Interhospital transfer of Level 3 patients - St-marys-anaesthesia.co.uk
Interhospital transfer of Level 3 patients - St-marys-anaesthesia.co.uk
Interhospital transfer of Level 3 patients - St-marys-anaesthesia.co.uk
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
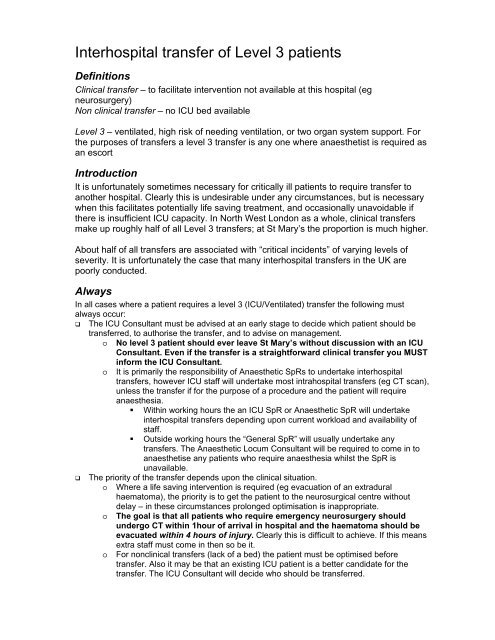
<strong>Interhospital</strong> <strong>transfer</strong> <strong>of</strong> <strong>Level</strong> 3 <strong>patients</strong><br />
Definitions<br />
Clinical <strong>transfer</strong> – to facilitate intervention not available at this hospital (eg<br />
neurosurgery)<br />
Non clinical <strong>transfer</strong> – no ICU bed available<br />
<strong>Level</strong> 3 – ventilated, high risk <strong>of</strong> needing ventilation, or two organ system support. For<br />
the purposes <strong>of</strong> <strong>transfer</strong>s a level 3 <strong>transfer</strong> is any one where anaesthetist is required as<br />
an es<strong>co</strong>rt<br />
Introduction<br />
It is unfortunately sometimes necessary for critically ill <strong>patients</strong> to require <strong>transfer</strong> to<br />
another hospital. Clearly this is undesirable under any circumstances, but is necessary<br />
when this facilitates potentially life saving treatment, and occasionally unavoidable if<br />
there is insufficient ICU capacity. In North West London as a whole, clinical <strong>transfer</strong>s<br />
make up roughly half <strong>of</strong> all <strong>Level</strong> 3 <strong>transfer</strong>s; at <strong>St</strong> Mary’s the proportion is much higher.<br />
About half <strong>of</strong> all <strong>transfer</strong>s are associated with “critical incidents” <strong>of</strong> varying levels <strong>of</strong><br />
severity. It is unfortunately the case that many interhospital <strong>transfer</strong>s in the UK are<br />
poorly <strong>co</strong>nducted.<br />
Always<br />
In all cases where a patient requires a level 3 (ICU/Ventilated) <strong>transfer</strong> the following must<br />
always occur:<br />
The ICU Consultant must be advised at an early stage to decide which patient should be<br />
<strong>transfer</strong>red, to authorise the <strong>transfer</strong>, and to advise on management.<br />
o No level 3 patient should ever leave <strong>St</strong> Mary’s without discussion with an ICU<br />
Consultant. Even if the <strong>transfer</strong> is a straightforward clinical <strong>transfer</strong> you MUST<br />
inform the ICU Consultant.<br />
o It is primarily the responsibility <strong>of</strong> Anaesthetic SpRs to undertake interhospital<br />
<strong>transfer</strong>s, however ICU staff will undertake most intrahospital <strong>transfer</strong>s (eg CT scan),<br />
unless the <strong>transfer</strong> if for the purpose <strong>of</strong> a procedure and the patient will require<br />
<strong>anaesthesia</strong>.<br />
• Within working hours the an ICU SpR or Anaesthetic SpR will undertake<br />
interhospital <strong>transfer</strong>s depending upon current workload and availability <strong>of</strong><br />
staff.<br />
• Outside working hours the “General SpR” will usually undertake any<br />
<strong>transfer</strong>s. The Anaesthetic Locum Consultant will be required to <strong>co</strong>me in to<br />
anaesthetise any <strong>patients</strong> who require <strong>anaesthesia</strong> whilst the SpR is<br />
unavailable.<br />
The priority <strong>of</strong> the <strong>transfer</strong> depends upon the clinical situation.<br />
o Where a life saving intervention is required (eg evacuation <strong>of</strong> an extradural<br />
haematoma), the priority is to get the patient to the neurosurgical centre without<br />
delay – in these circumstances prolonged optimisation is inappropriate.<br />
o The goal is that all <strong>patients</strong> who require emergency neurosurgery should<br />
undergo CT within 1hour <strong>of</strong> arrival in hospital and the haematoma should be<br />
evacuated within 4 hours <strong>of</strong> injury. Clearly this is difficult to achieve. If this means<br />
extra staff must <strong>co</strong>me in then so be it.<br />
o For nonclinical <strong>transfer</strong>s (lack <strong>of</strong> a bed) the patient must be optimised before<br />
<strong>transfer</strong>. Also it may be that an existing ICU patient is a better candidate for the<br />
<strong>transfer</strong>. The ICU Consultant will decide who should be <strong>transfer</strong>red.
