Medicare Part B Newsline April 2012 - Cahaba GBA
Medicare Part B Newsline April 2012 - Cahaba GBA
Medicare Part B Newsline April 2012 - Cahaba GBA
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>April</strong> <strong>2012</strong><br />
This bulletin should be shared with all health care practitioners and managerial members of the provider/supplier staff.<br />
Bulletins are available at no cost from our Web site at https://www.cahabagba.com.<br />
News From <strong>Cahaba</strong> <strong>GBA</strong><br />
Disclaimer………………….……………………....….… 2<br />
Please Route…………………………………………….. 3<br />
General <strong>Medicare</strong> Questions for <strong>Medicare</strong> Recipients….. 3<br />
Holiday Closure Schedule……………………………..... 4<br />
Provider Contact Center (PCC) Training Schedule……... 5<br />
Provider Contact Center (PCC) Telephone Numbers…... 5<br />
Using the Interactive Voice Response (IVR) System for<br />
Claim Status and Eligibility Requests......……….........… 6<br />
<strong>Medicare</strong> Health Insurance Claim (HIC) Number……… 7<br />
<strong>Cahaba</strong>’s E-Mail Notification Service………...………… 8<br />
<strong>Cahaba</strong> University………………………………………. 9<br />
AL-Top Five Reasons for Claim Rejections- Feb <strong>2012</strong>... 10<br />
GA-Top Five Reasons for Claim Rejections- Feb <strong>2012</strong>... 11<br />
MS-Top Five Reasons for Claim Rejections- Feb <strong>2012</strong>... 12<br />
TN-Top Five Reasons for Claim Rejections- Feb <strong>2012</strong>.... 13<br />
AL-Top 277CA Claim Rejections- Feb <strong>2012</strong>……..……. 14<br />
GA-Top 277CA Claim Rejections- Feb <strong>2012</strong>…………... 17<br />
MS-Top 277CA Claim Rejections- Feb <strong>2012</strong>…………... 20<br />
TN-Top 277CA Claim Rejections- Feb <strong>2012</strong>..…………. 22<br />
<strong>Medicare</strong> Coverage Database (MCD) Article:<br />
Educational Article- Chiropractor Services- Retired…… 25<br />
Local Coverage Determinations- Comment Period for<br />
Draft LCDs…………………………………………….... 26<br />
Claim Specific CERT Errors- February <strong>2012</strong>…………... 27<br />
<strong>Medicare</strong> B <strong>Newsline</strong> Quality Survey……….….............. 41<br />
News From CMS<br />
News Flash Messages From CMS………….……….…. 28<br />
Intensive Behavioral Therapy (IBT) for Obesity-<br />
Revised………………………………………………… 31<br />
Processing Form CMS-855O Submissions Instructions.. 37<br />
Revised Remittance Advice Remark Code (RARC)<br />
N103 when Denying Services Furnished to Federally<br />
Incarcerated Beneficiaries-Revised……………………. 39<br />
General <strong>Medicare</strong> Questions for <strong>Medicare</strong><br />
Recipients<br />
Do some of your patients have questions regarding their<br />
<strong>Medicare</strong> benefits and you are not sure how to answer?<br />
<strong>Medicare</strong> recipients should call 1-800-MEDICARE (1-800-<br />
633-4227) for all questions related to <strong>Medicare</strong> services.<br />
Questions regarding specific claims will be automatically<br />
routed to the appropriate <strong>Medicare</strong> contractor’s call center for<br />
response.<br />
Key For Icons<br />
All Providers<br />
Claims<br />
End Stage Renal Disease (ESRD)<br />
Radiology<br />
Skilled Nursing Facility (SNF)<br />
The <strong>Medicare</strong> B <strong>Newsline</strong> provides information for those providers who submit claims to <strong>Cahaba</strong> Government Benefit<br />
Administrators ® , LLC. The CPT codes, descriptors and other data only are copyright © 2011 American Medical Association. All<br />
rights reserved. Applicable FARS/DFARS apply.
Disclaimer<br />
This educational material was prepared as a tool to assist <strong>Medicare</strong> providers and other interested parties and is not intended to<br />
grant rights or impose obligations. Although every reasonable effort has been made to assure the accuracy of the information<br />
within this module, the ultimate responsibility for the correct submission of claims lies with the provider of services. <strong>Cahaba</strong><br />
<strong>GBA</strong>, LLC employees, agents, and staff make no representation, warranty, or guarantee that this compilation of <strong>Medicare</strong><br />
information is error-free and will bear no responsibility or liability for the results or consequences of the use of these materials.<br />
This publication is a general summary that explains certain aspects of the <strong>Medicare</strong> Program, but is not a legal document. The<br />
official <strong>Medicare</strong> Program provisions are contained in the relevant laws, regulations, and rulings.<br />
We encourage users to review the specific statues, regulations and other interpretive materials for a full and accurate statement<br />
of their contents. Although this material is not copyrighted, CMS prohibits reproduction for profit making purposes.<br />
American Medical Association Notice and Disclaimer<br />
CPT codes, descriptors and other data only are Copyright 2011 American Medical Association. All rights reserved.<br />
ICD-9 Notice<br />
The ICD-9-CM codes and descriptors used in this material are copyright 2011 under uniform copyright convention. All rights<br />
reserved.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 2
News From <strong>Cahaba</strong> <strong>GBA</strong> for All <strong>Part</strong> B Providers<br />
Please Route<br />
Remember that this newsletter, and all other <strong>Medicare</strong> publications, serves as your official notice of<br />
<strong>Medicare</strong> coverage and billing information. If you have any questions about the information included in this<br />
newsletter, please call your Provider Contact Center.<br />
This bulletin shall be shared with all health care practitioners and managerial members of your provider<br />
staff. Bulletins are available at no cost from our website<br />
https://www.cahabagba.com/part_b/education_and_outreach/newsletters/index.htm.<br />
Routing List<br />
Provider/Supplier<br />
Administrator<br />
Office/Clinic Manager<br />
Medical Personnel<br />
Billing/Insurance Staff<br />
Other Additional Staff<br />
General <strong>Medicare</strong> Questions for <strong>Medicare</strong> Recipients<br />
Do some of your patients have questions regarding their <strong>Medicare</strong> benefits and you are not sure how to<br />
answer? <strong>Medicare</strong> recipients should call 1-800-MEDICARE (1-800-633-4227) for all questions related to<br />
<strong>Medicare</strong> services. Questions regarding specific claims will be automatically routed to the appropriate<br />
<strong>Medicare</strong> contractor’s call center for response. Please do not ask your patients to contact <strong>Medicare</strong> on<br />
a claim that you accepted assignment on.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 3
Holiday Closure Schedule-<strong>2012</strong><br />
<strong>Cahaba</strong> <strong>GBA</strong>’s <strong>Medicare</strong> offices in Birmingham, AL; Douglasville, GA, Savannah, GA; and Chattanooga,<br />
TN are closed on the following days listed below in <strong>2012</strong>. In addition, all <strong>Medicare</strong> Provider Contact<br />
Centers (PCC) close on federal holidays for continuing education training; therefore, customer service<br />
representatives will not be available on those days to receive your calls.<br />
Holiday / Date<br />
New Year’s Day Observed<br />
January 2, <strong>2012</strong><br />
Monday<br />
Martin Luther King Birthday<br />
January 16, <strong>2012</strong><br />
Monday<br />
President’s Day<br />
February 20, <strong>2012</strong><br />
Monday<br />
Good Friday<br />
<strong>April</strong> 6, <strong>2012</strong><br />
Friday<br />
Memorial Day<br />
May 28, <strong>2012</strong><br />
Monday<br />
Independence Day<br />
July 4, <strong>2012</strong><br />
Wednesday<br />
Labor Day<br />
September 3, <strong>2012</strong><br />
Monday<br />
Columbus Day<br />
October 8, <strong>2012</strong><br />
Monday<br />
Veterans Day Observed<br />
November 12, <strong>2012</strong><br />
Monday<br />
Thanksgiving<br />
November 22-23, <strong>2012</strong><br />
Thursday/Friday<br />
Christmas<br />
December 24-25, <strong>2012</strong><br />
Monday/Tuesday<br />
New Year’s Day<br />
January 1, 2013<br />
Tuesday<br />
Closure Schedule<br />
All Offices Closed<br />
All Offices Closed<br />
PCC Closed for Training<br />
All Offices Closed<br />
All Offices Closed<br />
All Offices Closed<br />
All Offices Closed<br />
PCC Closed for Training<br />
PCC Closed for Training<br />
All Offices Closed<br />
All Offices Closed<br />
All Offices Closed<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 4
Provider Contact Center– Training Schedule<br />
<strong>Medicare</strong> is a continuously changing program, and it is important that we provide correct and accurate<br />
answers to your questions. To better serve the provider community, the Centers for <strong>Medicare</strong> & Medicaid<br />
Services (CMS) allows the Provider Contact Centers the opportunity to offer training to our Customer<br />
Service Representatives (CSRs). Listed below are the dates and times the Provider Contact Center will be<br />
closed for training.<br />
PCC Training Dates<br />
Friday, <strong>April</strong> 13, <strong>2012</strong><br />
Friday, <strong>April</strong> 20, <strong>2012</strong><br />
Friday, <strong>April</strong> 27, <strong>2012</strong><br />
Time<br />
9:30 a.m.- 11:30 a.m. CT/10:30 a.m.- 12:30 p.m. ET<br />
9:30 a.m.- 11:30 a.m. CT/10:30 a.m.- 12:30 p.m. ET<br />
9:30 a.m.- 11:30 a.m. CT/10:30 a.m.- 12:30 p.m. ET<br />
Provider Contact Center Telephone Numbers<br />
Alabama B, Georgia B, and Tennessee B: 877 567-7271<br />
Mississippi B: 866 419-9454<br />
Our Interactive Voice Response (IVR) system is designed to assist providers in obtaining answers to<br />
numerous issues through self-service options. Options on our IVR include information regarding patient<br />
eligibility, checks, claims, deductible and other general information. Please note that our Customer Service<br />
Representatives (CSRs) are available to answer questions that cannot be answered by the IVR. CSRs are<br />
physically located in Birmingham, Alabama and Savannah, Georgia. When your call is received, it is routed<br />
to the next available representative. CSRs are available Monday through Friday 8:00 a.m. until 4:00 p.m. in<br />
your time zone.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 5
Using the Interactive Voice Response (IVR) System for Claim Status and<br />
Eligibility Requests<br />
<strong>Cahaba</strong> Government Benefit Administrators®, LLC is experiencing a high volume of providers who are<br />
