Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
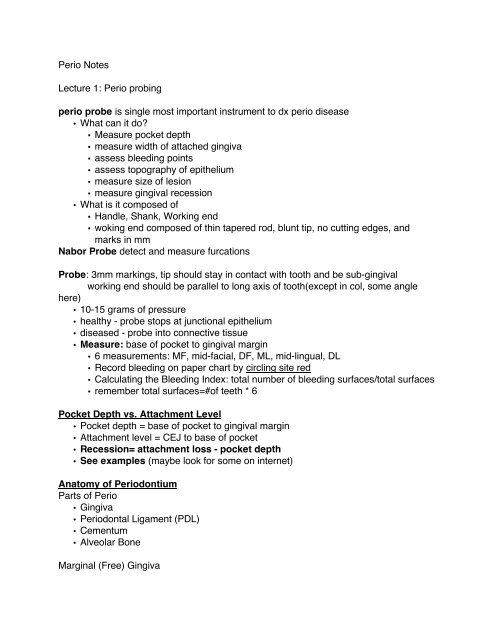
<strong>Perio</strong> <strong>Notes</strong><br />
Lecture 1: <strong>Perio</strong> probing<br />
perio probe is single most important instrument to dx perio disease<br />
• What can it do?<br />
• Measure pocket depth<br />
• measure width of attached gingiva<br />
• assess bleeding points<br />
• assess topography of epithelium<br />
• measure size of lesion<br />
• measure gingival recession<br />
• What is it composed of<br />
• Handle, Shank, Working end<br />
• woking end composed of thin tapered rod, blunt tip, no cutting edges, and<br />
marks in mm<br />
Nabor Probe detect and measure furcations<br />
Probe: 3mm markings, tip should stay in contact with tooth and be sub-gingival<br />
working end should be parallel to long axis of tooth(except in col, some angle<br />
here)<br />
• 10-15 grams of pressure<br />
• healthy - probe stops at junctional epithelium<br />
• diseased - probe into connective tissue<br />
• Measure: base of pocket to gingival margin<br />
• 6 measurements: MF, mid-facial, DF, ML, mid-lingual, DL<br />
• Record bleeding on paper chart by circling site red<br />
• Calculating the Bleeding Index: total number of bleeding surfaces/total surfaces<br />
• remember total surfaces=#of teeth * 6<br />
Pocket Depth vs. Attachment Level<br />
• Pocket depth = base of pocket to gingival margin<br />
• Attachment level = CEJ to base of pocket<br />
• Recession= attachment loss - pocket depth<br />
• See examples (maybe look for some on internet)<br />
Anatomy of <strong>Perio</strong>dontium<br />
Parts of <strong>Perio</strong><br />
• Gingiva<br />
• <strong>Perio</strong>dontal Ligament (PDL)<br />
• Cementum<br />
• Alveolar Bone<br />
Marginal (Free) Gingiva
• Portion of gingiva surrounding neck of tooth<br />
• not attached to tooth<br />
• soft tissue wall of gingival sulcus<br />
• Interdental papilla:part of marginal gingiva that fills the interdental space<br />
Free gingival groove AKA free marginal groove<br />
• Shallow depression dividing free from attached gingiva<br />
• only seen in 50% of patients<br />
Attached Gingiva<br />
• Portion of gingiva that extends apically from free gingiva to mucogingival junction<br />
• bound tightly to underlying bone<br />
Gingival Sulcus - pocket, where we probe<br />
Junctional Epithelium<br />
• Collar like band of non-keratinizing epithelia cells<br />
• form the base of the sulcus(pocket)<br />
• .25-1.35 mm in length<br />
Gingival Col<br />
• Saddle like depression<br />
• between facial and lingual papilla<br />
• non-keratinized<br />
Alveolar Mucosa<br />
• freely movable - not bound to bone<br />
• non-keratinized<br />
• not designed to withstand forces of mastication<br />
Mucogingival junction - sclloped line dividing keratinized gingiva from alveolar mucosa<br />
Measuring amount of attached gingiva<br />
• Measuring keratinized gingiva<br />
• gingival margin to mucogingival margin<br />
• subtract sulcus(pocket) depth<br />
• attached = keratinized - pocket depth<br />
• varies: 1-9mm<br />
• Greatest(thickest): Lingual of man molars, facial max ant<br />
• Least(thinnest): Man first premolars<br />
Gingival fibers<br />
• Brace marginal gingiva against tooth<br />
• provide rigidity(withstand mastication)
• unite marginal gingiva to cementum<br />
Cementum<br />
• Calcified structure that covers the anatomic root<br />
• inorganic content: 40-50%<br />
• Anchors tooth to bone via PDL<br />
PDL<br />
• Collagenous connective tissue - surrounds root of tooth<br />
• attaches tooth to alveolar process<br />
• Four Properties<br />
0. Supportive: anchors tooth to bone<br />
1. Formative: Helps maintain biologic activity of bone/cementum<br />
2. Nutritive: supplies nutrients, removes waste via blood/lymph<br />
3. Sensory: transmits tactile pressure and pain<br />
Alveolar Process<br />
• Portion of maxilla/mandible that supports the socket of teeth<br />
• Alveolar bone proper<br />
• Thin layer surrounding root and gives attachment to PDL<br />
• lamina dura in radiograph, AKA cribriform plate<br />
• supporting alveolar bone<br />
• Surrounds alveolar bone proper<br />
• gives support to sockets<br />
• Compact = cortical<br />
• Cancellous or trabecular = spongy<br />
Healthy Gingiva<br />
• Color = coral pink<br />
• contour = marginal gingiva follows scalloped line around each tooth<br />
• knife edge margin<br />
• papilla just fill embrasure<br />
• Consistency = firm / resilient<br />
• Surface texture = stippling (May or MAY NOT be there)<br />
• least reliable parameter<br />
Color influences: Inflammation, Vascularity, keratinization, pigmentation<br />
Unhealthy Gingiva<br />
• Color: Bright Red(acute) to bluish red(chronic)<br />
• Contour: rounded, rolled, blunted, flat, crater, bulbous<br />
• Consistency: spongy, edematous to fibrotic<br />
Gingival description (know which is good, which is bad)
• Location: general vs. local<br />
• Severity: slight, moderate, severe<br />
• Location: papillary, marginal, diffuse<br />
• Color: Coral Pink, red, bluish red<br />
• Contour: knife-edge, enlarged, bulbous, cratered<br />
• Consistency: firm and resilient, edematous, fibrotic<br />
• WNL is not acceptable<br />
Dentin hypersensitivity<br />
Defined<br />
• Short transient pain due to exposed dentin<br />
• usually occurs in response to stimuli (thermal, tactile, osmotic, chem)<br />
• Can occur after dental procedure, more likely to be self-limiting<br />
• cannot be attributed to some other pathology<br />
• What is required?<br />
• Dentin exposure<br />
• tubule open from pulp to oral cavity<br />
Hydrodynamic theory<br />
