Arizona Rural Health Clinic Designation Manual - Arizona Center for ...
Arizona Rural Health Clinic Designation Manual - Arizona Center for ...
Arizona Rural Health Clinic Designation Manual - Arizona Center for ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Arizona</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
<strong>Designation</strong> <strong>Manual</strong><br />
August 2008<br />
Version 3<br />
This publication is made possible with partial funding from:<br />
U.S. Department of <strong>Health</strong> and Human Services<br />
<strong>Health</strong> Resources and Services Administration<br />
Offi ce of <strong>Rural</strong> Healh Policy<br />
<strong>Rural</strong> Hospital Flexibility Program
Table of Contents<br />
Introduction.............……………....…………………………..............…….………3<br />
I. An Introduction to <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s............................................................4<br />
A. Background In<strong>for</strong>mation ……......….………………...…….............4<br />
B. <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s in <strong>Arizona</strong>......................................................... 7<br />
C. Number of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s in the United States.........................9<br />
D. Frequently Asked Questions………… .....……….….......................10<br />
E. Steps to Becoming a Certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>….......................14<br />
II. Licensing and Certification Requirements.......................................................16<br />
A. State Licensing…....…………………….…..........…………….......16<br />
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong>..………..........…...……....17<br />
C. See Addendum:Regulatory Guide: RHC/FQHC Proposed Rule...…28<br />
D. Preparing <strong>for</strong> the Certification Inspection…..……….......…............29<br />
E. 30 Most Common RHC Survey/Certification Deficiencies...............36<br />
F. RHC Cost Report...............................................................................39<br />
G. Important Resources.........................................................................44<br />
III. Appendices.......................................................................................................46<br />
A. Important Contact In<strong>for</strong>mation…...........................…………..….....46<br />
B. Definitions <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> <strong>Designation</strong>................……..….49<br />
C. Federal Primary Care HPSAs in <strong>Arizona</strong>…..........……...........….....51<br />
D. Federal MUAs in <strong>Arizona</strong>….……………………………................54<br />
E. Licensing Forms….………………….……………………..............56<br />
F. Certification Forms………………………..……………...........…....69<br />
G. <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Survey Report…..............……………..............82<br />
Cover photo taken by Alison Hughes.
Community Environment & Policy<br />
1295 Martin Avenue<br />
Phone (520) 626-3589 PO Box 245210<br />
FAX (520) 626-8009 Tucson, <strong>Arizona</strong> 85724<br />
<strong>Rural</strong> <strong>Health</strong> Office<br />
Introduction<br />
This is the third version of the <strong>Arizona</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> <strong>Designation</strong> <strong>Manual</strong>. Since the first<br />
manual was published in 2004, ten new rural health clinics received the designation in <strong>Arizona</strong> and<br />
others have designations pending. Hopefully the popularity of the designation can be attributed<br />
to some extent on the resource value of this document, as it was distributed to all eligible clinics<br />
shortly after its first publication.<br />
The contents of this document will help rural clinics assess whether or not the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
(RHC) designation is fiscally advantageous. It also provides a step-by-step guide to the application<br />
process <strong>for</strong> the designation. The document is made possible with funding support from the <strong>Arizona</strong><br />
<strong>Rural</strong> Hospital Flexibility (Flex) Grant Program located in the <strong>Rural</strong> <strong>Health</strong> Office.<br />
<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s have proliferated throughout the country since 1977 when Congress passed<br />
the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Act. The purpose of the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s program is to encourage and<br />
stabilize the provision of out-patient primary care in underserved rural areas through the use of<br />
physicians, nurse practitioners, physician assistants and certified nurse midwives.<br />
According to the National Association of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, there are currently over 3,000<br />
designated RHC’s in 47 states serving over seven million people. The small number of RHCs in<br />
<strong>Arizona</strong> was in part the result of lack of in<strong>for</strong>mation about the designation’s existence, but also in<br />
part because of the excellent work accomplished by the <strong>Arizona</strong> Association of Community <strong>Health</strong><br />
<strong>Center</strong>s to develop a strong network of CHCs in the state. To find out more about the difference<br />
between a CHC and an RHC, please refer to the <strong>Arizona</strong> <strong>Rural</strong> <strong>Health</strong> Resource <strong>Manual</strong> published<br />
by the <strong>Arizona</strong> <strong>Rural</strong> <strong>Health</strong> Office: http://www.rho.arizona.edu/Resources/resource_manual.<br />
aspx<br />
I wish to acknowledge the work of Leila Barraza, MPH, in preparing the original document. She<br />
has dedicated many hours and commitment to its preparation that it might contribute, in some<br />
small way, to improving the health of people who live in rural and remote areas of <strong>Arizona</strong>.<br />
Alison Hughes, MPA<br />
Director, Flex Program<br />
<strong>Rural</strong> <strong>Health</strong> Office<br />
Mel and Enid Zuckerman College of Public <strong>Health</strong><br />
August, 2008<br />
3
I. An Introduction to <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s<br />
A. Background In<strong>for</strong>mation<br />
What is a certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (RHCs) provide primary healthcare services in medically underserved areas<br />
and are certified under Medicare. <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s also receive an enhanced reimbursement<br />
rate from Medicare and Medicaid.<br />
What is required to be certified as a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
To be certified as a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> (RHC), a clinic must:<br />
• Be located in a non-urbanized area as determined by the U.S. Bureau of the Census;<br />
• Be located in a federally designated Medically Underserved Area (MUA), a federally<br />
designated <strong>Health</strong> Professional Shortage Area (HPSA), or in an area designated as<br />
underserved by the state’s Governor;<br />
• Provide outpatient primary care services and basic laboratory services;<br />
• Employ at least one midlevel practitioner (Nurse Practitioner, Certified Nurse Midwife,<br />
or Physician Assistant) who is on-site and available to see patients at least 50 percent of<br />
the time the clinic is open;<br />
• Meet health and safety requirements imposed by Medicare and Medicaid;<br />
• Must have a physician on staff who provides medical supervision, direction, and consultation;<br />
the physician must be present on-site at least one day every two weeks and avail<br />
able by telecommunication <strong>for</strong> assistance at all times.<br />
<strong>Clinic</strong> Ownership:<br />
<strong>Clinic</strong> ownership can be private, non-profit, or public.<br />
Provider-Based vs. Independent <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s:<br />
• Provider-based <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s are owned and operated by any entity defined by the<br />
Medicare statute as a “provider” (hospital, home health agency, or skilled nursing facility).<br />
The reimbursement <strong>for</strong> Provider-based RHCs is handled by the provider associated with the RHC.<br />
Provider-based <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s that are owned by a hospital with less than 50 beds are exempt<br />
from the per-visit reimbursement cap. The criteria <strong>for</strong> a facility being defined as “Provider-based”<br />
are not specific to the RHC program and apply to any department that seeks to be designated as<br />
4
A. Background In<strong>for</strong>mation (con’t)<br />
Provider-based. The criteria <strong>for</strong> Provider-based facilities are available online at: www.cms.hhs.<br />
gov/transmittals/downloads/a03030.pdf.<br />
• Independent RHCs are clinics not designated as Provider-based. An Independent RHC<br />
can be owned and operated by a hospital. Unless the hospital applies <strong>for</strong> and receives approval <strong>for</strong><br />
the clinic as Provider-based, it will be considered an Independent RHC. In addition to hospitals,<br />
independent RHCs can also be owned by physicians, physician assistants, nurse practitioners,<br />
certified nurse midwives, skilled nursing facilities, home health agencies, <strong>for</strong>-profit cooporations,<br />
not-<strong>for</strong>-profit corporations, or government entities. Independent RHCs are reimbursed through an<br />
RHC fiscal intermediary.<br />
Sources: National Association of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, RHC Technical Assistance, RHC Basics: Part II, http://www.<br />
narhc.org/home/RHC.php; <strong>Rural</strong> Assistance <strong>Center</strong>, <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, http://www.raconline.org/info_guides/<br />
clinics/rhc.php; U.S. Department of <strong>Health</strong> and Human Services, <strong>Health</strong> Resources and Services Administration,<br />
Office of <strong>Rural</strong> <strong>Health</strong> Policy, Starting a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>: A How-To <strong>Manual</strong>, http://ruralhealth.hrsa.gov/RHC/<br />
RHCmanual.htm.<br />
<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s Act- PL 95-210: An Overview<br />
The following is an overview, from the National Association of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, of the requirements<br />
clinics must meet in order to become certified as a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> (available<br />
online at: http://www.narhc.org/home/RHC.php).<br />
The purpose of the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s program is to encourage and stabilize the provision of out-patient<br />
primary care in underserved rural areas through the use of physicians, physician assistants (PAs) , nurse<br />
practitioners (NPs) and certifi ed nurse midwives (CNMs).<br />
1. Location - <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s must be located in communities that are both “rural” and “underserved.”<br />
For purposes of the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s Act, the following defi nitions apply to these terms:<br />
-<strong>Rural</strong> Areas - Census Bureau designation as “Non-urbanized”<br />
-Shortage Area - a federally designated <strong>Health</strong> Professional Shortage Area, a federally designated Medically<br />
Underserved Area or an Area designation by the state’s Governor as underserved.<br />
2. Physical Plant<br />
-May be permanent or mobile<br />
-Has a preventive maintenance program<br />
-Has non-medical emergency procedures<br />
3. Staffi ng<br />
-One or more physicians<br />
-One or more PAs, NPs or CNMs<br />
-PA, NP or CNM must be on-site and available to see patients 50% of the time the clinic open <strong>for</strong> patients.<br />
4. Provision of Services<br />
•Each <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> must be capable of delivering out-patient primary care services.<br />
•The <strong>Clinic</strong> must maintain written patient care policies:<br />
-Developed by a physician, physician assistant or nurse practitioner, and one health practitioner<br />
who is not a member of the clinic staff<br />
5
A. Background In<strong>for</strong>mation (con’t)<br />
-Describes the services provided directly by the clinic’s staff or through arrangement<br />
-Provide guidelines <strong>for</strong> medical management of health problems; and,<br />
-Provide <strong>for</strong> annual review of the policies<br />
-Direct Services (must be provided by clinic staff)<br />
•Provide diagnostic and therapeutic services that are commonly furnished in a physician’s offi ce<br />
•Provide basic laboratory services (6 tests)<br />
-Chemical examinations of urine<br />
-Hemoglobin or Hematocrit<br />
-Blood sugar<br />
-Examination of stool specimens <strong>for</strong> occult blood<br />
-Pregnancy test<br />
-Primary culturing <strong>for</strong> transmittal<br />
•Provide Emergency Services<br />
-First response to common life-threatening injuries and acute illnesses<br />
-Has available drugs used commonly in life-saving procedures<br />
•Services Provided through Arrangement (may be provided by individuals other than clinic staff)<br />
-In-patient hospital care<br />
-Specialized physician services<br />
-Specialized diagnostic and laboratory services<br />
-Interpreter <strong>for</strong> <strong>for</strong>eign language if indicated<br />
-Interpreter <strong>for</strong> deaf and devices to assist communication with blind<br />
5. Patient <strong>Health</strong> Records<br />
•Record System Guided by Written Policies and Procedures<br />
•Designated Professional Staff Member Responsible <strong>for</strong> Maintaining Records<br />
•Records must include the following in<strong>for</strong>mation<br />
-Identification data<br />
-Physicians’ orders<br />
-Physical exam fi ndings<br />
-Consultative fi ndings<br />
-Social data<br />
-Diagnostic and laboratory reports<br />
-Consent <strong>for</strong>ms<br />
-Medical history<br />
-<strong>Health</strong> status assessment<br />
-Signatures of the physician or other health care professionals<br />
•Protection of Record In<strong>for</strong>mation Policies<br />
-Maintenance of confi dentiality, safeguards against loss, destruction or unauthorized use<br />
-Written policies and procedures govern use and removal and release of in<strong>for</strong>mation<br />
-Written patient consent is required <strong>for</strong> release<br />
6
B. <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s in <strong>Arizona</strong> (as of 8/2008)<br />
1) Bouse Medical <strong>Clinic</strong><br />
Location: 44031 East Pulmosa Road<br />
Bouse, AZ 92885<br />
Mailing Address: Same as above<br />
Phone: (928) 512-1777<br />
Fax: (928) 849-3460<br />
Year of Certification:<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: La Paz Regional Hospital<br />
2) Community <strong>Health</strong> Care of Douglas, Inc<br />
Location: 2174 West Oak Avenue<br />
Douglas, AZ 85607<br />
Mailing Address: Same as above<br />
Phone: (520) 805-5880<br />
Fax: (520) 805-4187<br />
Year of Certification: 2007<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Southeast <strong>Arizona</strong><br />
Medical <strong>Center</strong><br />
3) Copper Queen Medical Associates- Bisbee<br />
Location: 101 Cole Avenue<br />
Bisbee, <strong>Arizona</strong> 85603<br />
Mailing Address: Same as Above<br />
Phone: (520) 432-2042<br />
Fax: (520) 432-2098<br />
Year of Certification: 2004<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Copper Queen Community<br />
Hospital<br />
4) Copper Queen Medical Associates- Douglas<br />
Location: 100 East 5th Street<br />
Douglas, <strong>Arizona</strong> 85607<br />
Mailing Address: Same as Above<br />
Phone: (520) 364-7659<br />
Fax: (520) 364-8541<br />
Year of Certification: 2004<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Copper Queen Community<br />
Hospital<br />
5) Greasewood <strong>Clinic</strong><br />
Location: Off Route 15<br />
Greasewood, AZ<br />
Mailing Address: P.O. Box 457<br />
Ganado, AZ 86505<br />
Phone: (928) 654-3208<br />
Fax: (928) 654-3478<br />
Year of Certification: 1999<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Sage Memorial Hospital<br />
6) La Paz Medical Services, Quartzsite<br />
Location: 150 East Tyson Road<br />
Quartzsite, AZ<br />
Mailing Address: P.O. Box 4618<br />
Quartzsite, AZ 85359<br />
Phone: (928) 927-8747<br />
Fax: (928) 927-8748<br />
Year of Certification: 2004<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: La Paz Regional Hospital<br />
7) Palominas Here<strong>for</strong>d <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
Location: 10524 East Highway 92<br />
Palomias, AZ 85615<br />
Mailing Address: Same as above<br />
Phone: (520) 366-0300<br />
Fax: (520) 432-1724<br />
Year of Certification: 2008<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Copper Queen Community<br />
Hospital<br />
8) Pleasant Valley Community Medical <strong>Center</strong><br />
Location: 288 Tewkbury<br />
Young, AZ 85554<br />
Mailing Address: Same as Above<br />
Phone: (928) 462-3435<br />
Fax: (928) 462-6644<br />
Year of Certification: 1995<br />
Type of <strong>Clinic</strong>: Independent<br />
Hospital Affiliation: Cobre Valley Community<br />
Hospital<br />
9) Regional <strong>Center</strong> <strong>for</strong> Border <strong>Health</strong>/San Luis<br />
Walk-In <strong>Clinic</strong><br />
Location: 1896 East Babbitt Lane, Suite D<br />
San Luis, <strong>Arizona</strong> 85349<br />
Mailing Address: Same as Above<br />
7
B. <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s in <strong>Arizona</strong> (con’t)<br />
Phone: (928) 722-6112<br />
Fax: (928) 722-6113<br />
Year of Certification: 2004<br />
Type of <strong>Clinic</strong>: Independent<br />
Hospital Affiliation: N/A<br />
10) Sage Outpatient <strong>Clinic</strong><br />
Location: Ganado, AZ<br />
Mailing Address: P.O. Box 457<br />
Ganado, AZ 86505<br />
Phone: (928) 755-4640<br />
Fax: N/A<br />
Year of Certification: 2000<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Sage Memorial Hospital<br />
11) Sulphur Springs Medical <strong>Center</strong><br />
Location: 900 W Scott Street<br />
Willcox, <strong>Arizona</strong> 85643<br />
Mailing Address: Same as Above<br />
Phone: (520) 384-4421<br />
Fax: (520) 384-4645<br />
Year of Certification: 2004<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Northern Cochise Community<br />
Hospital<br />
12) Sunsites Medical <strong>Clinic</strong><br />
Location: 225 Frontage Road<br />
Pearce, <strong>Arizona</strong> 85625<br />
Mailing Address: P.O. Box 186<br />
Pearce, <strong>Arizona</strong> 85625<br />
Phone: (520) 826-1088<br />
Fax: (520) 826-1089<br />
Year of Certification: 2004<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Northern Cochise Community<br />
Hospital<br />
13) Superior <strong>Clinic</strong><br />
Location: 14 N Magma Ave.<br />
Superior, AZ 85273<br />
Mailing Address: Same as Above<br />
Phone: (520) 689-2423<br />
Fax: (520) 689-5237<br />
Year of Certification: 2005<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Cobre Valley Community Hospital<br />
14) Tri-Valley Medical <strong>Center</strong><br />
Location: 39726 Harquahala Road<br />
Salome, AZ 85348<br />
Mailing Address: Same as Above<br />
Phone: (928) 859-3460<br />
Fax: (928) 859-3475<br />
Year of Certification: 2006<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: La Paz Regional Hospital<br />
15) Wickenburg Hospital <strong>Clinic</strong><br />
Location: 520 Rose Lane<br />
Wickenburg, AZ 85390<br />
Mailing Address: Same as above<br />
Phone: (928) 684-5421<br />
Fax: (928) 684-5081<br />
Year of Certification:<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Wickenburg Community<br />
Hospital<br />
16) Wide Ruins <strong>Clinic</strong><br />
Location: Wide Ruins, AZ<br />
Mailing Address: P.O. Box 457<br />
Ganado, AZ 86505<br />
Phone: (928) 652-3231<br />
Fax: N/A<br />
Year of Certification: 1997<br />
Type of <strong>Clinic</strong>: Provider-Based<br />
Hospital Affiliation: Sage Memorial Hospital<br />
Source: <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division<br />
of Licensing Services, Office of Medical Facilities<br />
8
C. Number of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s in the United States, 2004 1<br />
Total # of <strong>Clinic</strong>s<br />
United States 3,599<br />
Alabama 64<br />
Alaska 6<br />
<strong>Arizona</strong> 2 15<br />
Arkansas 72<br />
Cali<strong>for</strong>nia 343<br />
Colorado 35<br />
Connecticut 0<br />
Delaware 0<br />
District of Columbia 0<br />
Florida 152<br />
Georgia 95<br />
Hawaii 1<br />
Idaho 44<br />
Illinois 197<br />
Indiana 51<br />
Iowa 129<br />
Kansas 168<br />
Kentucky 115<br />
Louisiana 56<br />
Maine 49<br />
Maryland 0<br />
Massachusetts 0<br />
Michigan 156<br />
Minnesota 72<br />
Mississippi 137<br />
Missouri 271<br />
Montana 41<br />
Nebraska 89<br />
Nevada 6<br />
New Hampshire 18<br />
New Jersey 0<br />
New Mexico 11<br />
New York 9<br />
North Carolina 109<br />
North Dakota 59<br />
Ohio 17<br />
Oklahoma 42<br />
Oregon 44<br />
Pennsylvania 42<br />
Puerto Rico 0<br />
Rhode Island 1<br />
South Carolina 95<br />
South Dakota 54<br />
Tennessee 40<br />
Texas 344<br />
Utah 14<br />
Vermont 18<br />
Virgin Islands 0<br />
Virginia 55<br />
Washington 109<br />
West Virginia 63<br />
Wisconsin 62<br />
Wyoming 18<br />
1<br />
Source: <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid Services,<br />
Standard Online Survey and Certification Reporting<br />
System (OSCAR), Report 10. Accessed through: http://<br />
www.statehealthfacts.org.<br />
2<br />
According to the <strong>Arizona</strong> Department of <strong>Health</strong> Services,<br />
Division of Licensing Services, Office of Medical<br />
Facilities Licensing, <strong>Arizona</strong> has 15 certified <strong>Rural</strong><br />
<strong>Health</strong> <strong>Clinic</strong>s in as of 2008.<br />
9
D. Frequently Asked Questions<br />
Q: What are the benefits of being certified as a RHC<br />
A: RHCs receive enhanced Medicare and Medicaid reimbursement. Medicare visits are reimbursed<br />
based on allowable costs and Medicaid visits are reimbursed under the cost-based Prospective<br />
Payment System (PPS). Since certified RHCs are reimbursed on a cost-based reimbursement,<br />
as opposed to a fee-<strong>for</strong>-service reimbursement, RHC certification can increase revenues. RHCs<br />
may see improved patient flow through the utilization of NPs, PAs and CNMs, as well as more<br />
efficient clinic operations.<br />
Q: How do I know if becoming certified as a RHC could be financially beneficial <strong>for</strong> my clinic<br />
A: Experts say that a good rule of thumb to follow is if at least thirty-five to <strong>for</strong>ty percent of your<br />
patients are combined Medicare and Medicaid patients, then becoming a certified RHC could be<br />
financially beneficial to your clinic.<br />
Q: How does a certified RHC differ from a Federally Qualified <strong>Health</strong> <strong>Center</strong> (FQHC)<br />
A: Federally Qualified <strong>Health</strong> <strong>Center</strong>s are organizations that receive grants under section 330 of<br />
the Public <strong>Health</strong> Service Act. FQHCs must be open at least 32 hours per week, whereas RHCs<br />
have no minimum hours per week requirement. In addition, a <strong>for</strong>-profit clinic cannot be a FQHC<br />
but can be certified as an RHC. Unlike RHCs, FQHCs must be governed by a board of directors.<br />
FQHCs are required to provide mental health and substance abuse services, dental services, transportation<br />
services required <strong>for</strong> sufficient patient care, hospital and specialty care; RHCs are not<br />
required to provide these services.<br />
Q: Do I need a separate building to have an RHC<br />
A: No. An RHC can be in a stand-alone building, a part of another building or a mobile unit.<br />
Q: What types of services do RHCs provide<br />
A: RHCs must provide outpatient primary care services and basic laboratory services. They can<br />
also offer other services such as mental health services and vision services, however, such services<br />
may not be reimbursed based on allowable costs.<br />
Q: If a location loses its shortage designation, is it possible to remain a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
A: <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s located in rural areas that are no longer designated as medically underserved<br />
may apply <strong>for</strong> an exception. Proposed criteria <strong>for</strong> allowing an exception are spelled out in<br />
the Federal Register notice Medicare Program; <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s: Amendments to Participation<br />
Requirements and Payment Provisions; and Establishment of a Quality Assessment and Per<strong>for</strong>mance<br />
Improvement Program; Final Rule (see section II.C. Important Update from the National<br />
<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Association regarding the details and status of this CMS Final Rule).<br />
Q: Are there special staffing requirements <strong>for</strong> RHCs<br />
A: RHCs must employ at least one nurse practitioner (NP), physician assistant (PA), or certified<br />
nurse midwife (CNM). The NP, PA, or CNM must be on-site and available to see patients at least<br />
50% of the time the clinic is open. RHCs must have a physician present on-site and available to<br />
see patients at least one day every two weeks, unless greater on-site availability is required by state<br />
10
D. Frequently Asked Questions (con’t)<br />
law or state regulatory mechanism governing PA, NP or CNM practice.<br />
Q: What is the per visit upper payment limit <strong>for</strong> RHCs <strong>for</strong> 2008<br />
A: For CY 2008, the Medicare RHC upper payment limit per visit is $75.63. Provider-based clinics<br />
that are owned by a hospital with less than 50 beds are exempt from this per visit reimbursement<br />
cap. For more in<strong>for</strong>mation, visit the <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid Services at: www.<br />
cms.hhs.gov .<br />
Q: How does Medicare reimburse RHCs<br />
A: Certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s receive an interim payment rate throughout the clinic’s fiscal<br />
year, which is reconciled at the end of the fiscal year through cost reporting. The interim payment<br />
rate is determined by taking total allowable costs <strong>for</strong> RHC services divided by allowable visits<br />
provided to RHC patients receiving core RHC services. RHC staff should understand traditional<br />
Medicare regulations <strong>for</strong> coding and documentation as well as unique RHC billing requirements.<br />
Q: How does <strong>Arizona</strong> reimburse RHCs <strong>for</strong> Medicaid<br />
A: AHCCCS, <strong>Arizona</strong>’s Medicaid program, recognizes RHC services. The state reimburses RHCs<br />
under one of two different methodologies. The first is a prospective payment system. Under this<br />
methodology, <strong>for</strong> fiscal year 2001, the state calculated a per encounter rate based on an average of<br />
100 percent of the reasonable costs furnished in FY 1999 and FY 2000. For each succeeding year,<br />
this per encounter baseline rate is then increased by the Medicare Economic Index factor. The<br />
second rate setting methodology (the Alternative Payment Methodology) requires a rebase of the<br />
PPS rate every three years, and the physician services component of the CPI is used to inflate the<br />
rate during the interim years. The clinic must agree to this methodology, and the payment to the<br />
clinic must at least equal the payment under a prospective payment system.<br />
The <strong>Arizona</strong> reimbursement methodology can be downloaded at:<br />
http://www.azahcccs.gov/PlansProviders/FQHC_RHC/FQHC_RHC.asp<br />
Q: How is an RHC encounter defined<br />
A: An encounter is defined as a face-to to-face visit between a recognized provider (i.e., physician,<br />
PA, NP, CNM, or mental health provider) and a Medicare beneficiary <strong>for</strong> a medically necessary<br />
reason. <strong>Clinic</strong>s receive the RHC rate <strong>for</strong> Medicare patients <strong>for</strong> every encounter.<br />
Q: What is the difference between a UPIN and a PIN<br />
A UPIN (Unique Provider Identification Number) is a six-character alphanumeric identifier assigned<br />
to all Medicare physicians, medical groups and non-physician practitioners. A PIN (Provider<br />
Identification Number) is a unique number issued by payers to each provider to identify that<br />
provider as a credentialed and approved provider. This number is also known as a Medicare billing<br />
number.<br />
11
D. Frequently Asked Questions (con’t)<br />
Q: Can our doctors, during RHC time, treat patients at a residential care facility and assisted living<br />
care facility and be reimbursed Can our doctors do house calls and get paid<br />
A: If the medical provider treats patients in a Skilled Nursing Facility (SNF) (100-day Part A bed)<br />
in a nursing home, those services are billed to Part B, and cannot be included in Part A encounters<br />
like other nursing home visits. Only those patients in the 100-day Part A bed have to be billed to<br />
Part B. The rest of the nursing home visits are billed thru Part A as a regular RHC encounter, at the<br />
RHC encounter rate. Any time Part B is billed <strong>for</strong> a service provided, you must also “carve out”<br />
the associated cost of that service from the RHC cost report. Certainly, medical providers can still<br />
provide treatment <strong>for</strong> patients in a residential care facility, if that is the patient’s place of residence,<br />
and it is handled the same as a house call or home visit billed to Part A as an encounter. There are<br />
three places of service where the medical provider can bill as an RHC encounter. They are:<br />
1) In the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
2) In a nursing home (not a 100-day Part A stay) or other medical facility<br />
3) In the patient’s place of residence or at the scene of an accident.<br />
Q: Can our clinic at a satellite location offer health services outside of the RHC<br />
A: No. The Medicare program makes payments to the RHC <strong>for</strong> covered RHC services when provided<br />
to a patient at the clinic, skilled nursing facility or other medical facility, the patient’s place<br />
of residence, or elsewhere (i.e., at the scene of an accident).<br />
Q: How would the organizational relationships between a RHC and Critical Access Hospital<br />
(CAH) operate<br />
A: The RHC and CAH programs are two separate programs and have different participation criteria.<br />
If the facilities follow the individual criteria <strong>for</strong> their respective programs, then the two<br />
programs could co-exist. A CAH could be the owner of a certified RHC and operate the RHC<br />
as either a provider-based or independent clinic. From an economic standpoint, the CAH would<br />
be well advised to compare the payments <strong>for</strong> the clinic if operated as an RHC or as an outpatient<br />
department of the CAH. CAH outpatient payments are typically better than outpatient payments<br />
<strong>for</strong> traditional hospitals.<br />
Q: We are an RHC all day. For Medicare patients regarding CPT coding, can we use minutes vs.<br />
