Marymount Care Centre, 65, nursing home inspection report - hiqa.ie
Marymount Care Centre, 65, nursing home inspection report - hiqa.ie
Marymount Care Centre, 65, nursing home inspection report - hiqa.ie
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
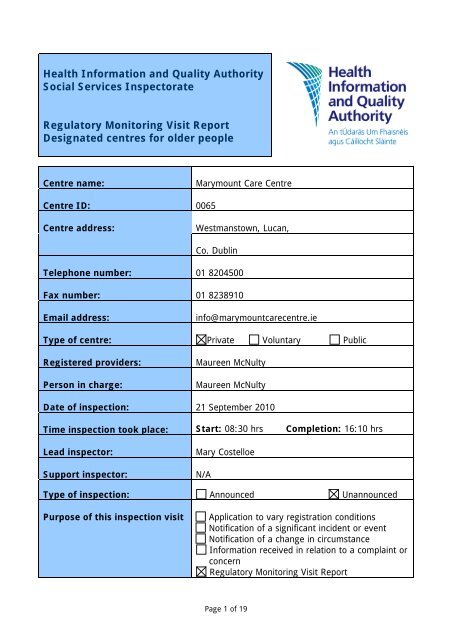
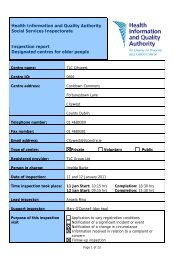
Health Information and Quality Authority<br />
Social Services Inspectorate<br />
Regulatory Monitoring Visit Report<br />
Designated centres for older people<br />
<strong>Centre</strong> name:<br />
<strong>Marymount</strong> <strong>Care</strong> <strong>Centre</strong><br />
<strong>Centre</strong> ID: 00<strong>65</strong><br />
<strong>Centre</strong> address:<br />
Westmanstown, Lucan,<br />
Co. Dublin<br />
Telephone number: 01 8204500<br />
Fax number: 01 8238910<br />
Email address:<br />
info@marymountcarecentre.<strong>ie</strong><br />
Type of centre: Private Voluntary Public<br />
Registered providers:<br />
Person in charge:<br />
Maureen McNulty<br />
Maureen McNulty<br />
Date of <strong>inspection</strong>: 21 September 2010<br />
Time <strong>inspection</strong> took place: Start: 08:30 hrs Completion: 16:10 hrs<br />
Lead inspector:<br />
Support inspector:<br />
Mary Costelloe<br />
N/A<br />
Type of <strong>inspection</strong>: Announced Unannounced<br />
Purpose of this <strong>inspection</strong> visit<br />
Application to vary registration conditions<br />
Notification of a significant incident or event<br />
Notification of a change in circumstance<br />
Information received in relation to a complaint or<br />
concern<br />
Regulatory Monitoring Visit Report<br />
Page 1 of 19
About the <strong>inspection</strong><br />
The purpose of <strong>inspection</strong> is to gather evidence on which to make judgments about the<br />
fitness of the registered provider and to <strong>report</strong> on the quality of the service. This is to<br />
ensure that providers are complying with the requirements and conditions of their<br />
registration and meet the Standards, that they have systems in place to both safeguard<br />
the welfare of service users and to provide information and evidence of good and poor<br />
practice.<br />
In assessing the overall quality of the service provided, inspectors examine how well the<br />
provider has met the requirements of the Health Act 2007, the Health Act 2007 (<strong>Care</strong> and<br />
Welfare of Residents in Designated <strong>Centre</strong>s for Older People) Regulations 2009 (as<br />
amended) and the National Quality Standards for Residential <strong>Care</strong> Settings for Older<br />
People in Ireland.<br />
Additional <strong>inspection</strong>s take place under the following circumstances:<br />
• to follow up on specific matters arising from a previous <strong>inspection</strong> to ensure that<br />
the action required of the provider has been taken<br />
• following a change in circumstances; for example, following a notification to the<br />
Health Information and Quality Authority’s Social Services Inspectorate that a<br />
provider has appointed a new person in charge<br />
• arising from a number of events including information received in relation to a<br />
concern/complaint or notification to the SSI of a significant event affecting the<br />
safety or well-being of residents<br />
• for centres that have not previously been inspected within a specific timeframe, a<br />
one-day regulatory monitoring visit may be carr<strong>ie</strong>d out to focus on key regulatory<br />
requirements.<br />
All <strong>inspection</strong>s can be announced or unannounced, depending on the reason for the<br />
<strong>inspection</strong> and may take place at any time of day or night.<br />
All <strong>inspection</strong> <strong>report</strong>s produced by the Health Information and Quality Authority will be<br />
published. However, in cases where legal or enforcement activity may arise from the<br />
findings of an <strong>inspection</strong>, the publication of a <strong>report</strong> will be delayed until that activity is<br />
resolved. The reason for this is that the publication of a <strong>report</strong> may prejudice any<br />
proceedings by putting evidence into the public domain.<br />
Page 2 of 19
About the centre<br />
Description of services and premises<br />
<strong>Marymount</strong> <strong>Care</strong> <strong>Centre</strong> is a purpose-built, two-storey building which opened in 1987. It<br />
was extended and refurbished in 2008 and has places for 91 residents. At the time of<br />
<strong>inspection</strong> there were 84 residents living in the centre; two residents were under <strong>65</strong> years<br />
of age and some residents had dementia.<br />
The building is set in a large, landscaped site. The main entrance is to the front of the<br />