opting out of the Interactive Voice Response (IVR) system to speak to a Customer Service Representative<br />
(CSR) for information that can be accessed through the IVR.<br />
The Centers for <strong>Medicare</strong> and Medicaid Services (CMS) Internet Only Manual (IOM) Chapter 6 Section<br />
50.1 states:<br />
“Providers shall be required to use IVRs to access claim status and beneficiary eligibility<br />
information. CSRs shall refer providers back to the IVR if they have questions about claims status<br />
or eligibility that can be handled by the IVR. CSRs may provide claims status and/or eligibility<br />
information if it is clear that the provider cannot access the information through the IVR because the<br />
IVR is not functioning.”<br />
If you are requesting whether <strong>Cahaba</strong> has received a claim or if a claim has finalized, this is<br />
considered a claim status request.<br />
In addition, according to IOM Chapter 6 Section 80.3.4, “If a CSR or written inquiry correspondent receives<br />
an inquiry about information that can be found on a Remittance Advice (RA), the CSR/correspondent<br />
should take the opportunity to educate the inquirer on how to read the RA, in an effort to encourage the use<br />
of self-service. The CSR/correspondent should advise the inquirer that the RA is needed in order to answer<br />
any questions for which answers are available on the RA. Providers should also be advised that any billing<br />
staff or representatives that make inquiries on his/her behalf will need a copy of the RA.”<br />
<strong>Cahaba</strong> CSRs have visibility as to the path the provider takes in the IVR and/or whether they opt out to<br />
speak with a representative up front. The CSR will instruct the provider to call back and utilize the IVR if<br />
they did not attempt to use this self service option as required by CMS.<br />
Provider Contact Center (PCC)<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 6
<strong>Medicare</strong> Health Insurance Claim (HIC) Number<br />
A <strong>Medicare</strong> card is issued to every person who is entitled to <strong>Medicare</strong> benefits and may be identified by its red, white<br />
and blue coloring. This card identifies the <strong>Medicare</strong> beneficiary and includes the following information:<br />
Name (exactly as it appears on the Social Security records);<br />
<strong>Medicare</strong> Health Insurance Claim (HIC) number;<br />
Beginning date of <strong>Medicare</strong> entitlement for hospital and/or medical insurance;<br />
Sex and Beneficiary's signature.<br />
Three of the top five reasons for claim rejection in any given month are for:<br />
The last name submitted for the beneficiary does not match the last name we have on record for the HIC<br />
number on the claim. The beneficiary's last name must include apostrophes, spaces, hyphens, etc., if they<br />
appear in the beneficiary's last name on his or her <strong>Medicare</strong> card.<br />
The first name submitted for the beneficiary does not match the first name we have on record for the HIC<br />
number on the claim. The beneficiary's first name must appear as it does on the beneficiary's <strong>Medicare</strong><br />
card. This includes spaces, hyphens, apostrophes, etc.<br />
The HIC number not matching the name we have on record. The <strong>Medicare</strong> Claim Number must appear on<br />
the claim exactly as it does on the beneficiary’s card, without the dashes and with no spaces.<br />
It is extremely important that you submit the patient’s complete name and HIC number to <strong>Medicare</strong> or any other<br />
health care provider you use (i.e. clinical laboratories, radiology imaging groups, or outpatient therapy providers,<br />
etc.). This will ensure that those providers have the correct patient information to file their claims as well.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 7
<strong>Cahaba</strong>’s E-mail Notification Service Subscription Process<br />
<strong>Cahaba</strong> <strong>GBA</strong> recently implemented changes that simplify the process in which providers subscribe to our e-<br />
mail notification service (Listserv). New members simply provide their name, city, state, zip code, e-mail<br />
address, and an optional password. In addition, they can select from two different lists to subscribe to:<br />
• J10 <strong>Part</strong> A News<br />
• J10 <strong>Part</strong> B News*<br />
Once you are a member, you can edit your profile to:<br />
• unsubscribe from all lists<br />
• subscribe to additional lists<br />
• update your e-mail address<br />
• change your name or address information<br />
• change what <strong>Cahaba</strong> lists you are subscribed to.<br />
Already a Member?<br />
If you enrolled to <strong>Cahaba</strong>’s Listserv prior to November 1, 2009, you will continue to receive messages.<br />
However, depending on the selections you made on the subscription form when you originally enrolled, you<br />
may receive messages from more than one <strong>Cahaba</strong> list. To change the list you are subscribed to, access the<br />
“Edit Your E-mail Notification Service Member Profile” Web page to review and edit your profile.<br />
In order to ensure that you receive your subscription emails and announcements from <strong>Cahaba</strong> <strong>GBA</strong>, please<br />
add us to your contact lists, adjust your spam settings, or follow the instructions from your email provider<br />
on how to prevent our emails from being marked “Spam” or “Junk Mail”.<br />
*Mississippi <strong>Medicare</strong> <strong>Part</strong> B providers will choose J10 <strong>Part</strong> B News for their selection to receive <strong>Medicare</strong><br />
<strong>Part</strong> B information.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 8
<strong>Cahaba</strong> University<br />
<strong>Cahaba</strong> University is an educational program designed to provide a broad variety of <strong>Medicare</strong> related<br />
training to meet the needs of <strong>Medicare</strong> health care providers and suppliers. It is powered by Centra, a<br />
learning management system that will allow registered users to manage their own learning. <strong>Cahaba</strong><br />
University allows for a blended e-learning environment. Blended means that users are allowed to register for<br />
Webinars, teleconferences, as well as assign self-paced learning tracks. It also provides centralized<br />
management and access to content created by the Provider Outreach and Education department for the<br />
provider community.<br />
Our staff of well-trained professionals wants every provider to be pleased with their learning experience.<br />
We know you’re just as concerned about your claims being processed for your facility as you are about the<br />
quality of care administered to your <strong>Medicare</strong> patients. That is why we always try to provide additional<br />
education and outreach activities to help improve this process.<br />
All providers are encouraged to create a user profile. Click the “Create a new account” link, and then select<br />
either a <strong>Part</strong> A or <strong>Part</strong> B account. You must create a username and password to login. Make sure all the<br />
appropriate fields are completed. Once the account is created, log in using your new user name and<br />
password. Remember, your username and password is case-sensitive!<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 9
Alabama <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Five Reasons for EDI Claim Rejections for February <strong>2012</strong><br />
Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, along<br />
with claims that were rejected and the reason for the rejection. Referring to this report will allow you to<br />
correct and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will also<br />
become aware of any major problems with your claims so they can be corrected before they create an<br />
interruption in your cash flow. Audit trail reports are available the next business day for files that are<br />
received before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your software<br />
vendor, billing service, or clearing house.<br />
See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that might<br />
be referenced in an edit.<br />
In order to increase the number of claims that successfully pass through audit trails and into processing<br />
<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For the<br />
month of February <strong>2012</strong>, these are:<br />
Claim Description<br />
Rejection<br />
382 NPI REQUIRED IN LOOP : XXXXXX WHEN<br />
PROVIDER IDENTI<br />
Provider information was submitted in the indicated loop but<br />
there was no XX qualifier in the NM108 for that provider.<br />
434 PROC CODE REQUIRES REFERRING NPI<br />
Procedure code billed was for a diagnostic procedure such as<br />
an x-ray or lab work which requires the NPI of the ordering<br />
physician, or a consultation, which requires the NPI of the<br />
referring physician, and this was not submitted on the claim.<br />
421 DIAG CODE (XXXXX) INVALID FOR DATE SVC<br />
The date of service was outside of the effective date range of<br />
the diagnosis code used. The invalid diagnosis code will<br />
appear inside the parenthesis.<br />
377 PAID & ADJUSTMENT AMOUNTS DO NOT EQUAL<br />
CLAIM CHARG<br />
The claim was submitted as <strong>Medicare</strong> Secondary Payer but the<br />
primary paid amount plus the primary adjustment amounts do<br />
not equal the total claim charge.<br />
888 INSTREAM REJECTION<br />
There was a problem involving HIPAA required loops,<br />
segments, or values. The specific loop will be identified, for<br />
example, 'ELEMENT N401 (D.E. 19) AT COL. 4 IS<br />
MISSING, THOUGH MARKED "MUST BE USED"<br />
(LOOP:2010BA POS:3140)'. The number after 'POS'<br />
indicates the position in the file where the error occurred<br />
Number of<br />
Claims<br />
1,139<br />
506<br />
497<br />
330<br />
246<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 10
Georgia <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Five Reasons for EDI Claim Rejections for February <strong>2012</strong><br />
Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, along<br />
with claims that were rejected and the reason for the rejection. Referring to this report will allow you to<br />
correct and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will also<br />
become aware of any major problems with your claims so they can be corrected before they create an<br />
