs of, the local Caribbean community 25 .<br />
Further exploration of the experiences of the family<br />
members also showed higher psychological morbidity<br />
among the Caribbean individuals, highlighting an urgent<br />
need for better focused support in primary care. The<br />
comparison of the bereavement effects on family and<br />
close friends of 50 deceased first generation black<br />
Caribbean and 50 native born white patients, using<br />
standardised scales, found that although there were no<br />
differences in the intensity of grief; depression and<br />
anxiety; was significantly higher among black Caribbean<br />
respondents (28 vs 21.2, T test = -2.28, p = 0.025).<br />
Multiple regression analysis revealed that this difference<br />
was best accounted for by the ethnicity of the deceased<br />
(OR 7.0, CI 0.08-13.14, p=0.03) and bereavement<br />
concerns such as legal and housing problems (OR 5.0,<br />
CI 0.07-9.37, p=0.02). The majority of respondents had<br />
visited their General Practitioner subsequent to<br />
bereavement suggesting this as a possible means of<br />
support 156 .<br />
Work in this area is progressing through a qualitative<br />
study exploring and comparing the experience of living<br />
with and dying from advanced cancer among the black<br />
Caribbean and white British communities living in south<br />
east <strong>London</strong> supported by the Guy’s and St Thomas’<br />
Charity. The study is exploring differences in the<br />
meaning of symptoms and mechanisms of support, in<br />
order that this information can be used to improve future<br />
treatment and care.<br />
2.4.4 Better Palliative Care for Older People<br />
The fastest growing section of the population is the<br />
“oldest old” and this trend is forecast to continue, but<br />
little research to date has focused on the needs,<br />
attitudes or the experience of this group. As preventive<br />
healthcare reduces disease-related death at a younger<br />
age, more people can expect to die eventually in old<br />
age, but data are scarce on the patterns of decline due<br />
to age-related causes of death. Disability, frailty and<br />
dementia are all increasingly common in advanced old<br />
age, and there is evidence of steeper cognitive decline<br />
preceding death.<br />
Although many of the studies reported elsewhere<br />
include partially, or often primarily older people (for<br />
example, research into renal palliative care 2.2.2), we<br />
have launched a specific programme seeking to improve<br />
palliative care for older people, supported by the Dunhill<br />
Medical Trust and <strong>Cicely</strong> <strong>Saunders</strong> International. Within<br />
this, three main sub-programmes have been developed:<br />
I. Supporting dignity at the end of life<br />
A systematic review of older peoples’ perceptions of<br />
dignity and interventions to support their dignity and a<br />
qualitative study to explore residents’ perceptions of<br />
dignity are underway. Pilot studies to assess the<br />
feasibility, acceptability effectiveness of a novel<br />
dignity therapy intervention for older people at the<br />
end-of-life are planned in collaboration with Professor<br />
Harvey Chochinov, Canada, who pioneered this<br />
approach. These will be conducted in two settings:<br />
care homes and hospital (people being seen by a<br />
hospital-based palliative care team).<br />
II. The effectiveness of interventions to improve<br />
palliative care for older people<br />
This includes (a) a systematic review to assess the<br />
21
effectiveness of palliative care interventions for older<br />
people in care homes, and (b) producing a booklet for<br />
the WHO on better practice in palliative care for older<br />
people, with additional support from the international<br />
charity, Fondazione Maruzza Lefebvre D’Ovidio<br />
Onlus.<br />
III. Exploring the barriers to implementing the Gold<br />
Standards Framework for Care Homes<br />
The Gold Standards Framework for Care Homes is<br />
one of the UK's national tools to improve end-of-life<br />
care, which has been developed and recognised<br />
nationally through the Department of Health’s End of<br />
Life Care Programme. Interviews with care home<br />
managers, nursing staff, care assistants, residents<br />
and their families are planned, in research supported<br />
by the Guy’s and St Thomas’s Charity.<br />
Dr Sue Hall (Lecturer) and Susan Longhurst (Research<br />
Associate) have been supported to work with Irene<br />
Higginson on the programme.<br />
In addition, Dr Morag Farquhar is providing a link and<br />
collaboration to the study on living and dying in extreme<br />
old age. This qualitative and quantitative study, from the<br />
Department of Public Health and Primary Care,<br />
University of Cambridge, and supported by the BUPA<br />
Foundation, aims to gain a fuller understanding of what<br />
it means to live so long and die so old.<br />
The long-running study of ageing, the Cambridge City<br />
over-75s Cohort, provides a unique opportunity to<br />
explore these issues by re-interviewing the survivors<br />
(now all aged 94-100), their family and other carers. The<br />
research takes account of personal experiences,<br />
attitudes and preferences using qualitative methods,<br />
and quantifies patterns of health, cognition, social<br />
networks and service support at the end of life, building<br />
on 20 years’ quantitative data.<br />
This BUPA Foundation funded study consists of three<br />
linked projects to examine living and dying in extreme<br />
old age within the framework of an on-going longitudinal<br />
observational study, the Cambridge City over-75s<br />
Cohort (baseline n=2609). King’s <strong>College</strong> <strong>London</strong> is a<br />
co-applicant on this phase of the study, providing<br />
expertise in qualitative methods, interviewing older<br />
people and quality of life measurement.<br />
22
3<br />
Policy, Guidelines and<br />
Needs Assessments<br />
The work of the department has had a considerable<br />
impact on policy, through the National <strong>Institute</strong> of<br />
Clinical Excellence (NICE) Guidance on Supportive and<br />
Palliative Care in Cancer, and through its general<br />
research being adopted in policy documents. In<br />
addition, work was undertaken by Turner-Stokes and<br />
colleagues on the National Service Framework for Long<br />
Term Neurological conditions. Many of the members of<br />
the department are members of local, national and<br />
international strategic groups, further aiding the<br />
development of the fields (see section 7).<br />
As Deputy Chair of the External Reference Group and as<br />
Chair of the Research and Evidence group, Professor<br />
Turner-Stokes played a key role in its development.<br />
Gathering the evidence to underpin the NSF recommendations<br />
was a major undertaking. As part of this, the<br />
group developed a new research typology that is quick<br />
and simple enough to be used by clinicians;<br />
encompasses both qualitative and quantitative research,<br />
providing it is rigorously conducted; and values the<br />
experience of users and carers who live with long term<br />
neurological conditions as well as research-based<br />
evidence 285 . Application of this typology allows different<br />
conclusions to be drawn from the literature than the much<br />
more restrictive approach of the Cochrane Review<br />
methodology, which may resonate more closely with the<br />
experience of users, carers and professionals in the field.<br />
3.1 Guidelines<br />
Professor Turner-Stokes chairs the Research and<br />
Clinical Standards Committee for the British Society of<br />
Rehabilitation Medicine and is also editor of the Concise<br />
Guidance series for the Royal <strong>College</strong> of Physicians.<br />
As part of this, guidelines have been produced in the<br />
following areas:<br />
3.2.1 Epidemiological Based Needs Assessment<br />
For the Open Society <strong>Institute</strong> we have conducted a<br />
global needs review collating all the data on all the<br />
different approaches to needs assessment which have<br />
been conducted across the globe, and are in the<br />
process of analysing this 326 .<br />
In addition, for a local hospice Longhurst, Shipman and<br />
Higginson conducted a needs review to assess how the<br />
local community and hospice would like to see that<br />
hospice develop in response to local need and available<br />
resources. This involved collating epidemiological data,<br />
interviewing relevant stakeholders, including patients,<br />
local doctors and nurses, the primary care trusts and,<br />
of course, hospice staff.<br />
3.2.2 Individual Based Needs Assessments<br />
Many of the measures described in section 2.2 are being<br />
used to assess needs. For example, many services<br />
across the globe are using POS to assess patient needs<br />
and to aid communication between staff. The Ministry of<br />
Health in Portugal has recommended it for all services,<br />
and in the UK it is proposed in End-of-Life and Palliative<br />
Care Guidance. In addition, Williams and Turner-Stokes<br />
have been developing the Northwick Park Nursing<br />
Dependency Care Needs Assessment (NPDS/NPCNA).<br />
While this assessment was designed to work in the<br />
community a preliminary evaluation of care hours<br />
demonstrated that the NPCNA over-estimated the time<br />
required to deliver nursing care in hospital when it was<br />
compared with the total nursing and care hours<br />
available. In addition, it failed to identify specialised<br />
interventions in a rehabilitation setting. The work will<br />
lead us to seek ways to improve and find the<br />
assessment tool for the future.<br />
• Vocational assessment and rehabilitation following<br />
acquired brain injury 73 ;<br />
• Rehabilitation following acquired brain injury 85 ;<br />
• Assessment and management of the use of<br />
anti-depressants following acquired brain injury 189 ;<br />
• Chronic kidney disease (Burden and Thompson,<br />
Clinical Medicine 2005;5:635-642);<br />
• Management of delirium in older people (George et al,<br />
Royal <strong>College</strong> of Physicians 2005 <strong>London</strong>).<br />
In addition, Cochrane reviews have been undertaken<br />
and the methodology developed (see In Focus 3.1).<br />
3.2 Needs Assessments<br />
The department is active in both epidemiologically/<br />
population based needs assessments to improve care<br />
for the community and also individual patient needs<br />
assessments, adapting many of its existing measures.<br />
23
In focus 3.1 –<br />
Cochrane Reviews<br />
The Cochrane library was set up in the 1980s to provide<br />
a database of randomised controlled clinical trial<br />
evidence which is regularly reviewed and updated.<br />
Whilst RCTs may not always be possible, or even<br />
appropriate, to answer all the questions that need to be<br />
answered, Cochrane reviews form an important contribution<br />
of the literature.<br />
In rehabilitation, the major part of our Cochrane<br />
programme has been undertaken in collaboration with<br />
colleagues in Melbourne, Australia – Dr Fary Khan and<br />
Professor Peter Disler, who is an honorary Visiting<br />
Professor within our department. During this three-year<br />
period we have completed four Cochrane systematic<br />
reviews:<br />
• Exercise for peripheral neuropathy 35<br />
• Multi-disciplinary rehabilitation for acquired brain<br />
injury in adults of working age 165 .<br />
• Multidisciplinary rehabilitation for adults with<br />
multiple sclerosis 327 .<br />
• Rehabilitation interventions for footdrop in<br />
neuromuscular disease 336 .<br />
The two reviews of multidisciplinary rehabilitation for<br />
Acquired Brain Injury (ABI) and for MS were large<br />
systematic reviews incorporating 14 and eight trials<br />
respectively. Pooling of data for meta-analysis was<br />
prohibited by heterogeneity in the trial methods, but<br />
both reviews used a novel ‘synthesis of best evidence’ to<br />
assimilate the trial findings.<br />
• The ABI review provided strong evidence that patients<br />
with moderate to severe brain injuries recover faster<br />
with more intensive rehabilitation programmes, and<br />
that continued out-patient rehabilitation can help to<br />
maintain these gains.<br />
• The MS review also showed strong evidence that<br />
patients with MS can benefit from an inpatient<br />
programme, and can function better, even though<br />
their underlying impairments do not change. Also that<br />
out-patient and community-based programmes can<br />
improve quality of life.<br />
Cochrane reviews are also underway to assess:<br />
• The effectiveness of non-pharmacological interventions<br />
in the management of breathlessness.<br />
• The effectiveness of antidepressants in the<br />
management of depression in physical illness<br />
(Hotopf et al).<br />
4<br />
Clinical Services<br />
There are well established clinical palliative care services<br />
at both King’s <strong>College</strong> Hospital NHS Trust (KCH, one<br />
hospital palliative care team) and at the Guy’s Foundation<br />
and St Thomas’ NHS Foundation Trust (GST, two hospital<br />
palliative care teams and two community palliative care<br />
teams). The services provide a seven day a week visiting<br />
service and consultant-delivered integrated 24-hour<br />
telephone advice across both Trusts and the University<br />
Hospital Lewisham.<br />
Two of the clinical consultants have honorary academic<br />
contracts with the Department of Palliative Care, Policy and<br />
Rehabilitation – Dr Polly Edmonds (lead clinician at KCH)<br />
and Dr Rachel Burman (KCH) and of course Professor<br />
Higginson is a consultant (honorary), primarily for KCH, but<br />
in on call integrated across all units. There are joint monthly<br />
clinical update meetings between the KCH palliative care<br />
team and academics from the Department of Palliative<br />
Care, Policy and Rehabilitation, in order to share key<br />
clinical issues, especially where they relate to policy and to<br />
update on research projects, and a joint journal club. The<br />
clinical services lead the delivery of the undergraduate<br />
curriculum – this is discussed more fully in section 5.4.<br />
4.1 Improving Care for People Affected by<br />
Multiple Sclerosis (MS): Translation of Study<br />
Outcomes to the Clinical Setting<br />
During its evaluation phase the new MS service saw 94<br />
patients, assessed by the referrer to be severely affected<br />
by their MS. Most of the people referred for assessment<br />
of symptom control problems had other specialist<br />
palliative care issues identified on assessment by the<br />
clinical service. This was less likely where referrals were<br />
made for other reasons. No patient required more than<br />
three visits by the clinical team, and only a minority of<br />
people (n=15, 16%) were subsequently referred on to<br />
community specialist palliative care services for ongoing<br />
management.<br />
Drawing on the lessons learned as part of this project,<br />
and following a detailed option appraisal, it was decided<br />
that the most realistic and sustainable option for the<br />
future was that of a step-down service leading to full<br />
integration of the MS palliative care service with the<br />
generic King’s <strong>College</strong> Hospital Palliative Care Team. In<br />
addition, a new referral pathway was developed (see<br />
figure 4.1).<br />
There are many examples where the research findings are<br />
influencing local, national and international clinical<br />
practice, but two specific local examples are given below.<br />
24
Pathway for Referral of Person Severely Affected by MS To Specialist Palliative Care<br />
Core Indicators<br />
• Recent, significant functional decline (loss of ADLs)<br />
• Dependence in ADLs or more<br />
• Multiple co–morbidities<br />
• Weight loss<br />
• Serum albumin 2<br />
• Kamofsky score 0<br />
• Severe progression of disease over recent months<br />
• Recent increase in infective episodes requiring hospitalisation<br />
Consider holistic assessment using palliative care approach having regard to<br />
• Quality of life • Comfort • Patient Choice<br />
Disease specific indicators<br />
Significant<br />
complex<br />
symptoms e.g.<br />
pain<br />
Communication<br />
difficulties e.g.<br />
Dysarthria /-<br />
fatigue<br />
Cognitive<br />
difficulties<br />
Swallowing<br />
difficulties/poor<br />
nutritional status<br />
Breathlessness<br />
/- aspiration<br />
Medical<br />
complication e.g.<br />
recurrent infection<br />
Ability to access<br />
hospital based<br />
review<br />
Difficulty<br />
verbalising choice<br />
es<br />
input from medical team, SLT, OT and dietician, physiotherapist or<br />
neuropsychiatrist as appropriate<br />
es<br />
No<br />
Suspect impaired<br />
ability to make<br />
decisions<br />
Consider PEG<br />
feeding tube<br />
Consider active management e.g.<br />
antibiotic and ventilation<br />
Refer to MDT<br />
including hospital<br />
palliative care<br />
No<br />
Patient wants active management<br />
es<br />
Refer to<br />
appropriate acute<br />
service<br />
No or not sure<br />
Home assesment<br />
for symptom<br />
control<br />
Advance directive<br />
End of life<br />
decisions<br />
and future<br />
management<br />
Symptom<br />
management<br />
and future care<br />
planning<br />
Need for end of<br />
life discussion /-<br />
preferred place<br />
of care<br />
Consider Referral to specialist Palliative Care<br />
Figure 4.1 Referral pathway arising from research and clinical collaboration<br />
Where new referrals are received by the clinical service,<br />
these are now triaged by one of the consultants in<br />
Palliative Medicine at King’s <strong>College</strong> Hospital NHS Trust,<br />
using the referral pathway based on the information<br />
available. The consultant then contacts the referrer by<br />
telephone to discuss the patient in more detail and give<br />
appropriate telephone advice with a view to:<br />
• Sign-posting patient to appropriate service(s);<br />
• If palliative care issues are identified as urgent and<br />
complex, the palliative care consultant facilitates<br />
referral to local community palliative care team (CPCT);<br />
• If it is difficult to engage the local CPCT or other<br />
professionals, the palliative care consultant could<br />
offer a joint patient assessment either with the CPCT,<br />
referrer, or other appropriate health or social care<br />
professional;<br />
• For one local area (Lambeth, Southwark and<br />
Lewisham) patients there is the option of an<br />
appointment in the neurology palliative care clinic.<br />
New patients may also be seen by the hospital palliative<br />
care team in the new complex MS patient clinic that is<br />
held monthly at King’s <strong>College</strong> Hospital NHS Trust, led<br />
by Dr Peter Brex.<br />
A further outcome from the project is the development<br />
of several resources to support people severely affected<br />
by MS, carers, health and social care professionals in<br />
learning from this project and developing local collaborations<br />
to improve care for those people with MS that<br />
are severely affected. These are:<br />
• A Resource for Health and Social Care Professionals;<br />
• MS Essentials series: Support for people severely<br />
affected by MS;<br />
• A Service Directory listing statutory and voluntary<br />
services in Southeast <strong>London</strong>; it is available as a paper<br />
version or via a website http://www.selmss.org.uk/.<br />
4.2 Improving Care for People with Chronic<br />
Heart Failure: Translation of Heart Failure Study<br />
to Clinical Setting<br />
This service development programme was designed to<br />
review current cardiology/palliative provision at Guy’s<br />
and St. Thomas’ NHS Foundation Trust for heart failure<br />
patients and to measure need for and appropriateness<br />
of a new service. Led by Beynon and Harding, and<br />
involving a multi-professional academic and clinical<br />
team, this study, which was funded by the Guy’s and St<br />
Thomas’ Charitable Foundation, aimed to identify areas<br />
of good practice and those where things worked less<br />
well. In order to do this, we undertook a census with a<br />
view to quantifying the number of inpatients likely to<br />
require palliative care, as well as conducting interviews<br />
with patients, their carers and staff in both palliative care<br />
and cardiology.<br />
The process of undertaking the research has led to an<br />
increased understanding between the clinical leaders in<br />
both cardiology and palliative care with a joint determination<br />
to implement the data to provide an improved<br />
service for patients nearing the end of their lives. Results<br />
from the project have informed the local, national and<br />
25
international debate, as well as leading to local service<br />
recommendations.<br />
The results from the project are currently being disseminated<br />
within the hospital trust but have already led to:<br />
• Agreed specific referral criteria to palliative care<br />
(see table 4.1);<br />
• A pilot parallel heart failure/palliative care<br />
outpatient service;<br />
• Discussions between ward staff and palliative<br />
care staff regarding available resources;<br />
• Review of psychological support to patients.<br />
• Review of information available to patients<br />
All cardiac patients being referred to the palliative care team must have:<br />
• been reviewed by the Heart Failure team (x81012);<br />
• know they have a diagnosis of heart failure;<br />
• both patient and medical team must agree to the referral.<br />
IN ADDITION one or more of the following merit referral:<br />
• Symptomatic (e.g. breathless at rest or on minimal exertion) despite optimal treatment;<br />
• Three or more admissions for heart failure within the past year;<br />
• Heart failure when hospital admission may not be the best/only/preferred option;<br />
• Stage IV patients (i.e. daily activities limited by dyspnoea) for whom hospice inpatient treatment may be<br />
of benefit, either immediately or in the future;<br />
• On optimal therapy but with marked or deteriorating physical or psychological symptoms*;<br />
• Those who may benefit from palliative day care or counselling*.<br />
* Where only psychological issues are present consider referral to psychology<br />
These guidelines have been compiled from a one year study undertaken at Guy’s and St. Thomas’ Hospital in<br />
collaboration with the Department of Palliative Care, Policy and Rehabilitation, Kings <strong>College</strong> <strong>London</strong> and St.<br />
Christopher’s Hospice. The study was supported by the Guy’s and St. Thomas’ Charity.<br />
Table 4.1: Referral criteria to Palliative Care at GSTT for patients with Heart Failure*<br />
26
5<br />
Education and Outreach<br />
5.1 General Education: Seminars, Masterclasses<br />
and Targeted Programmes<br />
The department is active in providing a programme of<br />
seminars and masterclasses as part of the COMPASS<br />
collaborative (see section 7 for details). We have<br />
undertaken a programme of masterclasses and open<br />
seminars (see table 5.1).<br />
Table 5.1 Open Seminars and COMPASS Collaborative Masterclasses <strong>2004</strong>/5-2006/7<br />
<strong>2004</strong><br />
Dr Sunny Kaul, UK<br />
Non-invasive Ventilation in MND<br />
Teresa Young, UK<br />
The European Organisation for Research and<br />
Treatment of Cancer - Approach to Quality of Life<br />
Measures: Past, Present and Future<br />
Dr Dan Munday, UK<br />
Palliative Care Research at the Edge of Chaos –<br />
looking through a complexity lens<br />
Dr Peter Fayers, UK<br />
Response Shift in Patients’ Reports of Quality of Life:<br />
What is it, why it matters, and how to assess it<br />
2005<br />
Prof Derick Wade, UK<br />
Do Biomedical Models of Illness Make for Good<br />
Healthcare Systems?<br />
Dr Bee Wee, UK<br />
Investigating Death Rattle: lessons learnt about<br />
research near the end of life<br />
Prof Harvey Chochinov, Canada<br />
Dying with Dignity: A contemporary challenge for end<br />
of life care<br />
Alicia O’Cathain, UK<br />
Communicating Purpose and Practice in Mixed<br />
Methods Studies<br />
Dr Stephen Barclay, UK<br />
Palliative Care in Primary Care: identifying and tracking<br />
deaths at home – development of a national study<br />
2006<br />
Prof Derick Wade, UK<br />
Getting Papers Published – how to avoid certain failure<br />
Dr Sandra Decker, USA<br />
Assessing Causality using Quasi-experiments<br />
Dr Magi Sque, UK<br />
Mixed Methods Research on Organ Donation<br />
Prof Derick Wade, UK<br />
Data, Data Everywhere but No Result in Sight<br />
Dr Lewis Cohen, USA<br />
Accusations of Euthanasia and Murder<br />
in End of Life Care<br />
Prof Alan Tennant, UK<br />
The role of Rasch Analysis in Medical Outcome<br />
Studies<br />
Prof Peter Disler, Australia<br />
Dimensions of Rehabilitation in Rural Australia<br />
Dr Richard Harding, UK<br />
Palliative Care in Sub-Saharan Africa – current<br />
evidence and activity<br />
Dr Stephen Barclay, UK<br />
Perspectives on Place of Death in Primary Care<br />
<strong>2007</strong><br />
Mandy Stratford, UK<br />
Dying to be at Home: relatives’ perceptions of caring<br />
for a loved one with advanced cancer<br />
Prof Allan Kellehear, Australia<br />
What is Health Promoting Palliative Care?<br />
Dr Patrick White, UK<br />
COPD and Palliative Care: does prognosis matter?<br />
Prof Jennifer Abbey, Australia<br />
The use of Photographs in Research with People with<br />
Late-stage Dementia<br />
Dr Wendy Magee<br />
Music Theraphy in Neuropalliative Rehabilitation<br />
Prof Amanda Ramirez<br />
Delivery Cancer Care in Multidisciplinary Teams:<br />
is it working?<br />
27
A specific ‘Palliative care for people with MS’ (PwMS)<br />
education programme was undertaken and evaluated,<br />
delivering a programme accessible to health and social<br />
care professionals working with PwMS across<br />
Southeast <strong>London</strong>. Nine study half days were<br />
undertaken and the education programme was formally<br />
evaluated, with 182 out of 234 (77%) participants<br />
describing each topic as quite or very useful.<br />
5.2 MSc, Postgraduate Diploma and Postgraduate<br />
Certificate in Palliative Care<br />
The philosophy underpinning the MSc in Palliative Care<br />
(and the new qualifications – the Postgraduate Diploma<br />
and Postgraduate Certificate) is to enable participating<br />
students to develop the skills required to appraise<br />
research and evidence on palliative care-related issues<br />
to inform their clinical practice and to develop relevant<br />
services. The MSc in Palliative Care, run in collaboration<br />
with St. Christopher’s Hospice and with the support of<br />
many talented external lecturers, who are experts in<br />
specific topics, is now very well established with a 10-<br />
year track record of providing a high class academic<br />
experience. It is distinctive from other national and<br />
international postgraduate palliative care degree courses<br />
in the following ways:<br />
1. The MSc is focused strongly on evidence and<br />
on understanding research relevant to palliative care.<br />
This is because palliative care is a relatively new<br />
specialty. Knowledge about which interventions have<br />
the potential to enhance quality of life for patients and<br />
their families, be they pharmacological, psychological,<br />
social or service-based, are still poorly<br />
understood or do not exist.<br />
2. The course is inter-professional. This allows<br />
students to explore similarities and differences in<br />
roles, skills, knowledge and their respective<br />
ideologies. It also provides scope for greater<br />
opportunity of open communication of all members<br />
within a group, consequently alleviating future<br />
hesitancy of single disciplines sharing knowledge<br />
with other professionals and non-professionals.<br />
3. The MSc, Postgraduate Diploma and Postgraduate<br />
Certificate courses are truly international. We<br />
have always encouraged applicants from beyond the<br />
UK because the different working experiences and<br />
cultures students bring with them enhance the<br />
entirety of the course. All students therefore learn<br />
about each others’ different funding arrangements for<br />
palliative care and related services, service configurations<br />
and their respective challenges, interventions to<br />
