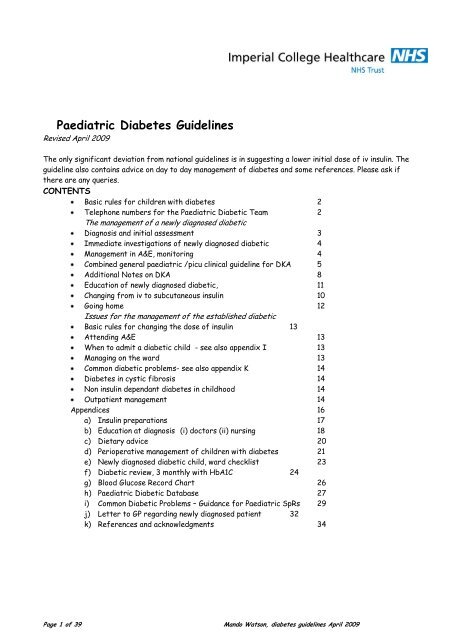
Paediatric Diabetes Guidelines - St-marys-anaesthesia.co.uk
Paediatric Diabetes Guidelines - St-marys-anaesthesia.co.uk
Paediatric Diabetes Guidelines - St-marys-anaesthesia.co.uk
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
THE MANAGEMENT OF A NEWLY DIAGNOSED DIABETICDiagnosis and initial assessmentThe diagnosis is usually obvious: Diabetics present in one of 3 ways:1- Osmotic symptoms, polyuria and polydipsia with weight loss and an elevatedblood glu<strong>co</strong>se, with glu<strong>co</strong>se and sometimes ketones in the urine.2- Diabetic Ketoacidosis (DKA). If the child has developed DKA there may besigns of dehydration, rapid respiration due to acidosis, or abdominal painThe presentation can occasionally be less clear, so check blood glu<strong>co</strong>se onchildren who are dehydrated and acidotic, or have unexplained abdominalsymptoms.3- Rarely children present with Hyperosmolar Hyperglycemic Non-Ketoticsyndrome (HHNKS)- BG > 33 mmol/L- Bicarbonate over 15 33 mmol/L- Osmolality over 320 mOsm/L- Absent or small ketonesThese children are likely to benefit from <strong>co</strong>nsiderably more fluid resuscitation,usually > 40mls/kg [Ref Canarie 2007]All new diabetic children must be seen urgently. Even children who seem well candeteriorate rapidly. Do not allow the child to sit around in A&E waiting for results ortransfer to the ward, start treatment at once.Most new diabetics are not significantly dehydrated, can tolerate oral fluids and arenot acidotic. These children do not need intravenous fluids or intravenous insulin tomanage their diabetes; they should be started on subcutaneous insulin at once. Seepages 10 and 13 for dosage information.If a child is more than 5% dehydrated, vomiting, not able to drink or clinicallyacidotic, they need iv treatment. A child with- a severe persistent acidosis- severe dehydration with shock- signs of raised intracranial pressure (ICP)- < 2 yrs- glu<strong>co</strong>se > 50with DKA should be <strong>co</strong>nsidered for admission to PICU.Page 3 of 39 Mando Watson, diabetes guidelines April 2009
Immediate investigations of all newly diagnosed diabeticWeigh the child or reliablyestimate a weightBlood glu<strong>co</strong>se- check withbedside meter and also send tolabU and E’sBone profileBlood gasesFBC and PCVHbA1CHb ElectrophoresisIslet Cell AntibodiesAnti GAD antibodiesThyroid functionThyroid antibodiesCoeliac screenMSU for dipstick and M,C and SFurther assessments to <strong>co</strong>nsider e.g. for those presenting with DKA or HHNKSBlood cultureCRP, if indicatedComplete infection screen,Calculate serum osmolality (see page 5 or 8)Most of these tests are on the Webpas order set named PNDB and apply to newlydiagnosed diabetics.Management in A&ENon-DKA Patients able to tolerate food and drinkTalk to the parents informing them of the diagnosesTalk to a member of the diabetes Home Care Team to plan management (seepage 2 for <strong>co</strong>ntact details)If blood sugars > 15mmol/l give a stat dose of 0.25 units/kg of Rapid Insulin(Humalog or Novorapid) SC.Arrange admission to the ward (some may not need admission)Monitor the blood sugars hourly while waiting to be admitted.Page 4 of 39 Mando Watson, diabetes guidelines April 2009
Diabetic KetoacidosisCOMBINED GENERAL PAEDIATRIC /PICU CLINICAL GUIDELINE1. AssessmentDiagnosis requires a <strong>co</strong>mbination of hyperglycaemia, acidosis and ketones.If all features not present <strong>co</strong>nsider alternative diagnoses: Hyperosmolar HyperglycemicNon-Ketotic syndrome (HHNKS), lactic acidosis, al<strong>co</strong>holic ketoacidosis, salicylateoverdose, inborn error of metabolism and sepsis.If diagnosis <strong>co</strong>nfirmed ask about:HistoryooNew presentation or acute on chronic?Usual insulin requirement if acute on chroni<strong>co</strong> Precipitating cause – focus of sepsis?Clinicalo Degree of dehydration (assume maximum of 10%)5% Dry mu<strong>co</strong>us membranes7.5% Sunken eyes, poor capillary refill time10% Poor perfusion, thready rapid pulseo Conscious levelRe<strong>co</strong>rd glasgow <strong>co</strong>ma s<strong>co</strong>reInstitute hourly neuro obsIf <strong>co</strong>matose <strong>co</strong>nsider instituting cerebral oedema management (see below)o Signs of cerebral oedemaHeadache, irritability, slow pulse, hypertension, reduced <strong>co</strong>nscious level,papilloedemao Abdominal pain/vomitingLaboratoryoBlood glu<strong>co</strong>se, U&E, blood gas, urine ketones, septic screen and calculate osmolality and<strong>co</strong>rrected sodium• Serum osmolality (mOsm/L) = [2 x (Na + K)] + blood glu<strong>co</strong>se + urea• Corrected Na = Measured Na + [1.6 x (blood glu<strong>co</strong>se- 5.5)/5.5]Commonest cause of mortality is:• Cerebral oedema. Risk factors include:o Bicarbonate administrationo Severe hypocapnoea at presentation (
2.1.15 Discuss with Dr Wassouf/Dr Watson as early as possible for family support andeducation.2.1.16 Consider Heparinisation when central Line is required in severe DKA (seeseparate <strong>Guidelines</strong> for this, discuss with the Haematologist)2.2 Cerebral oedema2.2.1 If signs of cerebral oedema present (see above) inform senior staff immediately2.2.2 Exclude hypoglycaemia2.2.3 Give mannitol 0.25 – 1 g/kg stat (discuss dose with PICU <strong>co</strong>nsultant on service) or3% sodium chloride 3mls/kg over 20 minutes as soon as warning signs occur.2.2.4 Restrict iv fluids to 2/3 maintenance2.2.5 Consider intubation and ventilation – discuss with PICU <strong>co</strong>nsultant prior tointubation2.2.6 Exclude other diagnosis (thrombosis, haemorrhage, infarction) by CT scan2.2.7 Repeat mannitol within 2h if no responseConsider transferring child to PICU ifo Persistent severe acidosiso Severe dehydration with shocko Signs of raised intracranial pressure (ICP)o < 2 yrso Glu<strong>co</strong>se > 503. Indications for intubation3.1 Tiring from tachypnoea3.2 Signs of raised ICP – discuss with PICU <strong>co</strong>nsultant prior to intubation4. Management post intubationIntubation and artificial respiration risks worsening of acidosis. If assisted ventilation isrequired, PaCO 2 goal should be that which the patient was achieving prior to intubation.Follow with end tidal CO 2 . Paralyse and sedate in order to facilitate ventilation strategy.4.1 Obtain central venous and arterial access.4.2 Use inotropes to maintain cerebral perfusion pressure if necessary.5. ReferencesDunger DB et al; European Society for <strong>Paediatric</strong> Endocrinology; Lawson WilkinsPediatric Endocrine Society. European Society for <strong>Paediatric</strong> Endocrinology/LawsonWilkins Pediatric Endocrine Society <strong>co</strong>nsensus statement on diabetic ketoacidosis inchildren and adolescents. Pediatrics. 