interruption in your cash flow. Audit trail reports are available the next business day for files that are<br />
received before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your software<br />
vendor, billing service, or clearing house.<br />
See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that might<br />
be referenced in an edit.<br />
In order to increase the number of claims that successfully pass through audit trails and into processing<br />
<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For the<br />
month of February <strong>2012</strong>, these are:<br />
Claim Description<br />
Rejection<br />
888 INSTREAM REJECTION<br />
There was a problem involving HIPAA required loops,<br />
segments, or values. The specific loop will be identified, for<br />
example, 'ELEMENT N401 (D.E. 19) AT COL. 4 IS MISSING,<br />
THOUGH MARKED "MUST BE USED" (LOOP:2010BA<br />
POS:3140)'. The number after 'POS' indicates the position in the<br />
file where the error occurred<br />
421 DIAG CODE (XXXXX) INVALID FOR DATE SVC<br />
The date of service was outside of the effective date range of the<br />
diagnosis code used. The invalid diagnosis code will appear<br />
inside the parenthesis.<br />
207 INVALID HIC NUMBER SUFFIX<br />
The suffix in the Health Insurance Claim (HIC) number<br />
submitted for the beneficiary is invalid. For an explanation of<br />
HIC numbers and suffixes please visit<br />
https://www.cahabagba.com/part_b/education_and_outreach/gen<br />
eral_billing_info/hic_suffixes.htm.<br />
434 PROC CODE REQUIRES REFERRING NPI<br />
Procedure code billed was for a diagnostic procedure such as an<br />
x-ray or lab work which requires the NPI of the ordering<br />
physician, or a consultation, which requires the NPI of the<br />
referring physician, and this was not submitted on the claim.<br />
375 PAID AMOUNT CANNOT BE GREATER THAN<br />
ALLOWED AMOUNT<br />
Claim was submitted as <strong>Medicare</strong> Secondary Payer (MSP) and the<br />
primary paid amount submitted was greater than the primary allowed<br />
amount.<br />
Number of<br />
Claims<br />
1,668<br />
1,121<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 11<br />
726<br />
596<br />
380
Mississippi <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Five Reasons for EDI Claim Rejections for February <strong>2012</strong><br />
Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, along<br />
with claims that were rejected and the reason for the rejection. Referring to this report will allow you to<br />
correct and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will also<br />
become aware of any major problems with your claims so they can be corrected before they create an<br />
interruption in your cash flow. Audit trail reports are available the next business day for files that are<br />
received before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your software<br />
vendor, billing service, or clearing house.<br />
See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that might<br />
be referenced in an edit.<br />
In order to increase the number of claims that successfully pass through audit trails and into processing<br />
<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For the<br />
month of February <strong>2012</strong>, these are:<br />
Claim Description<br />
Rejection<br />
888 INSTREAM REJECTION<br />
There was a problem involving HIPAA required loops, segments, or<br />
values. The specific loop will be identified, for example, 'ELEMENT<br />
N401 (D.E. 19) AT COL. 4 IS MISSING, THOUGH MARKED<br />
"MUST BE USED" (LOOP:2010BA POS:3140)'. The number after<br />
'POS' indicates the position in the file where the error occurred. If you<br />
need help locating specific positions in your 4010A1 file here is an<br />
article explaining one way you can do this:<br />
http://www.cahabagba.com/part_b/edi/hipaa_identifying_your_errors.<br />
htm.<br />
421 DIAG CODE (XXXXX) INVALID FOR DATE SVC<br />
The date of service was outside of the effective date range of the<br />
diagnosis code used. The invalid diagnosis code will appear inside the<br />
parenthesis.<br />
207 INVALID HIC NUMBER SUFFIX<br />
The suffix submitted for the beneficiary’s HIC number is invalid. For a<br />
list of valid suffixes and their meanings visit this article on our<br />
website;<br />
https://www.cahabagba.com/part_b/education_and_outreach/general_b<br />
illing_info/hic_suffixes.htm<br />
434 PROC CODE REQUIRES REFERRING NPI<br />
Procedure code billed was for a diagnostic procedure such as an x-ray<br />
or lab work which requires the NPI of the ordering physician, or a<br />
consultation, which requires the NPI of the referring physician, and<br />
this was not submitted on the claim<br />
202 RAILROAD<br />
The beneficiary’s HIC contains an alphabetic prefix, indicating that the<br />
patient is a Railroad Retiree. The claim should be submitted to<br />
Railroad <strong>Medicare</strong>.<br />
Number of<br />
Claims<br />
430<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 12<br />
361<br />
141<br />
110<br />
95
Tennessee <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Five Reasons for EDI Claim Rejections for February <strong>2012</strong><br />
Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, along<br />
with claims that were rejected and the reason for the rejection. Referring to this report will allow you to<br />
correct and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will also<br />
become aware of any major problems with your claims so they can be corrected before they create an<br />
interruption in your cash flow. Audit trail reports are available the next business day for files that are<br />
received before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your software<br />
vendor, billing service, or clearing house.<br />
See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that might<br />
be referenced in an edit.<br />
In order to increase the number of claims that successfully pass through audit trails and into processing<br />
<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For the<br />
month of February <strong>2012</strong>, these are:<br />
Claim Description<br />
Rejection<br />
421 DIAG CODE (XXXXX) INVALID FOR DATE SVC<br />
The date of service was outside of the effective date range of the<br />
diagnosis code used. The invalid diagnosis code will appear<br />
inside the parenthesis.<br />
434 PROC CODE REQUIRES REFERRING NPI<br />
Procedure code billed was for a diagnostic procedure such as an<br />
x-ray or lab work which requires the NPI of the ordering<br />
physician, or a consultation, which requires the NPI of the<br />
referring physician, and this was not submitted on the claim.<br />
888 INSTREAM REJECTION<br />
There was a problem involving HIPAA required loops,<br />
segments, or values. The specific loop will be identified, for<br />
example, 'ELEMENT N401 (D.E. 19) AT COL. 4 IS MISSING,<br />
THOUGH MARKED "MUST BE USED" (LOOP:2010BA<br />
POS:3140)'. The number after 'POS' indicates the position in the<br />
file where the error occurred<br />
202 RAILROAD<br />
The beneficiary’s HIC (<strong>Medicare</strong> number) began with an<br />
alphabetic prefix, indicating the beneficiary s a Railroad retiree.<br />
302 INVALID BILLING (NO CHARGES BILLED)<br />
Claim did not contain any items with an associated billed<br />
amount.<br />
Number of<br />
Claims<br />
926<br />
702<br />
555<br />
449<br />
364<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 13
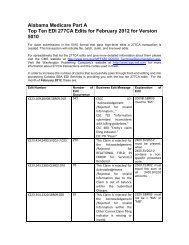
Alabama <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Ten EDI 277CA Edits for February <strong>2012</strong> for Version 5010<br />
For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. This<br />
transaction will indicate file, batch, claim, and line level edits.<br />
For spreadsheets that list the 277CA edits and give more detailed information about them please visit the<br />
CMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the Washington<br />
Publishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactions<br />
and the codes used in them.<br />
In order to increase the number of claims that successfully pass through front-end editing and into<br />
processing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month of<br />
February <strong>2012</strong>, these are:<br />
Production<br />
Edit Number<br />
Number of Edit<br />
Occurrences<br />
Business Edit<br />
Message<br />
X222.087.2010AA.NM109.050 8,692 This Claim is<br />
rejected for<br />
relational field due<br />
to Billing<br />
Provider's<br />
submitter not<br />
approved for<br />
electronic claim<br />
submissions on<br />
behalf of this<br />
Billing Provider.<br />
X222.351.2400.SV101-7.020 5,083 This Claim is<br />
rejected for<br />
relational field<br />
Information<br />
within the<br />
Detailed<br />
description of<br />
service.<br />
X222.196.2300.REF.010 4,094 This Claim is<br />
rejected for<br />
relational field<br />
Information<br />
submitted<br />
inconsistent with<br />
billing guidelines<br />
for the Other<br />
Insured's Policy<br />
Explanation of<br />
Edit<br />
2010AA.NM109<br />
billing provider<br />
must be<br />
"associated" to the<br />
submitter (from a<br />
trading partner<br />
management<br />
perspective) in<br />
1000A.NM109.<br />
2400.SV101-7<br />
must be present.<br />
when 2400.SV101-<br />
2 is present on the<br />
table of procedure<br />
codes that require a<br />
description.<br />
2300.REF with<br />
REF01 = "F8"<br />
must not be<br />
present.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 14
Number.<br />
X222.295.2320.SBR03.006 4,094 This Claim is<br />
rejected for<br />
relational field<br />
Information<br />
submitted<br />
inconsistent with<br />
billing guidelines<br />
for the Other<br />
Insured's Policy<br />
Number.<br />
X222.094.2010AA.REF02.050 4,042 This Claim is<br />
rejected for<br />
relational field<br />
Billing Provider's<br />
NPI (National<br />
Provider ID) and<br />
Tax ID.<br />
X222.087.2010AA.NM109.030 3,641 This Claim is<br />
rejected for<br />
Invalid<br />
Information in the<br />
Billing Provider's<br />
NPI (National<br />
Provider ID).<br />
X222.351.2400.SV101-2.020 2,704 This Claim is<br />
rejected for<br />
relational field<br />
Information<br />
within the<br />
HCPCS.<br />
X222.121.2010BA.NM109.020 2,312 This Claim is<br />
rejected for<br />
Invalid<br />
Information for a<br />
Subscriber's<br />
contract/member<br />
number.<br />
CSCC A8:<br />
"Acknowledgement<br />
/ Rejected for<br />
relational field in<br />
error"<br />
CSC 163: "Entity's<br />
