2013 Patient Assistance and Reimbursement Guide - Association of ...
2013 Patient Assistance and Reimbursement Guide - Association of ...
2013 Patient Assistance and Reimbursement Guide - Association of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
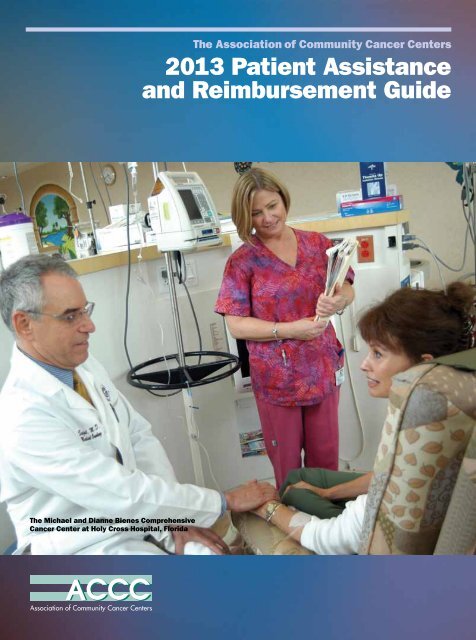
The Michael <strong>and</strong> Dianne Bienes Comprehensive<br />
Cancer Center at Holy Cross Hospital, Florida<br />
The <strong>Association</strong> <strong>of</strong> Community Cancer Centers<br />
<strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong><br />
<strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
SHOULDN’T A PATIENT SUPPORT PROGRAM<br />
BE EASY TO NAVIGATE<br />
Connecting your patients who are prescribed<br />
Jakafi ® (ruxolitinib), <strong>and</strong> who are eligible for the program, to<br />
ongoing support <strong>and</strong> resources during their treatment<br />
ACCESS AND REIMBURSEMENT SERVICES<br />
•Benefit verification<br />
•Prior authorization<br />
•Appeal support<br />
•Co-pay assistance<br />
•Free medication program<br />
•Referrals <strong>and</strong> assistance with<br />
independent not-for-pr<strong>of</strong>it<br />
organizations<br />
PATIENT EDUCATION AND SUPPORT<br />
•Access to trained nurses<br />
•Educational information to help teach your patients<br />
about their condition<br />
•<strong>Patient</strong> packet<br />
Visit www.IncyteCARES.com or call 1-855-4-JAKAFI (1-855-452-5234)<br />
Monday–Friday, 8 AM–8 PM ET, to learn more about how to connect<br />
your patients to IncyteCARES.<br />
Jakafi is a registered trademark <strong>of</strong> Incyte Corporation.<br />
© <strong>2013</strong>, Incyte Corporation. All rights reserved. RUX-1227a 04/13
The <strong>Association</strong> <strong>of</strong> Community Cancer Centers<br />
<strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong><br />
<strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong><br />
Financial <strong>Assistance</strong> Along the Cancer Treatment Continuum 4<br />
by Emmeline Madsen, MPH<br />
PAP Quick Reference <strong>Guide</strong> 12<br />
by Wendalyn Andrews<br />
PAP Flow Chart 20<br />
by Wendalyn Andrews<br />
Pharmaceutical Company <strong>Patient</strong> <strong>Assistance</strong><br />
<strong>and</strong> <strong>Reimbursement</strong> Programs<br />
Amgen, Inc. 34<br />
ARIAD Pharmaceuticals, Inc. 36<br />
Astellas Pharma US, Inc. 37<br />
Bayer HealthCare Pharmaceuticals, Inc. 39<br />
Boehringer Ingelheim Pharmaceuticals, Inc. 41<br />
Bristol-Myers Squibb 42<br />
Celgene Oncology 44<br />
Eisai Co., Ltd. 45<br />
Eli Lilly <strong>and</strong> Company 47<br />
EMD Serono 49<br />
Genentech, Inc. 50<br />
Genomic Health, Inc. 53<br />
GlaxoSmithKline 54<br />
Incyte Corporation 57<br />
Janssen Biotech 58<br />
Merck 60<br />
Millennium: The Takeda Oncology Company 62<br />
Novartis Pharmaceuticals Corporation 64<br />
Onyx Pharmaceuticals 66<br />
Pfizer Oncology 67<br />
ProStrakan 69<br />
San<strong>of</strong>i Oncology 71<br />
Seattle Genetics 73<br />
TEVA Oncology 74<br />
Other <strong>Patient</strong> <strong>Assistance</strong> Programs <strong>and</strong> Resources<br />
BenefitsCheckUp ® 75<br />
Co-Pay Relief 75<br />
HealthWell Foundation 75<br />
The Leukemia & Lymphoma Society 76<br />
NeedyMeds 77<br />
Partnership for Prescription <strong>Assistance</strong> 78<br />
<strong>Patient</strong> Access Network Foundation 79<br />
<strong>Patient</strong> Advocate Foundation 79<br />
RxAssist 80<br />
RxHope 81<br />
Rx Outreach ® 81<br />
Together Rx Access ® Card 81<br />
1<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
2<br />
<strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Assistance</strong> Programs by Drug or Product<br />
Abraxane ® for Injectable Suspension (paclitaxel<br />
protein-bound particles for injectable suspension) 44<br />
Actiq (oral transmucosal fentanyl citrate) [C-II] 74<br />
Adcetris ® (brentuximab vedotin) for injection 73<br />
Afinitor ® (everolimus tablets) 64<br />
Alimta ® (pemetrexed) 47<br />
Aloxi ® (palonosetron hydrochloride) 45<br />
Aranesp ® (darbepoetin alfa) 34<br />
Aromasin ® (exemestane tablets) 67<br />
Arranon ® (nelarabine) 54<br />
Arzerra ® (<strong>of</strong>atumumab) 54<br />
Avastin ® (bevacizumab) 50<br />
Bexxar ® (tositumomab) 54<br />
Bosulif ® (bosutinib) 67<br />
Camptosar ® (irinotecan hydrochloride injection) 67<br />
Dacogen ® (decitabine) for injection 45<br />
Doxil ® (doxorubicin HCl liposome injection) 58<br />
Elitek ® (rasburicase) 71<br />
Ellence ® (epirubicin hydrochloride injection) 67<br />
Eloxatin ® (oxaliplatin) 71<br />
Emcyt ® (estramustine phosphate sodium capsules) 67<br />
Emend ® (aprepitant) 60<br />
Emend ® (fosaprepitant dimeglumine) for injection 60<br />
Epogen ® (epoetin alfa) 34<br />
Erbitux ® (cetuximab) 42<br />
Erivedge (vismodegib) 50<br />
Exjade ® (deferasirox) 64<br />
Fareston ® (toremifene citrate) 69<br />
Femara ® (letrozole tablets) 64<br />
Fentora ® (fentanyl buccal tablet) [C-II] 74<br />
Fragmin ® (dalteparin sodium injection) 45<br />
Gardasil (Quadrivalent Human Papillomavirus<br />
Recombinant Vaccine) 60<br />
Gemzar ® (gemcitabine hydrochloride) 47<br />
Gleevec ® (imatinib mesylate) tablets 64<br />
Gliadel ® Wafer (polifeprosan 20 with carmustine<br />
implant) 45<br />
Halaven (eribulin mesylate) 45<br />
Herceptin ® (trastuzumab) 50<br />
Hexalen ® (altretamine) capsules 45<br />
Hycamtin ® (topotecan) capsules 54<br />
Hycamtin ® (topotecan hydrochloride) for injection 54<br />
Iclusig (ponatinib) 36<br />
Idamycin ® (idarubicin hydrochloride for injection,<br />
USP) 67<br />
Inlyta ® (axitinib) tablets 67<br />
Intron ® A (interferon alfa-2b, recombinant) for<br />
injection 60<br />
Istodax ® (romidepsin) for injection 44<br />
Ixempra (ixabepilone) 42<br />
Jakafi ® (ruxolitinib) tablets 57<br />
Jevtana ® (cabazitaxel) 71<br />
Kyprolis ® (carfilzomib) for injection 66<br />
Leukine ® (sargramostim) 71<br />
Leukeran (chlorambucil) 54<br />
Mozobil ® (plerixafor injection) 71<br />
Myleran ® (busulfan) 54<br />
Neulasta ® (pegfilgrastim) 34<br />
Neumega ® (oprelvekin) 67<br />
Neupogen ® (filgrastim) 34<br />
Nexavar ® (sorafenib) tablets 39<br />
Nplate ® (romiplostim) 34<br />
Oncotype DX ® Breast Cancer Assay ® 53<br />
Oncotype DX ® Colon Cancer Assay ® 53<br />
Ontak ® (denileukin diftitox) 45<br />
Perjeta (pertuzumab) 50<br />
Procrit ® (epoetin alfa) 58<br />
Prolia ® (denosumab) 34<br />
Promacta ® (eltrombopag) 54<br />
Revlimid ® (lenalidomide) 44<br />
Rituxan ® (rituximab) 50<br />
Sancuso ® (granisetron transdermal system) 69<br />
S<strong>and</strong>ostatin LAR ® Depot (octreotide acetate for<br />
injectable suspension) 64<br />
S<strong>and</strong>ostatin ® (octreotide acetate for injection) 64<br />
Sensipar ® (cinacalcet) 34<br />
Sprycel ® (dasatinib) 42<br />
Stivarga ® (regorafenib) tablets 39<br />
Sutent ® (sunitinib malate) 67<br />
Sylatron (peginterferon alfa-2b) for injection 60<br />
Tarceva ® (erlotinib) 50<br />
Targretin ® (bexarotene) capsules 45<br />
Targretin ® (bexarotene) gel 1% 45<br />
Tasigna ® (nilotinib) tablets 64<br />
Taxotere ® (docetaxel) 71<br />
Temodar ® (temozolomide) 60<br />
Temodar ® (temozolomide) for injection 60<br />
Thalomid ® (thalidomide) 44<br />
Thymoglobulin ® (anti-thymocyte globulin [rabbit]) 71<br />
Torisel ® (temsirolimus) injection 67<br />
Tre<strong>and</strong>a ® (bendamustine HCl) for injection 74<br />
Trisenox ® (arsenic trioxide) for injection 74<br />
Tykerb ® (lapatinib) 54<br />
Vectibix ® (panitumumab) 34<br />
Velcade ® (bortezomib) 62<br />
Vidaza ® (azacitidine) 44<br />
Votrient (pazopanib) 54<br />
Xalkori ® (crizotinib) capsules 67<br />
Xeloda ® (capecitabine) 50<br />
Xgeva (denosumab) 34<br />
X<strong>of</strong>igo ® (radium Ra 223 dichloride injection) 39<br />
Xt<strong>and</strong>i ® (enzalutamide) capsules 37<br />
Yervoy ® (ipilimumab) 42<br />
Zaltrap ® (ziv-aflibercept) 71<br />
Zelboraf ® (vemurafenib) 50<br />
Zinecard ® (dexrazoxane for injection) 67<br />
Zolinza (vorinostat) 60<br />
Zometa ® (zoledronic acid) injection 64<br />
Zytiga ® (abiraterone acetate) 58<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
<strong>Association</strong> <strong>of</strong> Community Cancer Centers<br />
National Oncology<br />
Conference<br />
October 2-5, <strong>2013</strong> • The Westin Boston<br />
Boston, Massachusetts<br />
SAVE THE DATE!<br />
Details at www.accc-cancer.org/oncologyconference
Financial <strong>Assistance</strong> Along<br />
the Cancer Treatment Continuum<br />
The Rex Healthcare Experience<br />
by Emmeline Madsen, MPH<br />
Figure 1. Percentage <strong>of</strong><br />
Uninsured Individuals<br />
4.4% – 9.9%<br />
10.0% – 14.0%<br />
14.1% – 16.0%<br />
16.1% – 19.0%<br />
19.1% – 23.7%<br />
Source: CRS analysis <strong>of</strong> data from 2010 American<br />
Community Survey, U.S. Census Bureau.<br />
4<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
The number <strong>of</strong> uninsured Americans under age 65 has grown<br />
significantly during the economic downturn <strong>of</strong> recent years. Most<br />
economists attribute this increase to loss <strong>of</strong> employment <strong>and</strong>,<br />
consequently, employer-sponsored insurance. Those 65 <strong>and</strong> older<br />
remain covered by Medicare, <strong>and</strong> children under 19 years <strong>of</strong><br />
age have maintained coverage because <strong>of</strong> incremental expansion<br />
in Medicaid <strong>and</strong> the Children’s Health Insurance Program.<br />
According to a November 11, 2011, report from the Congressional<br />
Research Service (CRS), the total U.S. civilian non-institutionalized<br />
population in 2010 was slightly more than 304 million. 1 Of those, 47.2<br />
million (15.5 percent) were uninsured. 1 Percentages by state <strong>and</strong> an<br />
average national percentage <strong>of</strong> uninsured individuals are shown in<br />
Figure 1, opposite page. In the ranking <strong>of</strong> percentage <strong>of</strong> uninsured<br />
individuals by state, North Carolina ranks thirty-fifth. 2 In addition,<br />
about 17.9 percent <strong>of</strong> the U.S. GDP (gross domestic product) is spent<br />
on healthcare, a figure expected to increase to more than 20 percent<br />
by 2021. 3 With these daunting figures in mind, it becomes even more<br />
imperative for healthcare organizations, such as Rex Healthcare, to<br />
develop financially sound ways to support patients—even when they<br />
are unable to afford their care.<br />
Karen Hansen, MSW, oncology<br />
social worker, Rex Healthcare<br />
Kimberly Fradel, MSW, LCSW, oncology<br />
social worker, Rex Healthcare<br />
The Rex Healthcare<br />
Response<br />
Our goal is to provide financial assistance<br />
to patients for all <strong>of</strong> the care they receive<br />
<strong>and</strong> to ensure ease <strong>of</strong> patient access to<br />
care. Every day, Rex Healthcare provides<br />
more than $100,000 in charity care <strong>and</strong><br />
write-<strong>of</strong>fs. We have an organized financial<br />
assistance program to help provide<br />
necessary care for our patients; however,<br />
these resources are limited to certain<br />
services <strong>and</strong> business entities <strong>of</strong> the Rex<br />
Healthcare system.<br />
For example, our financial assistance<br />
program, Rex Assist, is limited to<br />
hospital-based services <strong>and</strong> hospitalemployed<br />
physician practices. In addition,<br />
only medically necessary services<br />
are eligible for charity care consideration.<br />
Rex Healthcare screens all uninsured<br />
patients. <strong>Patient</strong>s without health insurance<br />
are automatically eligible for a 35<br />
percent discount for qualifying services,<br />
regardless <strong>of</strong> income or eligibility for<br />
charity care. For patients whose income<br />
is below the U.S. Federal Poverty <strong>Guide</strong>lines,<br />
we <strong>of</strong>fer assistance via a contracted<br />
third party that helps with the Medicaid<br />
application process <strong>and</strong> follow-up. If the<br />
patient does not qualify for Medicaid, our<br />
staff completes a Rex Assist charity care<br />
application <strong>and</strong> forwards it to our <strong>Patient</strong><br />
Financial Services. Criteria are in place<br />
to determine eligibility. Once approved,<br />
the patient is eligible for six months <strong>and</strong><br />
the assistance is applicable toward all balances<br />
incurred prior to the approved Rex<br />
Assist application. As Rex Healthcare is<br />
now a member <strong>of</strong> UNC Healthcare, Rex<br />
Assist is reciprocal with UNC Hospitals’<br />
charity care—saving patients <strong>and</strong> staff<br />
additional paperwork <strong>and</strong> frustration.<br />
<strong>Patient</strong>s with incomes equal to or less<br />
than 250 percent <strong>of</strong> the FPL <strong>Guide</strong>lines<br />
receive 100 percent coverage (see<br />
Table 1, page 6).<br />
Rex Healthcare physicians <strong>and</strong> practices<br />
also participate in Project Access,<br />
a physician pledge program through the<br />
Wake County Medical Society that provides<br />
care to uninsured individuals who<br />
qualify for the program based on medical<br />
necessity. For patients who qualify, this<br />
service, in conjunction with Rex Assist,<br />
<strong>of</strong>ten generates zero financial liability<br />
5<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Table 1. <strong>Patient</strong> Eligibility Criteria for Rex Assist<br />
<strong>and</strong> <strong>of</strong>fers the additional resources <strong>of</strong><br />
case management <strong>and</strong> referral within the<br />
community.<br />
The Oncology Continuum at<br />
Rex Healthcare<br />
Rex Cancer Center was the first in the<br />
region to earn national recognition as<br />
a Comprehensive Community Cancer<br />
Center through the American College <strong>of</strong><br />
Surgeons Commission on Cancer (CoC)<br />
<strong>and</strong> was also the first Comprehensive<br />
Breast Care Center in the area. In addition<br />
to the Rex Cancer Center, which<br />
houses medical <strong>and</strong> radiation oncology,<br />
many departments within Rex Healthcare<br />
<strong>and</strong> several physician practices<br />
provide care to oncology patients from<br />
detection to treatment. Because patient<br />
care spans across these business entities,<br />
financial assistance is complicated. As<br />
the patient moves through the cancer care<br />
continuum many additional bills may be<br />
generated. Some services do not qualify<br />
for Rex Financial <strong>Assistance</strong>; others have<br />
separate financial assessment <strong>and</strong> support<br />
programs. Non-eligible care furthers the<br />
complexity <strong>of</strong> resource management for<br />
patients. Given this complexity, our staff<br />
works to ensure that patients underst<strong>and</strong><br />
the differences in service delivery <strong>and</strong><br />
have access to the appropriate resources<br />
Forgiveness <strong>of</strong> Debt 2012 Federal Poverty Traditional Charity<br />
<strong>Guide</strong>lines<br />
Care 100% <strong>of</strong> Past<br />
<strong>and</strong> 6 Months Into<br />
the Future (Some<br />
Exceptions Apply)<br />
% <strong>of</strong> Federal Poverty <br />
<strong>Guide</strong>lines < = 250%<br />
Family Size <strong>of</strong> 1 $11,170 $27,925<br />
Family Size <strong>of</strong> 2 $15,130 $37,875<br />
Family Size <strong>of</strong> 3 $19,090 $47,725<br />
Family Size <strong>of</strong> 4 $23,050 $57,325<br />
Family Size <strong>of</strong> 5 $27,010 $67,525<br />
Family Size <strong>of</strong> 6 $30,970 $77,425<br />
Family Size <strong>of</strong> 7 $34,930 $87,325<br />
Family Size <strong>of</strong> 8 $38,890 $97,225<br />
For each additional person $3,820<br />
that are aligned with each service type<br />
(see Table 2, page 7).<br />
Navigation Services<br />
Seven years ago, the Rex <strong>Patient</strong> Care<br />
Navigation program was established with<br />
a Duke Endowment grant to provide<br />
navigation to breast cancer patients.<br />
Since then, our program has grown to<br />
4.7 FTE RNs, providing navigation<br />
services for those diagnosed with breast,<br />
gastrointestinal, <strong>and</strong> thoracic cancers.<br />
Our navigation team engages with<br />
patients whenever care is being provided<br />
within Rex Healthcare. These navigators:<br />
●●<br />
Assess patients for financial distress<br />
●●<br />
Refer appropriate patients to hospital<br />
<strong>and</strong>/or departmental resources<br />
●●<br />
Reassure patients about available<br />
resources<br />
●●<br />
Follow up with patients regarding<br />
the process <strong>of</strong> accessing financial<br />
resources.<br />
Often, our navigators are a trusted source<br />
<strong>of</strong> information that patients will turn<br />
to when reluctant to engage with other<br />
6<br />
A Legacy <strong>of</strong> Philanthropic Care<br />
In 1894 John Rex, a tanner from<br />
Raleigh, N.C., made several<br />
bequests to found Rex Hospital. His<br />
last will <strong>and</strong> testament directed:<br />
I give <strong>and</strong> bequeath...all<br />
money belonging to me...<br />
to provide a comfortable<br />
retreat for the sick <strong>and</strong> afflicted<br />
poor belonging to the<br />
city <strong>of</strong> Raleigh in which they<br />
may have the benefit <strong>of</strong><br />
skillful medical aid <strong>and</strong><br />
proper attention.<br />
Rex Healthcare has grown from a staff<br />
<strong>of</strong> seven working in the converted home<br />
<strong>of</strong> former Governor Charles Manly<br />
to becoming the leading healthcare<br />
provider for Wake County, N.C., <strong>and</strong> its<br />
surrounding communities.<br />
Now a member <strong>of</strong> UNC Health<br />
Care, Rex Healthcare is a private, notfor-pr<strong>of</strong>it<br />
healthcare system with more<br />
than 5,400 employees. Rex Healthcare<br />
has 660 beds <strong>and</strong> treats nearly 34,000<br />
inpatients annually. Rex Healthcare’s<br />
medical staff includes more than<br />
1,100 physicians <strong>and</strong> 1,700 nurses.<br />
Wherever patients enter the Rex<br />
Healthcare system, staff is available<br />
to address the financial concerns <strong>of</strong><br />
patients <strong>and</strong> families <strong>and</strong> ensure that<br />
they receive the best care possible.<br />
Rex Healthcare’s mission: to provide<br />
the best in health services by bringing<br />
together compassionate care <strong>and</strong><br />
leading-edge technology. Bottom line:<br />
Rex Healthcare is committed to providing<br />
the best health services to everyone<br />
in the communities that we serve—<br />
regardless <strong>of</strong> their ability to pay.<br />
Of course, when John Rex identified<br />
“the afflicted poor” in his bequest,<br />
he could not have foreseen the extraordinary<br />
rise in healthcare costs <strong>and</strong><br />
that these costs would consume<br />
an enormous percentage <strong>of</strong> the GDP,<br />
now at almost 20 percent. Today,<br />
a tumultuous economy <strong>and</strong> high<br />
unemployment have significantly<br />
reduced the number <strong>of</strong> people eligible<br />
for workplace-sponsored insurance,<br />
<strong>and</strong> increasing numbers <strong>of</strong> underinsured<br />
<strong>and</strong> uninsured patients enter<br />
our healthcare system daily to receive<br />
needed treatment for cancer.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
providers. To avoid extensive burden<br />
on our patient care navigation team, our<br />
navigators “connect” patients to available<br />
resources rather than “manage” their<br />
financial distress.<br />
Diagnostic Services<br />
<strong>Patient</strong>s receiving diagnostic services<br />
within Rex Hospital are eligible for<br />
Rex Assist. One hallmark program has<br />
extended diagnostic services for early<br />
detection further into the community <strong>and</strong><br />
assists with preventive early detection<br />
for breast cancer. Most other diagnostic<br />
services within the hospital system are<br />
linked to suspicious findings rather than<br />
to routine preventive care.<br />
If the patient’s diagnostic service<br />
results in a diagnosis <strong>of</strong> cancer, the<br />
patient is contacted the same day by<br />
the navigation team <strong>and</strong> provided with<br />
educational materials <strong>and</strong> referrals that<br />
include financial assistance programs.<br />
Engaging the patient at the start <strong>of</strong>ten<br />
helps allay many fears that come with the<br />
initial news <strong>of</strong> a cancer diagnosis. It also<br />
streamlines the patient’s path to initiating<br />
care.<br />
Fortunately, Rex Healthcare has several<br />
programs that encourage patients to<br />
manage their breast health proactively—<br />
even if personal funds are limited. The<br />
Susan G. Komen Foundation <strong>and</strong> the Rex<br />
Healthcare Foundation [a separate 501(c)<br />
(3) entity] support the Rex Healthcare<br />
Mammography Certificate Program.<br />
This program fills an important gap in<br />
Wake <strong>and</strong> surrounding counties that<br />
otherwise do not qualify for state Breast<br />
<strong>and</strong> Cervical Cancer Early Detection Program<br />
funds. Via the Certificate Program,<br />
medically underserved women in Wake<br />
<strong>and</strong> 15 surrounding counties receive<br />
a screening mammogram through the<br />
Rex Mobile Mammography Coach <strong>and</strong><br />
Table 2. Services Along the Rex Healthcare Continuum*<br />
Service Type Technical Fee Pr<strong>of</strong>essional Fee<br />
Diagnostic Services Rex Hospital* Private External Practice<br />
Surgery & Surgical Oncology<br />
Rex LLC or Private<br />
External Practice<br />
Surgical Services Rex Hospital* Rex LLC or Private<br />
External Practice<br />
Radiation Oncology<br />
Radiation Oncology Treatment<br />
Medical Oncology<br />
Medical Oncology Treatment<br />
Rex Hospital*<br />
Rex Hospital*<br />
*Services marked with an asterisk are eligible for Rex Assist.<br />
UNC Healthcare*<br />
Hospital-Based Practice*<br />
additional diagnostic imaging through<br />
the Rex Breast Care Center or its suburban<br />
sites. To qualify for this program,<br />
women must have a physician <strong>of</strong> record,<br />
be age 35 or older for screening, <strong>and</strong><br />
age 30 or older for diagnostic imaging<br />
<strong>and</strong> ultrasound with a physician’s order.<br />
If a patient then needs an ultrasound<br />
or biopsy, she is scheduled at the Rex<br />
Breast Care Center. If results indicate<br />
that surgery is required, the patient is<br />
immediately connected with Rex Surgical<br />
Specialists who accept payment from<br />
grant funds at the Medicare rate. Physicians<br />
with Rex Surgical Services are<br />
not employees <strong>of</strong> Rex Hospital <strong>and</strong> their<br />
agreement with the Breast Care Center is<br />
key to assuring that women are not only<br />
screened but treated.<br />
From April 2010 to March 2011, total<br />
program expenses for more than 1,500<br />
women served by the Rex Healthcare<br />
Mammography Certificate Program<br />
were $231,480. Funding<br />
from Susan G. Komen<br />
during the same time<br />
period was $74,425,<br />
or about 23 percent<br />
<strong>of</strong> total program<br />
costs. The remainder<br />
($157,055) was either<br />
supported by the Rex<br />
Healthcare Foundation<br />
or written <strong>of</strong>f<br />
as charity care. The<br />
next year (April 2011<br />
to March 2012) total<br />
program costs for about<br />
2,100 women served<br />
by the Rex Healthcare<br />
Mammography Certificate<br />
Program were<br />
$329,952. That year,<br />
Komen contributed<br />
Table 3. Financial Counseling Team Activities Report for FY 2011<br />
Month<br />
Billing<br />
Questions<br />
Collection<br />
Accts.<br />
Bad<br />
Debt<br />
Write-Off<br />
Balances<br />
Reviewed<br />
Active<br />
Drug<br />
<strong>Assistance</strong><br />
Active<br />
Co-pay<br />
<strong>Assistance</strong><br />
Co-pay<br />
Cards<br />
<strong>Patient</strong>s<br />
with<br />
Financial<br />
<strong>Assistance</strong><br />
Chemo Ed<br />
Sessions<br />
Totals 837 261 $28,054 8,893 602 306 76 800 251<br />
Monthly<br />
Avg. 70 22 $2,338 741 50 26 15 67 21<br />
7<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
8<br />
two grants: one for surgical expenses<br />
($26,400) <strong>and</strong> one for mammography<br />
($67,500), or 28 percent <strong>of</strong> total program<br />
costs. As in the previous year, the<br />
remaining costs were either reimbursed<br />
by the Rex Healthcare Foundation or<br />
considered charity write-<strong>of</strong>fs.<br />
Surgical Care & Surgical<br />
Services<br />
<strong>Patient</strong>s have numerous options for surgical<br />
management within our community.<br />
Many surgery practices participate in<br />
the county-wide Project Access for care,<br />
however, capacity is limited. A few<br />
additional resources exist for surgical<br />
management, but are limited to breast<br />
cancer care. <strong>Patient</strong>s seeking care with<br />
Rex Surgical Specialists (a non-Rex<br />
Hospital business entity) are immediately<br />
engaged in the Rex Assist program for<br />
imminent hospital-based charges <strong>and</strong> are<br />
also eligible for financial discounts <strong>and</strong><br />
payment plans, based on eligibility, for<br />
pr<strong>of</strong>essional fees.<br />
Radiation Oncology<br />
& Treatment<br />
Our radiation oncologists are UNCemployed<br />
physicians; therefore, patients<br />
receive a bill from UNC Physicians &<br />
Associates for pr<strong>of</strong>essional fees. More<br />
than two years ago, the charity care<br />
process was st<strong>and</strong>ardized for patients<br />
whether they received care at Rex Healthcare<br />
or UNC Healthcare. Prior to that<br />
time, patients had to complete two separate<br />
applications for assistance <strong>and</strong> wait<br />
for pending approval from both entities.<br />
St<strong>and</strong>ardizing this process has greatly<br />
increased efficiency, patient satisfaction,<br />
<strong>and</strong> patient compliance with care at both<br />
institutions.<br />
Treatment-associated costs for radiation<br />
oncology are hospital-based charges<br />
<strong>and</strong> are eligible for Rex Assist charity<br />
care.<br />
Prior to treatment, patients within<br />
radiation oncology are also provided<br />
with an estimated cost <strong>of</strong> care, which is<br />
aligned with an upfront collections process.<br />
We refer uninsured individuals or<br />
patients with concerns about the cost <strong>of</strong><br />
treatment to Rex Assist <strong>and</strong> our oncology<br />
social work team.<br />
Medical Oncology<br />
& Treatment<br />
Our medical oncologists are employed by<br />
Rex Healthcare. As such, patients are eligible<br />
for Rex Assist for pr<strong>of</strong>essional fees<br />
<strong>and</strong> hospital-based treatment costs. Due<br />
to the overwhelming cost <strong>of</strong> therapeutic<br />
agents, financial counselors meet with<br />
patients prior to the start <strong>of</strong> treatment to<br />
eliminate the financial burden as much<br />
as possible. The financial counselors<br />
conduct an assessment to determine<br />
insurance coverage <strong>and</strong> potential patient<br />
liability <strong>and</strong> identify individuals who<br />
are self-pay or uninsured (see Figure 2,<br />
page 9).<br />
For patients with insurance, prior to<br />
or during the session, financial counselors<br />
review:<br />
✔✔<br />
✔✔<br />
✔✔<br />
Verification <strong>of</strong> benefits<br />
Verification <strong>of</strong> out-<strong>of</strong>-pocket cost(s)<br />
Verification <strong>of</strong> deductible <strong>and</strong> determination<br />
if it has been met for that<br />
plan year.<br />
For patients who indicate that meeting<br />
out-<strong>of</strong>-pocket costs may be difficult,<br />
financial counselors identify additional<br />
assistance options, including:<br />
✔✔<br />
✔✔<br />
Co-pay assistance programs<br />
Payment plans.<br />
For those patients interested in payment<br />
plans, our team generally adheres to<br />
amounts per policy, but also maintains<br />
additional flexibility to lower payments<br />
to amounts comfortable for the patient.<br />
For uninsured patients, our financial<br />
counselors help them in applying for<br />
Rex Assist (if they have not already<br />
completed an application) <strong>and</strong> to reapply<br />
every six months. Our financial<br />
counselors also actively pursue assistance<br />
from pharmaceutical patient assistance<br />
programs.<br />
The team tracks the assistance<br />
that they <strong>of</strong>fer to patients (see Table 3,<br />
page 7). Not only do these metrics justify<br />
our financial counselor positions, they<br />
identify concrete benefits related to<br />
ongoing financial intervention <strong>and</strong> case<br />
management.<br />
Pr<strong>of</strong>essional Fees &<br />
Hospital Charges<br />
For medical oncology, pr<strong>of</strong>essional fee<br />
billing is managed within the practice.<br />
The financial counselors review accounts<br />
<strong>and</strong> write <strong>of</strong>f the eligible amounts linked<br />
to Rex Assist before sending the account<br />
to our contracted billing clearinghouse.<br />
We use our EMR to maintain a list <strong>of</strong><br />
individuals eligible for Rex Assist <strong>and</strong><br />
to generate monthly reports using the<br />
payer source designated as Rex Assist.<br />
Most <strong>of</strong>ten Rex Assist covers the full<br />
pr<strong>of</strong>essional fee costs. However, for those<br />
accounts with any remaining liability, our<br />
financial counselors work with patients to<br />
create payment plans.<br />
Hospital-based charges are submitted<br />
for chemotherapy <strong>and</strong> the associated<br />
administration <strong>and</strong> billed by Rex Healthcare<br />
<strong>Patient</strong> Financial Services. For those<br />
charges that have a Rex Assist payer<br />
source, charges are written <strong>of</strong>f per percentage<br />
eligibility. Each billing location<br />
that includes medical oncology reports<br />
monthly on the amount <strong>of</strong> charity care.<br />
<strong>Patient</strong>s can call a toll-free number to<br />
talk with Rex <strong>Patient</strong> Financial Services<br />
customer service team members about<br />
their bill, potential payment plans, <strong>and</strong>/<br />
or resources to help manage financial<br />
burdens. Our financial counseling team<br />
works closely with our social work team<br />
in this process.<br />
Pharmaceutical <strong>Patient</strong><br />
<strong>Assistance</strong> Programs<br />
After the initial consult, our financial<br />
counselors use the following process to<br />
manage self-pay or uninsured patients:<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
Physician writes order<br />
Chemo order is sent for authorization<br />
Authorization staff transfer self-pay<br />
patients to the financial counseling<br />
team<br />
Financial counseling team researches<br />
available patient assistance programs<br />
based on regimen<br />
At the Chemo Teaching Session,<br />
financial counselors work with<br />
patients to prepare <strong>and</strong> sign patient<br />
assistance applications, including<br />
identifying <strong>and</strong> gathering the necessary<br />
financial documents<br />
Financial counselors complete the<br />
application with pertinent <strong>and</strong> available<br />
information before the Chemo<br />
Consult with patient<br />
At the Chemo Consult, financial<br />
counselors review the final application<br />
with the patient <strong>and</strong> obtain final<br />
signature<br />
Financial counselors submit applica-<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Figure 2. H<strong>and</strong>out About Our<br />
Chemotherapy Education<br />
Session & Financial <strong>Assistance</strong><br />
Engagement<br />
✔✔<br />
tions that same day<br />
Financial counselors wait for approval<br />
<strong>and</strong> follow up as needed outside <strong>of</strong><br />
typical response window. Every effort<br />
is made to secure eligibility<br />
<strong>and</strong> approval before initiation <strong>of</strong><br />
treatment.<br />
Once approval is received, financial<br />
counselors proceed based on the type <strong>of</strong><br />
patient assistance program. For programs<br />
that provide drugs upfront, our financial<br />
counselors:<br />
✔✔<br />
✔✔<br />
✔✔<br />
Use chemo orders to ensure that the<br />
drug is shipped upfront<br />
Communicate with the oncology<br />
pharmacy<br />
Ensure that the pharmacy charge code<br />
assigned is indicative <strong>of</strong> the patient<br />
assistance program<br />
✔✔<br />
Notify <strong>Patient</strong> Financial Services for<br />
charge linkage.<br />
For drug replacement programs, our<br />
financial counselors:<br />
✔✔<br />
Track drug administration <strong>and</strong><br />
charges<br />
✔✔<br />
Work with the pharmacy department<br />
<strong>and</strong> pharmaceutical company to<br />
replace the drug.<br />
In the event <strong>of</strong> any unused drug, our<br />
financial counselors ensure that the drug<br />
is reassigned a lot number for indigent<br />
use; stock used in critical situations<br />
requires timely initiation <strong>of</strong> care.<br />
Each year the number <strong>of</strong> patients<br />
receiving patient assistance has grown<br />
(see Table 4, page 10). To date, we have<br />
been able to <strong>of</strong>fset these costs with the<br />
use <strong>of</strong> pharmaceutical patient assistance<br />
programs. Our financial counseling<br />
team is integral in securing this patient<br />
assistance. Securing approval <strong>of</strong> free<br />
chemotherapy drugs from a pharmaceutical<br />
company is time consuming;<br />
documentation is <strong>of</strong>ten daunting. Our<br />
financial counselors manage the paperwork<br />
<strong>and</strong> logistics<br />
related to<br />
each <strong>of</strong> the<br />
different<br />
pharmaceutical<br />
patient assistance<br />
programs, along<br />
with multiple<br />
grant applications<br />
<strong>and</strong> other community<br />
foundation<br />
applications.<br />
For fiscal year<br />
2011-2012, Rex<br />
Cancer Center’s<br />
credits for free<br />
chemotherapy drugs<br />
were more than<br />
$4 million, with<br />
another $500,000<br />
in free oral chemotherapy<br />
drugs. Our<br />
financial counselors<br />
were also able to<br />
obtain grants for<br />
$132,500 from various<br />
cancer-specific foundations<br />
<strong>and</strong> more than<br />
$29,000 through co-pay<br />
assistance cards.<br />
Inpatient Financial<br />
Assessment & <strong>Assistance</strong><br />
A third-party contractor, with support<br />
from the hospital’s social work<br />
<strong>and</strong> clinical case management teams,<br />
assesses <strong>and</strong> manages our uninsured<br />
inpatients. Two contract employees<br />
maintain a daily census list <strong>of</strong> uninsured<br />
individuals. The team works<br />
directly with inpatients to complete<br />
applications for Medicaid <strong>and</strong> SSI/SSD.<br />
Once applications are completed, the<br />
inpatient is given contact information<br />
for the contract company. Inpatients are<br />
assigned an advocate to represent them,<br />
9<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
in person, at any Medicaid appeal hearings.<br />
Additionally, the inpatient social<br />
work <strong>and</strong> case management team make<br />
assessments <strong>and</strong> community referrals<br />
for needed resources.<br />
For individuals who qualify for<br />
Medicaid based on disability <strong>and</strong>/or<br />
income, our outpatient social work team<br />
continues to work with those that are<br />
eligible <strong>and</strong>/or approved for Medicaid<br />
<strong>and</strong> who are receiving ongoing oncology<br />
care. Given that patients are eligible<br />
every six months, our team works with<br />
patients as treatment continues. The team<br />
also assists the patient with gathering<br />
all medical bills for pro<strong>of</strong> <strong>of</strong> continued<br />
eligibility.<br />
Outpatient Social Work<br />
Assessment<br />
Our oncology social workers routinely<br />
assess patients receiving outpatient medical<br />
oncology <strong>and</strong> radiation oncology to<br />
Table 4. Increasing Trend <strong>of</strong> <strong>Patient</strong>s Needing <strong>Patient</strong> <strong>Assistance</strong><br />
<strong>and</strong> the Impact on Rex Healthcare<br />
Number <strong>of</strong> <strong>Patient</strong>s Amount <strong>of</strong> Free<br />
Fiscal Year Receiving Free IV Medicines Drug Received<br />
2007-2008 29 $1,409,906.49<br />
2008-2009 29 $1,826,960.85<br />
2009-2010 40 $2,971,013.55<br />
2010-2011 46 $2,570,688.74<br />
2011-2012 60 $4,090,087.40<br />
2012-<strong>2013</strong> YTD 20 $880,619.92<br />
determine current stressors, which may<br />
include immediate financial issues exacerbated<br />
by a cancer diagnosis (see Table<br />
5, below). In a recent patient assessment,<br />
when asked about practical concerns <strong>and</strong><br />
issues related to treatment, 260 patients<br />
named cost <strong>of</strong> treatment (36 percent),<br />
insurance (33 percent), employment (20<br />
percent), <strong>and</strong> transportation (12 percent).<br />
