Units of pressure and their conversion
Units of pressure and their conversion
Units of pressure and their conversion
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
•Respiratory system<br />
•Biomechanics <strong>of</strong> breathing<br />
•Negative intrapleural <strong>pressure</strong> <strong>and</strong> its importance<br />
Lung volumes <strong>and</strong> capacities<br />
•Spirometry<br />
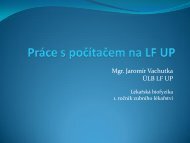
Dalton’s law<br />
Molecular properties <strong>of</strong> gasses<br />
states that the total <strong>pressure</strong> exerted by a gaseous<br />
mixture is equal to the sum <strong>of</strong> the partial<br />
<strong>pressure</strong>s <strong>of</strong> each individual component in a gas<br />
mixture<br />
p =<br />
p1 + p2<br />
+ +<br />
p n = p<br />
V<br />
i p<br />
i<br />
i = p<br />
V<br />
n<br />
i=<br />
1<br />
partial <strong>pressure</strong> p i<br />
<strong>of</strong> the i-th component we can determine from volume concentration<br />
V i<br />
/V <strong>and</strong> from total <strong>pressure</strong> <strong>of</strong> that mixture p
total atmospheric <strong>pressure</strong> P B<br />
= 101,325 kPa (760 Torr)<br />
Partial <strong>pressure</strong>s <strong>and</strong> contents <strong>of</strong> dry air<br />
Example 1. Calculate partial <strong>pressure</strong> N 2<br />
<strong>and</strong> O 2<br />
at P B<br />
= 101,3 kPa; N 2<br />
= 78,03 %, O 2<br />
= 20,95 %:<br />
pN 2<br />
= 0,7803 . 101,3 kPa = 79,11 kPa;<br />
pO 2<br />
= 0,2095 . 101,3 kPa = 21,23 kPa.<br />
Henry’s law<br />
At a constant temperature, the amount <strong>of</strong> a given gas dissolved in a given type<br />
<strong>and</strong> volume <strong>of</strong> liquid is directly proportional to the partial <strong>pressure</strong> <strong>of</strong> that gas.<br />
V<br />
p<br />
αpiV<br />
=<br />
p<br />
B<br />
k<br />
at P B<br />
= 101,3 kPa a T = 37 °C je: α O2<br />
= 0,024 ; α CO2<br />
= 0,57<br />
→ CO 2<br />
solubility in water is 24-times higher than for O 2<br />
In arterial blood pO 2<br />
= 12,0 kPa, pCO 2<br />
= 5,3 kPa;<br />
How much <strong>of</strong> O 2<br />
<strong>and</strong> CO 2<br />
is dissolved in 1L <strong>of</strong> blood:<br />
V p-O2<br />
= 0,024 . 12000 / 101300 = 2,84 ml .l –1<br />
V p-CO2<br />
= 0,57 . 5300 / 101300 = 29,82 ml.l –1
<strong>Units</strong> <strong>of</strong> <strong>pressure</strong> <strong>and</strong> <strong>their</strong> <strong>conversion</strong><br />
•SI unit: [Pa] = N/m 2<br />
•using height <strong>of</strong> liquid with the same <strong>pressure</strong> effect<br />
p = h.ρ.g<br />
h =height<br />
ρ =density<br />
g = gravitational acceleration<br />
1m<br />
1m<br />
Torricelli pokus:<br />
h<br />
p<br />
1 mm Hg = 1.36 cm H 2<br />
O<br />
Hg<br />
ρ = 13 546 kg.m -3<br />
h = 760 mm Hg = 760 torr …. 1 atm = 101 325 Pa<br />
H 2<br />
O<br />
ρ = 1000 kg.m -3<br />
h = 10.329 m H 2<br />
O<br />
…. 1 mm Hg (1 torr) = 133.322 Pa<br />
…. 1atm = 101 325 Pa<br />
…. 1 cm H 2<br />
O = 98.1 Pa<br />
http://brunelleschi.imss.fi.it<br />
The Respiratory System<br />
• Respiratory system<br />
designed for gas<br />
exchange<br />
• Regulates acid-base<br />
balance<br />
• Regulates blood <strong>pressure</strong><br />
• Prevention <strong>of</strong><br />
thromboembolism<br />
