Andrew's wish list - University Hospital Southampton NHS ...
Andrew's wish list - University Hospital Southampton NHS ...
Andrew's wish list - University Hospital Southampton NHS ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
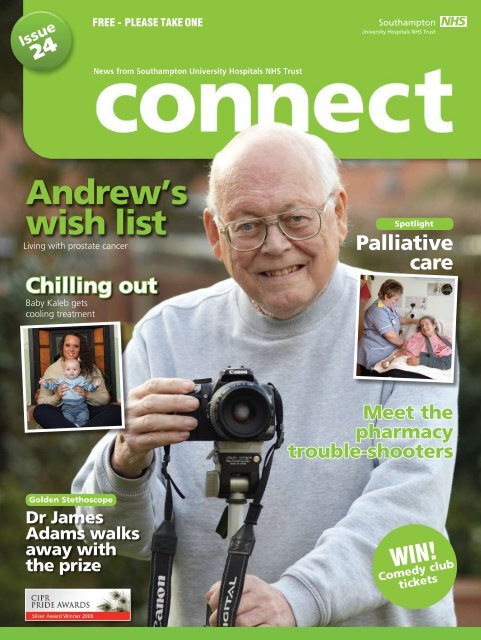
Issue<br />
24<br />
FREE - PLEASE TAKE ONE<br />
News from <strong>Southampton</strong> <strong>University</strong> <strong>Hospital</strong>s <strong>NHS</strong> Trust<br />
Andrew’s<br />
<strong>wish</strong> <strong>list</strong><br />
Living with prostate cancer<br />
Chilling out<br />
Baby Kaleb gets<br />
cooling treatment<br />
Spotlight<br />
Palliative<br />
care<br />
Meet the<br />
pharmacy<br />
trouble-shooters<br />
Golden Stethoscope<br />
Dr James<br />
Adams walks<br />
away with<br />
the prize<br />
WIN!<br />
Comedy club<br />
tickets
Welcome to issue 24 of Connect<br />
Connect has been given a fresh new look for 2010 which we hope our readers will approve of.<br />
As always, the magazine is jam-packed with patient stories, latest hospital news, behind-the-scenes features and all<br />
your regular favourites like Golden Stethoscope and Getting to Know.<br />
From this issue, we will also be publishing patient feedback (see back page).<br />
mediamonitor<br />
the latest SUHT news<br />
Reproduced with kind permission of the Southern Daily Echo<br />
MediaMonitor<br />
First ceramic skull<br />
implant in UK<br />
Consultant neurosurgeon Tony Belli has carried out a pioneering operation<br />
to replace part of a patient’s skull with a ceramic implant.<br />
PC Linda Butt underwent surgery after she was diagnosed with five brain<br />
tumours and Mr Belli needed to remove part of her skull to get to them.<br />
Linda is still receiving treatment<br />
for two tumours, but the<br />
ceramic implant means<br />
doctors can monitor them –<br />
a metal plate would have<br />
blocked images.<br />
It will also knit<br />
together with the<br />
remaining bone.<br />
Mr Belli said: “It is so<br />
much like natural bone<br />
in that if you fracture<br />
it, it will heal over<br />
and, in time, the<br />
bone will grow into<br />
the ceramic and<br />
knit together.”<br />
MediaMonitor<br />
This story was covered by The Sun, the Daily Mail, BBC South Today, BBC Radio<br />
Solent, BBC Hampshire Online.<br />
MediaMonitor<br />
MediaMonitor<br />
Secret agents<br />
They are the taskforce set to ensure<br />
the children’s wards are kept in tip-top<br />
condition…child secret agents. A new army<br />
of recruits, selected from young patients<br />
aged seven and above, are supplied with a<br />
disposable camera, hi-tech voice-recording<br />
pen, shades and a magnifying glass to carry<br />
out their top-secret mission to keep up<br />
hospital standards. They photograph and<br />
note down anything of interest during their<br />
stay and report back on what is being done<br />
well or what needs improving.<br />
This story was covered by Teletext, The Coast FM, Heart<br />
FM and the Southern Daily Echo.<br />
MediaMonitor<br />
Emergency department<br />
team make Christmas<br />
headlines<br />
The team at <strong>Southampton</strong><br />
General <strong>Hospital</strong>’s emergency<br />
department team made national<br />
headlines at Christmas with<br />
their bid to prevent a raft of<br />
common festive injuries.<br />
Consultant Dr John Heyworth<br />
warned of the dangers of carving<br />
the Christmas turkey while drunk<br />
and elderly relatives choking on<br />
the traditional holiday meat.<br />
“Every Christmas without fail, we see the same injuries caused by<br />
preparing and cooking the Christmas dinner,” he said.<br />
“People are likely to burn themselves on the oven or cut themselves as<br />
they carve the turkey – particularly if they have been drinking alcohol.”<br />
Eye casualty sister Emma Powditch urged caution when pulling presents<br />
from under the tree to avoid scratches to the eyeball and popping<br />
champagne corks near eyes, which can cause significant bruising and swelling<br />
to eyelids after impact.<br />
Among the more unusual problems seen by Emma and her colleagues<br />
over the years have been burns and swelling of the eyes cased by exploding<br />
Christmas lights, zips caught on eyelids when trying on new clothes, and<br />
injuries from snowballs with hidden stones.<br />
MediaMonitor<br />
This story was covered by the Daily Mail, The Daily Telegraph, The Sun, BBC News<br />
Online, the Daily Express, Marie Claire, The Scotsman, the Daily Echo, Galaxy FM,<br />
Absolute Radio and BBC Radio Solent.<br />
Top docs on<br />
rescue mission<br />
<strong>Southampton</strong>’s teaching hospitals supported the immediate response relief<br />
efforts in the earthquake-ravaged island of Haiti by releasing two doctors<br />
for deployment. Dr Nick Maskery, emergency department consultant, and<br />