manage care, as well as the diversity.<br />
Many students who have successfully completed the<br />
course have gone on to achieve promotion within their<br />
respective professions. Of these students a large<br />
number have attributed their progression directly to the<br />
course experience. For more detail about the perceived<br />
added-value of the MSc in Palliative Care please refer to<br />
the recent evaluation of the MSc published in the<br />
Journal of Palliative Care 155 .<br />
28
5.3 Successful MSc Alumni and their Research<br />
Study Project Titles MSc Dissertations<br />
<strong>2004</strong>-<strong>2007</strong><br />
<strong>2004</strong><br />
The effectiveness of the respiratory nurse specialists’<br />
role for people with chronic obstructive pulmonary<br />
disease: a systematic review<br />
Judy Mulligan<br />
An exploratory study of bereaved grandparents’<br />
experience of losing a grandchild to a primary central<br />
nervous system tumour<br />
Mandy Reynolds<br />
The timing of the do-not-attempt-resuscitation decision<br />
for cancer patients in an acute oncology setting: how<br />
early is too early, how late is too late?<br />
Ann Muls<br />
The management of depression and irritability and<br />
aggression in people with Huntingdon's disease - a<br />
systematic review of the literature<br />
Rachel Taylor<br />
The very old who die from cancer: epidemiology and<br />
place of death in England and Wales (1995 - 1999)<br />
Anna Lock<br />
The impact of weight loss on body image in advanced<br />
cancer<br />
Ros Hinsley<br />
What is the "pain" experienced by patients with heart<br />
failure and is there a role for specialist palliative care?<br />
Katherine Thompson<br />
Loss of appetite in advanced cancer patients: a retrospective<br />
study of the impact on the informal spousecarer<br />
and their perception of intervention instigated by<br />
health professionals<br />
Ginette Pilkington<br />
Palliative care needs at a district general hospital: the<br />
view of patients, carers and health professionals. A<br />
descriptive epidemiological survey<br />
Joan Hester<br />
Continuing care provision for palliative care patients<br />
Stella Whitehouse<br />
A pilot study to assess the effectiveness of palliative<br />
care clinic in improving the quality of life for patients with<br />
severe heart failure<br />
Paul Paes<br />
2005<br />
A qualitative study on attitudes of nursing staff to<br />
nursing patients with severe late Parkinson's disease<br />
Phillip Jones<br />
Attitudes of health care professionals to the palliative<br />
care needs of people with end-stage dementia.<br />
A pilot study.<br />
Juliet Hately<br />
The thoughts and concerns of young people with<br />
advanced cancer: the barriers encountered in<br />
conducting palliative care research<br />
Katharine Williamson<br />
Dying to be at home: relatives’ perceptions of caring for<br />
a loved one or dependent with advanced cancer at<br />
home - meta-ethnographic review of qualitative papers<br />
Mandy Stratford<br />
Drug interactions in palliative care: how much harm do<br />
we do? The results from the palliative care unit in the<br />
county hospital of St Gallen, Switzerland<br />
Daniel Buche<br />
Physicians' attitudes towards prognostication<br />
Lotte Rogg<br />
Palliative Care Outcome Scale (POS) - a pilot study in<br />
Dover Park Hospice: is it applicable in the Singapore<br />
setting?<br />
Ee Wan Toh<br />
A systematic review to assess the quality of the research<br />
evidence investigating the effectiveness of palliative<br />
radiotherapy in the control of ambulatory function in<br />
patients with metastatic spinal cord compression.<br />
Louise Armstrong<br />
A study to investigate the use and experiences of<br />
general practitioners of the palliative care services in the<br />
Bromley PCT<br />
Sabrina Bajwah<br />
A qualitative investigation into health care professionals'<br />
experiences of performing last offices and attitude<br />
towards carrying out this procedure with family<br />
members<br />
Mary Macadie<br />
Prospective randomised controlled trial: comparing<br />
winged vialon cannula with soft-set cannula for<br />
continuous subcutaneous infusion in palliative care<br />
Rosemary Herbert<br />
Is the Support Team Assessment Schedule (STAS) a<br />
good choice as a clinical audit tool in the specialist<br />
palliative care unit?<br />
Liam O'Siorain<br />
A systematic literature review to determine the effectiveness<br />
of administering megestrol acetate to cachexicanorexic<br />
patients with advanced non-hormone sensitive<br />
cancer<br />
Nicola Bland<br />
Unmet needs in home palliative care: is there a role for<br />
communication technologies?<br />
Penny Carleton<br />
Evaluating the effectiveness of a palliative care link nurse<br />
system in an acute hospital<br />
Annemieke Fox<br />
29
2006<br />
An exploration of palliative care nurses' decision-making<br />
in the use of pro re nata (as needed) sedation<br />
Pauline Ui Dhuibhir<br />
Coping with loss. Do religious or spiritual beliefs<br />
influence bereavement? A systematic review<br />
Gerhild Becker<br />
Specialist palliative care in the adult intensive care unit:<br />
a multi-method project to investigate the need for<br />
integrating a specialist service into the ICU of a heart<br />
and lung hospital<br />
Josephine Archer<br />
Outcomes of palliative care in Sub-Saharan Africa -<br />
initial steps in the development of an outcome measure<br />
Karen Frame<br />
Multi-Disciplinary perspectives of music therapy in adult<br />
palliative care<br />
Julian O'Kelly<br />
Developing and testing a model of place of death in a<br />
macro-analysis of the trends in home death<br />
Barbara Gomes da Silva<br />
A research study to explore how bereaved families<br />
experience the use of cold bedrooms that enable their<br />
child to remain at a children's hospice from the time of<br />
their death up to the funeral<br />
Lynne Forrester<br />
A description of the implementation of NICE guidelines<br />
on the palliative care of patients with chronic cardiac<br />
failure: an exploratory study in a community Setting<br />
Nigel Konzon<br />
Efficacy of intranasal ketamine for the treatment of<br />
breakthrough pain in patients with cancer pain: a<br />
randomised double-blind, placebo-controlled, crossover<br />
study<br />
Birgit Haberland<br />
Decision-making processes in adult Charedi Ashkenazi<br />
patients with cancer; an interpretative phenomenological<br />
analysis<br />
Catharine Coleman<br />
Complementary and alternative medicine (CAM) in<br />
metastatic colorectal cancer patients receiving chemotherapy<br />
Tanja Trarbach<br />
A pilot study to determine the effectiveness of electroacupuncture<br />
as an adjunctive treatment to control<br />
neuropathic pain in patients with cancer and diabetes<br />
Ollie Minton<br />
<strong>2007</strong><br />
Interprofessional and inter-agency communication and<br />
cooperation in an ambulatory and hospital concept of<br />
palliative care provision for cancer patients in Germany -<br />
a qualitative study of health care professionals’<br />
perception<br />
Sabine Bader<br />
The use of clinical supervision by palliative medicine<br />
consultants – a questionnaire survey<br />
Chi-Chi Cheung<br />
A survey of the attitudes and beliefs of patients<br />
regarding cancer associated weight loss and weight<br />
assessment<br />
Simon Coulter<br />
A systematic literature review to determine the analgesic<br />
effectiveness of topical administration of opioids in the<br />
palliative care setting – the role of case reports in<br />
evidence based medicine.<br />
Beata LeBon<br />
How is the meaning of life articulated in palliative care<br />
patients?<br />
Natalia Lorenzo Garcia<br />
Death and Dying in hospital – experiences of older<br />
people and their families<br />
Annelise Matthews<br />
A pilot study using a multiple case study design to<br />
evaluate the theory of dry wound management in<br />
palliative care using the product Youki<br />
Jane McManus<br />
Exploring the palliative care knowledge and symptom<br />
control skills of British Heart Foundation heart failure<br />
nurses<br />
Deborah O'Hanlon<br />
Does education of palliative care professionals improve<br />
confidence levels of health care assistants when caring<br />
for dying patients and their families?<br />
Jackie Aaron<br />
The management of death rattle in dying cancer patients<br />
Eleni Karatzia-Chrysostomou<br />
Supportive and palliative care for adults with Cystic<br />
Fibrosis - the perceptions of their bereaved parents<br />
Kate Heaps<br />
30
5.4 Undergraduate Education<br />
The King’s <strong>College</strong> <strong>London</strong> School of Medicine, at<br />
Guy’s, King’s and St Thomas’ Hospitals is one of the<br />
largest medical providers of health care education in<br />
Europe, with over 400 medical students in each year. Dr<br />
Polly Edmonds and Dr Rachel Burman have led the<br />
development of the undergraduate curriculum in<br />
Palliative Medicine, with the course operating as a<br />
vertical strand with teaching across the whole five years<br />
of the curriculum. This integrated programme of<br />
teaching provides students with a variety of experiences<br />
from seminars, symposia, special study modules (SSMs)<br />
and bedside clinical teaching to the hospice visits in<br />
year five. Using a variety of teaching techniques in all of<br />
the sessions, the course is always very well evaluated. It<br />
provides a comprehensive coverage of the undergraduate<br />
curriculum, which is unique for Palliative Medicine<br />
both in its range and time allocated.<br />
The most innovative aspects of the undergraduate<br />
curriculum are the year five hospice visits and special<br />
study module (SSM) opportunities. The final year<br />
hospice visit, developed in partnership with St Christopher’s<br />
Hospice, Trinity Hospice and Pilgrim’s Hospice in<br />
Canterbury, is particularly well evaluated and gives the<br />
students an opportunity to visit a hospice and meet<br />
members of the multi-professional team, to gain an<br />
understanding of how the work delivered in the hospice<br />
differs from other health care settings. During the visit<br />
students meet day centre patients as part of the highly<br />
rated goldfish bowl session 77 . Other hospices involved in<br />
these visits over the past three years include St<br />
Michael’s Hospice in Hastings and The Martlet’s<br />
Hospice in Brighton.<br />
Four SSMs are offered in year four of the curriculum: the<br />
management of pain in advanced cancer; the<br />
management of anorexia and cachexia in advanced<br />
cancer; the ethics of withdrawing and withholding<br />
treatment in advanced cancer and a generic palliative<br />
care SSM, delivered in conjunction with St Christopher’s<br />
and Trinity Hospices. This SSM has been designed to<br />
give interested students more detailed exposure to<br />
palliative care by attending palliative care ward rounds<br />
with the hospital palliative care team at King’s <strong>College</strong><br />
Hospital and spending two days at either Trinity Hospice<br />
or St Christopher’s Hospice to experience inpatient<br />
palliative care, community care and hospice day care.<br />
This SSM is in its second year and has been well<br />
evaluated by participating students.<br />
In addition to the formal undergraduate curriculum,<br />
elective placements have been undertaken for GKT and<br />
overseas students at King’s (with the hospital palliative<br />
care team and academic department), Trinity Hospice<br />
and St Christopher’s Hospice.<br />
Dr Edmonds is also deputy head of year 4 and the year 4<br />
OSCE co-ordinator.<br />
31
6<br />
The <strong>Cicely</strong> <strong>Saunders</strong><br />
<strong>Institute</strong> of Palliative Care<br />
The Department is working with <strong>Cicely</strong> <strong>Saunders</strong><br />
International, <strong>King's</strong> <strong>College</strong> <strong>London</strong> and associated<br />
hospitals to establish the world’s first purpose built<br />
institute of palliative care, a centre of excellence housing<br />
research, education, information, support and clinical<br />
care. The <strong>Cicely</strong> <strong>Saunders</strong> <strong>Institute</strong> of Palliative Care will<br />
bring together academics, healthcare professionals,<br />
community organisations, patients and carers in one<br />
centre and will act as the hub for a network of international<br />
research. By providing a comprehensive approach<br />
to the physical, social and psychological needs of<br />
people with progressive illness, the <strong>Institute</strong>’s research<br />
will feed quickly and directly into practice and policy<br />
around the world – improving palliative care and<br />
enabling people to live better, with dignity and the least<br />
possible suffering.<br />
held a number of meetings involving local patient groups<br />
such as Black Cancer Care, along with a user<br />
involvement workshop. We hope that these activities will<br />
ensure that patients and their carers can guide and<br />
participate in our vision for the <strong>Institute</strong>.<br />
Building plans are now well advanced. The first brick will<br />
be laid in 2008, with completion of the building<br />
anticipated in 2009. On the ground floor we will be<br />
displaying some of the letters, photographs and books<br />
of Dame <strong>Cicely</strong> <strong>Saunders</strong> which are held in the King’s<br />
<strong>College</strong> <strong>London</strong> Specialist Archive at the Strand<br />
campus. We are very grateful to the private individuals,<br />
foundations and other donors who have contributed so<br />
far to the project, including: The Garfield Weston<br />
Foundation, The Wolfson Foundation, Macmillan Cancer<br />
Support, Atlantic Philanthropies, PF Charitable Trust and<br />
The Kirby Laing Foundation.<br />
<strong>Cicely</strong> <strong>Saunders</strong> International is an international charity<br />
created in 2002 by Dame <strong>Cicely</strong> <strong>Saunders</strong>, the founder of<br />
the modern hospice movement. <strong>Cicely</strong> <strong>Saunders</strong><br />
International supports high-quality research and<br />
education to improve the care and treatment of all people<br />
with progressive illness, helping them to reach the end of<br />
their lives with dignity and with the least possible<br />
suffering see www.cicelysaundersfoundation.org.<br />
The <strong>Institute</strong> will be a welcoming and peaceful<br />
environment, sensitively designed in line with the principles<br />
of palliative care and in consultation with potential groups,<br />
patient groups and Macmillan Cancer Relief.<br />
The 1,600 m² of floor space will provide:<br />
• Office space for over 90 staff, including researchers,<br />
clinical staff and several professors in palliative care,<br />
rehabilitation and related disciplines.<br />
• Teaching space, including seminar, tutorial and<br />
workshop rooms and a lecture theatre.<br />
• An information and support centre for patients, carers<br />
and healthcare professionals.<br />
• Space for clinical palliative care and cancer staff,<br />
including offices, therapy rooms and clinical/<br />
consultation rooms.<br />
• A video conferencing suite for international lectures<br />
and seminars.<br />
It is essential that the planning of the <strong>Institute</strong> reflects<br />
and serves the interests of patients and their carers.<br />
To achieve this, and to ensure that patients and families<br />
continue to contribute to our activities, we have<br />
implemented a strategy for user involvement. We have<br />
32
7<br />
Research Collaborations,<br />
External Committee<br />
Work and International<br />
Keynote Lectures<br />
7.1 Collaborations<br />
The department benefits from, and is part of, extensive<br />
collaborations in research, teaching and clinical activity.<br />
These are too many to mention, but some new major<br />
collaborations are described.<br />
COMPASS Collaboration<br />
This collaborative was funded by the National Cancer<br />
Research <strong>Institute</strong> (NCRI) in May 2006 for five years, with<br />
the intention of developing collaborative research<br />
projects, to submit for grant funding.<br />
The COMPASS (COMPlex interventions: Assessment,<br />
trialS and implementation of Services) Collaborative<br />
seeks to:<br />
• unite researchers from 12 UK universities, and more<br />
than 65 affiliated individuals or organisations, and<br />
• create a strong research grouping that can effectively<br />
research the development, evaluation and implementation<br />
of supportive and palliative interventions.<br />
COMPASS is led jointly from three Universities: King’s<br />
<strong>College</strong> <strong>London</strong>, University of Edinburgh and University<br />
of Leeds. The collaborative and its work on interventions<br />
span the whole trajectory of cancer care, from prediagnosis<br />
to longevity or terminal care and bereavement.<br />
The research has three main strands – assessment (led<br />
by Higginson at King’s), interventions and implementation<br />
(led by Ramirez, also at King’s). In addition there is a<br />
Masterclass programme of seminars and capacity<br />
building. The work on assessment links appropriately<br />
with the existing expertise in outcome measurement.<br />
European Palliative Care Research Collaborative<br />
(EPCRC)<br />
As part of a European collaborative, work is being taken<br />
forward to improve the management of three symptoms.<br />
Led by Professor Kaasa in Norway the group includes<br />
experts in 10 centres across Europe. The research plan<br />
of the EPCRC is based upon questions raised in the<br />
clinic, with focus on cancer palliative care patients, thus<br />
using a “true” translated approach. The research<br />
focuses both on diagnosis and classification of these<br />
symptoms and understanding of the underlying<br />
mechanisms. To achieve the aims of EPCRC a multidisciplinary<br />
approach was needed, bringing together basic<br />
scientists and clinicians that will translate human<br />
genome data into practical applications for these<br />
patients. Assessment and classification of pain,<br />
depression and cachexia (fatigue) are the basis for<br />
diagnosis and subsequent treatment. By use of modern<br />
methods of molecular biology the project seeks to<br />
increase the understanding of the role of genetic<br />
variability for pain and cachexia. European evidence<br />
based internet guidelines will be developed by members<br />
of the EPCRC supported by an international advisory<br />
board. By recruiting a pan European panel, cultural,<br />
social and language barriers will be taken into consideration<br />
in the early phase of the guideline development.<br />
At King’s, Higginson, with Professor Hotopf (<strong>Institute</strong> of<br />
Psychiatry) are leading the strand on the development of<br />
clinical guidelines for the management of depression,<br />
and providing input into the work on improving the<br />
assessment of depression. A first step is a Cochrane<br />
review into the effectiveness of antidepressants.<br />
Breathlessness Collaborations<br />
As part of the project supported by <strong>Cicely</strong> <strong>Saunders</strong><br />
International we are establishing a Breathlessness<br />
Collaboration. We are developing a database of relevant<br />
work and extend collaborations with others working in<br />
this field. The breathlessness programme is working<br />
together productively with several other projects on<br />
breathlessness: (1) a study on palliative care needs of<br />
patients with COPD, led by Dr. White, and supported by<br />
the Charitable Foundation of King’s <strong>College</strong> <strong>London</strong>, to<br />
which Dr Gysels is a co-applicant and participant on the<br />
Advisory Committee of the project; (2) contact and<br />
support is provided to a project undertaken at Imperial<br />
<strong>College</strong> <strong>London</strong> on the development of a multidimensional<br />
measurement tool for dyspnoea.<br />
As part of this we organised a joint meeting with the<br />
Medical Research Council in 2005 213 , an international<br />
conference on Breathlessness in November 2006, and a<br />
think-tank/workshop in 2006 with additional support<br />
from the Novartis Foundation.<br />
Partnerships, Research and Capacity<br />
Building in Africa<br />
We have forged productive relationships with partner<br />
agencies across Africa, and international funders, to<br />
generate research activity and enhance research<br />
capacity in Africa.<br />
In recent years the palliative care movement has made<br />
enormous strides in teaching, providing and advocating<br />
for palliative care in Africa. The HIV epidemic has greatly<br />
increased the requirement for palliative care and is the<br />
leading diagnosis for most services. However, cancer<br />
and other non-malignant diseases also contribute<br />
greatly to the required public health response to<br />
palliative care in Sub-Saharan Africa.<br />
Our close partnership with two key organisations in<br />
Africa, the African Palliative Care Association (APCA)<br />
and the Hospice Palliative Care Association of South<br />
Africa, have been very rewarding and a great source of<br />
learning, for both sides.<br />
We were very pleased to attend Archbishop Desmond<br />
Tutu’s birthday party at the British High Commission,<br />
hosted by KCL, to celebrate the life and work of our<br />
alumni member and to look forward to KCL’s support in<br />
digitising his archive.<br />
We believe strongly that while our priority is to develop<br />
evidence and evaluation methods that are relevant and<br />
appropriate to Africa, this is best achieved through<br />
partnerships to enhance the capacity for the African<br />
palliative care community to conduct and report its own<br />
research activity.<br />
We have had a number of successes in capacity<br />
building. Firstly, a Union Internationale Contre Cancer<br />
33
award enabled Richard Harding to attend Hospice Africa<br />
Uganda to teach nurses on the Distance Learning<br />
Diploma. The week-long module on research methods<br />
was very successful and attended by nurses from<br />
across East Africa.<br />
This year we have the first students from Africa<br />
attending our postgraduate education and we hope that<br />
this will continue to be a route to enhance research<br />
methods and other specialist knowledge that can be<br />
shared by attendees in their home countries.<br />
A particularly important development has been the<br />
appointments of the first palliative care research nurses<br />
in Africa, under a grant from the Big Lottery to <strong>Cicely</strong><br />
<strong>Saunders</strong> International and King’s <strong>College</strong> <strong>London</strong>. We<br />
have been able to offer these specialist staff protected<br />
contracts to focus on research and quality improvement,<br />
and they have produced high quality research data in a<br />
number of areas. This very enjoyable and successful<br />
partnership is an innovative model we hope to expand,<br />
and the opportunity to attend locally-delivered research<br />
training from KCL staff has been particularly appreciated<br />
by the nurses.<br />
King’s Centre for Palliative Neurology<br />
The King’s Centre for Palliative Care in Neurology<br />
(KCPN) is an exciting development that builds on<br />
internationally recognised clinical and academic<br />
expertise in neurology and palliative care at King’s<br />
<strong>College</strong> <strong>London</strong>. Nowhere have these two activities<br />
been thoroughly integrated, despite evidence that many<br />
patients with long term and progressive conditions<br />
benefit from integrated approaches to care. The KCPN<br />
and the component departments have wide-ranging<br />
collaborations, with many hospitals, hospices,<br />
community services – too numerous to list. In addition<br />
there are collaborative projects with researchers and<br />
educators in many academic institutions and national<br />
and international organisations. The Centre is led by<br />
Professor Irene Higginson and Professor Nigel Leigh as<br />
Co-Directors, assisted by an executive team comprising<br />
key partners from the departments of Neurology,<br />
Palliative Care, Policy and Rehabilitation, and from<br />
King’s <strong>College</strong> Hospital NHS trust. The Management<br />
Advisory Group comprises representatives of relevant<br />
user groups and of the wider academic, clinical,<br />
community and national partnership. In addition the<br />
Directors and Management group are advised by a<br />
Scientific Board to foster collaboration between<br />
research programmes and organisations. Current<br />
members on the Scientific Board include representation<br />
from the Motor Neurone Disease Association,<br />
Parkinson’s Disease Society, Multiple Sclerosis Society,<br />
Royal Hospital of Neurodisability and clinicians and<br />
academics from a variety of settings.<br />
A Consortium for Neuro-palliative<br />
Rehabilitation (NPR)<br />
People often think of rehabilitation as a short-term<br />
intervention to restore someone to independence after<br />
an accident or injury. However, in the context of neurodegenerative<br />
diseases, many people have profound and<br />
complex neurological disability (P&CND) and rehabilitation<br />
in this setting is focused on improving quality of life<br />
for patients and their carers, often against a backdrop of<br />
deteriorating physical, cognitive, communication and<br />
psychosocial function. It is a life-long process, which we<br />
have termed ‘neuropalliative rehabilitation’.<br />
A UK Consortium for Neuropalliative Rehabilitation has<br />
recently been established which has its principal<br />
academic base within the Centre for Palliative Neurology<br />
within King’s <strong>College</strong> <strong>London</strong>. The consortium brings<br />
together the three leading UK clinical centres for<br />
P&CND, covering a large catchment population in the<br />
south east quarter of England, and is led by:<br />
• Professor Lynne Turner-Stokes (NW <strong>London</strong> Regional<br />
Rehabilitation network),<br />
• Professor Keith Andrews (RHN Putney),<br />
• Professor Derick Wade (Oxford Centre for<br />
Enablement).<br />
The consortium already co-ordinates a <strong>London</strong> and SE<br />
England research group for collaborative and multicentre<br />
research into complex neurological disorders,<br />
and in collaboration with the British Society of Rehabilitation<br />
Medicine (BSRM), setting up a national network of<br />
rehabilitation units involved in research in this area. In<br />
addition to its UK membership, the consortium has<br />
collaborative links internationally with key researchers in<br />
the USA, Australia, New Zealand and the Netherlands.<br />
The purpose of the consortium is to undertake a coordinated<br />
health services research programme in<br />
Neuro-palliative Rehabilitation to address innovation and<br />
interventions to empower and support people with<br />
complex neurological disabilities following brain injury<br />
and other related long term neurological conditions.<br />
The programme supports evidence-based services<br />
which improve the quality of long-term care offered to<br />
patients and their families, in line with user demand and<br />
with Government policy which emphasises patient<br />
choice, user-centred interventions and outcomes,<br />
integrated multi-agency care, and long-term evaluation.<br />
7.2 Involvement in External Committees<br />
<strong>2004</strong>/5 – 2006/7<br />
Professor Irene Higginson<br />
Chair<br />
• MS Society Applied Research Panel<br />
Membership<br />
• Canadian <strong>Institute</strong>s for Health Research<br />
• Multiple Sclerosis Society Grant Review Panel<br />
• Dunhill Medical Trust Grants and Research<br />
Committee<br />
• National Cancer Research <strong>Institute</strong> Palliative Care<br />
Study Development Group (and Primary Palliative<br />
Care and Breathlessness subgroups)<br />
• Cancer Research UK Feasibility Committee<br />
• Macmillan Cancer Support Observatory Group<br />
• Motor Neurone Disease Association Clinical<br />
Advisory Group<br />
• Guy’s and St Thomas’ Charitable Foundation Service<br />
Innovations and Development Group<br />
• Association for Palliative Medicine Science<br />
Committee<br />
