PERCUTANEOUS MANIPULATIONS OF THE BILIARY TRACT
PERCUTANEOUS MANIPULATIONS OF THE BILIARY TRACT
PERCUTANEOUS MANIPULATIONS OF THE BILIARY TRACT
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Cancer of the Pancreas<br />
<strong>PERCUTANEOUS</strong><br />
<strong>MANIPULATIONS</strong> <strong>OF</strong> <strong>THE</strong><br />
<strong>BILIARY</strong> <strong>TRACT</strong><br />
New Century<br />
New Teams<br />
New Techniques<br />
10/09/02<br />
CT, endoscopic US and biopsy -- adenocarcinoma of the pancreas in<br />
pancreatic head and neck.<br />
Extensive vascularity suggesting vascular invasion, collateral formation<br />
and neovascularity.<br />
The hepatic artery and PV appeared to enter the mass.<br />
The celiac trunk was free from tumor.<br />
The biliary and pancreatic ducts were dilated.<br />
ERCP stent placement and sphincterotomy unable to be done<br />
due to mass effect and vessels in area of ampulla.<br />
No mets to the liver at this time. Pt considered inoperable.<br />
4x3 loculated fluid collection in lesser sac, likely pseudocyst, and<br />
large spleen.<br />
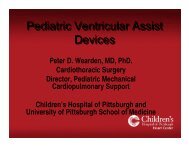
Jaundice and pruritis worsened.<br />
Approach for PTC?<br />
Technique for PTC?<br />
Catheter size?<br />
Stent?<br />
Immediate?<br />
Delayed?<br />
Uncovered?<br />
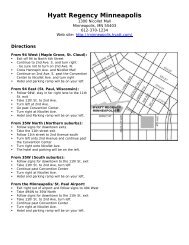
Left approach<br />
Easier echo<br />
Shorter tract<br />
More peripheral entry<br />
Less bleeding<br />
Stent placed<br />
Very slow flow<br />
Next step?<br />
The Left Approach<br />
Less Pain<br />
Less Dislodgement<br />
Easier care<br />
Stent ?? What type??
Balloon dilation to 10 mm<br />
Sudden give<br />
Stent opened<br />
What did the operator notice?<br />
What did anesthesia notice?<br />
What to do?<br />
So where is the bleeding from?<br />
Next step??<br />
Your Rx??<br />
Did you see the<br />
cavernous<br />
transformation<br />
that showed up<br />
on the<br />
cholangiogram?<br />
Acceptable?<br />
Next step?<br />
Patience can<br />
sometimes be a virtue<br />
Pt discharged day 5<br />
BP and Hgb stable<br />
Pruritis resolved<br />
Total Bili 1.8<br />
Tube capped<br />
When should tube be removed?
Percutaneous Transhepatic<br />
Cholangiography (PTC)<br />
Indications<br />
Percutaneous Transhepatic<br />
Cholangiography (PTC)<br />
Indications<br />
1. Not approachable with ERCP<br />
2. Define level of obstruction in patients with dilated bile<br />
ducts<br />
3. Evaluate for presence of suspected bile duct stones<br />
4. Determine etiology of cholangitis<br />
5. Evaluate suspected bile duct inflammatory disorders<br />
6. Demonstrate site of bile duct leak<br />
Dana R. Burke, et al. Quality Improvement Guidelines for<br />
Percutaneous Transhepatic Cholangiography and Biliary Drainage JVIR.<br />
2003, 14: 243S-246S.<br />
Hunter 2010<br />
GG – Hepatico-jejunostomy, elevated LFTs, stone<br />
CBD stricture<br />
CBD stone<br />
Biloma mass effect<br />
Post-Tx<br />
Anast<br />
Stricture<br />
Ascites<br />
Burke, et al<br />
PTC<br />
Success Rates<br />
Threshold<br />
(%)<br />
Opacify dilated ducts 95<br />
Opacify nondilated ducts 65
PTC<br />
Major Complications<br />
Burke, et al<br />
Reported<br />
rate %<br />
Suggested<br />
threshhold<br />
Sepsis, cholangitis, bile leak,<br />
hemorrhage or pneumothorax<br />
2 4<br />
PTCB<br />
Indications<br />
PTCB<br />
Indications<br />
1. Not approachable with ERCP<br />
2. Decompress obstructed biliary tree<br />
3. Dilate biliary strictures<br />
4. Remove bile duct stones<br />
5. Divert bile from and stent biliary leaks<br />
Dana R. Burke, et al, Quality Improvement Guidelines for<br />
Percutaneous Transhepatic Cholangiography and Biliary Drainage<br />
JVIR 2003 14: 243S-246S.<br />
Hunter 2010
GG – PSC<br />
Progressive worsening LFTs<br />
Candidate for liver Tx<br />
GG – Rendezvous<br />
For the L central duct<br />
GG – Low CBD<br />
Rendezvous<br />
GG- Fail to cross<br />
lower CBD stricture<br />
GG – Rendezvous<br />
R upper to<br />
R lower<br />
GG – R anterior<br />
R posterior
GG – R to L<br />
Rendevous<br />
GG – Rendezvous and push<br />