Dr Rob Dawes, specia<strong>list</strong> registrar in anaesthetics and intensive care, both<br />
flew out to support search and rescue missions. Dr Maskery was involved<br />
with the high profile rescue of Sonia Fleury, reported in The Times, who was<br />
found nearly 100 hours after the earthquake struck.<br />
Tell Michelle…<br />
We want to know what you think of your new-look Connect. Contact internal communications manager Michelle<br />
Harris with your comments, along with any news or feature ideas for future issues. Feedback can be sent via:<br />
Email: connect@suht.swest.nhs.uk<br />
Post: Communications, Mailpoint 18, <strong>Southampton</strong> General <strong>Hospital</strong>, Tremona Road <strong>Southampton</strong> SO16 6YD<br />
Telephone: 023 8079 4853<br />
Website: www.suht.nhs.uk<br />
CONNECT<br />
2 ISSUE 24<br />
Connect is produced by SUHT’s communications team. Printed on environmentally friendly paper.
Kaleb’s<br />
a cool<br />
customer<br />
After making a traumatic entrance into the<br />
world, baby Kaleb was given time to chill out.<br />
The tot was among the first babies<br />
at Princess Anne <strong>Hospital</strong> to receive<br />
a new hi-tech cooling treatment to<br />
prevent brain damage.<br />
As a SUHT employee, Larelle<br />
Jauncey, 19, from Shirley in<br />
<strong>Southampton</strong>, knows the Princess<br />
Anne better than most first-time<br />
mums – but she didn’t expect to<br />
spend so much time there after giving<br />
birth to Kaleb.<br />
She said: “My pregnancy had been<br />
fine, but I was nearly two weeks<br />
overdue, so I came to Princess Anne<br />
<strong>Hospital</strong> to be induced.<br />
“Everything seemed to be going<br />
OK, but then there were problems<br />
with Kaleb’s blood pressure and I<br />
had a very high temperature. As<br />
soon as he was born they took him<br />
away and started working on him,<br />
then he was taken to neonatal<br />
intensive care.”<br />
The first 48 hours of Kaleb’s life<br />
were critical and, at one point, he<br />
stopped breathing. Larelle and her<br />
boyfriend, Luke Wheeler, were<br />
warned they might want to consider<br />
getting their baby son christened in<br />
hospital, in case he did not survive.<br />
Doctors then decided to use a<br />
new treatment to cool Kaleb’s body<br />
temperature in a bid to prevent any<br />
brain damage that may have been<br />
caused when he was born.<br />
Kaleb was attached to a cold<br />
body wrap and connected to a<br />
hi-tech cooling machine, which was<br />
“<br />
The first 48 hours of Kaleb’s life were critical<br />
and, at one point, he stopped breathing<br />
used to drop his body temperature<br />
from the normal 37° to 33.5°. This<br />
hypothermia was maintained for<br />
around 72 hours before he was<br />
gradually warmed back to normal.<br />
Consultants Dr Robert Ironton<br />
and Dr Vijay Baral lead the new<br />
cooling treatment, which has been<br />
introduced following recent studies<br />
that suggest cooling a baby limits the<br />
severity of any brain injury.<br />
If the blood supply between a<br />
mother and baby becomes obstructed<br />
or cut – known as perinatal asphyxia<br />
– the baby can become severely<br />
deprived of oxygen.<br />
MediaMonitor<br />
This lack of oxygen sets off an<br />
inflammatory response in the brain<br />
cells that can lead to serious illness,<br />
or, in some cases, prove fatal.<br />
It is believed that cooling the body<br />
of an at-risk baby within six hours<br />
of birth, in addition to standard<br />
intensive care treatment, gives the<br />
brain time to recover by limiting<br />
inflammation and slowing the body’s<br />
energy needs.<br />
Dr Baral said: “Baby cooling is<br />
standard practice in many larger<br />
hospitals across the world and we<br />
are delighted to now be able to<br />
provide this new service for babies in<br />
<strong>Southampton</strong>.”<br />
MediaMonitor<br />
Larelle’s mum, Martina Jauncey,<br />
said: “It was a very difficult time for<br />
both families while Kaleb was in<br />
hospital, but the nurses were very<br />
good to us all.<br />
“Everyone was surprised how well<br />
Kaleb did and how quickly he got<br />
better.”<br />
Kaleb is now a happy, healthy<br />
baby, with no signs of his dramatic<br />
start in life, but will be regularly<br />
monitored for the first few years<br />
of his life.<br />
For more information visit<br />
www.suht.nhs.uk and search<br />
for ‘neonatal’<br />
SUHT’s new baby-cooling treatment has featured in the News of the World and the<br />
Nursing Times, as well as on ITV Meridian.<br />
Volunteer interpreters<br />
Agnieszka Burtt is an admin support assistant – but over the past year has<br />
helped many women and families during their pregnancies and births.<br />
Based at the Princess Anne <strong>Hospital</strong>,<br />
she is one of 61 members of staff<br />
at SUHT who have trained to be<br />