time spent with the patient<br />
A: Time cannot be a factor when deciding to code up or down. Coding depends on history, examination,<br />
and the medical decision needed. For example, one patient may take 30 minutes but have<br />
nothing wrong with them while another patient may be seen <strong>for</strong> only a few minutes be<strong>for</strong>e they<br />
are sent to the emergency room. Coding depends on the medical decision-making, not the amount<br />
of time.<br />
Q: If you make rounds at the nursing home and you see a patient who is on hospice, can you bill<br />
it as an RHC visit<br />
A: If the hospice patient receives services from you that are unrelated to the patient’s terminal condition,<br />
then you can then bill the visit to the RHC. However, if you are adjusting pain medications<br />
or providing supportive care, then you must bill hospice.<br />
12
D. Frequently Asked Questions (con’t)<br />
Q: Regarding supplies, in order to be covered in the RHC, what must the supply or service be<br />
A: The supply or service must be of a type that would be furnished in a physician’s office; a type<br />
that is commonly provided without charge or included in the RHC’s bill; and a type that is provided<br />
as incidental to the service of the physician, nurse practitioner, physician assistant, clinical<br />
social worker, certified midwife, or clinical psychologist.<br />
Q: Are RHCs subject to “incident to” regulations as it relates to the provision of services by the<br />
midlevel provider<br />
A: No. The physician does not need to be present in the facility when a midlevel provider sees the<br />
patient and midlevel providers can see patients new to the clinic.<br />
Q: Do I have to log every flu and pneumoccal shot including non-Medicare patients<br />
A: No. There is no requirement to log other payer types, however, the total flu and total pneumoccal<br />
shots provided are needed to complete the cost report correctly.<br />
Q: How are flu and pneumoccal shots billed in RHCs<br />
A: A log or roster of Medicare patients is maintained and submitted with the cost report at yearend.<br />
Medicare pays the cost of the shots. No bill is submitted to Medicare.<br />
Q: What does Medicare require regarding documentation in the flu and pneumoccal logs<br />
A: Patient Name, HIC Number (Medicare Number), and Date of service (shot).<br />
Q: Can RHC bill <strong>for</strong> both a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> visit and an inpatient admission on the same<br />
day<br />
A: No. Medicare would consider this double dipping.<br />
Q: If you per<strong>for</strong>m a surgery in the hospital using a global fee and the patient has a pre-op and a<br />
post-op visit in the RHC, can I bill Medicare Part A <strong>for</strong> the RHC visits<br />
A: No. Medicare would consider this double dipping.<br />
Sources: <strong>Rural</strong> Resource <strong>Center</strong>, <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, http://www.raconline.org/info_guides/clinics/rhc.php#faq;<br />
J.E. Estes, <strong>Health</strong>care Horizon; <strong>Rural</strong> Resource <strong>Center</strong>, Federally Qualified <strong>Health</strong> <strong>Center</strong>s, http://www.raconline.<br />
org/info_guides/clinics/fqhc.php.; National Association of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, RHC Technical Assistance, RHC<br />
The Basics: Part II; <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid Services, Announcement of Medicare <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s<br />
(RHCs) and Federally Qualified <strong>Health</strong> <strong>Center</strong>s (FQHCs) Payment Rate Increase, http://www.cms.hhs.gov/Transmittals/Downloads/R796CP.PDF;<br />
AHCCCS, <strong>Arizona</strong> state plan amendment (SPA) 03-007, http://www.ahcccs.state.<br />
az.us/Publications/PlansWaivers/Amendments/MedicaidSPAs/2003/03_007ApprovalCMS1_5_04.pdf; Oregon Office<br />
of <strong>Rural</strong> <strong>Health</strong>, <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, http://www.ohsu.edu/ohsuedu/outreach/oregonruralhealth/clinics/aboutclinics.cfm.<br />
13
E. Steps to Becoming a Certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
Step 1: Determine Eligibility <strong>for</strong> Certification. The interpretive guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong><br />
<strong>Clinic</strong>s are listed in section II. B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s of this manual.<br />
Step 2: Financial Feasibility Assessment. A financial study should assess the actual (<strong>for</strong> existing<br />
clinics) or estimated (<strong>for</strong> new clinics) data on payor mix (Medicare, Medicaid, and other). Experts<br />
say that a good rule of thumb to follow is if at least thirty-five to <strong>for</strong>ty percent of your patients are<br />
combined Medicare and Medicaid patients, then becoming a certified RHC could be financially<br />
beneficial. Additionally, if an existing practice does not currently employ an NP, PA, or CNM, the<br />
practice must decide whether the cost of hiring one would be offset by increased revenue.<br />
Step 3: File an RHC Application.<br />
If the site is already licensed as an Outpatient Treatment <strong>Center</strong> by the state of <strong>Arizona</strong>, the site<br />
must send a letter to the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services,<br />
Office of Medical Facilities Licensing (http://www.azdhs.gov/als/medical) stating that the site<br />
would like to be certified as a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>. The letter should also include a request <strong>for</strong> an<br />
RHC application packet. It is important that the site contact their Medicare fiscal intermediary<br />
be<strong>for</strong>e completing the CMS 855A provider/supplier enrollment application <strong>for</strong>m. If the site does<br />
not know who their fiscal intermediary is, they may check the <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid<br />
Service’s Intermediary Carrier Directory website (http://www.cms.hhs.gov/ContractingGeneralIn<strong>for</strong>mation/Downloads/02_ICdirectory.pdf)<br />
or they may contact the <strong>Arizona</strong> Department of <strong>Health</strong><br />
Services, Division of Licensing Services, Office of Medical Facilities Licensing.<br />
If the site is not already licensed as an Outpatient Treatment <strong>Center</strong> by the state of <strong>Arizona</strong>, the site<br />
must send a letter to the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services,<br />
Office of Medical Facilities Licensing (http://www.azdhs.gov/als/medical) stating that the site<br />
would like to be licensed as an Outpatient Treatment <strong>Center</strong> and certified as a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>.<br />
In the letter, the site should request both a licensing packet and an RHC application packet. It is<br />
important that the site contact their Medicare fiscal intermediary be<strong>for</strong>e completing the CMS 855A<br />
provider/supplier enrollment application <strong>for</strong>m (this <strong>for</strong>m can be obtained from the following website:<br />
http://www.cms.hhs.gov/CMSForms). If the site does not know who their fiscal intermediary<br />
is, they may check the <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid Service’s Intermediary Carrier Directory<br />
website (http://www.cms.hhs.gov/ContractingGeneralIn<strong>for</strong>mation/Downloads/02_ICdirectory.<br />
pdf).<br />
Please note: Facilities located on an Indian Reservation do NOT have to be licensed as an Outpatient Treatment <strong>Center</strong><br />
in order to apply <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> certification. In addition, private practice clinics not providing urgent care<br />
services may not be required to be licensed as an Outpatient Treatment <strong>Center</strong> in order to apply <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
certification. Contact the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services, Office of Medical<br />
Facilities Licensing <strong>for</strong> more in<strong>for</strong>mation.<br />
Step 4: RHC Certification Inspection. The site should contact the <strong>Arizona</strong> Department of<br />
<strong>Health</strong> Services, Division of Licensing Services, Office of Medical Facilities Licensing, in writing,<br />
and indicate when the site would be ready <strong>for</strong> an inspection. To be ready <strong>for</strong> the inspection, the site<br />
needs to be in compliance with RHC requirements and have seen patients at the site. The<br />
14
E. Steps to Becoming a Certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> (con’t)<br />
<strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services, Office of Medical Facilities<br />
Licensing will then conduct a survey.<br />
Step 5: <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Cost Report. Once a clinic has received its Medicare Provider Letter<br />
from the <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid Services, the clinic then files a projected cost<br />
report in order to have its Medicare Rate determined. Independent <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s complete<br />
the CMS-222-92 Form and Provider-based <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s complete Worksheet M of the<br />
CMS-2552-96 Form. These <strong>for</strong>ms are available from the CMS Web site (http://www.cms.hhs.<br />
gov/CMSForms/).<br />
Adapted from: <strong>Rural</strong> Assistance <strong>Center</strong>, <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s, http://www.raconline.org/info_guides/clinics/rhc.php.<br />
15
A. State Licensing<br />
II. Licensing and Certification Requirements<br />
A site must be licensed by the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services,<br />
Office of Medical Facilities Licensing as an Outpatient Treatment <strong>Center</strong> in order to become<br />
a certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> in <strong>Arizona</strong>. If a site is interested in becoming both licensed and a<br />
certified <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>, then the site may request both a licensing application packet and an<br />
RHC application packet from the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing<br />
Services, Office of Medical Facilities Licensing (see Appendix A. Important Contact In<strong>for</strong>mation).<br />
The requirements <strong>for</strong> licensing medical facilities are according to Title 9, Chapter 10 of the<br />
<strong>Arizona</strong> Administrative Code. To see the sections of the code pertaining to the licensing of health<br />
institutions in its entirety, please visit the following website http://www.azsos.gov/public_services/Title_09/9-10.htm<br />
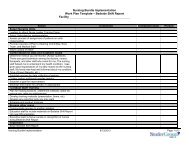
The <strong>for</strong>ms required <strong>for</strong> licensing (see Appendix E. Licensing Forms) can be printed from the internet<br />
from the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services, Office of<br />
Medical Facilities Licensing’s website (http://www.azdhs.gov/als/medical). If the site is applying<br />
<strong>for</strong> an initial license, the site must complete the “Initial Application <strong>for</strong> a <strong>Health</strong> Care Institution<br />
License.” The initial application is <strong>for</strong> a new facility just being licensed <strong>for</strong> the first time or <strong>for</strong><br />
an already licensed facility that has had a change in location or ownership. If the site is applying<br />
<strong>for</strong> a renewal of their license, the site must complete the “Renewal Application <strong>for</strong> a <strong>Health</strong> Care<br />
Institution License.” In addition, an Outpatient Facility In<strong>for</strong>mation sheet must accompany the<br />
initial or renewal application.<br />
An important aspect of licensing is that the facility’s floor plan must be contiguous. For example, if<br />
a patient must pass through a hallway in order to get to another area of the clinic, and that hallway<br />
is not licensed, then the patient of the clinic cannot pass through that hallway. There<strong>for</strong>e, once the<br />
patient comes into the licensed area, the patient must be able to stay in the licensed area <strong>for</strong> the<br />
duration of the visit. It is important to note that the <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division<br />
of Licensing Services, Office of Medical Facilities Licensing must be notified, in writing, if<br />
any changes are made to the site’s building, administration, or to the services offered by the site.<br />
Please note: Facilities located on an Indian Reservation do NOT have to be licensed as an Outpatient<br />
Treatment <strong>Center</strong> in order to apply <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> certification. In addition, private<br />
practice clinics not providing urgent care services may not be required to be licensed as an Outpatient<br />
Treatment <strong>Center</strong> in order to apply <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> certification. Contact the <strong>Arizona</strong><br />
Department of <strong>Health</strong> Services, Division of Licensing Services, Office of Medical Facilities<br />
Licensing <strong>for</strong> more in<strong>for</strong>mation.<br />
Source: <strong>Arizona</strong> Department of <strong>Health</strong> Services, Division of Licensing Services, Office of Medical Facilities Licensing,<br />
http://www.azdhs.gov/als/medical.<br />
16
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s<br />
A site must comply with the following guidelines in order to become a certified <strong>Rural</strong> <strong>Health</strong><br />
<strong>Clinic</strong>. These interpretive guidelines are available online from the National Association of <strong>Rural</strong><br />
<strong>Health</strong> <strong>Clinic</strong>s at: http://www.narhc.org/uploads/pdf/RHCmanual1.pdf The <strong>for</strong>ms required <strong>for</strong> certification<br />
as a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> are listed in Appendix F. Certification Forms.<br />
INTERPRETIVE GUIDELINES - RURAL HEALTH CLINICS<br />
Conditions <strong>for</strong> Certification<br />
I. COMPLIANCE WITH FEDERAL, STATE, AND LOCAL LAWS (42 CFR 491.4)<br />
The RHC and its staff are in compliance with applicable Federal, State, and local laws and regulations.<br />
A. Federal Laws and Regulations.--The Federal regulations governing the certifi cation of RHCs were<br />
published in the Federal Register on July 14, 1978, 43 FR 136. Conditions <strong>for</strong> certifi cation under those<br />
regulations are the subject of these guidelines.<br />
B. State Laws and Regulations. All States have practice acts that govern the activities of health professionals.<br />
While there is considerable variation in the States’ practice acts concerning physician assistants, nurse<br />
practitioners and certifi ed nurse-midwives, there is a broad mandate in the medical practice acts of all States<br />
giving physicians authority to diagnose and treat medical conditions. The extent to which the physician may<br />
delegate these responsibilities and to whom, and under what conditions, varies in the states. Some States<br />
have updated their practice acts since the advent of the physician assistant, nurse practitioner and certifi ed<br />
nurse-midwife health care professionals. In some instances, these updated practice acts have included<br />
defi nitions and specifi c references to permitted/prohibited activities, supervision/guidance required by a<br />
physician, and location/situations in which nurse practitioners, certifi ed nurse-midwives and physician<br />
assistants may function. In some States where nurse practice acts have not been signifi cantly updated,<br />
some functions of the nurse practitioner are viewed as an extension of the traditional nursing role as being<br />
covered by the existing nurse practice act.<br />
<strong>Rural</strong> health clinics can be certifi ed only if the State permits--that is, does not explicitly prohibit--the delivery<br />
of primary health care by a nurse practitioner, certifi ed nurse-midwife or a physician assistant. The surveyor<br />
will encounter wide variations in the wording, interpretation, and application of States’ practice acts as they<br />
affect the physician assistant, nurse practitioner and certifi ed nurse-midwife in the RHC setting.<br />
In situations where the State law is silent, or where the state law does not specifi cally prohibit the functioning<br />
of a physician assistant, nurse practitioner or certifi ed nurse-midwife with medical direction by a physician<br />
and with the degree of supervision, guidance, and consultation required by the RHC regulations, the<br />
surveyor may consider this condition as being met. Interpretations needed on specifi c aspects of the State’s<br />
practice act should be sought through the State regulatory agency or board(s) dealing with the practice and<br />
profession.<br />
II. LOCATION OF CLINIC (42 CFR 491.5)<br />
Consult with the Regional Offi ce (R.O.) to preliminarily ascertain that a clinic meets the basic requirement<br />
of location prior to scheduling a survey. The clinic must be located in a rural area that is designated as<br />
a shortage area. Applicants determined not qualifi ed under this requirement should be sent a letter (see<br />
Exhibit.27) with the appropriate notation.<br />
A. <strong>Rural</strong> Area Location. The law requires the clinic to be located in an area “that is not an urbanized area as<br />
defi ned by the Bureau of the Census.” The Bureau has published both a narrative defi nition of an urbanized<br />
17
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
area and maps displaying the land area of urbanized areas. Lists and maps of the urbanized areas are<br />
contained in the “number of inhabitants” census volume <strong>for</strong> that State (census of population series PC-<br />
80-1-A). Note that this definition is different from that of a metropolitan statistical area (MSA). Contact the<br />
Census Bureau <strong>for</strong> a determination on whether the clinic is located in a non-urbanized area.<br />
B. Shortage Area <strong>Designation</strong>. After it has been ascertained that the clinic is located in a non-urbanized<br />
area, the CMS RO will certify whether or not the clinic is located in a “currently” designated shortage<br />
area. The CMS RO, after consulting with PHS RO staff, promptly responds in writing to the request <strong>for</strong> a<br />
determination. This in<strong>for</strong>mation may be given by telephone as long as it is followed by a written response.<br />
This consultation explores designation:<br />
-- As an area with a shortage of personal health services under 5330(b)(3) or 1302(7) of the PHS<br />
Act;<br />
-- As a health professional shortage area described in 5332(a)(1)(A) of the PHS Act;<br />
-- As an area which includes a population group which the Secretary determines has a health<br />
professional shortage under 5332(a)(1)(B) of the PHS Act;<br />
-- As a high migrant impact area described in 5329(a)(5) of the PHS Act; or<br />
-- As an area designated by the chief executive offi cer of the State and certifi ed by the Secretary<br />
as an area with a shortage of personal health services.<br />
These designations are published periodically in the Federal Register by the PHS Bureau of <strong>Health</strong><br />
Care Delivery and Assistance. <strong>Designation</strong> under any section qualifi es a RHC location. The designation<br />
process is a continuing process, with additions of newly designated areas and deletions of previously<br />
designated areas occurring daily. <strong>Designation</strong> in<strong>for</strong>mation can also be obtained on-line by going to: http://<br />
datawarehouse.hrsa.gov/<br />
For HPSA in<strong>for</strong>mation, click on <strong>Health</strong> Professional Shortage Areas (HPSAs) under the <strong>Health</strong> Professions<br />
header and <strong>for</strong> MUA in<strong>for</strong>mation click on Medically Underserved Areas/Medically Underserved Populations<br />
which is under the Primary <strong>Health</strong> Care header.<br />
C. Mobile Units. The Conditions <strong>for</strong> Certifi cation must be met by a mobile unit <strong>for</strong> it to qualify as a RHC. In<br />
addition, it should be ascertained that the mobile unit has fi xed scheduled locations, each of which meet the<br />
rural and shortage area requirements.<br />
Since the mobile unit is a clinic, it is expected that the RHC services are provided in the unit and not in<br />
a permanent structure, with the unit serving only as a mobile repository <strong>for</strong> the equipment, supplies, and<br />
records. The only exception would be if the RHC services are furnished off the clinic’s premises (away from<br />
the unit) to homebound patients.<br />
Where a facility offers RHC services at a permanent structure as well as in a mobile unit, each facility must<br />
be certifi ed separately as a RHC. This is differentiated from the situation where a permanent structure<br />
provides RHC services off the premises, e.g., to homebound patients, with the use of a vehicle to transport<br />
supplies, equipment, records, and staff.<br />
D. Exceptions to the Location Requirement. There are two grandfather provisions applicable to the<br />
certifi cation process.<br />
1. Loss of Location Eligibility. This grandfather provision applies to the annual recertifi cation process. It<br />
should be used as a “yea” response to item J11 and on the CMS-30 when a facility which was previously<br />
certifi ed as being located in a nonurbanized and designated shortage area subsequently loses either or both<br />
of these characteristics. When this occurs, the facility does not lose its eligibility <strong>for</strong> continued participation<br />
in the program because it does not meet the location requirement. If J11 is marked yes, mark J17 and J18<br />
N/A.<br />
18
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
2. <strong>Clinic</strong>s Operating on July 1, 1977. Potential applicants under this grandfather provision still have to<br />
meet the rural location requirement. The other requirement under this provision is that the Secretary has<br />
determined that the area served has an insuffi cient supply of primary care physicians. Facilities providing<br />
services on July 1, 1977, in a nonurbanized area which is determined to have unmet needs <strong>for</strong> primary<br />
health care but which is not a designated shortage area are potential applicants. There<strong>for</strong>e, the facility may<br />
be primarily serving a designated area but not located in a designated shortage area. It must be determined<br />
whether the location of the clinic is an appropriate part of a service area which includes areas or populations<br />
which have been designated either as having a health manpower shortage, or as being medically<br />
underserved. Aiding this determination will be previous PHS decisions made on behalf of the Secretary.<br />
The answer to question V on CMS-29 is an important indicator. Several PHS programs provide or have<br />
provided grant support to enable the facility to provide health care to designated areas. These programs do<br />
not require that the facility be located in a designated shortage area. Many of these facilities were operating<br />
with PHS grant support prior to enactment of the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Services Act of 1977 (P.L.95-210) and<br />
may constitute certifi able RHC applicants.<br />
Some examples of these PHS programs are National <strong>Health</strong> Service Corps (KHSC), Migrant <strong>Health</strong>, <strong>Health</strong><br />
Underserved <strong>Rural</strong> Areas (HURA), and <strong>Rural</strong> <strong>Health</strong> Initiative (RHI). Prior to P.L.95-210 a number of states<br />
had programs to assist their rural areas with greater access to primary care. The location of the facilities<br />
developed by these programs was determined by valid criteria established by the State, although location<br />
in a designated shortage area may not have been one of them. These facilities are also potential applicants<br />
under this grandfather provision.<br />
When it is determined that an applicant clinic not located in a designated shortage area may be a potential<br />
applicant under this grandfather provision, develop the following in<strong>for</strong>mation and submit it to the CMS RO<br />
<strong>for</strong> a determination as to whether the facility meets the requirements of this ‘grandfather provision:<br />
-- A description of the geographic boundaries of the facility’s service area;<br />
-- In<strong>for</strong>mation developed through consultation with the PHS RO, staff about whether the area,<br />
or any portion of the area, had ever been reviewed <strong>for</strong> designation under any of the applicable<br />
sections of the PHS Act;<br />
-- Identification of any designated population group or institution in the facility’s service area;<br />
-- In<strong>for</strong>mation secured from the appropriate <strong>Health</strong> Systems Agency and the State <strong>Health</strong><br />
Planning and Development Agency and about the primary care resources available<br />
in the facility’s service area;<br />
-- In<strong>for</strong>mation about any planning, developmental, or operating funds awarded to the facility by<br />
the county, State, or Federal Government to assist in providing, greater access- to health care<br />
in the area;<br />
-- In<strong>for</strong>mation about the factors considered in determining where the facility was to be located;<br />
and<br />
-- Any additional in<strong>for</strong>mation the SA or RO feels is relevant.<br />
III. PHYSICAL PLANT AND ENVIRONMENT (42 CFR 491.6)<br />
A. Physical Plant Safety. To insure the safety of patients, personnel, and the public, the physical plant<br />
should be maintained consistent with appropriate State and local building, fi re, and safety codes. Reports<br />
prepared by State and local personnel responsible <strong>for</strong> insuring that the appropriate codes are met should<br />
be available <strong>for</strong> review. Determine whether the clinic has safe access and is free from hazards that may<br />
affect the safety of patients, personnel, and the public.<br />
B. Preventive Maintenance. A program of preventive maintenance should be followed by the clinic. This<br />
includes inspection of all clinic equipment at least yearly, or as the type, use, and condition of equipment<br />
dictates; the safe storage of drugs and biologicals (see 42 CFR 491.6(b)(2)) and inspection of the facility to<br />
assure that services are rendered in a clean and orderly environment. Inspection schedules and reports<br />
19
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
should be available <strong>for</strong> review by the surveyor.<br />
C. Non-medical Emergencies. Review written documentation and interview clinic personnel to determine<br />
what instructions <strong>for</strong> non-medical emergency procedures have been provided and whether clinic personnel<br />
are familiar with appropriate procedures. Non-medical emergency procedures may not necessarily be the<br />
same <strong>for</strong> each clinic.<br />
IV. ORGANIZATIONAL STRUCTURE (42 CFR 491.7)<br />
A. Basic Requirements. Ascertain that the clinic is under the medical direction of a physician(s), has a staff<br />
that meets the requirements of 5491.8,and has adequate written material covering organization policies,<br />
including lines of authority and responsibilities.<br />
B. Written Policies. Written policies should consist of both administrative and patient care policies.<br />
Patient care policies are discussed under 42 CFR 491.9(b). In addition to including lines of authority<br />
and responsibilities, administrative policies may cover topics such as personnel, fi scal, purchasing, and<br />
maintenance of building and equipment. Topics covered by, written policies may have been infl uenced<br />
by requirements of the founders of the clinic, as well as agencies that have participated in supporting the<br />
clinic’s operation.<br />
C. Disclosure of Names and Addresses. The clinic discloses names and addresses of the owner, person<br />
responsible <strong>for</strong> directing the clinic’s operation, and physician(s) responsible <strong>for</strong> medical direction. Any entity<br />
may organize itself as an owner of a RHC. The types of organizations being referred to are described in<br />
answers to question IV on the Request to Establish Eligibility. These range from:<br />
-- A physician in a private general practice located in a shortage area who employs either a nurse<br />
practitioner, certifi ed nurse-midwife or a physician assistant;<br />
-- A nurse practitioner, certified nurse-midwife or a physician assistant in solo practice in a<br />
shortage area who develops the required relationship with a physician <strong>for</strong> medical direction; to<br />
-- Organizations either <strong>for</strong> profi t or not <strong>for</strong> profi t who own primary care clinics located in shortage<br />
areas.<br />
Any change in ownership or physician(s) responsible <strong>for</strong> the clinic’s medical direction requires prompt notice<br />
to the RO. Neither of these changes requires resurvey or recertifi cation if the change can otherwise be<br />
adequately verifi ed. Notice of any change in the physician(s) responsible <strong>for</strong> providing the clinic’s direction<br />
should include evidence that the physician(s) is licensed to practice in the state.<br />
V. STAFFING AND STAFF RESPONSIBILITIES (42 CFR 491.8)<br />
A. Suffi cient Staffing. The staffi ng described in 42 CFR 491.8(a) is the minimum staffi ng requirement.<br />
However, you also determine whether the clinic is suffi ciently staffed to provide services essential to its<br />
operation. Because clinics are located in areas that have been designated as having shortages of health<br />
manpower or personnel health services, they frequently are not able to employ what would be considered<br />
suffi cient health care staffs. When item J42 on the SRF is marked no, explain, with reasonable detail,<br />
the circumstances (and ef<strong>for</strong>ts to overcome them) that make employment of additional needed staff not<br />
possible.<br />
Should the loss of a physician, physician assistant, certifi ed nurse-midwife or nurse practitioner member<br />
of the staff reduce the clinic’s staff below the required minimum, the clinic should be af<strong>for</strong>ded a reasonable<br />
time to comply with the staffi ng requirement. The clinic must provide some type of documentation showing<br />
the its good faith ef<strong>for</strong>t to obtain staff. The clinic should in<strong>for</strong>m the State of all actions taken to recruit a<br />
replacement and expected outcome. The loss of a physician assistant or nurse practitioner staff member<br />
may require a temporary adjustment of the clinic’s operating hours or services and an adjustment in the<br />
scheduled visits by the physician(s) providing medical direction. The loss of the physician member will<br />
20
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
require the clinic to make temporary arrangements <strong>for</strong> medical direction with another physician(s), and this<br />