Both right sites to duodenum<br />
GG – ERCP/IR<br />
GG – 1 yr f/u MRCP<br />
PTBD<br />
MOST COMMON USES<br />
• Laparoscopic duct avulsion<br />
• Severe bacterial cholangitis<br />
• Roux-N-Y loop<br />
– Transplant<br />
– Bariatric<br />
– Whipple<br />
• Severe lower or upper CBD stricture<br />
– Cholangio and other carcinomas<br />
– Sclerosing cholangitis<br />
• Duodenal problems<br />
– Stricture<br />
– Diverticulum<br />
– Edema<br />
PTCB<br />
Success Rates<br />
Burke, et al<br />
Procedural success<br />
Cannulation<br />
Dilated ducts 95%<br />
Nondilated ducts 70%<br />
Internal drainage (tube or stent) 90%<br />
Stone removal 90%<br />
Patency success<br />
Stricture dilatation (benign)<br />
Sclerosing cholangitis *<br />
Other *<br />
Palliative stents for malignant disease 50% @ 6m<br />
LAPARASOPIC<br />
COMMON BILE<br />
DUCT INJURY<br />
The ultimate<br />
multi-specialty case
11/13/03 Laparoscopic cholecystectomy,<br />
“uncomplicated”<br />
– 24 hrs later, abdominal pain, fever, rising WBC<br />
11/15/03 bile leak,<br />
missed on echo<br />
found on HIDA<br />
11/16/03 percutaneous drainage requested<br />
NEXT<br />
STEP?<br />
Try to cross the obstruction,<br />
“pop” it open and<br />
stent it for a VICTORY!!!<br />
Operating physician called<br />
“Weck” clip used to clip the<br />
“cystic duct”<br />
So now what?<br />
IR/Surgery team<br />
Clip removed<br />
Catheter advanced - post-op drain<br />
Bile leak stopped<br />
Biloma drain removed<br />
12/29/03 Re-admitted for<br />
BRBPR and hematemesis<br />
with a drop in hemoglobin to<br />
6.5<br />
Treatment???<br />
Resuscitated, bleeding<br />
stopped
Cross the leak<br />
“Get distal”<br />
Treating the Damaged<br />
Bile Duct<br />
Incidence of stricture<br />
Post Weck clip ?<br />
Post surgical repair of clip site ??<br />
Post biloma ???<br />
Assuming that 3-4 months of stenting would be<br />
optimal --- How to do it ????<br />
ERCP stents<br />
came out one<br />
month later<br />
Which is why<br />
combined procedures<br />
Are worthwhile<br />
Severe R side<br />
Cath site pain<br />
PTBD complications<br />
0.7% to 10%<br />
• Hemorrhage/hemobilia<br />
• Sepsis<br />
• Bile peritonitis (catheter dislodgement) - Right<br />
• Persistent pain at puncture site - Right<br />
• Pneumothorax - Right<br />
• Pleural effusion - Right<br />
• Pancreatitis<br />
PTBD<br />
Contraindications – all relative<br />
• Platelets < 50,000<br />
• INR prolonged<br />
• Ascites<br />
• Advanced metastatic disease<br />
– Life expectancy
PTCB DOING <strong>THE</strong> ERCP THING<br />
• Stone removal<br />
– 212 patients<br />
• 139 PTBD --- 73 T-tube tract<br />
• 8-10 Fr sheath<br />
• Dilate sphincter 10-12 mm (up to 16-18 mm)<br />
• 11.5 mm Fogarty balloon over super-stiff wire<br />
– Push or push plus flush<br />
– 90.4% technical success, 93% 2nd try<br />
• Mild pancreatitis 3/212<br />
• Severe arterial bleed 4/212 , temp venous bleed 6/212<br />
• Less bleeding, pancreatitis, cholangitis, and<br />
preserved sphincter function<br />
• Garcia L, AJR 2004; 182:663-70<br />
PTCB FOR<br />
CHOLANGIOCARCINOMA<br />
• Primarily for Type 3 and 4 tumors<br />
• ERCP success rates vary widely<br />
– 15% (*) - 100% (**)<br />
– Local expertise decides<br />
– PTCB less sepsis esp c/w failed attempt at ERCP<br />
• High quality MRCP planning<br />
• “Primary” duct target<br />
– Bilateral drainage has in past survived longer than unilateral (***)<br />
• Biopsy successful in 70-90% via tract with or without a<br />
choledochoscope (****)<br />
• * Lefebvre JF, Dig Dis Sci, 1992<br />
• ** Rauws EA, Eur J Surg, 2001<br />
• *** Deviere J, Gastrointest Endosc, 1988<br />
• *** Chou CY, Hepatogastroenterology, 1997 and 1998<br />
Metallic Stent Placement<br />
• Obstruction due to unresectable or<br />
inoperable malignancy<br />
• Postoperative tumor recurrence<br />
• Postoperative complications<br />
Tailored Stenting<br />
“T, Y, X”<br />
• Results in drainage of the entire ductal<br />
system<br />
• Requires bilateral access or<br />
overlapping of stents in one duct<br />