volunteer interpreters.<br />
Nearly six years ago, Agnieszka<br />
moved to <strong>Southampton</strong> from Poland,<br />
where she had been an English teacher.<br />
Since completing her training course<br />
in December 2008, Agnieszka has<br />
helped patients at appointments, births<br />
and over the phone.<br />
She said: “Even if families have been<br />
in the UK a long time and speak good<br />
English, medical vocabulary can cause<br />
problems. Sometimes I only need to<br />
interpret a few words to help women<br />
understand procedures.<br />
“I am very pleased that I can help<br />
our Polish patients. It can be a worrying<br />
and stressful time, especially if you don’t<br />
understand everything you are being<br />
told. I can help to explain everything and<br />
reassure them.”<br />
Using trained staff volunteers means<br />
clinicians can access interpreters very<br />
quickly. This is important in emergency<br />
situations, as volunteers are already on<br />
site, so doctors do not have to wait for an<br />
external translator to travel to the hospital.<br />
The in-house service provides crucial<br />
help for patients for whom English is not<br />
their first language.<br />
Often, these patients are anxious and<br />
confused, so just a few words from one<br />
of the interpreters can help put them at<br />
ease – enabling clinical staff to treat the<br />
patient more effectively.<br />
As well as being cheaper than<br />
external companies, saving the Trust<br />
money, the in-house interpretation<br />
service offers a more personal approach,<br />
providing face-to-face help rather than<br />
being a voice on the end of the phone.<br />
The Trust’s volunteer interpreters are in<br />
big demand and more recruits are needed<br />
to help out with interpretation work.<br />
If you are a member of staff who is<br />
fluent in another language and would like<br />
to find out more about training to become<br />
a volunteer interpreter, contact voluntary<br />
services manager Kim Sutton on ext 6062.<br />
• SUHT currently has 866<br />
volunteers, including 66<br />
interpreter volunteers<br />
• Between them, they speak<br />
41 languages<br />
• Languages range from Arabic<br />
to Urdu and everything in<br />
between<br />
• The number of call-outs for<br />
SUHT’s in-house interpreter<br />
service rose from 254 in 2005<br />
to 554 in 2009.81% to 84%<br />
Foundation<br />
Trust update<br />
The hospital’s board of directors<br />
has decided to postpone our bid to<br />
become a foundation trust.<br />
As you will have read in previous<br />
issues of Connect, the application<br />
had been proceeding well and the<br />
Trust was in a strong position to be<br />
authorised from February 1.<br />
However the financial situation<br />
that developed in the local health<br />
economy made it impossible for the<br />
board to be confident that we could<br />
manage some of the risks associated<br />
with being a foundation trust.<br />
The application will now be<br />
resumed once the hospital and its<br />
commissioners can agree plans that<br />
will bring affordable volumes of<br />
work to the hospital - probably not<br />
for at least 12 months.<br />
The Trust remains in healthy<br />
financial balance and there is strong<br />
support for the continued growth of<br />
our world-class specia<strong>list</strong> services.<br />
CONNECT<br />
ISSUE 24 3
spotlight<br />
on services<br />
Palliative care<br />
Connect has been taking an in-depth look at SUHT’s end<br />
of life care service.<br />
Releasing nursing time<br />
A project to free up nursing time at Countess Mountbatten<br />
House has halved the number of patient falls.<br />
The nurses have taken part in a<br />
Releasing Time to Care project,<br />
designed to improve the quality of<br />
patient care and the working lives of<br />
staff. Already it has increased direct<br />
patient care by 13% and led to a<br />
52% reduction in falls.<br />
Sister Jennie Dacombe explained<br />
the process to Connect: “The first<br />
thing we had to do was find out our<br />
starting position, so that we could<br />
measure our improvement.<br />
“This was calculated by following<br />
the nurses with a stopwatch and<br />
timing all of the interruptions to<br />
their patient care. This included<br />
interruptions from other staff,<br />
telephone calls and trying to find<br />
things around the ward.”<br />
The initial research found that<br />
44% of the nurses’ time was<br />
spent on patient care. A patient<br />
satisfaction survey at the same time<br />
gave some very positive results, with<br />
100% of patients reporting that the<br />
care they received was very good<br />
or excellent.<br />
However, there was some concern<br />
over the time taken for nurses to<br />
respond to patient buzzers. The<br />
team felt that this was linked to the<br />
number of patient falls, which they<br />