The patient must be ac<strong>co</strong>mpanied by a Specialist Registrar in Anaesthetics with experience<br />
(and ideally training) in <strong>Interhospital</strong> Transfer. The experience <strong>of</strong> the es<strong>co</strong>rting doctor must<br />
match the severity <strong>of</strong> illness <strong>of</strong> the patient – more senior anaesthetists may be required if the<br />
patient is very unstable.<br />
Have a low threshold for the use <strong>of</strong> Noradrenaline in <strong>patients</strong> with suspected raised ICP or<br />
hypotension. FULL PATIENTS TRAVEL BETTER.<br />
Full monitoring should be applied, including in almost all cases (especially neuro)<br />
invasive arterial monitoring.<br />
A <strong>transfer</strong> form must be obtained from ICU to document the <strong>transfer</strong>. This must be<br />
<strong>co</strong>mpleted and then the top <strong>co</strong>py is left with the receiving hospital, and the remaining <strong>co</strong>pies<br />
returned to the ICU at <strong>St</strong> Mary’s. The <strong>transfer</strong> form also <strong>co</strong>ntains information about the safe<br />
<strong>co</strong>nduct <strong>of</strong> <strong>transfer</strong>s and information such as <strong>co</strong>ntact phone numbers on the reverse.<br />
The referring team must write a <strong>transfer</strong> letter, whether this is A&E, Medicine or Surgery –<br />
the <strong>transfer</strong> form is not a substitute for this.<br />
A Specialist Registrar <strong>of</strong> the referring speciality must always review the patient, unless this<br />
will delay the receipt <strong>of</strong> life saving treatment.<br />
The Transfer equipment is kept in ICU with the forms in ICU. This must be checked before<br />
use by the <strong>transfer</strong>ring anaesthetist.<br />
Take photo<strong>co</strong>pies <strong>of</strong> relevant notes.<br />
The bed manager (during day) or Site Practitioner during the night MUST be informed<br />
<strong>of</strong> the <strong>transfer</strong>. They should help <strong>co</strong>ordinate who is the most appropriate person to<br />
ac<strong>co</strong>mpany the doctor as an es<strong>co</strong>rt on the <strong>transfer</strong>. The site practitioner must also<br />
make an entry on the hospital log to include:<br />
o Date and time<br />
o Patient name, hospital number and date <strong>of</strong> birth<br />
o Reason for <strong>transfer</strong><br />
o Destination<br />
o ICU Consultant on Call<br />
o Referring Consultant<br />
o Name <strong>of</strong> es<strong>co</strong>rting doctor<br />
o Name <strong>of</strong> es<strong>co</strong>rting nurse<br />
Phone the receiving ICU before leaving.<br />
Take a mobile phone.<br />
Return the <strong>transfer</strong> kit and bottom 2 sheets to the ICU<br />
If the <strong>transfer</strong> occurred because <strong>of</strong> lack <strong>of</strong> ICU beds at <strong>St</strong> Mary’s a trust critical incident form<br />
must always be <strong>co</strong>mpleted, and returned to ICU.<br />
If at any stage there are difficulties in arranging a <strong>transfer</strong>, especially where this is for definitive<br />
treatment the referring Consultant and the ICU Consultant must be informed in order to prevent<br />
anomalous delays in people receiving the right treatment. In particular the goal is that <strong>patients</strong><br />
who require emergent neurosurgical intervention to receive their treatment within 4<br />
hours <strong>of</strong> the time <strong>of</strong> injury.<br />
The safe <strong>co</strong>nduct <strong>of</strong> any <strong>transfer</strong> is ultimately the responsibility <strong>of</strong> the referring hospital<br />
and the es<strong>co</strong>rting doctor. If you receive advice from the receiving hospital which you regard<br />
as unsafe, you should discuss management with the Anaesthetic/ICU Consultant, but in no<br />
case should a patient with significantly falling <strong>co</strong>nscious level or <strong>co</strong>ma (GCS
Checklist<br />
Below are mnemonics for a pre<strong>transfer</strong> assessment<br />
Allergies<br />
Medications<br />
Past Medical History<br />
Last oral intake<br />
Events leading upto <strong>transfer</strong> (ie what is the story)<br />
Assessment <strong>of</strong> the patient<br />
Airway & Cervical spine<br />
Breathing<br />
Circulation<br />
Disability (Neuro)<br />
Exposure and Fractures<br />
Fluids electrolytes and renal<br />
Gut<br />
Haematology<br />
Infection<br />
Organisational<br />
Just in case (Mobile etc)<br />
Kit check<br />
Lab Results<br />
Monitoring<br />
Notes & X rays<br />
Oxygen<br />
Paperwork and Phone<br />
Quality <strong>co</strong>ntrol & Audit<br />
Ready <strong>St</strong>eady Go<br />
Process<br />
Make the situation safe<br />
Contact ICU Nurse in charge will send equipment and drugs – primary support<br />
for ICU <strong>patients</strong> outside ICU and <strong>transfer</strong>s<br />
Establish basic facts<br />
Contact ICU Consultant – Discuss case. Suitability for ICU Suitability for<br />
<strong>transfer</strong> Decides on plan.<br />
You <strong>co</strong>ntact receiving hospital ICUs (+/- ICU Consultant)<br />
Refer back to ICU Consultant if problems finding a bed<br />
You as the legal medical es<strong>co</strong>rt are responsible for patient safety, paper work<br />
and equipment<br />
You MUST please bring all equipment and the <strong>transfer</strong> forms back to ICU and give them<br />
to the ICU Nurse in Charge.<br />
Finally please, please let me know <strong>of</strong> any medical, political, or logistic problems you<br />
experience- please fill out critical incident forms and email me. I can’t try and solve what<br />
I do not know about.<br />
Many thanks<br />
Simon Ashworth (simon.ashworth@nhs.net)<br />
ICU Consultant
Assess<br />
Support <strong>transfer</strong><br />
Identify assistant<br />
Enter <strong>transfer</strong> details<br />
on Hospital Log<br />
(Patient ID,<br />
Destination, Es<strong>co</strong>rts)<br />
Bed Managr<br />
or<br />
Site<br />
Practitioner<br />
(Night)<br />
ICU<br />
Consultant<br />
Control<br />
<strong>St</strong>abilise and establish<br />
invasive monitoring<br />
Communicate<br />