2004;113:e133-40.6. SurveyIn 2008/2009 we are <strong>co</strong>nducting a survey of patients with diabetes admitted to PICU.Please ensure your patient is included in this study (discuss with on call <strong>co</strong>nsultant or DrNelly Ninis)Page 3 of 3PICU Clinical Guideline, Diabetic KetoacidosisPage 7 of 39 Mando Watson, diabetes guidelines April 2009
THE MANAGEMENT OF A NEWLY DIAGNOSED DIABETIC <strong>co</strong>ntinuedAdditional Notes on DKAThe risks of diabetic ketoacidosisIn the UK a number of children with DKA still die each year. Deaths are mainly due tocerebral oedema. Other causes of death are sepsis, shock and hypokalaemia.Sodium and osmolalityTotal body sodium is depleted in DKA. In addition the elevated osmolality inhyperglycaemia results in a dilutional effect on the measured sodium (ie the measuredsodium is falsely low because of the very high glu<strong>co</strong>se). “Corrected” sodium can becalculated as:Corrected Na = Measured Na + [1.6 x (blood glu<strong>co</strong>se- 5.5)/5.5] [ref. Krane 1987]If <strong>co</strong>rrected serum sodium is over 150mmol/l initially, <strong>co</strong>nsider an even slowerrehydration, as the risk of cerebral oedema in these children is higherThe measured serum sodium should rise as the glu<strong>co</strong>se falls. A falling serum sodiumwith rehydration has been linked in a number of studies to impending cerebraloedema. If serum sodium fails to rise or falls, <strong>co</strong>nsider increasing the sodium <strong>co</strong>ntentof the fluid, and monitor with increased vigilance for signs of cerebral oedema.Serum Osmolality should always be calculated in DKA. Repeated calculation should beused as a guide to the fluid management. Serum osmolality should fall by no more than3mOsm/hour. Serum osmolality can be measured directly or calculated-Serum osmolality (mOsm/L) = [2 x (Na + K)] + blood glu<strong>co</strong>se + urea [ref. Krane 1987]Cerebral oedemaOccurs in 0.4-1% of all children with DKA and carries a high mortality. The cause isunknown. Cerebral oedema is more <strong>co</strong>mmon in younger children and those withgreater metabolic upset, and <strong>co</strong>mmonly happens in the first 24 hours of rehydration.Retrospective studies looking for the cause of cerebral oedema have found anassociation with the use of large volumes of fluid at resuscitation and with rapidmetabolic <strong>co</strong>rrection It has also been suggested that very careful monitoring withprompt treatment of warning signs may be as important as the resuscitation proto<strong>co</strong>litself. If cerebral oedema is suspected, urgent assessment by senior paediatric staffand senior anaesthetist is required. Involve PICU if they are not already involved.Page 8 of 39 Mando Watson, diabetes guidelines April 2009
Notes on running an iv insulin infusionRemember the cells of the body are relatively starved in DKA- when you adddextrose to the iv fluids, this will help to <strong>co</strong>rrect the metabolic problems.Do not write up a sliding scale plan – Always start a fixed dose as part of theagreed regimen and go back for regular reviews adjusting the dose.The blood glu<strong>co</strong>se may fall with fluid administration but insulin is required for<strong>co</strong>rrection of the metabolic defect, so set up an insulin infusion as soon as possible.The dose of insulin needed to maintain normoglycaemia is very variable. A safestrategy is to start with a low dose and monitor the blood glu<strong>co</strong>se every half hourat first, adjusting as necessaryAdjusting insulin infusion doses: Look at the change in blood glu<strong>co</strong>se, and if thelevel is falling rapidly reduce the rate of infusion even if the glu<strong>co</strong>se is high. If theglu<strong>co</strong>se is high do not immediately turn the rate up to maximum, but try a smallincrease with the idea of achieving a slow fall.If glu<strong>co</strong>se falls to < 6 mmol/L, <strong>co</strong>nsider increasing to 10% glu<strong>co</strong>se or stoppinginsulin.If you stop insulin, remember the half-life is very short and do not let the glu<strong>co</strong>serise too high before you restart.MonitoringCommon sense must be used about the degree of monitoring- avoid intrusivemonitoring and frequent blood tests in well children. Clarify the monitoringrequired with the diabetic team. This will range from hourly TPR & BP, neuro obs,<strong>co</strong>ntinuous cardiac monitoring and fluid balance chart to twice daily TPR.Glu<strong>co</strong>se testing can be done with a bedside meter- check frequently (every30mins) as you start insulin and then hourly. By the time of discharge, childrenwill be testing just 4 times a day: pre main meal and pre bed (and if feelinghypoglycaemic)Check U and E’s and blood gas at 2 hourly intervals until the child is stable andthen 4 hourly.Education of new diabeticsThis process begins from the moment of arrival in A&E. Parents and patientsremember very well the day they presented with diabetes. Keep initial informationsimple. Dr Watson or Dr Wassouf will meet with the family early in the admission andwill spend time answering detailed questions. See appendix B for details of the topicsthat will be <strong>co</strong>vered.Page 9 of 39 Mando Watson, diabetes guidelines April 2009
