Guidelines for the Early Clinical and Public Health Management of ...
Guidelines for the Early Clinical and Public Health Management of ...
Guidelines for the Early Clinical and Public Health Management of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
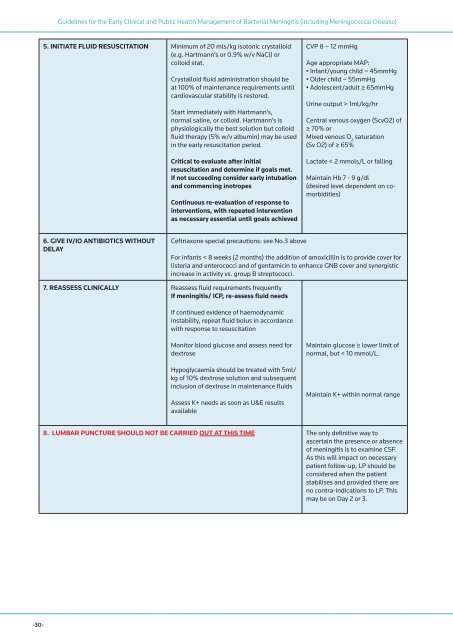
<strong>Guidelines</strong> <strong>for</strong> <strong>the</strong> <strong>Early</strong> <strong>Clinical</strong> <strong>and</strong> <strong>Public</strong> <strong>Health</strong> <strong>Management</strong> <strong>of</strong> Bacterial Meningitis (including Meningococcal Disease)<br />
5. INITIATE FLUID RESUSCITATION Minimum <strong>of</strong> 20 mls/kg isotonic crystalloid<br />
(e.g. Hartmann’s or 0.9% w/v NaCl) or<br />
colloid stat.<br />
Crystalloid fluid administration should be<br />
at 100% <strong>of</strong> maintenance requirements until<br />
cardiovascular stability is restored.<br />
Start immediately with Hartmann’s,<br />
normal saline, or colloid. Hartmann’s is<br />
physiologically <strong>the</strong> best solution but colloid<br />
fluid <strong>the</strong>rapy (5% w/v albumin) may be used<br />
in <strong>the</strong> early resuscitation period.<br />
Critical to evaluate after initial<br />
resuscitation <strong>and</strong> determine if goals met.<br />
If not succeeding consider early intubation<br />
<strong>and</strong> commencing inotropes<br />
Continuous re-evaluation <strong>of</strong> response to<br />
interventions, with repeated intervention<br />
as necessary essential until goals achieved<br />
CVP 8 – 12 mmHg<br />
Age appropriate MAP:<br />
• Infant/young child ~ 45mmHg<br />
• Older child ~ 55mmHg<br />
• Adolescent/adult ≥ 65mmHg<br />
Urine output > 1ml/kg/hr<br />
Central venous oxygen (ScvO2) <strong>of</strong><br />
≥ 70% or<br />
Mixed venous O 2<br />
saturation<br />
(Sv O2) <strong>of</strong> ≥ 65%<br />
Lactate < 2 mmols/L or falling<br />
Maintain Hb 7 - 9 g/dl<br />
(desired level dependent on comorbidities)<br />
6. GIVE IV/IO ANTIBIOTICS WITHOUT<br />
DELAY<br />
Ceftriaxone special precautions: see No.3 above<br />
For infants < 8 weeks (2 months) <strong>the</strong> addition <strong>of</strong> amoxicillin is to provide cover <strong>for</strong><br />
listeria <strong>and</strong> enterococci <strong>and</strong> <strong>of</strong> gentamicin to enhance GNB cover <strong>and</strong> synergistic<br />
increase in activity vs. group B streptococci.<br />
7. REASSESS CLINICALLY Reassess fluid requirements frequently<br />
If meningitis/ ICP, re-assess fluid needs<br />
If continued evidence <strong>of</strong> haemodynamic<br />
instability, repeat fluid bolus in accordance<br />
with response to resuscitation<br />
Monitor blood glucose <strong>and</strong> assess need <strong>for</strong><br />
dextrose<br />
Hypoglycaemia should be treated with 5ml/<br />
kg <strong>of</strong> 10% dextrose solution <strong>and</strong> subsequent<br />
inclusion <strong>of</strong> dextrose in maintenance fluids<br />
Assess K+ needs as soon as U&E results<br />
available<br />
Maintain glucose ≥ lower limit <strong>of</strong><br />
normal, but < 10 mmol/L.<br />
Maintain K+ within normal range<br />
8. LUMBAR PUNCTURE SHOULD NOT BE CARRIED OUT AT THIS TIME The only definitive way to<br />
ascertain <strong>the</strong> presence or absence<br />
<strong>of</strong> meningitis is to examine CSF.<br />
As this will impact on necessary<br />
patient follow-up, LP should be<br />
considered when <strong>the</strong> patient<br />
stabilises <strong>and</strong> provided <strong>the</strong>re are<br />
no contra-indications to LP. This<br />
may be on Day 2 or 3.<br />
-30-