Social work assessment <strong>and</strong> intervention<br />
includes the following to assess for <strong>and</strong><br />
respond to financial distress:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Identification <strong>of</strong> barriers to treatment<br />
Identification <strong>of</strong> areas <strong>of</strong> greatest need<br />
Identification <strong>of</strong> personal resources<br />
Identification <strong>of</strong> community resources<br />
Assessment <strong>of</strong> philanthropic Angel<br />
Fund as gap resource.<br />
The Rex Healthcare<br />
Foundation Angel Fund<br />
After assessment, social workers may<br />
determine that use <strong>of</strong> the Rex Healthcare<br />
Foundation Angel Fund is appropriate to<br />
meet minimal needs that are identified<br />
as high-need areas with no identified<br />
personal or community resources. While<br />
Table 5. Social Work Encounters to Help Manage Financial Burdens & Assess for Resources*<br />
Social Work Financial <strong>Assistance</strong> - Encounters<br />
July Aug Sept Oct Nov Dec Jan Feb March Apr May June TOTAL AVG<br />
Medicaid <strong>Assistance</strong> 15 21 16 24 24 11 25 21 15 13 8 19 212 17.67<br />
SSI/SSD <strong>Assistance</strong> 29 35 17 19 24 12 27 13 10 23 12 28 249 20.75<br />
Rex Assist 20 33 21 24 21 17 22 14 15 21 12 35 255 21.25<br />
COBRA 2 1 1 1 1 2 1 1 3 13 1<br />
Transportation 59 61 62 48 62 53 77 61 64 54 43 48 692 57.67<br />
Angel Fund 78 94 83 80 64 71 100 73 71 60 66 70 910 75.83<br />
Community Funds 17 11 15 5 12 6 3 4 6 3 5 2 89 7.42<br />
Community Resources 31 30 34 17 21 22 37 34 30 31 22 30 339 28.25<br />
*These encounters are in addition to an initial social work assessment to determine patient needs that <strong>of</strong>ten reveal financial issues.<br />
Table 6. Angel Fund Support for FY 2012<br />
<strong>Patient</strong>s 376<br />
Average Per <strong>Patient</strong> $262<br />
10<br />
Jul-11 Aug-11 Sep-11 Oct-11 Nov-11 Dec-11 Jan-12 Feb-12 Mar-12 Apr-12 May-12 Jun-12 TOTAL<br />
$8,920 $12,450 $10,545 $10,295 $6,242 $7,875 $8,273 $6,467 $5,695 $4,038 $7,054 $5,886 $93,738<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Case Study<br />
Rebecca is a 42-year-old married<br />
mother <strong>of</strong> two who was<br />
recently diagnosed with Stage<br />
III breast cancer. Rebecca has been<br />
working full-time as a housecleaner<br />
<strong>and</strong> trying to work overtime hours, as<br />
her husb<strong>and</strong> was recently laid <strong>of</strong>f from<br />
his job. Rebecca is uninsured. It is<br />
recommended that she have a mastectomy<br />
followed by chemotherapy <strong>and</strong><br />
radiation. Rebecca is terrified by her<br />
recent diagnosis, but knows that she is in<br />
good h<strong>and</strong>s with her medical team. She<br />
is extremely concerned—not only about<br />
the medical bills she will incur, but also<br />
at the thought <strong>of</strong> how her family will<br />
survive without income during this time.<br />
A patient care navigator met with<br />
Rebecca prior to her surgery to serve<br />
as her care coordinator for the day <strong>of</strong><br />
surgery <strong>and</strong> to align resources along<br />
her anticipated clinical pathway.<br />
The patient care navigator reassured<br />
Rebecca that she will be supported<br />
along her journey—not only by the<br />
navigation team but also by many other<br />
skilled clinicians <strong>and</strong> pr<strong>of</strong>essionals who<br />
will help meet her needs.<br />
The day after Rebecca’s mastectomy<br />
(while she is an inpatient) she is<br />
greeted in her room by a representative<br />
who screens for Medicaid <strong>and</strong> SSI/<br />
SSD programs. Rebecca learns that<br />
her applications are complete <strong>and</strong> this<br />
representative will be her advocate for<br />
securing these resources. She is also<br />
given the hospital patient assistance<br />
application to complete <strong>and</strong> told about<br />
how the program may cover a percentage<br />
<strong>of</strong> all hospital-based charges.<br />
Rebecca is told that the surgeon’s fees<br />
are the only component that will not be<br />
covered with this program, but that the<br />
surgical practice will work with her to<br />
establish a payment plan <strong>and</strong> identify<br />
any assistance options.<br />
Upon presentation for adjuvant<br />
consultation, financial counselors from<br />
the cancer center meet with Rebecca<br />
to complete applications for free drug<br />
assistance on the day <strong>of</strong> her chemo<br />
education session. On Rebecca’s first<br />
day <strong>of</strong> chemotherapy, she is greeted by<br />
the cancer center social worker who<br />
acknowledges Rebecca’s fears <strong>and</strong><br />
works closely with her throughout treatment<br />
to ensure that her financial needs<br />
outside <strong>of</strong> the medical cost <strong>of</strong> care are<br />
met. The oncology social worker links<br />
Rebecca to the hospital philanthropicsupported<br />
fund to assist with nominal<br />
financial needs related to transportation<br />
<strong>and</strong> antiemetic drugs, ensuring that<br />
Rebecca can move easily through her<br />
treatment.<br />
The social work team also identifies<br />
other community resources <strong>and</strong><br />
provides counseling <strong>and</strong> support to<br />
Rebecca <strong>and</strong> her entire family. Rebecca<br />
<strong>and</strong> her husb<strong>and</strong> had to make difficult<br />
choices along the way to treatment, but<br />
with the help <strong>of</strong> our financial specialists,<br />
they feel more than ever that they<br />
can get through this experience, one<br />
day at a time.<br />
a patient is in active treatment, the Angel<br />
Fund may be used for:<br />
●●<br />
Transportation expenses<br />
●●<br />
Prescriptions for supportive pharmaceuticals<br />
(antiemetics <strong>and</strong> pain<br />
management)<br />
●●<br />
●●<br />
Nutritional supplements <strong>and</strong>/or<br />
prostheses<br />
Lymphedema supplies.<br />
With the economic downturn, utilization<br />
<strong>of</strong> our Angel Fund was increasing<br />
at the beginning <strong>of</strong> FY 2012. To respond<br />
to the limited capacity <strong>of</strong> this fund <strong>and</strong><br />
maintain our ability to assist as many<br />
patients as possible, our social work team<br />
made the difficult decision to further<br />
limit the amount per patient. The marked<br />
decrease in spending after the first third<br />
<strong>of</strong> the fiscal year is due to more extensive<br />
intervention by the social work team<br />
<strong>and</strong> a better underst<strong>and</strong>ing <strong>of</strong> resource<br />
management (see Table 6, page 10).<br />
The Need & Commitment<br />
Continues<br />
As with many healthcare systems, a<br />
variety <strong>of</strong> business entities make up<br />
Rex Healthcare, including hospital<br />
services <strong>and</strong> physician-based services.<br />
Accordingly, patient financial resources<br />
must cross business lines in a way that<br />
best <strong>and</strong>, ideally, consistently provides<br />
financial resources to patients. While<br />
this complexity <strong>of</strong>ten creates operational<br />
challenges, we hope to mitigate these<br />
in the coming years with consistent <strong>and</strong><br />
unified EMRs <strong>and</strong> billing systems. Rex<br />
Healthcare is proud <strong>of</strong> its robust financial<br />
management for cancer patients<br />
along the continuum <strong>of</strong> care, but we<br />
recognize that there are still unmet<br />
needs <strong>and</strong> opportunity for improvement<br />
<strong>and</strong>/or integration to a more seamless<br />
system. UNC Healthcare <strong>and</strong> Rex<br />
Healthcare are committed over time to<br />
providing one bill for all services, thus<br />
ensuring ease <strong>of</strong> access for patients.<br />
However, this goal is not one that will<br />
be met immediately <strong>and</strong> will require<br />
continued resources to achieve. Until<br />
those additional measures <strong>and</strong> optimal<br />
realignment can be put into place,<br />
Rex Healthcare relies on collaboration<br />
between its business entities, departments,<br />
<strong>and</strong> providers to ensure that<br />
our patients receive needed care <strong>and</strong> a<br />
patient experience that is as seamless as<br />
possible.<br />
Emmeline Madsen, MPH, is manager,<br />
Cancer Specialty Services, Rex Cancer<br />
Center - Rex/UNC Healthcare, Raleigh,<br />
N.C.<br />
References<br />
1<br />
Newman D. Health Insurance Coverage<br />
by State <strong>and</strong> Congressional District, 2010.<br />
Congressional Research Service. October<br />
20, 2011. Available online at: http://<br />
healthreformgps.org/wp-content/uploads/<br />
health-insurance-coverage-by-statte-<strong>and</strong>-<br />
CD-CRS-RPT_R42055_2011-10-201.pdf.<br />
Last accessed Nov. 7, 2012.<br />
2<br />
Mach AL. The Uninsured by State <strong>and</strong> Congressional<br />
District, 2010. Penny Hill Press.<br />
November 17, 2011.<br />
3<br />
Centers for Medicare & Medicaid. National<br />
Health Expenditures Projections, 2011-2021.<br />
Available online at: www.cms.gov.<br />
The author would like to thank the following contributors to the article: Rose<br />
Auman, MSW, support services coordinator; Kimberly Fradel, LCSW, oncology<br />
social worker; <strong>and</strong> Wendy Avery, Mobile Mammography coordinator, Rex/UNC<br />
Healthcare, Raleigh, N.C.<br />
11<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
PAP Quick Reference <strong>Guide</strong><br />
Drug Name Br<strong>and</strong> Name Drug Company<br />
Benefit<br />
Verification<br />
<strong>and</strong><br />
Authorization<br />
Support<br />
Drug<br />
Company<br />
Co-Pay<br />
<strong>Assistance</strong><br />
Foundation<br />
<strong>Assistance</strong><br />
12<br />
13-cis-Retinoic Acid Accutane<br />
2-CdA Leustatin D, H<br />
2-Chlorodeoxyadenosine Leustatin D, H<br />
5-Azacitidine Vidaza Celgene X D, H, P<br />
5FU Adrucil D, H<br />
6-Mercaptopurine Purinethol H<br />
6-MP Purinethol H<br />
6-TG<br />
Thioguanine Tab<br />
6-Thioguanine<br />
Thioguanine Tab<br />
Actinomycin-D Cosmegen Lundbeck D, H<br />
Aldesleukin Proleukin Prometheus X<br />
Alitretinoin Panretin Eisai X<br />
Altretamine Hexalen Eisai X<br />
Amifostine Ethyol D, H<br />
Aminoglutethimide Cytadren H<br />
Anagrelide<br />
Agrylin<br />
Anastrozole Arimidex AstraZeneca A<br />
Aprepitant Emend Merck X<br />
ARA-C Cytosar-U H<br />
Arsenic trioxide Trisenox Teva Oncology X P<br />
Asparaginase Elspar Merck D, H<br />
Axitinib Inlynta Pfizer X X X<br />
ATRA<br />
Vesanoid<br />
Azacitidine Vidaza Celgene X D, H, P<br />
BCG TheraCys San<strong>of</strong>i<br />
BCNU BiCNU Bristol-Myers Squibb X D, H<br />
Bendamustine Tre<strong>and</strong>a Teva Oncology X H, P, A, F<br />
Bexarotene Targretin Eisai X P<br />
Bevacizumab Avastin Genentech X X D, H, P<br />
Bicalutamide Casodex AstraZeneca D, R, U<br />
Bleomycin Blenoxane H<br />
Bortezomib Velcade Millennium X D, H, P<br />
Bosutinib Bosulif Pfizer X X X<br />
Brentuximab vedotin Adcetris Seattle Genetics X X P<br />
Busulfan Myleran GlaxoSmithKline X H, P<br />
C225 Erbitux Bristol-Myers Squibb X D, H, P<br />
Capecitabine Xeloda Genentech X X D, H, P<br />
Carboplatin Paraplatin H<br />
Carfilzomib Kyprolis Onyx X X X<br />
Carmustine BiCNU Bristol-Myers Squibb X D, H<br />
Chlorambucil Leukeran GlaxoSmithKline X H, P<br />
Cetuximab Erbitux Bristol-Myers Squibb X D, H, P<br />
Cisplatin Platinol H<br />
Cisplatin Platinol-AQ Bristol-Myers Squibb H<br />
Cladribine Leustatin D, H<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Oral<br />
Prescription<br />
Savings<br />
<strong>and</strong>/or Free<br />
Medication<br />
IV &<br />
Injectable<br />
Drugs Ongoing<br />
<strong>and</strong>/or<br />
Replacement<br />
Program<br />
No Drug<br />
<strong>Assistance</strong><br />
Phone<br />
Number<br />
Website<br />
H = www.Healthwellfoundation.org<br />
F = www.patientadvocate.org<br />
P = www.panfoundation.org/fundingapplication<br />
D = www.diplomatpharmacy.com/funding<br />
A = www.pparx.org<br />
U = www.xubex.com<br />
M = www.rxoutreach.org<br />
O = www.rarediseases.org/patients-<strong>and</strong>-families<br />
X<br />
Foundation assistance only. Please see the legend provided.<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.800.931.8691 www.celgenepatientsupport.com<br />
Foundation assistance only. Please see the legend provided.<br />
U<br />
Foundation assistance only. Please see the legend provided.<br />
U<br />
Foundation assistance only. Please see the legend provided.<br />
T 1.800.444.4106 www.togetherrxaccess.com<br />
T 1.800.444.4106 www.togetherrxaccess.com<br />
X 1.866.209.7604 www.lundbeck.com/us<br />
X 1.877.776.5385 www.proleukin.com/mm/resources.aspx<br />
X 1.866.613.4724 www.eisaireimbursement.com<br />
X 1.866.613.4724 www.eisaireimbursement.com<br />
Foundation assistance only. Please see the legend provided.<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X<br />
X 1.800.292.6363 www.astrazeneca-us.com/help-affording-your-medicines<br />
X X 1.866.363.6379 www.merck.com/merckhelps<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.877.237.4881 www.cephalon.org/cephaloncares-foundation.html<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X<br />
X 1.800.931.8691 www.celgenepatientsupport.com<br />
X 1.866.801.5655 www.visitspconline.com<br />
X 1.800.736.0003 www.bmspaf.org<br />
X 1.888.587.3263 www.cephalononcologycore.com/<br />
X 1.866.613.4724 www.eisaireimbursement.com<br />
X 1.888.249.4918 www.genentech-access.com<br />
X 1.800.292.6363 www.astrazeneca-us.com/help-affording-your-medicines<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.866.835.2233 www.velcade.com/payingfortreatment.aspx<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X 1.855.473.2436 www.seagensecure.com<br />
1.866.265.6491 www.gsk-access.com<br />
X 1.800.861.0048 www.bmsaccesssupport.com<br />
X 1.888.249.4918 www.genentech-access.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.855.669.9360 www.kyprolis.com/resources<br />
X 1.800.736.0003 www.bmspaf.org<br />
1.866.265.6491 www.gsk-access.com<br />
X 1.800.861.0048 www.bmsaccesssupport.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
1.800.675.8416 www.healthwellfoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
13<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
PAP Quick Reference <strong>Guide</strong><br />
Drug Name Br<strong>and</strong> Name Drug Company<br />
Benefit<br />
Verification<br />
<strong>and</strong><br />
Authorization<br />
Support<br />
Drug<br />
Company<br />
Co-Pay<br />
<strong>Assistance</strong><br />
Foundation<br />
<strong>Assistance</strong><br />
14<br />
Cl<strong>of</strong>arabine Clolar Genzyme X<br />
CPT-11 Camptosar Pfizer X D, H, P<br />
Crizotinib Xalkori Pfizer X<br />
Cyclophosphamide Cytoxan H<br />
Cyclophosphamide Neosar H<br />
Cytarabine Cytosar-U H<br />
Dactinomycin Cosmegen Lundbeck D, H<br />
Dacarbazine DTIC H<br />
Darbepoetin Aranesp Amgen X H, P, F<br />
Dasatinib Sprycel Bristol-Myers Squibb X<br />
Daunorubicin<br />
Cerubidine<br />
Decitabine Dacogen Eisai X<br />
Deferasirox Exjade Novartis X<br />
Degarelix Firmagon Ferring X<br />
Denileukin diftitox Ontak Eisai X<br />
Denosumab Prolia Amgen X X H, P, F<br />
Denosumab Xgeva Amgen X X H, P, F<br />
Dexrazoxane Totect TopoTarget X X<br />
Dexrazoxane Zinecard Pfizer X X X<br />
Docetaxel Taxotere San<strong>of</strong>i X D, H, P<br />
Doxorubicin Adriamycin H<br />
Doxorubicin Liposome Doxil Janssen Products X D, H, P<br />
Eltrombopag Promacta GlaxoSmithKline X X H, A, F, P<br />
Enzalutamide Xt<strong>and</strong>i Astellas Oncology X X<br />
Epirubicin Ellence Pfizer X D, H<br />
Epoetin Alpha Procrit Janssen Products X D, H<br />
Erlotinib Tarceva Genentech X X H, P<br />
Erwinia Asparaginase Elspar D, H<br />
Estramustine Emcyt Pfizer X X P<br />
Etoposide Etopophos Bristol-Myers Squibb H<br />
Etoposide VePesid H<br />
Etoposide Toposar H<br />
Everolimus Afinitor Novartis X D, P<br />
Exemestane Aromasin Pfizer X X H, P, U<br />
Filgrastim Neupogen Amgen X D, H, P<br />
Finasteride Proscar Merck M<br />
Flourouracil 5FU D, H<br />
Floxuridine FUDR H<br />
Fludarabine Fludara H, P<br />
Fluoxymesterone Halotestin H<br />
Flutamide Eulexin H, P<br />
Fulvestrant Faslodex AstraZeneca D, H, P<br />
Gefitinib Iressa AstraZeneca H, P<br />
Gemcitibine Gemzar Eli Lilly D, H, P<br />
Gemtuzumab Ozogamicin Mylotarg Pfizer X X H, P, U<br />
Goserlin Zoladex AstraZeneca D, H, P<br />
Granisetron Sancuso ProStrakan X X X<br />
Hydroxyurea Droxia Bristol-Myers Squibb A<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Oral<br />
Prescription<br />
Savings<br />
<strong>and</strong>/or Free<br />
Medication<br />
IV &<br />
Injectable<br />
Drugs Ongoing<br />
<strong>and</strong>/or<br />
Replacement<br />
Program<br />
No Drug<br />
<strong>Assistance</strong><br />
Phone<br />
Number<br />
Website<br />
H = www.Healthwellfoundation.org<br />
F = www.patientadvocate.org<br />
P = www.panfoundation.org/fundingapplication<br />
D = www.diplomatpharmacy.com/funding<br />
A = www.pparx.org<br />
U = www.xubex.com<br />
M = www.rxoutreach.org<br />
O = www.rarediseases.org/patients-<strong>and</strong>-families<br />
X 1.800.792.5652 www.clolar.com/pediatric.asp<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
X 1.855.925.5674 www.pfizerhelpfulanswers.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
1.800.675.8416 www.healthwellfoundation.org<br />
1.800.675.8416 www.healthwellfoundation.org<br />
1.866.209.7604 www.lundbeck.com/us<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.888.427.7478 www.AmgenAssistOnline.com<br />
X 1.800.861.0048 www.bmsaccesssupport.com<br />
X<br />
X 1.866.613.4724 www.eisaireimbursement.com<br />
X 1.888.903.7277 www.oncologyaccessnow.com<br />
1.877.971.3778 https://firmagon.cmcopilot.com<br />
X 1.866.613.4724 www.eisaireimbursement.com<br />
X 1.888.427.7478 www.AmgenAssistOnline.com<br />
X 1.888.427.7478 www.AmgenAssistOnline.com<br />
1.877.456.4017 www.totect.com/reimbursement.html<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
X 1.888.847.4877 www.visitspconline.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.800.652.6227 www.jjpaf.org<br />
X 1.866.265.6491 www.caresbygsk.com<br />
X 1.855.898.2634 www.astellasaccess.com<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
X 1.800.652.6227 www.jjpaf.org<br />
X 1.888.249.4918 www.genentech-access.com<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
X 1.800.736.0003 www.bmspaf.org<br />
1.800.675.8416 www.healthwellfoundation.org<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.800.277.2254 www.oncologyaccessnow.com<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
X 1.888.762.6436 www.AmgenAssistOnline.com<br />
1.800.769.3880 www.rxoutreach.org<br />
Foundation assistance only. Please see the legend provided.<br />
1.800.675.8416 www.healthwellfoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
1.800.675.8416 www.healthwellfoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.800.292.6363 www.astrazeneca-us.com/help-affording-your-medicines<br />
X 1.800.292.6363 www.astrazeneca-us.com/help-affording-your-medicines<br />
X 1.855.559.8783 www.lillytruassist.com<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X 1.800.292.6363 www.astrazeneca-us.com/help-affording-your-medicines<br />
1.888.705.7851 www.patientrxsolutions.com<br />
X 1.800.736.0003 www.bmspaf.org<br />
15<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
PAP Quick Reference <strong>Guide</strong><br />
Drug Name Br<strong>and</strong> Name Drug Company<br />
Benefit<br />
Verification<br />
<strong>and</strong><br />
Authorization<br />
Support<br />
Drug<br />
Company<br />
Co-Pay<br />
<strong>Assistance</strong><br />
Foundation<br />
<strong>Assistance</strong><br />
16<br />
Hydroxyurea Hydrea H, U, M<br />
Ibritumomab Tiuxetin Zevalin Spectrum X X<br />
Pharmaceuticals<br />
Idarubicin Idamycin Pfizer X X X<br />
Ifosfamide Ifex H<br />
IL-2 Proleukin Prometheus X<br />
IL-11 Neumega Pfizer X X X<br />
Imatinib Gleevec Novartis X D, H, P, F<br />
Interferon alfa-2a Interferon H<br />
Interferon alfa-2b Intron A Merck X H, P<br />
Interleukin-2 Proleukin Prometheus X<br />
Interleukin-11 Neumega Pfizer X X X<br />
Irinotecan Camptosar Pfizer X X X<br />
Isotretinoin<br />
Accutane<br />
Ixabepilone Ixempra Bristol-Myers Squibb D, P<br />
Lapatinib Tykerb GlaxoSmithKline X X D, P<br />
Lenalidomide Revlimid Celgene X D, H, P<br />
Letrozole Femara Novartis X H, P, F<br />
Leucovorin Folinic Acid H<br />
Leuprolide Eligard San<strong>of</strong>i X D, H<br />
Leuprolide Acetate Lupron Abbott D, P<br />
Leuprolide Viadur D, P<br />
Levoleucovorin Fusilev Spectrum X X<br />
Pharmaceuticals<br />
Mechlorethamine Mustargen Lundbeck H, P<br />
Megastrol Megace H<br />
Mephalan Alkeran D, H<br />
Mesna Mesnex H<br />
Methotrexate Folex H, U, M<br />
Methotrexate Rheumatrex H, U, M<br />
Methotrexate Trexall H, U, M<br />
Mitomycin Mutamycin D, H, P<br />
Mitoxantrone Novantrone D, H, P<br />
Mustine Mustargen Lundbeck H, P<br />
Nelarabine Arranon GlaxoSmithKline X X H, P, F<br />
Nilotinib Tasigna Novartis X D, H, P, F<br />
Nilutamide Nil<strong>and</strong>ron San<strong>of</strong>i P<br />
Nitrogen Mustard Mustargen Lundbeck H, P<br />
Octreotide Acetate S<strong>and</strong>ostatin LAR Novartis X<br />
Ofatumumab Arzerra GlaxoSmithKline X<br />
Oprelvekin Neumega Pfizer X X H, P, F<br />
Oxaliplatin Eloxatin San<strong>of</strong>i X D, H, P<br />
Paclitaxel Onxal D, H<br />
Paclitaxel Taxol D, H, A<br />
Paclitaxel protein-bound Abraxane Celgene X X D, H, P, F<br />
Palonsetron Aloxi Eisai X<br />
Pamidronate<br />
Aredia<br />
Panitumumab Vectibix Amgen X D, H, P<br />
Pazopanib Votrient GlaxoSmithKline X X P<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Oral<br />
Prescription<br />
Savings<br />
<strong>and</strong>/or Free<br />
Medication<br />
IV &<br />
Injectable<br />
Drugs Ongoing<br />
<strong>and</strong>/or<br />
Replacement<br />
Program<br />
No Drug<br />
<strong>Assistance</strong><br />
Phone<br />
Number<br />
Website<br />
H = www.Healthwellfoundation.org<br />
F = www.patientadvocate.org<br />
P = www.panfoundation.org/fundingapplication<br />
D = www.diplomatpharmacy.com/funding<br />
A = www.pparx.org<br />
U = www.xubex.com<br />
M = www.rxoutreach.org<br />
O = www.rarediseases.org/patients-<strong>and</strong>-families<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.866.298.8433 www.zevalin.com/otherpages/reimbursement-financialsupport.aspx<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.877.776.5385 www.proleukin.com/mm/resources.aspx<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X 1.800.277.2254 www.oncologyaccessnow.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.866.363.6379 www.merck.com/merckhelps<br />
X 1.877.776.5385 www.proleukin.com/mm/resources.aspx<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X<br />
X 1.800.861.0048 www.bmsaccesssupport.com<br />
X 1.866.265.6491 www.gsk-access.com<br />
X 1.800.931.8691 www.celgenepatientsupport.com<br />
X 1.800.245.5356 www.patientassistancenow.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.888.847.4877 www.visitspconline.com<br />
X 1.800.222.6885 www.abbottpatientassistancefoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
1.888.537.8377 www.fusilev.com/reimbursement-information<br />
X 1.866.209.7604 www.lundbeck.com/us<br />
1.800.675.8416 www.healthwellfoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
1.800.675.8416 www.healthwellfoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
Foundation assistance only. Please see the legend provided.<br />
Foundation assistance only. Please see the legend provided.<br />
Foundation assistance only. Please see the legend provided.<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.866.209.7604 www.lundbeck.com/us<br />
X 1.866.265.6491 www.gsk-access.com<br />
X 1.800.277.2254 www.oncologyaccessnow.com<br />
X 1.888.847.4877 www.visitspconline.com<br />
X 1.866.209.7604 www.lundbeck.com/us<br />
X 1.800.277.2254 www.oncologyaccessnow.com<br />
X 1.866.265.6491 www.gsk-access.com<br />
X 1.877.744.5675 www.pfizerhelpfulanswers.com<br />
X 1.888.847.4877 www.visitspconline.com<br />
Foundation assistance only. Please see the legend provided.<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.800.931.8691 www.celgenepatientsupport.com<br />
X 1.866.613.4724 www.eisaireimbursement.com<br />
X<br />
X 1.888.762.6436 www.AmgenAssistOnline.com<br />
X 1.866.265.6491 www.gsk-access.com<br />
17<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
PAP Quick Reference <strong>Guide</strong><br />
Drug Name Br<strong>and</strong> Name Drug Company<br />
Benefit<br />
Verification<br />
<strong>and</strong><br />
Authorization<br />
Support<br />
Drug<br />
Company<br />
Co-Pay<br />
<strong>Assistance</strong><br />
Foundation<br />
<strong>Assistance</strong><br />
18<br />
Pegaspargase Oncaspar Sigma-Tau X X<br />
Pegfilgrastim Neulasta Amgen X X D, H<br />
Pemetrexed Alimta Eli Lilly D, H, P<br />
Pentostatin<br />
Nipent<br />
Plerixafor Mozobil San<strong>of</strong>i X X D, P<br />
Plicamycin<br />
Mithracin<br />
Ponatinib Iclusig Ariad Pharmaceuticals X X D<br />
Pralatrexate Folotyn Spectrum X O<br />
Pharmaceuticals<br />
Procarbazine Matulane Sigma-Tau X X H<br />
Radium Ra 223 dichloride X<strong>of</strong>igo Bayer Healthcare X X X<br />
Rasburicase Elitek San<strong>of</strong>i X H, P, F, O<br />
Regorafenib Stivarga Bayer Healthcare X X X<br />
Rituximab Rituxan Genentech X X D, H, P<br />
Romidepsin Istodax Celgene X P<br />
Romiplostim Nplate Amgen X X H, P, F<br />
Ruxolitinib Jakafi Tab Incyte X X X<br />
Sargramostim Leukine San<strong>of</strong>i X X H<br />
Sipuleucel-t Provenge Dendreon X P<br />
Sorafenib Nexavar Bayer Healthcare X X D, P<br />
Streptozocin<br />
Zanosar<br />
Sunitinib Sutent Pfizer X D, P<br />
Tamoxifen Nolvadex H, M<br />
Temozolomide Temodar Merck X D<br />
Temsirolimus Toresel Pfizer X P<br />
Teniposide Vumon Bristol-Myers Squibb H<br />
Thalidomide Thalomid Celgene X D, H, P<br />
Thiotepa Thioplex H<br />
Topotecan Oral Hycamptin Oral GlaxoSmithKline X X D, H, P<br />
Topotecan Hycamptin GlaxoSmithKline X X D, H, P<br />
Toremifene Fareston ProStrakan X X X<br />
Tositumomab Bexxar GlaxoSmithKline X H<br />
Trastuzumab Herceptin Genentech X X D, H, P<br />
Tretinoin (ATRA) Vesanoid Roche X<br />
Triptorelin Pamoate Trelstar Watson X<br />
Valrubicin<br />
Valstar<br />
Vemurafenib Zelboraf Genentech X X X<br />
Vinblastine Velban H<br />
Vincristine Oncovin D, H<br />
Vincristine sulfate liposome Marqibo Talon<br />
Vinorelbine Navelbine PF Pharmaceuticals H<br />
Vorinostat Zolinza Merck X D, P<br />
VP-16 Etopophos Bristol-Myers Squibb H<br />
VP-16 VePesid H<br />
Zidovudine Retrovir X<br />
Ziv-Aflibercept Zaltrap San<strong>of</strong>i X X<br />
Zoledronic acid Zometa Novartis X D, P<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Oral<br />
Prescription<br />
Savings<br />
<strong>and</strong>/or Free<br />
Medication<br />
IV &<br />
Injectable<br />
Drugs Ongoing<br />
<strong>and</strong>/or<br />
Replacement<br />
Program<br />
No Drug<br />
<strong>Assistance</strong><br />
Phone<br />
Number<br />
Website<br />
H = www.Healthwellfoundation.org<br />
F = www.patientadvocate.org<br />
P = www.panfoundation.org/fundingapplication<br />
D = www.diplomatpharmacy.com/funding<br />
A = www.pparx.org<br />
U = www.xubex.com<br />
M = www.rxoutreach.org<br />
O = www.rarediseases.org/patients-<strong>and</strong>-families<br />
X 1.800.490.3262 www.sigmatau.com/support/support_oncaspar.asp<br />
X 1.888.427.7478 www.AmgenAssistOnline.com<br />
X 1.855.559.8783 www.lillytruassist.com<br />
X<br />
X 1.888.847.4877 www.visitspconline.com<br />
X<br />
X 1.855.447.7277 www.ariadpass.com/healthcare-pr<strong>of</strong>essional<br />
X 1.877.272.7102 www.getasapinfo.com<br />
X 1.800.490.3262 www.sigmatau.com/support/support_oncaspar.asp<br />
X 1.855.696.3446 www.x<strong>of</strong>igo-us.com<br />
X 1.888.847.4877 www.visitspconline.com<br />
X 1.866.639.2827 www.stivarga-us.com/access.html<br />
X 1.888.249.4918 www.genentech-access.com<br />
X 1.800.931.8691 www.celgenepatientsupport.com<br />
X 1.888.427.7478 www.AmgenAssistOnline.com<br />
X 1.855.452.5234 www.incytecares.com<br />
X 1.888.847.4877 www.visitspconline.com<br />
X 1.877.336.3736 www.provenge.com/reimbursement.aspx<br />
X 1.866.639.2827 www.nexavar-us.com<br />
X<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
Foundation assistance only. Please see the legend provided.<br />
X 1.800.994.2111 www.merck.com/merckhelps<br />
X 1.866.706.2400 www.pfizerhelpfulanswers.com<br />
X 1.800.736.0003 www.bmspaf.org<br />
X 1.800.931.8691 www.celgenepatientsupport.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.866.265.6491 www.commitmenttoaccess.com<br />
X 1.866.265.6491 www.caresbygsk.com<br />
X 1.888.705.7851 www.patientsrxsolutions.com<br />
X 1.866.265.6491 www.commitmenttoaccess.com<br />
X 1.888.249.4918 www.genentech-access.com<br />
X 1.866.754.3315 www.trelstar.com/hcp-reimbursement-<strong>and</strong>-support.asp<br />
X<br />
X 1.888.249.4918 www.genentech-access.com<br />
1.800.675.8416 www.healthwellfoundation.org<br />
Foundation assistance only. Please see the legend provided.<br />
X<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.866.363.6379 www.merck.com/merckhelps<br />
X 1.800.736.0003 www.bmspaf.org<br />
1.800.675.8416 www.healthwellfoundation.org<br />
X 1.888.847.4877 www.visitspconline.com<br />
X 1.800.245.5356 www.patientassistancenow.com<br />
The PAP Quick Reference <strong>Guide</strong> was provided courtesy <strong>of</strong> Wendalyn Andrews, Practice Manager,<br />
Hematology <strong>and</strong> Oncology, The University <strong>of</strong> Arizona Cancer Center – North Campus.<br />
19<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
PAP Flow Chart<br />
Step 1 Step 2 Step 3<br />
Provider writes<br />
chemotherapy order<br />
for patient.<br />
Chemotherapy order<br />
is sent to finance staff.<br />
Staff identifies the patient’s<br />
financial status <strong>and</strong> follows the<br />
appropriate flow chart below.<br />
20<br />
s s s s s s s s s<br />
No insurance<br />
Medicaid Program<br />
Medicare Only<br />
Medicare & Supplemental<br />
Medicare & Secondary<br />
Medicare Advantage<br />
Other Government Programs<br />
Managed Care<br />
Commercial<br />
Identify if patient<br />
qualifies for any programs<br />
(SSDI, Medicaid,<br />
etc.). Identify if<br />
replacement drugs are<br />
available.<br />
Verify benefits.<br />
Verify benefits.<br />
Verify benefits.<br />
Verify benefits.<br />
Verify benefits.<br />
Verify benefits.<br />
Verify benefits.<br />
Verify benefits.<br />
Fill out forms for all<br />
programs. Complete<br />
forms for companies<br />
that have a replacement<br />
program if<br />
patient qualifies.<br />
Verify drugs are<br />
indicated for dx<br />
<strong>and</strong> authorize if<br />
necessary.<br />
Verify drugs are<br />
indicated for dx.<br />
Verify drugs are<br />
indicated for dx.<br />
Verify drugs are<br />
indicated for dx<br />
<strong>and</strong> authorize<br />
secondary insurance<br />
if necessary.<br />
Verify drugs are<br />
indicated for dx<br />
<strong>and</strong> authorize if<br />
necessary.<br />
Verify drugs are<br />
indicated for dx<br />
<strong>and</strong> authorize if<br />
necessary.<br />
Verify drugs are<br />
indicated for dx<br />
<strong>and</strong> authorize if<br />
necessary.<br />
Verify drugs are<br />
indicated for dx<br />
<strong>and</strong> authorize if<br />
necessary.<br />
Identify if foundation<br />
funding is available<br />
for anything not able<br />
to get replaced.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Identify if replacement<br />
drugs are<br />
available if necessary.<br />
Will need to appeal<br />
to receive drugs.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Identify patient’s<br />
responsibility.<br />
Identify patient’s<br />
responsibility.<br />
Identify patient’s<br />
responsibility <strong>and</strong><br />
if there is none start<br />
treatment.<br />
Identify patient’s<br />
responsibility.<br />
Identify patient’s<br />
responsibility.<br />
Identify patient’s<br />
responsibility.<br />
Identify patient’s<br />
responsibility.<br />
Identify patient’s<br />
responsibility.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
The PAP Flow Chart was provided courtesy <strong>of</strong> Wendalyn Andrews,<br />
Practice Manager, Hematology <strong>and</strong> Oncology,<br />
The University <strong>of</strong> Arizona Cancer Center – North Campus.<br />
s<br />
Identify if patient<br />
qualifies for charity<br />
care within the clinic<br />
or institution <strong>and</strong><br />
complete paperwork.<br />
Create payment<br />
plan for any balance<br />
if available or<br />
collect balance.<br />
s s s s s s s s<br />
Collect out-<strong>of</strong>-pocket<br />
costs.<br />
Identify if foundation<br />
assistance is available.<br />
If patient has responsibility,<br />
identify if<br />
foundation assistance is<br />
available.<br />
Identify if foundation<br />
assistance is available.<br />
Identify if foundation<br />
assistance is available.<br />
Identify if foundation<br />
assistance is available.<br />
Identify if manufacturer<br />
assistance is<br />
available <strong>and</strong> fill out<br />
forms if applicable.<br />
Identify if manufacturer<br />
assistance is<br />
available <strong>and</strong> fill out<br />
forms if applicable.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
If no manufacturer<br />
assistance, then<br />
identify if foundation<br />
assistance is<br />
available.<br />
If no manufacturer<br />
assistance, then<br />
identify if foundation<br />
assistance is<br />
available.<br />
Identify if patient<br />
qualifies for charity<br />
care within the clinic<br />
or institution <strong>and</strong><br />
complete paperwork.<br />
If patient qualifies,<br />
send in EOB <strong>and</strong>/or<br />
anything else to help<br />
verify amount for<br />
foundation to pay.<br />
If patient qualifies,<br />
send in EOB <strong>and</strong>/or<br />
anything else to help<br />
verify amount for<br />
foundation to pay.<br />
If patient qualifies,<br />
send in EOB <strong>and</strong>/or<br />
anything else to help<br />
verify amount for<br />
foundation to pay.<br />
If patient qualifies,<br />
send in EOB <strong>and</strong>/or<br />
anything else to help<br />
verify amount for<br />
foundation to pay.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Fill out forms for<br />
foundation funding<br />
that is available.<br />
Create payment plan<br />
for any balance if<br />
available or collect<br />
balance.<br />
If any balance, create<br />
payment plan or<br />
collect balance.<br />
If any balance, create<br />
payment plan or<br />
collect balance.<br />
If any balance, create<br />
payment plan or<br />
collect balance.<br />
If any balance, create<br />
payment plan or<br />
collect balance.<br />
If patient qualifies<br />
for manuafacturer or<br />
foundation assistance,<br />
send in EOB <strong>and</strong>/or<br />
anything else to help<br />
verify amount owed.<br />
If patient qualifies<br />
for manuafacturer or<br />
foundation assistance,<br />
send in EOB <strong>and</strong>/or<br />
anything else to help<br />
verify amount owed.<br />
Process payment<br />
using co-pay card or<br />
whatever form <strong>of</strong> payment<br />
the program has.<br />
Process payment<br />
using co-pay card or<br />
whatever form <strong>of</strong> payment<br />
the program has.<br />
If any balance create<br />
payment plan or<br />
collect balance from<br />
patient.<br />
If any balance, create<br />
payment plan or<br />
collect balance from<br />
patient.<br />
21<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
SUTENT IN TOUCH: Connecting your patients to our Oncology<br />
Certified Nurses to help support them during treatment.<br />
SUTENT IN TOUCH prOvIdES:<br />
Oncology Certified Nurses (OCNs) —Trained to support your<br />
SUTENT patients, these nurses provide timely information, including<br />
tips to help manage certain adverse reactions.<br />
Tools to Keep <strong>Patient</strong>s on Track —Throughout treatment, patients receive<br />
calls, e-mails, <strong>and</strong> mailings timed to align with their treatment schedule.<br />
yOUr paTIENTS CaN ENrOll by:<br />
• Returning the business reply card in the<br />
SUTENT <strong>Patient</strong> Resource Kit<br />
• Visiting SUTENT.com/InTouch<br />
• Calling 1-877-5-SUTENT (1-877-578-8368)<br />
SUTENT ® (sunitinib malate) is indicated for the treatment <strong>of</strong> advanced renal cell carcinoma (RCC), gastrointestinal<br />
stromal tumor (GIST) after disease progression on or intolerance to imatinib mesylate, <strong>and</strong> progressive, well-differentiated<br />
pancreatic neuroendocrine tumors (pNET) in patients with unresectable locally advanced or metastatic disease.<br />
Important Safety Information<br />
Hepatotoxicity has been observed in clinical trials <strong>and</strong> post-marketing experience.<br />
This hepatotoxicity may be severe, <strong>and</strong> deaths have been reported.<br />
Monitor liver function tests before initiation <strong>of</strong> treatment, during each cycle <strong>of</strong> treatment, <strong>and</strong> as clinically indicated. SUTENT<br />
should be interrupted for Grade 3 or 4 drug-related hepatic adverse events <strong>and</strong> discontinued if there is no resolution. Do not<br />
restart SUTENT if patients subsequently experience severe changes in liver function tests or have other signs <strong>and</strong> symptoms<br />
<strong>of</strong> liver failure.