e started in the morning with breakfastThe Basal Bolus (QDS) regime <strong>co</strong>nsists ofo approximately 40-50% of the total daily dose is given as long actinginsulin (usually Glargine)o 10-20% of the total daily dose is given with each main meal.Glargine is given before bed and the dose should be adjusted ac<strong>co</strong>rding to fastingblood sugars in the morning. The aim for this is to be between 4-7.All new rapid insulin should be given immediately before starting the meal.Glargine may be given without a meal any time during the day, but best before bed.If the BD regime is thought to be appropriate for the child then Biphasic insulin(Novorapid30 or humalog mix 25) is used. 2/3 of the total daily dose is given in themorning with breakfast and 1/3 in the evening with dinner.A snack between main meals is only required when biphasic insulin is used.the aim is to get the child out of hospital as soon as possible on subcutaneousinsulin and not to achieve perfect <strong>co</strong>ntrol.aim for a normal pattern of eating and activity.Do not try to <strong>co</strong>ntrol high blood glu<strong>co</strong>se levels by withholding meals or snacks ormaking the child do extra exercise.Children may be much more active at home so tight <strong>co</strong>ntrol on the ward may meanhypoglycaemia as soon as they get home.always make sure that the insulin dose is written up in advance. Asking to be calledwhen it is due results in delays, which make <strong>co</strong>ntrol more difficult.do not write up extra doses of insulin for high blood sugars- this will only delaydischarge because it be<strong>co</strong>mes difficult to decide on the <strong>co</strong>rrect regular insulindose, and runs the risk of inducing hypoglycaemia.Daily food and insulin routine for diabetic on twice daily insulin(mixed) insulin - usually Novomix 30 - 7.00 to 8.00 am, immediately before breakfast (if using Humalog Mix 25 or Novomix 30,or 20 minutes later if using older insulins)mid morning snacklunchafternoon snack(mixed) insulin - usually Novomix 30 - before evening meal (same interval between injection and food as for breakfast)evening mealsnack before going to bedDaily food and insulin routine for diabetic on three times daily insulin(mixed)insulin - usually Novomix 30 - 7.00 to 8.00 am, breakfast immediately aftermid morning snacklunchafternoon snack sometimes needed(short acting) insulin - usually Novorapid - immediately before evening mealnight time (long acting) insulin - usually glargine (Lantus) – before bed (which is given at a regular time each day, within a 2 hourtime frame)Page 11 of 39 Mando Watson, diabetes guidelines April 2009
Daily food and insulin routine for diabetic on four times daily insulin(short acting) insulin - usually Novorapid - 7.00 to 8.00 am, breakfast immediately after(short acting) insulin - usually Novorapid - immediately before lunch(short acting) insulin - usually Novorapid - immediately before evening mealnight time (long acting) insulin - usually glargine (Lantus) – before bed (see <strong>co</strong>mment above).Writing up insulinWrite clearly and write “units” as a word. Do not alter prescriptions if you changethe dose and make it clear when you want it given (eg “before breakfast” ). You needto specify what kind of insulin (type, type of mixture), the cartridge size (if relevant)and type of pen. Avoid changing between makes of insulin and also check that whatyou write is stocked in the pharmacy. See also appendices A and J.Going homePatients and families require a lot of education and equipment prior to discharge.Please refer to the checklist, appendix E.Discharge planningThis should be done in <strong>co</strong>njunction with Samir Wassouf, Jan Reddick, and MandoWatson. If the patient is to be discharged to the care of another diabetic team, e.g.for patients who live out of area, then close liaison with the receiving team is needed.See appendices E and J for further information on TTAs and a standard GP letterthat will need to be sent at discharge.Page 12 of 39 Mando Watson, diabetes guidelines April 2009
ISSUES FOR THE MANAGEMENT OF THE ESTABLISHED DIABETICBasic rules for changing the dose of insulinYou rarely need to make changes as an emergency or out of hoursOnly change when there is a genuine trend in glu<strong>co</strong>se over 3 days or moreMake one change at a time and wait before changing againGo in small steps (1 unit or 2 in older children) at a timeA prepubertal child will need about 0.5 – 1 units/kg/day to <strong>co</strong>ntrol his/herdiabetes. This may go up to over 1 unit/kg/day during puberty, although there is alot of individual variation.On the flexible regimens you are able to change to balance of long and short actingas well as the amount.Attending A&EThe whole idea of diabetes care is to keep the patients out of hospital- so do not tellparents to bring their child to casualty unless you really are going to dosomething, or they request it. They can read out the blood glu<strong>co</strong>se re<strong>co</strong>rd over thephone. You do not need to do a venous blood glu<strong>co</strong>se or U and E's unless you think youare going to put up a drip.When to admit a diabetic child - see also appendix IA diabetic child should be admitted ifnot tolerating oral fluidssignificantly dehydrated, acidotic or septicin some cases for a severe hypoglycaemic attack.Your threshold for admitting the younger ones should be lower. Terrible bloodglu<strong>co</strong>ses and poor <strong>co</strong>ntrol are not reasons to admit on their own, neither is failure todo any blood glu<strong>co</strong>se tests. Do not admit as an emergency to monitor blood glu<strong>co</strong>se, tostabilise <strong>co</strong>ntrol or to observe. Major psychological problems may precipitateadmission- usually the need is fairly obvious.Managing on the wardManage without a drip if you can. If you put up a drip for iv fluids, it may make senseto use an iv insulin infusion, but remember that there may be some long acting insulinaround from the last injection. Use the guideline for diabetic ketoacidosis for knowndiabetics as well as for new ones.Page 13 of 39 Mando Watson, diabetes guidelines April 2009