- upper respiratory tract is above vocal cords<br />
- lower respiratory tract is below vocal cords
Human angiotensinogen<br />
is 118 amino acids long<br />
Pathway <strong>of</strong> RAAS<br />
Trachea <strong>and</strong> Bronchial Tree
Terminal bronchiole Tree<br />
300 million air sacs.<br />
Large surface area (60 –<br />
80 m2).<br />
Cells Types <strong>of</strong> the Alveoli<br />
• Type I alveolar cells<br />
– simple squamous<br />
cells where gas<br />
exchange occurs<br />
• Type II alveolar cells<br />
(septal cells)<br />
– free surface has<br />
microvilli<br />
– secrete alveolar<br />
fluid containing<br />
surfactant<br />
• Alveolar dust cells<br />
– w<strong>and</strong>ering<br />
macrophages<br />
remove debris
Alveolar-Capillary Membrane<br />
• Respiratory membrane = 1/2 µm<br />
• Exchange <strong>of</strong> gas from alveoli to blood<br />
4 Layers <strong>of</strong> membrane to cross<br />
- alveolar epithelial wall <strong>of</strong><br />
type I cells<br />
- alveolar epithelial basement<br />
membrane<br />
- capillary basement<br />
membrane<br />
- endothelial cells <strong>of</strong> capillary<br />
Conductive <strong>and</strong> Respiratory Zones<br />
• Conductive zone (Dead volume)<br />
- Conducts air to respiratory zone<br />
- Humidifies, warms, <strong>and</strong> filters air<br />
Components:<br />
– Trachea<br />
– Bronchial tree<br />
– Bronchioles<br />
Respiratory zone<br />
- Exchange <strong>of</strong> gases between air<br />
<strong>and</strong> blood<br />
Components:<br />
– Terminal bronchioles<br />
– Respiratory bronchioles<br />
– Alveolar sacs
Breathing or Pulmonary Ventilation<br />
Dimensions <strong>of</strong> the Chest Cavity<br />
• Breathing in requires<br />
muscular activity &<br />
chest size changes<br />
• Contraction <strong>of</strong> the<br />
diaphragm flattens the<br />
dome <strong>and</strong> increases the<br />
vertical dimension <strong>of</strong> the<br />
chest<br />
Quiet Inspiration<br />
• Diaphragm moves 1 cm & ribs lifted by external intercostal muscles<br />
• Intrathoracic <strong>pressure</strong> falls <strong>and</strong> air is inhaled<br />
Quiet Expiration<br />
• Passive process with no muscle action<br />
• Elastic recoil & surface tension in alveoli pulls inward<br />
• Alveolar <strong>pressure</strong> increases & air is pushed out
Breathing or Pulmonary Ventilation<br />
Air moves into lungs when <strong>pressure</strong> inside lungs is less than atmospheric<br />
<strong>pressure</strong><br />
Air moves out <strong>of</strong> the lungs when <strong>pressure</strong> inside lungs is greater than<br />
atmospheric <strong>pressure</strong><br />
Intra-pleural<br />
Pressures<br />
• Helps keep parietal &<br />
visceral pleura stick<br />
together <strong>and</strong> alveoli inflated<br />
•Always subatmospheric<br />
(756 mm Hg)<br />
•As diaphragm contracts<br />
intrapleural <strong>pressure</strong><br />
decreases even more (754<br />
mm Hg)<br />
Atmospheric<br />
<strong>pressure</strong> = 1 atm<br />
or 760mm Hg<br />
Summary <strong>of</strong> Breathing
Compliance <strong>of</strong> the Lungs<br />
•Compliance refers to the distensibility <strong>of</strong> the lung <strong>and</strong> is defined as the change in<br />
lung volume produced by a change in <strong>pressure</strong>.<br />
• Ease with which lungs & chest<br />
