Medicare Part B Newsline March 2012 - Cahaba GBA
Medicare Part B Newsline March 2012 - Cahaba GBA
Medicare Part B Newsline March 2012 - Cahaba GBA
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
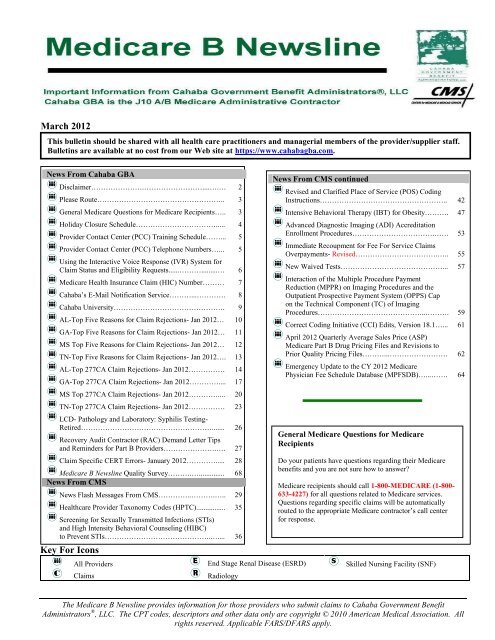
<strong>March</strong> <strong>2012</strong>This bulletin should be shared with all health care practitioners and managerial members of the provider/supplier staff.Bulletins are available at no cost from our Web site at https://www.cahabagba.com.News From <strong>Cahaba</strong> <strong>GBA</strong>Disclaimer………………….……………………....….… 2Please Route…………………………………………….. 3General <strong>Medicare</strong> Questions for <strong>Medicare</strong> Recipients….. 3Holiday Closure Schedule……………………………..... 4Provider Contact Center (PCC) Training Schedule……... 5Provider Contact Center (PCC) Telephone Numbers…... 5Using the Interactive Voice Response (IVR) System forClaim Status and Eligibility Requests......……….........… 6<strong>Medicare</strong> Health Insurance Claim (HIC) Number……… 7<strong>Cahaba</strong>’s E-Mail Notification Service………...………… 8<strong>Cahaba</strong> University………………………………………. 9AL-Top Five Reasons for Claim Rejections- Jan <strong>2012</strong>… 10GA-Top Five Reasons for Claim Rejections- Jan <strong>2012</strong>… 11MS Top Five Reasons for Claim Rejections- Jan <strong>2012</strong>… 12TN-Top Five Reasons for Claim Rejections- Jan <strong>2012</strong>…. 13AL-Top 277CA Claim Rejections- Jan <strong>2012</strong>…………… 14GA-Top 277CA Claim Rejections- Jan <strong>2012</strong>………….... 17MS Top 277CA Claim Rejections- Jan <strong>2012</strong>………….... 20TN-Top 277CA Claim Rejections- Jan <strong>2012</strong>…………… 23LCD- Pathology and Laboratory: Syphilis Testing-Retired………………………………………………....... 26Recovery Audit Contractor (RAC) Demand Letter Tipsand Reminders for <strong>Part</strong> B Providers………………….…. 27Claim Specific CERT Errors- January <strong>2012</strong>…………..... 28<strong>Medicare</strong> B <strong>Newsline</strong> Quality Survey……….….............. 68News From CMSNews Flash Messages From CMS…………..……….….. 29Healthcare Provider Taxonomy Codes (HPTC)................ 35Screening for Sexually Transmitted Infections (STIs)and High Intensity Behavioral Counseling (HIBC)to Prevent STIs……………………………………..….... 36Key For IconsAll ProvidersClaimsEnd Stage Renal Disease (ESRD)RadiologyNews From CMS continuedRevised and Clarified Place of Service (POS) CodingInstructions…………………………………………….. 42Intensive Behavioral Therapy (IBT) for Obesity………. 47Advanced Diagnostic Imaging (ADI) AccreditationEnrollment Procedures…………………………….…… 53Immediate Recoupment for Fee For Service ClaimsOverpayments- Revised…………………………….….. 55New Waived Tests……………………………………... 57Interaction of the Multiple Procedure PaymentReduction (MPPR) on Imaging Procedures and theOutpatient Prospective Payment System (OPPS) Capon the Technical Component (TC) of ImagingProcedures……………………………………...………. 59Correct Coding Initiative (CCI) Edits, Version 18.1…... 61April <strong>2012</strong> Quarterly Average Sales Price (ASP)<strong>Medicare</strong> <strong>Part</strong> B Drug Pricing Files and Revisions toPrior Quality Pricing Files………...…………………… 62Emergency Update to the CY <strong>2012</strong> <strong>Medicare</strong>Physician Fee Schedule Database (MPFSDB)…...……. 64General <strong>Medicare</strong> Questions for <strong>Medicare</strong>RecipientsDo your patients have questions regarding their <strong>Medicare</strong>benefits and you are not sure how to answer?<strong>Medicare</strong> recipients should call 1-800-MEDICARE (1-800-633-4227) for all questions related to <strong>Medicare</strong> services.Questions regarding specific claims will be automaticallyrouted to the appropriate <strong>Medicare</strong> contractor’s call centerfor response.Skilled Nursing Facility (SNF)The <strong>Medicare</strong> B <strong>Newsline</strong> provides information for those providers who submit claims to <strong>Cahaba</strong> Government BenefitAdministrators ® , LLC. The CPT codes, descriptors and other data only are copyright © 2010 American Medical Association. Allrights reserved. Applicable FARS/DFARS apply.
DisclaimerThis educational material was prepared as a tool to assist <strong>Medicare</strong> providers and other interested parties and is not intended togrant rights or impose obligations. Although every reasonable effort has been made to assure the accuracy of the informationwithin this module, the ultimate responsibility for the correct submission of claims lies with the provider of services. <strong>Cahaba</strong><strong>GBA</strong>, LLC employees, agents, and staff make no representation, warranty, or guarantee that this compilation of <strong>Medicare</strong>information is error-free and will bear no responsibility or liability for the results or consequences of the use of these materials.This publication is a general summary that explains certain aspects of the <strong>Medicare</strong> Program, but is not a legal document. Theofficial <strong>Medicare</strong> Program provisions are contained in the relevant laws, regulations, and rulings.We encourage users to review the specific statues, regulations and other interpretive materials for a full and accurate statementof their contents. Although this material is not copyrighted, CMS prohibits reproduction for profit making purposes.American Medical Association Notice and DisclaimerCPT codes, descriptors and other data only are Copyright 2011 American Medical Association. All rights reserved.ICD-9 NoticeThe ICD-9-CM codes and descriptors used in this material are copyright 2011 under uniform copyright convention. All rightsreserved.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 2
Holiday Closure Schedule-<strong>2012</strong><strong>Cahaba</strong> <strong>GBA</strong>’s <strong>Medicare</strong> offices in Birmingham, AL; Douglasville, GA, Savannah, GA; and Chattanooga,TN are closed on the following days listed below in <strong>2012</strong>. In addition, all <strong>Medicare</strong> Provider ContactCenters (PCC) close on federal holidays for continuing education training; therefore, customer servicerepresentatives will not be available on those days to receive your calls.Holiday / DateNew Year’s Day ObservedJanuary 2, <strong>2012</strong>MondayMartin Luther King BirthdayJanuary 16, <strong>2012</strong>MondayPresident’s DayFebruary 20, <strong>2012</strong>MondayGood FridayApril 6, <strong>2012</strong>FridayMemorial DayMay 28, <strong>2012</strong>MondayIndependence DayJuly 4, <strong>2012</strong>WednesdayLabor DaySeptember 3, <strong>2012</strong>MondayColumbus DayOctober 8, <strong>2012</strong>MondayVeterans Day ObservedNovember 12, <strong>2012</strong>MondayThanksgivingNovember 22-23, <strong>2012</strong>Thursday/FridayChristmasDecember 24-25, <strong>2012</strong>Monday/TuesdayNew Year’s DayJanuary 1, 2013TuesdayClosure ScheduleAll Offices ClosedAll Offices ClosedPCC Closed for TrainingAll Offices ClosedAll Offices ClosedAll Offices ClosedAll Offices ClosedPCC Closed for TrainingPCC Closed for TrainingAll Offices ClosedAll Offices ClosedAll Offices Closed<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 4
Provider Contact Center– Training Schedule<strong>Medicare</strong> is a continuously changing program, and it is important that we provide correct and accurateanswers to your questions. To better serve the provider community, the Centers for <strong>Medicare</strong> & MedicaidServices (CMS) allows the Provider Contact Centers the opportunity to offer training to our CustomerService Representatives (CSRs). Listed below are the dates and times the Provider Contact Center will beclosed for training.PCC Training DatesFriday, April 13, <strong>2012</strong>Friday, April 20, <strong>2012</strong>Friday, April 27, <strong>2012</strong>Time9:30 a.m.- 11:30 a.m. CST/10:30 a.m.- 12:30 p.m. EST9:30 a.m.- 11:30 a.m. CST/10:30 a.m.- 12:30 p.m. EST9:30 a.m.- 11:30 a.m. CST/10:30 a.m.- 12:30 p.m. ESTProvider Contact Center Telephone NumbersAlabama B, Georgia B, and Tennessee B: 877 567-7271Mississippi B: 866 419-9454Our Interactive Voice Response (IVR) system is designed to assist providers in obtaining answers tonumerous issues through self-service options. Options on our IVR include information regarding patienteligibility, checks, claims, deductible and other general information. Please note that our Customer ServiceRepresentatives (CSRs) are available to answer questions that cannot be answered by the IVR. CSRs arephysically located in Birmingham, Alabama and Savannah, Georgia. When your call is received, it is routedto the next available representative. CSRs are available Monday through Friday 8:00 a.m. until 4:00 p.m. inyour time zone.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 5
Using the Interactive Voice Response (IVR) System for Claim Status andEligibility Requests<strong>Cahaba</strong> Government Benefit Administrators®, LLC is experiencing a high volume of providers who areopting out of the Interactive Voice Response (IVR) system to speak to a Customer Service Representative(CSR) for information that can be accessed through the IVR.The Centers for <strong>Medicare</strong> and Medicaid Services (CMS) Internet Only Manual (IOM) Chapter 6 Section50.1 states:“Providers shall be required to use IVRs to access claim status and beneficiary eligibilityinformation. CSRs shall refer providers back to the IVR if they have questions about claims statusor eligibility that can be handled by the IVR. CSRs may provide claims status and/or eligibilityinformation if it is clear that the provider cannot access the information through the IVR because theIVR is not functioning.”If you are requesting whether <strong>Cahaba</strong> has received a claim or if a claim has finalized, this isconsidered a claim status request.In addition, according to IOM Chapter 6 Section 80.3.4, “If a CSR or written inquiry correspondent receivesan inquiry about information that can be found on a Remittance Advice (RA), the CSR/correspondentshould take the opportunity to educate the inquirer on how to read the RA, in an effort to encourage the useof self-service. The CSR/correspondent should advise the inquirer that the RA is needed in order to answerany questions for which answers are available on the RA. Providers should also be advised that any billingstaff or representatives that make inquiries on his/her behalf will need a copy of the RA.”<strong>Cahaba</strong> CSRs have visibility as to the path the provider takes in the IVR and/or whether they opt out tospeak with a representative up front. The CSR will instruct the provider to call back and utilize the IVR ifthey did not attempt to use this self service option as required by CMS.Provider Contact Center (PCC)<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 6
<strong>Medicare</strong> Health Insurance Claim (HIC) NumberA <strong>Medicare</strong> card is issued to every person who is entitled to <strong>Medicare</strong> benefits and may be identified by its red, whiteand blue coloring. This card identifies the <strong>Medicare</strong> beneficiary and includes the following information:Name (exactly as it appears on the Social Security records);<strong>Medicare</strong> Health Insurance Claim (HIC) number;Beginning date of <strong>Medicare</strong> entitlement for hospital and/or medical insurance;Sex and Beneficiary's signature.Three of the top five reasons for claim rejection in any given month are for:The last name submitted for the beneficiary does not match the last name we have on record for the HICnumber on the claim. The beneficiary's last name must include apostrophes, spaces, hyphens, etc., if theyappear in the beneficiary's last name on his or her <strong>Medicare</strong> card.The first name submitted for the beneficiary does not match the first name we have on record for the HICnumber on the claim. The beneficiary's first name must appear as it does on the beneficiary's <strong>Medicare</strong>card. This includes spaces, hyphens, apostrophes, etc.The HIC number not matching the name we have on record. The <strong>Medicare</strong> Claim Number must appear onthe claim exactly as it does on the beneficiary’s card, without the dashes and with no spaces.It is extremely important that you submit the patient’s complete name and HIC number to <strong>Medicare</strong> or any otherhealth care provider you use (i.e. clinical laboratories, radiology imaging groups, or outpatient therapy providers,etc.). This will ensure that those providers have the correct patient information to file their claims as well.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 7
<strong>Cahaba</strong>’s E-mail Notification Service Subscription Process<strong>Cahaba</strong> <strong>GBA</strong> recently implemented changes that simplify the process in which providers subscribe to our e-mail notification service (Listserv). New members simply provide their name, city, state, zip code, e-mailaddress, and an optional password. In addition, they can select from two different lists to subscribe to:• J10 <strong>Part</strong> A News• J10 <strong>Part</strong> B News*Once you are a member, you can edit your profile to:• unsubscribe from all lists• subscribe to additional lists• update your e-mail address• change your name or address information• change what <strong>Cahaba</strong> lists you are subscribed to.Already a Member?If you enrolled to <strong>Cahaba</strong>’s Listserv prior to November 1, 2009, you will continue to receive messages.However, depending on the selections you made on the subscription form when you originally enrolled, youmay receive messages from more than one <strong>Cahaba</strong> list. To change the list you are subscribed to, access the“Edit Your E-mail Notification Service Member Profile” Web page to review and edit your profile.In order to ensure that you receive your subscription emails and announcements from <strong>Cahaba</strong> <strong>GBA</strong>, pleaseadd us to your contact lists, adjust your spam settings, or follow the instructions from your email provideron how to prevent our emails from being marked “Spam” or “Junk Mail”.*Mississippi <strong>Medicare</strong> <strong>Part</strong> B providers will choose J10 <strong>Part</strong> B News for their selection to receive <strong>Medicare</strong><strong>Part</strong> B information.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 8
<strong>Cahaba</strong> University<strong>Cahaba</strong> <strong>GBA</strong> proudly introduces “<strong>Cahaba</strong> University,” an online self-service training tool for our providercommunity and their staff.<strong>Cahaba</strong> University is an educational program designed to provide a broad variety of <strong>Medicare</strong> relatedtraining to meet the needs of <strong>Medicare</strong> health care providers and suppliers. It is powered by Centra, alearning management system that will allow registered users to manage their own learning. <strong>Cahaba</strong>University allows for a blended e-learning environment. Blended means that users are allowed to register forWebinars, teleconferences, as well as assign self-paced learning tracks. It also provides centralizedmanagement and access to content created by the Provider Outreach and Education department for theprovider community.Our staff of well-trained professionals wants every provider to be pleased with their learning experience.We know you’re just as concerned about your claims being processed for your facility as you are about thequality of care administered to your <strong>Medicare</strong> patients. That is why we always try to provide additionaleducation and outreach activities to help improve this process.<strong>Cahaba</strong> University is located athttp://www.cahabagba.com/part_b/education_and_outreach/<strong>Cahaba</strong>University.pdf. All providers areencouraged to create a user profile. Click the “Create a new account” link, and then select either a <strong>Part</strong> A or<strong>Part</strong> B account. You must create a username and password to login. Make sure all the appropriate fields arecompleted. Once the account is created, log in using your new user name and password. Remember, yourusername and password is case-sensitive!<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 9
Alabama <strong>Medicare</strong> <strong>Part</strong> BTop Five Reasons for EDI Claim Rejections for January <strong>2012</strong>Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, alongwith claims that were rejected and the reason for the rejection. Referring to this report will allow you tocorrect and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will alsobecome aware of any major problems with your claims so they can be corrected before they create aninterruption in your cash flow. Audit trail reports are available the next business day for files that arereceived before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your softwarevendor, billing service, or clearing house.See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that mightbe referenced in an edit.In order to increase the number of claims that successfully pass through audit trails and into processing<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For themonth of January <strong>2012</strong>, these are:Claim DescriptionRejection213 INVALID PAYER ID OR QUAL IN 2010BBA payer ID or qualifier was submitted in the 2010BB loop(Payer Name) that is not valid for <strong>Medicare</strong> <strong>Part</strong> B.434 PROC CODE REQUIRES REFERRING NPIProcedure code billed was for a diagnostic procedure such as anx-ray or lab work which requires the NPI of the orderingphysician, or a consultation, which requires the NPI of thereferring physician, and this was not submitted on the claim.421 DIAG CODE (XXXXX) INVALID FOR DATE SVCThe date of service was outside of the effective date range ofthe diagnosis code used. The invalid diagnosis code will appearinside the parenthesis.888 INSTREAM REJECTIONThere was a problem involving HIPAA required loops,segments, or values. The specific loop will be identified, forexample, 'ELEMENT N401 (D.E. 19) AT COL. 4 ISMISSING, THOUGH MARKED "MUST BE USED"(LOOP:2010BA POS:3140)'. The number after 'POS' indicatesthe position in the file where the error occurred377 PAID & ADJUSTMENT AMOUNTS DO NOT EQUALCLAIM CHARGThe claim was submitted as <strong>Medicare</strong> Secondary Payer but theprimary paid amount plus the primary adjustment amounts donot equal the total claim charge.Number ofClaims701689595447439<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 10