• General Medical Council Guidance on Withholding<br />
and Withdrawing Treatment<br />
34
• International Psycho Oncology Society National<br />
Scientific Committee for <strong>2007</strong> World Congress<br />
• European Association for Palliative Care Scientific<br />
Committee for 5th Forum on Research<br />
• HEFCE Research Assessment Exercise Panel – Subpanel<br />
2, Cancer Studies<br />
• COMPASS Collaborative Management Board<br />
Professor Lynne Turner-Stokes<br />
Chair<br />
• Research and Clinical Standards Subcommittee,<br />
British Society of Rehabilitation Medicine<br />
• Multi-professional and Health Service Research<br />
Group, NWLHT<br />
• <strong>London</strong> Neurosciences Modernisation Team: Neuro<br />
Rehab Executive Working Group<br />
• Guideline Development Group for updating<br />
guidelines for use of botulinum toxin in spasticity<br />
management. BSRM / RCP guidelines<br />
• Healthcare Resource Group (HRG) Expert Working<br />
Panel for rehabilitation, implementing Payment<br />
by Results<br />
• Research and Evidence Subgroup for the National<br />
Service Framework in Long-Term Conditions<br />
• <strong>London</strong> Neuro-rehabilitation Specialised Commissioning<br />
Consortium: Chair of Clinical and Audit<br />
Committee<br />
• External Reference Group for the National Service<br />
Framework in Long-Term Conditions (Deputy Chair)<br />
• Research Evidence Subgroup for the National<br />
Service Framework in Long Term Conditions<br />
Membership<br />
• Royal <strong>College</strong> of Physicians (RCP) Rehabilitation<br />
Medicine Committee<br />
• Medical Defence Union Council and Cases<br />
Committee<br />
• RCP Joint Specialist Society Clinical Effectiveness<br />
Forum<br />
• Expert Working Group: Payment by Results. Chapter<br />
A (Nervous System)<br />
• Northwick Park <strong>Institute</strong> of Medical Research<br />
Academic Board<br />
• NWLHT Clinical Governance Committee<br />
• NWLHT R&D Executive Committee<br />
• NWLHT R&D Peer Review Committee<br />
• NW <strong>London</strong> Sector Specialist Commissioning Group<br />
for Neurosciences<br />
• Pan <strong>London</strong> Neuro-rehabilitation Specialist Commissioning<br />
Group<br />
• Trust Board for the <strong>Institute</strong> of Complex Disability,<br />
Royal Hospital for Neuro-disability, Putney<br />
• BSRM working party for report on Musculo-skeletal<br />
Rehabilitation<br />
• RCP working party: Chronic Disease Management<br />
in the NHS<br />
• Working party: Guidelines for referral for spasticity<br />
management<br />
• Access to rehabilitation: a group convened by the<br />
Civil Justice Council<br />
• National <strong>Institute</strong> for Palliative Care: Long Term<br />
Neurological Conditions Committee<br />
Dr Polly Edmonds<br />
Membership<br />
• <strong>London</strong>/Kent Surrey Sussex Speciality Training<br />
Committee for Palliative Medicine (Director)<br />
• Southeast <strong>London</strong> Cancer Research Network<br />
• NCRI Breathlessness Subgroup<br />
• King’s <strong>College</strong> Hospital Cancer Services Committee<br />
and Cancer Management Team<br />
• Specialist Medicine Care Group<br />
• King’s <strong>College</strong> Hospital Clinical Effectiveness and<br />
Audit Committee<br />
• Southeast <strong>London</strong> Cancer Network Palliative Care<br />
Coordinating Group<br />
• Southeast <strong>London</strong> Cancer Network Upper GI Cancer<br />
Subgroup<br />
• Lambeth and Southwark Cancer Forum<br />
• <strong>London</strong> Regional Group of the National Council for<br />
Hospice and Palliative Care Services<br />
Dr Rachel Burman<br />
Membership<br />
• <strong>London</strong>/Kent Surry Sussex Speciality Training<br />
Committee for Palliative Medicine (Director)<br />
• King’s <strong>College</strong> Hospital Resuscitation Committee<br />
• St Christopher’s Hospice Ethics Committee<br />
• University of <strong>London</strong> Senate Subject Panel<br />
in Medical Ethics<br />
Dr Richard Harding<br />
Membership<br />
• International AIDS Society<br />
• African Palliative Care Association<br />
• International Association of Hospice Palliative Care<br />
• Worldwide Forum for Hospice and Palliative Care<br />
Jonathan Koffman<br />
Membership<br />
• Palliative Care Section, Royal Society of Medicine<br />
• Research Ethics Committee, King’s <strong>College</strong> <strong>London</strong>/<br />
St Christopher’s Hospice<br />
Dr Sue Hall<br />
Membership<br />
• NCRI Brain Tumour Studies Group Palliative Care<br />
Sub-group<br />
Dr Fliss Murtagh<br />
Membership<br />
• Working Party on use of the Liverpool Care Pathway<br />
for Renal Patients<br />
Dr Morag Farquhar<br />
Membership<br />
• NCRI Palliative Care Breathlessness Sub-Group<br />
Dr Claudia Bausewein<br />
Membership<br />
• Advisory Board for Palliative Medicine in Bavaria for<br />
the Bavarian Ministry for Work, Social Services,<br />
Family and Women (Board Member)<br />
• German Association for Palliative Medicine (Vicepresident)<br />
35
7.3 International and Keynote Lectures<br />
<strong>2004</strong><br />
Professor Irene Higginson<br />
Supportive and palliative care: the state of the evidence<br />
base. British Psychosocial Oncology Society. Helping<br />
people live with cancer. UK plans for action.<br />
Goodenough <strong>College</strong>, Mecklenburgh Square, <strong>London</strong>.<br />
December <strong>2004</strong>.<br />
Lessons from other nations. National <strong>Institute</strong>s of Health<br />
State of the Science Conference on Improving Care at<br />
the End of Life, Bethesda, USA. December <strong>2004</strong>.<br />
Latest progress with the Palliative Care Outcome Scale<br />
(POS).12th Palliative Care Study Day, Norfolk and<br />
Norwich University Hospital, Norwich. Park Farm Hotel,<br />
Norwich. November <strong>2004</strong>.<br />
Complex Interventions in Palliative Care Study Day.<br />
Hulme Hall, University of Manchester. November <strong>2004</strong>.<br />
The MRC Framework in palliative care: lessons from the<br />
development of group support for carers and a new<br />
service for patients with multiple sclerosis.<br />
Palliative care in Sub-Saharan Africa: An appraisal.<br />
Presentation of the main findings and recommendations.<br />
Palliative Care in Sub-Saharan Africa: An<br />
Appraisal. The County Hall, <strong>London</strong>. May <strong>2004</strong>. Joint<br />
with Dr Richard Harding.<br />
Advancing palliative care for the world’s aging<br />
population. Harold Hatch International Lectureship in<br />
Geriatrics and Oncology, International Longevity Center,<br />
Mount Sinai, New York, USA. April <strong>2004</strong>.<br />
NICE work: reviewing the effectiveness of palliative<br />
cancer care for the UK government National <strong>Institute</strong> of<br />
Clinical Excellence (NICE).Medicine Grand Rounds,<br />
Mount Sinai Hospital, New York, USA. April <strong>2004</strong>.<br />
Effectiveness of palliative care: scientific evidence and<br />
unanswered questions. Regional Conference of the Italian<br />
Society of Palliative Care. Biella, Italy. February <strong>2004</strong>.<br />
Professor Lynne Turner-Stokes<br />
How to be an effective expert witness. Workshop:<br />
Doctors Update, Belle Plagne, France. Feb <strong>2004</strong>.<br />
Demonstrating functional benefits from Botulinum Toxin<br />
injection. Symposium: Botulinum toxin - current practice<br />
in spasticity management. 14th European Congress in<br />
Physical and Rehabilitation Medicine, Vienna, Austria.<br />
May <strong>2004</strong>.<br />
The challenges of spasticity management following<br />
acquired brain injury – a European perspective.<br />
Extended lecture tour of Australia to give a series of<br />
lectures on this topic area: Symposia in Perth, Sydney,<br />
Melbourne and Brisbane, Australia. September <strong>2004</strong>.<br />
Jonathan Koffman<br />
Multi-professional palliative care education: does it<br />
make a difference? 3rd Research Forum of the European<br />
Association of Palliative Care, Stressa, Italy. June <strong>2004</strong>.<br />
2005<br />
Professor Irene Higginson<br />
Latest developments with the Palliative Outcome Scale<br />
and the Support Team Assessment Schedule.<br />
Measuring Palliative Care. Our Lady’s Hospice, Dublin.<br />
October 2005.<br />
The future of palliative medicine. World Day on Hospice<br />
and Palliative Care. Klinik und Poliklinik für Palliativmedizin,<br />
Cologne. October 2005.<br />
Palliative Care. Ageing and Research at King’s: ARK.<br />
Wolfson Centre for Age-Related Disease, King’s <strong>College</strong><br />
<strong>London</strong>. October 2005.<br />
Is there evidence of effectiveness for palliative care:<br />
what, for whom and when? NCRI Cancer Conference.<br />
ICC, Birmingham. October 2005.<br />
From clinical experience to testable hypothesis. Swiss<br />
National Research Day. Kantonsspital, St Gallen<br />
Switzerland. September 2005.<br />
Migliore cure palliative per le personne anziane [Better<br />
palliative care for older people]. Conference on Palliative<br />
Care in the Elderly. National Cancer <strong>Institute</strong>, Italy.<br />
September 2005.<br />
Hospice Education <strong>Institute</strong> Hospice and Palliative Care<br />
Study Seminar. King’s Fund, <strong>London</strong>. March 2005<br />
Ethical issues of evaluating a new palliative care service<br />
for patients with Multiple Sclerosis. Dimensions in<br />
palliative care. Earl Mountbatten Hospice. New<br />
Holmwood Hotel, Isle of Wight. March 2005.<br />
Professor Lynne Turner-Stokes<br />
Evaluation of the evidence for rehabilitation following<br />
acquired brain injury.<br />
George Burniston Oration: Australian Faculty of Rehabilitation<br />
Medicine and International Brain Injury<br />
Association, Melbourne, Australia. May 2005.<br />
Strategies for spasticity management – an individualised<br />
approach. Extended lecture tour: Symposia in<br />
Melbourne, Sydney and Auckland, Australia. May 2005.<br />
Management of depression in acquired brain injury.<br />
Australian Faculty of Rehabilitation Medicine and<br />
International Brain Injury Association, Melbourne,<br />
Australia. May 2005.<br />
UK National Service Frameworks and evidence for<br />
effectiveness in Rehabilitation.<br />
Auckland University of Technology. New Zealand.<br />
May 2005.<br />
36
Assessment and Treatment of Depression in Acquired<br />
Brain Injury. Moss Rehabilitation. Philadelphia, USA.<br />
October 2005.<br />
Evaluation of the evidence for rehabilitation following<br />
acquired brain injury. Moss Rehabilitation. Philadelphia,<br />
USA. October 2005.<br />
Dr Richard Harding<br />
Research in palliative care: an agenda for Africa. Mind,<br />
Body, Spirit Conference of the Hospice Palliative Care<br />
Association of South Africa, Cape Town, South Africa.<br />
December 2005.<br />
We were delighted that the International AIDS Society<br />
held a special session on palliative care at its conference<br />
in Toronto in August 2006, where Dr Richard Harding<br />
was an invited panel speaker.<br />
Dr Fliss Murtagh<br />
Symptom management in patients with end-stage renal<br />
disease managed without dialysis. European Dialysis<br />
and Transplant Nurses Association/European Renal<br />
Care Association 34th International Conference, Vienna,<br />
Austria. September 2005.<br />
Jonathan Koffman<br />
A systematic review of race, ethnicity and culture<br />
as variables in palliative care research. European<br />
Association of Palliative Care. Aachen, Germany.<br />
April 2005.<br />
2006<br />
Professor Irene Higginson<br />
Being at home at the end of life: is it better? Lecture for<br />
receiving the Mendelssohn Award for outstanding<br />
contribution to palliative care. 10th Annual Interdisciplinary<br />
Approach to Symptom Control, Palliative and<br />
Hospice Care Conference. MD Anderson Cancer<br />
Centre, Texas, USA. October 2006.<br />
Extending palliative care beyond cancer: past, present<br />
and future (Plenary lecture) plus 3 workshop sessions<br />
- Non-Cancer end of life care – Discussion; Overview of<br />
measurement tools for quality improvement and care in<br />
palliative care; Dying at home – making it an achievable<br />
goal; <strong>Cicely</strong> <strong>Saunders</strong> International – Future Plans. 16th<br />
International Congress on Care of the Terminally Ill.<br />
Palais des Congress, Montreal, Quebec, Canada.<br />
September 2006.<br />
Evaluating effectiveness of intervention in progressive<br />
conditions. Measuring effectiveness against a<br />
background of deterioration. Joint Summer Meeting of<br />
the British Society of Rehabilitation Medicine & The<br />
Society for Research in Rehabilitation. University of<br />
Westminster, Marylebone Campus, <strong>London</strong>. July 2006.<br />
Better palliative care for older people: a global strategy?<br />
World Health Organisation 8th Global Conference on<br />
Ageing. Copenhagen, Denmark. June 2006.<br />
Better palliative care for older people: World Health<br />
Organisation perspective to national issues. Palliative<br />
Care for Older People. European Association of Palliative<br />
Care Conference on Older People, Our Lady’s Hospice,<br />
Dublin. April 2006.<br />
1. What are the new partnerships in palliative care<br />
research? 2. What effect does palliative day care on<br />
patient outcomes: non-randomised comparison? 6th<br />
Palliative Care Congress, University of Sheffield,<br />
Sheffield. April 2006.<br />
Outcome measurement in palliative care. Outcome<br />
measurement in palliative care: Beyond the NICE<br />
guidance. National Council for Palliative Care, <strong>London</strong>.<br />
March 2006.<br />
Professor Lynne Turner-Stokes<br />
The Mental Capacity Act 2005 – what will it mean for<br />
surgeons? Plenary session: Doctors updates. Belle<br />
Plagne, France. 2006.<br />
Spinal cord injury – management of patient and their<br />
bladder. Doctors updates. Belle Plagne, France. 2006.<br />
Botulinum toxin in neurogenic bladder dysfunction – a<br />
review of the evidence. Doctors updates. Belle Plagne,<br />
France. 2006.<br />
Goal attainment scaling – a realistic alternative to<br />
standardised outcome measurement?<br />
BTX for upper-limb spasticity – individualised treatment<br />
or standard treatment algorithms? Extended lecture<br />
tour: Symposia in Melbourne, Sydney, Australia. 2006.<br />
Dr Richard Harding<br />
Palliative care: research in Sub-Saharan Africa.<br />
European Association of Palliative Care. Venice, Italy.<br />
May 2006.<br />
HIV palliative care in the era of antiretroviral therapy.<br />
International AIDS Society. Toronto, Canada. August<br />
2006.<br />
Jonathan Koffman<br />
Factors associated with understanding palliative care:<br />
results from a survey of oncology out-patients. 4th<br />
Research Forum of the European Association of<br />
Palliative Care. Venice, Italy. May 2006.<br />
37
8<br />
Publication List<br />
PUBLICATIONS - <strong>2004</strong><br />
PAPERS IN SCIENTIFIC JOURNALS<br />
1. BAUSEWEIN C, HIGGINSON IJ. Appropriate<br />
methods to assess the effectiveness and efficacy of treatments<br />
or interventions to control cancer pain. Journal of Palliative<br />
Medicine <strong>2004</strong>;7:423-430<br />
2. BURT J, SHIPMAN C, BARCLAY SIG, Marshall N,<br />
Stimson A, Young J. Continuity within primary palliative care:<br />
an audit of general practice out-of-hours co-operatives.<br />
Journal of Public Health <strong>2004</strong>;26:275-276<br />
3. Elkington H, White P, ADDINGTON-HALL JM, Higgs<br />
R, Pettinari C. The last year of life of COPD: a qualitative study<br />
of symptoms and services. Respiratory Medicine <strong>2004</strong>:98:439-<br />
445<br />
4. Ewing G, Todd C, Rogers M, BARCLAY SIG, McCabe<br />
J, Martin A. Validation of a symptom measure suitable for use<br />
among palliative care patients in the community: CAMPAS-R.<br />
Journal of Pain and Symptom Management <strong>2004</strong>;27:287-299<br />
5. Francis HP, WADE DT, TURNER-STOKES L,<br />
Kingswell RS, Dott CS, Coxon EA. Does reducing spasticity<br />
translate into functional benefit? An exploratory meta-analysis.<br />
Journal of Neurology, Neurosurgery and Psychiatry<br />
<strong>2004</strong>;75:1547-1551<br />
6. GOMES B, HIGGINSON IJ. Home or hospital?<br />
Choices at the end of life. Journal of the Royal Society of<br />
Medicine <strong>2004</strong>;97:413-414<br />
7. Grande GE, FARQUHAR MC, BARCLAY SIG, Todd CJ.<br />
Caregiver bereavement outcome: relationship with Hospice at<br />
Home, satisfaction with care, and home death. Journal of<br />
Palliative Care <strong>2004</strong>;20:69-77<br />
8. Gruenewald DA, HIGGINSON IJ, VIVAT B,<br />
EDMONDS PM, BURMAN RE. Quality of life measures for the<br />
palliative care of people severely affected by multiple sclerosis:<br />
a systematic review. Multiple Sclerosis <strong>2004</strong>;10: 690-725<br />
9. GYSELS M, Richardson A, HIGGINSON IJ.<br />
Communication training for health professionals who care for<br />
patients with cancer: a systematic review of effectiveness.<br />
Supportive Care in Cancer <strong>2004</strong>;12:692-700<br />
10. GYSELS M, HUGHES R, ASPINAL F, ADDINGTON-<br />
HALL JM, HIGGINSON IJ. What methods do stakeholders<br />
prefer for feeding back performance data: a qualitative study in<br />
palliative care. International Journal for Quality in Health Care<br />
<strong>2004</strong>;16:375-381<br />
11. HALL S, Weinman J, Marteau TM. The<br />
motivating impact of information informing women of a link<br />
between smoking and cervical cancer: the role of coherence.<br />
Health Psychology <strong>2004</strong>;23:419-424<br />
carers of patients attending a home palliative care service.<br />
Journal of Pain and Symptom Management <strong>2004</strong>;27:396-408<br />
13. HARDING R, Bensley J, Corrigan N, Franks L,<br />
Stratman J, Waller Z, Warner J. Outcomes and lessons from a<br />
pilot RCT of a community-based HIV prevention multi-session<br />
group intervention for gay men. AIDS Care <strong>2004</strong>;16:581-585<br />
14. HARDING R, Bensley J, Corrigan N. Targeting<br />
smoking cessation to high prevalence communities: outcomes<br />
from a pilot intervention for gay men. BMC Public Health<br />
<strong>2004</strong>;4:43<br />
15. HIGGINSON IJ. It would be NICE to have more<br />
evidence? Palliative Medicine <strong>2004</strong>;18:85-86 Editorial<br />
16. HIGGINSON IJ, DONALDSON N. Relationship<br />
between three palliative care outcome scales. Health and<br />
Quality of Life Outcomes <strong>2004</strong>;2:68-75<br />
17. HUGHES RA, Down K, Sinha A, HIGGINSON IJ,<br />
Leigh PN. Building user involvement in motor neurone disease:<br />
key lessons. Journal of Interprofessional Care <strong>2004</strong>;18:80-81<br />
18. HUGHES RA, Sinha A, Aspinal F, Dunckley M,<br />
ADDINGTON-HALL JM, HIGGINSON IJ. What is the potential<br />
for the use of clinical outcome measures to be computerised?<br />
Findings from a qualitative study. International Journal of<br />
Health Care Quality Assurance <strong>2004</strong>;17:47-52<br />
19. HUGHES RA, ADDINGTON-HALL JM, Aspinal F,<br />
Dunckley M, HIGGINSON IJ. Developing methods to improve<br />
the quality of end-of-life care. Journal of Interprofessional Care<br />
<strong>2004</strong>;18:200-201<br />
20. HUGHES RA, Aspinal F, ADDINGTON-HALL JM,<br />
Dunckley M, Faull C, HIGGINSON IJ. It just didn’t work: the<br />
realities of quality assessment in the English health care context.<br />
International Journal of Nursing Studies <strong>2004</strong>;41:705-712<br />
21. HUGHES RA, Aspinal F, HIGGINSON IJ, ADDINGTON-<br />
HALL JM, Dunckley M, Faull C, Sinha A. Assessing palliative care<br />
outcomes for people with motor neurone disease living at home.<br />
International Journal of Palliative Nursing <strong>2004</strong>;10:449-453<br />
22. Kalra L, Evans A, Perez I, Melbourn A, Patel A, Knapp M,<br />
DONALDSON N. Training carers of stroke patients:<br />
randomised controlled trial. British Medical Journal<br />
<strong>2004</strong>;328:1099-1101<br />
23. Karus D, Raveis VH, Marconi K, Hanna B, Selwyn P,<br />
Alexander C, Perrone M, HIGGINSON IJ. Service needs of<br />
patients with advanced HIV disease: a comparison of client and<br />
staff reports at three palliative care projects. AIDS Patient Care<br />
and STDs. <strong>2004</strong>;18:145-158<br />
12. HARDING R, HIGGINSON IJ, Leam C,<br />
DONALDSON N, Pearce A, George R, Robinson V, Taylor L.<br />
Evaluation of a short-term group intervention for informal<br />
38
24. Karus D, Raveis VH, Marconi K, Selwyn P, Alexander C,<br />
Hanna B, HIGGINSON IJ. Mental health status of clients from<br />
three HIV/AIDS palliative care projects. Palliative and<br />
Supportive Care <strong>2004</strong>;2:125-138<br />
25. KOFFMAN J, HIGGINSON IJ. Dying to be home? Preferred<br />
location of death of first-generation black Caribbean and<br />
native-born white patients in the United Kingdom. Journal of<br />
Palliative Medicine <strong>2004</strong>;7:628-636<br />
26. Lowton K. Only when I cough? Adults’ disclosure of cystic<br />
fibrosis. Qualitative Health Research <strong>2004</strong>;14:167-186<br />
27. McPherson CJ, ADDINGTON-HALL JM. How do proxies’<br />
perceptions of patients’ pain, anxiety, and depression change<br />
during the bereavement period? Journal of Palliative Care<br />
<strong>2004</strong>;20:12-19<br />
28. MAGEE WL, Davidson JW. Singing In Therapy: Monitoring<br />
disease process in chronic degenerative illness. British Journal<br />
of Music Therapy <strong>2004</strong>;18:65-77.<br />
29. MAGEE WL and Davidson, JW. Music therapy in Multiple<br />
Sclerosis: results of a systematic qualitative analysis.<br />
Music Therapy Perspectives <strong>2004</strong>;22:39-51.<br />
30. Murray SA, Boyd K, Sheikh A, Thomas K, HIGGINSON IJ.<br />
Developing primary palliative care. British Medical Journal<br />
<strong>2004</strong>;329:1056-1057. Editorial<br />
31. POTTER J, HIGGINSON IJ. Pain experienced by lung<br />
cancer patients: a review of prevalence, causes and pathophysiology.<br />
Lung Cancer <strong>2004</strong>;43:247-257<br />
32. <strong>Saunders</strong> Y, Ross JR, Broadley KE, EDMONDS PM, Patel<br />
S. Systematic review of bisphosphonates for hypercalcaemia<br />
of malignancy. Palliative Medicine <strong>2004</strong>;18:418-431<br />
33. SPECK PW, HIGGINSON IJ, ADDINGTON-HALL JM.<br />
Spiritual needs in health care. British Medical Journal<br />
<strong>2004</strong>;329:123-124<br />
34. Vigano A, DONALDSON N, HIGGINSON IJ, Bruera E,<br />
Mahmud S, Suarez-Almazor M. Quality of life and survival<br />
prediction in terminal cancer patients. Cancer <strong>2004</strong>;101:1090-<br />
1098<br />
35. White C, Pritchard J, TURNER-STOKES L. Exercise for<br />
people with peripheral neuropathy. The Cochrane Database of<br />
Systematic Reviews <strong>2004</strong>;Oct 18, Issue 4:CD003904<br />
BOOKS<br />
36. ARMES J, Krishnasamy M, HIGGINSON IJ (Eds). Fatigue<br />
in Cancer. Oxford: Oxford University Press, <strong>2004</strong><br />
37. DAVIES E, HIGGINSON IJ. Palliative Care: The Solid Facts.<br />
World Health Organization. <strong>2004</strong><br />
38. DAVIES E, HIGGINSON IJ. Better palliative care for older<br />
people. World Health Organisation. <strong>2004</strong><br />
39. EDMONDS PM, Sykes N, Wiles J (Eds). Management of<br />
Advanced Disease. <strong>London</strong>: Arnold Publishers. 4th Edition.<br />
<strong>2004</strong><br />
BOOK CHAPTERS<br />
40. ADDINGTON-HALL JM. Referral patterns and access to<br />
specialist palliative care. In: Payne S, Seymour J, Ingleton C<br />
(Eds). Palliative Care Nursing: Principles and Evidence for<br />
Practice <strong>London</strong>: Open University Press <strong>2004</strong>;pp90-107<br />
41. ADDINGTON-HALL JM. Clinical challenges in nonmalignant<br />
disease: overview. In: Sykes N, EDMONDS PM,<br />
Wiles J. Management of Advanced Disease <strong>London</strong>: Arnold<br />
Publishers. 4th Edition. <strong>2004</strong>;pp319-326<br />
42. ARMES J. The experience of cancer-related fatigue. In:<br />
ARMES J, Krishnasamy M, HIGGINSON IJ (Eds). Fatigue in<br />
Cancer. Oxford: Oxford University Press. <strong>2004</strong>;pp137-155<br />
43. Aspinal F, HIGGINSON IJ. Audit, outcomes and quality of<br />
life in palliative care. In: Sykes N, EDMONDS P, Wiles J.<br />
Management of Advanced Disease <strong>London</strong>: Arnold Publishers.<br />
<strong>2004</strong>;pp27-47<br />
44. Borasio GD, Rogers A, Voltz R. Palliative medicine in<br />
non-malignant neurological disorders. Doyle D, Hanks G,<br />
Cherny N, Calman K (Eds). In: Oxford Textbook of Palliative<br />
Medicine. Oxford: Oxford University Press. <strong>2004</strong>;pp925-934<br />
45. EDMONDS PM, Cox S. Symptoms and Palliation.Jones R,<br />
Britten N, Culpepper L, Gass D, Grol R, Mant D, Silagy C (Eds).<br />
In: Oxford Textbook of Primary Medical Care – Volume 2:<br />
Clinical Management. Oxford: Oxford University Press.<br />
<strong>2004</strong>;pp1295-1299<br />
46. EDMONDS PM. Symptom Assessment. In: Sykes N,<br />
EDMONDS PM, Wiles J, (Eds.) Management of Advanced<br />
Disease. <strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>;pp51-54<br />
47. EDMONDS PM. Breathlessness. In: Sykes N, EDMONDS<br />
PM, Wiles J, (Eds). Management of Advanced Disease.<br />
<strong>London</strong>: Arnold Publishers . 4th Edition. <strong>2004</strong>; pp73-82<br />
48. EDMONDS PM. Cough. In: Sykes N, EDMONDS PM,<br />
Wiles J, (Eds). Management of Advanced Disease. <strong>London</strong>:<br />
Arnold Publishers 4th Edition. <strong>2004</strong>; pp101-105<br />
39
49. EDMONDS PM, Wiles J. Pleural Effusions. In: Sykes N,<br />
EDMONDS PM, Wiles J, (Eds). Management of Advanced<br />
Disease. <strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>;<br />
pp289-294<br />
50. EDMONDS PM, Wiles J. Travel Abroad. In: Sykes N,<br />
EDMONDS PM, Wiles J, (Eds). Management of Advanced<br />
Disease. <strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>; pp545-<br />
548<br />
51. HIGGINSON IJ, Hearn J, ADDINGTON-HALL JM.<br />
Epidemiology of cancer pain. Series Eds: Warfield C, Rice A,<br />
McGrath P and Justins D. Volume (Eds): Sykes N, Fallon MT,<br />
Patt RB. In: Clinical Pain Management – Cancer Pain. <strong>London</strong>:<br />
Arnold Publishers. <strong>2004</strong>; pp21-32<br />
52. HIGGINSON IJ, COSTANTINI M, EDMONDS PM,<br />
Viterbori P. The dying patient and their family. Jones R, Britten<br />
N, Culpepper L, Gass D, Grol R, Mant D, Silagy C (Eds).<br />
In: Oxford Textbook of Primary Medical Care – Volume 2:<br />
Clinical Management. Oxford: Oxford University Press.<br />
<strong>2004</strong>;pp1271-1277<br />
53. HIGGINSON IJ, EDMONDS PM, Viterbori P,<br />
COSTANTINI M, Cox S. Terminal and palliative care. Jones<br />
R, Britten N, Culpepper L, Gass D, Grol R, Mant D, Silagy C<br />
(Eds). In: Oxford Textbook of Primary Medical Care – Volume<br />
1: Principles and Concepts. Oxford: Oxford University Press.<br />
<strong>2004</strong>;pp259-264<br />
54. HIGGINSON IJ, ADDINGTON-HALL JM. The epidemiology<br />
of death and symptoms. Doyle D, Hanks G, Cherny N,<br />
Calman K (Eds). In: Oxford Textbook of Palliative Medicine.<br />
Oxford: Oxford University Press. <strong>2004</strong>;pp14-24<br />
55. HIGGINSON IJ, ARMES J, Krishnasamy M. Introduction.<br />
In: ARMES J, Krishnasamy M, HIGGINSON IJ (Eds). Fatigue in<br />
Cancer. Oxford: Oxford University Press. <strong>2004</strong>;pp17-21<br />
56. HIGGINSON IJ. Clinical and organizational audit in<br />
palliative medicine. In: Oxford Textbook of Palliative Medicine.<br />
Doyle D, Hanks G, Cherny N, Calman K. Oxford (Eds): Oxford<br />
University Press. <strong>2004</strong>;pp184-196<br />
57. KOFFMAN J, Camps M. No way in: including the excluded<br />
at the end of life. In: Payne S, Seymour J, Ingleton C (Eds).<br />
Palliative Care Nursing: Principles and Evidence for Practice<br />
<strong>London</strong>: Open University Press <strong>2004</strong>;pp364-384<br />
58.KOFFMAN J, HIGGINSON IJ. Equal access in palliative<br />
care. In: Sykes N, EDMONDS PM, Wiles J (Eds). Management<br />
of Advanced Disease 4th Edition. <strong>London</strong>: Arnold Publishers<br />
<strong>2004</strong>; pp461-470<br />
59. MALIK FA, Hall EJ, EDMONDS P. The palliative<br />
management of raised intra-cranial pressure. In: BOOTH S,<br />
Bruera E (Eds). Palliative Care Consultations in Primary and<br />
Metastatic Brain Tumours Oxford: Oxford University Press<br />
<strong>2004</strong>;pp61-81<br />
60. SPECK PW. Spiritual Concerns. In: Sykes N, EDMONDS<br />
PM, Wiles J, (Eds). Management of Advanced Disease.<br />
<strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>; pp471-481<br />
61. Swann D, EDMONDS PM. Dysphagia. In: Sykes N,<br />
EDMONDS PM, Wiles J, (Eds). Management of Advanced<br />
Disease. <strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>; pp136-145<br />
62. Swann D, EDMONDS PM. Sweating. In: EDMONDS PM,<br />
Sykes N, Wiles J, (Eds). Management of Advanced Disease.<br />
<strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>; pp213-218<br />
63. Swann D, EDMONDS PM. The Management of Urinary<br />
Symptoms. In: Sykes N, EDMONDS PM, Wiles J, (Eds).<br />
Management of Advanced Disease. <strong>London</strong>: Arnold Publishers.<br />
4th Edition. <strong>2004</strong>; pp219-224<br />
64. Thorns A, EDMONDS PM. Pruritis. In: Sykes N,<br />
EDMONDS PM, Wiles J, (Eds). Management of Advanced<br />
Disease. <strong>London</strong>: Arnold Publishers. 4th Edition. <strong>2004</strong>; pp206-<br />
213<br />
65. Wiles J, Rutter D, Exton L, Carey I, EDMONDS PM, Sykes<br />
N. Management of Pain. In: Sykes N, EDMONDS PM, Wiles J,<br />
(Eds). Management of Advanced Disease. <strong>London</strong>: Arnold<br />
Publishers. 4th Edition. <strong>2004</strong>; pp176-205<br />
REPORTS<br />
66. Burt J, SHIPMAN C, ADDINGTON-HALL JM. Cancer and<br />
palliative care within primary care: a review of the recent<br />
literature. Report for Macmillan Cancer Relief. February <strong>2004</strong>.<br />
Department of Palliative Care and Policy, King’s <strong>College</strong><br />
<strong>London</strong><br />
67. DAVIES E. What are the palliative care needs of older<br />
people and how might they be met? WHO Regional Office for<br />
Europe’s Health Evidence Network. August <strong>2004</strong>. http://www.<br />
euro.who.int/document/E83747.pdf<br />
68. GYSELS M, HIGGINSON IJ. Improving supportive and<br />
palliative care for adults with cancer: Research Evidence.<br />
National <strong>Institute</strong> for Clinical Excellence. <strong>2004</strong> http://www.nice.<br />
org.uk/pdf/csgspresearchevidence.pdf<br />
69. HARDING R, HIGGINSON IJ. Palliative care in Sub-<br />
Saharan Africa. An appraisal. The Diana, Princess of Wales<br />
Memorial Fund. <strong>2004</strong>. http://www.theworkcontinues.org/<br />
causes/pall_library.asp<br />
70. HARDING R. Palliative care in Sub-Saharan Africa. AIDS<br />
Treatment Update. <strong>2004</strong> http://www.nam.org.uk/en/docs/<br />
9FBC7A1D-5D5E-4655-AC9B-1A6E2DE8E2DE.asp<br />
71. LOWTON K, HIGGINSON IJ, Thomas J, Jones C, Kraus F,<br />
Monroe B. Supporting bereaved students in primary and<br />
secondary schools. King’s <strong>College</strong> <strong>London</strong> and National<br />
Council for Hospice and Specialist Palliative Care Services.<br />
<strong>2004</strong><br />
72. Ross JR, <strong>Saunders</strong> Y, EDMONDS PM, Patel S, Wonderling D,<br />
Normand C, Broadley K. A Systematic review of the role of<br />
bisphosphonates in metastatic disease. Health Technology<br />
Assessment. NHS R&D HTA Programme. Health Technology<br />
Assessment <strong>2004</strong>;8 http://www.ncchta.org/fullmono/mon804.pdf<br />
73. Tyerman A, Meehan M (TURNER-STOKES L Ed)<br />
Vocational assessment and rehabilitation after acquired brain<br />
injury: Inter-agency Guidelines. Prepared in collaboration with<br />
Jobcentre Plus, British Society of Rehabilitation Medicine.<br />
Royal <strong>College</strong> of Physicians, <strong>2004</strong><br />
40
RESEARCH LETTERS<br />
74. ALLOWAY L, BURT J, HARDING R, HIGGINSON IJ.<br />
Study of white coat effect on the prognosis of women with<br />
breast cancer. European Journal of Cancer Care <strong>2004</strong>;13:193<br />
75. Cartledge P, HARDING R, Mpanga Sebuyira L,<br />
HIGGINSON IJ. Prevalence, severity, duration and<br />
measurement of pain in Sub-Saharan Africa. Palliative<br />
Medicine <strong>2004</strong>;18:737-738<br />
PUBLICATIONS IN OTHER JOURNALS<br />
76. EDMONDS PM. Organization of palliative care services.<br />
Medicine <strong>2004</strong>;32:2-3<br />
77. EDMONDS PM, BURMAN R, Sinnott C. The goldfish bowl.<br />
European Journal of Palliative Care <strong>2004</strong>;11;69-71<br />
78. HARDING R, Mwangi-Powell F. The role of advocacy in<br />
expanding palliative care. African Palliative Care Association<br />
Journal of Palliative Care <strong>2004</strong>;1:24-25<br />
79. HARDING R. AIDS in Africa (2nd Edition) by Essex M,<br />
Mboup S, Kanki PH, Marlink RG (Eds). AIDS Care <strong>2004</strong>:16:132-<br />
133. Book Review<br />
80. HIGGINSON IJ. Effectiveness in palliative care: gathering the<br />
evidence. Beyond the randomised trial: evidence and effectiveness<br />
in palliative care. Report of a conference of the Scottish<br />
Partnership for Palliative Care 10 September 2003 <strong>2004</strong>;7-9<br />
81. Lowton K, HIGGINSON IJ. Bereavement in the classroom.<br />
European Journal of Palliative Care <strong>2004</strong>;11:28-31<br />
82. MURTAGH FEM, Preston M, HIGGINSON IJ. Patterns of<br />
dying: palliative care for non-malignant disease. Clinical<br />
Medicine <strong>2004</strong>;4:39-44<br />
83. Ramsdale DR, TURNER-STOKES L. Prophylaxis and<br />
treatment of infective endocarditis in adults: a concise guide.<br />
Clinical Medicine <strong>2004</strong>;4:545-550<br />
84. TURNER-STOKES L. The evidence for the cost-effectiveness<br />
of rehabilitation following acquired brain injury. Clinical<br />
Medicine <strong>2004</strong>;4:10-12<br />
85. TURNER-STOKES L, WADE D. Rehabilitation following<br />
acquired brain injury: concise guidance. Clinical Medicine<br />
<strong>2004</strong>;4:61-65<br />
PUBLISHED ABSTRACTS<br />
86. Ali S, Sykes N, Hall E, Buchan J, Lowton K, Emmitt K.<br />
The prevalence of MRSA in a hospice. Palliative Medicine<br />
<strong>2004</strong>;18:160<br />
87. ALLOWAY L, Brayden P, Gleeson C. Out-of-hours<br />
specialist palliative care: a prospective study of calls<br />
concerning patient care. Palliative Medicine <strong>2004</strong>;18:154<br />
88. ALLOWAY L, Minton O. The accuracy of the clinical<br />
prediction of survival: a comparison of doctors and nurses<br />
estimations and the failure to validate the palliative prognostic<br />
(PAP) score in a hospice. Palliative Medicine <strong>2004</strong>;18:155<br />
89. ARMES J, ADDINGTON-HALL JM, Hotopf M. A<br />
systematic review of nonpharmacological interventions for<br />
cancer-related fatigue. Palliative Medicine <strong>2004</strong>;18:150<br />
90. BARCLAY SIG, Todd C, McCabe J, Ewing G, Rogers M,<br />
ADDINGTON-HALL JM. How accurate are GP’s prognostic<br />
estimates? Palliative Medicine <strong>2004</strong>;18:155-156<br />
91. BURMAN R, VIVAT B, EDMONDS PM, Silber E,<br />
HIGGINSON IJ. Palliative care needs of people severely<br />
affected by multiple sclerosis (MS): views of healthcare<br />
professionals. Palliative Medicine <strong>2004</strong>;18:163<br />
92. BURT J, ADDINGTON-HALL JM, SHIPMAN C,<br />
Richardson A, Ream E, Beynon T. Out-of-hours care in the last<br />
months of life: the needs of cancer and noncancer patients.<br />
Palliative Medicine <strong>2004</strong>;18:157-158<br />
93. BURT J, ADDINGTON-HALL JM, SHIPMAN C,<br />
Richardson A, Ream E. Is access to community nursing for<br />
palliative care patients equitable? Palliative Medicine<br />
<strong>2004</strong>;18:368<br />
94. BURT J, ADDINGTON-HALL JM, SHIPMAN C,<br />
Richardson A, Beynon T. Postal questionnaires to bereaved<br />
carers – are they still feasible and ethical in England? Palliative<br />
Medicine <strong>2004</strong>;18:387-388<br />
95. Grande G, FARQUHAR MC, BARCLAY SIG, Todd CJ.<br />
Changes in informal carers’ retrospective evaluations of<br />
palliative care. Palliative Medicine <strong>2004</strong>;18:388<br />
96. GYSELS M, HIGGINSON IJ. Gaps and pitfalls in collating<br />
the evidence for policy on service delivery in supportive and<br />
palliative care. Palliative Medicine <strong>2004</strong>;18:352<br />
97. GYSELS M, HIGGINSON IJ, Richardson A. Communicatietraining<br />
voor gezondheidswerkers die zorgen voor patienten<br />
met gevorderde kanker: een systematische review. Nederlands<br />
Tijdschrift voor Palliative Zorg <strong>2004</strong>;4:91<br />
98. JACKSON D, Horn S, Kersten P, WILLIAMS H, TURNER-<br />
STOKES L. Stroke patients’ experiences of shoulder pain.<br />
Clinical Rehabilitation <strong>2004</strong>;18:931<br />
99. KOFFMAN J, HIGGINSON IJ, DONALDSON N. Outcomes<br />
of bereavement among relatives or close friends of deceased<br />
first generation Caribbean and native-born white patients with<br />
advanced disease: does ethnicity matter? Palliative Medicine<br />
<strong>2004</strong>;18:152-153<br />
100. KOFFMAN J, HIGGINSON IJ. Multi-professional palliative<br />
care education: does it make a difference? Palliative Medicine<br />
<strong>2004</strong>;18:351-352<br />
101. PAYNE JA, HIGGINSON IJ. Resuscitation preferences of<br />
terminally ill patients: influencing factors and stability over time:<br />
a systematic review. Palliative Medicine <strong>2004</strong>;18:166<br />
102. POTTER J, HIGGINSON IJ, Quigley C, Scadding J. Pain<br />
experienced by patients attending a diabetes outpatient clinic:<br />
prevalence, severity and impact on psychosocial function.<br />
Palliative Medicine <strong>2004</strong>;18:163<br />
103. Robinson V, George R, SPECK PW. Examining qualitative<br />
research systematically: a way of evaluating the rigour and<br />
quality of papers on spiritual care. Palliative Medicine<br />
<strong>2004</strong>;18:355<br />
41
104. SALEEM T, HUGHES RA, ADDINGTON-HALL JM.<br />
Assessing cultural acceptability, sensitivity and appropriateness<br />
of translated versions of palliative care evaluations in<br />
south Asian communities. Palliative Medicine <strong>2004</strong>;18:152<br />
105. SHIPMAN C, ADDINGTON-HALL J, Richardson A,<br />
BURT J, Ream E, Beynon T. 24-hour district nursing services<br />
for palliative care patients: the challenge for cancer networks.<br />
Palliative Medicine <strong>2004</strong>;18:153-154<br />
106. SHIPMAN C, DONALDSON N, Richardson A, ADDING-<br />
TON-HALL JM, BURT J, Beynon T. Does palliative care<br />
education impact on district nursing confidence? Palliative<br />
Medicine <strong>2004</strong>;18:162<br />
107. SHIPMAN C, Richardson A, BURT J, Ream E. When<br />
randomised controlled trials are not possible – design issues<br />
from a national evaluation. Palliative Medicine <strong>2004</strong>;18:312<br />
108. SHIPMAN C, Richardson A, ADDINGTON-HALL JM,<br />
BURT J, Beynon T. Evaluating a community nurse palliative<br />
care educational programme: the views of family doctors.<br />
Palliative Medicine <strong>2004</strong>;18:361<br />
109. Todd C, Ewing G, Rogers M, BARCLAY SIG, McCabe A,<br />
Martin J. A symptom measure for palliative care in the<br />
community: CAMPAS-R. Palliative Medicine <strong>2004</strong>;18:309<br />
110. TURNER-STOKES L, Kalmus M, Clegg F. Validity of the<br />
DISCs - a simple screening tool for depression in patients<br />
following acquired brain injury. Archives of Physical Medicine<br />
and Rehabilitation <strong>2004</strong>;85:6<br />
111. TURNER-STOKES L, Kalmus M, Clegg F. Sensitivity to<br />
change of the depression intensity scale circles: A simple rating<br />
scale for depression in patients after brain injury. Archives of<br />
Physical Medicine and Rehabilitation <strong>2004</strong>; 85:14-15<br />
112. VIVAT B, EDMONDS PM, BURMAN R, Silber E,<br />
HIGGINSON IJ. Developing a palliative care and neurological<br />
service for people severely affected by multiple sclerosis (MS)<br />
in southeast <strong>London</strong>. Palliative Medicine <strong>2004</strong>;18:337<br />
113. VIVAT B, BURMAN R, EDMONDS PM, Silber E,<br />
HIGGINSON IJ. Palliative care needs of people severely<br />
affected by multiple sclerosis (MS): views of people with MS<br />
and their informal carers. Palliative Medicine <strong>2004</strong>;18:158<br />
OTHER MEETING ABSTRACTS<br />
114. Bensley J, Corrigan N, HARDING R. The biology of<br />
transmission: outcomes from a national groupwork program.<br />
XV International AIDS Conference. Bangkok, <strong>2004</strong>.<br />
115. BURT J, ADDINGTON-HALL JM, SHIPMAN C,<br />
Richardson A, BEYNON T. Postal questionnaires to bereaved<br />
carers – are they still feasible and ethical in England. Oral<br />
Presentation. 3rd Research Forum of the European Association<br />
for Palliative Care Stresa, Italy, June <strong>2004</strong><br />
116. BURT J, ADDINGTON-HALL JM, SHIPMAN C,<br />
Richardson A, Ream E. Is access to community nursing for<br />
palliative care patients equitable? Poster presentation. 3rd<br />
Research Forum of the European Association for Palliative Care<br />
Stresa, Italy, June <strong>2004</strong><br />
117. BURT J, ADDINGTON-HALL JM, SHIPMAN C,<br />
Richardson A, Ream E, Beynon T. Out-of-hours care in the last<br />
months of life: the needs of cancer and non-cancer patients.<br />
Oral Presentation. 5th Palliative Care Congress, University of<br />
Warwick, March <strong>2004</strong><br />
118. Francis HP, WADE DT, TURNER-STOKES L, Kingswell<br />
RS, Dott CS, Coxon EA. Does reducing spasticity translate into<br />
functional benefit? An exploratory meta-analysis. Poster<br />
presentation: 14th European Congress in Physical and<br />
Rehabilitation Medicine, Vienna, May <strong>2004</strong><br />
119. Pahl N, HARDING R, Smith P. Informal carers in palliative<br />
care: underserved and overlooked. 15th International<br />
Conference on Care of the Terminally Ill, Montreal, <strong>2004</strong>.<br />
120. SHIPMAN C, ADDINGTON-HALL JM, Richardson A, BURT<br />
J, Ream E. When randomised controlled trials are not possible –<br />
design issues from a national evaluation. Oral presentation. 3rd<br />
Research Forum of the European Association for Palliative Care<br />
Stresa, Italy, June <strong>2004</strong><br />
121. SHIPMAN C, ADDINGTON-HALL JM, Richardson A, BURT<br />
J, Beynon T. Evaluating a community nurse palliative care<br />
educational programme: the views of family doctors. Poster<br />
presentation. 3rd Research Forum of the European Association<br />
for Palliative Care, Stresa, Italy, June <strong>2004</strong><br />
122. SHIPMAN C, ADDINGTON-HALL JM, Richardson A, BURT<br />
J, Ream E, Beynon T. 24 hour district nursing services for<br />
palliative care patients – the challenge for cancer networks.<br />
Oral Presentation. 5th Palliative Care Congress, University of<br />
Warwick, March <strong>2004</strong><br />
123. SHIPMAN C, DONALDSON N, Richardson A,<br />
ADDINGTON-HALL JM, BURT J, Beynon T. Does palliative<br />
care education impact on district nursing confidence? Poster<br />
presentation. 5th Palliative Care Congress, University of<br />
Warwick, March <strong>2004</strong>.<br />
124. TURNER-STOKES L, WILLIAMS H, Paul S. The cost<br />
efficiency of rehabilitation in severe complex brain injury.<br />
Poster Presentation. 14th European Congress in Physical and<br />
Rehabilitation Medicine, Vienna, May <strong>2004</strong><br />
125. TURNER-STOKES L. Being an effective expert witness.<br />
Oral Presentation. Royal Society of Medicine Section of<br />
Urology, Winter meeting, Beaver Creek, Colorado, April <strong>2004</strong><br />
126. TURNER-STOKES L. Assessment of shoulder pain<br />
following stroke. sensitivity of the ShoulderQ. Oral Presentation:<br />
14th European Congress in Physical and Rehabilitation<br />
Medicine, Vienna, May <strong>2004</strong><br />
127. TURNER-STOKES L, ASHFORD S, Nyein K. Goal<br />
attainment scaling to detect functional gains from botulinum<br />
toxin injection for management of the spastic upper limb.<br />
Poster Presentation: 14th European Congress in Physical and<br />
Rehabilitation Medicine, Vienna, May <strong>2004</strong><br />
128. Wolf RC, Butler M, de Lister M, Weise G, Placenia F,<br />
Pappas G, HARDING R, van Praag E, Marconi KM. Piloting<br />
palliative care assessment methods in the Dominican Republic.<br />
XV International AIDS Conference, Bangkok, <strong>2004</strong>.<br />
42
PUBLICATIONS - 2005<br />
PAPERS IN SCIENTIFIC JOURNALS<br />
129. ADDINGTON-HALL JM, Karlsen S. A national survey of<br />
health professionals and volunteers working in voluntary hospice<br />
services in the UK. I. Attitudes to current issues affecting<br />
hospices and palliative care. Palliative Medicine 2005;19:40-48<br />
130. ADDINGTON-HALL JM, Karlsen S. A national survey of<br />
health professionals and volunteers working in voluntary<br />
hospices in the UK. II. Staff and volunteers’ experiences of<br />
working in hospices. Palliative Medicine 2005;19:49-57<br />
131. ASHFORD S. Why is the functional independence<br />
measure used to identify some rehabilitation needs in stroke<br />
survivors when there are better tools? Physiotherapy Research<br />
International 2005;10:182-184<br />
132. BAUSEWEIN C, Fegg M, Radbruch L, Nauck F, von<br />
Mackensen S, Borasio GD, HIGGINSON IJ. Validation and<br />
clinical application of the German version of the Palliative Care<br />
Outcome Scale (POS). Journal of Pain and Symptom<br />
Management 2005;30:51-62<br />
133. BURT J, SHIPMAN C. Palliative care: challenges in caring<br />
for dying people. British Journal of Nursing 2005;14:306<br />
134. Catt S, Blanchard M, ADDINGTON-HALL JM, J, Zis M,<br />
Blizard R, King M. Older adults’ attitudes to death, palliative<br />
treatment and hospice care. Palliative Medicine 2005;19:402-410<br />
135. Catt S, Blanchard M, ADDINGTON-HALL JM, Zis M,<br />
Blizard B, King M. The development of a questionnaire to<br />
assess the attitudes of older people to end-of-life issues<br />
(AEOLI). Palliative Medicine 2005;19:397-401<br />
136. Disler P, TURNER-STOKES L, WADE DT, Sackley C.<br />
Rehabilitation interventions for footdrop in neuromuscular<br />
disease (Protocol for a Cochrane Review 2002). The Cochrane<br />
Library <strong>2004</strong>; Issue 2. Oxford: Update Software<br />
137. DAVIES E, HIGGINSON IJ. Systematic review of specialist<br />
palliative day-care for adults with cancer. Supportive Care in<br />
Cancer 2005;13:607-627<br />
138. Douglas H-R, Normand C, HIGGINSON IJ, Goodwin D. A<br />
new approach to eliciting patients’ preferences for palliative<br />
day care: the choice experiment method. Journal of Pain and<br />
Symptom Management 2005:29:435-445<br />
139. Dunckley M, Aspinal F, ADDINGTON-HALL JM, HUGHES<br />
R, HIGGINSON IJ. A research study to identify facilitators and<br />
barriers to outcome measure implementation. International<br />
Journal of Palliative Nursing 2005:11:218 - 225<br />
140. EDMONDS PM, Rogers A, ADDINGTON-HALL JM,<br />
McCoy A, Coats AJS, Gibbs SR. Patient descriptions of<br />
breathlessness in heart failure. International Journal of<br />
Cardiology 2005;98:61-66<br />
141. Elkington H, White P, ADDINGTON-HALL JM, Higgs R,<br />
EDMONDS PM. The healthcare needs of chronic obstructive<br />
pulmonary disease patients in the last year of life. Palliative<br />
Medicine 2005;19:485-491<br />
142. FARQUHAR MC, BARCLAY SIG, Earl H, Grande GE,<br />
Emery J, Crawford RAF. Barriers to effective communication<br />
across the primary/secondary interface: examples from the<br />
ovarian cancer patient journey (a qualitative study). European<br />
Journal of Cancer 2005;14:359-366<br />
143. GYSELS M, HIGGINSON IJ, Richardson A. Communication<br />
training for health professionals who care for patients with<br />
cancer: a systematic review of training methods. Supportive<br />
Care in Cancer 2005;13:356-366<br />
144. GYSELS M, Pool R, Nyanzi R. The adventures of the randy<br />
professor and Angela the sugar mummy: sex in fictional series<br />
in Ugandan popular magazines. AIDS Care 2005;17:967-977<br />
145. HALL S, Vogt F, Marteau TM. A short report: Survey of<br />
practice nurses’ attitudes towards giving smoking cessation<br />
advice. Family Practice 2005;22:614-616<br />
146. HARDING R, Karus D, Easterbrook P, Raveis VH,<br />
HIGGINSON IJ, Marconi K. Does palliative care improve<br />
outcomes for patients with HIV/AIDS? A systematic review of<br />
the evidence. Sexually Transmitted Infections 2005;81:5-14<br />
147. HARDING R, Easterbrook P, HIGGINSON IJ, Karus D,<br />
Raveis V, Marconi K. Access and equity in HIV/AIDS palliative<br />
care: a review of the evidence and responses. Palliative<br />
Medicine 2005;19:251-258<br />
148. HARDING R, HIGGINSON IJ. Palliative Care in Sub-<br />
Saharan Africa. The Lancet 2005:365:1971-1978<br />
149. HARDING R, Leam C. Clinical notes for informal carers in<br />
palliative care: recommendations from a random patient file<br />
audit. Palliative Medicine 2005;19:639-642<br />
150. HIGGINSON IJ, KOFFMAN J. Public health and palliative<br />
care. Clinics in Geriatric Medicine 2005;21:45-55<br />
151. HIGGINSON IJ. End-of-life care: lessons from other<br />
nations. Journal of Palliative Medicine 2005;8:S161-S173<br />
152. HUGHES RA, Sinha A, HIGGINSON IJ, Down K, Leigh<br />
PN. Living with motor neurone disease: lives, experiences of<br />
services and suggestions for change. Health and Social Care in<br />
the Community 2005;13:64-74<br />
153. HUGHES RA, SALEEM T, ADDINGTON-HALL JM.<br />
Towards a culturally acceptable end-of-life survey questionnaire:<br />
a Bengali translation of VOICES. International Journal of<br />
Palliative Nursing 2005;11:116-123<br />
154. HUGHES RA, Addington-Hall JM. Feeding back survey<br />
research findings within palliative care. Findings from<br />
qualitative research. International Journal of Nursing Studies<br />
2005;42:449-456<br />
155. KOFFMAN J, HIGGINSON IJ. Assessing the effectiveness<br />
and acceptability of interprofessional palliative care<br />
education. Journal of Palliative Care 2005;21:262-269<br />
156. KOFFMAN J, DONALDSON N, Hotopf M, HIGGINSON<br />
IJ. Does ethnicity matter? Bereavement outcomes in two<br />
ethnic groups living in the United Kingdom. Palliative and<br />
Supportive Care 2005;3:183-190<br />
157. Lock A, HIGGINSON IJ. Patterns and predictors of place<br />
of cancer death for the oldest old. BMC Palliative Care 2005;4:6<br />
43
158. Logie DE, HARDING R. An evaluation of a morphine<br />
public health programme for cancer and AIDS pain relief in<br />
sub-Saharan Africa. BMC Public Health 2005;5:82<br />
159. MAGEE WL. Music therapy with patients in low<br />
awareness states: assessment and treatment approaches in<br />
multidisciplinary care. Neuropsychological Rehabilitation<br />
2005;15:522-536.<br />
160. Rajasekaran M, EDMONDS PM, HIGGINSON IJ.<br />
Systematic review of hypnotherapy for treating symptoms in<br />
terminally ill adult cancer patients. Palliative Medicine<br />
2005;19:418-426<br />
161. ROGERS A, ADDINGTON-HALL JM. Care of the dying<br />
stroke patient in the acute setting. Journal of Research in<br />
Nursing 2005;10:153-167<br />
162. SHIPMAN C, ADDINGTON-HALL JM, Richardson A,<br />
BURT J, Ream E, Beynon T. Palliative care services in England:<br />
a survey of district nurses’ views. British Journal of Community<br />
Nursing 2005;10:381-386<br />
163. Thomas VN, SALEEM T, Abraham R. Barriers to effective<br />
uptake of cancer screening among black and minority ethnic<br />
groups. International Journal of Palliative Nursing 2005:11:562-571<br />
164. TURNER-STOKES L, Kalmus M, Hirani D, Clegg F. The<br />
Depression Anxiety Scale Circles (DISCs): a first evaluation of a<br />
simple assessment tool for depression in the context of brain<br />
injury. Journal of Neurology, Neurosurgery and Psychiatry<br />
2005:76:1273-1278<br />
165. TURNER-STOKES L, Disler PB, Nair A, WADE DT. Multidisciplinary<br />
rehabilitation for acquired brain injury in adults of<br />
working age. The Cochrane Database of Systematic Reviews<br />
2005:Issue 3;1-30<br />
166. TURNER-STOKES L. Evaluation of the evidence for<br />
rehabilitation following acquired brain injury. Brain Impairment<br />
2005;6:161-168<br />
167. TURNER-STOKES L. The national service framework for<br />
long term conditions: a novel approach for a “new style” NSF.<br />
Journal of Neurology, Neurosurgery and Psychiatry<br />
2005:76;901-902<br />
168. Vejlgaard T, ADDINGTON-HALL JM. Attitudes of Danish<br />
doctors and nurses to palliative and terminal care. Palliative<br />
Medicine 2005;19:119-127<br />
169. Vogt F, HALL S, Marteau TM. General practitioners’ and<br />
family physicians’ negative beliefs and attitudes towards<br />
discussing smoking cessation with patients: a systematic<br />
review. Addiction 2005;100:1223-1231<br />
BOOK CHAPTERS<br />
170. ASHFORD S, McIntyre A, Minns T. Body structures and<br />
body functions: Part 1. In: McIntyre A, Atwal A (Eds). Occupational<br />
Therapy and Older People. Blackwell Publishing Ltd:<br />
Oxford 2005, pp105-129<br />
171. HARDING R. Carers – current research and developments.<br />
In: Olivier D, Luft G (Eds). Loss Change and<br />
Bereavement in Palliative Care. Open University Press:<br />
Maidenhead. 2005, pp15-166<br />
172. KOFFMAN J, HIGGINSON IJ. Rights, needs and social<br />
exclusion at the end of life. In: Faull C, Carter Y, Daniels L (Eds).<br />
Handbook of Palliative Care 2nd Edition. Blackwell Publishing:<br />
<strong>London</strong> 2005. pp43-60<br />
173. MAGEE WL. Music therapy with patients in low<br />
awareness states: assessment and treatment approaches in<br />
multidisciplinary care. In: Coleman M (Ed). The Assessment<br />
and Rehabilitation of Vegetative and Minimally Conscious<br />
Patients. Psychology Press: <strong>London</strong> 2005. pp522-536.<br />
174. MAGEE WL. Vokalimprovisation zur Förderung<br />
nonverbaler Interaktion. In: Jochims S (Ed). Musiktherapie in<br />
der Neurologie / Neurorehabilitation. Erwachsener: Weltweite<br />
Konzepte, Forschung und Praxis. Hippocampus Verlag KG:<br />
Bad Honnef, Germany 2005. pp252-256.<br />
175. MAGEE, WL. Sprachrehabilitation durch Singtechniken.<br />
In: Jochims S (Ed). Musiktherapie in der Neurologie / Neurorehabilitation.<br />
Erwachsener: Weltweite Konzepte, Forschung und<br />
Praxis. Hippocampus Verlag KG: Bad Honnef, Germany 2005.<br />
pp 285-291.<br />
176. MAGEE WL, Davidson JW. Beeinflussung der Stimmung<br />
durch Musictherapie bei neurologishcen Patienten – Eine<br />
Pilotstudie. In: Jochims S (Ed). Musiktherapie in der Neurologie<br />
/ Neurorehabilitation. Erwachsener: Weltweite Konzepte,<br />
Forschung und Praxis. Hippocampus Verlag KG: Bad Honnef,<br />
Germany 2005. pp355-363.<br />
177. MAGEE WL. Angesichts der Progression von Chorea<br />
Huntington. In: Jochims S (Ed). Musiktherapie in der Neurologie<br />
/ Neurorehabilitation. Erwachsener: Weltweite Konzepte,<br />
Forschung und Praxis. Hippocampus Verlag KG: Bad Honnef,<br />
Germany 2005. pp 323-336.<br />
178. MURTAGH FEM, BURMAN R, EDMONDS PM. Breathlessness<br />
in neurological disease. In: BOOTH S, Dudgeon D<br />
(Eds). Dyspnoea in Advanced Disease: A Guide to Clinical<br />
Management Oxford University Press: Oxford 2005. pp 99-112<br />
RESEARCH LETTERS<br />
179. ASHFORD S. Why is the functional independence<br />
measure used to identify some rehabilitation needs in stroke<br />
survivors when there are better tools? Physiotherapy Research<br />
International 2005;10:57-58<br />
180. HARDING R, Easterbrook P, Dinat N, HIGGINSON IJ. Pain<br />
and symptom control in HIV disease: under-researched and<br />
poorly managed. Clinical Infectious Diseases 2005;40:491-492<br />
181. Henderson M, ADDINGTON-HALL JM, Hotopf M. The<br />
willingness of palliative care patients to participate in research.<br />
Journal of Pain and Symptom Management 2005;29:116-118<br />
44
182. MURTAGH FEM, Thorns A. Taking an ‘ethics history’.<br />
Journal of the Royal Society of Medicine 2005;98:442-443<br />
183. Oliver D, MURTAGH FEM, Jusic A. Palliative care in<br />
Croatia: an international collaboration. European Journal of<br />
Palliative Care 2005;12:127-129 Commentary<br />
184. Senyimba C, Mwebesa E, Kennelly S, Frame K, HARDING<br />
R. A theme issue by, for, and about Africa. Palliative care and<br />
antiretroviral treatment can be integrated. British Medical<br />
Journal 2005;331:778-779<br />
REPORTS<br />
185. BURT J, SHIPMAN C, ADDINGTON-HALL JM, White P.<br />
Palliative care. Perspectives on caring for dying people in<br />
<strong>London</strong>. <strong>London</strong>, King’s Fund. 2005<br />
186. Down K, HUGHES RA, Sinha A, HIGGINSON IJ Leigh<br />
PN. Involving users in shaping motor neurone disease services.<br />
Joseph Rowntree Foundation. 2005<br />
187. FARQUHAR M, BARCLAY SIG, Corrie P, Wilson C, Emery<br />
J and Sutton S. The transition from hospital to community for<br />
the final stage of the colo-rectal cancer patient journey:<br />
passing on the baton. Report to the Addenbrooke’s Charities.<br />
