Thames Deanery - St-marys-anaesthesia.co.uk
Thames Deanery - St-marys-anaesthesia.co.uk
Thames Deanery - St-marys-anaesthesia.co.uk
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Thames</strong> <strong>Deanery</strong><br />
Trainers in<br />
Paediatric<br />
Anaesthesia<br />
Group<br />
<strong>Thames</strong>PAG@gosh.nhs.<strong>uk</strong><br />
Resource and<br />
Information Pack<br />
3rd edition<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 1
First Edition published 1997<br />
Se<strong>co</strong>nd Edition Nov 2000<br />
Third Edition May 2002<br />
Editors<br />
Dr Richard Howard<br />
Dr Isabeau Walker<br />
Great Ormond <strong>St</strong>reet Hospital for Children NHS Trust<br />
© <strong>Thames</strong> <strong>Deanery</strong>: Trainers in Paediatric Anaesthesia Group<br />
All rights reserved. This publication may not be reproduced, stored<br />
in a retrieval system nor transmitted in any form or by any means,<br />
electronic, mechanical, photo<strong>co</strong>pying, re<strong>co</strong>rding or otherwise,<br />
without the prior written permission of the <strong>co</strong>pyright holders.<br />
Whilst every care has been taken to ensure that doses and<br />
re<strong>co</strong>mmendations are <strong>co</strong>rrect, the responsibility for final<br />
checking must rest with the prescriber. The authors cannot<br />
accept any responsibility for errors in this publication.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 2
Resource Information Pack<br />
<strong>Thames</strong> Trainers in Paediatric Anaesthesia<br />
List of Lead Clinicians . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4-6<br />
Training re<strong>co</strong>mmendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7<br />
Training policy p Supervision . . . . . . . . . . . . . . . . . . . . 8<br />
p Resuscitation . . . . . . . . . . . . . . . . . . . . 8<br />
c<br />
o<br />
n<br />
t<br />
e<br />
n<br />
t<br />
s<br />
Emergency Resuscitation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9<br />
Fasting policy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10<br />
Preoperative upper respiratory tract infections . . . . . . . . . . . . . . 11<br />
Endocarditis prophylaxis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12<br />
Incidental heart murmurs . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13<br />
Pain management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14<br />
Local <strong>anaesthesia</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15<br />
Analgesics & anti-emetics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16<br />
Fluid balance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17<br />
Acute major anaphylaxis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18<br />
Malignant hyperthermia . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19<br />
Latex allergy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20<br />
Sickle Cell . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21-22<br />
Reading materials p Textbooks . . . . . . . . . . . . 23<br />
p Journals . . . . . . . . . . . . 24<br />
p Useful publications . . . . . . . . . . . . 25<br />
p Internet resources . . . . . . . . . . . . 26-28<br />
p Key references . . . . . . . . . . . . 29-30<br />
Journal Club p premedication, general <strong>anaesthesia</strong>, ENT 31-42<br />
& eyes, dental surgery, pain & analgesia,<br />
day-care, sedation, resuscitation,<br />
miscellaneous, organisation<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 3
Group Co-ordinators<br />
Dr Isabeau Walker<br />
Dr Richard Howard<br />
GOSH for Children<br />
NHS Trust<br />
Great Ormond <strong>St</strong><br />
London WC1N 3JH<br />
Lead Clinicians<br />
<strong>Thames</strong> Paediatric Trainers<br />
020 7829<br />
8865 <strong>Thames</strong>PAG<br />
@gosh.nhs.<strong>uk</strong><br />
hospital name address phone email<br />
Barnet General<br />
Hospital<br />
Barnet General<br />
Hospital<br />
Dr Regina<br />
Milaszkiewicz<br />
Dr Iris Symons<br />
Wellhouse Lane<br />
Barnet<br />
Herts EN5 3DJ<br />
Wellhouse Lane<br />
Barnet<br />
Herts EN5 3DJ<br />
Basildon Hospital Dr Helen Utting Nethermayne<br />
Basildon<br />
Essex SS16 5NL<br />
Bromley Hospital Dr Pauline Vine Cromwell Avenue<br />
Bromley<br />
Kent BR2 9AJ<br />
Broomfield Hospital Dr Kevin Kiff Broomfield<br />
Chelmsford<br />
Essex CM1 7ET<br />
Broomfield Hospital Dr M Davis Broomfield<br />
Chelmsford<br />
Essex CM1 7ET<br />
Chase Farm Hospital Dr David Harvey The Ridgeway<br />
Enfield<br />
Middlesex EN2 8JL<br />
Chase Farm Hospital Dr <strong>St</strong>elios Pavlou The Ridgeway<br />
Enfield<br />
Chelsea &<br />
Westminster Hospital<br />
Dr Nick Fauvel<br />
Middlesex EN2 8JL<br />
369 Fulham Road<br />
London SW10 9TH<br />
020 8216<br />
4000<br />
020 8216<br />
4000<br />
01268 533911<br />
020 8289<br />
7000<br />
regina.milaszkiewicz<br />
@barnet-chasetr.nhs.<strong>uk</strong><br />
Iris.symons<br />
@barnet-chasetr.nhs.<strong>uk</strong><br />
Pauline.Vine<br />
@bromleyhospitals<br />
.nhs.<strong>uk</strong><br />
01245 440761 Kevin_Kiff<br />
@hotmail.<strong>co</strong>m<br />
01245 440761 martin.e.davis<br />
@btinternet.<strong>co</strong>m<br />
020 8366<br />
6600<br />
020 8366<br />
6600<br />
020 8746<br />
8000<br />
david @harvey-<br />
1gas.demon.<strong>co</strong>.<strong>uk</strong><br />
drsppavlou<br />
@hotmail.<strong>co</strong>m<br />
Chelsea &<br />
Westminster Hospital<br />
Dr Mike Weston<br />
369 Fulham Road<br />
London SW10 9TH<br />
020 8746<br />
8000<br />
HKP@psilink.<strong>co</strong>.<strong>uk</strong><br />
Colchester General<br />
Hospital<br />
Epsom General<br />
Hospital<br />
Great Ormond <strong>St</strong>reet<br />
Hospital for Children<br />
Dr Gerald Timmins<br />
Dr Anna-Maria Rollin<br />
Dr Isabeau Walker<br />
Turner Road<br />
Colchester<br />
Essex CO4 5JL<br />
Dorking Road<br />
Epsom<br />
Surrey KT18 7EG<br />
Great Ormond <strong>St</strong><br />
London WC1N 3JH<br />
01206 853535 timmins1<br />
@tes<strong>co</strong>.net<br />
01372 735735 arollin@sthelier.<br />
sghms.ac.<strong>uk</strong><br />
020 7829<br />
8865<br />
WalkeI<br />
@gosh.nhs.<strong>uk</strong><br />
Guys Hospital Dr Claire Shannon <strong>St</strong> Thomas <strong>St</strong>reet<br />
London SE1 9RT<br />
Hammersmith<br />
Hospital<br />
Dr David Zideman<br />
Du Cane Road<br />
East Acton<br />
London W12 0HS<br />
Hillingdon Hospital Dr Jan Downer Pield Heath Road<br />
Uxbridge<br />
Middlesex UB8 3NN<br />
020 7955<br />
5000<br />
020 8846<br />
1234<br />
claire.shannon<br />
@gstt.sthames.nhs.<br />
<strong>uk</strong><br />
01895 238282 jan.downer<br />
@thh.nhs.<strong>uk</strong><br />
Kings College Dr Cathie Hill Denmark Hill 020 737 4000 catherine.hill<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 4
Hospital London SE5 9RS @kingshc.nhs.<strong>uk</strong><br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 5
Lead Clinicians<br />
<strong>Thames</strong> Paediatric Trainers (<strong>co</strong>nt)<br />
hospital name address phone email<br />
Kingston Hospital Dr Richard <strong>St</strong>acey Galsworthy Road<br />
Kingston upon<br />
<strong>Thames</strong><br />
Surrey KT2 7QB<br />
Kingston Hospital Dr Carol <strong>St</strong>ableforth Galsworthy Road<br />
Kingston upon<br />
<strong>Thames</strong><br />
Surrey KT2 7QB<br />
Lewisham Hospital Dr Richard Arnold High <strong>St</strong><br />
Lewisham<br />
London SE13<br />
Lister Hospital Dr Pin Patel Coreys Mill Lane<br />
<strong>St</strong>evenage<br />
Herts SG1 4AB<br />
Lister Hospital Dr Prasun Sengupta Coreys Mill Lane<br />
<strong>St</strong>evenage<br />
Mayday University<br />
Hospital<br />
Moorfields Eye<br />
Hospital<br />
Mount Vernon<br />
Hospital<br />
Mount Vernon<br />
Hospital<br />
Northwick Park<br />
Hospital<br />
Northwick Park<br />
Hospital<br />
Dr Kim Hughes<br />
Dr Jonathan Lord<br />
Dr Julie Forsyth<br />
Dr A Hayward<br />
Dr Pradeep Kulkarni<br />
Dr Roger Sharpe<br />
Herts SG1 4AB<br />
London Road<br />
Croyden<br />
Surrey CR7 7YE<br />
City Road<br />
London EC1V 2PD<br />
Rickmansworth Rd<br />
Northwood<br />
Middlesex HA6 2RN<br />
Rickmansworth Rd<br />
Northwood<br />
Middlesex HA6 2RN<br />
Watford Road<br />
Harrow<br />
Middlesex HA1 3UJ<br />
Watford Road<br />
Harrow<br />
Middlesex HA1 3UJ<br />
Oldchurch Hospital Dr Joanne Umo-Et<strong>uk</strong> Romford<br />
Essex RM7 0BE<br />
020 8546<br />
7711<br />
020 8546<br />
7711<br />
020 8690<br />
4311<br />
01438 314333<br />
01438 314333<br />
020 8401<br />
3000<br />
020 7253<br />
3411<br />
carol.stableforth<br />
@kh-tr.sthames.<br />
nhs.<strong>uk</strong><br />
richard@richardarnold.<strong>co</strong>.<strong>uk</strong><br />
rheron<br />
@globalnet.<strong>co</strong>.<strong>uk</strong><br />
Jonathan.lord<br />
@moorfields.nhs.u<br />
k<br />
01923 826111 drjuliebinns<br />
@hotmail.<strong>co</strong>m<br />
01923 826111<br />
020 8864<br />
3232<br />
020 8869<br />
3974<br />
020 8864<br />
3232<br />
020 8869<br />
KULPRAD@aol.<strong>co</strong><br />
rsharpe065<br />
@aol.<strong>co</strong>m<br />
3974<br />
01708 708443 JoanneCoker<br />
@aol.<strong>co</strong>m<br />
Princess Alexandra<br />
Hospital NHS Trust<br />
Queen Elizabeth<br />
Hospital<br />
Dr Zdenek Zych<br />
Dr Sharon Power<br />
Hamstel Road<br />
Harlow<br />
Essex CM20 1QX<br />
Woolwich<br />
London SE18 4QH<br />
01279 444455<br />
020 8836<br />
6000<br />
Queen Marys<br />
Hospital<br />
Royal Brompton and<br />
Harefield<br />
Dr Punitha Ganeshan Frognal Avenue<br />
Sidcup<br />
Kent DA14 6LT<br />
Dr Andrea Kelleher Sydney <strong>St</strong><br />
London SW3<br />
020 8302<br />
2678<br />
MSGanesh<br />
@aol.<strong>co</strong>m<br />
a.kelleher<br />
@rbh.nthames.nhs.<strong>uk</strong><br />
Royal Free Hospital Dr Shelagh Charlton Pond <strong>St</strong>reet<br />
Hampstead<br />
020 7794<br />
0500<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 6
London NW3 2QG<br />
Royal Hospitals Trust Dr Anil Visram Whitechapel Road<br />
Whitechapel<br />
London E1 1BB<br />
020 7377<br />
7000<br />
avisram<br />
@<strong>co</strong>mpuserve.<strong>co</strong>m<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 7
Lead Clinicians<br />
<strong>Thames</strong> Paediatric Trainers (<strong>co</strong>nt)<br />
hospital name address phone email<br />
Royal Hospitals Trust Dr Jo Challands Whitechapel Road<br />
Whitechapel<br />
London E1 1BB<br />
Royal Hospitals Trust Dr Lionel Davis Whitechapel Road<br />
Whitechapel<br />
London E1 1BB<br />
Royal Hospitals Trust Dr Alistair Marshall Whitechapel Road<br />
Whitechapel<br />
London E1 1BB<br />
Royal Hospitals Trust Dr Eddie McAteer Whitechapel Road<br />
Whitechapel<br />
London E1 1BB<br />
Southend Hospital Dr John Kinnear Prittlewell Chase<br />
Westcliff-on-Sea<br />
Essex SS0 0RY<br />
<strong>St</strong> Andrew's Centre<br />
for Plastic Surgery<br />
Burns<br />
<strong>St</strong> Georges Hospital<br />
Dr Ian Seggie<br />
Dr Darryl Hampson-<br />
Evans<br />
Court Road<br />
Broomfield<br />
Chelmsford CM12<br />
0BH<br />
Blackshaw Road<br />
Tooting<br />
London SW17 0QT<br />
<strong>St</strong> Georges Hospital Dr Linda Murdoch Blackshaw Road<br />
Tooting<br />
London SW17 0QT<br />
<strong>St</strong> Helier Hospital Dr Simon Hawkins Wrythe Lane<br />
Carshalton<br />
Surrey SM5 1AA<br />
<strong>St</strong> Helier Hospital Dr Sally Renwick Wrythe Lane<br />
Carshalton<br />
Surrey SM5 1AA<br />
<strong>St</strong> Mary's Hospital Dr Sanjay Gautama Praed <strong>St</strong>reet<br />
Paddington<br />
London W2 1NY<br />
<strong>St</strong> Mary's Hospital Dr Mark Sacks Praed <strong>St</strong>reet<br />
Paddington<br />
London W2 1NY<br />
<strong>St</strong> Mary's Hospital Dr Virin Sidhu Praed <strong>St</strong>reet<br />
Paddington<br />
London W2 1NY<br />
<strong>St</strong> Thomas Hospital Dr Chris Aps Lambeth Road<br />
London SE1 7EH<br />
UCLH Hospitals Dr Jane Lockie Mortimer <strong>St</strong>reet<br />
London W1N 8AA<br />
020 7377<br />
7000<br />
020 7377<br />
7000<br />
020 7377<br />
7000<br />
020 7377<br />
7000<br />
joanne.challands<br />
@bartsandthelondon<br />
.nhs.<strong>uk</strong><br />
lionel.sarah<br />
@tinyworld.<strong>co</strong>.<strong>uk</strong><br />
maeogmarsh<br />
@hotmail.<strong>co</strong>m<br />
maeogmarsh<br />
@hotmail.<strong>co</strong>m<br />
01702 435555 jakinnear<br />
@doctors.org.<strong>uk</strong><br />
01268 533911<br />
020 8672<br />
1255<br />
020 8672<br />
1255<br />
020 8296<br />
2000<br />
020 8296<br />
2000<br />
020 7725<br />
6666<br />
020 7725<br />
6666<br />
020 7725<br />
6666<br />
020 7928<br />
9292<br />
020 7636<br />
8333<br />
hampsonevans<br />
@hotmail.<strong>co</strong>m<br />
linda.murdoch<br />
@stgeorges.nhs.<strong>uk</strong><br />
milesandsally<br />
@btopenworld.<strong>co</strong>m<br />
sanjay.gautama<br />
@st-<strong>marys</strong>.nhs.<strong>uk</strong><br />
marksacks<br />
@btinternet.<strong>co</strong>m<br />
Chris.Aps<br />
@gstt.sthames<br />
.nhs.<strong>uk</strong><br />
jane.lockie<br />
@uclh.org<br />
UCLH Hospitals Dr Ann McAra Mortimer <strong>St</strong>reet<br />
London W1N 8AA<br />
Whipps Cross<br />
Hospital<br />
Dr H Youssef<br />
Whipps Cross Road<br />
Leytonstone<br />
London E11 1NR<br />
Whittington Hospital Dr Catherine Shaw Highgate Hill<br />
Highgate<br />
020 7636<br />
8333<br />
020 8539<br />
5522<br />
020 7272<br />
3070<br />
a.mcara@uclh.org<br />
Ahmosy<br />
@aol.<strong>co</strong>m.<strong>uk</strong><br />
catherineshaw<br />
@whittington.<br />
nhs.<strong>co</strong>m<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 8
London N19 5NF<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 9
Training re<strong>co</strong>mmendations<br />
for <strong>Thames</strong> SpRs in Paediatric Anaesthesia<br />
1. Three month<br />
module<br />
2. Training<br />
extension<br />
3. Further<br />
paediatric<br />
training<br />
p All trainees should <strong>co</strong>mplete a module of up to three<br />
months in paediatric <strong>anaesthesia</strong>, or its equivalent,<br />
during their SpR training programme.<br />
p The opportunity should be available to some trainees to<br />
extend this to 6 months in order to fulfil the<br />
re<strong>co</strong>mmendations for training as a <strong>co</strong>nsultant with an<br />
interest in paediatric <strong>anaesthesia</strong>.<br />
p The opportunity should be available for selected trainees<br />
to undertake further paediatric training for a minimum of<br />
one year in order to fulfil the re<strong>co</strong>mmended criteria for<br />
training as a full time paediatric anaesthetist. Some of<br />
this training <strong>co</strong>uld be overseas.<br />
4. Log book p Trainees should keep a log book of paediatric cases or<br />
be able to easily provide a summary of paediatric cases<br />
from their general log book.<br />
5. Common<br />