Georgia <strong>Medicare</strong> <strong>Part</strong> BTop Five Reasons for EDI Claim Rejections for January <strong>2012</strong>Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, alongwith claims that were rejected and the reason for the rejection. Referring to this report will allow you tocorrect and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will alsobecome aware of any major problems with your claims so they can be corrected before they create aninterruption in your cash flow. Audit trail reports are available the next business day for files that arereceived before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your softwarevendor, billing service, or clearing house.See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that mightbe referenced in an edit.In order to increase the number of claims that successfully pass through audit trails and into processing<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For themonth of January <strong>2012</strong>, these are:Claim DescriptionRejection434 PROC CODE REQUIRES REFERRING NPIProcedure code billed was for a diagnostic procedure such as anx-ray or lab work which requires the NPI of the orderingphysician, or a consultation, which requires the NPI of thereferring physician, and this was not submitted on the claim.888 INSTREAM REJECTIONThere was a problem involving HIPAA required loops,segments, or values. The specific loop will be identified, forexample, 'ELEMENT N401 (D.E. 19) AT COL. 4 IS MISSING,THOUGH MARKED "MUST BE USED" (LOOP:2010BAPOS:3140)'. The number after 'POS' indicates the position in thefile where the error occurred385 CLAIM CONTAINS A MEDICARE LEGACY ID IN LOOP: XXXXThe indicated loop contained a legacy provider number, such asa commercial insurance number or a UPIN.421 DIAG CODE (XXXXX) INVALID FOR DATE SVCThe date of service was outside of the effective date range of thediagnosis code used. The invalid diagnosis code will appearinside the parenthesis.207 INVALID HIC NUMBER SUFFIXThe suffix in the Health Insurance Claim (HIC) numbersubmitted for the beneficiary is invalid. For an explanation ofHIC numbers and suffixes please visithttps://www.cahabagba.com/part_b/education_and_outreach/general_billing_info/hic_suffixes.htm.Number ofClaims2,2371,5371,3021,2331,135<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 11
Mississippi <strong>Medicare</strong> <strong>Part</strong> BTop Five Reasons for EDI Claim Rejections for January <strong>2012</strong>Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, alongwith claims that were rejected and the reason for the rejection. Referring to this report will allow you tocorrect and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will alsobecome aware of any major problems with your claims so they can be corrected before they create aninterruption in your cash flow. Audit trail reports are available the next business day for files that arereceived before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your softwarevendor, billing service, or clearing house.See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that mightbe referenced in an edit.In order to increase the number of claims that successfully pass through audit trails and into processing<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For themonth of January <strong>2012</strong>, these are:Claim DescriptionRejection888 INSTREAM REJECTIONThere was a problem involving HIPAA required loops,segments, or values. The specific loop will be identified, forexample, 'ELEMENT N401 (D.E. 19) AT COL. 4 IS MISSING,THOUGH MARKED "MUST BE USED" (LOOP:2010BAPOS:3140)'. The number after 'POS' indicates the position in thefile where the error occurred. If you need help locating specificpositions in your 4010A1 file here is an article explaining oneway you can do this:http://www.cahabagba.com/part_b/edi/hipaa_identifying_your_errors.htm.307 DIAG CODE (XXXXX) INVALID OR INACTIVEThe diagnosis code indicated is invalid, or was inactive on thedate of service billed.434 PROC CODE REQUIRES REFERRING NPIProcedure code billed was for a diagnostic procedure such as anx-ray or lab work which requires the NPI of the orderingphysician, or a consultation, which requires the NPI of thereferring physician, and this was not submitted on the claim421 DIAG CODE (XXXXX) INVALID FOR DATE SVCThe date of service was outside of the effective date range of thediagnosis code used. The invalid diagnosis code will appearinside the parenthesis.302 INVALID BILLING (NO CHARGES BILLED)Claim must contain at least one item with an associated billedamount.Number ofClaims3,0571,564609539226<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 12
Tennessee <strong>Medicare</strong> <strong>Part</strong> BTop Five Reasons for EDI Claim Rejections for January <strong>2012</strong>Audit trails show which of your claims were accepted by the <strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A processing system, alongwith claims that were rejected and the reason for the rejection. Referring to this report will allow you tocorrect and resubmit claims quickly, resulting in a dramatically reduced turnaround time. You will alsobecome aware of any major problems with your claims so they can be corrected before they create aninterruption in your cash flow. Audit trail reports are available the next business day for files that arereceived before 3:30 p.m. Central Time. If you are not receiving your audit trails contact your softwarevendor, billing service, or clearing house.See Audit Trail Explanations for a more complete list of edits, along with descriptions of loops that mightbe referenced in an edit.In order to increase the number of claims that successfully pass through audit trails and into processing<strong>Cahaba</strong> <strong>GBA</strong> <strong>Part</strong> A EDI Services is providing you with the top five reasons for claim rejections. For themonth of January <strong>2012</strong>, these are:Claim DescriptionRejection888 INSTREAM REJECTIONThere was a problem involving HIPAA required loops,segments, or values. The specific loop will be identified, forexample, 'ELEMENT N401 (D.E. 19) AT COL. 4 IS MISSING,THOUGH MARKED "MUST BE USED" (LOOP:2010BAPOS:3140)'. The number after 'POS' indicates the position in thefile where the error occurred434 PROC CODE REQUIRES REFERRING NPIProcedure code billed was for a diagnostic procedure such as anx-ray or lab work which requires the NPI of the orderingphysician, or a consultation, which requires the NPI of thereferring physician, and this was not submitted on the claim.421 DIAG CODE (XXXXX) INVALID FOR DATE SVCThe date of service was outside of the effective date range of thediagnosis code used. The invalid diagnosis code will appear inside theparenthesis.207 INVALID HIC NUMBER SUFFIXThe suffix in the beneficiary’s <strong>Medicare</strong> number was not valid. For anexplanation of HIC numbers and their suffixes please visithttps://www.cahabagba.com/part_b/education_and_outreach/general_billing_info/hic_suffixes.htm.202 RAILROADThe beneficiary’s HIC (<strong>Medicare</strong> number) began with an alphabeticprefix, indicating the beneficiary s a Railroad retiree.Number ofClaims1,3651,187729478324<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 13
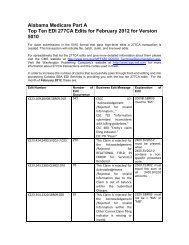
Alabama <strong>Medicare</strong> <strong>Part</strong> BTop Ten EDI 277CA Edits for January <strong>2012</strong> for Version 5010For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. Thistransaction will indicate file, batch, claim, and line level edits.For spreadsheets that list the 277CA edits and give more detailed information about them please visit theCMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the WashingtonPublishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactionsand the codes used in them.In order to increase the number of claims that successfully pass through front-end editing and intoprocessing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month ofJanuary <strong>2012</strong>, these are:ProductionEdit NumberNumber ofEditOccurrencesX222.087.2010AA.NM109.050 14,764Business EditMessageThis Claim isrejected forrelational fielddue to BillingProvider'ssubmitter notapproved forelectronicclaimsubmissions onbehalf of thisBillingProvider.X222.351.2400.SV101-7.020 8,637 This Claim isrejected forrelational fieldInformationwithin theDetaileddescription ofservice.X222.094.2010AA.REF02.050 7,451 This Claim isrejected forrelational fieldBillingProvider's NPI(NationalExplanation ofEdit2010AA.NM109billing providermust be"associated" to thesubmitter (from atrading partnermanagementperspective) in1000A.NM109.2400.SV101-7must be present.when 2400.SV101-2 is present on thetable of procedurecodes that require adescription.2010AA.REF mustbe associated withthe provideridentified in2010AA.NM109.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 14
Provider ID)and Tax ID.X222.295.2320.SBR03.006 6,993 This Claim isrejected forrelational fieldInformationsubmittedinconsistentwith billingguidelines forthe OtherInsured'sPolicy Number.X222.087.2010AA.NM109.030 6,489 This Claim isrejected forInvalidInformation inthe BillingProvider's NPI(NationalProvider ID).X222.273.2310C.N403.020 4,068 This Claim isrejected forInvalidInformation fora ServiceLocation'sPostal/Zip.X222.430.2420A.NM108.020 3,102 This Claim isrejected forMissingInformationwithin theRenderingProvider'sNationalProviderIdentifier (NPI)and IdentifierQualifier.X222.196.2300.REF.010 2,994 This Claim isrejected forInvalidInformationwithin thePayer AssignedCSCC A8:"Acknowledgement/ Rejected forrelational field inerror"CSC 163: "Entity'sPolicy Number"CSC 732"Informationsubmittedinconsistent withbilling guidelines."EIC: GB OtherInsured2010AA.NM109must be a valid NPIon the Crosswalkwhen evaluatedwith1000B.NM109.2310C.N403 mustbe a valid 9 digitZip Code.2420A.NM108must be present.2300.REF withREF01 = "F8"must not bepresent.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 15
Claim ControlNumberInformationsubmittedinconsistentwith billingguidelines.X222.351.2400.SV101-2.020 2,500 This Claim isrejected forrelational fieldInformationwithin theHCPCS.X999.DUPE 2,022 Rejected due toduplicateST/SEsubmission.When2400.SV101-1 ="HC",2400.SV101-2must be a validHCPCS Code onthe date in2400.DTP03 whenDTP01 = "472".Exact duplicate ofa previouslysubmittedtransaction set.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 16
Georgia <strong>Medicare</strong> <strong>Part</strong> BTop Ten EDI 277CA Edits for January <strong>2012</strong> for Version 5010For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. Thistransaction will indicate file, batch, claim, and line level edits.For spreadsheets that list the 277CA edits and give more detailed information about them please visit theCMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the WashingtonPublishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactionsand the codes used in them.In order to increase the number of claims that successfully pass through front-end editing and intoprocessing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month ofJanuary <strong>2012</strong>, these are:Production:Edit NumberX222.087.2010AA.NM109.050Number ofEditOccurrencesBusiness EditMessage22,737 This Claim isrejected forrelational fielddue to BillingProvider'ssubmitter notapproved forelectronicclaimsubmissionson behalf ofthis BillingProvider.X222.351.2400.SV101-7.020 19,008 This Claim isrejected forrelational fieldInformationwithin theDetaileddescription ofservice.X999.DUPE 11,462 Rejected dueto duplicateST/SEsubmission.X222.121.2010BA.NM109.0203,506 This Claim isrejected forExplanation ofEdit2010AA.NM109billing providermust be"associated" to thesubmitter (from atrading partnermanagementperspective) in1000A.NM109.2400.SV101-7must be present.when 2400.SV101-2 is present on thetable of procedurecodes that require adescription.Exact duplicate ofa previouslysubmittedtransaction set.2010BA.NM109must be 10 - 11<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 17
InvalidInformationfor aSubscriber'scontract/member number.X222.192.2300.REF02.060 3,105 This Claim isrejected forInvalidInformationwithin theAuthorization/certificationnumber.X222.273.2310C.N403.020 3,081 This Claim isrejected forInvalidInformationfor a ServiceLocation'sPostal/Zip.X222.351.2400.SV101-2.020 2,922 This Claim isrejected forrelational fieldInformationwithin theHCPCS.X222.295.2320.SBR03.006 2,590 This Claim isrejected forrelational fieldInformationsubmittedinconsistentwith billingguidelines forthe OtherInsured'sPolicyNumber.positions in theformat ofNNNNNNNNNAorNNNNNNNNNAAorNNNNNNNNNANwhere “A”represents an alphacharacter and “N”represents anumeric digit.2300.REF02 mustbe a validMammographyCertificationNumber.2310C.N403 mustbe a valid 9 digitZip Code.When2400.SV101-1 ="HC",2400.SV101-2must be a validHCPCS Code onthe date in2400.DTP03 whenDTP01 = "472".CSCC A8:"Acknowledgement / Rejected forrelational field inerror"CSC 163: "Entity'sPolicy Number"CSC 732"Informationsubmittedinconsistent withbilling guidelines."EIC: GB Other<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 18
X222.242.2300.HI01-2.020 2,322 This Claim isrejected forInvalidInformationwithin theNUBCConditionCode(s).X222.094.2010AA.REF02.0502,284 This Claim isrejected forrelational fieldBillingProvider's NPI(NationalProvider ID)and Tax ID.Insured2300.HI01-2 mustbe a validCondition code.2010AA.REF mustbe associated withthe provideridentified in2010AA.NM109.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 19
Mississippi <strong>Medicare</strong> <strong>Part</strong> BTop Ten EDI 277CA Edits for January <strong>2012</strong> for Version 5010For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. Thistransaction will indicate file, batch, claim, and line level edits.For spreadsheets that list the 277CA edits and give more detailed information about them please visit theCMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the WashingtonPublishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactionsand the codes used in them.In order to increase the number of claims that successfully pass through front-end editing and intoprocessing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month ofJanuary <strong>2012</strong>, these are:Production:Edit NumberX222.087.2010AA.NM109.050X222.351.2400.SV101-7.020Number ofEditOccurrencesDisposition/ErrorCode9,102 This Claim isrejected forrelational field dueto BillingProvider's submitternot approved forelectronic claimsubmissions onbehalf of thisBilling Provider.7,136 This Claim isrejected forrelational fieldInformation withinthe Detaileddescription ofservice.X222.273.2310C.N403.020 6,167 This Claim isrejected for InvalidInformation for aService Location'sPostal/Zip.X222.094.2010AA.REF02.0504,236 This Claim isrejected forrelational fieldExplanation ofEdit2010AA.NM109billing providermust be"associated" tothe submitter(from a tradingpartnermanagementperspective) in1000A.NM109.2400.SV101-7must be present.when2400.SV101-2 ispresent on thetable ofprocedure codesthat require adescription.2310C.N403must be a valid 9digit Zip Code.2010AA.REFmust beassociated with<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 20
Billing Provider'sNPI (NationalProvider ID) andTax ID.X222.295.2320.SBR03.006 3,621 This Claim isrejected forrelational fieldInformationsubmittedinconsistent withbilling guidelinesfor the OtherInsured's PolicyNumber.X999.DUPE 2,588 Rejected due toduplicate ST/SEsubmission.X222.351.2400.SV101-2.020X222.087.2010AA.NM109.0302,165 This Claim isrejected forrelational fieldInformation withinthe HCPCS.1,691 This Claim isrejected for InvalidInformation in theBilling Provider'sNPI (NationalProvider ID).X222.336.2330D.NM1.010 1,631 This Claim isrejected forrelational fieldInformationsubmittedinconsistent withbilling guidelinesfor the RenderingProvider's Nationalthe provideridentified in2010AA.NM109.CSCC A8:"Acknowledgement / Rejected forrelational field inerror"CSC 163:"Entity's PolicyNumber"CSC 732"Informationsubmittedinconsistent withbillingguidelines."EIC: GB OtherInsuredExact duplicateof a previouslysubmittedtransaction set.When2400.SV101-1 ="HC",2400.SV101-2must be a validHCPCS Code onthe date in2400.DTP03when DTP01 ="472".2010AA.NM109must be a validNPI on theCrosswalk whenevaluated with1000B.NM109.Segment mustnot be present.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 21
Provider Identifier(NPI).X222.403.2400.REF02.070 1,478 This Claim isrejected for InvalidInformation withintheAuthorization/certification number.2400.REF02must be a validMammographyCertificationNumber.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 22
Tennessee <strong>Medicare</strong> <strong>Part</strong> BTop Ten EDI 277CA Edits for January <strong>2012</strong> for Version 5010For claim submissions in the 5010 format that pass high-level edits a 277CA transaction is created. Thistransaction will indicate file, batch, claim, and line level edits.For spreadsheets that list the 277CA edits and give more detailed information about them please visit theCMS website at http://www.cms.gov/MFFS5010D0/20_TechnicalDocumentation.asp. Visit the WashingtonPublishing Company’s website at http://www.wpc-edi.com for more information about 277CA transactionsand the codes used in them.In order to increase the number of claims that successfully pass through front-end editing and intoprocessing <strong>Cahaba</strong> <strong>GBA</strong> EDI Services is providing you with the top ten 277CA edits. For the month ofJanuary <strong>2012</strong>, these are:Production:Edit NumberNumber ofEditOccurrencesBusiness EditMessageX223.352.2310F.REF.010 3,403 This Claim isrejected for theAcknowledgement /Rejected forInvalidInformationwithin theReferringProvider'sAdditional/Secondary Identifier.X223.109.2000B.SBR09.010 3,260 CSCC A7:"Acknowledgement /Rejected forInvalidInformation…"CSC 732"Informationsubmittedinconsistent withbillingguidelines."CSC 480"Entity's claimfiling indicator."EIC: PR "Payer"Explanation ofEdit2310F.REF mustnot be present.2000B.SBR09must be "MA".X223.424.2400.SV202- 2,172 This Claim is 2400.SV202-7<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 23