wanted to work to reduce.<br />
The project was divided<br />
into modules, with two nurses<br />
championing each module.<br />
The first change was to improve<br />
• Releasing Time to Care has<br />
been rolled out to 40 out of<br />
46 inpatient wards around the<br />
Trust<br />
• Direct care time has increased<br />
from 39% to 53%<br />
• Patient satisfaction has<br />
increased from 96% to 100%<br />
• Staff satisfaction has increased<br />
from 81% to 84%<br />
the patient status<br />
board, to enable staff<br />
to see all information<br />
at a glance. They<br />
introduced colour<br />
coding for the<br />
consultants as well as<br />
additional physiotherapy and<br />
infection control information for each<br />
patient.<br />
One of the biggest improvements<br />
was in the storage of equipment. By<br />
rearranging cupboards, the length of<br />
time taken to find things was reduced<br />
from six minutes to six seconds.<br />
There is now a cupboard in each<br />
bay, which is topped up with stock<br />
after every shift. Every cupboard is<br />
arranged in the same way, so that<br />
nurses know where to look for<br />
items, no matter which bay they are<br />
working in.<br />
Involving volunteers and<br />
housekeepers in serving breakfast<br />
made another major improvement.<br />
This has released the time of two<br />
healthcare assistants, totalling 730<br />
hours of nursing time each year.<br />
Jennie said: “The project is<br />
ongoing and we look forward<br />
to making more improvements.<br />
Everyone has got involved and made<br />
a difference and we have had visits<br />
from our matron, Trust Board and<br />
divisional heads of nursing.<br />
“It is great to see the reduction<br />
in falls as a result of the increased<br />
patient contact time, and a survey<br />
of staff showed that morale has<br />
improved too.”<br />
For more information visit<br />
www.suht.nhs.uk and search<br />
for ‘palliative’<br />
CONNECT<br />
4ISSUE 24
Andrew’s<br />
<strong>wish</strong> <strong>list</strong><br />
Andrew Middleton is a man on a mission.<br />
The retired engineer was diagnosed<br />
with prostate cancer two years ago<br />
and had been doing well until his<br />
condition forced him to cut short a<br />
holiday in Spain.<br />
After treatment at <strong>Southampton</strong><br />
General <strong>Hospital</strong>, he was able to<br />
return home but was readmitted a<br />
few months later when he suffered<br />
acute renal failure.<br />
The life-threatening condition was<br />
the start of a four-month hospital<br />
stay, which included two weeks in<br />
intensive care.<br />
As his condition improved, he was<br />
moved to Countess Mountbatten<br />
House, SUHT’s hospice at West End,<br />
near <strong>Southampton</strong>, to recuperate.<br />
Far from feeling sorry for himself,<br />
Andrew set about a plan to get<br />
mobile again as quickly as possible.<br />
Every day, he would walk around<br />
the hospice with either his frame or<br />
sticks, relying on the nursing staff to<br />
keep count of his laps.<br />
Andrew also enjoyed the benefits<br />
of aromatherapy and physiotherapy<br />
during his stay.<br />
Now back home in Woolston,<br />
<strong>Southampton</strong>, with wife Anne, his<br />
number one aim is to get strong<br />
enough to take the couple’s<br />
cocker spaniel, Ben, for a walk.<br />
Once that has been accomplished,<br />
he plans to get back to restoring<br />
his pride and joy, a Porsche 911 – a<br />
project that has already taken him<br />
19 years.<br />
Third on the <strong>wish</strong> <strong>list</strong> is his<br />
ultimate goal – to actually drive<br />
the car.<br />
In the meantime, he is a keen<br />
“<br />
I didn’t really know what to expect there<br />
but it was more like a high-class hotel.<br />
photographer and spends many<br />
hours in his garden, capturing<br />
birds and insects on camera.<br />
Andrew speaks extremely<br />
highly of the care he received at<br />
Countess Mountbatten House.<br />
“I didn’t really know what to<br />
expect there but it was more like<br />
a high-class hotel. Being there was a<br />
huge advantage for me,” he said.<br />
Being a vegetarian, Andrew was<br />
impressed with the personalised<br />
meals that were prepared for him –<br />
not to mention the “tipple” that was<br />
offered before dinner.<br />
Sadly, medications prevented him<br />
from being able to indulge, but he<br />
said this was just one example of<br />
the personal touch offered by the<br />
Countess Mountbatten team.<br />
Andrew returned home in<br />
January. He and Anne have been<br />
amazed at all the equipment made<br />
available to them – everything from<br />
a bed, chairs and cushions to frames,<br />
sticks and a wheelchair.<br />
The couple also have a team of<br />
nurses, doctors and carers who are<br />
ready and willing to call in at various<br />