Policy Number"<br />
CSC 732<br />
"Information<br />
submitted<br />
inconsistent with<br />
billing guidelines."<br />
EIC: GB "Other<br />
Insured"<br />
2010AA.REF must<br />
be associated with<br />
the provider<br />
identified in<br />
2010AA.NM109.<br />
2010AA.NM109<br />
must be a valid NPI<br />
on the Crosswalk<br />
when evaluated<br />
with<br />
1000B.NM109.<br />
When<br />
2400.SV101-1 =<br />
"HC",<br />
2400.SV101-2<br />
must be a valid<br />
HCPCS Code on<br />
the date in<br />
2400.DTP03 when<br />
DTP01 = "472".<br />
2010BA.NM109<br />
must be 10 - 11<br />
positions in the<br />
format of<br />
NNNNNNNNNA<br />
or<br />
NNNNNNNNNAA<br />
or<br />
NNNNNNNNNAN<br />
where “A”<br />
represents an alpha<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 15
X222.273.2310C.N403.020 1,839 This Claim is<br />
rejected for<br />
Invalid<br />
Information for a<br />
Service Location's<br />
Postal/Zip.<br />
X222.262.2310B.NM109.030 1,701 This Claim is<br />
rejected for<br />
Invalid<br />
Information for a<br />
Rendering<br />
Provider's<br />
National Provider<br />
Identifier (NPI).<br />
character and “N”<br />
represents a<br />
numeric digit.<br />
2310C.N403 must<br />
be a valid 9 digit<br />
Zip Code.<br />
2310B.NM109<br />
must be a valid NPI<br />
on the Crosswalk<br />
when evaluated<br />
with<br />
1000B.NM109.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 16
Georgia <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Ten EDI 277CA Edits for February <strong>2012</strong> for Version 5010<br />
For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. This<br />
transaction will indicate file, batch, claim, and line level edits.<br />
For spreadsheets that list the 277CA edits and give more detailed information about them please visit the<br />
CMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the Washington<br />
Publishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactions<br />
and the codes used in them.<br />
In order to increase the number of claims that successfully pass through front-end editing and into<br />
processing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month of<br />
February <strong>2012</strong>, these are:<br />
Production:<br />
Edit Number<br />
Number of<br />
Edit<br />
Occurrences<br />
Business Edit<br />
Message<br />
X222.087.2010AA.NM109.050 23,172 This Claim is<br />
rejected for<br />
relational field due<br />
to Billing Provider's<br />
submitter not<br />
approved for<br />
electronic claim<br />
submissions on<br />
behalf of this<br />
Billing Provider.<br />
X999.DUPE 15,499 Rejected due to<br />
duplicate ST/SE<br />
submission.<br />
X222.351.2400.SV101-7.020. 5,657 This Claim is<br />
rejected for<br />
relational field<br />
Information within<br />
the Detailed<br />
description of<br />
service.<br />
X222.121.2010BA.NM109.020 5,192 This Claim is<br />
rejected for Invalid<br />
Information for a<br />
Subscriber's<br />
contract/member<br />
number.<br />
Explanation of<br />
Edit<br />
2010AA.NM109<br />
billing provider<br />
must be<br />
"associated" to the<br />
submitter (from a<br />
trading partner<br />
management<br />
perspective) in<br />
1000A.NM109.<br />
Exact duplicate of<br />
a previously<br />
submitted<br />
transaction set.<br />
2400.SV101-7<br />
must be present.<br />
when 2400.SV101-<br />
2 is present on the<br />
table of procedure<br />
codes that require a<br />
description.<br />
2010BA.NM109<br />
must be 10 - 11<br />
positions in the<br />
format of<br />
NNNNNNNNNA<br />
or<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 17
X222.094.2010AA.REF02.050 4,318 This Claim is<br />
rejected for<br />
relational field<br />
Billing Provider's<br />
NPI (National<br />
Provider ID) and<br />
Tax ID.<br />
X222.295.2320.SBR03.006 3,221 This Claim is<br />
rejected for<br />
relational field<br />
Information<br />
submitted<br />
inconsistent with<br />
billing guidelines<br />
for the Other<br />
Insured's Policy<br />
Number.<br />
NNNNNNNNNAA<br />
or<br />
NNNNNNNNNAN<br />
where “A”<br />
represents an alpha<br />
character and “N”<br />
represents a<br />
numeric digit.<br />
2010AA.REF must<br />
be associated with<br />
the provider<br />
identified in<br />
2010AA.NM109.<br />
CSCC A8:<br />
"Acknowledgement<br />
/ Rejected for<br />
relational field in<br />
error"<br />
CSC 163: "Entity's<br />
Policy Number"<br />
CSC 732<br />
"Information<br />
submitted<br />
inconsistent with<br />
billing guidelines."<br />
EIC: GB "Other<br />
Insured".<br />
X222.351.2400.SV103.020 3,089 This Claim is<br />
rejected for Invalid<br />
Information<br />
submitted<br />
inconsistent with<br />
billing guidelines<br />
for the Unit or<br />
Basis for<br />
Measurement<br />
Code..<br />
2400.SV103 must<br />
be "MJ" when<br />
SV101-3, SV101-<br />
4, SV101-5, or<br />
SV101-6 is an<br />
anesthesia modifier<br />
(AA, AD, QK, QS,<br />
QX, QY or QZ).<br />
Otherwise, must be<br />
"UN".<br />
X222.351.2400.SV101-2.020 2,754 This Claim is<br />
rejected for<br />
relational field<br />
Information within<br />
the HCPCS.<br />
When<br />
2400.SV101-1 =<br />
"HC",<br />
2400.SV101-2<br />
must be a valid<br />
HCPCS Code on<br />
the date in<br />
2400.DTP03 when<br />
DTP01 = "472".<br />
X222.087.2010AA.NM109.030 2,714 This Claim is 2010AA.NM109<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 18
ejected for Invalid<br />
Information in the<br />
Billing Provider's<br />
NPI (National<br />
Provider ID).<br />
X222.273.2310C.N403.020 2,598 This Claim is<br />
rejected for Invalid<br />
Information for a<br />
Service Location's<br />
Postal/Zip.<br />
must be a valid NPI<br />
on the Crosswalk<br />
when evaluated<br />
with<br />
1000B.NM109.<br />
2310C.N403 must<br />
be a valid 9 digit<br />
Zip Code.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 19
Mississippi <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Ten EDI 277CA Edits for February <strong>2012</strong> for Version 5010<br />
For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. This<br />
transaction will indicate file, batch, claim, and line level edits.<br />
For spreadsheets that list the 277CA edits and give more detailed information about them please visit the<br />
CMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the Washington<br />
Publishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactions<br />
and the codes used in them.<br />
In order to increase the number of claims that successfully pass through front-end editing and into<br />
processing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month of<br />
February <strong>2012</strong>, these are:<br />
Production:<br />
Edit Number<br />
X222.087.2010AA.NM109.<br />
050<br />
X222.094.2010AA.REF02.<br />
050<br />
Number of<br />
Edit<br />
Occurrences<br />
Disposition/Error<br />
Code<br />
5,889 This Claim is rejected<br />
for relational field due<br />
to Billing Provider's<br />
submitter not approved<br />
for electronic claim<br />
submissions on behalf<br />
of this Billing Provider.<br />
5,301 This Claim is rejected<br />
for relational field<br />
Billing Provider's NPI<br />
(National Provider ID)<br />
and Tax ID.<br />
X222.273.2310C.N403.020 3,534 This Claim is rejected<br />
for Invalid Information<br />
for a Service Location's<br />
Postal/Zip.<br />
X222.136.2010BB.N403.02<br />
0<br />
X222.351.2400.SV101-<br />
7.020<br />
2,674 This Claim is rejected<br />
for Invalid Information<br />
for a Payer's Postal/Zip<br />
Code.<br />
2,518 This Claim is rejected<br />
for relational field<br />
Information within the<br />
Detailed description of<br />
service.<br />
Explanation of Edit<br />
2010AA.NM109<br />
billing provider must<br />
be "associated" to the<br />
submitter (from a<br />
trading partner<br />
management<br />
perspective) in<br />
1000A.NM109.<br />
2010AA.REF must be<br />
associated with the<br />
provider identified in<br />
2010AA.NM109.<br />
2310C.N403 must be a<br />
valid 9 digit Zip Code.<br />
2010BB.N403 must be<br />
a valid Zip Code.<br />
2400.SV101-7 must be<br />
present when<br />
2400.SV101-2 is<br />
present on the table of<br />
procedure codes that<br />
require a description.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 20
X222.087.2010AA.NM109.<br />
030<br />
2,458 This Claim is rejected<br />
for Invalid Information<br />
in the Billing Provider's<br />
NPI (National Provider<br />
ID).<br />
X222.295.2320.SBR03.006 2,043 This Claim is rejected<br />
for relational field<br />
Information submitted<br />
inconsistent with<br />
billing guidelines for<br />
the Other Insured's<br />
Policy Number.<br />
X222.206.2300.REF02.020 1,608 This Claim is rejected<br />
for Invalid within the<br />
Information Care Plan<br />
Oversight Number's<br />
National Provider<br />
Identifier (NPI) and<br />
Care Plan Oversight<br />
Number.<br />
X222.403.2400.REF02.070 1,593 This Claim is rejected<br />
for Invalid Information<br />
within the<br />
Authorization/certificat<br />
X222.351.2400.SV101-<br />
2.020<br />
ion number.<br />
1,473 This Claim is rejected<br />
for relational field<br />
Information within the<br />
HCPCS.<br />
2010AA.NM109 must<br />
be a valid NPI on the<br />
Crosswalk when<br />
evaluated with<br />
1000B.NM109.<br />
CSCC A8:<br />
"Acknowledgement /<br />
Rejected for relational<br />
field in error"<br />
CSC 163: "Entity's<br />
Policy Number"<br />
CSC 732 "Information<br />
submitted inconsistent<br />
with billing<br />
guidelines."<br />
EIC: GB "Other<br />
Insured"<br />
2300.REF02 must be<br />
valid according to the<br />
NPI algorithm.<br />
2400.REF02 must be a<br />
valid Mammography<br />
Certification Number.<br />
When 2400.SV101-1 =<br />
"HC", 2400.SV101-2<br />
must be a valid HCPCS<br />
Code on the date in<br />
2400.DTP03 when<br />
DTP01 = "472".<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 21
Tennessee <strong>Medicare</strong> <strong>Part</strong> B<br />
Top Ten EDI 277CA Edits for February <strong>2012</strong> for Version 5010<br />
For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. This<br />
transaction will indicate file, batch, claim, and line level edits.<br />
For spreadsheets that list the 277CA edits and give more detailed information about them please visit the<br />
CMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the Washington<br />
Publishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactions<br />
and the codes used in them.<br />
In order to increase the number of claims that successfully pass through front-end editing and into<br />
processing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month of<br />