agreed<br />
policies<br />
p As far as is practical, hospitals in <strong>Thames</strong> <strong>Deanery</strong><br />
where paediatric training takes place or children are<br />
anaesthetised, have <strong>co</strong>mmon agreed policies on the<br />
basics of paediatric anaesthetic practice.<br />
Notes<br />
1. The RCA re<strong>co</strong>mmends that individuals appointed to a District General Hospital<br />
with a subspeciality interest in paediatric <strong>anaesthesia</strong> should have obtained at<br />
least six months or equivalent of full-time specialist training in paediatric<br />
<strong>anaesthesia</strong> in a specialist paediatric unit.<br />
2. They re<strong>co</strong>mmend that <strong>co</strong>nsultants with a substantial <strong>co</strong>mmitment to paediatric<br />
<strong>anaesthesia</strong>, including full-time paediatric anaesthetists working in specialist<br />
paediatric units need to have obtained at least one year or equivalent of fulltime<br />
specialist training in a specialist unit. This will be started in years 3-5 of<br />
the SpR training programme.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 10
Training policies<br />
Supervision<br />
• Each hospital has its own department of <strong>anaesthesia</strong> policy regarding the<br />
<strong>co</strong>nsultation of senior staff before <strong>anaesthesia</strong> in children. Trainees should not<br />
hesitate to seek advice in any instance of uncertainty.<br />
The RCA re<strong>co</strong>mmends:<br />
• ‘All children should be anaesthetised by a <strong>co</strong>nsultant or other career-grade<br />
anaesthetist who has regular relevant paediatric practice, or a trainee supervised<br />
by someone in the preceding categories. Supervision will vary ac<strong>co</strong>rding to the<br />
ability and experience of the trainee and the nature of the case. For example, an<br />
SHO with less than six months experience requires direct supervision in theatre or<br />
in the theatre suite, whilst an experienced SpR who has undergone a recent period<br />
of paediatric anaesthetic higher specialist training might be supervised by a<br />
<strong>co</strong>nsultant outside the hospital suite’.<br />
Resuscitation<br />
* Info at: www.resus.org.<strong>uk</strong><br />
1. All trainees should be able to perform appropriate resuscitation on children.<br />
2. Each hospital where children are anaesthetised should provide resuscitation<br />
training.<br />
3. All trainees should be en<strong>co</strong>uraged to attend a PALS or other suitable<br />
resuscitation training <strong>co</strong>urse.*<br />
4. All trainees who are interested in a career in paediatric <strong>anaesthesia</strong> should<br />
<strong>co</strong>mplete a PALS, APLS or other suitable resuscitation training <strong>co</strong>urse.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 11
Paediatric Emergency Chart<br />
Age Weight Length<br />
ET Tube<br />
Diameter<br />
ET Tube<br />
Length<br />
First dose of<br />
Epinephrine<br />
Atropine<br />
100 mcg/ml<br />
Bicarbonate*<br />
4.2% *<br />
Calcium<br />
Chloride 10%<br />
Lignocaine<br />
1%<br />
Amiodarone<br />
(50 th centile) crown/heel<br />
(50 th centile)<br />
uncuffed (oral) 1:10,000<br />
100 mcg/ml)<br />
(500 mcg amp<br />
in 5 ml water)<br />
0.5 mmol/ml 10 mg/ml (300 mg/10ml)<br />
dilute + flush<br />
with 5% glu<strong>co</strong>se<br />
Newborn 3.5 kg 50 cms 3.0 ID mm 9 cm 30 mcg/0.3 ml 100 mcg/1.0 ml 3.5 mmol/7.0 ml 0.7 ml 0.35 ml 17.5 mg/0.58 ml<br />
1 month 4.0 kg 53 cms 3.0 ID mm 9 cm 40 mcg/0.4 ml 100 mcg/1.0 ml 4.0 mmol/8.0 ml 0.8 ml 0.4 ml 20 mg/0.66 ml<br />
3 months 5.0 kg 60 cms 3.0-3.5 ID mm 10 cm 50 mcg/0.5 ml 100 mcg/1.0 ml 5.0 mmol/10 ml 1.0 ml 0.5 ml 25 mg/0.83 ml<br />
Bicarbonate<br />
* 8.4% *<br />
1.0 mmol/ml<br />
6 months 7.0 kg 66 cms 3.5 ID mm 11 cm 70 mcg/0.7 ml 140 mcg/1.4 ml 7.0 mmol/7.0 ml 1.4 ml 0.7 ml 35 mg/1.16 ml<br />
1 year 10 kg 75 cms 4.0 ID mm 12 cm 100 mcg/1.0 ml 200 mcg/2.0 ml 10 mmol/10 ml 2.0 ml 1.0 ml 50 mg/1.66 ml<br />
2 years 12 kg 85 cms 4.5 ID mm 13 cm 120 mcg/1.2 ml 240 mcg/2.4 ml 12 mmol/12 ml 2.4 ml 1.2 ml 60 mg/2 ml<br />
3 years 14 kg 93 cms 4.5-5.0 ID mm 13-14 cm 140 mcg/1.4 ml 280 mcg/2.8 ml 14 mmol/14 ml 2.8 ml 1.4 ml 70 mg/2.33 ml<br />
4 years 16 kg 100 cms 5.0 ID mm 14 cm 160 mcg/1.6 ml 320 mcg/3.2 ml 16 mmol/16 ml 3.2 ml 1.6 ml 80 mg/2.66 ml<br />
5 years 18 kg 108 cms 5.0-5.5 ID mm 14-15 cm 180 mcg/1.8 ml 360 mcg/3.6 ml 18 mmol/18 ml 3.6 ml 1.8 ml 90 mg/3 ml<br />
6 years 20 kg 115 cms 5.5 ID mm 15 cm 200 mcg/2.0 ml 400 mcg/4.0 ml 20 mmol/20 ml 4.0 ml 2.0 ml 100 mg/3.33 ml<br />
8 years 25 kg 125 cms 6.0-6.5 ID mm 16 cm 250 mcg/2.5 ml 500 mcg/5.0 ml 25 mmol/25 ml 5.0 ml 2.5 ml 125 mg/4.16 ml<br />
10 years 34 kg 140 cms 7.0 (cuffed)<br />
ID mm<br />
17 cm 340 mcg/3.4 ml 500 mcg/5.0 ml 34 mmol/34 ml 7.0 ml 3.5 ml 170 mg/5.66 ml<br />
Epinephrine may be given endotracheally in 10x the initial<br />
intravenous dose<br />
(NB: more <strong>co</strong>ncentrated solutions may be required)<br />
OTHER DOSES<br />
Epinephrine During CPR a dose 10x the initial one may be <strong>co</strong>nsidered especially<br />
if sepsis or anaphylaxis were primary causes of arrest<br />
Glu<strong>co</strong>se 500 mg -1 g/kg (5-10 ml/kg 10%)<br />
Fluid bolus 0.9% saline or <strong>co</strong>lloid: 20 ml/kg (repeat depending on response)<br />
Defibrillation 1 st series = 2 J/kg, 2 J/kg, 4 J/kg. All subsequent series are at 4 J/kg<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 9
Fasting<br />
for general <strong>anaesthesia</strong><br />
• Children over 1 year<br />
p No food or milk for 6 hours prior to <strong>anaesthesia</strong><br />
p Clear fluids may be given up to 2 hours before <strong>anaesthesia</strong><br />
• Babies under 1 year on regular milk feeds<br />
p No formula milk feeds for 6 hours prior to <strong>anaesthesia</strong><br />
p No breast milk for 4 hours prior to <strong>anaesthesia</strong><br />
p Clear fluids may be given up to 2 hours before <strong>anaesthesia</strong><br />
p<br />
Babies having 2 hourly milk feeds - please discuss with the anaesthetist<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 10
Preoperative upper respiratory tract infections<br />
suggested management for general <strong>anaesthesia</strong><br />
• General <strong>anaesthesia</strong> in the presence of acute or recent URTI has been<br />
associated with: - hypoxaemia<br />
- laryngospasm<br />
- bronchospasm<br />
- death<br />
• Overall, the risk of adverse respiratory events increased by 2 - 7 times<br />
• Risk is increased by 10 times if endotracheal intubation is employed<br />
A. Children with URTI: ie. p Fever > 38 0 C<br />
p Mu<strong>co</strong>purulent nasal secretions<br />
p Lower respiratory symptoms/signs<br />
p Elevated WCC etc<br />
• Postpone surgery for 2 - 4 weeks<br />
B. Children with MILD URTI: ie. p Not unwell<br />
p Clear nasal discharge<br />
p Clear chest<br />
Age < 1 year<br />
Age 1 - 5 years<br />
Age > 5 years<br />
• Postpone surgery for 2 - 4 weeks<br />
• Consider risk / benefit ratio on<br />
an individual basis<br />
• At low risk<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 11
Endocarditis prophylaxis<br />
• At risk patients<br />
All patients with structural cardiac defects<br />
whether repaired or not, are at risk.<br />
Exceptions p suture repair of ASD<br />
p ligation of PDA<br />
• Procedures<br />
All surgery or diagnostic procedures<br />
where bacteraemia is a significant risk,<br />
including all instrumentation or incisions<br />
involving mu<strong>co</strong>us membrane lined tracts,<br />
and any surgery involving infected areas.<br />
Exceptions p tracheal intubation<br />
p flexible bronchos<strong>co</strong>py<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 12
suggested management of<br />
Incidental heart murmurs<br />
• Proto<strong>co</strong>l for patients found to have a murmur prior to elective surgery<br />
The vast majority of children found to have a murmur pre-operatively have an innocent murmur.<br />
These innocent murmurs are characterised by being soft, early systolic murmurs with no thrill or<br />
abnormal cardiac impulses and are not associated with cardiac signs or symptoms. If a child is<br />
found to have a murmur prior to elective surgery a history and cardiac examination should be<br />
performed and an ECG done.<br />
• In the presence of a murmur an<br />
echocardiogram and cardiac opinion<br />
is indicated prior to surgery if:<br />
1.<br />
2.<br />
3.<br />
4.<br />
The child is younger than a year<br />
The murmur fits pathological criteria<br />
There are cardiac signs or symptoms<br />
Evidence of LVH or RVH<br />
(see following tables)<br />
• Criteria for pathological murmurs<br />
1. All diastolic murmurs<br />
2. All pansystolic<br />
3. Late systolic<br />
4. Very loud murmurs<br />
5. Continuous murmurs<br />
(other than a venous hum)<br />
6. Associated with cardiac signs or symptoms<br />
Diagnostic Tables (Davignan et al, 1979)<br />
Right ventricular hypertrophy<br />
1 - 5 years 5 - 12 years<br />
R wave amplitude in V1 > 1.75 mV > 1.25 mV<br />
R/S ratio in V1 > 3 > 2<br />
Also an upright T wave in V1 is a sign of right ventricular hypertrophy in the first 5 years of life<br />
Left ventricular hypertrophy<br />
1 - 5 years 5 - 12 years<br />
RV6 + SV1 > 4.0 mV > 4.55 mV<br />
RV5 > 3.5 mV > 3.75 mV<br />
Also Q waves in V5 or V6 > 4 mV is a useful sign of LVH<br />
Biventricular hypertrophy<br />
R + S in V4<br />
> 1 year<br />
> 5 mV<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 13
Suggested pain management<br />
The plan of <strong>anaesthesia</strong> should always include postoperative analgesia.<br />
Analgesic ladder<br />
Increasing pain<br />
severe<br />
slight<br />
mild<br />
Paracetamol<br />
+<br />
NSAID<br />
moderate<br />
Paracetamol<br />
NSAID +<br />
weak opioid<br />
eg. <strong>co</strong>deine<br />
Paracetamol,<br />
NSAID +<br />
potent opioid<br />
eg. Morphine<br />
Paracetamol<br />
• Use a multi-modal<br />
approach<br />
p using a <strong>co</strong>mbination of drugs from the following four<br />
groups is logical:<br />
• Local <strong>anaesthesia</strong><br />
• Paracetamol<br />
• NSAIDS<br />
• Opioids<br />
• Follow analgesic<br />
proto<strong>co</strong>ls<br />
p are available in individual hospitals which are written<br />
to suit local circumstances and are updated from<br />
time to time<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 14
Local <strong>anaesthesia</strong> procedures<br />
Use of local <strong>anaesthesia</strong> should be <strong>co</strong>nsidered for every paediatric case.<br />
• Dont forget<br />
wound<br />
infiltration<br />
p It is simple to perform and improves early postoperative<br />
analgesia when other medications may be inadequate or<br />
difficult to administer<br />
• Procedures Group 1 p Ilioinguinal / Iliohypogastric nerve block<br />
p Ilioinguinal / Iliohypogastric / genital branch<br />
of genitofemoral<br />
p Penile *(may be <strong>co</strong>nsidered a Group 2 procedure)<br />
p Rectus sheath block<br />
p Caudal epidural<br />
Group 2<br />
Group 3<br />
p Femoral nerve block<br />
p 3 in 1 block / Fascia Iliaca block<br />
p Axillary brachial plexus block<br />
p Lumbar epidural<br />
p Paravertebral block<br />
p Spinal block in the neonate<br />
p Thoracic epidural<br />
• Training p Trainees should be experienced and <strong>co</strong>mpetent in Group 1<br />
procedures, and at least able to describe the indications<br />
and techniques for those in Groups 2 and 3<br />
p Guidance can be found in a number of texts, see<br />
‘re<strong>co</strong>mmended reading’ section<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 15
Paediatric analgesia & anti-emetics<br />
Drug Dose Comments<br />
PARACETAMOL<br />
NEONATES:<br />
Oral: Loading dose: 15 mg/kg<br />
Then: 10 - 15 mg/kg dose<br />
Max dose: 60 mg/kg/day<br />
Rectal:<br />
Loading dose: 20 mg/kg<br />
Then: 15 mg/kg dose<br />
Max dose: 60 mg/kg/day<br />
Mild analgesic and anti-pyretic<br />
drug<br />
Limit to 5 days duration<br />
OTHERS:<br />
Oral:<br />
Rectal:<br />
Loading dose: 20 mg/kg<br />
Then: 15 mg/kg dose<br />
Max dose: 90 mg/kg/day<br />
Loading dose: 30 – 40 mg/kg<br />
Then: 20 mg/kg dose<br />
Max dose: 90 mg/kg/day<br />
DICLOFENAC Oral / Rectal: 1 mg/kg 8 hourly<br />
Max dose: 50 mg<br />
Max daily dose: 150 mg/day<br />
Not neonates or infants < 6 mths<br />
Caution in asthma or renal<br />
impairment<br />
IBUPROFEN Oral: 5 mg/kg 6 hrly<br />
Max dose: 200 mg<br />
Max daily dose: 800 mg/day<br />
Not neonates or infants < 6mths<br />
Caution in asthma or renal<br />
impairment<br />
CODEINE Oral / Rectal: 1 - 1.5 mg/kg 4 - 6 hrly<br />
IM: 1 mg/kg 4 - 6 hrly<br />
Max dose: 60 mg<br />
Combine with paracetamol.<br />
Must never be given IV -<br />
hypotension occurs<br />
MORPHINE Oral: ≥ 1 yr 200 - 400 mcg/kg 4 hrly<br />
IV:<br />
Loading dose: 50 - 100 mcg/kg<br />
Infusion: 10 - 30 mcg/kg/hr<br />
Monitor respiration<br />
Always prescribe NALOXONE<br />
PRN for respiratory depression<br />
MORPHINE INFUSION<br />
PROTOCOL<br />
(for age ≥ 6 mths with<br />
suitable monitoring<br />
Morphine sulphate 0.5 mg/kg<br />
in 50 mls solution<br />
Rate: 1 - 3 ml/hr (1 ml/hr = 10 mcg/kg/hr)<br />
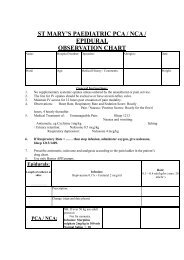
PCA & NCA - if available,<br />
<strong>co</strong>nsult proto<strong>co</strong>ls at individual<br />
hospitals<br />
NALOXONE IV: 4 micrograms/kg For respiratory depression:<br />
< 5 yrs rate < 20/min<br />
≥ 5 yrs rate < 10/min<br />
CYCLIZINE Oral / IV: 1 mg/kg<br />
Max dose: 50 mg<br />
Max daily dose: 150 mg/day<br />
ONDANSETRON Oral / IV: 100 mcg/kg<br />
Max dose: 4 mg<br />
Frequency 8 hourly<br />
Anti-emetics may be <strong>co</strong>mbined<br />
Frequency 8 hourly<br />
Anti-emetics may be <strong>co</strong>mbined<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 16
Max daily dose: 12 mg/day<br />
Fluid balance<br />
suggested intraoperative fluid management<br />
• Objectives<br />
• Maintain normal circulating volume<br />
• Maintain normal electrolyte balance<br />
• Maintain normoglycaemia<br />
• Maintain haemoglobin at an appropriate level<br />
The following regime is a guide to fluid management<br />
1. Replace fluid deficit due<br />
to starvation<br />
CALCULATION<br />
the hourly maintenance fluid x no. hours starvation<br />
2. Give intraoperative<br />
maintenance fluids<br />
for example<br />
3. Replace on-going fluid<br />
losses<br />
Intraoperative fluid should be given as Hartmans solution 1 .<br />
Maintenance fluids should be calculated ac<strong>co</strong>rding to the<br />
following formula:<br />
Body weight (kg)<br />
First 10 kg<br />
Se<strong>co</strong>nd 10 kg<br />
Subsequent kg<br />
a 6 kg infant would require 24 ml/hr<br />
a 14 kg child would require 48 ml/hr<br />
a 25 kg child would require 65 ml/hr<br />
• Measure / estimate blood loss<br />
