BP - Health Care Compliance Association
BP - Health Care Compliance Association
BP - Health Care Compliance Association
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
RAC demonstrations and inpatient rehabilitation – Vision of things to come? ...continued from page 21<br />
The impact on inpatient rehabilitation<br />
The RAC demonstration project resulted in the<br />
identification of approximately $1.03 billion in<br />
improper payments (actual figures vary slightly,<br />
based on source). Of that amount, $59.7 million<br />
or 6% of the total was identified from inpatient<br />
rehabilitation providers. (These figures represent<br />
the dollar amounts without adjustment for<br />
successful appeal processes.) The efforts focusing<br />
on inpatient rehabilitation providers did not take<br />
place in all three RAC demonstration states, but<br />
only in California. The most recent evaluation<br />
of the demonstration project reports: “The RAC<br />
demonstration had a limited financial impact<br />
on most providers,” however this was clearly not<br />
the case for the inpatient rehabilitation providers<br />
in California. Moreover, even an informal<br />
extrapolation to all of the 50 states will provide<br />
the reader with the potential impact of these<br />
denials on a larger scale.<br />
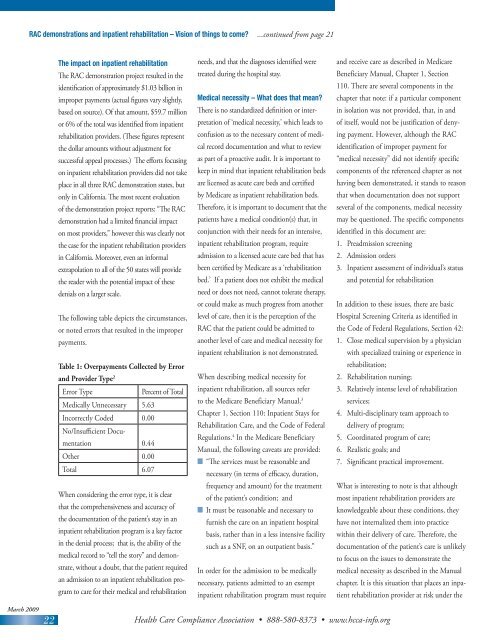
The following table depicts the circumstances,<br />
or noted errors that resulted in the improper<br />
payments.<br />
Table 1: Overpayments Collected by Error<br />
and Provider Type 2<br />
Error Type<br />
Percent of Total<br />
Medically Unnecessary 5.63<br />
Incorrectly Coded 0.00<br />
No/Insufficient Documentation<br />
0.44<br />
Other 0.00<br />
Total 6.07<br />
When considering the error type, it is clear<br />
that the comprehensiveness and accuracy of<br />
the documentation of the patient’s stay in an<br />
inpatient rehabilitation program is a key factor<br />
in the denial process; that is, the ability of the<br />
medical record to “tell the story” and demonstrate,<br />
without a doubt, that the patient required<br />
an admission to an inpatient rehabilitation program<br />
to care for their medical and rehabilitation<br />
needs, and that the diagnoses identified were<br />
treated during the hospital stay.<br />
Medical necessity – What does that mean?<br />
There is no standardized definition or interpretation<br />
of ‘medical necessity,’ which leads to<br />
confusion as to the necessary content of medical<br />
record documentation and what to review<br />
as part of a proactive audit. It is important to<br />
keep in mind that inpatient rehabilitation beds<br />
are licensed as acute care beds and certified<br />
by Medicare as inpatient rehabilitation beds.<br />
Therefore, it is important to document that the<br />
patients have a medical condition(s) that, in<br />
conjunction with their needs for an intensive,<br />
inpatient rehabilitation program, require<br />
admission to a licensed acute care bed that has<br />
been certified by Medicare as a ‘rehabilitation<br />
bed.’ If a patient does not exhibit the medical<br />
need or does not need, cannot tolerate therapy,<br />
or could make as much progress from another<br />
level of care, then it is the perception of the<br />
RAC that the patient could be admitted to<br />
another level of care and medical necessity for<br />
inpatient rehabilitation is not demonstrated.<br />
When describing medical necessity for<br />
inpatient rehabilitation, all sources refer<br />
to the Medicare Beneficiary Manual, 3<br />
Chapter 1, Section 110: Inpatient Stays for<br />
Rehabilitation <strong>Care</strong>, and the Code of Federal<br />
Regulations. 4 In the Medicare Beneficiary<br />
Manual, the following caveats are provided:<br />
n “The services must be reasonable and<br />
necessary (in terms of efficacy, duration,<br />
frequency and amount) for the treatment<br />
of the patient’s condition; and<br />
n It must be reasonable and necessary to<br />
furnish the care on an inpatient hospital<br />
basis, rather than in a less intensive facility<br />
such as a SNF, on an outpatient basis.”<br />
In order for the admission to be medically<br />
necessary, patients admitted to an exempt<br />
inpatient rehabilitation program must require<br />
and receive care as described in Medicare<br />
Beneficiary Manual, Chapter 1, Section<br />
110. There are several components in the<br />
chapter that note: if a particular component<br />
in isolation was not provided, that, in and<br />
of itself, would not be justification of denying<br />
payment. However, although the RAC<br />
identification of improper payment for<br />
“medical necessity” did not identify specific<br />
components of the referenced chapter as not<br />
having been demonstrated, it stands to reason<br />
that when documentation does not support<br />
several of the components, medical necessity<br />
may be questioned. The specific components<br />
identified in this document are:<br />
1. Preadmission screening<br />
2. Admission orders<br />
3. Inpatient assessment of individual’s status<br />
and potential for rehabilitation<br />
In addition to these issues, there are basic<br />
Hospital Screening Criteria as identified in<br />
the Code of Federal Regulations, Section 42:<br />
1. Close medical supervision by a physician<br />
with specialized training or experience in<br />
rehabilitation;<br />
2. Rehabilitation nursing;<br />
3. Relatively intense level of rehabilitation<br />
services;<br />
4. Multi-disciplinary team approach to<br />
delivery of program;<br />
5. Coordinated program of care;<br />
6. Realistic goals; and<br />
7. Significant practical improvement.<br />
What is interesting to note is that although<br />
most inpatient rehabilitation providers are<br />
knowledgeable about these conditions, they<br />
have not internalized them into practice<br />
within their delivery of care. Therefore, the<br />
documentation of the patient’s care is unlikely<br />
to focus on the issues to demonstrate the<br />
medical necessity as described in the Manual<br />
chapter. It is this situation that places an inpatient<br />
rehabilitation provider at risk under the<br />
March 2009<br />
22<br />
<strong>Health</strong> <strong>Care</strong> <strong>Compliance</strong> <strong>Association</strong> • 888-580-8373 • www.hcca-info.org