S:10 in<br />
T:10.75 in<br />
SUTENT ® (sunitinib malate) is indicated for the treatment <strong>of</strong><br />
advanced renal cell carcinoma (RCC), gastrointestinal stromal<br />
tumor (GIST) after disease progression on or intolerance to<br />
imatinib mesylate, <strong>and</strong> progressive, well-differentiated pancreatic<br />
neuroendocrine tumors (pNET) in patients with unresectable<br />
locally advanced or metastatic disease.<br />
Important Safety Information<br />
Hepatotoxicity has been observed in clinical trials <strong>and</strong> postmarketing<br />
experience. This hepatotoxicity may be severe, <strong>and</strong><br />
deaths have been reported. Monitor liver function tests before<br />
initiation <strong>of</strong> treatment, during each cycle <strong>of</strong> treatment, <strong>and</strong> as<br />
clinically indicated. SUTENT should be interrupted for Grade 3<br />
or 4 drug-related hepatic adverse events <strong>and</strong> discontinued if there<br />
is no resolution. Do not restart SUTENT if patients subsequently<br />
experience severe changes in liver function tests or have other<br />
signs <strong>and</strong> symptoms <strong>of</strong> liver failure.<br />
Women <strong>of</strong> childbearing potential should be advised <strong>of</strong> the<br />
potential hazard to the fetus <strong>and</strong> to avoid becoming pregnant.<br />
Given the potential for serious adverse reactions (ARs) in nursing<br />
infants, a decision should be made whether to discontinue<br />
nursing or SUTENT.<br />
Cardiovascular events, including heart failure, myocardial<br />
disorders, <strong>and</strong> cardiomyopathy, some <strong>of</strong> which were fatal, have<br />
been reported. Monitor patients for signs <strong>and</strong> symptoms <strong>of</strong><br />
congestive heart failure (CHF) <strong>and</strong>, in the presence <strong>of</strong> clinical<br />
manifestations, discontinuation is recommended. <strong>Patient</strong>s<br />
who presented with cardiac events, pulmonary embolism, or<br />
cerebrovascular events within the previous 12 months were<br />
excluded from clinical studies.<br />
SUTENT has been shown to prolong QT interval in a dosedependent<br />
manner, which may lead to an increased risk for<br />
ventricular arrhythmias including torsades de pointes, which has<br />
been seen in
HIGHLIGHTS OF PRESCRIBING INFORMATION<br />
These highlights do not include all the information needed to use SUTENT safely<br />
<strong>and</strong> effectively. See full prescribing information for SUTENT.<br />
SUTENT ® (sunitinib malate) capsules, oral<br />
Initial U.S. Approval: 2006<br />
WARNING: HEPATOTOXICITY<br />
See full prescribing information for complete boxed warning.<br />
Hepatotoxicity has been observed in clinical trials <strong>and</strong> post-marketing experience.<br />
This hepatotoxicity may be severe, <strong>and</strong> deaths have been reported. [See Warnings<br />
<strong>and</strong> Precautions (5.1)]<br />
----------------------------------RECENT MAJOR CHANGES----------------------------------<br />
Warnings <strong>and</strong> Precautions, Osteonecrosis <strong>of</strong> the Jaw (5.7) 4/2012<br />
Warnings <strong>and</strong> Precautions, Tumor Lysis Syndrome (5.8) 4/2012<br />
----------------------------------INDICATIONS AND USAGE----------------------------------<br />
SUTENT is a kinase inhibitor indicated for the treatment <strong>of</strong>:<br />
• Gastrointestinal stromal tumor (GIST) after disease progression on or intolerance<br />
to imatinib mesylate. (1.1)<br />
• Advanced renal cell carcinoma (RCC). (1.2)<br />
• Progressive, well-differentiated pancreatic neuroendocrine tumors (pNET) in<br />
patients with unresectable locally advanced or metastatic disease. (1.3)<br />
-------------------------------DOSAGE AND ADMINISTRATION-------------------------------<br />
GIST <strong>and</strong> RCC:<br />
• 50 mg orally once daily, with or without food, 4 weeks on treatment followed by<br />
2 weeks <strong>of</strong>f. (2.1)<br />
pNET:<br />
• 37.5 mg orally once daily, with or without food, continuously without a scheduled<br />
<strong>of</strong>f-treatment period. (2.2)<br />
Dose Modification:<br />
• Dose interruptions <strong>and</strong>/or dose adjustments <strong>of</strong> 12.5 mg recommended based on<br />
individual safety <strong>and</strong> tolerability. (2.3)<br />
-----------------------------DOSAGE FORMS AND STRENGTHS----------------------------<br />
• Capsules: 12.5 mg, 25 mg, 50 mg (3)<br />
-------------------------------------CONTRAINDICATIONS------------------------------------<br />
• None (4)<br />
-------------------------------WARNINGS AND PRECAUTIONS-------------------------------<br />
• Hepatotoxicity, including liver failure, has been observed. Monitor liver function<br />
tests before initiation <strong>of</strong> treatment, during each cycle <strong>of</strong> treatment, <strong>and</strong> as clinically<br />
indicated. SUTENT should be interrupted for Grade 3 or 4 drug-related hepatic<br />
adverse events <strong>and</strong> discontinued if there is no resolution. Do not restart SUTENT if<br />
patients subsequently experience severe changes in liver function tests or have<br />
other signs <strong>and</strong> symptoms <strong>of</strong> liver failure. (5.1)<br />
• Women <strong>of</strong> childbearing potential should be advised <strong>of</strong> the potential hazard to the<br />
fetus <strong>and</strong> to avoid becoming pregnant. (5.2)<br />
• Cardiac toxicity including left ventricular ejection fraction declines to below the<br />
lower limit <strong>of</strong> normal <strong>and</strong> cardiac failure including death have occurred. Monitor<br />
patients for signs <strong>and</strong> symptoms <strong>of</strong> congestive heart failure. (5.3)<br />
• Prolonged QT intervals <strong>and</strong> Torsade de Pointes have been observed. Use with<br />
caution in patients at higher risk for developing QT interval prolongation. When<br />
using SUTENT, monitoring with on-treatment electrocardiograms <strong>and</strong> electrolytes<br />
should be considered. (5.4)<br />
• Hypertension may occur. Monitor blood pressure <strong>and</strong> treat as needed. (5.5)<br />
• Hemorrhagic events including tumor-related hemorrhage have occurred. Perform<br />
serial complete blood counts <strong>and</strong> physical examinations. (5.6)<br />
• Osteonecrosis <strong>of</strong> the jaw has been reported. Consider preventive dentistry prior to<br />
treatment with SUTENT. If possible, avoid invasive dental procedures, particularly<br />
in patients receiving intravenous bisphosphonate therapy. (5.7)<br />
• Cases <strong>of</strong> Tumor Lysis Syndrome (TLS) have been reported primarily in patients<br />
with RCC <strong>and</strong> GIST with high tumor burden. Monitor these patients closely <strong>and</strong><br />
treat as clinically indicated. (5.8)<br />
• Thyroid dysfunction may occur. <strong>Patient</strong>s with signs <strong>and</strong>/or symptoms suggestive <strong>of</strong><br />
hypothyroidism or hyperthyroidism should have laboratory monitoring <strong>of</strong> thyroid<br />
function performed <strong>and</strong> be treated as per st<strong>and</strong>ard medical practice. (5.9)<br />
• Temporary interruption <strong>of</strong> therapy with SUTENT is recommended in patients<br />
undergoing major surgical procedures. (5.10)<br />
• Adrenal hemorrhage was observed in animal studies. Monitor adrenal function in<br />
case <strong>of</strong> stress such as surgery, trauma or severe infection. (5.11)<br />
------------------------------------ADVERSE REACTIONS-------------------------------------<br />
• The most common adverse reactions (≥20%) are fatigue, asthenia, fever, diarrhea,<br />
nausea, mucositis/stomatitis, vomiting, dyspepsia, abdominal pain, constipation,<br />
hypertension, peripheral edema, rash, h<strong>and</strong>-foot syndrome, skin discoloration, dry<br />
skin, hair color changes, altered taste, headache, back pain, arthralgia, extremity<br />
pain, cough, dyspnea, anorexia, <strong>and</strong> bleeding. (6)<br />
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer, Inc. at 1-800-438-1985<br />
or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.<br />
------------------------------------DRUG INTERACTIONS-------------------------------------<br />
• CYP3A4 Inhibitors: Consider dose reduction <strong>of</strong> SUTENT when administered with<br />
strong CYP3A4 inhibitors. (7.1)<br />
• CYP3A4 Inducers: Consider dose increase <strong>of</strong> SUTENT when administered with<br />
CYP3A4 inducers. (7.2)<br />
See 17 for PATIENT COUNSELING INFORMATION <strong>and</strong> FDA-approved patient labeling.<br />
Revised: 11/2012<br />
FULL PRESCRIBING INFORMATION: CONTENTS*<br />
WARNING: HEPATOTOXICITY<br />
1 INDICATIONS AND USAGE<br />
1.1 Gastrointestinal stromal tumor<br />
1.2 Advanced renal cell carcinoma<br />
1.3 Advanced pancreatic neuroendocrine tumors<br />
2 DOSAGE AND ADMINISTRATION<br />
2.1 Recommended Dose for GIST <strong>and</strong> RCC<br />
2.2 Recommended Dose for pNET<br />
2.3 Dose Modification<br />
3 DOSAGE FORMS AND STRENGTHS<br />
4 CONTRAINDICATIONS<br />
5 WARNINGS AND PRECAUTIONS<br />
5.1 Hepatotoxicity<br />
5.2 Pregnancy<br />
5.3 Left Ventricular Dysfunction<br />
5.4 QT Interval Prolongation <strong>and</strong> Torsade de Pointes<br />
5.5 Hypertension<br />
5.6 Hemorrhagic Events<br />
5.7 Osteonecrosis <strong>of</strong> the Jaw<br />
5.8 Tumor Lysis Syndrome<br />
5.9 Thyroid Dysfunction<br />
5.10 Wound Healing<br />
5.11 Adrenal Function<br />
5.12 Laboratory Tests<br />
6 ADVERSE REACTIONS<br />
6.1 Adverse Reactions in GIST Study A<br />
6.2 Adverse Reactions in the Treatment-Naïve RCC Study<br />
6.3 Adverse Reactions in the Phase 3 pNET Study<br />
6.4 Venous Thromboembolic Events<br />
6.5 Reversible Posterior Leukoencephalopathy Syndrome<br />
6.6 Pancreatic <strong>and</strong> Hepatic Function<br />
6.7 Post-marketing Experience<br />
7 DRUG INTERACTIONS<br />
7.1 CYP3A4 Inhibitors<br />
7.2 CYP3A4 Inducers<br />
7.3 In Vitro Studies <strong>of</strong> CYP Inhibition <strong>and</strong> Induction<br />
8 USE IN SPECIFIC POPULATIONS<br />
8.1 Pregnancy<br />
8.3 Nursing Mothers<br />
8.4 Pediatric Use<br />
8.5 Geriatric Use<br />
8.6 Hepatic Impairment<br />
8.7 Renal Impairment<br />
10 OVERDOSAGE<br />
11 DESCRIPTION<br />
12 CLINICAL PHARMACOLOGY<br />
12.1 Mechanism <strong>of</strong> Action<br />
12.3 Pharmacokinetics<br />
12.4 Cardiac Electrophysiology<br />
13 NONCLINICAL TOXICOLOGY<br />
13.1 Carcinogenesis, Mutagenesis, Impairment <strong>of</strong> Fertility<br />
14 CLINICAL STUDIES<br />
14.1 Gastrointestinal Stromal Tumor<br />
14.2 Renal Cell Carcinoma<br />
14.3 Pancreatic Neuroendocrine Tumors<br />
16 HOW SUPPLIED/STORAGE AND HANDLING<br />
17 PATIENT COUNSELING INFORMATION<br />
17.1 Gastrointestinal Disorders<br />
17.2 Skin Effects<br />
17.3 Other Common Events<br />
17.4 Musculoskeletal Disorders<br />
17.5 Concomitant Medications<br />
17.6 FDA-Approved <strong>Patient</strong> Labeling<br />
* Sections or subsections omitted from the full prescribing information are not listed.
FULL PRESCRIBING INFORMATION<br />
WARNING: HEPATOTOXICITY<br />
Hepatotoxicity has been observed in clinical trials <strong>and</strong> post-marketing experience.<br />
This hepatotoxicity may be severe, <strong>and</strong> deaths have been reported. [See Warnings<br />
<strong>and</strong> Precautions (5.1)]<br />
1 INDICATIONS AND USAGE<br />
1.1 Gastrointestinal Stromal Tumor (GIST)<br />
SUTENT is indicated for the treatment <strong>of</strong> gastrointestinal stromal tumor after disease<br />
progression on or intolerance to imatinib mesylate.<br />
1.2 Advanced Renal Cell Carcinoma (RCC)<br />
SUTENT is indicated for the treatment <strong>of</strong> advanced renal cell carcinoma.<br />
1.3 Advanced Pancreatic Neuroendocrine Tumors (pNET)<br />
SUTENT is indicated for the treatment <strong>of</strong> progressive, well-differentiated pancreatic<br />
neuro endocrine tumors in patients with unresectable locally advanced or metastatic<br />
disease.<br />
2 DOSAGE AND ADMINISTRATION<br />
2.1 Recommended Dose for GIST <strong>and</strong> RCC<br />
The recommended dose <strong>of</strong> SUTENT for gastrointestinal stromal tumor (GIST) <strong>and</strong><br />
advanced renal cell carcinoma (RCC) is one 50 mg oral dose taken once daily, on a<br />
schedule <strong>of</strong> 4 weeks on treatment followed by 2 weeks <strong>of</strong>f (Schedule 4/2). SUTENT may<br />
be taken with or without food.<br />
2.2 Recommended Dose for pNET<br />
The recommended dose <strong>of</strong> SUTENT for pancreatic neuroendocrine tumors (pNET) is<br />
37.5 mg taken orally once daily continuously without a scheduled <strong>of</strong>f-treatment period.<br />
SUTENT may be taken with or without food.<br />
2.3 Dose Modification<br />
Dose interruption <strong>and</strong>/or dose modification in 12.5 mg increments or decrements is<br />
recommended based on individual safety <strong>and</strong> tolerability. The maximum dose administered<br />
in the Phase 3 pNET study was 50 mg daily.<br />
Strong CYP3A4 inhibitors such as ketoconazole may increase sunitinib plasma<br />
concentrations. Selection <strong>of</strong> an alternate concomitant medication with no or minimal<br />
enzyme inhibition potential is recommended. A dose reduction for SUTENT to a minimum<br />
<strong>of</strong> 37.5 mg (GIST <strong>and</strong> RCC) or 25 mg (pNET) daily should be considered if SUTENT must<br />
be co-administered with a strong CYP3A4 inhibitor [see Drug Interactions (7.1) <strong>and</strong><br />
Clinical Pharmacology (12.3)].<br />
CYP3A4 inducers such as rifampin may decrease sunitinib plasma concentrations.<br />
Selection <strong>of</strong> an alternate concomitant medication with no or minimal enzyme induction<br />
potential is recommended. A dose increase for SUTENT to a maximum <strong>of</strong> 87.5 mg<br />
(GIST <strong>and</strong> RCC) or 62.5 mg (pNET) daily should be considered if SUTENT must be coadministered<br />
with a CYP3A4 inducer. If dose is increased, the patient should be monitored<br />
carefully for toxicity [see Drug Interactions (7.2) <strong>and</strong> Clinical Pharmacology (12.3)].<br />
3 DOSAGE FORMS AND STRENGTHS<br />
12.5 mg capsules<br />
Hard gelatin capsule with orange cap <strong>and</strong> orange body, printed with white ink “Pfizer”<br />
on the cap <strong>and</strong> “STN 12.5 mg” on the body.<br />
25 mg capsules<br />
Hard gelatin capsule with caramel cap <strong>and</strong> orange body, printed with white ink “Pfizer”<br />
on the cap <strong>and</strong> “STN 25 mg” on the body.<br />
50 mg capsules<br />
Hard gelatin capsule with caramel top <strong>and</strong> caramel body, printed with white ink<br />
“Pfizer” on the cap <strong>and</strong> “STN 50 mg” on the body.<br />
4 CONTRAINDICATIONS<br />
None<br />
5 WARNINGS AND PRECAUTIONS<br />
5.1 Hepatotoxicity<br />
SUTENT has been associated with hepatotoxicity, which may result in liver failure or<br />
death. Liver failure has been observed in clinical trials (7/2281 [0.3%]) <strong>and</strong> post-marketing<br />
experience. Liver failure signs include jaundice, elevated transaminases <strong>and</strong>/or hyperbilirubinemia<br />
in conjunction with encephalopathy, coagulopathy, <strong>and</strong>/or renal failure. Monitor<br />
liver function tests (ALT, AST, bilirubin) before initiation <strong>of</strong> treatment, during each cycle <strong>of</strong><br />
treatment, <strong>and</strong> as clinically indicated. SUTENT should be interrupted for Grade 3 or 4 drugrelated<br />
hepatic adverse events <strong>and</strong> discontinued if there is no resolution. Do not restart<br />
SUTENT if patients subsequently experience severe changes in liver function tests or have<br />
other signs <strong>and</strong> symptoms <strong>of</strong> liver failure.<br />
Safety in patients with ALT or AST >2.5 x ULN or, if due to liver metastases, >5.0 x<br />
ULN has not been established.<br />
5.2 Pregnancy<br />
SUTENT can cause fetal harm when administered to a pregnant woman. As<br />
angio genesis is a critical component <strong>of</strong> embryonic <strong>and</strong> fetal development, inhibition <strong>of</strong><br />
angiogenesis following administration <strong>of</strong> SUTENT should be expected to result in<br />
adverse effects on pregnancy. In animal reproductive studies in rats <strong>and</strong> rabbits, sunitinib<br />
was teratogenic, embryotoxic, <strong>and</strong> fetotoxic. There are no adequate <strong>and</strong> well-controlled<br />
studies <strong>of</strong> SUTENT in pregnant women. If this drug is used during pregnancy, or if the<br />
patient becomes pregnant while taking this drug, the patient should be apprised <strong>of</strong> the<br />
potential hazard to a fetus. Women <strong>of</strong> childbearing potential should be advised to avoid<br />
becoming pregnant while receiving treatment with SUTENT.<br />
5.3 Left Ventricular Dysfunction<br />
In the presence <strong>of</strong> clinical manifestations <strong>of</strong> congestive heart failure (CHF), discontinuation<br />
<strong>of</strong> SUTENT is recommended. The dose <strong>of</strong> SUTENT should be interrupted <strong>and</strong>/or<br />
reduced in patients without clinical evidence <strong>of</strong> CHF but with an ejection fraction 20% below baseline.<br />
Cardiovascular events, including heart failure, myocardial disorders <strong>and</strong> cardiomyo -<br />
pathy, some <strong>of</strong> which were fatal, have been reported through post-marketing experience.<br />
For GIST <strong>and</strong> RCC, more patients treated with SUTENT experienced decline in left ventricular<br />
ejection fraction (LVEF) than patients receiving either placebo or interferon-a (IFN-a). In<br />
the double-blind treatment phase <strong>of</strong> GIST Study A, 22/209 patients (11%) on SUTENT <strong>and</strong><br />
3/102 patients (3%) on placebo had treatment-emergent LVEF values below the lower limit<br />
<strong>of</strong> normal (LLN). Nine <strong>of</strong> 22 GIST patients on SUTENT with LVEF changes recovered without<br />
intervention. Five patients had documented LVEF recovery following intervention (dose<br />
reduction: one patient; addition <strong>of</strong> antihypertensive or diuretic medications: four patients).<br />
Six patients went <strong>of</strong>f study without documented recovery. Additionally, three patients on<br />
SUTENT had Grade 3 reductions in left ventricular systolic function to LVEF 20% below<br />
baseline <strong>and</strong> to below 50%. Left ventricular dysfunction was reported in four patients (1%)<br />
<strong>and</strong> CHF in two patients (
eported in post-marketing experience in patients treated with SUTENT for MRCC, GIST <strong>and</strong><br />
metastatic lung cancer. SUTENT is not approved for use in patients with lung cancer.<br />
Treatment-emergent Grade 3 <strong>and</strong> 4 tumor hemorrhage occurred in 5/202 patients (3%)<br />
with GIST receiving SUTENT on Study A. Tumor hemorrhages were observed as early as<br />
Cycle 1 <strong>and</strong> as late as Cycle 6. One <strong>of</strong> these five patients received no further drug following<br />
tumor hemorrhage. None <strong>of</strong> the other four patients discontinued treatment or experienced<br />
dose delay due to tumor hemorrhage. No patients with GIST in the Study A placebo arm<br />
were observed to undergo intratumoral hemorrhage. Clinical assessment <strong>of</strong> these events<br />
should include serial complete blood counts (CBCs) <strong>and</strong> physical examinations.<br />
Serious, sometimes fatal gastrointestinal complications including gastrointestinal<br />
perforation, have occurred rarely in patients with intra-abdominal malignancies treated<br />
with SUTENT.<br />
5.7 Osteonecrosis <strong>of</strong> the Jaw (ONJ)<br />
ONJ has been observed in clinical trials <strong>and</strong> has been reported in post-marketing<br />
experience in patients treated with sunitinib. Concomitant exposure to other risk factors,<br />
such as bisphosphonates or dental disease, may increase the risk <strong>of</strong> osteonecrosis <strong>of</strong><br />
the jaw.<br />
5.8 Tumor Lysis Syndrome (TLS)<br />
Cases <strong>of</strong> TLS, some fatal, have been observed in clinical trials <strong>and</strong> have been reported in<br />
post-marketing experience, primarily in patients with RCC or GIST treated with SUTENT.<br />
<strong>Patient</strong>s generally at risk <strong>of</strong> TLS are those with high tumor burden prior to treatment.<br />
These patients should be monitored closely <strong>and</strong> treated as clinically indicated.<br />
5.9 Thyroid Dysfunction<br />
Baseline laboratory measurement <strong>of</strong> thyroid function is recommended <strong>and</strong> patients<br />
with hypothyroidism or hyperthyroidism should be treated as per st<strong>and</strong>ard medical practice<br />
prior to the start <strong>of</strong> SUTENT treatment. All patients should be observed closely for<br />
signs <strong>and</strong> symptoms <strong>of</strong> thyroid dysfunction on SUTENT treatment. <strong>Patient</strong>s with signs<br />
<strong>and</strong>/or symptoms suggestive <strong>of</strong> thyroid dysfunction should have laboratory monitoring <strong>of</strong><br />
thyroid function performed <strong>and</strong> be treated as per st<strong>and</strong>ard medical practice.<br />
Treatment-emergent acquired hypothyroidism was noted in eight GIST patients (4%)<br />
on SUTENT versus one (1%) on placebo. Hypothyroidism was reported as an adverse<br />
reaction in sixty-one patients (16%) on SUTENT in the treatment-naïve RCC study <strong>and</strong> in<br />
three patients (1%) in the IFN-a arm. Hypothyroidism was reported as an adverse<br />
reaction in 6/83 patients (7%) on SUTENT in the Phase 3 pNET study <strong>and</strong> in 1/82 patients<br />
(1%) in the placebo arm.<br />
Cases <strong>of</strong> hyperthyroidism, some followed by hypothyroidism, have been reported in<br />
clinical trials <strong>and</strong> through post-marketing experience.<br />
5.10 Wound Healing<br />
Cases <strong>of</strong> impaired wound healing have been reported during SUTENT therapy.<br />
Temporary interruption <strong>of</strong> SUTENT therapy is recommended for precautionary reasons in<br />
patients undergoing major surgical procedures. There is limited clinical experience regarding<br />
the timing <strong>of</strong> reinitiation <strong>of</strong> therapy following major surgical intervention. Therefore,<br />
the decision to resume SUTENT therapy following a major surgical intervention should be<br />
based upon clinical judgment <strong>of</strong> recovery from surgery.<br />
5.11 Adrenal Function<br />
Physicians prescribing SUTENT are advised to monitor for adrenal insufficiency in<br />
patients who experience stress such as surgery, trauma or severe infection.<br />
Adrenal toxicity was noted in non-clinical repeat dose studies <strong>of</strong> 14 days to 9 months<br />
in rats <strong>and</strong> monkeys at plasma exposures as low as 0.7 times the AUC observed in clinical<br />
studies. Histological changes <strong>of</strong> the adrenal gl<strong>and</strong> were characterized as hemorrhage,<br />
necrosis, congestion, hypertrophy <strong>and</strong> inflammation. In clinical studies, CT/MRI obtained<br />
in 336 patients after exposure to one or more cycles <strong>of</strong> SUTENT demonstrated no evidence<br />
<strong>of</strong> adrenal hemorrhage or necrosis. ACTH stimulation testing was performed in approximately<br />
400 patients across multiple clinical trials <strong>of</strong> SUTENT. Among patients with normal<br />
baseline ACTH stimulation testing, one patient developed consistently abnormal test<br />
results during treatment that are unexplained <strong>and</strong> may be related to treatment with<br />
SUTENT. Eleven additional patients with normal baseline testing had abnormalities in the<br />
final test performed, with peak cortisol levels <strong>of</strong> 12-16.4 mcg/dL (normal >18 mcg/dL)<br />
following stimulation. None <strong>of</strong> these patients were reported to have clinical evidence <strong>of</strong><br />
adrenal insufficiency.<br />
5.12 Laboratory Tests<br />
CBCs with platelet count <strong>and</strong> serum chemistries including phosphate should be<br />
performed at the beginning <strong>of</strong> each treatment cycle for patients receiving treatment<br />
with SUTENT.<br />
6 ADVERSE REACTIONS<br />
The data described below reflect exposure to SUTENT in 660 patients who participated<br />
in the double-blind treatment phase <strong>of</strong> a placebo-controlled trial (n=202) for the treatment<br />
<strong>of</strong> GIST [see Clinical Studies (14.1)], an active-controlled trial (n=375) for the treatment <strong>of</strong><br />
RCC [see Clinical Studies (14.2)] or a placebo-controlled trial (n=83) for the treatment <strong>of</strong><br />
pNET [see Clinical Studies (14.3)]. The GIST <strong>and</strong> RCC patients received a starting oral<br />
dose <strong>of</strong> 50 mg daily on Schedule 4/2 in repeated cycles, <strong>and</strong> the pNET patients received a<br />
starting oral dose <strong>of</strong> 37.5 mg daily without scheduled <strong>of</strong>f-treatment periods.<br />
The most common adverse reactions (≥20%) in patients with GIST, RCC or pNET<br />
are fatigue, asthenia, fever, diarrhea, nausea, mucositis/stomatitis, vomiting, dyspepsia,<br />
abdominal pain, constipation, hypertension, peripheral edema, rash, h<strong>and</strong>-foot syndrome,<br />
skin discoloration, dry skin, hair color changes, altered taste, headache, back pain,<br />
arthralgia, extremity pain, cough, dyspnea, anorexia, <strong>and</strong> bleeding. The potentially serious<br />
adverse reactions <strong>of</strong> hepatotoxicity, left ventricular dysfunction, QT interval prolongation,<br />
hemorrhage, hypertension, thyroid dysfunction, <strong>and</strong> adrenal function are discussed in<br />
Warnings <strong>and</strong> Precautions (5). Other adverse reactions occurring in GIST, RCC <strong>and</strong> pNET<br />
studies are described below.<br />
Because clinical trials are conducted under widely varying conditions, adverse reaction<br />
rates observed in the clinical trials <strong>of</strong> a drug cannot be directly compared to rates in the<br />
clinical trials <strong>of</strong> another drug <strong>and</strong> may not reflect the rates observed in practice.<br />
6.1 Adverse Reactions in GIST Study A<br />
Median duration <strong>of</strong> blinded study treatment was two cycles for patients on SUTENT<br />
(mean 3.0, range 1-9) <strong>and</strong> one cycle (mean 1.8, range 1-6) for patients on placebo at the<br />
time <strong>of</strong> the interim analysis. Dose reductions occurred in 23 patients (11%) on SUTENT<br />
<strong>and</strong> none on placebo. Dose interruptions occurred in 59 patients (29%) on SUTENT <strong>and</strong><br />
31 patients (30%) on placebo. The rates <strong>of</strong> treatment-emergent, non-fatal adverse<br />
reactions resulting in permanent discontinuation were 7% <strong>and</strong> 6% in the SUTENT <strong>and</strong><br />
placebo groups, respectively.<br />
Most treatment-emergent adverse reactions in both study arms were Grade 1 or 2 in<br />
severity. Grade 3 or 4 treatment-emergent adverse reactions were reported in 56% versus<br />
51% <strong>of</strong> patients on SUTENT versus placebo, respectively, in the double-blind treatment<br />
phase <strong>of</strong> the trial. Table 1 compares the incidence <strong>of</strong> common (≥10%) treatment-emergent<br />
adverse reactions for patients receiving SUTENT <strong>and</strong> reported more commonly in patients<br />
receiving SUTENT than in patients receiving placebo.<br />
Table 1. Adverse Reactions Reported in Study A in at Least 10% <strong>of</strong> GIST <strong>Patient</strong>s who<br />
Received SUTENT in the Double-Blind Treatment Phase <strong>and</strong> More Commonly Than in<br />
<strong>Patient</strong>s Given Placebo*<br />
GIST<br />
Adverse Reaction, SUTENT (n=202) Placebo (n=102)<br />
n (%) All Grades Grade 3/4 All Grades Grade 3/4<br />
Any 114 (56) 52 (51)<br />
Gastrointestinal<br />
Diarrhea 81 (40) 9 (4) 27 (27) 0 (0)<br />
Mucositis/stomatitis 58 (29) 2 (1) 18 (18) 2 (2)<br />
Constipation 41 (20) 0 (0) 14 (14) 2 (2)<br />
Cardiac<br />
Hypertension 31 (15) 9 (4) 11 (11) 0 (0)<br />
Dermatology<br />
Skin discoloration 61 (30) 0 (0) 23 (23) 0 (0)<br />
Rash 28 (14) 2 (1) 9 (9) 0 (0)<br />
H<strong>and</strong>-foot syndrome 28 (14) 9 (4) 10 (10) 3 (3)<br />
Neurology<br />
Altered taste 42 (21) 0 (0) 12 (12) 0 (0)<br />
Musculoskeletal<br />
Myalgia/limb pain 28 (14) 1 (1) 9 (9) 1 (1)<br />
Metabolism/Nutrition<br />
Anorexia a 67 (33) 1 (1) 30 (29) 5 (5)<br />
Asthenia 45 (22) 10 (5) 11 (11) 3 (3)<br />
* Common Terminology Criteria for Adverse Events (CTCAE), Version 3.0<br />
a Includes decreased appetite<br />
In the double-blind treatment phase <strong>of</strong> GIST Study A, oral pain other than<br />
mucositis/stomatitis occurred in 12 patients (6%) on SUTENT versus 3 (3%) on placebo.<br />
Hair color changes occurred in 15 patients (7%) on SUTENT versus 4 (4%) on placebo.<br />
Alopecia was observed in 10 patients (5%) on SUTENT versus 2 (2%) on placebo.<br />
Table 2 provides common (≥10%) treatment-emergent laboratory abnormalities.<br />
Table 2. Laboratory Abnormalities Reported in Study A in at Least 10% <strong>of</strong> GIST <strong>Patient</strong>s<br />
Who Received SUTENT or Placebo in the Double-Blind Treatment Phase*<br />
GIST<br />
Laboratory SUTENT (n=202) Placebo (n=102)<br />
Parameter, n (%) All Grades* Grade 3/4* a All Grades* Grade 3/4* b<br />
Any 68 (34) 22 (22)<br />
Gastrointestinal<br />
AST / ALT 78 (39) 3 (2) 23 (23) 1 (1)<br />
Lipase 50 (25) 20 (10) 17 (17) 7 (7)<br />
Alkaline phosphatase 48 (24) 7 (4) 21 (21) 4 (4)<br />
Amylase 35 (17) 10 (5) 12 (12) 3 (3)<br />
Total bilirubin 32 (16) 2 (1) 8 (8) 0 (0)<br />
Indirect bilirubin 20 (10) 0 (0) 4 (4) 0 (0)<br />
Cardiac<br />
Decreased LVEF 22 (11) 2 (1) 3 (3) 0 (0)<br />
Renal/Metabolic<br />
Creatinine 25 (12) 1 (1) 7 (7) 0 (0)<br />
Potassium decreased 24 (12) 1 (1) 4 (4) 0 (0)<br />
Sodium increased 20 (10) 0 (0) 4 (4) 1 (1)<br />
Hematology<br />
Neutrophils 107 (53) 20 (10) 4 (4) 0 (0)<br />
Lymphocytes 76 (38) 0 (0) 16 (16) 0 (0)<br />
Platelets 76 (38) 10 (5) 4 (4) 0 (0)<br />
Hemoglobin 52 (26) 6 (3) 22 (22) 2 (2)<br />
LVEF=Left ventricular ejection fraction<br />
* Common Terminology Criteria for Adverse Events (CTCAE), Version 3.0<br />
a Grade 4 laboratory abnormalities in patients on SUTENT included alkaline phosphatase<br />
(1%), lipase (2%), creatinine (1%), potassium decreased (1%), neutrophils (2%),<br />
hemoglobin (2%), <strong>and</strong> platelets (1%).<br />
b Grade 4 laboratory abnormalities in patients on placebo included amylase (1%), lipase<br />
(1%), <strong>and</strong> hemoglobin (2%).<br />
After an interim analysis, the study was unblinded, <strong>and</strong> patients on the placebo arm<br />
were given the opportunity to receive open-label SUTENT treatment [see Clinical Studies<br />
(14.1)]. For 241 patients r<strong>and</strong>omized to the SUTENT arm, including 139 who received<br />
SUTENT in both the double-blind <strong>and</strong> open-label treatment phases, the median duration
<strong>of</strong> SUTENT treatment was 6 cycles (mean 8.5, range 1 – 44). For the 255 patients who<br />
ultimately received open-label SUTENT treatment, median duration <strong>of</strong> study treatment was<br />
6 cycles (mean 7.8, range 1 – 37) from the time <strong>of</strong> the unblinding. A total <strong>of</strong> 118 patients<br />
(46%) required dosing interruptions, <strong>and</strong> a total <strong>of</strong> 72 patients (28%) required dose<br />
reductions. The incidence <strong>of</strong> treatment-emergent adverse reactions resulting in permanent<br />
discontinuation was 20%. The most common Grade 3 or 4 treatment-related adverse<br />
reactions experienced by patients receiving SUTENT in the open-label treatment phase<br />
were fatigue (10%), hypertension (8%), asthenia (5%), diarrhea (5%), h<strong>and</strong>-foot<br />
syndrome (5%), nausea (4%), abdominal pain (3%), anorexia (3%), mucositis (2%),<br />
vomiting (2%), <strong>and</strong> hypothyroidism (2%).<br />
6.2 Adverse Reactions in the Treatment-Naïve RCC Study<br />
The as-treated patient population for the treatment-naive RCC study included 735<br />
patients, 375 r<strong>and</strong>omized to SUTENT <strong>and</strong> 360 r<strong>and</strong>omized to IFN-a. The median duration<br />
<strong>of</strong> treatment was 11.1 months (range: 0.4 – 46.1) for SUTENT treatment <strong>and</strong> 4.1 months<br />
(range: 0.1 – 45.6) for IFN-a treatment. Dose interruptions occurred in 202 patients (54%)<br />
on SUTENT <strong>and</strong> 141 patients (39%) on IFN-a. Dose reductions occurred in 194 patients<br />
(52%) on SUTENT <strong>and</strong> 98 patients (27%) on IFN-a. Discontinuation rates due to adverse<br />
reactions were 20% for SUTENT <strong>and</strong> 24% for IFN-a. Most treatment-emergent adverse<br />
reactions in both study arms were Grade 1 or 2 in severity. Grade 3 or 4 treatmentemergent<br />
adverse reactions were reported in 77% versus 55% <strong>of</strong> patients on SUTENT<br />
versus IFN-a, respectively.<br />
Table 3 compares the incidence <strong>of</strong> common (≥10%) treatment-emergent adverse<br />
reactions for patients receiving SUTENT versus IFN-a.<br />
Table 3. Adverse Reactions Reported in at Least 10% <strong>of</strong> <strong>Patient</strong>s with RCC Who<br />
Received SUTENT or IFN-a*<br />
Treatment-Naïve RCC<br />
Adverse Reaction, SUTENT (n=375) IFN-a (n=360)<br />
n (%) All Grades Grade 3/4 a All Grades Grade 3/4 b<br />
Any 372 (99) 290 (77) 355 (99) 197 (55)<br />
Constitutional<br />
Fatigue 233 (62) 55 (15) 202 (56) 54 (15)<br />
Asthenia 96 (26) 42 (11) 81 (22) 21 (6)<br />
Fever 84 (22) 3 (1) 134 (37) 1 (
Table 5. Adverse Reactions Reported in the Phase 3 pNET Study in at Least 10% <strong>of</strong><br />
<strong>Patient</strong>s who Received SUTENT <strong>and</strong> More Commonly Than in <strong>Patient</strong>s Given Placebo*<br />
pNET<br />
Adverse Reaction, SUTENT (n=83) Placebo (n=82)<br />
n (%) All Grades Grade 3/4 a All Grades Grade 3/4<br />
Any 82 (99) 45 (54) 78 (95) 41 (50)<br />
Constitutional<br />
Asthenia 28 (34) 4 (5) 22 (27) 3 (4)<br />
Fatigue 27 (33) 4 (5) 22 (27) 7 (9)<br />
Weight decreased 13 (16) 1(1) 9 (11) 0 (0)<br />
Gastrointestinal<br />
Diarrhea 49 (59) 4 (5) 32 (39) 2 (2)<br />
Stomatitis/oral 40 (48) 5 (6) 15 (18) 0 (0)<br />