• Brannstrom and Astron proposition<br />
• opening of tubules => movement of dentinal fluids<br />
• movement indirecty stimulates the extremities of plural nerves, causing pain<br />
• exact mechanism of stimulation not understood<br />
Pain dependent on<br />
• Age (peak at 30, majority 20-40)<br />
• Gender (females>males)<br />
• Situation<br />
• Past dental experience<br />
• Patient expectations<br />
Some Causes<br />
• Gingival recession and tooth wear (erosion)<br />
• Most common sites: buccal-cervical sites of premolars and canines<br />
• DH most commonly caused by recession<br />
• Removal of smear layer also initiates<br />
• <strong>Perio</strong>dontal therapy are 2-3 times more likely<br />
• 73-98% perio patients<br />
• self-limiting - tubules will occlude<br />
• bleaching<br />
Management<br />
• plaque control is paramount<br />
• soft brush, less aggressive brushing
• desensitizing toothpaste<br />
• professionally applied agents<br />
• No cure-all product<br />
Desensitizing toothpastes<br />
• Active ingredient: KNO3 most common<br />
• others: Strontium chloride, sodium citrate, sodium fluoride, stannous fluoride<br />
• 2-3 weeks of use required before improvement<br />
• Max relief 8-12 weeks<br />
• Patience compliance critical<br />
• do not rinse after brushing - only spit<br />
Potassium Nitrate<br />
• Action: Does NOT occlude tubules by crystals (like other agents)<br />
• Inc concentration extracellular K around nerve-fiber,<br />
• causes depol, prevents re-pol<br />
• not enough evidence to show effectiveness<br />
Others still used: NaF, stannous fluoride<br />
• obliteration of tubules through precipitation of CaPO4 onto dentin<br />
• Abrasives may contribute through creation of smear layer<br />
• use LESS water and do NOT rinse<br />
• prescription level: 1.1%<br />
Crest Pro-health: Stannous Fl, obliterates tubules<br />
Professional<br />
• Fl treatments/varnishes: creates barrier of CaF crystals<br />
• can be dissolved over time through saliva<br />
• benefits from varnish base<br />
• crystals in tubules(60-70um) are more difficult to remove<br />
GLUMA 5% gluteraldehyde, 35% HEMA and water: occlude tubules and decreases fluid<br />
flow<br />
Colgate Pro-Relief: 8% Arginine and Calcium Carbonate - occludes tubules<br />
Inflammatory <strong>Perio</strong>dontal Diseases<br />
<strong>Perio</strong> Disease: Any pathologic process that affects the periodontium<br />
Plaque-related inflammatory perio disease<br />
• gingivitis - inflammation of gingiva<br />
• Chronic periodontitis - progressive inflammation, involves: BONE, PDL, GINGIVA<br />
• Classification<br />
• Gingivitis
• chronic periodontitis<br />
• Aggressive periodontitis<br />
• <strong>Perio</strong>dontitis as a manifestation of systemic disease<br />
• Necrotizing periodontal disease<br />
• Abscesses of the periodontium<br />
• <strong>Perio</strong>dontitis associated with LEO<br />
• Degree of Destruction = Severity of local factors X Freq of Energy X Duration of<br />
Injury X Host response<br />
Gingivitis (Case Type I)<br />
• Gingival erythema<br />
• No bone loss<br />
• Bleeding on probing<br />
• increases pocket depth (3-5mm)<br />
• Increase in GCF<br />
• NO PAIN<br />
<strong>Perio</strong>dontitis<br />
• Apical migration of JE, Bone loss<br />
• Bacteria associated<br />
• Aa - Aggregatibacter actinomycetemcomitans<br />
• Pg - Porphyromonas gingivalis<br />
• Pi - Prevotella intermedia<br />
• Tf - tannerella forsythia<br />
• Td - Treponema denticola<br />
Gingivitis CAN be reversed; <strong>Perio</strong>dontitis CANNOT be reversed<br />
• Gingi always preceeds Peri; but gingi does not always become peri<br />
• no single indicator to diagnose periodontal disease or health<br />
Early <strong>Perio</strong>dontitis (Case Type II)<br />
• Mild bone loss (50% bone loss<br />
• Attachment loss > 5mm, pocket depth > 7mm<br />
• Furcations involvement, mobility likely, suppurtation - pus feeling
• Pain more likely<br />
Case Type V<br />
• Refractory periodontitis<br />
• uncommon periodontal diseases: aggressive periodontitis (LJP, RAP)<br />
• RAP - rapidly advancing periodontitis<br />
• LJP - localized juvenile periodontitis<br />
Radiographs and probings needed to properly dx<br />
Etiology<br />
• Primary: PLAQUE - always<br />
• Secondary<br />
• Local<br />
• Overhangs, poor crown margins<br />
• Calculus, furcations<br />
• crowded teeth, ortho<br />
• large carious lesions<br />
• Food impaction, smoking<br />
• Xerostomia<br />
• Systemic<br />
• Smoking<br />
• diabetes<br />
• immune-compromised<br />
• aging<br />
• stress => ANUG<br />
• Nutritional deficiencies<br />
• medications<br />
Classifications of Pockets<br />
• Gingival Pocket - pseudo-pocket, false pocket<br />
• Pocket caused by hyperplasia; coronal movement of gingival margin<br />
• No apical migration of JE and No bone loss<br />
• <strong>Perio</strong>dontal Pocket: pocket caused by bone loss due to apical migration of JE<br />
• Suprabony - bottom of pocket is coronal to the crest of the alveolar bone<br />
• Infrabony - bottom of pocket is apical to crest of alveolar bone<br />
Tooth Deposits<br />
Non-mineralized - pellicle, plaque, materia alba, food debris<br />
mineralized - calculus<br />
Acquired Pellicle<br />
• Thin, structureless, forms over teeth/restorations/calculus<br />
• a glycoprotein from saliva or GCF subgingival
• fills mico voids<br />
• reforms immediately after removal<br />
• 1 week to completely form into mature stage<br />
• Significance<br />
• Nidus (niche) - place for bacteria to attach<br />
• serves as nutrient source<br />
• protective barrier<br />
• calculus attachment<br />
Dental Plaque<br />