might alter the scheduled times the physician is present in the clinic. Follow these situations closely, and<br />
make recommendations about approvals pending correction of defi ciencies, compliance, or decertifi cation.<br />
It in the responsibility of the clinic to promptly advise you of any changes in staffi ng which would affect its<br />
certifi cation status.<br />
B. Staffi ng Availability. A physician, nurse practitioner, certifi ed nurse-midwife (meeting the defi nition in<br />
42 CFR 405.2401(b)(10)) or physician assistant must be available to furnish patient care services at all<br />
times the clinic operates. Only the scheduled operating hours the clinic is offerring RHC services are to be<br />
considered (as distinguished from other ambulatory services or related health activities).<br />
A nurse practitioner, certifi ed nurse-midwife or physician assistant must be available to furnish patient care<br />
services at least 50 percent of the scheduled operating hours during which RHC services are offered, even<br />
though a physician is present in the clinic on a full-time basis during the time RHC services are offered. The<br />
phrase “available to furnish patient care services” means (1) providing RHC services in the clinic; (2) being<br />
physically present in the clinic even though not providing RHC services; or (3) providing RHC services to<br />
clinic patients outside the clinic. These services must be RHC services. Items (1) and (2) indicate that a<br />
physician, physician assistant, certifi ed nurse-midwife or nurse practitioner is present on the premises, not<br />
on call, during the scheduled operating hours when RHC services are offered at the facility. Item (3) refers<br />
to that part of the clinic’s operating schedule utilized in providing RHC services outside the clinic.<br />
A RHC’s total operating schedule, there<strong>for</strong>e, consists of offering RHC services at the clinic, as well as<br />
providing RHC services to patients outside the clinic. Determinants of how a clinic schedules its operating<br />
time include the size of the required staff, patient population, and where the services need to be provided.<br />
Some clinics, within their scheduled hours, may be able to concurrently offer RHC services both on and off<br />
the clinic’s premises, whereas other clinics may have to schedule separate hours <strong>for</strong> offering the services<br />
on and off the clinic’s premises (e.g., a clinic’s total operating schedule may be from 9 a.m. to 5 p.m. daily,<br />
with on-premises services offered from 9 a.m. to 3 p.m., and off-premises services offered from 3 p.m. to<br />
5 P.M.).<br />
Section 1861(aa)(2)(J) of the Act requires that a physician assistant, certifi ed nurse-midwife or nurse<br />
practitioner must be available to provide patient care services during at least 50 percent of the RHC’s<br />
total operating schedule. There<strong>for</strong>e, a physician must provide needed services at other times during the<br />
clinic’s scheduled operating hours. A RHC which does not have a physician, physician assistant, certifi ed<br />
nurse-midwife or nurse practitioner on the premises to render services during the scheduled operating<br />
hours of the clinic does not meet the requirements of S1861(aa)(2) of-the Act, even though the 50 percent<br />
requirement may be met.<br />
The following are examples of how determinations regarding these requirements may be made. A clinic has<br />
a total operating schedule of from 9 to 5 Monday through Friday, and from 9 to 1 on Saturday (44 hours a<br />
week). RHC services are offered from 10 to 5 Tuesday through Friday (28 hours a week, which satisfi es the<br />
51 percent requirement). A physician, nurse practitioner, certifi ed nurse-midwife, or a physician assistant<br />
must be available to furnish patient care services from 10 to 5 Tuesday through Friday (28 hours a week).<br />
Of these 28 hours, a nurse practitioner, certifi ed nurse-midwife or physician assistant must be available at<br />
least 14 hours (5.0 percent of 28 hours) to furnish patient care services.<br />
In some cases, the clinic’s weekly schedule may not be a logical period of time on which to base these<br />
determinations, and consideration of the biweekly or even a monthly schedule may be more appropriate.<br />
Such a situation may occur when a clinic has a very limited total operating schedule and the schedule<br />
offering RHC services is concentrated in a specifi ed period of the biweekly or monthly total, schedule.<br />
An example would be a clinic that is open only every other Tuesday and Friday from 10 to 4 (24 hours a<br />
month), and RHC services are offered every other Tuesday from 10 to 4, and one Friday a month from 10<br />
21
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
to 4 (18 hours a month). In this situation, it is appropriate to consider the clinic’s total monthly operating<br />
schedule <strong>for</strong> determining whether RHC services are offered during at least 51 percent of the schedule. A<br />
physician, a nurse practitioner, certifi ed nurse-midwife, or a physician assistant must be available to furnish<br />
patient care services every other Tuesday from 10 to 4, and one Friday from 10 to 4 (18 hours a month).<br />
Of these 18 hours, a nurse practitioner, certifi ed nurse-midwife or physician assistant must be available at<br />
least 9.18 hours to furnish patient care services.<br />
C. Staff Responsibilities. The requirement that a physician, physician assistant, certifi ed nurse-midwife,<br />
and/or nurse practitioner participate jointly in the development of the clinic’s written policies does not require<br />
the development of new policies in the event of changes in these staff members. Nevertheless, each staff<br />
member must review, agree with, and adhere to, or propose amendments to the clinic’s policies. Compliance<br />
with this requirement has a special relationship to the clinic’s written patient care guidelines. There should<br />
be suffi cient written documentation that this requirement is appropriately carried out. There should be some<br />
mechanism to ensure that new clinic personnel are completely familiar with these policies.<br />
1. Physician Responsibilities. Ascertain through written documentation, such as dates and signatures, that<br />
the physician staff member satisfactorily meets the requirement of periodically reviewing the clinic’s patient<br />
records, provides medical orders, and provides medical care services to the patients.<br />
A physician member is required to be present in the clinic <strong>for</strong> suffi cient periods of time to per<strong>for</strong>m the duties<br />
and responsibilities described in 42 CFR 491.8(b)(i), (ii), and (iii). The term “suffi cient periods of time”<br />
requires relative evaluations. There are a number of elements to consider in weighing what would constitute<br />
a reasonable time suffi cient to discharge the physician member’s responsibilities. These elements include:<br />
patient case load and mix (type), number of patient care records which must be reviewed in order to<br />
establish a good overview <strong>for</strong> adherence to policies and principles of quality patient care, number of patient<br />
care records which require review and discussion of specifi c health problems and regimens of therapy;<br />
need <strong>for</strong> consultative time with other members of the clinic’s staff; need <strong>for</strong> revision to the clinic’s patient<br />
care guidelines; and need <strong>for</strong> time to provide medical care to patients.<br />
Time required to accomplish these activities will fl uctuate. Thus, the “sufficient time” the physician must<br />
spend in the clinic will vary. The survey should verify the time spent in the clinic by the physician <strong>for</strong><br />
consulting records, etc. Extraordinary circumstances which constitute exceptions to the requirement that<br />
the physician Member be present in the clinic at least once every 2 weeks <strong>for</strong> “suffi cient time to discharge<br />
the physician’s responsibilities are primarily nonrecurring circumstances beyond the control of the physician<br />
and which postpone (not cancel) the visit. These circumstances include illness, extreme weather or driving<br />
conditions of short duration, or those emergencies which occur in the physician’s practice and require his<br />
presence elsewhere. When nonrecurring circumstances cause postponement of the physician’s visit, they<br />
should be documented in the clinic’s records.<br />
In some instances, recurring extraordinary circumstances may constitute reasonable exception to the<br />
physician’s presence requirement. This type of exception requires specifi c approval from the CMS RO <strong>for</strong><br />
certifi cation purposes, and must be documented by the surveyor. The essential areas <strong>for</strong> consideration of<br />
this exception would include:<br />
-- The remoteness of the clinic (due to extraordinary distance and inaccessibility of the terrain)<br />
make frequent travel impossible or unreasonable;<br />
-- The remoteness of the physician members location has already placed the physician in an<br />
extraordinary extended practice and/or designated shortage area and required visits at<br />
least once in every 2 week period to a clinic located at a great distance would severely detract<br />
from the physician’s practice; or<br />
-- It is clearly established in advance that continuing conditions are known to be expected (snow,<br />
fl ood, bridge repair, etc.) which will make reasonable access to the clinic not possible<br />
<strong>for</strong> extended periods of time.<br />
22
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
2. Physician Assistant, Nurse Practitioner and Certifi ed Nurse Midwife Responsibilities. The surveyor<br />
verifi es through appropriate written documentation that the physician assistant, certifi ed nurse-midwife<br />
and/or nurse practitioner is periodically per<strong>for</strong>ming the necessary responsibilities listed under J51, CMS<br />
30.<br />
VI. PROVISION OF SERVICES (42 CFR 491.9)<br />
A. Basic Requirements<br />
1. State and Local Laws. Know the State’s position, generally, with respect to implementing the Federal<br />
RHC requirements vis-a-vis the State’s Medical Practice Act, Nurse Practice Act, the Pharmacy Act and<br />
the Comprehensive Drug Abuse Prevention and Control Act of 1970 (P.L. .91513) and the general scope of<br />
practice permitted <strong>for</strong> nurse practitioners, certifi ed nurse-midwives and physician assistants.<br />
Some States may have legal impediments because applicable practice acts prohibit nurse practitioners,<br />
certifi ed nurse-midwives and/or physician assistants from independent acts of medical diagnosis and<br />
treatment precluding the fullest implementation of the Federal RHC requirements.<br />
This does not necessarily preclude participation by a RHC that provides RHC services (physician-type<br />
services) furnished by nurse practitioners, certifi ed nurse-midwives and/or physician assistants under the<br />
direct supervision (as distinguished from indirect supervision) of a physician.<br />
There<strong>for</strong>e, inquiries to State authorities about compliance with the Federal RHC requirements, as well as<br />
decisions concerning applicant RHCs, must be weighed against several determinations, including:<br />
-- The medical direction and supervision described in the regulations is the minimum requirement;<br />
many participating RHCs operate with greater medical direction and supervision than<br />
these minimums.<br />
-- The word “supervision” does not automatically equate with direct, over the shoulder<br />
supervision. Many States requiring physician supervision of medical acts per<strong>for</strong>med by a nurse<br />
practitioner or a physician assistant have held that per<strong>for</strong>mances of such medical acts under<br />
written patient care guidelines developed and/or approved by a licensed physician satisfy the<br />
requirement of supervision.<br />
2. Providing <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Services. The law describes a RHC as a facility primarily engaged in<br />
providing RHC services as defi ned in this subpart. Under this defi nition, a facility may provide services in<br />
addition to RHC services; usually, related health care services such as the “other ambulatory services”<br />
covered by Medicaid State plans. Certifi cation as a RHC applies to the facility as a whole and the total<br />
operating schedule of the facility (the hours it is open) is considered when determining if the facility is<br />
primarily engaged in providing RHC services. If onsite observation of services provided and discussion with<br />
the staff indicate that the majority of the services provided by the clinic are primary medical care (treatment<br />
of acute or chronic medical problems which usually bring a patient to a physician’s offi ce), then the clinic<br />
may satisfy the “primarily engaged” requirement providing that RHC services are offered at least 51 percent<br />
of the total operating schedule. The time RHC services are offered may differ from the total operating<br />
schedule of the facility, but may not be less than 51 percent of this total operating schedule.<br />
If there is a question about this condition, review a sample of patient health records covering a reasonable<br />
period of time to determine the majority of specifi c services actually furnished.<br />
An example of a clinic schedule that combines RHC services and “other ambulatory services” would be a<br />
clinic in which primary medical care is offered from 9 to 4 Monday through Thursday, and dental services<br />
are offered from 9 to 4 on Friday.<br />
23
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
B. Patient Care Policies Requirements. Review the clinic’s policies and ascertain who developed them.<br />
Where changes in clinic personnel and/or clinic administration make it impossible or not relevant to ascertain<br />
who developed the policies, it is necessary to ascertain that the current physician member(s) and<br />
the nurse practitioner, certifi ed nurse-midwife, and/or physician assistant member(s) of the staff have an<br />
indepth knowledge of the policies and have had the opportunity to discuss them, adopt them as is, or make<br />
any agreed-to written changes in them. If a clinic’s organizational structure includes a governing body,<br />
ascertain whether the governing body has ultimate authority in approving the patient care policies and, if<br />
so, when such approval was last given., While clinics frequently seek the participation of other health care<br />
professionals in developing patient care policies (particularly the written guidelines <strong>for</strong> the medical management<br />
of health problems) the term “a group of professional personnel” is not restricted to health care<br />
professionals. In some cases, the clinic will have involved health care professionals representatives to a<br />
hospital with which the clinic has an agreement <strong>for</strong> patient referral. In any event, one member of the group<br />
of three or more may not be a member of the clinic’s staff, and professions which are not directly related to<br />
health care delivery (attorneys, community planners, etc.) are potentially useful.<br />
C. Description of Services. A description of the services the clinic furnishes directly and those furnished<br />
through agreement or arrangement. The services furnished by the clinic should be described in a manner<br />
that in<strong>for</strong>ms potential patients of the types of health care available at the clinic, as well as setting the<br />
parameters of the scope of what services are furnished through referral. Such statements as the<br />
following suffi ciently-describe services: Taking complete medical histories, per<strong>for</strong>ming complete physical<br />
examinations, assessments of health status, routine lab tests, diagnosis and treatment <strong>for</strong> common acute<br />
and chronic health problems and medical conditions, immunization programs, family planning, complete<br />
dental care, emergency medical care. Statements such as “complete management of common acute and<br />
chronic health problems” standing alone, do not suffi ciently describe services.<br />
Additional services, furnished through referral, are suffi ciently described in such statements as: Arrangements<br />
have been made with X hospital <strong>for</strong> clinic patients to receive the following services if required: specialized<br />
diagnostic and laboratory testing, specialized therapy, inpatient hospital care, physician services, outpatient<br />
and emergency care when clinic is not operating, referral <strong>for</strong> medical cause when clinic is operating.<br />
2. Guidelines <strong>for</strong> Medical Management. The clinic’s written guidelines <strong>for</strong> the medical management of health<br />
problems include a description of the scope of medical acts which may be undertaken by the physician<br />
assistant, certifi ed nurse-midwife, and/or nurse practitioner. They represent an agreement between the<br />
physician providing the clinic’s medical direction and the clinic’s physician assistant, certifi ed nurse-midwife,<br />
and/or nurse practitioner on the privileges and limits of those acts of medical diagnosis and treatment which<br />
maybe undertaken without direct, over the shoulder physician supervision. They describe the regimens to<br />
be followed and stipulate the conditions in the illness or health care management at which consultation or<br />
referral is required.<br />
Acceptable guidelines may follow various <strong>for</strong>mats. Some guidelines are collections of general protocols,<br />
arranged by presenting symptoms; some are statements of medical directives arranged by the various<br />
systems of the body (such as disorders of the gastrointestinal system); some are standing orders covering<br />
major categories such as health maintenance, chronic health problems, common acute self-limiting health<br />
problems, and medical emergencies.<br />
The manner in which these guidelines describe the criteria <strong>for</strong> diagnosing and treating health conditions<br />
may also vary. Some guidelines will incorporate clinical assessment systems that include branching logic.<br />
Others may be in a more narrative <strong>for</strong>mat with major sections covering specifi c medical conditions in which<br />
such topics as the following are discussed: The defi nition of the condition, its etiology, its clinical features,<br />
recommended laboratory studies, differential diagnosis, treatment procedures, complications, consultationreferral<br />
required, and follow-up.<br />
24
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
Even though approaches to describing guidelines may vary, acceptable guidelines <strong>for</strong> the medical<br />
management of health problems must include the following essential elements. They:<br />
-- Are comprehensive enough to cover most health problems that patients usually see a physician<br />
about;<br />
-- Describe the medical procedures available to the nurse practitioner, certifi ed nurse-midwife,<br />
and/or physician assistant;<br />
-- Describe the medical conditions, signs, or developments that require consultation or referral;<br />
and<br />
-- Are compatible with applicable State laws.<br />
A number of patient care guidelines have been published by members of the medical profession. Should a<br />
clinic choose to adopt such guidelines (or adopt them essentially with noted modifi cations), this would be<br />
acceptable if the guidelines include the essential elements described above.<br />
3. Drugs and Biologicals. Written policies cover at least the following elements:<br />
-- Requirements dealing with the storage of drugs and biologicals in original manufacturer’s containers to<br />
assure that they maintain their proper labeling and packaging;<br />
-- Requirements dealing with outdated, deteriorated, or adulterated drugs and biologicals being stored q<br />
separately so that they are not mistakenly used in patient care prior to their disposal in<br />
compliance with applicable laws;<br />
-- Requirements dealing with storage in a space that provides proper humidity, temperature, and light to<br />
maintain the quality of drugs and biologicals;<br />
-- Requirements <strong>for</strong> a securely constructed locked compartment <strong>for</strong> storing drugs classifi ed under<br />
Schedule II of the Comprehensive Drug Abuse Prevention and Control Act of 1970;<br />
-- Requirements dealing with the maintenance of adequate records of receipt-and distribution of<br />
controlled drugs that account <strong>for</strong> all drugs in Schedules 11, 111, IV, and V; with Schedule II drugs<br />
being accounted <strong>for</strong> separately;<br />
-- Requirements that containers used to dispense drugs and biologicals to patients con<strong>for</strong>m to the Poison<br />
Prevention Packaging Act of 1970;<br />
-- Requirements dealing with the complete and legible labeling of containers used to dispense drugs and<br />
biologicals to patients;<br />
-- Requirements concerning the availability of current drug references and antidote in<strong>for</strong>mation; and<br />
-- Requirements dealing with prescribing and dispensing drugs in compliance with applicable State laws.<br />
4. Review of Policies. The group of professional personnel, which can be the governing body acting as the<br />
group, is responsible <strong>for</strong> an annual review of patient care policies.<br />
C. Direct services. The purpose of the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Services Act is primarily to make available<br />
outpatient or ambulatory care of the nature typically provided in a physician’s offi ce or outpatient clinic and<br />
the like. The regulations specify the services which must be made available by the clinic, including specifi ed<br />
types of diagnostic examination, laboratory services, and emergency treatments.<br />
The clinic’s laboratory is to be treated as a physician’s offi ce <strong>for</strong> the purpose of licensure and meeting health<br />
and safety standards. The listed laboratory services are considered essential <strong>for</strong> the immediate diagnosis<br />
and treatment of the patient. To the extent they can be provided under State and local law, the six services<br />
listed in J61, CMS-30, are considered the minimum the clinic should make available through use of its own<br />
resources.<br />
If any of these laboratory services cannot be provided at the clinic under State or local law, that laboratory<br />
service is not required <strong>for</strong> certifi cation. Some clinics are not able to furnish the six services, even though they<br />
may be allowed to do so under State and local law, without involving an arrangement with a Medicare<br />
25
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
approved laboratory.<br />
Those clinics unable to furnish all six services directly when allowed to by State and local law should be<br />
given defi ciencies. Such defi ciencies should not be considered suffi ciently signifi cant to warrant termination<br />
if the clinic has an agreement or arrangement with an approved laboratory to furnish the basic laboratory<br />
service it does not furnish directly, especially if the clinic is making an ef<strong>for</strong>t to meet this requirement.<br />
VII.PATIENT HEALTH RECORDS (42 CFR 491.10)<br />
A. Records System. The clinic is to maintain patient health records in accordance with its written policies<br />
and procedures. These records are the responsibility of a designated member of the clinic’s professional<br />
staff and should be maintained <strong>for</strong> each person receiving health care services. All records should be kept at<br />
the clinic site so that they are available when patients may need unscheduled medical care.<br />
Examine a randomly selected sample of health records to determine if appropriate in<strong>for</strong>mation, as related<br />
in J70 of the SRF and 42 CFR 491.10(a)(3), is included. This listing is the minimum requirement <strong>for</strong> record<br />
maintenance. If defi ciencies are found while reviewing the records, review additional records to determine<br />
the prevalence of these defi ciencies. Record on the SRF the number of records reviewed and defi ciencies<br />
found, if any, and as questions arise concerning the records, discuss them with the person responsible <strong>for</strong><br />
record maintenance.<br />
B. Protection of Record In<strong>for</strong>mation.--The clinic must ensure the confi dentiality of the patient’s health records<br />
and provide safeguards against loss, destruction or unauthorized use of record in<strong>for</strong>mation. Ascertain that<br />
in<strong>for</strong>mation regarding the use and removal of records from the clinic and the conditions <strong>for</strong> release of record<br />
in<strong>for</strong>mation is in the clinic’s written policies and procedures. The patient’s written consent is necessary<br />
be<strong>for</strong>e any in<strong>for</strong>mation not authorized by law may be released.<br />
C. Retention of Records. Review the clinic policy pertaining to the retention of patient health records. This<br />
policy refl ects the necessity of retaining records at least 6 years from the last entry date or longer if required<br />
by State statute.<br />
VIII. PROGRAM EVALUATION (42 CFR 491.11)<br />
An evaluation of a clinic’s total operation including the overall organization, administration, policies and<br />
procedures covering personnel, fi scal and patient care areas must be done at least annually. This evaluation<br />
may be done by the clinic, the group of professional personnel required under 42 CFR 491.9(b)(2), or<br />
through arrangement with other appropriate professionals. The surveyor clarifi es <strong>for</strong> the clinic that the State<br />
survey does not constitute any part of this program evaluation.<br />
The total evaluation does not have to be done all at once or by the same individuals. It is acceptable to<br />
do parts of it throughout the year, and it is not necessary to have all parts of the evaluation done by the<br />
same personnel. However, if the evaluation is not done all at once, no more than a year should elapse<br />
between evaluating the same parts. For example, a clinic may have its organization, administration, and<br />
personnel and fi scal policies evaluated by a health care administrator(s) at the end of each fi scal year; and<br />
its utilization of clinic services, clinic records, and health care policies evaluated 6 months later by a group<br />
of health care professionals.<br />
If the facility has been in operation <strong>for</strong> at least a year at the time of the initial survey and has not had an<br />
evaluation of its total program, report this as a defi ciency. It is incorrect to consider this requirement as not<br />
applicable (N/A) in this case.<br />
A facility operating less than a year or in the start-up phase may not have done a program evaluation.<br />
However, the clinic should have a written plan that specifi es who is to do the evaluation, when and how it is<br />
to be done, and what will be covered in the evaluation. What will be covered should be consistent with the<br />
26
B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (con’t)<br />
requirements of 42 CFR 491.11. Record this in<strong>for</strong>mation under the explanatory statements on the SRF.<br />
Review dated reports of recent program evaluations to verify that such items are included in these<br />
evaluations. When corrective action has been recommended to the clinic, verify that such action has been<br />
taken or that there is sufficient evidence indicating the clinic has initiated corrective action.<br />
27
C. See Addendum: Regulatory Guide:<br />
RHC/FQHC Proposed Rule<br />
28
D. Preparing <strong>for</strong> the Certification Inspection<br />
This section will help your clinic prepare <strong>for</strong> the certification inspection. In <strong>Arizona</strong>, the <strong>Arizona</strong><br />
Department of <strong>Health</strong> Services, Division of Licensing Services, Office of Medical Facilities Licensing<br />
is the state agency that conducts the inspection. The four key elements to preparing <strong>for</strong> the<br />
RHC Certification inspection are: 1) Policy and Procedure <strong>Manual</strong> Review, 2) Medical Records<br />
Review, 3) Facility Inspection, and 4) Program Evaluation.<br />
The following is an excerpt from Starting a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> - A How-To <strong>Manual</strong>, published by<br />
the U.S. Department of <strong>Health</strong> and Human Services, <strong>Health</strong> Resources and Services Administration,<br />
Office of <strong>Rural</strong> <strong>Health</strong> Policy. The complete manual is available online at: http://ruralhealth.<br />
hrsa.gov/RHC/RHCmanual.htm. The <strong>for</strong>m used by the surveyor during the inspection can be<br />
referenced in Appendix G. <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Survey Report.<br />
The RHC Policy and Procedure <strong>Manual</strong><br />
The policy and procedure manual should cover key human resource policies, administrative policies,<br />
clinical procedures and protocols, and medical guidelines per RHC Code of Federal Regulations (CFR)<br />
§491.7(a)(2) [available online at: http://www.access.gpo.gov/nara/cfr/waisidx_02/42cfr491_02.html]. Each<br />
clinic’s policy and procedures manual should be drafted with that clinic in mind. This document should be<br />
an accurate refl ection of how the clinic truly intends to operate.<br />
The Policy and Procedures <strong>Manual</strong> section of the RHC Interpretive Guidelines states, “Written policies<br />
should consist of both administrative and patient care policies. Patient care policies are discussed under<br />
42 CFR 491.9(b). In addition to including lines of authority and responsibilities, administrative policies may<br />
cover topics such as personnel, fi scal, purchasing, and maintenance of building and equipment. Topics<br />
covered by written policies may have been infl uenced by requirements of the founders of the clinic, as well<br />
as agencies that have participated in supporting the clinic’s operation.”<br />
When looking at developing human resource policies there are several laws, administrative rules, acts, and<br />
regulations that must be considered: RHC Code of Federal Regulations [available online at: http://www.<br />
access.gpo.gov/nara/cfr/waisidx_02/42cfr491_02.html], RHC Interpretative Guidelines [see section II.B.<br />
Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s], State and Federal Laws, State Public <strong>Health</strong> Code, and<br />
Professional Practice Standards.<br />
The Human Resource policies should include:<br />
• job descriptions<br />
• benefits, compensation and pay practice<br />
• employment criteria and conditions of employment<br />
• smoking, drug use/possession and distribution<br />
• appointment of providers/credentialing<br />
• confidentiality<br />
• personnel fi les (organization, management, and access)<br />
• harassment, and employee privacy<br />
The Code of Federal Regulations <strong>for</strong> the RHC program and the RHC Interpretive Guidelines [see the following<br />
website <strong>for</strong> the Code of Federal Regulations: http://www.access.gpo.gov/nara/cfr/waisidx_02/42cfr491_<br />