Common diabetic problems- see appendix K<strong>Diabetes</strong> in cystic fibrosisThese patients have a kind of diabetes which is in between Type 1 and Type 2. Mostare managed on insulin, but their requirements may be different. Some only needinsulin to <strong>co</strong>ver food and are able to maintain a “background” of insulin secretion.<strong>Diabetes</strong> must be managed to maintain optimum nutrition- these patients are notgiven the same advice about diet as ordinary Type 1 diabetics.Non insulin dependant diabetes in childhoodThere are a number of very rare types of inherited diabetes- among these so called“maturity onset diabetes of the young” or MODY, which are defects in the insulinsecretion mechanism. These individuals are distinct from the increasing number ofadolescents who present with Type 2 diabetes. In these individuals obesity is themost significant factor although there is usually a strong family history. ConsiderType 2 diabetes if there is obesity, a family history of Type 2, acanthosis nigricansor a very gradual onset without ketoacidosis.Outpatient managementClinicsThe majority of support is provided to patients in the family home, with home visits.Children and families are seen on a Friday afternoons on the 6 th floor for paediatricpatients, and on Wednesday afternoons in Mint Wing for Young Adults (usually from13 years).Each visit: height, weight, BP, urine dipstick, HbA1CAnnually: thyroid function, <strong>co</strong>eliac screen and lipidsAnnually in those over 12 : eye check, urine albumin creatinine ratioHome monitoringTelephone <strong>co</strong>ntact by <strong>Paediatric</strong> Home Care takes place as often as required –sometimes daily. <strong>Paediatric</strong> Home Care keeps the blood glu<strong>co</strong>se re<strong>co</strong>rd. See appendixG.The HbA1c is measured every 3-4 months, at the same time as a <strong>co</strong>mprehensivereview. See attached review sheet, appendix F.Page 14 of 39 Mando Watson, diabetes guidelines April 2009
Aims of outpatient monitoringTight <strong>co</strong>ntrol (as measured by HbA1c) in postpubertal individuals is related toreduced rate of onset of <strong>co</strong>mplications, and reduced progression of established<strong>co</strong>mplications. The situation in children is less clear but tighter <strong>co</strong>ntrol reduces thechances of <strong>co</strong>mplications.In children there are other issues as well as achieving tight diabetic <strong>co</strong>ntrol;Avoiding damaging hypos particularly in the very youngThe ability of the family to deal with the diabetesEducationNormal psychological developmentDeveloping independenceRigid diabetic <strong>co</strong>ntrol throughout childhood is of no use if this means that the childrebels as an adolescent and never attends clinic or does a blood test again.Page 15 of 39 Mando Watson, diabetes guidelines April 2009
Appendicesa) Insulin preparationsb) Education at diagnosisc) Dietary adviced) Perioperative management of children with diabetese) Newly diagnosed diabetic child, ward checklistf) Diabetic review, 3 monthly with HbA1Cg) Blood Glu<strong>co</strong>se Re<strong>co</strong>rd Charth) <strong>Paediatric</strong> Diabetic Databasei) Common Diabetic Problems – Guidance for <strong>Paediatric</strong> SpRsj) Letter to GP regarding newly dignosed patientk) References and acknowledgmentsPage 16 of 39 Mando Watson, diabetes guidelines April 2009
Appendix AInsulin Preparations We use at <strong>St</strong> Mary’sname of insulin Name of favoured pen proportion short and long actingShort acting% short % long.NovoRapid C,P,V (insulin aspart) Novopen 3 or Flexpen 100 0Humalog C,P,V (insulin lispro),P via Humalog PenHumaPen Ergo 100 0Actrapid v For IV use only 100 0Very Long acting (up to 24hours)Lantus C,,V,P (Insulin Glargine) autopen 24 or Solostar 100Levemir C,P (Insulin Detemir) Novopen 3 or Flexpen 100Mixed (Rapid and intermediate) %rapid %intermediateNovomix 30 C,P,V (BiphasicInsulin Aspart)P via FlexpenHumalog Mix 25 C,P,V(biphasic insulin Lispro)Novopen 3 or Flexpen 30 70HumaPen Ergo 25 75Bold indicates the insulins most used by our service and are stocked on Great Western Ward.The pens which we favour are also in bold and are supplied by the <strong>Paediatric</strong> Home Care Team.V= available in vialC = available in cartridgeP = available in preloaded (disposable) penPage 17 of 39 Mando Watson, diabetes guidelines April 2009
Appendix B (i)Education at diagnosisThese topics are <strong>co</strong>vered by senior doctors in discussion with parents whenever a child is newlydiagnosed with diabetes. The list can be printed off and filed in the notes to document the discussion.1. how diagnosis made, reason for symptoms2. uncertain cause for DM, no blame3. need immediate insulin, how it works4. what is glu<strong>co</strong>se, normal BG, glu<strong>co</strong>se targets5. injecting, blood & urine testing, reasons for monitoring6. basic dietetic advice7. explain hypo, glu<strong>co</strong>se always available8. during illness; do not omit insulin9. home/school; effects of exercise10. alert bracelets etc11. diabetic help groups etc12. psychological adjustment13. emergency phone numbersPage 18 of 39 Mando Watson, diabetes guidelines April 2009
Appendix B (ii)Checklist for Newly Diagnosed Diabetic – NursesNAMEDOB:HOSP NO:1. Explanations of the following:2. What is diabetes?3. Diabetic diet (dietician)4. Possible causes and symptoms of hypoglycaemia5. Management of hypoglycaemia (dietary, hypostop + glucagon)6. Signs and symptoms of hyperglycaemia (DKA)7. Management of hyperglycaemia8. How to use blood glu<strong>co</strong>se monitor9. How and when to test urine for ketones10. How to use insulin pen11. Use of NovoRapid or Humalog12. Types and storage of insulin13. How to rotate injections sites14. How to dispose of sharps safely15. How to use re<strong>co</strong>rd book (diary)16. <strong>Paediatric</strong> <strong>Diabetes</strong> Home Care Team and how to use it17. Support group information – JDF + <strong>Diabetes</strong> UK18. Relevant Literature – list in evaluation19. Medic alert system20. Disability Living Allowance information21. Ensure that family have PDHCT numbers and 1202 bleep22. Letter to G.P. re: supplies23. Contact with School/Nursery School/ Nursery Talk givenPage 19 of 39 Mando Watson, diabetes guidelines April 2009