GPPCRU, University of Cambridge. 2005<br />
188. Lowton K. Relatives’ experiences of care given to young<br />
people who have died from cystic fibrosis. Final report to The<br />
<strong>Cicely</strong> <strong>Saunders</strong> Foundation. King’s <strong>College</strong> <strong>London</strong>. 2005.<br />
189. TURNER-STOKES L. Concise guidance for the use of antidepressant<br />
medication in adults undergoing recovery or<br />
rehabilitation following acquired brain injury. Prepared in<br />
collaboration the British Society of Rehabilitation Medicine, British<br />
Geriatrics Society. Royal <strong>College</strong> of Physicians, <strong>London</strong>. 2005<br />
PUBLICATIONS IN OTHER JOURNALS<br />
190. Cartledge P, Clausen S, HARDING R, Mpanga-Sebuyira<br />
L. A pilot study: the use of paediatric faces pain scales to<br />
assess pain in adults in a Sub-Saharan hospice. Palliative Care<br />
Association of Uganda Journal of Palliative Care 2005;7:14-18<br />
191. HIGGINSON IJ. The state of play. Cancer Nursing Practice<br />
2005;4(Supp):4<br />
192. TURNER-STOKES L, MacWalter R. Use of antidepressant<br />
medication following acquired brain injury: concise<br />
guidance. Clinical Medicine 2005;5:268-274<br />
193. TURNER-STOKES L, Whitworth D. The National Service<br />
Framework for Long Term Conditions: the challenges ahead.<br />
Clinical Medicine 2005:5;203-206<br />
PUBLISHED ABSTRACTS<br />
194. De Lima L, HARDING R, Pereira J, Norval D. Palliative<br />
Care Research and Education in the Developing World: Is It<br />
Possible? European Journal of Palliative Care 2005:EAPC<br />
195. GOMES B, HIGGINSON IJ. Factors affecting the place<br />
where cancer patients die: a systematic review. European<br />
Journal of Palliative Care 2005:EAPC<br />
196. GOMES B, HARDING R, HIGGINSON IJ. Meeting<br />
existential needs at the end of life: a systematic review of<br />
interventions. European Journal of Palliative Care 2005:EAPC<br />
197. Grande G, FARQUHAR MC, BARCLAY SIG, Todd C.<br />
Patient access to palliative home care: the role of caregiver<br />
age. European Journal of Palliative Care 2005:EAPC<br />
198. GYSELS M, HIGGINSON IJ, Richardson A. Do patientheld<br />
records improve continuity in cancer and palliative care: a<br />
systematic review. European Journal of Palliative Care 2005:<br />
EAPC<br />
199. HARDING R, Leam C. The assessment and response to<br />
needs among informal carers: findings from a closed file audit.<br />
European Journal of Palliative Care 2005:EAPC<br />
200. HIGGINSON IJ, EDMONDS PM, VIVAT B, BURMAN R,<br />
Silber E. Do people with MS have palliative care needs?<br />
European Journal of Palliative Care 2005:EAPC<br />
201. HIGGINSON IJ. Audit in Palliative Care – does it work?<br />
European Journal of Palliative Care 2005:EAPC<br />
202. HIGGINSON IJ. Choosing the right research design.<br />
European Journal of Palliative Care 2005:EAPC<br />
203. HIGGINSON IJ. Response shift in studies assessing<br />
quality of life: should we abandon all measurement? European<br />
Journal of Palliative Care 2005:EAPC<br />
204. KOFFMAN J, HIGGINSON IJ. Do words matter? A<br />
systematic review of race, ethnicity and culture as variables in<br />
palliative care research. European Journal of Palliative Care<br />
2005:81 EAPC<br />
205. Lock A, HIGGINSON IJ. Place of death in advanced<br />
cancer among older people: A qualitative systematic literature<br />
review. European Journal of Palliative Care 2005:EAPC<br />
OTHER MEETING ABSTRACTS<br />
206. De Lima L, HARDING R, HIGGINSON IJ. Palliative care<br />
research in the developing world: how can we move forward?<br />
9th Congress of the European Association for Palliative Care.<br />
Aachen, 2005.<br />
207. HARDING R, Cartledge P, Mpanga–Sebuyira L, Clausen<br />
S. Pain and symptom prevalence and measurement: findings<br />
from an audit in a Ugandan Hospice. 7th International AIDS<br />
Impact Conference. Cape Town, 2005.<br />
208. SALEEM T, Hughes R, ADDINGTON-HALL JM (<strong>2004</strong>).<br />
Assessing the cultural acceptability, sensitivity and appropriateness<br />
of translated versions of palliative care evaluation<br />
surveys in South Asian communities. The 5th Palliative Care<br />
Congress abstracts, Warwick, March 2005.<br />
45
PUBLICATIONS - 2006<br />
PAPERS IN SCIENTIFIC JOURNALS<br />
209. ASHFORD S, TURNER-STOKES L. Goal attainment for<br />
spasticity management using botulinum toxin. Physiotherapy<br />
Research International 2006;11:24-34<br />
210. Aspinal F, HUGHES RA, Dunckley M, ADDINGTON-HALL<br />
JM. What is important to measure in the last months and<br />
weeks of life? A modified nominal group study. International<br />
Journal of Nursing Studies 2006;43:393-403<br />
211. BAUSEWEIN C, Kühnbach R, Haberland B. Adrenal<br />
insufficiency caused by bilateral adrenal metastases – a rare<br />
treatable cause for recurrent nausea and vomiting in metastatic<br />
breast cancer. Onkologie 2006;29:203-205<br />
212. BOOTH S, FARQUHAR MC, GYSELS M, BAUSEWEIN<br />
C, HIGGINSON IJ. The impact of a breathlessness intervention<br />
service (BIS) on the lives of patients with intractable dyspnea: A<br />
qualitative phase I study. Palliative and Supportive Care<br />
2006;4:287-293<br />
213. BOOTH S. Improving research methodology in breathlessness:<br />
a meeting convened by the MRC Clinical Trials Unit<br />
and The <strong>Cicely</strong> <strong>Saunders</strong> Foundation. Palliative Medicine<br />
2006;20:219-220<br />
214. Braun SM, Beurskens AJ, Borm PJ, Schack T, WADE DT.<br />
The effects of mental practice in stroke rehabilitation: a<br />
systematic review. Archives of Physical Medicine and Rehabilitation<br />
2006;87:842-852<br />
215. Bugge E, HIGGINSON IJ. Palliative care and the need for<br />
education – do we know what makes a difference? A limited<br />
systematic review. Health Education Journal 2006;65:101-125<br />
216. BURT J, SHIPMAN C, White P, ADDINGTON-HALL JM.<br />
Roles, service knowledge and priorities in the provision of<br />
palliative care: a postal survey of <strong>London</strong> GPs. Palliative<br />
Medicine 2006;20:487-492<br />
217. Casarett DJ, Teno J, HIGGINSON IJ. How should nations<br />
measure the quality of end-of-life care for older adults?<br />
Recommendations for an international minimum dataset.<br />
Journal of the American Geriatric Society 2006;54:1765-1771<br />
218. Dawes H, Scott OM, Roach NK, WADE DT. Exertional<br />
symptoms and exercise capacity in individuals with brain injury.<br />
Disability and Rehabilitation 2006;28:1243-1250<br />
219. Dawes H, Korpershoek N, Freebody J, Elsworth C, van<br />
Tintelen N, WADE DT, Izadi H, Jones DH. A pilot randomised<br />
controlled trial of a home-based exercise programme aimed at<br />
improving endurance and function in adults with neuromuscular<br />
disorders. Journal of Neurology, Neurosurgery and<br />
Psychiatry 2006;77:959-962<br />
220. Decker SL, HIGGINSON IJ. A tale of two cities: factors<br />
affecting place of cancer death in <strong>London</strong> and New York.<br />
European Journal of Public Health 2006:doi:10.1093/eurpub/<br />
ckl243<br />
221. EVANS AR, Wiggins RD, Mercer CH, Bolding GJ, Elford J.<br />
Men who have sex with men in Britain: comparison of a selfselected<br />
internet sample with a national probability sample.<br />
Sexually Transmitted Infections 2006;doi:10.1136/sti.<br />
s006.023383<br />
222. Farmer SA, HIGGINSON IJ. Chest pain: physician<br />
perceptions and decision making in a <strong>London</strong> emergency<br />
department. Annals of Emergency Medicine 2006;48:77-85<br />
223. Farmer SA, Roter DL, HIGGINSON IJ. Chest pain:<br />
communication of symptoms and history in a <strong>London</strong><br />
emergency department. Patient Education and Counseling<br />
2006;63:138-144<br />
224. Gage H, Kaye J, Owen C, Trend P, WADE DT. Evaluating<br />
rehabilitation using cost-consequences analysis: an example<br />
of Parkinson's disease. Clinical Rehabilitation 2006;20:232-238<br />
225. GOMES B, HIGGINSON IJ. Factors influencing death at<br />
home in terminally ill patients with cancer: systematic review.<br />
British Medical Journal 2006;332:515-521<br />
226. Grande G, FARQUHAR MC, BARCLAY SIG, Todd CJ.<br />
The influence of patient and carer age in access to palliative<br />
care services. Age and Ageing 2006;35:267-273<br />
227. HALL S, Reid E, Marteau TM. Attitudes towards sex<br />
selection for non-medical reasons: a review. Prenatal Diagnosis<br />
2006;26:619-626<br />
228. HALL S, Bishop AJ, Marteau TM. Does changing the<br />
order of threat and efficacy information influence the persuasiveness<br />
of threat messages? British Journal of Health<br />
Psychology 2006;11:333-43<br />
229. HARDING R, Molloy T, Easterbrook P, Frame K,<br />
HIGGINSON IJ. Is antiretroviral therapy associated with<br />
symptom prevalence and burden? International Journal of STD<br />
& AIDS 2006;17:400-405<br />
230. Harley C, Boyd JE, Cockburn J, Collin C, Haggard P,<br />
Wann JP, WADE DT. Disruption of sitting balance after stroke:<br />
influence of spoken output. Journal of Neurology, Neurosurgery<br />
and Psychiatry 2006;77:674-676<br />
231. HIGGINSON IJ, HART S, Silber E, BURMAN R,<br />
EDMONDS PM. Symptom prevalence and severity in people<br />
severely affected by Multiple Sclerosis. Journal of Palliative<br />
Care 2006;22:158-165<br />
232. HIGGINSON IJ, VIVAT B, Silber E, SALEEM T, BURMAN<br />
R, HART S, EDMONDS PM. Study protocol: delayed intervention<br />
randomised controlled trial within the Medical Research<br />
Council (MRC) Framework to assess the effectiveness of a new<br />
palliative care service. BMC Palliative Care 2006;5:7<br />
233. HUGHES RA, HIGGINSON IJ. Discussion of quality and<br />
audit in health. Journal of Health and Social Policy 2006;22:29-<br />
38<br />
234. JACKSON D, Horn S, Kersten P, TURNER-STOKES L.<br />
A pictorial scale of pain intensity (SPIN) for patients with<br />
communication impairments. International Journal of Therapy<br />
and Rehabilitation 2006;13:457-463<br />
46
235. Khan F, McPhail T, Brand C, TURNER-STOKES L,<br />
Kilpatrick T. Multiple sclerosis: disability profile and quality of<br />
life in an Australian community cohort. International Journal of<br />
Rehabilitation Research 2006;29:87-96<br />
236. KOFFMAN J. The language of diversity: controversies<br />
relevant to palliative care research. European Journal of<br />
Palliative Care 2006;13:18-21<br />
237. Low J, Cloherty M, Wilkinson S, BARCLAY SIG, Hibble A.<br />
A UK-wide postal survey to evaluate palliative care education<br />
amongst General Practice Registrars. Palliative Medicine<br />
2006;20;463-469<br />
238. MAGEE WL, Brumfitt SM, Freeman M, Davidson JW. The<br />
role of music therapy in an interdisciplinary approach to<br />
address functional communication in complex neurocommunication<br />
disorders: a case report. Disability and<br />
Rehabilitation 2006;28:1221-1229.<br />
239. Mpinga EK, Pennec S, GOMES B, Cohen J, HIGGINSON<br />
IJ, Wilson D, Rapin C-H. First International Symposium on<br />
places of death: an Agenda or the 21st Century. Journal of<br />
Palliative Care 2006;22:293-296<br />
240. MURTAGH FEM, ADDINGTON-HALL JM, Donohoe P,<br />
HIGGINSON IJ. Symptom management in patients with<br />
established renal failure managed without dialysis. EDTNA/<br />
ERCA Journal 2006;32:93-98<br />
241. MURTAGH FEM, Murphy E, Shepherd KA, Donohoe P,<br />
EDMONDS PM. End-of-life care in end-stage renal disease:<br />
renal and palliative care. British Journal of Nursing 2006;15:8-11<br />
242. MURTAGH FEM, Thorns A. Exploring patient preferences:<br />
evaluation of a tool to help clinicians explore patient<br />
preferences for information and involvement in decisions.<br />
Journal of Medical Ethics 2006;32:311-315<br />
243. Pappas G, Wolf RC, Morineau G, HARDING R. Validity of<br />
survey questionnaire items related to pain and symptoms in<br />
HIV/AIDS infected households in resources poor settings:<br />
results from Dominican Republic and Cambodia. BMC<br />
Palliative Care 2006;5:3<br />
244. Potter S, Leigh E, WADE DT, Fleminger S. The Rivermead<br />
Post Concussion Symptoms questionnaire. A confirmatory<br />
factor analysis. Journal of Neurology 2006;253:1603-1614<br />
245. Price A, Hotopf M, HIGGINSON IJ, Monroe B, Henderson<br />
M. Psychological services in hospices in the UK and Republic<br />
of Ireland. Journal of the Royal Society of Medicine<br />
2006;99:637-639<br />
246. Sackley C, WADE DT, Mant D, Atkinson JC, Yudkin P,<br />
Cardoso K, Levin S, Blanchard V, Reel K. Cluster randomized pilot<br />
controlled trial of an occupational therapy intervention for<br />
residents with stroke in UK care homes. Stroke 2006;37:2336-<br />
2341<br />
247. Saini T, MURTAGH FEM, Dupont PJ, McKinnon PM,<br />
Hatfield P, <strong>Saunders</strong> Y. Comparative pilot study of symptoms<br />
and quality of life in cancer patients and patients with end<br />
stage renal disease. Palliative Medicine 2006;20:631-636<br />
249. Smeets rjem, WADE DT, Hidding A, Van Leeuwen PJCM,<br />
Vlaeyen JWS, Knottnerus JA. The association of physical<br />
deconditioning and chronic low back pain: a hypothesisorientated<br />
systematic review. Disability and Rehabilitation<br />
2006;28:673-693<br />
250. Solano JP, GOMES B, HIGGINSON IJ. A comparison of<br />
symptom prevalence in far advanced cancer, AIDS, heart<br />
disease, chronic obstructive pulmonary disease (COPD), and<br />
renal disease. Journal of Pain and Symptom Management<br />
2006;31:58-69<br />
251. TURNER-STOKES L, Paul S, WILLIAMS H. Efficiency of<br />
specialist rehabilitation in reducing dependency and costs of<br />
continuing care for adults with complex acquired brain injuries.<br />
Journal of Neurology, Neurosurgery and Psychiatry<br />
2006;77:634-639<br />
252. TURNER-STOKES L, JACKSON D. Assessment of<br />
shoulder pain in hemiplegia: Sensitivity of the ShoulderQ.<br />
Disability and Rehabilitation 2006;28:389-395<br />
253. van den Berg M, Dawes H, WADE DT, Newman M,<br />
Burridge J, Izadi H, Sackley CM. Treadmill training for<br />
individuals with multiple sclerosis: a pilot randomised trial.<br />
Journal of Neurology, Neurosurgery and Psychiatry<br />
2006;77:531-533<br />
254. Vogt F, HALL S, Marteau TM. General practitioners’<br />
beliefs about effectiveness and intentions to prescribe smoking<br />
cessation medications: qualitative and quantitative studies.<br />
BMC Public Health 2006;6:277<br />
255. WADE DT, Makela PM, House H, Bateman C, Robson P.<br />
Long-term use of a cannabis-based medicine in the treatment<br />
of spasticity and other symptoms in multiple sclerosis. Multiple<br />
Sclerosis 2006;12:639-645<br />
256. WADE DT. Clinical Rehabilitation, past and future.<br />
Editorial. Clinical Rehabilitation 2006;20:1-3<br />
257. WADE DT. Why physical medicine, physical disability and<br />
physical rehabilitation? We should abandon Cartesian dualism.<br />
Editorial. Clinical Rehabilitation2006;20:185-190<br />
258. WADE DT. Rehabilitation omniana. Editorial. Clinical<br />
Rehabilitation 2006;20:1021-1022<br />
259. WADE DT. Rehabilitation in practice: a new section in<br />
Clinical Rehabilitation. Editorial. Clinical Rehabilitation<br />
2006;20:93-96<br />
260. Winkens I, Van Heugten C, Fasotti L, Duits AA, WADE DT.<br />
Manifestations of mental slowness in the daily life of patients<br />
with stroke: a qualitative study. Clinical Rehabilitation<br />
2006;20:827-834<br />
261. Wu HY, MALIK FA, HIGGINSON IJ. End of life content in<br />
geriatric textbooks: what is the current situation? BMC<br />
Palliative Care 2006;5:5<br />
248. Skinner A, TURNER-STOKES L. The use of standardized<br />
outcome measures in rehabilitation centres in the UK. Clinical<br />
Rehabilitation 2006;20:609-615<br />
47
BOOKS<br />
262. Bruera E, HIGGINSON IJ, Ripamonti C, von Gunten C<br />
(Eds). Textbook of Palliative Medicine. <strong>London</strong>: Hodder Arnold,<br />
2006<br />
BOOK CHAPTERS<br />
263. BURMAN R. Neurological diseases. In: Bruera E,<br />
HIGGINSON IJ, Ripamonti C, von Gunten C (Eds). Textbook of<br />
Palliative Medicine. <strong>London</strong>: Hodder Arnold. 2006, pp911-917<br />
264. Ford-Carleton P, Lugn N, Colquitt N, Reissig M,<br />
HIGGINSON IJ, Kvedar JC. Congestive heart failure. In:<br />
Wootton R, Dimmick SL, Kvedar JC (Eds). Home Telehealth:<br />
Connecting Welfare Within the Community. <strong>London</strong>: Royal<br />
Society of Medicine Press Ltd. 2006, pp184-197<br />
265. HIGGINSON IJ. Challenges of research in palliative<br />
medicine. In: Bruera E, HIGGINSON IJ, Ripamonti C, von<br />
Gunten C (Eds). Textbook of Palliative Medicine. <strong>London</strong>:<br />
Hodder Arnold. 2006, pp163-170<br />
266. HIGGINSON IJ, von Gunten CF. Population-based needs<br />
assessment for patient and family care. In: Bruera E,<br />
HIGGINSON IJ, Ripamonti C, von Gunten C (Eds). Textbook of<br />
Palliative Medicine. <strong>London</strong>: Hodder Arnold. 2006, pp251-258<br />
267. KOFFMAN J. Transcultural and ethnic issues at the end of<br />
life. In: Cooper J (Ed). Stepping Into Palliative Care 1: Relationships<br />
and Responses. 2nd Edition. Oxford: Radcliffe<br />
Publishing. 2006, pp171-186<br />
268. KOFFMAN J, MURTAGH FEM. Ethics in palliative care<br />
research. In: Bruera E, HIGGINSON IJ, Ripamonti C, von<br />
Gunten C (Eds). Textbook of Palliative Medicine. <strong>London</strong>:<br />
Hodder Arnold. 2006, pp192-201<br />
269. MALIK FA, HIGGINSON IJ. Quality of life at the end of<br />
life. In: Rose BD (Ed). UpToDate Wellesley, MA. 2006<br />
270. MAGEE WL, Wheeler B. Music Therapy for Patients with<br />
Traumatic Brain Injury. In: Murrey G (Ed). Alternative Therapies in<br />
the Treatment of Brain Injury and Neurobehavioural Disorders: A<br />
Practical Guide. NY: Haworth Press 2006, pp51-74.<br />
271. MURTAGH FEM, HIGGINSON IJ. Cancer neuropathic<br />
pain. In: Bennett M (Ed). Neuropathic Pain. Oxford Pain<br />
Management Library. Oxford: Oxford University Press. 2006,<br />
pp67-75<br />
272.Schaefer S, Murrey MA, MAGEE WL, Wheeler B. Melodic<br />
Intonation Therapy with Brain-Injured Patients. In: Murrey G<br />
(Ed). Alternative Therapies in the Treatment of Brain Injury and<br />
Neurobehavioural Disorders: A Practical Guide. NY: Haworth<br />
Press 2006, pp75-87.<br />
273. Von Gunten CF, HIGGINSON IJ. The future of palliative<br />
medicine. In: Bruera E, HIGGINSON IJ, Ripamonti C, von<br />
Gunten C (Eds). Textbook of Palliative Medicine. <strong>London</strong>:<br />
Hodder Arnold. 2006, pp77-82<br />
REPORTS<br />
274. JACKSON D, TURNER-STOKES L, McPHERSON K,<br />
Leese M, Murray J, McCrone P. Acquired Brain Injury: Impact<br />
on Carers. Report to the Department of Health. May 2006<br />
275. MAGEE WL, Burland K. Exploring the use of electronic<br />
music technologies in clinical music therapy: Establishing<br />
definitions and scope of practice. Final report, September<br />
2006. <strong>London</strong>: Royal Hospital for Neuro-disability.<br />
276. TURNER-STOKES L. The Northwick Park Therapy<br />
Dependency Score (NPTDA): Development, preliminary<br />
evaluation and application. Department of Health R&D Project<br />
Grant Report ref 030/0066; 2006.<br />
RESEARCH LETTERS<br />
277. HARDING R, MURTAGH FEM. Palliative care for<br />
management of small-cell lung cancer. The Lancet<br />
2006;367:474<br />
278. Karavitaki N, Wass J, Henderson Slater JD, WADE DT. A<br />
case of post traumatic isolated ACTH deficiency with<br />
spontaneous recovery 9 months after the event. Journal of<br />
Neurology, Neurosurgery, and Psychiatry 2006;77:276-277<br />
PUBLICATIONS IN OTHER JOURNALS<br />
279. HARDING R. Palliative care. A basic human right.<br />
Editorial. Id21 Insights Health 2006;February:1-2<br />
280. JACKSON D, Horn S, Kersten P, TURNER-STOKES L.<br />
Development of a pictorial scale of pain intensity for patients<br />
with communication impairments: initial validation in a general<br />
population. Clinical Medicine 2006;6:580-585<br />
281. KOFFMAN J. Thursday’s child has far to go. Comment.<br />
European Journal of Palliative Care 2006;13:223<br />
282. MAGEE WL. Music Therapy in Rehabilitation: A<br />
Perspective from the UK. [Contribution to Moderated<br />
Discussions] Voices: A World Forum for Music Therapy 2006.<br />
Retrieved from http://www.voices.no/discussions/discm56_<br />
01.html<br />
283. MAGEE WL. Review of ‘Music Therapy and Neurological<br />
Rehabilitation’, David Aldridge (Ed). Australian Journal of Music<br />
Therapy 2006;17:102-104.<br />
284. Thomas V, SALEEM T, Richardson A. Does bilingual<br />
advocacy improve Bengali patients’ satisfaction with cancer<br />
services? Cancer Nursing Practice 2006;5:25-32<br />
285. TURNER-STOKES L, HARDING R, Sergeant J, Lupton<br />
C, McPHERSON K. Generating the evidence base for the<br />
National Service Framework for Long Term Conditions: a new<br />
research typology. Clinical Medicine 2006;6:91-97<br />
48
PUBLISHED ABSTRACTS<br />
286. ADDINGTON-HALL JM, Young A, Rogers A, SALEEM T.<br />
The last three days of life of a random sample of people who<br />
died in the South of England following a stroke: views of<br />
bereaved relatives. Palliative Medicine 2006;20:245<br />
287. BAUSEWEIN C, FARQUHAR MC, GYSELS M,<br />
HIGGINSON IJ, BOOTH S. Measurement of breathlessness on<br />
palliative care: a systematic review. Palliative Medicine<br />
2006;20:331<br />
288. EDMONDS PM, BURMAN R, Silber E, HART S,<br />
HIGGINSON IJ. Evaluation of a novel palliative care service for<br />
patients severely affected by multiple sclerosis. Palliative<br />
Medicine 2006;20:245<br />
289. EDMONDS PM, BURMAN R, Silber E, HART S,<br />
HIGGINSON IJ. Are there differences between those patients<br />
severely affected by multiple sclerosis included in and<br />
excluded from a randomised controlled trial of a new palliative<br />
care service? Palliative Medicine 2006;20:354<br />
290. Ewing G, Rogers M, BARCLAY SIG, McCabe J, Campbell<br />
M, Todd C. Home based palliative care patients: how well do<br />
lay carers estimate their symptoms? Palliative Medicine<br />
2006;20:152-153<br />
291. FARQUHAR MC, BOOTH S, Fagan P, HIGGINSON IJ.<br />
Patients’ and carers’ perception of a breathlessness intervention<br />
service for intractable breathlessness. Palliative Medicine<br />
2006;20:144<br />
292. FARQUHAR MC, BOOTH S, GYSELS M, Fagan P,<br />
HIGGINSON IJ. Patients’ and carers’ perceptions of a<br />
breathlessness intervention service for intractable breathlessness.<br />
Family Practice 2006;23:105<br />
293. GOMES B, HIGGINSON IJ. What is the evidence on the<br />
factors shaping place of death in cancer? Palliative Medicine<br />
2006;20:264<br />
294. GOMES B, HIGGINSON IJ. Dying at home: making it an<br />
achievable end. Journal of Palliative Care 2006;22:203<br />
295. Grande GE, FARQUHAR MC, BARCLAY SIG, Todd CJ.<br />
Self reported quality of life and survival in palliative lung and<br />
colorectal cancer patients. Palliative Medicine 2006;20:137<br />
296. Grande F, Todd C, FARQUHAR MC, BARCLAY SIG.<br />
The role of self reported Quality of Life in prediction of survival:<br />
A consideration of methodological issues. Palliative Medicine<br />
2006;20:293<br />
297. GYSELS M, SHIPMAN C, HIGGINSON IJ. “I will do it if it<br />
will help others”: motivations and distress among patients<br />
taking part in qualitative studies on palliative care. Palliative<br />
Medicine 2006;20:255<br />
298. GYSELS M, HIGGINSON IJ. Systematic review<br />
methodology for qualitative studies: Its benefits and<br />
challenges. Palliative Medicine 2006;20:295<br />
299. Hall E, Bracewell A, White P, EDMONDS PM, Carey I.<br />
Use of specialist palliative care services by chronic obstructive<br />
pulmonary disease (COPD) patients in south east <strong>London</strong>.<br />
Palliative Medicine 2006;20:153-154<br />
300. HARDING R, SELMAN L, Hodson F, Coady E, Beynon T.<br />
A mixed methods approach to generate an evidence-based<br />
chronic heart failure palliative care service. Palliative Medicine<br />
2006;20:246<br />
301. HARDING R, Sherr L, Molloy T. Sampling methods in pain<br />
and symptom research: Do online and clinic samples differ?<br />
Palliative Medicine 2006;20:296<br />
302. HIGGINSON IJ, Normand C, Douglas H-R, Amesbury B,<br />
DONALDSON N. What effect does palliative day care have on<br />
patient outcomes: a non-randomised comparison? Palliative<br />
Medicine 2006;20:140-141<br />
303. JACKSON D, TURNER-STOKES L, Murray J, Leese M,<br />
McPherson K. Acquired brain injury: impact on carers. Clinical<br />
Rehabilitation 2006;20:1106-1107<br />
304. JACKSON D, TURNER-STOKES L, Murray J, Leese M,<br />
Mcpherson K. Validation of the memory and behaviour<br />
problems checklist for use in acquired brain injury. Clinical<br />
Rehabilitation 2006;20:1112<br />
305. KOFFMAN J, Dias A, Raval B, Burke G, Daniels C. Factors<br />
associated with understanding palliative care: results from a<br />
survey of oncology out-patients. Palliative Medicine<br />
2006;20:243<br />
306. McDermott E, SELMAN L, Clark D. Hospice and palliative<br />
care development in India: A review of services and<br />
experiences. Palliative Medicine 2006;20:318<br />
307. MURTAGH FEM, HIGGINSON IJ, ADDINGTON-HALL JM.<br />
Experience of cognitive interviewing techniques in palliative care<br />
research. Palliative Medicine 2006;20:293<br />
308. Rogers MS, Ewing G, BARCLAY SIG, McCabe J, Campbell<br />
M, Todd CJ. Symptom assessment in primary palliative care: how<br />
are we doing? Palliative Medicine 2006;20:135<br />
309.Rogers A, ADDINGTON-HALL JM, JONES E.<br />
Decision making for incompetent patients. Palliative Medicine<br />
2006;20:247<br />
310. SELMAN L, HARDING R, BEYNON T, Hodson F, Coady<br />
E, HIGGINSON IJ. Modelling a palliative care service in heart<br />
failure. Palliative Medicine 2006;20:139-140<br />
311. SHIPMAN C, ADDINGTON-HALL JM, Richardson A, Ream<br />
E, BURT J. What impact did the English national education and<br />
support programme for District and community nurses in the<br />
principles and practice of palliative care have on their confidence<br />
and knowledge? Palliative Medicine 2006;20:268<br />
312. Swann D, Whitmore D, Sugg L, EDMONDS PM, Waight C,<br />
Jones E, Crook T, Rudgyard K. Transportation of patients with<br />
specialist palliative care needs by a local ambulance provider –<br />
policy shaping. Palliative Medicine 2006;20:146<br />
313. TURNER-STOKES L. Specialised rehabilitation for<br />
complex neurodisability - do longer stay programmes provide<br />
value for money. Archives of Physical Medicine and Rehabilitation<br />
2006;87:e10-e11<br />
314. TURNER-STOKES L, Paul S, WILLIAMS H. Is rehabilitation<br />
cost-efficient for patients with complex rehabilitation<br />
needs following acquired brain injury? Archives of Physical<br />
Medicine and Rehabilitation 2006;87:e11<br />
49
315. Young A, ADDINGTON-HALL JM, Rogers A, SALEEM T.<br />
Care at home in the last three months of life for people in the<br />
South of England following a stroke. Views of bereaved<br />
relatives. Palliative Medicine 2006;20:364<br />
PUBLICATIONS - <strong>2007</strong><br />
PAPERS IN SCIENTIFIC JOURNALS<br />
316. Atijosan O, Kuper H, Rischewski D, SIMMS V, Lavy C.<br />
Musculoskeletal impairment survey in Rwanda: design of<br />
survey tool, survey methodology, and results of the pilot study<br />
(a cross sectional survey). BMC Musculoskeletal Disorders<br />
<strong>2007</strong>;8:30<br />
317. BAUSEWEIN C, FARQUHAR M, BOOTH S, GYSELS M,<br />
HIGGINSON IJ. Measurement of breathlessness in advanced<br />
disease: a systematic review. Respiratory Medicine<br />
<strong>2007</strong>:101;399-410<br />
318. EDMONDS PM, VIVAT B, BURMAN R, Silber E,<br />
HIGGINSON IJ. Loss and change: experiences of people<br />
severely affected by multiple sclerosis. Palliative Medicine<br />
<strong>2007</strong>;21:101-10<br />
319. EDMONDS PM, VIVAT B, BURMAN R, Silber E,<br />
HIGGINSON IJ. “Fighting for everything”: service experiences<br />
of people severely affected by multiple sclerosis. Multiple<br />
Sclerosis <strong>2007</strong>;doi:10.1177/1352458506071789<br />
320. GYSELS M, HIGGINSON IJ. Interactive technologies and<br />
videotapes for patient education in cancer care: systematic<br />
review and meta-analysis of randomised trials. Supportive<br />
Care in Cancer <strong>2007</strong>;15:7-20<br />
321. GYSELS M, Richardson A, HIGGINSON IJ. Does the<br />
patient-held record improve continuity and related outcomes in<br />
cancer care: a systematic review. Health Expectations<br />
<strong>2007</strong>;10:75-91<br />