times of day to look after Andrew’s<br />
every need.<br />
“We are just overwhelmed,” said<br />
Anne. “You hear so much bad news<br />
about the <strong>NHS</strong>, but we just cannot<br />
speak highly enough of it.<br />
“As a family, we would like to<br />
thank everyone who has shown such<br />
dedication and professional care to<br />
Andrew over what has been a very<br />
long and worrying time.”<br />
get<br />
involved<br />
Making the link<br />
Every clinical area across <strong>Southampton</strong>’s university hospitals is<br />
encouraged to have at least one palliative care link nurse.<br />
Known as spiritual, palliative and end of life (SPEL) nurses, they act as an<br />
advocate on the ward for patients and their families, as well as being a central<br />
resource for ward staff.<br />
SPEL nurses have responsibility for passing on their specia<strong>list</strong> knowledge to<br />
colleagues as well as taking charge of palliative care issues in their own area.<br />
End of Life Care Month<br />
March 2010 is End of Life Care Month across <strong>Southampton</strong> <strong>University</strong><br />
<strong>Hospital</strong>s <strong>NHS</strong> Trust.<br />
Patients, relatives and staff will have a wide range of opportunities to learn more<br />
about palliative and end of life care, both at <strong>Southampton</strong> General <strong>Hospital</strong> and<br />
Countess Mountbatten House.<br />
Details will be publicised soon or call Julie Francere on 023 8047 5564 to find out more.<br />
Patients, carers, family members and bereaved relatives can<br />
play an active part in the future of Countess Mountbatten<br />
House and the palliative care service.<br />
The newly formed Countess Mountbatten Patient<br />
Partnership Forum welcomes feedback and ideas from<br />
anyone who has used the service.<br />
Telephone 023 8047 5581 to find out more.<br />
Countess Mountbatten House<br />
Countess Mountbatten House is a<br />
regional <strong>NHS</strong> palliative care service for<br />
patients with advancing cancer.<br />
The hospice is set in gardens at West<br />
End, near <strong>Southampton</strong>.<br />
This coordinated, interprofessional<br />
hospice, community and hospital service<br />
for those in the greater <strong>Southampton</strong> area<br />
includes:<br />
• More than 20 specia<strong>list</strong> palliative<br />
care beds<br />
• An award-winning specia<strong>list</strong><br />
palliative care team in the<br />
community<br />
• An enthusiastic specia<strong>list</strong> hospital<br />
palliative care team<br />
• A dedicated day care service<br />
• An award-winning education team<br />
• A research environment to improve<br />
the care and support offered.<br />
The work of CMH is supported by the Countess Mountbatten Hospice Charity. For more<br />
information on their fundraising events and how you can get involved, contact Kat Linsley<br />
Hood on 023 8047 5345 or email kat@cmhcharity.co.uk.<br />
CONNECT<br />
ISSUE 24 5
getting<br />
to know<br />
Helen Staples procedure pack co-ordinator<br />
Tell us a little bit about your background<br />
I grew up in rural Staffordshire and at the seaside<br />
in Worthing, Sussex. I arrived in <strong>Southampton</strong> in 1965 to<br />
start my nurse training.<br />
My first year was spent living in what is now known<br />
as the old nurses’ home, under the watchful eye of the<br />
‘home warden’ (when a night out meant back by 10pm!).<br />
During my student placement in theatre, I realised<br />
that this was where I wanted to work once qualified.<br />
After living in the Channel Islands and 27 years<br />
of family life in Peterborough, combined with work<br />
in theatres and intensive care, I changed direction<br />
and became an inaugural member of the Trust<br />
transformation team.<br />
Five years later I came full circle, returning to SGH at<br />
the end of my career.<br />
What does your role at SUHT involve?<br />
When I arrived at SUHT six years ago, my job<br />
was a first for the Trust, and a rarity nationwide.<br />
I work with pack suppliers to maintain a consistent<br />
and cost effective supply of procedure packs to the many<br />
theatres and departments Trust wide.<br />
A theatre procedure pack is a customised product<br />
consisting of a collection of consumable items regularly<br />
used for a given procedure, packed in a sterile, theatreready<br />
presentation.<br />
I also work as a link nurse, liaising between my<br />
clinical colleagues and our procurement colleagues,<br />
offering advice and researching product alternatives<br />
for out of stock items and new product trials,<br />
while constantly supporting standardisation and<br />
rationalisation of theatre consumables.<br />
What do you get up to in your spare time?<br />
Touring the UK and Europe with our trusty<br />
tent, long lazy days at our beach hut at<br />