wall exp<strong>and</strong> depends upon<br />
1. Elastic recoil <strong>of</strong> lungs &<br />
2. surface tension<br />
• Some diseases reduce<br />
compliance<br />
– tuberculosis forms scar tissue<br />
– pulmonary edema => fluid in lungs<br />
& reduced surfactant<br />
Thin layer <strong>of</strong> fluid in alveoli<br />
causes inwardly directed<br />
force = surface tension, water<br />
molecules strongly attracted to<br />
each other causes alveoli to<br />
remain as small as possible<br />
Detergent-like substance called<br />
surfactant produced by Type II<br />
alveolar cells lowers alveolar<br />
surface tension<br />
If surface<br />
tension is<br />
high much<br />
energy must<br />
be used to<br />
exp<strong>and</strong><br />
alveoli<br />
Laplace’s Law tells us that the<br />
<strong>pressure</strong> within a spherical<br />
structure with surface tension,<br />
such as the alveolus, is inversely<br />
proportional to the radius <strong>of</strong> the<br />
sphere (P=2T/r). That is, at a<br />
constant surface tension, small<br />
alveoli will generate bigger<br />
<strong>pressure</strong>s within them than will<br />
large alveoli.<br />
Compliance <strong>of</strong> the Lungs<br />
Emphysema is a disease characterized by dilation <strong>of</strong> the alveolar spaces <strong>and</strong><br />
destruction <strong>of</strong> the alveolar walls. With <strong>their</strong> loss, much <strong>of</strong> the elastic recoil <strong>of</strong> the lung<br />
is also lost.<br />
C = ∆V /∆P<br />
Normal values are about 200 ml cmH 2 O -1<br />
Airway’s resistance<br />
this is a measure <strong>of</strong> the resistance to airflow in the airways expressed as the air<br />
<strong>pressure</strong> divided by the flow. Normal adult values are about 2 cmH 2<br />
Ol -1 s
Determination <strong>of</strong> Pulmonary Function<br />
•To evaluate symptoms <strong>and</strong> signs <strong>of</strong> lung disease<br />
•To assess the progression <strong>of</strong> lung disease<br />
•To monitor the effectiveness <strong>of</strong> therapy<br />
•To evaluate preoperative patients<br />
•Screen people at risk <strong>of</strong> pulmonary disease<br />
•To monitor for potentially toxic effects <strong>of</strong> certain<br />
drugs/chemicals<br />
Basic techniques:<br />
peak air flow measurement<br />
determination <strong>of</strong> lung volumes <strong>and</strong> capacities<br />
forced expiratory volume measurement<br />
flow/volume curve recording
Lung Volumes <strong>and</strong> Capacities<br />
• Tidal volume TV = amount<br />
air moved during quiet<br />
breathing<br />
• Minute ventilation MVR= is<br />
amount <strong>of</strong> air moved in a<br />
minute<br />
• Maximum voluntary<br />
ventilation MVV = volume <strong>of</strong><br />
air inspired per minute during<br />
maximum voluntary hyper<br />
ventilation. The patient is<br />
asked to breathe at 50 min-1<br />
as deeply as possible for 15 s.<br />
The total volume <strong>of</strong> inspired<br />
air is measured <strong>and</strong> multiplied<br />
by four. Normal values for<br />
men are about 150 l min-1,<br />
• Reserve volumes = amount<br />
you can breathe either in or<br />
out above that amount <strong>of</strong> tidal<br />
volume (IRV, ERV)<br />
• Residual volume RV = 1200<br />
mL permanently trapped air in<br />
system (in the mouth, trachea<br />