Appendix CDietary Advice for Newly Diagnosed Diabetic Children1. Have regular meals to keep blood sugars stable. NEVER miss a meal.2. Choose low sugar, sugar free, or reduced sugar products, e.g. diet fizzy drinks,plain biscuits, low sugar squash, plain cereals, and artificial sweeteners toreplace sugar.Remember, if the label says “no added sugar”, the product may still <strong>co</strong>ntainsugar3. Have a starchy food at every meal or snacke.g. bread, rice, pasta, potato or breakfast cereal4. You may need to take a snack mid-morning and mid-afternoon and before bedto keep your blood glu<strong>co</strong>se stable. e.g. banana, teacake, sandwich or 2 plainbiscuits5. NEVER eat sweet foods on an empty stomach (except during a hypo) e.g. youmay occasionally have a small bowl of ice cream after a main meal.6. All fruits are good but should be <strong>co</strong>nsumed in moderate quantities due to theirnatural sugar <strong>co</strong>ntent. Have up to three fruits a day – 1 at a time and spread out overa day7. If your blood sugars are low this is called HYPOGLYCAEMIA. You mayexperience a few symptoms (sweaty, dizzy, loss of <strong>co</strong>ncentration, nausea)1. Take a fast acting sugare.g. 2 dextrose / Lu<strong>co</strong>zade tabletsor sugary drink (Cola, lu<strong>co</strong>zade)(try not to use sweets or cho<strong>co</strong>lates)followed by2. A long acting sugar e.g. a sandwich, toast or a main mealThe <strong>Paediatric</strong> Dietitian will see you before you go home to answer any questionsyou may have and provide more detailed information on your dietPage 20 of 39 Mando Watson, diabetes guidelines April 2009
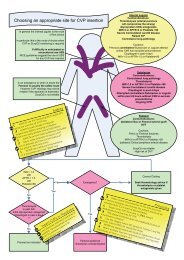
Appendix DPeri operative management of children with diabetesA <strong>co</strong>py of this document should be in the hospital notes and a <strong>co</strong>py given to the familyRegardless whether the child is on biphasic BD injections, the semi flexible regime, or the basal bolusregime, there are two options:The Subcutaneous Regime (SC) is used when the operation is first on the list in the morning, is brief andthe child is likely to be re<strong>co</strong>vered and having breakfast by lunch time.The Infusion Regime is used for long operations, where there will be prolonged post operative fasting,for sick children and when patients have difficult to <strong>co</strong>ntrol diabetes.Many specialists care for children with diabetes. In order to streamline care, the following managementplan has been agreed:The patient will be put first on the list if possible.Fasting time is kept to a minimum. Clear fluids 2 hours, breast milk 4 hours, other milk & solids 6hours.Name of ChildType of OperationDate of OperationFor this case, fasting time will beas decided by:For this case, the Subcutaneous Regime/Infusion Regime is planned.As decided by:If the SC Regime is planned:Give the usual insulin the evening before the operationThe child may be admitted on the morning of the operationDo not give the morning dose of insulin pre opOnly put in a cannula if possible with minimal traumaCheck the blood glu<strong>co</strong>se hourly from the start of the fast until the child can drink normally. Theglu<strong>co</strong>se will probably rise gradually and this is acceptablePost op insulino If the child is on BD injections, and if the child is fully re<strong>co</strong>vered, back on the wardbefore 10:30 and able to have breakfast, the usual morning dose of biphasic insulin maybe given with breakfasto otherwise, irrespective of usual regimen, give a bolus of rapid Insulin sc (Novorapid) withthe next meal after re<strong>co</strong>very, based on 1 unit of Insulin for each 10 grams ofcarbohydrate <strong>co</strong>nsumed.Peri operative management of children with diabetes page 1 of 2Page 21 of 39 Mando Watson, diabetes guidelines April 2009
The aim is not perfect <strong>co</strong>ntrol but safety, and allowing the blood glu<strong>co</strong>se to run at 10-12 makessudden hypoglycaemia unlikelyIf the glu<strong>co</strong>se level be<strong>co</strong>mes very high, (using > 20 mmol/L as a rough guide), give a bolus of scinsulinIf the glu<strong>co</strong>se level falls, (using < 5 mmol/L as a rough guide), put up iv dextroseGo back to the normal insulin regimen in the evening providing the child is able to eat and drink.Replace carbohydrate intake with sweet drinks if the child is not eating well.If the Infusion Regime is planned:The patient must be admitted at least the evening before surgery.An iv cannula is sited the evening before surgery. Diabetic children are reliant on daily bloodglu<strong>co</strong>se measurements and insulin injections. To minimise needle phobia, an iv cannula will be put inby the most experienced clinician available.<strong>St</strong>abilising a child on an insulin infusion may take a long time; allow several hours or evenovernight to settle things.Insulin infusion: 50 units (0.5mls) diluted to 50 mls normal saline in a syringe (1 unit/ml), run at0.05 units /kg/hour to start and adjust ac<strong>co</strong>rding to ½ hourly blood glu<strong>co</strong>se.Maintenance fluids (5% dextrose or dextrose 5%/saline 0.45% with maintenance potassium 10 or20 mmol per 500mls) and insulin run into the same line using a one way valveThe aim is not perfect <strong>co</strong>ntrol but safety, and allowing the blood glu<strong>co</strong>se to run at 10-12 makessudden hypoglycaemia unlikely.Do not manage high blood glu<strong>co</strong>se measurements with boluses of iv or s/c soluble insulin. Do notuse a “sliding scale” of s/c soluble insulin.Check the blood glu<strong>co</strong>se hourly if child is stable, until the child can drink normally.Check U and E’s at least 4 hourly, while on insulin infusion (after the surgery)Restart normal insulin when drinking normallyGo back to the normal insulin regimen as soon as the child can drink. Replace carbohydrate intakewith sweet drinks if needed. Get back onto the normal insulin regimen as soon as possible even ifthis means allowing the blood glu<strong>co</strong>se to run high.For advice at any time, please <strong>co</strong>ntact the paediatric diabetic team: Samir Wassouf, x 6292 or 6482 orpager Mando Watson, x 6905 or mobile, Jan Reddick, x 1315 or mobile 07876 257560.Produced by Dr M Watson, Consultant <strong>Paediatric</strong>ian, In association with, Dr S Gautama, Consultant <strong>Paediatric</strong> Anaesthetist, Dr SWassouf, <strong>Paediatric</strong>ian, Mr Madden, Consultant <strong>Paediatric</strong> Surgeon, Helen Braggins, Senior <strong>Paediatric</strong> Nurse, Julia Simmons,<strong>Paediatric</strong> Pharmacist, Katie Elwig, <strong>Paediatric</strong> Dietician, Mandy Green, CCNPeri operative management of children with diabetes page 2 of 2Page 22 of 39 Mando Watson, diabetes guidelines April 2009