• Dense, non-calcified, ORGANIZED mass of bacterial colonies in a gel-like intracell<br />
matrix - not random bacteria<br />
• Buzz word: bacterial biofilm<br />
• Biofilm<br />
• Cooperating communities of back<br />
• micro-colonies - surrounded by protective matrix creating differing environ<br />
• Microorg communicate via chemical signals<br />
• resistant to Ab, antimicrobials, host response<br />
• Factors influencing plaque build-up<br />
• Mechanical removal<br />
• availability of nutrients<br />
• undisturbed environment<br />
• interaction between bacteria and host immune response<br />
• RESULT: bacteria accumulate in sheltered environ => disease<br />
• Plaque Formation<br />
• initial formation: 2 hours<br />
• gram positive aerobic and facultative organisms<br />
• actinomyces and streptococcus<br />
• 47-85% cocci in first 4 hours<br />
• isolated colonies in proximal surfaces, fissures, sulcus, irregularities<br />
• 2 days to double in mass (visual at this point)<br />
• white, grey, or yellowish<br />
• secondary colonizers - not on clean tooth<br />
• Pi, Pg, Capnocytophaga species, spirochetes, motile rods<br />
• gram negatives and anaerobic bacteria<br />
• initiators of dental caries and perio ds<br />
• Intracellular plaque matrix<br />
• matrix that surround the bacteria with the biofilm<br />
• inorganic and organic components from bacteria<br />
• Major components: polysac from metabolism of CHO<br />
• Minor components: salivary glycoproteins<br />
• Dental Plaque metabolism<br />
• Energy source (sucrose) introduced<br />
• Production of Acid, Intracell polysac (E storage), Extracell poly sac
• Extracell polysac:<br />
• glucans - dextrans - sticky, help anchor/stabilize plaque mass<br />
• fructans - levans - energy source<br />
• Plaque CANNOT be removed by water spray<br />
• matures => more resistant to mechanical removal<br />
• Anaerobic glycolysis results in pH from 7 -> 4.5 (tooth demin)<br />
• Bacteria look for foor, go subgingival<br />
• Host defends itself via inflammatory response and gingivitis inititiated<br />
Materia Alba - not plaque, very different<br />
• UNORGANIZED - soft mixture of saliva proteins, bacteria, desquam epi cells<br />
Food Debris - not plaque, we floss away plaque<br />
Dental Calculus<br />
• Major role in inflammatory perio diseases<br />
• KEEPS PLAQUE CLOSE contact with gingiva<br />
• Calculus not the problem, its the plaque under<br />
• Primary issue: Calculus prevents removal of plaque; not being a mechanical irritant<br />
Supragingival Calculus<br />
• coronal to gingival margin<br />
• white or whitish yellow<br />
• hard, cake-like consistency<br />
• more common: Lower anteriors and buccal of max molars (next to salivary gland<br />
ducts)<br />
Subgingival Calculus<br />
• Below crest if marginal gingiva, not visible clinically<br />
• detect: explorer and radiographs<br />
• dense, dark brown to greenish black (blood and bacteria)<br />
• flint like, firm attachment<br />
Mineralization<br />
• Percipitation of Ca and PO4 from saliva and GCF<br />
• some Mg, Zn, Fl, carbonate<br />
• Not all plaque mineralizes, but plaque destined to mineralize does so within a few<br />
days<br />
• mineralization - starts extracellularly first, then produced intracell<br />
• Occaisionally begin within the cells and spread to intracell matrix<br />
• Four Main Crystalline forms:<br />
• Hydroxyapatite<br />
• whitlockite<br />
• octacalcium phosphate<br />
• brushite
• General Rule: subgingival calculus: 60% min, supra: 30% min<br />
• mineralization starts between day 1-14 of plaque formation<br />
• Not all plaque mineralizes<br />
• Mineral source: supra:saliva, sub:GCF and exudate<br />
Fluorides<br />
Systemic: Water fluoridation, supplements, food/beverages<br />
Topical: Water fluoridation, fluoride products, in-office treatments, food/bev<br />
Mechanism<br />
• Systemmic: ingested and incorporated in enamel during development<br />
• Topical: promote remin, prevent demin, inhibit glycolysis in microbes<br />
Benefits of water fluoridation<br />
• 30% reduction in<br />
• caries for primary dentition<br />
• children/adolescent perm dentition<br />
• coronal caries / root caries<br />
• Most cost effective preventative dental programs<br />
Optimum level of fluoridation: 1 ppm (min caries and min flurosis)<br />
Topical Fluoride<br />
• Mode of Action<br />
• Fl deposition in enamel maturation phase<br />
• Highest conc in outermost portion (5-10um)<br />
• Fl ion substituted into hydroxyapatite crystal - stable, more compact bond<br />
• DOES NOT CAUSE FLUOROSIS (only occurs through systemic)<br />
• Acidic or high conc Fl forms CaFl2; neutral Fl fluoroapatite<br />
• initial deposition not permanent - rapid loss in frost 24, continues over weeks<br />
• Each professional application increases amount of permanently bound Fl<br />
• Fluorhydroxyapatite: most desirable form<br />
• Calcium Fluoride (CaFl2): Fl source for remin<br />
• Benefit of topical related to frequency of treatment<br />
• no benefit for sound enamel, regardless of type of treatment<br />
• Professional applications: 8% Stannous Fl, 2% NaF; 1.23% Acidulated Phosphate<br />
Fl (APF)<br />
• no difference in efficacy; stannous no longer used<br />
• 8% Stannous Fl<br />
• Forms stannous fuorophosphate and CaF<br />
• Acidic, Bitter, metallic taste<br />
• Stains clothes and teeth (brown)<br />
• prepared immediately prior to use
• liquid and messy<br />
• 2% NaF (neutral)<br />
• Results in fluoroapatite and CaF<br />
• gels and foam - ready to use<br />
• Absent of taste<br />
• No stain or tissue irritation<br />
• 1.23% Acidulated Phosphate<br />
• Results in fluorohydroxyapatite and CaF<br />