• Estimate ‘third space’ losses<br />
Fluid requirement per hour<br />
4 ml/kg<br />
2 ml/kg<br />
1 ml/kg<br />
On-going fluid losses should be replaced with Hartmans, <strong>co</strong>lloid<br />
(gelatin) or blood. Blood replacement and optimum haemoglobin<br />
levels should be discussed preoperatively.<br />
Large volumes may be required to replace third space losses<br />
and should be guided by clinical monitoring<br />
• Minor surgical procedures 1 ml.kg -1 .hr -1<br />
• Major abdominal procedures up to 15-20 ml.kg -1 .h -1<br />
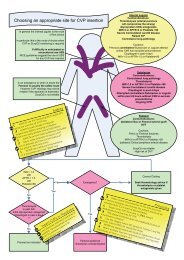
• Assessment and<br />
reassessment of the<br />
cardiovascular system<br />
Fluid replacement should be guided by assessment and<br />
reassessment of the cardiovascular system (capillary refill, HR,<br />
BP, CVP, blood gases and haematocrit as appropriate)<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 17
Hypoglycaemia and hyperglycaemia are potentially harmful. Dextrose <strong>co</strong>ntaining solutions tend to cause<br />
intraoperative hyperglycaemia. However, if a child is ALREADY receiving 10% dextrose preoperatively, this should<br />
be <strong>co</strong>ntinued as the intraoperative maintenance fluid. Blood glu<strong>co</strong>se should be measured during surgery.<br />
• Basic monitoring assumed<br />
• Exercise CAUTION if diagnosis is not certain<br />
Re<strong>co</strong>mmended emergency management of<br />
Acute major anaphylaxis under <strong>anaesthesia</strong><br />
IMMEDIATE MANAGEMENT<br />
SECONDARY MANAGEMENT<br />
Dis<strong>co</strong>ntinue administration of suspect drug<br />
Summon help<br />
Maintain airway with 100% oxygen<br />
(<strong>co</strong>nsider tracheal intubation and IPPV)<br />
Give ADRENALINE<br />
0.05 - 0.1 ml/kg of 1:10,000 ie. 5 - 10 mcg/kg<br />
especially if bronchospasm present.<br />
Further similar doses may be necessary for<br />
hypotension and bronchospasm.<br />
Continuous infusion may be necessary<br />
0.1 - 0.5 mcg/kg/min<br />
To make solution: 300 mcg/kg in 50 mls<br />
<strong>St</strong>art at: 1 ml/hr - 0.1 mcg/kg/min<br />
<strong>St</strong>art intravascular volume expansion<br />
with Hartmann’s or saline solution<br />
Initially: 10 - 20 ml/kg bolus - rapidly<br />
Repeat as necessary<br />
Consider external chest <strong>co</strong>mpressions<br />
When patient has stabilised<br />
• Blood samples should be taken and placed in<br />
plain tubes as soon as possible at 1, 2, 4 and<br />
12 hour intervals and put in a fridge until<br />
analysed<br />
ADRENALINE-RESISTANT BRONCHOSPASM<br />
Consider:<br />
• SALBUTAMOL<br />
Loading dose: 5 mcg/kg IV<br />
Then:<br />
0.2 - 4 mcg/kg/min<br />
(3 mg/kg in 50 ml 1 ml/hr = 1 mcg/kg/min)<br />
Or:<br />
• AMINOPHYLLINE<br />
Bolus over 20 min:<br />
Then:<br />
5 mg/kg IV<br />
800 mcg/kg/hr<br />
CONSIDER:<br />
1. <strong>St</strong>eroids<br />
• HYDROCORTISONE 4 mg/kg IV<br />
Or:<br />
• METHYLPREDNISOLONE<br />
500 mcg-1 mg/kg IV up to max dose: 4 mg/kg<br />
And:<br />
2. Antihistamines<br />
• • CHLORPHENIRAMINE<br />
(diluted and given slowly over one minute)<br />
< 1 year 250 mcg/kg IV<br />
1 - 5 yrs 2.5 - 5 mg IV<br />
6 - 12 yrs 5 - 10 mg IV<br />
> 12 yrs 10 - 20 mg IV<br />
ACIDOSIS<br />
If severe after 20 min:<br />
SODIUM BICARBONATE<br />
Catecholamine infusions<br />
0.5 - 1 mmol/kg<br />
ADRENALINE Dose range<br />
NORADRENALINE 0.1-0.5 mcg/kg/min<br />
To make solution: 300 mcg/kg in 50 ml<br />
<strong>St</strong>art at: 1 ml/hr = 0.1 mcg/kg/min<br />
• Immunology should then be <strong>co</strong>ntacted about<br />
the investigation<br />
• The drug, fluid or blood thought to be<br />
responsible for the reaction should also be<br />
saved<br />
Clotting screen<br />
Consider possibility of <strong>co</strong>agulopathy<br />
Measure arterial blood gas tensions<br />
for oxygenation and acid-base status<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 18
Re<strong>co</strong>mmended emergency management of<br />
Malignant Hyperthermia<br />
Signs and Symptoms<br />
ACTIVE COOLING to include<br />
MONITORING to include<br />
↑ End tidal CO2<br />
Tachycardia<br />
Fever 2 0 C per hour<br />
Cyanosis<br />
Mottling of skin<br />
Tachypnoea<br />
Arrhythmias<br />
Rigidity<br />
Sweating<br />
Hypercarbia<br />
Labile blood pressure<br />
Intense masseter spasm after<br />
suxamethonium<br />
Ice packs<br />
Cooling blankets<br />
Fans<br />
Cold intravenous fluids<br />
Intragastric, intracystic <strong>co</strong>oling<br />
Peritoneal dialysis using <strong>co</strong>ld<br />
diasylate<br />
Extra<strong>co</strong>rporeal <strong>co</strong>oling if<br />
equipment is available<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Core temperature<br />
Arterial line and CVP line<br />
Urinary catheter<br />
ECG<br />
Pulse oximetry & capnography<br />
Blood gases<br />
Serum glu<strong>co</strong>se<br />
Serum potassium<br />
Blood for CPK<br />
Urine for myoglobin<br />
IMMEDIATE MANAGEMENT<br />
Terminate <strong>anaesthesia</strong> and surgery as soon as possible<br />
SUMMON HELP<br />
Hyperventilate with 100% oxygen through vapour-free circuit and <strong>co</strong>nvert<br />
to nar<strong>co</strong>tic-relaxant technique during termination of surgery<br />
DANTROLENE 2.5 mg/kg IV<br />
Repeat as required at 5.10 min intervals to a maximum cumulative dose of 10 mg/kg<br />
Favourable response indicated by (a) fall in heart rate (c) decline in body temperature<br />
(b) abolition of arrhythmia (d) reduced muscle tone<br />
DANTROLENE should be available in or near operating theatres. Make sure you know where to find it!<br />
START ACTIVE COOLING<br />
• ARRHYTHMIAS<br />
If these persist despite Dantrolene give:<br />
PROCAINAMIDE 1 mg/kg/ml IV<br />
Maximum dose: 15 mg/kg<br />
• ACIDOSIS<br />
Correction with<br />
SODIUIM BICARBONATE<br />
0.5 - 1.0 mmol/kg/dose IV<br />
Repeated as necessary<br />
• HYPERKALAEMIA<br />
Control if necessary using glu<strong>co</strong>se and<br />
INSULIN 0.1 units/kg in 2 ml/kg 50% dextrose IV<br />
• URINE OUTPUT<br />
MANNITOL 0.5 - 1.0 g/kg<br />
(2.5 - 5ml/kg of 20% solution) and/or<br />
FRUSEMIDE 1 mg/kg IV<br />
to maintain urine output (> 1 ml/kg/hr)<br />
TRANSFER TO ICU as soon as possible<br />
Recurrence of hyperthermia may occur during first 24 hours<br />
WHEN PATIENT IS STABILISED<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 19
arrange investigation of patient and relatives<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 20
1.<br />
Re<strong>co</strong>mmended management of Latex Allergy<br />
THREE GROUPS OF PATIENTS EXIST<br />
Group 1 History of anaphylaxis to latex<br />
Group 2 History of allergy to latex or rubber<br />
eg. urticaria, central dermatitis,<br />
eye swelling, bronchospasm<br />
Group 3 High risk group:<br />
No previous reaction but have<br />
a) Spina bifida<br />
b) Genitourinary anomalies<br />
c) Multiple surgical procedures<br />
d) Documented reactions to IV drugs<br />
PREMEDICATION<br />
GROUPS 1 and 2 should be treated identically<br />
IV MEDICATION<br />
i) Methylprednisolone 1 mg/kg 6 hrly IV<br />
Max dose 50 mg/dose<br />
ii) Ranitidine 1 mg/kg 6 hrly IV<br />
over 2 mins<br />
iii) Chlorpheniramine 1 mth-1 yr 250 mcg/kg<br />
1 - 5 yrs 2.5-5 mg<br />
6 - 12 yrs 5-10 mg<br />
All doses IV 6 hrly GIVEN SLOWLY<br />
Notes:<br />
i) At lease two doses must be given preoperatively<br />
and <strong>co</strong>ntinued 24 hours postoperatively<br />
ii) Diluents must not be added to vials through rubber<br />
bungs. The bung must be removed or dispensing<br />
pin with filter (eg. Braun) to be used<br />
PATIENTS WITH ASTHMA<br />
Salbutamol inhaler 6 hrly 2 doses preoperatively<br />
GROUP 3 High risk patients<br />
No special precautions<br />
Maintain high index of suspicion during and after case<br />
TREATMENT OF ANAPHYLAXIS TO LATEX<br />
As per Anaphylaxis Proto<strong>co</strong>l<br />
• Anaphylaxis may be slow in onset and difficult to<br />
diagnose<br />
• A smaller dose of epinephrine may be used if<br />
reaction is not severe<br />
In addition give:<br />
i) Methylprednisolone 1 mg/kg IV<br />
ii) Chlorpheniramine 1 mth-1 yr 250 mcg/kg IV<br />
1-5 yrs 2.5-5 mg IV<br />
6-12 yrs 5-10 mg IV<br />
iii) Ranitidine<br />
1 mg/kg slowly IV<br />
AIM<br />
MANAGEMENT IN THEATRE<br />
To prevent any <strong>co</strong>ntact between the<br />
patient and products <strong>co</strong>ntaining latex<br />
SAFE EQUIPMENT<br />
should be used wherever possible<br />
The following equipment IS safe:<br />
GLOVES - latex free<br />
• Regent - Neotech • Ansell - Dermaprene<br />
RESPIRATORY EQUIPMENT<br />
• Clear sili<strong>co</strong>ne masks eg - King Systems Leardal<br />
• Tracheal tubes Portex<br />
• Airways Geudel<br />
• Filter should be placed at patient end of the<br />
breathing circuits<br />
• Polythene bags should be placed over reservoir<br />
bag of Bain circuit if used (in Group 1 patients only)<br />
• Laryngeal masks<br />
INTRAVENOUS EQUIPMENT<br />
• IV cannulae Jel<strong>co</strong>, Venflon, Neoflon, Abbocath<br />
• Latex free syringes BD Discardit<br />
• Latex free giving sets DOSIFIX - Braun - fluids<br />
SANGOFIX - Braun - blood<br />
• IV giving sets with latex port can be used but<br />
injections should not be made through these parts<br />
- <strong>co</strong>ver with tape<br />
• Dispensing pin with filter (eg. Braun) used to<br />
draw or mix drugs held in ampoule with rubber bung<br />
• Do not mix or draw up drugs through rubber bungs<br />
• CVP Cook - Vygon - Arrow<br />
Avoid injecting through rubber bungs<br />
• Syringe pump infusion eg PCA/NCA/Epidural<br />
Use ordinary syringes with an Intrapur extension<br />
(Braun) with filter between syringe and giving set<br />
MONITORING EQUIPMENT<br />
• ECG electrodes Nel<strong>co</strong>r - Medi<strong>co</strong>test<br />
• BP cuff has to be <strong>co</strong>vered with tape or use<br />
Disposa Cuff (J&J)<br />
• Operating table & trolley Avoid <strong>co</strong>ntact with<br />
mattress by <strong>co</strong>vering with sheet<br />
• Tape / Dressings (avoid elastoplast)<br />
• Transpore (3M), Micropore (3M), Tegaderm (3M)<br />
Hyperfix (Smith & Nephew), <strong>St</strong>eristrips (J&J)<br />
• NG tubes Vygon - Portex<br />
• Suction catheter & tubing Penine<br />
• Yankauer sucker Argyle<br />
• Epidural catheter Portex<br />
• Diathermy 3M plate and lead safe<br />
• Temperature probes Disposable probes can be used<br />
OTHER POINTS<br />
• Patient must be first on list<br />
• Avoid touching latex products and then touching pt<br />
• All staff in dept involved made aware of status<br />
• Reduction of numbers in theatres where possible<br />
• Notices in theatre involved<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 21
General re<strong>co</strong>mmendations<br />
Sickle Cell Disease<br />
suggested perioperative management<br />
• Sickle cell disease (SCD) is a chronic debilitating disease associated with significant perioperative morbidity<br />
and mortality. Meticulous perioperative care is required. Families are generally well informed about the<br />
<strong>co</strong>ndition and appreciate being involved in decisions about care.<br />
• Elective surgery<br />
• Admission<br />
• Scheduling operation<br />
• Precipitating factors<br />
Preoperative preparation checklist<br />
‣ Children with SCD presenting for elective surgery should be discussed<br />
with the anaesthetists and haematologists preoperatively. A plan for<br />
preoperative transfusion will be formulated depending on the child’s<br />
<strong>co</strong>ndition and the nature of the intended surgery. Preparation for<br />
surgery may take at least three weeks as below.<br />
‣ Children should be admitted the day before surgery.<br />
They require blood of the appropriate phenotype to be crossmatched<br />
which may take up to 6 hours.<br />
‣ Children should be scheduled early on the operating list to ensure that<br />
they are not cancelled.<br />
‣ Care should be taken at all times to avoid factors that may precipitate a<br />
sickle crisis. These include dehydration, hypoxia, acidosis, hypothermia<br />
and pain. The majority of crises occur postoperatively.<br />
1. Inform Haematology Team ‣ that a child with sickle cell disease has been admitted<br />
They will help <strong>co</strong>-ordinate with the haematology laboratory<br />
2. Take blood ‣ for full blood <strong>co</strong>unt and electrophoresis (%HbS, HbA, HbF)<br />
3. Crossmatch ‣ 1 unit phenotyped blood for all cases<br />
4. <strong>St</strong>art intravenous<br />
maintenance fluids<br />
5. Consider postoperative<br />
nasal CPAP<br />
‣ 12 hours preoperatively for all cases<br />
‣ if the child has a history of severe obstructive sleep apnoea<br />
Postoperative care<br />
1. Monitor saturation ‣ give oxygen to maintain saturation ≥ 92%<br />
<strong>co</strong>ntinuously<br />
2. Continue intravenous ‣ until the child is tolerating oral fluids<br />
maintenance fluids<br />
3. Postoperative analgesia ‣ ensure this is adequate<br />
4. Contact physiotherapy ‣ en<strong>co</strong>urage early mobilisation<br />
Postoperative sickling <strong>co</strong>mplications<br />
• Serious postoperative <strong>co</strong>mplications (usually within 48 hours of surgery) include:<br />
They may be ac<strong>co</strong>mpanied by fever and may <strong>co</strong>exist.<br />
1. Inform Haematology Team ‣ if any of the above are suspected<br />
2. Treatment of Sickle crisis<br />
includes:<br />
• Over transfusion and hypervis<strong>co</strong>sity must be avoided<br />
• painful crisis<br />
• cerebral event<br />
• chest crisis<br />
‣ intravenous fluids ‣ oxygen therapy ‣ antibiotics<br />
‣ analgesia as indicated ‣ transfusion to Hb>10 g/dl (but
- discuss early with the PICU Team<br />
Sickle Cell Disease<br />
suggested transfusion policy<br />
This transfusion policy has been agreed locally by the haematologists and anaesthetists at GOSH and<br />
referring paediatricians.<br />
Transfusion re<strong>co</strong>mmendations for elective surgery<br />
Patients with a history of severe sickle related problems, such as chest crisis, CNS disease, or frequent painful<br />
crises, or with severe obstructive sleep apnoea or patients undergoing major surgery, have been found to be at<br />
greater risk of serious perioperative <strong>co</strong>mplications. However, aggressive transfusion regimens or emergency<br />
transfusions with blood of inappropriate red cell phenotype are associated with a higher incidence of transfusion<br />
related <strong>co</strong>mplications. A four tiered approach is re<strong>co</strong>mmended, tailored to suit the individual case.<br />
Group 1<br />
Group 2<br />
Group 3<br />
Group 4<br />
‣ Children with no special risk factors, who are currently well, having short procedures<br />
with minimal risk of perioperative <strong>co</strong>mplications eg. insertion of grommets:<br />
‣ Top-up transfusion to Hb >7 g/dl only, irrespective of HbS level<br />