Syndromes b<br />
Nausea 37 (45) 1 (1) 24 (29) 1 (1)<br />
Abdominal pain c 32 (39) 4 (5) 28 (34) 8 (10)<br />
Vomiting 28 (34) 0 (0) 25 (31) 2 (2)<br />
Dyspepsia 12 (15) 0 (0) 5 (6) 0 (0)<br />
Cardiac<br />
Hypertension 22 (27) 8 (10) 4 (5) 1 (1)<br />
Dermatology<br />
Hair color changes 24 (29) 1 (1) 1 (1) 0 (0)<br />
H<strong>and</strong>-foot syndrome 19 (23) 5 (6) 2 (2) 0 (0)<br />
Rash 15 (18) 0 (0) 4 (5) 0 (0)<br />
Dry skin 12 (15) 0 (0) 9 (11) 0 (0)<br />
Neurology<br />
Dysgeusia 17 (21) 0 (0) 4 (5) 0 (0)<br />
Headache 15 (18) 0 (0) 11 (13) 1 (1)<br />
Musculoskeletal<br />
Arthralgia 12 (15) 0 (0) 5 (6) 0 (0)<br />
Psychiatric<br />
Insomnia 15 (18) 0 (0) 10 (12) 0 (0)<br />
Hemorrhage/Bleeding<br />
Bleeding events d 18 (22) 0 (0) 8 (10) 3 (4)<br />
Epistaxis 17 (21) 1 (1) 4 (5) 0 (0)<br />
*Common Terminology Criteria for Adverse Events (CTCAE), Version 3.0<br />
a Grade 4 ARs in patients on SUTENT included fatigue (1%).<br />
b Includes aphthous stomatitis, gingival pain, gingivitis, glossitis, glossodynia, mouth<br />
ulceration, oral discomfort, oral pain, tongue ulceration, mucosal dryness, mucosal<br />
inflammation, <strong>and</strong> dry mouth.<br />
c Includes abdominal discomfort, abdominal pain, <strong>and</strong> abdominal pain upper.<br />
d Includes hematemesis, hematochezia, hematoma, hemoptysis, hemorrhage, melena, <strong>and</strong><br />
metrorrhagia.<br />
Table 6 provides common (≥10%) treatment-emergent laboratory abnormalities.<br />
Table 6. Laboratory Abnormalities Reported in the Phase 3 pNET Study in at Least 10%<br />
<strong>of</strong> <strong>Patient</strong>s Who Received SUTENT<br />
pNET<br />
Laboratory SUTENT Placebo<br />
Parameter, n (%) N All Grades* Grade 3/4* a N All Grades* Grade 3/4* b<br />
Gastrointestinal<br />
AST increased 82 59 (72) 4 (5) 80 56 (70) 2 (3)<br />
ALT increased 82 50 (61) 3 (4) 80 44 (55) 2 (3)<br />
Alkaline phosphatase 82 52 (63) 8 (10) 80 56 (70) 9 (11)<br />
increased<br />
Total bilirubin increased 82 30 (37) 1 (1) 80 22 (28) 3 (4)<br />
Amylase increased 74 15 (20) 3 (4) 74 7 (10) 1 (1)<br />
Lipase increased 75 13 (17) 4 (5) 72 8 (11) 3 (4)<br />
Renal/Metabolic<br />
Glucose increased 82 58 (71) 10 (12) 80 62 (78) 14 (18)<br />
Albumin decreased 81 33 (41) 1 (1) 79 29 (37) 1 (1)<br />
Phosphorus decreased 81 29 (36) 6 (7) 77 17 (22) 4 (5)<br />
Calcium decreased 82 28 (34) 0 (0) 80 15 (19) 0 (0)<br />
Sodium decreased 82 24 (29) 2 (2) 80 27 (34) 2 (3)<br />
Creatinine increased 82 22 (27) 4 (5) 80 22 (28) 4 (5)<br />
Glucose decreased 82 18 (22) 2 (2) 80 12 (15) 3 (4)<br />
Potassium decreased 82 17 (21) 3 (4) 80 11 (14) 0 (0)<br />
Magnesium decreased 52 10 (19) 0 (0) 39 4 (10) 0 (0)<br />
Potassium increased 82 15 (18) 1 (1) 80 9 (11) 1 (1)<br />
Hematology<br />
Neutrophils decreased 82 58 (71) 13 (16) 80 13 (16) 0 (0)<br />
Hemoglobin decreased 82 53 (65) 0 (0) 80 44 (55) 1 (1)<br />
Platelets decreased 82 49 (60) 4 (5) 80 12 (15) 0 (0)<br />
Lymphocytes decreased 82 46 (56) 6 (7) 80 28 (35) 3 (4)<br />
*Common Terminology Criteria for Adverse Events (CTCAE), Version 3.0<br />
a Grade 4 laboratory abnormalities in patients on SUTENT included creatinine (4%), lipase<br />
(4%), glucose decreased (2%), glucose increased (2%), neutrophils (2%), ALT (1%), AST<br />
(1%), platelets (1%), potassium increased (1%) <strong>and</strong> total bilirubin (1%).<br />
b Grade 4 laboratory abnormalities in patients on placebo included creatinine (3%), alkaline<br />
phosphatase (1%), glucose increased (1%) <strong>and</strong> lipase (1%).<br />
6.4 Venous Thromboembolic Events<br />
Seven patients (3%) on SUTENT <strong>and</strong> none on placebo in the double-blind treatment<br />
phase <strong>of</strong> GIST Study A experienced venous thromboembolic events; five <strong>of</strong> the seven were<br />
Grade 3 deep venous thrombosis (DVT), <strong>and</strong> two were Grade 1 or 2. Four <strong>of</strong> these seven<br />
GIST patients discontinued treatment following first observation <strong>of</strong> DVT.<br />
Thirteen (3%) patients receiving SUTENT for treatment-naïve RCC had venous<br />
thrombo embolic events reported. Seven (2%) <strong>of</strong> these patients had pulmonary embolism,<br />
one was Grade 2 <strong>and</strong> six were Grade 4, <strong>and</strong> six (2%) patients had DVT, including three<br />
Grade 3. One patient was permanently withdrawn from SUTENT due to pulmonary<br />
embolism; dose interruption occurred in two patients with pulmonary embolism <strong>and</strong><br />
one with DVT. In treatment-naïve RCC patients receiving IFN-a, six (2%) venous<br />
thromboembolic events occurred; one patient (
7.2 CYP3A4 Inducers<br />
CYP3A4 inducers such as rifampin may decrease sunitinib plasma concentrations.<br />
Selection <strong>of</strong> an alternate concomitant medication with no or minimal enzyme induction<br />
potential is recommended. Concurrent administration <strong>of</strong> SUTENT with the strong CYP3A4<br />
inducer, rifampin, resulted in a 23% <strong>and</strong> 46% reduction in the combined (sunitinib +<br />
primary active metabolite) C max <strong>and</strong> AUC 0-∞ values, respectively, after a single dose <strong>of</strong><br />
SUTENT in healthy volunteers. Co-administration <strong>of</strong> SUTENT with inducers <strong>of</strong> the CYP3A4<br />
family (e.g., dexamethasone, phenytoin, carbamazepine, rifampin, rifabutin, rifapentin,<br />
phenobarbital, St. John’s Wort) may decrease sunitinib concentrations. St. John’s Wort<br />
may decrease sunitinib plasma concentrations unpredictably. <strong>Patient</strong>s receiving SUTENT<br />
should not take St. John’s Wort concomitantly. A dose increase for SUTENT should be<br />
considered when it must be co-administered with CYP3A4 inducers [see Dosage <strong>and</strong><br />
Administration (2.2)].<br />
7.3 In Vitro Studies <strong>of</strong> CYP Inhibition <strong>and</strong> Induction<br />
In vitro studies indicated that sunitinib does not induce or inhibit major CYP enzymes.<br />
The in vitro studies in human liver microsomes <strong>and</strong> hepatocytes <strong>of</strong> the activity <strong>of</strong> CYP<br />
is<strong>of</strong>orms CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1,<br />
CYP3A4/5, <strong>and</strong> CYP4A9/11 indicated that sunitinib <strong>and</strong> its primary active metabolite are<br />
unlikely to have any clinically relevant drug-drug interactions with drugs that may be<br />
metabolized by these enzymes.<br />
8 USE IN SPECIFIC POPULATIONS<br />
8.1 Pregnancy<br />
Pregnancy Category D [see Warnings <strong>and</strong> Precautions (5.2)].<br />
SUTENT can cause fetal harm when administered to a pregnant woman. As<br />
angiogenesis is a critical component <strong>of</strong> embryonic <strong>and</strong> fetal development, inhibition <strong>of</strong><br />
angiogenesis following administration <strong>of</strong> SUTENT should be expected to result in adverse<br />
effects on pregnancy. In animal reproductive studies in rats <strong>and</strong> rabbits, sunitinib was<br />
teratogenic, embryotoxic, <strong>and</strong> fetotoxic. There are no adequate <strong>and</strong> well-controlled<br />
studies <strong>of</strong> SUTENT in pregnant women. If this drug is used during pregnancy, or if the<br />
patient becomes pregnant while taking this drug, the patient should be apprised <strong>of</strong> the<br />
potential hazard to a fetus. Women <strong>of</strong> childbearing potential should be advised to avoid<br />
becoming pregnant while receiving treatment with SUTENT.<br />
Sunitinib was evaluated in pregnant rats (0.3, 1.5, 3.0, 5.0 mg/kg/day) <strong>and</strong> rabbits<br />
(0.5, 1, 5, 20 mg/kg/day) for effects on the embryo. Significant increases in the incidence <strong>of</strong><br />
embryolethality <strong>and</strong> structural abnormalities were observed in rats at the dose <strong>of</strong><br />
5 mg/kg/day (approximately 5.5 times the systemic exposure [combined AUC <strong>of</strong> sunitinib +<br />
primary active metabolite] in patients administered the recommended daily doses [RDD]).<br />
Significantly increased embryolethality was observed in rabbits at 5 mg/kg/day while developmental<br />
effects were observed at ≥1 mg/kg/day (approximately 0.3 times the AUC in patients<br />
administered the RDD <strong>of</strong> 50 mg/day). Developmental effects consisted <strong>of</strong> fetal skeletal malformations<br />
<strong>of</strong> the ribs <strong>and</strong> vertebrae in rats. In rabbits, cleft lip was observed at 1 mg/kg/day <strong>and</strong><br />
cleft lip <strong>and</strong> cleft palate were observed at 5 mg/kg/day (approximately 2.7 times the AUC in<br />
patients administered the RDD). Neither fetal loss nor malformations were observed in rats<br />
dosed at ≤3 mg/kg/day (approximately 2.3 times the AUC in patients administered the RDD).<br />
Sunitinib (0.3, 1.0, 3.0 mg/kg/day) was evaluated in a pre- <strong>and</strong> postnatal development<br />
study in pregnant rats. Maternal body weight gains were reduced during gestation <strong>and</strong> lactation<br />
at doses ≥1 mg/kg/day but no maternal reproductive toxicity was observed at doses<br />
up to 3 mg/kg/day (approximately 2.3 times the AUC in patients administered the RDD). At<br />
the high dose <strong>of</strong> 3 mg/kg/day, reduced body weights were observed at birth <strong>and</strong> persisted<br />
for <strong>of</strong>fspring <strong>of</strong> both sexes during the pre-weaning period <strong>and</strong> in males during post-weaning<br />
period. No other developmental toxicity was observed at doses up to 3 mg/kg/day<br />
(approximately 2.3 times the AUC in patients administered the RDD).<br />
8.3 Nursing Mothers<br />
Sunitinib <strong>and</strong> its metabolites are excreted in rat milk. In lactating female rats<br />
administered 15 mg/kg, sunitinib <strong>and</strong> its metabolites were extensively excreted in milk at<br />
concentrations up to 12-fold higher than in plasma. It is not known whether this drug or<br />
its primary active metabolite are excreted in human milk. Because many drugs are excreted<br />
in human milk <strong>and</strong> because <strong>of</strong> the potential for serious adverse reactions in nursing<br />
infants from SUTENT, a decision should be made whether to discontinue nursing or to<br />
discontinue the drug taking into account the importance <strong>of</strong> the drug to the mother.<br />
8.4 Pediatric Use<br />
The safety <strong>and</strong> efficacy <strong>of</strong> SUTENT in pediatric patients have not been established.<br />
Physeal dysplasia was observed in cynomolgus monkeys with open growth plates<br />
treated for ≥ 3 months (3 month dosing 2, 6, 12 mg/kg/day; 8 cycles <strong>of</strong> dosing 0.3, 1.5,<br />
6.0 mg/kg/day) with sunitinib at doses that were > 0.4 times the RDD based on systemic<br />
exposure (AUC). In developing rats treated continuously for 3 months (1.5, 5.0 <strong>and</strong><br />
15.0 mg/kg) or 5 cycles (0.3, 1.5, <strong>and</strong> 6.0 mg/kg/day), bone abnormalities consisted <strong>of</strong><br />
thickening <strong>of</strong> the epiphyseal cartilage <strong>of</strong> the femur <strong>and</strong> an increase <strong>of</strong> fracture <strong>of</strong> the tibia<br />
at doses ≥ 5 mg/kg (approximately 10 times the RDD based on AUC). Additionally, caries<br />
<strong>of</strong> the teeth were observed in rats at >5 mg/kg. The incidence <strong>and</strong> severity <strong>of</strong> physeal<br />
dysplasia were dose-related <strong>and</strong> were reversible upon cessation <strong>of</strong> treatment; however,<br />
findings in the teeth were not. A no effect level was not observed in monkeys treated<br />
continuously for 3 months, but was 1.5 mg/kg/day when treated intermittently for 8 cycles.<br />
In rats the no effect level in bones was ≤ 2 mg/kg/day.<br />
8.5 Geriatric Use<br />
Of 825 GIST <strong>and</strong> RCC patients who received SUTENT on clinical studies, 277 (34%)<br />
were 65 <strong>and</strong> over. In the Phase 3 pNET study, 22 (27%) patients who received SUTENT<br />
were 65 <strong>and</strong> over. No overall differences in safety or effectiveness were observed between<br />
younger <strong>and</strong> older patients.<br />
8.6 Hepatic Impairment<br />
No dose adjustment to the starting dose is required when administering SUTENT to<br />
patients with Child-Pugh Class A or B hepatic impairment. Sunitinib <strong>and</strong> its primary<br />
metabolite are primarily metabolized by the liver. Systemic exposures after a single dose<br />
<strong>of</strong> SUTENT were similar in subjects with mild or moderate (Child-Pugh Class A <strong>and</strong> B)<br />
hepatic impairment compared to subjects with normal hepatic function. SUTENT was not<br />
studied in subjects with severe (Child-Pugh Class C) hepatic impairment. Studies in<br />
cancer patients have excluded patients with ALT or AST >2.5 x ULN or, if due to liver<br />
metastases, >5.0 x ULN.<br />
8.7 Renal Impairment<br />
No adjustment to the starting dose is required when administering SUTENT to patients<br />
with mild, moderate, <strong>and</strong> severe renal impairment. Subsequent dose modifications should<br />
be based on safety <strong>and</strong> tolerability [see Dose Modification (2.3)]. In patients with<br />
end-stage renal disease (ESRD) on hemodialysis, no adjustment to the starting dose is<br />
required. However, compared to subjects with normal renal function, the sunitinib exposure<br />
is 47% lower in subjects with ESRD on hemodialysis. Therefore, the subsequent<br />
doses may be increased gradually up to 2 fold based on safety <strong>and</strong> tolerability.<br />
10 OVERDOSAGE<br />
Treatment <strong>of</strong> overdose with SUTENT should consist <strong>of</strong> general supportive measures.<br />
There is no specific antidote for overdosage with SUTENT. If indicated, elimination<br />
<strong>of</strong> unabsorbed drug should be achieved by emesis or gastric lavage. A few cases <strong>of</strong><br />
accidental overdose have been reported; these cases were associated with adverse<br />
reactions consistent with the known safety pr<strong>of</strong>ile <strong>of</strong> SUTENT, or without adverse reactions.<br />
A case <strong>of</strong> intentional overdose involving the ingestion <strong>of</strong> 1,500 mg <strong>of</strong> SUTENT in an<br />
attempted suicide was reported without adverse reaction. In non-clinical studies mortality<br />
was observed following as few as 5 daily doses <strong>of</strong> 500 mg/kg (3000 mg/m 2 ) in rats. At this<br />
dose, signs <strong>of</strong> toxicity included impaired muscle coordination, head shakes, hypoactivity,<br />
ocular discharge, piloerection <strong>and</strong> gastrointestinal distress. Mortality <strong>and</strong> similar signs <strong>of</strong><br />
toxicity were observed at lower doses when administered for longer durations.<br />
11 DESCRIPTION<br />
SUTENT, an oral multi-kinase inhibitor, is the malate salt <strong>of</strong> sunitinib. Sunitinib<br />
malate is described chemically as Butanedioic acid, hydroxy-, (2S)-, compound with<br />
N-[2-(diethylamino)ethyl]-5-[(Z)-(5-fluoro-1,2-dihydro-2-oxo-3H-indol-3-ylidine)methyl]-<br />
2,4-dimethyl-1H-pyrrole-3-carboxamide (1:1). The molecular formula is C 22 H 27 FN 4 O 2 •<br />
C 4 H 6 O 5 <strong>and</strong> the molecular weight is 532.6 Daltons.<br />
The chemical structure <strong>of</strong> sunitinib malate is:<br />
Sunitinib malate is a yellow to orange powder with a pKa <strong>of</strong> 8.95. The solubility<br />
<strong>of</strong> sunitinib malate in aqueous media over the range pH 1.2 to pH 6.8 is in excess <strong>of</strong><br />
25 mg/mL. The log <strong>of</strong> the distribution coefficient (octanol/water) at pH 7 is 5.2.<br />
SUTENT (sunitinib malate) capsules are supplied as printed hard shell capsules<br />
containing sunitinib malate equivalent to 12.5 mg, 25 mg or 50 mg <strong>of</strong> sunitinib together<br />
with mannitol, croscarmellose sodium, povidone (K-25) <strong>and</strong> magnesium stearate as<br />
inactive ingredients.<br />
The orange gelatin capsule shells contain titanium dioxide, <strong>and</strong> red iron oxide. The<br />
caramel gelatin capsule shells contain titanium dioxide, red iron oxide, yellow iron oxide<br />
<strong>and</strong> black iron oxide. The white printing ink contains shellac, propylene glycol, sodium<br />
hydroxide, povidone <strong>and</strong> titanium dioxide.<br />
12 CLINICAL PHARMACOLOGY<br />
12.1 Mechanism <strong>of</strong> Action<br />
Sunitinib is a small molecule that inhibits multiple receptor tyrosine kinases (RTKs),<br />
some <strong>of</strong> which are implicated in tumor growth, pathologic angiogenesis, <strong>and</strong> metastatic<br />
progression <strong>of</strong> cancer. Sunitinib was evaluated for its inhibitory activity against a variety <strong>of</strong><br />
kinases (>80 kinases) <strong>and</strong> was identified as an inhibitor <strong>of</strong> platelet-derived growth factor<br />
receptors (PDGFRa <strong>and</strong> PDGFRb), vascular endothelial growth factor receptors (VEGFR1,<br />
VEGFR2 <strong>and</strong> VEGFR3), stem cell factor receptor (KIT), Fms-like tyrosine kinase-3 (FLT3),<br />
colony stimulating factor receptor Type 1 (CSF-1R), <strong>and</strong> the glial cell-line derived neurotrophic<br />
factor receptor (RET). Sunitinib inhibition <strong>of</strong> the activity <strong>of</strong> these RTKs has been<br />
demonstrated in biochemical <strong>and</strong> cellular assays, <strong>and</strong> inhibition <strong>of</strong> function has been<br />
demonstrated in cell proliferation assays. The primary metabolite exhibits similar potency<br />
compared to sunitinib in biochemical <strong>and</strong> cellular assays.<br />
Sunitinib inhibited the phosphorylation <strong>of</strong> multiple RTKs (PDGFRb, VEGFR2, KIT) in<br />
tumor xenografts expressing RTK targets in vivo <strong>and</strong> demonstrated inhibition <strong>of</strong> tumor<br />
growth or tumor regression <strong>and</strong>/or inhibited metastases in some experimental models<br />
<strong>of</strong> cancer. Sunitinib demonstrated the ability to inhibit growth <strong>of</strong> tumor cells expressing<br />
dysregulated target RTKs (PDGFR, RET, or KIT) in vitro <strong>and</strong> to inhibit PDGFRb- <strong>and</strong><br />
VEGFR2-dependent tumor angiogenesis in vivo.<br />
12.3 Pharmacokinetics<br />
The pharmacokinetics <strong>of</strong> sunitinib <strong>and</strong> sunitinib malate have been evaluated in 135<br />
healthy volunteers <strong>and</strong> in 266 patients with solid tumors.<br />
Maximum plasma concentrations (C max ) <strong>of</strong> sunitinib are generally observed between 6<br />
<strong>and</strong> 12 hours (T max ) following oral administration. Food has no effect on the bioavailability<br />
<strong>of</strong> sunitinib. SUTENT may be taken with or without food.<br />
Binding <strong>of</strong> sunitinib <strong>and</strong> its primary active metabolite to human plasma protein<br />
in vitro was 95% <strong>and</strong> 90%, respectively, with no concentration dependence in the range <strong>of</strong><br />
100 – 4000 ng/mL. The apparent volume <strong>of</strong> distribution (Vd/F) for sunitinib was 2230 L.<br />
In the dosing range <strong>of</strong> 25 - 100 mg, the area under the plasma concentration-time curve<br />
(AUC) <strong>and</strong> C max increase proportionately with dose.<br />
Sunitinib is metabolized primarily by the cytochrome P450 enzyme, CYP3A4,<br />
to produce its primary active metabolite, which is further metabolized by CYP3A4. The<br />
primary active metabolite comprises 23 to 37% <strong>of</strong> the total exposure. Elimination is<br />
primarily via feces. In a human mass balance study <strong>of</strong> [ 14 C]sunitinib, 61% <strong>of</strong> the dose was
eliminated in feces, with renal elimination accounting for 16% <strong>of</strong> the administered dose.<br />
Sunitinib <strong>and</strong> its primary active metabolite were the major drug-related compounds<br />
identified in plasma, urine, <strong>and</strong> feces, representing 91.5%, 86.4% <strong>and</strong> 73.8% <strong>of</strong> radio -<br />
activity in pooled samples, respectively. Minor metabolites were identified in urine <strong>and</strong><br />
feces but generally not found in plasma. Total oral clearance (CL/F) ranged from 34 to<br />
62 L/hr with an inter-patient variability <strong>of</strong> 40%.<br />
Following administration <strong>of</strong> a single oral dose in healthy volunteers, the terminal<br />
half-lives <strong>of</strong> sunitinib <strong>and</strong> its primary active metabolite are approximately 40 to 60 hours<br />
<strong>and</strong> 80 to 110 hours, respectively. With repeated daily administration, sunitinib accumulates<br />
3- to 4-fold while the primary metabolite accumulates 7- to 10-fold. Steady-state<br />
concentrations <strong>of</strong> sunitinib <strong>and</strong> its primary active metabolite are achieved within 10 to 14<br />
days. By Day 14, combined plasma concentrations <strong>of</strong> sunitinib <strong>and</strong> its active metabolite<br />
ranged from 62.9 – 101 ng/mL. No significant changes in the pharmacokinetics <strong>of</strong> sunitinib<br />
or the primary active metabolite were observed with repeated daily administration<br />
or with repeated cycles in the dosing regimens tested.<br />
The pharmacokinetics were similar in healthy volunteers <strong>and</strong> in the solid tumor patient<br />
populations tested, including patients with GIST <strong>and</strong> RCC.<br />
Pharmacokinetics in Special Populations<br />
Population pharmacokinetic analyses <strong>of</strong> demographic data indicate that there are no<br />
clinically relevant effects <strong>of</strong> age, body weight, creatinine clearance, race, gender, or ECOG<br />
score on the pharmacokinetics <strong>of</strong> SUTENT or the primary active metabolite.<br />
Pediatric Use: The pharmacokinetics <strong>of</strong> SUTENT have not been evaluated in pediatric<br />
patients.<br />
Renal Insufficiency: Sunitinib systemic exposure after a single dose <strong>of</strong> SUTENT was<br />
similar in subjects with severe renal impairment (CL cr 80 mL/min). Although sunitinib was not eliminated<br />
through hemodialysis, the sunitinib systemic exposure was 47% lower in subjects with<br />
ESRD on hemodialysis compared to subjects with normal renal function.<br />
Hepatic Insufficiency: Systemic exposures after a single dose <strong>of</strong> SUTENT were similar<br />
in subjects with mild exocrine (Child-Pugh Class A) or moderate (Child-Pugh Class B)<br />
hepatic impairment compared to subjects with normal hepatic function.<br />
12.4 Cardiac Electrophysiology<br />
See Warnings <strong>and</strong> Precautions (5.4).<br />
13 NONCLINICAL TOXICOLOGY<br />
13.1 Carcinogenesis, Mutagenesis, Impairment <strong>of</strong> Fertility<br />
The carcinogenic potential <strong>of</strong> sunitinib has been evaluated in two species: rasH2 transgenic<br />
mice <strong>and</strong> Sprague-Dawley rats. There were similar positive findings in both species.<br />
In rasH2 transgenic mice gastroduodenal carcinomas <strong>and</strong>/or gastric mucosal hyperplasia,<br />
as well as an increased incidence <strong>of</strong> background hemangiosarcomas were observed at<br />
doses <strong>of</strong> ≥25 mg/kg/day following daily dose administration <strong>of</strong> sunitinib in studies <strong>of</strong> 1 or<br />
6 months duration. No proliferative changes were observed in rasH2 transgenic mice at<br />
8 mg/kg/day. Similarly, in a 2-year rat carcinogenicity study, administration <strong>of</strong> sunitinib in<br />
28-day cycles followed by 7-day dose-free periods resulted in findings <strong>of</strong> duodenal<br />
carcinoma at doses as low as 1 mg/kg/day (approximately 0.9 times the AUC in patients<br />
given the RDD <strong>of</strong> 50 mg/day). At the high dose <strong>of</strong> 3 mg/kg/day (approximately 7.8 times<br />
the AUC in patients at the RDD <strong>of</strong> 50 mg/day) the incidence <strong>of</strong> duodenal tumors was<br />
increased <strong>and</strong> was accompanied by findings <strong>of</strong> gastric mucous cell hyperplasia <strong>and</strong> by an<br />
increased incidence <strong>of</strong> pheochromocytoma <strong>and</strong> hyperplasia <strong>of</strong> the adrenal. Sunitinib did<br />
not cause genetic damage when tested in in vitro assays (bacterial mutation [AMES<br />
Assay], human lymphocyte chromosome aberration) <strong>and</strong> an in vivo rat bone marrow<br />
micronucleus test.<br />
Effects on the female reproductive system were identified in a 3-month repeat dose<br />
monkey study (2, 6, 12 mg/kg/day), where ovarian changes (decreased follicular development)<br />
were noted at 12 mg/kg/day (≥5.1 times the AUC in patients administered the RDD),<br />
while uterine changes (endometrial atrophy) were noted at ≥2 mg/kg/day (≥0.4 times the<br />
AUC in patients administered the RDD). With the addition <strong>of</strong> vaginal atrophy, the uterine <strong>and</strong><br />
ovarian effects were reproduced at 6 mg/kg/day in the 9-month monkey study (0.3, 1.5 <strong>and</strong><br />
6 mg/kg/day administered daily for 28 days followed by a 14 day respite; the 6 mg/kg dose<br />
produced a mean AUC that was ≥0.8 times the AUC in patients administered the RDD).<br />
A no effect level was not identified in the 3 month study; 1.5 mg/kg/day represents a no<br />
effect level in monkeys administered sunitinib for 9 months.<br />
Although fertility was not affected in rats, SUTENT may impair fertility in humans. In<br />
female rats, no fertility effects were observed at doses <strong>of</strong> ≤5.0 mg/kg/day [(0.5, 1.5,<br />
5.0 mg/kg/day) administered for 21 days up to gestational day 7; the 5.0 mg/kg dose<br />
produced an AUC that was ≥5 times the AUC in patients administered the RDD], however<br />
significant embryolethality was observed at the 5.0 mg/kg dose. No reproductive effects<br />
were observed in male rats dosed (1, 3 or 10 mg/kg/day) for 58 days prior to mating with<br />
untreated females. Fertility, copulation, conception indices, <strong>and</strong> sperm evaluation<br />
(morphology, concentration, <strong>and</strong> motility) were unaffected by sunitinib at doses<br />
≤10 mg/kg/day (the 10 mg/kg/day dose produced a mean AUC that was ≥25.8 times the<br />
AUC in patients administered the RDD).<br />
14 CLINICAL STUDIES<br />
14.1 Gastrointestinal Stromal Tumor<br />
GIST Study A<br />
Study A was a two-arm, international, r<strong>and</strong>omized, double-blind, placebo-controlled<br />
trial <strong>of</strong> SUTENT in patients with GIST who had disease progression during prior imatinib<br />
mesylate (imatinib) treatment or who were intolerant <strong>of</strong> imatinib. The objective was to<br />
compare Time-to-Tumor Progression (TTP) in patients receiving SUTENT plus best<br />
supportive care versus patients receiving placebo plus best supportive care. Other<br />
objectives included Progression-Free Survival (PFS), Objective Response Rate (ORR), <strong>and</strong><br />
Overall Survival (OS). <strong>Patient</strong>s were r<strong>and</strong>omized (2:1) to receive either 50 mg SUTENT or<br />
placebo orally, once daily, on Schedule 4/2 until disease progression or withdrawal from<br />
the study for another reason. Treatment was unblinded at the time <strong>of</strong> disease progression.<br />
<strong>Patient</strong>s r<strong>and</strong>omized to placebo were then <strong>of</strong>fered crossover to open-label SUTENT, <strong>and</strong><br />
patients r<strong>and</strong>omized to SUTENT were permitted to continue treatment per investigator<br />
judgment.<br />
At the time <strong>of</strong> a pre-specified interim analysis, the intent-to-treat (ITT) population<br />
included 312 patients. Two-hundred seven (207) patients were r<strong>and</strong>omized to the SUTENT<br />
arm, <strong>and</strong> 105 patients were r<strong>and</strong>omized to the placebo arm. Demographics were<br />
comparable between the SUTENT <strong>and</strong> placebo groups with regard to age (69% vs 72%<br />
There was a statistically significant advantage for SUTENT over IFN-a in the endpoint <strong>of</strong><br />
PFS (see Table 8 <strong>and</strong> Figure 2). In the pre-specified stratification factors <strong>of</strong> LDH (>1.5 ULN<br />
vs. ≤1.5 ULN), ECOG performance status (0 vs. 1), <strong>and</strong> prior nephrectomy (yes vs. no),<br />
the hazard ratio favored SUTENT over IFN-a. The ORR was higher in the SUTENT arm (see<br />
Table 8).<br />
Table 8. Treatment-Naïve RCC Efficacy Results (interim analysis)<br />
Efficacy Parameter<br />
SUTENT IFN-a P-value HR<br />
(n=375) (n=375) (log-rank test) (95% CI)<br />
Progression-Free 47.3 22.0
17 PATIENT COUNSELING INFORMATION<br />
See 17.6 for FDA-Approved <strong>Patient</strong> Labeling.<br />
17.1 Gastrointestinal Disorders<br />
Gastrointestinal disorders such as diarrhea, nausea, stomatitis, dyspepsia, <strong>and</strong> vomiting<br />
were the most commonly reported gastrointestinal events occurring in patients who<br />
received SUTENT. Supportive care for gastrointestinal adverse events requiring treatment<br />
may include anti-emetic or anti-diarrheal medication.<br />
17.2 Skin Effects<br />
Skin discoloration possibly due to the drug color (yellow) occurred in approximately<br />
one third <strong>of</strong> patients. <strong>Patient</strong>s should be advised that depigmentation <strong>of</strong> the hair or skin<br />
may occur during treatment with SUTENT. Other possible dermatologic effects may<br />
include dryness, thickness or cracking <strong>of</strong> skin, blister or rash on the palms <strong>of</strong> the h<strong>and</strong>s<br />
<strong>and</strong> soles <strong>of</strong> the feet.<br />
17.3 Other Common Events<br />
Other commonly reported adverse events included fatigue, high blood pressure,<br />
bleeding, swelling, mouth pain/irritation <strong>and</strong> taste disturbance.<br />
17.4 Musculoskeletal Disorders<br />
Prior to treatment with SUTENT, a dental examination <strong>and</strong> appropriate preventive dentistry<br />
should be considered. In patients being treated with SUTENT, who have previously<br />
received or are receiving bisphosphonates, invasive dental procedures should be avoided,<br />
if possible.<br />
17.5 Concomitant Medications<br />
<strong>Patient</strong>s should be advised to inform their health care providers <strong>of</strong> all concomitant<br />
medications, including over-the-counter medications <strong>and</strong> dietary supplements [see Drug<br />
Interactions (7)].<br />
17.6 FDA-Approved <strong>Patient</strong> Labeling<br />
LAB-0317-17.0<br />
Distributed by<br />
Pfizer Labs<br />
Division <strong>of</strong> Pfizer Inc, NY, NY 10017<br />
MEDICATION GUIDE<br />
SUTENT (su TENT)<br />
(sunitinib malate)<br />
capsules<br />
Read the Medication <strong>Guide</strong> that comes with SUTENT before you start taking<br />
it <strong>and</strong> each time you get a refill. There may be new information. This<br />
Medication <strong>Guide</strong> does not take the place <strong>of</strong> talking to your healthcare<br />
provider about your medical condition or treatment. If you have any<br />
questions about SUTENT, ask your healthcare provider or pharmacist.<br />
What is the most important information I should know about SUTENT<br />
SUTENT can cause serious liver problems, including death.<br />
• Tell your healthcare provider right away if you develop any <strong>of</strong> the<br />
following signs <strong>and</strong> symptoms <strong>of</strong> liver problems during treatment<br />
with SUTENT:<br />
• itching<br />
• yellow eyes or skin,<br />
• dark urine, <strong>and</strong><br />
• pain or discomfort in the right upper stomach area.<br />
• Your healthcare provider should do blood tests to check your liver<br />
function before you start taking SUTENT <strong>and</strong> during treatment.<br />
What is SUTENT<br />
SUTENT is a prescription medicine used to treat people with:<br />
• a rare cancer <strong>of</strong> the stomach, bowel, or esophagus called GIST<br />
(gastrointestinal stromal tumor) <strong>and</strong> when:<br />
• the medicine Gleevec ® (imatinib mesylate) did not stop the<br />
cancer from growing, or<br />
• you cannot take Gleevec ® .<br />
• advanced kidney cancer (advanced renal cell carcinoma or RCC)<br />
• a type <strong>of</strong> pancreatic cancer known as pancreatic neuroendocrine<br />
tumors (pNET), that has progressed <strong>and</strong> cannot be treated with<br />
surgery.<br />
It is not known if SUTENT is safe <strong>and</strong> effective in children.<br />
What should I tell my healthcare provider before taking SUTENT<br />
Before taking SUTENT tell your healthcare provider if you:<br />
• have any heart problems<br />
• have high blood pressure<br />
• have thyroid problems<br />
• have kidney function problems (other than cancer)<br />
• have liver problems<br />
• have any bleeding problem<br />
• have seizures<br />
• have or have had pain in the mouth, teeth or jaw, swelling or sores inside<br />
the mouth, numbness or a feeling <strong>of</strong> heaviness in the jaw, or loosening <strong>of</strong><br />
a tooth<br />
• have any other medical conditions<br />
• are pregnant, could be pregnant or plan to become pregnant. SUTENT may<br />
harm an unborn baby. You should not become pregnant while taking<br />
SUTENT. Tell your healthcare provider right away if you become pregnant<br />
while taking SUTENT.<br />
• are breastfeeding or plan to breastfeed. You <strong>and</strong> your healthcare provider<br />
should decide if you will take SUTENT or breastfeed. You should not do both.<br />
Tell all <strong>of</strong> your healthcare providers <strong>and</strong> dentists that you are taking SUTENT.<br />
They should talk to the healthcare provider who prescribed SUTENT for you,<br />
before you have any surgery, or medical or dental procedure.<br />
Tell your healthcare provider about all the medicines you take, including<br />
prescription medicines <strong>and</strong> non-prescription medicines, vitamins, <strong>and</strong> herbal<br />
supplements. Using SUTENT with certain other medicines can cause serious<br />
side effects.<br />
You may have an increased risk <strong>of</strong> severe jaw bone problems (osteonecrosis)<br />
if you take SUTENT <strong>and</strong> a bisphosphonate medicine. Especially tell your<br />
healthcare provider if you are taking or have taken Actonel, Aredia, Boniva,<br />
Didronel, Fosamax, Reclast, Skelid or Zometa.