322. HALL S, Chitty L, Dormandy E, Hollywood A, Wildschutt<br />
HIJ, Fortuny A, Masturzo B, Šantavý J, Kabra M, M R, Marteau<br />
TM. Undergoing prenatal screening for Down’s syndrome:<br />
presentation of choice and information in Europe and Asia.<br />
European Journal of Human Genetics <strong>2007</strong>;doi:10.1038/sj.<br />
ejhg.5201790<br />
323.HALL S, Reid E, Ukoummune OC, Weinmann J, Marteau<br />
TM. Brief smoking cessation advice from practice nurses<br />
during routine cervical smear test appointments: a cluster<br />
randomised controlled trial assessing feasibility, acceptability<br />
and potential effectiveness. British Journal of Cancer<br />
<strong>2007</strong>;96:1057-1061<br />
324. HARDING R, Dinat N, Mpanga Sebuyira L. Measuring and<br />
improving palliative care in South Africa: multi–professional<br />
clinical perspectives on development and application of<br />
appropriate outcome tools. Progress in Palliative Care<br />
<strong>2007</strong>;15:55-59<br />
325. HIGGINSON IJ, Davies E, Tsouros A. The end of life:<br />
unknown and unplanned? European Journal of Public Health<br />
<strong>2007</strong>;doi:10.1093/Eurpub/ckm003<br />
326. HIGGINSON IJ, HART S, KOFFMAN J, SELMAN L,<br />
HARDING R. Needs assessment in palliative care: an appraisal<br />
of definitions and approaches used. Journal of Pain and<br />
Symptom Management <strong>2007</strong>;33:500-505<br />
327. Khan F, TURNER-STOKES L, Ng L, Kilpatrick T. Multidisciplinary<br />
rehabilitation for adults with multiple sclerosis<br />
(Review). Cochrane Database of Systematic Reviews <strong>2007</strong>,<br />
Issue 2; CD006036. DOI 10.1002/14651858.CD006036.pub2<br />
328. KOFFMAN J, Burke G, Dias A, Raval B, Byrne J, Gonzalez<br />
J, Daniels C. Demographic factors and awareness of palliative<br />
care and related services. Palliative Medicine <strong>2007</strong>;21:145-153<br />
329. MAGEE WL, Andrews K. Multi-disciplinary perceptions of<br />
music therapy in complex neuro-rehabilitation. International<br />
Journal of Therapy and Rehabilitation <strong>2007</strong>;14:70-75.<br />
330. MAGEE WL. Electronic technologies in clinical music<br />
therapy: a survey of practice and attitudes. Technology and<br />
Disability <strong>2007</strong>;18:139-146<br />
331. MURTAGH FEM, ADDINGTON-HALL JM, HIGGINSON IJ.<br />
The prevalence and symptoms in end-stage renal disease: a<br />
systematic review. Advances in Chronic Kidney Disease<br />
<strong>2007</strong>;14:82-99<br />
332. MURTAGH FEM, ADDINGTON-HALL JM, HIGGINSON IJ.<br />
The value of cognitive interviewing techniques in palliative care<br />
research. Palliative Medicine <strong>2007</strong>;21:87-93<br />
333. MURTAGH FEM, Marsh JE, Donohoe P, Ekbal NJ,<br />
Sheerin NS, Harris FE. Dialysis or not? A comparative survival<br />
study of patients over 75 years which chronic kidney disease<br />
stage 5. Nephrology, Dialysis and Transplantation<br />
<strong>2007</strong>;doi:10.1093/ndt/gfm153<br />
334. Newman MA, Dawes H, van den Berg M, WADE DT,<br />
Burridge J, Izadi H. Can aerobic treadmill training reduce the<br />
effort of walking and fatigue in people with multiple sclerosis: a<br />
pilot study. Multiple Sclerosis <strong>2007</strong>;13:113-119<br />
335. Powell RA, Downing J, HARDING R, Mwangi-Powell F,<br />
Connor S. Development of the APCA African Palliative<br />
Outcome Scale. Journal of Pain and Symptom Management<br />
<strong>2007</strong>;33:229-232<br />
336. Sackley C, Disler PB, TURNER-STOKES L, WADE DT.<br />
Rehabilitation interventions for foot drop in neuromuscular<br />
disease (Review). Cochrane Database of Systematic Reviews<br />
<strong>2007</strong>, Issue 2; CD003908. DOI 10.1002/14651858.CD003908.<br />
pub2<br />
337. SELMAN L, HARDING R, Beynon T, Hodson F, Coady E,<br />
Hazeldine C, Walton M, Gibbs LME, HIGGINSON IJ. Improving<br />
end of life care for chronic heart failure patients – “Let’s hope<br />
it’ll get better, when I know in my heart of hearts it won’t”. Heart<br />
BMJ <strong>2007</strong>;doi:10.1136/hrt.2006.106518<br />
338. Shabab L, HALL S, Marteau TM. Showing smokers with<br />
vascular disease images of their arteries to motivate cessation: a<br />
pilot study. British Journal of Health Psychology <strong>2007</strong>;12:275-283<br />
339. Winward CE, Halligan PW, WADE DT. Somatosensory<br />
recovery: a longitudinal study of the first 6 months after<br />
unilateral stroke. Disability and Rehabilitation <strong>2007</strong>;29:293-299<br />
50
BOOKS<br />
340. ADDINGTON-HALL JM, Bruera E, HIGGINSON IJ,<br />
Payne S. (Eds) Research Methods in Palliative Care Oxford:<br />
Oxford University Press, <strong>2007</strong><br />
BOOK CHAPTERS<br />
341. COSTANTINI M, HIGGINSON IJ. Experimental and<br />
quasi-experimental designs. In: ADDINGTON-HALL JM,<br />
Bruera E, HIGGINSON IJ, Payne S (Eds). Research Methods in<br />
Palliative Care Oxford: Oxford University Press. <strong>2007</strong>;pp85-97<br />
342. HIGGINSON IJ, GYSELS M. Systematic reviews. In:<br />
ADDINGTON-HALL JM, Bruera E, HIGGINSON IJ, Payne S<br />
(Eds). Research Methods in Palliative Care Oxford: Oxford<br />
University Press, <strong>2007</strong>:pp115-136<br />
343. HIGGINSON IJ, HARDING R. Outcome measurement. In:<br />
ADDINGTON-HALL JM, Bruera E, HIGGINSON IJ, Payne S<br />
(Eds). Research Methods in Palliative Care Oxford: Oxford<br />
University Press. <strong>2007</strong>;pp99-113<br />
344. SPECK PW. How to gain research ethics approval. In:<br />
ADDINGTON-HALL JM, Bruera E, HIGGINSON IJ, Payne S<br />
(Eds). Research Methods in Palliative Care Oxford: Oxford<br />
University Press. <strong>2007</strong>;pp275-282<br />
RESEARCH LETTERS<br />
345. HARDING R, Gwyther L, Mwangi–Powel F. Treating HIV/<br />
AIDS patients until the end of life. Journal of Acquired Immune<br />
Deficiency Syndrome <strong>2007</strong>;44:364-365<br />
346. Minton O, HIGGINSON IJ. Electroacupuncture as an<br />
adjunctive treatment to control neuropathic pain in patients<br />
with cancer. Journal of Pain and Symptom Management<br />
<strong>2007</strong>;33:115-117<br />
REPORTS<br />
347. Royal <strong>College</strong> of Physicians. The changing face of renal<br />
medicine in the UK: the future of the speciality. (Contribution by<br />
FEM MURTAGH) Report of a Working Party. <strong>London</strong>: RCP, <strong>2007</strong><br />
PUBLICATIONS IN OTHER JOURNALS<br />
348. HARDING R, Dinat N, MPanga–Sebuyira. Measuring and<br />
improving palliative care in South Africa: multi–professional<br />
clinical perspectives on development and application of<br />
appropriate outcome tools. Progress in Palliative Care<br />
<strong>2007</strong>;15:55-59<br />
349. MAGEE WL. A comparison between the use of songs and<br />
improvisation in music therapy with adults living with acquired<br />
and chronic illness. Australian Journal of Music Therapy<br />
<strong>2007</strong>;www.austmta.org.au/downloadabledocs/<strong>2007</strong>ajmtvol18/<br />
magee<strong>2007</strong>_vol18_inpress%20(2).doc<br />
350. SELMAN L. Yoga in palliative care. A Winston Churchill<br />
Fellowship in India. Yoga and Health Magazine <strong>2007</strong>.<br />
351. TURNER-STOKES L, Sykes N, Silber E, Sutton L, Young<br />
E. From diagnosis to death: exploring the interface between<br />
neurology, rehabilitation and palliative care in managing people<br />
with long term neurological conditions. Clinical Medicine<br />
<strong>2007</strong>;7:129-136<br />
MEETING ABSTRACTS<br />
352. BAUSEWEIN C, BOOTH S, GYSELS M, HIGGINSON IJ.<br />
Non-pharmacological interventions for breathlessness in<br />
advanced stages of malignant and non-malignant diseases: a<br />
Cochrane review. European Journal of Palliative Care <strong>2007</strong>:<br />
EAPC<br />
353. Beccaro M, COSTANTINI M, Merlo F. Inequity in the<br />
provision of and access to palliative care services for cancer<br />
patients in Italy. Results from the Italian survey of the dying of<br />
cancer (ISDOC). European Journal of Palliative Care <strong>2007</strong>:<br />
EAPC<br />
354. COSTANTINI M, Morasso G, Beccaro M. High prevalence<br />
of depressive symptoms among Italian surviving caregivers.<br />
Results from the Italian Survey of the dying of cancer (ISDOC).<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
355. Douglas C, Ellershaw J, MURTAGH FEM, Chambers J,<br />
Meyer M, Howse M, Chesser A, Gomm S, EDMONDS PM,<br />
Murphy D. Adapting the Liverpool Care of the Dying Pathway<br />
for patients dying of end stage renal disease: a national pilot.<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
356. Downing J, HARDING R, Powell R, Alexandra C, Cameron<br />
S, Connor S, Defilippi K, Garanganga E, Kikule E, Mwangi-<br />
Powell F. Use of the APCA African Palliative Outcome Scale<br />
(POS) improves nursing assessment of palliative care patients.<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
357. FARQUHAR MC, BOOTH S, Fagan P, HIGGINSON IJ.<br />
Developing a breathlessness intervention service using the<br />
MRC framework for the development and evaluation of<br />
complex interventions. European Journal of Palliative Care<br />
<strong>2007</strong>:EAPC<br />
358. FARQUHAR MC, Grande G, BARCLAY SIG, Todd C.<br />
Carers’ health, functional status and caregiver burden in end of<br />
life care: trajectories, interrelationships and relation to cancer<br />
patients’ status. European Journal of Palliative Care <strong>2007</strong>:<br />
EAPC<br />
359. GOMES B, GYSELS M, HIGGINSON IJ. Reporting<br />
cancer and dying in the news: a study of Portuguese<br />
newspapers and magazines. European Journal of Palliative<br />
Care <strong>2007</strong>:EAPC<br />
360. GOMES B, HIGGINSON IJ. How and where will we die by<br />
2030: an analysis of future needs in an ageing population.<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
361. Gwyther L, HARDING R, SELMAN L, Mashao T, Dinat N,<br />
Mpanga-Sebuyira L, Mmoledi K, Agupio G, Gillespie C,<br />
Panatovic B. Symptom prevalence and factors associated with<br />
burden indices among palliative care patients: a multicentre<br />
study in 2 Sub-Saharan African countries. European Journal of<br />
Palliative Care <strong>2007</strong>:EAPC<br />
362. GYSELS M, HIGGINSON IJ. Coping with breathlessness<br />
through self-management by COPD patients. European Journal<br />
of Palliative Care <strong>2007</strong>:EAPC<br />
51
363. HARDING R, Panatovic B, Agupio G, Gillespie C, Mashao<br />
T, Mmoledi K, Ndlovu P, Dinat N, Gwyther L, Mpanga-Seburia<br />
L. Measuring pain and symptoms in resource-poor settings: a<br />
comparison of verbal, visual and hand scoring methods in<br />
Sub-Saharan Africa. European Journal of Palliative Care <strong>2007</strong>:<br />
EAPC<br />
364. HARDING R, SELMAN L, Beynon T, Hodson F, Coady E,<br />
Hazeledene C, HIGGINSON IJ. Improving end of life care for<br />
chronic heart failure patients: let’s hope it’ll get better, when I<br />
know in my heart of hearts it won’t? European Journal of<br />
Palliative Care <strong>2007</strong>:EAPC<br />
365. HIGGINSON IJ. Guidelines for depression in palliative<br />
care: current challenges and research agenda. Representing<br />
the EPCRC research group. European Journal of Palliative Care<br />
<strong>2007</strong>:EAPC<br />
366. HIGGINSON IJ. Developing a common language towards<br />
consensus based quality palliative care – Why are definitions<br />
important? European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
367. KOFFMAN J, Morgan M, EDMONDS PM, HIGGINSON IJ.<br />
Culture and pain: a qualitative study of Caribbean and white<br />
British patients with advanced cancer living in <strong>London</strong>. European<br />
Journal of Palliative Care <strong>2007</strong>:EAPC<br />
368. LONGHURST S, KOFFMAN J, SHIPMAN C, Taylor E,<br />
Dewar S. Dying for information: an evaluation of a telephone<br />
helpline for patients with advanced disease and their families.<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
369. LONGHURST S, KOFFMAN J, SHIPMAN C, Taylor E,<br />
Dewar S. A learning curve: developing and operating a<br />
telephone helpline for patients with advanced disease and their<br />
families and professional carers. European Journal of Palliative<br />
Care <strong>2007</strong>:EAPC<br />
370. MURTAGH FEM, ADDINGTON-HALL JM, EDMONDS<br />
PM, Donohoe P, Jenkins K, HIGGINSON IJ. Renal patients<br />
have symptoms too – a cross-sectional survey of symptoms in<br />
stage 5 chronic kidney disease managed without dialysis.<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
371. Perkins P, BOOTH S, Vowler S, BARCLAY SIG. What are<br />
patients’ research priorities for palliative care? European<br />
Journal of Palliative Care <strong>2007</strong>:EAPC<br />
372. Pilkington G, KOFFMAN J. Appetite loss in advanced<br />
cancer – the informal caregivers’ perspective. European<br />
Journal of Palliative Care <strong>2007</strong>:EAPC<br />
373. Rapisarda E, Bertone G, Beccaro M, COSTANTINI M.<br />
Dissatisfaction with home and hospital care during the last<br />
three months of life of Italian cancer patients. European Journal<br />
of Palliative Care <strong>2007</strong>:EAPC<br />
374. Remi C, BAUSEWEIN C. Coadministration of Metamizole<br />
(Dipyrone), Midazolam and Morphine: compatibility and<br />
stability. European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
375. SALEEM T, Leigh N, HIGGINSON IJ. Symptom<br />
prevalence against people affected by advanced and<br />
progressive neurological conditions – a systematic review.<br />
European Journal of Palliative Care <strong>2007</strong>: EAPC<br />
376. SELMAN L, Agupio G, Gillespie C, Mashao T, Mmoledi K,<br />
Ndlovu P, Dinat N, Gwyther L, Mpanga-Sebuyira, Panatovic B.<br />
The needs and experiences of palliative care patients in South<br />
Africa and Uganda. European Journal of Palliative Care <strong>2007</strong>:<br />
EAPC<br />
377. SHIPMAN C, HIGGINSON IJ, GYSELS M, White P, Worth<br />
A, Murray S, BARCLAY SIG, Forrest S, Shepherd J, Dale J.<br />
What is end of life care? Definitions from a national consultation<br />
and implications for practice. European Journal of<br />
Palliative Care <strong>2007</strong>:EAPC<br />
378. SPECK PW, Mills M, Coleman P. Pastoral care of the<br />
elderly: do clergy have an attitude problem? European Journal<br />
of Palliative Care <strong>2007</strong>:EAPC<br />
379. SPECK PW. Team working – fulfilling or frustrating.<br />
European Journal of Palliative Care <strong>2007</strong>:EAPC<br />
PUBLICATIONS IN PRESS<br />
380. Eisenchlas JH, HARDING R, Daud ML, Pérez M, De<br />
Simone GG, HIGGINSON IJ. Use of the Palliative Outcome<br />
Scale in Argentina: A cross-cultural adaptation and validation<br />
study. Journal of Pain and Symptom Management<br />
381. GYSELS M, BAUSEWIEN C, HIGGINSON IJ.<br />
Experiences of breathlessness: a systematic review of the<br />
qualitative literature. Palliative and Supportive Care<br />
382. HALL S, Marteau TM. Practice nurses’ reports of giving<br />
opportunistic smoking cessation advice in three contexts.<br />
Nicotine and Tobacco Research<br />
383. JACKSON D, TURNER-STOKES L, Murray J, Leese M.<br />
Validation of the Memory and Behavior Problems Checklist –<br />
1990R for use in acquired brain injury. Brain Injury<br />
384. Karus D, Raveis VH, Ratcliffe M, Rosefield Jr, HA,<br />
HIGGINSON IJ. Health status and service needs of male<br />
inmates seriously ill with HIV/AIDS at two large urban jails.<br />
American Journal of Men’s Health<br />
385. LONGHURST S, KOFFMAN J, SHIPMAN C, Taylor E,<br />
Dewar S. Helping people access information at the end of life:<br />
evaluating a helpline. King’s Fund Publications<br />
386. MAGEE WL. Music as a diagnostic tool in low awareness<br />
states: Considering limbic responses. Brain Injury<br />
387. MAGEE WL. A comparison between the use of songs and<br />
improvisation in music therapy with adults living with acquired<br />
and chronic illness. Australian Journal of Music Therapy<br />
388. MURTAGH FEM, Chai MO, Donohoe P, EDMONDS PM,<br />
HIGGINSON IJ. The use of opioid analgesia in end-stage renal<br />
disease patients managed without dialysis: recommendation for<br />
practice. Journal of Pain and Palliative Care Pharmacotherapy<br />
389. SELMAN L, HARDING R, Beynon T, Hodson F, Coady E,<br />
Hazeldine C, Walton M, Gibbs L, HIGGINSON IJ. Improving end<br />
of life care for chronic heart failure patients. “Let’s hope it’ll get<br />
better, when I know in my heart of hearts it won’t”. Heart BMJ<br />
52
390. SELMAN L, HARDING R, Hodson F, Coady E, Beynon T.<br />
Modelling services to meet the palliative care needs of chronic<br />
heart failure patients and their families: current practice in the<br />
UK. Palliative Medicine<br />
391. TURNER-STOKES L, Disler R, WILLIAMS H. The<br />
Rehabilitation Complexity Scale: a simple, practical tool to<br />
identify ‘complex specialised’ services in neurological<br />
rehabilitation. Clinical Medicine<br />
392. WILLIAMS H, Harris R, TURNER-STOKES L. Can the<br />
Northwick Park Care Needs Assessment be used to estimate<br />
nursing staff requirements in an in-patient rehabilitation<br />
setting? Clinical Rehabilitation<br />
393. WILLIAMS H, Harris R, TURNER-STOKES L. Northwick<br />
Park Care Needs Assessment: adaptation for inpatient<br />
neurological rehabilitation settings. Journal of Advanced<br />
Nursing<br />
9<br />
Research Support<br />
We thank the following organisations who have supported<br />
research, teaching and development in our department. Most<br />
funding is won through peer review grants.<br />
Addenbrooke's Hospital<br />
The Big Lottery UK<br />
Cancer Research UK<br />
<strong>Cicely</strong> <strong>Saunders</strong> International<br />
Commission of the European Communities<br />
Department of Health (UK)<br />
Diana Princess of Wales Memorial Fund<br />
Dunhill Medical Trust<br />
Fondazione Floriani<br />
Gatsby Foundation<br />
Gulbenkian Foundation<br />
Guy’s & St Thomas’ Charity<br />
Harris HospisCare<br />
Hospice Africa UK<br />
Human BSE Foundation<br />
<strong>King's</strong> Fund (<strong>London</strong>)<br />
<strong>King's</strong> <strong>College</strong> Hospital NHS Foundation Trust<br />
Maruzza Lefebvre D’Ovidio Foundation<br />
Mildmay International<br />
Multiple Sclerosis Society<br />
National Cancer Research <strong>Institute</strong> (NCRI) – a consortium of<br />
MRC, Department of Health, Cancer Research UK and other<br />
charities<br />
National Centre for NHS Service Delivery and Organisation<br />
National Hospice Palliative Care Organization (USA)<br />
Open Society <strong>Institute</strong>/Soros Foundation<br />
Pfizer Ltd<br />
President's Emergency Plan for AIDS Relief (PEPFAR)<br />
St Christopher's Hospice<br />
St Luke's Hospice<br />
University <strong>College</strong> <strong>London</strong><br />
University of North Carolina<br />
We also thank the following who have pledged capital support<br />
for The <strong>Cicely</strong> <strong>Saunders</strong> <strong>Institute</strong> for Palliative Care.<br />
The Weston Foundation<br />
The Wolfson Foundation<br />
Macmillan Cancer Support<br />
PF Charitable Trust<br />
Atlantic Philanthropies<br />
53
10<br />
Developments<br />
in Staffing<br />
During this period we welcomed many new staff, or ones<br />
returning into more senior roles. Academic Rehabilitation,<br />
led by Professor Lynne Turner-Stokes, joined forces<br />
with Palliative Care in 2003, but over the last three years<br />
the department has expanded to include a further parttime<br />
chair (Professor Derick Wade), a Senior Lecturer,<br />
Senior Clinical Research Fellow and four honorary<br />
Research Fellows. Through their respective clinical<br />
services in Northwick Park and Oxford Professors<br />
Turner-Stokes and Wade provide a broad clinical base<br />
for the research programme. A consortium formed in<br />
collaboration with Professor Keith Andrews in the<br />
<strong>Institute</strong> for Neuro-palliative Rehabilitation, Putney,<br />
provides the largest research group for complex<br />
neurological disability in the UK (see section 7). In<br />
addition, two Visiting Chairs (Professor Peter Disler<br />
(Australia) and Professor Kath McPherson (New<br />
Zealand)) support the active research programme.<br />
In Palliative Care, Dr Richard Harding was appointed as<br />
a new Lecturer in Palliative Care, and was promoted to<br />
Senior Lecturer from September <strong>2007</strong>. Dr Sue Hall, a<br />
health psychologist, was appointed as a new Lecturer in<br />
Palliative Care to work on a new programme on palliative<br />
care for older people supported by the Dunhill Medical<br />
Trust and <strong>Cicely</strong> <strong>Saunders</strong> International. Dr Gao Wei is a<br />
new Statistician in Palliative Care, part funded by King’s<br />
<strong>College</strong> <strong>London</strong> and part by the new five year collaborative<br />
in Supportive and Palliative Care from the UK<br />
National Cancer Research <strong>Institute</strong>, which we are coleading<br />
with colleagues across King’s, Leeds and<br />
Edinburgh Universities. In <strong>2007</strong> Professor Massimo<br />
Costantini and Professor Peter Fayers were both<br />
appointed as Visiting Professors for a period of five<br />
years. We also benefited from working with individuals<br />
who spent several months with us on sabbaticals,<br />
including Dr David Gruenewald from the United States,<br />
Dr Joao Paulo Solano from Brazil, and medical students<br />
Troy Cartwright and Michael Walton.<br />
We have also said farewell to some significant members<br />
of our group. Often they have moved on to new, more<br />
senior posts. However, we continue to collaborate with<br />
many individuals, because of continuing and sometimes<br />
new projects, through honorary contracts and because<br />
happily for us some have remained close by with King’s<br />
<strong>College</strong> <strong>London</strong>. There are too many to mention, but<br />
they include Professor Julia Addington-Hall, who moved<br />
to take up a chair in End of Life Care in the School of<br />
Nursing at the University of Southampton. Within King’s<br />
<strong>College</strong> <strong>London</strong>, Dr Nora Donaldson was awarded a<br />
Readership in Statistics in the School of Dentistry and<br />
Dr Elizabeth Davies a Senior Lectureship in the Thames<br />
Cancer Registry. We congratulated three successful<br />
PhD graduates, Dr Jean Potter, supported for three<br />
years from Mrs Coco Marcus, who has now taken up a<br />
new post as consultant in palliative medicine, Dr<br />
Christine McPherson, who is now following a career in<br />
palliative care research in Canada, and Dr Jo Armes,<br />
who took up a post in the School of Nursing, King’s<br />
<strong>College</strong> <strong>London</strong>.<br />
54
Staff Biographies<br />
Professor Irene Higginson BMedSci BMBS FFPHM<br />
PhD FRCP<br />
Professor of Palliative Care and Policy,<br />
Head of Department of Palliative Care,<br />
Policy & Rehabilitation, Honorary Consultant<br />
King’s <strong>College</strong> Hospital<br />
Irene qualified in medicine from the University of<br />
Nottingham and won her PhD from University <strong>College</strong><br />
<strong>London</strong>. She has extensive experience in leading<br />
national and international multidisciplinary collaboration<br />
in palliative care. She has dual training in palliative<br />
medicine and epidemiology/public health having worked<br />
in a wide range of medical settings, hospices and in<br />
public health and health services research. For the past<br />
ten years she has been Head of Department and<br />
Professor of Palliative Care and Policy at King’s <strong>College</strong><br />
<strong>London</strong> and prior to that was Director of Research and<br />
Development in a <strong>London</strong> health authority, as well as<br />
Senior Lecturer at the <strong>London</strong> School of Hygiene and<br />
Tropical Medicine. She is currently leading the<br />
assessment strand of one of the two collaboratives in<br />
supportive and palliative care, leading the strand on<br />
assessment and measurement. This collaborative<br />
(COMPASS – Complex Interventions: Assessment, Trials<br />
and Implementation of Services) brings together over 61<br />
Universities and associated hospitals, hospices and<br />
other services in the UK, and seeks to foster collaboration<br />
of research in supportive and palliative, including<br />
end of life, cancer care. In addition, Irene co-ordinated<br />
the production of the WHO guidance on palliative care<br />
(Palliative Care – The Solid Facts, Better Palliative Care<br />
for Older People). This project, undertaken for the WHO<br />
in Europe, in collaboration with the European<br />
Association of Palliative Care, and the European <strong>Institute</strong><br />
of Oncology, brought together evidence from over 15<br />
countries and wide ranging literature to provide<br />
guidance on ways to improve palliative care for the<br />
future. Irene is a member of the European Palliative Care<br />
Research Collaborative (EPCRC). She has over 180<br />
scientific papers published in peer review journals, has<br />
published 14 books on palliative and end of life care.<br />
She is an advisor to many governments in research and<br />
policy in palliative care, including recently reviewing for<br />
the Italian Ministry of Health, as well as being an advisor<br />
on the end of life care proposals in the United Kingdom<br />
and led the development of the National <strong>Institute</strong> of<br />
Clinical Excellence (NICE) Guidance for Supportive and<br />
Palliative Care for those affected by cancer. She is<br />
currently leading the scoping exercise for the NHS<br />
Service Delivery and Organisation programme on<br />
identifying the research needs on the delivery and<br />
organisation of generalist services for end of life care.<br />
Professor Irene Higginson<br />
Sarah Baber<br />
Executive Assistant to Professor Higginson /<br />
Department Manager<br />
Sarah is Professor Higginson’s Executive Assistant and<br />
is usually the first point of contact for Professor<br />
Higginson. She is also Department Manager and<br />
manages the administrative staff.<br />
Sarah has a BA English from Sussex University. After<br />
graduating she worked briefly at Kingston University in<br />
the Faculty of Health, in the Curriculum and Quality<br />
Office. She then went onto work at <strong>London</strong> South Bank<br />
University as a Faculty Quality Assurance Administrator<br />
in the Faculty of Arts and Human Sciences. Sarah began<br />
working at King’s <strong>College</strong> in July <strong>2007</strong>.<br />
55
Professor Lynne Turner-Stokes DM, FRCP<br />
Herbert Dunhill Chair of Academic Rehabilitation, Head<br />
of Department of Academic Rehabilitation<br />
Lynne was educated at Oxford University, qualified in<br />
Medicine at University <strong>College</strong> Hospital. After ten years<br />
in general medicine and rheumatology she accredited in<br />
Rheumatology and Rehabilitation, and took up her<br />
consultant appointment to set up and direct the<br />
Regional Rehabilitation Unit (RRU) at Northwick Park<br />
Hospital. The unit provides tertiary specialist rehabilitation<br />
services for younger adult patients with severe<br />
complex disabilities, mainly resulting from acquired<br />
brain injury. Lynne and her colleagues have built up a<br />
co-ordinated network of specialist rehabilitation services<br />
across North-West Thames. Within this network, the<br />
RRU act as a central focus for research and training for<br />
all professionals involved in rehabilitation, and has a<br />
national and international reputation as a leading service<br />
in the field of neurological rehabilitation.<br />
Lynne was appointed the Herbert Dunhill Chair of<br />
Rehabilitation at KCL in 2001, with a view to developing<br />
a two-site academic department of rehabilitation<br />
between KCL and Northwick Park. Academic Rehabilitation<br />
joined forces with the Department of Palliative Care<br />
and Policy in 2003. Her research interests include the<br />
development of outcome measures, establishment of<br />
the evidence base for effective intervention in rehabilitation,<br />
and development of evidence-based guidelines<br />
and integrated care-pathways to support best practice<br />
in clinical care. She is on the editorial board of Clinical<br />
Rehabilitation and is guest editor of the series ‘Concise<br />
Clinical Guidelines’ for Clinical Medicine. Lynne has a<br />
major interest in the development of NHS policy to<br />
improve rehabilitation services in the NHS. Since 1997<br />