as well as the rest in the<br />
lungs) This volume increases<br />
with age <strong>and</strong> is slightly lower<br />
in women.<br />
• Vital capacity & total lung<br />
capacity are sums <strong>of</strong> the<br />
other volumes<br />
Vital capacity (VC) is a change <strong>of</strong><br />
air volume in the lung which is<br />
measured between the maximum<br />
inspiration level <strong>and</strong> the maximum<br />
expiration level. This<br />
measurement which starts with<br />
inspiration from the maximum<br />
expiration level is called<br />
inspiratory vital capacity (IVC).<br />
The examination which starts with<br />
expiration from the maximum<br />
inspiration level is called<br />
expiratory vital capacity (EVC).<br />
VC = IRV + TV + ERV<br />
The functional residual capacity<br />
(FRC) is an amount <strong>of</strong> air which<br />
remains in the lung after normal<br />
expiration.<br />
Lung Volumes <strong>and</strong> Capacities<br />
FRC = ERV + RV<br />
The total lung capacity (TLC) is the air volume in the lung at the end <strong>of</strong> maximum inspiration.<br />
TLC = IRV + TV + ERV + RV
Forced Expiratory Volume Measurement<br />
The forced expiration volume per second<br />
(FEV1) is an air volume in liters which an<br />
examined person expires in the first second<br />
<strong>of</strong> forced expiration after maximum<br />
inspiration.<br />
This measured expiratory volume is <strong>of</strong>ten<br />
expressed as a percentage <strong>of</strong> the forced<br />
vital capacity, FEV1 /FVC <strong>and</strong> is called the<br />
Tiffenea index [%].<br />
FEV1 is called the second vital capacity or<br />
distributed forced expiration per first second.<br />
FEV1/FVC = 80%<br />
Dynamic values <strong>of</strong> lung ventilation - flow/volume curve recording<br />
Respiration frequency (df) [min-1] is a number <strong>of</strong> breaths in a given time<br />
interval. It is usually given in units per minute. The normal respiration rate for a<br />
baby is about 60 min -1 but, by the age <strong>of</strong> one year, this has fallen to 30-40 min -1<br />
<strong>and</strong>, in an adult, 12-15 min -1 .<br />
The respiration rate is not completely regular <strong>and</strong> changes with exercise, during talking <strong>and</strong> according to<br />
the environment. The control centre for breathing is in the medulla <strong>of</strong> the brain <strong>and</strong> the major influence on<br />
this is the CO 2<br />
<strong>and</strong> O 2<br />
level in the blood. The medulla, through its influence on the nerves supplying the<br />
respiratory muscles <strong>and</strong> the diaphragm, can increase or decrease respiration rate <strong>and</strong> tidal volume.<br />
Maximum expiratory flow values at 25% FVC –<br />
(MEF25, also FEF25 ) [l.s -1 ], at 50% FVC (MEF50,<br />
also FEF50), <strong>and</strong> at 75% FVC (MEF75, also FEF75).<br />
They are usually given in liters per second <strong>and</strong> inform<br />
us about expiratory flows <strong>of</strong> important segments <strong>of</strong> a<br />
distributed forced expiration curve, respectively the<br />
flow – volume curve.<br />
The peak expiratory flow (PEF) [l.s -1 ], also called<br />
the top expiratory velocity is the greatest flow<br />
achieved during forced expiration from the<br />
maximum inspiration.
