Physical Examination
Physical Examination
Physical Examination
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
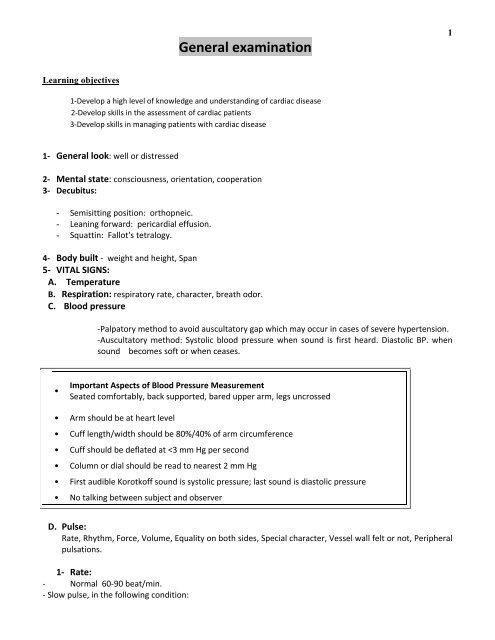
General examination<br />
1<br />
Learning objectives<br />
1‐Develop a high level of knowledge and understanding of cardiac disease<br />
2‐Develop skills in the assessment of cardiac patients<br />
3‐Develop skills in managing patients with cardiac disease<br />
1‐ General look: well or distressed<br />
2‐ Mental state: consciousness, orientation, cooperation<br />
3‐ Decubitus:<br />
- Semisitting position: orthopneic.<br />
- Leaning forward: pericardial effusion.<br />
- Squattin: Fallot's tetralogy.<br />
4‐ Body built ‐ weight and height, Span<br />
5‐ VITAL SIGNS:<br />
A. Temperature<br />
B. Respiration: respiratory rate, character, breath odor.<br />
C. Blood pressure<br />
‐Palpatory method to avoid auscultatory gap which may occur in cases of severe hypertension.<br />
‐Auscultatory method: Systolic blood pressure when sound is first heard. Diastolic BP. when<br />
sound becomes soft or when ceases.<br />
Important Aspects of Blood Pressure Measurement<br />
•<br />
Seated comfortably, back supported, bared upper arm, legs uncrossed<br />
• Arm should be at heart level<br />
• Cuff length/width should be 80%/40% of arm circumference<br />
• Cuff should be deflated at
• Sinus bradycardia.<br />
• Nodal rhythm.<br />
• Heart block.<br />
Rapid pulse.<br />
• Sinus tachycardia.<br />
• Atrial tachycardia.<br />
• Atrial flutter.<br />
2<br />
2‐Rhythm:<br />
- Regular irregularity: it is regular pulse (can feel 4 regular beats) with occasional premature beats.<br />
- Irregular irregularity, pulse i.e completely irregular as in Atrial Fibrillation and multiple ventricular<br />
premature contraction. To differentiate → Exercise<br />
• A.F becomes worse.<br />
• Premature contractions disappear.<br />
Regular tachycardia<br />
• Sinus tachycardia.<br />
• Paroxysmal tachycardia.<br />
• Artrial flutter.<br />
Irregular tachycardia<br />
• Atrial fibrillation.<br />
• Atrial flutter with variable block.<br />
• Multiple premature beats.<br />
Regular Bradycardia<br />
• Sinus bradycardia.<br />
• Nodal rhythm.<br />
• 2:1 heart block.<br />
• Complete heart block.<br />
Irregular Bradycardia<br />
• Slow AF.<br />
3‐ Force of the pulse: related to systolic blood pressure, assessed by the pressure needed to obliterate the<br />
radial pulse.<br />
4‐ Volume: related to pulse pressure, assessed by the degree of expansion of the radial artery at the arrival<br />
of each pulse wave.<br />
5‐Vessel wall: Palpate the radial artery against bone normally not felt, but it is felt in the medial sclerosis<br />
(Monckeberg sclerosis).<br />
6‐ Character of the pulse<br />
Normal pulse tracing<br />
P= percussion wave (left ventricular injection early in systole).<br />
T= tidal wave (reflection from periphery late in systole).<br />
D= dicrotic wave = diminished blood pressure by aortic valve closure.<br />
N= Anacrotic notch.