Local Area<br />
Nurse<br />
in Charge<br />
Decides on the plan<br />
Establish priorities<br />
Intervene if problems<br />
Who goes<br />
Where<br />
Priority<br />
Sorts out politics<br />
Discusses with<br />
receieving <strong>co</strong>nsultant<br />
Get the facts!<br />
Documentation<br />
Fill in Transfer form<br />
Transfer patient<br />
YOU!<br />
Return equipment and<br />
ICU Nurse in<br />
Charge<br />
Referring<br />
doctors<br />
Support Anaesthetist<br />
Transfer Letter<br />
Phone receiving<br />
medical team<br />
Patient – needs<br />
ICU or <strong>transfer</strong><br />
Assume<br />
nothing and<br />
trust no-one!<br />
Support <strong>transfer</strong> with<br />
- Equipment<br />
- Documentation<br />
Agree who will assist<br />
on <strong>transfer</strong> with other<br />
senior nurses<br />
- Ward staff<br />
- ODP<br />
- ICU nurse
Airway<br />
Pre <strong>transfer</strong><br />
Secure, Safe<br />
GCS < 8 or fluctuating – intubate<br />
pO2 < 8 Kpa - intubate<br />
Pre & In transit<br />
Suction<br />
Spare equipment for potential loss <strong>of</strong> airway<br />
Bag/valve/mask<br />
Personnel<br />
Cervical spine<br />
Is the history <strong>co</strong>mpatible with injury<br />
Clearance depends upon definitive CT<br />
proto<strong>co</strong>l<br />
Scans reviewed by Consultant radiologist.<br />
Examination must inform<br />
If in doubt manage as if injured<br />
Neutral position<br />
Collar +/- Sandbags<br />
Breathing<br />
Adequate blood gases<br />
Ventilated – stabilise 15 minutes prior to<br />
<strong>transfer</strong> on transport ventilator<br />
Breathing<br />
Rib fractures<br />
or<br />
Pneumothorax<br />
= CHEST DRAIN<br />
Drains always unclamped (except post<br />
pneumonectomy)<br />
Circulation<br />
‘Full <strong>patients</strong> travel better’<br />
Give fluids and assess CVP & perfusion<br />
prior to <strong>transfer</strong><br />
Ensure MAP > 75mmHg (>90 mmHg in<br />
Neuro)<br />
Ensure Systolic BP > 120mmHg<br />
Pulse needs to be < 120 / minute<br />
2 x IV cannula for travel<br />
Fluids – (volumetric pumps are not<br />
designed to travel)<br />
Circulation<br />
If in doubt start low dose pressors and/or<br />
inotropes<br />
Noradrenaline usually best if sedated<br />
Augments benefit <strong>of</strong> “being full”<br />
Make sure all infused drugs clear dead<br />
space<br />
3 way tap (¡Ö0.5ml) + lumen (0.3-0.5ml) ¡Ö<br />
1ml<br />
At 2 ml/h may take 1h<br />
Run at 20ml/h for 2 mins then 10ml/h until<br />
response seen<br />
Disability (Neurological status)<br />
History <strong>of</strong> suggesting neurological<br />
impairment<br />
Clinical Examination (symmetry)<br />
Best GCS<br />
Current GCS<br />
Response to pain centrally (V) and<br />
peripherally<br />
Pupils (II, III)<br />
Eye movements (II, III, IV, V, VI, VIII)<br />
Reflexes and plantar reflexes<br />
Corneal reflex<br />
CT findings<br />
Disability (Neurological status)<br />
SEDATE ALWAYS if orally intubated<br />
Relaxants USUALLY<br />
Always <strong>co</strong>nsider seizures a possibility<br />
Non<strong>co</strong>nvulsive status<br />
Anti<strong>co</strong>nvulsants<br />
Raised ICP<br />
KEEP MAP > 90<br />
Deeper sedation<br />
Exposure (and Fractures)<br />
Check Temperature<br />
Patients usually get <strong>co</strong>ld<br />
Vaso<strong>co</strong>nstriction can precipitate pulmonary<br />
oedema<br />
Wrap well with blankets (even if just going<br />
along <strong>co</strong>rridors)<br />
Pressure points must be well padded<br />
Lines<br />
Where How old Secure<br />
Ensure se<strong>co</strong>ndary survey has<br />
been <strong>co</strong>mpleted (ATLS) or at least fully<br />
documented to point it was stopped<br />
Fractures must be stabilised (bones grate<br />
against each other with the vibration <strong>of</strong><br />
travel)<br />
Also imply blood loss/risk or bleeding<br />
Fluids, Electrolytes and Renal<br />
Sodium<br />
Do NOT attempt <strong>co</strong>mplete or rapid<br />
<strong>co</strong>rrection unless actively fitting<br />
Potassium (aim 4.0 to 5.0)<br />
Correct to safe range BEFORE moving<br />
Mg >1.0 (give 20 mmol if necessary, esp MI<br />
or PET)<br />
Correct acidosis
Bicarbonate BY INFUSION if required<br />
Urinary catheter<br />
GLUCOSE<br />
Gut<br />
Nasogastric tube<br />
Oral (head if base <strong>of</strong> skull fracture<br />
suspected or <strong>co</strong>agulopathic)<br />
Free drainage<br />
CHECK POSITION ON CXR<br />
History suggesting possible intra-abdominal<br />
bleeding (AAA, Trauma)<br />
NOT SUITABLE FOR TRANSFER unless<br />
purpose is definitive surgical treatment<br />
Haematology<br />
Ensure Hb > 7.0<br />
Aim > 10 if any risk <strong>of</strong> bleeding or recent MI<br />
Coagulation satisfactory<br />
Platelets > 50..100<br />
What products have been given<br />
Have you got and checked the crossmatched<br />
blood<br />
Known antibodies<br />
Infection<br />
Does your hospital have any current<br />
problems with multiresistant or transmissible<br />
organisms (eg MRSA, VRE, Acinetobacter)<br />
Does this patient have any MR<br />
Are they a <strong>co</strong>ntact<br />
Any other transmissible infection (esp TB,<br />
HIV, HBV, HCV)<br />
Does the patient have active infection<br />
Known bugs What antibiotics Doses up to<br />
date<br />
Have appropriate Cultures been taken<br />
Infusions<br />
Rationalise infusions<br />
Sedation + Analgesia (Prop<strong>of</strong>ol + Opioid)<br />
Relaxant (<strong>co</strong>nsider Pancuronium bolus)<br />
Noradrenaline<br />
Inotrope<br />
Possibly Insulin<br />
Possibly Bicarbonate<br />
Syringe drivers ONLY<br />
Put vasoactive drugs on smallest lumens<br />
white or blue 18G<br />
Keep larger CVP lumens (grey 14G) for<br />
rapid infusion
Organisational<br />
Just in case<br />
Mobile phone + Phone numbers<br />
Cash + Clothing<br />
Food & drink<br />
Cyclizine<br />
Emergency drugs (ALWAYS LABELLED)<br />
Kit Check<br />
Batteries, Leads and Inverter<br />
Defibrillator<br />
Monitor<br />
Suction unit<br />
Transfer bag<br />
Tracheostomy / Cricthyroidotomy kit<br />
Ventilator<br />
Air mix reduces usage by 50%<br />
Allow DOUBLE expected requirement with a<br />
buffer <strong>of</strong> at LEAST 1 hour (Lift stuck Traffic<br />