FORCED EXPIRATION TEST<br />
• Simplest test<br />
• One <strong>of</strong> the most informative<br />
• Requires minimal equipment<br />
• Trivial calculations<br />
• Majority <strong>of</strong> patients with lung disease: abnormal forced<br />
expiration<br />
Classification <strong>of</strong> ventilation defects<br />
•obstructive<br />
•restrictive<br />
•combined<br />
Obstructive ventilation defect<br />
With purely obstructive ventilation defect, the expiratory flows are<br />
significantly reduced, while the vital lung capacity is relatively well maintained.<br />
The basic criterion for specifying the obstructive ventilation defect, that means a<br />
reduced ability to ventilate lungs, is reduction <strong>of</strong> the FEV1 value.<br />
A low degree <strong>of</strong> the obstructive ventilation defect is considered a reduction <strong>of</strong><br />
the FEV1 value from 60 % to the bottom limit <strong>of</strong> the st<strong>and</strong>ard, respectively to 80%<br />
<strong>of</strong> the st<strong>and</strong>ard reference value.<br />
A medium severe degree is considered a FEV1 reduction from 45 % to 59 % <strong>of</strong><br />
the reference value,<br />
a severe degree is then a FEV1 reduction under 45 %.<br />
These criteria are accurate enough only in the case that FEV1/VC index is lower<br />
than the bottom limit <strong>of</strong> the st<strong>and</strong>ard (approximately 60 % <strong>and</strong> depends on age ).
Common Obstructive Lung Diseases<br />
Asthma<br />
COPD (chronic bronchitis, emphysema <strong>and</strong> the overlap between them)<br />
Cystic fibrosis<br />
-Airflow is reduced because the airways narrow <strong>and</strong> the FEV1 is reduced<br />
-Spirogram may continue to rise for more than 6 seconds because lung take<br />
longer to empty<br />
-FVC may also be reduced because gas is trapped behind obstructed bronchi but<br />
this reduction to a lesser extent than FEV1<br />
Asthma is characterized by airway<br />
hyperresponsiveness, which results in reversible<br />
increases in bronchial smooth muscle tone, <strong>and</strong><br />
variable amounts <strong>of</strong> inflammation <strong>of</strong> the bronchial<br />
mucosa.During an acute<br />
asthma attack, the already<br />
inflamed airways narrow<br />
further due to bronchospasm,<br />
which leads to increased<br />
airway resistance<br />
COPD<br />
http://www.youtube.com/watch?v=aktIMBQSXMo
Large Airway Obstruction<br />
1. Fixed obstruction<br />
2. Variable extrathoracic obstruction<br />
3. Variable intrathoracic obstruction<br />
Fixed obstruction<br />
1. Post intubation stenosis<br />
2. Endotracheal neoplasms<br />
3. Bronchial stenosis<br />
Maximum airflow is limited to a similar extent in both inspiration <strong>and</strong> expiration<br />
Variable extrathoracic Obstruction<br />
1. Bilateral <strong>and</strong> unilateral vocal cord paralysis<br />
2. Vocal cord constriction<br />
3. Airway burns<br />
The obstruction worsens in inspiration because the negative <strong>pressure</strong> narrows the<br />
trachea <strong>and</strong> inspiratory flow is reduced to a greater extent than expiratory flow<br />
Large Airway Obstruction<br />
In variable intrathoracic obstruction<br />
1. Tracheomalacia<br />
2. Polychondritis<br />
3. Tumors <strong>of</strong> the lower trachea or main bronchus.<br />
The narrowing is maximal in expiration because <strong>of</strong> increased intrathoracic <strong>pressure</strong><br />
compressing the airway.<br />
The flow volume loop shows a greater reduction in the expiratory phase
Restrictive ventilation defect<br />
With a classic restrictive ventilation defect during forced expiration, the patient<br />
expires a smaller air volume from lungs <strong>and</strong> this happens at normal or only slightly<br />
lower speed.<br />
The criterion for a restrictive ventilation defect for a tentative screening<br />
examination <strong>of</strong> a lung function is a lower absolute value <strong>of</strong> the vital capacity VC with<br />
normal values <strong>of</strong> FEV1/VC or FEV1/FVC indexes.<br />
The vital capacity is considered lower if its value drops under 80 % <strong>of</strong> the reference<br />
value.<br />
When assessing seriousness, a low degree <strong>of</strong> RVD is considered a VC reduction<br />