7.025 rejected for theAcknowledgement /Rejected forRELATIONALFIELD INERROR forService(s)Rendered.X223.090.2010AA.REF02.050X223.084.2010AA.NM109.0401,691 This Claim isrejected forAcknowledgement / Rejected forrelational field inerror within theBilling Provider'sNational ProviderIdentifier (NPI)and BillingProvider's tax id.1,399 This Claim isrejected forAcknowledgement / Rejected forrelational field inerror within theBilling Provider'sNational ProviderIdentifier (NPI)X223.354.2320.SBR09.020 936 This Claim isrejected for theAcknowledgement /Rejected forInvalidInformationwithin the OtherCarrier Claimfiling indicator ismissing orinvalid.X223.358.2320.CAS04.020 897 CSCC A7:"Acknowledgement /Rejected forInvalidInformation…"CSC 694:"Amount mustnot be equal tozero"must be present.when 2400.SV202-2 contains a nonspecificprocedurecode.2010AA.REF mustbe associated withthe provideridentified in2010AA.NM109.2010AA.NM109must be a valid NPIon the Crosswalkwhen evaluatedwith1000B.NM109.2320.SBR09 mustnot be = "MA" or"MB".2320.CAS04 mustnot = 0.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 24
X223.424.2400.SV202-2.020CSC 520:"AdjustmentQuantity"EIC: GB "OtherInsured".765 This Claim isrejected for theAcknowledgement /Rejected forInvalidInformationwithin theHCPCS.X223.424.2400.SV205.030 710 CSCC A7:"Acknowledgement /Rejected forInvalidInformation…"CSC 507:"HCPCS"X223.112.2010BA.NM109.020465 This Claim isrejected forAcknowledgement /Rejected forInvalidInformationwithin theSubscriber'scontract/membernumber.When2400.SV202-1 ="HC",2400.SV202-2must be a validHCPCS Code.When2400.SV202-1 ="HC",2400.SV202-2must be a validHCPCS Code.2010BA.NM109must be 7 - 12positions in theformat ofANNNNNN,AANNNNNN,ANNNNNNNNN,AANNNNNNNNN, AAANNNNNN,orAAANNNNNNNNN where “A”represents an alphacharacter and “N”represents anumeric digit.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 25
LCD – Pathology and Laboratory: Syphilis Testing- RetiredJ10 MAC B (Alabama, Georgia, Tennessee) (L30013)Carrier 00512 (Mississippi) (L31293)Effective November 7, 2011 the Local Coverage Determinations (LCDs) for Pathology and Laboratory:Syphilis Testing is retired. :<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 26
Recovery Audit Contractor (RAC) Demands Letters Tips and Remindersfor <strong>Part</strong> B ProvidersWith the implementation of Change Request (CR) 7436, responsibility for the issuance of Recovery AuditContractor (RAC) demand letters was shifted to the <strong>Medicare</strong> Administrative Contractors (MACs) effectiveJanuary 1, <strong>2012</strong>. Connolly Healthcare, the RAC for J10 and Mississippi <strong>Part</strong> B providers, will continue tosubmit claims adjustments to <strong>Cahaba</strong> Government Benefit Administrators ® , LLC (<strong>Cahaba</strong> <strong>GBA</strong>). <strong>Cahaba</strong><strong>GBA</strong> will process the adjustments based upon the review conducted by Connolly Healthcare and issue anautomated demand letter.The demand letters are generated based on an automated system setup by CMS which creates letter addressinformation for your practice or office that was obtained from your provider enrollment data. This addressis defined as the “Special Payment” address (e.g., remittance notices, special payments) in Section 4B onyour Provider/Supplier Enrollment application, CMS Form-855B. Providers may choose to update theiraddress information via the CMS Form-855B. Please note this change would impact other demand lettercorrespondence (non-RAC) that is also generated from the “Special Payment” address.Connolly Healthcare continues to be responsible for communicating to providers the rationale for claimadjustments initiated by their office. Connolly Healthcare will also continue sending letters to providerswith this information and is responsible for responding to providers regarding the rationale for the claimadjustments.Providers may visit the Connolly Healthcare RAC website at www.connollyhealthcare.com/RAC to reviewthe rationale for RAC transactions. To access the Provider Portal Login, enter the state abbreviation,<strong>Medicare</strong> provider number and the total charge amount listed for the appropriate ICN.Contact information for Connolly Healthcare is provided below:Connolly Healthcare RAC OfficeThe Navy Yard Corporate CenterOne Crescent Drive, Suite 300-APhiladelphia, PA 19112Toll-free phone number: (866) 360-2507Fax number: (203) 529-2995For additional information issued review the CMS MLN Matters article athttps://www.cms.gov/MLNMattersArticles/downloads/MM7436.pdf.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 27
Claim Specific CERT Errors- January <strong>2012</strong>J10 MAC B (Alabama, Georgia, Tennessee)Carrier 00512 (Mississippi)The Comprehensive Error Rate Testing (CERT) Program was implemented by the Centers for <strong>Medicare</strong> &Medicaid Services (CMS) to monitor the accuracy of claims processing by <strong>Medicare</strong> contractors, like<strong>Cahaba</strong>. Contractors are then notified by CERT of the errors and findings.We would like to remind you that should you receive an Additional Documentation Request (ADR) such asa request for records to support services that are involved in a CERT review, you should submit theappropriate documentation to support the services billed, including but not limited to progress note(s) tomatch the DOS billed, lab results, operative reports, diagnostic tests, physician orders, etc. <strong>Medicare</strong>requires a legible identifier for services provided/ordered. The method used shall be hand written or anelectronic signature (stamp signatures are not acceptable) to sign an order or other medical recorddocumentation for medical review purposes.Providers may appeal unfavorable decisions with additional supporting documentation. For detailedinformation regarding the Appeals Process, refer to the following link:www.cahabagba.com/part_b/claims/appeals_process.htm.Please contact the Provider Contact Center for individual questions concerning CERT errors:Alabama, Georgia and Tennessee Providers – 1-877-567-7271Mississippi Providers – 1-866-419-9454This summary provides examples of <strong>Cahaba</strong>'s errors identified by CERT. We encourage all providers toreview this listing to educate you on common errors. This information will be updated periodically. Theintent in providing this information is to prompt you to conduct an internal analysis of <strong>Medicare</strong> billing andreduce future denials by <strong>Medicare</strong>.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 28
News Flash Messages from CMS For All <strong>Part</strong> B ProvidersPresident Obama Signs the Middle Class Tax Relief and Job CreationAct of <strong>2012</strong>--New Law Includes Physician Update Fix through December <strong>2012</strong>--On Wednesday, February 22, <strong>2012</strong>, President Obama signed into law the Middle Class Tax Reliefand Job Creation Act of <strong>2012</strong> (Job Creation Act). This new law prevents a scheduled payment cutfor physicians and other practitioners who treat <strong>Medicare</strong> patients from taking effect on <strong>March</strong> 1,<strong>2012</strong>. The new law extends the current zero percent update for such services through December 31 ,<strong>2012</strong>. President Obama remains committed to a permanent solution to eliminating the SustainableGrowth Rate reductions, which result from the existing statutory methodology. The Administrationwill continue to work with Congress to achieve this goal, as well as implement the policies in theAffordable Care Act to move toward a patient-centered, quality oriented system.The new law extends several provisions of the Temporary Payroll Tax Cut Continuation Act of 2011(Continuation Act). Specifically, the following <strong>Medicare</strong> fee-for-service policies have been extended.We also have included <strong>Medicare</strong> billing and claims processing information associated with the newlegislation. Please note that these provisions do not reflect all of the <strong>Medicare</strong> provisions in th e newlaw, as some provisions are effective later in the year and more information about those provisionswill be forthcoming.Section 3003 - Physician Payment Update - The new law extends the current zero percent update forclaims with dates of service on or after <strong>March</strong> 1, <strong>2012</strong>, through December 31, <strong>2012</strong>. However, thenew law does not extend Sections 307 and 309 of the Continuation Act, the five percent physician feeschedule mental health add-on payment and the special 2011 payment rates for bone massmeasurement, respectively. The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) is currentlyrevising the <strong>2012</strong> <strong>Medicare</strong> Physician Fee Schedule (MPFS) to reflect the expiration of both of theseprovisions. In order to allow sufficient time to develop, test, and implement the revised MPFS,<strong>Medicare</strong> claims administration contractors may hold mental health and bone density claims with<strong>March</strong> <strong>2012</strong> dates of service for up to 10 business days. We expect these claims to be released intoprocessing no later than <strong>March</strong> 15, <strong>2012</strong>. Other <strong>March</strong> <strong>2012</strong> claims will be unaffected by this claimhold. Claims with dates of service prior to <strong>March</strong> 1, <strong>2012</strong>, also are unaffected. Finally, <strong>Medicare</strong>contractors will be posting the new mental health and bone density rates on their websites no laterthan <strong>March</strong> 15, <strong>2012</strong>.Section 3004 - Extension of <strong>Medicare</strong> Physician Work Geographic Adjustment Floor - Theexisting 1.0 floor on the physician work geographic practice cost index is extended through December31, <strong>2012</strong>. As with the physician payment update, this extension will be reflected in the revised <strong>2012</strong>MPFS.Section 3001 - Extension of <strong>Medicare</strong> Modernization Act Section 508 Reclassifications -Section 3001 extends Section 508 reclassifications and certain special exception wage indexes fromDecember 1, 2011, through <strong>March</strong> 31, <strong>2012</strong>. For the period beginning on December 1, 2011, and ending on<strong>March</strong> 31, <strong>2012</strong>, section 3001 also requires (as did section 302 of the Continuation Act) removing Section508 and special exception wage data from the calculation of the reclassified wage index if doing so raisesthe reclassified wage index. All hospitals receiving section 508 reclassifications and inpatient specialexception reclassifications under the Continuation Act and the Job Creation Act shall be assigned a specialwage index effective for October 2011 through <strong>March</strong> <strong>2012</strong>. We will apply these provisions to both<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 29
inpatient and outpatient hospital payments. A special wage index will be applicable, from January 1, <strong>2012</strong>,through June 30, <strong>2012</strong>, for hospital outpatient payments, to special exception hospitals and reclassifiedhospitals affected by these extensions. Hospital inpatient and outpatient payments under both section 302 ofthe Continuation Act and section 3001 of the Job Creation Act will be made by June 30, <strong>2012</strong>.Section 3002 - Extension of Outpatient Hold Harmless Payments - Section 3002 extends outpatienthold harmless payments for rural hospitals and sole community hospitals with 100 or fewer beds throughDecember 31, <strong>2012</strong>. However, hold harmless payments for sole community hospitals with more than 100beds were not extended by this provision and are set to expire on February 29, <strong>2012</strong>.Section 3005 - Extension of Exceptions Process for <strong>Medicare</strong> Therapy Services - Section 3005extends the exceptions process for outpatient therapy caps from <strong>March</strong> 1, <strong>2012</strong>, until December 31, <strong>2012</strong>,with some modifications to current therapy policies. Providers of outpatient therapy services are required tosubmit the KX modifier on their therapy claims, when an exception to the cap is requested for medicallynecessary services furnished through December 31, <strong>2012</strong>. In addition, the new law includes changes relatedto therapy services furnished in a hospital outpatient department (OPD). These changes impact the annualtherapy cap in <strong>2012</strong> as well as the applicability of the therapy cap exception process. More informationabout the changes affecting hospital OPDs will be forthcoming in a future issuance. Additional informationabout the exception process for therapy services may be found in the <strong>Medicare</strong> Claims Processing Manual,Pub.100-04, Chapter 5, Section 10.3: http://www.cms.gov/manuals/downloads/clm104c05.pdf.The therapy caps are determined for a beneficiary on a calendar year basis, so all beneficiaries began a newcap for outpatient therapy services received on January 1, <strong>2012</strong>. For physical therapy and speech languagepathology services combined, the <strong>2012</strong> limit for a beneficiary on incurred expenses is $1,880. There is aseparate cap for occupational therapy services which is $1,880 for <strong>2012</strong>. Deductible and coinsuranceamounts applied to therapy services count toward the amount accrued before a cap is reached, and alsoapply for services above the cap where the KX modifier is used.Section 3005 also mandates that <strong>Medicare</strong> perform manual medical review of therapy services furnishedbeginning on October 1, <strong>2012</strong>, for which an exception was requested when the beneficiary has reached adollar aggregate threshold amount of $3,700 for therapy services, including OPD therapy services, for ayear. There are two separate $3,700 aggregate annual thresholds: (1) physical therapy and speech-languagepathology services, and (2) occupational therapy services.Finally, Section 3005 requires that all claims for therapy services furnished on or after October 1, <strong>2012</strong>,include the National Provider Identifier of the physician who reviews the therapy plan.CMS will issue additional information about all of these new requirements later in the year.Section 3006 - Extension of Moratorium On Qualified Pathologists and Independent LaboratoryBilling for the Technical Component of Physician Pathology Services Furnished to Hospital Patients -Section 3006 extends the moratorium through June 30, <strong>2012</strong>. Therefore, those qualified pathologistsand independent laboratories that are eligible may continue to submit claims to <strong>Medicare</strong> for thetechnical component of physician pathology services furnished to patients of a hospital, regardless of thebeneficiary's hospitalization status (inpatient or outpatient) on the date that the service was furnished. Thispolicy continues to be effective for claims with dates of service on or after <strong>March</strong> 1, <strong>2012</strong>, through June 30,<strong>2012</strong>.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 30
Section 3007 - Extension of Ambulance Add-On Payments - Section 3007 extends through December31, <strong>2012</strong>, the following three Continuation Act ambulance payment provisions: (1) the 3 percent increasein the ambulance fee schedule amounts for covered ground ambulance transports that originate in rural areasand the 2 percent increase for covered ground ambulance transports that originate in urban areas; (2) theprovision relating to air ambulance services that continues to treat as rural any area that was designated asrural on December 31, 2006, for purposes of payment under the ambulance fee schedule; and (3) theprovision relating to payment for ground ambulance services that increases the base rate for transportsoriginating in an area that is within the lowest 25 th percentile of all rural areas arrayed by population density(known as the “super rural” bonus). Suppliers of ambulance services affected by these provisions maycontinue billing as usual.Be on the alert for more information about the Job Creation Act and the provisions which take effectlater in the year.HIPAA Version 5010On January 1, <strong>2012</strong>, standards for electronic health care transactions changed from Version 4010/4010A1to Version 5010. These electronic health care transactions include, among others, claims processing,eligibility inquiries, and remittance advice. Unlike the current Version 4010/4010A1, Version 5010accommodates the International Classification of Diseases, 10th Revision, Clinical Modification/ProcedureCoding System (ICD-10-CM/PCS) codes, and must be in place first before the changeover to ICD-10. Thetransition to ICD-10 is dependent on a successful Version 5010 implementation. The Version 5010 changeoccurs well before the ICD-10 implementation date to allow adequate Version 5010 testing andimplementation time. Failure to prepare for these changes may result in rejection of claims or othertransactions and delays in claim reimbursement. Important Dates to Remember:January 1, <strong>2012</strong>- All electronic claims must use Version 5010Keep Up to Date on Version 5010 and ICD-10. Please visit the websites at http://www.cms.gov/icd10 andhttp://www.cms.gov/Versions5010andD0/, for the latest news and sign up for Version 5010 and ICD-10 e-mail updates!HIPAA Version 5010On November 17, 2011, the Centers for <strong>Medicare</strong> & Medicaid Services’ Office of E-Health Standards andServices (OESS) announced that it would not initiate enforcement with respect to any Health InsurancePortability and Accountability Act (HIPAA) covered entity that is not in compliance on January 1, <strong>2012</strong>,with the ASC X12 Version 5010 (Version 5010), National Council for Prescription Drug Programs(NCPDP) Telecom D.0 (NCPDP D.0) and NCPDP Medicaid Subrogation 3.0 (NCPDP 3.0) standards until<strong>March</strong> 31, <strong>2012</strong>. Notwithstanding OESS’ discretionary application of its enforcement authority, thecompliance date for use of these new standards remains January 1, <strong>2012</strong>. (Small health plans have untilJanuary 1, 2013, to comply with NCPDP 3.0.)<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 31