Milford-on-Sea and furiously energetic<br />
aquarobics sessions at the local pool.<br />
“<br />
…the <strong>NHS</strong> won<br />
me over and<br />
after 45 years<br />
I think I will<br />
stay!<br />
What’s the best book you’ve ever read?<br />
A Thousand Splendid Suns by Khaled Hosseini.<br />
Favourite film?<br />
Lawrence of Arabia (1962), a David Lean<br />
‘Panavision’ epic with fabulous surround sound.<br />
Hundreds in the cast and not a computerised image<br />
to be seen.<br />
What three items would you take with you on<br />
a desert island?<br />
A king-size Hungarian goose down duvet, an unlimited<br />
supply of Nestle condensed milk in tubes and a pair of<br />
scissors, as a ‘proper’ nurse should never leave home<br />
without!<br />
Who has inspired your career?<br />
The team of learned theatre sisters who tutored me<br />
intensively when I joined the staff of Twin Theatres at<br />
<strong>Southampton</strong> General <strong>Hospital</strong> back in 1968. There was<br />
an infectious precision about the way they worked which<br />
ensured high standards of patient care even without the<br />
sophisticated equipment of today.<br />
Why did you choose to work for the <strong>NHS</strong>?<br />
Once I had qualified, private sector healthcare<br />
was still in its infancy and not a very secure option at<br />
the time. I did give it a whirl and admired the business<br />
approach to healthcare. However, the <strong>NHS</strong> won me over<br />
and after 45 years I think I will stay!<br />
next<br />
issue<br />
In the next issue of Connect, we’ll be putting Alastair<br />
Matthews, director of finance, in the hotseat. If you<br />
would like to suggest a question, email it to<br />
connect@suht.swest.nhs.uk by Friday 19 March.<br />
Offside<br />
comedy<br />
club<br />
WIN!<br />
Tell us what you think about<br />
Connect’s new look and you could<br />
win a pair of tickets to<br />
<strong>Southampton</strong>’s new comedy night,<br />
the Offside Comedy Club.<br />
The Offside Comedy Club takes place at St Mary’s<br />
Stadium, <strong>Southampton</strong>. For more information visit<br />
www.offsidecomedy.com.<br />
To be in with a chance of winning, just email<br />
connect@suht.swest.nhs.uk with your views on<br />
Connect’s new look.<br />
The winner will be picked on 19 March 2010.<br />
Congratulations to Arlene Brady from the emergency<br />
department, who won a bottle of champagne in issue<br />
23’s reader survey prize draw.<br />
Three cheers for Toby<br />
Back in issue 6, we<br />
featured the story of<br />
Toby Dobson, who<br />
was born three and a<br />
half months early.<br />
Toby has just celebrated his third birthday, so<br />
his mum Lyndsay and dad Alastair contacted<br />
Connect to tell us how he’s been getting on.<br />
After being born so early, Toby’s lungs did<br />
not develop properly, and he still relies on an<br />
oxygen supply 24 hours a day.<br />
Toby also had some bleeding on his brain<br />
when he was born, and has since been<br />
diagnosed with cerebral palsy. This affects his<br />
motor skills, and he is not able to sit or walk yet.<br />
Lyndsay said: “It is a miracle that Toby survived at all,<br />
and he is getting stronger all the time – he can move<br />
himself across the floor to his favourite spot in front of the<br />
television! He is also trying to talk now and has learnt how<br />
to click his tongue.”<br />
Toby eats pureed food, but last summer had a<br />
gastrostomy tube fitted so that he can still be fed even when<br />
he is unable to eat.<br />
Lyndsay and Alastair have now set up a charity, Team<br />
Toby, to help fund some of the specia<strong>list</strong> equipment that<br />
their son needs. So far they have raised more than £2,300<br />
and have more events planned.<br />
Lyndsay said: “He’s such a happy child and brings so<br />
much to our lives despite his disabilities. We are so lucky<br />
to have him and hope that his story inspires other parents<br />
who are in the same situation.”<br />
For more information about the charity visit www.teamtoby.co.uk<br />
CONNECT<br />
6 ISSUE 24
meet the<br />
team<br />
Pharmacy’s trouble-shooters<br />
Tucked away in the pharmacy department is a team helping thousands<br />
of patients a year – usually without them knowing it.<br />
Staff in the medicines information<br />
centre, a specia<strong>list</strong> unit based at<br />
<strong>Southampton</strong> General <strong>Hospital</strong>,<br />
advise doctors, nurses and<br />
pharmacists about treating patients<br />
with complex clinical needs.<br />
The team helps identify which<br />
medicines have caused side effects,<br />
finds suitable treatments when the<br />
usual ones have failed, and advises<br />
doctors how to prescribe safely for<br />
patients who are already taking lots<br />
of drugs.<br />
Dr Simon Wills, who runs the unit,<br />
said: “People phone us to ask literally<br />