Appendix ENEWLY DIAGNOSED DIABETIC CHILD, WARD CHECKLISTChild and family will have the following explained to them during their stay:What is <strong>Diabetes</strong>? - Doctor.Diabetic Diet - dietician.How to give insulin injection – ward and specialist nurseMonitoring - blood glu<strong>co</strong>se and urine testing – ward and specialist nurseHypoglycaemia – symptoms and management - allInsulin treatment and regimen - allJan Reddick or Samir Wassouf will provide:Needles for the insulin pensGlu<strong>co</strong>se monitor and stripsFinger pricking device and lancetsSharps bin (on discharge)Information leaflets/bookletsRe<strong>co</strong>rd diaryID bracelet information – eg: medicalert<strong>Diabetes</strong> UK and/or JDRF informationPHCT <strong>co</strong>ntact numbers and 1202 bleepGlu<strong>co</strong>se tabletsThe following should be prescribed as TTAs:Regular Insulin - choice will vary but is usually Novorapid and Lantus cartridges. The <strong>Paediatric</strong>Home Care Team for <strong>Diabetes</strong> or GP will provide the ac<strong>co</strong>mpanying Novopen 3 and Autopen 24.1 x GlucaGen Kit 1 mg injectionAnd the standard letter (appendix J) should be sent to the GPPlease ensure that Samir Wassouf and Jan Reddick are informed as soon as possibleafter admission so that we can liaise with you as needed, to ensure early planneddischarge. Dr Wassouf x 6482 (answerphone) or x 6292, fax x 6219. Jan Reddick x1315 or 07876 257560.Page 23 of 39 Mando Watson, diabetes guidelines April 2009
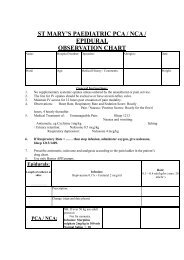
Appendix FPAEDIATRIC DIABETES HOME CARE TEAMST MARY’S HOSPITALPATIENT DIABETES REVIEW RECORDSurname: Forename: Date of Birth:Date of Review:Current Insulin Regime:Undertaken By: (Sign and PrintName)Injection Sites:Date Next Review Due:Pre Breakfast:Pre Lunch:Checked: Yes/NoReason if No:Pre Dinner:Pre Bed:Arms: Yes/NoLegs: Yes/NoOk/Avoid:Ok/Avoid:Changes to Insulin Regime: Yes/NoAbdomen: Yes/No Ok/AvoidChanges made:Buttocks: Yes/NoOk/AvoidInsulin Expiry:Novorapid/ Humalog present foremergency:Yes/No Expiry Date:Calves: Yes/No Ok/AvoidNeedle size: 5mm/6mm/8mm/12mmCorrect: Yes/ NoComments:Blood Glu<strong>co</strong>se Range:Severe Hypo’s: Yes/ NoAmount:Admission:DKA: Yes/NoAmount:Admission:Previous HBA1C:Current HBA1CEquipment Present:Blood Glu<strong>co</strong>se <strong>St</strong>rips: Yes/No Expiry:Blood/ Urine Ketone <strong>St</strong>rips: Yes/No Expiry:Sharps Bin: Yes/ NoHypostop: Yes/NoGlucagon: Yes/NoExpiry:Expiry:Current Blood Glu<strong>co</strong>se Meter: CheckedYes/NoPage 24 of 39 Mando Watson, diabetes guidelines April 2009
Diet Review:Breakfast:Lunch:Dinner:Snacks:Other Checks:Referrals Needed Yes/NoDr M Watson/ Dr S Wassouf: Yes/NoReferral date:Reason:Dietician (Mae Said): Yes/NoReferral date:Reason:Mental Health Liaison Nurse (Jo Squires):Yes/NoReferral date:Reason:Patient Issues:Last Ophthalmic Review:Last Dentist Review:Last Podiatrist review:<strong>Diabetes</strong> Management Plan:Page 25 of 39 Mando Watson, diabetes guidelines April 2009
PreBreakfastPre LunchPre DinnerPre BedOtherPreBreakfast2hrs PostPre Lunch2hrs PostPre dinner2hrs PostPre Bed2hrs PostDuringNightAppendix GPAEDIATRIC DIABETES HOME CARE TEAMST MARY’S HOSPITALBLOOD GLUCOSE RECORD SHEETNR = NovorapidG = GlargineD = LevimerNM = Novomix 30HL = HumalogHM = HumamixINSULIN DOSAGE AND TYPE(CODE ABOVE)NAME:HOSP NO:BLOOD GLUCOSE READINGS (MMOLS/L)DATECommentsPage 26 of 39 Mando Watson, diabetes guidelines April 2009
Appendix H<strong>Paediatric</strong> <strong>Diabetes</strong> DatabaseThe following data are kept within <strong>Paediatric</strong> Home Care, for Diabetic children cared for by the <strong>Paediatric</strong> Home Care Team.<strong>St</strong> Mary's Hospital <strong>Paediatric</strong> Diabetic Service Data SheetSURNAME: …… HOSPITAL NO: …..FIRST NAME: ….. ETHNIC ORIGINDATE OF BIRTH:DATE OF DIAGNOSIS:NAMED NURSE:MODE OF PRESENTATION:e.g. osmotic symptoms, ketoacidosisWeightevery 3 months in infants or where weight is a problem (& height when available)Date Wt (kg) Ht (cm) Date Wt (kg) Ht (cm) Date Wt (kg) Ht (cm)HbA1C at least every 3 months, (optimum < 7.6) At diagnosis:Date Result (%) Date Result (%) Date Result (%)% % % %% % % %% % % %<strong>Paediatric</strong> Clinic visitsenter dates attendedyoung adult clinic visitsenter dates attendedward admissions date brief summaryother informationPage 27 of 39 Mando Watson, diabetes guidelines April 2009
PAGE 2SURNAME: …… FIRST NAME: ….. HOSP NO:Islet cell antibodiesdate/resultThyroid antibodiesdate/resultmeasure just once, soon after diagnosismeasure just once, soon after diagnosisThyroid functionmeasure annually, (normal free T4 10.5 -22.7 pmol/L, TSH 0.35 - 5.5 mU/L)Date fT4 (pmol/L) TSH (mU/L ) Date fT4 (pmol/L) TSH (mU/L ) Date fT4 (pmol/L) TSH (mU/L )Coeliac antibodiesmeasure annually (normal antigliadin IgG