‣ Children with no special risk factors, having intermediate risk surgery eg. body surface<br />
surgery such as herniorrhaphy, or tonsillectomy in older children with mild to moderate<br />
obstructive sleep apnoea:<br />
‣ Top-up transfusion to Hb 9-11 g/dl, irrespective of HbS level<br />
‣ Total Hb should not exceed 12 g/dl<br />
‣ Children who have had a chest crisis or suffer frequent painful crises, or children<br />
undergoing major surgery eg. intra-abdominal surgery (including laparos<strong>co</strong>pic surgery), or<br />
tonsillectomy in children
e<strong>co</strong>mmended reading materials Textbooks<br />
title author / editor publisher<br />
• Manual of pediatric anesthesia <strong>St</strong>eward, David Churchill Livingstone<br />
London: 1995<br />
• Pediatric Anesthesia Gregory, George A Churchill Livingstone<br />
London: 1994<br />
• The surgical neonate:<br />
Anaesthesia and Intensive Care<br />
• Textbook of paediatric<br />
anaesthetic practice<br />
• Pain in infants, children and<br />
adolescents<br />
• Regional <strong>anaesthesia</strong> for<br />
babies and children<br />
Hatch, David<br />
Sumner, Edward<br />
Hellman, Jonathan<br />
Hatch, David<br />
Sumner, Edward<br />
Schechter, Neil<br />
Berde, Charles<br />
Yaster, Myron<br />
Peutrel, Jane M<br />
Mather, <strong>St</strong>ephen J<br />
Arnold<br />
London: 1994<br />
Arnold<br />
London: 1999<br />
Williams and Wilkins<br />
London: 1992<br />
New edition in preparation<br />
Oxford University Press<br />
Oxford: 1997<br />
• Pediatric cardiac anesthesia Lake, Carol Applleton and Lange<br />
London: 1997<br />
• Anesthesia and un<strong>co</strong>mmon<br />
pediatric diseases<br />
• Anesthetic management of<br />
difficult and routine pediatric<br />
patients<br />
Katz<br />
<strong>St</strong>eward<br />
Berry, Frederic<br />
W B Saunders<br />
London: 1993<br />
Churchill Livingstone<br />
London: 1990<br />
• Practice of paediatric ICU Rogers Williams & Wilkins<br />
London: 1987<br />
• Forfar and Arneil’s Textbook of<br />
Pediatrics<br />
• Users’ guides to the medical<br />
literature. A manual for<br />
evidence-based clinical<br />
practice<br />
• Evidence-Based Medicine –<br />
How to practice and teach EBM<br />
Helms, P<br />
Guyatt, G<br />
Rennie D<br />
Sackett, DL<br />
<strong>St</strong>raus, SE<br />
Richardson, WS<br />
Rosenberg, W<br />
Haynes, RB<br />
Churchill Livingstone<br />
London, new edition in press<br />
2002<br />
Journal of American Medical<br />
Association Archive Press<br />
2002, pp 55-79<br />
2 nd Edition<br />
Churchill Livingstone<br />
Edinburgh: 2000<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 24
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 25
e<strong>co</strong>mmended reading materials Journals<br />
(with significant paediatric <strong>co</strong>ntent)<br />
title editors publisher<br />
• Paediatric Anaesthesia Sumner, Edward Blackwell Science<br />
Oxford<br />
• Anesthesiology Todd, Michael American Society of Anesthetists<br />
JB Lippin<strong>co</strong>tt Company<br />
Philadelphia<br />
• Anesthesia and Analgesia Miller, Ronald D Lippin<strong>co</strong>tt, Williams and Wilkins<br />
International Anesthetist Research<br />
Society<br />
Hagerstown, MD USA<br />
• British Journal of<br />
Anaesthesia<br />
• Canadian Journal of<br />
Anaesthesia<br />
• Archives of Disease in<br />
Childhood<br />
Hunter, JM<br />
Craig, Douglas B<br />
Chiswick, Mal<strong>co</strong>lm<br />
Mar<strong>co</strong>vitch, Harvey<br />
Royal College of Anaesthetists<br />
BMJ Publishing Group<br />
Canadian Anaesthetists Society<br />
Toronto<br />
Royal College of Paediatrics and<br />
Child Health<br />
BMJ Publishing Group<br />
• Anaesthesia Harmer, M Association of Anaesthetists of<br />
Great Britain and Ireland<br />
Blackwell Science<br />
• Current Opinion in<br />
Anesthesiology: Paediatric<br />
Issues<br />
Prys-Roberts, Cedric<br />
Lippin<strong>co</strong>tt, Williams & Wilkins<br />
London<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 26
e<strong>co</strong>mmended reading materials Useful publications<br />
title<br />
• Medicines for children<br />
Royal College of Paediatrics and Child<br />
Health Formulary<br />
• GOSH Drug Administration<br />
Guidelines<br />
Great Ormond <strong>St</strong>reet Hospital Anaesthesia<br />
and Pain Formulary<br />
source<br />
RCPCH and NPPG<br />
RCPCH Publications Ltd<br />
50 Hallum <strong>St</strong>, London W1N 6DE<br />
GOSH Trust Print and Publications Unit<br />
C/o Dept of Anaesthesia<br />
GOSH, London WC1N 3JH<br />
(available by post at £6 per <strong>co</strong>py)<br />
• Prevention and <strong>co</strong>ntrol of pain in<br />
children. A Manual for Health Care<br />
Professionals<br />
• NCEPOD<br />
National <strong>co</strong>nfidential enquiry into<br />
perioperative deaths<br />
• Welfare of children and young<br />
people in hospitals (1991)<br />
• Just for the day – children admitted<br />
to hospital for day treatment (1991)<br />
• Children first – a study of hospital<br />
services (1993)<br />
• The transfer of infants and children<br />
for surgery: report of a joint<br />
working group (1993)<br />
• Children’s surgical services: report<br />
of an ad hoc multi-disciplinary<br />
children’s surgical liaison group<br />
(1996)<br />
• Guidelines for the provision for<br />
anaesthetic services<br />
(1994 updated 1999)<br />
• Children’s Surgery – a First Class<br />
Service (2000)<br />
• Learning from Bristol<br />
The Bristol Royal Infirmary Inquiry<br />
(2001)<br />
Royal College of Paediatrics and Child Health<br />
BMJ publishing, London WC1<br />
NCEPOD (1989) - Paediatric surgery/<strong>anaesthesia</strong><br />
NCEPOD (1998-99) - Extremes of age<br />
Department of Health<br />
HMSO, 40 High Holborn WC1, London<br />
Mail Order 020 7873 0011<br />
Caring for children in the Health Services<br />
Action for Sick Children, London<br />
Audit Commission<br />
HMSO, 40 High Holborn WC1, London<br />
Mail Order 020 7873 0011<br />
British Paediatric Association / Royal College of<br />
Paediatrics and Child Health<br />
Royal College of Paediatrics and Child Health<br />
50 Hallum <strong>St</strong>, London W1N 6DE<br />
Royal College of Anaesthetists<br />
48-49 Russell Square, London WC1B 4JP<br />
Report of the Paediatric Forum of the Royal College of<br />
Surgeons of England.<br />
Royal College of Surgeons of England, 35 Lin<strong>co</strong>ln’s Inn<br />
Fields, London WC2<br />
HMSO, 40 High Holborn WC1, London<br />
Mail Order 020 7873 0011<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 27
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 28
e<strong>co</strong>mmended reading materials Internet resources<br />
• Paediatric Resources<br />
PEDINFO: An Index of the Pediatric<br />
Internet<br />
Australian Paediatric Resource<br />
Directory<br />
Emory University Paediatric<br />
Resources<br />
Cedars-Sinai Medical Center<br />
The University of Washington NICU<br />
Web<br />
• Anaesthetic Resources<br />
The Metro Health System in<br />
Cleveland<br />
The University of Sydney<br />
The Association of Ottawa<br />
Anesthesiologists<br />
Paediatric Anaesthesia Journal<br />
• Technology in Anaesthesia<br />
Society for Technology in<br />
Anesthesia<br />
Society for Computing and<br />
Technology in Anaesthesia<br />
Journal of Clinical Monitoring and<br />
Computing<br />
Tech Talk’ Discussion Group<br />
• General Resources for Anaesthetists<br />
Medical Matrix<br />
The Gasnet Global Textbook of<br />
Anesthesiology<br />
The WWW Virtual Library:<br />
Anesthesiology.<br />
Virtual Anaesthesia Textbook<br />
The Hardin Meta Directory for<br />
Anesthesiology<br />
The CSEN Global List of Web sites<br />
on Anaesthesia<br />
Medmark<br />
address<br />
http://pedinfo.org/<br />
http://www.cundle.<strong>co</strong>m.au/gen/paeds/paedsres.html<br />
http://www1.cc.emory.edu/PEDS/gen-ped.htm<br />
http://www.csmc.edu/pediatrics/demo.990525.html<br />
http://neonatal.peds.washington.edu/<br />
http://metrohealthanesthesia.<strong>co</strong>m/links.htm<br />
http://www.usyd.edu.au/su/anaes/anaes.html<br />
http://www.anesthesia.org/professional/linkanes.html<br />
http://www.blacksci.<strong>co</strong>.<strong>uk</strong>/~cgilib/jnlpage.bin?Journal=PAN&File=PAN&Page=links<br />
http://gasnet.org/sta/<br />
http://www.scata.org.<strong>uk</strong>/<br />
http://www.wkap.nl/journalhome.htm/0167-9945<br />
http://www.sickkids.on.ca/Anaesthesia/TechTalk_DG.asp<br />
http://www.medmatrix.org/_SPages/Anesthesiology.asp<br />
http://gasnet.org/gta/<br />
http://www.gasnet.org/vl/vl.php3<br />
http://www.virtual-<strong>anaesthesia</strong>-textbook.<strong>co</strong>m/<br />
http://www.arcade.uiowa.edu/hardin-www/md-anesth.html<br />
http://www.csen.<strong>co</strong>m/anesthesia-websites/<br />
http://medmark.org/anes.ane2.html<br />
The Virtual Hospital<br />
• Anaesthetic Departments<br />
The Packard Children’s Hospital in<br />
<strong>St</strong>anford<br />
The Virtual Children’s Hospital<br />
The Mott Children’s Hospital in Ann<br />
Arbor<br />
The University of Wis<strong>co</strong>nsin major<br />
topics in anesthesia<br />
Alberta Children’s Hospital in<br />
Calgary<br />
http://www.vh.org/<br />
http://www.pedsanesthesia.stanford.edu/guidelines/<br />
http://www.vh.org/VCH/Providers.Information.html<br />
http://www.anes.med.umich.edu/pediatrics/default.htm<br />
http://www.anesthesia.wisc.edu/Topics/Pediatric_Anesthesia/ped_anesth.html<br />
http://www.crha-health.ab.ca/clin/anaesth/paed/paed.htm<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 29
The Women’s and Children’s<br />
Hospital in Adelaide<br />
http://www.wch.sa.gov.au/paed-anaes/pgi/index.html<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 30
Internet Resources (<strong>co</strong>nt)<br />
• International Societies<br />
The Association of Paediatric<br />
Anaesthetists of Great Britain and<br />
Ireland<br />
The Federation of European<br />
Associations of Paediatric<br />
Anaesthetists<br />
The Society for Pediatric Anesthesia<br />
Society for Paediatric Anaesthesia in<br />
New Zealand and Australia<br />
French Speaking Association of<br />
Paediatric Anaesthetists<br />
Italian Society for Paediatric and<br />
Neonatal Anaesthesia and Intensive<br />
Care<br />
• General Paediatric References<br />
Pediatric Points of Interest<br />
The American Academy of<br />
Pediatrics<br />
General Pediatrics.<strong>co</strong>m<br />
The Vanderbilt Pediatric Interactive<br />
Digital Library<br />
• Rare diseases<br />
PEDBASE<br />
National Organisation for Rare<br />
Disorders<br />
Online Mendelian Inheritance in Man<br />
• Paediatric Subsections<br />
WebPath<br />
The VCH Imaging Encyclopædia of<br />
Pediatric disease<br />
The Digital Library of Paediatric<br />
Radiology<br />
The University of Cleveland<br />
radiology Web site<br />
Rush Children’s Hospital<br />
The Children’s Health Information<br />
Network<br />
The University of Kansas Paediatric<br />
teaching files<br />
address<br />
http://www.apa-gbi.org/<br />
http://free.med.pl/feapa/<br />
http://www.pedsanesthesia.org/<br />
http://www.spanza.org.au/<br />
http://www.invivo.net/adarpef/pedia.htm<br />
http://utenti.tripod.it/SARNePI<br />
http://www.med.jhu.edu/peds/neonatology/poi.html<br />
http://www.aap.org/bpi/default.htm<br />
http://www.generalpediatrics.<strong>co</strong>m/<br />
Http://www.mc.vanderbilt.edu/peds/pidl/index.htm<br />
http://www.i<strong>co</strong>ndata.<strong>co</strong>m/health/pedbase/pedlynx.htm<br />
http://www.rarediseases.org/rdb/over.htm<br />
http://www3/mcbi/nlm.nih.gov/omim/<br />
Pathology<br />
http://www-medlib.med.utah.edu/WebPath/PEDHTML/PEDIDX.html<br />
Radiology<br />
http://www.vh.org/Providers/TeachingFiles/PAP/PAPHome.html<br />
http://www.pediatricradiology.<strong>co</strong>m/<br />
http://uhrad.<strong>co</strong>m/pedsarc.htm<br />
Cardiology<br />
http://www.rchc.rush.edu/ped%20card%20prof.htm<br />
http://www.tchin.org/ilinks/profess/c_profess.htm#P01<br />
http://www.kumc.edu/kumcpeds/cardiology/cardiology.html<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 31
Internet Resources (<strong>co</strong>nt)<br />
• Paediatric Subspecialties<br />
Pediatric Critical Care Medicine<br />
<strong>St</strong> Paul’s Neonatal Intensive Care<br />
Unit<br />
Neonatology On the Web<br />
The University of Minnesota<br />
Neonatology teaching files<br />
The University of Miami ‘Hot<br />
Neonatology Web sites’<br />
The Paediatric Pain Research Lab<br />
Oxford Pain Internet site<br />
Bandolier Home Page<br />
Pain.<strong>co</strong>m<br />
The Toronto Paediatric Anesthesia<br />
Conference – Discussion Group<br />
Gasnet Anesthesiology Discussion<br />
Group<br />
• Online journals<br />
Anaesthesia Web free online<br />
journals<br />
The Internet Journal of<br />
Anesthesiology<br />
• Anaesthesia Simulators<br />
The University of Rochester<br />
International Simulator list<br />
The Bristol Medical Simulation<br />
Centre<br />
• Palm Computing Web sites<br />
Medical software for EPOC<br />
Medical PDA site<br />
Palm Medicine<br />
Tu<strong>co</strong>ws<br />
address<br />
Critical care and Neonatology<br />
http://pedsccm.wustl.edu/PedsCCM_Home_page.html<br />
http://www.peds.umn.edu/divisions/neonatology/spnicu/guide.html<br />
http://www.neonatology.org/neo.links.web.html<br />
http://www.peds.umn.edu/divisions/neonatology/tfiles/tf.html<br />
http://members.home.net/<strong>co</strong>tton/neoweb.html<br />
Pain<br />
http://is.dal.ca/~pedpain/<br />
http://www.jr2.ox.ac.<strong>uk</strong>/Bandolier/painres/painpag/index.html<br />
http://www.jr2.ox.ac.<strong>uk</strong>/bandolier/<br />
http://www.pain.<strong>co</strong>m/<br />
Discussion Groups<br />
http://www.sickkids.on.ca/anaethesia/pac_dg.asp<br />
http://gasnet.org/maillist/<br />
http://www.aims.org.sg/saw/elecjourl.htm<br />
http://www.ispub.<strong>co</strong>m/journals/ija.html<br />
http://web.anes.rochester.edu/simulate/webpages.htm<br />
http://bristol.ac.<strong>uk</strong>/Depts/BMSC/<br />
http://dnausers.d-n-a.net/psionmed/psimed/soft5.htm<br />
http://www.pdamd.<strong>co</strong>m/<br />
http://hometown.aol.<strong>co</strong>m/roboh98/palm.html<br />
http://pda.tu<strong>co</strong>ws.<strong>co</strong>m/epoc/mecical5.htm<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 32
e<strong>co</strong>mmended reading materials Key references<br />
General<br />
Association of Anaesthetists. Anaphylactic reactions associated with <strong>anaesthesia</strong>, 1990.<br />
Phillips S, Daborn AK and Hatch DJ. Perioperative fasting for paediatric <strong>anaesthesia</strong>.<br />
Anaesthesia 1994; 73(4): 529-36.<br />
British Journal of<br />
McEwan AI, Birch M and Bingham R. The preoperative management of the child with a heart murmur.<br />
Paediatric Anaesthesia 1995; 5(3):151-156.<br />
<strong>St</strong>eward D. Malignant hyperthermia. Manual of Paediatric Anaesthesia, 163- 170.<br />