anything about medicines.<br />
“But most of our calls are about<br />
individual patients with a problem<br />
that has stumped other professionals,<br />
and it’s good to be able to help.<br />
“We don’t just cover this Trust –<br />
The team’s training<br />
materials are used<br />
across the world<br />
we take calls from Oxford to the Isle<br />
of Wight and from Weymouth to<br />
Portsmouth so it’s quite a big area.<br />
We even take calls from GPs and<br />
<strong>NHS</strong> Direct.”<br />
Angela Emerson, the team’s<br />
longest serving member, said:<br />
“We were recently asked to go to<br />
Germany to help them learn about<br />
our role in <strong>Southampton</strong> because<br />
they’d like to copy what we do here.<br />
“Although we’re well-known<br />
as innovators in the UK, it’s nice to<br />
think that even in Europe there are<br />
people who look to <strong>Southampton</strong><br />
for leadership.”<br />
In fact, the unit’s fame goes<br />
beyond Europe because the training<br />
materials they have developed<br />
are now used by pharmacists in<br />
Australia, New Zealand, Turkey,<br />
Malta and Uganda.<br />
Members of the team have highly<br />
specialised clinical skills and are often<br />
called upon for an expert opinion –<br />
which means carefully weighing up<br />
the pros and cons of various courses<br />
of action in difficult situations.<br />
Frequently, queries are about safe<br />
prescribing in pregnancy or the use<br />
of unusual medicines in infants.<br />
Pharmacist Helen Jones enjoys<br />
the variety. “Every day is different<br />
because every enquiry we receive is<br />
different,” she said.<br />
“One minute I’ll be talking<br />
to a GP, then a hospital nurse,<br />
then maybe writing a letter to<br />
a consultant. And the variety of<br />
topics is huge – antibiotics, herbal<br />
medicines, painkillers, psychiatry<br />
medicines – you name it.<br />
“People often phone because<br />
they’ve exhausted all the other avenues<br />
for information so it’s good when we<br />
can help them solve a patient’s problem<br />
– and we nearly always can.”<br />
Golden Stethoscope<br />
Among the serious work, the<br />
trouble-shooters are occasionally<br />
asked some very unusual<br />
questions. Past ones have included:<br />
What is the dose of antibiotic for a<br />
killer whale?<br />
Can eating artist’s oil paints cause<br />
mental illness?<br />
What oral contraceptives are<br />
available in Bulgaria?<br />
A patient has eaten a whole tub<br />
of E45 because she thought it was<br />
vanilla ice cream. Is this harmful?<br />
What treatments were available<br />
for angina in 1948?<br />
A patient has just injected himself<br />
with his dog’s insulin by mistake.<br />
What should he do?<br />
Is it safe to spray WD40 on the legs<br />
to treat stiff knees?<br />
Can my medication make me<br />
allergic to eyebrow dye?<br />
I’ve been taking my wife’s<br />
contraceptives instead of my<br />
migraine medicines for a month.<br />
Will it do me any harm?<br />
I’m allergic to the main antidote to<br />
radiation poisoning. What should I<br />
do if there’s a nuclear war?<br />
It’s official – Dr James Adams is a man with his<br />
finger on the pulse.<br />
James, who works as a consultant physician<br />
WINNER!<br />
in medicine for older people, is the winner of this year’s<br />
Golden Stethoscope award, SUHT’s reality check to see if our<br />
consultants are living in the real world.<br />
He scored an impressive 8/10, correctly answering questions on<br />
everything from music and film to Formula 1 and pot noodles.<br />
The battle for the next Golden Stethoscope award will<br />
commence in our next issue. Who would you like to see facing the<br />
10-question challenge? Email connect@suht.swest.nhs.uk<br />
CONNECT<br />
ISSUE 24 7
talkback<br />
The fundraising<br />
connection<br />
Call <strong>Southampton</strong> <strong>Hospital</strong> Charity on 023 8079 8881 or visit www.suht.nhs.uk/charity.<br />
Dear Connect<br />
Just over a year ago, we spent<br />
several weeks at Princess Anne<br />
and <strong>Southampton</strong> General<br />
hospitals, after our son Jozsef<br />
was born ten weeks premature<br />
on 11 December 2008.<br />
Through the hard work and<br />
dedication of the doctors and nurses<br />
on the neonatal ward, he came<br />
home on 30 December.<br />
Unfortunately, Jozsef contracted<br />
an infection and on 14 January 2009<br />
his condition deteriorated rapidly<br />
and he was rushed to the General,<br />
to ward G1, where the doctors and<br />
nurses saved his life. Words cannot<br />
express what we went through<br />
that night, but the team were<br />
tremendous. They kept us informed<br />
with everything that was happening<br />
and tried their best to comfort and<br />
reassure us at all times.<br />
The next chapter involved the<br />
paediatric intensive care unit. The<br />