• gel and foam - ready to use<br />
• stable in plastic<br />
• No irritation or discoloration<br />
• Can etch ceramic or porcelin<br />
• Use NaF for<br />
• composites<br />
• porcelain crowns, veneers<br />
• exposed root surfaces<br />
• glass ionomers<br />
• Indications<br />
• High caries activity<br />
• sensitive or exposed roots<br />
• Deteriorating restorations<br />
• Overdentures<br />
• xerostomia - Hx of head/neck radiation, meds<br />
• Newly erupted teeth -really good uptake here<br />
• Absence of other fluoride exposures<br />
• Why? everyone benefits, no risks to topical<br />
Professional Treatments<br />
• NaF Neutral<br />
• 9000ppm, pH 7.0<br />
• slow uptake - requires 4 minutes to reach 1000ppm<br />
• 4 minutes application<br />
• No side effects<br />
• APF<br />
• 12,000 ppm, pH 3.5<br />
• Rapid uptake - 12,000 ppm within 1 minute<br />
• 4 minutes application (yes, even though uptake is rapid)<br />
• May etch porcelain or composite<br />
Gel vs Foam<br />
• uptake is comparable between the two<br />
• Foam requires less material, decrease chance of swallow<br />
Fluoride Toxicity
• Probable Toxic dose (PTD) based on weight<br />
• 5mg F/kg of body weight<br />
• if less than PTD consumed, give Ca, Al, Mg products in office<br />
• over PTD - same as above plus hospital observation<br />
• over 15mg F/kg - same as above, but call 911<br />
• Signs and symptoms<br />
• Nausea, vomiting, diarrhea, abdominal cramps<br />
• Increased salivation, dehydration<br />
• Treatment<br />
• time is everything, blood levels reach max 30 to 60 min from ingestion<br />
• Milk and eggs or other Ca, Mg, Al<br />
• binds Fl<br />
• Coats membranes of GI preventing burns<br />
• Fluids also help to dissolve<br />
• Do not induce vomiting, but patient will often vomit anyway<br />
Application<br />
• Ribbon into tray - DO NOT OVERFILL (may ingest)<br />
• Pt - upright; dry teeth<br />
• place tray then saliva ejector<br />
• instruct pt to chew slightly<br />
• 4 minute application regardless of which used<br />
• do not leave unattended<br />
• After: expectorate excess Fl, no eat or drink for 30 minutes<br />
Fluoride Varnish<br />
• 5% NaF (26,000ppm)<br />
• FDA: use for dentin hypersensitivity, not reducing caries (ADA does endorse this)<br />
• Can by applied every 6 months to prevent caries in high risk population<br />
• Application<br />
• apply thin layer (.5 mm)<br />
• Post op - forego brushing soft diet that evening<br />
• may discolor teeth and restorations, but not permanent<br />
Fluoride prophy paste: does not replace fluoride application<br />
• prophy removes about .1-1.0 micron of Fl-rich enamel<br />
• At best, Fl in prophy replaces what it removed<br />
• not approved as a Fl treatment<br />
Fl in Dentifrice (toothpaste)<br />
• 1000ppm<br />
• NaF with compatible abrasive is most effective<br />
• Fluorosis/toxicity risk if swallowed
Additional Fl products<br />
Home Fluoride<br />
• Prescription: 1.1% NaF gel<br />
• OTC: .4% stannous (gel)<br />
• OTC: 225ppm NaF some 100ppm<br />
Caries Reduction protocol:<br />
• Pts in high risk category: CHX 1/day for one week, for 6 months - I dunno<br />
• CHX after dinner , Fl at bedtime<br />
• Low risk: OTC mouth rinse for maintenance<br />
Plaque Control and Oral Hygiene aids - not comprehensive details, but important<br />
points<br />
Oral health cannot be attained or preserved with plaque control<br />
Toothbrush<br />
• Bristle shape<br />
• End rounded vs. blunt cut<br />
• round, tapered, or smooth were less abrasive<br />
• Round tip is recommended<br />
• Bristle texture<br />
• Soft: .007-.009 inches<br />
• AVerage life toothbrush - 3 months<br />
• ADA: "Brush regularly"; School: twice a day, 2 minutes each time<br />
• Brushing Techniques<br />
• Bass (modified)<br />
• Bristle angled 45 degrees toward gingival margin<br />
• gently press bristles to enter sulcus and embrasures<br />
• subgingival cleansing and gingival stimulation<br />
• Fones (circular)<br />
• 90 degrees to tooth<br />
• large circles over teeth and gingiva<br />
• easy for children or limited dexterity<br />
• Others: Rolling, Stillman, Charters, Leonard, Horizontal, Smith-modified<br />
• ADA Guidelines for electric toothbrushes<br />
1. Laboratory evidence of electrical safety<br />
2. Clinical evidence of hard/soft tissue safety under under unsupervised<br />
conditions<br />
3. Clinical evidence of plaque and gingivitis when compared to other ADA<br />
accepted toothbrush<br />
4. Evidence of proper labeling and advertising claims<br />
Chocrane review: rotation, oscillation is better than manual toothbrushes at removing<br />
plaque and reducing gum inflammation<br />
Interproximal Plaque Control
• Based on:<br />
• Size of interdental spaces<br />
• presence of furcations<br />
• ortho or fixed appliance<br />
• tooth alignment<br />
• Flossing: remove interproximal plaque, not dislodge food wedged between<br />
teeth<br />
• spool method good for those with less dexterity<br />
• see-saw motion, not pop through<br />
• Platyplus ortho flosser and Super floss - good for getting around brackets<br />
• Interdental brushes (proxy brush)<br />
• large embrasures<br />
• teeth with concavities<br />
• around fixed appliances<br />
• ortho appliances<br />
• furcations (class III, IV)<br />
• Oral irrigators - result in disruption of loosely attached or unattached<br />
supra/subgingival plaque<br />
• not indicated for patients who have effective oral hygiene or no inflammation<br />
• alone not effective at reducing inflammation<br />
• best if combined with toothbrusing<br />
• Cleaning Dentures<br />
• After meals - warm (NOT HOT) water<br />
• Use soap - NOT TOOTHPASTE<br />