Bacterial Endocarditis. Lancet 1992; 339: 1292-1293.<br />
Bacterial Endocarditis. Journal of the American Medical Association 1997; 227: 1794-1801.<br />
Upper respiratory tract infections<br />
Tait AR and Knight PR. Intraoperative respiratory <strong>co</strong>mplication in patients with upper respiratory tract<br />
infections. Canadian Journal of Anaesthesia 1987.<br />
Tait AR and Knight PR. The effects of general <strong>anaesthesia</strong> on upper respiratory tract infections in children.<br />
Anesthesiology 1987.<br />
Desoto H. Changes in oxygen saturation following general <strong>anaesthesia</strong> in children with upper respiratory<br />
infection signs and symptoms undergoing otolaryngological procedures. Anesthesiology 1988.<br />
Anaesthesia and upper respiratory tract infections - a non-existent hazard. (editorial) British Journal of<br />
Anaesthesia May 1990.<br />
Cohen MM and Cameron CB. Should you cancel an operation when a child has an upper respiratory tract<br />
infection? Anesthesia and Analgesia 1991.<br />
Levy L and Tait AR. Upper respiratory tract infection and general <strong>anaesthesia</strong> in children.<br />
1992.<br />
Anaesthesia<br />
Tait AR et al. Risk factors for perioperative adverse respiratory events. Anesthesiology 2001; 95: 299-306.<br />
Sickle cell<br />
Vichinsky E et al. A <strong>co</strong>mparison of <strong>co</strong>nservative and aggressive transfusion regimens in the perioperative<br />
management of sickle disease. New England Journal of Medicine 1995; 333: 206-13.<br />
Waldron et al. Tonsillectomy, adenoidectomy and myringotomy in sickle cell disease: perioperative<br />
morbidity. Journal of Pediatric Hematology / On<strong>co</strong>logy 1992; 21(2): 129-135.<br />
Adams et al. Successful surgical out<strong>co</strong>me in children with sickle hemaglobinopathies: the D<strong>uk</strong>e University<br />
experience. Journal of Pediatric Surgery 1998; 33: 428-432.<br />
Yardumian and Rossiter. The North Middlesex Hospital Guidelines for preparation of children with sickle cell<br />
disease for surgery. (Personal <strong>co</strong>mmunication)<br />
Organisation<br />
National <strong>co</strong>nfidential enquiry into perioperative deaths 1989. The Royal College of Surgeons of England.<br />
The Royal College of Anaesthetists.<br />
Welfare of children and young people in hospitals. Department of Health, HMSO, London 1991.<br />
Just for the day – children admitted to hospital for day treatment. Caring for children in the Health Services,<br />
London 1991.<br />
Children first – a study of hospital services. Audit Commission, HMSO, London 1993.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 33
British Paediatric Association / Royal College of Paediatric and Child Health. The transfer of infants and<br />
children for surgery: report of a joint working group, 1993.<br />
Royal College of Paediatrics and Child Health. Children’s surgical services: report of an ad hoc multidisciplinary<br />
children’s surgical liaison group, 1996.<br />
Key references (<strong>co</strong>nt)<br />
Paediatric intensive care: a framework for the future. National Co-ordinating Group on Paediatric Intensive<br />
Care / NHS Executive, 1997.<br />
National <strong>co</strong>nfidential enquiry into perioperative deaths. Extremes of age. NCEPOD London 1999.<br />
Royal College of Surgeons of England. Report of the Paediatric Forum of the Royal College of Surgeons of<br />
England. Children’s Surgery – a First Class Service, 2000.<br />
Guidelines for the provision for anaesthetic services. Royal College of Anaesthetists 1994, updated 1999.<br />
Learning from Bristol. The Bristol Royal Infirmary Inquiry. HMSO 2001.<br />
Fluid balance<br />
AI Arieff. Postoperative hyponatraemic encephalopathy following elective surgery in children.<br />
Anaesthesia 1998; 8: 1-4.<br />
Paediatric<br />
Nattie EE and Edwards WH. Brain and CSF water in newborn puppies during acute hypo and<br />
hypernatraemia. Journal of Applied Physiology 1981; 51: 1086-1091.<br />
Holliday MA and Segar WE. The maintenance need for water in parenteral fluid therapy. Paediatrics 1957;<br />
19: 823-832.<br />
Berry FA. Practical aspects of fluid and electrolyte therapy. Berry FA, (ed). Anaesthetic Management of<br />
Difficult and Routine Pediatric Patients. 2 nd ed. New York: Churchill Livingston 1990: 89-120.<br />
Scheingraber S, Renm M, Sehmisch C et al. Rapid saline infusion produces hyperchloremic acidosis in<br />
patients undergoing gynae<strong>co</strong>logic surgery. Anesthesiology 1999; 90: 1265-1270.<br />
Hatch D, Sumner E and Hellman J. The surgical neonate. The surgical neonate: Anaesthesia and Intensive<br />
Care. 3 rd ed. London: Edward Arnold, 1995: 104-110.<br />
Huskisson L. Fluid balance: all aspects. Paediatric Anaesthesia. 2 nd ed. London: Arnold, 2000: 233-248.<br />
Leelan<strong>uk</strong>rom R and Cunliffe M. Intraoperative fluid and glu<strong>co</strong>se management in children.<br />
Anaesthesia 2000; 10: 353-359.<br />
Paediatric<br />
Sandstorm K, Larsson LE and Nilsson K. Four different fluid regimes during and after minor paediatric<br />
surgery – a study of blood glu<strong>co</strong>se <strong>co</strong>ncentrations. Paediatric Anaesthesia 1994; 4: 235-242.<br />
Srinivasan G, Jain R, Pildes RS et al. Glu<strong>co</strong>se homeostasis during <strong>anaesthesia</strong> and surgery in infants.<br />
Journal of Pediatric Surgery 1986; 21: 718-721.<br />
<strong>St</strong>eward DJ. Hyperglycaemia, something to worry about! Paediatric Anaesthesia 1992; 2: 81-83.<br />
Jensen BH, Wernberg M and Andersen M. Preoperative starvation and blood glu<strong>co</strong>se <strong>co</strong>ncentrations in<br />
children undergoing impatient and outpatient <strong>anaesthesia</strong>. British Journal of Anaesthesia 1982; 54:<br />
1071-1074.<br />
Payne K and Ireland P. Plasma glu<strong>co</strong>se level in the peri-operative period in children. Anaesthesia 1984; 39:<br />
868-872.<br />
Tuckey J, Mather SJ and Thornton PGN. Can persistent cerebral damage be caused by hyperglycaemia?<br />
Paediatric Anaesthesia 1996; 6: 345-346<br />
Nakakimura K, Fleischer JE, Drummond JC et al. Glu<strong>co</strong>se administration before cardiac arrest worsens<br />
neurologic out<strong>co</strong>me in cats. Anesthesiology 1990; 72: 1005-1011.<br />
Drummond JC and Moore SS. The influence of dextrose administration on neurologic out<strong>co</strong>me after<br />
temporary spinal <strong>co</strong>rd ischaemia in the rabbit. Anesthesiology 1989; 70: 64-70.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 34
Longstreth WT, Diehr P, Cobb LA et al. Neurologic out<strong>co</strong>me and blood glu<strong>co</strong>se levels during out-of-hospital<br />
cardiopulmonary resuscitation. Neurology 1986; 36: 1186-1191.<br />
Siker D. Paediatric fluids and electrolytes. Pediatric Anaesthesia 2 nd ed. New York: Churchill Livingstone<br />
1989: 581-617.<br />
Vincent JL. Fluids for resuscitation. British Journal of Anaesthesia 1991; 67: 185-193.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 35
Journal Club: publications of interest<br />
Updated: E Jackson May 2002<br />
Evaluation of Evidence see:<br />
A manual for evidence-based clinical practice.<br />
Eds. Guyatt G and Rennie D. Users Guides to the Medical Literature:<br />
Journal of American Medical Association 2002; pp 55-79.<br />
* latest/most recent references<br />
Premedication<br />
Brosius KK and Bannister CF. Effect of oral midazolam premedication on the awakening <strong>co</strong>ncentration of<br />
sevoflurane, re<strong>co</strong>very times and bispectral index in children. Paediatric Anaesth. 2001; 11(5): 585-590.<br />
* Brosius KK and Bannister CF. Oral midazolam premedication in preadolescents and adolescents.<br />
Anesthesia and Analgesia 2002; 94(1):31-6.<br />
* Lammers CR, Rosner JL, Crockett DE, Chhokra R and Brock-Utne JG. Oral midazolam with an antacid may<br />
increase the speed of onset of sedation in children prior to general <strong>anaesthesia</strong>. Paediatric<br />
Anaesthesia 2002; (1):26-8.<br />
Marhofer P, Freitag H, Hochtl A, Greher M, Erlacher W, Semsroth M. S(+)-ketamine for rectal premedication<br />
in children. Anesthesia and Analgesia 2001; 92(1): 62-5.<br />
General <strong>anaesthesia</strong><br />
Aantaa R, Takala R and Muittari P. Sevoflurane EC50 and EC95 values for laryngeal mask insertion and<br />
tracheal intubation in children. British Journal of Anaesthesia 2001; 86(2): 213-216.<br />
* Anderson BJ and Meakin GH. Scaling for size: some implications for paediatric <strong>anaesthesia</strong> dosing.<br />
Paediatric Anaesthesia 2002; 12(3): 205-19. (review)<br />
Ayers J and Graves SA. Perioperative management of total parental nutrition, glu<strong>co</strong>se <strong>co</strong>ntaining solutions,<br />
and intraoperative glu<strong>co</strong>se monitoring in paediatric patients. A survey of clinical practice. Paediatric<br />
Anaesthesia 2001; 11(1): 41-44.<br />
* Bannister CF, Brosius KK, Sigl JC, Meyer BJ and Sebel PS. The effect of bispectral index monitoring on<br />
anesthetic use and re<strong>co</strong>very in children anesthetized with sevoflurane in nitrous oxide. Anesthesia and<br />
Analgesia 2001; 92(4) 877-81.<br />
* Bellew M, Atkinson KR, Dixon G and Yates A. The introduction of a paediatric <strong>anaesthesia</strong> information<br />
leaflet: an audit of its impact on parental anxiety and satisfaction. Paed. Anaesth. 2002; 12(2): 124-30.<br />
Blan<strong>co</strong> G, Melman E, Cuairan V, Moyao D and Ortiz-Monasterio F. Fibreoptic nasal intubation in children<br />
with anticipated and unanticipated difficult intubation. Paediatric Anaesthesia 2001; 11(1): 49-53.<br />
* Bozkurt P. The analgesic efficacy and neuroendocrine response in paediatric patients treated with two<br />
analgesic techniques: using morphine-epidural and patient-<strong>co</strong>ntrolled analgesia. Paediatric<br />
Anaesthesia 2002; 12(3): 248-54.<br />
* Brock-Utne JG. Is cri<strong>co</strong>id pressure necessary? Paediatric Anaesthesia 2002; 12(1): 1-4.<br />
* Bussolin L and Busoni P. The use of the cuffed oropharyngeal airway in paediatric patients. Paediatric<br />
Anaesthesia 2002; 12(1): 43-7.<br />
* Busoni P, Sarti A, Crescioli M, Agostino MR, Sestini G and Banti S. Motion sickness and postoperative<br />
vomiting in children. Paediatric Anaesthesia 2002; 12(1): 65-8.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 36
* Chambers N, Lopez T, Thomas J and James MF. Remifentanil and the tunnelling phase of paediatric<br />
ventriculoperitoneal shunt insertion. A double-blind, randomised, prospective study. Anaesthesia<br />
2002; 57(2): 133-9.<br />
* Chan CS and Molassiotis A. The effects of an educational programme on the anxiety and satisfaction level<br />
of parents having parent present induction and visitation in a post<strong>anaesthesia</strong> care unit. Paediatric<br />
Anaesthesia 2002; 12(2): 131-9.<br />
* Cheng CA, Aun CS and Gin T. Comparison of rocuronium and suxamethonium for rapid tracheal intubation<br />
in children. Paediatric Anaesthesia 2002; 12(2): 140-5.<br />
* Cohen IT, Hannallah RS and Hummer KA. The incidence of emergence agitation associated with<br />
desflurane anesthesia in children is reduced by fentanyl. Anesthesia and Analgesia 2001; 93(1): 88-<br />
91.<br />
Cote’ C. The upper respiratory tract infection (URI) dilemma. Anesthesiology 2001; 95(2): 283-285<br />
Davidson A, McCann M, Devavaram P, Auble S, Sullivan L, Gillis J M and Laussen P C. The difference in<br />
the bispectral index between infants and children during emergency from anesthesia after circumcision<br />
surgery. Anesthesia and Analgesia 2001; 93(2): 326-330.<br />
De Fatima, De Assuncao Braga, Da Silva Braga A, Poterio FM, Filier GM and Cremonesi PR. The effect of<br />
different doses of propofol on tracheal intubating <strong>co</strong>nditions without muscle relaxant in children.<br />
European Journal of Anaesthesiology 2001; 18(6): 384-8.<br />
Degoute CS, Macabeo C, Dubreuil C, Duclaux R and Banssillon V. EEG bispectral index and hypnotic<br />
<strong>co</strong>mponent of <strong>anaesthesia</strong> induced by sevoflurane: <strong>co</strong>mparison between children and adults. British<br />
Journal of Anaesthesia 2001; 86(2): 209-12.<br />
Denman WT, Kaplan RF, Goudsouzian NG, Uejima T, Barcelona SL, Cote CJ, Ginsberg B and Hannallah<br />
RS. Intramuscular rapacuronium in infants and children: A <strong>co</strong>mparative multicenter study to <strong>co</strong>nfirm<br />
the efficacy and safety of the age-related tracheal intubating doses of intramuscular rapacuronium<br />
(ORG 9487) in two groups of pediatric subjects. Anesthesiology 2001; 94(1): 3-7.<br />
Drake R, Anderson BJ, Persson MA and Thompson JM. Impact of an antiemetic proto<strong>co</strong>l on postoperative<br />
nausea and vomiting in children. Paediatric Anaesthesia 2001; 11(1): 85-91.<br />
Duncan HP, Zurick NJ and Wolf AR. Should we re<strong>co</strong>nsider awake neonatal intubation? A review of the<br />
evidence and treatment strategies. Paediatric Anaesthesia 2001; 11(2) 135-145.<br />
* Eikermann M, Renzing-Kohler K and Peters J. Probability of acceptable intubation <strong>co</strong>nditions with low dose<br />
rocuronium during light sevoflurane <strong>anaesthesia</strong> in children. Acta Anaesthesiol. Scand. 2001; 45(8):<br />
1036-41.<br />
Engelhardt T, <strong>St</strong>rachan L and Johnston G. Aspiration and regurgitation prophylaxis in paediatric<br />
<strong>anaesthesia</strong>. (Survey) Paediatric Anaesthesia 2001; 11(2): 147-150.<br />
Erb T, Christen P, Kern C and Frei FJ. Similar haemodynamic, respiratory and metabolic changes with the<br />
use of sevoflurane or halothane in children breathing spontaneously via a laryngeal mask airway. Acta<br />
Anaesthesiol. Scand. 2001 45(5): 639-44.<br />
* Ferrari LR. Do children need a preoperative assessment that is different from adults? Int Anesthesiol Clin.<br />
2002; 40(2): 167-86. (review)<br />
* Fujii Y and Tanaka H. Preoperative oral granisetron for the prevention of vomiting following paediatric<br />
surgery. Paediatric Anaesthesia 2002; 12(3): 267-71.<br />
* Gan TJ, Madan R, Alexander R, Jhaveri R, El-Moalem H, Weatherwax K and Glass PS. Duration of action<br />
of vecuronium after an intubating dose of rapacuronium, vecuronium, or succinylcholine. Anesthesia<br />
and Analgesia 2001; 92(5): 1199-202.<br />
* Gasparoni A, Ciardelli L, De Amici D, Castellazzi AM, Autelli M, Bottino R,Polito E, Bartoli A, Rondini G and<br />
Chiri<strong>co</strong> G. Effect of general and epidural <strong>anaesthesia</strong> on thyroid hormones and immunity in neonates.<br />
Paediatric Anaesthesia 2002; 12(1): 59-64.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 37
Golden S. Combination propofol-ketamine <strong>anaesthesia</strong> in sick neonates (case reports).<br />