from 60 % to the bottom limit <strong>of</strong> the st<strong>and</strong>ard, respectively to 80 % <strong>of</strong> the reference<br />
value.<br />
A medium severe degree <strong>of</strong> RVP is considered a VC reduction from 45 % to x60<br />
%,<br />
a severe degree <strong>of</strong> RVP is considered a reduction under 45 %.<br />
Restrictive Lung Diseases<br />
A. Intrinsic Restrictive Lung Disorders<br />
Sarcoidosis<br />
Idiopathic pulmonary fibrosis<br />
Interstitial pneumonitis<br />
Tuberculosis<br />
Pnuemonectomy (loss <strong>of</strong> lung)<br />
Pneumonia<br />
B. Extrinsic Restrictive Lung Disorders<br />
Scoliosis, Kyphosis<br />
Ankylosing Spondylitis<br />
Pleural Effusion<br />
Pregnancy<br />
Gross Obesity<br />
Tumors<br />
Ascites<br />
Pain on inspiration - pleurisy, rib fractures
Restrictive Lung Diseases<br />
C. Neuromuscular Restrictive Lung Disorders<br />
Generalized Weakness – malnutrition<br />
Paralysis <strong>of</strong> the diaphragm<br />
Myasthenia Gravis<br />
Muscular Dystrophy<br />
Poliomyelitis<br />
Amyotrophic Lateral Sclerosis<br />
Restrictive Lung Diseases<br />
Restrictive lung disease :<br />
Full lung expantion is prevented by fibrotic<br />
tissue in the lung parenchyma <strong>and</strong> the FVC<br />
is reduced .<br />
Elastic recoil may increased by fibrotic<br />
tissue lead to increase the airflow<br />
Both FEV1 <strong>and</strong> FVC may be reduced<br />
because the lungs are small <strong>and</strong> stiff ,but<br />
the peak expiratory flow may be preserved<br />
or even higher than predicted leads to<br />
tall,narrow <strong>and</strong> steep flow volume loop in<br />
expiratory phase.
A combined, restrictively – obstructive ventilation defect<br />
reduced FVC <strong>and</strong> also FEV1 but the FEV1 is lowered disproportionately more<br />
than the FVC <strong>and</strong> therefore the FEV1/FVC ratio is also lower.<br />
Parameter<br />
Obstruction<br />
Restriction<br />
Mixed<br />
FEV1<br />
Reduced<br />
Reduced<br />
Reduced<br />
FVC<br />
Normal<br />
Reduced<br />
Reduced<br />
FEV1/FVC<br />
Reduced<br />
Normal<br />
Reduced
Age :<br />
FVC <strong>and</strong> flow rates decline with age. The value <strong>of</strong> FVC increases up to 24<br />
years <strong>of</strong> age <strong>and</strong> remain stable to age 35.<br />
-Elastic tissues deteriorate:<br />
reducing lung compliance<br />
lowering vital capacity<br />
-Arthritic changes:<br />
restrict chest movements<br />
limit respiratory minute volume<br />
-Emphysema:<br />
affects individuals over age 50<br />
depending on exposure to respiratory irritants (e.g., cigarette smoke)<br />
Height :<br />
All spirometric measurements increase with body weight. It is due to an<br />
increase in number <strong>and</strong>/or size <strong>of</strong> alveoli relative to airways, the larger lungs<br />
are likely to take longer than smaller one.<br />
Sex :<br />
Most pulmonary function values are lower in female than male.<br />
Weight :<br />
A spirometric results are positively correlated with weight to the extent that<br />
increased weight means growth or muscle mass. Beyond this (in obesity)<br />
spirometric values (<strong>and</strong> lung values specially ERV) decrease with greater<br />
weight.<br />
Instrumentation for measuring lung ventilation – volumes, airflows<br />
- Bell spirometers – closed system<br />
- Pneumotachographs with volume - flow integration – open system<br />
- Whole-body plethysmograph<br />
Pneumo comes from Greek <strong>and</strong> means lungs, so that the pneumograph is an instrument which gives a<br />
graph <strong>of</strong> lung function; this is actually a graph <strong>of</strong> lung volume against lime. Tacho is also a Greek word <strong>and</strong><br />
means speed so that the pneumotachograph produces a graph <strong>of</strong> the speed <strong>of</strong> airflow into or out <strong>of</strong> the<br />
lungs. Spiro is the Latin word meaning breath so that the spirometer is an instrument which measures<br />
breath. The measurement is usually <strong>of</strong> volume. Pletho is another Greek word meaning fullness so that the<br />
plethysmograph is an instrument which gives a graph <strong>of</strong> fullness. The body plethysmograph gives a<br />
measurement <strong>of</strong> lung fullness.