building which opens into a central reception area. The centre is made up of two sections,<br />
namely the Maple and the Orchard. The Maple is a single-storey section to the left of the<br />
main reception area, while the Orchard is two- storey and on the right.<br />
There are 37 single bedrooms with en suite shower and toilets, 11 twin bedrooms with<br />
shower and toilet en suite, and four single and two twin bedrooms without en suite<br />
facilit<strong>ie</strong>s on the ground floor. There are 14 single and five twin bedrooms, all with en suite<br />
toilet and shower on the first floor. The centre has six additional assisted bathrooms with<br />
specialised baths located throughout the building.<br />
There are a var<strong>ie</strong>ty of communal spaces throughout the building, including four sitting<br />
rooms, a library, as well as several seating alcoves and a computer workstation area. The<br />
main dining room is on the ground floor of the Orchard area beside the kitchen and<br />
additional dining areas are also provided in the Maple and Orchard areas. Residents also<br />
have access to the ground floor oratory, shop, gymnasium, hairdressing and therapy<br />
rooms.<br />
Residents have access to several garden and outdoor seating areas. There are two<br />
enclosed secure garden areas, a sensory garden, roof terrace and balcony. Residents can<br />
also go out into the extensive landscaped grounds surrounding the building.<br />
There are two lifts and three staircases between floors. There is a nurses’ station,<br />
kitchenette, sluice cum utility room provided in each area and on each floor. The laundry<br />
is on the first floor.<br />
The building is wheelchair accessible throughout. There is adequate parking for staff and<br />
visitors provided around the building.<br />
Location<br />
The centre is located approximately two kilometres from Lucan village in County Dublin.<br />
There is a bus stop at the main entrance.<br />
Date centre was first established: 1987<br />
Number of residents on the date of<br />
<strong>inspection</strong> 84<br />
Page 3 of 19
Dependency level of<br />
current residents<br />
Max High Medium Low<br />
Number of residents 22 20 27 15<br />
Management structure<br />
The Provider and Person in Charge is Maureen McNulty and she is referred to as the<br />
Person in Charge throughout the <strong>report</strong>. Fergus McNulty, the Financial Director, Kay<br />
Downey-Ennis the Quality and Education Director, Conor McNulty the Business Manager<br />
and Karla Walsh the Assistant Director of Nursing (ADON) form the management team<br />
who all <strong>report</strong> directly to the Person in Charge. Clinical Nurse Managers (CNMs), staff<br />
nurses and care assistants <strong>report</strong> to the ADON who in turn <strong>report</strong>s to the Person in<br />
Charge. Housekeeping and catering staff <strong>report</strong> directly to their manager/supervisor who<br />
in turn <strong>report</strong> to the Business Manager.<br />
Staff<br />
designation<br />
Number of<br />
staff on duty<br />
on day of<br />
<strong>inspection</strong><br />
Person<br />
in<br />
Charge<br />
Nurses<br />
<strong>Care</strong><br />
staff<br />
Catering<br />
staff<br />
Cleaning<br />
and<br />
laundry<br />
staff<br />
Admin<br />
staff<br />
Other<br />
staff<br />
1 6 13 4 7 * 6<br />
* Other staff working on the day of <strong>inspection</strong> included: I Receptionist, 2 Maintenance, 1<br />
Activit<strong>ie</strong>s coordinator, 1 Business Manager, I Director of Quality and Education.<br />
Page 4 of 19
Summary of findings from this <strong>inspection</strong><br />
This was the first <strong>inspection</strong> carr<strong>ie</strong>d out by the Health Information and Quality Authority<br />
(the Authority) and it was an unannounced regulatory monitoring <strong>inspection</strong>. The<br />
inspector focussed on key regulatory requirements of governance, resident care and<br />
environment to assess the extent to which the management of care ensured positive and<br />
safe outcomes for residents.<br />
The inspector met with residents, relatives, ADON, business manager, director of quality<br />
and education, CNM, staff nurses, and other members of staff. Records examined included<br />
staff rotas, register of residents, written polic<strong>ie</strong>s on health and safety as well as fire safety<br />
records and accident/incident <strong>report</strong> forms.<br />
On the day of <strong>inspection</strong>, the inspector was satisf<strong>ie</strong>d that residents received a good quality<br />
of care in a safe environment and that their <strong>nursing</strong> and healthcare needs were being met.<br />
Some improvements were required to update the register of residents and finalise the<br />