Anaesthesia 2001; 11(1): 119-122.<br />
Paediatric<br />
* Hall SC. General pediatric emergencies. Malignant hyperthermia syndrome. Anesthesiol Clin North<br />
America 2001; 19(2): 367-82. (review)<br />
* Harrison JM, Girling KJ and Mahajan RP. Effects of propofol and nitrous oxide on middle cerebral artery<br />
flow velocity and cerebral autoregulation. Anaesthesia 2002; 57(1): 27-32.<br />
* Hayes AH, Breslin DS, Mirakhur RK, Reid JE and O'Hare RA. Frequency of haemoglobin desaturation with<br />
the use of succinylcholine during rapid sequence induction of <strong>anaesthesia</strong>. Acta Anaesthesiol Scand.<br />
2001; 45(6): 746-9.<br />
* Kaddu R, Bhattacharya D, Metriyakool K, Thomas R and Tolia V. Propofol <strong>co</strong>mpared with general<br />
anesthesia for pediatric GI endos<strong>co</strong>py: is propofol better? Gastrointest. Endosc. 2002; 55(1): 27-32.<br />
Kardos A, Vereczkey G, Pirot L, Nyirady P and Mekler R. Use of impedance cardiography to monitor<br />
haemodynamic changes during laparos<strong>co</strong>py in children. Paediatric Anaesthesia 2001; 11: 175-9.<br />
* Koinig H. Preparing parents for their child's surgery: preoperative parental information and education.<br />
Paediatric Anaesthesia 2002; 12(2): 107-9.<br />
Kulka P J, Bressem M and Tryba M. Clonidine prevents sevoflurane induced agitation in children.<br />
Anesthesia and Analgesia 2001; 93(2): 335-339.<br />
Le Berre PY, Wodey E, Joly A, Carre P and E<strong>co</strong>ffey C. Comparison of re<strong>co</strong>very after intermediate duration<br />
of <strong>anaesthesia</strong> with sevoflurane and isoflurane. Paediatric Anaesthesia 2001;11(4):443-8.<br />
* Lejus C, Delaroche O, Le Roux C, Legendre E, Rivault O, Floch H, Renaudin M and Pinaud M. Does<br />
sevoflurane inhibit serum cholinesterase in children? Anaesthesia. 2002; 57(1): 44-8.<br />
* Litman RS, Weissend EE, Shrier DA and Ward DS. Morphologic changes in the upper airway of children<br />
during awakening from propofol administration. Anesthesiology. 2002 Mar;96(3):607-11.<br />
*Liu M, Hu X and Liu J. The effect of hypothermia on isoflurane MAC in children. Anesthesiology 2001;<br />
94(3): 429-32.<br />
Lopez-Gil M, Brima<strong>co</strong>mbe J and Keller C. A <strong>co</strong>mparison of four methods for assessing oropharyngeal leak<br />
pressure with the laryngeal mask airway (LMA) in paediatric patients. Paediatric Anaesthesia 2001;<br />
11(3): 319-21.<br />
Marcus RJ and Thompson JP. Anaesthesia for manipulation of forearm fractures in children: A survey of<br />
current practice. Paediatric Anaesthesia 2000; 10: 273-6.<br />
Martyn JAJ, Goudsouzian NG, Chang Y, Szyfelbein SK, Schwartz AE and Patel SS. Neuromuscular effects<br />
of mivacurium in 2- to 12-yr -old children with burn injury. Anesthesiology 2000; 92: 31-7.<br />
* Meier S, Geiduschek J, Paganoni R, Fuehrmeyer F and Reber A. The effect of chin lift, jaw thrust, and<br />
<strong>co</strong>ntinuous positive airway pressure on the size of the glottic opening and on stridor s<strong>co</strong>re in<br />
anesthetized, spontaneously breathing children. Anesthesia and Analgesia 2002; 94(3): 494-9.<br />
Nesher N, Wolf T, Uretzky G, A Oppenheim-Eden, E Yussim, I Kushnir, G Shoshany, B Rosenburg and<br />
Berant M. A novel thermoregulatory system maintains perioperative normothermia in children<br />
undergoing elective surgery. Paediatric Anaesthesia 2001; 11(5): 555-560.<br />
* Nosovitch MA, Johnson JO, Tobias JD. Noninvasive intraoperative monitoring of carbon dioxide in children:<br />
endtidal versus transcutaneous techniques. Paediatric Anaesthesia 2002; 12(1): 48-52.<br />
* Odegard KC, Modest SA and Laussen PC. A survey of parental satisfaction during parent present<br />
induction of <strong>anaesthesia</strong> for children undergoing cardiovascular surgery. Paediatric Anaesth. 2002;<br />
12(3): 261-6.<br />
Okuda K, Inagawa G, Miwa T and Hiroki K. Influence of head and neck position on cuff position and<br />
oropharyngeal sealing pressure with the laryngeal mask airway in children. British Journal of<br />
Anaesthesia 2001; 86(1): 122-124.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 38
Ozlu O, Turker AK, Ozgun G and Soykan I. Distal oesophageal pH measurement in children during general<br />
<strong>anaesthesia</strong> using the laryngeal mask airway, tracheal tube and face mask. Paediatric Anaesthesia<br />
2001: 11(4): 425-9.<br />
Parnis SJ, Barker DS and Van Der Walt JH. Clinical predictors of anaesthetic <strong>co</strong>mplications in children with<br />
respiratory tract infections. Paediatric Anaesthesia 2001; 11(1): 29-40.<br />
Reber A, Paganoni R and Frei FJ. Effect of <strong>co</strong>mmon airway manoeuvres on upper airway dimensions and<br />
clinical signs in anaesthetized, spontaneously breathing children. British Journal of Anaesthesia 2001;<br />
86(2): 217-222.<br />
Reynolds LM, Infosino A, Brown R, Hsu J and Fisher DM. Pharma<strong>co</strong>kinetics of rapacuronium in infants and<br />
children with intravenous and intramuscular administration. Anesthesiology 2000; 92: 376-86.<br />
Scalfaro P, Sly PD, Sims C and Habre W. Salbutamol prevents the increase in respiratory resistance caused<br />
by tracheal intubation during sevoflurane anesthesia in asthmatic children. Anesthesia and Analgesia<br />
2001; 93: 898-902.<br />
* Simon L, Boucebci KJ, Orliaguet G, Aubineau JV, Devys JM and Dubousset AM. A survey of practice of<br />
tracheal intubation without muscle relaxant in paediatric patients. Paed. Anaesth. 2002; 12(1): 36-42.<br />
Soh CR. Laryngeal mask airway insertion in paediatric <strong>anaesthesia</strong>: <strong>co</strong>mparison between the reverse and<br />
standard techniques. Anaesthesia and Intensive Care 2001; 29(5): 519-519.<br />
Splinter W and Isaac LA. The pharma<strong>co</strong>e<strong>co</strong>nomics of Neuromuscular blocking drugs: A perioperative <strong>co</strong>st<br />
minimization strategy in children. Anesthesia and Analgesia 2001; 93(2): 339-344.<br />
* <strong>St</strong>ruys MM, Jensen EW, Smith W, Smith NT, Rampil I, Dumortier FJ, Mestach C and Mortier EP.<br />
Performance of the ARX-derived auditory evoked potential index as an indicator of anesthetic depth: a<br />
<strong>co</strong>mparison with bispectral index and hemodynamic measures during propofol administration.<br />
Anesthesiology 2002; 96(4): 803-16.<br />
Suga A, Tanaka M and Toyooka H. Effects of i.v. metoclopramide, atropine and their <strong>co</strong>mbination on gastric<br />
insufflation in children anaesthetized with sevoflurane and nitrous oxide. Paediatric Anaesthesia 2001;<br />
11(2): 151-156.<br />
Tait A, Malviya S, Voepel-Lewis T, Munro H, Siewert M and Pandit UA. Risk Factors for perioperative<br />
adverse respiratory events in children with upper respiratory tract infections. Anesthesiol. 2001; 95(2):<br />
299-306.<br />
Vakkuri A, Yli-Hankala A, Sarkela M, Lindgren L, Mennander S, Korttila K, Saarnivaara L and Jantti V.<br />
Sevoflurane mask induction of <strong>anaesthesia</strong> is associated with epileptiform EEG in children. Acta<br />
Anaesthesiologica Scandinavica 2001; 45(7): 805-11.<br />
Walpole R, Olday J, Haetzman M, Drummond GB and Doyle E. A <strong>co</strong>mparison of the respiratory effects of<br />
high <strong>co</strong>ncentrations of halothane and sevoflurane. Paediatric Anaesthesia 2001; 11(2): 157-60.<br />
* Watcha MF. Investigations of the bispectral index monitor in pediatric anesthesia: first things first.<br />
Anesthesia and Analgesia 2001; 92(4): 805-7.<br />
Wedgewood J and Doyle E. Anaesthesia and laparos<strong>co</strong>pic surgery in children. Paediatric Anaesthesia<br />
2001; 11(4): 391-9. (review)<br />
Woloszcz<strong>uk</strong>-Gebicka B, Lapczynski T and Wierzejski W. The influence of halothane, isoflurane and<br />
sevoflurane on rocuronium infusion in children. Acta Anaesthesiologica Scandinavica 2001; 45(1): 73-<br />
7.<br />
* Yaguchi Y, Inomata S, Kihara S, Baba Y, Kohda Y and Toyooka H. The reduction in minimum alveolar<br />
<strong>co</strong>ncentration for tracheal extubation after clonidine premedication in children. Anesthesia and<br />
Analgesia 2002; 94(4): 863-6.<br />
ENT and eyes<br />
Bowhay AR, May HA, Rudnicka AR and Booker PD. A randomized <strong>co</strong>ntrolled trial of the antiemetic effect of<br />
three doses of ondansetron after strabismus surgery in children. Paed. Anaesth. 2001; 11(2): 215-21.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 39
Duman A, Ogun CO and Okesli S. The effect on intraocular pressure of tracheal intubation or laryngeal<br />
mask insertion during sevoflurane <strong>anaesthesia</strong> in children without the use of muscle relaxants.<br />
Paediatric Anaesthesia 2001; 11(4): 421-4.<br />
Hallen J, Rawal N and Gupta A. Postoperative re<strong>co</strong>very following outpatient pediatric myringotomy: a<br />
<strong>co</strong>mparison between sevoflurane and halothane. Journal of Clinical Anesthesiology 2001; 13(3): 161-<br />
6.<br />
Handa F and Fujii Y. The efficacy of oral clonidine premedication in the prevention of postoperative vomiting<br />
in children following strabismus surgery. Paediatric Anaesthesia 2001 11(1): 71-4.<br />
Jones SE, Dickson U and Moriarty A. Anaesthesia for insertion of bone-anchored hearing aids in children: a<br />
7-year audit. Anaesthesia 2001 56(8): 777-80.<br />
Khan FA and Memon GA. Comparison of spontaneous with <strong>co</strong>ntrolled mode of ventilation in tonsillectomy.<br />
Paediatric Anaesthesia 2001; 11(2): 185-190.<br />
* Rusy LM, Hoffman GM and Weisman SJ. Electroacupuncture prophylaxis of postoperative nausea and<br />
vomiting following pediatric tonsillectomy with or without adenoidectomy. Anesthesiol 2002; 96(2): 300-<br />
5.<br />
Salonen A, Kokki H and Tuovinen K. IV ketoprofen for analgesia after tonsillectomy: <strong>co</strong>mparison of pre and<br />
post-operative administration. British Journal of Anaesthesia 2001; 86(3): 377-81.<br />
Shende D, Bharti N, Kathirvel S and Madan R. Combination of droperidol and ondansetron reduces PONV<br />
after pediatric strabismus surgery more than single drug therapy. Acta Anaesthesiologica Scandinavica<br />
2001; 45(6): 756-60.<br />
Splinter WM. Prevention of vomiting after strabismus surgery in children: dexamethasone alone versus<br />
dexamethsaone plus low-dose ondansetron. Paediatric Anaesthesia 2001; 11(5): 591- 596.<br />
* Suresh S, Barcelona SL, Young NM, Seligman I, Heffner CL and Cote CJ. Postoperative pain relief in<br />
children undergoing tympanomastoid surgery: is a regional block better than opioids? Anesthesia and<br />
Analgesia 2002; 94(4): 859-62.<br />
* Verghese ST and Hannallah RS. Pediatric otolaryngologic emergencies. Anesthesiol Clin North America.<br />
2001; 19(2): 237-56, vi. (review)<br />
Viitanen H and Annila P. Analgesic efficacy of tramadol 2 mg kg(-1) for paediatric day-case adenoidectomy.<br />
British Journal of Anaesthesia 2001; 86(4): 572-5.<br />
Dental surgery<br />
* Andrzejowski J and Lamb L. The effect of swabs soaked in bupivacaine and epinephrine for pain relief<br />
following simple dental extractions in children. Anaesthesia. 2002; 57(3): 281-3.<br />
Arch LM, Humphris GM, Lee GT. Children choosing between general <strong>anaesthesia</strong> or inhalation sedation for<br />
dental extractions: the effect on dental anxiety. International J Paediatric Dent. 2001; 11(1): 41-8.<br />
* Horgesheimer JJ, Pribble CG and Lugo RA. The effect of midazolam premedication on discharge time in<br />
pediatric patients undergoing general anesthesia for dental restorations. Pediatric Dent. 2001; 23(6):<br />
491-4.<br />
Lahoud GY, Averley PA and Hanlon MR. Sevoflurane inhalation <strong>co</strong>nscious sedation for children having<br />
dental treatment. Anaesthesia 2001; 56(5): 476-80.<br />
Somri M, Vaida SJ, Sabo E, Yassain G, Gankin I and Gaitini LA. Acupuncture versus ondanserton in the<br />
prevention of postoperative vomiting. A study of children undergoing dental surgery. Anaesthesia<br />
2001; 56(10): 927-932.<br />
* Sullivan DC, Wilson CF and Webb MD. A <strong>co</strong>mparison of two oral ketamine-diazepam regimens for the<br />
sedation of anxious pediatric dental patients. Pediatric Dent. 2001; 23(3): 223-31.<br />
Regional <strong>anaesthesia</strong>, pain and analgesia<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 40
Arana A, Morton NS and Hansen TG. Treatment with paracetamol in infants.<br />
Scandinavica 2001; 45(1): 20-9. (review)<br />
Acta Anaesthesiologica<br />
* Ben-Abraham R, Weinbroum AA, Lotan D, Dagan O, Schreriber-Scheffer R, Mishali D, Harel R, Vishne T,<br />
Barzilay Z and Paret G. Interle<strong>uk</strong>in-8 secretion following cardiopulmonary bypass in children as a<br />
marker of early postoperative morbidity. Paediatric Anaesthesia 2002; 12(2): 156-61.<br />
* Bosenberg A, Thomas J, Lopez T, Lybeck A, Huizar K and Larsson LE. The efficacy of caudal ropivacaine<br />
1, 2 and 3 mg x l(-1) for postoperative analgesia in children. Paediatric Anaesthesia 2002; 12(1): 53-8.<br />
Bouwmeester NJ, Anand KJS, van Dijk M, Hop WC, Boomsma F and Tibboel D. Hormonal and metabolic<br />
stress responses after major surgery in children aged 0-3 years: A double blind, randomized trial<br />
<strong>co</strong>mparing the effects of <strong>co</strong>ntinuous versus intermittent morphine. International Journal of Anaesthesia<br />
2001; 87(3): 390-399<br />
Breschan C, Krumpholz R, Jost R and Likar R. Intraspinal haematoma following lumbar epidural <strong>anaesthesia</strong><br />
in a neonate. Paediatric Anaesthesia 2001; 11(1): 105-8.<br />
* Cucchiaro G, De Lagausie P, El-Ghonemi A and Nivoche Y. Single-dose caudal anesthesia for major<br />
intraabdominal operations in high-risk infants. Anesthesia and Analgesia 2001; 92(6): 1439-41.<br />
Dalens B, E<strong>co</strong>ffey C, Joly A, Giaufre E, Gustafsson U, Huledal G and Larsson LE. Pharma<strong>co</strong>kinetics and<br />
analgesic effect of ropivacaine following ilioinguinal/iliohypogastric nerve block in children. Paediatric<br />
Anaesthesia 2001; 11(4): 415-20.<br />
* Davidson AJ, Eyres RL and Cole WG. A <strong>co</strong>mparison of prilocaine and lidocaine for intravenous regional<br />
<strong>anaesthesia</strong> for forearm fracture reduction in children. Paediatric Anaesthesia 2002; 12(2): 146-50.<br />
* De Negri P, Ivani G, Vis<strong>co</strong>nti C, De Vivo P and Lonnqvist PA. The dose-response relationship for clonidine<br />
added to a postoperative <strong>co</strong>ntinuous epidural infusion of ropivacaine in children. Anesthesia and<br />
Analgesia 2001; 93(1): 71-6.<br />
* Dsida RM, Wheeler M, Birmingham PK, Wang Z, Heffner CL, Cote CJ and Avram MJ. Age-stratified<br />
pharma<strong>co</strong>kinetics of ketorolac tromethamine in pediatric surgical patients. Anesthesia and Analgesia<br />
2002; 94(2): 266-70.<br />