February <strong>2012</strong>, these are:<br />
Production:<br />
Edit Number<br />
Number of<br />
Edit<br />
Occurrences<br />
Business Edit<br />
Message<br />
X222.094.2010AA.REF02.050 8,247 This Claim is<br />
rejected for<br />
relational field<br />
Billing Provider's<br />
NPI (National<br />
Provider ID) and<br />
Tax ID.<br />
X222.087.2010AA.NM109.050 6,566 This Claim is<br />
rejected for<br />
relational field due<br />
to Billing Provider's<br />
submitter not<br />
approved for<br />
electronic claim<br />
submissions on<br />
behalf of this<br />
Billing Provider.<br />
X222.351.2400.SV101-7.020 5,490 This Claim is<br />
rejected for<br />
relational field<br />
Information within<br />
the Detailed<br />
description of<br />
service.<br />
X222.121.2010BA.NM109.020 3,812 This Claim is<br />
rejected for Invalid<br />
Information for a<br />
Explanation of<br />
Edit<br />
2010AA.REF must<br />
be associated with<br />
the provider<br />
identified in<br />
2010AA.NM109.<br />
2010AA.NM109<br />
billing provider<br />
must be<br />
"associated" to the<br />
submitter (from a<br />
trading partner<br />
management<br />
perspective) in<br />
1000A.NM109.<br />
2400.SV101-7<br />
must be present.<br />
when 2400.SV101-<br />
2 is present on the<br />
table of procedure<br />
codes that require a<br />
description.<br />
2010BA.NM109<br />
must be 10 - 11<br />
positions in the<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 22
Subscriber's<br />
contract/member<br />
number.<br />
X222.087.2010AA.NM109.030 3,174 This Claim is<br />
rejected for Invalid<br />
Information in the<br />
Billing Provider's<br />
NPI (National<br />
Provider ID).<br />
X222.351.2400.SV101-2.020 2,519 This Claim is<br />
rejected for<br />
relational field<br />
Information within<br />
the HCPCS.<br />
X222.273.2310C.N403.020 2,468 This Claim is<br />
rejected for Invalid<br />
Information for a<br />
Service Location's<br />
Postal/Zip.<br />
X222.196.2300.REF.010 1,844 This Claim is<br />
rejected for Invalid<br />
Information within<br />
the Payer Assigned<br />
Claim Control<br />
Number<br />
Information<br />
submitted<br />
inconsistent with<br />
billing guidelines.<br />
X222.262.2310B.NM109.030 1,655 This Claim is<br />
rejected for Invalid<br />
Information for a<br />
Rendering<br />
Provider's National<br />
Provider Identifier<br />
(NPI).<br />
format of<br />
NNNNNNNNNA<br />
or<br />
NNNNNNNNNAA<br />
or<br />
NNNNNNNNNAN<br />
where “A”<br />
represents an alpha<br />
character and “N”<br />
represents a<br />
numeric digit.<br />
2010AA.NM109<br />
must be a valid NPI<br />
on the Crosswalk<br />
when evaluated<br />
with<br />
1000B.NM109.<br />
When<br />
2400.SV101-1 =<br />
"HC",<br />
2400.SV101-2<br />
must be a valid<br />
HCPCS Code on<br />
the date in<br />
2400.DTP03 when<br />
DTP01 = "472".<br />
2310C.N403 must<br />
be a valid 9 digit<br />
Zip Code.<br />
2300.REF with<br />
REF01 = "F8"<br />
must not be<br />
present.<br />
2310B.NM109<br />
must be a valid NPI<br />
on the Crosswalk<br />
when evaluated<br />
with<br />
1000B.NM109.<br />
X222.305.2320.AMT.030 1,337 This Claim is If 2000B.SBR01 =<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 23
ejected for Missing<br />
Information within<br />
the Other payer's<br />
Explanation of<br />
Benefits/payment<br />
information<br />
"S" then one 2320<br />
loop with an AMT<br />
segment with<br />
AMT01 = "D"<br />
must be present.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 24
<strong>Medicare</strong> Coverage Database (MCD) Article: Educational Article -<br />
Chiropractic Services - Retired<br />
J10 MAC B (Alabama, Georgia, Tennessee) (A51055)<br />
Carrier 00512 (Mississippi) (A51056)<br />
Effective March 31, <strong>2012</strong>, the <strong>Medicare</strong> Coverage Database (MCD) Articles titled Educational Article –<br />
Chiropractic Services are retired.<br />
Effective <strong>April</strong> 1, <strong>2012</strong>, please refer to the Local Coverage Determinations (LCDs) listed below for<br />
coverage guidance for chiropractic services:<br />
Medicine: Chiropractic Services (L32342) - J10 MAC B<br />
Medicine: Chiropractic Services (L32351) - Carrier 00512<br />
LCDs and Articles can be accessed from the Local Coverage Determinations (LCDs) and Articles page of<br />
our website (choose your state and select ‘Articles’).<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 25
Local Coverage Determinations - Comment Period for Draft LCDs<br />
J10 MAC B (Alabama, Georgia, Tennessee)<br />
Carrier 00512 (Mississippi)<br />
The Comment Period for the Local Coverage Determinations (LCDs) listed below is from March 9, <strong>2012</strong><br />
through <strong>April</strong> 23, <strong>2012</strong>:<br />
J10 MAC B<br />
Medicine: Noninvasive Peripheral Arterial and Venous Studies (DL30040)<br />
Transportation Services: Ambulance (DL30022)<br />
Carrier 00512<br />
Medicine: Noninvasive Peripheral Arterial and Venous Studies (DL30622)<br />
Transportation Services: Ambulance (DL32498)<br />
The Draft LCDs are accessible from the <strong>Cahaba</strong> <strong>GBA</strong> website at Local Coverage Determinations (LCDs)<br />
and Articles (select ‘Status of Draft LCDs’ for your state).<br />
Comments on the draft LCDs may be submitted via e-mail to: J10LCDComment@<strong>Cahaba</strong>gba.com or in<br />
writing to the Medical Director at the address listed below.<br />
<strong>Cahaba</strong> Government Benefit Administrators®, LLC<br />
Comments for Draft LCDs<br />
ATTN: Contractor Medical Director (CMD)<br />
P.O. Box 13384<br />
Birmingham, AL 35202-3384<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 26
Claim Specific CERT Errors- February <strong>2012</strong><br />
J10 MAC B (Alabama, Georgia, Tennessee)<br />
Carrier 00512 (Mississippi)<br />
The Comprehensive Error Rate Testing (CERT) Program was implemented by the Centers for <strong>Medicare</strong> &<br />
Medicaid Services (CMS) to monitor the accuracy of claims processing by <strong>Medicare</strong> contractors, like<br />
<strong>Cahaba</strong>. Contractors are then notified by CERT of the errors and findings.<br />
We would like to remind you that should you receive an Additional Documentation Request (ADR) such as<br />
a request for records to support services that are involved in a CERT review, you should submit the<br />
appropriate documentation to support the services billed, including but not limited to progress note(s) to<br />
match the DOS billed, lab results, operative reports, diagnostic tests, physician orders, etc. <strong>Medicare</strong><br />
requires a legible identifier for services provided/ordered. The method used shall be hand written or an<br />
electronic signature (stamp signatures are not acceptable) to sign an order or other medical record<br />
documentation for medical review purposes.<br />
Providers may appeal unfavorable decisions with additional supporting documentation. For detailed<br />
information regarding the Appeals Process, refer to the following link:<br />
www.cahabagba.com/part_b/claims/appeals_process.htm.<br />
Please contact the Provider Contact Center for individual questions concerning CERT errors:<br />
Alabama, Georgia and Tennessee Providers – 1-877-567-7271<br />
Mississippi Providers – 1-866-419-9454<br />
This summary provides examples of <strong>Cahaba</strong>'s errors identified by CERT. We encourage all providers to<br />
review this listing to educate you on common errors. This information will be updated periodically. The<br />
intent in providing this information is to prompt you to conduct an internal analysis of <strong>Medicare</strong> billing and<br />
reduce future denials by <strong>Medicare</strong>.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 27
News Flash Messages from CMS For All <strong>Part</strong> B Providers<br />
Extension of Enforcement Discretion Period for Updated HIPAA 5010<br />
Transaction Standards through June 30, <strong>2012</strong><br />
The Centers for <strong>Medicare</strong> & Medicaid Services’ Office of E-Health Standards and Services (OESS) is<br />
announcing that it WILL NOT INITIATE enforcement action for an additional THREE (3) months,<br />
through June 30, <strong>2012</strong>, against any covered entity that is required to comply with the updated transactions<br />
standards adopted under the Health Insurance Portability and Accountability Act of 1996 (HIPAA): ASC<br />
X12 Version 5010 and NCPDP Versions D.0 and 3.0.<br />
On November 17, 2011, OESS announced that, for a 90-day period, it would not initiate enforcement action<br />
against any covered entity that was not compliant with the updated versions of the standards by the January<br />
1, <strong>2012</strong> compliance date. This was referred to as enforcement discretion, and during this period, covered<br />
entities were encouraged to complete outstanding implementation activities including software installation,<br />
testing and training.<br />
Health plans, clearinghouses, providers, and software vendors have been making steady progress: the<br />
<strong>Medicare</strong> Fee-for-Service (FFS) program is currently reporting successful receipt and processing of over 70<br />
percent of all <strong>Part</strong> A claims and over 90 percent of all <strong>Part</strong> B claims in the Version 5010 format.<br />
Commercial plans are reporting similar numbers. State Medicaid agencies are showing progress as well, and<br />
some have made a full transition to Version 5010.<br />
Covered entities are making similar progress with Version D.0. At the same time, OESS is aware that there<br />
are still a number of outstanding issues and challenges impeding full implementation. OESS believes that<br />
these remaining issues warrant an extension of enforcement discretion to ensure that all entities can<br />
complete the transition. OESS expects that transition statistics will reach 98 percent industry wide by the<br />
end of the enforcement discretion period.<br />
Given that OESS will not initiate enforcement actions through June 30, <strong>2012</strong>, industry is urged to<br />
collaborate more closely on appropriate strategies to resolve remaining problems. OESS is stepping up its<br />
existing outreach to include more technical assistance for covered entities. OESS is also partnering with<br />
several industry groups as well as <strong>Medicare</strong> FFS and Medicaid to expand technical assistance opportunities<br />
and eliminate remaining barriers. Details will be provided in a separate communication.<br />