emergency plan.<br />
These areas for improvement are addressed in the Action Plan at the end of the <strong>report</strong>.<br />
Page 5 of 19
Comments by residents and relatives<br />
The inspector spoke with a number of residents and some relatives during the <strong>inspection</strong>.<br />
Residents were satisf<strong>ie</strong>d with the level of care they received, commenting “Everything is<br />
great here, no complaints at all”, “We are all very happy here”.<br />
Residents were complimentary about the staff, stating that staff were very kind and<br />
caring; comments included “Staff are very good and very caring” and “Everybody is lovely<br />
here”. Residents and relatives spoken to said that all staff were very approachable and<br />
they listened to what was being said.<br />
Residents told the inspector that the centre was family run, comments included “The<br />
person in charge and her family are always here, they are very approachable, they have a<br />
presence here all of the time”.<br />
Residents were satisf<strong>ie</strong>d with meals, choice of food and portion sizes. They stated that the<br />
food was always very good, and that they could have whatever they wanted.<br />
Many residents spoken to said that they enjoyed the var<strong>ie</strong>ty of activit<strong>ie</strong>s available,<br />
commenting that “we have lots to do, we are kept busy”. Residents told the inspector that<br />
they can choose to do as they wish, for example, get up and go to bed when they wish,<br />
have meals in the dining room or in their bedroom and receive visitors at any time.<br />
Relatives stated that the ethos of care was very good: “During the bad weather some staff<br />
stayed over in case staff could not get to work in the morning”. “This is like a <strong>home</strong> from<br />
<strong>home</strong>”, and “There is always something going on, we have had lovely days as a family<br />
here”.<br />
Page 6 of 19
Governance<br />
Article 5: Statement of Purpose<br />
The person in charge had submitted the statement of purpose in advance of the<br />
<strong>inspection</strong> which had been developed in accordance with the requirements of the<br />
Regulations. It reflected the categor<strong>ie</strong>s of care provided at the time of <strong>inspection</strong>. Most<br />
residents were over <strong>65</strong> years of age with general care needs and many had dementia.<br />
There were two residents under <strong>65</strong> years of age, one of whom was receiving respite care.<br />
Article 15: Person in Charge<br />
The person in charge worked full-time. She had 22 years management exper<strong>ie</strong>nce of<br />
operating a designated centre and was on leave at the time of <strong>inspection</strong>. The inspector<br />
spoke with the ADON who deputised in the absence of the person in charge. She told the<br />
inspector that she and the person in charge were on call at week ends and out-of-hours<br />
and that both are rostered on-duty on alternative weekends.<br />
The ADON told the inspector that there was a CNM on-duty each day and that there was<br />
always a senior nurse on-duty to supervise the delivery of care. Staff spoken to and<br />
staffing rotas rev<strong>ie</strong>wed by the inspector confirmed this to be the case.<br />
Article 16: Staffing<br />
The inspector noted that there were adequate numbers of staff on-duty to meet the needs<br />
of residents. The roster showed that there were usually five staff nurses, 13 care<br />
assistants, a clinical nurse manager and the person in charge or ADON on-duty during the<br />
daytime, while two staff nurses and four carers were on-duty at night-time. The assistant<br />
director of <strong>nursing</strong> told the inspector that one care assistant always remained on the first<br />
floor at night-time to attend to residents’ needs. There were adequate catering and<br />
housekeeping staff on-duty. Two activit<strong>ie</strong>s coordinators worked from Monday to Friday<br />
and staffing rotas confirmed this. Staff and residents said they were satisf<strong>ie</strong>d with the<br />
present staffing levels.<br />
All staff spoken to said that they had received mandatory training in fire safety and<br />
evacuation and moving and handling. Training records rev<strong>ie</strong>wed by the inspector indicated<br />
that the majority of staff had received such training and further training was scheduled for<br />
recently recruited staff and to update existing staff. The inspector was shown<br />
documentation indicating that moving and handling training was scheduled to take place<br />
on the 24 September 2010 and fire safety training on the 20 October 2010 and 2<br />
November 2010.<br />