Appendix I Common Problems with diabetics - Guidance for <strong>Paediatric</strong> SpRs.HyperglycemiaOnly rapid insulin should be given for extra bolusesIf Blood sugar is >15 mmol/l, the child is well, there are no ketones in the urine andthe last insulin dose was given at least 3 hours earlier, an extra dose of 50% of theprevious dose taken may be given.If an insulin dose has been omitted, the whole dose should be given as soon as it isrealised, up to 2 hours after eating. Blood sugars then should be observed hourlyuntil the next dose is due which should not be given at least for 4 hours regardlessof its nature (rapid or biphasic)If an insulin dose was missed and was dis<strong>co</strong>vered only an hour or two before thenext dose is due, then extra rapid insulin may be given with the next dose up to50% of the missed dose depending how high the blood sugar is.If high blood sugar is due to a treated episode of hypoglycemia then no extrainsulin should be given until the next dose is due.Hyperglycemia with illnessMore frequent blood sugars are essential during illnessThe basal bolus regime is ideal for diabetics during illness. If the child is on thetds regime simply switch to basal bolus keeping the basal insulin at the same doseand adjusting the rapid insulin ac<strong>co</strong>rding to blood sugar values and intake ofcarbohydratesIf the child is not tolerating drinks, and is developing ketonuria, ask the family toattend A&E.Errors in insulin dosageIf an in<strong>co</strong>rrect dose of insulin was given (too much or too little) monitor blood sugarand act ac<strong>co</strong>rdingly. Remember:Rapid insulin action persists for 3-4 hoursBiphasic insulin action persists for 8-12 hoursHypoglycemia Blood glu<strong>co</strong>se < 4 mmol/lIf the child is <strong>co</strong>nscious advise that he/she should be given 3 glu<strong>co</strong>se tablets (or150mls sugary drink) followed by a snack e.g. sandwich or biscuits. It is good andsafe practice to <strong>co</strong>mbine simple and <strong>co</strong>mplex carbohydrate in the treatment ofHypos.If the child is un<strong>co</strong>operative, but has a normal level of <strong>co</strong>nsciousness, Glu<strong>co</strong>gel(Hypostop) may be applied to the inside of the mouth, between the cheeks andgums. Once the child started to <strong>co</strong>operate, then a snack should be givenPage 29 of 39 Mando Watson, diabetes guidelines April 2009
If the child is un<strong>co</strong>nscious or fitting, IM Glucagon, (the emergency injection in anorange box kept at home) can be administered by the parents, and an ambulancecalled.Dose of glucagon (im, or sc): 1 month to 4 years 500 micrograms; over 5 years 500micrograms- 1mg.In A&E for an un<strong>co</strong>nscious or fitting childo give glu<strong>co</strong>se - 2ml/kg of 10% glu<strong>co</strong>se given slowly (10 minutes) then setup maintenance fluids and monitor the blood glu<strong>co</strong>se.o use glucagon if there is no iv access and the child is un<strong>co</strong>nsciouso Once the blood glu<strong>co</strong>se is normal there is no benefit in giving moreboluses of glu<strong>co</strong>se, just maintain it in the normal range. Glu<strong>co</strong>se takestime to diffuse into the cells.o <strong>co</strong>nsider other causes of un<strong>co</strong>nsciousness if the child does not wake upo There have been deaths related to the use of high <strong>co</strong>ncentration glu<strong>co</strong>sesolution. 50% glu<strong>co</strong>se is not dangerous of itself, but when a child remainsun<strong>co</strong>nscious the temptation is to give more and the deaths have beenrelated to hyperosmolar <strong>co</strong>ma. This is remarkably easy to do in anemergency and is the reason for using 10% glu<strong>co</strong>se.Blood glu<strong>co</strong>se may rebound following a 'hypo'. The child must <strong>co</strong>ntinue with normalsnacks and food, and the regular insulin dose given.The blood glu<strong>co</strong>se must be monitored until it returns to normal limits.If Glucagon is given, warn the parents the child may vomit and there is a danger ofa reactionary 'hypo' six hours later if the levels are not monitored and sufficientcarbohydrate taken.Identify the cause for the 'hypo' to try to avoid in the future.Equipment ProblemsIf the parents report the pen device is broken, a spare one can be obtained from theGreat Western ward. If they are out of the area, i.e. on holiday, go to local A&E toobtain a new device.Page 30 of 39 Mando Watson, diabetes guidelines April 2009
Appendix JLetter to GP regarding newly diagnosed patientsThe following standard letter has been prepared to ensure early <strong>co</strong>mmunication withthe GP when a newly diagnosed diabetic is discharged to the <strong>co</strong>mmunity. This isessential to ensure the family have adequate supplies. It should be <strong>co</strong>mpleted in<strong>co</strong>njunction with the <strong>Paediatric</strong> Home Care Team for <strong>Diabetes</strong>.Page 31 of 39 Mando Watson, diabetes guidelines April 2009
<strong>St</strong> Mary’s <strong>Paediatric</strong> <strong>Diabetes</strong> Home Care team will <strong>co</strong>ntinue to offer support andmonitoring of this young person and their family in the <strong>co</strong>mmunity with regularreview in clinic. Please do not hesitate to <strong>co</strong>ntact us if you have any furtherquestions about this young person.Yours sincerelyJan Reddick<strong>Paediatric</strong> <strong>Diabetes</strong> Nurse Specialist.Tel: 020 7886 6482Page 33 of 39 Mando Watson, diabetes guidelines April 2009
Appendix KReferences on DKAConsensus guidelines 2000. International society for pediatric and adolescent<strong>Diabetes</strong>. Published by ISPAD or can be viewed on www.ispad.org, or www.novo.dkGlaser N, Barnett P, McCaslin I, et al. Risk factors for cerebral edema in childrenwith diabetic ketoacidosis. New England Journal of Medicine 2001; 344:264-9.Edge JA. Management of diabetic ketoacidosis in childhood. British Journal ofHospital Medicine 55:508-12;1996.Silink M. Practical management of diabetic ketoacidosis in childhood and adolescence.Acta <strong>Paediatric</strong>a. Supplement 425:63-6;1998.Green SM, Rothrock SG, Ho JD, Gallant RD, Borger R, Thomas TL. Failure ofadjunctive bicarbonate therapy to improve out<strong>co</strong>me in severe pediatric diabeticketoacidosis. Annals of Emergency Medicine 31:41-8;1998.Hale PM, Rezvani I, Braunstein AW, Lipman TH, Martinez N, Garibaldi L. Factorspredicting cerebral edema in young children with diabetic ketoacidosis and new onsettype 1 diabetes. Acta <strong>Paediatric</strong>a 86:626-31; 1997.Canarie MF, Bogue CW, Banasiak KJ, Weinzimer SA, Tamborlane WV.De<strong>co</strong>mpensated hyperglycemic hyperosmolarity without significant ketoacidosis in theadolescent and young adult population: J Pediatr Endocrinol Metab. 2007Oct;20(10):1115-24..Other referencesConsensus guidelines 2000. International society for pediatric and adolescent<strong>Diabetes</strong>. Published by ISPAD or can be viewed on www.ispad.org, or www.novo.dkRecent review article:Therapeutic <strong>co</strong>ntroversy: Prevention and treatment of diabetes in children.Rosenbloom AL, Schatz DA, Krischer JP, et al Journal of clinical Endocrinology andMetabolism. 2000;85:494-522.Other refs:Krane EJ Diabetic ketoacidosis. Biochemistry, physiology, treatment, and preventionPage 34 of 39 Mando Watson, diabetes guidelines April 2009