02.html; see section II.B. Interpretive Guidelines <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s) are often the best place to start<br />
when developing RHC policies. CFR Section 491.8 Staffi ng and staff responsibilities, outlines some of the<br />
program requirements <strong>for</strong> physician assistants, nurse practitioners and certifi ed nurse midwives. The<br />
29
D. Preparing <strong>for</strong> the Certification Inspection (con’t)<br />
regulations state that, “A nurse practitioner or a physician assistant is available to furnish patient care<br />
services at least 50 percent of the time the clinic operates.” When developing the job description of the<br />
PA/NP/CNM, part of their responsibilities should include the following: “The PA/NP/CNM will be scheduled<br />
in the clinic and available to provide patient care services <strong>for</strong> at least 50 percent of the time the clinic<br />
operates.”<br />
As you develop your Administrative section, you will want to consider the following resources: RHC Code<br />
of Federal Regulations and Interpretative Guidelines, State and Federal Laws, State Court Rules, Federal<br />
and State OSHA Standards, Medicare and Medicaid reimbursement policy, State Public <strong>Health</strong> Code, Administrative<br />
rules, and the Freedom of In<strong>for</strong>mation Act.<br />
Administrative policies should include:<br />
• Life safety<br />
• Confidentiality<br />
• Exposure control plan<br />
• Hazardous materials<br />
• <strong>Health</strong> services<br />
• In<strong>for</strong>med consent<br />
• Medical records (storage, release of in<strong>for</strong>mation, documentation standards)<br />
• Reporting of suspected child neglect/abuse and abandonment<br />
• TB screening <strong>for</strong> health care workers<br />
• Medical waste management<br />
• Organizational structure<br />
• Personal accident/incident<br />
• Physical plant and environment<br />
• Patient compliant-grievance procedure<br />
• Per<strong>for</strong>mance improvement plan<br />
• Preventative maintenance<br />
• Patient rights and responsibilities<br />
• Quality assurance<br />
• Medicare bad debt<br />
• Cleaning<br />
When developing your Administrative section, the best place to start is with the Code of Federal Regulations<br />
(CFR). An example of an Administrative policy would be Preventive Maintenance. CFR Section 491.6(b)<br />
States, “The clinic has a preventive maintenance program to ensure that: (1) All essential mechanical, electrical<br />
and patient care equipment is maintained in safe operating condition.” The RHC Interpretive Guideline<br />
<strong>for</strong> this regulation defi nes the requirement further, “A program of preventive maintenance should be followed<br />
by the clinic. This includes inspection of all clinic equipment at least yearly, or as the type, use, and<br />
condition of equipment dictates.” By using these two resources the preventive maintenance policy could<br />
contain the following statements:<br />
1. All <strong>Clinic</strong> equipment will be inspected at least yearly, or as the type, use, and condition of equipment<br />
dictates. Each time an inspection or repair occurs, an entry will be made in the Inspection and Maintenance<br />
Log and signed by the service person to verify the event.<br />
2. The medical/clinical assistant prior to each use must inspect all equipment.<br />
3. An electrician or bio-medical engineer will inspect each piece of bio-medical equipment. The inspection<br />
will ensure that the equipment is in proper operating condition, is safe to use, and is calibrated properly.<br />
30
D. Preparing <strong>for</strong> the Certification Inspection (con’t)<br />
When developing clinical procedures/protocols, it is helpful to keep in mind that this section refers to those<br />
procedures that are per<strong>for</strong>med by support personnel, e.g., nurse, certifi ed medical assistant, registered radiologic<br />
technologist, clinical assistant, etc. Resources that you would want to consider as you develop this<br />
section are: RHC Regulations and Interpretive Guidelines, manufacturer recommendations, professional<br />
practice standards, pharmacy regulations and administrative rules, American Heart Association, Federal<br />
and State OSHA standards, CLIA [<strong>Clinic</strong>al Laboratory Improvement Amendments] regulations, CDC [<strong>Center</strong>s<br />
<strong>for</strong> Disease Control and Prevention], State Public <strong>Health</strong> Code, American Academy of Pediatrics, and<br />
PHS Standards <strong>for</strong> Pediatric Immunization Practices.<br />
<strong>Clinic</strong>al policies should include:<br />
• Administration of Sub-Q, IM, or IV Medications<br />
• Policies <strong>for</strong> all invasive procedures per<strong>for</strong>med<br />
• Vaccine administration, handling and storage<br />
• Procedures <strong>for</strong> the operation of all medical equipment<br />
• Medications (stock and sample)<br />
• Laboratory services<br />
• Communicable disease care<br />
• HIV testing<br />
• Universal Precautions<br />
• Diagnostic tracking<br />
• Adverse drug reactions<br />
• Policies that address the testing and quality control of all lab/diagnostic test(s) per<strong>for</strong>med<br />
• Storage of sterile supplies, sterilization of sterile supplies and instruments<br />
As with the Human Resources and Administrative sections, the fi rst resources to consider are the Code of<br />
Federal Regulations and the Interpretive Guidelines. Using the Code you can easily start to put together<br />
your clinical procedures/protocol section. For example, CFR Section 491.6(b)(2) states, “The clinic has a<br />
preventive maintenance program to ensure that drugs and biologicals are appropriately stored.” Based on<br />
this regulation, the medication policy could contain the following Statements (among others):<br />
1. Medications will be refrigerated as necessary and will be kept separate from any food substances. Refrigerator<br />
and freezer temperatures will be obtained and recorded on a daily basis.<br />
2. On a monthly basis, medications will be checked <strong>for</strong> expiration dates and those which are outdated will<br />
be discarded in the following manner: Given back to drug representative or discarded via the biohazard<br />
container. A log will be maintained to indicate when monthly checks are done and by whom.<br />
3. All medications stored on the <strong>Clinic</strong> premises will be kept in cabinets, shelves, drawers, and/or refrigerators<br />
and locked during non-patient care hours.<br />
Finally, the RHC program requires that the clinic have guidelines <strong>for</strong> the medical management of health<br />
problems which include the conditions requiring medical consultation and/or patient referral, the maintenance<br />
of health care records, and procedures <strong>for</strong> the periodic review and evaluation of the services furnished<br />
by the clinic. Acceptable guidelines may follow various <strong>for</strong>mats.<br />
Some guidelines are collections of general protocols, arranged by presenting symptoms; some are Statements<br />
of medical directives arranged by the various systems of the body (such as disorders of the gastrointestinal<br />
system); some are standing orders covering major categories such as health maintenance, chronic<br />
health problems, common acute self-limiting health problems, and medical emergencies.<br />
31
D. Preparing <strong>for</strong> the Certification Inspection (con’t)<br />
Even though approaches to describing guidelines may vary, acceptable guidelines <strong>for</strong> the medical management<br />
of health problems must include the following essential elements:<br />
• They are comprehensive enough to cover most health problems that patients usually see a physician<br />
about;<br />
• They describe the medical procedures available to the nurse practitioner, certifi ed nurse-midwife,<br />
and/or physician assistant; and<br />
• They are compatible with applicable State laws.<br />
The professional organizations of the health professionals typically found in an RHC (physician, PA, NP and<br />
CNM) have published a number of patient care guidelines. Should a clinic choose to adopt such guidelines<br />
(or adopt them essentially with noted modifi cations), this would be acceptable if the guidelines include the<br />
a<strong>for</strong>ementioned essential elements.<br />
Often the regulations will over lap and you need to be aware of the areas where this occurs. Policy and<br />
procedure development is one area. The physician and PA, NP or CNM responsibilities include participation<br />
in developing, executing, and periodic reviewing of the clinic’s written policies. Additionally, the policies are<br />
developed with the advice of a group of professional personnel that includes one or more physicians and<br />
one or more physician assistants or nurse practitioners. At least one member of the advisory group must<br />
not be a member of the clinic staff.<br />
Medical Records<br />
The RHC program has been recognized <strong>for</strong> its emphasis on documented patient care. This is the direct result<br />
of the requirements and expectations clearly stated in the Code of Federal Regulations. The clinic has<br />
written policies and procedures of how it will maintain confi dentiality of patient health records and provide<br />
a safeguard against: loss, destruction, or unauthorized use of patients’ health record. CFR Section 491.10<br />
Patient health records of the Code, outlines expectations <strong>for</strong> medical record confi dentiality, maintenance,<br />
organization, content, protection, release and retention. As part of the Certifi cation Survey process, a representative<br />
sample of the clinic’s medical records will be reviewed. The focus should be on Medicare and<br />
Medicaid records only. The clinic may have the opportunity to select the records <strong>for</strong> review. If not, it will be<br />
the surveyor who determines the records to be reviewed.<br />
Documentation must include but is not limited to:<br />
• Identification and social data, evidence of consent <strong>for</strong>ms, pertinent medical history, assessment<br />
of the health status and health care needs of the patient, and a brief summary of the episode,<br />
disposition and instructions to the patient;<br />
• Reports of physical examinations, diagnostic and laboratory test results and consultative fi ndings;<br />
• All provider orders, reports of treatments and medications and other pertinent in<strong>for</strong>mation necessary<br />
to monitor the patient’s progress; and<br />
• Signatures of the provider and other health care professionals.<br />
In addition to these program expectations, the clinic must also comply with reimbursement policy, legal expectations,<br />
and standard of practice guidelines. Remember, if it wasn’t documented, it wasn’t done.<br />
Facility<br />
Preparing the facility is not only a requirement of the RHC program but may also be a requirement <strong>for</strong> compliance<br />
with local, State and Federal laws. An inspection of the physical plant is one of the key elements of<br />
the survey process. Some of the regulations, laws, rules, and standards that impact the facility are: RHC<br />
32
D. Preparing <strong>for</strong> the Certification Inspection (con’t)<br />
Code of Federal Regulations, Clean Indoor Air Act, OSHA Hazardous Communication Standard, local<br />
building, zoning and, fi re ordinances, and State laws <strong>for</strong> storage and disposal of medical waste.<br />
To insure the safety of patients, personnel, and the public, the physical plant should be maintained consistent<br />
with appropriate State and local building, fi re, and safety codes. Reports prepared by State and local<br />
personnel responsible <strong>for</strong> insuring that the appropriate codes are met should be available <strong>for</strong> review. The<br />
facility must have safe access and be free from hazards that may affect the safety of patients, personnel,<br />
and the public. The clinic must also be constructed, arranged, and maintained to insure access to and<br />
safety of patients, and provide adequate space <strong>for</strong> the provision of direct services. The clinic must provide<br />
laboratory services directly to its patients. Each clinic must have, at a minimum, its own CLIA certifi cate of<br />
waiver. Provider-based RHCs may not use the CLIA certifi cate of the parent hospital. The clinic must have a<br />
preventive maintenance program to ensure that all essential mechanical, electrical, and patient-care equipment<br />
is maintained in safe operating condition. The clinic must make provisions <strong>for</strong> the appropriate storage<br />
of drugs and biologicals and the premises must be clean and orderly. The clinic is responsible <strong>for</strong> assuring<br />
the safety of patients in case of non-medical emergencies that include, placing exit signs in appropriate<br />
locations and taking other appropriate measures that are consistent with the particular conditions of the<br />
area in which the clinic is located.<br />
Program Evaluation<br />
An evaluation of the clinic’s total operation including the overall organization, administration, policies and<br />
procedures covering personnel, fi scal and patient care areas must be done at least annually. This evaluation<br />
may be done by the clinic; an outside group of professional personnel that includes one or more physicians<br />
and one or more physician assistants or nurse practitioners and at least one individual who is not part<br />
of the clinic staff; or through arrangement with other appropriate professionals. The State survey does not<br />
constitute any part of this program evaluation.<br />
The total evaluation does not have to be done all at once or by the same individuals. It is acceptable to<br />
do parts of it throughout the year, and it is not necessary to have all parts of the evaluation done by the<br />
same staff person. However, if the evaluation is not done all at once, no more than one year should elapse<br />
between evaluating the same parts. For example, a clinic may have its organization, administration, and<br />
personnel and fi scal policies evaluated by a health care administrator(s) at the end of the fi scal year; and<br />
its utilization of clinic services, clinic records, and health care policies evaluated six months later by a group<br />
of health care professionals.<br />
If the facility has been operational <strong>for</strong> at least a year at the time of the survey and has not completed an<br />
evaluation of its total program, the surveyor must report this as a defi ciency. If the facility has been operational<br />
<strong>for</strong> less than one year or is in the start-up phase, it is not required to complete a program evaluation.<br />
However, the clinic should have a written plan that specifi es who is to do the evaluation, when it is to be<br />
done, how it is to be done, and what will be covered in the evaluation.<br />
The evaluation must include a review of the following:<br />
• Utilization of clinic services (including at least the number of patients served and the volume of<br />
services)<br />
• A representative sample of both active and closed clinical records, and<br />
• The clinic’s health care policies<br />
The purpose of the evaluation is to determine whether: the utilization of services was appropriate; the established<br />
policies were followed; and whether any changes are needed.<br />
33
D. Preparing <strong>for</strong> the Certification Inspection (con’t)<br />
The clinic staff or a group of professional personnel must consider the fi ndings of the evaluation and take<br />
corrective action if necessary. The Balanced Budget Act of 1997 requires RHCs to have a clinical quality<br />
assurance plan. However as of the writing of this manual, CMS had not published the rules outlining how<br />
RHCs can meet this requirement. Many State surveyors expect to see such a plan in the policy and procedures<br />
manual.<br />
Once the clinic submits its Letter of Readiness to the State agency, the State agency has 90 days in which<br />
to schedule the RHC Certifi cation Survey. Some clinics may experience a delay in the process depending<br />
on national initiatives and budget constraints.<br />
The State agency does have the option, under certain conditions, of giving clinics a 48-hour notice of the<br />
scheduled survey. Some States, however, will not exercise this option and the survey will be unannounced.<br />
To ensure a successful survey, have a plan and prepare ahead. [In <strong>Arizona</strong>, the <strong>Arizona</strong> Department<br />
of <strong>Health</strong> Services, Division of Licensing Services, Offi ce of Medical Facilities Licensing conducts unannounced<br />
survey visits <strong>for</strong> the Medicare <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> certifi cation inspection].<br />
The following documents should be prepared and available to the surveyor.<br />
Policy and Procedure <strong>Manual</strong>:<br />
• All Professional Group, Staff, and Provider mtg. minutes<br />
• Fire and Evacuation Training logs CLIA Certifi cate<br />
• Exposure Control and Blood borne Pathogen Training<br />
• Personnel Files<br />
• X-ray Certifi cate (if applicable)<br />
• Sample Drug Log<br />
MSDS <strong>Manual</strong>:<br />
• Minimum of 10 medical records (Medicare/Medicaid only) – mix of all life cycles and providers<br />
• CLIA Certifi cate<br />
• Quality Assurance and Per<strong>for</strong>mance Improvement Activity<br />
• Preventative Maintenance Reports<br />
• Laboratory Control Logs<br />
• Diagnostic Results Tracking System<br />
When the Certifi cation Survey results in no defi ciencies, the State agency has ten (10) calendar days to<br />
prepare the Survey Packet <strong>for</strong> the CMS Regional Offi ce (RO) with a recommendation of approval. The RO<br />
has 60 days to review and approve the survey packet and issue the Medicare Provider Letter to the clinic.<br />
For those clinics that fi le their application as a Provider-based entity, the provider-based request must be<br />
submitted to the RO with the survey packet. The RO will make the Provider-based determination and will<br />
notify the appropriate Fiscal Intermediary via the Medicare Tie-In Notice.<br />
Should the survey result in defi ciencies or citations, a Statement of Defi ciencies will be sent to the clinic by<br />
the State agency within ten (10) days of the survey. The clinic will have 10 days to develop a Plan of Correction<br />
(POC) and submit the POC back to the State agency. An initial applicant to the Medicare program<br />
cannot be certifi ed or approved unless they are in compliance with the Conditions <strong>for</strong> Coverage. If in the<br />
judgement of the surveyor, the defi ciencies evince non-compliance at the Condition level, then the applicant<br />
cannot be approved until those defi ciencies have been corrected and the corrections have been verifi ed<br />
through a follow-up survey. If there are defi ciencies but they do not constitute non-compliance at the condition<br />
level, then the facility can be approved <strong>for</strong> participation with an approved plan of correction in place. A<br />
sample “Plan of Correction with Defi ciencies” appears at the end of this chapter. The State agency will then<br />
review the POC <strong>for</strong> completeness.<br />
34
D. Preparing <strong>for</strong> the Certification Inspection (con’t)<br />
Key elements to a POC include: it must be doable or realistic, it must have completion dates, it must specifi<br />
cally address the citation, and if appropriate, the clinic must be able to document proof of compliance.<br />
There are no time constraints placed on the State agency when reviewing a POC. Once the State agency<br />
has found the POC to be acceptable, they will submit the survey packet with recommendations to the RO.<br />
The RO has 60 days to review and approve the survey packet and issue the Medicare Provider Letter to<br />
the clinic. For those clinics that fi le their application as a Provider-based entity, the provider-based request<br />
must be submitted to the RO with the survey packet. The RO will make the Provider-based determination<br />
and will notify the Fiscal Intermediary via the Medicare Tie-In Notice.<br />
Once the Medicare Provider Letter has been received by the clinic, the clinic is eligible to fi le a projected<br />
cost report and have their Medicare Rate determined.<br />
Source: U.S. Department of <strong>Health</strong> and Human Services, <strong>Health</strong> Resources and Services Administration, Office of<br />
<strong>Rural</strong> <strong>Health</strong> Policy, Starting a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>: A How-To <strong>Manual</strong>, http://ruralhealth.hrsa.gov/RHC/RHCmanual.htm.<br />
35
30 Most Common RHC Survey/Certification Deficiencies<br />
Surveyor Code CFR Section Summary of Requirement<br />
J20<br />
491.6(a)<br />
The clinic is constructed, arranged, and maintained to ensure<br />
access to and safety of patients, and provides adequate space<br />
<strong>for</strong> the provision of direct services.<br />
J22<br />
491.6(b)(1)<br />
The clinic has a preventive maintenance program to ensure<br />
that all essential mechanical, electrical and patient-care<br />
equipment is maintained in safe operating condition.<br />
J23<br />
491.6(b)(2)<br />
The clinic has a preventive maintenance program to ensure<br />
that drugs and biologicals are appropriately stored.<br />
J24<br />
491.6(b)(3)<br />
The clinic has a preventive maintenance program to ensure<br />
that the premises are clean and orderly.<br />
J26<br />
491.6(c)(1)<br />
The clinic assures the safety of patients in case of non-medical<br />
emergencies by training staff in handling emergencies.<br />
J28<br />
491.6(c)(3)<br />
The clinic assures the safety of patients in case of non-medical<br />
emergencies by taking other appropriate measures that are<br />
consistent with the particular conditions of the area in which<br />
the clinic is located.<br />
J32<br />
491.7(a)(2)<br />
The organization's policies and it's lines of authority and<br />
responsibilities are clearly set <strong>for</strong>th in writing.<br />
J41<br />
491.8(a)(6)<br />
A physician, nurse practitioner, or physician's assistant is<br />
available to furnish patient care services at all times during the<br />
clinic's regular hours of operation. A nurse practitioner or a<br />
physician's assistant is available to furnish patient care<br />
services during at least 50 percent of the clinic's regular hours<br />
of operation.<br />
J47<br />
491.8(b)(2)<br />
Physician responsibilities: In conjunction with the physician<br />
assistant and/or nurse practitioner member(s), the physician<br />
participates in developing, executing and periodically<br />
reviewing the clinic's written policies and the services provided<br />
to Federal program patients.<br />
J48<br />
491.8(b)(3)<br />
Physician responsibilities: The physician periodically reviews<br />
the clinic's patient records, provides medical orders, and<br />
provides medical care services to the patients of the clinic.<br />
Physician assistant and the nurse practitioner responsibilities.<br />
The physician assistant and the nurse practitioner members of<br />
the clinic's staff:<br />
J51<br />
491.8(c)<br />
I. Participate in the development, execution and periodic<br />
review of the written policies governing the services<br />
the clinic furnishes;<br />
II. Provide services in accordance with those policies;<br />
III. Arrange <strong>for</strong>, or refer patients to, needed services that<br />
cannot be provided at the clinic;<br />
IV. Assure that adequate patient health records are<br />
maintained and transferred as required when patients<br />
are referred; and<br />
V. Participate with a physician in a periodic review of the<br />
patient's health records.<br />
36
30 Most Common RHC Survey/Certification Deficiencies (Con’t)<br />
J55<br />
J56<br />
J57<br />
J58<br />
491.9(b)(1)<br />
491.9(b)(2)<br />
491.9(b)(3)(iii)<br />
491.9(b)(4)<br />
The clinic's health care services are furnished in accordance<br />
with appropriate written policies, which are consistent with<br />
applicable State law.<br />
The patient care policies are developed with the advice of a<br />
group of professional personnel that includes one or more<br />
physicians and one or more physician's assistants or nurse<br />
practitioners. At least one member of the group is not a<br />
member of the clinic's staff.<br />
The policies include guidelines <strong>for</strong> the medical management<br />
of health problems, which include the conditions requiring<br />
medical consultation and/or patient referral, the maintenance<br />
of health care records, and procedures <strong>for</strong> the periodic review<br />
and evaluation of the services furnished by the clinic.<br />
These policies are reviewed at least annually by the group of<br />
professional personnel as required under 491.9(b)(2), and<br />
reviewed as necessary by the clinic.<br />
The clinic provides basic laboratory services essential to the<br />
immediate diagnosis and treatment of the patient, including:<br />
J61<br />
491.9(c)(2)<br />
1. Chemical examinations of urine by stick or tablet<br />
methods or both (including urine ketones);<br />
2. Hemoglobin or hematocrit;<br />
3. Blood sugar;<br />
4. Examination of stool specimens <strong>for</strong> occult blood;<br />
5. Pregnancy tests; and<br />
6. Primary culturing <strong>for</strong> transmittal to a certified<br />
laboratory.<br />
J62 491.9(3)<br />
The clinic provides medical emergency procedures as a first<br />
response to common life-threatening injuries and acute<br />
illness, and has available the drugs and biologicals commonly<br />
used in life saving procedures, such as analgesics,<br />
anesthetics (local), antibiotics, anticonvulsants, antidotes and<br />
emetics, serums and toxoids.<br />
37
30 Most Common RHC Survey/Certification Deficiencies (Con’t)<br />
For each patient receiving health care services, the clinic<br />
maintains a record that includes, as applicable:<br />
J70<br />
491.10(a)(3)<br />
1. Identification and social data, evidence of consent<br />
<strong>for</strong>ms, pertinent medical history, assessment of the<br />
health status and health care needs of the patient,<br />
and brief summary of the episode, disposition, and<br />
instructions to the patient;<br />
2. Reports of physical examinations, diagnostic and<br />
laboratory test results, and consultative findings;<br />
3. All physician's orders, reports of treatments and<br />
medications and other pertinent in<strong>for</strong>mation<br />
necessary to monitor the patient's progress;<br />
4. Signatures of the provider or other health care<br />
professional.<br />
J72<br />
491.10(b)(1)<br />
The clinic maintains the confidentiality of record in<strong>for</strong>mation<br />
and provides safeguards against loss, destruction, or<br />
unauthorized use.<br />
J76 491.11 Program evaluation<br />
J77<br />
491.11(a)<br />
The clinic carries out, or arranges <strong>for</strong>, an annual evaluation of<br />
its total program.<br />
J78 491.11(b) Reviews included in evaluation<br />
J79<br />
491.11(b)(1)<br />
The evaluation includes review of the utilization of clinic<br />
services, including at least the number of patients served and<br />
the volume of services.<br />
J80<br />
491.11(b)(2)<br />
The evaluation includes review of a representative sample of<br />
both active and closed clinical records.<br />
J81<br />
491.11(b)(3)<br />
The evaluation includes review of the clinic's health care<br />
policies.<br />
J82 491.11(c) Purpose of the evaluation<br />
J83<br />
491.11(c)(1)<br />
The purpose of the evaluation is to determine whether the<br />
utilization of services was appropriate.<br />
J84<br />
491.11(c)(2)<br />
The purpose of the evaluation is to determine whether the<br />
established policies were followed.<br />
J85<br />
491.11(c)(3)<br />
The purpose of the evaluation is to determine whether any<br />
changes are needed.<br />
J86<br />
491.11(d)<br />
The clinic staff considers the findings of the evaluation and<br />
takes corrective action if necessary.<br />
38
F. RHC Cost Report<br />
The Medicare cost report is a required <strong>for</strong>m that is completed annually by all <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s.<br />
Independent RHCs must complete the CMS 222-92 <strong>for</strong>m and provider-based RHCs are required<br />
to complete Worksheet M of <strong>for</strong>m CMS 2552-96.<br />
The following is an excerpt from the U.S. Department of <strong>Health</strong> and Human Services, <strong>Health</strong> Resources<br />
and Services Administration, Office of <strong>Rural</strong> <strong>Health</strong> Policy’s Starting a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong><br />
- A How-To <strong>Manual</strong> (Available online at: http://ruralhealth.hrsa.gov/RHC/RHCmanual.htm):<br />
This chapter will discuss the rural health clinic cost report, the process <strong>for</strong> fi ling the cost report, and an example<br />
of a completed cost report. It is intended to provide you with an overall summary of the cost reporting<br />
process. By also providing you with defi nitions of terms and a sample of a cost report, we hope to give you<br />
a better understanding of how the process works.<br />
We cannot emphasize enough the importance of getting expert advice. Expert advice should be from individuals<br />
with experience with cost reports and specifi cally with the CMS-222 (or Schedule M) Cost Report,<br />
as it relates to issues such as calculation of FTE, reassignment of costs, and the completion of an independent<br />
or provider-based RHC Cost Report.<br />
While it is possible <strong>for</strong> individual practices without signifi cant experience to complete the cost report, in<br />
many instances there are multiple errors that occur and this is often to the fi nancial detriment of the clinic.<br />
In addition, it is important to acknowledge that the accuracy of the data provided can have a signifi cant<br />
fi nancial impact on the year-end cost report. We, there<strong>for</strong>e, recommend getting appropriate expert advice<br />
when attempting to complete a Medicare Cost Report.<br />
Form 222, the Medicare RHC cost report, (schedule M of the hospital, nursing home or home health cost<br />
report), is a required <strong>for</strong>m that is completed on an annual basis by all rural health clinics.<br />
The cost report is a statement of costs and provider utilization that occurred during the time period covered<br />
by the cost report. The cost report is the means by which Medicare determines how much money is due to<br />
the provider, or due back from the provider, <strong>for</strong> RHC services rendered to Medicare benefi ciaries during the<br />
cost reporting period. The cost report typically covers a twelve (12) month period of time and is due fi ve (5)<br />
months from the date of the end of the fiscal year of the RHC.<br />
There are exceptions to the twelve (12) month period covered by a cost report. The exceptions would be<br />
due to the sale of the RHC or a change in ownership of the RHC during the twelve (12) month period; leaving<br />
a shorter time period than twelve (12) months that would be covered by the cost report. If a clinic experiences<br />