Know the medicines you take. Keep a list <strong>of</strong> them to show your healthcare<br />
provider <strong>and</strong> pharmacist when you get a new medicine. Talk with your healthcare<br />
provider before starting any new medicines.<br />
How should I take SUTENT<br />
• Take SUTENT exactly the way your healthcare provider tells you.<br />
• Take SUTENT 1 time each day with or without food.<br />
• If you take SUTENT for GIST or RCC, you will usually take your medicine for<br />
4 weeks (28 days) <strong>and</strong> then stop for 2 weeks (14 days). This is 1 cycle <strong>of</strong><br />
treatment. You will repeat this cycle for as long as your healthcare provider<br />
tells you to.<br />
• If you take SUTENT for pNET, take it one time each day until your healthcare<br />
provider tells you to stop.<br />
• Do not open the SUTENT capsules.<br />
• Do not drink grapefruit juice or eat grapefruit during your treatment with<br />
SUTENT. They may cause you to have too much SUTENT in your body.<br />
• Your healthcare provider may do blood tests before each cycle <strong>of</strong><br />
treatment.<br />
• If you miss a dose, take it as soon as you remember. Do not take it if it is<br />
close to your next dose. Just take the next dose at your regular time. Do not<br />
take more than 1 dose <strong>of</strong> SUTENT at a time. Tell your healthcare provider<br />
about any missed dose.<br />
• Call your healthcare provider right away, if you take too much SUTENT.<br />
What are possible side effects <strong>of</strong> SUTENT<br />
SUTENT may cause serious side effects including:<br />
• See “What is the most important information I should know about<br />
SUTENT”<br />
• Heart problems. Heart problems may include heart failure <strong>and</strong> heart<br />
muscle problems (cardiomyopathy) that can lead to death. Tell your<br />
healthcare provider if you feel very tired, are short <strong>of</strong> breath, or have<br />
swollen feet <strong>and</strong> ankles.<br />
• Abnormal heart rhythm changes. Your healthcare provider may do<br />
electrocardiograms <strong>and</strong> blood tests to watch for these problems during<br />
your treatment with SUTENT. Tell your healthcare provider if you feel dizzy,<br />
faint, or have abnormal heartbeats while taking SUTENT.<br />
• High blood pressure. Your healthcare provider may check your blood<br />
pressure during treatment with SUTENT. Your healthcare provider may<br />
prescribe medicine for you to treat high blood pressure, if needed.<br />
• Bleeding sometimes leading to death. Tell your healthcare provider right<br />
away if you have any <strong>of</strong> these symptoms or a serious bleeding problem<br />
during treatment with SUTENT.<br />
• painful, swollen stomach (abdomen)<br />
• vomiting blood<br />
• black, sticky stools<br />
• bloody urine<br />
• headache or change in your mental status<br />
Your healthcare provider can tell you other symptoms to watch for.<br />
• Jaw-bone problems (osteonecrosis) Severe jaw bone problems may<br />
happen when you take SUTENT. Your healthcare provider should examine<br />
your mouth before you start SUTENT. Your healthcare provider may tell you<br />
to see your dentist before you start SUTENT.<br />
• Tumor lysis syndrome (TLS). TLS is caused by the fast breakdown <strong>of</strong><br />
cancer cells <strong>and</strong> may lead to death. TLS may cause you to have nausea,<br />
shortness <strong>of</strong> breath, irregular heartbeat, clouding <strong>of</strong> urine <strong>and</strong> tiredness<br />
associated with abnormal laboratory test results (high potassium, uric acid<br />
<strong>and</strong> phosphorous levels <strong>and</strong> low calcium levels in the blood) that can lead<br />
to changes in kidney function <strong>and</strong> acute kidney failure. Your healthcare<br />
provider may do blood tests to check you for TLS.<br />
• Hormone problems, including thyroid <strong>and</strong> adrenal gl<strong>and</strong> problems. Your<br />
healthcare provider may do tests to check your thyroid <strong>and</strong> adrenal gl<strong>and</strong><br />
function during SUTENT treatment. Tell your doctor if you have any <strong>of</strong> the<br />
following signs <strong>and</strong> symptoms during treatment with SUTENT:<br />
• tiredness that worsens <strong>and</strong> does not go away<br />
• loss <strong>of</strong> appetite<br />
• heat intolerance<br />
• feeling nervous or agitated, tremors<br />
• sweating<br />
• nausea or vomiting<br />
• diarrhea<br />
• fast heart rate<br />
• weight gain or weight loss<br />
• feeling depressed<br />
• irregular menstrual periods or no menstrual periods<br />
• headache<br />
• hair loss<br />
Common side effects <strong>of</strong> SUTENT include:<br />
• The medicine in SUTENT is yellow, <strong>and</strong> it may make your skin look<br />
yellow. Your skin <strong>and</strong> hair may get lighter in color.<br />
• tiredness<br />
• weakness<br />
• fever<br />
• gastrointestinal symptoms, including diarrhea, nausea, vomiting, mouth<br />
sores, upset stomach, abdominal pain, <strong>and</strong> constipation. Talk with your<br />
healthcare provider about ways to h<strong>and</strong>le these problems.<br />
• rash or other skin changes, including drier, thicker, or cracking skin.<br />
• blisters or a rash on the palms <strong>of</strong> your h<strong>and</strong>s <strong>and</strong> soles <strong>of</strong> your feet.<br />
• taste changes<br />
• loss <strong>of</strong> appetite<br />
• pain or swelling in your arms or legs<br />
• cough<br />
• shortness <strong>of</strong> breath<br />
• bleeding, such as nosebleeds or bleeding from cuts.<br />
Call your healthcare provider if you have any swelling or bleeding during<br />
treatment with SUTENT.<br />
These are not all the possible side effects <strong>of</strong> SUTENT. For more information,<br />
ask your healthcare provider or pharmacist. Call your doctor for medical<br />
advice about side effects. You may report side effects to FDA at 1-800-FDA-<br />
1088.<br />
How do I store SUTENT<br />
• Store SUTENT at room temperature, between 59°F to 86°F (15°C to 30°C).<br />
Keep SUTENT <strong>and</strong> all medicines out <strong>of</strong> the reach <strong>of</strong> children.<br />
General information about SUTENT<br />
Medicines are sometimes prescribed for purposes other than those listed in<br />
a Medication <strong>Guide</strong>. Do not use SUTENT for a condition for which it was not<br />
prescribed. Do not give SUTENT to other people, even if they have the same<br />
symptoms you have. It may harm them.<br />
This Medication <strong>Guide</strong> gives the most important information about SUTENT.<br />
For more information about SUTENT, talk with your healthcare provider or<br />
pharmacist. You can ask your healthcare provider or pharmacist for information<br />
about SUTENT that is written for health pr<strong>of</strong>essionals.<br />
For more information go to www.SUTENT.com or call 1-877-5-SUTENT.<br />
What are the ingredients in SUTENT<br />
Active ingredient: sunitinib malate<br />
Inactive ingredients: mannitol, croscarmellose sodium, povidone (K-25),<br />
magnesium stearate Orange gelatin capsule shell: titanium dioxide, red iron<br />
oxide Caramel gelatin capsule shell: titanium dioxide, red iron oxide, yellow<br />
iron oxide, black iron oxide White printing ink: shellac, propylene glycol,<br />
sodium hydroxide, povidone, titanium dioxide<br />
This Medication <strong>Guide</strong> has been approved by the U.S. Food <strong>and</strong> Drug<br />
Administration.<br />
Gleevec ® is a registered trademark <strong>of</strong> Novartis Pharmaceuticals Corp<br />
LAB-0361-5.0<br />
April 2012<br />
Distributed by<br />
Pfizer Labs<br />
Division <strong>of</strong> Pfizer Inc, NY, NY 10017
Amgen, Inc.<br />
34<br />
www.amgen.com<br />
Oncology-related products: Aranesp ® (darbepoetin alfa), Epogen ®<br />
(epoetin alfa), Neulasta ® (pegfilgrastim), Neupogen ® (filgrastim),<br />
Nplate ® (romiplostim), Prolia ® (denosumab), Sensipar ® (cinacalcet),<br />
Vectibix ® , (panitumumab), Xgeva (denosumab)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.amgenassistonline.com<br />
<strong>Patient</strong> <strong>Assistance</strong><br />
Commercial Co-Pay <strong>Assistance</strong><br />
Coupon Support<br />
Amgen <strong>of</strong>fers co-pay coupon programs<br />
for Neulasta ® , Nplate ® , <strong>and</strong> Xgeva<br />
to help eligible patients who are commercially<br />
insured with their deductible,<br />
co-insurance, <strong>and</strong>/or co-payment requirements.<br />
To confirm your eligibility <strong>and</strong><br />
enroll in one <strong>of</strong> these programs, please<br />
call 1.888.65.STEP1 (888.657.8371) or<br />
visit www.amgenfirststep.com.<br />
Co-Pay Support<br />
<strong>Patient</strong>s who are commercially <strong>and</strong> government<br />
insured (including Medicare),<br />
but need financial assistance, can be<br />
referred to independent non-pr<strong>of</strong>it co-pay<br />
foundations. Amgen makes donations to<br />
these foundations that, in turn, help qualifying<br />
insured patients with out-<strong>of</strong>-pocket<br />
costs, including co-payments <strong>and</strong> premiums,<br />
to cover the medicines they need.<br />
●●<br />
●●<br />
●●<br />
HealthWell ® Foundation<br />
(www.healthwellfoundation.org)<br />
<strong>Patient</strong> Advocate Foundation<br />
(www.patientadvocate.org)<br />
<strong>Patient</strong> Access Network<br />
(www.panfoundation.org)<br />
Uninsured <strong>Patient</strong>s<br />
The Safety Net Foundation is a non-pr<strong>of</strong>it<br />
patient assistance program that helps<br />
qualifying uninsured patients access<br />
Amgen medicines at no cost. <strong>Patient</strong>s<br />
may be able to receive Amgen medications<br />
at no cost from The Safety Net<br />
Foundation if they meet the following<br />
eligibility requirements:<br />
●●<br />
Are a resident <strong>of</strong> the US or its<br />
territories<br />
●●<br />
●●<br />
●●<br />
Satisfy income eligibility requirements<br />
Have no or limited drug coverage<br />
Do not have any other insurance<br />
options. Note: Qualifying Medicare<br />
Part D patients may also be eligible.<br />
To enroll in The Safety Net Foundation,<br />
patients must complete the <strong>Patient</strong> Application<br />
Form in English (www.safetynetfoundation.com/pdf/SNF_<strong>Patient</strong>_Application_08012012_v3_FINAL.pdf)<br />
or<br />
Spanish (www.safetynetfoundation.com/<br />
pdf/SNF_<strong>Patient</strong>_Application_Spanish_08012012_v1_FINAL.pdf)<br />
<strong>and</strong> meet<br />
program eligibility requirements. For<br />
prospective model products, the patient<br />
can apply directly to the Foundation. Providers<br />
do not need to be enrolled in the<br />
Foundation for prospective products.<br />
Take this online course <strong>and</strong> learn about<br />
the insurance process from two perspectives<br />
as an advocate at a non-pr<strong>of</strong>it<br />
foundation <strong>and</strong> a practice manager in a<br />
cancer program share their combined<br />
knowledge about:<br />
■■<br />
■■<br />
■■<br />
The Medicare <strong>and</strong> Medicaid<br />
programs, MAC carriers, <strong>and</strong> the<br />
Part D drug benefit, including<br />
the “donut” hole <strong>and</strong> its effect on<br />
patients.<br />
The prescription drug benefits<br />
<strong>of</strong> private payers, such as drug<br />
formularies <strong>and</strong> drug tiers.<br />
Benefit verification, secondary<br />
benefits, prior authorizations,<br />
re-authorizations, <strong>and</strong> more.<br />
For drug replacement, the provider<br />
must apply to the Foundation on the<br />
patient’s behalf. The provider must first<br />
enroll in the Foundation before they can<br />
enroll a patient. Download the Facility<br />
Application form in English (www.<br />
safetynetfoundation.com/pdf/SNF_Facility_Application_08012012_v2_FINAL.<br />
pdf ) or Spanish (www.safetynetfoundation.com/pdf/SNF_<strong>Patient</strong>_Application_Spanish_08012012_v1_FINAL.pdf.<br />
Once enrolled, providers can complete<br />
the Product Replacement Request Form<br />
(www.safetynetfoundation.com/pdf/<br />
SNF_Product_Replacement_Request_<br />
Form_08012012_v2_FINAL.pdf).<br />
Institutions that have enrolled as Individual<br />
<strong>Patient</strong> <strong>Assistance</strong> Program (IPAP)<br />
facilities may use the IPAP <strong>Patient</strong> Application<br />
to enroll their patients. The form is<br />
available in both English (www.safetynetfoundation.com/pdf/SNF_IPAP_<strong>Patient</strong>_<br />
Application_08012012_v2_FINAL.pdf)<br />
<strong>and</strong> Spanish (www.safetynetfoundation.<br />
com/pdf/SNF_IPAP_<strong>Patient</strong>_Application_08012012_v2_FINAL.pdf).<br />
Questions Call 1.888.762.6436.<br />
REIMBURSEMENT ASSISTANCE<br />
Amgen Assist ® Online<br />
Amgen Assist Online gives patients <strong>and</strong><br />
healthcare providers a single destination<br />
for access to online services <strong>and</strong> forms,<br />
<strong>and</strong> makes it easier to find a program that<br />
would best meet each patient’s unique<br />
needs.<br />
Underst<strong>and</strong>ing the Insurance Process<br />
■■<br />
■■<br />
■■<br />
How to estimate the patient’s<br />
responsibility, including co-pays<br />
<strong>and</strong> deductibles.<br />
The appeals process.<br />
Disability, including eligibility,<br />
the application process, <strong>and</strong><br />
coverage.<br />
Register at: www.accc-cancer.org/<br />
education/FinancialCounseling-<br />
Courses.asp. This course is part<br />
<strong>of</strong> ACCC’s Financial Information<br />
<strong>and</strong> Learning Network educational<br />
program.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Pennrose – St. Francis Health<br />
Services, Colorado<br />
●●<br />
●●<br />
●●<br />
●●<br />
Insurance verification<br />
Prior authorization<br />
Billing <strong>and</strong> claims processing support<br />
<strong>and</strong> tracking<br />
Policy <strong>and</strong> program updates.<br />
Online tools include:<br />
●●<br />
Benefit verification forms<br />
●●<br />
<strong>Patient</strong> consent forms<br />
●●<br />
Sample letters <strong>of</strong> appeal<br />
●●<br />
Sample letters <strong>of</strong> medical necessity.<br />
Register today at: www.amgenassistonline.com/Registration/Registration.<br />
aspx. You can also call Amgen Assist<br />
at 1.888.4ASSIST <strong>and</strong> speak with an<br />
Amgen <strong>Reimbursement</strong> Counselor<br />
specific to your region for support with<br />
reimbursement or patient assistance.<br />
You can contact Amgen Assist by<br />
phone to request insurance verifications<br />
regarding Amgen products <strong>and</strong> for<br />
reimbursement <strong>and</strong> assistance information.<br />
Available Monday–Friday, 9 am–<br />
8 pm EST. After-hours calls are returned<br />
within one business day.<br />
Amgen <strong>Reimbursement</strong> Counselors<br />
You will be assigned a dedicated Amgen<br />
<strong>Reimbursement</strong> Counselor—a single<br />
point <strong>of</strong> contact with regional expertise<br />
responsible for coordinating all reimbursement<br />
activity for providers <strong>and</strong><br />
patients. Your Amgen <strong>Reimbursement</strong><br />
Counselor will assist you with:<br />
●●<br />
●●<br />
Comprehensive insurance<br />
verifications<br />
Prior authorization support, when<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
required by the insurance company<br />
Billing <strong>and</strong> claims processing support<br />
Claims review <strong>and</strong> tracking, when<br />
requested to assist status <strong>and</strong> payment<br />
tracking<br />
Appeals process research <strong>and</strong> status<br />
tracking, when prior authorizations or<br />
claims are denied<br />
General payer policy research<br />
Initiating recertification for patients<br />
continuing on therapy<br />
Identifying patient financial assistance<br />
programs, for those patients<br />
requiring financial assistance.<br />
In addition, Amgen <strong>Reimbursement</strong><br />
Counselors will be available upon request<br />
by providers to assist patients with<br />
counseling to underst<strong>and</strong> their insurance<br />
benefits <strong>and</strong> referrals to financial<br />
assistance programs.<br />
Billing <strong>and</strong> Claims Processing<br />
Support<br />
Amgen has more than 20 years <strong>of</strong> experience<br />
addressing coverage, coding, <strong>and</strong><br />
payment issues regarding its products.<br />
Our reimbursement experts can provide<br />
timely answers to billing questions about<br />
Medicare, Medicaid, commercial<br />
insurers, <strong>and</strong> managed care.<br />
Appeals Support<br />
If an insurance claim is denied or underpaid,<br />
or if a prior authorization request is<br />
denied, our staff can work with insurers<br />
to help resolve the issues. We can also<br />
help physicians <strong>and</strong> patients underst<strong>and</strong><br />
the payer <strong>and</strong> plan appeals process. Your<br />
Amgen <strong>Reimbursement</strong> Counselor can:<br />
●●<br />
Research a plan’s appeal requirements<br />
<strong>and</strong> procedures<br />
●●<br />
Discuss the requirements <strong>and</strong> answer<br />
your questions to facilitate the<br />
appeals process<br />
●●<br />
●●<br />
Provide letters <strong>of</strong> medical necessity<br />
forms to help streamline the process<br />
Track the appeal status with the payer<br />
<strong>and</strong> provide updates <strong>and</strong> results.<br />
Insurance Verification<br />
You can now initiate insurance verification<br />
requests online, as well as track<br />
service requests <strong>and</strong> outcomes on a<br />
patient-specific level. You can also<br />
contact Amgen Assist by phone to<br />
request insurance verifications regarding<br />
Amgen products. Amgen Assist will<br />
help you:<br />
●●<br />
●●<br />
Verify patients’ benefits <strong>and</strong> identify<br />
insurer coverage guidelines<br />
Obtain prior authorization (PA)<br />
when needed. Amgen Assist staff<br />
will quickly research the patient’s<br />
PA requirements to help you obtain<br />
authorization before treatment.<br />
Prior Authorization<br />
Amgen Assist can:<br />
●●<br />
Verify patients’ benefits <strong>and</strong> coverage<br />
for Amgen products<br />
●●<br />
Assist with submitting PA requests<br />
●●<br />
Follow up with providers to ensure<br />
form requirements are met<br />
●●<br />
Work with Amgen to resolve payer<br />
issues.<br />
35<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
ARIAD Pharmaceuticals, Inc.<br />
www.ariad.com<br />
Oncology-related products: Iclusig (ponatinib)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.ariadpass.com<br />
<strong>Patient</strong> <strong>Assistance</strong><br />
ARIAD PASS<br />
ARIAD is pleased to introduce the<br />
ARIAD <strong>Patient</strong> Access & Support<br />
Services (ARIAD PASS) program to<br />
help providers <strong>and</strong> their patients access,<br />
afford, <strong>and</strong> adhere to treatment. At<br />
ARIAD PASS benefit coordinators are<br />
available to help providers <strong>and</strong> their<br />
ARIAD<br />
PA S S <br />
<strong>Patient</strong> Access &<br />
Support Services<br />
ICLUSIG<br />
patients with ASSURANCE<br />
patient assistance (free<br />
product) <strong>and</strong> co-pay assistance programs.<br />
ARIAD PPASS Aalso <strong>of</strong>fers S dedicated<br />
oncology-certified nurses to<br />
S<br />
assist patients ICLUSIG with treatment support,<br />
disease education, QUICKSTART<br />
<strong>and</strong> referrals to other<br />
assistance programs, upon request. The<br />
ARIAD PASS Pbenefits A coordinator S S<br />
provides eligible patients with an array <strong>of</strong><br />
financial assistance ICLUSIG options, including copay<br />
or coinsurance COPAY support based on their<br />
insurance coverage <strong>and</strong> financial need.<br />
To enroll Pyour Apatient Sin this Sprogram,<br />
download the ARIAD PASS Enrollment<br />
Form at: www.ariadpass.com/ARIAD_<br />
PASS_Enrollment_Form.pdf. Completed<br />
forms should be faxed to: 1.855.557.<br />
PASS (1.855.557.7277). Questions Call<br />
1.855.447.PASS (1.855.447.7277) Monday<br />
through Friday, 7:00 am-7:00 pm CST.<br />
REIMBURSEMENT ASSISTANCE<br />
ARIAD PASS<br />
ARIAD PASS <strong>of</strong>fers coverage <strong>and</strong><br />
reimbursement support to providers<br />
<strong>and</strong> patients. To ensure that patients can<br />
promptly begin therapy, a benefits coordinator<br />
can help providers determine:<br />
●●<br />
A patient’s level <strong>of</strong> insurance<br />
coverage<br />
●●<br />
Additional requirements, such as<br />
prior authorizations<br />
●●<br />
Any preferred specialty pharmacy.<br />
To enroll your patient in this program,<br />
download the ARIAD PASS Enrollment<br />
Form at: www.ariadpass.com/ARIAD_<br />
PASS_Enrollment_Form.pdf. Completed<br />
forms should be faxed to: 1.855.557.<br />
PASS (1.855.557.7277). Questions Call<br />
1.855.447.PASS (1.855.447.7277) Monday<br />
through Friday, 7:00 am-7:00 pm CST.<br />
36<br />
Palo Alto Medical Foundation,<br />
California<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Astellas Pharma US, Inc.<br />
www.us.astellas.com<br />
Oncology-related products: Tarceva ® (erlotinib) tablets (co-marketed<br />
with Genentech, Inc.), Xt<strong>and</strong>i ® (enzalutamide) capsules<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.astellasaccess.com<br />
<strong>Patient</strong> <strong>Assistance</strong><br />
Xt<strong>and</strong>i Access Services<br />
This program helps guide providers <strong>and</strong><br />
patients, from underst<strong>and</strong>ing patient<br />
cost-sharing obligations to addressing<br />
financial barriers to Xt<strong>and</strong>i. Cost-sharing<br />
is expected to be similar for Xt<strong>and</strong>i as for<br />
other oral anti-cancer agents.<br />
Xt<strong>and</strong>i Access Services can determine<br />
whether a patient is eligible for one<br />
<strong>of</strong> several avenues <strong>of</strong> assistance available<br />
to patients who may not be able to afford<br />
their cost-sharing obligations. There are<br />
three ways in which patients may be<br />
able to obtain assistance with accessing<br />
Xt<strong>and</strong>i:<br />
1. <strong>Patient</strong>s with private insurance may<br />
be eligible to participate in the Xt<strong>and</strong>i<br />
<strong>Patient</strong> Savings Program.<br />
2. Medicare patients may be referred to<br />
independent co-pay foundations.<br />
3. Uninsured patients may be eligible for<br />
the Astellas Access Program.<br />
Need help determining which type <strong>of</strong><br />
patient assistance a patient qualifies<br />
for Take the online <strong>Patient</strong> <strong>Assistance</strong><br />
Eligibility Questionnaire at: www.astellasaccess.com/home/hcp/xt<strong>and</strong>i/patient_<br />
assistance/eligibility_questions.aspx or<br />
call Xt<strong>and</strong>i Access Services directly to<br />
discuss available assistance options at:<br />
1.855.8XTANDI (1.855.898.2634).<br />
Xt<strong>and</strong>i <strong>Patient</strong> Savings Program<br />
This program is for patients who have<br />
commercial <strong>and</strong>/or private health insurance<br />
but who may have trouble paying<br />
their out-<strong>of</strong>-pocket costs. <strong>Patient</strong>s may<br />
expect to pay no more than $20 out<strong>of</strong>-pocket<br />
per drug fill. The program<br />
will cover the remaining cost-sharing<br />
obligation up to $1,500 per month <strong>and</strong><br />
up to $12,000 in prescription costs per<br />
calendar year. Note: income eligibility<br />
rules apply <strong>and</strong> void where prohibited by<br />
law. The program is not valid for patients<br />
who have coverage under Medicare<br />
(including Medicare Part D), Medicaid,<br />
Medicare Advantage, TRICARE,<br />
CHAMPUS, Puerto Rico government<br />
health insurance, or any other federal– or<br />
state-funded pharmaceutical benefit program.<br />
Contact Xt<strong>and</strong>i Access Services at<br />
1.855.8XTANDI (1.855.898.2634) or your<br />
preferred specialty pharmacy to determine<br />
whether a patient is eligible for enrollment<br />
in the program or to learn more.<br />
Astellas Access Program<br />
This program is designed for patients<br />
who have no health insurance. It provides<br />
free Xt<strong>and</strong>i to patients who qualify<br />
for enrollment based on insurance <strong>and</strong><br />
household income status. <strong>Patient</strong>s may be<br />
eligible for the Astellas Access Program<br />
if they meet all <strong>of</strong> the following criteria:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Have been prescribed Xt<strong>and</strong>i for an<br />
FDA-approved indication or an authorized<br />
compendia listing<br />
Are uninsured or awaiting determination<br />
from public assistance (such as<br />
Medicaid)<br />
Satisfy the income criteria<br />
Have a verifiable shipping address<br />
within the United States.<br />
To enroll a patient, providers must<br />
complete <strong>and</strong> submit<br />
a request with a<br />
valid prescription.<br />
The quickest way to<br />
apply for assistance<br />
is via Astellas Access<br />
eService at: www.<br />
astellasaccess.com/<br />
home/hcp/xt<strong>and</strong>i/<br />
reimbursement_services/eservice_portal.<br />
aspx. Providers can<br />
also submit a request<br />
by completing the<br />
<strong>Patient</strong> Enrollment<br />
Form (www.<br />
astellasaccess.com/<br />
Docs/XTANDI/<br />
XAS_<strong>Patient</strong>_Enrollment_Form.pdf)<br />
Sanford Cancer Center,<br />
South Dakota<br />
<strong>and</strong> faxing it to 1.855.982.6341. When<br />
applying, providers must retain one <strong>of</strong><br />
the following as pro<strong>of</strong> <strong>of</strong> income for your<br />
patient:<br />
●●<br />
Copy <strong>of</strong> the patient’s most recent tax<br />
return<br />
●●<br />
Copy <strong>of</strong> the patient’s most recent W-2<br />
form<br />
●●<br />
Copy <strong>of</strong> the patient’s 1099 Social<br />
Security form<br />
●●<br />
Copy <strong>of</strong> the patient’s most recent<br />
Social Security benefit letter<br />
●●<br />
Copy <strong>of</strong> the patient’s latest pay stub<br />
for a consecutive 30 days.<br />
Once the patient is approved for assistance,<br />
we will notify both the prescriber<br />
<strong>and</strong> patient that they have been enrolled.<br />
An initial 30-day supply <strong>of</strong> Xt<strong>and</strong>i is<br />
then shipped directly to the patient’s<br />
home. Subsequent 30-day refills are then<br />
sent automatically to the patient’s home<br />
throughout the approval period. <strong>Patient</strong>s<br />
may be approved for assistance with<br />
Xt<strong>and</strong>i for up to one year. The Astellas<br />
Access Program will contact patients <strong>and</strong><br />
their healthcare providers 45 days before<br />
the approval period is scheduled to end to<br />
discuss re-enrollment needs. Healthcare<br />
providers can then re-apply on behalf <strong>of</strong><br />
their patients.<br />
REIMBURSEMENT ASSISTANCE<br />
Xt<strong>and</strong>i Access Services<br />
The program <strong>of</strong>fers an array <strong>of</strong> resources<br />
to help facilitate product coverage <strong>and</strong><br />
payment, including:<br />
●●<br />
Answering questions about<br />
37<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Xt<strong>and</strong>i Access Services Model<br />
Submit <strong>Patient</strong> Enrollment Form to either Xt<strong>and</strong>i Access Services or<br />
a specialty pharmacy within our preferred network.<br />
Xt<strong>and</strong>i Access<br />
Services<br />
Specialists<br />
Verify patient coverage for Xt<strong>and</strong>i.<br />
Assist with prior authorization, if required.<br />
Address financial barriers for patients through the Astellas Access<br />
Program, the Xt<strong>and</strong>i <strong>Patient</strong> Savings Program, or referrals to independent,<br />
not-for-pr<strong>of</strong>it foundations.<br />
Xt<strong>and</strong>i Access<br />
Services<br />
Specialists<br />
Specialty<br />
Pharmacy<br />
<strong>Patient</strong>s receive Xt<strong>and</strong>i from the specialty pharmacy or<br />
in-<strong>of</strong>fice pharmacy.<br />
38<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
reimbursement, coverage, <strong>and</strong> payment<br />
for Xt<strong>and</strong>i<br />
Verifying patient insurance coverage<br />
<strong>and</strong> cost-sharing<br />
Helping verify insurance requirements<br />
<strong>and</strong> track prior authorizations<br />
Providing assistance when prior authorizations<br />
are denied or when a patient’s<br />
insurer does not cover Xt<strong>and</strong>i<br />
Helping coordinate with a specialty<br />
pharmacy within our network that is<br />
contracted with your patients’ insurers<br />
to dispense Xt<strong>and</strong>i<br />
Determining whether patients are<br />
eligible for financial assistance for<br />
out-<strong>of</strong>-pocket costs associated with<br />
Xt<strong>and</strong>i<br />
Providing 24/7 access to status<br />
updates on requests for patient<br />
assistance via our eService at: www.<br />
astellasaccess.com<br />
Directing patients to additional information<br />
about Xt<strong>and</strong>i treatment.<br />
To enroll your patient in Xt<strong>and</strong>i Access<br />
Services, complete the <strong>Patient</strong> Enrollment<br />
Form at: www.astellasaccess.com/<br />
Docs/XTANDI/XAS_<strong>Patient</strong>_Enrollment_Form.pdf<br />
in its entirety (required<br />
fields marked with an asterisk), including<br />
the signatures section, <strong>and</strong> return via<br />
fax to 1.855.982.6341. The completed<br />
signature section allows Xt<strong>and</strong>i Access<br />
Services to:<br />
●●<br />
Perform the necessary service(s) to<br />
assist with patient access to Xt<strong>and</strong>i<br />
●●<br />
●●<br />
Astellas Access Program for<br />
Xt<strong>and</strong>i<br />
Log onto Astellas eService at: www.astellasaccess.com/home/hcp/<br />
xt<strong>and</strong>i/reimbursement_services/eservice_portal.aspx.<br />
Select “Initiate Access Application” <strong>and</strong> provide required information.<br />
Requests must be submitted by the prescribing physician or<br />
authorized facility employee.<br />
Retain copies <strong>of</strong> patient’s pro<strong>of</strong> <strong>of</strong> income.<br />
If the patient meets eligibility criteria, he or she will be enrolled into<br />
the program. Both the patient <strong>and</strong> provider will receive notification<br />
<strong>of</strong> enrollment.<br />
<strong>Patient</strong>s will receive their Xt<strong>and</strong>i shipment within 2 to 5 business<br />
day <strong>of</strong> approval notification.<br />
Triage the completed prescription(s)<br />
to a specialty pharmacy in the Xt<strong>and</strong>i<br />
Access Services network<br />
View patient’s Personal Health<br />
Information, including a patient’s<br />
financial information to determine<br />
the most appropriate form <strong>of</strong> financial<br />
assistance as appropriate.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Bayer HealthCare<br />
Pharmaceuticals, Inc.<br />
www.pharma.bayer.com<br />
Oncology-related product: Nexavar ® (sorafenib) tablets (co-marketed<br />
with Onyx Pharmaceuticals), Stivarga ® (regorafenib) tablets, X<strong>of</strong>igo ®<br />
(radium Ra 223 dichloride injection)<br />
<strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong><br />
<strong>Reimbursement</strong> Website<br />
www.nexavar-us.com<br />
www.stivarga-us.com/hcp/<br />
gist/support.html<br />
PATIENT ASSISTANCE<br />
REACH ® – Commercial Co-pay<br />
<strong>Assistance</strong><br />
<strong>Patient</strong>s with private insurance may<br />
be eligible to receive co-pay assistance<br />
through REACH (Resources for Expert<br />
<strong>Assistance</strong> <strong>and</strong> Care Helpline). This program<br />
is designed to reduce the monthly<br />
co-pay <strong>of</strong> patients with private insurance.<br />
<strong>Patient</strong>s covered by Medicare are<br />
not eligible for this program. A REACH<br />
counselor can tell you if your patient is<br />
eligible for co-pay assistance. If eligible,<br />
co-pays range from $0 to a maximum<br />
<strong>of</strong> $100 per prescription. REACH works<br />
directly with the specialty pharmacy<br />
<strong>and</strong> no special cards or coupons will be<br />
necessary. To enroll your patient, call<br />
1.866.639.2827 to speak with a REACH<br />
counselor. Enrollment forms are also<br />
available online:<br />
●●<br />
●●<br />
English: www.nexavar-us.com/html/<br />
pdf/consumer/English_REACH_<br />
form.pdf<br />
Spanish: www.nexavar-us.com/html/<br />
pdf/consumer/Spanish_REACH_<br />
form.pdf.<br />
Note: REACH is not for patients receiving<br />
prescription reimbursement under<br />
Florida Hospital, Waterman<br />
Cancer Institute, Florida<br />
any federal-, state-, or governmentfunded<br />
insurance programs or where<br />
prohibited by law.<br />
The REACH Program for Stivarga<br />
<strong>and</strong> Nexavar<br />
The REACH support program provides<br />
a single point <strong>of</strong> contact for healthcare<br />
pr<strong>of</strong>essionals prescribing Stivarga or<br />
Nexavar <strong>and</strong> their patients. REACH first<br />
works with providers, their staff, <strong>and</strong> the<br />
specialty-pharmacy network to coordinate<br />
the prescription-filling <strong>and</strong> reimbursement<br />
process. REACH will then work directly<br />
with patients receiving therapy to provide<br />
ongoing support. To enable a patient to<br />
obtain Stivarga or Nexavar:<br />
1. Fill out the REACH enrollment<br />
forms, including writing the prescription<br />
on the form. Download the form<br />
at: www.stivarga-us.com/downloads/<br />
reach_enrollment_ form.pdf<br />
2. Sign the form in the space provided<br />
under “Physician Declaration”<br />
3. Have your patient sign the form in<br />
the space provided under “<strong>Patient</strong><br />
Authorization”<br />
4. Fax both pages <strong>of</strong> the form to:<br />
1.866.639.5181.<br />
REACH counselors will then evaluate<br />
your patient’s coverage <strong>and</strong> provide a<br />
summary <strong>of</strong> benefits <strong>and</strong> in-network<br />
SPP options to you <strong>and</strong> your patient. For<br />
more information, contact REACH at<br />
1.866.639.2827.<br />
REACH Counselors can help patients<br />
identify other sources to help get their<br />
prescriptions, including:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Broad insurance plan coverage for<br />
Nexavar <strong>and</strong> Stivarga. A REACH<br />
counselor can contact your insurance<br />
company to help determine coverage<br />
for your therapy.<br />
Medicare Part D plans cover<br />
these therapies. A REACH counselor<br />
can help determine coverage.<br />
The patient assistance program<br />
provides eligible patients with a<br />
30-day supply <strong>of</strong> drug shipped to their<br />
home. <strong>Patient</strong>s approved for the program<br />
will receive assistance for one<br />
year, after which they must reapply.<br />
Temporary patient assistance<br />
programs <strong>of</strong>fer financial help so<br />
patients may pay for Nexavar or<br />
Stivarga while waiting for insurance<br />
approval. In addition, a REACH<br />
counselor can contact the insurance<br />
39<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
X<strong>of</strong>igo Access Services ®<br />
This program <strong>of</strong>fers comprehensive<br />
support for X<strong>of</strong>igo patients, either<br />
through finding coverage sources, helping<br />
eligible uninsured <strong>and</strong> underinsured<br />
patients through drug assistance<br />
programs, or assisting eligible insured<br />
patients with their co-share obligations.<br />
<strong>Patient</strong> assistance. X<strong>of</strong>igo Access<br />
Services provides X<strong>of</strong>igo free <strong>of</strong> charge<br />
for eligible patients who are uninsured<br />
or who are insured but do not have<br />
coverage for X<strong>of</strong>igo. To qualify for<br />
assistance, patients must meet certain<br />
eligibility criteria, including: financial<br />
criteria based on adjusted gross household<br />
income; residency in the U.S.,<br />
including the District <strong>of</strong> Columbia,<br />
Puerto Rico, Guam, or the U.S. Virgin<br />
Isl<strong>and</strong>s; <strong>and</strong> treatment provided in an<br />
outpatient setting. Providers must apply<br />
for assistance on behalf <strong>of</strong> their patients<br />
by submitting a completed application.<br />
Call 1.855.696.3446 to obtain more<br />
information <strong>and</strong> request an application.<br />
Co-pay assistance. <strong>Patient</strong>s with<br />
private commercial insurance may<br />
be eligible for co-pay or coinsurance<br />
assistance for X<strong>of</strong>igo if they<br />
meet eligibility criteria, including:<br />
financial criteria based on adjusted<br />
gross household income; residency<br />
in the U.S., including the District <strong>of</strong><br />
Columbia, Puerto Rico, Guam, or the<br />
U.S. Virgin Isl<strong>and</strong>s; <strong>and</strong> treatment<br />
provided in an outpatient setting.<br />
Providers must apply for assistance<br />
on behalf <strong>of</strong> their patients by submitting<br />
a completed application. Co-pay<br />
assistance funds are sent directly<br />
to the provider. Access Counselors<br />
can provide information <strong>and</strong> support<br />
through the application process. Call<br />
1.855.696.3446 to obtain more information<br />
<strong>and</strong> request an application.<br />
<strong>Patient</strong>s with public insurance, such<br />
as Medicare or other government payers,<br />
are not eligible for co-pay assistance<br />
through the X<strong>of</strong>igo Commercial<br />
Co-pay <strong>Assistance</strong> Program. Access<br />
Counselors can provide information<br />
about independent co-pay assistance<br />
foundations that may be able to help<br />
these patients.<br />
Alternate funding sources. Access<br />
Counselors can research potential<br />
alternate sources <strong>of</strong> funding, such<br />
as Medicaid or other state <strong>and</strong> local<br />
assistance programs. If your patient<br />
is eligible for one <strong>of</strong> these programs,<br />
an Access Counselor can provide<br />
information about the program <strong>and</strong><br />
how to apply.<br />
Insurance benefits. X<strong>of</strong>igo Access<br />
Services can providers research insurance<br />
benefits <strong>and</strong> confirm coverage for<br />
treatment with X<strong>of</strong>igo. If the patient’s<br />
insurance does not cover treatment with<br />
X<strong>of</strong>igo, Access Counselors can help<br />
research alternate sources <strong>of</strong> funding<br />
for treatment.<br />
For more information about X<strong>of</strong>igo<br />
Access Services, call 1.855.6XOFIGO<br />
(1.855.696.3446), Monday through<br />
Friday, 9:00 am to 8:00 pm EST, or go<br />
online to www.x<strong>of</strong>igo-us.com.<br />
40<br />
●●<br />
●●<br />
company to help with the approval<br />
process. Note: this program is not<br />
for patients receiving prescription<br />
reimbursement under any federal-,<br />
state-, or government-funded insurance<br />
programs or where prohibited<br />
by law.<br />
State pharmaceutical assistance<br />
programs provide prescription coverage<br />
<strong>and</strong> payment assistance for the<br />
disabled <strong>and</strong> low-income seniors that<br />
qualify. REACH counselors can find<br />
out information about this program in<br />
the patient’s state.<br />
Other sources <strong>of</strong> assistance include<br />
referrals to charitable foundations or<br />
support groups that can assist with<br />
your co-pay or other related medical<br />
expenses. Ask a REACH counselor to<br />
help identify these resources.<br />
REACH Education & Support<br />
Materials for Nexavar<br />
The REACH program provides patients<br />
with the materials they will need<br />
throughout their treatment with Nexavar.<br />
Once patients join the REACH program,<br />
they will receive the following materials:<br />
✔✔<br />
Your <strong>Guide</strong> to Nexavar brochure—<br />
everything patients need to know<br />
about Nexavar, including:<br />
■■<br />
■■<br />
■■<br />
Getting the most out <strong>of</strong> their<br />
therapy<br />
Proactively h<strong>and</strong>ling potential side<br />
effects<br />
Important items to discuss<br />
with their doctor <strong>and</strong> insurance<br />
provider<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
■■<br />
■■<br />
■■<br />
■■<br />
Weekly treatment tracker<br />
Reminder stickers<br />
Dosing reminder card<br />
Helpful resources <strong>and</strong> tips for<br />
patients <strong>and</strong> caregivers, such as<br />
finding strength <strong>and</strong> staying active<br />
Pillbox<br />
Coupons<br />
Udder smooth cream<br />
Dermal therapy lotion<br />
Prescribing Information.<br />
<strong>Patient</strong>s can also expect a call from a<br />
REACH oncology nurse to help answer<br />
any questions they may have about<br />
their Nexavar therapy. In addition,<br />
REACH counselors are available to<br />
provide you with the support you need:<br />
1.866.639.2827. Enroll online today at<br />
www.nexavar-us.com/scripts/pages/en/<br />
patient/patient-support/support-materials/enroll-in-reach.<br />
REACH Education & Support<br />
Materials for Stivarga<br />
Once Stivarga has been prescribed,<br />
patients will get a Starter Kit with these<br />
materials:<br />
✔✔<br />
✔✔<br />
The Stivarga Brochure (www.<br />
stivarga-us.com/downloads/Stivarga_Brochure.pdf)<br />
provides an<br />
overview <strong>of</strong> what Stivarga is, how it<br />
can help, <strong>and</strong> what to expect during<br />
treatment<br />
The Stivarga Treatment Journal<br />
(www.stivarga-us.com/downloads/<br />
Stivarga_<strong>Patient</strong>_Treatment_Journal.pdf)<br />
helps patients keep track<br />
✔✔<br />
✔✔<br />
<strong>of</strong> taking their Stivarga tablets <strong>and</strong><br />
record their general health<br />
Lotion <strong>and</strong> therapeutic socks for<br />
h<strong>and</strong>-foot skin reaction (HFSR)<br />
Lotion coupon to help with ordering<br />
<strong>and</strong> purchasing more lotion.<br />
REIMBURSEMENT ASSISTANCE<br />
A REACH counselor can help patients<br />
underst<strong>and</strong> their insurance options <strong>and</strong><br />
get the best coverage possible. Simply<br />
call 1.866.639.2827 <strong>and</strong> a specially<br />
trained REACH counselor will:<br />
●●<br />
Communicate with insurance companies<br />
<strong>and</strong> help patients obtain coverage<br />
for Nexavar or Stivarga—from obtaining<br />
authorization <strong>of</strong> coverage to following<br />
through if coverage is denied<br />
●●<br />
●●<br />
●●<br />
Help to determine if patients qualify<br />
for various financial assistance programs<br />
<strong>and</strong> assist with the application<br />
process<br />
Identify a specialty pharmacy provider<br />
(SPP) that will fill the prescription <strong>and</strong><br />
send it directly to patient’s home.<br />
Enrollment forms are available at:<br />
English: www.nexavar-us.com/html/<br />
pdf/consumer/English_REACH_<br />
form.pdf<br />
●●<br />
Spanish: www.nexavar-us.com/html/<br />
pdf/consumer/Spanish_REACH_<br />
form.pdf.<br />
Enrollment forms can also be obtained<br />
by calling 1.866.639.2827, Monday<br />
through Friday, 9:00 am to 8:00 pm EST.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Boehringer Ingelheim<br />
Pharmaceuticals, Inc.<br />
http://us.boehringer-ingelheim.com<br />
Building on scientific expertise <strong>and</strong><br />
excellence in the fields <strong>of</strong> pulmonary<br />
<strong>and</strong> cardiovascular medicine, metabolic<br />
disease, neurology, virology, <strong>and</strong><br />
immunology, Boehringer Ingelheim has<br />
embarked on a major research program<br />
to develop innovative cancer treatments.<br />
Working in close collaboration with the<br />
international scientific community <strong>and</strong><br />
a number <strong>of</strong> the world’s leading cancer<br />
centers, Boehringer Ingelheim’s commitment<br />