The <strong>Medicare</strong> FFS program will continue to host separate provider calls to address outstanding issues related to<br />
<strong>Medicare</strong> programs and systems. The <strong>Medicare</strong> Administrative Contractors (MAC) will continue to work closely with<br />
clearinghouses, billing vendors, or healthcare providers requiring assistance in submitting and receiving Version 5010<br />
compliant transactions.<br />
The Medicaid program staff at CMS will continue to work with individual States regarding their program readiness.<br />
Issues related to implementation problems with the States may be sent to Medicaid5010@cms.hhs.gov.<br />
OESS strongly encourages industry to come together in a collaborative, unified way to identify and resolve all<br />
outstanding issues that are impacting full compliance, and looks forward to seeing extensive engagement in the<br />
technical assistance initiative to be launched over the next few weeks.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 28
HHS Announces Intent to Delay ICD-10 Compliance Date<br />
As part of President Obama’s commitment to reducing regulatory burden, Health and Human Services<br />
Secretary Kathleen G. Sebelius announced that HHS will initiate a process to postpone the date by which<br />
certain health care entities have to comply with International Classification of Diseases, 10th Edition<br />
diagnosis and procedure codes (ICD-10).<br />
The final rule adopting ICD-10 as a standard was published in January 2009 and set a compliance date of<br />
October 1, 2013 – a delay of two years from the compliance date initially specified in the 2008 proposed<br />
rule. HHS will announce a new compliance date moving forward.<br />
“ICD-10 codes are important to many positive improvements in our health care system,” said HHS<br />
Secretary Kathleen Sebelius. “We have heard from many in the provider community who have concerns<br />
about the administrative burdens they face in the years ahead. We are committing to work with the provider<br />
community to reexamine the pace at which HHS and the nation implement these important improvements to<br />
our health care system.”<br />
ICD-10 codes provide more robust and specific data that will help improve patient care and enable the<br />
exchange of our health care data with that of the rest of the world that has long been using ICD-10. Entities<br />
covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required to<br />
use the ICD-10 diagnostic and procedure codes.<br />
Enrolling In the <strong>Medicare</strong> Program Fact Sheets<br />
Several fact sheets that provide education to specific provider types on how to enroll in the <strong>Medicare</strong><br />
Program and maintain their enrollment information using Internet-based Provider Enrollment, Chain, and<br />
Ownership System (PECOS) have been recently updated and are available in downloadable format from the<br />
<strong>Medicare</strong> Learning Network® (MLN). Please visit<br />
http://www.CMS.gov/<strong>Medicare</strong>ProviderSupEnroll/downloads/<strong>Medicare</strong>_Provider-<br />
Supplier_Enrollment_National_Education_Products.pdf for a complete list of all MLN products related to<br />
<strong>Medicare</strong> provider-supplier enrollment.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 29
Primary Care Incentive Payment (PCIP) program<br />
Per Section 5501(a) of the Affordable Care Act, the Primary Care Incentive Payment (PCIP) program<br />
authorizes an incentive payment of 10% of <strong>Medicare</strong>'s program payments to be paid to qualifying primary<br />
care physicians and non-physician practitioners for services rendered from Sunday, January 1, 2011, to<br />
Thursday, December 31, 2015. CMS has published 22 Frequently Asked Question (FAQ) items related to<br />
the PCIP program. These new FAQs can be found here. Alternatively, these FAQ items can be found by<br />
visiting http://questions.CMS.hhs.gov/ and searching for “PCIP” or “Primary Care Incentive Payment.”<br />
Electronic Funds Transfer (EFT)<br />
Existing regulations at 42 CFR 424.510(e)(1)(2) require that at the time of enrollment, enrollment change<br />
request or revalidation, providers and suppliers that expect to receive payment from <strong>Medicare</strong> for services<br />
provided must also agree to receive <strong>Medicare</strong> payments through Electronic Funds Transfer (EFT). Section<br />
1104 of the Affordable Care Act further expands Section 1862 (a) of the Social Security Act by mandating<br />
federal payments to providers and suppliers only by electronic means. As part of <strong>Medicare</strong>’s revalidation<br />
efforts, all suppliers and providers who are not currently receiving EFT payments will be identified, and<br />
required to submit the CMS 588 EFT form with the Provider Enrollment Revalidation application. For more<br />
information about provider enrollment revalidation, review the <strong>Medicare</strong> Learning Network’s Special<br />
Edition Article SE1126 titled, “Further Details on the Revalidation of Provider Enrollment Information” at<br />
http://www.cms.gov/MLNMattersArticles/downloads/SE1126.pdf.<br />
Revalidation Notice<br />
Has <strong>Medicare</strong> sent you a notice to revalidate your enrollment? If you are not sure, you can find lists of<br />
providers sent notices to revalidate their <strong>Medicare</strong> enrollment by scrolling to the "Downloads" section at<br />
http://www.CMS.gov/<strong>Medicare</strong>ProviderSupEnroll/11_Revalidations.asp on the Centers for <strong>Medicare</strong> &<br />
Medicaid Services (CMS) website. That site currently contains links to lists of providers sent notices from<br />
September, 2011 through January, <strong>2012</strong>. Information on revalidation letters sent in February will be posted<br />
in late March. For ease of reference, the lists are in order by National Provider Identifier and the date the<br />
notice was sent.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 30
News from CMS For <strong>Part</strong> B Providers<br />
Intensive Behavioral Therapy (IBT) for Obesity- Revised<br />
Note: This article was revised on March 9, <strong>2012</strong> to reflect the revised Change Request (CR) 7641 issued on<br />
March 7. In this article, the CR release date, transmittal number, and the Web address for accessing CR7641<br />
were revised. All other information is unchanged.<br />
Provider Types Affected<br />
This MLN Matters® article is intended for primary care physicians and other primary care practitioners<br />
billing <strong>Medicare</strong> contractors (carriers, Fiscal Intermediaries (FIs) and A/B <strong>Medicare</strong> Administrative<br />
Contractors (A/B MACs)) for services provided to <strong>Medicare</strong> beneficiaries in a primary care setting.<br />
Provider Action Needed<br />
This article is based on Change Request (CR) 7641, which informs <strong>Medicare</strong> contractors about<br />
implementing coverage of Intensive Behavioral Therapy (IBT) for obesity.<br />
Effective for claims with dates of service November 29, 2011, and later, <strong>Medicare</strong> beneficiaries with<br />
obesity, defined as Body Mass Index (BMI) equal to or greater than 30 kg/m2, who are competent and alert<br />
at the time that counseling is provided and whose counseling is furnished by a qualified primary care<br />
physician or other primary care practitioner in a primary care setting, are eligible for:<br />
One face-to-face visit every week for the first month;<br />
One face-to-face visit every other week for months 2-6; and<br />
One face-to-face visit every month for months 7-12, if the beneficiary meets the 3kg (6.6 lbs) weight<br />
loss requirement during the first 6 months.<br />
<strong>Medicare</strong> coinsurance and <strong>Part</strong> B deductible are waived for this service.<br />
See the ‘Background’ and ‘Additional Information’ sections of this article for further details regarding this<br />
change. Be sure your staffs are aware of this new coverage determination and that Healthcare Common<br />
Procedure Coding System (HCPCS) code G0447 (Face-to-Face Behavioral Counseling for Obesity, 15<br />
minutes) will be used to bill for these services.<br />
This code was effective November 29, 2011, and will appear in the January <strong>2012</strong> quarterly update of the<br />
<strong>Medicare</strong> Physician Fee Schedule Database (MPFSDB) and the Integrated Outpatient Code Editor (IOCE).<br />
Background<br />
Based upon authority in the Social Security Act to cover “additional preventive services” for <strong>Medicare</strong><br />
beneficiaries if certain statutory requirements are met, and the services are reasonable and necessary for the<br />
prevention or early detection of illness or disability, the Centers for <strong>Medicare</strong> & Medicaid Services (CMS)<br />
initiated a new national coverage analysis on IBT for obesity. Screening for obesity in adults is a "B"<br />
recommendation by the U.S. Preventive Services Task Force (USPSTF) and is appropriate for individuals<br />
entitled to benefits under <strong>Medicare</strong> <strong>Part</strong> A and <strong>Part</strong> B.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 31
In 2003, the USPSTF found good evidence that BMI “is reliable and valid for identifying adults at increased<br />
risk for mortality and morbidity due to overweight and obesity.” The USPSTF also found fair to good<br />
evidence that high intensity counseling combined with behavioral interventions in obese adults (as defined<br />
by a BMI ≥30 kg/m2) “produces modest, sustained weight loss.”<br />
Effective for claims with dates of service on or after November 29, 2011, <strong>Medicare</strong> beneficiaries with<br />
obesity (BMI ≥30 kg/m2), who are competent and alert at the time that counseling is provided and whose<br />
counseling is furnished by a qualified primary care physician or other primary care practitioner in a primary<br />
care setting are eligible for:<br />
One face-to-face visit every week for the first month;<br />
One face-to-face visit every other week for months 2-6; and<br />
One face-to-face visit every month for months 7-12, if the beneficiary meets the 3kg (6.6 lbs) weight<br />
loss requirement during the first 6 months as discussed below.<br />
At the 6-month visit, a reassessment of obesity and a determination of the amount of weight loss should be<br />
performed. To be eligible for additional face-to-face visits occurring once a month for months 7-12,<br />
beneficiaries must have achieved a reduction in weight of at least 3kg (6.6 lbs.), over the course of the first 6<br />