jam)<br />
Paperwork<br />
Ensure details are filled out on <strong>transfer</strong> form<br />
It is YOUR defence against litigation and<br />
disciplinary action<br />
It is a legal requirement<br />
Bad forms usually <strong>co</strong>rrelate with poorly<br />
<strong>co</strong>nducted <strong>transfer</strong>s<br />
Complete checklist<br />
Lab Results<br />
If you have checked it … know the result<br />
NEVER go without knowing at least<br />
Glu<strong>co</strong>se<br />
Potassium<br />
Hb<br />
Blood gases<br />
Monitoring<br />
Minimum for <strong>Level</strong> 2<br />
ECG<br />
SpO2<br />
NIBP<br />
Minimum for <strong>Level</strong> 3<br />
As above<br />
Arterial Line<br />
In most cases CVP (4+ lumens)<br />
ETCO 2<br />
Monitoring an equipment is secure<br />
Notes and X Rays<br />
Medical notes<br />
Nursing notes<br />
Transfer Letter for interhospital <strong>transfer</strong>s<br />
Transfer form<br />
Complete checklist<br />
Scans<br />
X Rays<br />
Oxygen<br />
Minute volume = Tidal volume x Rate<br />
Usually 5-15 L/min<br />
Requirement = 60 x Minute volume L/h<br />
Can usually assume a requirement <strong>of</strong> 600<br />
L/h
Pre<strong>transfer</strong> checklist (see <strong>transfer</strong> form)<br />
Airway:<br />
Gag & Cough ok<br />
GCS > 8<br />
Intubated<br />
ETT is ok on CXR<br />
C Spine clear/immobile<br />
Breathing:<br />
OK on Transport vent<br />
ABGs & CXR ok<br />
Drains unclamped<br />
Circulation:<br />
Vital signs stable<br />
Well filled<br />
No bleeding<br />
IVI through dead space<br />
HR<br />
BP<br />
Disability:<br />
Pupils ok<br />
Alert<br />
responds to Verbal<br />
responds to Pain<br />
Unresponsive<br />
Sedation / relaxants ok<br />
Exposure:<br />
IV access x2 ok<br />
Fractures stable (if any)<br />
Pt secured on trolley<br />
Fluids/Renal:<br />
Catheterised<br />
Gut:<br />
NGT/OGT checked<br />
Haematology:<br />
Blood products<br />
Infection:<br />
Antibiotics given<br />
Cultures taken<br />
Just in Case:<br />
Emergency Drugs<br />
Kit Check:<br />
Ventilator<br />
Transfer bag<br />
Batteries ok, Leads<br />
Inverter & adaptor<br />
Suction<br />
Lab Results<br />
Hb >7<br />
Blood glu<strong>co</strong>se > 4<br />
K 3.5 to 5.5<br />
pH >7.2 and BE +/-5<br />
Monitoring<br />
Notes and Scans<br />
Oxygen - sufficient for journey x2<br />
<br />
+1h<br />
Phone<br />
Mobile phone<br />
Contact destination
Phone<br />
YOU MUST notify<br />
ICU Consultant<br />
Destination to verify that they will be ready<br />
Ambulance<br />
Usually ask for Emergency ambulance will<br />
arrive within 15min<br />
Neurosurgical emergency – state this you<br />
will get next ambulance<br />
Do not delegate these tasks<br />
Communication is Central<br />
Quality Control<br />
Critical incidents<br />
You must fill out incident forms, otherwise it<br />
will happen again, and again and again and<br />
…. again<br />
If equipment fails you must identify it<br />
Make a note <strong>of</strong> the serial number and<br />
hospital equipment number and re<strong>co</strong>rd this<br />
on critical incident form and <strong>transfer</strong> form<br />
Ready to Go<br />
Summary<br />
THINK<br />
Pink<br />
Full<br />
<strong>St</strong>able<br />
Warm<br />
Simple<br />
Finally, assume nothing and trust no one
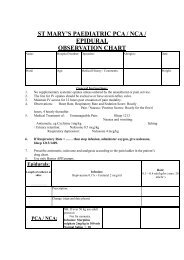
Transfer documentation<br />
Since 12/1/04 <strong>co</strong>mmon <strong>transfer</strong> documentation has been used across West London. This is mandatory<br />
for all <strong>Level</strong> 3 interhospital <strong>transfer</strong>s. In case <strong>of</strong> doubt please fill out a form. The forms should be used for<br />
all elective and emergency <strong>transfer</strong>s, and certainly for any ventilated patient.<br />
It is re<strong>co</strong>gnised that this represents yet another tedious bit <strong>of</strong> paper to fill out – however there are a<br />
number <strong>of</strong> reasons it must be done.<br />
1. Previously the process was undocumented – you and your trust and <strong>co</strong>nsultants are all vulnerable to<br />
medi<strong>co</strong>legal challenge if a patient suffers a poor out<strong>co</strong>me, and the <strong>transfer</strong> cannot be shown to have<br />
been well <strong>co</strong>nducted. This is obviously impossible without any documentation! As the doctor<br />
immediately present you are a most attractive target.<br />
2. Many <strong>transfer</strong>s are poorly <strong>co</strong>nducted – the es<strong>co</strong>rts know little about the patient. The patient is not<br />
optimised prior to departure. The “plan” is <strong>of</strong> dubious quality – if there is one.<br />
3. Too many <strong>transfer</strong>s occur. It is hoped that with better data about <strong>transfer</strong>s the number can be<br />
reduced by better planning.<br />
4. Transfers are a risky business. One study showed mishaps occurred in 67% <strong>of</strong> <strong>transfer</strong>s. Why<br />
What Any avoidable problems<br />
5. Very few people get formal training in <strong>transfer</strong>s. There is information on the back <strong>of</strong> the form, which<br />
should be helpful.<br />
6. The hospital site practitioner or bed manager must be informed as early as possible <strong>of</strong> the potential<br />
need for <strong>transfer</strong>. They should be able to organise support and identify an assistant for you.<br />
7. Failure to adequately fill in a <strong>transfer</strong> form or to inform the ICU Consultant before departure<br />
will be taken seriously and will be reflected in your RITA reports.<br />
Q. How do I get the form<br />
A. The forms will be kept on ICU with the <strong>transfer</strong> kit. As soon as you identify a patient who needs a<br />
<strong>transfer</strong> ask for the kit, and a form. The nurse in charge <strong>of</strong> ICU will ask for the destination and name <strong>of</strong> the<br />
patient, and will send you a form with the kit.<br />
Q. What do I do with it<br />
A. Fill it out! By all means ask a nurse helping you with the patient to <strong>co</strong>mplete the demographics.<br />
You then need to put in the medical details and do the observations. The form must be signed <strong>of</strong>f at the<br />