• soft toothbrush or denture brush<br />
• Soaking also works - 6 hours<br />
Sweeteners<br />
Xylitol<br />
• Polyol, sweetness similar to sucrose<br />
• 40% few calories (2.4 cal/g)<br />
• From birch trees, corncobs, waste of sugar cane<br />
• Non-acidogenic, thus non-cariogenic<br />
• S mutans and level of lactic acid<br />
• slowly absorbed by GI<br />
• Main side effect diarrhea (occurs at 4-5 times that needed for caries prevention)<br />
• FDA approved since 1960<br />
• First trial (60's): 3 groups: Xylitol, fructose, sucrose for 2 years (125 volunteers)<br />
• Results in DMFT (decayed, missing, filled teeth)<br />
• Xylitol: 0.0 (some lesions of early demin of smooth surface caries)<br />
• Fructose: 3.8<br />
• Sucrose: 7.2<br />
• 1995 trial: large sample group - 1277 over 40 months<br />
• Results: most effective at caries prevention: Xylitol followed by xylitol/sorbitol mix<br />
then sorbitol
• Why does it work?<br />
• not metabolized by S. Mutans, pH not lowered => demin prevented<br />
• Also saliva flow is stimulated, enhances buffering<br />
• Highly toxic to dogs<br />
• How? rapid and severe increase in insulin production leads to hypoglycemia<br />
• only takes .15g/kg to start seeing effects<br />
• Higher amounts (1.4-2.0 g/kg) can cause hepatic failure/necrosis and death<br />
• Therapeutic dose: 6-10 g per day over 3-7 consumptions<br />
• more than this does not see more caries prevention<br />
• less than 3 times a day also not as effective<br />
What doe the ADA seal mean for chewing gum? Basically chewing for 20 min after<br />
eating stimulates enough saliva to help prevent cavities<br />
• Company must show one or more of the following:<br />
2. reduces plaque acids<br />
3. promoting re-min of the tooth<br />
4. reduce caries and/or gingivitis<br />
• Ice cubes: 1.15 g xylitol per cube<br />
• trident .17 gram per piece<br />
• if xylitol is not the #1 lecture<br />
Xylitot lollies - no xylitol<br />
Sorbitol: most common polyol used in US, from plants<br />
• 60% as sweet as sucrose, 2.6 cal/ g<br />
• low-cariogenic (organisms can learn to use sorbitol if sugar supply is depleted)<br />
Mannitol: Polyol from seaweed<br />
• 50-70% as sweet as sucrose, 1.6 cal/g<br />
• non-cariogenic<br />
• non-hygroscopic - used as dusting agent in gum<br />
Intense Sweeteners<br />
• Saccharin<br />
• 200-700 times sweeter than sucrose<br />
• non-cariogenic; non-nutritive<br />
• largest volume / lowest cost sweetener in the world<br />
• Aspartame<br />
• 200 times sweeter than sucrose<br />
• 4 cal/g (negligible due to small amount that is used)<br />
• Sucralose<br />
• 600 times sweeter than sucrose<br />
• non-cariogenic; non-nutritive
"<br />
!"#$#%&'&($#)!#"(*+*%&(,-)<br />
../.0/1223)<br />
4567'%&)8'(%&#%'%,#)<br />
!<br />
"# $%&'!()*!+,-./0%1.'!<br />
(# 2.!(,3.!04!%*!05.!5.(3056!%&73()080%''9.'!<br />
,# 2.!(,3.!04!%*!05.!:(%3%);8
"<br />
%%%# a44'.!%&73()0!,4*6!<br />
,# H(W.!(!@(*%4;@(75!<br />
/# b(6!)..*!04!@.&41.!05.!/@4?)8,@%*;.!04!.1(39(0.!%&73()0!,4*6!*%@./036!<br />
c# d4?!04!F3(/.!()!B&73()0!<br />
(# U(,@%/(0.!@(*%4;@(75%/8'9@;%/(3!;9%*.!)4?!649@!7.@%4*4)0(3!7(054;.)'!
"<br />
"# B%(,'&(%BH)(%,7>+(%B)<br />
(# M09*6!&4*.3'!()*!75404'!<br />
,# \(NG97!<br />
/# $*.]9(0.!@(*%434;6!K.#;#!%GA$HL!<br />
"Q# A3(''%/!A3%)%/(3!U%)*%);'!<br />
(# d.(305!<br />
%# O44*!;%);%1(3!/434@D!/4)049@D!/4)'%'0.)/.!<br />
%%# J4!,3..*%);!4)!7@4,%);!<br />
"# M7./%
"<br />
(# $33!%&73()0'!@.]9%@.!&.0%/9349'!54&.!/(@.!('!'44)!('!05.!%&73()0!%'!.N74'.*!04!05.!4@(3!/(1%06!<br />
,# T43.!4
"<br />
!<br />
E# H5(0!?(6!649!*4)C0!@9)!05.!@%'W!4
Antimicrobials<br />
11/9/10 2:02 PM<br />
Terminology<br />
• Adverse Effect: harmful to patient<br />
o Side effect(which is different): may be harmful, useful,<br />
beneficial<br />
• Compliance: patients ability, desire, and motivation to use the<br />
product<br />
• Substantivity (know this term): ability of an agent to absorb to<br />
teeth and surfaces and be released at therapeutic levels<br />
o We want this to be high because that means less times the<br />
patient has to use in order to have the effect<br />
Considerations with chemical plaque control<br />
• What effect will it have on oral flora and associated disease?<br />
• Is the effect significant?<br />
• Are there adverse effects on the oral flora?<br />
• Are hard/soft tissues adversely effected?<br />
• Are dental restorative materials adversely effected?<br />
• Do usage and properties support compliance?<br />
• Are the any contraindications to product use?<br />
Delivery systems<br />
• Local: paste, gel, liquid, fibers<br />
• Systemic: antibiotics<br />
Three levels of regulation (prescription and OTC drugs)<br />
• Governmental level: Food and Drug administration<br />
o Evaluates both prescription and OTC<br />
o Therapeutic claims must be backed with proof<br />
o Protects consumers from useless or harmful products<br />
• Professional Level: ADA<br />
o Council on scientific affairs of the ADA<br />
• Consumer Level:<br />
o Advocacy groups<br />
o Federal trade Commission (FTC)<br />
ADA Seal of Acceptance
• Program is voluntary<br />
• Started in 1930 to “help consumers make wise choices”<br />
• Products submitted for seal must have independent, controlled<br />
studies to demonstrate effectiveness and safety<br />
• Seal is found on consumer products<br />
o Professional seal has been phased out<br />
o Professional product review replaces the ADA seal<br />
• Example: ADA seal for antiplaque/antigingivitis agents<br />
o Do not worry about the details<br />
• PER PRODUCT:<br />
o New product submission: 14,500$<br />
o Annual maintenance fee: 3000$<br />