The inspector rev<strong>ie</strong>wed documentation for a number of staff and confirmed that up-todate<br />
registration numbers were recorded for <strong>nursing</strong> staff. Confirmation of Garda Síochána<br />
clearance was in place for most staff and the remaining applications were being<br />
processed.<br />
Page 7 of 19
Article 23: Directory of Residents<br />
The inspector rev<strong>ie</strong>wed the directory of residents and noted that the required details were<br />
not fully completed in the case of a number of residents. The dates of transfer to and from<br />
hospital had not been recorded in the case of one resident.<br />
Article 31: Risk Management Procedures<br />
The inspector found that robust risk management procedures were in place.<br />
The inspector rev<strong>ie</strong>wed the process for recording incidents and accidents. A detailed<br />
clinical incident <strong>report</strong> form was completed for each incident and maintained on the<br />
residents’ file. The incidents were also logged on the computerised system. A root cause<br />
analysis and monthly audit was completed by the director of quality and education. A<br />
matrix had been completed of all residents at high risk of falls. Evidence of learning and<br />
improvements made were documented. For example, sensor mats, chair sensors, floor<br />
sensors and low profile beds were in use for some residents. The inspector rev<strong>ie</strong>wed the<br />
file of a resident who had fallen and noted that the recommendations made by managers<br />
had been documented and implemented. The falls risk assessment had been rev<strong>ie</strong>wed and<br />
an updated care plan was in place.<br />
The inspector rev<strong>ie</strong>wed the risk management policy dated January 2010 and the health<br />
and safety policy dated May 2010. Both were found to be comprehensive; hazards were<br />
identif<strong>ie</strong>d and risks were assessed in-line with the requirements of the Regulations. A<br />
health and safety committee was in place made up of all grades of staff; meetings were<br />
held monthly and issues identif<strong>ie</strong>d were acted upon. The inspector read the minutes of the<br />
last meeting displayed on the staff notice board.<br />
The inspector was shown the draft emergency plan which was in the process of being<br />
finalised. The plan was comprehensive and gave clear guidance to staff on what to do in<br />
the event of a var<strong>ie</strong>ty of emergency situations, including fire, bomb threat, loss of power,<br />
heating failure, flooding and evacuation of residents.<br />
Article 39: Complaints<br />
The inspector rev<strong>ie</strong>wed the complaints policy and found that it was comprehensive. It<br />
contained a quick reference guide to the management of complaints and the details of an<br />
independent appeals process. The complaints procedure was clearly displayed in the<br />
entrance area. A complaints officer had been appointed. Separate forms were available to<br />
document both written and verbal complaints. Complaints were all logged on the<br />
computerised system. The director of quality and education told the inspector that no<br />
written complaints had been received to date this year. She provided details of 24 verbal<br />
complaints and the inspector observed that all complaints had been resolved and closed<br />
off. Most complaints had been resolved quickly. Outcomes and actions taken on foot of<br />
the complaints were documented.<br />
Page 8 of 19
Article 36: Notification of incidents<br />
The assistant director of <strong>nursing</strong> was aware of the legal requirement to notify the Ch<strong>ie</strong>f<br />
Inspector regarding incidents and accidents. To date all relevant incidents had been<br />
notif<strong>ie</strong>d to the Ch<strong>ie</strong>f Inspector by the person in charge.<br />
Page 9 of 19
Resident <strong>Care</strong><br />
Article 9: Health <strong>Care</strong><br />
All residents had access to general practitioner (GP) services and could choose to retain<br />
their own GP if they so wished. There was an out-of-hours service available. The<br />
medication prescribing records checked by the inspector confirmed that all medications<br />
were rev<strong>ie</strong>wed on a three-monthly basis.<br />
The inspector noted that residents had access to a wide range of all<strong>ie</strong>d health<br />
professionals and the records of appointments were maintained in residents’ files.<br />
Physiotherapy was available in-house on a weekly basis and more often if required on<br />
referral from the GP. The d<strong>ie</strong>tician visited residents on a monthly basis and was available<br />
to give advice as required. The chiropodist attended every two weeks and was available<br />