she has led on the development of guidelines and<br />
clinical standards for the British Society of Rehabilitation<br />
Medicine. From 2002-5 she was the Deputy Chair and<br />
Clinical Lead of the External Reference Group of the<br />
National Service Framework (NSF) for Long Term<br />
Conditions, and continues as advisor to the Department<br />
of Health, providing in lead role in rehabilitation and<br />
research towards implementation of the NSF. She is<br />
committed to enhancing the quality of rehabilitation and<br />
support services for patients with chronic disability and<br />
also to championing the views of users and carers in<br />
development of better services for the future.<br />
Stephen Ashford MSc MCSP<br />
Clinical Specialist in Physiotherapy<br />
Steve qualified in Physiotherapy at Salford University<br />
1993 and undertook a part-time MSc in Neurorehabilitation<br />
at Brunel University between 1996 and 1998. He<br />
was a sessional lecturer at Brunel University, while<br />
working clinically, and undertaking a Post Graduate<br />
Certificate in Education between 1998 and 2001. He<br />
became course co-ordinator for the MSc in Neurorehabilitation<br />
at Brunel University from 2001 until 2003, while<br />
working clinically on the Regional Rehabilitation Unit,<br />
Northwick Park Hospital. In October 2003, he moved full<br />
time to the Regional Rehabilitation Unit, Northwick Park<br />
Hospital to conduct research on the functional<br />
evaluation of outcome following spasticity management<br />
intervention. Steve is currently registered for a PhD at<br />
King’s <strong>College</strong> <strong>London</strong>, Department of Palliative Care,<br />
Policy and Rehabilitation. Research interests include the<br />
evaluation and measurement of functional outcome in<br />
the upper limb following focal interventions and this is<br />
the focus of his PhD thesis. Other research interests<br />
include evaluation of the effectiveness of botulinum toxin<br />
intervention in the hemiparetic upper limb and<br />
management of complex disability.<br />
Stephen’s current clinical role involves co-ordinating the<br />
outreach service from the Regional Rehabilitation Unit at<br />
Northwick Park Hospital Harrow and the related<br />
spasticity management service. The service provides<br />
consulting input to professionals, patients and families in<br />
the management of complex neurodisability including<br />
spasticity.<br />
56
Dr Stephen Barclay MA MB BCh MSc FRCGP MD<br />
Honorary Senior Lecturer<br />
Stephen joined the Department as an Honorary Senior<br />
Research Associate in 2002, becoming Honorary Senior<br />
Lecturer in Primary Palliative Care in the Department in<br />
2006. He works as a General Practitioner in Cambridge,<br />
where he is also Honorary Consultant Physician in<br />
Palliative Medicine at the Cambridge Hospice, Specialty<br />
Director for Palliative Care teaching in the Clinical School<br />
and Macmillan Post-Doctoral Research Fellow in the<br />
University General Practice and Primary Care Research<br />
Unit. His research focuses on Palliative Care in the<br />
Primary Care setting, and he has collaborated with Cathy<br />
Shipman and Julia Addington-Hall over several years.<br />
He was awarded the University of Cambridge Ralph<br />
Noble prize for his MD thesis entitled "General Practitioner<br />
provision of Palliative Care in the United Kingdom"<br />
in 2005 and in 2006 was granted a Department of Health<br />
/ Macmillan Post-Doctoral Fellowship, which is to be at<br />
the Kings Department part of the time.<br />
Dr Claudia Bausewein MD MSc<br />
<strong>Cicely</strong> <strong>Saunders</strong> International Research Training Fellow<br />
Claudia went to Medical School at the University of<br />
Munich. She completed her MD on the situation of<br />
terminally ill cancer patients on admission to hospital.<br />
Although her background is internal medicine, she has<br />
been involved in Palliative Care in Germany for 15 years.<br />
She is now working as a consultant in palliative medicine<br />
at the Interdisciplinary Centre for Palliative Medicine at<br />
the University of Munich. Claudia is Vice-President of<br />
the German Association for Palliative Medicine and coeditor<br />
of the German Journal for Palliative Medicine.<br />
Claudia completed the MSc in Palliative Care at KCL in<br />
2003. Her research project focussed on the validation of<br />
the German version of the Palliative Care Outcome<br />
Scale. Through the MSc Claudia developed her interest<br />
in research and undertook more training in research<br />
methods. She is currently undertaking a PhD funded by<br />
<strong>Cicely</strong> <strong>Saunders</strong> International focusing on breathlessness,<br />
looking particularly into the course of breathlessness<br />
in patients with COPD or cancer and their relatives.<br />
Within her PhD Claudia conducted a systematic review<br />
on measurement of breathlessness and is currently<br />
undertaking a Cochrane Review on non-pharmacological<br />
interventions in breathlessness in advanced disease.<br />
Besides breathlessness her main research and clinical<br />
interests are palliative medicine for non-oncological<br />
patients, pharmacotherapy and subcutaneous<br />
application of drugs.<br />
57
Sian Best BA<br />
Department Administrator<br />
Sian has a BA Hons from the University of Warwick.<br />
After spending a year in postgraduate teacher training,<br />
she decided that she would prefer a career in publishing.<br />
She has worked mainly in publishing, initially in<br />
marketing and public relations, and then as a picture<br />
researcher and picture editor for national newspapers<br />
and magazines. She was also a company secretary. She<br />
joined King’s <strong>College</strong> <strong>London</strong> part time in 2005, helping<br />
to organise a series of conferences for the Social Care<br />
Workforce Research Unit, and moved to the Department<br />
of Palliative Care, Policy & Rehabilitation in July 2005.<br />
She is responsible for the administration of the MSc, PG<br />
Diploma and PG Certificate in Palliative Care. There are<br />
currently 49 students enrolled on the course. Sian is also<br />
responsible for the administration of research grants,<br />
financial transactions including purchasing, and for the<br />
general administration of the department.<br />
Dr Sara Booth FFARCSI and FRCP<br />
Honorary Senior Lecturer<br />
Sara joined the Department in 2003 as an Honorary<br />
Senior Research Fellow, becoming an Honorary Senior<br />
Lecturer in Palliative Care in 2006. She is a Lead Clinician<br />
at Cambridge University NHS Hospitals Foundation Trust<br />
where she was appointed to set up a multi-disciplinary<br />
palliative care service. Sara has had an interest in<br />
breathlessness since her first post in palliative care at St<br />
Christopher’s Hospice in 1991 and has researched the<br />
topic of clinical management of breathlessness since<br />
then. This work led to the development of a Breathlessness<br />
Intervention Service at Addenbrooke’s which started<br />
seeing patients in 2003 and led to the collaboration with<br />
Professor Irene Higginson at King’s <strong>College</strong> <strong>London</strong> to<br />
research its effectiveness. During 2006/7 she has been<br />
the holder of a SuPaC Award to help develop her skills in<br />
clinical trials and research.<br />
Toki Allison<br />
Secretary / Transcriber<br />
After working in both the care and service industries,<br />
Toki gained a Foundation Degree in Media Practice at<br />
the <strong>London</strong> <strong>College</strong> of Communication, University of the<br />
Arts. She joined the department in August <strong>2007</strong> to assist<br />
as transcriber and secretary, specifically assigned to aid<br />
those researching the effects of the Gold Standards<br />
Framework for Care Homes.<br />
Dr Sara Booth<br />
58
Dr Rachel Burman FRCP MA<br />
Consultant in Palliative Care, Honorary Senior Lecturer<br />
Rachel has been a consultant in palliative care since 1997.<br />
She is working part time with the palliative care team at<br />
King’s <strong>College</strong> Hospital Foundation Trust where she leads<br />
on the development of palliative care for people with<br />
neurodegenerative disorders and is a member of the multiprofessional<br />
MND Centre. She worked in cardiology and<br />
neurology before entering a career in palliative care. This<br />
has left a commitment to the palliative care needs of<br />
patients with a non-malignant diagnosis. She has just<br />
finished as the lead consultant on a research project<br />
funded by the MS Society looking at the needs of people<br />
severely affected by MS and their carers. A Masters in<br />
Medical Law and Ethics informs her interest in planning<br />
and decision making in advanced disease and also the<br />
relevance of the Human Rights Act to healthcare provision.<br />
She is a collaborator on an ongoing research project<br />
funded by the Department of Health Defining the Palliative<br />
Care Needs of People with late stage Parkinsonism. She is<br />
a member of the Management and Scientific Board of the<br />
King’s Centre for Palliative Care in Neurology.<br />
Emma Camplejohn BSc<br />
Project Assistant<br />
Emma has a BSc Geography degree from Queen<br />
Mary's, University of <strong>London</strong>. She joined <strong>King's</strong> after<br />
completing her degree in July 2005 and is currently<br />
working as the Project Assistant for Dr Richard Harding<br />
and Dr Marjolein Gysels who have a number of research<br />
interests in palliative care.<br />
59
Jo Clark<br />
Research PA to Professor Lynne Turner-Stokes<br />
Jo is the PA to Professor Lynne Turner-Stokes, working<br />
between sites of Northwick Park Hospital and the<br />
Weston Education Centre. She has qualifications at HNC<br />
level in Business and Computer Management. Previous<br />
to working for King’s <strong>College</strong> <strong>London</strong> Jo was the Clerical<br />
Assistant for the Therapy Teams on the Regional<br />
Rehabilitation Unit based at Northwick Park Hospital.<br />
She has also worked in varying positions in other multiprofessional<br />
organisations.<br />
Professor Massimo Costantini MD<br />
Visiting Professor<br />
Massimo qualified in medicine in 1985 at the University<br />
of Genoa (Italy). He spent the next five years specialising<br />
in oncology and training in clinical epidemiology at the<br />
National Cancer <strong>Institute</strong> (IST) of Genoa.<br />
Since 1990 his main interests have focused on palliative<br />
care. He worked as a palliative home care physician, at<br />
the G Ghirotti Association of Genoa for two years. Since<br />
1992, when he was appointed as full time consultant<br />
epidemiologist at the Clinical Epidemiology Unit of the<br />
National Cancer <strong>Institute</strong>, his research interests have<br />
increasingly focused on the areas of palliative care,<br />
quality of life, and psycho-oncology. He has published<br />
over 80 papers in peer-reviewed journals, and a number<br />
of book chapters on methodological aspects of palliative<br />
care research. His recent research activities have<br />
focused on studying multidimensional problems of<br />
terminal cancer patients and on investigating the effect<br />
of palliative care services on quality of care. He co-ordinated<br />
the Italian Survey of the Dying of Cancer (ISDOC),<br />
a post bereavement Italian survey that is providing a<br />
national picture of the problems experienced by terminal<br />
cancer patients and of the type and quality of provided<br />
care. As first step of a project funded by the Ministry of<br />
Health, he is co-ordinating the first Italian implementation<br />
of the Liverpool Care Pathway (LCP) for the dying in<br />
an Italian hospital. The programme involves a clusterrandomised<br />
trial aimed at assessing the effectiveness of<br />
LCP in improving the quality of end-of-life care in<br />
hospital.<br />
Massimo is involved in Health Service development and<br />
assessment. He was a member of the study group of the<br />
Italian Ministry of Health that developed the national<br />
guidelines and standards for palliative care organisation.<br />
At present, he is co-ordinator of the regional group for<br />
development of the Palliative Care Network, with the<br />
mission to implement for each of the five Local Health<br />
Districts of Liguria a network of specialised palliative<br />
care services, quality assurance and total quality<br />
management programmes and, according to different<br />
60
needs, educational programmes in palliative care.<br />
Massimo is a member of the Scientific Committee of the<br />
Maruzza Lefebvre d’Ovidio Foundation (Rome) leading<br />
the development of a qualified programme of research<br />
and teaching in palliative care. From 2002 to <strong>2004</strong> he<br />
was Medical Director of the “G Ghirotti” Hospice of<br />
Genoa. In <strong>2007</strong>, he was appointed Visiting Professor in<br />
Palliative Care at the Department of Palliative Care,<br />
Policy and Rehabilitation, at King’s <strong>College</strong> <strong>London</strong>.<br />
Dr Polly Edmonds MBBS FRCP<br />
Consultant in Palliative Care, Honorary Senior Lecturer<br />
in Palliative Medicine<br />
Polly is a consultant and lead clinician in Palliative<br />
Medicine at <strong>King's</strong> <strong>College</strong> Hospital NHS Trust and<br />
honorary senior lecturer in the Department of Palliative<br />
Care, Policy & Rehabilitation, <strong>King's</strong> <strong>College</strong> <strong>London</strong>.<br />
She qualified from St Mary’s Hospital Medical School,<br />
and trained in General Medicine, Medical Oncology and<br />
Palliative Medicine prior to taking up her consultant post<br />
in 1997. She has led the development of the clinical<br />
Palliative Care Team at King’s and is closely involved in<br />
the undergraduate curriculum at the King’s <strong>College</strong><br />
<strong>London</strong> School of Medicine, as Palliative Medicine<br />
teaching lead, deputy head of year 4 and year 4 OSCE<br />
coordinator. Jointly with Rachel Burman, Polly is<br />
programme director for the <strong>London</strong> and KSS Deanery<br />
Specialty Training Programme for Palliative Medicine.<br />
She has previously chaired the South East <strong>London</strong><br />
Palliative Care coordinating Group of the South East<br />
<strong>London</strong> Cancer Network and remains an active<br />
participant. Her research interests include palliative care<br />
for non-cancer patients.<br />
Dr Alison Evans PhD MSc<br />
Research Fellow<br />
Alison completed her first degree in Psychology at<br />
University <strong>College</strong> <strong>London</strong> (1983 - 1986). She taught<br />
English in Spain and Japan and worked as a university<br />
administrator before returning to study to complete the<br />
MSc in Social Research Methods at City University<br />
(2000 - 2001). She went on to pursue her interest in<br />
research methods over the course of her PhD at City<br />
University (2003 - 2006) where she undertook a methodological<br />
investigation into use of the Internet as a<br />
social research tool for collecting data on sexual<br />
behaviour among gay and bisexual men. The PhD was<br />
supervised by Professors Dick Wiggins and Jonathan<br />
Elford and funded by the Economic and Social Research<br />
Council. Following this, she took up a one-year postdoctoral<br />
research fellowship at City University which<br />
provided the opportunity to develop her methodological<br />
research and publish work from her PhD thesis. She<br />
joined the department in <strong>2007</strong> and is currently working<br />
with Professors Irene Higginson and Matthew Hotopf on<br />
the development of evidence-based clinical guidelines<br />
for the management of depression in palliative care.<br />
61
Dr Morag Farquhar BSc MSc PhD (Hons) RGN<br />
Research Associate<br />
Morag has worked in health services research for nearly<br />
20 years, with the past 12 focusing on palliative care.<br />
During this time she has worked for health authorities in<br />
<strong>London</strong>, and within the universities of <strong>London</strong>,<br />
Manchester and Cambridge. A graduate nurse by<br />
background (King’s <strong>College</strong> <strong>London</strong>), she went on to<br />
obtain a Masters in Medical Sociology (Royal Holloway &<br />
Bedford New <strong>College</strong>) and PhD (QMUL) on the definition<br />
and measurement of quality of life in older people living<br />
at home. Research interests include palliative care,<br />
quality of life, older people, chronic disease, informal<br />
carers, service evaluation, breathlessness and the use of<br />
mixed methods (qualitative and quantitative). Morag is<br />
currently conducting an evaluation of the Breathlessness<br />
Intervention Service at Addenbrooke’s NHS Trust in<br />
Cambridge, modelled on the MRC Framework for the<br />
Evaluation of Complex Interventions. She is also<br />
collaborating on another Cambridge-based study of<br />
‘Living and dying in extreme old age’ with colleagues in<br />
the Department of Public Health & Primary Care,<br />
University of Cambridge.<br />
Professor Peter Fayers BSc PhD CSTAT<br />
Visiting Professor<br />
Peter joined the Department of Public Health at<br />
Aberdeen University as Professor of Medical Statistics<br />
in 2000. After graduating in statistics at University<br />
<strong>College</strong> <strong>London</strong> he worked in various branches of the<br />
Medical Research Council (Statistical Research and<br />
Services Unit, Tuberculosis and Chest Diseases Unit,<br />
Cancer Trials Office and the Clinical Trials Unit) before<br />
coming to Aberdeen.<br />
Peter's PhD in quality of life research (Open University)<br />
was completed whilst on sabbatical at Trondheim<br />
University (NTNU) in Norway, 1997, and he continues to<br />
work part time at NTNU as Professor of medical<br />
statistics. His main research interest remains in the area<br />
of patient reported outcomes and subjective indicators,<br />
particularly in quality of life research, he has written four<br />
books on the subject (see below). Peter was president of<br />
the International Society for Quality of Life Research<br />
(ISOQOL) 2005-2006. He was associate editor of Quality<br />
of Life Research, from 1998, and is currently a member<br />
of the editorial board. Oncology and palliative care have<br />
been two of his particular interests, and he chaired the<br />
Quality of Life Group of the European Organisation for<br />
Research and Treatment of Cancer (EORTC) for the four<br />
years until 2003.<br />
Currently, Peter is working on HRQL assessment in<br />
diverse clinical areas: oncology, palliative care, children<br />
with asthma, Alzheimer’s patients, home parenteral<br />
nutrition, Paget’s disease, and orthopaedics.<br />
Peter's other interests include clinical trials in oncology<br />
and other fields, data monitoring and stopping rules, and<br />
sample size estimation. He was advisor to the World<br />
Health Organisation's Human Reproduction Programme,<br />
and has taught extensively in China and Outer Mongolia.<br />
In <strong>2007</strong> he was appointed Visiting Professor to the<br />
Department of Palliative Care, Policy and Rehabilitation.<br />
62
Dr Wei Gao PhD MMed BMed<br />
Medical Statistician<br />
Wei Gao has a medical background and a PhD in<br />
epidemiology and health statistics. Before joining the<br />
Department as a medical statistician in April <strong>2007</strong>, she<br />
worked at Imperial <strong>College</strong> <strong>London</strong> in the Infectious<br />
Disease Epidemiology department. She gained considerable<br />
experience in analyzing data from various disease<br />
registries, population-based epidemiology surveys and<br />
gene-environmental interaction studies through her<br />
working with the National University of Singapore from<br />
2002 to 2005. She is a statistical reviewer for the Lancet<br />
and three Lancet series journals. She has expertise in<br />
generating statistical and epidemiologic hypothesis,<br />
describing large observational data and assessing<br />
population disease burdens, survival analysis, advanced<br />
modelling with traditional statistical models and artificial<br />
neural networks, ROC analysis, research design,<br />
computerised record linkage and data management.<br />
Her research interests are extending from previous<br />
statistical epidemiology and experimental medicine to<br />
palliative care and psychosocial medicine. She is<br />
contributing to Strand I of COMPASS (COMPlex<br />
interventions: Assessment, trialS and implementation of<br />
Services) to develop assessment and outcome<br />
measures. She also provides statistical support for the<br />
researchers in the department and teaches MSc<br />
students.<br />
Cassie Goddard BSC MSc<br />
Research Assistant<br />
Cassie studied for her BSc in Applied Psychology at<br />
Liverpool John Moores University, and was awarded an<br />
MSc in Health Promotion and Psychology from the<br />
University of Nottingham in 2006, where her research<br />
interests focused predominantly around smoking<br />
cessation. Following her undergraduate degree, Cassie<br />
worked as Clinical Trials Support Officer on the AspECT<br />
Trail - A Phase III, randomised, study of aspirin and<br />
esomerpazole chemoprevention in Barrett’s Metaplasia.<br />
In May <strong>2007</strong> Cassie joined the Department of Palliative<br />
Care, Policy and Rehabilitation at King’s <strong>College</strong> <strong>London</strong><br />
School of Medicine as a Research Assistant, her main<br />
focus of work concerns the study “Facilitating Implementation<br />
of Gold Standards Framework for Care<br />
Homes”, researching into issues surrounding the<br />
provision of end of life care in care homes. The project is<br />
funded by Guy’s and St Thomas’ Charity.<br />
63
Barbara Gomes BSc MSc<br />
<strong>Cicely</strong> <strong>Saunders</strong> International PhD Research<br />
Training Fellow<br />
Barbara completed her first degree in Psychology and<br />
Health at the University of Porto, Portugal and an MSc in<br />
Palliative Care at <strong>King's</strong> <strong>College</strong> <strong>London</strong>. Having gained<br />
experience in research (in topics such as healthcare<br />
staff training, the integration of vocational guidance in<br />
the school curriculum and family influence on life<br />
expectations), she spent one year as a psychologist in a<br />
Portuguese palliative care unit. Together with Professor<br />
Irene Higginson she has been leading a long-term<br />
project supported by <strong>Cicely</strong> <strong>Saunders</strong> International<br />
aiming to understand where people die and to discover<br />
ways of empowering patients who wish to die at home.<br />
Barbara’s PhD is looking at ways of improving the quality<br />
of palliative care at home and to discover more costeffective<br />
models of home care. Barbara's interests and<br />
projects include: decision-making at the end of life<br />
regarding place of care and death, quality of care and<br />
patient-centred care, cost-effectiveness, the role of the<br />
media on public education about palliative care,<br />
symptom prevalence in advanced disease, understanding<br />
risk, trends analysis and the evaluation of palliative<br />
care services.<br />
Dr Marjolein Gysels MA PhD<br />
Senior Research Fellow<br />
Marjolein completed an MA at the University of Ghent in<br />
Belgium and received a PhD in anthropology at the<br />
University of Amsterdam in 1996. She has carried out<br />
research in the Democratic Republic of the Congo on<br />
Swahili and oral literature. She worked for the TANESA<br />
project on AIDS in Tanzania on female infertility and for<br />
the MRC (UK) Programme on AIDS in Uganda on<br />
commercial sex work. At King’s <strong>College</strong> <strong>London</strong>, she<br />
collaborated on the PROMOTE Project, and she worked<br />
on the Research Evidence Manual which is part of the<br />
NICE Guidance for Supportive and Palliative Care for<br />
those affected by cancer. Since September <strong>2004</strong> she<br />
has been co-managing a programme on breathlessness<br />
in advanced and progressive disease, which is primarily<br />
supported by <strong>Cicely</strong> <strong>Saunders</strong> International. She is<br />
currently also involved in the literature scoping on the<br />
delivery and organisation of generalist services for<br />
adults at the end of life for a project funded by NHS<br />
Service Delivery and Organisation (SDO).<br />
64
Dr Sue Hall BSc PhD CPsychol<br />
The Dunhill Lecturer in Palliative Care<br />
Sue studied Psychology at the Polytechnic of East<br />
<strong>London</strong> and received a PhD in Health Psychology at<br />
King’s <strong>College</strong> <strong>London</strong>. Her first academic appointment<br />
was on a study exploring quality of life for patients with<br />
brain tumours. For most of the next 11 years, she<br />
worked with the Psychology & Genetics Research<br />
Group, King’s <strong>College</strong> <strong>London</strong>, running national and<br />
international studies focusing on adjustment to serious<br />
negative life events, behaviour change, and facilitating<br />
informed choice. During this time she spent a year at the<br />
Centre for Health Care Research, at the University of<br />
Brighton as Research Fellow and NHS R&D Consultant.<br />
In March 2006, she joined the Department of Palliative<br />
Care, Policy and Rehabilitation as Lecturer in Palliative<br />
Care. She is currently developing a programme of work<br />
to improve palliative care for older people. This includes<br />
producing a new booklet for the World Health Organisation<br />
Solid Facts Series on better palliative care for older<br />
people, understanding the barriers and facilitators of<br />
implementing the Gold Standards Framework for Care<br />
Homes, exploring views of dignity of older people in care<br />
homes, and evaluating dignity therapy for older people<br />
in care homes.<br />
Dr Richard Harding BSc MSc DipSW PhD<br />
Senior Lecturer in Palliative Care<br />
Richard originally read Social Anthropology and<br />
conducted field work in the Netherlands before taking a<br />
Masters and Diploma in Social Work at the <strong>London</strong><br />
School of Economics. He undertook his Doctoral studies<br />
in the Department of Palliative Care, Policy & Rehabilitation<br />
at <strong>King's</strong> <strong>College</strong> <strong>London</strong>, developing and testing an<br />
intervention for informal carers. He has worked in<br />
diverse care settings as care provider, care manager,<br />
and social worker and in voluntary sector settings in<br />
group work and training. His interests are primarily<br />
in non-cancer (HIV, heart failure) and in developing an<br />
evidence base for palliative care in Sub-Saharan Africa<br />
where he collaborates in a number of exciting,<br />
productive and enjoyable partnerships with palliative<br />
care and academic settings.<br />
65
Dr Diana Jackson PhD MSc MCSP<br />
Senior Research Fellow<br />
Diana trained as a physiotherapist at King’s <strong>College</strong><br />
Hospital and worked in a variety of clinical settings<br />
before specialising in neurological rehabilitation. After<br />
taking an MSc in rehabilitation studies at Southampton<br />
University, she joined the Regional Rehabilitation Unit at<br />
Northwick Park Hospital in 1996. There she has carried<br />
out a series of research studies into aspects of the<br />
rehabilitation and after care of people with complex<br />
problems after acquired brain injury. A particular focus<br />
has been the design and evaluation of pain assessment<br />
tools accessible to patients with communication and<br />
cognitive deficits. This on-going work formed the basis<br />
of her PhD. Another main research interest concerns<br />
carers. In collaboration with researchers from the<br />
<strong>Institute</strong> of Psychiatry, she has recently completed a<br />
Department of Health funded national study into the<br />
needs and experiences of carers of adults with acquired<br />
brain injury. Findings are being widely disseminated and<br />
will inform service development for carers as part of the<br />
National Service Framework for Long-Term Conditions.<br />
Extension of this work to compare and contrast the<br />
