Summer 2010 - The British Pain Society
Summer 2010 - The British Pain Society
Summer 2010 - The British Pain Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
that is completely counter intuitive<br />
to most non medical outsiders.<br />
Ultimately intractable pain, from<br />
whatever cause, many being non<br />
malignant, should never been<br />
seen as an absolute birthright to<br />
potent narcotics.<br />
Big Pharma and the real cost<br />
Pharma companies have been<br />
very active in promoting their<br />
medications. This has taken<br />
the familiar form of promotion<br />
masquerading as medical<br />
education. When was the last<br />
meeting that you attended that<br />
wasn’t sponsored? Many leading<br />
specialist have been paid to speak<br />
and to advise companies with<br />
the amounts paid undisclosed.<br />
International conferences, flights,<br />
and accommodation have been<br />
gifted widely to the medical<br />
community, including pain<br />
physicians and GPs. None of this<br />
over steps common professional<br />
boundaries but has lead to a<br />
dominance of therapeutics in the<br />
mind set of the pain community<br />
and undoubtedly increased the<br />
uptake of new medications.<br />
I could quote corporate billions<br />
but this is difficult to conceptualize.<br />
So in table 1, I have set at the<br />
cost to the NHS for commonly<br />
prescribed opioids to illustrate<br />
the personal implications of our<br />
prescribing patterns. This explains<br />
why the industry is so benevolent<br />
with its money for education.<br />
Chronic medical conditions are<br />
industries golden geese. <strong>The</strong> more<br />
pain, the more medication and the<br />
more profit – this a simple and<br />
hugely effective business model<br />
– a monster goose. This is no anti<br />
pharma conspiracy but merely a<br />
statement of fact.<br />
<strong>The</strong> industry is active in all areas<br />
of public lobbying. But most<br />
insidiously with patient groups.<br />
Emotions drives health care,<br />
not science, and the emotion of<br />
suffering patients is marketing<br />
dynamite. <strong>The</strong> American <strong>Pain</strong><br />
<strong>Society</strong> suggests no one should<br />
suffer pain and has a campaign<br />
“Dream no Small Dreams “.<br />
This same society has received<br />
$ 500,000 from a single<br />
pharmaceutical company. I wonder<br />
who is doing the dreaming?<br />
Always promoting the simplistic<br />
message on pain – that is it is<br />
both under diagnosed and under<br />
treated. Pharma money pollutes<br />
many patient charities and suffers<br />
to reinforce the medical model of<br />
care and the use of therapeutics.<br />
Harms<br />
But even if we assume that current<br />
practice does good, do we know<br />
if it does harm? Most pharma<br />
research is short by design for<br />
both efficacy and harms. Also<br />
study populations are carefully<br />
chosen to be the groups most<br />
likely to benefit and are often very<br />
different from general practice<br />
populations. This research is then<br />
applied inappropriately to different<br />
and unrepresentative populations<br />
e.g. research in a group of 300<br />
attending a pain clinic is quite<br />
different from a general practice<br />
population. Lastly, because pain<br />
has such a wide cultural variation,<br />
research should be country<br />
specific. Good critical appraisal<br />
skills are essential- don’t always<br />
believe the research at face value.<br />
Opioids are associated with<br />
tolerance and significant<br />
withdrawal when stopped. Once<br />
started opioids are difficult to<br />
stop and seem to be taken for<br />
decades. Opioids cause both<br />
a physical and psychological<br />
addiction. But what is the long<br />
effect on social functioning, like<br />
work, relationships and the rest?<br />
Key systematic and literature<br />
reviews highlight the “scarcity of<br />
evidence” [5] and huge variation<br />
in reported incidence of addiction<br />