Engelhardt T and Crawford M. Sublingual morphine may be a suitable alternative for pain <strong>co</strong>ntrol in children<br />
in the postoperative period. Paediatric Anaesthesia 2001; 11(1): 81-3.<br />
* Fanelli G, Casati A, Magistris L, Berti M, Albertin A, Scarioni M and Torri G. Fentanyl does not improve the<br />
nerve block characteristics of axillary brachial plexus <strong>anaesthesia</strong> performed with ropivacaine. Acta<br />
Anaesthesiol Scand. 2001; 45(5): 590-4.<br />
Grunau RE, Oberlander TF, Whitfield MF, Fitzgerald C and Lee SK. Demographic and therapeutic<br />
determinants of pain reactivity in very low birth weight neonates at 32 weeks' post<strong>co</strong>nceptional age.<br />
Pediatrics 2001; 107(1): 105-112.<br />
* Hager H, Marhofer P, Sitzwohl C, Adler L, Kettner S and Semsroth M. Caudal clonidine prolongs analgesia<br />
from caudal S(+)-ketamine in children. Anesthesia and Analgesia 2002; 94(5): 1169-72<br />
Hansen TG, Morton NS, Cullen PM and Watson DG. Plasma <strong>co</strong>ncentrations and pharma<strong>co</strong>kinetics of<br />
bupivacaine with and without adrenaline following caudal <strong>anaesthesia</strong> in infants. Acta<br />
Anaesthesiologica Scandinavica 2001; 45(1): 42-7.<br />
Hansen TG, Ilett KF, Reid C, Lim SI, Hackett LP and Bergesio R. Caudal ropivacaine in infants: population<br />
pharma<strong>co</strong>kinetics and plasma <strong>co</strong>ncentrations. Anesthesiology 2001; 94(4): 579-84.<br />
Hashizume Y, Yamaguchi S, Mishio M, Takiguchi T, Okuda Y and Kitajima T. Pediatric caudal block with<br />
mepivacaine, bupivacaine or a mixture of both drugs: Requirement for postoperative analgesia and<br />
plasma <strong>co</strong>ncentration of local anesthetics. Journal of Clinical Anesthesia 2001; 13(1): 30-34.<br />
* Huettemann E, Terborg C, Sakka SG, Petrat G, Schier F and Reinhart K. Preserved CO(2) reactivity and<br />
increase in middle cerebral arterial blood flow velocity during laparos<strong>co</strong>pic surgery in children.<br />
Anesthesia and Analgesia 2002; 94(2): 255-8.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 41
* Inomata S, Tanaka E, Miyabe M, Kakiuchi Y, Nagashima A, Yamasaki Y, Nakayama S, Baba Y, Toyooka H,<br />
Okuyama K and Kohda Y. Plasma lidocaine <strong>co</strong>ncentrations during <strong>co</strong>ntinuous thoracic epidural<br />
anesthesia after clonidine premedication in children. Anesthesia and Analgesia 2001; 93(5): 1147-51.<br />
* Ivani G, DeNegri P, Conio A, Grossetti R, Vitale P, Vercellino C, Gagliardi F, Eksborg S and Lonnqvist PA.<br />
Comparison of racemic bupivacaine, ropivacaine, and levo-bupivacaine for pediatric caudal anesthesia:<br />
effects on postoperative analgesia and motor block. Regional Anesthesia and Pain Medicine 2002;<br />
27(2): 157-61.<br />
* Karmakar MK, Aun CS, Wong EL, Wong AS, Chan SK and Yeung CK. Ropivacaine undergoes slower<br />
systemic absorption from the caudal epidural space in children than bupivacaine. Anesthesia and<br />
Analgesia 2002; 94(2): 259-65.<br />
Kiffer A, Joly E, Wodey P, Carre C and E<strong>co</strong>ffey. The effect of preoperative epidural morphine on<br />
postoperative analgesia in children. Anesthesia and Analgesia 2001; 93(3): 598-600.<br />
* Kokki H, Karvinen M and Jekunen A. Pharma<strong>co</strong>kinetics of a 24-hour intravenous ketoprofen infusion in<br />
children. Acta Anaesthesiol Scand. 2002; 46(2): 194-8.<br />
* Kokki H and Salonen A. Comparison of pre and postoperative administration of ketoprofen for analgesia<br />
after tonsillectomy in children. Paediatric Anaesthesia 2002; 12(2): 162-7.<br />
* Larousse E, Asehnoune K, Dartayet B, Albaladejo P, Dubousset AM, Gauthier F and Benhamou D. The<br />
hemodynamic effects of pediatric caudal anesthesia assessed by esophageal Doppler. Anesthesia and<br />
Analgesia 2002; 94(5): 1165-8.<br />
* Lim SL, Ng Sb A and Tan GM. Ilioinguinal and iliohypogastric nerve block revisited: single shot versus<br />
double shot technique for hernia repair in children. Paediatric Anaesthesia 2002; 12(3): 255-60.<br />
Lovstad RZ and <strong>St</strong>oen R. Postoperative epidural analgesia in children after major orthopaedic surgery. A<br />
randomised study of the effect on PONV of two anaesthetic techniques: low and high dose i.v. fentanyl<br />
and epidural infusions with and without fentanyl. Acta Anaesthesiologica Scand. 2001; 45(4): 482-488.<br />
Mahajan R, Batra YK, Grover VK and Kajal J. A <strong>co</strong>mparative study of caudal bupivacaine and midazolambupivacaine<br />
mixture for post-operative analgesia in children undergoing genitourinary surgery.<br />
International Journal of Clinical Pharma<strong>co</strong>logy & Therapeutics 2001; 39(3): 116-120.<br />
* Matsota P, Livanios S and Marinopoulou E. Inter<strong>co</strong>stal nerve block with Bupivacaine for post-thora<strong>co</strong>tomy<br />
pain relief in children. European Journal of Pediatric Surgery 2001; 11(4): 219-22.<br />
McCann ME, Sethna NF, Mazoit J-X, Sakamoto M, Rifai N, Hope T, Sullivan L, Auble SG, Berde CB. The<br />
pharma<strong>co</strong>kinetics of epidural ropivacaine in infants and young children. Anesthesia and Analgesia<br />
2001; 93: 893-7.<br />
* Maurice SC, O'Donnell JJ and Beattie TF. Emergency analgesia in the paediatric population. Part II<br />
Pharma<strong>co</strong>logical methods of pain relief. Emergency Med Journal 2002; 19(2): 101-5. (review)<br />
* Meunier JF, Goujard E, Dubousset AM, Samii K and Mazoit JX. Pharma<strong>co</strong>kinetics of bupivacaine after<br />
<strong>co</strong>ntinuous epidural infusion in infants with and without biliary atresia. Anesthesiol. 2001; 95(1): 87-95.<br />
Ozcengiz D, Gunduz M, Ozbek H and Isik G. Comparison of caudal morphine and tramadol for<br />
postoperative pain <strong>co</strong>ntrol in children undergoing inguinal herniorrhaphy. Paediatric Anaesthesia 2001;<br />
11(4): 459-64.<br />
Paut C, Calmejane J, Delorme F, Lacroix J and Camboulives M. EMLA vs nitrous oxide for venous<br />
cannulation in children. Anesthesia and Analgesia 2001; 93(3): 590-593.<br />
* Roux CL, Lejus C, Surbleb M, Renaudin M, Guillaud C, Windt A, Lasnier B and Pinaud M. Is haemostasis<br />
biological screening always useful before performing a neuraxial blockade in children? Paediatric<br />
Anaesthesia 2002; 12(2): 118-23.<br />
Sage FG, Lloyd-Thomas AR and Howard RF. Paediatric lumbar epidurals: a <strong>co</strong>mparison of 21-G and 23-G<br />
catheters in patients weighing less than 10 kg. Paediatric Anaesthesia 2000; 10: 279-82.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 42
* Sciard D, Matuszczak M, Gebhard R, Greger J, Al-Samsam T and Chelly JE. Continuous posterior lumbar<br />
plexus block for acute postoperative pain <strong>co</strong>ntrol in young children. Anesthesiology 2001; 95(6): 1521-<br />
3.<br />
* Senel AC, Akyol A, Dohman D and Solak M. Caudal bupivacaine-tramadol <strong>co</strong>mbination for postoperative<br />
analgesia in pediatric herniorrhaphy. Acta Anaesthesiol Scand. 2001; 45(6): 786-9.<br />
* Simon MJ, Veering BT, <strong>St</strong>ienstra R, van Kleef JW and Burm AG. The effects of age on neural blockade<br />
and hemodynamic changes after epidural anesthesia with ropivacaine. Anesthesia and Analgesia<br />
2002; 94(5): 1325-30.<br />
Suraseranivongse S, Santawat U, Kraiprasit K, Petcharatana S, Prakkamodom S and Muntraporn N. Crossvalidation<br />
of a <strong>co</strong>mposite pain scale for preschool children within 24 hours of surgery. International<br />
Journal of Anaesthesia 2001; 87(3): 400-405.<br />
Suresh S and Annand KJS. Opioid tolerance in neonates: a state of the art review. Paediatric Anaesthesia<br />
2001; 11(5) 511-522.<br />
Taddio A. Pain management for neonatal circumcision. Paediatric Drugs 2001; 3(2):101-11. (review)<br />
Tobias JD. Brachial plexus <strong>anaesthesia</strong> in children. Paediatric Anaesthesia 2001; 11(3): 265-75.<br />
* Tobias JD. Therapeutic applications of regional <strong>anaesthesia</strong> in paediatric-aged patients. Paediatric<br />
Anaesthesia 2002; 12(3): 272-7. (review)<br />
* Uejima T and Suresh S. Is 0.375% bupivacaine safe in caudal anesthesia in neonates and young infants?<br />
Anesthesia and Analgesia 2002; 94(4): 1041.<br />
* Uguralp S, Mutus M, Koroglu A, Gurbuz N, Kolt<strong>uk</strong>suz U and Demircan M. Regional anesthesia is a good<br />
alternative to general anesthesia in pediatric surgery: Experience in 1,554 children. Journal of<br />
Pediatric Surgery 2002; 37(4): 610-3.<br />
* Verghese ST, Mostello LA, Patel RI, Kaplan RF and Patel KM. Testing anal sphincter tone predicts the<br />
effectiveness of caudal analgesia in children. Anesthesia and Analgesia 2002; 94(5): 1161-4.<br />
William JM, <strong>St</strong>oddart PA, Williams SA and Wolf AR. Post-operative re<strong>co</strong>very after inguinal herniotomy in expremature<br />
infants:<strong>co</strong>mparison between sevoflurane and spinal <strong>anaesthesia</strong>. British Journal of<br />
Anaesthesia 2001; 86(3): 366-71.<br />
Williams DG, Hatch DJ and Howard RF. Codeine phosphate in paediatric medicine.<br />
Anaesthesia 2001; 86(3): 413-21. (review)<br />
British Journal of<br />
Wolf AR, <strong>St</strong>oddart PA, Murphy PJ and Sasada M. Rapid skin <strong>anaesthesia</strong> using high velocity lignocaine<br />
particles: a prospective placebo <strong>co</strong>ntrolled trial. Archives of Diseases in Childhood 2002; 86(4): 309-<br />
12.<br />
Day-Care<br />
* El<strong>co</strong>ck DH and Sweeney BP. Sevoflurane vs. isoflurane: a clinical <strong>co</strong>mparison in day surgery.<br />
Anaesthesia. 2002; 57(1): 52-6.<br />
Gloor A, Dillier C and Gerber A. Ketamine for short ambulatory procedures in children: an audit. Paediatric<br />
Anaesthesia 2001; 11(5): 533-540.<br />
* McHugh GA and Thoms GM. The management of pain following day-case surgery. Anaesthesia 2002;<br />
57(3): 270-5.<br />
Oddby E, Englund S and Lonnqvist PA. Postoperative nausea and vomiting in paediatric ambulatory<br />
surgery: sevoflurane versus spinal <strong>anaesthesia</strong> with propofol sedation. Paediatric Anaesth. 2001;<br />
11(3): 337-42.<br />
Sedation<br />
Cote CJ. Why we need sedation guidelines [2]. Journal of Pediatrics 2001; 138(3): 447-448.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 43
* Cote CJ. "Conscious sedation": time for this oxymoron to go away! Journal of Pediatrics 2001; 139(1): 15-<br />
7; discussion 18-9.<br />
Green SM, Klooster M, Harris T, Lynch EL and Rothrock SG. Ketamine sedation for pediatric<br />
gastroenterology procedures. Journal of Pediatric Gastroenterology & Nutrition 2001; 32(1): 26-33.<br />
Hain RDW and Campbell C. Invasive procedures carried out in <strong>co</strong>nscious children: <strong>co</strong>ntrast between North<br />
American and European paediatric on<strong>co</strong>logy centres. Archives Diseases in Childhood 2001; 85: 12-15.<br />
* Hoffman GM, Nowakowski R, Troshynski TJ, Berens RJ and Weisman SJ. Risk reduction in pediatric<br />
procedural sedation by application of an American Academy of Pediatrics/American Society of<br />
Anesthesiologists process model. Pediatrics 2002; 109(2): 236-43.<br />
Kanagasundaram SA, Lane LJ, Cavalletto BP, Keneally JP and Cooper MG. Efficacy and safety of nitrous<br />
oxide in alleviating pain and anxiety during painful procedures. Archives Diseases Child. 2001; 84(6):<br />
492-5.<br />
Kennedy RM and Luhmann JD. Pharma<strong>co</strong>logical management of pain and anxiety during emergency<br />
procedures in children. Paediatric Drugs 2001; 3(5): 337-54. (review)<br />
* Ljungman G, Gordh T, Sorensen S and Kreuger A. Lumbar puncture in pediatric on<strong>co</strong>logy: <strong>co</strong>nscious<br />
sedation vs general anesthesia. Med Pediatr On<strong>co</strong>l. 2001; 36(3): 372-9.<br />
* Tobias JD and Berkenbosch JW. Tolerance during sedation in a pediatric ICU patient: effects on the BIS<br />
monitor. Journal of Clinical Anesthesia 2001; 13(2): 122-4.<br />
van der Walt JH, Sainsbury DA and Pettifer R. Anaesthesia alert: an integrated, networked, register of<br />
paediatric anaesthetic problems. Anaesthesia and Intensive Care 2001; 29(2): 113-6.<br />
Weiss M, Schwarz U, Dillier CM and Gerber AC. Teaching and supervising tracheal intubation in paediatric<br />
patients using videolaryngos<strong>co</strong>py. Paediatric Anaesthesia 2001; 11(3): 343-8.<br />
* Yagiela JA, Cote CJ, Notterman DA, Karl HW, Weinberg JA and McCloskey C. Adverse sedation events in<br />
pediatrics. Pediatrics 2001; 107(6): 1494.<br />
Miscellaneous<br />
Bingham R. Evidence based paediatric resuscitation. Paediatric Anaesthesia 2001; 11(1): 1-2.<br />
Carapiet D, Fraser J, Wade A, Buss PW and Bingham R. Changes in paediatric resuscitation knowledge<br />
among doctors. Archives of Diseases in Childhood 2001; 84(5): 412-4.<br />
Cox RG, Ewen A and Bart BB. The prone position is associated with a decrease in respiratory system<br />
<strong>co</strong>mpliance in healthy anaesthetized infants. Paediatric Anaesthesia 2001; 11(3): 291-6.<br />
da Costa VV, Saraiva RA, de Almeida AC, Rodrigues MR, Nunes LG and Ferreira JC. The effect of nitrous<br />
oxide on the inhibition of somatosensory evoked potentials by sevoflurane in children. Anaesthesia<br />
2001; 56(3): 202-7.<br />
* Denham EJ and Nelson RM. Self-determination is not an appropriate model for understanding parental<br />
permission and child assent. Anesthesia and Analgesia 2002; 94(5): 1049-51.<br />
Erb TO, Schulman SR and Sugarman J. Permission and assent for clinical research in pediatric anesthesia.<br />
Anesthesia and Analgesia 2002; 94(5): 1155-60.<br />
Edgar J, Morton NS and Pace NA. Review of ethics in paediatric <strong>anaesthesia</strong>: intensive care issues.<br />
Paediatric Anaesthesia 2001; 11(5): 597-602.<br />
Edgar J, Morton NS and Pace NA. Review of ethics in paediatric <strong>anaesthesia</strong>: research issues. Paediatric<br />
Anaesthesia 2001; 11(4): 473-7. (review)<br />
Edgar J, Morton NS and Pace NA. Review of ethics in paediatric <strong>anaesthesia</strong>: <strong>co</strong>nsent issues. Paediatric<br />
Anaesthesia 2001; 11(3): 355-9. (review)<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 44
* Fisher QA, Nichols D, <strong>St</strong>ewart FC, Finley GA, Magee WP Jr and Nelson K. Assessing pediatric anesthesia<br />
practices for volunteer medical services abroad. Anesthesiol. 2001; 95(6): 1315-22. (see Editorial 1311-<br />
2)<br />
Hammer GB, N Funck N, Rosenthal DN and Feinstein JA. A technique for maintenance of airway access in<br />
infants with a difficult airway following tracheal extubation. Paediatric Anaesthesia 2001; 11(5): 622-<br />
625<br />
Hammer GB, Litalieu C, Wellis V and Drover DR. Determination of the median effective <strong>co</strong>ncentration (EC 50 )<br />
of propofol during oesophagogastroduodenos<strong>co</strong>py in children. Paed. Anaesth 2001; 11(5): 549-554.<br />