Pediatr Clin North Am. 1987 Aug;34(4):935-60.Warner DP, McKinney PA, Law GR, Bodansky HJ. Mortality and diabetes from apopulation based register in Yorkshire 1978-93. Archives of disease in childhood1998;78:435-8.DCCT research Group. The effect of intensive diabetes treatment on thedevelopment and progression of long term <strong>co</strong>mplications in insulin dependant diabetesmellitus. New England Journal of Medicine 1993; 329:977-986.Davis EA, Keating B, Byrne GC, Russell M, Jones TW. Impact of improved glycaemic<strong>co</strong>ntrol on rates of hypoglycaemia in insulin dependant diabetes mellitus. Archives ofdisease in childhood 1997; 78: 111-115Moore THM, Shield JPH (microalbuminuria in diabetic adolescents and childrenresearch group). Prevalence of abnormal urinary albumin excretion in adolescents andchildren with insulin dependant diabetes mellitus. Archives of disease in childhood2000; 83:239-243.Lafferty AR, Werther GA, Clarke CF. Ambulatory blood pressure, microalbuminuriaand autonomic neuropathy in adolescents with type 1 diabetes. <strong>Diabetes</strong> care 2000;23:533-538.Holl RW, Lang GE, Grabert M, Heinze E, Lang GK, Debatain KM. Diabetic retinopathyin pediatric patients with type1 diabetes- effect of diabetes duration, prepubertaland pubertal onset of diabetes, and metabolic <strong>co</strong>ntrol. Journal of Pediatrics1998;132:790-4.APLS guidelines, Third EditionISPAD Consensus <strong>Guidelines</strong> 2000NSF for Children, Young People, and Maternity Services(http://www.dh.gov.<strong>uk</strong>/PolicyAndGuidance/HealthAndSocialCareTopics/ChildrenServices/ChildrenServicesInformation/ChildrenServicesInformationArticle/fs/en?CONTENT_ID=4089111&chk=U8Ecln)NSF for <strong>Diabetes</strong> (http://www.dh.gov.<strong>uk</strong>/assetRoot/04/05/89/38/04058938.pdf)<strong>Guidelines</strong> for the management of diabetic ketoacidosis in children and adolescents(http://www.bsped.org.<strong>uk</strong>/professional/guidelines/docs/BSPEDDKAApr04.pdf)Page 35 of 39 Mando Watson, diabetes guidelines April 2009
AcknowledgementsThis guideline is based on the guideline produced by Dr Ni<strong>co</strong>la Bridges, Consultant<strong>Paediatric</strong> Endocrinologist at Chelsea and Westminster Hospital.Contributions and support has <strong>co</strong>me from Dr Samir Wassouf, Dr Simon Nadel, Dr IanMa<strong>co</strong>nochie, Julia Simmons, Dr David Inwald, Debbie Hammond, Mae Said, KatieElwig, Dr Claire Holt and many others.Page 37 of 39 Mando Watson, diabetes guidelines April 2009
IMPLEMENTATIONTraining required for staffIf yes, who will provide trainingWhen will training be provided?Date for implementation of guidelineNoMando Watson, Consultantpaediatrician, and the paediatricdiabetes teamAt induction of new medical staffnowMONITORING / AUDITWhen will this guideline be audited?Who will be responsible for auditing this guideline?Are there any other specific re<strong>co</strong>mmendations for audit?Part of regular annual audit reviewMando Watson, Consultantpaediatrician, and the paediatricdiabetes teamnoREVIEWWho will review this guideline?Please indicate frequency of review:Drug related guidance should be reviewed every 2 yearsTherapy related guidance should be reviewed every 5 yearsClinical treatment guidance should be reviewed every 3 – 5 yearsMando Watson, Consultant<strong>Paediatric</strong>ian, and the paediatricdiabetes team2 yearlyDate of next review 2011GUIDELINE DETAIL<strong>St</strong>art Date: (date of final approval by CPG) 19.06.09Dates approved by: <strong>Paediatric</strong> <strong>Guidelines</strong> Group 8.5.09<strong>Paediatric</strong> Quality and Safety Committee 14.5.09Have all relevant stakeholders (Trust sites, CPGs anddepartments) been included in the development ofthis guideline?Who will you be notifying of the existence of thisguidance?Related documents:Author/further information:Document review history:Next review due January 2011This guideline replaces:Penny Fletcher – pharmacySanjay Gautama – anaestheticsNicky Coote – HH paediatric leadAll paediatric medical staff, senior nursing staff, seniorAHPs and managersAll other documents relating to paediatric diabetes will beremoved from the intranet. The “Hyperglycaemia SOP -emergency management of patients presenting with newlydiagnosed diabetes mellitus” currently on the intranet must berenamed to specify that it is for adults onlyDr Mando Watson, Consultant <strong>Paediatric</strong>ian, CPG 5, <strong>St</strong>Mary’s Hospital. Telephone extension 6905mando.watson@imperial.nhs.<strong>uk</strong>NA(SMH)<strong>Diabetes</strong> Perioperative management (Paeds Anaesthetics)(SMH)<strong>Diabetes</strong> Periopertive Management <strong>co</strong>ver (PaedsAnaesthetics)(SMH)<strong>Diabetes</strong> including Ketoacidosis (Paed General)(SMH)<strong>Diabetes</strong> including Ketoacidosis Infosheet (Paed General)Page 38 of 39 Mando Watson, diabetes guidelines April 2009
INTRANET HOUSEKEEPINGKey wordsWhich CPG does this belong to?Which subdivision of the guidelines spine should thisbelong to?Title for the intranet if different from the document (pleasenote that documents sit alphabetically so should not startwith “guideline for…”)diabetes, diabetic, insulin, ketoacidosis, hypoglycaemia,adolescent, paediatric, child, children, glucagon, glu<strong>co</strong>se,novomix 30, humalog mix 25, novomix, NovoRapid, insulinaspart, Humalog, insulin lispro, Actrapid, Lantus, InsulinGlargine, Levemir, Insulin Detemir, Mixtard 30, Novomix 30,Biphasic Insulin Aspart, biphasic insulin Lispro,CPG5The whole document belongs in general paediatricsIt has 2 subsections – diabetic ketoacidsosis for PICU andperioperative care of children with diabetes that will reside inPICU and anaesthetics respectively.As abovePage 39 of 39 Mando Watson, diabetes guidelines April 2009