to oncology is underpinned by<br />
using advances in science to develop a<br />
range <strong>of</strong> targeted therapies for various<br />
solid tumors <strong>and</strong> hematological cancers.<br />
The current focus <strong>of</strong> late-stage research<br />
includes compounds in three areas:<br />
1. Signal transduction inhibition<br />
2. Angiogenesis inhibition<br />
3. Cell-cycle kinase inhibition.<br />
If you or someone you know is interested<br />
in participating in a Boehringer<br />
Ingelheim clinical trial, please visit<br />
www.bicancertrials.com. If you are a<br />
healthcare provider <strong>and</strong> are interested in<br />
learning more about BI clinical trials in<br />
oncology, please visit www.inoncologyus.<br />
com for additional information.<br />
Afatinib Exp<strong>and</strong>ed Access Program<br />
(EAP)<br />
Boehringer Ingelheim’s exp<strong>and</strong>ed<br />
access program for its investigational,<br />
oncology compound, afatinib, is for<br />
eligible U.S. patients with locally<br />
advanced or metastatic non-small<br />
cell lung cancer (NSCLC) who have<br />
an epidermal growth factor receptor<br />
(EGFR) mutation. (Note: afatinib is<br />
an investigational agent. Its safety <strong>and</strong><br />
efficacy have not been established.)<br />
Afatinib is an investigational therapy<br />
<strong>and</strong> has not been approved by the U.S.<br />
Food <strong>and</strong> Drug Administration (FDA).<br />
The afatinib EAP (clinical trial identifier<br />
NCT01649284) is an open-label, U.S.<br />
multi-center trial for patients with locally<br />
advanced or metastatic NSCLC who have<br />
an EGFR mutation. <strong>Patient</strong>s not previously<br />
treated with an EGFR-targeted therapy, as<br />
well as those previously treated with these<br />
agents, may be eligible for the afatinib<br />
EAP. As a single-arm trial, afatinib will<br />
not be compared to another anti-cancer<br />
therapy. Enrollment criteria are available<br />
on www.clinicaltrials.gov <strong>and</strong> include<br />
patients with:<br />
●●<br />
Locally advanced or metastatic<br />
NSCLC<br />
●●<br />
Positive test for EGFR mutation(s)<br />
●●<br />
Performance status between 0 <strong>and</strong> 2.<br />
Healthcare pr<strong>of</strong>essionals <strong>and</strong> patients can<br />
learn more about the afatinib EAP by<br />
calling 1.855.EAP.BIPI (855.327.2474) or<br />
by visiting www.clinicaltrials.gov.<br />
Exempla Saint Joseph Comprehensive<br />
Cancer Center, Colorado<br />
41<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Bristol-Myers Squibb<br />
42<br />
<strong>Assistance</strong> for Uninsured <strong>Patient</strong>s<br />
For patients without prescription drug<br />
insurance, Access Support can refer them<br />
to independent charitable foundations<br />
that may be able to provide financial support,<br />
including, the Bristol-Myers Squibb<br />
<strong>Patient</strong> <strong>Assistance</strong> Foundation, a charitable<br />
organization that provides mediwww.bms.com<br />
Oncology-related products: Erbitux ® (cetuximab), Ixempra ®<br />
(ixabepilone), Sprycel ® (dasatinib), Yervoy ® (ipilimumab)<br />
<strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong><br />
<strong>Reimbursement</strong> Website<br />
www.bmsaccesssupport.com<br />
PATIENT ASSISTANCE<br />
Access Support<br />
Access Support <strong>of</strong>fers patient assistance<br />
support, benefits investigation, prior<br />
authorization support, <strong>and</strong> appeals assistance.<br />
Program counselors are available<br />
Monday through Friday, from 8:00 am to<br />
8:00 pm EST at 1.800.861.0048. Access<br />
Support can help identify financial assistance<br />
programs for patients who need<br />
help managing the cost <strong>of</strong> treatment. The<br />
appropriate program will depend on the<br />
patient’s coverage:<br />
●●<br />
For patients with commercial<br />
insurance, product-specific co-pay<br />
programs may be available<br />
●●<br />
●●<br />
For patients with federally-funded<br />
insurance, co-pay support from independent<br />
foundations may be available<br />
For patients with no insurance, product<br />
donations from the BMS <strong>Patient</strong><br />
<strong>Assistance</strong> Program may be available.<br />
BMS Oncology Co-Pay Program for<br />
Yervoy<br />
This program is designed to assist with<br />
out-<strong>of</strong>-pocket co-payment<br />
or co-insurance<br />
requirements for eligible,<br />
commercially<br />
insured patients<br />
who have been<br />
prescribed certain<br />
BMS products, per<br />
the FDA-approved<br />
indications. <strong>Patient</strong>s<br />
with federally-funded<br />
insurance plans are<br />
not eligible for this<br />
co-pay program.<br />
Enrolled patients pay<br />
the first $50 <strong>of</strong> their<br />
co-pay per infusion.<br />
BMS will cover the remaining amount<br />
up to $5,000 per year. If patient out-<strong>of</strong>pocket<br />
expenses exceed $5,000 per year,<br />
the patient is responsible for 5% <strong>of</strong> the<br />
remaining out-<strong>of</strong>-pocket expenses. BMS<br />
will then pay 95% <strong>of</strong> the remaining out<strong>of</strong>-pocket<br />
expenses. BMS will contribute<br />
a maximum <strong>of</strong> $25,000 per year, per<br />
patient. <strong>Patient</strong> must have an annual<br />
household income <strong>of</strong> less than or equal<br />
to $100,000 to qualify for the program.<br />
Other restrictions may apply. Final determination<br />
<strong>of</strong> program eligibility is based<br />
upon review <strong>of</strong> completed application.<br />
In order to enroll a patient in the BMS<br />
Oncology Co-Pay Program, the following<br />
information is required:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Name<br />
Address<br />
Insurance carrier<br />
Member ID<br />
Your <strong>of</strong>fice identification number.<br />
To enroll a patient, complete the application<br />
form (www.bmsaccesssupport.com/<br />
PublishingImages/YERVOY-Enrollment-<br />
Form.pdf) <strong>and</strong> fax it to Access Support at<br />
1.888.776.2370.<br />
Southern Ohio<br />
Medical Center<br />
Cancer Services,<br />
Ohio<br />
cine, free <strong>of</strong> charge, to eligible, uninsured<br />
patients who have an established financial<br />
hardship. The Bristol-Myers Squibb<br />
<strong>Patient</strong> <strong>Assistance</strong> Foundation accepts<br />
the Access Support application. <strong>Patient</strong>s<br />
may be eligible for assistance through the<br />
Bristol-Myers Squibb <strong>Patient</strong> <strong>Assistance</strong><br />
Foundation if they:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Do not have public or private<br />
insurance that helps to pay for their<br />
prescription medications. If the<br />
patient is enrolled in Medicare Part<br />
D, call the Bristol-Myers Squibb<br />
<strong>Patient</strong> <strong>Assistance</strong> Foundation, Inc.<br />
for more information. The number is<br />
1.800.736.0003.<br />
Have a yearly income <strong>of</strong> less than<br />
~250% <strong>of</strong> the Federal Poverty Level:<br />
✔ ✔ $27,925 or less for a single person<br />
✔ ✔ $37,825 or less for a family size<br />
<strong>of</strong> two<br />
✔✔<br />
Larger family sizes are adjusted<br />
accordingly<br />
✔✔<br />
Medications that are injected may<br />
be subject to higher limits.<br />
Are being treated with Bristol-Myers<br />
Squibb medications.<br />
Live in the United States, Puerto<br />
Rico, or the US Virgin Isl<strong>and</strong>s.<br />
Are being treated by a doctor or other<br />
healthcare provider who is licensed<br />
in the US.<br />
Are being treated as an outpatient.<br />
These are just some <strong>of</strong> the eligibility<br />
requirements. Other eligibility criteria<br />
may apply. For more information<br />
about eligibility, call the Bristol-Myers<br />
Squibb <strong>Patient</strong> <strong>Assistance</strong> Foundation,<br />
at 1.800.736.0003. To enroll a patient,<br />
complete the appropriate application<br />
form below <strong>and</strong> fax it to Access Support<br />
at 1.888.776.2370.<br />
●●<br />
●●<br />
●●<br />
●●<br />
Erbitux: www.bmsaccesssupport.<br />
com/PublishingImages/ERBITUX-<br />
Enrollment-Form.pdf<br />
Ixempra: www.bmsaccesssupport.<br />
com/PublishingImages/IXEMPRA-<br />
Enrollment-Form.pdf<br />
Sprycel: www.bmsaccesssupport.<br />
com/docs/SPRYCEL-Enrollment-<br />
Form.pdf<br />
Yervoy: www.bmsaccesssupport.com/<br />
PublishingImages/YERVOY-Enrollment-Form.pdf<br />
<strong>Assistance</strong> for <strong>Patient</strong>s with<br />
Federally-Funded Insurance Plans<br />
<strong>Patient</strong>s with federally-funded insur-<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
BMS Prior Authorization Algorithm<br />
STEP 1 STEP 2 STEP 3 STEP 4 STEP 5 STEP 6<br />
Step 1:<br />
Verify <strong>Patient</strong><br />
Coverage. Is your<br />
patient insured<br />
Yes. No.<br />
Step 2:<br />
Benefits Investigation.<br />
Step 3:<br />
Is Prior Authorization<br />
Required<br />
Yes. No.<br />
If prior authorization<br />
is not needed,<br />
click next to<br />
continue.<br />
Step 4:<br />
Was Prior<br />
Authorization<br />
Received<br />
Yes. No.<br />
Step 5:<br />
You Now<br />
Have Payer<br />
Authorization.<br />
Step 6:<br />
Claim Approved<br />
<strong>and</strong> <strong>Patient</strong><br />
Received<br />
Medication.<br />
Yes. No.<br />
ance plans are not eligible for co-pay<br />
assistance programs sponsored by<br />
Bristol-Myers Squibb. However, there are<br />
independent foundations that can help.<br />
Access Support can refer providers to<br />
the foundation <strong>of</strong>fering the best support<br />
for their specific patient <strong>and</strong> help them<br />
through the application process.<br />
It is important to note that these foundations<br />
are independent <strong>and</strong> not affiliated<br />
with Bristol-Myers Squibb. Each foundation<br />
has its own eligibility criteria <strong>and</strong><br />
evaluation process. Bristol-Myers Squibb<br />
cannot guarantee that a patient will<br />
receive assistance.<br />
<strong>Reimbursement</strong> <strong>Assistance</strong><br />
Access Support: Benefits<br />
Investigation<br />
Bristol-Myers Squibb Oncology is committed<br />
to helping appropriate patients<br />
get access to our medications by providing<br />
reimbursement support services<br />
for healthcare pr<strong>of</strong>essionals. After a<br />
treatment decision has been made by<br />
a healthcare pr<strong>of</strong>essional, work with<br />
Access Support as early as possible, so<br />
each case can be tracked through all<br />
required steps for coverage <strong>and</strong> your<br />
eligible patients can benefit from all<br />
programs we have available. Our Access<br />
Support counselors are assigned to<br />
specific geographies to enable continuity<br />
<strong>of</strong> support <strong>and</strong> deeper underst<strong>and</strong>ing<br />
<strong>of</strong> the local environment. Each time you<br />
call, you will speak to a specialist who is<br />
familiar with your <strong>of</strong>fice, the details <strong>of</strong><br />
your patients’ cases, <strong>and</strong> the insurers in<br />
your area.<br />
With signed authorization from a<br />
patient, Access Support can investigate<br />
the patient’s coverage <strong>and</strong> benefits for<br />
Bristol-Myers Squibb products under<br />
federally-funded health plans. Access<br />
Support can also help identify potential<br />
or additional sources <strong>of</strong> coverage, such<br />
as Medicaid, Veterans’ Affairs, or Low<br />
Income Subsidy for Medicare Part D<br />
enrollees.<br />
To initiate the benefits investigation<br />
process, access the appropriate<br />
enrollment form below. Type in your<br />
information <strong>and</strong> save it to your desktop.<br />
Once the form is completed, fax it to:<br />
1.888.776.2370 <strong>and</strong> confirm receipt <strong>of</strong> the<br />
fax by calling: 1.800.861.0048.<br />
●●<br />
●●<br />
●●<br />
●●<br />
Erbitux: www.bmsaccesssupport.<br />
com/PublishingImages/ERBITUX-<br />
Enrollment-Form.pdf<br />
Ixempra: www.bmsaccesssupport.<br />
com/PublishingImages/IXEMPRA-<br />
Enrollment-Form.pdf<br />
Sprycel: www.bmsaccesssupport.<br />
com/docs/SPRYCEL-Enrollment-<br />
Form.pdf<br />
Yervoy: www.bmsaccesssupport.com/<br />
PublishingImages/YERVOY-Enrollment-Form.pdf.<br />
Access Support: Prior Authorization<br />
<strong>Assistance</strong><br />
Access Support can help physicians<br />
obtain a prior authorization form when<br />
one is required by the patient’s health<br />
plan. See the algorithm above to see an<br />
example process flow that serves as an<br />
aid to underst<strong>and</strong>ing the reimbursement<br />
<strong>and</strong> appeals processes. To receive prior<br />
authorization assistance from Access<br />
Support you will need:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
<strong>Patient</strong> demographics<br />
Complete insurance information <strong>and</strong><br />
copy <strong>of</strong> card<br />
Physician demographics <strong>and</strong> signature<br />
Diagnosis<br />
Drug.<br />
Access Support: Appeals <strong>Assistance</strong><br />
Access Support can assist in navigating<br />
the appeals process. However, the preparation<br />
<strong>and</strong> submission <strong>of</strong> documents to<br />
support the appeal is the responsibility <strong>of</strong><br />
the patient <strong>and</strong>/or healthcare provider. Providers<br />
<strong>and</strong> patients can appeal an insurer’s<br />
decision to deny coverage for an item or<br />
service. Some claims may be denied coverage<br />
due to the evolving nature <strong>of</strong> many<br />
drug therapies. Use the information below<br />
as a reminder when filing an appeal:<br />
1. Coverage decisions may be made<br />
by an insurer before the treatment<br />
is rendered or after a claim is filed.<br />
Coverage decisions that are made<br />
before a treatment regimen is initiated<br />
are <strong>of</strong>ten referred to as “prior<br />
authorizations” or “coverage determinations.”<br />
2. Medicare Part B <strong>and</strong> many other<br />
health insurers will not make a coverage<br />
decision regarding individual<br />
patients before a claim is filed; coverage<br />
is considered only at the time a<br />
claim is presented for payment.<br />
3. The billing provider can usually<br />
appeal an insurer’s decision to deny<br />
coverage for a claim. Appeals are<br />
almost always subject to timeliness<br />
requirements; the window <strong>of</strong> time<br />
allowed for a provider to appeal an<br />
unfavorable coverage decision usually<br />
begins on the date a claim was adjudicated<br />
(processed) by the insurer.<br />
4. If the health insurer approves an<br />
appeal, you will be notified <strong>and</strong> the<br />
claim will be reconsidered.<br />
If the health insurer denies the appeal,<br />
contact Access Support for further assistance<br />
at the Support Center by going to:<br />
www.bmsaccesssupport.com <strong>and</strong> clicking<br />
on the “Support Center” tab.<br />
43<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Celgene Oncology<br />
44<br />
www.celgene.com<br />
Oncology-related products: Abraxane ® for Injectable Suspension<br />
(paclitaxel protein-bound particles for injectable suspension),<br />
Istodax ® (romidepsin) for Injection, Revlimid ® (lenalidomide),<br />
Thalomid ® (thalidomide), Vidaza ® (azacitidine)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.celgenepatientsupport.<br />
com<br />
PATIENT ASSISTANCE<br />
Celgene Free Medication Program<br />
<strong>Patient</strong>s who cannot pay for a Celgene<br />
medication that their doctor prescribed<br />
may be eligible for this program.<br />
<strong>Patient</strong>s must meet financial criteria to<br />
be eligible for assistance. Eligibility is<br />
based on household income <strong>and</strong> assets, as<br />
described below:<br />
Income<br />
●●<br />
Salary/wages<br />
●●<br />
Pension<br />
●●<br />
Social Security<br />
●●<br />
Disability<br />
●●<br />
Earnings from dividends<br />
●●<br />
Earnings from rental property.<br />
Assets<br />
Savings, checking, money market<br />
accounts<br />
CDs<br />
Estimated market value <strong>of</strong> IRAs<br />
Estimated market value <strong>of</strong> stocks,<br />
mutual funds<br />
Estimated market value <strong>of</strong> bonds.<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Note: Assets do not include: household<br />
items, personal property, house, or car.<br />
To determine a patient’s eligibility,<br />
contact Celgene <strong>Patient</strong> Support at:<br />
1.800.931.8691 or email: patientsupport@celgene.com.<br />
Depending on the<br />
type <strong>of</strong> help needed, the Celgene <strong>Patient</strong><br />
Support Specialist may ask patients to<br />
complete the following forms:<br />
●●<br />
<strong>Patient</strong> <strong>Assistance</strong> Application<br />
(www.celgenepatientsupport.com/<br />
pdf/PAA-form.pdf). The application<br />
has two parts: one for the provider to<br />
●●<br />
●●<br />
complete, <strong>and</strong> one for the patient to<br />
complete.<br />
Appointment <strong>of</strong> Representative<br />
Release Form (www.celgenepatientsupport.com/pdf/AORR-form.pdf).<br />
This form is needed so that Celgene<br />
may help with appeals upon a denial<br />
from an insurance company. By<br />
completing this form, patients are<br />
allowing Celgene <strong>Patient</strong> Support to<br />
call their insurance company <strong>and</strong> ask<br />
questions on the patients’ behalf.<br />
Medicare Low-Income Subsidy<br />
(“Extra Help”) Form (https://secure.<br />
ssa.gov/i1020/start).The low-income<br />
subsidy provides extra help in paying<br />
for prescription drug costs.<br />
Co-pay <strong>Assistance</strong> Programs<br />
Even if patients have insurance, they still<br />
may not be able to pay for their medication.<br />
There are programs <strong>and</strong> foundations<br />
that may help patients pay for<br />
co-payments <strong>and</strong> out-<strong>of</strong>-pocket expenses.<br />
A Celgene <strong>Patient</strong> Support Specialist<br />
will guide providers <strong>and</strong> patients through<br />
the available resources. Contact Celgene<br />
Celgene <strong>Patient</strong><br />
Support Checklist<br />
Your Celgene <strong>Patient</strong> Support<br />
Specialist may need the following<br />
information so they can assist you.<br />
Have this information available<br />
when you call.<br />
<strong>Patient</strong> Information<br />
●●<br />
Name<br />
●●<br />
Social Security Number<br />
●●<br />
Date <strong>of</strong> Birth<br />
●●<br />
Address<br />
●●<br />
Phone Number<br />
●●<br />
Medical Insurance Card(s)<br />
●●<br />
Prescription Drug Card(s)<br />
<strong>Patient</strong> Medical Information<br />
Medication<br />
Diagnosis<br />
Physician’s Name<br />
Physician’s Phone Number<br />
●●<br />
●●<br />
●●<br />
●●<br />
<strong>Patient</strong> Support at: 1.800.931.8691 or<br />
email: patientsupport@celgene.com.<br />
These pr<strong>of</strong>essionals can:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Connect patients with organization(s)<br />
that may provide financial assistance.<br />
<strong>Guide</strong> patients through filling out<br />
the forms. (Note these pr<strong>of</strong>essionals<br />
cannot complete the paperwork for<br />
patients.)<br />
Let the provider’s <strong>of</strong>fice know about<br />
options available to patients.<br />
Regularly follow up with patients<br />
<strong>and</strong> providers about applications for<br />
assistance.<br />
Let the provider’s <strong>of</strong>fice know about<br />
the final resolution.<br />
Remember that each organization has<br />
their own rules for helping patients.<br />
Celgene <strong>Patient</strong> Support cannot influence<br />
decisions by organizations on providing<br />
assistance. The Celgene <strong>Patient</strong> Support<br />
Specialist may need certain information<br />
to help providers <strong>and</strong> patients. Download<br />
the Celgene Support Checklist at: www.<br />
celgenepatientsupport.com/pdf/CPSchecklist.pdf.<br />
REIMBURSEMENT ASSISTANCE<br />
Celgene <strong>Patient</strong> Support<br />
Celgene <strong>Patient</strong> Support helps providers<br />
<strong>and</strong> patients navigate the challenges <strong>of</strong><br />
reimbursement, providing information<br />
about co-pay assistance, <strong>and</strong> answering<br />
questions about obtaining Celgene products.<br />
Celgene <strong>Patient</strong> Support Specialists<br />
work with providers <strong>and</strong> patients to:<br />
●●<br />
Explain benefits<br />
●●<br />
Facilitate prior authorization<br />
●●<br />
Assist with appeal support after insurance<br />
denials<br />
●●<br />
Navigate your Medicare coverage<br />
●●<br />
Assess co-pay options<br />
●●<br />
Follow up on prescription status<br />
●●<br />
Help apply for the Celgene free medication<br />
program<br />
●●<br />
Offer guidance through Celgene<br />
products <strong>and</strong> restricted distribution<br />
programs.<br />
For more help, contact Celgene <strong>Patient</strong><br />
Support at 1.800.931.8691. Your Celgene<br />
<strong>Patient</strong> Support Specialist is a dedicated,<br />
central point <strong>of</strong> contact who will work<br />
to coordinate resources available to<br />
providers <strong>and</strong> patients. Together, we will<br />
exhaust all options to help providers <strong>and</strong><br />
patients get the information they need.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Eisai Co., Ltd.<br />
www.eisai.com<br />
Oncology-related products: Aloxi ®<br />
(palonosetron hydrochloride),<br />
Dacogen ® (decitabine) for<br />
Injection, Fragmin (dalteparin<br />
sodium injection), Gliadel ®<br />
(polifeprosan 20 with carmustine<br />
implant) Wafer, Halaven<br />
(eribulin mesylate), Hexalen ®<br />
(altretamine) Capsules, Ontak ®<br />
(denileukin diftitox), Targretin ®<br />
(bexarotene) capsules, Targretin ®<br />
(bexarotene) gel 1%<br />
Sample Letter <strong>of</strong> Appeal for Aloxi<br />
Date<br />
Name <strong>of</strong> Health Insurance Company<br />
PO Box or Street Address<br />
City, State, Zip Code<br />
Appeal (or Request for Reconsideration): Aloxi ® (palonosetron HCl) injection – J2469<br />
Beneficiary: <strong>Patient</strong> Name<br />
HIC Number or Member Number<br />
Dates <strong>of</strong> Service: [mm-dd-yy through mm-dd-yy]<br />
Claim Number(s): [List each ICN claim number for each date <strong>of</strong> service denied]<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website:<br />
www.eisaireimbursement.com<br />
PATIENT ASSISTANCE<br />
The Eisai <strong>Assistance</strong> Program<br />
The Eisai <strong>Patient</strong> <strong>Assistance</strong> Program<br />
provides Eisai medicines at no cost to<br />
financially needy patients who meet<br />
program eligibility criteria. To prescreen<br />
your patients for eligibility go to:<br />
www.eisaipatientassistance.com. This<br />
prescreening tool is intended to assist<br />
healthcare pr<strong>of</strong>essionals in:<br />
●●<br />
Determining if a patient may be<br />
eligible for the patient assistance<br />
program<br />
●●<br />
Pre-populating enrollment forms to<br />
be submitted for the patient assistance<br />
program.<br />
The prescreening process is an initial<br />
step to determine if a patient may be<br />
eligible. A final enrollment determination<br />
will be made once a complete <strong>and</strong><br />
signed enrollment form <strong>and</strong> prescription<br />
are submitted via fax to: 1.866.57EISAI<br />
(1.866.5734724). Other online tools<br />
include:<br />
●●<br />
The Eisai <strong>Patient</strong> <strong>Assistance</strong><br />
Program Enrollment Form (www.<br />
eisaireimbursement.com/Aloxi/<br />
downloads/Eisai_Oncology_PAP_<br />
App_ALv_010411_pg2_writable.pdf).<br />
The same form is used for all Eisai<br />
drugs.<br />
●●<br />
To Whom It May Concern:<br />
The above claims were denied as not medically necessary <strong>and</strong> not covered under<br />
Medicare Part B. We are requesting a re-determination <strong>of</strong> the denial <strong>of</strong> coverage for<br />
Aloxi (palonosetron HCl) injection 0.25 mg. Aloxi is indicated for the prevention <strong>of</strong><br />
acute nausea <strong>and</strong> vomiting associated with initial <strong>and</strong> repeat courses <strong>of</strong> moderately<br />
<strong>and</strong> highly emetogenic cancer chemotherapy, as well as the prevention <strong>of</strong> delayed<br />
nausea <strong>and</strong> vomiting associated with initial <strong>and</strong> repeat courses <strong>of</strong> moderately emetogenic<br />
cancer chemotherapy.<br />
[In the second paragraph, outline the patient’s history, diagnosis, <strong>and</strong> chemotherapy<br />
treatment. Provide rationale for Aloxi treatment.]<br />
In light <strong>of</strong> the above, I believe Aloxi should be covered by Medicare for this patient.<br />
Use <strong>of</strong> Aloxi was medically necessary, <strong>and</strong> it was an appropriate drug for my patient<br />
at the time to prevent [state complication]. Relevant documentation is enclosed with<br />
this request for re-determination. Also enclosed are copies <strong>of</strong> claims submitted for<br />
payment <strong>and</strong> explanation(s) <strong>of</strong> Medicare benefits received showing the reason for the<br />
original determination(s).<br />
Respectfully submitted,<br />
[Physician Name, Signature]<br />
Enclosures:<br />
Explanation <strong>of</strong> Medicare benefits<br />
Copies <strong>of</strong> claim forms submitted (CMS-1500 or CMS-1450)<br />
Copies <strong>of</strong> patient medical records<br />
The Eisai <strong>Assistance</strong> Program<br />
Insurance Verification Form (www.<br />
eisaireimbursement.com/Aloxi/<br />
downloads/Eisai_Oncology_IV_<br />
Form_113010.pdf). The same form is<br />
used for all Eisai drugs.<br />
This program can help qualified<br />
indigent, underinsured, <strong>and</strong> uninsured<br />
patients obtain medication <strong>and</strong> find<br />
alternative sources <strong>of</strong> coverage. To<br />
learn more about the Eisai <strong>Assistance</strong><br />
Program <strong>and</strong> gain access to our team <strong>of</strong><br />
dedicated reimbursement consultants,<br />
call 1.866.61.EISAI (1.866.613.4724).<br />
<strong>Reimbursement</strong> consultants are available<br />
Monday through Friday, from<br />
8:00 am to 8:00 pm EST.<br />
45<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
The Michael <strong>and</strong> Dianne Bienes Comprehensive<br />
Cancer Center at Holy Cross Hospital, Florida<br />
46<br />
REIMBURSEMENT ASSISTANCE<br />
The Eisai <strong>Assistance</strong> Program<br />
The Eisai <strong>Assistance</strong> Program helps<br />
providers minimize payer access <strong>and</strong><br />
coverage challenges. The program is the<br />
first-line resource for information relating<br />
to your patients’ insurance coverage.<br />
What to expect when you contact the<br />
Eisai <strong>Assistance</strong> Program:<br />
●●<br />
●●<br />
Product-specific reimbursement<br />
information<br />
Underst<strong>and</strong>ing <strong>of</strong> coverage, coding,<br />
<strong>and</strong> payment issues<br />
●●<br />
●●<br />
●●<br />
●●<br />
Insurance verification processing<br />
Prior authorization assistance<br />
General guidance for appealing a<br />
denied claim<br />
Payer policy information.<br />
Online Tools<br />
The Eisai <strong>Assistance</strong> Program <strong>of</strong>fers<br />
providers a wide range <strong>of</strong> online tools<br />
for each <strong>of</strong> its products, including:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Product information<br />
Billing forms<br />
ICD-9-CM diagnosis codes<br />
ICD-9-CM supplementary<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
classification codes<br />
CPT drug administration codes<br />
HCPCS Level II codes<br />
National drug codes<br />
Revenue codes<br />
Medicare reimbursement rates<br />
A checklist for claims submission<br />
Sample appeal letters (see box,<br />
page 45)<br />
Sample letters <strong>of</strong> medical necessity<br />
Coverage policies for physician<br />
<strong>of</strong>fices, hospital outpatient<br />
departments, <strong>and</strong> ambulatory<br />
surgical centers.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Eli Lilly <strong>and</strong> Company<br />
www.lilly.com<br />
Oncology-related products: Alimta ® (pemetrexed), Erbitux ®<br />
(cetuximab) co-marketed with Bristol-Myers Squibb, Gemzar ®<br />
(gemcitabine hydrochloride)<br />
<strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong><br />
<strong>Reimbursement</strong> Website<br />
www.lillytruassist.com<br />
www.lillypatientone.com<br />
PATIENT ASSISTANCE<br />
Lilly TruAssist<br />
Lilly TruAssist (www.lillytruassist.com)<br />
is the collection <strong>of</strong> Lilly patient assistance<br />
programs that <strong>of</strong>fer assistance to help<br />
people obtain the Lilly medicines they<br />
need. This site includes all <strong>of</strong> Lilly’s<br />
patient assistance programs with individual<br />
program details. Finding programs<br />
that <strong>of</strong>fer Lilly medicines for free is easy<br />
with the Program Finder Tool: www.<br />
lillytruassist.com/pages/FindProgram.<br />
aspx. The tool finder allows patients<br />
<strong>and</strong> providers to search for an appropriate<br />
program one product at a time. Just<br />
answer a few questions to see which<br />
program may be right for your patient.<br />
<strong>Patient</strong>One<br />
<strong>Patient</strong>One (www.lillypatientone.com) is<br />
the program that addresses financial <strong>and</strong><br />
coverage issues for qualified uninsured,<br />
underinsured, <strong>and</strong> insured patients<br />
who are prescribed a Lilly Oncology<br />
product. <strong>Patient</strong>s are encouraged to<br />
contact their healthcare pr<strong>of</strong>essional for<br />
information regarding support for a Lilly<br />
Oncology product.<br />
Uninsured <strong>Patient</strong>s<br />
<strong>Patient</strong>One can help provide replacement<br />
vials for ongoing therapy for qualified<br />
uninsured patients earning up to 500%<br />
<strong>of</strong> the federal poverty level who are<br />
prescribed a Lilly Oncology product.<br />
Federal poverty level depends on family<br />
size. <strong>Patient</strong>s must meet basic points <strong>of</strong><br />
eligibility:<br />
✔✔<br />
✔✔<br />
<strong>Patient</strong> has no medical insurance or<br />
his or her insurance does not cover<br />
therapy<br />
A qualified Lilly Oncology drug will<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
be administered in the U.S.<br />
<strong>Patient</strong> is in ongoing therapy<br />
Pro<strong>of</strong> <strong>of</strong> residency in the United<br />
States or Puerto Rico<br />
<strong>Patient</strong> meets the financial guidelines<br />
for the program<br />
The date <strong>of</strong> service must be within<br />
180 days from the date <strong>Patient</strong>One<br />
receives the application<br />
Treatment is or will be provided in<br />
an outpatient setting (provider is<br />
community-based billing on CMS-<br />
1500 or outpatient-facility billing<br />
on UB-04).<br />
If patients meet these eligibility<br />
requirements, download the enrollment<br />
application (www.lillypatientone.<br />
com/Documents/application.pdf ) <strong>and</strong><br />
dosage tracking form (www.lillypatientone.com/Documents/pdf/dosage_<br />
tracking_ form.pdf). Providers can also<br />
call 1.866.4PatOne (1.866.472.8663)<br />
to receive enrollment forms. Fax completed<br />
application <strong>and</strong> pro<strong>of</strong> <strong>of</strong> income<br />
to 1.888.242.6230. <strong>Patient</strong>’s eligibility<br />
is confirmed within two business<br />
days. <strong>Patient</strong>One will also determine if<br />
there are alternate methods <strong>of</strong> coverage<br />
available to the patient, including<br />
Medicaid, VA, other payers, state<br />
pharmacy assistance programs, or<br />
charitable foundations. If patients apply<br />
for Medicaid, Medicare, VA, or other<br />
coverage, they may be temporarily<br />
approved for the Lilly <strong>Patient</strong> <strong>Assistance</strong><br />
Program. Eligible patients will<br />
be enrolled into the <strong>Patient</strong> <strong>Assistance</strong><br />
Program. Approved dates <strong>of</strong><br />
service will be determined based on<br />
the submitted Dosage Tracking Form.<br />
Replacement vials for ongoing therapy<br />
will be sent to the provider’s <strong>of</strong>fice.<br />
Note: This is not a replacement program—it<br />
is only for ongoing therapy.<br />
Underinsured <strong>Patient</strong>s<br />
Co-pays <strong>and</strong> deductibles can <strong>of</strong>ten be<br />
financial distractions. <strong>Patient</strong>One provides<br />
assistance in identifying programs<br />
that can help qualified patients who are<br />
prescribed a Lilly Oncology product<br />
cover these expenses. <strong>Patient</strong>One can:<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
Learn about the patient’s needs <strong>and</strong><br />
assess our ability to help<br />
Provide information on co-pay assistance<br />
programs<br />
Transfer to a specific foundation upon<br />
request<br />
Conduct a complete benefits investigation<br />
for eligible Lilly Oncology<br />
products.<br />
The <strong>Patient</strong>One Hotline accepts calls<br />
from <strong>and</strong> provides support for:<br />
<strong>Patient</strong>s<br />
Caregivers<br />
Physicians<br />
Administrators<br />
Cancer practice pr<strong>of</strong>essionals.<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Call 1.866.4PatOne (1.866.472.8663)<br />
Monday through Friday, 9:00 am to 7:00<br />
pm EST <strong>and</strong> select option 1.<br />
If the patient meets basic points <strong>of</strong> eligibility,<br />
complete <strong>and</strong> fax a <strong>Patient</strong> <strong>Assistance</strong><br />
Program Application Form (www.<br />
lillypatientone.com/Documents/application.pdf)<br />
<strong>and</strong> Certification <strong>of</strong> Br<strong>and</strong> Drug<br />
Usage Form (www.lillypatientone.com/<br />
Documents/pdf/gc67769_certification_<br />
<strong>of</strong> _br<strong>and</strong>_drug_usage_ form_ fa.pdf) if<br />
applicable to: 888.242.6230. The treating<br />
physician will receive a written response<br />
from <strong>Patient</strong>One, regarding eligibility<br />
for drug replacement. We will review the<br />
patient’s eligibility for the <strong>Patient</strong> <strong>Assistance</strong><br />
Program based on the submitted<br />
application. If the patient meets eligibility<br />
requirements, replacement vials will be<br />
sent to the provider’s <strong>of</strong>fice for ongoing<br />
therapy.<br />
Insured <strong>Patient</strong>s<br />
When an insurance claim is denied<br />
for patients receiving an eligible Lilly<br />
Oncology product, <strong>Patient</strong>One can<br />
provide assistance with the claim appeal<br />
process. <strong>Patient</strong>One can conduct a complete<br />
benefits investigation for applications<br />
with an approved diagnosis for<br />
eligible Lilly Oncology products at no<br />
cost to patients. Healthcare pr<strong>of</strong>essionals<br />
may contact us at 1.866.4PatOne to<br />
request that a <strong>Reimbursement</strong> <strong>Assistance</strong><br />
Application Form be faxed to you,<br />
or download <strong>and</strong> fill out the <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Application Form at:<br />
www.lillypatientone.com/Documents/<br />
pdf/Appeals<strong>and</strong><strong>Reimbursement</strong><strong>Assistance</strong>Application.pdf.<br />
Fax completed<br />
form <strong>and</strong> Certification <strong>of</strong> Br<strong>and</strong> Drug<br />
47<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
48<br />
Usage Form 9 (www.lillypatientone.<br />
com/Documents/pdf/gc67769_certification_<strong>of</strong><br />
_br<strong>and</strong>_drug_usage_ form_<br />
fa.pdf) if applicable to: 888.242.6230.<br />
The treating physician will receive<br />
a written response from <strong>Patient</strong>One,<br />
Take this online course <strong>and</strong> learn how<br />
to deliver financial assistance in a<br />
thoughtful <strong>and</strong> sensitive manner, as<br />
well as strategies to help patients maintain<br />
control <strong>of</strong> their finances so they<br />
can better focus energies on treatment<br />
<strong>and</strong> recovery.<br />
An experienced oncology social<br />
worker provides strategies <strong>and</strong> tips<br />
about:<br />
■■<br />
■■<br />
■■<br />
■■<br />
<strong>Patient</strong> Counseling 101<br />
Communicating with empathy<br />
The basics <strong>of</strong> customer service<br />
<strong>Patient</strong> <strong>and</strong> family assessments<br />
<strong>and</strong> interventions<br />
Non-compliance assessment <strong>and</strong><br />
regarding eligibility for drug replacement.<br />
We also provide templates, forms,<br />
<strong>and</strong> checklists that may assist you in<br />
filing an appeal for denied claims for<br />
eligible Lilly Oncology products.<br />
Upon request we can contact the<br />
■■<br />
Spartanburg Regional Medical Center,<br />
The Marsha <strong>and</strong> Jimmy Gibbs Regional<br />
Cancer Center, South Carolina<br />
interventions<br />
Situational case studies <strong>of</strong> “hard<br />
to h<strong>and</strong>le” situations.<br />
Register at: www.accc-cancer.org/education/FinancialCounseling-Courses.<br />
asp. This course is part <strong>of</strong> ACCC’s<br />
Financial Information <strong>and</strong> Learning<br />
Network educational program.<br />
insurance provider to determine the<br />
status <strong>of</strong> your appeal submission <strong>and</strong><br />
can notify you <strong>of</strong> the insurance provider’s<br />
decisions. If the appeals process<br />
does not result in a favorable decision,<br />
after two levels <strong>of</strong> appeal have been<br />
completed or all appeals have been<br />
exhausted, we will review the patient’s<br />
eligibility for the <strong>Patient</strong> <strong>Assistance</strong><br />
Program based on the submitted Application.<br />
If the patient meets eligibility<br />
requirements, replacement vials will be<br />
sent to the provider’s <strong>of</strong>fice for ongoing<br />
therapy.<br />
REIMBURSEMENT ASSISTANCE<br />
Lilly <strong>Patient</strong>One <strong>Reimbursement</strong><br />
Services<br />
Eli Lilly <strong>and</strong> Company recognizes that<br />
medical insurance issues for oncology<br />
patients may be numerous <strong>and</strong> <strong>of</strong>ten<br />
complex. Lilly <strong>Patient</strong>One provides<br />
medical pr<strong>of</strong>essionals, on behalf <strong>of</strong> their<br />
patients, with access to current reimbursement<br />
information <strong>and</strong> support programs.<br />
The resources provided here are<br />
designed to assist providers with some<br />
<strong>of</strong> the complex issues associated with<br />
securing health insurance reimbursement<br />
for their oncology patients. The<br />
purpose <strong>of</strong> this information is to help<br />
ensure accurate coverage, coding, <strong>and</strong><br />
allowable payments for Lilly’s Oncology<br />
products. Tools <strong>of</strong>fered include:<br />
●●<br />
A denied claims checklist: www.<br />
lillypatientone.com/Documents/<br />
MG73325.Checklist.pdf<br />
●●<br />
●●<br />
●●<br />
●●<br />
Attestation statement: www.<br />
lillypatientone.com/Documents/<br />
MG63241.L.Attestation.Statement.<br />
Legal.pdf<br />
Letter <strong>of</strong> Medical Necessity information:<br />
www.lillypatientone.com/<br />
Documents/MG73487.L.6_LOMN.<br />
<strong>Guide</strong>.pdf<br />
First <strong>and</strong> second level appeal letter for<br />
commercial <strong>and</strong> third-party payers:<br />
www.lillypatientone.com/Pages/reimbursement.aspx<br />
First <strong>and</strong> second level Medicare<br />
Review letters: www.lillypatientone.<br />
com/Pages/reimbursement.aspx.<br />
If you have any questions about the<br />
program, please call us at 1.866.4PatOne<br />
(1.866.472.8663) Monday through Friday,<br />
9:00 am-7:00 pm EST.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
EMD Serono<br />
www.emdserono.com<br />
EMD Serono is the biopharmaceutical<br />
division <strong>of</strong> Merck KGaA, Darmstadt,<br />
Germany, a global pharmaceutical <strong>and</strong><br />
chemical group. EMD Serono is growing<br />
its presence in oncology in the U.S, with<br />
a focus on developing novel first-in-class<br />
therapies targeting the cancer disease<br />
process. Their oncology research <strong>and</strong><br />
development focuses on three areas:<br />
●●<br />
●●<br />
●●<br />
The tumor cell<br />
The tumor environment<br />
The immune system.<br />
EMD Serono supports a variety <strong>of</strong> patient<br />
<strong>and</strong> reimbursement assistance programs,<br />
including:<br />
MS Lifelines ® (www.mslifelines.com)<br />
services include:<br />
●●<br />
<strong>Reimbursement</strong> Specialists. The<br />
knowledgeable <strong>and</strong> dedicated team<br />
<strong>of</strong> <strong>Reimbursement</strong> Specialists helps<br />
patients underst<strong>and</strong> their health<br />
insurance coverage <strong>and</strong> options, <strong>and</strong><br />
may also discuss available assistance<br />
programs, including programs <strong>of</strong>fered<br />
by MS LifeLines.<br />
●●<br />
●●<br />
●●<br />
Nurse Support. The MS LifeLines<br />
Nurse Network provides education,<br />
training, <strong>and</strong> support for people with<br />
relapsing MS.<br />
Peer Support. MS LifeLines<br />
Ambassadors are people living with<br />
relapsing MS who want to share<br />
their experiences, <strong>and</strong> can <strong>of</strong>fer hope<br />
<strong>and</strong> encouragement to patients <strong>and</strong><br />
families.<br />
Telephone Support. MS Lifelines<br />
provides 24/7 telephone support.<br />
Call 1.877.447.3243 to speak with a<br />
live representative at any time, day<br />
or night.<br />
Fertility Lifelines<br />
(www.fertilitylifelines.com)<br />
Fertility LifeLines is staffed with highly<br />
trained customer service representatives,<br />
infertility nurses, <strong>and</strong> benefits specialists<br />
ready to assist callers with:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
General infertility information<br />
Insurance benefit verification<br />
Find a fertility specialist tool<br />
EMD Serono product support<br />
Emotional support through compassionate<br />
listening to help put the<br />
patient journey into perspective <strong>and</strong><br />
provide information about additional<br />
support <strong>and</strong> resources.<br />
Call 1.866.LETSTRY(1.866.538.7879)<br />
Monday through Friday, 9:00 am–<br />
5:30 pm EST.<br />
Florida Hospital, Waterman<br />
Cancer Institute, Florida<br />
49<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Genentech, Inc.<br />
www.gene.com<br />
Oncology-related products: Avastin ® (bevacizmuab),<br />
Erivedge (vismodegib), Herceptin ® (trastuzumab), Perjeta<br />
(pertuzumab), Rituxan ® (rituximab), Tarceva ® (erlotinib),<br />
Xeloda ® (capecitabine), Zelboraf ® (vemurafenib)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.genentech-access.com<br />
PATIENT ASSISTANCE<br />
Genentech Access Solutions:<br />
The Genentech Access to Care<br />
Foundation ®<br />
The Genentech Access to Care Foundation<br />
(GATCF) was created to help<br />
patients who are uninsured—or who<br />
have been denied coverage by their<br />
health plans. GATCF might be able to<br />
help those patients receive treatment if<br />
they meet specific financial <strong>and</strong> medical<br />
criteria. For your patient to be eligible<br />
for help from GATCF, certain specific<br />
criteria must be met:<br />
●●<br />
●●<br />
●●<br />
Your patient must have no health<br />
insurance or the health plan has<br />
denied coverage<br />
Your patient’s annual household<br />
adjusted gross income must be<br />
$100,000 or less (special consideration<br />
may be given to patients with<br />
unique circumstances)<br />
Your patient must meet medical<br />