months of intensive therapy. This determination must be documented in the physician office records for<br />
applicable beneficiaries consistent with usual practice. For beneficiaries who do not achieve a weight<br />
loss of at least 3kg (6.6 lbs.) during the first 6 months of intensive therapy, a reassessment of their readiness<br />
to change and BMI is appropriate after an additional 6-month period.<br />
IBT for obesity consists of the following:<br />
1. Screening for obesity in adults using measurement of BMI calculated by dividing weight in<br />
kilograms by the square of height in meters (expressed kg/m2);<br />
2. Dietary (nutritional) assessment; and,<br />
3. Intensive behavioral counseling and behavioral therapy to promote sustained weight loss through<br />
high intensity interventions on diet and exercise.<br />
Intensive behavioral intervention for obesity should be consistent with the 5-A framework:<br />
1. Assess: Ask about/assess behavioral health risk(s) and factors affecting choice of behavior change<br />
goals/methods.<br />
2. Advise: Give clear, specific, and personalized behavior change advice, including information about<br />
personal health harms and benefits.<br />
3. Agree: Collaboratively select appropriate treatment goals and methods based on the patient’s<br />
interest in and willingness to change the behavior.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 32
4. Assist: Using behavior change techniques (self-help and/or counseling), aid the patient in achieving<br />
agreed-upon goals by acquiring the skills, confidence, and social/environmental supports for<br />
behavior change, supplemented with adjunctive medical treatments when appropriate.<br />
5. Arrange: Schedule follow-up contacts (in person or by telephone) to provide ongoing<br />
assistance/support and to adjust the treatment plan as needed, including referral to more intensive or<br />
specialized treatment.<br />
Billing Requirements<br />
Diagnostic Codes<br />
Effective for claims with dates of service on or after November 29, 2011, <strong>Medicare</strong> will recognize HCPCS<br />
code G0447, Face-to-Face Behavioral Counseling for Obesity, 15 minutes. G0447 must be billed along with<br />
1 of the ICD-9 codes for BMI 30.0 and over (V85.30-V85.39, V85.41-V85.45). The type of service (TOS)<br />
for G0447 is 1. (ICD-10 codes will be Z68.30-Z68.39.9, Z68.41- Z68.45)<br />
Effective for claims with dates of service on or after November 29, 2011, <strong>Medicare</strong> contractors will deny<br />
claims for HCPCS G0447 that are not submitted with the appropriate diagnostic code (V85.30-V85.39,<br />
V85.41-V85.45).<br />
Claims submitted with HCPCS G0447 that are not submitted with these diagnosis codes will be denied with<br />
the following messages:<br />
Claim Adjustment Reason Code (CARC) 167 – "This (these) diagnosis(es) is (are) not covered.<br />
Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment<br />
Information REF), if present."<br />
Remittance Advice Remark Code (RARC) N386 – "This decision was based on a National Coverage<br />
Determination (NCD). An NCD provides a coverage determination as to whether a particular item or<br />
service is covered. A copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not<br />
have web access, you may contact the contractor to request a copy of the NCD."<br />
Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if a<br />
claim is received with a GA modifier indicating a signed ABN is on file).<br />
Group Code CO (Contractual Obligation) assigning financial liability to the provider (if a claim is<br />
received with a GZ modifier indicating no signed ABN is on file).<br />
Note: Per MLN Matters® article MM7228, when modifier GZ is used, contractors will use CARC 50<br />
(These services are non-covered services because this is not deemed a “medical necessity” by the payer.).<br />
This is true with all denials noted below that have the Group Code CO. MM7228 may be found at<br />
http://www.cms.gov/MLNMattersArticles/downloads/MM7228.pdf on the CMS website.<br />
Specialty Codes<br />
Effective for services on or after November 29, 2011, <strong>Medicare</strong> will pay claims for G0447, only when<br />
services are submitted by the following provider specialty types found on the provider’s <strong>Medicare</strong><br />
enrollment record:<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 33
01 - General Practice<br />
08 - Family Practice<br />
11 - Internal Medicine<br />
16 - Obstetrics/Gynecology<br />
37 - Pediatric Medicine<br />
38 - Geriatric Medicine<br />
50 - Nurse Practitioner<br />
89 - Certified Clinical Nurse Specialist<br />
97 - Physician Assistant<br />
If your specialty type is not one of the above, your claim will be denied using the following codes:<br />
CARC of 185 – "The rendering provider is not eligible to perform the service billed. NOTE: Refer to<br />
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if<br />
present.),"<br />
RARC N95 - "This provider type/provider specialty may not bill this service."<br />
Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if a<br />
claim is received with a GA modifier indicating a signed ABN is on file), and<br />
Group Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim is<br />
received with a GZ modifier indicating no signed ABN is on file).<br />
Place of Service (POS) Codes<br />
Effective for services on or after November 29, 2011, <strong>Medicare</strong> will pay for obesity counseling claims<br />
containing HCPCS G0447 only when services are provided with the following POS codes:<br />
11 - Physician’s Office<br />
22 - Outpatient Hospital<br />
49 - Independent Clinic<br />
71 - State or local public health clinic.<br />
Line items on claims for G0447 will be denied if not performed in these POSs using the following codes:<br />
CARC 58 – "Treatment was deemed by the payer to have been rendered in an inappropriate or invalid POS.<br />
Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information<br />
REF), if present."<br />
RARC N428 - "Not covered when performed in this place of service."<br />
Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if a claim is<br />
received with a GA modifier indicating a signed ABN is on file)and<br />
Group Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim is received<br />
with a GZ modifier indicating no signed ABN is on file).<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 34
Frequency Limitation<br />
Effective July 2, <strong>2012</strong>, for claims processed with dates of service on or after November 29, 2011, <strong>Medicare</strong><br />
will pay for G0447 with an ICD-9 code of V85.30-V85.39, V85.41-V85.45, no more than 22 times in a 12-<br />
month period. Line items on claims beyond the 22 limit will be denied using the following codes: (Note:<br />
When applying this frequency limitation, a claim for the professional service and a claim for a facility<br />
fee will be allowed.)<br />
CARC 119 – "Benefit maximum for this time period or occurrence has been reached."<br />
RARC N362 - "The number of days or units of service exceeds our acceptable maximum."<br />
Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if a<br />
claim is received with a GA modifier indicating a signed ABN is on file), and<br />
Group Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim is<br />
received with a GZ modifier indicating no signed ABN is on file).<br />
Note: Your contractor will not search their files for claims that may have been paid in error. However,<br />
contractors may adjust claims that are brought to their attention.<br />
Institutional Claims Notes<br />
Claims submitted with either a Type of Bill (TOB) 13X or TOB 85X (where the revenue code is not 096X,<br />
097X, or 098X) will be identified as facility fee service claims.<br />
Claims submitted with TOBs 71X, 77X, or 85X (where the revenue code is 096X, 097X, or 098X) will be<br />
identified as professional service claims.<br />
<strong>Medicare</strong> will pay for G0447 on institutional claims in hospital outpatient departments TOB 13X based on<br />
OPPS and in Critical Access Hospitals TOB 85X based on reasonable cost.<br />
The CAH Method II payment is for G0447 with revenue codes 096X, 097X, or 098X is based on 115% of<br />
the lesser of the fee schedule amount or submitted charge. Deductible and coinsurance do not apply.<br />
<strong>Medicare</strong> will line-item deny any claim submitted with G0447 when the TOB is not 13X, 71X, 77X, or 85X<br />
with the following:<br />
CARC 5 - "The procedure code/bill type is inconsistent with the Place of Service. Note: Refer to the<br />
835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if<br />
present."<br />
RARC M77 - "Missing/incomplete/invalid place of service."<br />
Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if a<br />
claim is received with a GA modifier indicating a signed ABN is on file) and<br />
Group Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim is<br />
received with a GZ modifier indicating no signed ABN is on file).<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 35
Note: <strong>Medicare</strong> will hold institutional claims received before July 2, <strong>2012</strong>, with TOBs 13X, 71X, 77X, and<br />
85X reporting G0447.<br />
Rural Health Clinics and Federally Qualified Health Centers Claims Notes<br />
Rural Health Clinics, using TOB 71X, and Federally Qualified Health Centers, using TOB 77X, must<br />
submit HCPCS code G0447 on a separate service line to ensure coinsurance and deductible are not appliced<br />
to this service. Such claims will be paid based on the all-inclusive payment rate.<br />
For RHC and FQHC services that contain HCPCS code G0447 with another encounter/visit with the same<br />
line item DOS, the service line with HCPCS G0447 will be denied with the following messages:<br />
Claim Adjustment Reason Code (CARC) 97 – "The benefit for this service is included in the<br />
payment/allowance for another service/procedure that has already been adjudicated. Note: Refer to<br />
the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF) if<br />
present" and<br />
Group Code CO (Contractual Obligation)<br />
Note: Obesity counseling is not separately payable with another encounter/visit on the same day. This does<br />
not apply for Initial Preventive Physical Examination (IPPE) claims, claims containing modifier 59, and<br />
77X claims containing Diabetes Self-Management Training and Medical Nutrition Therapy services.<br />
Additional Information<br />