Evaluating product claims – What to look for with the “research”<br />
• Published vs. non-published<br />
• Sponsor<br />
• Peer review<br />
o Not Peer Reviewed<br />
! Journal of clinical dentistry – 800$ per page to publish<br />
(Quick way for industry to publish)<br />
" NOT AS CREDITABLE<br />
o Reviewed:<br />
! JADA<br />
! Jour of <strong>Perio</strong>dontology<br />
! Jour of clinical periodontology<br />
• Length and duration<br />
Alcohol in mouthrinses/mouthwashes<br />
• Used as solvent for active ingredient<br />
o NOT ACTIVE INGREDIENT<br />
• High content can cause hyper-keratotic lesions<br />
• Possible link to oral cancer – inconclusive, heavily debated<br />
Chlorhexidine<br />
• 0.12% CHX<br />
• Peridex, <strong>Perio</strong>-grad and others
• Cytoplasmic poison – causes rupture of cell membrane allowing<br />
leakage<br />
• Binds to mucins, reducing pellicle formation and inhibiting<br />
colonization<br />
• Binds to bacteria, inhibiting their adhesion onto teeth<br />
• Substantivity: 12-24 hours (only one that’s long enough to merit<br />
mentioning(<br />
• 12% alcohol<br />
• 35-40% decrease in plaque and gingivitis<br />
Alcohol – free chlorhexidine<br />
• .12% CHX<br />
• Alcohol free<br />
• Therapeutically equivalent<br />
• Available only in dental offices<br />
CHX<br />
• Side effects<br />
o Staining<br />
o Altered taste - bad<br />
o Supragingival calculus<br />
o Mucositis<br />
• Dosage: 15ml, bid, 30 seconds each time<br />
• Most effect anti-plaque agent available at this time<br />
• Available with prescription<br />
• FDA approved – no longer carries ADA seal due to change in<br />
program<br />
• CHX on established biofilm will have only superficial effects<br />
• Is more effective when plaque is removed professionally prior to<br />
rinsing<br />
• The biofilm will adapt and protect itself from the effects of CHX<br />
• Inactivated by toothpaste – important to rinse well with water<br />
PRIOR to rinsing or wait 30 minutes before use<br />
• DO NOT rinse with water immediately after rinsing with CHX<br />
• Rec for patients who cannot or will not maintain adequate plaque<br />
control
• Post surgical cases<br />
• Caries protocol cases<br />
Phenolic Compounds – Listerine antiseptic and its generic equivalents<br />
• Active ingrediants: Essential Oils (GOT TO KNOW It)<br />
o Thymol<br />
o Eucalyptol<br />
o Methyl salicylate<br />
o Menthol<br />
• Org formula: 26.9%, cool mint 21.6%<br />
o Twice as much alcohol as CHX<br />
• Alters cell membranes causing leakage and cell death<br />
• 18-25% decrease in plaque and gingivitis<br />
o about half as effective as CHX (good to know)<br />
• low substantivity<br />
• Does it replace floss???<br />
o NO!!! Benefit is in conjunction with brushing and flossing<br />
• Side Effects<br />
o Bad taste<br />
o Burning sensation<br />
o Tooth staining (?) – not a big issue, but one study tried to<br />
show it<br />
• Dose: Rinse with 20ml, bid, for 30 sec<br />
• Before ADA seal – use with minor cuts and infectious dandruff<br />
Listerine Zero<br />
• Introduced in 2010<br />
• Claims:<br />
o “4 essential oil formula”<br />
o “for patients who want/need alcohol-free rinse”<br />
• BUT ITS NOT Listerine antiseptic without alcohol<br />
o It’s a cosmetic rinse – freshens breath<br />
• Essential oils is for flavoring – not a therapeutic concentration
Cetylpyridinium Chloride – CPC (breath freshners, not antimicrobial)<br />
• Ingredient in cosmetic mouthwashes<br />
• Quaternary Ammonium compound<br />
• Marginally effective in reduction of plaque / gingivitis<br />
• Little to no substantivity<br />
Pro-Health Rinse<br />
• .7%CPC<br />
• no alcohol<br />
• studies show plaque and gingivitis reduction comparable to Listerine<br />
• Mechanism of action: ruptures cell wall; also may alter bacterial<br />
metabolism and inhibit cell growth<br />
• Pro-health night – same product, different flavor<br />
CPC vs CHX<br />
• CPC binds to tooth structure and plaque, but not as strongly as CHX<br />
• CPC is rapidly released from binding sites so it is not as efficacious<br />
as CHX<br />
Viadent – former active ingredient was sanguinarine (blood root plant)<br />
• Mid to late 90’s, higher than normal incidence of leukoplakia seen<br />
• Sanguinarine determined to be the cause<br />
• Pts were 8-11 times more likely to develop leukoplakia<br />
• Lesions seen in former users – 5 years after use<br />
• Risk was highest in patients who used both mouth rinse and<br />
toothpaste<br />
Viadent – Now, new formulation without sanguinarine<br />
• Active ingredient: cetylpyridinium chloride (CPC)<br />
• Neutralizes malodor<br />
• No ADA seal<br />
• Cosmetic<br />
Plax<br />
• Marketed as pre-brushing rinse
• Ingredients: surfactants(detergents), sodium bicarbonate, glycerin,<br />
alcohol (7.5%)<br />
• Claims unsubstantiated with sound research<br />
• “the data provided do not support the use of PLAX dental rinse as<br />
part of an oral hygiene”<br />
Listerine Whitening pre-brushing rinse<br />
• Ingredients: water, 8% alcohol, hydrogen peroxide, sodium<br />
phosphate, sodium laurel sulfate<br />
• DOES NOT CONTAIN essential oils<br />
• DOES NOT REDUCE plaque and gingivitis<br />
• Doesn’t really whiten teeth either<br />
Crest Whitening Rinse<br />
• Not marketed to professionals<br />
o Doesn’t really whiten or kill bacteria or protect from future<br />
stains<br />
Triclosan – poor man’s CHX<br />
• Broad-spectrum antibacterial agent<br />
• Widely used in soaps etc<br />
• Anti-bacterial action not effected by sodium lauryl sulfate (SLS)<br />
• Found in mouth rinses in Europe<br />
• Found in some toothpastes in US<br />