more often if necessary. Occupational therapy (OT) and speech and language therapy<br />
were available on referral from the GP. The optician visited annually and assessed<br />
residents as required. Arrangements were made locally with the dental clinic for residents<br />
requiring dental care. The centre had strong links with the psychiatry of later life team<br />
from Connolly Hospital who visited and were also available for advice.<br />
Article 33: Ordering, Prescribing, Storing and Administration of Medicines<br />
The inspector rev<strong>ie</strong>wed the medication policy which was found to be comprehensive and<br />
gave clear guidance to <strong>nursing</strong> staff on areas such as medication prescribing,<br />
administration and storage.<br />
The inspector spoke to the clinical nurse manager about the medication policy, medication<br />
administering procedures and found her to be knowledgeable in relation to the policy,<br />
legislation and best practice.<br />
Medications requiring strict controls were appropriately stored and managed in a double<br />
locked cupboard in the clinical room. Records indicated that these were counted and<br />
signed by two nurses at each change of shift.<br />
Medications requiring strict temperature control were stored appropriately in a refrigerated<br />
unit in the locked clinical room. The temperature of the refrigerator was monitored and<br />
recorded on a daily basis.<br />
Medication audits were being carr<strong>ie</strong>d out on a six-monthly basis by the pharmacist. The<br />
last audit was completed in March 2010. Documentation rev<strong>ie</strong>wed by the inspector<br />
showed that actions highlighted in the audits had been acted upon and their completion<br />
date had been recorded.<br />
Page 10 of 19
Article 6: General Welfare and Protection<br />
The inspector rev<strong>ie</strong>wed the policy on the prevention and detection of elder abuse dated<br />
February 2010 which was found to be comprehensive. Staff spoken to confirmed that they<br />
had received training in relation to elder abuse and were knowledgeable on the issue.<br />
Training records rev<strong>ie</strong>wed confirmed that the majority of staff had received training in this<br />
area; further training was scheduled for recently recruited staff on 24 September. Two<br />
members of staff had qualif<strong>ie</strong>d as ‘train the trainers’ in the prevention and detection of<br />
elder abuse which meant that all staff could receive in-house training.<br />
There had been one allegation of abuse during the past 12 months. An investigation had<br />
been carr<strong>ie</strong>d out by the director of quality and education and this complaint was not<br />
upheld. The inspector was satisf<strong>ie</strong>d that this allegation had been dealt with appropriately<br />
and in accordance with the policy. The details regarding this complaint had been notif<strong>ie</strong>d<br />
to the Ch<strong>ie</strong>f Inspector.<br />
There were two activit<strong>ie</strong>s coordinators employed and there were a var<strong>ie</strong>ty of activit<strong>ie</strong>s<br />
going on during the <strong>inspection</strong> so that residents had opportunit<strong>ie</strong>s for meaningful<br />
occupation. Staff informed the inspector that a resident assessment and activity plan was<br />
completed for all residents; the inspector observed this in residents’ files. Residents<br />
spoken to said that they enjoyed the var<strong>ie</strong>ty of activit<strong>ie</strong>s taking place, such as baking,<br />
painting, quizzes, music, bingo, arts and crafts. Many told the inspector that they enjoyed<br />
outings during the summer to the ‘Titanic’ exhibition, the Guinness brewery, Newbridge<br />
Silver and the Concert Hall as well as garden part<strong>ie</strong>s and treasure hunts on the grounds.<br />
Staff informed the inspector that they were presently in the process of developing a ‘My<br />
life history book’ for all residents. Staff had completed it for some residents and said that<br />
they found it beneficial, particularly when reminiscing with residents who had dementia.<br />
Article 20: Food and Nutrition<br />
The inspector observed that residents were offered a var<strong>ie</strong>d and nutritious d<strong>ie</strong>t. Some<br />
residents required special d<strong>ie</strong>ts or a modif<strong>ie</strong>d consistency d<strong>ie</strong>t and their needs were met.<br />
The quality, choice and presentation of the meals were of a high standard and residents<br />
confirmed this. Residents were offered a daily choice at lunch and evening meals. The<br />
daily menu was displayed in the dining room. The inspector met with the chef who was<br />
able to show documentation about residents’ likes, dislikes, special d<strong>ie</strong>tary needs and<br />