HHS Announces Intent to Delay ICD-10 Compliance DateAs part of President Obama’s commitment to reducing regulatory burden, Health and Human ServicesSecretary Kathleen G. Sebelius announced that HHS will initiate a process to postpone the date by whichcertain health care entities have to comply with International Classification of Diseases, 10th Editiondiagnosis and procedure codes (ICD-10).The final rule adopting ICD-10 as a standard was published in January 2009 and set a compliance date ofOctober 1, 2013 – a delay of two years from the compliance date initially specified in the 2008 proposedrule. HHS will announce a new compliance date moving forward.“ICD-10 codes are important to many positive improvements in our health care system,” said HHSSecretary Kathleen Sebelius. “We have heard from many in the provider community who have concernsabout the administrative burdens they face in the years ahead. We are committing to work with the providercommunity to reexamine the pace at which HHS and the nation implement these important improvements toour health care system.”ICD-10 codes provide more robust and specific data that will help improve patient care and enable theexchange of our health care data with that of the rest of the world that has long been using ICD-10. Entitiescovered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) will be required touse the ICD-10 diagnostic and procedure codes.Vaccinate Early to Protect Against the Flu /2011-<strong>2012</strong> Influenza VaccinePrices Are Now AvailableThe Centers for Disease Control (CDC) recommends a yearly flu vaccination as the most important step inprotecting against flu viruses. Remind your patients that annual vaccination is recommended for optimalprotection. Under <strong>Medicare</strong> <strong>Part</strong> B, <strong>Medicare</strong> pays for the flu vaccine and its administration for seniors andother <strong>Medicare</strong> beneficiaries with no co-pay or deductible. Take advantage of each office visit and startprotecting your patients as soon as your 2011-<strong>2012</strong> seasonal flu vaccine arrives. And don’t forget toimmunize yourself and your staff. Get the Flu Vaccination – Not the Flu.CMS has posted the 2011-<strong>2012</strong> seasonal influenza vaccine payment limits at:http://www.CMS.gov/Mcr<strong>Part</strong>BDrugAvgSalesPrice/10_VaccinesPricing.asp on the CMS website.Influenza vaccine is NOT a <strong>Part</strong> D-covered drug. For information about <strong>Medicare</strong>’s coverage of theinfluenza vaccine, its administration, and educational resources for healthcare professionals and their staff,visit http://www.CMS.gov/MLNProducts/35_PreventiveServices.asp on the CMS website.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 32
Enrolling In the <strong>Medicare</strong> Program Fact SheetsSeveral fact sheets that provide education to specific provider types on how to enroll in the <strong>Medicare</strong>Program and maintain their enrollment information using Internet-based Provider Enrollment, Chain, andOwnership System (PECOS) have been recently updated and are available in downloadable format from the<strong>Medicare</strong> Learning Network® (MLN). Please visithttp://www.CMS.gov/<strong>Medicare</strong>ProviderSupEnroll/downloads/<strong>Medicare</strong>_Provider-Supplier_Enrollment_National_Education_Products.pdf for a complete list of all MLN products related to<strong>Medicare</strong> provider-supplier enrollment.Primary Care Incentive Payment (PCIP) programPer Section 5501(a) of the Affordable Care Act, the Primary Care Incentive Payment (PCIP) programauthorizes an incentive payment of 10% of <strong>Medicare</strong>'s program payments to be paid to qualifying primarycare physicians and non-physician practitioners for services rendered from Sunday, January 1, 2011, toThursday, December 31, 2015. CMS has published 22 Frequently Asked Question (FAQ) items related tothe PCIP program. These new FAQs can be found here. Alternatively, these FAQ items can be found byvisiting http://questions.CMS.hhs.gov/ and searching for “PCIP” or “Primary Care Incentive Payment.”Electronic Funds Transfer (EFT)Existing regulations at 42 CFR 424.510(e)(1)(2) require that at the time of enrollment, enrollment changerequest or revalidation, providers and suppliers that expect to receive payment from <strong>Medicare</strong> for servicesprovided must also agree to receive <strong>Medicare</strong> payments through Electronic Funds Transfer (EFT). Section1104 of the Affordable Care Act further expands Section 1862 (a) of the Social Security Act by mandatingfederal payments to providers and suppliers only by electronic means. As part of <strong>Medicare</strong>’s revalidationefforts, all suppliers and providers who are not currently receiving EFT payments will be identified, andrequired to submit the CMS 588 EFT form with the Provider Enrollment Revalidation application. For moreinformation about provider enrollment revalidation, review the <strong>Medicare</strong> Learning Network’s SpecialEdition Article SE1126 titled, “Further Details on the Revalidation of Provider Enrollment Information” athttp://www.cms.gov/MLNMattersArticles/downloads/SE1126.pdf.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 33
Advanced Diagnostic Imaging (ADI)Remember: Beginning Sunday, January 1, <strong>2012</strong>, suppliers who furnish the Technical Component (TC) ofAdvanced Diagnostic Imaging (ADI) must be accredited to bill <strong>Medicare</strong> for certain services. MRI, CT,nuclear medicine imaging, and positron emission tomography. X-ray, ultrasound, fluoroscopy, and hospitaloutpatient procedures are excluded. For Dates of Service on or after Sunday, January 1, <strong>2012</strong>, <strong>Medicare</strong>Administrative Contractors (MACs) will deny claims for the Technical Component of ADI that aresubmitted under the Physician Fee Schedule by suppliers who have not yet been accredited. For moreinformation, please refer to the Advanced Diagnostic Imaging Accreditation web page and MLN Matters®Special Edition Article #SE1122.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 34
News from CMS For <strong>Part</strong> B ProvidersHealthcare Provider Taxonomy Codes (HPTC) Update April <strong>2012</strong>BackgroundThe Healthcare Provider Taxonomy Code (HPTC) set is maintained by the National Uniform ClaimCommittee (NUCC) for standardized classification of health care providers. The NUCC updates the code settwice a year with changes effective April 1 and October 1. The HPTC list is available for view or fordownload from the Washington Publishing Company (WPC) Web site at www.wpc-edi.com/codes.The changes to the code set include the addition of a new code and addition of definitions to existing codes.When reviewing the Health Care Provider Taxonomy code set online, revisions made since the last releasecan be identified by the color code; new items are green, modified items are orange, and inactive items arered.PolicyHealth Insurance Portability and Accountability Act (HIPAA) requires that covered entities comply with therequirements in the electronic transaction format implementation guides adopted as national standards. Theinstitutional and professional claim electronic standard implementation guides (X12 837-I and 837-P) eachrequire use of valid codes contained in the HPTC set when there is a need to report provider type orphysician, practitioner, or supplier specialty for a claim. Valid HPTCs are those codes approved by theNUCC for current use. Terminated codes are not approved for use after a specific date and newly approvedcodes are not approved for use prior to the effective date of the code set update in which each new code firstappears. Although the NUCC generally posts their updates on the WPC Web page 3 months prior to theeffective date, changes are not effective until April 1 or October 1 as indicated in each update. Specialtyand/or provider type codes issued by any entity other than the NUCC are not valid, and <strong>Medicare</strong> would beguilty of non-compliance with HIPAA if <strong>Medicare</strong> contractors accepted claims that contain invalid HPTCs.Change Request (CR) 7742<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 35
Screening for Sexually Transmitted Infections (STIs) and High IntensityBehavioral Counseling (HIBC) to Prevent STIsProvider Types AffectedThis MLN Matters® article is intended for all physicians, providers, and suppliers submitting claims to<strong>Medicare</strong> contractors (Fiscal Intermediaries (FIs), carriers, and A/B <strong>Medicare</strong> Administrative Contractors(MACs)) for <strong>Medicare</strong> beneficiaries.Provider Action NeededEffective for dates of service on or after November 8, 2011, the Centers for <strong>Medicare</strong> & Medicaid Services(CMS) will cover screening for Sexually Transmitted Infections (STIs) - specifically chlamydia, gonorrhea,syphilis, and hepatitis B - with the appropriate Food and Drug Administration (FDA) approved/clearedlaboratory tests when ordered by the primary care provider. The tests must be used consistent with FDAapproved labeling and in compliance with the Clinical Laboratory Improvement Act (CLIA) regulations andperformed by an eligible <strong>Medicare</strong> provider for these services.In addition, <strong>Medicare</strong> will cover High Intensity Behavioral Counseling (HIBC) to prevent STIs. Ensure thatyour billing staffs are aware of these changes.BackgroundPursuant to Section 1861(ddd) of the Social Security Act, CMS may add coverage of "additional preventiveservices" through the National Coverage Determination (NCD) process. The preventive services must be:1) Reasonable and necessary for the prevention or early detection of illness or disability;2) Recommended with a grade of A or B by the United States Preventive Services Task Force(USPSTF); and3) Appropriate for individuals entitled to benefits under <strong>Part</strong> A or enrolled under <strong>Part</strong> B.CMS reviewed the USPSTF recommendations and supporting evidence for screening for STIs and HIBC toprevent STIs and determined that the criteria listed above were met, enabling CMS to cover these preventiveservices. Therefore, effective November 8, 2011, CMS will cover screening for the indicated STIs andHIBC to prevent STIs. The covered screening lab tests must be ordered by the primary care provider. TheHIBC must be provided by primary care providers in primary care settings such as by the beneficiary’sfamily practice physician, internal medicine physician, or nurse practitioner (NP) in the doctor’s office.A new Healthcare Common Procedure Coding System (HCPCS) code, G0445 (high-intensity behavioralcounseling to prevent sexually transmitted infections, face-to-face, individual, includes: education, skillstraining, and guidance on how to change sexual behavior, performed semi-annually, 30 minutes), has beencreated for use when reporting HIBC to prevent STIs, effective November 8, 2011. This code is included inthe January <strong>2012</strong> <strong>Medicare</strong> Physician Fee Schedule Database (MPFSDB) and Integrated Outpatient CodeEditor (IOCE) updates.This code may be paid on the same date of service as an annual wellness visit (AWV), evaluation andmanagement (E&M) code, or during the global billing period for obstetrical care, but only one G0445 may<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 36
e paid on any one date of service. If billed on the same date of service with an E&M code, the E&M codeshould have a distinct diagnosis code other than the diagnosis code used to indicate high/increased risk forSTIs for the G0445 service. An E&M code should not be billed when the sole reason for the visit isHIBC to prevent STIs.The use of the correct diagnosis code(s) on the claims is imperative to identify these services aspreventive services and to show that the services were provided within the guidelines for coverage aspreventive services. The patient’s medical record must clearly support the diagnosis of high/increasedrisk for STIs and clearly reflect the components of the HIBC service provided – education, skillstraining, and guidance on how to change sexual behavior - as required for coverage.The appropriate screening diagnosis code (ICD-9-CM V74.5 (screening bacterial – sexually transmitted) orV73.89 (screening, disease or disorder, viral, specified type NEC)), when used with the screening lab testsidentified by Change Request (CR) 7610, will indicate that the test is a screening test covered by <strong>Medicare</strong>.Diagnosis code V69.8 (other problems related to life style) is used to indicate that the beneficiary is athigh/increased risk for STIs. Providers should also use V69.8 for sexually active adolescents when billingG0445 counseling services.Diagnosis codes V22.0 (supervision of normal first pregnancy), V22.1 (supervision of other normalpregnancy), or V23.9 (supervision of unspecified high-risk pregnancy) are also to be used when appropriate.For services provided on an annual basis, this is defined as a 12-month period.Further DetailsCMS will cover screening for Chlamydia (86631, 86632, 87110, 87270, 87320, 87490, 87491, 87810,87800 (used for combined Chlamydia and gonorrhea testing), gonorrhea (87590, 87591, 87850, 87800 (usedfor combined Chlamydia and gonorrhea testing), syphilis (86592, 86593, 86780), and hepatitis B (hepatitisB surface antigen) 87340, 87341)) with the appropriate FDA approved/cleared laboratory tests, usedconsistent with FDA-approved labeling and in compliance with the CLIA regulations, when ordered by theprimary care provider, and performed by an eligible <strong>Medicare</strong> provider for these services. As per therequirements, the presence of V74.5 or V73.89 and V69.8, denoting STI screening and high-risk behavior,respectively, and/or V22.0, V22.1, or V23.9, denoting pregnancy as appropriate, must also be present on theclaim for STI services along with one of the procedure codes above.Screening for chlamydia and gonorrhea:Pregnant women who are 24 years old or younger when the diagnosis of pregnancy is known andthen repeat screening during the third trimester if high-risk sexual behavior has occurred since theinitial screening test;Pregnant women who are at increased risk for STIs when the diagnosis of pregnancy is known andthen repeat screening during the third trimester if high-risk sexual behavior has occurred since theinitial screening test; andWomen at increased risk for STIs annually.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 37
Screening for syphilis:Pregnant women when the diagnosis of pregnancy is known and then repeat screening during thethird trimester and at delivery if high-risk sexual behavior has occurred since the previous screeningtest; andMen and women at increased risk for STIs annually.Screening for hepatitis B:Pregnant women at the first prenatal visit when the diagnosis of pregnancy is known and then rescreeningat the time of delivery for those with new or continuing risk factors.Coverage for HIBCCMS will also cover up to two, individual, 20- to 30-minute, face-to-face counseling sessions annually for<strong>Medicare</strong> beneficiaries for HIBC to prevent STIs (G0445) for all sexually active adolescents and for adultsat increased risk for STIs (V69.8), if referred for this service by a primary care provider and provided by a<strong>Medicare</strong> eligible primary care provider in a primary care setting. HIBC is defined as a program intended topromote sexual risk reduction or risk avoidance which includes each of these broad topics, allowingflexibility for appropriate patient-focused elements:Education;Skills training; and,Guidance on how to change sexual behavior.The high/increased risk individual sexual behaviors, based on the USPSTF guidelines, include any of thefollowing:Multiple sex partners;Using barrier protection inconsistently;Having sex under the influence of alcohol or drugs;Having sex in exchange for money or drugs;Age (24 years of age or younger and sexually active for women for chlamydia and gonorrhea);Having an STI within the past year;IV drug use (hepatitis B only); and,In addition, for men – men having sex with men (MSM) and engaged in high-risk sexual behavior,but no regard to age.Community social factors such as high prevalence of STIs in the community populations should also beconsidered in determining high/increased risk for chlamydia, gonorrhea, syphilis, and in recommendingHIBC.High/increased risk sexual behavior for STIs is determined by the primary care provider by assessing thepatient’s sexual history which is part of any complete medical history, typically part of an AWV or prenatalvisit and considered in the development of a comprehensive prevention plan. The medical record should bea reflection of the service provided.For the purposes of this NCD, a primary care setting is defined as the provision of integrated, accessiblehealth care services by clinicians who are accountable for addressing a large majority of personal health care<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 38