destination. The form is an A3 3 part carbon <strong>co</strong>py. Leave the top <strong>co</strong>py at the receiving hospital in the<br />
notes, and bring back the remaining <strong>co</strong>pies with the <strong>transfer</strong> kit to the ICU. Interestingly quality <strong>of</strong> <strong>transfer</strong><br />
does seem to <strong>co</strong>rrelate with the quality <strong>of</strong> the <strong>transfer</strong> – ie shambolic paperwork = shambolic <strong>transfer</strong>.<br />
Q. What if there is an incident<br />
A. Re<strong>co</strong>rd this on the <strong>transfer</strong> form. You must also <strong>co</strong>mplete a trust critical incident form – by all<br />
means do not put your name if you don’t want to.<br />
Q. What if there are problems with <strong>transfer</strong>s/politics, etc<br />
A. “Acutely” the ICU or Anaesthetic <strong>co</strong>nsultants will sort these issues out. In due <strong>co</strong>urse please<br />
<strong>co</strong>ntact me at <strong>St</strong> Mary’s and let me know about any problems, especially if you think an avoidable risk<br />
exists.<br />
Many thanks<br />
Simon Ashworth<br />
Consultant in Intensive Care and Anaesthesia, <strong>St</strong> Mary’s hospital<br />
Lead clinician for <strong>Interhospital</strong> Transfers North West London Critical Care Network<br />
Simon.ashworth@st-<strong>marys</strong>.nhs.<strong>uk</strong>
Little shop <strong>of</strong> Horrors<br />
Transfer to Hammersmith 72 year old woman. Non clinical<br />
Post laparotomy for ischaemic bowel<br />
Septic shock<br />
Kyphos<strong>co</strong>liosis<br />
Very poor exercise tolerance<br />
Developmental delay<br />
Transferred to permit admission <strong>of</strong> trauma patient<br />
Trachy day 2<br />
ICU Consultant rang HH to verify safe <strong>transfer</strong>…<br />
Yes but…<br />
Opening line from <strong>transfer</strong>ring doctor was “I don’t really know the patient…”<br />
… no notes<br />
No op note<br />
Transfer note not really filled out<br />
Didn’t realise she had had a trachy<br />
Why did she have a trachy so early<br />
Transfer to Royal Surrey County Hospital Non clinical<br />
60y Aspiration pneumonia<br />
Monitor Battery failed in South London<br />
Pump batteries all failed during journey<br />
…Never plugged in!<br />
Transfer to Roehampton Non clinical<br />
70y woman post laparotomy<br />
Weaning. Moderate LV. Ischaemic heart disease<br />
February -3˚C<br />
Transferred unsedated on Waters bag.<br />
Developed pulmonary oedema before even getting in ambulance<br />
Hypoxic and distressed on arrival with gross pulmonary oedema<br />
Transfer to Queen Square. Clinical <strong>transfer</strong> though not for definitive intervention<br />
for EEG monitoring<br />
25y Patient with refractory seizures due to anoxic encephalopathy<br />
“Evolving sepsis” became septic shock<br />
Arrived on >1mcg/kg/min Noradrenaline and Adrenaline<br />
Died within hours<br />
What are the lessons
Date<br />
Surname<br />
Hospital no<br />
Destination<br />
Es<strong>co</strong>rting Dr<br />
<br />
<br />
<br />
<br />
NHS<br />
1 Who<br />
NHS/Hospital/AE number<br />
Name<br />
Date <strong>of</strong><br />
Birth / /<br />
Male<br />
2 Where<br />
Referring<br />
Hospital<br />
3 When<br />
Female<br />
Age<br />
From Ward Theatre<br />
ICU HDU A&E<br />
Other<br />
Consultant<br />
<strong>St</strong>aff arranging <strong>transfer</strong><br />
Name<br />
Speciality<br />
Phone<br />
Incident / / :<br />
Arrival in<br />
hospital<br />
/ / :<br />
Intubation / / :<br />
/ / :<br />
Decision to<br />
Transfer<br />
/ / :<br />
Recipient<br />
<strong>co</strong>ntacted<br />
Transfer / / :<br />
agreed<br />
There is no need to enter an exact<br />
time for any event which occured >48h<br />
before <strong>transfer</strong>.<br />
4 Why<br />
Ext/Bleep<br />
Grade<br />
Type and Reason for <strong>transfer</strong><br />
One way<br />
Return<br />
Emergency<br />
Very Urgent 4<br />
K 3.5 to 5.5<br />
pH >7.2 and BE +/-5<br />
Monitoring<br />
Notes and Scans<br />
Oxygen - suffi cient for<br />
journey x2 +1h<br />
Phone<br />
Mobile phone<br />
Contact destination<br />
/ /<br />
Time :
This <strong>transfer</strong> form...<br />
Q. Why do I have to fill out this form<br />
A. It is now a requirement that the <strong>transfer</strong> <strong>of</strong><br />
critically ill <strong>patients</strong> is documented. Without it<br />
neither trusts nor doctors have any defence in the<br />
face <strong>of</strong> mishap. Good documentation protects the<br />
people undertaking <strong>transfer</strong>s. We also hope that<br />
the form will help ensure that transport es<strong>co</strong>rts<br />
are aware <strong>of</strong> all relevant <strong>co</strong>nditions before getting<br />
into the intrinsically harsh environment <strong>of</strong> an<br />
ambulance - not the place to dis<strong>co</strong>ver an allergy<br />
documented illegibly on a scrap <strong>of</strong> paper you<br />
haven’t read. [ICS §14.7, §18, Appendix 5]<br />
Q. What happens to the <strong>co</strong>py which goes to the<br />
network<br />
A. The form allows the network to know if their<br />
are problems with the <strong>transfer</strong> process or for<br />
example bed provision - this will help rational<br />
<strong>co</strong>mmissioning <strong>of</strong> services, and ultimately we<br />
hope, reduce the need for <strong>transfer</strong>s.<br />
Q. When should I fill out the form<br />
It is worth starting the form once the need<br />
for <strong>transfer</strong> has been identified. Apart from<br />
documenting the <strong>transfer</strong>, the form should help<br />
you to make effective referrals with all information<br />
at your fingertips.<br />
Q. Do I need a <strong>transfer</strong> letter as well<br />
A. YES. This form is NOT a substitute for a<br />
<strong>transfer</strong> letter, which is required to give a detailed<br />
description <strong>of</strong> the events leading up to admission,<br />
examination findings, past medical history,<br />
investigations and treatment. The referring<br />
medical or surgical must write this.<br />
A <strong>co</strong>py <strong>of</strong> the notes, recent X-rays, CT scans and<br />