3<br />
Abnormal Characters of arterial pulse:<br />
1‐ Water hammer pulse: Occurs in aortic regurgitation, there is an abrupt upstroke then rapid descent.<br />
You elevate the arm of the patient to assist the collapsing pulse (pulse pressure > 60 mmHg).<br />
2‐ Bounding pulse: Pulse pressure 40‐60 mmHg (increased volume and rapid rise), occurs in hyperkinetic<br />
states.<br />
3‐ Plateau pulse: occurs in aortic stenosis, slow rise, maintenance, Slow descend.<br />
4‐ Anacrotic pulse: Slow upstroke, anacrotic wave on the upstroke. Small volume as in aortic stenosis.<br />
5‐ Pulses tardus et parvus: fixed obstruction of the left ventricular outflow tract, as in aortic stenosis.<br />
6‐ Pulses bisferiens: double headed pulse in aortic stenosis + aortic regurge , Hpertrophic obstructive<br />
cardiomyopathy + aortic regurge, Subaortic membrane + aortic regurge.<br />
7‐ Dicrotic pulse: exaggerated dicrotic wave in fever.<br />
8‐ Pulsus alternans: Regular pulse with alternating strong and weak beats , it occurs in heart failure.<br />
9‐ Pulsus paradoxus: Pulse becomes smaller with deep inspiration, the systolic BP decrease by >10 mmHg<br />
during deep inspiration. Causes:<br />
- Constrictive pericarditis.<br />
- Pericardial effusion.<br />
- Bronchial asthma.<br />
7‐Equality on both sides as regard force and volume, not rate.<br />
Causes of unequality:<br />
1‐ Thrombosis.<br />
2‐ Embolism.<br />
3‐ Compression by tumour.<br />
4‐ Cervical rib: irritation of the sympathetic nerves leading to vasoconstriction (not compression).<br />
6. SKIN, MUCOUS MEMBRANE, and APPENDAGES:<br />
A. SKIN:<br />
I. COLOR
• Pallor:<br />
o Pheumatic activity.<br />
o Infective endocarditis.<br />
o Low cardiac output.<br />
o Shock.<br />
o Anaemia.<br />
• Cyanosis: Cyanosis in heart disease (reduced Hb >5g/dl to be clinically overt).<br />
Central cyanosis: detected in lips and tongue occurs in :<br />
o Congenital cyanotic heart disease.<br />
o Acute pulmonary edema.<br />
o Pulmonary arteriovenous fistula.<br />
o Hypoxic cor‐pulmonale.<br />
Peripheral cyanosis detected only in the hands and feet:<br />
o Heart failure.<br />
• Jaundice.<br />
4<br />
II. TEXTURE<br />
III. ERUPTION<br />
B.MUCOUS MEMBRANE:<br />
Conjunctiva, mouth and tongue<br />
Comment on color, signs of vitamin deficiency.<br />
C. HAIR:<br />
- Somatic<br />
- Sexual<br />
- Comment on presence, thickness, luster<br />
D. NAILS:<br />
Clubbing, dystrophies, brittleness, color, spooning, spider angiomata and Capillary pulsation.<br />
CLUBBING:<br />
Due to proliferation of the soft tissue at the nail bed, occurs in:<br />
- Congenital cyanotic heart disease.<br />
- Infective endocarditis.<br />
- Hypoxic cor pulmonale.<br />
- Unilateral clubbing in thoracic inlet syndrome and Aortic aneurysm.<br />
Normally angle of nail is 160‐165 degree (obtuse angle), clubbing has four grades:<br />
- First degree → Obliteration of the angle at the nail bed.<br />
- Second degree → increased convexity longitudinally and side by side.<br />
- Third degree → drum stick appearance due to thickening and increase diameter of terminal phalanx.<br />
- Fourth degree → pulmonary osteoarthropathy where there is thickening of the synovial membrane of<br />
the hands and feet.<br />
7. SUBCUTANEOUS TISSUE:<br />
Masses, Nodules, and Oedema
SYSTEMATIC EXAMINATION:<br />
5<br />
Head <strong>Examination</strong>:<br />
Size and Shape<br />
Face: Expression and Symmetry<br />
Eyes: Lids, Eye balls, Conjunctiva , Sclera (color), Cornea, Pupils, Lens, Eye brow and eye lashes.<br />
Nose: Nasal bridge, Discharge<br />
Ears: Setting, Discharge<br />
Cheeks: Malar flush as in mitral stenosis.<br />
Mouth: Lips, Teeth, Gums, Tongue, Tonsils<br />
NECK:<br />
NECK VEINS:<br />
The jugular venous pressure is perhaps the single most important hemodynamic measurement to ascertain<br />
volume status at the bedside. The external (EJV) or internal (IJV) jugular veins may be used, although the IJV is<br />