needs, developing a sustained partnership with patients, and practicing in the context of family andcommunity. Emergency departments, inpatient hospital settings, ambulatory surgical centers (ASCs),independent diagnostic testing facilities, skilled nursing facilities (SNFs), inpatient rehabilitationfacilities, clinics providing a limited focus of health care services, and hospice are examples of settingsnot considered primary care settings under this definition.For the purposes of this NCD, a “primary care physician” and “primary care practitioner” will be definedconsistent with existing sections of the Social Security Act (Sections 1833(u)(6), 1833(x)(2)(A)(i)(I) and1833(x)(2)(A)(i)(II)), as follows:1833(u) (6) Physician Defined.—For purposes of this paragraph, the term “physician” means aphysician described in Section 1861(r)(1) and the term “primary care physician” means a physicianwho is identified in the available data as a general practitioner, family practice practitioner, generalinternist, or obstetrician or gynecologist.1833(x)(2)(A)(i) (I) is a physician (as described in Section 1861(r)(1)) who has a primary specialtydesignation of family medicine, internal medicine, geriatric medicine, or pediatric medicine; or (II)is a nurse practitioner, clinical nurse specialist, or physician assistant (as those terms are defined inSection 1861(aa)(5)).Billing RemindersInstitutional providers should note that coverage requires services be performed in a primary caresetting. Consequently, if STI services are billed on Types of Bill (TOB) other than 13X, 14X and 85X(when the revenue code on the 85X is not 096X, 097X, or 098X), OR, if G0445 is submitted on a TOBother than 13X, 71X, 77X, or 85X, payment for the services will be denied using the following:o Claim Adjustment Reason Code (CARC) 170 – “Payment is denied when performed/billed by thistype of provider. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110Service Payment Information REF), if present.”o Remittance Advice Remark Code (RARC) N428 – “This service was denied because <strong>Medicare</strong> onlycovers this service in certain settings.”When applying frequency limitations to HIBC services, contractors will allow both a claim for theprofessional service and a claim for the facility fee. Institutional claims may be identified as facility feeclaims for screening services if they contain G0445, and TOB 13X or TOB 85X (when the revenue codeis not 096X, 097X, or 098X). All other claims should be identified as professional service claims forHIBC services (professional claims, and institutional claims with TOB 71X or 77X, or 85X when therevenue code is 096X, 097X, or 098X.Contractors will allow institutional claims, TOBs 71X and 77X, to submit additional revenue lines onclaims with G0445. Also, HCPCS G0445 will not pay separately with another encounter/visit on thesame day for TOBs 71X and 77X with the exception of: initial preventive physical claims, claimscontaining modifier 59, and 77X claims containing diabetes self-management training and medicalnutrition therapy services. If HCPCS G0445 is present on revenue lines along with an encounter/visitwith the same line-item date of service, contractors will assign group code CO and reason code 97 –“The benefit for this service is included in the payment/allowance for another service/procedure that hasalready been adjudicated. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110Services Payment Information REF), if present.”<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 39
G0445 on institutional claims in hospital outpatient departments (TOB 13X) are paid based on OPPS, incritical access hospitals (TOB 85X, not equal to 096X, 097X, or 098X) based on reasonable cost.HCPCS G0445 with revenue codes 096X, 097X, or 098X, when billed on TOB 85X Method II is paidbased on 115 percent of the lesser of the MPFS amount or submitted charge.<strong>Medicare</strong> will enforce the frequency requirement for STI services, as mentioned above. <strong>Medicare</strong> willdeny line items that exceed the coverage frequency requirements using the following:o CARC 119 – “Benefit maximum for this period or occurrence has been reached.”o RARC N362 – “The number of days or units of service exceeds our acceptable maximum.”<strong>Medicare</strong> will deny line items on claims submitted for screening for STIs if the claim lacks theappropriate ICD-9-CM code as mentioned earlier. Such services will be denied payment using:o CARC 50 – “These are non-covered services because this is not deemed a “medical necessity” bythe payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 ServicePayment Information REF), if present.”o ARC N386 – “This decision was based on a National Coverage Determination (NCD), An NCDprovides a coverage determination as to whether a specific item or service is covered. A copy of thispolicy is available at http://www.cms.gov/mcd/search.asp If you do not have web access, you maycontact the contractor to request a copy of the NCD.”The presence of ICD-9 code V74.5 or V73.89 identifies STI laboratory tests as screening lab testspayable under CR7610 rather than as diagnostic tests.Screening for STIs must be ordered by a primary care provider, and HIBC services, G0445, must beperformed by a primary care provider in a primary care setting, with one of the following specialtycodes:o 01 – General Practiceo 08 – Family Practiceo 11 – Internal Medicineo 16 – Obstetrics/Gynecologyo 37 – Pediatric Medicineo 38 – Geriatric Medicineo 42 – Certified Nurse Midwifeo 50 – Nurse Practitionero 89 – Certified Clinical Nurse Specialisto 97 – Physician AssistantSTI screenings ordered by other than the above types of providers will be denied payment whensubmitted on professional claims using:o CARC 184 – “The prescribing/ordering provider is not eligible to prescribe/order the service billed.Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service PaymentInformation REF), if present.”<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 40
<strong>Medicare</strong> will deny line items for G0445 if performed by other than the above types of providers whensubmitted on professional claims using:o CARC 185 – “The rendering provider is not eligible to perform the service billed. Note: Refer to the835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), ifpresent.”o RARC N95 – “This provider type/provider specialty may not bill this service.”Claims for G0445 must be for services performed in the following Places of Service (POS):o 11 – Physician Office;o 22 – Outpatient Hospital;o 49 – Independent Clinic; oro 71 – State or local public health clinic.<strong>Medicare</strong> will deny line items for G0445 if the POS code is other than 11, 22, 49, or 71, using thefollowing:o CARC 58 – “Treatment was deemed by the payer to have been rendered in an inappropriate orinvalid place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110Service Payment Information REF), if present.”o RARC N428 – “Not covered when performed in this Place of Service.”Upon full implementation in <strong>Medicare</strong> systems on July 2, <strong>2012</strong>, providers may submit eligibilityinquiries in order to identify the next eligible date that beneficiaries may receive these services.Until systems are implemented, contractors will hold institutional claims received before July 2, <strong>2012</strong>,with TOBs 13X, 71X, 77X, and 85X reporting HCPCS G0445, or TOBs 13X, 14X, and 85X, when therevenue code is not 096X, 097X, or 098X, for STI services.Effective for dates of service on or after November 8, 2011, contractors will not apply deductible orcoinsurance to claim lines containing HCPCS G0445, HIBC services.Contractors will load HCPCS G0445 to their HCPCS file with an effective date of November 8, 2011.Additional InformationThe official instruction, CR7610, was issued to your FI, carrier and A/B MAC regarding this change via twotransmittals. The first updates the “<strong>Medicare</strong> Claims Processing Manual” and it is athttp://www.cms.gov/Transmittals/downloads/R2402CP.pdf on the CMS website. The second transmittalconveys the NCD and it is at http://www.cms.gov/Transmittals/downloads/R141NCD.pdf on the same site.MLN Matters® MM7610<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 41
Revised and Clarified Place of Service (POS) Coding InstructionsProvider Types AffectedThis article is for physicians, providers, and suppliers billing <strong>Medicare</strong> contractors (carriers and <strong>Medicare</strong>Administrative Contractors (A/B MACs)) for services paid for under the <strong>Medicare</strong> Physician Fee Schedule(MPFS). This article also applies to certain services provided by independent laboratories.What You Need To KnowThis article is based on Change Request (CR) 7631. It revises and clarifies national policy for POS codeassignment. Instructions are provided in CR7631 regarding the assignment of POS for all services paidunder the MPFS and for certain services provided by independent laboratories. In addition to establishing anational policy for the correct assignment of POS codes, instructions are provided for the interpretation orProfessional Component (PC) and the Technical Component (TC) of diagnostic tests. Please make sure yourbilling staff is aware of these changes.BackgroundAs an entity covered under the Health Insurance Portability and Accountability Act of 1996 (HIPAA),<strong>Medicare</strong> must comply with standards and their implementation guides adopted by regulation under thisstatute. The currently adopted professional implementation guide for the ASC X12N 837 standard requiresthat each electronic claim transaction includes a POS code from the POS code set maintained by the Centersfor <strong>Medicare</strong> & Medicaid Services (CMS). Under <strong>Medicare</strong>, the correct POS code assignment is alsorequired on the paper CMS 1500 Claim Form (or its electronic equivalent). While CMS currently maintainsthe National POS code set, it is used by all other public and private health insurers, including Medicaid.At the time a POS code is developed, CMS determines whether a MPFS facility or non-facility payment rateis appropriate for that setting and <strong>Medicare</strong> contractors are required to make payment at the MPFS ratedesignated for each POS code. Under the MPFS, physicians and other suppliers are required to report thesetting, by selecting the most appropriate POS code, in which medically necessary services are furnished tobeneficiaries. While <strong>Medicare</strong> contractors cannot create new POS codes, they are instructed to develop localpolicies that develop or clarify POS setting definitions in situations where national POS policy is lacking orunclear.The importance of this national policy is underscored by consistent findings, in annual and/orbiennial reports from Calendar Year (CY) 2002 through CY 2007, by the Office of the InspectorGeneral (OIG) that physicians and other suppliers frequently incorrectly report the POS in whichthey furnish services. This improper billing is particularly problematic when physician and other suppliersfurnish services in outpatient hospitals and in Ambulatory Surgical Centers (ASCs). In a sample of paidservices (for services possessing both non-facility and facility practice expenses), the OIG found asignificant percent of the sampled physician/practitioner claims were incorrectly reported byphysician/practitioners as occurring in the office POS when those services were furnished in outpatienthospitals or ASCs. As such, these claims were paid by the <strong>Medicare</strong> contractor at the non-facility rate --rather than the lower facility MPFS payment rate assigned to the POS codes for outpatient hospitals andASCs.The OIG has called on CMS to strengthen the education process and reemphasize to physicians (includingnon-physician practitioners and other suppliers) and their billing agents the importance of correctly coding<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 42
the POS. Consequently, CR7631 adds special considerations provisions regarding use of POS codes 22 and24, for outpatient hospitals and ASCs.A previous CMS instruction, Transmittal 1873 (now rescinded) regarding the assignment of POS codes,instructed physicians to use the 2-digit POS code to describe where he/she was physically when renderingthe service; in this instance, the POS code corresponded to the service location. (CMS 1500 Claim FormItems 24B and 32, respectively, and the corresponding loops on the ANSI 12X N 837-P electronic formatinformation). The service location information is used by physicians/practitioners/suppliers to report thename, address and ZIP code of the service location where they furnished services (e.g., hospital, clinic, oroffice) and is used by contractors to determine the applicable “locality” and Geographic Practice Cost Index(GPCI)-adjusted payment for each service paid under the MPFS.CR7631 establishes that for all services – with two (2) exceptions -- paid under the MFPS, that thePOS code to be used by the physician and other supplier will be assigned as the same setting in whichthe beneficiary received the face-to-face service. Because a face-to-face encounter with aphysician/practitioner is required for nearly all services paid under the MPFS and anesthesia services, thisrule will apply to the overwhelming majority of MPFS services. In cases where the face-to-face requirementis obviated such as those when a physician/practitioner provides the PC/interpretation of a diagnostic test,from a distant site, the POS code assigned by the physician /practitioner will be the setting in which thebeneficiary received the TC of the service. For example: A beneficiary receives an MRI at an outpatienthospital near his/her home. The hospital submits a claim that would correspond to the TC portion of theMRI. The physician furnishes the PC portion of the beneficiary’s MRI from his/her office location – POScode 22 will be used on the physician’s claim for the PC to indicate that the beneficiary received the face-tofaceportion of the MRI, the TC, at the outpatient hospital.There are two (2) exceptions to this face-to-face provision/rule in which the physician always uses the POScode where the beneficiary is receiving care as a hospital inpatient or an outpatient of a hospital, regardlessof where the beneficiary encounters the face-to-face service. The correct POS code assignment will be forthat setting in which the beneficiary is receiving inpatient or outpatient care from a hospital, including theinpatient hospital (POS code 21) or the outpatient hospital (POS code 22). "The <strong>Medicare</strong> ClaimsProcessing Manual" already requires this for physician services (and for certain independent laboratoryservices) provided to beneficiaries in the inpatient hospital and CR7631 clarifies this exception and extendsit to beneficiaries of the outpatient hospital, as well.Facility and Non-Facility Payment AssignmentsThe list of settings where a physician’s services are paid at the facility rate include:Inpatient Hospital (POS code 21);Outpatient Hospital (POS code 22);Emergency Room-Hospital (POS code 23);<strong>Medicare</strong>-participating Ambulatory Surgical Center (ASC) for a Healthcare Common ProcedureCoding System (HCPCS) code included on the ASC approved list of procedures (POS code 24);<strong>Medicare</strong>-participating ASC for a procedure not on the ASC list of approved procedures with datesof service on or after January 1, 2008. (POS code 24);Skilled Nursing Facility (SNF) for a <strong>Part</strong> A resident (POS code 31);Hospice – for inpatient care (POS code 34);Ambulance – Land (POS code 41);Ambulance – Air or Water (POS code 42);<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 43
Inpatient Psychiatric Facility (POS code 51);Psychiatric Facility -- <strong>Part</strong>ial Hospitalization (POS code 52);Community Mental Health Center (POS code 53);Psychiatric Residential Treatment Center (POS code 56); andComprehensive Inpatient Rehabilitation Facility (POS code 61).Physicians’ services are paid at non-facility rates for procedures furnished in the following settings:Pharmacy (POS code 01);School (POS code 03);Homeless Shelter (POS code 04);Prison/Correctional Facility (POS code 09);Office (POS code 11);Home or Private Residence of Patient (POS code 12);Assisted Living Facility (POS code 13);Group Home (POS code 14);Mobile Unit (POS code 15);Temporary Lodging (POS code 16);Walk-in Retail Health Clinic (POS code 17);Urgent Care Facility (POS code 20);Birthing Center (POS code 25);Nursing Facility and Skilled Nursing Facilities (SNFs) to <strong>Part</strong> B residents - (POS code 32);Custodial Care Facility (POS code 33);Independent Clinic (POS code 49);Federally Qualified Health Center (POS code 50);Intermediate Health Care Facility/Mentally Retarded (POS code 54);Residential Substance Abuse Treatment Facility (POS code 55);Non-Residential Substance Abuse Treatment Facility (POS code 57);Mass Immunization Center (POS code 60);Comprehensive Outpatient Rehabilitation Facility (POS code 62);End-Stage Renal Disease Treatment Facility (POS code 65);State or Local Health Clinic (POS code 71);Rural Health Clinic (POS code 72);Independent Laboratory (POS code 81); andOther Place of Service (POS code 99).Special Guidance for Selected POS CodesCR7631 adds clarifying or special consideration provisions for other settings as well. Those provisions areas follows:Special Considerations for Mobile Unit Settings (Code 15)When services are furnished in a mobile unit, they are often provided to serve an entity for whichanother POS code exists. For example, a mobile unit may be sent to a physician’s office or a SNF. Ifthe mobile unit is serving an entity for which another POS code already exists, providers should usethe POS code for that entity. However, if the mobile unit is not serving an entity which could bedescribed by an existing POS code, the providers are to use the Mobile Unit POS code 15. <strong>Medicare</strong>will apply the non-facility rate to payments for services designated as being furnished in POS code<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 44