criteria determined by the GATCF<br />
Clinical Advisory Board.<br />
To determine if your patient qualifies,<br />
request a GATCF Eligibility Screening<br />
when you conduct the initial benefits<br />
investigation. To apply to GATCF, providers<br />
must:<br />
✔✔<br />
✔✔<br />
✔✔<br />
Complete <strong>and</strong> submit the Statement<br />
<strong>of</strong> Medical Necessity form: www.<br />
genentech-access.com/sites/default/<br />
files/product-documents/avastin/<br />
Healthcare%20Pr<strong>of</strong>essionals/Statement-<strong>of</strong>-Medical-Necessity_1.pdf<br />
Have the patient complete <strong>and</strong> submit<br />
a <strong>Patient</strong> Authorization <strong>and</strong> Notice <strong>of</strong><br />
Release <strong>of</strong> Information form: www.<br />
genentech-access.com/sites/default/<br />
files/product-documents/avastin/<br />
Healthcare%20Pr<strong>of</strong>essionals/<strong>Patient</strong>-<br />
Authorization-<strong>and</strong>-Notification_1.pdf<br />
Submit the forms online via My<br />
<strong>Patient</strong> Solutions (www.mypatientsolutions.com)<br />
or fax completed forms<br />
to: 888.249.4919.<br />
Once we receive your patient’s information,<br />
GATCF will contact the patient<br />
within 24 hours with further instructions.<br />
50<br />
Mary Bird Perkins Cancer Center, Louisiana<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
This may include verifying financial<br />
eligibility. Note: GATCF has the right to<br />
modify or end this program at any time<br />
<strong>and</strong> to verify the accuracy <strong>of</strong> the information<br />
you submit.<br />
Additional GATCF Program details:<br />
●●<br />
●●<br />
●●<br />
<strong>Patient</strong>s are eligible for free medicine<br />
for one year; patients must reapply<br />
annually<br />
<strong>Patient</strong> assistance support may be<br />
given before treatment or up to one<br />
year post-treatment<br />
GATCF assists with the cost <strong>of</strong> drug<br />
only, not the administration costs.<br />
If you have concerns about your<br />
patient’s insurance coverage for drugs,<br />
ask for a GATCF Eligibility Screening<br />
at the time you submit the Statement <strong>of</strong><br />
Medical Necessity. We can then assess<br />
whether a patient’s medical condition<br />
<strong>and</strong> self-reported income meet GATCF<br />
criteria. If the patient’s insurer denies<br />
coverage after treatment begins, your<br />
patient could be eligible for free drugs<br />
through GATCF. To start the GATCF<br />
Eligibility Screening, check the appropriate<br />
box under Services Requested<br />
on the Statement <strong>of</strong> Medical Necessity<br />
form. Your patient must also certify<br />
that his or her household adjusted gross<br />
income is $100,000 per year or less on<br />
the <strong>Patient</strong> Authorization <strong>and</strong> Notice <strong>of</strong><br />
Release Information form.<br />
A GATCF Eligibility Screening<br />
approval letter does not guarantee<br />
acceptance into GATCF. It only states<br />
that your patient appears to meet the<br />
GATCF medical <strong>and</strong> financial criteria<br />
based on a review <strong>of</strong> the documents.<br />
GATCF still needs to confirm the<br />
complete lack <strong>of</strong> insurance coverage<br />
for Genentech products. This includes<br />
exhausting the appeals process.<br />
GATCF also needs to verify the medical<br />
<strong>and</strong> financial qualifications based<br />
on the documentation supplied by your<br />
patient.<br />
Within 24 hours <strong>of</strong> receiving completed<br />
Statement <strong>of</strong> Medical Necessity<br />
<strong>and</strong> <strong>Patient</strong> Authorization <strong>and</strong> Notice<br />
<strong>of</strong> Release Information forms, Access<br />
Solutions will fax a letter to the provider.<br />
A GATCF Eligibility Screening outcome<br />
notification will follow.<br />
Questions Call Access Solutions<br />
Support Line at: 888. 249.4918. Calls are<br />
taken 6:00 am-5:00 pm PST, Monday<br />
through Friday.<br />
GATCF Extension Program for<br />
Medicare Part D<br />
Administered through GATCF, the<br />
GATCF Extension for Medicare Part D<br />
program provides Erivedge, Tarceva, or<br />
Zelboraf at no cost to financially eligible<br />
patients who have a Medicare Part D plan<br />
<strong>and</strong> who do not qualify for co-pay assistance<br />
from a co-pay assistance foundation.<br />
Please note: <strong>Patient</strong>s must meet the<br />
GATCF medical <strong>and</strong> financial criteria.<br />
Genentech BioOncology Co-pay<br />
Card<br />
Genentech <strong>of</strong>fers the Genentech<br />
BioOncology Co-pay Card to help<br />
qualified patients with the out-<strong>of</strong>-pocket<br />
costs associated with their prescription.<br />
Eligible patients must be 18 years <strong>of</strong><br />
age or older <strong>and</strong> covered by commercial<br />
insurance (non-governmental). <strong>Patient</strong>s<br />
are considered not eligible if they are:<br />
●●<br />
●●<br />
●●<br />
Participating in Medicare, Medicaid,<br />
Medigap, VA, DoD, or TRICARE<br />
(or any other federal- or state-funded<br />
benefit programs, including government<br />
employee programs)<br />
Uninsured (refer to Genentech Access<br />
to Care Foundation or currently<br />
participating in GATCF)<br />
Currently residing or receiving services<br />
in Massachusetts or Vermont.<br />
Eligible patients are responsible for 20<br />
percent <strong>of</strong> the out-<strong>of</strong>-pocket costs for<br />
their Genentech cancer therapy. They<br />
may have access to up to $4,000 over<br />
one year to help with their co-pay.<br />
<strong>Patient</strong>s who make a household income<br />
greater than $100,000 per year have a<br />
yearly limit <strong>of</strong> $1,500. <strong>Patient</strong>s only need<br />
to provide a verbal statement to verify<br />
their income when they enroll. Pro<strong>of</strong><br />
<strong>of</strong> documentation at a later date may<br />
be required. Call 855.MYCOPAY (855.<br />
692.6729) to confirm patient eligibility<br />
<strong>and</strong> activate the card.<br />
Referrals to Co-pay <strong>Assistance</strong><br />
Foundations<br />
If your patients need help with their<br />
medication co-pays, Access Solutions<br />
can connect them to co-pay assistance<br />
foundations supporting their disease<br />
state. Genentech does not influence or<br />
control the operations <strong>of</strong> these co-pay<br />
assistance foundations, but Access Solutions<br />
can assist patients in navigating the<br />
process <strong>of</strong> seeking co-pay assistance by<br />
making an appropriate referral based on<br />
a patient’s diagnosis <strong>and</strong> by assisting with<br />
the application process. We cannot guarantee<br />
co-pay assistance once a patient has<br />
been referred by Access Solutions. The<br />
foundations to which we refer patients<br />
each have their own criteria for patient<br />
eligibility, including financial eligibility.<br />
How it works:<br />
1. <strong>Patient</strong> or caregiver contacts Access<br />
Solutions <strong>and</strong> expresses concerns<br />
about his or her co-pay.<br />
2. An Access Solutions specialist will:<br />
■■<br />
■■<br />
■■<br />
■■<br />
Connect the patient to a co-pay<br />
assistance foundation with available<br />
funding<br />
Support patients throughout the<br />
enrollment process, answering any<br />
questions they might have as they<br />
fill out the application<br />
Notifiy the provider <strong>of</strong> the<br />
patient’s referral to a co-pay assistance<br />
foundation<br />
Reach out to patients to check on<br />
the process.<br />
3. Once the patient informs us that he<br />
or she has been approved, the Access<br />
Solutions specialist informs the physician<br />
<strong>of</strong> the results via fax.<br />
Key points to remember about<br />
co-pay assistance foundations:<br />
●●<br />
For some foundations, approval can<br />
occur in less than 30 days with possible<br />
contingent approval sooner<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
If the patient is denied assistance<br />
by one foundation, he or she can be<br />
referred to a different foundation, if<br />
one is available<br />
Although each foundation <strong>of</strong>fers<br />
some form <strong>of</strong> assistance, it might not<br />
be a full award<br />
The application process might require<br />
some form <strong>of</strong> financial verification<br />
All aspects <strong>of</strong> application processing<br />
can vary by foundation <strong>and</strong> are<br />
determined by each foundation<br />
<strong>Patient</strong>s should be sure to submit the<br />
application <strong>and</strong> required documentation<br />
in a timely manner to avoid<br />
delays or gaps in coverage.<br />
Avastin <strong>Patient</strong> <strong>Assistance</strong> Program<br />
The Avastin <strong>Patient</strong> <strong>Assistance</strong> Program<br />
was developed in response to concerns<br />
about increased costs associated with the<br />
higher doses <strong>of</strong> the new indications the<br />
FDA approved in 2006. By limiting the<br />
51<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
52<br />
overall annual cost <strong>of</strong> Avastin, the program<br />
can help oncologists <strong>and</strong> patients<br />
pursue clinically appropriate on-label<br />
treatment without concern about additional<br />
costs. How the program works:<br />
●●<br />
●●<br />
●●<br />
The program provides an opportunity<br />
for physicians <strong>and</strong> eligible patients<br />
who reach an annual dosage <strong>of</strong><br />
10,000 mg to receive free Avastin<br />
from Genentech for the remainder <strong>of</strong><br />
the 12-month period.<br />
Participation in the program is voluntary.<br />
The treating oncologist identifies<br />
eligible patients for enrollment in the<br />
program.<br />
The treatment year for each patient is<br />
measured independently <strong>and</strong> begins<br />
with the patient’s first infusion.<br />
●●<br />
At the end <strong>of</strong> the patient’s first 12<br />
●●<br />
months <strong>of</strong> therapy, the patient <strong>and</strong>/or<br />
payer resumes financial responsibility<br />
until the 10,000 mg limit is reached in<br />
the next 12 months.<br />
<strong>Patient</strong>s are eligible to receive free<br />
Avastin only if they are treated by<br />
the same provider throughout the<br />
period when the 10,000 mg <strong>of</strong> Avastin<br />
accrues. <strong>Patient</strong>s who change providers<br />
while receiving free Avastin under<br />
the program will be eligible only if<br />
the new location is within the original<br />
provider’s organization.<br />
REIMBURSEMENT ASSISTANCE<br />
Access Solutions Benefits<br />
Investigation<br />
Access Solutions conducts a Benefits<br />
Investigation to help you better underst<strong>and</strong><br />
your patient’s health plan coverage<br />
for some or all <strong>of</strong> the costs associated<br />
with treatment. The investigation can<br />
also determine if a prior authorization or<br />
patient assistance might be needed. To<br />
have Access Solutions conduct an investigation,<br />
request our assistance on the<br />
signed Statement <strong>of</strong> Medical Necessity<br />
form. There are three possible outcomes<br />
<strong>of</strong> a benefits investigation:<br />
●●<br />
●●<br />
●●<br />
Treatment is covered<br />
Prior authorization is required<br />
Treatment is denied.<br />
To begin with Access Solutions, you<br />
must complete <strong>and</strong> submit the Statement<br />
<strong>of</strong> Medical Necessity (www.genentechaccess.com/sites/default/files/productdocuments/avastin/Healthcare%20<br />
Pr<strong>of</strong>essionals/Statement-<strong>of</strong>-Medical-<br />
Necessity_1.pdf) <strong>and</strong> have your patient<br />
complete <strong>and</strong> submit a <strong>Patient</strong> Authorization<br />
<strong>and</strong> Notice <strong>of</strong> Release <strong>of</strong> Information<br />
form (www.genentech-access.com/sites/<br />
default/files/product-documents/avastin/<br />
Healthcare%20Pr<strong>of</strong>essionals/<strong>Patient</strong>-<br />
Authorization-<strong>and</strong>-Notification_1.pdf).<br />
Submit the forms online via My<br />
<strong>Patient</strong> Solutions (www.mypatientsolutions.com)<br />
or fax completed forms to:<br />
888.249.4919. <strong>Patient</strong>s can submit the<br />
<strong>Patient</strong> Authorization <strong>and</strong> Notice <strong>of</strong><br />
Release <strong>of</strong> Information form online at:<br />
https://pan.iassist.com/forms/bioonc.<br />
Access Solutions Prior Authorization<br />
<strong>Assistance</strong><br />
Access Solutions can help providers<br />
identify whether a prior authorization is<br />
needed <strong>and</strong> help them in the process <strong>of</strong><br />
securing it. All we need to begin are a<br />
completed <strong>and</strong> signed Statement <strong>of</strong> Medical<br />
Necessity form requesting our assistance<br />
with the prior authorization, as well<br />
as a signed <strong>and</strong> dated <strong>Patient</strong> Authorization<br />
<strong>and</strong> Notice <strong>of</strong> Release <strong>of</strong> Information<br />
form. Access Solutions can help providers<br />
as they submit the required forms <strong>and</strong><br />
documentation. If the prior authorization<br />
is not granted, Access Solutions can work<br />
with providers to determine the next steps.<br />
Access Solutions Appeals<br />
If your program has prescribed a Genentech<br />
product, but your patient’s insurer<br />
has denied coverage, you can appeal that<br />
decision. Access Solutions might be able<br />
to help providers as they resolve the situation.<br />
Here is what providers can do:<br />
1. Underst<strong>and</strong> why the request or claim<br />
has been denied. This should be in<br />
the insurer’s letter <strong>of</strong> denial or the<br />
patient’s Explanation <strong>of</strong> Benefits<br />
(EOB) letter<br />
2. Contact Access Solutions for guidance<br />
as they put together an appeal.<br />
Use these resources to help them<br />
gather the documents <strong>and</strong> information<br />
they need for a successful appeal<br />
3. Complete <strong>and</strong> submit the required<br />
forms <strong>and</strong> documents to the insurer<br />
before the appeal deadline. Access<br />
Solutions can provide information<br />
about this process.<br />
Questions Call 866.4ACCESS (866.<br />
422.2377) 6:00 am-5:00 pm PST, Monday<br />
through Friday.<br />
My <strong>Patient</strong> Solutions<br />
My <strong>Patient</strong> Solutions (www.mypatientsolutions.com)<br />
connects your program<br />
with our program. We’re available<br />
online to help providers with access <strong>and</strong><br />
reimbursement whenever a Genentech<br />
medicine is prescribed. It’s the most efficient<br />
way to work with Access Solutions<br />
to get patients on therapy as soon as possible.<br />
Features <strong>of</strong> My <strong>Patient</strong> Solutions:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Online enrollment. Prescriber<br />
electronic signatures <strong>and</strong> scanned<br />
document attachments allow for a<br />
completely paperless patient enrollment<br />
process.<br />
Benefits investigation reports. Your<br />
patients’ full benefits investigation<br />
reports are uploaded to My <strong>Patient</strong><br />
Solutions in real time so you can<br />
know exactly what is covered before<br />
beginning treatment.<br />
Search your patient cases. Search<br />
for patient cases initiated via fax or<br />
through My <strong>Patient</strong> Solutions for<br />
easier patient case management.<br />
Genentech Access to Care Foundation<br />
refill requests. Request refills for<br />
GATCF prescriptions online via My<br />
<strong>Patient</strong> Solutions to avoid interruption<br />
in therapy.<br />
Alerts. Get alerts (e.g., Statement<br />
<strong>of</strong> Medical Necessity expiring in<br />
30 days) to learn what actions you<br />
should take to connect your patients<br />
to their medicine. You can opt<br />
to receive these alerts via email<br />
as well.<br />
Information you need to register<br />
your practice. You will need the<br />
following information in order to<br />
successfully register your practice:<br />
1. Primary Genentech products<br />
prescribed by your practice<br />
2. User information including email<br />
addresses (you may add additional<br />
users at a later date)<br />
3. Practice location information (you<br />
may add additional locations at a<br />
later date)<br />
4. Prescriber licensing information,<br />
including a Prescriber National<br />
Provider Identifier <strong>and</strong> State<br />
license number (required).<br />
You will be asked to agree to the My<br />
<strong>Patient</strong> Solutions Practice Agreement.<br />
You must agree to these terms to proceed<br />
with My <strong>Patient</strong> Solutions.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Genomic Health, Inc.<br />
www.genomichealth.com<br />
Oncology-related products: Oncotype DX ® Breast Cancer Assay ® ,<br />
Oncotype DX ® Colon Cancer Assay ®<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.oncotypedx.com<br />
authorized healthcare provider. However,<br />
in the rare cases where all appeals are<br />
exhausted <strong>and</strong> the claim is not fully paid,<br />
the patient will ultimately be responsible<br />
for any balance remaining on the invoice.<br />
Genomic Health provides a comprehensive<br />
financial assistance program for<br />
patients with financial hardship <strong>and</strong> a<br />
program for uninsured <strong>and</strong> underinsured<br />
patients based on financial eligibility.<br />
GAP has been designed to assist<br />
patients <strong>and</strong> authorized healthcare providers<br />
with any billing or reimbursement<br />
issues related to the Oncotype DX test.<br />
Genomic Health welcomes questions<br />
<strong>and</strong> encourages you to contact GAP<br />
if you have questions. Call Genomic<br />
Health Customer Service at:<br />
866.ONCOTYPE (866.662.6897)<br />
or visit: www.oncotypedx.com.<br />
PATIENT ASSISTANCE<br />
Genomic Health provides a comprehensive<br />
financial assistance program for<br />
patients with financial hardship <strong>and</strong> a<br />
program for uninsured <strong>and</strong> underinsured<br />
patients based on financial eligibility.<br />
Call Genomic Health Customer Service<br />
at: 866.ONCOTYPE (866.662.6897) for<br />
more information.<br />
REIMBURSEMENT ASSISTANCE<br />
Genomic Access Program<br />
The Genomic Access Program (GAP)<br />
assists patients throughout the process<br />
<strong>of</strong> determining coverage <strong>and</strong> billing<br />
insurance.<br />
Genomic Health is prepared to<br />
bill insurance plans directly on behalf<br />
<strong>of</strong> insured patients in the U.S. whose<br />
authorized healthcare providers order<br />
the Oncotype DX test. Many insurance<br />
plans have established favorable coverage<br />
policies for the Oncotype DX test for<br />
node-negative, estrogen-receptor-positive<br />
breast cancer patients. These insurance<br />
plans include Medicare, UnitedHealthcare,<br />
CIGNA, Aetna, Kaiser Permanente,<br />
Health Net, Humana, Blue Shield <strong>of</strong><br />
California, WellPoint, <strong>and</strong> many others.<br />
Through GAP, the patient’s authorized<br />
healthcare provider can request a<br />
Benefits Investigation to help determine<br />
if the Oncotype DX test is covered by the<br />
patient’s insurance plan. Some insurers<br />
require a prior authorization before processing<br />
the patient’s specimen; the GAP<br />
team can also help facilitate this process.<br />
If a claim is denied on first review,<br />
the GAP team can assist in appealing<br />
this denial, with input from the patient’s<br />
Cancer Care Northwest, Washington<br />
Take this online course <strong>and</strong> learn the<br />
skills you need to <strong>of</strong>fer financial assistance<br />
services to patients in an efficient<br />
<strong>and</strong> sensitive manner. An experienced<br />
patient advocate discusses:<br />
■■<br />
■■<br />
■■<br />
■■<br />
Financial Counseling 101<br />
Service line assessment. What<br />
financial assistance services does<br />
your program currently <strong>of</strong>fer<br />
What services would your program<br />
like to <strong>of</strong>fer in the future<br />
Strategies for developing<br />
<strong>and</strong>/or growing financial assistance<br />
services.<br />
Process mapping. How to flowchart<br />
your process, including the<br />
steps <strong>and</strong> staff members involved<br />
in providing financial assistance<br />
services. How to look for ways to<br />
improve or streamline processes.<br />
Required job skills for staff<br />
■■<br />
■■<br />
delivering financial assistance<br />
services.<br />
Position descriptions.<br />
Performance metrics. How does<br />
or will your program measure<br />
how financial assistance services<br />
affect quality <strong>of</strong> care, patient <strong>and</strong><br />
provider satisfaction, <strong>and</strong> more.<br />
Register at: www.accc-cancer.org/education/FinancialCounseling-Courses.<br />
asp. This course is part <strong>of</strong> ACCC’s<br />
Financial Information <strong>and</strong> Learning<br />
Network educational program.<br />
53<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
GlaxoSmithKline<br />
www.gsk.com<br />
Oncology-related products: Arranon ® (nelarabine), Arzerra ®<br />
(<strong>of</strong>atumuab), Bexxar ® (tositumomab), Hycamtin ® (topotecan)<br />
capsules, Hycamtin ® (topotecan hydrochloride) for Injection, Leukeran<br />
(chlorambucil), Myleran ® (busulfan), Promacta ® (eltrombopag),<br />
Tykerb ® (lapatinib), Votrient (pazopanib)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.commitmenttoaccess.<br />
com<br />
PATIENT ASSISTANCE<br />
Commitment to Access Program<br />
Commitment to Access is GlaxoSmith-<br />
Kline’s patient assistance program that<br />
provides GSK oncology <strong>and</strong> specialty<br />
pharmacy products—at little or no<br />
cost—to qualified patients. <strong>Patient</strong>s must<br />
meet eligibility criteria to qualify for<br />
assistance. All patients must be enrolled<br />
through an Advocate (i.e., someone such<br />
as a healthcare worker, social worker,<br />
or case worker, who is involved in the<br />
delivery <strong>of</strong> the patient’s healthcare).<br />
■■<br />
■■<br />
■■<br />
3-person household: Total monthly<br />
income $7,954.17 (48 states,<br />
DC, <strong>and</strong> Puerto Rico); $9,945.83<br />
(Alaska); <strong>and</strong> $9,150.00 (Hawaii).<br />
4-person household: Total monthly<br />
income $9,604.17 (48 states, DC,<br />
<strong>and</strong> Puerto Rico); $12,008.33<br />
(Alaska); <strong>and</strong> $11,045.83 (Hawaii).<br />
For each additional person, add:<br />
$1,650.00 (48 states, DC, <strong>and</strong><br />
Puerto Rico); $2,062.50 (Alaska);<br />
<strong>and</strong> $1,895.83 (Hawaii).<br />
Pro<strong>of</strong> <strong>of</strong> income <strong>and</strong> other requested<br />
documents must be submitted along with<br />
the completed <strong>and</strong> signed application.<br />
In addition, a prescription with refills, if<br />
medically appropriate, must be submitted<br />
for mail-order refills.<br />
If the applicant filed income tax or<br />
was listed as a dependent on someone<br />
else’s income tax for the most recently<br />
filed tax year, attach a copy <strong>of</strong> page one<br />
<strong>of</strong> the tax form. If no tax was filed or if<br />
the tax form does not represent current<br />
income, attach pro<strong>of</strong> <strong>of</strong> income from all<br />
sources for the most recent 30-day period<br />
for the applicant <strong>and</strong> all members <strong>of</strong> the<br />
household. Please provide copies, not<br />
original documentation, <strong>of</strong> pay stubs,<br />
unemployment stubs, Social Security<br />
statements, pension statements, <strong>and</strong> any<br />
other sources <strong>of</strong> income. The following<br />
are examples <strong>of</strong> acceptable pro<strong>of</strong> <strong>of</strong><br />
income.<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Income tax form. A copy <strong>of</strong> page<br />
one <strong>of</strong> the most recently filed 1040,<br />
1040A, or 1040EZ.<br />
Salary <strong>and</strong> wages. One month consecutive<br />
salary or wages documentation,<br />
copy <strong>of</strong> pay stub with year-todate<br />
income, letter indicating salary<br />
<strong>and</strong> wages on company letterhead,<br />
notarized statement from employer, or<br />
bank statement showing salaries <strong>and</strong><br />
wages deposited by employer.<br />
Self-employment income. 1099 form,<br />
including Schedule C from the most<br />
recent tax return.<br />
Social Security retirement. Benefit<br />
statement for current year or copy <strong>of</strong><br />
most recent check or check stub.<br />
Supplemental Security Income. Benefit<br />
statement for current year or copy<br />
<strong>of</strong> most recent check or check stub.<br />
Social Security Disability. Benefit<br />
statement for current year or copy <strong>of</strong><br />
most recent check or check stub.<br />
Unemployment. Unemployment<br />
54<br />
To Qualify for Commitment to Access,<br />
<strong>Patient</strong>s:<br />
1. Cannot have prescription drug benefits,<br />
unless the coverage is limited to<br />
generic prescription medicine only<br />
2. Cannot be eligible for Medicaid or<br />
Puerto Rico Government Health Plan<br />
(Reforma)<br />
3. Can be a Medicare Part D participant<br />
who has spent $600 on prescription<br />
medicines this year<br />
4. Must live in one <strong>of</strong> the 50 states, the<br />
District <strong>of</strong> Columbia, or Puerto Rico<br />
5. Must have gross monthly household<br />
income at or below the following:<br />
■■<br />
■■<br />
1-person household: Total monthly<br />
income $4,654.17 (48 states,<br />
DC, <strong>and</strong> Puerto Rico); $5,820.83<br />
(Alaska); <strong>and</strong> $5,358.33 (Hawaii).<br />
2-person household: Total monthly<br />
income $6,304.17 (48 states,<br />
DC, <strong>and</strong> Puerto Rico); $7,883.33<br />
(Alaska); <strong>and</strong> $7,254.17 (Hawaii).<br />
Take this online course <strong>and</strong> learn how<br />
to improve your revenue cycle <strong>and</strong><br />
your cancer program’s bottom line.<br />
An experienced cancer program<br />
administrator <strong>of</strong>fers strategies to:<br />
■■<br />
■■<br />
■■<br />
■■<br />
■■<br />
Evaluating & Improving Your Revenue Cycle<br />
Improve the coding <strong>and</strong> billing<br />
processes.<br />
Improve efficiency within the<br />
revenue cycle, including tips for<br />
submitting clean claims.<br />
Develop a system to track denials<br />
<strong>and</strong> appeals.<br />
Develop <strong>and</strong> manage a drug<br />
replacement program.<br />
Establish a process for data collection.<br />
What information needs<br />
to be collected <strong>and</strong> how Sample<br />
spreadsheets to help track information<br />
related to claims, denials,<br />
appeals, <strong>and</strong> more.<br />
Register at: www.accc-cancer.org/education/FinancialCounseling-Courses.<br />
asp. This course is part <strong>of</strong> ACCC’s<br />
Financial Information <strong>and</strong> Learning<br />
Network educational program.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Gr<strong>and</strong> View Hospital Cancer Program, Pennsylvania<br />
●●<br />
●●<br />
●●<br />
●●<br />
award letter on company letterhead<br />
indicating amount <strong>and</strong> time period<br />
covered or copy <strong>of</strong> most recent unemployment<br />
check or check stub.<br />
Alimony <strong>and</strong> child support. Court<br />
award letter indicating amount <strong>and</strong><br />
time period covered, Child Support<br />
Enforcement Agency letter, letter<br />
from attorney stating amount <strong>and</strong><br />
time period covered, copy <strong>of</strong> one<br />
month’s check, or bank statement<br />
with the amount indicated.<br />
Veterans Benefits. Benefit statement<br />
for current year, copy <strong>of</strong> most<br />
recent bank statement showing direct<br />
deposit, or copy <strong>of</strong> most recent check<br />
or check stub.<br />
Pension <strong>and</strong> retirement earnings.<br />
Benefit statement for current year,<br />
copy <strong>of</strong> most recent bank statement<br />
showing direct deposit, or copy <strong>of</strong><br />
most recent check or check stub.<br />
Other. Benefits statement, award<br />
letter, bank statement from payer or<br />
source, copy <strong>of</strong> check(s), or judgment<br />
statement.<br />
Providers <strong>and</strong> patients can go online to:<br />
www.commitmenttoaccess.com/calculator/do-i-qualify.html<br />
<strong>and</strong> answer a few<br />
short questions to find out whether the<br />
patient may be eligible for Commitment<br />
to Access or another GSK patient assistance<br />
program.<br />
How to Enroll<br />
There are three steps to enrollment.<br />
1. Complete <strong>and</strong> print an online application<br />
at: www.commitmenttoaccess.<br />
com/enrollment/phone-application.<br />
html. Then the Advocate must<br />
call Commitment to Access at<br />
1.8ONCOLOGY1 (1.866.265.6491)<br />
to enroll the patient. Be sure the<br />
patient signs <strong>and</strong> dates the “<strong>Patient</strong><br />
Authorization to Release <strong>and</strong> Disclose<br />
Medical Information” section. Each<br />
application has a unique 9-digit<br />
identification number that serves as<br />
the patient’s Commitment to Access<br />
ID number for as long as the patient<br />
remains in the program. Because the<br />
application has a unique ID number, it<br />
may not be photocopied.<br />
2. Gather income documentation (see<br />
“<strong>Patient</strong> Eligibility”).<br />
3. Select an Advocate. Select someone<br />
involved in healthcare to enroll the<br />
patient into Commitment to Access<br />
by telephone (see “Registering the<br />
Advocate”). The Advocate <strong>and</strong> patient<br />
should review the completed application.<br />
The Advocate will then call<br />
1.8ONCOLOGY1 (1.866.265.6491)<br />
to find out if the patient is eligible to<br />
receive medicine. If eligible, the first<br />
fill <strong>of</strong> medication will automatically<br />
be sent to the address provided on the<br />
application.<br />
Registering the Advocate<br />
Commitment to Access is a program that<br />
requires enrollment by a registered Advocate.<br />
An Advocate is anyone involved in<br />
the delivery <strong>of</strong> a patient’s healthcare, such<br />
as a healthcare provider, social worker, or<br />
case worker. Specifically, Commitment<br />
to Access Advocates:<br />
●●<br />
Help patients obtain, complete, <strong>and</strong><br />
55<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
56<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
sign the enrollment application<br />
Enroll patients by phone<br />
Submit documentation once the<br />
phone enrollment is complete<br />
Order refills for patients if they<br />
require assistance<br />
Look up the patient’s prescription<br />
number<br />
Help patients re-enroll after a year, if<br />
needed<br />
Inform GSK <strong>of</strong> any prescription,<br />
address, or income changes<br />
Follow up with the patient at intervals<br />
as needed by the program.<br />
Advocates must register online at: https://<br />
www.commitmenttoaccess.com/users/<br />
register.html.<br />
How to Re-enroll<br />
<strong>Patient</strong>s need to re-apply to Commitment<br />
to Access every 12 months. Medicare Part<br />
D patients must re-apply each calendar<br />
year. <strong>Patient</strong>s are eligible once they have<br />
spent $600 on prescription medicines. A<br />
re-enrollment application will be mailed to<br />
the Advocate when it is time to re-apply. A<br />
re-enrollment phone call is not necessary.<br />
If the re-enrollment form is lost, another<br />
form can be used, but the <strong>Patient</strong> Identification<br />
Number on the new form must be<br />
crossed out <strong>and</strong> the actual <strong>Patient</strong> Identification<br />
Number must be clearly written.<br />
Receiving Medication<br />
All Commitment to Access medicines<br />
except for Bexxar* are mailed directly to<br />
the provider or patient, based on program<br />
guidelines per medication. In order to<br />
receive medicine by mail, Commitment<br />
to Access must receive the patient<br />
application, income documentation,<br />
<strong>and</strong> a prescription for GlaxoSmithKline<br />
medicine. The Advocate must fax the<br />
prescription (with up to 13 refills if medically<br />
appropriate) to: 1.800.750.9832. The<br />
patient ID number, name, <strong>and</strong> date-<strong>of</strong>birth<br />
must be included.<br />
Upon receipt <strong>and</strong> approval <strong>of</strong> a<br />
completed re-enrollment application,<br />
pro<strong>of</strong> <strong>of</strong> income, <strong>and</strong> a valid prescription,<br />
re-enrollment patients will be authorized<br />
to receive up to 360 days <strong>of</strong> additional<br />
medicine, shipped in 30-day increments.<br />
*Bexxar distribution is h<strong>and</strong>led<br />
through the BEXXAR Service Center.<br />
Advocates enrolling Bexxar patients will<br />
be advised how to obtain Bexxar at the<br />
time <strong>of</strong> enrollment.<br />
Ordering Refills<br />
To order refills, call 1.8ONCOLOGY1<br />
(1.866.265.6491). The Advocate or the<br />
patient can request refills for oral tablets;<br />
IV drug refills must be requested by<br />
the Advocate. Be sure to order refills at<br />
least two weeks before the patient runs<br />
out <strong>of</strong> medicine or 7-10 days before the<br />
next treatment. Refills will not be sent<br />
automatically. Refills are sent at no cost<br />
for up to 12 months after enrollment in<br />
Commitment to Access. Refills can be<br />
sent to the provider’s <strong>of</strong>fice or directly<br />
to the patient’s home based on program<br />
guidelines per medication.<br />
If re-enrollment patients are determined<br />
eligible for continued assistance<br />
through Commitment to Access, the<br />
first fill will automatically be sent to the<br />
address provided on the application. The<br />
patient <strong>and</strong> the Advocate should continue<br />
to order refills as needed by calling<br />
1.8ONCOLOGY1 (1.866.265.6491) at<br />
least two weeks before the medicine supply<br />
runs out or 7-10 days before the next<br />
scheduled treatment. Refills will not be<br />
sent automatically.<br />
<strong>Patient</strong>s Taking Arzerra ®<br />
<strong>Patient</strong>s with prescription drug benefits<br />
through Medicare Part B or through<br />
a commercial plan may be eligible for<br />
Commitment to Access when they have<br />
a co-payment that exceeds $2,000,<br />
subject to the criteria listed above.<br />
Advocates may call 1.8ONCOLOGY1<br />
(1.866.265.6491) for more information.<br />
Co-Pay <strong>Assistance</strong><br />
This program is for people who have<br />
prescription coverage but who need<br />
extra help paying for their oral medicine.<br />
<strong>Patient</strong>s may qualify for co-pay<br />
assistance if they have commercial<br />
prescription drug coverage <strong>and</strong> live in<br />
one <strong>of</strong> the 50 States or the District <strong>of</strong><br />
Columbia (excluding residents <strong>of</strong> Massachusetts).<br />
<strong>Patient</strong>s who: 1) have come to<br />
the United States seeking healthcare <strong>and</strong><br />
live outside the United States; 2) have<br />
insurance coverage through a government-funded<br />
program, such as Medicare<br />
or Medicaid; <strong>and</strong> 3) are enrolled in a<br />
health plan that does not permit members<br />
to participate in co-pay assistance<br />
programs are not eligible.<br />
<strong>Patient</strong> co-pay amounts are dependent<br />
on household income. <strong>Patient</strong>s are<br />
responsible for paying the approved<br />
co-pay amount for each fill <strong>of</strong> the qualifying<br />
GSK medicine as listed below:<br />
●●<br />
0% to 250% <strong>of</strong> FPL, patient pays $25<br />
●●<br />
251% to 500% <strong>of</strong> FPL, patient pays<br />
$50<br />
●●<br />
More than 500% FPL: Not eligible for<br />
co-pay assistance.<br />
For updated co-pay information call:<br />
1.888.663.4752. Applicants with<br />
co-payments or coinsurance that<br />
exceeds 50% will be responsible for<br />
any remaining costs not covered by<br />
their insurance plan or GSK Co-Pay<br />
<strong>Assistance</strong> Program.<br />
REIMBURSEMENT ASSISTANCE<br />
CARES by GSK<br />
CARES by GSK (www.caresbygsk.<br />
com) <strong>of</strong>fers a variety <strong>of</strong> reimbursement<br />
services, including:<br />
●●<br />
Verification <strong>of</strong> benefits. <strong>Reimbursement</strong><br />
counselors will verify coverage<br />
for patients with all types <strong>of</strong><br />
insurance, including Medicare,<br />
Medicaid, private payers, Veterans<br />
Affairs/VHA, TRICARE, AIDS<br />
drug assistance programs, children’s<br />
health insurance programs, state<br />
elderly drug assistance programs,<br />
<strong>and</strong> other state <strong>and</strong> local payers<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Prior authorization assistance.<br />
Counselors can help patients<br />
proactively overcome obstacles to<br />
accessing treatment by researching<br />
prior authorization requirements for<br />
payer-restricted drugs<br />
Coding <strong>and</strong> billing assistance.<br />
Counselors are available to answer<br />
questions about HCPCS, CPT, <strong>and</strong><br />
ICD-9-CM codes for all applicable<br />
oncology medications<br />
Coverage analysis. Counselors can<br />
research <strong>and</strong> provide patients with<br />
detailed coverage information, including<br />
a co-pay forecast<br />
Denied <strong>and</strong> underpaid claims<br />
assistance. Counselors can research<br />
denied <strong>and</strong> underpaid claims to<br />
confirm that they were processed<br />
appropriately<br />
Case management. Counselors<br />
can research foundations <strong>and</strong> assess<br />
eligibility for GSK’s patient assistance<br />
programs<br />
Researching specialty pharmacies.<br />
Counselors will research specialty<br />
pharmacies that <strong>of</strong>fer low co-pays.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Incyte Corporation<br />
www.incyte.com<br />
Oncology-related products: Jakafi ® (ruxolitinib) tablets<br />
✔✔<br />
✔✔<br />
The amount <strong>of</strong> the co-pay, if it is<br />
known.<br />
Household income. If the patient has<br />
a pay stub, tax return, or disability<br />
form, have it on h<strong>and</strong>.<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.incytecares.com<br />
<strong>Patient</strong> <strong>Assistance</strong><br />
Uninsured <strong>Patient</strong>s<br />
The IncyteCARES (Connecting to<br />
Access, <strong>Reimbursement</strong>, Education <strong>and</strong><br />
Support) patient assistance program helps<br />
people who don’t have a healthcare plan.<br />
It can also help people whose plans have<br />
turned them down for Jakafi treatment. If<br />
patients qualify, they may be able to get<br />
Jakafi for free. To qualify for financial<br />
support through IncyteCARES, patients<br />
must meet the following criteria:<br />
●●<br />
No prescription drug coverage or a<br />
healthcare plan that has said it won’t<br />
pay for Jakafi <strong>and</strong> an appeal was<br />
turned down<br />
●●<br />
●●<br />
●●<br />
Earn less than $100,000 per year or<br />
up to 500% <strong>of</strong> the FPL, based on<br />
household size<br />
Be a U.S. resident<br />
Use <strong>of</strong> Jakafi is FDA-approved.<br />
Call 1.855.4.Jakafi (1.855.452.5234),<br />
Monday through Friday, 8:00 am<br />
to 5:00 pm, to learn more about<br />
IncyteCARE’s patient assistance program.<br />
Co-pay <strong>Assistance</strong><br />
<strong>Patient</strong>s with private or commercial<br />
prescription insurance may be eligible to<br />
receive Jakafi for no more than $50 per<br />
month, depending upon their income.<br />
To qualify for co-pay assistance through<br />
IncyteCARES, patients must meet the<br />
following criteria:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Commercially or privately insured<br />
Earn less than $100,000 per year or<br />
up to 500% <strong>of</strong> the FPL, based on<br />
household size<br />
Be a U.S. resident<br />
Use <strong>of</strong> Jakafi is FDA-approved.<br />
Call 1.855.4.Jakafi (1.855.452.5234),<br />
Monday through Friday, 8:00 am<br />
PeaceHealth Southwest Regional<br />
Cancer Center, Vancouver,<br />
Washington<br />
to 5:00 pm, to learn more about<br />
IncyteCARE’s co-pay assistance program.<br />
Referral to an INO<br />
IncyteCARE may also refer patients with<br />
Medicare Part D plan or other type <strong>of</strong><br />
insurance to an independent, nonpr<strong>of</strong>it<br />
organization (INO). The INO can find<br />
ways to help patients with the co-pay.<br />
Each INO has its own set <strong>of</strong> rules. While<br />
IncyteCARES does not influence or<br />
control the INOs, it can help patients<br />
through the process <strong>of</strong> applying for help<br />
from an INO. IncyteCARES can also<br />
refer patients to the INO <strong>of</strong>fering the best<br />
help for them. IncyteCARES can find out<br />
if patients qualify for federal help.<br />
To apply to an INO, patients should<br />
gather the following information:<br />
✔✔<br />
The medical condition <strong>and</strong> the drug<br />
the doctor wants the patient to use, in<br />
this case Jakafi.<br />
✔✔<br />
✔✔<br />
The doctor’s name, address, telephone<br />
number, <strong>and</strong> fax number.<br />
The patient’s healthcare plan information.<br />
Have the insurance card ready.<br />
If the patient has more than one<br />
healthcare plan, have all the information<br />
ready.<br />
If IncyteCARES refers a patient to an<br />
INO, they will need to fill out an application.<br />
Here are some questions patients<br />
might want to ask the INO to get started:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
How long does the approval process<br />
take after the application is received<br />
How will I be told if I am approved<br />
for or denied help from you<br />
Will my doctor also be told what you<br />
decide<br />
If I am approved, where are the<br />
payments sent<br />
For how many months can I expect<br />
to receive this help<br />
Each application requires patients to<br />
verify their financial needs. It can take<br />
from 2 weeks to 30 days for an INO to<br />
review your application. If the patient is<br />
turned down by one INO, IncyteCARES<br />
can refer the patient to another. However,<br />
IncyteCARE’s role is limited to making<br />
referrals for patients. IncyteCARES does<br />
not control the process. Nor does it control<br />
the decision the INO might make.<br />
<strong>Patient</strong> Education & Support<br />
IncyteCARE’s patient education <strong>and</strong><br />
support include:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Education information to help teach<br />
patients about MF <strong>and</strong> Jakafi<br />
<strong>Patient</strong> Starter Packet<br />
IncyteCARE’s Welcome Packet<br />
Access to trained nurse pr<strong>of</strong>essionals.<br />
Visit www.incytecares.com to learn<br />
more.<br />
REIMBURSEMENT ASSISTANCE<br />
Access & <strong>Reimbursement</strong> Services<br />
Incyte provides the following services:<br />
●●<br />
Benefit verification<br />
●●<br />
Prior authorization<br />
●●<br />
Appeal support<br />
●●<br />
Jakafi delivery information<br />
●●<br />
Co-pay assistance<br />
●●<br />
Free medication.<br />
Call 1.855.4.Jakafi (1.855.452.5234),<br />
Monday through Friday, 8:00 am<br />
to 5:00 pm, to learn more about<br />
IncyteCARE’s reimbursement services.<br />
57<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Janssen Biotech<br />
www.janssenbiotech.com<br />
Oncology-related products: Doxil ® (doxorubicin HCl liposome<br />