a change of ownership or decides to discontinue operation as an RHC, a cost report is due 150 days<br />
from the date of ownership change or RHC termination.<br />
On July 26, 2002, the <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid Services (CMS) published a proposed rule that,<br />
if adopted, would have required electronic submission of all RHC cost reports <strong>for</strong> cost reporting periods<br />
ending after December 31, 2002. As of the publication of this book, that rule has not be fi nalized. The proposed<br />
rule indicated that exceptions would be available <strong>for</strong> providers who can demonstrate that electronic<br />
submission would represent a hardship. However, no details of the exception process were provided. The<br />
authors anticipate the proposed rule will be fi nalized and electronic submission of RHC costs reports will<br />
be mandatory at some point.<br />
The maximum time period that can be covered by a fi led cost report is thirteen (13) months. There are no<br />
extensions to file cost reports except under special circumstances, such as a natural disaster (i.e. fl ood,<br />
earthquake, fi re, etc.). The Fiscal Intermediary generally will grant this type of extension. [A listing of the F.<br />
39
F. RHC Cost Report (con’t)<br />
Fiscal Intermediaries <strong>for</strong> the independent RHCs is available online at: http://www.cms.hhs.gov/apps/contacts/incardir.asp].<br />
As has been previously noted, there are two types of RHC’s - Independent and Provider-based. Each must<br />
fi le a cost report, but the cost report is different <strong>for</strong> each of the two types of RHC’s.<br />
All <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s are presumed to be independent unless the clinic requests designation as a provider-based<br />
facility. Whereas, an independent RHC can be owned by any type of entity authorized under<br />
State law to own a medical practice: physicians; physician assistants; nurse practitioners; certifi ed nurse<br />
midwives; hospitals; skilled nursing facilities; home health agencies; <strong>for</strong>-profi t corporations; not-<strong>for</strong>-profi t<br />
corporations; or government entities; only those entities recognized by Medicare as a “provider” can own<br />
a provider-based RHC. Entities designated by Medicare as providers are: hospitals, skilled nursing facilities,<br />
and home health agencies. Although this chapter will focus on the fi ling of an independent RHC cost<br />
report, the provider-based RHC cost report is very similar. A provider-based cost report is fi led as a part of<br />
the sponsoring provider’s cost report. It is prepared on Schedule M.<br />
The following list includes the title and explanation of each worksheet contained in the RHC cost report:<br />
•Worksheet S<br />
This is the statistical data and certifi cation statement (requires original signature when submitted). The<br />
statistical data includes in<strong>for</strong>mation such as: whether the cost report is based on actual or projected cost,<br />
time period covered, provider name, Medicare number, location, provider numbers of physicians/PAs/NPs/<br />
CNMs, operational control, hours of operation, etc.<br />
•Worksheet A, Columns 1 & 2<br />
Worksheet A is used to record the trial balance of expense accounts from the provider books and records<br />
<strong>for</strong> the cost reporting period stated. The total dollar amount of Column 1 and 2 should tie to the records of<br />
the provider <strong>for</strong> total expenses. (Column 1 is <strong>for</strong> compensation amounts, while column 2 reports amounts<br />
other than compensation). Column 3 is the total of Column 1 & 2. This worksheet also provides <strong>for</strong> the necessary<br />
reclassifi cations (Column 4) and adjustments (Column 6) to certain accounts.<br />
•Worksheet A-1, Column 4<br />
This worksheet provides <strong>for</strong> reclassifi cation of any amounts in order to refl ect the proper cost allocation in<br />
a given cost center. This worksheet “moves” certain amounts from one cost center to another cost center.<br />
Supporting documentation is needed <strong>for</strong> each reclassifi cation made on this worksheet.<br />
•Worksheet A-2, Column 6<br />
This worksheet provides <strong>for</strong> adjustments, which are necessary under the Medicare principles of reimbursement.<br />
Types of items to be entered on this Worksheet are 1) those needed to adjust expenses incurred {accrual<br />
accounting} 2) those that represent recovery of expenses through refunds, sales, etc. 3) those needed<br />
to adjust expenses that are non-allowable <strong>for</strong> Medicare purposes 4) those needed to adjust expenses in<br />
accordance with offsets from “other/miscellaneous” income received. Supporting documentation is needed<br />
<strong>for</strong> each adjustment made on this worksheet.<br />
•Worksheet A-2-1, Column 6, Flows thru Worksheet A-1<br />
This worksheet fl ows into the above worksheet A-2 at the net amount of the total adjustment. It provides<br />
<strong>for</strong> in<strong>for</strong>mation and amounts on related parties of the organization including costs applicable to services,<br />
facilities, and supplies furnished to providers by a related organization or by common ownership. This worksheet<br />
allows <strong>for</strong> any adjustments that are needed to reduce related party transactions amounts to allowable<br />
Medicare amounts.<br />
40
F. RHC Cost Report (con’t)<br />
•Worksheet B<br />
This worksheet is used to summarize the number of facility visits to be used in the rate determination. The<br />
visits include the visits furnished by the provider’s health care staff and any physicians under agreement.<br />
This worksheet also calculates the overhead cost incurred which applies to the services.<br />
•Worksheet B-1<br />
The cost and administration of Pneumococcal and Infl uenza vaccines to Medicare benefi ciaries are 100<br />
percent reimbursable by Medicare. This worksheet calculates the cost per injection of each of these vaccines<br />
and determines the total amount of reimbursement <strong>for</strong> the vaccines administered to Medicare benefi<br />
ciaries.<br />
•Worksheet C<br />
This worksheet provides <strong>for</strong> the determination of the provider’s cost per visit and calculates the total amount<br />
due the provider or due the intermediary. Part I calculates the cost per visit and Part II determines the total<br />
Medicare payment due the provider <strong>for</strong> services furnished to Medicare benefi ciaries. This worksheet also<br />
allows the provider to claim reimbursement <strong>for</strong> bad debts related to uncollectible Medicare deductible and<br />
coinsurance amounts.<br />
The following is in<strong>for</strong>mation that needs to be gathered in order to complete a rural health clinic cost report:<br />
1) Financial statements <strong>for</strong> the cost reporting period; to include the trial balance.<br />
2) Total number of visits <strong>for</strong> the cost reporting period <strong>for</strong> each of the following health care providers (individual<br />
by name):<br />
A. Physicians<br />
B. PAs/NPs/CNMs<br />
C.Any Other <strong>Health</strong> Care Providers (list on worksheet by name and title)<br />
Total visits broken down by the following, per health care provider listed above.<br />
I. Medicare Visits<br />
II. Regular Medicaid Fee-For-Service Visits<br />
III. Crossover Visits (Medicare Primary and Regular Medicaid Secondary)<br />
IV. Medicaid HMO (Qualifi ed <strong>Health</strong> Plan) Visits per each HMO Crossover Visit (Medicare Primary<br />
and Medicaid HMO Secondary per each HMO)<br />
V. Private Visits (workers’ comp., commercial, self pay, sliding fee, etc.)<br />
3) The clinic’s hours of operation per week.<br />
4) Individual average hours worked per week <strong>for</strong> the following health care providers:<br />
1. Physicians<br />
2. PA/NP’s<br />
3. Any Other <strong>Health</strong> Care Providers<br />
5) Total average hours worked per week <strong>for</strong> each of the above health care providers broken down by the<br />
following:<br />
1. Administrative hours<br />
2. Patient Care hours<br />
3. Inpatient hours<br />
Job titles and wages should be broken down <strong>for</strong> all employees of the RHC <strong>for</strong> the cost reporting period. Be<br />
specifi c <strong>for</strong> those employees related to a lab technician job description <strong>for</strong> actual hours worked as “lab tech”<br />
and other hours worked.<br />
41
F. RHC Cost Report (con’t)<br />
Fringe Benefi ts and Employer related payroll taxes of each employee.<br />
6) Total number of vaccines given <strong>for</strong> the following vaccinations <strong>for</strong> all insurances totaled together:<br />
A. Pneumovax<br />
B. Infl uenza<br />
Total number of above vaccines given - broken down by the following:<br />
I. Medicare vaccines given <strong>for</strong> Pneumo and Infl uenza listed separately.<br />
II. Medicaid vaccines given <strong>for</strong> Pneumo and Infl uenza listed separately.<br />
III. Vaccine logs <strong>for</strong> Medicare Pneumovax and Infl uenza vaccines to include Patients name, HIC<br />
Number, and Date of Injection to support the above Medicare vaccinations.<br />
IV. Cost per dose of each vaccine.<br />
7) Payments Received <strong>for</strong> the following:<br />
A. Medicare Payments<br />
B. Medicaid Straight or Regular FFS Payments<br />
C. Medicaid HMO Payments per each HMO<br />
D. Medicare Crossover Payments made by Medicare<br />
E. Medicaid Crossover Payments made by Medicare<br />
F. Medicaid Other Third Party Payments (i.e. primary insurance’s, besides Medicare, that have<br />
paid when Medicaid is the secondary insurance)<br />
G. Medicare Benefi ciary Deductible Received (Payments made by the Medicare Patient)<br />
8) Any new assets purchased If so, submit the following:<br />
A. Date Asset Purchased<br />
B. Description of Asset<br />
C. Cost of Asset<br />
D. Depreciation Schedule to match depreciated expenses in Financial Statement<br />
9) Listing of Medicare Bad Debts with Medicare Patients, to include the following in<strong>for</strong>mation:<br />
A. Beneficiary Name<br />
B. Beneficiary HIC Number<br />
C. Date(s) of Service<br />
D. Date of First Bill<br />
E. Medicare Paid Date<br />
F. Date of Write-Off<br />
G. Amount of Debt<br />
H. Medicare Deductible and Coinsurance amount<br />
I. Medicaid Payment Amount<br />
In order to be considered “allowable bad debt”, debt must be written off during cost reporting period.<br />
NOTE: Reasonable collection ef<strong>for</strong>ts may be waived <strong>for</strong> Medicare indigent patients. A Medicare benefi ciary<br />
who also qualifi es <strong>for</strong> Medicaid may be considered indigent automatically. For other Medicare benefi ciaries,<br />
the provider should apply its customary practices <strong>for</strong> determining indigency. Please refer to PRM Section<br />
312 <strong>for</strong> the factors, which should be incorporated into the provider’s indigency guidelines. The bad debt <strong>for</strong><br />
an indigent patient may be written off and claimed upon discharge or upon the determination of indigency,<br />
whichever is later. If indigency is determined, please indicate Medicaid number of recipient, if applicable,<br />
to claim as bad debt to Medicare.<br />
10) Copy of PSR from Medicare Fiscal Intermediary to compare clinic visit and payment in<strong>for</strong>mation <strong>for</strong> the<br />
cost reporting period.<br />
42
F. RHC Cost Report (con’t)<br />
11) Listing of each Medicaid HMO (QHP) [Qualifi ed <strong>Health</strong> Plan] contracted with to include the following<br />
in<strong>for</strong>mation:<br />
A. Name of Medicaid HMO (QHP)<br />
B. Address of Medicaid HMO (QHP)<br />
C. Contact and phone number of HMO (QHP)<br />
D. Provider Number of HMO (QHP)<br />
E. Total the number of members assigned per each HMO (QHP) <strong>for</strong> each month of the cost reporting<br />
period - these numbers are then added up to make one complete total <strong>for</strong> the entire<br />
year.<br />
F. Visits and Payments broken down per Medicaid HMO (QHP) by capitation payments and FFS<br />
payments.<br />
12) Please Note: In<strong>for</strong>mation is needed <strong>for</strong> any “Lab Tech” personnel employed/contracted by the clinic<br />
not solely considered a lab tech and who provides services outside of lab tech services; please break<br />
hours down <strong>for</strong> the year based on description of job per<strong>for</strong>med by lab tech duties vs. all other RHC duties<br />
(2 categories needed): Other duties include, but are not limited to; billing, administrative, nursing, medical<br />
assistant, etc. This is only needed <strong>for</strong> lab tech’s that per<strong>for</strong>m other job functions other than lab technician<br />
services, as any cost beginning January 1, 2001 related to lab tech services is a non-allowable RHC cost.<br />
43
G. Important Resources<br />
1) Starting a <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>- A How-to <strong>Manual</strong>, U.S. Department of <strong>Health</strong> and Human<br />
Services, <strong>Health</strong> Resources and Services Administration, Office of <strong>Rural</strong> <strong>Health</strong> Policy, 2004<br />
Available online at: http://ruralhealth.hrsa.gov/RHC/RHCmanual.htm<br />
This manual includes the following in<strong>for</strong>mation:<br />
-Overview of the RHC Program<br />
-Getting Started - Does Your Site Qualify<br />
-Feasibility Analysis - Is The RHC Program For You<br />
-How to File the RHC Application<br />
-Preparing <strong>for</strong> the RHC Certification Inspection<br />
-Completing the Cost Report<br />
-RHC Coding and Billing Issues<br />
-State Survey and Certification Agencies<br />
-State Offices of <strong>Rural</strong> <strong>Health</strong><br />
-Criteria <strong>for</strong> <strong>Designation</strong> as a HPSA or MUA<br />
-Sample Policy and Procedures <strong>Manual</strong><br />
-Other Resources<br />
2) Medicare Benefit Policy <strong>Manual</strong>: Chapter 13 - <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> (RHC) and Federally Qualified<br />
<strong>Health</strong> <strong>Center</strong> (FQHC) Services<br />
Available online at: http://www.cms.hhs.gov/manuals/Downloads/bp102c13.pdf<br />
This manual includes the following in<strong>for</strong>mation:<br />
-<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (RHCs) Defined<br />
-<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> and Federally Qualified <strong>Health</strong> <strong>Center</strong> Service Defined<br />
-Physician Services<br />
-Services and Supplies Furnished Incident to Physician’s Services<br />
-Nurse Practitioner, Certified Nurse Midwife, and Physician Assistant Services<br />
-Services and Supplies Incident to Nurse Practitioner’s, Certified Nurse Midwives’s<br />
-Conditions <strong>for</strong> Coverage of Visiting Nurse Services<br />
-<strong>Clinic</strong>al Psychologist Services Away and at the RHC/FQHC <strong>Clinic</strong> or <strong>Center</strong><br />
-<strong>Clinic</strong>al Social Worker (CSW) Services Away and at the RHC/FQHC <strong>Clinic</strong> or <strong>Center</strong><br />
3) Medicare Claims Processing <strong>Manual</strong>: Chapter 9 - <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s/Federally Qualified<br />
<strong>Health</strong> <strong>Center</strong>s<br />
Available online at: http://www.cms.hhs.gov/manuals/downloads/clm104c09.pdf<br />
This manual includes the following in<strong>for</strong>mation:<br />
-General Differences Between RHCs and FQHCs<br />
-Method of Medicare Payment <strong>for</strong> RHC and FQHC Services<br />
44
G. Important Resources (con’t)<br />
-Annual Reconciliation With Cost Report<br />
-Allowable Costs<br />
-Deductible and Coinsurance<br />
-Mental <strong>Health</strong> Services Limit<br />
-Determining How Much to Charge Patient Be<strong>for</strong>e Billing Is Submitted <strong>for</strong> Part B Pay<br />
ment<br />
-General Billing Requirements <strong>for</strong> Preventive Services<br />
-Laboratory Services<br />
-FI/Carrier Coordination<br />
-Agreements Between CMS and RHC/FQHC<br />
-Content and Terms of Agreements<br />
-Termination of Agreement<br />
45
IV. Appendices<br />
Appendix A. Important Contact In<strong>for</strong>mation<br />
<strong>Arizona</strong> Department of <strong>Health</strong> Services<br />
Division of Licensing Services<br />
Office of Medical Facilities Licensing<br />
150 North 18th Avenue<br />
4th Floor<br />
Phoenix, AZ 85007<br />
(602) 364-3030<br />
(602) 364-4806 Fax<br />
http://www.azdhs.gov/als/medical/index.htm<br />
For in<strong>for</strong>mation regarding RHC Certification,<br />
contact: Helena Hoover at the above phone<br />
number.<br />
For in<strong>for</strong>mation regarding Licensing, contact<br />
the Office of Medical Facilities Licensing at the<br />
phone number listed above.<br />
<strong>Rural</strong> <strong>Health</strong> Office<br />
Mel and Enid Zuckerman College of Public<br />
<strong>Health</strong><br />
The University of <strong>Arizona</strong><br />
P.O. Box 245177<br />
Tucson, AZ 85724<br />
(520) 626-5823<br />
(520) 626-3101 Fax<br />
http://www.rho.arizona.edu/<br />
The mission of the <strong>Rural</strong> <strong>Health</strong> Office is to<br />
promote the health of rural and medically underserved<br />
individuals, families, and communities<br />
through service, education, and research.<br />
They can provide technical assistance to groups<br />
wishing to apply <strong>for</strong> RHC certification. Contact<br />
Alison Hughes at (520) 626-6253.<br />
<strong>Health</strong>care Horizon<br />
J.E. Estes, Owner<br />
Route 5 Box 226<br />
Bartlesville, OK 74003<br />
(800) 399-0874<br />
(918) 336-6269 Fax<br />
http://www.healthcarehorizon.com<br />
<strong>Health</strong>care Horizon has offered consultation<br />
services to <strong>Rural</strong> <strong>Health</strong> providers across the<br />
nation since 1989. With health experience dating<br />
back to 1976, this firm is well rooted and established<br />
in the <strong>Rural</strong> <strong>Health</strong> field. <strong>Health</strong>care<br />
Horizon provides clients with a powerful<br />
combination of knowledge, experience, and integrity.<br />
The <strong>Center</strong>s <strong>for</strong> Medicare and Medicaid<br />
Services (CMS)<br />
7500 Security Boulevard<br />
Baltimore, Maryland 21244-1850<br />
1-877-267-2323<br />
http://www.cms.hhs.gov<br />
The <strong>Center</strong>s <strong>for</strong> Medicare & Medicaid Services<br />
(CMS) is a Federal agency within the U.S. Department<br />
of <strong>Health</strong> and Human Services. Programs<br />
<strong>for</strong> which CMS is responsible include<br />
Medicare, Medicaid, State Children’s <strong>Health</strong> Insurance<br />
Program (SCHIP), HIPAA, and CLIA.<br />
1735 Babcock Road<br />
San Antonio, Texas 78229<br />
(800) 782-5621<br />
(210) 349-0015<br />
(210) 349-0225 Fax<br />
46
Appendix A. Important Contact In<strong>for</strong>mation (con’t)<br />
M& M Computer Services<br />
Contact Name: John Linn<br />
http://mnm-medical.com<br />
M & M Computer Services is the originator and<br />
sole owner of the Medical Accounts Receivable<br />
System (M.A.R.S.), the leading Medicare certified<br />
<strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> billing and in<strong>for</strong>mation<br />
system software in the country.<br />
National Association of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s<br />
2 East Main Street<br />
Fremont, MI 49412<br />
info@narhc.org<br />
(866) 306-1961<br />
info@narhc.org<br />
http://www.narhc.org<br />
The National Association of <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s<br />
(NARHC) is the only national organization<br />
dedicated exclusively to improving the delivery<br />
of quality, cost-effective health care in rural under<br />
served areas through the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s<br />
(RHC) Program. NARHC works with Congress,<br />
federal agencies, and rural health allies<br />
to promote, expand, and protect the RHC Program.<br />
Through the association, NARHC members<br />
become actively engaged in the legislative<br />
and regulatory process.<br />
National <strong>Rural</strong> <strong>Health</strong> Association<br />
Headquarters<br />
521 East 63rd Street<br />
Kansas City, MO 64110<br />
(816) 756-3140<br />
(816) 765-3144<br />
Government Affairs Office<br />
1108 K Street NW<br />
Washington DC, 20005<br />
(202) 639-0550<br />
(202) 639-0559 Fax<br />
National <strong>Rural</strong> <strong>Health</strong> Association (con’t)<br />
http://www.nrharural.org<br />
The National <strong>Rural</strong> <strong>Health</strong> Association is a<br />
national nonprofit membership organization,<br />
whose mission is to improve the health and<br />
health care of rural Americans and to provide<br />
leadership on rural issues through advocacy,<br />
communications, education, and research.<br />
Office of <strong>Rural</strong> <strong>Health</strong> Policy<br />
<strong>Health</strong> Resources and Services Administration<br />
5600 Fishers Lane, 9A-55<br />
Rockville, MD 20857<br />
(301) 443-0835<br />
(301) 443-2803 Fax<br />
http://ruralhealth.hrsa.gov<br />
The Office of <strong>Rural</strong> <strong>Health</strong> Policy (ORHP)<br />
promotes better health care service in rural<br />
America. Established in August 1987 by the<br />
Administration, the Office was subsequently<br />
authorized by Congress in December 1987 and<br />
located in the <strong>Health</strong> Resources and Services<br />
Administration. Congress charged the Office<br />
with in<strong>for</strong>ming and advising the Department of<br />
<strong>Health</strong> and Human Services on matters affecting<br />
rural hospitals and health care, coordinating<br />
activities within the department that relate<br />
to rural health care, and maintaining a national<br />
in<strong>for</strong>mation clearinghouse.<br />
<strong>Rural</strong> In<strong>for</strong>mation <strong>Center</strong><br />
National Agricultural Library<br />
10301 Baltimore Avenue, Room 132<br />
Beltsville, MD 20705<br />
ric@nal.usda.gov<br />
1-800-633-7701<br />
(301) 504-5181 Fax<br />
http://ric.nal.usda.gov<br />
47
Appendix A. Important Contact In<strong>for</strong>mation (con’t)<br />
<strong>Rural</strong> In<strong>for</strong>mation <strong>Center</strong> (con’t)<br />
The <strong>Rural</strong> In<strong>for</strong>mation <strong>Center</strong> (RIC) of the National<br />
Agricultural Library provides in<strong>for</strong>mation<br />
and referral services to local, tribal, state,<br />
and federal government officials; community<br />
organizations; rural electric and telephone cooperatives;<br />
libraries; businesses; and, citizens<br />
working to maintain the vitality of America’s<br />
rural areas.<br />
<strong>Rural</strong> Assistance <strong>Center</strong><br />
School of Medicine and <strong>Health</strong> Sciences,<br />
Room 4520<br />
501 North Columbia Road Stop 9037<br />
Grand Forks, ND 58202<br />
1-800-270-1898<br />
1-800-270-1913 Fax<br />
info@raconline.org<br />
http://www.raconline.org<br />
A product of the U.S. Department of <strong>Health</strong><br />
and Human Services’ <strong>Rural</strong> Initiative, the <strong>Rural</strong><br />
Assistance <strong>Center</strong> (RAC) was established<br />
in December 2002 as a rural health and human<br />
services “in<strong>for</strong>mation portal.” RAC helps rural<br />
communities and other rural stakeholders access<br />
the full range of available programs, funding,<br />
and research that can enable them to provide<br />
quality health and human services to rural<br />
residents.<br />
48
Appendix B. Definitions <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> <strong>Designation</strong><br />
<strong>Rural</strong>:<br />
The U.S. Census Bureau defines rural as “all territory, population, or housing unit located outside<br />
of UAs [urbanized areas] and UCs [urbanized clusters].”<br />
Source: United States Census Bureau, Census 2000 Urban and <strong>Rural</strong> Classification, http://www.census.gov/geo/www/<br />
ua/ua_2k.html.<br />
Urban:<br />
“For Census 2000, the Census Bureau classifies as ‘urban’ all territory, population, and housing<br />
units located within an urbanized area (UA) or an urban cluster (UC). It delineates UA and UC<br />
boundaries to encompass densely settled territory, which consists of core census block groups or<br />
blocks that have a population density of at least 1,000 people per square mile and surrounding<br />
census blocks that have an overall density of at least 500 people per square mile.”<br />
Source: United States Census Bureau, Census 2000 Urban and <strong>Rural</strong> Classification, http://www.census.gov/geo/www/<br />
ua/ua_2k.html.<br />
Urbanized Area:<br />
According to the U.S. Census Bureau, an urbanized area “consists of contiguous, densely settled<br />
census block groups (BGs) and census blocks that meet minimum population density requirements,<br />
along with adjacent densely settled census blocks that together encompass a population of at least<br />
50,000 people.”<br />
Source: United States Bureau of the Census, Urban Area Criteria <strong>for</strong> Census 2000, http://www.census.gov/geo/www/<br />
ua/uafedreg031502.txt.<br />
Urban Cluster:<br />
According to the U.S. Census Bureau, an urban cluster “consists of contiguous, densely settled<br />
census [block groups] and census blocks that meet minimum population density requirements,<br />
along with adjacent densely settled census blocks that together encompass a population of at least<br />
2,500 people, but fewer than 50,000 people.”<br />
Source: United States Bureau of the Census, Urban Area Criteria <strong>for</strong> Census 2000, http://www.census.gov/geo/www/<br />
ua/uafedreg031502.txt.<br />
<strong>Health</strong> Professional Shortage Area (HPSA):<br />
The purpose of the HPSA designation is to identify an area or population that has a shortage of<br />
dental, mental, and primary health care providers. The HPSA designation is based on the following<br />
three criteria: the geographic area involved must be rational <strong>for</strong> delivery of health services; a<br />
49
Appendix B. Definitions <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> <strong>Designation</strong> (con’t)<br />
specified population-to-provider ratio representing shortage must be exceeded within the area;<br />
resources in contiguous areas must be shown to be overutilized, excessively distant, or otherwise<br />
inaccessible. A HPSA designation may be <strong>for</strong> a geographic area, a certain population (i.e., lowincome),<br />
or a facility. HPSA designation criteria are developed by the Shortage <strong>Designation</strong> Branch<br />
in the HRSA Bureau of <strong>Health</strong> Professions, National <strong>Center</strong> <strong>for</strong> <strong>Health</strong> Work<strong>for</strong>ce Analysis. For<br />
in<strong>for</strong>mation on how to apply <strong>for</strong> a HPSA designation, visit: http://bhpr.hrsa.gov/shortage/hpsapply.<br />
htm.<br />
In addition, automatic facility HPSA status is available <strong>for</strong> all Federally Qualified <strong>Health</strong> <strong>Center</strong>s<br />
(FQHCs) and those <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>s (RHCs) that meet the requirement of providing access to<br />
care regardless of ability to<br />
pay. For more in<strong>for</strong>mation, visit: http://bhpr.hrsa.gov/shortage/autoscore.htm.<br />
Sources: <strong>Arizona</strong> Department of <strong>Health</strong> Services, Office of <strong>Health</strong> Systems Development, <strong>Health</strong> Professional Shortage<br />
Areas, http://www.azdhs.gov/hsd/hpsa.htm; HRSA Bureau of <strong>Health</strong> Professions, Shortage <strong>Designation</strong>, http://bhpr.<br />
hrsa.gov/shortage/; HRSA Bureau of <strong>Health</strong> Professions, Shortage <strong>Designation</strong>: Automatic Facility HPSA Scoring,<br />
http://bhpr.hrsa.gov/shortage/autoscore.htm.<br />
Medically Underserved Area (MUA):<br />
The purpose of the MUA designation is to identify areas that are in need of medical services on the<br />
basis of demographic data. The designation is dependent on the area having an Index of Medical<br />
Underservice (IMU) score of 62.0 points or less. The IMU is a weighted score and is based on<br />
the following four criteria: ratio of primary medical care physicians per 1,000 population, infant<br />
mortality rate, percentage of population below the federal poverty level, and percentage of the<br />
population 65 years and older.<br />
Source: <strong>Arizona</strong> Department of <strong>Health</strong> Services, Office of <strong>Health</strong> Systems Development, Federal Medically<br />
Underserved Areas and Populations, http://www.azdhs.gov/hsd/mua_mup.htm.<br />
50
Appendix C. Federal Primary Care HPSAs in <strong>Arizona</strong> (as of 3/2007)<br />
APACHE<br />
• Chinle<br />
<strong>Designation</strong> Type: Geographic<br />
• Ganado<br />
<strong>Designation</strong> Type: Geographic<br />
• Kayenta<br />
<strong>Designation</strong> Type: Geographic<br />
• Sanders<br />
<strong>Designation</strong> Type: Geographic<br />
• St. Johns/Springerville<br />
<strong>Designation</strong> Type: Geographic<br />
COCHISE<br />
• Benson<br />
Destination Type: Population Low<br />
Income<br />
• Bisbee<br />
<strong>Designation</strong> Type: Geographic<br />
• Douglas<br />
<strong>Designation</strong> Type: Geographic<br />
• <strong>Arizona</strong> State Prison Complex-Douglas<br />
<strong>Designation</strong> Type: Facility<br />
• Elfrida<br />
<strong>Designation</strong> Type: Geographic<br />
• Sierra Vista/ Tombstone<br />
<strong>Designation</strong> Type: Geographic<br />
COCONINO<br />
• Fredonia<br />
<strong>Designation</strong> Type: Geographic<br />
• Grand Canyon Village<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Hopi<br />
<strong>Designation</strong> Type: Geographic<br />
• Page/Tuba City<br />
<strong>Designation</strong> Type: Geographic<br />
GILA<br />
• Globe<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
GILA (con’t)<br />
• Hayden<br />
<strong>Designation</strong> Type: Geographic<br />
• Northern Young<br />
<strong>Designation</strong> Type: Geographic<br />
• Young<br />
<strong>Designation</strong> Type: Geographic<br />
GRAHAM<br />
• <strong>Arizona</strong> State Prison Complex- Saf<strong>for</strong>d<br />
<strong>Designation</strong> Type: Facility<br />
• Federal Correctional Institution-<br />
Saf<strong>for</strong>d<br />
<strong>Designation</strong> Type: Facility<br />
• Graham County<br />
<strong>Designation</strong> Type: Geographic<br />
GREENLEE<br />
• Entire County<br />
<strong>Designation</strong> Type: Geographic<br />
LA PAZ<br />
• Entire County<br />
<strong>Designation</strong> Type: Geographic<br />
MARICOPA<br />
• Adobe Mountain School<br />
<strong>Designation</strong> Type: Facility<br />
• <strong>Arizona</strong> State Prison Complex- Lewis<br />
<strong>Designation</strong> Type: Facility<br />
• Avondale/Tolleson<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Buckeye<br />
<strong>Designation</strong> Type: Geographic<br />
• Chandler<br />
<strong>Designation</strong> Type: Geographic<br />
• El Mirage<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Federal Correctional Institution-<br />
Phoenix<br />
51
Appendix C. Federal Primary Care HPSAs in <strong>Arizona</strong> (con’t)<br />