15 and apply the appropriate facility or non-facility rate for the POS code designated when a codeother than the mobile unit code is indicated.A physician or practitioner's office, even if mobile, qualifies to serve as a telehealth originating site.Assuming such an office also fulfills the requirement that it be located in either a rural healthProfessional Shortage Area as defined under Section 332(a)(1)(A) of the Public Health Service Act(42 U.S.C. 254e(a)(1)(A)) or in a county that is not included in a Metropolitan Statistical Area asdefined in Section 1886(d)(2)(D) of the Social Security Act, the originating physician's office shoulduse POS code 11 (Office) in order to ensure appropriate payment for services on the list of <strong>Medicare</strong>Telehealth Services.Special Considerations for Walk-In Retail Health Clinic (Code 17) (Effective no later thanMay 1, 2010)It should be noted that, while some entities in the industry may elect to use code 17 to track thesetting of immunizations, <strong>Medicare</strong> continues to require its billing rules for immunizations claims,which are found in Chapter 18, Section 10 of the "<strong>Medicare</strong> Claims Processing Manual" found athttp://www.cms.gov/manuals/downloads/clm104c18.pdf on the CMS website. Providers andsuppliers of immunizations must continue to follow these <strong>Medicare</strong> billing rules. However, <strong>Medicare</strong>contractors will accept and adjudicate claims containing POS code 17, even if its presence on aclaim is contrary to these billing instructions.Special Considerations for Inpatient Hospital (Code 21)In the case of a physician/practitioner/supplier who provides services to a patient who is an inpatientof a hospital, the inpatient hospital POS code 21 will be used irrespective of the setting where thepatient actually receives the face-to-face encounter.Special Considerations for Outpatient Hospital (Code 22)Physicians/practitioners who furnish services to a hospital outpatient, including in a hospitaloutpatient department (including in a provider-based department of that hospital) or underarrangement to a hospital will use POS code 22.NOTE: Physicians/practitioners who perform services in a hospital outpatient department will usePOS code 22 (Outpatient Hospital) unless the physician maintains separate office space in thehospital or on hospital campus and that physician office space is not considered a provider-baseddepartment of the hospital as defined in 42. C.F.R. 413.65. Physicians will use POS code 11 (office)when services are performed in a separately maintained physician office space in the hospital or onhospital campus and that physician office space is not considered a provider-based department of thehospital as defined in 42.C.F.R. 413.6. Use of POS code 11(office) in the hospital outpatientdepartment or on hospital campus is subject to the physician self-referral provisions set forth in 42C.F.R 411.353 through 411.357.Special Consideration for Ambulatory Surgical Centers (Code 24)When a physician/practitioner furnishes services to a patient in a <strong>Medicare</strong>-participating ASC, thePOS code 24 (ASC) will be used.NOTE: Physicians/practitioners who perform services in a <strong>Medicare</strong>-participating ASC will usePOS code 24 (ASC). Physicians are not to use POS code 11 (office) for ASC based services unlessthe physician has an office at the same physical location of the ASC which meets all otherrequirements for operating as a physician office at the same physical location as the ASC – including<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 45
meeting the “distinct entity” criteria defined in the ASC State Operations Manual that precludes theASC and an adjacent physician office from being open at the same time -- and the physician servicewas actually performed in the office suite portion of the facility. That information is in Appendix Lof that manual which is at http://www.cms.gov/manuals/Downloads/som107ap_l_ambulatory.pdf onthe CMS website.Special Considerations for Hospice (Code 34)When a physician/practitioner furnishes services to a patient under the hospice benefit, use thefollowing guidelines to identify the appropriate POS.When a beneficiary is in an “inpatient” respite or general “inpatient” care stay, the POS code 34(hospice) will be used. When a beneficiary who has elected coverage under the Hospice benefit isreceiving inpatient hospice care in a hospital, SNF, or hospice inpatient facility, POS code 34(Hospice) will be used to designate the POS on the claim.For services provided to a hospice beneficiary in an outpatient setting, such as thephysician/nonphysician practitioner’s office (POS 11); the beneficiary’s home (POS 12), i.e., notoperated by the hospice; or other outpatient setting (e.g., outpatient hospital (POS 22)), the patient’sphysician or nonphysician practitioner or hospice independent attending physician or nursepractitioner, will assign the POS code that represents that setting, as appropriate.There may be use of nursing homes as the hospice patient’s “home,” where the patient resides in thefacility but is receiving a home level of care. In addition, hospices are also operating “houses” orhospice residential entities where hospice patients receive a home level of care. In these cases,physicians and nonphysician practitioners, including the patient’s independent attending physician ornurse practitioner, will use the appropriate POS code representing the particular setting, e.g., POScode 32 for nursing home, POS code 13 for an assisted living facility, or POS code 14 for grouphome.Additional InformationThe official instruction, CR7631 issued to your carrier and/or A/B MAC regarding this change may beviewed at http://www.cms.gov/transmittals/downloads/R2407CP.pdf on the CMS website.MLN Matters® MM7631<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 46
Intensive Behavioral Therapy (IBT) for ObesityProvider Types AffectedThis MLN Matters® article is intended for primary care physicians and other primary care practitionersbilling <strong>Medicare</strong> contractors (carriers, Fiscal Intermediaries (FIs) and A/B <strong>Medicare</strong> AdministrativeContractors (A/B MACs)) for services provided to <strong>Medicare</strong> beneficiaries in a primary care setting.Provider Action NeededThis article is based on Change Request (CR) 7641, which informs <strong>Medicare</strong> contractors aboutimplementing coverage of Intensive Behavioral Therapy (IBT) for obesity.Effective for claims with dates of service November 29, 2011, and later, <strong>Medicare</strong> beneficiaries withobesity, defined as Body Mass Index (BMI) equal to or greater than 30 kg/m2, who are competent and alertat the time that counseling is provided and whose counseling is furnished by a qualified primary carephysician or other primary care practitioner in a primary care setting, are eligible for:One face-to-face visit every week for the first month;One face-to-face visit every other week for months 2-6; andOne face-to-face visit every month for months 7-12, if the beneficiary meets the 3kg (6.6 lbs) weightloss requirement during the first 6 months.<strong>Medicare</strong> coinsurance and <strong>Part</strong> B deductible are waived for this service.See the ‘Background’ and ‘Additional Information’ sections of this article for further details regarding thischange. Be sure your staffs are aware of this new coverage determination and that Healthcare CommonProcedure Coding System (HCPCS) code G0447 (Face-to-Face Behavioral Counseling for Obesity, 15minutes) will be used to bill for these services.This code was effective November 29, 2011, and will appear in the January <strong>2012</strong> quarterly update of the<strong>Medicare</strong> Physician Fee Schedule Database (MPFSDB) and the Integrated Outpatient Code Editor (IOCE).BackgroundBased upon authority in the Social Security Act to cover “additional preventive services” for <strong>Medicare</strong>beneficiaries if certain statutory requirements are met, and the services are reasonable and necessary for theprevention or early detection of illness or disability, the Centers for <strong>Medicare</strong> & Medicaid Services (CMS)initiated a new national coverage analysis on IBT for obesity. Screening for obesity in adults is a "B"recommendation by the U.S. Preventive Services Task Force (USPSTF) and is appropriate for individualsentitled to benefits under <strong>Medicare</strong> <strong>Part</strong> A and <strong>Part</strong> B.In 2003, the USPSTF found good evidence that BMI “is reliable and valid for identifying adults at increasedrisk for mortality and morbidity due to overweight and obesity.” The USPSTF also found fair to goodevidence that high intensity counseling combined with behavioral interventions in obese adults (as definedby a BMI ≥30 kg/m2) “produces modest, sustained weight loss.”Effective for claims with dates of service on or after November 29, 2011, <strong>Medicare</strong> beneficiaries withobesity (BMI ≥30 kg/m2), who are competent and alert at the time that counseling is provided and whose<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 47
counseling is furnished by a qualified primary care physician or other primary care practitioner in a primarycare setting are eligible for:One face-to-face visit every week for the first month;One face-to-face visit every other week for months 2-6; andOne face-to-face visit every month for months 7-12, if the beneficiary meets the 3kg (6.6 lbs) weightloss requirement during the first 6 months as discussed below.At the 6-month visit, a reassessment of obesity and a determination of the amount of weight loss should beperformed. To be eligible for additional face-to-face visits occurring once a month for months 7-12,beneficiaries must have achieved a reduction in weight of at least 3kg (6.6 lbs.), over the course of the first 6months of intensive therapy. This determination must be documented in the physician office records forapplicable beneficiaries consistent with usual practice. For beneficiaries who do not achieve a weightloss of at least 3kg (6.6 lbs.) during the first 6 months of intensive therapy, a reassessment of their readinessto change and BMI is appropriate after an additional 6-month period.IBT for obesity consists of the following:1. Screening for obesity in adults using measurement of BMI calculated by dividing weight inkilograms by the square of height in meters (expressed kg/m2);2. Dietary (nutritional) assessment; and,3. Intensive behavioral counseling and behavioral therapy to promote sustained weight loss throughhigh intensity interventions on diet and exercise.Intensive behavioral intervention for obesity should be consistent with the 5-A framework:1. Assess: Ask about/assess behavioral health risk(s) and factors affecting choice of behavior changegoals/methods.2. Advise: Give clear, specific, and personalized behavior change advice, including information aboutpersonal health harms and benefits.3. Agree: Collaboratively select appropriate treatment goals and methods based on the patient’sinterest in and willingness to change the behavior.4. Assist: Using behavior change techniques (self-help and/or counseling), aid the patient in achievingagreed-upon goals by acquiring the skills, confidence, and social/environmental supports forbehavior change, supplemented with adjunctive medical treatments when appropriate.5. Arrange: Schedule follow-up contacts (in person or by telephone) to provide ongoingassistance/support and to adjust the treatment plan as needed, including referral to more intensive orspecialized treatment.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 48
Billing RequirementsDiagnostic CodesEffective for claims with dates of service on or after November 29, 2011, <strong>Medicare</strong> will recognize HCPCScode G0447, Face-to-Face Behavioral Counseling for Obesity, 15 minutes. G0447 must be billed along with1 of the ICD-9 codes for BMI 30.0 and over (V85.30-V85.39, V85.41-V85.45). The type of service (TOS)for G0447 is 1. (ICD-10 codes will be Z68.30-Z68.39, Z68.41- Z68.45)Effective for claims with dates of service on or after November 29, 2011, <strong>Medicare</strong> contractors will denyclaims for HCPCS G0447 that are not submitted with the appropriate diagnostic code (V85.30-V85.39,V85.41-V85.45).Claims submitted with HCPCS G0447 that are not submitted with these diagnosis codes will be denied withthe following messages:Claim Adjustment Reason Code (CARC) 167 – "This (these) diagnosis(es) is (are) not covered.Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service PaymentInformation REF), if present."Remittance Advice Remark Code (RARC) N386 – "This decision was based on a National CoverageDetermination (NCD). An NCD provides a coverage determination as to whether a particular item orservice is covered. A copy of this policy is available at www.cms.gov/mcd/search.asp. If you do nothave web access, you may contact the contractor to request a copy of the NCD."Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if aclaim is received with a GA modifier indicating a signed ABN is on file).Group Code CO (Contractual Obligation) assigning financial liability to the provider (if a claim isreceived with a GZ modifier indicating no signed ABN is on file).Note: Per MLN Matters® article MM7228, when modifier GZ is used, contractors will use CARC 50(These services are non-covered services because this is not deemed a “medical necessity” by the payer.).This is true with all denials noted below that have the Group Code CO. MM7228 may be found athttp://www.cms.gov/MLNMattersArticles/downloads/MM7228.pdf on the CMS website.Specialty CodesEffective for services on or after November 29, 2011, <strong>Medicare</strong> will pay claims for G0447, only whenservices are submitted by the following provider specialty types found on the provider’s <strong>Medicare</strong>enrollment record:01 - General Practice08 - Family Practice11 - Internal Medicine16 - Obstetrics/Gynecology37 - Pediatric Medicine38 - Geriatric Medicine50 - Nurse Practitioner89 - Certified Clinical Nurse Specialist97 - Physician Assistant<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 49
If your specialty type is not one of the above, your claim will be denied using the following codes:CARC of 185 – "The rendering provider is not eligible to perform the service billed. NOTE: Refer tothe 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), ifpresent.),"RARC N95 - "This provider type/provider specialty may not bill this service."Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if aclaim is received with a GA modifier indicating a signed ABN is on file), andGroup Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim isreceived with a GZ modifier indicating no signed ABN is on file).Place of Service (POS) CodesEffective for services on or after November 29, 2011, <strong>Medicare</strong> will pay for obesity counseling claimscontaining HCPCS G0447 only when services are provided with the following POS codes:11 - Physician’s Office22 - Outpatient Hospital49 - Independent Clinic71 - State or local public health clinic.Line items on claims for G0447 will be denied if not performed in these POSs using the following codes:CARC 58 – "Treatment was deemed by the payer to have been rendered in an inappropriate orinvalid POS. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 ServicePayment Information REF), if present."RARC N428 - "Not covered when performed in this place of service."Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if aclaim is received with a GA modifier indicating a signed ABN is on file)andGroup Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim isreceived with a GZ modifier indicating no signed ABN is on file).Frequency LimitationEffective July 2, <strong>2012</strong>, for claims processed with dates of service on or after November 29, 2011, <strong>Medicare</strong>will pay for G0447 with an ICD-9 code of V85.30-V85.39, V85.41-V85.45, no more than 22 times in a 12-month period. Line items on claims beyond the 22 limit will be denied using the following codes: (Note:When applying this frequency limitation, a claim for the professional service and a claim for a facilityfee will be allowed.)CARC 119 – "Benefit maximum for this time period or occurrence has been reached."RARC N362 - "The number of days or units of service exceeds our acceptable maximum."<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 50
Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if aclaim is received with a GA modifier indicating a signed ABN is on file), andGroup Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim isreceived with a GZ modifier indicating no signed ABN is on file).Note: Your contractor will not search their files for claims that may have been paid in error. However,contractors may adjust claims that are brought to their attention.Institutional Claims NotesClaims submitted with either a Type of Bill (TOB) 13X or TOB 85X (where the revenue code is not 096X,097X, or 098X) will be identified as facility fee service claims.Claims submitted with TOBs 71X, 77X, or 85X (where the revenue code is 096X, 097X, or 098X) will beidentified as professional service claims.<strong>Medicare</strong> will pay for G0447 on institutional claims in hospital outpatient departments TOB 13X based onOPPS and in Critical Access Hospitals TOB 85X based on reasonable cost.The CAH Method II payment is for G0447 with revenue codes 096X, 097X, or 098X is based on 115% ofthe lesser of the fee schedule amount or submitted charge. Deductible and coinsurance do not apply.<strong>Medicare</strong> will line-item deny any claim submitted with G0447 when the TOB is not 13X, 71X, 77X, or 85Xwith the following:CARC 5 - "The procedure code/bill type is inconsistent with the Place of Service. Note: Refer to the835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), ifpresent."RARC M77 - "Missing/incomplete/invalid place of service."Group Code PR (Patient Responsibility), assigning financial responsibility to the beneficiary (if aclaim is received with a GA modifier indicating a signed ABN is on file) andGroup Code CO (Contractual Obligation), assigning financial liability to the provider (if a claim isreceived with a GZ modifier indicating no signed ABN is on file).Note: <strong>Medicare</strong> will hold institutional claims received before July 2, <strong>2012</strong>, with TOBs 13X, 71X, 77X, and85X reporting G0447.Rural Health Clinics and Federally Qualified Health Centers Claims NotesRural Health Clinics, using TOB 71X, and Federally Qualified Health Centers, using TOB 77X, mustsubmit HCPCS code G0447 on a separate service line to ensure coinsurance and deductible are not applicedto this service. Such claims will be paid based on the all-inclusive payment rate.For RHC and FQHC services that contain HCPCS code G0447 with another encounter/visit with the sameline item DOS, the service line with HCPCS G0447 will be denied with the following messages:<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 51