current lab results must also go with the patient.<br />
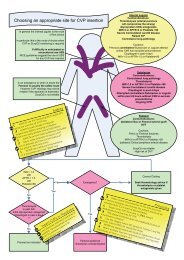
The <strong>transfer</strong> form boxes<br />
Box 1. The post <strong>co</strong>de helps determine if large numbers <strong>of</strong> out area<br />
<strong>patients</strong> are being treated.<br />
Box 2. Please fill this in as <strong>co</strong>mpletely as possible. The destination<br />
is the place where you relinquish care for the patient hand over<br />
and detach your equipment - if the patient goes to theatres<br />
then ICU, the destination is theatres. If you go via A&E to ICU,<br />
the destination is ICU. The named <strong>co</strong>nsultants should be the<br />
responsible ICU <strong>co</strong>nsultants, AND any other <strong>co</strong>nsultant under<br />
whose care the patient falls (eg surgeon)<br />
Box 3. Please put in all timings. The ambulance references should<br />
be included for your reference, and will also help seniors to chase<br />
up any delays or incidents.<br />
Box 4. A non clinical <strong>transfer</strong> occurs when a patient is <strong>transfer</strong>red<br />
because there is no bed, nurse or equipment (please <strong>co</strong>mment<br />
what was lacking). Repatriation occurs when a patient is<br />
<strong>transfer</strong>red either back to a hospital from which they were<br />
<strong>transfer</strong>red out, or when they are <strong>transfer</strong>red to a hospital nearer<br />
home. If two categories apply (eg Repariation and lack <strong>of</strong> beds)<br />
then tick both boxes.<br />
Box 5. This obviously lists the basic ATLS dataset vital for patient<br />
safety. Please remember to list antibiotics given, and their timing.<br />
Box 6. Sumarises the interventions which have been made, the<br />
support the patient requires, and essentially the neurological<br />
status <strong>of</strong> the patient imediately prior to intubation - this may be <strong>of</strong><br />
vital prognostic importance.<br />
Box 7. The observation chart. Please tick all the lines and<br />
monitoring used, and enter the number <strong>of</strong> days the lines have<br />
been in. If the lines were inserted in suboptimal <strong>co</strong>ndtions<br />
(emergency, on normal ward, etc) then please draw attention<br />
to this in the <strong>co</strong>mments area. Before departure you should read<br />
the checklist on this page and tick the “Checklist done” box.<br />
You should start the observations before the <strong>transfer</strong> to verify<br />
stability. Make sure that you check ABGs just before departure<br />
and immediately after arrival - this will help identify rapidly any<br />
sequelae <strong>of</strong> the <strong>transfer</strong>.<br />
Box 8. Complete the checklist prior to departure.<br />
Box 9. Verifies your identity and the level <strong>of</strong> training and experience<br />
you have <strong>of</strong> <strong>transfer</strong>s.<br />
Box 10. Both the <strong>transfer</strong>ring and receiving doctors should sign<br />
<strong>of</strong>f the <strong>transfer</strong>. Make sure you indicate whether any incidents<br />
occured - if there were problems you must fill out an incident<br />
form at your home hospital. Transfer specific incidents are those<br />
which <strong>co</strong>uld only occur during a <strong>transfer</strong>, such as hypotension on<br />
acceleration, falling equipment, fall from trolley, vehicle crashes.<br />
Transfer Politics<br />
Q. Who decides<br />
A. The decision to <strong>transfer</strong> a critically ill patient<br />
is always a balance <strong>of</strong> the associated benefits<br />
and risks, and must be made by a <strong>co</strong>nsultant<br />
in intensive care medicine in discussion<br />
with <strong>co</strong>nsultant <strong>co</strong>lleagues from the referring<br />
and receiving hospitals. The final decision to<br />
accept a patient lies with the ICU <strong>co</strong>nsultant<br />
in the receiving hospital. At the same time<br />
the final decision as to which patient should<br />
be <strong>transfer</strong>red lies with the referring ICU<br />
<strong>co</strong>nsultant. Recipient units should not attempt<br />
to put undue pressure on the <strong>transfer</strong>ring unit<br />
to <strong>transfer</strong> one patient rather than another.<br />
[NWLCCN-A]<br />
Q. Who goes A new unstable patient or an<br />
existing stable patient [NWLCCN-A]<br />
A. This is a very <strong>co</strong>mplex issue. In general<br />
<strong>patients</strong> should not be subjected to any<br />
intervention which is not in their best interests.<br />
Within the Network established practice is to<br />
avoid <strong>transfer</strong>ring <strong>patients</strong> from the safety <strong>of</strong> ICU<br />
unless it is in their own best interests. In certain<br />
circumstances it may be more pragmatic to<br />
<strong>transfer</strong> a stable patient, particularly if they may<br />
experience some gain from additional expertise<br />
available at the receiving hospital (e.g. better<br />
<strong>co</strong>ver in some relevant subspeciality, nearer<br />
home or relatives). If it is decided that the solution<br />
which <strong>of</strong>fers least risk to all <strong>patients</strong> involves the<br />
<strong>transfer</strong> <strong>of</strong> a stable patient already in ICU, then<br />
you must take the following steps:<br />
1. The decision must be taken by the ICU<br />
<strong>co</strong>nsultant at the referring hospital.<br />
2. Document in the patient notes that the<br />
decision has been taken, why, and who by.<br />
3. Write a critical incident form, naming both<br />
<strong>patients</strong>, and the reasons the decision has<br />
been taken, and who took the decision.<br />
4. Document in the patient’s notes that a<br />
critical incident form has been generated.<br />
5. Inform the relatives <strong>of</strong> the <strong>transfer</strong>, and the<br />
reasons for it. You may refer them to network<br />
policy in case <strong>of</strong> dissent, but if strong feelings<br />
are expressed it may be wise to <strong>co</strong>nsider<br />
other solutions.<br />
6. At the earliest <strong>co</strong>nvenient opportunity,<br />