MARICOPA (con’t)<br />
<strong>Designation</strong> Type: Facility<br />
• Gila Bend<br />
<strong>Designation</strong> Type: Geographic<br />
• Glendale<br />
<strong>Designation</strong> Type: Geographic<br />
• Maricopa County Jails<br />
<strong>Designation</strong> Type: Facility<br />
• Rio Salado<br />
<strong>Designation</strong> Type: Geographic<br />
• South Central Phoenix<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• South Mountain<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Southwest Phoenix<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• West Phoenix<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Wickenburg<br />
<strong>Designation</strong> Type: Geographic<br />
MOHAVE<br />
• Bullhead City<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Dolan Springs<br />
<strong>Designation</strong> Type: Geographic<br />
• Fort Mohave<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Kingman<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Mohave North<br />
<strong>Designation</strong> Type: Geographic<br />
NAVAJO<br />
• <strong>Arizona</strong> State Prison Complex-<br />
Winslow<br />
<strong>Designation</strong> Type: Facility<br />
• Chinle<br />
<strong>Designation</strong> Type: Geographic<br />
• Dilkon<br />
<strong>Designation</strong> Type: Geographic<br />
• Heber/Overgaard<br />
<strong>Designation</strong> Type: Geographic<br />
• Hopi<br />
<strong>Designation</strong> Type: Geographic<br />
• Kayenta<br />
<strong>Designation</strong> Type: Geographic<br />
• Showlow<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
• Snowflake<br />
<strong>Designation</strong> Type: Geographic<br />
• Winslow<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
PIMA<br />
• Ajo<br />
<strong>Designation</strong> Type: Geographic<br />
• Arivaca<br />
<strong>Designation</strong> Type: Geographic<br />
• <strong>Arizona</strong> State Prison Complex- Tucson<br />
<strong>Designation</strong> Type: Facility<br />
• Children’s Rehabilitative Services of<br />
Tucson<br />
<strong>Designation</strong> Type: Facility<br />
• Continental<br />
<strong>Designation</strong> Type: Geographic<br />
• Federal Correctional Institution-<br />
Tucson<br />
<strong>Designation</strong> Type: Facility<br />
• Marana<br />
<strong>Designation</strong> Type: Geographic<br />
• Tucson Central<br />
<strong>Designation</strong> Type: Geographic<br />
52
Appendix • C. Federal Primary Care HPSAs in <strong>Arizona</strong> (con’t)<br />
PIMA (con’t)<br />
Tucson Southeast<br />
<strong>Designation</strong> Type: Geographic<br />
• Tucson Southwest<br />
<strong>Designation</strong> Type: Geographic<br />
PINAL<br />
• Apache Junction<br />
<strong>Designation</strong> Type: Geographic<br />
• <strong>Arizona</strong> State Prison Complex- Eyman<br />
<strong>Designation</strong> Type: Facility<br />
• Central/West Pinal<br />
<strong>Designation</strong> Type: Population Low<br />
Income/Migrant Farm Worker<br />
• Florence Prison, INS<br />
<strong>Designation</strong> Type: Facility<br />
• San Pedro Valley<br />
<strong>Designation</strong> Type: Geographic<br />
• Superior/Kearny<br />
<strong>Designation</strong> Type: Population Low<br />
Income<br />
SANTA CRUZ<br />
• Entire County<br />
<strong>Designation</strong> Type: Geographic<br />
YAVAPAI<br />
• Ash Fork<br />
<strong>Designation</strong> Type: Geographic<br />
• Cordes Junction<br />
<strong>Designation</strong> Type: Geographic<br />
• Yavapai South<br />
<strong>Designation</strong> Type: Geographic<br />
YUMA<br />
• <strong>Arizona</strong> State Prison Complex- Yuma<br />
<strong>Designation</strong> Type: Facility<br />
• Yuma County<br />
<strong>Designation</strong> Type: Geographic<br />
Source: <strong>Arizona</strong> Department of <strong>Health</strong> Services, Office<br />
of <strong>Health</strong> Systems Development, Primary Care HPSAs<br />
(by County), http://www.azdhs.gov/hsd/pc_hpsa.htm.<br />
53
Appendix D. Federal MUAs/MUP in <strong>Arizona</strong> (as of 6/2007)<br />
APACHE<br />
• Entire County<br />
<strong>Designation</strong> Type: MUA<br />
COCHISE<br />
• Benson Division<br />
<strong>Designation</strong> Type: MUA<br />
• Bisbee<br />
<strong>Designation</strong> Type: MUP - Low Income<br />
• Bowie/Willcox<br />
<strong>Designation</strong> Type: MUA<br />
• Douglas<br />
<strong>Designation</strong> Type: MUA<br />
• Elfrida Division<br />
<strong>Designation</strong> Type: MUA<br />
• Sierra Vista Division<br />
<strong>Designation</strong> Type: MUA<br />
COCONINO<br />
• Flagstaff- Medically Indigent<br />
Population<br />
<strong>Designation</strong> Type: Governor’s Request<br />
• Kaibab Division<br />
<strong>Designation</strong> Type: MUA<br />
• Tuba City<br />
<strong>Designation</strong> Type: MUA<br />
GILA<br />
• Entire County<br />
<strong>Designation</strong> Type: MUP - Low Income<br />
GREENLEE<br />
• Duncan Division<br />
<strong>Designation</strong> Type: MUA<br />
LA PAZ<br />
• Parker<br />
<strong>Designation</strong> Type: MUP - Low Income<br />
• Quartzsite<br />
<strong>Designation</strong> Type: MUA<br />
• Salome<br />
<strong>Designation</strong> Type: MUA<br />
MARICOPA<br />
• Avendale/Tollesm<br />
<strong>Designation</strong> Type: MUP<br />
• Chandler<br />
<strong>Designation</strong> Type: MUA<br />
• El Mirage<br />
<strong>Designation</strong> Type: MUA<br />
• Gila Bend Division<br />
<strong>Designation</strong> Type: MUA<br />
• Glendale<br />
<strong>Designation</strong> Type: MUA<br />
• Guadalupe<br />
<strong>Designation</strong> Type: MUA<br />
• North Tempe<br />
<strong>Designation</strong> Type: MUA<br />
• Rio Salado<br />
<strong>Designation</strong> Type: MUA<br />
• South Central Phoenix<br />
<strong>Designation</strong> Type: MUP - Low Income<br />
• South Mountain<br />
<strong>Designation</strong> Type: MUA<br />
• West Phoenix<br />
<strong>Designation</strong> Type: MUA<br />
• Wickenburg<br />
<strong>Designation</strong> Type: MUA<br />
MOHAVE<br />
• Bullhead City<br />
<strong>Designation</strong> Type: MUP<br />
• Dolan Springs<br />
<strong>Designation</strong> Type: MUA<br />
• FT Mojave<br />
<strong>Designation</strong> Type: MUP<br />
• Kingman<br />
<strong>Designation</strong> Type: MUA<br />
• Mohave North Division<br />
<strong>Designation</strong> Type: MUA<br />
• Peach Springs<br />
<strong>Designation</strong> Type: MUA<br />
54
Appendix D. Federal MUAs in <strong>Arizona</strong> (con’t)<br />
NAVAJO<br />
• Entire County<br />
<strong>Designation</strong> Type: MUA<br />
PIMA<br />
• Arivaca<br />
<strong>Designation</strong> Type: MUA<br />
• Marana<br />
<strong>Designation</strong> Type: MUA<br />
• South Tucson<br />
<strong>Designation</strong> Type: MUA<br />
PINAL<br />
• Apache Junction<br />
<strong>Designation</strong> Type: MUA<br />
• Central-West Pinal<br />
<strong>Designation</strong> Type: MUP - Low Income<br />
• Gila River Division<br />
<strong>Designation</strong> Type: MUA<br />
• Superior<br />
<strong>Designation</strong> Type: MUA<br />
SANTA CRUZ<br />
• Entire County<br />
<strong>Designation</strong> Type: MUA<br />
YAVAPI<br />
• Entire County<br />
<strong>Designation</strong> Type: MUP - Low Income<br />
YUMA<br />
• Yuma North<br />
<strong>Designation</strong> Type: MUA<br />
• Yuma West<br />
<strong>Designation</strong> Type: MUA<br />
Source: <strong>Arizona</strong> Department of <strong>Health</strong> Services, Office<br />
of <strong>Health</strong> Systems Development, Federal Medically<br />
Underserved Areas and Populations, http://www.azdhs.<br />
gov/hsd/mua_mup.htm.<br />
55
Appendix E. Licensing Forms<br />
1. INSTRUCTIONS FOR COMPLETING THE APPLICATION FOR A HEALTH<br />
INSTITUTION LICENSE- Page 57<br />
2. INITIAL APPLICATION FOR A HEALTH CARE INSTITUTION LICENSE-<br />
Pages 58-60<br />
3. INITIAL APPLICATION CHECKLIST- Page 63<br />
4. RENEWAL APPLICATION FOR A HEALTH CARE INSTITUTION<br />
LICENSE- Pages 63-64<br />
5. RENEWAL APPLICATION CHECKLIST- Pages 66<br />
6. OUTPATIENT FACILITY INFORMATION- Pages 67-68<br />
56
Instructions <strong>for</strong> completing HCI Application<br />
PLEASE TYPE OR PRINT IN BLACK INK.<br />
Please submit the application, with all required attachments and the required fee. This<br />
application will not be complete until all required attachments and fees have been submitted to<br />
the Department. If any corrections are made to the application using correction fluid or<br />
correction tape, the application will be returned. If you make a mistake filling out the application,<br />
put a line through the mistake and your initials.<br />
I. HEALTH CARE INSTITUTION INFORMATION<br />
Provide all required in<strong>for</strong>mation.<br />
“Tax ID number” means a numeric identifier that a person uses to report financial in<strong>for</strong>mation to the<br />
United States Internal Revenue Services. (If you are using an individual’s Social Security Number, it will<br />
be treated as confidential in<strong>for</strong>mation and redacted from the copy of the application in the facility’s public<br />
file.)<br />
According to <strong>Arizona</strong> Revised Statutes, Title 36, Chapter 4, or <strong>Arizona</strong> Administrative Code, Title 9,<br />
Chapter 10, a person may apply <strong>for</strong> a license as a health care institution class or subclass, which are<br />
listed below. Select one of the following classifications and write it on the application.<br />
Abortion clinic<br />
Adult day health care facility<br />
Adult foster care<br />
Assisted living center<br />
Assisted living home<br />
Home health agency<br />
Hospice inpatient facility<br />
Hospice<br />
Hospital<br />
Nursing care institution<br />
Outpatient surgical center<br />
Outpatient treatment center<br />
Recovery care center<br />
Unclassified <strong>Health</strong> Care Institution.<br />
II. OWNER INFORMATION<br />
“Owner” means a person who appoints, elects, or otherwise designates a health care institution’s<br />
governing authority. “Proprietary” means an owner or owners. “Non-Proprietary means a leased<br />
business, franchise, or in certain instances, a Governmental Agency.<br />
III. GOVERNING AUTHORITY<br />
“Governing authority” means the individual, agency, group or corporation, appointed, elected or<br />
otherwise designated, in which the ultimate responsibility and authority <strong>for</strong> the conduct of the health care<br />
institution are vested.<br />
IV. CHIEF ADMINISTRATIVE OFFICER<br />
“Chief administrative officer” means the individual implementing a governing authority’s direction in a<br />
health care institution. This is the on-site administrator, or the certified manager.<br />
V. SIGNATURES<br />
According to A.R.S, § 36-422(B) the application must be signed, as follows:<br />
(1) If an individual, by the owner of the institution;<br />
(2) If a partnership or corporation, by two of the partners or corporate officers; or<br />
(3) If a governmental unit, the head of the governmental department having jurisdiction.<br />
G:/Instructions <strong>for</strong> completing HCI ApplicationMEDICAL.doc 06/05/08<br />
57
ARIZONA DEPARTMENT OF HEALTH SERVICES<br />
DIVISION OF LICENSING SERVICES<br />
150 N. 18 th Avenue, Suite 450, Phoenix, <strong>Arizona</strong> 85007 *** 400 W. Congress, #116, Tucson, <strong>Arizona</strong> 85701<br />
INITIAL APPLICATION FOR A HEALTH CARE INSTITUTION LICENSE<br />
A.R.S. Title 36, Chapter 4 and A.A.C. Title 9<br />
I. HEALTH CARE INSTITUTION INFORMATION<br />
Name of health care institution<br />
Street address<br />
City Zip code Phone number<br />
Tax I.D. number Fax number E-mail address<br />
Mailing address<br />
City State Zip code<br />
Requested health care institution class or subclass:(listed in R9-10-102)<br />
Requested Licensed Capacity:<br />
A. Is the proposed health care institution (except <strong>for</strong> a home health agency or a hospice service agency) located within<br />
1/4 mile of agricultural land<br />
Yes No If yes:<br />
1. Include on a separate sheet of paper the names and addresses of owners or lessees of any agricultural land<br />
within 1/4 mile of the proposed health care institution, and<br />
2. Attach a copy of the written agreement between the health care institution owner and the owner or lessee of<br />
agricultural land prescribed in A.R.S. ' 36-421(D).<br />
B. Is the proposed health care institution located in a leased facility<br />
Yes No If yes, attach a copy of the lease showing rights and responsibilities of the parties.<br />
C. If a proposed health care institution is not exempt from submitting architectural plans and specifications pursuant to<br />
A.R.S. ' 36-422(E) attach one of the following:<br />
1. A copy of DHS approval of the proposed health care institution=s architectural plans and specifications, or<br />
2. The architectural plans and specifications <strong>for</strong> the proposed health care institution required in A.A.C. R9-10-<br />
105(A)(5)(a).<br />
D. Is the proposed health care institution ready <strong>for</strong> an inspection by Department representatives<br />
Yes No If no, date the proposed health care institution will be ready<br />
II. OWNER INFORMATION (Name of Corporation, LLC, etc.)<br />
Owner’s name<br />
Address<br />
City<br />
Telephone number<br />
Zip code<br />
Fax number<br />
The owner is a: (check one) Proprietary (<strong>for</strong> profit) Non-proprietary (non-profit)<br />
The owner is a: (check one) _____Sole proprietorship _____Partnership<br />
_____Limited liability company _____Corporation _____Governmental Agency<br />
58
A. PLEASE LIST IN THE SPACE PROVIDED BELOW:<br />
If the owner is a partnership, the name of each partner;<br />
If the owner is a limited liability company, the name of the designated manager, or if no manager is designated, the<br />
names of any 2 members of the limited liability company;<br />
If the owner is a corporation, the name and title of each corporate officer; or<br />
If the owner is a governmental agency, the name and title of the individual in charge of the governmental agency or<br />
the individual designated in writing by the individual in charge of the governmental agency.<br />
Name<br />
Name<br />
Name<br />
Title<br />
Title<br />
Title<br />
Name<br />
Title<br />
B. If applicable, attach a copy of the articles of incorporation, the partnership documents, or the limited liability<br />
company documents.<br />
C. Has the person applying <strong>for</strong> a license or a person with 10% or more business interest in the health care institution had<br />
a health care professional license or certificate denied, revoked or suspended<br />
____Yes ____ No<br />
D. Has the person applying <strong>for</strong> a license or a person with 10% or more business interest in the health care institution had<br />
a license to operate a health care institution denied, revoked or suspended<br />
____Yes ____ No<br />
E. If either of the above questions is answered yes, include on a separate sheet of paper <strong>for</strong> each yes answer:<br />
1. The reason <strong>for</strong> the denial, suspension, or revocation;<br />
2. The date of the denial, suspension, or revocation;<br />
3. The name and address of the licensing agency that denied, suspended, or revoked the license.<br />
Statutory agent (or individual designated to accept service of process and subpoenas)<br />
Name<br />
Address<br />
Title<br />
Telephone number<br />
III. GOVERNING AUTHORITY<br />
Name<br />
IV. CHIEF ADMINISTRATIVE OFFICER (Facility Administrator)<br />
Name<br />
Title<br />
Education (list the highest educational degree obtained and any instruction related to the health care institution class or subclass<br />
<strong>for</strong> which licensure is requested)<br />
Experience (list work experience related to the health care institution class or subclass <strong>for</strong> which licensure is requested)<br />
59
V. SIGNATURES<br />
According to A.R.S. ' 36-422(B) an application must be signed, as follows:<br />
(1) If an individual, by the owner of the institution;<br />
(2) If a partnership or corporation, by two of the partners or corporate officers; or<br />
(3) If a governmental unit, the head of the governmental department having jurisdiction.<br />
_____________________________________________<br />
Signature<br />
Date<br />
_____________________________________________<br />
Title<br />
_____________________________________________<br />
Signature<br />
Date<br />
_____________________________________________<br />
Title<br />
VI. TIME FRAME<br />
Pursuant to A.R.S. § 41-1075 The applicant agrees to extend the substantive review time frame if necessary. This will not exceed 25% of the<br />
overall time frame.<br />
Provider Signature:_______________________________________ Representative of DHS:______________________________________<br />
Attach:<br />
1. Documentation from the local jurisdiction of compliance with all applicable local building codes and ordinances.<br />
2. If accredited by a nationally recognized health care accreditation agency, a copy of the current accreditation.<br />
For DHS use only: Correct application fee enclosed: Yes No Check #:<br />
60
MEDICAL FACILITIES LICENSING<br />
150 N. 18 th Avenue, Suite 450-Phoenix, <strong>Arizona</strong> 85007<br />
400 W. Congress, Suite 116-Tucson, <strong>Arizona</strong> 85701<br />
HEALTH CARE INSTITUTION INITIAL APPLICATION<br />
AND LICENSE FEE REMITTANCE FORM<br />
PLEASE RETURN THIS FORM WITH THE PAYMENT TO THE ADDRESS ABOVE<br />
FACILITY I.D. #: LICENSE #: LEVEL OF CARE<br />
OR SERVICES<br />
APPLICANT/ENTITY NAME:<br />
FACILITY NAME:<br />
STREET ADDRESS: SUITE #:<br />
CITY: STATE: ZIP:<br />
PHYSICAL ADDRESS:<br />
CITY: STATE: ZIP:<br />
FEES<br />
Application Fee<br />
(Please do not submit the application fee if the fee has already been paid.)<br />
AMOUNT DUE<br />
$ 50.00<br />
LICENSED CAPACITY<br />
Check One: Licensed Capacity: Base Fee: Number of Beds x<br />
$10.00 each:<br />
Total base fee plus number<br />
of beds fee:<br />
None $ 100.00 $<br />
1 to 59 beds 100.00<br />
60 to 99 beds 200.00<br />
100 to 149 beds 300.00<br />
150 or more beds 500.00<br />
TOTAL AMOUNT DUE $<br />
Payment should be by cashier=s check, money order or business check made payable to:<br />
ARIZONA DEPARTMENT OF HEALTH SERVICES<br />
Write the Facility I.D. # on the check.<br />
Cash and personal checks are not accepted.<br />
AMOUNT ENCLOSED $<br />
ALL FEES ARE NON-REFUNDABLE pursuant to A.R.S. ' 36-405(c), 36-882(f) and 36-897.01(c), except as provided in<br />
A.R.S. ' 41-1077.<br />
61
CHECKLIST FOR<br />
HEALTH CARE INSTITUTION<br />
LICENSE APPLICATION<br />
AND<br />
REQUIRED ATTACHMENTS<br />
INITIAL<br />
Your license application packet must include the following:<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
License Application For <strong>Health</strong> Care Institution<br />
$50.00 Application Fee (Please include name of facility/agency)<br />
Services Provided and Staffing Form (Forms provided in package)<br />
Medical Specialties (if applicable)<br />
Current Fire Inspection Report from local municipality<br />
Resume <strong>for</strong> Administrator<br />
Lease Agreement (if applicable)<br />
Board of Directors list or list of Officers of the Corporation<br />
Licensed Capacity (if applicable)<br />
Full Accreditation Report and Cover Letter (if applicable)<br />
Certificate of Occupancy<br />
Zoning Authority Clearance (original with signatures)<br />
Floor Plan indicating entrance/exits and rooms being used<br />
Food Service Report (if applicable)<br />
Home <strong>Health</strong> Agency - Roster <strong>for</strong> T.B./Fingerprinting of staff & Area Map<br />
NOTE:<br />
1. Applications are legal documents. DO NOT use correction fluid or correction tape on the<br />
license application. Applications must have original signatures. Photocopies of<br />
signatures will not be accepted.<br />
2. The Fees must be made payable to the <strong>Arizona</strong> Department of <strong>Health</strong> Services. Please<br />
include the name of the facility/agency on check.<br />
3. Full Accreditation Report must be from a Nationally Recognized Organization; such as:<br />
i.e.; JCAHO, AAAHC, AOA, CARF and CHAP. The report must include all surveyed<br />
locations.<br />
62
ARIZONA DEPARTMENT OF HEALTH SERVICES<br />
DIVISION OF LICENSING SERVICES<br />
150 N. 18 th Avenue, Suite 450, Phoenix, <strong>Arizona</strong> 85007 *** 400 W. Congress, #116, Tucson, <strong>Arizona</strong> 85701<br />
RENEWAL APPLICATION FOR A HEALTH CARE INSTITUTION LICENSE<br />
A.R.S. Title 36, Chapter 4 and A.A.C. Title 9<br />
I. HEALTH CARE INSTITUTION INFORMATION<br />
Name of <strong>Health</strong> Care Institution<br />
Physical Address (optional) City State Zip Code<br />
Mailing Address City State Zip Code<br />
Telephone number Fax number E-mail address (optional)<br />
<strong>Health</strong> care institution class or subclass: License Number Expiration Date<br />
II. OWNER INFORMATION (Name of Corporation or LLC, etc.)<br />
Owner’s name<br />
Address<br />
City<br />
Telephone number<br />
Zip code<br />
Fax number<br />
The owner is a: (check one) Proprietary (For Profit) Non-proprietary (Non-Profit)<br />
The owner is a: (check one) _____Sole proprietorship _____Partnership<br />
_____Limited liability company _____Corporation _____Governmental Agency<br />
A. PLEASE LIST IN THE SPACE PROVIDED BELOW:<br />
If the owner is a partnership, the name of each partner;<br />
If the owner is a limited liability company, the name of the designated manager, or if no manager is designated, the names<br />
of any 2 members of the limited liability company;<br />
If the owner is a corporation, the name and title of each corporate officer; or<br />
If the owner is a governmental agency, the name and title of the individual in charge of the governmental agency or the<br />
individual designated in writing by the individual in charge of the governmental agency.<br />
Name<br />
Name<br />
Name<br />
Title<br />
Title<br />
Title<br />
Name<br />
Title<br />
B. Has the person applying <strong>for</strong> a license or a person with 10% or more business interest in the health care institution had a<br />
license to operate a health care institution denied, revoked or suspended since the last application was submitted<br />
____Yes ____ No.<br />
C. Has the person applying <strong>for</strong> a license or a person with 10% or more business interest in the health care institution had a<br />
health care professional license or certificate denied, revoked or suspended since the last application was submitted<br />
____Yes ____ No.<br />
63
D. If either of the previous questions is answered yes, include on a separate sheet of paper <strong>for</strong> each yes answer:<br />
1. The reason <strong>for</strong> the denial, suspension, or revocation;<br />
2. The date of the denial, suspension, or revocation;<br />
3. The name and address of the licensing agency that denied, suspended, or revoked the license.<br />
Statutory agent (or individual designated to accept service of process and subpoenas)<br />
Name<br />
Title<br />
Address<br />
III. GOVERNING AUTHORITY<br />
Telephone number<br />
Name<br />
IV. CHIEF ADMINISTRATIVE OFFICER (Facility Administrator)<br />
Name<br />
Title<br />
Education (list the highest educational degree obtained and any instruction related to the health care institution class or subclass<br />
<strong>for</strong> which licensure is requested)<br />
Experience (list work experience related to the health care institution class or subclass <strong>for</strong> which licensure is requested)<br />
V. SIGNATURES<br />
According to A.R.S. § 36-422(B) the application must be signed, as follows:<br />
(1) If an individual, by the owner of the institution;<br />
(2) If a partnership or corporation, by two of the partners or corporate officers; or<br />
(3) If a governmental unit, the head of the governmental department having jurisdiction.<br />
_____________________________________________<br />
Signature<br />
Date<br />
_____________________________________________<br />
Title<br />
_____________________________________________<br />
Signature<br />
Date<br />
_____________________________________________<br />
Title<br />
VI. TIME FRAME<br />
Pursuant to A.R.S. § 41-1075 The applicant agrees to extend the substantive review time frame if necessary. This will not exceed 25% of the<br />
overall time frame.<br />
Provider Signature:______________________________________ Representative of DHS:_______________________________________<br />
For DHS use only: Correct application fee enclosed: Yes No Check #:<br />
64
MEDICAL FACILITIES LICENSING<br />
150 N. 18 th Avenue, Suite 450<br />
Phoenix, <strong>Arizona</strong> 85007<br />
HEALTH CARE INSTITUTION RENEWAL APPLICATION<br />
AND LICENSE FEE REMITTANCE FORM<br />
PLEASE RETURN THIS FORM WITH THE PAYMENT TO THE ADDRESS ABOVE<br />
FACILITY I.D. #: LICENSE #: LEVEL OF CARE<br />
OR SERVICES<br />
APPLICANT/ENTITY NAME:<br />
FACILITY NAME:<br />
STREET ADDRESS: SUITE #:<br />
CITY: STATE: ZIP:<br />
PHYSICAL ADDRESS:<br />
CITY: STATE: ZIP:<br />
FEES<br />
Application Fee<br />
(Please do not submit the application fee if the fee has already been paid.)<br />
AMOUNT DUE<br />
$ 50.00<br />
LICENSED CAPACITY<br />
Check One: Licensed Capacity: Base Fee: Number of Beds x<br />
$10.00 each:<br />
Total base fee plus number<br />
of beds fee:<br />
None $ 100.00 $<br />
1 to 59 beds 100.00<br />
60 to 99 beds 200.00<br />
100 to 149 beds 300.00<br />
150 or more beds 500.00<br />
TOTAL AMOUNT DUE $<br />
Payment should be by cashier=s check, money order or business check made payable to:<br />
ARIZONA DEPARTMENT OF HEALTH SERVICES<br />
Write the Facility I.D. # on the check.<br />
Cash and personal checks are not accepted.<br />
AMOUNT ENCLOSED $<br />
ALL FEES ARE NON-REFUNDABLE pursuant to A.R.S. ' 36-405(c), 36-882(f) and 36-897.01(c), except as provided in<br />
A.R.S. ' 41-1077.<br />
65
LICENSE APPLICATION FOR HEALTH<br />
CARE INSTITUTION AND REQUIRED<br />
ATTACHMENTS CHECKLIST<br />
RENEWAL<br />
Your license application packet must include the following:<br />
9 License Application For <strong>Health</strong> Care Institution<br />
9 $50.00 Application Fee (Please include license number of<br />
facility/agency).<br />
9 License Fee (See Remittance Form <strong>for</strong> License Fees)<br />
9 Services and Staffing Provided Form<br />
9 Current Fire Inspection Report<br />
9 Resume <strong>for</strong> Administrator<br />
9 Lease Agreement (if applicable)<br />
9 Board of Directors or list of Officers of the Corporation<br />
9 Bed Count (if applicable)<br />
9 Accreditation Report and Cover Letter (if applicable)<br />
9 Current Food Service Report (if applicable)<br />
9 Roster <strong>for</strong> T.B. and Fingerprinting <strong>for</strong> the current 12 months of Home<br />
<strong>Health</strong> Agency staff.<br />
9 FOR SURGERY CENTERS: Please contact the Architectural Review<br />
Unit at (602) 364-3055 <strong>for</strong> Architect Certification For <strong>Health</strong> Care<br />
Institutions application.<br />
NOTE:<br />
1. DO NOT use correction fluid or correction tape on the license application.<br />
Applications must have original signatures. Photocopies of signatures will<br />
not be accepted.<br />
2. The Application Fee must be made payable to the <strong>Arizona</strong> Department of<br />
<strong>Health</strong> Services. Please include the license number of the facility/agency.<br />
3. Accreditation Report must be from a Nationally Recognized Organization;<br />
such as: ie; JCAHO, AAAHC, AOA, CARF, AAASF, AABB, ASHI,<br />
COLA, CAP and CHAP. The report must include all surveyed locations.<br />
66
http://www.azdhs.gov/als/<strong>for</strong>ms/otcstaff.htm<br />
Page 1 of 2<br />
8/14/2008<br />
OUTPATIENT FACILITY INFORMATION<br />
Name<br />
Date<br />
Address<br />
Phone<br />
1. Hours of operation: (indicate hours clinic is open, i.e., 8-4; 12-6)<br />
Sun Mon Tue Wed Thur Fri Sat<br />
2. A. Medical Director _______________________________________________<br />
(if applicable)<br />
(name)<br />
B. Director of Nursing _______________________________________________<br />
(if applicable)<br />
(name)<br />
C. Number of Staff Physicians (excluding Medical Director) F/T _____ P/T _____<br />
3. Administrative Staff:<br />
Person in charge of Medical Records ___________________________________<br />
4.<br />
Other Employees Staffing F/T P/T Other Employees Staffing F/T P/T<br />
Nurse Practitioners Housekeeping<br />
Physician Assistants Maintenance<br />
R.N.'s X-ray Techs<br />
L.P.N.'s Social Workers<br />
Nurse's Aides Respiratory Therapists<br />
Pharmacists Nutritionists<br />
Laboratory Techs Others<br />
5. SERVICES OFFERED:<br />
Dental<br />
Emergency Care<br />
E.K.G.<br />
Family Planning<br />
Home <strong>Health</strong> Care<br />
Immunizations<br />
Inhalation Therapy<br />
Laboratory<br />
Maternity<br />
Outpatient Surgery<br />
Pharmacy<br />
Podiatric Services<br />
Social Services<br />
Substance Abuse Services<br />
T.B. Screening<br />
Well-baby <strong>Clinic</strong><br />
W.I.C. Program<br />
67
http://www.azdhs.gov/als/<strong>for</strong>ms/otcstaff.htm<br />
Page 2 of 2<br />
8/14/2008<br />
X-ray<br />
V.D. Detection/Treatment<br />
Opth. Testing<br />
Other<br />
68
Appendix F. Certification Forms<br />
1. CMS-29 REQUEST TO ESTABLISH ELIGIBILITY TO PARTICIPATE IN HEALTH<br />
INSURANCE I FOR AGED/DISABLED TO PROVIDE RURAL HEALTH CLINIC SER<br />
VICES- Pages 71-73<br />
2. CMS-1561A HEALTH INSURANCE BENEFIT AGREEMENT- RURAL HEALTH CLINIC-<br />
Page 74<br />
**Please note: THREE ORIGINAL COPIES of this <strong>for</strong>m are required to be submitted with the<br />
application packet.<br />
3. CMS-1513 DISCLOSURE OF OWNERSHIP & CONTROL INTEREST STATEMENT-<br />
Pages 75-78<br />
4. HHS-690 CIVIL RIGHTS ASSURANCE OF COMPLIANCE- Page 79<br />
**Please note: THREE ORIGINAL COPIES of this <strong>for</strong>m are required to be submitted with the<br />
application packet.<br />
5. CMS-855A MEDICARE ENROLLMENT APPLICATION- INSTITUTIONAL PROVID-<br />
ERS- Page 80<br />
**Please note: This <strong>for</strong>m must be submitted directly to the FISCAL INTERMEDIARY.<br />
Only the cover page of the 42-page CMS-855A Form has been included in this manual.<br />
To obtain a complete copy of the CMS - 855A Application please go to<br />
http://www.cms.hhs.gov/cms<strong>for</strong>ms/downloads/cms855a.pdf<br />
6. CMS-222-92 INDEPENDENT RURAL HEALTH CLINIC WORKSHEET (Cost Report)-<br />
Pages 81-82<br />
All CMS <strong>for</strong>ms are available online at: http://www.cms.hhs.gov/CMSForms/CMSForms/list.<br />
asp#TopOfPage<br />
69
INSTRUCTIONS FOR COMPLETING REQUEST TO ESTABLISH ELIGIBILITY TO PARTICIPATE IN THE<br />
HEALTH INSURANCE FOR THE AGED AND DISABLED PROGRAM<br />
TO PROVIDE RURAL HEALTH CLINIC SERVICES<br />
The filing of this request <strong>for</strong> eligibility will initiate the process of obtaining a decision as to whether the conditions <strong>for</strong> certification are met.<br />
Please do not delay returning the <strong>for</strong>m. Assistance in filling out the <strong>for</strong>m is available from the State agency.<br />
Please answer all questions as of the current date.<br />
GENERAL INSTRUCTIONS<br />
Return the <strong>for</strong>m to the State agency in the envelope provided; retain a copy <strong>for</strong> your files. If a return envelope is not provided, the name and<br />
address of the State agency may be obtained from the nearest Social Security Administration district office.<br />
Detailed Instructions <strong>for</strong> Specific Questions<br />