preferred because the EJV is valved and not directly in line with the superior vena cava (SVC) and right atrium<br />
(RA). The EJV is easier to visualize when distended, and its appearance has been used to discriminate between<br />
a low and high central venous pressure.<br />
Distinguishing the Jugular Venous Pulse from the Carotid Pulse<br />
Feature Internal Jugular Vein Carotid Artery<br />
Appearance of pulse Undulating two troughs and two peaks for every cardiac<br />
cycle (biphasic)<br />
Single brisk upstroke<br />
(monophasic)<br />
Response to<br />
inspiration<br />
Height of column falls and troughs become more<br />
prominent<br />
No respiratory change to<br />
contour<br />
Palpability Generally not palpable (except in severe TR) Palpable<br />
Effect of Pressure<br />
Can be obliterated with gentle pressure at base of<br />
vein/clavicle<br />
Cannot be obliterated<br />
The venous pressure Jugular venous pressure should be initially estimated with the patient lying with upper<br />
trunk elevated at 30 0 . In this position, at normal jugular venous pressure, no pulsations are visible. This<br />
correlates roughly to a jugular venous pressure less than 6‐10 cm. When the jugular venous pulsations are<br />
visible, the venous pressure is measured as the vertical distance between the top of the venous pulsations<br />
and the sternal angle (angle of Louis).
6<br />
The Jugular venous pulse waves:<br />
Normal Jugular venous pulse waves, they reflect changes in the right atrial pressure:<br />
- "a" wave →rise in the right atrial pressure secondary to atrial systole.<br />
- "X" wave → drop in the right atrial pressure secondary to atrial relaxation<br />
- "c" wave → coincide with the onset of ventricular systole. It results from movement of tricuspid valve<br />
ring in to the right atrium causing a rise in the right atrial pressure.<br />
- “X I ” wave: drop in the pressure secondary to downward displacement of the AV ring during ventricular<br />
contraction.<br />
- "V" wave → caused by rise in pressure which occurs when the right atrium fills with blood during<br />
ventricular systole with the tricuspid valve is closed.<br />
- "Y" wave or descent → drop in the pressure secondary to opening of the tricuspid valve, and blood<br />
flowing from the right atrium to the right ventricle in the rapid filling phase.
7<br />
The abdominojugular reflux:<br />
is performed using firm and consistent pressure over the upper abdomen, preferably the right upper<br />
quadrant, for at least 10 seconds. A sustained rise of >3 cm in the venous pressure for at least 15 seconds<br />
after resumption of spontaneous respiration is a positive response. The abdominojugular reflex is useful in<br />
predicting right sided heart failure .<br />
Comment:<br />
• Congestion, filling of the veins above normal.<br />
• Level of congestion is vertical distance between two horizontal planes (one from the Lewis angle<br />
and the other from the upper level of congestion).<br />
• Normal venous pressure is 5‐9 cm H 2 O.<br />
• Venous pressure = level of congestion + 5 cm (distance between Lewis angle and the Rt. Atrium).
8<br />
JVP abnormalities<br />
Probable cause<br />
Large "a" wave<br />
Cannon wave<br />
Steep "x", "y" descent<br />
Large "v" wave<br />
Tricuspid stenosis, pulmonary hypertension, pulmonary stenosis<br />
Complete heart block, VVI pacing, ventricular tachycardia (a cannon wave occurs when<br />
the right atrium contracts against a closed tricuspid valve)<br />
Constrictive pericarditis, cardiac tamponade<br />
Tricuspid regurgitation<br />
Pulsations:<br />
Pulsating or not. Non‐pulsating neck veins means obstruction of the central veins (SVC obstruction).<br />
Abnormalities of the jugular venous pressure (JVP)<br />
Relation of neck veins to respirations:<br />
Normal: there is inspiratory emptying of neck veins due to increased negative thoracic pressure.<br />
Kussmaul's sign: Inspiratory filling occurs in constrictive pericarditis.