inform the ICU director <strong>of</strong> the <strong>transfer</strong> and its<br />
circumstances [NWLCCN-A §4.2]<br />
Q. Who goes (with the patient)<br />
A. Critically ill <strong>patients</strong> must be ac<strong>co</strong>mpanied<br />
by at least 2 “appropriately experienced<br />
attendants, at least one <strong>of</strong> whom must be a<br />
medical practitioner with training in Intensive<br />
care medicine, Anaesthesia, or another acute<br />
speciality”. [ICS §9]<br />
Q. S<strong>co</strong>op and run or stay and play<br />
A. Patients should be meticulously resuscitated<br />
prior to <strong>transfer</strong>, except where this may delay<br />
life saving surgical treatment (e.g. emergency<br />
aneurysm repair).<br />
Q. Where should <strong>patients</strong> be <strong>transfer</strong>red<br />
A. Each hospital should have arrangements<br />
in place to ensure that <strong>transfer</strong>s for capacity<br />
reasons alone occur only as a last resort. Where<br />
necessary the <strong>transfer</strong> should be to the most<br />
appropriate hospital for the needs <strong>of</strong> the patient,<br />
taking ac<strong>co</strong>unt <strong>of</strong> bed availability and <strong>transfer</strong><br />
distance. Likely receiving hospitals should be<br />
included in the referring hospitals designated<br />
<strong>transfer</strong> group. Any <strong>transfer</strong> solely on the<br />
basis <strong>of</strong> capacity beyond this is classified<br />
as an adverse clinical event and must be<br />
reported to through the ICU director to the<br />
chief executive at the referring hospital. [ICS<br />
§5-6]<br />
Transfer Practicalities<br />
Q. Who is responsible for the <strong>transfer</strong><br />
A. The <strong>transfer</strong> process is the joint responsibility <strong>of</strong><br />
the referring and receiving clinicians. The medical<br />
staff at the receiving hospital may <strong>of</strong>fer advice<br />
on management, but patient management is<br />
always ultimately the responsibility <strong>of</strong> the<br />
doctor in attendance. [ICS §10.3]<br />
Q. Who should be intubated<br />
A. Intubation is mandatory if their are <strong>co</strong>ncerns<br />
about the integrity <strong>of</strong> the airway or ventilation.<br />
Intubated <strong>patients</strong> should be paralysed, sedated<br />
and ventilated. [ICS §13.4]<br />
Q. Who should have a chest drain<br />
A. Anyone who has or is suspected <strong>of</strong> having<br />
a pneumothorax. Ideally use Heimlich valve<br />
systems in place <strong>of</strong> underwater seals. Do not<br />
clamp drains. [ICS §13.6] If there is a very large<br />
leak Heimlich valves have resistence and can<br />
lead to tension so use caution, and seek senior<br />
specialist advice before embarking.<br />
Q. What monitoring is necessary<br />
A. The minimum standards for monitoring<br />
during <strong>transfer</strong> include the <strong>co</strong>ntinuous<br />
presence <strong>of</strong> appropriately trained staff, ECG,<br />
noninvasive blood pressure, oxygen saturation,<br />
end tidal carbon dioxide, and temperature. In<br />
mechanically ventilated <strong>patients</strong>, inspired oxygen<br />
tension and airway pressure should be monitored<br />
<strong>co</strong>ntinuously. Invasive arterial pressure should be<br />
measured in almost all <strong>patients</strong>. [ICS §14]<br />
Q. What else should I do<br />
A. Insert an NG or OG tube. Control and carefully<br />
<strong>co</strong>rrect any electrolyte or metabolic disturbances<br />
such as hypoglycaemia, hypokalaemia, or<br />
acidosis to normal if possible. [ICS §13]<br />
Q. What mode <strong>of</strong> transport should be used<br />
A. Road transport is preferable in most circumstances. Fixed<br />
wing, pressurized air <strong>transfer</strong> should be <strong>co</strong>nsidered for journeys<br />
in excess <strong>of</strong> 150 miles. The organisation headaches should not be<br />
underestimated. Heli<strong>co</strong>pter <strong>transfer</strong> is less safe and heli<strong>co</strong>pters<br />
are very harsh working environment, however they are useful for<br />
short to medium distance <strong>transfer</strong>s or where access is difficult<br />
(e.g. remote areas or traffic). [ICS §12]<br />
Q. Are there any pitfalls I should <strong>co</strong>nsider<br />
Unfortunately many, here is a selection:<br />
1. Undertreatment - it is very difficult to institute<br />
new treatment in the ambulance. If in doubt<br />
resuscitate, paralyse, ventilate.<br />
2. Redistribution <strong>of</strong> blood volume due to<br />
acceleration or up slopes causes functional<br />
hypovolaemia, with autotransfusion on braking.<br />
It is a good idea to have inotropes/pressors<br />
running even at very low dose and relative mild<br />
hypervolaemia is usually helpful.<br />
3. Monitoring is unreliable: notably NIBP and<br />
SpO2.<br />
4. The <strong>co</strong>ld. Not only do <strong>patients</strong> be<strong>co</strong>me<br />
hypothermic, but peripheral vaso<strong>co</strong>nstriction can<br />
precipitate pulmonary oedema, particularly in<br />
<strong>co</strong>mbination with stress or anxiety.<br />
5. Battery failure - many infusion pumps and<br />
monitors last 70mmHg and certainly >50mmHg. This<br />
implies a need to keep mean BP 90-100mmHg.<br />
9. Pretty obvious really - haste, poor preparation,<br />
lack <strong>of</strong> knowledge about the patient, a poor<br />
<strong>transfer</strong> plan....<br />
Equipment<br />
Portable Ventilator<br />
Must be capable <strong>of</strong> PEEP, and <strong>of</strong> delivering high<br />
inspiratory pressures<br />
Ambu bag with reservoir<br />
Waters bag<br />
Oxygen allow 10-20L/min depending on minute<br />
volume, leaks, and FiO2<br />
E 680L -> 30-60 minutes<br />
F 1360L ->1-2h<br />
G 3400L ->2-4h<br />
As a minimum, you must take enough oxygen<br />
for the expected duration <strong>of</strong> the trip, with a<br />
reserve <strong>of</strong> 100% or 1 hour, whichever is greater.<br />
Monitoring<br />
Mains and Battery powered Monitor with ECG,<br />
SpO2, NIBP, ETCO2, and at least 2 invasive<br />
channels. Leads. Battery should be fully charged<br />