These instructions are designed to clarify certain questions on the <strong>for</strong>m. Instructions are listed in question order <strong>for</strong> easy reference. No<br />
instructions have been given <strong>for</strong> questions considered self-explanatory.<br />
The Following to be Completed by the Applicant<br />
Question I — Identifying In<strong>for</strong>mation<br />
Insert the full name under which the clinic operates. A rural health clinic site is the location at which health services are furnished. If a <br />
central organization operates more than one clinic site, a seperate Request to Establish Eligibility Application <strong>for</strong> each rural health clinic<br />
site must be submitted. In these instances, the location of the health clinic site, rather than the central organization, will determine eligibility<br />
to participate and the applicant site must be situated in a rural area which is designated as either an area with a shortage of personal health<br />
services or as a health manpower shortage area because of its shortage of primary medical care manpower. If the name of the rural health<br />
clinic site does not identify the owner(s), the name and address of the owner(s) is to be inserted in the space provided, otherwise, that space<br />
is to be left blank.<br />
Question II — Medical Direction<br />
Insert the name and address of the physician(s) responsible <strong>for</strong> providing medical direction <strong>for</strong> the health clinic site.<br />
Question III — <strong>Clinic</strong> Personnel<br />
(A), (B), and (C) – Personnel are to be described in terms of full-time equivalents. To arrive at full-time equivalents, add the total number of<br />
hours worked by personnel in each category in the week ending prior to the week of filing the request and divide by the number of hours in<br />
the standard work week (as determined by clinic policies). If the result is not a whole number, express it as a quarter fraction only (e.g., .00,<br />
.25, .50, or .75).<br />
Exclude all trainees and volunteers.<br />
A nurse practitioner and/or physician assistant in addition to the physician, is required <strong>for</strong> clinic eligibility and must be shown in B and/or C<br />
respectively.<br />
(D) – Where other types of personnel are utilized (e.g., technicians, aides, etc.), the discipline, by name, is to be indicated in addition to the<br />
full-time equivalents.<br />
Under (A), (B) and (C), include in the count only those defined as follows:<br />
Physician — A doctor of medicine or osteopathy legally authorized to practice medicine and surgery by the State in which such function<br />
or action is per<strong>for</strong>med. (A physician listed in II. above, should be included in this category <strong>for</strong> purposes of determining full-time<br />
equivalents.)<br />
Nurse Practitioner — A registered professional nurse who is currently licensed to practice in the State, who meets the State's requirements<br />
governing the qualifications of nurse practitioners and who meets one of the following conditions:<br />
1. Is currently certified as a primary care Nurse Practitioner by the American Nurses Association or by the National Board of Pediatric<br />
Nurse Practitioners and Associates; or<br />
2. Has satisfactorily completed a <strong>for</strong>mal one academic year educational program that:<br />
(i) prepares registered nurses to per<strong>for</strong>m an expanded role in the delivery of primary care;<br />
(ii) includes at least four months (in the aggregate) of classroom instruction and a component of supervised clinic practice; and<br />
(iii) awards a degree, diploma, or certificate to persons who successfully complete the program; or<br />
Form CMS-29 (05/78) INSTRUCTIONS 70
3. Has successfully completed a <strong>for</strong>mal educational program <strong>for</strong> preparing registered nurses to per<strong>for</strong>m an expanded role in the delivery<br />
of primary care that does not meet the requirements of paragraph (2) of this section, and has been per<strong>for</strong>ming an expanded role in<br />
the delivery of primary care <strong>for</strong> a total of 12 months during the 18-month period immediately preceding the effective date of this<br />
subpart.<br />
Physician Assistant — A person who meets the applicable State requirements governing the qualifications <strong>for</strong> assistants to primary care<br />
physicians and who meets at least one of the following conditions:<br />
1. Is currently certified by the National Commission on Certification of Physician Assistants to assist primary care physicians: or<br />
2. Has satisfactorily completed a program <strong>for</strong> preparing physician's assistants that:<br />
(i) was at least one academic year in length;<br />
(ii) consisted of supervised clinical practice and at least four months (in the aggregate) of classroom instruction directed toward<br />
preparing students to deliver health care; and<br />
(iii) was accredited by the American Medical Association's Committee on Allied <strong>Health</strong> Education and Accreditation; or<br />
3. Has satisfactorily completed a <strong>for</strong>mal educational program <strong>for</strong> preparing physician assistants that does not meet the requirements of<br />
paragraph (2) of this section and has been assisting primary care physicians <strong>for</strong> a total of 12 months during the 18-month period<br />
immediately preceding the effective date of this subpart.<br />
Question IV – Type of Control<br />
Identify the rural health clinic in terms of its control by checking the appropriate part of A, B, C or D. Nonprofit status is based on<br />
Internal Revenue Service tax exemption interpretation; i.e., section 501 of the Internal Revenue Code of 1954.<br />
The following, where applicable, is to be completed in addition to the above. Those rural health clinic sites which are associated with any<br />
existing Medicare provider; i.e., both are licensed as a single health entity; the rural health clinic site and the provider are subject to the<br />
bylaws and operating decisions of the same governing body; and the medical personnel of the rural health clinic site are considered by<br />
the governing body to be subject to the rules of the provider's medical staff, are to indicate this alliance by showing the Medicare provider<br />
number of the facility in the appropriate space.<br />
State Agency Responsibility<br />
The State agency, when reviewing IV. Type of Control, should refer to 2208 of the State Operations <strong>Manual</strong>.<br />
A function of the resurvey process is to obtain updated statistical in<strong>for</strong>mation on organizations providing rural health clinic services. At<br />
the time of resurvey, the surveyor will bring this <strong>for</strong>m with him and request that a representative of the organization complete, sign, and<br />
date it and return it to him at the completion of the onsite visit. The surveyor will review the <strong>for</strong>m <strong>for</strong> completeness and accuracy and<br />
place his initials after the signature of the organization's representative. On all resurveys insert the clinic's assigned six-digit provider<br />
number. Do not complete the categories identified as State/County or State Region at anytime; the regional office will complete these<br />
items.<br />
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of in<strong>for</strong>mation unless it displays a valid<br />
0MB control number. The valid 0MB control number <strong>for</strong> this in<strong>for</strong>mation collection is 0938-0074. The time required to complete this in<strong>for</strong>mation<br />
collection is estimated to average 15 minutes per response, including the time to review instructions, search existing data resources, gather<br />
the data needed, and complete and review the in<strong>for</strong>mation collection. If you have any comments concerning the accuracy of the time<br />
estimate(s) or suggestions <strong>for</strong> improving this <strong>for</strong>m, please write to CMS, Attn: PRA Reports Clearance Officer, 7500 Security Boulevard,<br />
Baltimore, Maryland 21244-1850.<br />
71
DEPARTMENT OF HEALTH AND HUMAN SERVICES<br />
CENTERS FOR MEDICARE & MEDICAID SERVICES<br />
REQUEST TO ESTABLISH ELIGIBILITY TO PARTICIPATE IN THE<br />
HEALTH INSURANCE FOR THE AGED AND<br />
DISABLED PROGRAM TO PROVIDE RURAL HEALTH CLINIC SERVICES<br />
PROVIDER NO.<br />
FORM APPROVED<br />
OMB N0. 0938-0074<br />
Each rural health clinic site providing rural health clinic services and desiring<br />
STATE/COUNTY (RH2)<br />
to establish eligibility in the health insurance program should complete this<br />
<strong>for</strong>m and return it to the State agency that is handling the certification process.<br />
If a return envelope is not provided, the name and address of the State<br />
STATE REGION (RH3)<br />
agency may be obtained from the nearest Social Security Administration<br />
district office.<br />
I.<br />
NAME OF CLINIC<br />
STREET ADDRESS<br />
IDENTIFYING<br />
INFORMATION<br />
(TO BE COMPLETED<br />
FOR EACH CLINIC SITE) CITY, COUNTY AND STATE<br />
ZIP CODE<br />
TELEPHONE NO. (Including Area Code)<br />
(RH1)<br />
(RH2)<br />
(RH3)<br />
(RH4)<br />
NAME AND<br />
ADDRESS<br />
OF<br />
CLINIC OWNER(S)<br />
II.<br />
(RH5)<br />
MEDICAL<br />
DIRECTION<br />
III.<br />
IV.<br />
CLINIC<br />
PERSONNEL<br />
(FULL TIME<br />
EQUIVALENTS)<br />
(A) PHYSICIAN<br />
(B) NURSE<br />
PRACTITIONER<br />
(C) PHYSICIAN<br />
ASSISTANT<br />
(D) OTHER<br />
(RH6) (RH7) (RH8) (RH9)<br />
A. INDIVIDUAL B. CORPORATION C. PARTNERSHIP D. GOVERNMENT<br />
TYPE OF<br />
CONTROL<br />
(check one)<br />
1. PROFIT<br />
2. NON-<br />
PROFIT<br />
STATE<br />
3.<br />
LOCAL<br />
4.<br />
FEDERAL<br />
5.<br />
V.<br />
FEDERAL<br />
SUPPORT<br />
(RH10)<br />
If the rural health clinic site is part of an existing<br />
Medicare provider, indicate the provider number___________________<br />
Is this clinic site receiving support from a Federal Program<br />
to provide health services in a medically underserved area<br />
or in an area with a shortage of primary care health manpower YES NO<br />
TITLE OF FEDERAL PROGRAM: ____________________________________________<br />
Is this clinic participating in the Physician Extender Experiment<br />
Program (Section 222)<br />
YES NO<br />
(RH11)<br />
(RH12)<br />
(RH13)<br />
(RH14)<br />
I certify that this application is true, correct, and complete. I agree, if approval is granted, that all services rendered by the<br />
clinic shall be in con<strong>for</strong>mity with Federal, State, and local laws. I further understand that a violation of such laws will<br />
constitute grounds <strong>for</strong> withdrawal of approval under the regulations. This in<strong>for</strong>mation will not be released to any persons or<br />
organizations outside the official administrative channels unless the undersigned individual specifically requests in writing<br />
that such disclosures be made. (Privacy Act of 1974 Public Law 93–579.)<br />
SIGNATURE OF AUTHORIZED OFFICIAL TITLE DATE<br />
Form CMS-29 (05/78) 72<br />
(RH15)
DEPARTMENT OF HEALTH AND HUMAN SERVICES<br />
FORM APPROVED<br />
CENTERS FOR MEDICARE & MEDICAID SERVICES OMB No. 0938-0832<br />
HEALTH INSURANCE BENEFITS AGREEMENT<br />
(Agreement with <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> Pursuant to<br />
Section 1861(aa)(2)(K)(ii) of the Social Security Act)<br />
For the purpose of establishing eligibility <strong>for</strong> payment under Title XVIII of the Social Security Act,<br />
hereafter referred to as the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong>, hereby agrees:<br />
(Insert name of clinic)<br />
(A) to maintain compliance with the conditions <strong>for</strong> certification set <strong>for</strong>th in part 491 of chapter IV, title 42 of the Code of Federal<br />
Regulations, and to report promptly to the <strong>Center</strong>s <strong>for</strong> Medicare & Medicaid Services any failure to do so;<br />
(B) not to charge the beneficiary or any other person <strong>for</strong> items and services <strong>for</strong> which the beneficiary is entitled to have payment<br />
made under the provisions of part 405 of chapter IV, title 42 of the Code of Federal Regulations (or <strong>for</strong> which the beneficiary<br />
would have been entitled if the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> had filed a request <strong>for</strong> payment in accordance with §410.165 of chapter IV),<br />
except <strong>for</strong> any deductible or coinsurance amounts <strong>for</strong> which the beneficiary is liable under §405.2410;<br />
(C) to refund as promptly as possible any money incorrectly collected from a beneficiary or from someone on his or her behalf;<br />
(D) to accept beneficiaries <strong>for</strong> care and treatment without limitations, except as it may impose on all other persons;<br />
(E) to accept any additional provisions that the Secretary finds necessary or desirable <strong>for</strong> the efficient and effective administration<br />
of the Medicare program.<br />
This agreement, upon submission by the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> and upon acceptance <strong>for</strong> filing by the Secretary of <strong>Health</strong> and Human<br />
Services, shall be binding on the <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> and the Secretary. The agreement may be terminated by either party in<br />
accordance with regulations. In the event of termination, payment will not be available <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> services furnished on<br />
or after the effective date of termination.<br />
This agreement shall become effective on the date specified below by the Secretary or the Secretary’s delegate, and shall remain in<br />
effect unless terminated.<br />
In the event of a transfer of ownership, the agreement is automatically assigned to the new owner subject to the conditions specified<br />
in this agreement and 42 CFR 489, to include existing plans of correction and the duration of this agreement, if the agreement is<br />
time limited.<br />
ATTENTION: Read the following provision of Federal law carefully be<strong>for</strong>e signing.<br />
Whoever, in any matter within the jurisdiction of any department or agency of the United States knowingly and willfully falsifies,<br />
conceals or covers up by any trick, scheme or device a material fact, or make any false, fictitious or fraudulent statement or<br />
representation, or makes or uses any false writing or document knowing the same to contain any false, fictitious or fraudulent<br />
statement, or entry, shall be fined not more than $10,000 or imprisoned not more than 5 years or both (18 U.S.C. section 1001).<br />
Accepted <strong>for</strong> <strong>Rural</strong> <strong>Health</strong> <strong>Clinic</strong> by:<br />
NAME (SIGNATURE)<br />
TITLE<br />
DATE<br />
Accepted <strong>for</strong> the Secretary of <strong>Health</strong> and Human Services by:<br />
NAME (SIGNATURE)<br />
TITLE<br />
DATE<br />
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of in<strong>for</strong>mation unless it displays a valid<br />
OMB control number. The valid OMB control number <strong>for</strong> this in<strong>for</strong>mation collection is 0938-0832. The time required to complete this in<strong>for</strong>mation<br />
collection is estimated to average 5 minutes per response, including the time to review instructions, search existing data resources, gather the data<br />
needed, and complete and review the in<strong>for</strong>mation collection. If you have any comments concerning the accuracy of the time estimate(s) or<br />
suggestions <strong>for</strong> improving this <strong>for</strong>m, please write to CMS, 7500 Security Boulevard, N2-14-26, Baltimore, Maryland 21244-1850.<br />
Form CMS-1561A (4-02) Previous version obsolete 73
DEPARTMENT OF HEALTH AND HUMAN SERVICES<br />
CENTERS FOR MEDICARE & MEDICAID SERVICES<br />
INSTRUCTIONS FOR COMPLETING DISCLOSURE OF<br />
OWNERSHIP AND CONTROL INTEREST STATEMENT (CMS-1513)<br />
Completion and submission of this <strong>for</strong>m is a condition of participation, certification, or recertification under any of the programs established by titles V,<br />
XVIII, XIX, and XX, or as a condition of approval or renewal of a contractor agreement between the disclosing entity and the Secretary of appropriate<br />
State agency under any of the above-titled programs, a full and accurate disclosure of ownership and financial interest is required. Failure to submit<br />
requested in<strong>for</strong>mation may result in a refusal by the Secretary or appropriate State agency to enter into an agreement or contract with any such<br />
institution or in termination of existing agreements.<br />
SPECIAL INSTRUCTIONS FOR TITLE XX PROVIDERS<br />
Form Approved<br />
OMB No. 0938-0086<br />
All title XX providers must complete part II (a) and (b) of this <strong>for</strong>m. Only those title XX providers rendering medical, remedial, or health related homemaker<br />
services must complete parts II and III. Title V providers must complete parts II and Ill.<br />
General Instructions<br />
For definitions, procedures and requirements, refer to the appropriate<br />
Regulations:<br />
Title V – 42CFR 51a.144<br />
Title XVIII – 42CFR 420.200 – 206<br />
Title XIX – 42CFR 455.100 – 106<br />
Title XX – 45CFR 228.72 – 73<br />
Please answer all questions as of the current date. If the yes block <strong>for</strong><br />
any item is checked, list requested additional in<strong>for</strong>mation under the<br />
Remarks section on page 2, referencing the item number to be<br />
continued. If additional space is needed use an attached sheet.<br />
Return the original and second and third copies to the State<br />
agency; retain the first copy <strong>for</strong> your files.<br />
This <strong>for</strong>m is to be completed annually. Any substantial delay in<br />
completing the <strong>for</strong>m should be reported to the State survey agency.<br />
DETAILED INSTRUCTIONS<br />
These instructions are designed to clarify certain questions on the<br />
<strong>for</strong>m. Instructions are listed in question order <strong>for</strong> easy reference. No<br />
instructions have been given <strong>for</strong> questions considered self-explanatory.<br />
IT IS ESSENTIAL THAT ALL APPLICABLE QUESTIONS BE<br />
ANSWERED ACCURATELY AND THAT ALL INFORMATION BE<br />
CURRENT.<br />
Item I (a) Under identifying in<strong>for</strong>mation specify in what capacity the<br />
entity is doing business as (DBA), example, name of<br />
trade or corporation.<br />
(b) For Regional Office Use Only. If the yes box is checked <strong>for</strong><br />
item VII, the Regional Office will enter the 5-digit<br />
number assigned by CMS to chain organizations.<br />
Item II - Self-explanatory.<br />
Item III - List the names of all individuals and organizations having<br />
direct or indirect ownership interests, or controlling interest separately<br />
or in combination amounting to an ownership interest of 5 percent or<br />
more in the disclosing entity.<br />
Direct ownership interest is defined as the possession of stock, equity<br />
in capital or any interest in the profits of the disclosing entity. A<br />
disclosing entity is defined as a Medicare provider or supplier, or other<br />
entity that furnishes services or arranges <strong>for</strong> furnishing services under<br />
Medicaid or the Maternal and Child <strong>Health</strong> program, or health related<br />
services under the social services program.<br />
Indirect ownership interest is defined as ownership interest in an entity<br />
that has direct or indirect ownership interest in the disclosing entity.<br />
The amount of indirect ownership in the disclosing entity that is held by<br />
any other entity is determined by multiplying the percentage of<br />
ownership interest at each level. An indirect ownership interest must be<br />
reported if it equates to an ownership interest of 5 percent or more in<br />
the disclosing entity. Example: if A owns 10 percent of the stock in a<br />
corporation that owns 80 percent of the stock of the disclosing entity,<br />
A's interest equates to an 8 percent indirect ownership and must be<br />
reported.<br />
Controlling interest is defined as the operational direction or<br />
management of a disclosing entity which may be maintained by any or<br />
all of the following devices: the ability or authority, expressed or<br />
reserved, to amend or change the corporate identity (i.e., joint venture<br />
agreement, unincorporated business status) of the disclosing entity; the<br />
ability or authority to nominate or name members of the Board of<br />
Directors or Trustees of the disclosing entity; the ability or authority,<br />
expressed or reserved, to amend or change the by-laws, constitution,<br />
or other operating or management direction of the disclosing entity; the<br />
right to control any or all of the assets or other property of the<br />
disclosing entity upon the sale or dissolution of that entity; the ability or<br />
authority, expressed or reserved, to control the sale of any or all of the<br />
assets, to encumber such assets by way of mortage or other<br />
indebtedness, to dissolve the entity, or to arrange <strong>for</strong> the sale or<br />
transfer of the disclosing entity to new ownership or control.<br />
Items IV – VII - Changes in Provider Status<br />
Change in provider status is defined as any change in management<br />
control. Examples of such changes would include: a change in Medical<br />
or Nursing Director, a new Administrator, contracting the operation of<br />
the facility to a management corporation, a change in the composition<br />
of the owning partnership which under applicable State law is not<br />
considered a change in ownership, or the hiring or dismissing of any<br />
employees with 5 percent or more financial interest in the facility or in<br />
an owning corporation, or any change of ownership.<br />
For Items IV – VII, if the yes box is checked, list additional in<strong>for</strong>mation<br />
requested under Remarks. Clearly identify which item is being continued.<br />
Item IV - (a & b) If there has been a change in ownership within the<br />
last year or if you anticipate a change, indicate the date in the<br />
appropriate space.<br />
Item V - If the answer is yes, list name of the management firm and<br />
employer identification number (EIN), or the name of the leasing<br />
organization. A management company is defined as any organization<br />
that operates and manages a business on behalf of the owner of that<br />
business, with the owner retaining ultimate legal responsibility <strong>for</strong><br />
operation of the facility.<br />
Item VI - If the answer is yes, identify which has changed<br />
(Administrator, Medical Director, or Director of Nursing) and the date<br />
the change was made. Be sure to include name of the new<br />
Administrator, Director of Nursing or Medical Director, as appropriate.<br />
Item VII - A chain affiliate is any free-standing health care facility that is<br />
either owned, controlled, or operated under lease or contract by an<br />
organization consisting of two or more free-standing health care<br />
facilities organized within or across State lines which is under the<br />
ownership or through any other device, control and direction of a<br />
common party. Chain affiliates include such facilities whether public,<br />
private, charitable or proprietary. They also include subsidiary<br />
organizations and holding corporations. Provider-based facilities, such<br />
as hospital-based home health agencies, are not considered to be<br />
chain affiliates.<br />
Item VIII - If yes, list the actual number of beds in the facility now and<br />
74 the previous number.
DEPARTMENT OF HEALTH AND HUMAN SERVICES<br />
Form Approved<br />
CENTERS FOR MEDICARE & MEDICAID SERVICES OMB NO. 0938-0086<br />
DISCLOSURE OF OWNERSHIP AND CONTROL INTEREST STATEMENT<br />
I. Identifying In<strong>for</strong>mation<br />
(a) Name of Entity<br />
D/B/A<br />
Provider No.<br />
Vendor No.<br />
Telephone No.<br />
Street Address<br />
City, County, State<br />
Zip Code<br />
(b) (To be completed by CMS Regional Office) Chain Affiliate No. ■ ■ ■ ■ ■ LB1<br />
II. Answer the following questions by checking "Yes" or "No." If any of the questions are answered "Yes," list names and addresses of individuals or corporations<br />
under Remarks on page 2. Identify each item number to be continued.<br />
(a) Are there any individuals or organizations having a direct or indirect ownership or control interest of 5 percent or more in the institution, organizations,<br />
or agency that have been convicted of a criminal offense related to the involvement of such persons, or organizations in any of the programs established<br />
by titles XVIII, XIX, or XX<br />
■ Yes ■ No LB2<br />
(b) Are there any directors, officers, agents, or managing employees of the institution, agency or organization who have ever been convicted of a criminal<br />
offense related to their involvement in such programs established by titles XVIII, XIX, or XX<br />
■ Yes ■ No LB3<br />
(c) Are there any individuals currently employed by the institution, agency, or organization in a managerial, accounting, auditing, or similar capacity who<br />
were employed by the institution's, organization's, or agency's fiscal intermediary or carrier within the previous 12 months (Title XVIII providers only)<br />
■ Yes ■ No LB4<br />
Ill. (a) List names, addresses <strong>for</strong> individuals, or the EIN <strong>for</strong> organizations having direct or indirect ownership or a controlling interest in the entity. (See instructions <strong>for</strong><br />
definition of ownership and controlling interest.) List any additional names and addresses under "Remarks" on page 2. If more than one individual is<br />
reported and any of these persons are related to each other, this must be reported under Remarks.<br />
Name Address EIN<br />
LB5<br />
(b) Type of Entity:<br />
■ Sole Proprietorship ■ Partnership ■ Corporation LB6<br />
■ Unincorporated Associations<br />
■ Other (Specify)<br />
(c) If the disclosing entity is a corporation, list names, addresses of the Directors, and EINs <strong>for</strong> corporations under Remarks.<br />
Check appropriate box <strong>for</strong> each of the following questions:<br />
(d) Are any owners of the disclosing entity also owners of other Medicare/Medicaid facilities (Example: sole proprietor, partnership or members of Board<br />
of Directors.) If yes, list names, addresses of individuals and provider numbers.<br />
■ Yes ■ No LB7<br />
Name Address Provider Number<br />
75<br />
CMS-1513 (5/86) Page 1
DEPARTMENT OF HEALTH AND HUMAN SERVICES<br />
Form Approved<br />
CENTERS FOR MEDICARE & MEDICAID SERVICES OMB NO. 0938-0086<br />
IV. (a) Has there been a change in ownership or control within the last year<br />
If yes, give date _____________ ■ Yes ■ No LB8<br />
(b) Do you anticipate any change of ownership or control within the year<br />
If yes, when _______________ ■ Yes ■ No LB9<br />
(c) Do you anticipate filing <strong>for</strong> bankruptcy within the year<br />
If yes, when _______________ ■ Yes ■ No LB10<br />
V. Is this facility operated by a management company, or leased in whole or part by another organization<br />
If yes, give date of change in operations ____________ ■ Yes ■ No LB11<br />
VI. Has there been a change in Administrator, Director of Nursing, or Medical Director within the last year<br />
■ Yes ■ No LB12<br />
VII. (a) Is this facility chain affiliated (If yes, list name, address of Corporation, and EIN)<br />
Name EIN # ■ Yes ■ No LB13<br />
Address<br />
LB14<br />
VII. (b) If the answer to Question VII.a. is No, was the facility ever affiliated with a chain<br />
(If yes, list Name, Address of Corporation, and EIN)<br />
Name EIN # ■ Yes ■ No LB18<br />
Address<br />
LB19<br />
VIII. Have you increased your bed capacity by 10 percent or more or by 10 beds, whichever is greater, within the last 2 years<br />
■ Yes ■ No LB15<br />
If yes, give year of change ____________<br />
Current beds _____________ LB16 Prior beds _____________ LB17<br />
WHOEVER KNOWINGLY AND WILLFULLY MAKES OR CAUSES TO BE MADE A FALSE STATEMENT OR REPRESENTATION OF THIS STATEMENT, MAY<br />
BE PROSECUTED UNDER APPLICABLE FEDERAL OR STATE LAWS. IN ADDITION, KNOWINGLY AND WILLFULLY FAILING TO FULLY AND ACCURATELY<br />
DISCLOSE THE INFORMATION REQUESTED MAY RESULT IN DENIAL OF A REQUEST TO PARTICIPATE OR WHERE THE ENTITY ALREADY PARTICIPATES,<br />
A TERMINATION OF ITS AGREEMENT OR CONTRACT WITH THE STATE AGENCY OR THE SECRETARY, AS APPROPRIATE.<br />
Name of Authorized Representative (Typed)<br />
Title<br />
Signature<br />
Date<br />
Remarks<br />
CMS-1513 (5/86) 76<br />
Page 2
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of in<strong>for</strong>mation unless it displays a valid 0MB control<br />
number. The valid 0MB control number <strong>for</strong> this in<strong>for</strong>mation collection is 0938-0086. The time required to complete this in<strong>for</strong>mation collection is estimated to<br />
average 30 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the<br />
in<strong>for</strong>mation collection. If you have any comments concerning the accuracy of the time estimate(s) or suggestions <strong>for</strong> improving this <strong>for</strong>m, please write to CMS,<br />
7500 Security Boulevard, N2-14-26, Baltimore, Maryland 21244-1850.<br />
77
ASSURANCE OF COMPLIANCE<br />
ASSURANCE OF COMPLIANCE WITH TITLE VI OF THE CIVIL RIGHTS ACT OF 1964, SECTION 504 OF THE REHABILITATION ACT OF<br />
1973, TITLE IX OF THE EDUCATION AMENDMENTS OF 1972, AND THE AGE DISCRIMINATION ACT OF 1975<br />
The Applicant provides this assurance in consideration of and <strong>for</strong> the purpose of obtaining Federal grants, loans, contracts, property, discounts<br />
or other Federal financial assistance from the Department of <strong>Health</strong> and Human Services.<br />
THE APPLICANT HEREBY AGREES THAT IT WILL COMPLY WITH:<br />
1. Title VI of the Civil Rights Act of 1964 (Pub. L. 88-352), as amended, and all requirements imposed by or pursuant to the Regulation<br />
of the Department of <strong>Health</strong> and Human Services (45 C.F.R. Part 80), to the end that, in accordance with Title VI of that Act and the<br />
Regulation, no person in the United States shall, on the ground of race, color, or national origin, be excluded from participation in, be<br />
denied the benefits of, or be otherwise subjected to discrimination under any program or activity <strong>for</strong> which the Applicant receives<br />
Federal financial assistance from the Department.<br />
2. Section 504 of the Rehabilitation Act of 1973 (Pub. L. 93-112), as amended, and all requirements imposed by or pursuant to the<br />
Regulation of the Department of <strong>Health</strong> and Human Services (45 C.F.R. Part 84), to the end that, in accordance with Section 504 of<br />
that Act and the Regulation, no otherwise qualified handicapped individual in the United States shall, solely by reason of his handicap,<br />
be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity<br />
<strong>for</strong> which the Applicant receives Federal financial assistance from the Department.<br />
3. Title IX of the Educational Amendments of 1972 (Pub. L. 92-318), as amended, and all requirements imposed by or pursuant to the<br />
Regulation of the Department of <strong>Health</strong> and Human Services (45 C.F.R. Part 86), to the end that, in accordance with Title IX and the<br />