recommendations from the d<strong>ie</strong>tician. There was a four-weekly rolling menu and the chef<br />
told the inspector that residents’ preferences were taken into account when compiling<br />
them. She said that she regularly chatted with residents and asked them if there was<br />
anything that they would like. Residents confirmed this, saying that they could have<br />
anything they wish.<br />
The inspector noted that all residents were offered a var<strong>ie</strong>ty of drinks with their meals and<br />
were encouraged to take drinks throughout the day. Kitchenettes were located in each<br />
area and on each floor. Residents confirmed that they could have drinks and refreshments<br />
as desired.<br />
Page 11 of 19
The clinical nurse manager told the inspector that all residents were nutritionally assessed<br />
using a validated tool and that their weights were routinely recorded on a monthly basis.<br />
She stated that residents who were nutritionally at risk were weighed more often. The<br />
inspector rev<strong>ie</strong>wed some residents’ files and nutritional assessments and monthly weights<br />
were recorded. The inspector noted that a resident who had been losing weight had been<br />
referred to the d<strong>ie</strong>tician and to the GP.<br />
The d<strong>ie</strong>tician’s recommendations were documented and the care plan reflected the<br />
recommendations made. The chef was aware of these recommendations and had a copy<br />
on file in the kitchen. The GP had also prescribed drink supplements.<br />
Page 12 of 19
Environment<br />
Article 19: Premises<br />
The building was found to be clean and bright throughout. The front entrance reception<br />
area was welcoming and was carpeted and furnished with comfortable chairs. There were<br />
lamps, side tables, framed wall pictures, a fire place and vases of fresh flowers in this<br />
area. The receptionist sat at the reception desk and the inspector noted that residents<br />
chatted with the receptionist as they passed by.<br />
The design of the building was suitable for its purpose. The circulation areas, such as<br />
corridors, were wide and allowed plenty of space for wheelchair access. The building was<br />
designed around two internal garden courtyards; the gardens were easily accessible from<br />
the corridors and day areas. The gardens were landscaped and well maintained with a<br />
var<strong>ie</strong>ty of outdoor furniture provided for residents’ use. Residents could access the sensory<br />
garden which also housed a chicken coup for interest and stimulation.<br />
There was a var<strong>ie</strong>ty of day areas provided; the rooms were comfortably furnished and<br />
domestic in character. Residents could also sit and relax in the front hallway, the library<br />
and outdoor verandas. The inspector saw residents using all the day areas and some<br />
residents confirmed that they enjoyed the v<strong>ie</strong>ws of the gardens.<br />
Bedroom accommodation met residents’ needs for privacy, leisure and comfort. All<br />
bedrooms were spacious and furnished with high quality coordinating curtains and bed<br />
linen. The décor and colour schemes created a restful, relaxing environment. There were<br />
specialised beds, ample personal storage space, screens in shared rooms, wall mounted<br />
TV, telephone line, internet access, nurse call bell facilit<strong>ie</strong>s and a var<strong>ie</strong>ty of armchairs.<br />
Residents had personalised their own rooms with furniture, photographs and religious<br />
ornaments.<br />
The inspector visited the kitchen and found it to be clean, spacious and well-equipped.<br />
Separate staff toilet and changing facilit<strong>ie</strong>s were provided for catering staff.<br />
The inspector noted that infection control practices in hand hyg<strong>ie</strong>ne were robust. Wall<br />
mounted dispensers containing hand sanitising gel were located at the front entrance and<br />
throughout the building. Wash-hand basins were provided for staff on the corridors<br />
adjacent to bedroom areas. Suitable signage was in place reminding people to wash their<br />
hands and use the sanitisers; staff were observed to be vigilant in their use.<br />
The front door was fitted with a coded key pad. The door leading to the Maple area was<br />
also fitted with a coded key pad to ensure additional security for residents with dementia.<br />
The inspector had a concern that the doors to the sluice/utility rooms were open. Cleaning<br />
chemicals and equipment were stored in these areas and posed a potential risk to<br />
residents and visitors.<br />
Page 13 of 19
Article 32: Fire Precautions and Records<br />
The inspector rev<strong>ie</strong>wed fire polic<strong>ie</strong>s and procedures. Records indicated that all fire fighting<br />