experiences of carers according to their differential<br />
family circumstances, and the condition-specific<br />
problems they have to cope with, in a range of other<br />
long-term neurological conditions is now underway.<br />
Jonathan Koffman BSc MSc<br />
Lecturer in Palliative Care, MSc Course Co-ordinator<br />
Jonathan has a BSc in Social Administration and an<br />
MSc in Sociology with Special Reference to Medicine<br />
from Royal Holloway and Bedford New <strong>College</strong>.<br />
Jonathan's previous work experience involved health<br />
services research and health services commissioning<br />
for a number of health authorities. He is now Lecturer in<br />
Palliative Care and Course Co-ordinator for the interprofessional<br />
Postgraduate Certificate, Diploma and MSc<br />
in Palliative Care run in collaboration with St. Christopher's<br />
Hospice. His research interests include the endof-life<br />
experiences of black and minority ethnic groups,<br />
social exclusion, and palliative care education. He has<br />
published in the following areas: culture and ethnicity,<br />
older people, needs assessment, social exclusion and<br />
palliative care, palliative care education, HIV and AIDS,<br />
as well as mental health and homelessness. He is<br />
currently completing his PhD that has explored the<br />
experience of living with, and dying from, advanced<br />
cancer among black Caribbean and white patients living<br />
in south east <strong>London</strong>.<br />
66
Anna Kolliakou BA MSc<br />
Maruzza Foundation Research Assistant<br />
Anna has a BA in Psychology from the University of Essex<br />
and was awarded an MSc in Clinical and Public Health<br />
Aspects of Addiction from the <strong>Institute</strong> of Psychiatry,<br />
King’s <strong>College</strong> <strong>London</strong>. Following her studies she worked<br />
at the <strong>Institute</strong> of Psychiatry for The Cochrane Collaboration<br />
Depression, Anxiety and Neurosis Group on an<br />
online European mental health library and went on to<br />
become a Research Assistant at the MRC Social Genetic<br />
and Developmental Psychiatry Centre, on a genetic study<br />
investigating issues in unipolar and bipolar depression.<br />
During this time she also held a post at Imperial <strong>College</strong><br />
as a fieldwork interviewer on a co-morbidity study on<br />
mental health and substance use. Most of her work has<br />
been completed at the National Addiction Centre<br />
focusing on motivational interviewing in reducing drug<br />
use and drug related harm in young adults. She rejoined<br />
King’s <strong>College</strong>, after a year-long break, as a Research<br />
Associate for the Department of Palliative Care, Policy<br />
and Rehabilitation on producing a WHO booklet in Better<br />
Practice in Palliative Care for Older People. The project is<br />
funded by the Maruzza Lefebvre D'Ovidio Foundation.<br />
Janet Law OT MSc<br />
Honorary Research Associate<br />
Janet trained in occupational therapy in South Africa. In<br />
addition to her work in South Africa, she has worked in<br />
America, and more recently in <strong>London</strong>. Through the<br />
years, she developed a clinical interest in neurological<br />
rehabilitation, which led to the completion of her MSc in<br />
Neuro-rehabilitation at Brunel University. Her MSc<br />
dissertation focused on Further Evaluation of the United<br />
Kingdom Functional Assessment Measure and<br />
Functional Independence Measure (UK FIM+FAM)<br />
extended activities of daily living items. Janet now<br />
combines her work as a senior occupational therapist on<br />
the Regional Rehabilitation Unit at Northwick Park<br />
Hospital, with a part-time role in research within the<br />
Department of Palliative Care, Policy and Rehabilitation<br />
at King’s <strong>College</strong> Hospital. Her interests lie within<br />
evaluation and development of outcome measures for<br />
neurological rehabilitation, of which her current projects<br />
include the Northwick Park Therapy Dependency<br />
Assessment Scale and Rehabilitation Complexity Scale<br />
with the rehabilitation research team.<br />
67
Susan Longhurst BSc<br />
Research Associate<br />
Susan has a BSc in Law and Social Science from Brunel<br />
University. Previously based in the Department of<br />
General Practice at King’s <strong>College</strong> <strong>London</strong>, Susan<br />
conducted research investigating the recruitment and<br />
retention of GP registrars and was also involved with the<br />
formation of the GP co-operative, SELDOC. Susan<br />
joined the Department in 2005 to work on a needs<br />
review for a local hospice. She was also involved in the<br />
evaluation of Compass, a pilot telephone helpline,<br />
funded by the King’s Fund, targeting people in South<br />
East <strong>London</strong> who are living with a life-limiting illness and<br />
their carers. She is currently working on a study to<br />
describe the perceptions of dignity of older people living<br />
in care homes, along with a Cochrane systematic review<br />
focusing specifically on palliative care interventions for<br />
this target population group.<br />
Jennifer Lunan EN AAMS<br />
PA to Professor Irene Higginson and Dr Susan Hall<br />
Jenny qualified as an Enrolled Nurse and went on to<br />
qualify as a Medical Secretary following her nursing<br />
training, gaining an AMPSAR Certificate. Prior to joining<br />
the <strong>College</strong> Jenny worked as PA/Secretary in the Health<br />
Centre at University <strong>College</strong> <strong>London</strong> for three years<br />
before joining the Imperial Cancer Research Fund (now<br />
CRUK), firstly based in the Clinical Oncology Unit at<br />
Guy’s Hospital as PA to a Consultant Histopathologist<br />
and a Biochemist, and then at the ICRF Laboratories at<br />
Lincoln’s Inn Fields as PA/Floor secretary to Senior<br />
Scientists and researchers. She worked as Professor<br />
Irene Higginson’s PA since joining the <strong>College</strong> in 1999,<br />
firstly based at St Christopher’s Hospice, then moving<br />
into new offices on the second floor of the Weston<br />
Education Centre, then moving into newer offices on the<br />
third floor of the Weston Education Centre. Jenny, along<br />
with previous colleagues, was a founding member of the<br />
Administrative Team and, with the current members of<br />
the Administrative Team, supports the activity of the<br />
department.<br />
68
Dr Wendy Magee PhD NMT ARCM<br />
Honorary Senior Research Fellow<br />
Wendy trained as a music therapist at the University of<br />
Melbourne, Australia, before coming to study and work in<br />
the UK in 1989. She is a specialist in neuropalliative<br />
rehabilitation having worked since 1990 as a clinician,<br />
researcher and manager at the Royal Hospital for Neurodisability<br />
in Putney. Her doctorate was awarded by the<br />
University of Sheffield for researching the experience of<br />
music therapy for people living with chronic and complex<br />
Multiple Sclerosis. She has completed research projects<br />
using both quantitative and qualitative methodologies<br />
examining the effects of music therapy in collaborative<br />
practice to address communication and well-being after<br />
stroke, and exploring of the use of electronic music<br />
technologies in music therapy practice. She currently<br />
holds a postdoctoral fellowship at the <strong>Institute</strong> of Neuropalliative<br />
Rehabilitation, Putney, <strong>London</strong>. She has<br />
published widely on Multiple Sclerosis, low awareness<br />
states, Huntington’s Disease and neuro-rehabilitation.<br />
Current research activity focuses on music therapy in the<br />
treatment of neurological disorders and the development<br />
and validation of evaluation tools with this population.<br />
Dr Farida Malik BSc(Hons), MBBS, MRCP, MSc<br />
<strong>Cicely</strong> <strong>Saunders</strong> International Research Training Fellow<br />
Farida studied medicine at UMDS, University of <strong>London</strong>,<br />
qualifying in 1996. Following this she trained in hospital<br />
general medicine before joining the South Thames<br />
Specialist Registrar Training Scheme in Palliative<br />
Medicine. She has previously undertaken an intercalated<br />
BSc in Psychology (University of <strong>London</strong>) and an MSc in<br />
Palliative Care at King’s <strong>College</strong> <strong>London</strong>. Farida joined<br />
the department in 2005. She is currently undertaking a<br />
PhD funded by the <strong>Cicely</strong> <strong>Saunders</strong> International<br />
Programme for Research into Breathlessness looking at<br />
the experience of caregivers of breathless patients with<br />
advanced disease. Farida’s research interests include<br />
breathlessness and sleep disturbance, steroids in brain<br />
tumours, symptom and quality of life assessment.<br />
69
Professor Kathryn McPherson PhD<br />
Visiting Professor<br />
Kathryn has a clinical background in nursing training in<br />
Australia before moving to the United Kingdom to study<br />
midwifery and then Health Visiting, both in Edinburgh.<br />
Whilst working as a health visitor, Kath undertook a<br />
psychology degree then took up a research position at<br />
the Astley Ainslie Hospital in Edinburgh and then went<br />
on to complete her PhD exploring the effects of brain<br />
injury on the individual and their family in the transition<br />
from inpatient rehabilitation to home. Prior to her current<br />
appointment, she held academic posts at the University<br />
of Edinburgh, the University of Otago (New Zealand) and<br />
the University of Southampton. She continues to cosupervise<br />
PhD students at both the University of Otago<br />
and the University of Southampton. Kath’s research<br />
focus is on: investigating outcomes in ways that matter<br />
most to people with chronic conditions (both conceptual<br />
and psychometric issues); improving effectiveness of<br />
rehabilitation processes such as goals and goal setting<br />
and teamwork; clinical decision making in rehabilitation;<br />
and rehabilitation workforce development. She has been<br />
an Associate Editor with the BMJ group journal Quality<br />
and Safety in Healthcare since 2001. She is also on the<br />
editorial board of Disability and Rehabilitation, Clinical<br />
Rehabilitation and the International Journal of Nursing<br />
Studies. In her role as Visiting Professor at the<br />
Department of Palliative Care, Policy & Rehabilitation<br />
Palliative Care and Rehabilitation, Kath works with<br />
Professor Lynne Turner-Stokes and others in continuing<br />
work addressing the identified lack of knowledge about<br />
the impact of chronic neurological conditions and the<br />
development of more robust and relevant evidence base<br />
in rehabilitation.<br />
Dr Fliss Murtagh MBBS MRCGP MSc<br />
Clinical Research Training Fellow<br />
Fliss is a graduate of the Royal Free Hospital Medical<br />
School, <strong>London</strong>. She worked as a general practitioner<br />
with a special interest in palliative care for 10 years<br />
before specialising in palliative care from 2000. She<br />
completed the MSc in Palliative Care within the<br />
department in 2003, and has published work from her<br />
MSc dissertation on facilitating patient preferences in<br />
decision-making in the Journal of Medical Ethics. She<br />
has now completed consultant training in palliative<br />
medicine, and is currently undertaking a PhD<br />
researching the palliative care needs of patients with<br />
advanced chronic kidney disease who are managed<br />
conservatively, without dialysis. Together with<br />
Professors Irene Higginson and Julia Addington-Hall,<br />
she has completed a systematic review of symptoms in<br />
end stage renal disease, as well as a review of the use of<br />
opioids in conservatively-managed end stage renal<br />
disease. She is also part of the working group<br />
developing a renal version of the Liverpool Care Pathway<br />
for national implementation in the UK. Other interests<br />
include ethics, palliative care for other non-cancer<br />
conditions, and teaching palliative care.<br />
70
Dr Suzanne Penfold BSc PhD<br />
Research Fellow<br />
Suzanne originally studied pharmacology at<br />
Southampton University but later changed to a career in<br />
public health research. Her appointments thus far have<br />
taken her to Bristol, Edinburgh and Aberdeen Universities.<br />
During these appointments Suzanne gained<br />
experience of conducting research evaluations in several<br />
aspects of reproductive health, including Scottish male<br />
reproductive health, Scottish teenage sexual health (PhD<br />
research project) and maternal health in developing<br />
countries. In this department she is working with<br />
Richard Harding to undertake an evaluation of PEPFARfunded<br />
services in Kenya and Uganda offering palliative<br />
care for people living with HIV/AIDS. This longitudinal<br />
study explores links between components of care and<br />
health outcomes. Suzanne’s research interests include<br />
reproductive health research, evaluating complex<br />
interventions, health research in developing countries<br />
and infectious disease epidemiology.<br />
Dr Wendy Prentice MBBS, MA, FRCP<br />
Consultant in Palliative Medicine<br />
Wendy qualified in 1992 and has a background in<br />
general medicine and a broad experience of palliative<br />
medicine in a variety of settings. She commenced her<br />
first consultant / honorary clinical senior lecturer post in<br />
the North East in 2002. Within this post she led a multiprofessional<br />
palliative care team working in primary and<br />
secondary care and also developed the undergraduate<br />
palliative medicine curriculum for Newcastle University.<br />
Wendy joined the palliative care team at Kings <strong>College</strong><br />
Hospital towards the end of 2006.<br />
Throughout her career Wendy has been interested in the<br />
better integration of specialist palliative care services<br />
within non-specialist settings. She is also interested in<br />
the development and delivery of education, as well as<br />
the various factors influencing end of life decision<br />
making. In 2002 she completed an MA in the Ethics of<br />
Cancer and Palliative Care, her dissertation within this<br />
focused on the issues of justice and resource allocation.<br />
Diana Opio<br />
Research Associate<br />
Dr Wendy Prentice<br />
After training as a nurse Diana completed a degree in<br />
Humanities then joined St Christopher’s Hospice where<br />
she worked as a palliative care nurse for 3 years. She<br />
also undertook a post graduate certificate in education<br />
and completed the diploma in palliative care awarded by<br />
King’s <strong>College</strong>, <strong>London</strong>, before proceeding to Leuven in<br />
Belgium where she gained a master’s in applied ethics.<br />
Diana and her family then moved to Uganda where she<br />
was appointed as a lecturer at Uganda Martyrs<br />
University, following which she worked for 3 years as<br />
consultant education advisor at Hospice Africa Uganda<br />
in Kampala developing clinical and distance learning<br />
courses in palliative care. She then moved to The<br />
Mildmay Centre also in Kampala, where she worked for<br />
a further 3 years running the BSc programme ‘A health<br />
systems approach to HIV/AIDS’ with students from<br />
Uganda, Kenya and Tanzania validated by The University<br />
of Manchester. In Uganda her special area of interest<br />
was developing effective palliative home based care<br />
services. During her time in Uganda she also gained a<br />
diploma in health services management run as a<br />
distance learning programme with the RCN.<br />
On returning to the UK, Diana joined in the Department<br />
of Palliative Care, Policy and Rehabilitation in September<br />
<strong>2007</strong>, and is currently working on a research project<br />
looking at the palliative care needs of the elderly.<br />
71
Tariq Saleem BSc MSc<br />
Research Fellow<br />
Tariq has a degree in Psychology from the University of<br />
<strong>London</strong> and an MSc in Health Psychology. Currently he<br />
has a leading role as Research Fellow and centre<br />
coordinator for the King’s Centre in Palliative Care in<br />
Neurology. The centre’s mission is to improve the<br />
treatment, rehabilitation and care of people affected by<br />
long term and progressive neurological conditions<br />
through research and development. He has published in<br />
the following areas: stroke, multiple sclerosis,<br />
Parkinson’s disease, progressive neurological<br />
conditions, cancer screening, sickle cell & thalassaemia,<br />
health psychology, anxiety and worrying, culture and<br />
ethnicity, bilingual health advocacy and palliative care.<br />
He is currently conducting a three year longitudinal<br />
study funded by the Department of Health looking at the<br />
symptoms and care needs in advanced Parkinson’s<br />
disease, multiple symptoms atrophy and progressive<br />
supranuclear palsy.<br />
Lucy Selman BA MPhil Cert Pall Care<br />
Research Associate<br />
Lucy read Philosophy at Nottingham University, and<br />
received an MPhil in Philosophy from Birkbeck <strong>College</strong>,<br />
specialising in Philosophy of Science. In 2006 she<br />
completed the Certificate in Palliative Care at King’s.<br />
After working for Help the Hospices, she travelled in<br />
India, undertaking fieldwork for the International<br />
Observatory on End of Life Care at Lancaster University.<br />
In June 2005 she joined the department to work on a<br />
project modelling a palliative care service for heart<br />
failure patients at St Thomas’ NHS Foundation Trust.<br />
She is currently working for <strong>Cicely</strong> <strong>Saunders</strong> International<br />
on the ENCOMPASS project, validating a version<br />
of the Palliative Care Outcome Scale for use in the<br />
African context. ENCOMPASS is a collaboration<br />
between King’s and palliative care centres in South<br />
Africa and Uganda, with preliminary development and<br />
validation of the POS through the African Palliative Care<br />
Association. Her academic interests include qualitative<br />
research, palliative care in the developing world,<br />
psycho-spiritual interventions and complementary<br />
therapies. A qualified yoga teacher and Thai massage<br />
practitioner, in 2006 Lucy was awarded a Churchill<br />
Travelling Fellowship to conduct research in India into<br />
the use of yoga and meditation in end of life care.<br />
72
Cathy Shipman BA MSc<br />
Senior Research Fellow<br />
Cathy’s background is in medical sociology and her<br />
previous work has included research on out of hours<br />
care, transition to community settings for people with<br />
learning disabilities, health needs assessment, mental<br />
health promotion, local history and the impact of<br />
unemployment on the work of health and social service<br />
professionals. Currently, her main area of interest is<br />
palliative care in primary care. She is working on a<br />
scoping exercise on generalist end of life care commissioned<br />
by the SDO and is supporting the evaluation of a<br />
palliative care helpline for NHS Direct and the evaluation<br />
of the Policy Unit for the National Council of Palliative<br />
Care. She has conducted a needs review for a hospice<br />
and a pilot study developing methods for a longitudinal<br />
study of cancer patients over time. She has worked on<br />
the national evaluation of the Department of Health<br />
funded palliative care education and support<br />
programmes for district and community nurses, and on<br />
work with PCTs concerning palliative care service<br />
development and commissioning. Cathy also works in<br />
the Department of General Practice & Primary Care at<br />
KCL, on a study investigating the palliative care needs of<br />
COPD patients.<br />
Victoria Simms BSc MSc<br />
Research Associate<br />
Vicky has a BSc in Natural Sciences from Durham<br />
University and an MSc in Public Health in Developing<br />
Countries from the <strong>London</strong> School of Hygiene and<br />
Tropical Medicine. She has previously worked on trials<br />
of environmental and sanitary improvements to reduce<br />
trachoma in The Gambia, community-based surveys in<br />
Sudan, and a national survey of physical disability in<br />
Rwanda, which included a case-control study of the<br />
relationship between disability and poverty. She is now<br />
working with Dr Richard Harding on an evaluation of<br />
palliative care provision for people with HIV in Kenya and<br />
Uganda, funded by PEPFAR. Vicky’s research interests<br />
include sanitation, communicable disease epidemiology,<br />
statistics and study design, and healthcare provision in<br />
Africa.<br />
73
Reverend Peter Speck BSc MA<br />
Researcher & Former Health Care Chaplain, Honorary<br />
Senior Lecturer<br />
Peter graduated with a first degree in Biochemistry and<br />
zoology before studying for an MA in Theology. His<br />
thesis focused on the Theological Aspects of Visiting in<br />
Times of Illness. Following a position in a Parish Ministry<br />
in North Wales and then hospital chaplain in Sheffield,<br />
Peter became Chaplain and Honorary Senior Lecturer<br />
(medical ethics) at the Royal Free Hospital in <strong>London</strong>. He<br />
was Trust Chaplaincy Team Leader for Southampton<br />
University NHS Trust until 2002. Currently Visiting Fellow<br />
(Faculty of Medicine) at Southampton University and<br />
Honorary Senior Lecturer, King’s <strong>College</strong> <strong>London</strong><br />
(Palliative Care, Policy & Rehabilitation), Peter is author<br />
of several books on pastoral care, chapters on aspects<br />
of palliative care, and spiritual care and bereavement.<br />
He was a member of the Editorial Board of Palliative<br />
Medicine and served on the Editorial Board of NICE<br />
producing “Supportive Care in Palliative Care”<br />
Guidance. He is a Fellow and Member of the Council of<br />
Palliative Care section of the Royal Society of Medicine.<br />
His research interests include belief systems and<br />
whether they influence outcomes in illness or ageing,<br />
with several peer reviewed papers published.<br />
Frances Stewart BSc<br />
Research Assistant<br />
Frances graduated from Sheffield University in<br />
<strong>2004</strong> with a 2:1 in Psychology. She then worked as a<br />
Research Assistant for the University of Sheffield where<br />
her main role was developing a disease-specific 'Quality<br />
of Life' questionnaire for use in young adults with<br />
Growth Hormone Deficiency. Her other research areas<br />
have included studying the impact of Cancer on<br />
childhood and adolescence Quality of Life.<br />
Following the completion of this study Frances joined<br />
King’s <strong>College</strong> <strong>London</strong> as a research assistant in <strong>2007</strong>.<br />
Currently her main area of research is a study to evaluate<br />
the success and barriers to the implementation of a Gold<br />
Standard Framework in care homes to improve palliative<br />
and end-of-life care.<br />
Laura Skingle<br />
Research Assistant<br />
Laura studied for her BSc in Psychology & Human<br />
Biology at University <strong>College</strong> Northampton and was later<br />
awarded an MSc in Health Psychology from the University<br />
of Bath in 2005. Whilst there Laura undertook a<br />
placement at the Royal Marsden Hospital in Sutton to<br />
study the impact of maternal breast cancer on children’s<br />
social and adaptive functioning. The research was<br />
undertaken in the context of an international multicentre<br />
research project entitled “Children of Somatically Ill<br />
Parents (COSIP)”.<br />
Laura joined the Department of Palliative Care, Policy &<br />
Rehabilitation at King’s <strong>College</strong> <strong>London</strong> School of<br />
Medicine as a Research Assistant in July <strong>2007</strong>. Her main<br />
focus of research is “Improving End of Life Care for the<br />
Elderly at the Hospital Community Interface: An A&E<br />
Audit”. This research will involve understanding the<br />
patterns of emergency department admission for the<br />
elderly with palliative care needs including if admissions<br />
to emergency departments are preventable for this<br />
population. The project is funded by Guy’s & St Thomas’<br />
Charity & <strong>King's</strong> <strong>College</strong> Hospital Charity.<br />
Frances Stewart<br />
74
Professor Derick Wade MA MB BChi, MD FRCP<br />
Honorary part-time Chair of Rehabilitation<br />
In addition to his general medical training, Derick trained<br />
in several specialities related to his current posts<br />
including neurology, neurosurgery, psychiatry and<br />
neurophysiology. He has expertise in many clinical<br />
areas, including: stroke, head injury rehabilitation,<br />
management of multiple sclerosis and motor neurone<br />
disease, assessment of patients in the Permanent<br />
Vegetative State, and the management of patients who<br />
have disability without any underlying disease. His<br />
research activities cover a wide area and he has<br />
published over 180 papers in peer reviewed journals on<br />
many different studies. He is starting studies on mental<br />
practice as a rehabilitation technique. He writes books<br />
and book chapters on many aspects of disabling<br />
neurological disease and has edited Clinical Rehabilitation,<br />
since 1994. He is involved in training doctors and<br />
other professions who are specialising in rehabilitation<br />
and supervises and examines higher degrees.<br />
Heather Williams MSc RN ONC<br />
Dunhill Research Training Fellow<br />
Heather is a qualified Orthopaedic nurse. She worked<br />
for many years as an orthopaedic ward sister at<br />
Northwick Park Hospital before moving into Clinical<br />
Audit. Heather completed further education in<br />
“Evaluation of Clinical Practice”, which helped to<br />
develop her research interests. She joined the Regional<br />
Rehabilitation Unit at Northwick Park in February 2002,<br />
and is currently conducting a research project to further<br />
develop the Northwick Park Dependency Score to<br />
calculate in-patient nursing staff provision within a<br />
rehabilitation setting.<br />
Derick is closely involved in health service management<br />
and development. He has been an advisor to<br />
Oxfordshire Health Authority and been involved in local<br />
working parties on many aspects of neurological<br />
rehabilitation. He has been involved in many national<br />
groups and committees. He has also been involved in<br />
WHO groups and advised national groups in the USA<br />
and New Zealand. In 2001, he was appointed Visiting<br />
Professor in Community Rehabilitation at the University<br />
of Maastricht, the Netherlands. In June 2002, he was<br />
made an honorary fellow of the <strong>College</strong> of Occupational<br />
Therapists; and in October 2005, he became a part-time<br />
professor in neurological rehabilitation at King’s <strong>College</strong><br />
Hospital <strong>London</strong>.<br />
75
Previous Members of the Department (since <strong>2004</strong>)<br />
NAME POSITION YEAR OF<br />
DEPARTURE<br />
Professor Julia Addington-Hall Professor of Palliative Care Research <strong>2004</strong><br />
and Policy/Deputy Head of Department<br />
Bimpe Akinwunmi PA to Professor Addington-Hall <strong>2004</strong><br />
Dr Lara Alloway Specialist Registrar <strong>2004</strong><br />
Jo Armes CRUK Research Fellow <strong>2004</strong><br />
Jenni Burt Research Associate <strong>2004</strong><br />
Floss Chittenden Data Entry Clerk <strong>2004</strong><br />
Dr Elizabeth Davies Clinical Senior Research Fellow <strong>2004</strong><br />
Darryl De Prez Head of Fundraising, <strong>Cicely</strong> <strong>Saunders</strong> International <strong>2007</strong><br />
Sam Hart Research Associate 2006<br />
Dr Rhidian Hughes Senior Research Fellow <strong>2004</strong><br />
Maggie Johnson Departmental Administrator 2005<br />
Julie Payne Student <strong>2004</strong><br />
Sally Plumb Honorary Research Associate 2005<br />
Dr Jean Potter Mrs Coco Marcus Clinical PhD Research <strong>2004</strong><br />
Training Fellow<br />
Carolin Seitz Project Support Officer 2006<br />
Joel Sheridan Research Assistant Psychologist <strong>2004</strong><br />
Amanda Tadrous Research Assistant Psychologist <strong>2004</strong><br />
Bella Vivat Research Fellow <strong>2004</strong><br />
76