Regulation, no person in the United States shall, on the basis of sex, be excluded from participation in, be denied the benefits of, or<br />
be otherwise subjected to discrimination under any education program or activity <strong>for</strong> which the Applicant receives Federal financial<br />
assistance from the Department.<br />
4. The Age Discrimination Act of 1975 (Pub. L. 94-135), as amended, and all requirements imposed by or pursuant to the Regulation of<br />
the Department of <strong>Health</strong> and Human Services (45 C.F.R. Part 91), to the end that, in accordance with the Act and the Regulation, no<br />
person in the United States shall, on the basis of age, be denied the benefits of, be excluded from participation in, or be subjected to<br />
discrimination under any program or activity <strong>for</strong> which the Applicant receives Federal financial assistance from the Department.<br />
The Applicant agrees that compliance with this assurance constitutes a condition of continued receipt of Federal financial assistance, and that it<br />
is binding upon the Applicant, its successors, transferees and assignees <strong>for</strong> the period during which such assistance is provided. If any real<br />
property or structure thereon is provided or improved with the aid of Federal financial assistance extended to the Applicant by the Department,<br />
this assurance shall obligate the Applicant, or in the case of any transfer of such property, any transferee, <strong>for</strong> the period during which the real<br />
property or structure is used <strong>for</strong> a purpose <strong>for</strong> which the Federal financial assistance is extended or <strong>for</strong> another purpose involving the provision<br />
of similar services or benefits. If any personal property is so provided, this assurance shall obligate the Applicant <strong>for</strong> the period during which it<br />
retains ownership or possession of the property. The Applicant further recognizes and agrees that the United States shall have the right to seek<br />
judicial en<strong>for</strong>cement of this assurance.<br />
The person or persons whose signature(s) appear(s) below is/are authorized to sign this assurance, and commit the Applicant to the above<br />
provisions.<br />
Date<br />
Signature and Title of Authorized Official<br />
Name of Applicant or Recipient<br />
Street<br />
Mail Form to:<br />
DHHS/Office <strong>for</strong> Civil Rights<br />
Office of Program Operations<br />
Humphrey Building, Room 509F<br />
200 Independence Ave., S.W.<br />
Washington, D.C. 20201<br />
Form HHS-690<br />
5/97<br />
City, State, Zip Code<br />
78
MEDICARE ENROLLMENT APPLICATION<br />
INSTITUTIONAL PROVIDERS<br />
CMS-855A<br />
SEE PAGE 1 TO DETERMINE IF YOU ARE COMPLETING THE CORRECT APPLICATION<br />
SEE PAGE 2 FOR INFORMATION ON WHERE TO MAIL THIS APPLICATION.<br />
SEE PAGE 41 TO FIND A LIST OF THE SUPPORTING DOCUMENTATION THAT MUST BE<br />
SUBMITTED WITH THIS APPLICATION.<br />
79
03-02 Form CMS 222-92<br />
2990 (Cont.)<br />
FORM APPROVED<br />
OMB NO: 0938-0107<br />
WORKSHEET S - PART I<br />
INDEPENDENT RURAL HEALTH CLINIC/FREESTANDING For Intermediary Use<br />
FEDERALLY QUALIFIED HEALTH CENTER WORKSHEET Date Received<br />
STATISTICAL DATA AND CERTIFICATION STATEMENT<br />
This report is required by law (42 USC. 1395g: CFR 413.20(b)). Failure to report can<br />
Intermediary Number<br />
result in all payments made during the reporting period being deemed overpayments (42 USC 1395g).<br />
PART I - STATISTICAL DATA [ ] Projected Cost Report [ ] Actual/Final Cost Report<br />
1. Facility Name and Address 1a. County<br />
2. Facility Number 3. <strong>Designation</strong> 4. Reporting Period<br />
From<br />
To<br />
5. Type of Control (Check One)<br />
A. Voluntary Non Profit B. Proprietary C. Government<br />
[ ] Corporation [ ] Individual [ ] Partnership [ ] Federal [ ] County<br />
[ ] Other (Specify) [ ] Corporation [ ] Other (Specify) [ ] State [ ] Other<br />
(Specify)<br />
[ ] City<br />
6. Source of Federal Funds GRANT AWARD DATE<br />
NUMBER<br />
A. Community <strong>Health</strong> <strong>Center</strong> (Section 330(d),<br />
Public <strong>Health</strong> Service Act)<br />
B. Migrant <strong>Health</strong> <strong>Center</strong><br />
(Section 329 (d), PHS Act)<br />
C. <strong>Health</strong> Services <strong>for</strong> the Homeless<br />
(Section 340(d), PHS Act)<br />
D. Appalachian Regional Commission<br />
E . Look-Alikes<br />
F. Other (Specify)<br />
7. Names of Physicians Furnishing Services At The <strong>Health</strong> Facility or Under Agreement<br />
(As Described In Instructions) And Medicare Billing Numbers (Include All Part B Billing Numbers)<br />
Name<br />
Billing Number<br />
8. Supervisory Physicians<br />
Name Hours of Supervision<br />
For Reporting Period<br />
FORM CMS-222-92 (10/96) (INSTRUCTIONS FOR THIS WORKSHEET ARE PUBLISHED IN CMS PUB. 15-II,<br />
SECTIONS 2903 and 2903.1)<br />
Rev. 5 29-303<br />
80
2990 (Cont.) Form CMS 222-92<br />
03-02<br />
INDEPENDENT RURAL HEALTH CLINIC/<br />
WORKSHEET S<br />
FEDERALLY QUALIFIED HEALTH CENTER WORKSHEET<br />
PART I (Cont.) &<br />
STATISTICAL DATA AND CERTIFICATION STATEMENT<br />
PART II<br />
PART I (CONTINUED)-STATISTICAL DATA<br />
9. If the facility operates as other than an RHC or FQHC (i.e., as a physicians office, independent<br />
laboratory, etc.) check yes and specify what type of operation and what days and hours RHC/FQHC<br />
services and other than RHC or FQHC services are provided at the facility as instructed below.<br />
YES [ ] NO [ ]<br />
Type of Operation ______________________________________________________________________<br />
Identify days and hours by listing the time the facility operates as an RHC or FQHC next to the applicable da<br />
Sunday _____________________<br />
Monday ____________________<br />
Tuesday ____________________<br />
Wednesday _________________<br />
Thursday ____________________<br />
Friday ______________________<br />
Saturday ____________________<br />
Identify days and hours by listing the time the facility operates as other than an RHC or FQHC next to<br />
the applicable day(s)<br />
Sunday _______________________<br />
Monday ______________________<br />
Tuesday ______________________<br />
Wednesday ___________________<br />
Thursday _______________________<br />
Friday __________________________<br />
Saturday ________________________<br />
PART II - CERTIFICATION BY OFFICER OR ADMINISTRATOR<br />
MISREPRESENTATION OR FALSIFICATION OF ANY INFORMATION CONTAINED IN THIS COAT REPORT M<br />
BE PUNISHABLE BY CRIMINAL, CIVIL AND ADMINISTRATIVE ACTION, FINE AND/OR IMPRISONMENT UND<br />
FEDERAL LAW. FURTHERMORE, IF SERVICES IDENTIFIED IN THIS REPORT WERE PROVIDED OR PROC<br />
THROUGH THE PAYMENT DIRECTLY OR INDIRECTLY OF A KICKBACK OR WHERE OTHERWISE ILLEGAL<br />
CRIMINAL, CIVIL AND ADMINISTRATIVE ACTION, FINES AND/OR IMPRISONMENT MAY RESULT.<br />
CERTIFICATION BY OFFICER OR ADMINISTRATOR<br />
I HEREBY CERTIFY that I have read the above statement and that I have examined the accompanying cost<br />
report prepared by<br />
(Provider Name and Number) <strong>for</strong> the<br />
cost report period beginning and ending and that to the best of my knowle<br />
and belief, it is a true, correct and complete statement prepared from the books and records of the<br />
Provider in accordance with the laws and regulations regarding the Provider in accordance with the laws and<br />
regulations regarding the provision of health care services and that the services identified in this cost report w<br />
provided in compliance with such laws and regulations.<br />
(Signed)<br />
Officer or Administrator of Facility Title Date<br />
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of in<strong>for</strong>mation unless it displays a<br />
valid OMB control number. The valid OMB control number <strong>for</strong> this in<strong>for</strong>mation collection is 0938-0107. The time required to complete this<br />
in<strong>for</strong>mation collection is estimated to average 50 hours per response, including the time to review instructions, search existing data<br />
resources, gather the data needed, and complete and review the in<strong>for</strong>mation collection. If you have any comments concerning the<br />
accuracy of the time estimate(s) or suggestions <strong>for</strong> improving this <strong>for</strong>m, please write to: <strong>Center</strong>s <strong>for</strong> Medicare & Medicaid Services, 7500<br />
Security Boulevard, N2-14-26, Baltimore, Maryland 21244-1850.<br />
FORM CMS-222-92 (10/96) (INSTRUCTIONS FOR THIS WORKSHEET ARE PUBLISHED IN CMS PUB. 15-II,<br />
SECTIONS 2903 and 2903.2)<br />
29-304 Rev. 5<br />
81
APPENDEX G.<br />
RURAL HEALTH CLINIC<br />
SURVEY REPORT<br />
82
RURAL HEALTH CLINIC SURVEY REPORT<br />
Form Approved<br />
OMB No. 0938-0074<br />
§ 481.2 Definitions.<br />
As used in this subpart, unless the context indicates otherwise:<br />
(a)“Direct services” means services provided by the clinic's staff.<br />
(b)“Nurse practitioner” means a registered professional nurse who is<br />
currently licensed to practice in the State, who meets the State's<br />
requirements governing the qualifications of nurse practitioners, and who<br />
meets one of the following conditions:<br />
(1) Is currently certified as a primary care Nurse Practitioner by the<br />
American Nurses' Association or by the National Board of Pediatric<br />
Nurse Practitioners and Associates; or<br />
(2) Has satisfactorily completed a <strong>for</strong>mal 1 academic year educational<br />
program that:<br />
(i) prepares registered nurses to per<strong>for</strong>m an expanded role in the<br />
delivery of primary care;<br />
(ii) includes at least 4 months (in the aggregate) of classroom<br />
instruction and a component of supervised clinical practice; and<br />
(iii) awards a degree, diploma, or certificate to persons who successfully<br />
complete the program; or<br />
(3) Has successfully completed a <strong>for</strong>mal educational program <strong>for</strong> preparing<br />
registered nurses to per<strong>for</strong>m an expanded role in the delivery of primary<br />
care that does not meet the requirements of paragraph (b)(2) of this<br />
section, and<br />
(i) has been per<strong>for</strong>ming an expanded role in the delivery of primary<br />
care <strong>for</strong> a total of 12 months during the 18-month period<br />
immediately preceding the effective date of this subpart.<br />
(c)“Physician” means a doctor of medicine or osteopathy legally authorized<br />
to practice medicine or surgery in the State.<br />
(d) “Physician assistant” means a person who meets the applicable State<br />
requirements governing the qualifications <strong>for</strong> assistants to primary care<br />
physicians, and who meets at least one of the following conditions:<br />
(1) Is currently certified by the National Commission on Certification on<br />
Physician Assistants to assist primary care physicians; or<br />
(2) Has satisfactorily completed a program <strong>for</strong> preparing physician’s assistants<br />
that:<br />
(i) was at least 1 academic year in length;<br />
(ii) consisted of supervised clinical practice and at least 4 months in the<br />
aggregate of classroom instruction directed toward preparing students<br />
to deliver health care; and<br />
(iii) is accredited by the American Medical Association’s Committee on<br />
Allied <strong>Health</strong> Education and Accreditation; or<br />
(3) Has satisfactorily completed a <strong>for</strong>mal educational program <strong>for</strong> preparing<br />
physician assistants that does not meet the requirements of paragraph (d)(2)<br />
of this section, and<br />
(i) has been assisting primary care physicians <strong>for</strong> a 12-month period<br />
in the 18 month period immediately preceding the effective date of<br />
this subpart.<br />
(e) “<strong>Rural</strong> area” means an area that is not delineated as an urbanized area by the<br />
Bureau of the Census.<br />
(f) “<strong>Rural</strong> health clinic” or “clinic” means a clinic that is located in a rural area<br />
designated as a shortage area, is not a rehabilitation agency or a facility<br />
primarily <strong>for</strong> the care and treatment of mental diseases, and meets all other<br />
requirements of this subpart.<br />
(g)“Shortage area” means a defined geographic area designated by the<br />
Department as having either a shortage of personal health services (under<br />
section 1302(7) of the Public <strong>Health</strong> Service Act) or a shortage<br />
of primary medical care manpower (under section 332 of that Act).<br />
(h) “Secretary” means the Secretary of <strong>Health</strong> and Human Services, or<br />
any official to whom he has delegated the pertinent authority.<br />
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of in<strong>for</strong>mation unless it displays a valid OMB control number. The valid OMB control number <strong>for</strong> this in<strong>for</strong>mation<br />
collection is 0938-0074. The time required to complete this in<strong>for</strong>mation collection is estimated to average 1.5 hours per response, including the time to review instructions, search existing data resources, gather the data<br />
needed, and complete and review the in<strong>for</strong>mation collection. If you have any comments concerning the accuracy of the time estimate(s) or suggestions <strong>for</strong> improving this <strong>for</strong>m, please write to: CMS, Attn: PRA Reports<br />
Clearance Officer, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.<br />
Form CMS-30 (05/78) EF 10/2004 83
DEPARTMENT OF HEALTH AND HUMAN SERVICES<br />
Form Approved<br />
CENTERS FOR MEDICARE & MEDICAID SERVICES OMB No. 0938-0074<br />
PROVIDER NUMBER<br />
RURAL HEALTH CLINIC SURVEY REPORT<br />
(J1)<br />
NAME OF CLINIC STREET NUMBER CITY COUNTY STATE ZIP CODE<br />
SURVEYED BY<br />
SURVEYOR’S PROFESSIONAL TITLE<br />
■ INITIAL SURVEY<br />
■ RESURVEY (J2)<br />
LIST ADDITIONAL SURVEYOR’S NAMES TITLE PARTICIPATION UNDER TITLES 18 AND 19<br />
DATE SURVEYED<br />
A clinic certified under Medicare will be deemed to meet<br />
the standards <strong>for</strong> certification under Medicaid.<br />
CODE YES NO N/A<br />
J3<br />
■ MET<br />
■ NOT MET<br />
EXPLANATORY STATEMENTS<br />
CLINIC LICENSE NUMBER (IF APPLICABLE)<br />
II. §481.4 Compliance with Federal, State and local laws.<br />
The rural health clinic and its staff are in compliance with<br />
applicable Federal, State and local laws and regulations.<br />
PHYSICIAN(S) NAME LIC. NO. CERT. NO. REG. NO.<br />
J4 ■ MET ■ NOT MET ■ N/A<br />
(a) Licensure of clinic.<br />
The clinic is licensed pursuant to applicable State and local law.<br />
NURSE PRACTITIONER(S) NAME LIC. NO. CERT. NO. REG. NO.<br />
J5 ■ MET ■ NOT MET<br />
PHYSICIAN ASSISTANT(S) NAME LIC. NO. CERT. NO. REG. NO.<br />
(b) Licensure, certification or registration of personnel.<br />
Staff of the clinic are licensed, certified or registered in<br />
accordance with applicable State and local laws.<br />
OTHER LICENSED PERSONNEL – IDENTIFY<br />
Form CMS-30 (05/78) EF 10/2004 1<br />
84
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J6 ■ MET ■ NOT MET<br />
II. §481.5 Location of <strong>Clinic</strong>.<br />
J7 ■ MET ■ NOT MET<br />
(a) Basic requirement.<br />
The clinic is located in a rural area that is designated as a<br />
shortage area, and may be a permanent or a mobile unit.<br />
J8<br />
(1) Permanent unit.<br />
The objects, equipment and supplies necessary<br />
<strong>for</strong> the provision of the services furnished<br />
directly by the clinic are housed in a permanent<br />
structure. If clinic services are regularly furnished at<br />
permanent units in more than one location, each unit<br />
will be independently considered <strong>for</strong> certification as a<br />
rural health clinic.<br />
J9<br />
(2) Mobile unit.<br />
The objects, equipment and supplies necessary<br />
<strong>for</strong> the provision of the services furnished<br />
directly by the clinic are housed in a mobile structure<br />
which has a fixed, scheduled location(s).<br />
List schedule of operation — day, time and location<br />
Form CMS-30 (05/78) EF 10/2004 2<br />
85
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J10 ■ MET ■ NOT MET<br />
(b) Does the facility meet location eligibility in a rural<br />
health shortage area through either of the following<br />
exceptions.<br />
J11<br />
J12<br />
(1) A facility certified under this subpart will not be<br />
disqualified if the area in which it is located subsequently<br />
fails to meet the definition of rural, shortage area.<br />
(2) A private, nonprofit facility that meets all other<br />
conditions of this subpart except <strong>for</strong> location in a<br />
shortage area will be certified if, on July 1, 1977, it was<br />
operating in a rural area that is determined by the<br />
Secretary (on the basis of the ratio of primary care<br />
physicians to the general population) to have an<br />
insufficient supply of physicians to meet the needs of<br />
the area served. Determinations on these exceptions will<br />
be made by the Secretary upon application by the facility.<br />
J13 ■ MET ■ NOT MET<br />
(c) The facility meets rural area requirements under one<br />
of the following criteria.<br />
J14<br />
(1) <strong>Rural</strong> areas are areas not delineated as urbanized areas<br />
in the last census conducted by the Census Bureau.<br />
J15<br />
(2) Included in the rural area classification are those<br />
portions of extended cities that the Census Bureau has<br />
determined to be rural.<br />
Form CMS-30 (05/78) EF 10/2004 3<br />
86
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J16 ■ MET ■ NOT MET<br />
(d) The facility meets the shortage area requirements<br />
under one of the following criteria.<br />
J17<br />
(1) Determination of shortage of personal health services<br />
(under section 1302(7) of the Public <strong>Health</strong> Service Act).<br />
J18<br />
(2) Determination of shortage of primary medical care<br />
manpower (under section 332(a) (1) (A) of the Public<br />
<strong>Health</strong> Service Act).<br />
Form CMS-30 (05/78) EF 10/2004 4<br />
87
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J19 ■ MET ■ NOT MET<br />
III. §481.6 Physical plant and environment.<br />
J20 ■ MET ■ NOT MET<br />
(a) Construction.<br />
The clinic is constructed, arranged, and maintained to ensure<br />
access to and safety of patients, and provides adequate space<br />
<strong>for</strong> the provision of direct services.<br />
J21 ■ MET ■ NOT MET<br />
(b) Maintenance.<br />
The clinic has a preventive maintenance program to ensure<br />
that:<br />
J22<br />
J23<br />
J24<br />
(1) All essential mechanical, electrical and patient-care<br />
equipment is maintained in safe operating condition;<br />
(2) Drugs and biologicals are appropriately stored; and<br />
(3) The premises are clean and orderly.<br />
J25 ■ MET ■ NOT MET<br />
(c) Emergency procedures.<br />
The clinic assures the safety of patients in case of non-medical<br />
emergencies by:<br />
J26<br />
J27<br />
J28<br />
(1) Training staff in handling emergencies;<br />
(2) Placing exit signs in appropriate locations; and<br />
(3) Taking other appropriate measures that are consistent<br />
with the particular conditions of the area in which the<br />
clinic is located.<br />
Form CMS-30 (05/78) EF 10/2004 5<br />
88
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J29 ■ MET ■ NOT MET<br />
IV. §481.7 Organizational structure.<br />
J30 ■ MET ■ NOT MET<br />
(a) Basic requirements.<br />
J31<br />
(1) The clinic is under the medical direction of a physician,<br />
and has a health care staff that meets the requirements<br />
of §481.8.<br />
J32<br />
(2) The organization’s policies and its lines of authority and<br />
responsibilities are clearly set <strong>for</strong>th in writing.<br />
J33 ■ MET ■ NOT MET<br />
(b) Disclosure.<br />
List names and addresses of owners:<br />
J34<br />
The clinic discloses the names and addresses of:<br />
(1) Its owners, in accordance with section 1124 of the Social<br />
Security Act (42 USC 132 A-3);<br />
J35<br />
(2) The person principally responsible <strong>for</strong> directing the operation<br />
of the clinic; and<br />
J36<br />
(3) The person responsible <strong>for</strong> medical direction.<br />
Form CMS-30 (05/78) EF 10/2004 6<br />
89
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J37 ■ MET ■ NOT MET<br />
IV. §481.8 Staffing and Staff Responsibilities.<br />
J38 ■ MET ■ NOT MET<br />
(a) Staffing.<br />
J43<br />
For each qualified nurse practitioner, indicate the number<br />
qualifying under the respective parts of §481.2(b):<br />
(1)<br />
(2)<br />
(3)<br />
J39<br />
(1) The clinic has a health care staff that includes one or more<br />
physicians and one or more physician’s assistants or nurse<br />
practitioners.<br />
For each qualified physician’s assistant, indicate the number<br />
qualifying under the respective parts of §481.2(d):<br />
J40<br />
(2) The staff, i.e., the nurse practitioner(s), physician(s), or<br />
physician’s assistant(s) meets qualification requirements in<br />
section 481.2(b), (c), (d).<br />
J44<br />
(1)<br />
(2)<br />
(3)<br />
J41<br />
(3) A physician, nurse practitioner, or physician’s assistant is<br />
available to furnish patient care services at all times during<br />
the clinic’s regular hours of operation. A nurse practitioner<br />
or a physician’s assistant is available to furnish patient care<br />
services during at least 60% of the clinic’s regular hours of<br />
operation.<br />
<strong>Clinic</strong>’s regular weekly operating schedule:<br />
Nurse practitioner or physician’s assistant regular weekly on<br />
duty schedule:<br />
J42<br />
(4) The staff is sufficient to provide the services essential to<br />
the operation of the clinic.<br />
Form CMS-30 (05/78) EF 10/2004 7<br />
90
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J45 ■ MET ■ NOT MET<br />
(b) Physician responsibilities:<br />
J46<br />
J47<br />
J48<br />
(1) The physician provides medical direction <strong>for</strong> the clinic’s<br />
health care activities and consultation <strong>for</strong>, and medical<br />
supervision of the health care staff.<br />
(2) In conjunction with the physician’s assistant and/or nurse<br />
practitioner member(s), the physician participates in<br />
developing, executing and periodically reviewing the clinic’s<br />
written policies and the services provided to Federal<br />
program patients; and<br />
(3) The physician periodically reviews the clinic’s patient<br />
records, provides medical orders, and provides medical<br />
care services to the patients of the clinic.<br />
J49<br />
(4) A physician is present <strong>for</strong> sufficient periods of time, at least<br />
once in every 2 week period (except in extraordinary<br />
circumstances), to provide the medical direction, medical<br />
care services, consultation and supervision described in<br />
paragraph(b)(1) of this section, and, is available through<br />
direct telecommunication <strong>for</strong> consultation, assistance with<br />
medical emergencies, or patient referral. The extraordinary<br />
circumstances are documented in the records of the clinic.<br />
Form CMS-30 (05/78) EF 10/2004 8<br />
91
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J50 ■ MET ■ NOT MET<br />
(c) Physician’s assistant and nurse practitioner<br />
responsibilities.<br />
J51<br />
(1) The physician’s assistant and the nurse practitioner<br />
members of the clinic’s staff:<br />
(i) participate in the development, execution and periodic<br />
review of the written policies governing the services<br />
the clinic furnishes;<br />
(ii) provide services in accordance with those policies;<br />
(iii) arrange <strong>for</strong>, or refer patients to, needed services<br />
that cannot be provided at the clinic;<br />
(iv) assure that adequate patient health records are<br />
maintained and transferred as required when<br />
patients are referred; and<br />
(v) participate with a physician in a periodic review of<br />
the patients’ health records.<br />
J52 ■ MET ■ NOT MET<br />
VI. §481.9 Provision of services.<br />
J53 ■ MET ■ NOT MET<br />
(a) Basic requirements<br />
The clinic is primarily engaged in providing outpatient health<br />
services as described in §481.9 (c).<br />
Form CMS-30 (05/78) EF 10/2004 9<br />
92
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J54 ■ MET ■ NOT MET<br />
(b) Patient care policies.<br />
J55<br />
(1) The clinic’s health care services are furnished in<br />
accordance with appropriate written policies which are<br />
consistent with applicable State law.<br />
J56<br />
(2) The policies are developed with the advice of a group of<br />
professional personnel that includes one or more physicians<br />
and one or more physician’s assistants or nurse practitioners.<br />
At least one member of the group is not a member of the<br />
clinic’s staff.<br />
J57<br />
J58<br />
(3) The policies include:<br />
(i) a description of the services the clinic furnishes directly<br />
and those furnished through agreement or arrangement;<br />
(ii) guidelines <strong>for</strong> the medical management of health<br />
problems which include the conditions requiring medical<br />
consultation and/or patient referral, the maintenance of<br />
health care records,and procedures <strong>for</strong> the periodic<br />
review and evaluation of the services furnished by the<br />
clinic;<br />
(iii) rules <strong>for</strong> the storage, handling, and administration<br />
of drugs and biologicals.<br />
(4) These policies are reviewed at least annually by the group<br />
of professional personnel required under (b)(2) above in this<br />
section, and reviewed as necessary by the clinic.<br />
Form CMS-30 (05/78) 10/2004 10<br />
93
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J59 ■ MET ■ NOT MET<br />
(c) Direct services.<br />
J60<br />
(1) General.<br />
The clinic staff furnishes those diagnostic and therapeutic<br />
services and supplies that are commonly furnished in a<br />
physician’s office or at the entry point into the health care<br />
delivery system. These include medical history, physical<br />
examination, assessment of health status, and treatment<br />
<strong>for</strong> a variety of medical conditions.<br />
J61<br />
(2) Laboratory.<br />
The clinic provides basic laboratory services essential to<br />
the immediate diagnosis and treatment of the patient,<br />
including:<br />
(i) chemical examinations of urine by stick or tablet<br />
methods or both (including urine ketones);<br />
(ii) microscopic examination of urine sediment;<br />
(iii) hemoglobin or hematacrit;<br />
(iv) blood sugar;<br />
(v) gram stain;<br />
(vi) examination of stool specimens <strong>for</strong> occult blood;<br />
(vii) pregnancy tests;<br />
(viii) primary culturing <strong>for</strong> transmittal to a certified<br />
laboratory; and<br />
(ix) test <strong>for</strong> pinworms.<br />
Form CMS-30 (05/78) EF 10/2004 11<br />
94
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J62<br />
(3) Emergency.<br />
The clinic provides medical emergency procedures as a<br />
first response to common life-threatening injuries and acute<br />
illness, and has available the drugs and biologicals<br />
commonly used in life saving procedures, such as<br />
analgesics, anesthetics (local), antibiotics, anticonvulsants,<br />
antidotes and emetics, serums and toxoids.<br />
J63 ■ MET ■ NOT MET<br />
(d) Services provided through agreements or<br />
arrangements.<br />
J64<br />
(1) The clinic has agreements or arrangements with one or<br />
more providers or suppliers participating under Medicare or<br />
Medicaid to furnish other services to its patients, including:<br />
(i) inpatient hospital care;<br />
(ii) physician(s) services (whether furnished in the hospital, the<br />
office, the patient’s home, a skilled nursing facility, or<br />
elsewhere); and<br />
(iii) additional and specialized diagnostic and laboratory<br />
services that are not available at the clinic.<br />
J65<br />
(2) If the agreements are not in writing, there is evidence that<br />
patients referred by the clinic are being accepted and treated.<br />
Form CMS-30 (05/78) EF 10/2004 12<br />
95
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J66 ■ MET ■ NOT MET<br />
VII. §481.10 Patient health records.<br />
J67 ■ MET ■ NOT MET<br />
(a) Records system.<br />
J68<br />
J69<br />
(1) The clinic maintains a clinical record system in accordance<br />
with written policies and procedures.<br />
(2) A designated member of the professional staff is responsible<br />
<strong>for</strong> maintaining the records and <strong>for</strong> ensuring that they are<br />
completely and accurately documented, readily accessible,<br />
and systematically organized.<br />
J70<br />
(3) For each patient receiving health care services, the clinic<br />
maintains a record that includes, as applicable:<br />
(i) identification and social data, evidence of consent <strong>for</strong>ms,<br />
pertinent medical history, assessment of the health status<br />
and health care needs of the patient, and a brief summary<br />
of the episode, disposition, and instructions to the patient;<br />
(ii) Reports of physical examinations, diagnostic and<br />
laboratory test results, and consultative findings;<br />
(iii) all physician’s orders, reports of treatments and<br />
medications and other pertinent in<strong>for</strong>mation necessary<br />
to monitor the patient’s progress;<br />
(iv) signatures of the physician or other health care<br />
professional.<br />
Form CMS-30 (05/78) EF 10/2004 13<br />
96
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J71 ■ MET ■ NOT MET<br />
(b) Protection of record in<strong>for</strong>mation.<br />
J72<br />
J73<br />
J74<br />
(1) The clinic maintains the confidentiality of record in<strong>for</strong>mation<br />
and provides safeguards against loss, destruction or<br />
unauthorized use.<br />
(2) Written policies and procedures govern the use and removal<br />
or records from the clinic and the conditions <strong>for</strong> release of<br />
in<strong>for</strong>mation.<br />
(3) The patient’s written consent is required <strong>for</strong> release of<br />
in<strong>for</strong>mation not authorized by law.<br />
J75 ■ MET ■ NOT MET<br />
(c) Retention of records.<br />
The records are retained <strong>for</strong> at least 6 years from date of<br />
last entry, and longer if required by State statute.<br />
J76 ■ MET ■ NOT MET<br />
VIII. §481.11 Program evaluation.<br />
J77 ■ MET ■ NOT MET<br />
(a) The clinic carries out, or arranges <strong>for</strong>, an annual evaluation<br />
of its total program.<br />
Form CMS-30 (05/78) EF 10/2004 14<br />
97
NAME<br />
CODE YES NO N/A EXPLANATORY STATEMENTS<br />
J78 ■ MET ■ NOT MET<br />
(b) The evaluation includes review of:<br />
J79<br />
(1) the utilization of clinic services, including at least the<br />
number of patients served and the volume of services;<br />
J80<br />
(2) a representative sample of both active and closed clinical<br />
records; and<br />
J81<br />
(3) the clinic’s health care policies.<br />
J82 ■ MET ■ NOT MET<br />
(c) The purpose of the evaluation is to determine whether:<br />
J83<br />
J84<br />
J85<br />
(1) the utilization of services was appropriate;<br />
(2) the established policies were followed; and<br />
(3) any changes are needed.<br />
J86 ■ MET ■ NOT MET<br />
(d) The clinic staff considers the findings of the evaluation and<br />
takes corrective action if necessary.<br />
Form CMS-30 (05/78) EF 10/2004 15<br />
98