The official instruction, CR7641, issued to your FI, carrier, and A/B MAC regarding this change, was issued<br />
in 2 transmittals at http://www.cms.gov/transmittals/downloads/R2421CP.pdf and<br />
http://www.cms.gov/transmittals/downloads/R142NCD.pdf on the CMS website.<br />
MLN Matters® MM7641<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 36
Instructions for Processing Form CMS-855O Submissions<br />
Provider Types Affected<br />
This MLN Matters® Article is intended for physicians and non-physician practitioners who submit a Form<br />
CMS-855O for the sole purpose of ordering and referring items and/or services to beneficiaries in the<br />
<strong>Medicare</strong> program.<br />
What You Need To Know<br />
This article is based on Change Request (CR) 7723, which furnishes instructions to <strong>Medicare</strong> contractors<br />
(carriers and <strong>Medicare</strong> Administrative Contractors (A/B MACs)) regarding the processing of Form CMS-<br />
855O submissions. Specific topics in CR 7723 include, but are not limited to: (1) initial applications, (2)<br />
changes of information, and (3) revocations. Model letters that <strong>Medicare</strong> contractors will use in<br />
communicating with providers on these issues are also provided in CR7723, which is available at<br />
http://www.cms.gov/Transmittals/downloads/R410PI.pdf on the Centers for <strong>Medicare</strong> & Medicaid Services<br />
(CMS) website.<br />
Background<br />
Generally, depending upon State law, the following physicians and non-physician practitioners are<br />
permitted to order or refer items or services for <strong>Medicare</strong> beneficiaries:<br />
Doctors of medicine or osteopathy;<br />
Doctors of dental surgery or dental medicine;<br />
Doctors of podiatry;<br />
Doctors of optometry;<br />
Physician assistants;<br />
Certified clinical nurse specialists;<br />
Nurse practitioners;<br />
Clinical psychologists;<br />
Certified nurse midwives; and<br />
Clinical social workers.<br />
Most physicians and non-physician practitioners enroll in <strong>Medicare</strong> so they can receive reimbursement for<br />
covered services to <strong>Medicare</strong> beneficiaries. However, some physicians and non-physician practitioners who<br />
are not enrolled in <strong>Medicare</strong> via the Form CMS-855I may wish to order or refer items or services for<br />
<strong>Medicare</strong> beneficiaries. These individuals can become eligible to do so by completing the Form CMS-855O<br />
via paper or the Internet-based Provider Enrollment, Chain and Ownership System (PECOS) process.<br />
It is important to note that physicians and non-physician practitioners that complete the Form CMS-855O do<br />
not and will not send claims to a <strong>Medicare</strong> contractor for services they furnish. They are not afforded<br />
<strong>Medicare</strong> billing privileges for the purpose of submitting claims to <strong>Medicare</strong> directly for services that they<br />
furnish to beneficiaries.<br />
Key Points of CR7723<br />
Upon receipt of an initial Form CMS-855O or a Form CMS-855O change of information request (or<br />
a certification statement for PECOS submissions), the <strong>Medicare</strong> contractor shall pre-screen the form.<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 37
Unless stated otherwise in another CMS directive, the contractor shall verify all of the information<br />
on an initial Form CMS-855O submission.<br />
If, at any time during the pre-screening or verification process for an initial Form CMS-855O<br />
submission or a Form CMS-855O change of information request, the contractor needs additional or<br />
clarifying information from the supplier, it shall follow existing CMS instructions for obtaining this<br />
data.<br />
Upon completion of its review of an initial Form CMS-855O submission or a Form CMS-855O<br />
change of information request, the contractor shall approve, deny, or reject the submission.<br />
The contractor shall reject an initial Form CMS-855O submission or a Form CMS-855O change of<br />
information request, if the supplier fails to furnish all required information on the form within 30<br />
calendar days of the contractor’s request to do so.<br />
When denying or rejecting a Form CMS-855O submission, the contractor shall: (1) switch the<br />
PECOS record to a “denied” or “rejected” status (as applicable), and (2) send a letter to the supplier<br />
notifying him or her of the denial or rejection and the reason(s) for it.<br />
For suppliers whose Form CMS-855O submissions are approved, the contractor shall treat the<br />
supplier as a non-participating supplier.<br />
If the contractor approves an initial Form CMS-855O submission, the contractor shall: (1) switch the<br />
PECOS record to an “approved” status, and (2) send a letter (via mail or e-mail) to the supplier<br />
notifying him or her of the approval.<br />
If the contractor determines that grounds exist for revoking a supplier’s Form CMS-855O<br />
enrollment, it shall: (1) switch the supplier’s PECOS record to a “revoked” status, (2) end-date the<br />
PECOS record, and (3) send a letter to the supplier stating that his or her Form CMS-855O<br />
enrollment has been revoked.<br />
Additional Information<br />
The official instruction, CR 7723 issued to your carrier or A/B MAC regarding this change may be viewed<br />
at http://www.cms.gov/Transmittals/downloads/R410PI.pdf on the CMS website.<br />
MLN Matters® MM7723<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 38
Use of Revised Remittance Advice Remark Code (RARC) N103 When<br />
Denying Services Furnished to Federally Incarcerated Beneficiaries -<br />
Revised<br />
Note: This article was revised on March 9, <strong>2012</strong> to reflect the revised CR7678 issued on March 7. In this<br />
article, the CR release date, transmittal number, and the Web address for accessing CR7678 were revised.<br />
All other information is the same.<br />
Provider Types Affected<br />
Providers submitting claims to <strong>Medicare</strong> contractors (Fiscal Intermediaries (FIs), carriers, A/B <strong>Medicare</strong><br />
Administrative Contractors (MACs) and Durable Medical Equipment MACs or DME MACs) for <strong>Medicare</strong><br />
beneficiaries who are incarcerated in a Federal facility.<br />
Provider Action Needed<br />
This article is based on Change Request (CR) 7678 which informs <strong>Medicare</strong> contractors that the Centers for<br />
<strong>Medicare</strong> & Medicaid Services (CMS) is amending Remittance Advice Remark Code (RARC) N103 to<br />
include language that further explains the newly modified RARC N103—denying claims for services to<br />
federally incarcerated beneficiaries.<br />
CR7678 is limited to providers billing for services for beneficiaries while they are in Federal, State, or local<br />
custody and the goal of this CR7678 is to be more specific in explaining the accompanying adjustment.<br />
See the ‘Background’, ‘Key Points’, and ‘Additional Information’ sections of this article for details<br />
regarding these changes.<br />
Background<br />
The following exclusions presumptively apply to individuals who are incarcerated in a Federal facility under<br />
Federal authority:<br />
According to Federal regulations at 42 Code of Federal Regulations (CFR) Section 411.4 <strong>Medicare</strong><br />
does not pay for services furnished to a beneficiary who has no legal obligation to pay for the service<br />
and no other person or organization has a legal obligation to provide or pay for the service;<br />
Under 42 CFR 411.6, <strong>Medicare</strong> does not pay for services furnished by a federal provider of services<br />
or by a federal agency; and<br />
Under 42 CFR 411.8, <strong>Medicare</strong> does not pay for services that are paid for directly or indirectly by a<br />
governmental entity.<br />
Key Points<br />
When denying claims for services furnished to federally incarcerated <strong>Medicare</strong> beneficiaries, the newly<br />
modified RARC N103 will be used (in addition to remittance advice language already in use) and it reads as<br />
follows:<br />
“Social Security records indicate that this patient was a prisoner when the service was rendered. This payer<br />
does not cover items and services furnished to an individual while he or she is in a Federal facility, or while<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 39
he or she is in State or local custody under a penal authority, unless under State or local law, the individual<br />
is personally liable for the cost of his or her health care while incarcerated and the State or local government<br />
pursues such debt in the same way and with the same vigor as any other debt.”<br />
Additional Information<br />
The official instruction, CR7678, issued to your <strong>Medicare</strong> contractors (FIs, A/B MACs, DME MACs, and<br />
carriers) regarding this change, may be viewed at<br />
http://www.cms.gov/Transmittals/downloads/R1054OTN.pdf on the CMS website.<br />
If you have any questions, please contact your <strong>Medicare</strong> contractor at their toll-free number, which may be<br />
found at http://www.cms.gov/MLNProducts/.<br />
MLN Matters® MM7678<br />
<strong>Medicare</strong> B <strong>Newsline</strong> <strong>April</strong> <strong>2012</strong> 40
<strong>Medicare</strong> B <strong>Newsline</strong> Quality Survey<br />
Please take a moment to let us know your thoughts regarding this issue of the <strong>Medicare</strong> B <strong>Newsline</strong>.<br />
Your Name (optional):<br />
Telephone Number (optional):<br />
1. Usefulness of the information.<br />
Please rate the publication by circling the number of your choice.<br />
(10 = Excellent, 5 = Satisfactory, 1 = Unacceptable)<br />
1 2 3 4 5 6 7 8 9 10<br />
2. Organization and layout of the information.<br />
1 2 3 4 5 6 7 8 9 10<br />
3. Design and physical appearance of the publication.<br />
1 2 3 4 5 6 7 8 9 10<br />
4. Value of <strong>Medicare</strong> A <strong>Newsline</strong> as a reference item.<br />
1 2 3 4 5 6 7 8 9 10<br />
5. Do you use the website to obtain copies of the <strong>Medicare</strong> newsletter?<br />
Yes<br />
No<br />
6. What can we do to make <strong>Medicare</strong> B <strong>Newsline</strong> a more effective publication?<br />
Thank you for your time. You can email your response by clicking SUBMIT.<br />
Fax or mail your response to:<br />
<strong>Cahaba</strong> Government Benefit Administrators, LLC<br />
Provider Outreach and Education<br />
PO Box 12967<br />
Birmingham, Alabama 35202<br />
Fax: 205 220-1531<br />
<strong>Medicare</strong> B <strong>Newsline</strong>