Claim Adjustment Reason Code (CARC) 97 – "The benefit for this service is included in thepayment/allowance for another service/procedure that has already been adjudicated. Note: Refer tothe 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF) ifpresent" andGroup Code CO (Contractual Obligation)Note: Obesity counseling is not separately payable with another encounter/visit on the same day. This doesnot apply for Initial Preventive Physical Examination (IPPE) claims, claims containing modifier 59, and77X claims containing Diabetes Self-Management Training and Medical Nutrition Therapy services.Additional InformationThe official instruction, CR7641, issued to your FI, carrier, and A/B MAC regarding this change, was issuedin 2 transmittals at http://www.cms.gov/transmittals/downloads/R2409CP.pdf andhttp://www.cms.gov/transmittals/downloads/R142NCD.pdf on the CMS website.MLN Matters® MM7641<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 52
Advanced Diagnostic Imaging (ADI) Accreditation Enrollment Procedures.(Change Request (CR) 7681 Fully Rescinds and Replaces CR 7177)- RevisedNote: This article was revised on February 10, <strong>2012</strong>, to reflect the revised CR7681 issued on February 9,<strong>2012</strong>. In the article, the CR release date, transmittal number, and the Web address for accessing CR7681were revised. All other information is the same.Provider Types AffectedPhysicians, providers, and suppliers submitting claims to <strong>Medicare</strong> contractors (carriers and/or A/B<strong>Medicare</strong> Administrative Contractors (A/B MACs)) for Advanced Diagnostic Imaging (ADI) servicesprovided to <strong>Medicare</strong> beneficiaries.Provider Action NeededThis article is based on Change Request (CR) 7681 which fully rescinds and replaces CR7177.CR7177 established that ADI providers/suppliers would need to provide their ADI accreditation informationby completing an Internet-based Provider Enrollment, Chain, and Ownership System (PECOS) applicationor a CMS-855 application.. CR7681 changes this requirement and allows for the accrediting organizationsto provide the listing of who is accredited through a weekly file. Since this change, providers/suppliers nolonger need to complete the ADI information in Internet-based PECOS or on a CMS-855 form(s).See the ‘Background’ and ‘Additional Information’ sections of this article for further details regarding thesechanges.BackgroundThe <strong>Medicare</strong> Improvements for Patients and Providers Act of 2008 (MIPPA - Section 135(a); seehttp://www.gpo.gov/fdsys/pkg/PLAW-110publ275/pdf/PLAW-110publ275.pdf on the Internet) amendedthe Social Security Act (Section 1834(e); see http://www.ssa.gov/OP_Home/ssact/title18/1834.htm on theInternet) and required the Secretary of the U.S. Department of Health and Human Services (HHS) todesignate organizations to accredit suppliers, including but not limited to physicians, non-physicianpractitioners, and Independent Diagnostic Testing Facilities, that furnish the Technical Component (TC) ofADI services.MIPPA specifically defines Advanced Diagnostic Imaging (ADI) procedures as including diagnosticMagnetic Resonance Imaging (MRI), Computed Tomography (CT), and Nuclear Medicine Imaging (NMI)such as Positron Emission Tomography (PET). The law also authorizes the HHS Secretary to specify otherdiagnostic imaging services in consultation with physician specialty organizations and other stakeholders.In order to furnish the TC of advanced diagnostic imaging services for <strong>Medicare</strong> beneficiaries,providers/suppliers must be accredited by January 1, <strong>2012</strong>.The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) implemented (effective January 1, <strong>2012</strong>) therequirement that ADI providers and/or suppliers must be accredited for ADI services specific to eachmodality for which they will submit claims. Originally, CMS required the providers/suppliers to providetheir accreditation information on their respective CMS-855 form, or through the internet-based PECOS.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 53
Change Request (CR) 7681 establishes a new process that allows for ADI providers and/or suppliers tobypass ADI information collection on the appropriate CMS 855 form or in the internet-based PECOS webapplication. CR7681 instructs that <strong>Medicare</strong> contractors will:Not require documentation from the ADI provider/supplier for proof of their accreditation; andNot require providers/suppliers to complete the ADI section in the internet-based PECOS applicationnor in the appropriate CMS-855 form.Instead, <strong>Medicare</strong> and its contractors will receive this information directly from the accreditingorganizations.Additional InformationThe official instruction, CR7681, issued to your carriers and A/B MACs regarding this change may beviewed at http://www.cms.gov/Transmittals/downloads/R407PI.pdf on the CMS website.MLN Matters® MM7681<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 54
Immediate Recoupment for Fee for Service Claims OverpaymentsNote: This article was revised on February 10, <strong>2012</strong>, to reflect the revised CR7688 issued on February 9,<strong>2012</strong>. In the article, the CR release date, transmittal number, and the Web address for accessing CR7688were revised. All other information is the same.Provider Types AffectedThis MLN Matters® article is intended for all <strong>Part</strong> A, and all <strong>Part</strong> B Providers, Physicians, and Supplierswho bill <strong>Medicare</strong> contractors (carriers, Fiscal Intermediaries (FIs), Regional Home Health Intermediaries(RHHIs), <strong>Medicare</strong> Administrative Contractors (A/B MACs) Durable Medical Equipment (DME MACs),)for services to <strong>Medicare</strong> beneficiaries.Provider Action NeededChange Request (CR) 7688 is policy that implements a standard “immediate recoupment” process that givesproviders the option to avoid interest from accruing on claims overpayments when the debt is recouped infull prior to or by the 30th day from the initial demand letter date. See the ‘Key Points’ section of this articlefor specifics.BackgroundCurrently, <strong>Medicare</strong> contractors begin recoupment of an overpayment on Day 41 from the date of the initialdemand letter. Interest accrues and assesses on an overpayment if not paid in full by day 30.Key PointsThe “immediate recoupment” process implemented in CR7688 allows providers to request that recoupmentbegin prior to day 41. Providers who elect this option may avoid paying interest if the overpayment isrecouped in full prior to day 31.Key to understanding this change is that providers who request an immediate recoupment must realize it isconsidered a voluntary repayment1. Providers who choose immediate recoupment must do so in writing to the contractors. . Also, notethe following:2. The request may be for:a one-time request for a specific demanded overpayment (the total amount of the demandedoverpayment); ora permanent request for the specific demanded overpayment and all future overpayments.3. The request may be submitted via regular mail, facsimile, or e-mail and the request must include theProvider’s name, contact phone number, <strong>Medicare</strong> number and/or National Provider Identifier (NPI),Provider or Chief Financial Officer's signature, demand letter number and what option the provideris requesting.4. By choosing immediate recoupment, providers must understand that they are waiving their rights tointerest under Section 935 of the <strong>Medicare</strong> Modernization Act (MMA) should the overpayment bereversed at the Administration Law Judge level (ALJ) or subsequent higher levels.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 55
5. Providers can terminate the immediate recoupment process at anytime. The request to terminatemust be in writing.Providers should note that <strong>Medicare</strong> contractors will not consider any recoupment after QualifiedIndependent Contractor (QIC) proceedings (30 days after a QIC decision) as voluntary payments. <strong>Medicare</strong>contractors will follow the rules proscribed by Section 935 of the MMA for all recoupment activity after aQIC decision. These rules are explained in Chapter 3, Section 200 of the “<strong>Medicare</strong> Financial ManagementManual” that is available at http://www.cms.gov/manuals/downloads/fin106c03.pdf on the Centers for<strong>Medicare</strong> & Medicaid Services (CMS) website.You may further review all of the specifics of this change along with the applicable manual section changesby reading the official instruction for CR7688 issued to your <strong>Medicare</strong> contractor. The web address forCR7688 is listed in the ‘Additional Information’ section of this article.Additional InformationThe official instruction, CR7688, issued to your <strong>Medicare</strong> contractor regarding this change may be viewedat http://www.cms.gov/Transmittals/downloads/R205FM.pdf on the Centers for <strong>Medicare</strong> & MedicaidServices (CMS) website.MLN Matters® MM7688<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 56
New Waived TestsProvider Types AffectedThis MLN Matters® Article is intended for clinical laboratories and providers who submit claims to<strong>Medicare</strong> contractors (carriers and <strong>Medicare</strong> Administrative Contractors (MACs)) for laboratory testservices provided to <strong>Medicare</strong> beneficiaries are affected.Provider Action NeededThere are eleven newly waived tests under the Clinical Laboratory Improvement Amendments of 1988(CLIA).Change Request (CR) 7694 from which this article is taken announces that (effective April 2, <strong>2012</strong>,) theFood and Drug Administration (FDA) has approved new waived tests under CLIA.The codes for these tests are in a table in the ‘Background’ section.You should ensure that your billing staffs are aware of these new waived tests.BackgroundClinical Laboratory Improvement Amendments of 1988 (CLIA) regulations require a facility to beappropriately certified for each test that it performs. To ensure that <strong>Medicare</strong> and Medicaid only pay forlaboratory tests categorized as waived complexity under CLIA in facilities with a CLIA certificate ofwaiver, laboratory claims are currently edited at the CLIA certificate level.CR7694, from which this article is taken, announces the latest 11 tests approved by the FDA as waived testsunder CLIA (effective April 2, <strong>2012</strong>). The Current Procedural Terminology (CPT) codes for the followingnew tests must have the modifier QW, defined as CLIA waived test, to be recognized as a waived test.However, the tests displayed at the beginning of the following table (i.e., CPT codes: 81002, 81025, 82270,82272, 82962, 83026, 84830, 85013, and 85651) do not require a QW modifier to be recognized as a waivedtest.TESTS GRANTED WAIVED STATUS UNDER CLIACPT Code Effective Date Description82274QWSeptember 8, 2004 Hemosure One-Step Fecal Occult Blood TestG0328QW81003QW October 28, 2009 Acon Mission U120 Urine AnalyzerG0434QW May 5, 2011 Premier Integrity Solutions P/Tox Drug ScreenCup {OTC}81003QW June 2, 2011 BTNX Rapid Response U120 Urine AnalyzerG0434QW July 7, 2011 Instant Technologies, Inc. iCassette DX DrugScreen TestG0434QW July 19, 2011 Express Diagnostic Int’l Inc DrugCheck WaiveRT (Model 9308z)80061QW, 82465QW,82947QW, 82950QW,82951QW, 82952QW,August 16, 2011 Alere Cholestech LDX {Whole Blood}<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 57
83718QW, 84450QW,84460QW, 84478QW82055QW September 13, 2011 Acon Laboratories Inc. Mission Saliva AlcoholTest StripG0434QW September 13, 2011 Amedica Biotech Instant Test Cup81003QW September 26, 2011 Immunostics Inc., Detector Uristrip+ Analyzer82055QW October 4, 2011 Teco Diagnostics Saliva Alcohol Test86386QW January 1, <strong>2012</strong> Alere NMP22 BladderChek Test (PrescriptionHome Use)86386QW January 1, <strong>2012</strong> Alere NMP22 BladderChek Test (ProfessionalUse)For <strong>2012</strong>, the new CPT code 86386 was developed for the Nuclear Matrix Protein 22 (NMP22), qualitativetest. Therefore, the CPT code assigned to the Matritech, Inc. NMP22® BladderCheck Test forProfessional and Prescription Home Use is changed to 86386QW with an effective date of January 1, <strong>2012</strong>.Please note that your carrier or A/B MAC will not search their files to either retract payment or retroactivelypay claims; however, should adjust claims you bring to their attention.Additional InformationThe official instruction, CR7694, issued to your carrier and A/B MAC regarding this change may be viewedhttp://www.cms.gov/transmittals/downloads/R2408CP.pdf on the Centers for <strong>Medicare</strong> & MedicaidServices (CMS) website.MLN Matters® MM7694<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 58
Interaction of the Multiple Procedure Payment Reduction (MPPR) onImaging Procedures and the Outpatient Prospective Payment System(OPPS) Cap on the Technical Component (TC) of Imaging ProceduresProvider Types AffectedPhysicians, providers, and suppliers submitting professional claims to <strong>Medicare</strong> contractors (carriers and/orA/B <strong>Medicare</strong> Administrative Contractors (A/B MACs)) for providing diagnostic imaging services to<strong>Medicare</strong> beneficiaries.Provider Action NeededThis article is based on Change Request (CR) 7703 which announces that, effective January 1, <strong>2012</strong>, theCenters for <strong>Medicare</strong> & Medicaid Services (CMS) is discontinuing the use of the “global cap” amount incalculating global payments of certain diagnostic imaging procedures. <strong>Medicare</strong> implemented the MultipleProcedure Payment Reduction (MPPR) rule on the TC of certain diagnostic imaging procedures effectiveJanuary 1, 2006, and CR7703 is a reminder that effective January 1, <strong>2012</strong>, the MPPR will also be applied tothe Professional Component (PC) of such services.The MPPR rule applies to PC-only services, to TC-only services, and to PC and TC portions of globalservices. Full payment is made for the PC service with the highest payment under the <strong>Medicare</strong> PhysicianFee Schedule (MPFS). Payment is made at 75 percent for subsequent PC services furnished by the samephysician to the same patient in the same session on the same day. Full payment is made for the TC servicewith the highest payment under the MPFS. Payment is made at 50 percent for subsequent TC servicesfurnished by the same physician to the same patient in the same session on the same day. The individual PCand TC services with the highest payments under the MPFS of globally billed services must be determinedin order to calculate the reduction.See the ‘Background’ and ‘Additional Information’ sections of this article for further details regarding thesechanges.BackgroundThe Deficit Reduction Act of 2005 (Section 5102(b); seehttp://www.govtrack.us/congress/billtext.xpd?bill=s109-1932 on the Internet) provided for capping thepayment for the TC of certain diagnostic imaging procedures based on the Outpatient Prospective PaymentSystem (OPPS) payment.The MPPR rule on diagnostic imaging applies when multiple services are furnished by the same physicianto the same patient in the same session on the same day, and it is applied prior to the application of theOPPS cap. <strong>Medicare</strong> implemented the MPPR on the TC of certain diagnostic imaging procedures effectiveJanuary 1, 2006, and effective January 1, <strong>2012</strong>, the MPPR is also applied to the PC of such services.Currently, global services are compared against a “global cap” derived from adding the TC capped amountto the PC. However, with the implementation of the MPPR on the PC, this could result in a situation where,although the global payment amount is lower than the “global cap” amount, the TC is higher than the TCcap amount and is not appropriately being reduced. Therefore, CR7703 announces that CMS isdiscontinuing calculation and use of the “global cap” amount.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 59
The TC of global services, and TC-only services, will be compared to the OPPS cap amount on the TC todetermine the lower of the two.Full payment is made for the PC service with the highest payment under the MPFS. Payment is made at 75percent for subsequent PC services furnished by the same physician to the same patient in the same sessionon the same day. Full payment is made for the TC service with the highest payment under the MPFS.Payment is made at 50 percent for subsequent TC services furnished by the same physician to the samepatient in the same session on the same day. The individual PC and TC services with the highest paymentsunder the MPFS of globally billed services must be determined in order to calculate the reduction.Additional InformationThe official instruction, CR7703, issued to your carriers and A/B MACs, regarding this change, may beviewed at http://www.cms.gov/transmittals/downloads/R1040OTN.pdf on the CMS website.MLN Matters® MM7703<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 60