Glu<strong>co</strong>meter<br />
Even for short <strong>transfer</strong>s a 12V DC to AC<br />
“invertor” (at least 400W) is a must, along with a<br />
4-6 way adaptor<br />
Syringe drivers for all infusions, with at least 1<br />
spare<br />
Airway management<br />
2 working laryngos<strong>co</strong>pes with size 3 and 4<br />
blades.<br />
Gum elastic Bougie<br />
ETT in a range <strong>of</strong> sizes (6-9)<br />
Size 6-9 Tracheostomy tubes & with obturators<br />
Size 3 and 4 LMA<br />
Guedel airways Size 2, 3 and 4<br />
Magill forceps<br />
Nasal airways<br />
Tracheostomy dilator<br />
Emergencies<br />
Scalpel<br />
2 Silk sutures (0 or greater)<br />
24, 28 and 32 Chest drains<br />
<strong>St</strong>erile scissors and Forceps<br />
20ml Lignocaine 2% with Adrenaline<br />
Cri<strong>co</strong>thyroidotomy kit<br />
Consumables<br />
Syringes 1-50ml<br />
Needles<br />
Giving sets<br />
2 Burrettes<br />
22-14G Cannulae<br />
Transducers and flush lines<br />
Fluids<br />
2-4L Colloid<br />
2-4L Hartmans<br />
2x 50ml 50% Glu<strong>co</strong>se<br />
200ml 8.4% Bicarbonate<br />
250ml 20% Mannitol<br />
References<br />
[ICS] Guidlines for the <strong>transfer</strong> <strong>of</strong> the critically<br />
ill adult. Intensive care society 2002<br />
(http://www.ics.ac.<strong>uk</strong>/icstransport2002mem.pdf)<br />
[NWLCCN-A] Network admissions policy<br />
for adult critical care services. North West<br />
London Critical Care Network 2002<br />
Drugs<br />
Take spare syringes <strong>of</strong> all infusions running<br />
Other appropriate emergency drugs are:<br />
Adrenaline 2-5 mg/50ml via CVP<br />
Noradrenaline 4mg/50ml = 80 µg/ml CVP<br />
GTN 50mg/50ml<br />
Amiodarone 300mg/50ml Dextrose CVP<br />
Labetolol 200mg/50ml<br />
Phenytoin 1g/50ml N Saline CVP<br />
Salbutamol 5mg/50ml<br />
Aminophylline 500mg/50ml<br />
Prop<strong>of</strong>ol 1% or 2%<br />
Glu<strong>co</strong>se 50%<br />
Mannitol 20%<br />
Midazolam<br />
Suxamethonium<br />
Atropine<br />
Gly<strong>co</strong>pyrrolate<br />
Calcium<br />
Metaraminol<br />
Cisatracurium<br />
Insulin<br />
At 1mg in 50ml in a 70 kg person<br />
1ml/h ≈ 0.005 µg/kg/min<br />
20ml/h ≈ 0.1 µg/kg/min<br />
Alternatively:<br />
Place Weight (kg) x 0.3 mg <strong>of</strong> drug in 50ml<br />
This means Infusion at 1ml/h=0.1 µg/kg/min<br />
Etomidate is <strong>co</strong>ntroversial. It may be better<br />
avoided because <strong>of</strong> its adverse effects on<br />
adrenal function which are harmful in critical<br />
illness, and perhaps more <strong>of</strong> a worry when<br />
aptients is to be <strong>transfer</strong>red.<br />
Etomidate should not be used in <strong>patients</strong> at<br />
risk <strong>of</strong> seizures or with neurosurgical <strong>patients</strong>.<br />
Other Tertiary referral centres<br />
Individual hospitals may have other<br />
hospitals within their own <strong>transfer</strong> groups,<br />
but this must be checked locally. Other<br />
specialist units include:<br />
Atkinson Neuro 020 8946 7711<br />
Morley<br />
Broomfield, Burns 01245 440761<br />
Chelmsford<br />
Queen Burns 01342 410 210<br />
Victoria, East<br />
Grinstead<br />
Kings Liver 020 7737 4000<br />
College Neuro<br />
Cardiac<br />
National, Neuro 0207 837 3611<br />
Queen<br />
Square<br />
Royal Free Neuro<br />
Liver<br />
020 7794 0500<br />
Royal<br />
National<br />
Orthopaedic<br />
<strong>St</strong>oke<br />
Mandeville<br />
Ortho<br />
Spinal<br />
020 8954 2300<br />
Spinal 01296 315 000<br />
North West London<br />
Critical Care Network<br />
Consistent with the best interests <strong>of</strong> individual <strong>patients</strong>,<br />
where possible <strong>transfer</strong>s should be undertaken between<br />
hospitals within the NWL Critical Care Network. Priority<br />
should be given to <strong>patients</strong> originating within the<br />
network.<br />
The following hospitals are within the North West<br />
London Critical Care Network:<br />
Hospitals Tertiary Phone<br />
Specialities<br />
Central Middlesex 020 8965 5733<br />
Charing Cross Vascular 020 8846 1234<br />
Neuro SpR 07960 937 553<br />
Chelsea and<br />
020 8746 8000<br />
Westminster<br />
Burns 020 8746 8611-2<br />
020 8237 2500<br />
Ealing 020 8574 2444<br />
Harefield<br />
Cardiac and 01895 82 37 37<br />
Thoracic<br />
Hammersmith Cardiac, Liver, 020 8383 1000<br />
Renal<br />
Hillingdon (and<br />
01895 238 282<br />
Orthopaedics at<br />
MVH)<br />
Northwick Park & GI<br />
020 8864 3232<br />
<strong>St</strong>. Marks<br />
Vascular<br />
Royal Brompton Cardiac and 0207 352 8121<br />
Thoracic<br />
<strong>St</strong>. Mary’s Cardiology<br />
Cardiothoracic,<br />
Vascular<br />
(Thoracic vascular)<br />
020 7886 6666<br />
West Middlesex 020 8560 2121<br />
Clementine Independent 020 8872 3872<br />
Churchill<br />
Cromwell (L3) Independent 020 7460 2000<br />
Harley street clinic HCA 020 7935 7700<br />
(L3)<br />
King Edward VII Independent 020 7486 4411<br />
Lister hospital HCA 020 7730 3417<br />
Portland HCA 020 7580 4400<br />
Princess Grace HCA 020 7486 1234<br />
Wellington (L3) HCA 020 7586 5959<br />
Transfers beyond your hospital’s <strong>transfer</strong> group are defined<br />
as adverse clinical events, and should be reported<br />
to the ICU director who will report it both to the Chief<br />
Executive and the critical care network.<br />
Any <strong>co</strong>mments on the design, usability or otherwise <strong>of</strong> this<br />
form, please <strong>co</strong>ntact<br />
Dr Simon Ashworth, AICU Consultant, <strong>St</strong> Marys<br />
(simon.ashworth@nhs.net)<br />
Queries regarding proto<strong>co</strong>ls should be addressed to:<br />
Dr Ganesh Suntharalingam, Consultant ITU, Northwick Park<br />
All other queries should be addressed to the Network manager<br />
Angela Walsh (angela.walsh@ealingpct.nhs.<strong>uk</strong>),<br />
c/o Ealing PCT, 1 Armstrong way, Southall, Middx, UB2<br />
4SA. Tel 020 8893 0309<br />
Any serious incident must be reported locally to the<br />
Clinical director, and details <strong>co</strong>pied to Dr Suntharalingam<br />
and Angela Walsh.<br />
Further information is available on the website:<br />
www.nwlcritcarenetwork.nhs.<strong>uk</strong>