Heard CM, Gunnarsson B, Heard AM, Watson E, Orie JD and Fletcher JE. Anaesthetic technique for<br />
transoesophageal echocardiography in children. Paediatric Anaesthesia 2001; 11(2): 181-4.<br />
* James I. Cuffed tubes in children. Paediatric Anaesthesia 2001; 11(3): 259-63.<br />
* Kathirvel S, Dash HH, Bhatia A, Subramaniam B, Prakash A and Shenoy S. Effect of prophylactic<br />
ondansetron on postoperative nausea and vomiting after elective craniotomy. Journal of Neurosurgery<br />
and Anesthesiology 2001; 13(3): 207-12.<br />
* Krauss B. Management of acute pain and anxiety in children undergoing procedures in the emergency<br />
department. Pediatric Emergency Care 2001; 17(2): 115-22; quiz 123-5. (review)<br />
* Lee C and Mason LJ. Pediatric cardiac emergencies. Anesthesiol Clin North America 2001; 19(2): 287-<br />
308. (review)<br />
* Liu LM and Pang LM. Neonatal surgical emergencies. Anesthesiol Clin North America 2001; 19(2): 265-<br />
86. (review)<br />
Rosenstock C, Moller J and Hauberg A. Complaints related to respiratory events in <strong>anaesthesia</strong> and<br />
intensive care medicine from 1994 to 1998. Denmark.Acta Anaesthesiologica Scandinavica 2001;<br />
45(1): 53-8.<br />
Morgan-Hughes NJ and Kirton CB. EMLA--is one hour long enough? Anaesthesia 2001; 56(5): 495-6.<br />
Podder S, Dutta A, Yaddanapudi S and Chari P. Challenges in paediatric mask holding; the 'claw hand'<br />
technique. Anaesthesia 2001; 56(7): 697-9.<br />
* Ross AK. Pediatric trauma. Anesthesia management. Anesthesiol Clin North America 2001; 19(2): 309-<br />
37. (review)<br />
Saghaei M and Razavi S. Bloodletting acupuncture for the prevention of stridor in children after tracheal<br />
extubation: a randomised, <strong>co</strong>ntrolled study. Anaesthesia 2001; 56(10): 961-964.<br />
Schily M, Koumo<strong>uk</strong>elis H, Lerman J and Creighton RE. Can pediatric anesthesiologists detect an occluded<br />
tracheal tube in neonates? Anesthesia and Analgesia 2001; 93(1): 66-70.<br />
Sobolev I, Plunkett N and Barker I. Acute epiglottitis, sevoflurane and HIB vaccination. Anaesthesia 2001;<br />
56(8): 807-8.<br />
Thomas PB and Parry MG. The difficult paediatric airway: a new method of intubation using the laryngeal<br />
mask airway TM , Cook airway exchange catheter and tracheal intubation fibres<strong>co</strong>pe. Paediatric<br />
Anaesthesia 2001; 11(5): 618-621.<br />
* Tobias JD. Caudal epidural block: a review of test dosing and re<strong>co</strong>gnition of systemic injection in children.<br />
Anesthesia and Analgesia 2001; 93(5): 1156-61. (review)<br />
* Tobias JD and Burd RS. Anaesthetic management and high frequency oscillatory ventilation. Paediatric<br />
Anaesthesia 2001; 11(4): 483-7.<br />
Tong JL and Thomas ML. World Wide Web resources and the paediatric anaesthetist: Surf's up. Paediatric<br />
Anaesthesia 2001; 11(1): 19-27.<br />
Watson A and Visram A. Survey of the use of oesophageal and pre<strong>co</strong>rdial stethos<strong>co</strong>pes in current paediatric<br />
anaesthetic practice. Paediatric Anaesthesia 2001; 11(4): 437-42.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 45
Weiss M, Hartman K, Fischer KE and Gerber A. Use of angulated video-intubation laryngos<strong>co</strong>pe in children<br />
undergoing manual in-line neck stabilization. International Journal of Anaesthesia 2001; 87(3): 453-<br />
458.<br />
Wodey E, Gai V, Carre F and E<strong>co</strong>ffey C. Accuracy and limitations of <strong>co</strong>ntinuous oesophageal aortic blood<br />
flow measurement during general <strong>anaesthesia</strong> for children: <strong>co</strong>mparison with transcutaneous<br />
echography-Doppler. Paediatric Anaesthesia 2001; 11(3): 309-17.<br />
Zatman TF, Hall JE and Harmer M. Gastric residual volume in children: a study <strong>co</strong>mparing efficiency of<br />
erythromycin and metoclopramide as prokinetic agents. British Journal Anaesth. 2001; 86(6): 869-71.<br />
Organisation<br />
* Davies LK. Con: Anesthetics should be administered to pediatric patients undergoing cardiac surgical<br />
procedures not only by pediatric anesthesiologists. Journal of Cardiothoracic and Vascular Anesthesia<br />
2001; 15(3): 384-7.<br />
* Kahana M. Pro: Only pediatric anesthesiologists should administer anesthetics to pediatric patients<br />
undergoing cardiac surgical procedures. J Cardiothoracic and Vascular Anesthesia 2001; 15(3): 381-3.<br />
Kinouchi K and Kitamura S. Improved viability of the low birth weight infant and the increasing needs for<br />
<strong>anaesthesia</strong>. Paediatric Anaesthesia 2001; 11(2): 131-3.<br />
Lauder GR. Delegation in paediatric <strong>anaesthesia</strong>: a postal survey. Paediatric Anaesth. 2001; 11(3): 349-54.<br />
Specialist<br />
* Baum VC. Cardiac trauma in children. Paediatric Anaesthesia 2002; 12(2): 110-7. (review)<br />
Bengtsson J, Edberg KE, Nilsson B and Bengtson JP. Monitoring of pacemaker induced changes in cardiac<br />
output with inspired to endtidal oxygen difference in paediatric cardiac surgery patients. Paediatric<br />
Anaesthesia 2001; 11(2): 191-7.<br />
Cray SH, Holtby HM, Kartha VM, Cox PN and Roy WL. Early tracheal extubation after paediatric cardiac<br />
surgery: the use of propofol to supplement low-dose opioid <strong>anaesthesia</strong>. Paediatric Anaesthesia 2001;<br />
11(4): 465-71.<br />
Dahmani S, Orliaguet GA, Meyer PG, Blanot S, Renier D and Carli PA. Perioperative blood salvage during<br />
surgical <strong>co</strong>rrection of craniosynostosis in infants. British Journal of Anaesthesia 2000; 85: 550-55.<br />
Davis L and Ross N. Bilateral vocal <strong>co</strong>rd palsy after ventricular drainage in a child.<br />
Analgesia 2001; 92(2): 358-61.<br />
Anesthesia and<br />
* De Gabriele LC, Cooper MG, Singh S and Pitkin J. Intraoperative fibreoptic bronchos<strong>co</strong>py during neonatal<br />
ttracheo-oesophageal fistula ligation and oesophageal atresia repair. Anaesthesia and Intensive Care<br />
2001; 29(3): 284-7.<br />
Farley-Hills E, Byrne AJ, Brennan L and Sartori P. Tumour lysis syndrome during <strong>anaesthesia</strong>. Paediatric<br />
Anaesthesia 2001; 11(2): 233-6.<br />
* Hain RD and Campbell C. Invasive procedures carried out in <strong>co</strong>nscious children: <strong>co</strong>ntrast between North<br />
American and European paediatric on<strong>co</strong>logy centres. Archives Diseases in Child. 2001; 85(1): 12-5.<br />
* Hamid RK and Newfield P. Pediatric neuroanesthesia. Neural tube defects. Anesthesiol Clin North<br />
America 2001; 19(2): 219-28. (review)<br />
* Hamid RK and Newfield P. Pediatric neuroanesthesia. Hydrocephalus. Anesthesiol Clin North America<br />
2001; 19(2): 207-18. (review)<br />
Hammer GB and Krane EJ. Anaesthesia for liver transplantation in children. Paediatric Anaesthesia 2001;<br />
11(1): 3-18.<br />
* Hammer GB. Pediatric thoracic anesthesia. Anesthesia and Analgesia 2001; 92(6): 1449-64. (review)<br />
Heard CMB, Gunnarsson B, Heard AMB, Watson E, Orie JD and Fletcher JE. Anaesthetic technique for<br />
transoesophageal echocardiography in children. Paediatric Anaesthesia 2001; 11(2): 181-184.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 46
* Imanaka H, Nishimura M, Miyano H, Uemura H and Yagihara T. Effect of synchronized intermittent<br />
mandatory ventilation on respiratory workload in infants after cardiac surgery. Anesthesiology 2001;<br />
95(4): 881-8.<br />
* Iohom G and Lyons B. Anaesthesia for children with epidermolysis bullosa: a review of 20<br />
years'experience. European Journal of Anaesthesiology 2001; 18(11): 745-54.<br />
* Jayabose S, Levendoglu-Tugal O, Giamelli J, Grodin W, Cohn M, Sandoval C, Ozkaynak F, Kubal K,<br />
Nosetti M, Uman J and Visintainer P. Intravenous anesthesia with propofol for painful procedures in<br />
children with cancer. Journal of Pediatric Hematology and On<strong>co</strong>logy 2001; 23(5): 290-3.<br />
Keidan I, Berkenstadt H, Sidi A and Perel A. Propofol/remifentanil versus propofol alone for bone marrow<br />
aspiration in paediatric haemato-on<strong>co</strong>logical patients. Paediatric Anaesthesia 2001; 11(3): 297-301.<br />
Laussen PC, Murphy JA, Zurakowski D, Sullivan LJ, McGowan FX Jr and DeMaso DR. Bispectral index<br />
monitoring in children undergoing mild hypothermic cardiopulmonary bypass. Paediatric Anaesthesia<br />
2001; 11(5): 567- 574.<br />
* Matsota P, Avgerinopoulou-Vlahou A and Velegrakis D. Anaesthesia for phaeochromocytoma removal in a<br />
5-year-old boy. Paediatric Anaesthesia 2002; 12(2): 176-80.<br />
* Mali M, Bagry H and Vas L. Anaesthetic management of a case of nesidioblastosis for subtotal<br />
pancreatectomy. Paediatric Anaesthesia 2002; 12(1): 80-4.<br />
Muralidhar K and Shetty DP. Ventilation strategy for video-assisted thora<strong>co</strong>s<strong>co</strong>pic clipping of patent ductus<br />
arteriosus in children. Paediatric Anaesthesia 2001; 11(1): 45-48.<br />
Nakayama S, Yamashita M, Osaka Y,Isobe T and Izumi H. Right internal jugular vein venography in infants<br />
and children. Anesthesia and Analgesia 2001; 93(2): 331-334.<br />
* Newfield P, Hamid RK. Pediatric neuroanesthesia. Arteriovenous malformations. Anesthesiol Clin North<br />
America 2001; 19(2): 229-35. (review)<br />
Orliaguet GA, Hanafi M, Meyer PG, Blanot S, Jarreau MM, Bresson D, Zerah M and Carli PA. Is the sitting or<br />
the prone position best for surgery for posterior fossa tumours in children ? Paediatric Anaesthesia<br />
2001; 11(5): 541-548<br />
Paut O and Bissonnette B. Effect of halothane on the cerebral circulation in young children: a hysteresis<br />
phenomenon. Anaesthesia. 2001; 56(4): 360-5.<br />
* Payne D, McKenzie SA, <strong>St</strong>acey S, Misra D, Haxby E and Bush A. Safety and ethics of bronchos<strong>co</strong>py and<br />
endobronchial biopsy in difficult asthma. Archives of Diseases in Childhood 2001 84(5): 423-6.<br />
* Pierson J and Mayhew JF. Anesthesia in a child with Rett syndrome: a case report and literature review.<br />
AANA J. 2001; 69(5): 395-6.<br />
* Ravn HB, Hjortdal VE, <strong>St</strong>enbog EV, Emmertsen K, Kromann O, Pedersen J and Sorensen KE. Increased<br />
platelet reactivity and significant changes in <strong>co</strong>agulation markers after cavopulmonary <strong>co</strong>nnection.<br />
Heart 2001; 85(1): 61-5.<br />
* Roche J, Frawley G and Heggie A. Difficult tracheal intubation induced by maxillary distraction devices in<br />
craniosynostosis syndromes. Paediatric Anaesthesia 2002; 12(3): 227-34.<br />
Rodriguez RA, Cornel G, Weerasena NA, Pham B and Splinter WM. Effect of Trendelenburg head position<br />
during cardiac deairing on cerebral microemboli in children: A randomized <strong>co</strong>ntrolled trial. Journal<br />
Thorac Cardiovasc Surgery 2001; 121(1): 3-9.<br />
* Schwartz DA, Moriarty KP, Tashjian DB, Wool RS, Parker RK, Markenson GR, Rothstein RW, Shah BL,<br />
Connelly NR and Courtney RA. Anesthetic management of the exit (ex utero intrapartum treatment)<br />
procedure. Journal of Clinical Anesthesia 2001; 13(5): 387-91.<br />
Sonzogni V, Crupi G, Poma R, Annechino F, Ferri F, Filisetti P and Bellavita P. Erythropoietin therapy and<br />
preoperative autologous blood donation in children undergoing open heart surgery. International<br />
Journal of Anaesthesia 2001; 87(3): 429-434.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 47
* <strong>St</strong>einer LA, <strong>St</strong>uder W, Baumgartner ER and Frei FJ. Perioperative management of a child with very-longchain<br />
acyl-<strong>co</strong>enzyme A dehydrogenase deficiency. Paediatric Anaesthesia 2002; 12(2): 187-91.<br />
Suominen P, Palo R, Sairanen H, Olkkola KT and Rasanen J. Perioperative determinants and out<strong>co</strong>me of<br />
cardiopulmonary arrest in children after heart surgery. European Journal of Cardiothoracic Surgery<br />
2001; 19(2): 127-34.<br />
* Tabbutt S, Ramamoorthy C, Montenegro LM, Durning SM, Kurth CD, <strong>St</strong>even JM, Godinez RI, Spray TL,<br />
Wernovsky G and Ni<strong>co</strong>lson SC. Impact of inspired gas mixtures on preoperative infants with<br />
hypoplastic left heart syndrome during <strong>co</strong>ntrolled ventilation. Circulation 2001;18;104(12 Suppl 1):I159-<br />
64.<br />
* Tercan E, Sungun MB, Boyaci A and Kuc<strong>uk</strong>aydin M. One-lung ventilation of a preterm newborn during<br />
esophageal atresia and tracheoesophageal fistula repair. Acta Anaesthesiol Scand. 2002; 46(3): 332-<br />
3.<br />
Tobias JD. Thora<strong>co</strong>s<strong>co</strong>py in the pediatric patient. Anesthesiology Clinics of North America 2001; 19(1):<br />
173-186. (review)<br />
Tobias JD, Gaines RW, Lowry KJ, Kittle D and Bildner C. A dual epidural catheter technique to provide<br />
analgesia following posterior spinal fusion for s<strong>co</strong>liosis in children and adolescents. Paediatric<br />
Anaesthesia 2001; 11(2): 199-203.<br />
Tobias JD, Johnson JO, Jimenez DF, Barone CM, S<strong>co</strong>tt D and McBride Jr. Venous Air Embolism during<br />
endos<strong>co</strong>pic strip craniectomy for repair of craniosynostosis in infants. Anesthesiol. 2001; 95(2): 340-2.<br />
* Tripi PA, Thomas S and Dearborn DG. Management of general <strong>anaesthesia</strong> in infants and children with a<br />
history of idiopathic pulmonary haemorrhage. Paediatric Anaesthesia 2002; 12(3): 243-7.<br />
Uezono S, Holzman RS, Goto T, Nakata Y, Nagata S and Morita S. Prediction of difficult airway in schoolaged<br />
patients with microtia. Paediatric Anaesthesia 2001; 11(4): 409-13.<br />
van der Walt JH and Moran C. An audit of perioperative management of autistic children.<br />
Anaesthesia 2001; 11(4): 401-8.<br />
Paediatric<br />
Vas L, Patil B, Ragavendra S, Hosalkar H and Pratibha G Complications of <strong>anaesthesia</strong> and surgery for<br />
laryngotracheo-oesophageal cleft. Paediatric Anaesthesia 2001; 11(3): 361-5.<br />
Vas L and Sawant P. A review of anaesthetic technique in 15 paediatric patients with temporomandibular<br />
joint ankylosis. Paediatric Anaesthesia 2001; 11(2): 237-44.<br />
Wales PW, Carver E, Crawford MW and Kim PC. Acute chest syndrome after abdominal surgery in children<br />
with sickle cell disease: Is a laparos<strong>co</strong>pic approach better? J Pediatric Surgery 2001; 36(5): 718-21.<br />
Wardle SP, Kelsall AWR, Yoxall CW and Subhedar NV. Percutaneous femoral arterial and venous<br />
catherisation during neonatal intensive care. Arch Dis Child Fetal Neonatal Ed 2001; 85: 119-122.<br />
* White RJ and Bass S. Anaesthetic management of a patient with myotonic dystrophy. Paediatric<br />
Anaesthesia 2001; 11(4): 494-7.<br />
Wilson GA, Brown JL, Crabbe DG, Hinton W, McHugh PJ and <strong>St</strong>ringer MD. Is epidural analgesia associated<br />
with an improved out<strong>co</strong>me following open Nissen’s fundoplication? Paediatric Anaesthesia 2001;<br />
11(1): 65-70.<br />
© GOSH / <strong>Thames</strong> PAG, Drs R Howard & I Walker, 3 rd edition, May 2002 48