equipment had been serviced in January 2010 and the fire alarm had been serviced in<br />
June 2010. Fire orders were displayed throughout the centre and all means of escape<br />
were found to be unobstructed. Staff interv<strong>ie</strong>wed were knowledgeable on what to do in<br />
the event of fire. The last fire drill and fire training took place in September 2010. Two<br />
recently recruited staff had not received fire safety training, this training was scheduled for<br />
20 October 2010.<br />
Page 14 of 19
Closing the visit<br />
At the close of the <strong>inspection</strong> visit a feedback meeting was held with deputy person in<br />
charge, business manager and director of quality and education to <strong>report</strong> on the<br />
inspector’s findings, which highlighted both good practice and where improvements were<br />
needed.<br />
Acknowledgements<br />
The inspectors wish to acknowledge the cooperation and assistance of the residents,<br />
relatives, provider and staff during the <strong>inspection</strong>.<br />
Report compiled by:<br />
Mary Costelloe<br />
Inspector of Social Services<br />
Social Services Inspectorate<br />
Health Information and Quality Authority<br />
22 September 2010<br />
Page 15 of 19
Health Information and Quality Authority<br />
Social Services Inspectorate<br />
Action Plan<br />
Provider’s response to <strong>inspection</strong> <strong>report</strong><br />
<strong>Centre</strong>:<br />
<strong>Marymount</strong> <strong>Care</strong> <strong>Centre</strong><br />
<strong>Centre</strong> ID: 00<strong>65</strong><br />
Date of <strong>inspection</strong>: 21 September 2010<br />
Date of response: 20 October 2010<br />
Requirements<br />
These requirements set out what the registered provider must do to meet the Health Act<br />
2007, the Health Act 2007 (<strong>Care</strong> and Welfare of Residents in Designated <strong>Centre</strong>s for Older<br />
People) Regulations 2009 (as amended) and the National Quality Standards for Residential<br />
<strong>Care</strong> Settings for Older People in Ireland.<br />
1. The person in charge has failed to comply with a regulatory requirement in<br />
the following respect:<br />
The directory of residents did not contain the required details as required by the<br />
Regulations.<br />
Action required:<br />
Ensure that the directory of residents includes the information specif<strong>ie</strong>d in schedule 3 of<br />
the Regulations.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 23: Directory of Residents<br />
Standard 32: Register and Residents’ Records<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Timescale:<br />
Page 16 of 19
Provider’s response:<br />
The directory of residents is now updated and maintained as per<br />
Schedule 3 of the Regulations.<br />
Complete<br />
2. The provider has failed to comply with a regulatory requirement in the<br />
following respect:<br />
The emergency plan was in draft format and had not been finalised.<br />
Action required:<br />
Ensure that there is an emergency plan in place for responding to emergenc<strong>ie</strong>s.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 31: Risk Management Procedures<br />
Standard 26: Health and Safety<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Timescale:<br />
Provider’s response:<br />
The emergency plan has been finalised and is now in place.<br />
Complete<br />
3. The provider has failed to comply with a regulatory requirement in the<br />
following respect:<br />
Cleaning chemicals were stored in the unlocked sluice rooms on both floors.<br />
Action required:<br />
Ensure that a comprehensive risk management policy is in place that covers the<br />
identification and assessment of all risks throughout the centre.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 31: Risk Management Procedures<br />
Standard 26: Health and Safety<br />
Please state the actions you have taken or are planning to<br />
take following the <strong>inspection</strong> with timescales:<br />
Timescale:<br />
Page 17 of 19
Provider’s response:<br />
The comprehensive risk management policy which was in place at the<br />
time of <strong>inspection</strong> has been amended to include ‘the storage of<br />
household chemicals are maintained under a locked coded system’.<br />
Complete<br />
Page 18 of 19
Any comments the provider may wish to make:<br />
Provider’s response:<br />
On behalf of the management and staff of <strong>Marymount</strong> <strong>Care</strong> <strong>Centre</strong> we wish to express our<br />
thanks to the Inspector for her professionalism and courtesy shown during the <strong>inspection</strong><br />
visit.<br />
Provider’s name: Maureen McNulty<br />
Date: 20 October 2010<br />
Page 19 of 19