• No proven benefit over single side stent<br />
– Theoretically should be improvement in<br />
• Cholangitis<br />
• Abcess rate<br />
• LFT normalization
Metal Stent Outcomes<br />
• Clinical success<br />
– Serum bilirubin decreases 63-100%<br />
• Quality of survival<br />
– Solves hydration and K + loss problems<br />
– Physiological antegrade bile flow<br />
– Shortens hospitalization time<br />
• Stent patency — 58 to 93% over 3 - 12 months<br />
• Reintervention rate decreased vs plastic<br />
• Nitinol (78%) better 6 mo patency than Z-<br />
stents (30%) and tantalum (20%)<br />
– (Rossi P, JVIR, 1994)<br />
Lee KH. et al. Biliary intervention for cholangiocarcinoma.<br />
Abdominal Imaging. 29(5):581-9, 2004 Sep-Oct.<br />
PTFE COVERED STENTS<br />
FOR MALIGNANT <strong>BILIARY</strong> OBSTRUCTION<br />
• Prospective multicenter safety and efficacy<br />
trial in Europe<br />
• 42 pts -- 38 unilateral - 4 bilateral stents<br />
• Technical success 100%<br />
• 4/42 (10%) branch obstruction<br />
• 2/42 (5%) complications<br />
– Entry site bile leak (1) and hematoma (1)<br />
– Only 1 mild case of lab pancreatitis (not complication)<br />
• 8/41 (20%) 30 day mortality - none biliary<br />
• Median primary patency 138 days<br />
• 6/41 (15%) obstruction mean 106 days<br />
• 3, 6,12 mo primary patency 90%, 76%, 76%<br />
– Schoder M et al, Radiol 2002; 225:35-42<br />
COVERED VS UNCOVERED STENTS<br />
DOES CANCER TYPE MATTER?<br />
• 73 patients with cancer<br />
– Covered stents (CS) 42, Uncovered stents (US) 31<br />
• Cholangio ca 12, gb ca 22, pancreas ca 12<br />
– 6 mo patency CS US<br />
• Overall 81% 50%<br />
– Mean time of patency CS US<br />
• Cholangio ca 15 mo 28 mo<br />
• Gb ca 13 mo 3 mo<br />
• Pancreas ca 12 mo 10 mo<br />
– Kawamoto H, Hepato-gastroenterology, 2005; 52(65): 1351-6<br />
IR Management of<br />
Liver Transplant Complications<br />
• Most recipients will have a complication<br />
– Arterial<br />
• Thrombosis 6.8% (high mortality)<br />
• Steal 5.9%<br />
– Portal 1.8%<br />
– Caval
Biliary Complications of Liver Transplants<br />
Improvements in Dilation Technique<br />
• Possibly better with cutting balloon<br />
– 12 pts, 49 dilations with technical success of<br />
100%, 90% 93% for<br />
primary, recurrent, and fail non-cutting balloon<br />
• Saad, WEA, JVIR, 2006<br />
• Success much less at 12 months with arterial<br />
stenosis or occlusion<br />
– 0% with arterial problem<br />
– 45% with patent artery<br />
• Saad WEA, JVIR, 2005<br />
Late Biliary Complications of<br />
LIVER TRANSPLANTS<br />
• Mechanisms<br />
– Ischemia<br />
• 85% associated with arterial problems<br />
– CMV infection<br />
– Cold ischemia >12 h<br />
• Lesions are diffuse, extensive<br />
– Chronic repeated dilations<br />
• Sludge, debris<br />
– Treatment: Flushing (percutaneous) or lithotripsy<br />
(endoscopic) or rheolytic (Loehr SP, AJR 2002)<br />
– Risks: Infection, sepsis<br />
Denys A, IR in the Management of Complications after Liver Transplantation<br />
Eur Radiol (2004) 14:431<br />
TREATING REFRACTORY<br />
TRANSPLANT STENOSES<br />
JS – Age 1-12<br />
LFTs always a<br />
little elevated<br />
• 8 patients -- 9 stenoses<br />
– 33 previous interventions<br />
• Dilation 27<br />
• Prolonged catheters 3, surgery 1, metal stent 1, atherectomy 1<br />
– 11 home made “Z-stent” plus gortex stent-grafts with<br />
gortex “tethers”<br />
• 2 left in 1 pt due to clinical deterioration, patent at autopsy<br />
• 9 planned for retrieval in 7 patients -- 8 stenoses<br />
– 9/9 retrieved successfully -- 2 with difficulty<br />
– 4/8 stenoses recur in 7 patients (40,90,90,90 %)<br />
» 1/7 to surgery<br />
» 6/7 observed, all still asymptomatic mean 12 mo later<br />
• 5 migrate or removed 1-3 months with reocclusion in all<br />
– Petersen B, JVIR 2000; 11:919-20<br />
Dr J. Garcia<br />
Says<br />
Be a team,<br />
Play together,<br />
Forget yourself.<br />
Remember,<br />
Patients First<br />
Or maybe,<br />
Second<br />
After Love<br />
We are nothing<br />
If we do not<br />
Sacrifice<br />
Some part<br />
Of ourself<br />
To every song<br />
We sing