Quarterly Update to Correct Coding Initiative (CCI) Edits, Version 18.1,Effective April 1, <strong>2012</strong>Provider Types AffectedThis article is for physicians submitting claims to <strong>Medicare</strong> Carriers and/or A/B <strong>Medicare</strong> AdministrativeContractors (A/B MACs) for services provided to <strong>Medicare</strong> beneficiaries.Provider Action NeededThis article is based on Change Request (CR) 7726 which provides a reminder for physicians to take note ofthe quarterly updates to Correct Coding Initiative (CCI) edits. The last quarterly release of the edit modulewas issued in January, <strong>2012</strong>.BackgroundThe Centers for <strong>Medicare</strong> & Medicaid Services (CMS) developed the National Correct Coding Initiative(CCI) to promote national correct coding methodologies and to control improper coding that leads toinappropriate payment in <strong>Part</strong> B claims.The coding policies developed are based on coding conventions defined in the:American Medical Association’s (AMA’s) Current Procedural Terminology (CPT) Manual;National and local policies and edits;Coding guidelines developed by national societies;Analysis of standard medical and surgical practice; and byReview of current coding practice.The latest package of CCI edits, Version 18.1, is effective April 1, <strong>2012</strong>, and includes all previous versionsand updates from January 1, 1996, to the present. It will be organized in two tables:Column I/Column 2 Correct Coding Edits, andMutually Exclusive Code (MEC) Edits.Additional information about the CCI, including the current CCI and Mutually Exclusive Code (MEC) edits,is available at http://www.cms.gov/NationalCorrectCodInitEd on the CMS website.Additional InformationThe CCI and MEC file formats are defined in the “<strong>Medicare</strong> Claims Processing Manual,” (Chapter 23,Section 20.9) which is available at http://www.cms.gov/manuals/downloads/clm104c23.pdf on the CMSwebsite.The official instruction, CR7726, issued to your carrier or and A/B MAC regarding this change may beviewed at http://www.cms.gov/Transmittals/downloads/R2384CP.pdf on the CMS website.MLN Matters® MM7726<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 61
April <strong>2012</strong> Quarterly Average Sales Price (ASP) <strong>Medicare</strong> <strong>Part</strong> B DrugPricing Files and Revisions to Prior Quarterly Pricing FilesProvider Types AffectedPhysicians, providers, and suppliers submitting claims to <strong>Medicare</strong> contractors (carriers, FiscalIntermediaries (FIs), A/B <strong>Medicare</strong> Administrative Contractors (A/B MACs), Durable Medical Equipment<strong>Medicare</strong> Administrative Contractors (DME MACs), and/or Regional Home Health Intermediaries(RHHIs)) for services provided to <strong>Medicare</strong> beneficiaries.Provider Action Needed<strong>Medicare</strong> will use the April <strong>2012</strong> quarterly Average Sales Price (ASP) <strong>Medicare</strong> <strong>Part</strong> B drug pricing files todetermine the payment limit for claims for separately payable <strong>Medicare</strong> <strong>Part</strong> B drugs processed orreprocessed on or after April 2, <strong>2012</strong>, with dates of service April 1, <strong>2012</strong>, through June 30, <strong>2012</strong>.Change Request (CR) 7734, from which this article is taken, instructs your <strong>Medicare</strong> contractors todownload and implement the April <strong>2012</strong> Average Sales Price (ASP) <strong>Medicare</strong> <strong>Part</strong> B drug pricing file for<strong>Medicare</strong> <strong>Part</strong> B drugs and, if released by the Centers for <strong>Medicare</strong> & Medicaid Services (CMS), to alsodownload and implement the revised January <strong>2012</strong>, October 2011, July 2011, and April 2011 files.You should make sure that your billing staffs are aware of the release of these April <strong>2012</strong> ASP <strong>Medicare</strong><strong>Part</strong> B drug files.BackgroundThe <strong>Medicare</strong> Modernization Act of 2003 (MMA; Section 303(c); (seehttp://www.cms.gov/MMAUpdate/downloads/PL108-173summary.pdf on the Centers for <strong>Medicare</strong> &Medicaid Services (CMS) website) revised the payment methodology for <strong>Part</strong> B covered drugs andbiologicals that are not priced on a cost or prospective payment basis.The Average Sales Price (ASP) methodology is based on quarterly data submitted to CMS bymanufacturers. CMS will supply <strong>Medicare</strong> contractors with the ASP and Not Otherwise Classified (NOC)drug pricing files for <strong>Medicare</strong> <strong>Part</strong> B drugs on a quarterly basis. Payment allowance limits under the OPPSare incorporated into the Outpatient Code Editor (OCE) through separate instructions that can be located inthe "<strong>Medicare</strong> Claims Processing Manual" (Chapter 4 (<strong>Part</strong> B Hospital (Including Inpatient Hospital <strong>Part</strong> Band OPPS)), Section 50 (Outpatient PRICER); see http://www.cms.gov/manuals/downloads/clm104c04.pdfon the CMS website.)The following table shows how the quarterly payment files will be applied:FilesEffective for Dates of ServiceApril <strong>2012</strong> ASP and ASP NOC April 1, <strong>2012</strong>, through June 30, <strong>2012</strong>January <strong>2012</strong> ASP and ASP NOC January 1, <strong>2012</strong>, through <strong>March</strong> 31, <strong>2012</strong>October 2011 ASP and ASP NOC October 1, 2011, through December 31, 2011July 2011 ASP and ASP NOC July 1, 2011, through September 30, 2011April 2011 ASP and ASP NOC files April 1, 2011, through June 30, 2011<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 62
Additional InformationYou can find the official instruction, Change Request (CR) 7344, issued to your FI, carrier, A/B MAC,RHHI, or DME MAC by visiting http://www.cms.gov/Transmittals/downloads/R2396CP.pdf on the CMSwebsite.MLN Matters® MM7734<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 63
Emergency Update to the CY <strong>2012</strong> <strong>Medicare</strong> Physician Fee ScheduleDatabase (MPFSDB)Provider Types AffectedPhysicians, non-physician practitioners, and providers who bill <strong>Medicare</strong> contractors (Fiscal Intermediaries(FIs), Regional Home Health Intermediaries (RHHIs), carriers or A/B <strong>Medicare</strong> Administrative Contractors(A/B MACs)) for services provided to <strong>Medicare</strong> beneficiaries are affected.What You Need To KnowThis article is based on Change Request (CR) 7737, which informs you that new <strong>Medicare</strong> Physician FeeSchedule (MPFS) payment files have been created and are available to <strong>Medicare</strong> contractors.Payment files were issued to <strong>Medicare</strong> contractors based upon the CY <strong>2012</strong> <strong>Medicare</strong> Physician FeeSchedule (MPFS) Final Rule, issued on November 1, 2011, and published in the “Federal Register”on November 28, 2011.CR7737 amends those payment files to include corrections described in the CY <strong>2012</strong> MPFS FinalRule Correction Notice, as well as relevant statutory changes applicable January 1, <strong>2012</strong>.Background<strong>Medicare</strong> Physician Fee Schedule Revisions and UpdatesSome physician work, practice expense, and malpractice Relative Value Units (RVUs) published in the CY<strong>2012</strong> MPFS Final Rule have been revised to align their values with the CY <strong>2012</strong> MPFS Final Rule policies.These changes are discussed in the CY <strong>2012</strong> MPFS Final Rule Correction Notice and revised RVU valuesare found in Addendum B and Addendum C of the CY <strong>2012</strong> MPFS Final Rule Correction Notice.In addition to RVU revisions, changes have been made to some HCPCS code payment indicators in order toreflect the appropriate payment policy. Procedure status indicator changes will also be reflected inAddendum B and Addendum C of the CY <strong>2012</strong> MPFS Final Rule Correction Notice.Other payment indicator changes will be included, along with the RVU and procedure status indicatorchanges, in the CY <strong>2012</strong> MPFS Final Rule Correction Notice public use data files, which are located at:http://www.cms.gov/PhysicianFeeSched/PFSRVF/list.asp#TopOfPage on the CMS website.Changes to the physician work RVUs and payment indicators can be found in the attachment associatedwith CR7737, which is cited in the Additional Information section below. Changes to practice expenseRVUs are reflected in Addendum B and Addendum C of the CY <strong>2012</strong> MPFS Final Rule Correction Notice.Legislative changes subsequent to issuance of the CY <strong>2012</strong> MPFS Final Rule, specifically, theTemporary Payroll Tax Cut Continuation Act of 2011 (TPTCCA), have led to the further revision ofthe values published in the CY <strong>2012</strong> MPFS Final Rule Correction Notice, including a change to theconversion factor. This new law prevents a scheduled payment cut for physicians and other practitionerswho treat <strong>Medicare</strong> patients from taking effect immediately. While the negative update for the <strong>2012</strong> MPFSis now scheduled to take effect on <strong>March</strong> 1, <strong>2012</strong>, the Administration remains strongly opposed to lettingthis cut take effect. The Centers for <strong>Medicare</strong> & Medicaid Services (CMS) will work quickly to updateMPFS payment rates in the event Congress passes legislation to prevent the negative update from going intoeffect. Please be on the alert for more information about the <strong>2012</strong> physician update as it becomes available.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 64
Temporary Payroll Tax Cut Continuation Act of 2011On December 23, 2011, President Obama signed into law the Temporary Payroll Tax Cut Continuation Actof 2011 (TPTCCA). This law contains a number of <strong>Medicare</strong> provisions, which extend current <strong>Medicare</strong>fee-for-service program policies, and, as previously mentioned, prevents a scheduled payment cut forphysicians and other practitioners who treat <strong>Medicare</strong> patients from taking effect immediately. A summaryof the TPTCCA provisions relevant to the MPFS payment files are provided below.<strong>Medicare</strong> Physician Payment UpdateSection 301 of the TPTCCA prevents a payment cut for physicians that would have taken effect on January1, <strong>2012</strong>. An update of zero percent is effective for claims with dates of service January 1, <strong>2012</strong>,through February 29, <strong>2012</strong>. While the physician fee schedule update will be zero percent, other changes tothe relative value units used to calculate the fee schedule rates must be budget neutral. To make thosechanges budget neutral, the conversion factor must be adjusted for <strong>2012</strong>. Therefore, the conversion factorwill not be unchanged in CY <strong>2012</strong> from CY 2011. The revised conversion factor to be used for physicianpayment as of January 1, <strong>2012</strong>, is $34.0376. The calculation of the CY <strong>2012</strong> conversion factor is illustratedin the following table.December 2011Conversion FactorTPTCCA of 2011“Zero PercentUpdate”CY <strong>2012</strong> RVUBudget NeutralityAdjustment$33.9764 0.0 percent (1.000) 0.2 percent (1.0018) $34.0376CY <strong>2012</strong> ConversionFactor thru 2/29/12The revised CY <strong>2012</strong> MPFS payment files will reflect this conversion factor through February 29, <strong>2012</strong>.Extension of <strong>Medicare</strong> Physician Work Geographic Adjustment FloorCurrent law requires payment rates under the MPFS to be adjusted geographically to reflect area differencesin the cost of practice. The following three components of the MPFS payment are adjusted: physician work,practice expense (PE), and malpractice expense. Section 303 of the TPTCCA extends the existing 1.0floor on the physician work geographic practice cost index through February 29, <strong>2012</strong>. This change isincluded in the revised CY <strong>2012</strong> MPFS payment files. Updated CY <strong>2012</strong> geographic practice cost indices(GPCI) are included in the attachment to CR7737. See the “Additional Information” section below forinformation on accessing CR7737.Extension of MPFS Mental Health Add-OnFor calendar year 2011, certain mental health services' payment rates continued to be increased by fivepercent over what they would otherwise be paid using the standard MPFS payment methodology. Section307 of the TPTCCA extends the five percent increase in payments for these mental health servicesthrough February 29, <strong>2012</strong>. This five percent increase is reflected in the revised CY <strong>2012</strong> MPFS paymentfiles. The lists of Psychiatry Current Procedural Terminology (CPT) codes that represent the specifiedservices subject to this payment policy are included in the attachment to CR7737.Extension of Exceptions Process for <strong>Medicare</strong> Therapy CapsSection 304 of the TPTCCA extends the exceptions process for outpatient therapy caps. Outpatienttherapy service providers may continue to submit claims with the KX modifier (Specific requireddocumentation on file), when an exception is appropriate, for services furnished on or after January 1, <strong>2012</strong>,through February 29, <strong>2012</strong>.<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 65
The therapy caps are determined on a calendar year basis, so all patients begin a new cap year on January 1,<strong>2012</strong>. For physical therapy and speech language pathology services combined, the limit on incurredexpenses is $1,880. For occupational therapy services, the limit is $1,880. Deductible and coinsuranceamounts applied to therapy services count toward the amount accrued before a cap is reached and also applyfor services above the cap where the KX modifier is used.Extension of Payment for the Technical Component (TC) of Certain Physician Pathology ServicesIn the CY 2000 PFS Final Rule, published in the “Federal Register” on November 2, 1999, CMS finalized apolicy to pay only the hospital for the TC of physician pathology services furnished to hospital patients.Under prior policy, independent laboratories continued to be paid for the TC of a pathology serviceprovided to a hospital patient. At the request of the industry, to allow those independent laboratories thatwere separately paid for the TC of a physician pathology service provided to a hospital patient sufficienttime to negotiate new arrangements with hospitals, the implementation of this rule was administrativelydelayed until 2001. Subsequent legislation formalized a moratorium on the implementation of the rule.Although the most recent extension of the moratorium expired at the end of 2011, section 305 of theTPTCCA restores the moratorium through February 29, <strong>2012</strong>. Therefore, those independentlaboratories that are eligible may continue to submit claims to <strong>Medicare</strong> for the TC of physician pathologyservices furnished to patients of a hospital, regardless of the beneficiary's hospitalization status (inpatient oroutpatient) on the date that the service was furnished. This policy is effective for claims with dates ofservice on or after January 1, <strong>2012</strong>, through February 29, <strong>2012</strong>.Extension of the Minimum Payment for Bone Mass MeasurementSection 3111(a) of the Affordable Care Act changed the payment calculation for dual-energy x-rayabsorptiometry (DXA) services described CPT codes 77080 (Dual-energy X-ray absorptiometry (DXA),bone density study, 1 or more sites; axial skeleton (e.g., hips, pelvis, spine)) and 77082 (Dual-energy X-rayabsorptiometry (DXA), bone density study, 1 or more sites; vertebral fracture assessment) for CYs 2010 and2011. This provision required payment for these services at 70 percent of the product of the CY 2006 RVUsfor these DXA codes, the CY 2006 conversion factor (CF), and the geographic adjustment for the relevantpayment year. CMS provided for payment in CYs 2010 and 2011 under the Physician Fee Schedule (PFS)for CPT codes 77080 and 77082 at the specified rates. Because this provision did not include CY <strong>2012</strong>, theCY <strong>2012</strong> PFS final rule with comment period listed resource-based, rather than imputed, RVUs for CPTcodes 77080 and 77082. However, Section 309 of the TPTCCA extended the Affordable Care Actminimum payment for bone mass measurement for the first two months of CY <strong>2012</strong>. For claims withdates of service on or after January 1, <strong>2012</strong>, through February 29, <strong>2012</strong>, CPT codes 77080 and 77082will be paid at 70 percent of the product of the CY 2006 RVUs, the CY 2006 CF, and the geographicadjustment for the CY <strong>2012</strong>. The revised CY <strong>2012</strong> work, PE, and malpractice RVUs for CPT codes 77080and 77082 are shown below.CPTCodeMod WorkRVURVUs for DXA CPT Codes 77080 and 77082,January 1, <strong>2012</strong> through February 29, <strong>2012</strong>Fully Transitional FullyImplemented Non- ImplementedNon-Facility Facility PE Facility PEPE RVU RVU RVUTransitionalFacility PERVU77080 0.23 2.50 2.50 N/A N/A 0.1477080 TC 0.00 2.42 2.42 N/A N/A 0.1377080 26 0.23 0.08 0.08 0.08 0.08 0.0177082 0.13 0.63 0.63 N/A N/A 0.05MalpracticeRVU<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 66
77082 TC 0.00 0.58 0.58 N/A N/A 0.0477082 26 0.13 0.05 0.05 0.05 0.05 0.01Additional InformationThe official instruction, CR 7737, issued to your FI, RHHI, carrier and A/B MAC regarding this change,may be viewed at http://www.cms.gov/Transmittals/downloads/R1015OTN.pdf on the CMS website.MLN Matters® MM7737<strong>Medicare</strong> B <strong>Newsline</strong> <strong>March</strong> <strong>2012</strong> 67
<strong>Medicare</strong> B <strong>Newsline</strong> Quality SurveyPlease take a moment to let us know your thoughts regarding this issue of the <strong>Medicare</strong> B <strong>Newsline</strong>.Your Name (optional):Telephone Number (optional):1. Usefulness of the information.Please rate the publication by circling the number of your choice.(10 = Excellent, 5 = Satisfactory, 1 = Unacceptable)1 2 3 4 5 6 7 8 9 102. Organization and layout of the information.1 2 3 4 5 6 7 8 9 103. Design and physical appearance of the publication.1 2 3 4 5 6 7 8 9 104. Value of <strong>Medicare</strong> A <strong>Newsline</strong> as a reference item.1 2 3 4 5 6 7 8 9 105. Do you use the website to obtain copies of the <strong>Medicare</strong> newsletter?YesNo6. What can we do to make <strong>Medicare</strong> B <strong>Newsline</strong> a more effective publication?Thank you for your time. You can email your response by clicking SUBMIT.Fax or mail your response to:<strong>Cahaba</strong> Government Benefit Administrators, LLCProvider Outreach and EducationPO Box 12967Birmingham, Alabama 35202Fax: 205 220-1531<strong>Medicare</strong> B <strong>Newsline</strong>