Alameda County Social Services Agency
Alameda County Social Services Agency
Alameda County Social Services Agency
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
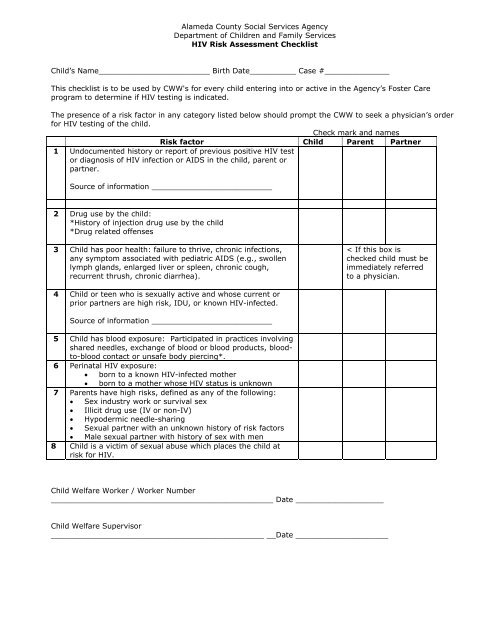
<strong>Alameda</strong> <strong>County</strong> <strong>Social</strong> <strong>Services</strong> <strong>Agency</strong><br />
Department of Children and Family <strong>Services</strong><br />
HIV Risk Assessment Checklist<br />
Child’s Name________________________ Birth Date__________ Case #______________<br />
This checklist is to be used by CWW's for every child entering into or active in the <strong>Agency</strong>’s Foster Care<br />
program to determine if HIV testing is indicated.<br />
The presence of a risk factor in any category listed below should prompt the CWW to seek a physician’s order<br />
for HIV testing of the child.<br />
Check mark and names<br />
Risk factor Child Parent Partner<br />
1 Undocumented history or report of previous positive HIV test<br />
or diagnosis of HIV infection or AIDS in the child, parent or<br />
partner.<br />
Source of information __________________________<br />
2 Drug use by the child:<br />
*History of injection drug use by the child<br />
*Drug related offenses<br />
3 Child has poor health: failure to thrive, chronic infections,<br />
any symptom associated with pediatric AIDS (e.g., swollen<br />
lymph glands, enlarged liver or spleen, chronic cough,<br />
recurrent thrush, chronic diarrhea).<br />
< If this box is<br />
checked child must be<br />
immediately referred<br />
to a physician.<br />
4 Child or teen who is sexually active and whose current or<br />
prior partners are high risk, IDU, or known HIV-infected.<br />
Source of information __________________________<br />
5 Child has blood exposure: Participated in practices involving<br />
shared needles, exchange of blood or blood products, bloodto-blood<br />
contact or unsafe body piercing*.<br />
6 Perinatal HIV exposure:<br />
• born to a known HIV-infected mother<br />
• born to a mother whose HIV status is unknown<br />
7 Parents have high risks, defined as any of the following:<br />
• Sex industry work or survival sex<br />
• Illicit drug use (IV or non-IV)<br />
• Hypodermic needle-sharing<br />
• Sexual partner with an unknown history of risk factors<br />
• Male sexual partner with history of sex with men<br />
8 Child is a victim of sexual abuse which places the child at<br />
risk for HIV.<br />
Child Welfare Worker / Worker Number<br />
________________________________________________ Date ___________________<br />
Child Welfare Supervisor<br />
______________________________________________ __Date ____________________
Instructions for completing the ‘HIV Risk Assessment Checklist’<br />
DO NOT write “unknown” or “did not ask.”<br />
Identify by name the person to whom the information applies, if any, as well as the source of the<br />
information.<br />
The HIV antibody test by itself is not adequate or sufficient to confirm a diagnosis of HIV in babies<br />
under 18 months old. Thus, an infant born to an HIV-positive mother needs a series of special<br />
tests to clarify HIV infection. This testing requires referral to a special HIV clinic, such as Children’s<br />
Hospital & Research Center at Oakland.<br />
Item 5, Unsafe blood practices:<br />
The CDC knows of no instances of HIV transmission through tattooing or body piercing, although<br />
hepatitis B virus has been transmitted during some of these practices. One case of HIV<br />
transmission from acupuncture has been documented. The medical complications for body piercing<br />
appear to be greater than for tattoos. Healing of piercings generally will take weeks, and<br />
sometimes even months, and the pierced tissue could conceivably be abraded (torn or cut) or<br />
inflamed even after healing. Therefore, a theoretical HIV transmission risk does exist if the<br />
unhealed or abraded tissues come into contact with an infected person’s blood or other infectious<br />
body fluid. Additionally, HIV could be transmitted if instruments contaminated with blood are not<br />
sterilized or disinfected between clients.<br />
Item 2, Drug Use by Child:<br />
Intravenous drug use is the direct injection of a drug into a vein. Intramuscular use is injection into<br />
a muscle, and “skin popping” is injection under the skin. Drug use involving the sharing of needles<br />
puts the user at very high risk of HIV infection. Drugs commonly administered intravenously are<br />
heroin, PCP, crack cocaine and crank (amphetamines). Drugs commonly administered<br />
intramuscularly or in the skin include amphetamines and psychedelics, including PCP and LSD.<br />
Young children of parents who deny recent injection drug use but have a history of using heroin,<br />
PCP, cocaine (crack) and amphetamine (crank) must be tested, as current research indicates a<br />
high correlation of use of these drugs with HIV infection, regardless of route of administration.<br />
Revised June 10, 2005