PICU team are tasked with the most<br />
difficult job imaginable and our hats<br />
go off to them all; they really are<br />
something special. I would like to<br />
single out Gemma, who cared for our<br />
son with such care, dedication and<br />
sincerity. Without the support she<br />
gave us we would have undoubtedly<br />
cracked under the pressure.<br />
After a short hop into ward G2,<br />
where the staff allowed us to bond<br />
with our son and learn how to feed<br />
and bath him again, we finally took<br />
him home on 28 January.<br />
Jozsef is now a confident and<br />
content one year old and we are just<br />
so lucky to have him here. This was<br />
truly down to all the staff involved in<br />
his care through Princess Anne and<br />
the General <strong>Hospital</strong>.<br />
The hardest thing we thought we<br />
may struggle with is the bonding<br />
with a child who you lost (in theory)<br />
to the hospitals and nurses for nearly<br />
two months, at such a vital and<br />
vulnerable time. However, if truth<br />
be known, we feel this experience<br />
has made him the contented, placid<br />
little boy he is – everyone says what a<br />
pleasure he is when they meet him.<br />
Thanks again for everyone’s<br />
support and help – your staff are<br />
truly remarkable people – Jozsef’s<br />
guardian angels!<br />
Yours sincerely<br />
The Kovacs family – John, Lou<br />
and Jozsef<br />
Alan’s ultimate<br />
challenge<br />
After life-saving brain surgery, Alan Charlesworth wanted to set<br />
himself the biggest challenge possible.<br />
The 39-year-old from <strong>Southampton</strong> decided on Iron Man UK<br />
2009 – a gruelling 140 mile race which includes a 2.4 mile swim, a<br />
112 mile bike ride and a 26.3 mile run.<br />
Alan was treated in the Wessex Neurological Unit at <strong>Southampton</strong><br />
General <strong>Hospital</strong> after suffering a serious head injury five years ago.<br />
He underwent emergency neurosurgery to remove an extradural<br />
haematoma, a potentially life-threatening blood clot on the brain,<br />
and has since made a full recovery.<br />
Alan took part in Iron Man UK to support the unit that provided<br />
such vital care for his recovery, raising £1,365 through sponsorship.<br />
He said: “It was the biggest challenge that I could think to set<br />
myself. When I came out of my accident, it really made me realise<br />
how precious life is, and I wanted to give something back.”<br />
Miranda Gardner, head injury nurse specia<strong>list</strong>, said: “Alan’s<br />
fundraising was more than a marathon effort. We are enormously<br />
grateful to him for raising such a substantial amount of money.<br />
“Considering the serious nature of his injury, Alan’s achievement in<br />
completing Iron Man UK is more than we could ever have hoped for.<br />
We shall be purchasing a special low-level bed with the money,<br />
to protect patients who are at risk of falling.”<br />
Alan has further ambitions to fundraise in the future, hinting<br />
that he hopes to compete in the half-Iron Man event, and is also<br />
considering an accelerated freefall skydive.<br />
i<br />
Find out more... Sign up to <strong>Southampton</strong> <strong>Hospital</strong> Charity’s newsletter to receive<br />
more news and fundraising information. Email charity@suht.swest.nhs.uk.<br />
SUHT Sudoku<br />
challenge<br />
Win a meal at the Old Delhi Eatery<br />
Enter numbers from 1 to 9 into the blank squares, so that every row,<br />
every column and every 3x3 square has one of each digit.<br />
Send your entry in the internal post to Connect, Mailpoint 18, to<br />
be in with a chance of winning a meal at the Old Delhi Eatery worth<br />
up to £25. Entries close Friday 19 March.<br />
Congratulations to Simon Morris, from the residency department,<br />
who successfully completed Issue 23’s puzzle to scoop the prize.<br />
www.olddelhi.co.uk<br />
Win £2,010<br />
in 2010<br />
1st prize – £2,010 cash prize<br />
2nd prize – ‘Silver Lining’, a<br />
beautiful handmade quilt<br />
3rd prize – Canon Power Shot<br />
A470 digital camera<br />
Winter Raffle tickets cost £1<br />
The draw will take place on 22<br />
March 2010 (tickets on sale until<br />
16 March 2010)<br />
Tickets on sale at <strong>Southampton</strong><br />
General <strong>Hospital</strong>:<br />
• <strong>Southampton</strong> <strong>Hospital</strong> Charity<br />
(Trust Management Offices,<br />
opposite the Emergency<br />
Department)<br />
• Main hospital reception<br />
• Various wards and departments<br />
Killimanjaro<br />
challenge<br />
Support medical staff on Princess<br />
Anne <strong>Hospital</strong>’s neonatal<br />
unit, in their Killimanjaro<br />
challenge in October 2010.<br />
Visit www.justgiving.co.uk/<br />
pahneonatalchallenge to make a<br />
donation today, or call 023 8079<br />
8881 to find out more.<br />
WIN