• Mild to moderate reduction in plaque and gingivitis<br />
• Considered safe and effective for use in toothpastes and mouth<br />
rinses<br />
When do we recommend a mouth rinse<br />
• Determine need (caries, periodontal)<br />
• Caries Risk (OTC fluoride, Rx fluoride, or caries reduction protocol)<br />
• Patients who are unable to mechanically remove plaque<br />
• Patients who, despite their best attempts, need adjunctive<br />
measures<br />
• Patients with ANUG<br />
• Pre/post periodontal surgery
• Patients undergoing disease control therapy<br />
ADA has always stressed the importance of good oral hygiene by advising<br />
consumers to:<br />
• Brush your teeth twice a day with an ADA accepted fluoride<br />
toothpaste<br />
• Clean between teeth daily with an ADA accepted floss or an ADA<br />
accepted inter-dental cleaner<br />
• Eat a balanced diet and limit between meal snacks<br />
• Visit your dentist regularly for professional cleanings and oral<br />
exams<br />
• In addition to the basic oral hygiene recommendations, consumers<br />
should be aware of the oral health benefits of other ADA accepted<br />
procedure, such certain kinds of mouth rinses and toothpastes<br />
The council wants consumers to know that:<br />
• Use of an ADA accepted antimicrobial mouth rinse or toothpaste<br />
helps prevent and reduce plaque and gingivitis<br />
• Use of an ADA Accepted fluoride mouth rinse helps prevent and<br />
reduce tooth decay<br />
RECAP<br />
Therapeutic:<br />
• Peridex (CHX)<br />
• Listerine antiseptic<br />
• Crest pro health (.07% CPC)<br />
Cosmetic<br />
• Listerine zero or whitening<br />
• Viadent, Scope, Cepecol, Lavoris<br />
• Crest Whitening
Dentifrices<br />
11/9/10 2:02 PM<br />
In the beginning…<br />
• A little history on toothpaste<br />
o Earliest ref = 4 th century<br />
! Iris flowers, strawberries, bones<br />
o 18 th century<br />
! Burnt bread, charcoal, dragons blood, cinnamon, burnt<br />
alum<br />
Early Dentifrices<br />
• Toothpowders<br />
o 1 st on market for general use in 19 th century<br />
o primarily water, soap, flavor<br />
o home versions: chalk, pulverized brick, salt<br />
o pulverized charcoal also recommended for use<br />
o many of these did more harm than good<br />
• Toothpastes<br />
o Became available thanks to lead packaging<br />
! Plastic was used after WWII<br />
! Pump introduced in 1984 by Colgate<br />
! Separate stripes by Lever Bros (still used by some)<br />
! Mentadent used separate chambers for H 2 O 2 and baking<br />
powder – mostly a gimmick<br />
o Fluoride first added in 1914<br />
! 30’s ADA said not good<br />
! 50’s they changed and said it was good<br />
o By 1970: $355 million market<br />
! By 2012 expected to reach $12.7 billion worldwide<br />
• Dentifrices today: Powders, Pastes, Gels<br />
o Gels and pastes use same ingredients<br />
o Gels have more thickening agents vs pastes<br />
o Both equally effective<br />
What’s in Toothpaste?<br />
• Fluoride<br />
• Abrasive (20-40%)<br />
o Types
! Silicas<br />
" Silicon Dioxides, Aluminum oxides<br />
! Carbonates<br />
" Sodium bicarbonate, Chalk (calcium carbonate)<br />
! Phosphate<br />
" Calcium pyrophosphate, dicalcium phosphate<br />
dehydrate<br />
o Dulls teeth requiring a polishing agent to be added (restore<br />
luster)<br />
! Aluminum, calcium, tin, zirconium<br />
! Chalk and silica can both polish and abrade<br />
o Dependent on<br />
! Hardness of abrasive<br />
! Size (slides have mm, I think its µm)<br />
" Smaller (1mm) = polish<br />
" Larger (20mm) = abrasive<br />
! Shaper<br />
! If done wrong:<br />
" Brushing technique<br />
" Pressure on brush<br />
" Hardness of strokes<br />
• Humectant (20-40%)<br />
o Purpose: Maintain moisture, prevent evaporation and<br />
hardening, extends shelf life<br />
o Requires use of preservative to prevent bacterial growth<br />
o Top humectants:<br />
! Sorbitol, mannitol, glycerol, propylene glycol<br />
• Binder (2%)<br />
o Thickening or binding agents to stabilize formula<br />
! Prevents solids from settling out<br />
o Examples: Natural gums, synthetic cellulose, seaweed colloids<br />
• Foaming agent (1-2%)<br />
o Soaps<br />
! Used in early toothpastes as a cleansing agent<br />
" Foaming aided in loosening/removing debris<br />
! Disadvantages:
" Irritation to mucosal membrane<br />
" Nauseating taste difficult to mask<br />
" Incompatibility with other ingredients like calcium<br />
o Detergents<br />
! SLS – sodium lauryl sulfate – MOST WIDELY USED<br />
! Stable and compatible with other ingredients<br />
! Some antimicrobial properties<br />
! Flavor easy to mask<br />
! Low surface tension<br />
" Allows flow of dentifrice over teeth<br />
" Neutral pH<br />
! May cause irritation especially if patient has oral<br />
mucosal disease like herpes or allergies<br />
" Some dentifrices marketed as low SLS for this<br />
reason<br />
" SLS free: Biotene, pro-namel/reg Sensodyne<br />
• Flavoring agent (2%)<br />
o This is the main reason we use to pick our dentifrice<br />
! Product appeal linked to flavor<br />
o Flavor needs to be pleasant, immediate, last for a reasonable<br />
amount of time<br />
o Synthtic flavors (majority used): Spearmint, peppermint,<br />
wintergreen, cinnamon, vanilla, citrus<br />
o Essential ois: thymol, menthol, eucalyptol, methyl salicylate<br />
• Sweetners (2%)<br />
o Early Sweetners:<br />
! Sugar and honey – lower pH, cariogenic<br />
o Non-cariogenic sweetners:<br />
! Saccharin, cyclamate, xylitol<br />
! Sorbitol, mannitol, glycerin (also in humectant list)<br />
ADA stipulations<br />
• Must contain fluoride<br />
• Cannot contain sugar<br />
Therapeutic dentifrice – therapeutic agent – 5%
• Anti-caries<br />