Bell spirometers – closed system<br />
http://ulb.upol.cz/videa/spirometry.mpg<br />
An inverted cylindrical container floats in a liquid<br />
<strong>and</strong> the volume <strong>of</strong> gas in the container can be<br />
calculated from the vertical displacement <strong>of</strong> the<br />
cylinder.<br />
Actually a correction factor has to be applied to<br />
allow for the fact that the air cools <strong>and</strong> thus<br />
contracts when it passes from the patient into<br />
the spirometer.<br />
Pneumotachographs with volume - flow integration – open system<br />
measures flow rate by means <strong>of</strong> a transducer through which the patient breathes.<br />
The air passes through a fine mesh which <strong>of</strong>fers a small resistance to flow, with the<br />
result that there will be a <strong>pressure</strong> drop across the mesh in proportion to the flow<br />
rate.<br />
the instrument also calculates volume by integrating the flow signal
FORCED EXPIRATION TEST<br />
http://www.nationalasthma.org.au/HTML/management/spiro_res/vid_spiro.asp<br />
FORCED EXPIRATION TEST<br />
http://www.nationalasthma.org.au/HTML/management/spiro_res/vid_spiro.asp
Whole-body plethysmograph<br />
A body plethysmograph consists <strong>of</strong> a box in<br />
which the patient sits <strong>and</strong> breathes through<br />
a hole in the side. Each time the patient<br />
inhales volume V, the total volume <strong>of</strong> <strong>their</strong><br />
body increases <strong>and</strong> so the <strong>pressure</strong> in the<br />
box increases. If the initial <strong>pressure</strong> in the<br />
box, Pb, <strong>and</strong> the air volume, Vb, are known,<br />
then the reduction in volume, V, can be<br />
calculated from the <strong>pressure</strong> rise, p, during<br />
inspiration.<br />
Boyle’s law (P · V = constant)<br />
PbVb = (Pb+p)(Vb-V)<br />
Residual Volume Measurement<br />
• Helium dilution<br />
• Spirometer <strong>of</strong> known volume <strong>and</strong><br />
helium concentration connected to the<br />
patient<br />
• Closed circuit<br />
• Law <strong>of</strong> conservation <strong>of</strong> mass<br />
At beginning<br />
After several minutes<br />
[He] initial · V s = [He] final · (V s + V L )<br />
Unknown lung volume can be calculated<br />
We solve for the volume after (the volume <strong>of</strong> the lung <strong>and</strong> spirometer), subtract out<br />
the volume <strong>of</strong> the spirometer, <strong>and</strong> we get the volume <strong>of</strong> the lung.<br />
Helium poorly soluble in water <strong>and</strong> thus diffuses very poorly across the alveolar wall.<br />
Subjects breath a gas that cannot escape from the lungs
RESIDUAL VOLUME<br />
RV = FRC - ERV<br />
Peak-flow meter<br />
Peak-flow meters are instruments used to measure peak expiratory flow rate<br />
(PEFR).<br />
The patient expires as forcefully as possible into the flowmeter which balances the<br />
<strong>pressure</strong> exerted by the flow <strong>of</strong> air past a movable vane against a spiral spring.