of 0-50%. [2]. <strong>The</strong>re is also little<br />
evidence to support better social<br />
functional and new evidence<br />
comments “it is remarkable that<br />
a opioids treatment of long-term/<br />
chronic non-cancer pain does not<br />
fulfill any of the key outcomes<br />
of opioids treatment goals: pain<br />
relief, improved quality of life and<br />
improved functional capacity” [1]<br />
But other hard end point data<br />
is beyond refute - opioids<br />
are associated with abuse,<br />
unintentional overdose and<br />
deaths. <strong>The</strong> numbers dying in<br />
the UK are not known, but if we<br />
look to the USA, the increase<br />
in mortality mirrors increasing<br />
prescribing. So the doubling in<br />
prescriptions has likely doubled<br />
iatrogenic death. [4]. We need<br />
urgent UK research, not anecdote,<br />
to inform the issue of balance<br />
versus harm for the rapid and<br />
widespread use of opioids.<br />
<strong>The</strong> Future<br />
<strong>The</strong> pain community has been<br />
a great advocate for improved<br />
pain relief ( a problem often<br />
ignored) and they should be<br />
rightly proud of the improvements<br />
in care. <strong>The</strong> problem is those<br />
pain clinics are detached<br />
from the community and lack<br />
continuity. In recent times many<br />
GPs complain that pain clinics<br />
purse a policy of inconsistent<br />
polypharmacy, new medicines<br />
and rapid dose escalation. <strong>The</strong>re<br />
are new regional pain syndromes<br />
that many are skeptical of. And<br />
despite the assertion of pain<br />
clinic are multidisciplinary with a<br />
broad view of pain - intervention<br />
seems dominated by therapeutics.<br />
<strong>The</strong> pain community needs to<br />
acknowledge these concerns for<br />
they are the key opinion leaders.<br />
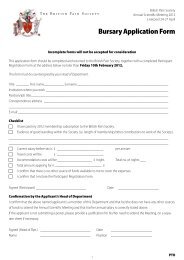
Table 1<br />
Medication* Monthly Cost * Real 10 year Cost<br />
Butrans 10 Patch £32 £3,840<br />
Patch Oxycontin 40mg £101 £12,120<br />
Durogesic 100 £163 £19,560<br />
*as per BNF<br />
GPs need better guidance and<br />
monitoring of prescribing activity.<br />
<strong>The</strong>re also needs to be serious<br />
consideration from both pain<br />
clinicians and GPs as to whether<br />
they need to distance themselves<br />
from the Pharma industry due<br />
to the huge financial conflicts<br />
of interest. At the very least the<br />
amounts paid to leading specialists<br />
needs full disclosure and a<br />
move away from the traditional<br />
sponsored educational events.<br />
How we do this is a thorny issue<br />
but transparency is key. We must<br />
monitor the prescribing trends<br />
and halt the rate of rise. Lastly,<br />
we need to redefine the notion<br />
that “pain is what the patient says<br />
it is” for this is clearly not the<br />
case and rebalance the doctor<br />
patient relationship. I maintain<br />
that the rapid increase in opioids<br />
prescribing in non malignant pain<br />
is generating significant iatrogenic<br />
harm, is bad for patients and is<br />
bad medicine.<br />
References<br />
[1] Eriksen J et al. Critical<br />
issues on opioids in chronic<br />
non-cancer pain: an<br />
epidemiological study. <strong>Pain</strong><br />
2006;125:172-179<br />
[2] Hǿjsted J, Sjǿgren P. Addiction<br />
to opioids in chronic pain<br />
patients: A literature review<br />
European Journal of <strong>Pain</strong><br />
2007;11:490-518<br />
[3] Oye Gureje, MBBS, PhD,<br />
FWACP; Michael Von Korff,<br />
ScD; Gregory E. Simon,<br />
MD, MPH; Richard Gater,<br />
MRCPsych Persistent <strong>Pain</strong> and<br />
Well-being A World Health<br />
Organization Study in Primary<br />
Care JAMA. 1998;280:147-151.<br />
[4] http://www.<br />
agencymeddirectors.wa.gov/<br />
Files/AGReportFinal.pdf<br />
[5] Ballantyne J and LaForge<br />
KS. Opioid dependence<br />
and addiction during opioid<br />
treatment of chronic pain. <strong>Pain</strong><br />
2007;129:235-25<br />
PAI N N E W S S U M M E R <strong>2010</strong> 37