• Anti-hypersensitivity<br />
• Anti-gingivitis<br />
Anti-Caries<br />
• First accepted therapeutic by ADA in 1960<br />
o Stannous fluoride – issue was it stained teeth<br />
• Fluoride- most common used therapeutic agent<br />
• Most OTC toothpastes are 1000ppm<br />
o Aim extra strength – 1500ppm<br />
• Types of fluoride<br />
o Sodium Fluoride (NaF) – 0.22% at 1100ppm<br />
o Sodium monofluorophosphate (MFP) – 0.76% at 1000ppm<br />
! Colgate<br />
o Stannous Fluoride (SnF 2 ) 0.4% at 1000ppm<br />
! Crest<br />
• Not all fluorinated toothpastes have anti-cavity effects – need<br />
certain amount<br />
o Max ppm established by FDA – 1450ppm<br />
o Crest clinical is 1415ppm<br />
• Stannous fluoride<br />
o Activity against caries, plaque, gingivitis<br />
o Used in Crest Pro-Health<br />
! Stabilized stannous fluoride – 0.454%<br />
! Sodium hexamataphophate<br />
! Research shows superior efficacy in<br />
" Antimicrobial<br />
" Plaque acidogenicity<br />
" Gingivitis/ gingival bleeding<br />
" Calculus control<br />
! Approved for multiple benefits<br />
Anti-hypersensitivity<br />
• Potassium nitrate – penetrates dentinal tubules causing<br />
depolarization of neurons and preventing repolarization
• Strontium Chloride and Sodium Citrate – blocking of exposed dental<br />
tubules<br />
• ADA seal for anti-hypersensitivity effects<br />
Anti-gingivitis<br />
• Stannous Fluoride – Crest Pro-Health<br />
• Triclosan – broad spectrum antibacterial agent – Colgate<br />
• Essential Oils – Listerine total care (same stuff that’s in their<br />
mouthwash, just more concentrated)<br />
Baking Soda Toothpastes<br />
• Contains:<br />
o Small amount of bicarbonate<br />
o Silicate<br />
o Standard fluoride compatible abrasives<br />
• ADA seal (if it has it) is NOT due to baking soda<br />
• Not any more effective than regular toothpaste<br />
Cosmetic<br />
• Purpose is to clean and polish the teeth<br />
• Tartar control toothpaste (not recognized by ADA)<br />
o Crystalline growth inhibitors interrupt process of<br />
mineralization<br />
o Soluble pyrophosphates<br />
o ADA seal NOT awarded for anti-calculus claim<br />
o Does NOT change tooth color<br />
• Whitners<br />
o May 1998: guidelines for whitening product implemented<br />
o Controls stain through<br />
! Physical method – abrasives (intermediate level)<br />
! Chemical method – surface active agents or bleaching<br />
agent/oxidizing agent<br />
" NO Bleaching agent in USA toothpastes<br />
! Polishing or chemical agents that remove stain<br />
" Hydrated silica, titanium dioxide, hydrogen<br />
peroxide, carbamide peroxide
! Whitening toothpaste may carry seal for removal of<br />
surface stain<br />
• Biotene and similar Products<br />
o Contains beneficial bio-active enzymes found in saliva<br />
! Helps to maintain oral environment<br />
! Helps provide protection against dry-mouth<br />
o Contains NO sodium lauryl sulfate (SLS)
11/9/10 2:02 PM<br />
3 types of staining:<br />
• Stain may adhere directly to the tooth<br />
• Stain is contained within the plaque and calculus<br />
• Stain is incorporated in the tooth structure<br />
Classified by location<br />
• Extrinsic – occurs on external surface of the tooth<br />
• Intrinsic – occurs within the tooth<br />
Classified by source<br />
• Exogenous – originate from sources outside the mouth<br />
o Can be intrinsic or extrinsic<br />
• Endogenous – originate from withing the tooth<br />
o ALWAYS INTRINSIC<br />
Stains are not considered etiologic factors for any dental disease. Therefore<br />
removal is for esthetic purposes only.<br />
Extrinsic Stains<br />
Yellow stain<br />
• Dull, yellowish discoloration of plaque<br />
• Common in all ages<br />
• Associated with presence of dental plaque<br />
• Usually related to poor oral hygiene<br />
• Etiology: usually food pigments<br />
Green stain<br />
• Light or yellowing green to a very dark green<br />
• Embedded in plaque<br />
• Usually found on facial cervical third of maxillary anteriors<br />
• Often covered with layer of gray debris or material alba<br />
• Dark green stain may become incorporated into tooth surface<br />
• May occur at any age, but primarily childhood<br />
• Etiology: poor oral hygiene, chromogenic bacteria and gingical<br />
bleeding
Black line stain<br />
• Forms along cervical third near gingival margin<br />
• Continuous or interrupted fine line, about 1mm wide with no<br />
thickness<br />
• Appears black at base of pits/fissures<br />
• Composed of microorganisms embedded in intermicrobial substance<br />
(gram positive rods, primarily actinomyces)<br />
• Attached via pellicle-like structure<br />
• All ages, more common in children and women<br />
• Tends to reform after removal<br />
• Predisposing factors: ?, natural tendency<br />
Tobacco stain<br />
• Light brown to dark leathery brown/black<br />
• Usually diffuse staining of dental plaque; may be incorporated into<br />
calculus<br />
• Heavier deposits (especially from chewing tobacco) may become<br />
intrinsic<br />
• Usually cervical 1/3, pits and fissures, frequently on lingual<br />
• Composition: tar products<br />
• Predisposing factors: natural tendencies<br />
Other brown stains<br />
• Stannous fluoride<br />
• Foodstuffs<br />
• Anti-plaque agents<br />
• Betel leaf<br />
Orange or red stain<br />
• Usually appear at cervical third<br />
• More frequently on anterior teeth rather than posterior<br />
• Rare<br />
• Etiology: chromogenic bacteria<br />
Intrinsic stains<br />
• Pulpless teeth (yellow-brown to gray to brown to bluish-black)
• Drugs (tetracycline)<br />
• Restorative materials<br />
• Imperfect tooth development (hypoplasia, fluorosis, genetics)