injection), Procrit ® (epoetin alfa), Zytiga ® (abiraterone acetate)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.janssenaccessone.com<br />
PATIENT ASSISTANCE<br />
access2wellness ®<br />
If a patient does not have coverage for<br />
Doxil, Procrit, or Zytiga, this program<br />
can be the gateway to assistance for eligible<br />
patients that meet specific medical<br />
<strong>and</strong> financial criteria. Reach an access-<br />
2wellness specialist at: 866.317.2775,<br />
Monday through Friday, 9:00 am to<br />
5:00 pm EST. Providers can also help<br />
patients determine their eligibility<br />
<strong>and</strong> the programs that are right for<br />
them with the tools available at: www.<br />
access2wellness.com. Here are tips to<br />
help you get started.<br />
Online Process<br />
1. Use the online Eligibility Tool (www.<br />
access2wellness.com/a2w/hcp-helping.html)<br />
to determine your patient’s<br />
eligibility to receive prescription<br />
medicines.<br />
2. If your patient appears to qualify<br />
for the Johnson & Johnson <strong>Patient</strong><br />
<strong>Assistance</strong> Foundation, a link to the<br />
online application will be provided in<br />
the Eligibility Tool results.<br />
3. Help your patient fill out the patient<br />
portion <strong>of</strong> the application. Fill out<br />
the prescriber’s portion <strong>and</strong> click<br />
SUBMIT.<br />
4. A representative will contact both<br />
you <strong>and</strong> your patient to complete the<br />
application process.<br />
5. A program specialist will review the<br />
application <strong>and</strong> a determination will<br />
be made within several days.<br />
6. If your patient appears to qualify for<br />
58<br />
R<strong>and</strong>olph Cancer Center,<br />
North Carolina<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
programs other than the Johnson &<br />
Johnson <strong>Patient</strong> <strong>Assistance</strong> Foundation,<br />
links to program websites <strong>and</strong><br />
Call Centers may also be provided.<br />
Paper Application Process<br />
(Note: The following process only<br />
applies to the Johnson & Johnson <strong>Patient</strong><br />
<strong>Assistance</strong> Foundation.)<br />
1. Print the Johnson & Johnson <strong>Patient</strong><br />
<strong>Assistance</strong> Foundation application. It<br />
is available online at: www.jjpaf.org/<br />
resources/jjpaf-application.pdf.<br />
2. Help your patient fill out the patient<br />
portion <strong>of</strong> the application <strong>and</strong> fill out<br />
your portion.<br />
3. Be certain your patient has included<br />
a copy <strong>of</strong> his or her Federal Income<br />
Tax Return when applicable, <strong>and</strong><br />
an “Authorization to Share Health<br />
Information for <strong>Patient</strong> <strong>Assistance</strong>”<br />
(included with application), signed by<br />
the patient.<br />
4. Mail the completed application to:<br />
Johnson & Johnson <strong>Patient</strong> <strong>Assistance</strong><br />
Foundation, PO Box 221857,<br />
Charlotte, NC 28222-1857. You<br />
can also fax the application to:<br />
888.526.5168.<br />
5. After the application is received, it is<br />
reviewed <strong>and</strong> a determination is made<br />
within several days. Note: Incomplete<br />
applications <strong>of</strong>ten cause delays. For<br />
information on issues that may cause<br />
delay, visit our Frequently Asked<br />
Questions at: www.access2wellness.<br />
com/a2w/hcp-faq.html.<br />
REIMBURSEMENT ASSISTANCE<br />
Accessone ®<br />
This reimbursement portal (www.<br />
janssenaccessone.com) <strong>of</strong>fers general<br />
reimbursement information <strong>and</strong> news.<br />
By clicking on a product logo, providers<br />
can access drug-specific reimbursement<br />
information.<br />
The information provided represents<br />
no statement, promise, or guarantee by<br />
Janssen Products, LP, concerning levels <strong>of</strong><br />
reimbursement. Please consult your payer<br />
organizations with regard to local or actual<br />
coverage <strong>and</strong> reimbursement policies <strong>and</strong><br />
determination processes.<br />
DOXILine<br />
(www.janssenaccessone.com/pages/doxil/<br />
index.jsp)<br />
This website provides easy access to<br />
reimbursement information <strong>and</strong> support<br />
including:<br />
●●<br />
Benefit verification. An online benefit<br />
verification form is available online<br />
at: www.janssenaccessone.com/<br />
assets/doxil/benefit.verification.pdf.<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Prior authorization research.<br />
Appeal process <strong>and</strong> procedure<br />
research.<br />
Alternate sources <strong>of</strong> payment.<br />
General billing <strong>and</strong> coding questions.<br />
Information regarding patient<br />
assistance.<br />
Under the “Helpful Resources” button<br />
(www.janssenaccessone.com/pages/doxil/<br />
pubs/publications.jsp), providers can<br />
access publications <strong>and</strong> toolkits for billing<br />
pr<strong>of</strong>essionals to help with reimbursement<br />
issues, including:<br />
●●<br />
●●<br />
●●<br />
●●<br />
A reimbursement overview.<br />
A reimbursement toolkit (www.<br />
janssenaccessone.com/pages/doxil/<br />
pubs/tool/onc.jsp) where providers<br />
can download tools to help prepare<br />
claims. A sample Evaluation<br />
<strong>and</strong> Management Progress Note is<br />
available online at: www.janssenaccessone.com/pages/doxil/pubs/tool/<br />
emp.jsp. A sample chemotherapy<br />
treatment notes/flow sheet is available<br />
online at: www.janssenaccessone.<br />
com/pages/doxil/pubs/tool/ctn.jsp.<br />
Full prescribing information.<br />
Online reimbursement <strong>and</strong> healthcare<br />
resources that provide links to medical<br />
<strong>and</strong> journal sites, Medicare Part A<br />
fiscal intermediaries, Medicare Part<br />
B Carrier sites, payer directories, <strong>and</strong><br />
more.<br />
For more information, call 1.800.609.1083,<br />
Monday through Friday, 8:00 am to<br />
8:00 pm EST.<br />
PROCRITline<br />
(www.janssenaccessone.com/pages/procrit/patientassist/intro.jsp)<br />
This website provides easy access to<br />
reimbursement information <strong>and</strong> support<br />
including:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Benefit verification. An online benefit<br />
verification form is available online<br />
at: www.janssenaccessone.com/<br />
assets/procrit/benefit.verification.pdf<br />
Prior authorization research<br />
Appeal process <strong>and</strong> procedure<br />
research<br />
Alternate sources <strong>of</strong> payment<br />
●●<br />
●●<br />
General billing <strong>and</strong> coding<br />
questions<br />
Information regarding patient<br />
assistance.<br />
Under the “Helpful Resources” button<br />
(http://www.janssenaccessone.com/<br />
pages/procrit/pubs/publications.jsp),<br />
providers can access publications <strong>and</strong><br />
toolkits for billing pr<strong>of</strong>essionals to help<br />
with reimbursement issues, including:<br />
●●<br />
●●<br />
●●<br />
●●<br />
A reimbursement overview<br />
Articles on current topics in Medicare<br />
reimbursement<br />
Reference guides to ICD-9-CM<br />
Diagnosis Codes<br />
Full prescribing information.<br />
ZytigaOne Support<br />
(www.janssenaccessone.com/pages/<br />
zytiga/index.jsp)<br />
This website provides easy access to<br />
reimbursement information <strong>and</strong> support<br />
including:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
ZytigaOne Support <strong>Patient</strong> Brochure<br />
(www.janssenaccessone.com/assets/<br />
zytiga/<strong>Patient</strong>_Brochure.pdf).<br />
ZytigaOne Support Provider Brochure<br />
(www.janssenaccessone.com/<br />
assets/zytiga/Provider_Brochure.<br />
pdf).<br />
ZytigaOne Instant Savings Program<br />
Flashcard (www.janssenaccessone.<br />
com/assets/zytiga/instant_savings.<br />
pdf).<br />
ZytigaOne Support Enrollment Form<br />
(www.janssenaccessone.com/assets/<br />
zytiga/PEF.pdf). This form combines<br />
the benefit investigation request,<br />
patient authorization, ZytigaOne<br />
support enrollment, <strong>and</strong> prescription<br />
information into one form.<br />
A sample letter <strong>of</strong> medical necessity<br />
(www.janssenaccessone.com/assets/<br />
zytiga/Sample_LMN.pdf).<br />
Specialty pharmacy information<br />
(www.janssenaccessone.com/assets/<br />
zytiga/SPP.pdf). This is a list <strong>of</strong><br />
specialty pharmacy provider phone<br />
numbers for you to use as a resource<br />
for therapy with Zytiga. It includes<br />
a listing <strong>of</strong> key services provided by<br />
ZytigaOne Support.<br />
A Business Associate Agreement<br />
(www.janssenaccessone.com/assets/<br />
zytiga/BAA.pdf). Use this Janssen<br />
Biotech, Inc. Support System HIPAA<br />
Business Associate Agreement to be<br />
HIPAA compliant.<br />
59<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Merck<br />
www.merck.com<br />
Oncology-related products: Emend ® (aprepitant), Emend ®<br />
(fosaprepitant dimeglumine) for Injection, Emend ® (fosaprepitant<br />
dimeglumine) for Injection, Intron ® A (interferon alfa-2b, recombinant)<br />
for Injection, Sylatron(peginterferon alfa-2b) for Injection, Temodar ®<br />
(temozolomide), Temodar ® (temozolomide) for Injection, Zolinza<br />
(vorinostat)<br />
Vaccine: Gardasil (Quadrivalent Human Papillomavirus Recombinant<br />
Vaccine)<br />
3. Take the completed application to the<br />
provider. Both the provider <strong>and</strong> the<br />
patient must sign the application.<br />
4. When complete, fax the enrollment<br />
application to: 866.363.6389.<br />
Providers <strong>and</strong> patients can also call the<br />
ACT Program at: 1.866.363.6379 to<br />
request a brochure <strong>and</strong> enrollment form.<br />
ACT Program Specialists are available<br />
Monday through Friday from 8:00 am to<br />
8:00 pm EST to answer questions about<br />
the program.<br />
60<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.merck.com/merckhelps<br />
PATIENT ASSISTANCE<br />
The ACT Program<br />
This program provides free reimbursement<br />
support services to help answer<br />
questions related to insurance coverage<br />
<strong>and</strong> reimbursement. The ACT Program<br />
also refers patients to patient assistance<br />
programs, which provide certain medicines<br />
free <strong>of</strong> charge to eligible individuals,<br />
primarily the uninsured, who cannot<br />
afford their Merck medicines. Many<br />
Merck medicines are included in this<br />
program. A partial list <strong>of</strong> Merck medicines<br />
follows. Call The ACT Program at<br />
1.866.363.6379 for the full list <strong>of</strong> covered<br />
products.<br />
●●<br />
Emend (aprepitant)<br />
●●<br />
Emend (fosaprepitant dimeglumine)<br />
for Injection<br />
●●<br />
Intron A (interferon alfa-2b, recombinant)<br />
for Injection<br />
●●<br />
Sylatron (peginterferon alfa-2b)<br />
●●<br />
Temodar (temozolomide)<br />
●●<br />
Zolinza (vorinostat).<br />
<strong>Patient</strong> <strong>Assistance</strong> for Eligible <strong>Patient</strong>s<br />
Program Specialists can also help<br />
providers apply for the patient assistance<br />
program that provides certain Merck<br />
medicines free <strong>of</strong> charge to eligible<br />
patients who do not have insurance<br />
coverage. <strong>Patient</strong>s may qualify for patient<br />
assistance if they meet all three <strong>of</strong> the<br />
following conditions:<br />
1. They are a U.S. resident <strong>and</strong> have a<br />
prescription for a Merck medicine<br />
from a doctor licensed in the United<br />
States.<br />
2. They do not have insurance or other<br />
coverage for their prescription<br />
medicine.<br />
3. They cannot afford to pay for their<br />
medicine. They may qualify for the<br />
patient assistance program if they<br />
have a household income <strong>of</strong> $55,850<br />
or less for individuals, $75,650 or less<br />
for couples, or $115,250 or less for a<br />
family <strong>of</strong> four.<br />
At Merck we realize that sometimes<br />
exceptions need to be made based on<br />
the patient’s individual circumstances.<br />
<strong>Patient</strong>s that do not meet the prescription<br />
drug coverage criteria <strong>and</strong> whose income<br />
meets the program criteria <strong>and</strong> who have<br />
special circumstances <strong>of</strong> financial <strong>and</strong><br />
medical hardship that apply to their<br />
situation can request that an exception<br />
be made.<br />
Enrollment<br />
ACT Program Specialists can help<br />
providers <strong>and</strong> patients answer questions<br />
related to insurance coverage <strong>and</strong> reimbursement.<br />
They can also explain program<br />
requirements <strong>and</strong> available options.<br />
The patient <strong>and</strong> the healthcare provider<br />
must complete an enrollment form. In<br />
brief, here are enrollment instructions:<br />
1. Download the enrollment application<br />
at: www.merck.com/merckhelps/pdf/<br />
ACT_Enrollment_Form.pdf (English)<br />
<strong>and</strong> www.merck.com/merckhelps/<br />
pdf/El_Programa_ACT_espanol.pdf<br />
(Spanish).<br />
2. Complete all information on the<br />
application form. <strong>Patient</strong>s can fill in<br />
the fields online <strong>and</strong> print or they may<br />
print the form <strong>and</strong> fill it out by h<strong>and</strong><br />
using a black ballpoint pen.<br />
Merck Co-Pay <strong>Assistance</strong> Program<br />
This program is available to eligible,<br />
privately insured patients who may need<br />
help affording their co-pay on certain<br />
Merck oncology medicines. If patients<br />
have been prescribed one <strong>of</strong> the Merck<br />
medicines included in the program <strong>and</strong><br />
they are privately insured, they may be<br />
eligible for the Merck Co-Pay <strong>Assistance</strong><br />
Program if they meet the full program<br />
criteria. A partial list <strong>of</strong> Merck medicines<br />
covered in this program include:<br />
●●<br />
●●<br />
●●<br />
●●<br />
Intron A (interferon alfa-2b,<br />
recombinant) for Injection<br />
Sylatron (peginterferon alfa-2b)<br />
for Injection<br />
Temodar (temozolomide)<br />
Zolinza (vorinostat).<br />
Selected criteria for Merck’s Co-Pay<br />
<strong>Assistance</strong> Program includes:<br />
●●<br />
The program is not available for all<br />
Merck products. Call the number<br />
below to find out if the medicine<br />
the patient has been prescribed is<br />
included.<br />
●●<br />
●●<br />
●●<br />
●●<br />
<strong>Patient</strong>s must meet the program’s<br />
income eligibility criteria.<br />
Financial assistance is not transferable.<br />
It cannot be combined with any<br />
coupon, free trial, discount, prescription<br />
savings card, or other form <strong>of</strong><br />
patient assistance.<br />
Financial assistance is not insurance.<br />
The Merck Co-Pay Program is valid<br />
for patients with private insurance. It<br />
is not valid for cash-paying patients<br />
or patients covered under Medicaid,<br />
Medicare, a Medicare Part D or<br />
Medicare Advantage Plan (regardless<br />
<strong>of</strong> whether a specific prescription<br />
is covered), TRICARE, CHAM-<br />
PUS, Puerto Rico Government<br />
Health Insurance Plan (“Healthcare<br />
Reform”), or any other state or federal<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Take this online course <strong>and</strong> learn how<br />
<strong>of</strong>fering financial assistance services<br />
can improve the patient (<strong>and</strong> provider)<br />
experience. An experienced cancer<br />
program administrator outlines<br />
strategies for:<br />
■■<br />
■■<br />
■■<br />
Improving how patients move<br />
through your cancer program.<br />
Flow chart the patient experience<br />
<strong>and</strong> look for ways to improve or<br />
streamline services.<br />
Developing patient <strong>and</strong> provider<br />
education materials.<br />
Marketing financial assistance<br />
services to increase referrals from<br />
primary care physicians.<br />
medical or pharmaceutical benefit<br />
program or pharmaceutical patient<br />
assistance program.<br />
Not valid for residents <strong>of</strong><br />
Massachusetts.<br />
The program can only be used by<br />
eligible U.S. or Commonwealth <strong>of</strong><br />
Puerto Rico residents at participating<br />
eligible retail or mail-order pharmacies<br />
in the United States or the Commonwealth<br />
<strong>of</strong> Puerto Rico. Product<br />
must originate in the United States or<br />
the Commonwealth <strong>of</strong> Puerto Rico.<br />
Merck reserves the right to rescind,<br />
revoke, or amend the <strong>of</strong>fer at any time<br />
without notice.<br />
Financial assistance is provided for up<br />
to 12 months <strong>of</strong> therapy. If necessary,<br />
patients must reapply for assistance<br />
annually.<br />
The program may not cover all <strong>of</strong> the<br />
patient’s out-<strong>of</strong>-pocket expenses.<br />
It is illegal to sell, purchase, or trade,<br />
or <strong>of</strong>fer to sell, purchase, or trade the<br />
financial assistance. Void where prohibited<br />
by law, taxed, or restricted.<br />
There is no guarantee funding will be<br />
R<strong>and</strong>olph Cancer Center, North Carolina<br />
Improving the <strong>Patient</strong> Experience<br />
■■<br />
■■<br />
available in any subsequent year or<br />
timeframe.<br />
Visit www.merck.com/product/ to view<br />
<strong>Patient</strong> Information <strong>and</strong> discuss with<br />
your patient. For full program criteria or<br />
more information, call 855.263.1774.<br />
Vaccine <strong>Patient</strong> <strong>Assistance</strong> Program<br />
<strong>Patient</strong>s who want to receive the Gardasil<br />
vaccine may be eligible for the program<br />
if all three <strong>of</strong> the following conditions<br />
apply:<br />
●●<br />
●●<br />
●●<br />
Marketing financial assistance<br />
services to patients <strong>and</strong> families.<br />
Measuring patient <strong>and</strong> provider<br />
satisfaction with these services.<br />
Register at: www.accc-cancer.org/education/FinancialCounseling-Courses.<br />
asp. This course is part <strong>of</strong> ACCC’s<br />
Financial Information <strong>and</strong> Learning<br />
Network educational program.<br />
<strong>Patient</strong>s reside in the U.S. <strong>and</strong> are age<br />
19 or older. (Note: <strong>Patient</strong>s do not<br />
have to be U.S. citizens.)<br />
<strong>Patient</strong>s have no health insurance<br />
coverage. (Some examples <strong>of</strong> health<br />
insurance coverage include private<br />
insurance, HMOs, PPOs, college<br />
health plans, Medicaid, Veterans’’<br />
assistance, or any other social service<br />
agency support.)<br />
<strong>Patient</strong>s have an annual household<br />
income less than: $44,680 for individuals,<br />
$60,520 for couples, or $92,200<br />
for a family <strong>of</strong> four. (For income<br />
limits in Alaska, Hawaii, Puerto Rico,<br />
U.S. Virgin Isl<strong>and</strong>s, <strong>and</strong> Guam, please<br />
call 1.800. 293.3881.)<br />
Enrollment is easy.<br />
1. Complete <strong>and</strong> sign the application<br />
form. It is available online at: www.<br />
merck.com/merckhelps/vaccines/<br />
mvpap_app.pdf (English) <strong>and</strong> www.<br />
merck.com/merckhelps/vaccines/<br />
mvpap_app_span.pdf (Spanish).<br />
Providers <strong>and</strong> their <strong>of</strong>fice personnel<br />
can also call 800.293.3881 to obtain<br />
enrollment applications for patients<br />
<strong>and</strong> to request additional information<br />
about the program.<br />
2. Fax the completed form to:<br />
800.528.2551 from a participating<br />
licensed provider’s <strong>of</strong>fice. The application<br />
must be submitted <strong>and</strong> approved<br />
prior to administration <strong>of</strong> vaccine<br />
in order to qualify. Forms will be<br />
processed quickly—with a goal <strong>of</strong> less<br />
than 10 minutes—<strong>and</strong> the provider’s<br />
<strong>of</strong>fice will be notified by phone so that<br />
qualifying patients can receive the<br />
Merck vaccine during that visit.<br />
3. A new application will need to be<br />
completed <strong>and</strong> submitted to the<br />
Merck Vaccine <strong>Patient</strong> <strong>Assistance</strong><br />
Program for eligibility assessment<br />
prior to a patient receiving a subsequent<br />
dose in a multi-dose series or<br />
for another Merck vaccine.<br />
REIMBURSEMENT ASSISTANCE<br />
The ACT Program<br />
The ACT Program assists providers with<br />
insurance coverage <strong>and</strong> reimbursement<br />
questions. ACT Program Specialists can<br />
help providers answer questions related to<br />
insurance coverage <strong>and</strong> reimbursement.<br />
Services include:<br />
●●<br />
Researching medical insurance <strong>and</strong><br />
prescription plan benefits<br />
●●<br />
Verifying out-<strong>of</strong>-pocket costs<br />
●●<br />
Conducting searches for other sources<br />
<strong>of</strong> assistance<br />
●●<br />
Referring individuals to patient<br />
assistance programs.<br />
For additional information <strong>and</strong> reimbursement<br />
support, call the ACT Program<br />
at 866.363.6379, Monday through<br />
Friday, 8:00 am to 8:00 pm EST.<br />
The ACT Program does not guarantee<br />
either coverage or a specific reimbursement<br />
rate for any Merck medicine.<br />
61<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Millennium: The Takeda Oncology Company<br />
www.millennium.com<br />
Oncology-related Product: Velcade ® (bortezomib)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.velcade-hcp.com/<br />
reimbursement<br />
<strong>Patient</strong> <strong>Assistance</strong><br />
If a patient has no insurance coverage for<br />
Velcade, he or she may be eligible to participate<br />
in the company’s <strong>Patient</strong> <strong>Assistance</strong><br />
Program. For patients who qualify<br />
for the program, free Velcade product<br />
will be delivered to their healthcare<br />
pr<strong>of</strong>essionals. For patients with denied<br />
insurance coverage, please contact your<br />
dedicated Velcade <strong>Reimbursement</strong> <strong>Assistance</strong><br />
Program (VRAP) case manager by<br />
calling 866.VELCADE (866.835.2233)<br />
<strong>and</strong> choosing option 2 to inquire about<br />
potential product replacement.<br />
Enrollment Process<br />
<strong>Patient</strong>s who do not have insurance<br />
coverage for Velcade must apply for<br />
assistance through their healthcare<br />
pr<strong>of</strong>essionals. To demonstrate eligibility,<br />
they must complete an enrollment form<br />
<strong>and</strong> provide income documentation, as<br />
well as health insurance information. The<br />
form is available online at: www.velcade-<br />
hcp.com/reimbursement/forms/VEL-<br />
CADE_VRAP_Enrollment_Form.pdf.<br />
You can also receive the enrollment form<br />
by calling 866.VELCADE (866.835.2233)<br />
<strong>and</strong> choosing option 2. It is strongly recommended<br />
that you enroll patients into<br />
the <strong>Patient</strong> <strong>Assistance</strong> Program prior to<br />
the start <strong>of</strong> their treatment with Velcade.<br />
All enrollment forms must be received<br />
within six months <strong>of</strong> the first treatment<br />
for complete assistance.<br />
Enrollment Assessment<br />
VRAP will respond by telephone within<br />
two business days to any completed<br />
enrollment application. A follow-up letter<br />
explaining the determination will be<br />
sent to the healthcare pr<strong>of</strong>essional. If the<br />
patient qualifies, your dedicated case manager<br />
will contact your <strong>of</strong>fice to schedule a<br />
shipment <strong>of</strong> the first cycle <strong>of</strong> Velcade.<br />
Enrollment Management<br />
One week prior to every cycle, your<br />
dedicated case manager will contact you<br />
to confirm that the patient will continue<br />
to receive Velcade <strong>and</strong> that the patient’s<br />
information remains unchanged. <strong>Patient</strong>s<br />
are eligible to participate in the <strong>Patient</strong><br />
<strong>Assistance</strong> Program for 12 months if they<br />
remain qualified. If they are still receiving<br />
Velcade after 12 months, they will<br />
need to re-enroll in the program.<br />
62<br />
Four Steps to Access Velcade<br />
1. Talk to Your <strong>Patient</strong>s. Discuss any questions<br />
patients may have regarding treatment <strong>and</strong><br />
the impact it will have on their out-<strong>of</strong>-pocket<br />
expenses. You are a resource for patients<br />
regarding what to expect from their treatment<br />
<strong>and</strong> how different treatment regimens may be<br />
impacted by their insurance coverage. You can<br />
also refer patients to other useful resources.<br />
2. Provide Insurance Information. Make sure<br />
that you have your patient’s current insurance<br />
information so that you can verify coverage.<br />
Research your patient’s insurance coverage to<br />
determine if Velcade will be covered, if additional<br />
documentation will need to be submitted<br />
to the insurance company, <strong>and</strong> how much<br />
patients will need to pay for their treatment<br />
based on their insurance plan. If the patient’s<br />
insurance covers Velcade, move on to the<br />
payment <strong>and</strong> scheduling processes outlined in<br />
steps 3 <strong>and</strong> 4. If the insurance company requests<br />
additional information, you may need to submit<br />
a letter stating the reason(s) why your patient<br />
should be treated with Velcade. The insurance<br />
company will notify both you <strong>and</strong> your patient<br />
about their decision. If coverage is approved,<br />
move on to the payment <strong>and</strong> scheduling processes<br />
outlined in steps 3 <strong>and</strong> 4. If the patient’s<br />
insurance company requests additional information<br />
<strong>and</strong> does not approve treatment based on<br />
what you have provided, then you may be able to<br />
get assistance through the Velcade <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Program (VRAP).<br />
3. Underst<strong>and</strong> the Payment Process. Depending<br />
on the patient’s specific insurance coverage,<br />
his or her out-<strong>of</strong>-pocket expense will vary. It<br />
is important to help your patients underst<strong>and</strong><br />
these details, <strong>and</strong> to know where they can<br />
go for help. Ensure that your patients know<br />
exactly what dollar amount they are going to<br />
be responsible for paying, according to their<br />
insurance policy.<br />
4. Schedule the Treatment. Once you have<br />
helped your patient determine how he or she<br />
will be able to pay for Velcade, schedule the<br />
treatment. Velcade is given as a 3- to 5-second<br />
IV injection in a doctor’s <strong>of</strong>fice or at a hospital<br />
outpatient clinic.<br />
Source: www.velcade.com.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Reimbursment <strong>Assistance</strong><br />
The Velcade <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Program<br />
Today’s economy has made it more<br />
challenging than ever for patients receiving<br />
therapy. Millennium Pharmaceuticals,<br />
Inc., underst<strong>and</strong>s that challenge <strong>and</strong><br />
has responded with an enhanced Velcade<br />
<strong>Reimbursement</strong> <strong>Assistance</strong> Program<br />
service model.<br />
●●<br />
●●<br />
One-to-one support model. You<br />
now have a dedicated case manager<br />
waiting for your call. Millennium has<br />
invested in a dedicated case manager<br />
model so that, each time you call, you<br />
will be assisted by the same person.<br />
Targeted solutions. <strong>Patient</strong>s’ needs<br />
differ significantly, depending on<br />
many factors. The “one-to-one” support<br />
model allows case managers to be<br />
experts at identifying resources that<br />
are specific to the state, county, or city<br />
in which your patient either lives or<br />
receives therapy. Increasing dem<strong>and</strong><br />
on the national resources available to<br />
patients makes it more important than<br />
ever to identify available resources for<br />
a patient. Whether a patient’s need is<br />
related to a complex prior authorization<br />
process or identifying viable transportation<br />
resources, your “one-to-one”<br />
case manager is waiting to help.<br />
When healthcare providers, patients, or<br />
caregivers call VRAP, dedicated case<br />
managers are available to answer<br />
questions <strong>and</strong> provide helpful information.<br />
For more information, call 866.<br />
VELCADE (866.835.2233) <strong>and</strong> choose<br />
option 2. VRAP services are available<br />
Monday through Friday, from 8:00 am<br />
to 8:00 pm EST. Information can also be<br />
mailed or faxed to the provider’s <strong>of</strong>fice or<br />
the home <strong>of</strong> a patient or caregiver.<br />
●●<br />
●●<br />
●●<br />
any questions you have about coding<br />
<strong>and</strong> billing for Velcade, provide you<br />
with sample claim forms, <strong>and</strong> help<br />
you track <strong>and</strong> monitor claim forms.<br />
Claim appeals support. Identify<br />
reasons for underpayment or denial<br />
<strong>of</strong> claims, contact insurers to gather<br />
information about the appeal process,<br />
<strong>and</strong> assist you in developing an appeal<br />
strategy, including sample letters <strong>of</strong><br />
medical necessity <strong>and</strong> appeal. (Note:<br />
VRAP does not file claims or appeal<br />
claims for callers, nor can it guarantee<br />
that you will be successful in obtaining<br />
reimbursement.)<br />
Alternate funding searches. Determine<br />
additional sources <strong>of</strong> support for<br />
uninsured <strong>and</strong> underinsured patients<br />
on Velcade <strong>and</strong> assist in the application<br />
process.<br />
Transportation resources. Identify<br />
transportation resources for patients<br />
on Velcade.<br />
Velcade.com for Healthcare<br />
Pr<strong>of</strong>essionals<br />
As part <strong>of</strong> the enhanced Velcade <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Program, you<br />
can also find Velcade reimbursement<br />
information online at: www.velcade.com/<br />
payingfortreatment.aspx. The healthcare<br />
pr<strong>of</strong>essional reimbursement section<br />
<strong>of</strong>fers tools that will help you navigate<br />
the healthcare coverage environment for<br />
Velcade, including:<br />
●●<br />
●●<br />
Coverage. Find information about<br />
Medicare, Medicaid, <strong>and</strong> private<br />
payer coverage for Velcade.<br />
Payment for Velcade. Learn about<br />
the payment methodologies used<br />
by different payers to determine<br />
reimbursement for Velcade.<br />
●●<br />
●●<br />
Coding. Find information on coding<br />
claims for Velcade.<br />
A Forms Library. Download sample<br />
claims forms <strong>and</strong> letters, including:<br />
1. A Quick Reference <strong>Guide</strong><br />
containing information for<br />
payer coding <strong>and</strong> payment<br />
information for Velcade at: www.<br />
velcade-hcp.com/reimbursement/<br />
forms/QRG_PI.pdf.<br />
2. Sample CMS-1500 Claim Form at:<br />
www.velcade-hcp.com/reimbursement/forms/CMS-1500_withPI.pdf.<br />
3. Sample CMS-1450 (UB-04) Claim<br />
Form at: www.velcade-hcp.com/<br />
reimbursement/forms/CMS-1450_<br />
withPI.pdf.<br />
4. Sample Letter Supporting Medical<br />
Necessity for Velcade at: www.<br />
velcade-hcp.com/reimbursement/<br />
formslibrary_ form_3.aspx.<br />
5. Sample Letter Appealing a<br />
Denied Claim for Velcade at:<br />
www.velcade-hcp.com/reimbursement/forms/Appeal_withPI.pdf.<br />
6. Sample Letter to Obtain Consistent<br />
Medicare Coverage at: www.<br />
velcade-hcp.com/reimbursement/<br />
forms/Obtain_withPI.pdf.<br />
Velcade.com for Your <strong>Patient</strong>s<br />
At www.velcade.com, you will also find<br />
reimbursement information for your<br />
patients, including:<br />
●●<br />
●●<br />
●●<br />
Health insurance coverage <strong>and</strong> payment<br />
options for Velcade<br />
The coverage process from the<br />
patient’s perspective<br />
Questions to ask their doctor’s <strong>of</strong>fice.<br />
<strong>Reimbursement</strong><br />
Trained reimbursement case managers<br />
are available to provide timely <strong>and</strong> accurate<br />
information <strong>and</strong> services, including:<br />
●●<br />
●●<br />
●●<br />
Insurance verification. Verify health<br />
insurance coverage <strong>and</strong> eligibility for<br />
each patient being treated with<br />
Velcade, facilitate the prior authorization<br />
process, <strong>and</strong> determine any<br />
co-payment obligations.<br />
Research payer policies. Provide published<br />
policies for public <strong>and</strong> private<br />
payers.<br />
Coding <strong>and</strong> billing support. Discuss<br />
63<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Novartis Pharmaceuticals Corporation<br />
64<br />
www.novartisoncology.com<br />
Oncology-related products: Oncology-related products: Afinitor ®<br />
(everolimus tablets), Exjade ® (deferasirox), Femara ® (letrozole<br />
tablets), Gleevec ® (imatinib mesylate) tablets, S<strong>and</strong>ostatin LAR ®<br />
Depot (octreotide acetate for injectable suspension), S<strong>and</strong>ostatin ®<br />
(octreotide acetate for injection), Tasigna ® (nilotinib) tablets, <strong>and</strong><br />
Zometa ® (zoledronic acid) Injection<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.patientassistancenow.<br />
com<br />
PATIENT ASSISTANCE<br />
The Novartis <strong>Patient</strong> <strong>Assistance</strong><br />
Foundation<br />
The Novartis <strong>Patient</strong> <strong>Assistance</strong> Foundation<br />
(PAF) provides assistance to patients<br />
experiencing financial hardship who<br />
have no third-party insurance coverage<br />
for their medicines. To be eligible for<br />
the Novartis PAF, patients must:<br />
●●<br />
Be a U.S. resident<br />
●●<br />
Meet income criteria, which vary<br />
by medication, <strong>and</strong> provide pro<strong>of</strong> <strong>of</strong><br />
income. Financial eligibility program<br />
requirements are 250% to 500% <strong>of</strong><br />
the Federal Poverty Level (FPL),<br />
depending on the Novartis Medicine.<br />
The Federal Poverty Level defines the<br />
minimum yearly income that a person<br />
or family needs in order to provide<br />
for its basic needs. It is adjusted each<br />
year by the Department <strong>of</strong> Health<br />
<strong>and</strong> Human Services (HHS). This<br />
level dictates a set <strong>of</strong> guidelines for<br />
use for administrative purposes—for<br />
instance, determining financial eligibility<br />
for certain federal programs.<br />
●●<br />
Not have private or public prescription<br />
coverage. (Note: There is an<br />
exception process for patients who<br />
cannot afford their Medicare Part D<br />
or B cost share.)<br />
<strong>Patient</strong>s must reapply <strong>and</strong> requalify<br />
annually. Questions Contact the<br />
Novartis <strong>Patient</strong> <strong>Assistance</strong> Foundation<br />
at: 800.277.2254 or go online to: www.<br />
patientassistancenow.com.<br />
Enrolling in the PAF is quick <strong>and</strong><br />
easy. To provide the best possible<br />
customer service, we recommend that<br />
the provider or patient call our hotline.<br />
Providers or patients will be asked a few<br />
qualifying questions to determine patient<br />
eligibility for the program. To get started,<br />
call 1.800.277.2254 <strong>and</strong> select the appropriate<br />
phone prompts. (Please note: for<br />
patients prescribed Exjade, the provider<br />
Skagit Valley Hospital Regional<br />
Cancer Care Center, Washington<br />
or patient should call the EPASSnPrescription<br />
<strong>and</strong> <strong>Reimbursement</strong> Hotline at:<br />
1.888.903.7277.)<br />
If the patient appears to be eligible<br />
based on the initial phone screening,<br />
PAF will provide a temporary supply <strong>of</strong><br />
medication <strong>and</strong> an application will be<br />
mailed directly to the patient’s home.<br />
Once received, the provider <strong>and</strong> patient<br />
must complete the first four sections<br />
<strong>of</strong> the application. Include the patient’s<br />
signature, the date, a copy <strong>of</strong> the patient’s<br />
most recent federal tax return, <strong>and</strong> a copy<br />
<strong>of</strong> his or her insurance card/prescription<br />
card, if applicable. The provider must<br />
complete <strong>and</strong> sign the lower portion <strong>of</strong><br />
the enrollment application.<br />
Applications are available online<br />
at: www.pharma.us.novartis.com/cs/<br />
groups/public/@nph_us_it/documents/<br />
contentpage/n_int_050277.pdf (English)<br />
<strong>and</strong> www.pharma.us.novartis.com/cs/<br />
groups/public/@nph_us_it/documents/<br />
contentpage/n_int_050278.pdf (Spanish).<br />
Completed applications should be<br />
faxed to: 1.866.277.9335 or mailed to:<br />
Novartis Oncology <strong>Patient</strong> <strong>Assistance</strong><br />
Program, PO Box 6655, St. Louis, MO<br />
63166-6559. Once received, we will<br />
assess for full eligibility for the patient<br />
assistance program. Qualified individuals<br />
are eligible for up to one year <strong>of</strong> assistance,<br />
or until a prescription drug benefit<br />
becomes available. Upon approval, up<br />
to a year supply <strong>of</strong> medication will<br />
be shipped directly to the provider or<br />
patient.<br />
<strong>Patient</strong> <strong>Assistance</strong> NOW Oncology<br />
(www.oncologyaccessnow.com/index.jsp)<br />
Novartis <strong>Patient</strong> <strong>Assistance</strong> NOW<br />
Oncology (PANO) <strong>of</strong>fers quick <strong>and</strong> easy<br />
access to information about the many<br />
reimbursement <strong>and</strong> support programs<br />
available. PANO helps you underst<strong>and</strong><br />
the issues, options, <strong>and</strong> requirements<br />
pertinent to patients’ access to therapies,<br />
with:<br />
●●<br />
●●<br />
<strong>Patient</strong> access to treatment<br />
Provider portals to access PANO<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Total Yearly Income Range<br />
Onyx Pharmaceuticals<br />
66<br />
www.onyx.com<br />
Oncology-related products: Kyprolis ® (carfilzomib) for Injection,<br />
Nexavar ® (sorafenib) tablets (co-marketed with Bayer HealthCare<br />
Pharmaceuticals, Inc.<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.onyx.com/therapies/<br />
patient-access/onyx-360<br />
PATIENT ASSISTANCE<br />
Onyx 360<br />
This comprehensive, personalized<br />
program is designed to support providers<br />
<strong>and</strong> patients in their health journey by<br />
providing services <strong>and</strong> referrals that meet<br />
their individual needs, including:<br />
●●<br />
Free product assistance for uninsured<br />
patients or those rendered uninsured<br />
through payer denial <strong>and</strong> who meet<br />
●●<br />
●●<br />
certain income eligibility criteria<br />
Referral to transportation assistance<br />
services for those patients who<br />
qualify <strong>and</strong> need assistance paying<br />
for gas, lodging, tolls, <strong>and</strong> parking<br />
in connection with receiving therapy<br />
Referral to support services for<br />
patients, families, <strong>and</strong> caregivers that<br />
provide product information, local<br />
transportation to scheduled appointments,<br />
support group information,<br />
nutritional information, <strong>and</strong> side<br />
effect management, along with practical<br />
matters related to the patient’s<br />
condition.<br />
Download <strong>and</strong> complete the enrollment<br />
form at: www.onyx.com/file.<br />
cfm/623/docs/5608%20Enrollment%20<br />
Form_Corp_Web_Version_0712-<br />
ONYX-109_072312.pdf. Please see<br />
required information below for each<br />
Reporting Financial <strong>Assistance</strong> Processes <strong>and</strong><br />
Data Back to Internal Stakeholders<br />
Take this online course <strong>and</strong> learn how<br />
to identify <strong>and</strong> collect the right data<br />
to ensure your program is delivering<br />
high-quality <strong>and</strong> efficient financial<br />
assistance services. An experienced<br />
quality <strong>and</strong> improvement manager<br />
shares how to:<br />
■■<br />
■■<br />
■■<br />
Identify data sets to track <strong>and</strong><br />
report back to stakeholders, such<br />
as percent <strong>of</strong> charity care, costs<br />
<strong>of</strong> drugs obtained through drug<br />
replacement programs, <strong>and</strong> more<br />
Forecast the number <strong>of</strong> patients<br />
that may need financial assistance<br />
services<br />
Forecast the revenue (drug<br />
replacement) or savings (reduced<br />
bad debt, write-<strong>of</strong>fs, <strong>and</strong> charity<br />
care) that financial assistance<br />
services may bring to the cancer<br />
program<br />
■■<br />
Develop a process for tracking<br />
metrics, including the number <strong>of</strong><br />
patients that use these services,<br />
revenues <strong>and</strong> cost-savings,<br />
improvements in patient compliance,<br />
<strong>and</strong> improved patient <strong>and</strong><br />
provider satisfaction.<br />
Register at: www.accc-cancer.org/education/FinancialCounseling-Courses.<br />
asp. This course is part <strong>of</strong> ACCC’s<br />
Financial Information <strong>and</strong> Learning<br />
Network educational program.<br />
requested service. Failure to include all<br />
information will delay the process.<br />
For insurance verification:<br />
✔✔<br />
Complete sections 1, 2, <strong>and</strong> 3<br />
✔✔<br />
Physician signature is required<br />
✔✔<br />
Fax a copy <strong>of</strong> the front <strong>and</strong> back <strong>of</strong><br />
the patient’s insurance card with the<br />
enrollment form.<br />
For free product assistance:<br />
✔✔<br />
Complete sections 1, 2, 3, 4, <strong>and</strong> 5<br />
✔✔<br />
<strong>Patient</strong>’s financial documentation will<br />
be required (i.e., most recent 1040<br />
federal tax return, W-2, or social<br />
security statement)<br />
✔✔<br />
Physician <strong>and</strong> patient signatures are<br />
required.<br />
For co-pay assistance (for eligible<br />
patients):<br />
✔✔<br />
Complete sections 1, 2, <strong>and</strong> 3<br />
✔✔<br />
Physician <strong>and</strong> patient signatures are<br />
required.<br />
For referrals to transportation cost<br />
assistance:<br />
✔✔<br />
Complete sections 1 <strong>and</strong> 2<br />
✔✔<br />
<strong>Patient</strong> signature is required.<br />
For referral to patient support services:<br />
✔✔<br />
Complete sections 1, 2, <strong>and</strong> 5<br />
✔✔<br />
<strong>Patient</strong> signature is required.<br />
Please fax completed forms to Onyx 360<br />
at: 1.855.669.9329. Upon submission <strong>of</strong><br />
the enrollment form to Onyx 360, an<br />
oncology nurse advocate will confirm<br />
receipt with the provider <strong>and</strong> initiate<br />
the services requested on behalf <strong>of</strong> the<br />
patient(s). Questions Oncology nurse<br />
advocates are available Monday through<br />
Friday, from 9:00 am to 8:00 pm EST<br />
at 1.855.ONYX.360 (1.855.669.9360)<br />
to help guide providers <strong>and</strong> patients<br />
through the specifics <strong>of</strong> the program(s)<br />
<strong>and</strong> answer any questions.<br />
REIMBURSEMENT ASSISTANCE<br />
Onyx 360 provides the following reimbursement<br />
assistance to providers:<br />
●●<br />
Co-pay <strong>and</strong> co-insurance assistance<br />
●●<br />
Comprehensive insurance verification<br />
●●<br />
Prior authorization <strong>and</strong> appeals<br />
process support.<br />
To learn more about these services, call:<br />
1.855.ONYX.360 (1.855.669.9360).<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Pfizer Oncology<br />
www.pfizer.com<br />
Oncology-related products: Aromasin ® (exemestane tablets),<br />
Bosulif ® (bosutinib) tablets, Camptosar ® (irinotecan HCI injection),<br />
Ellence ® (epirubicin hydrochloride injection), Emcyt ® (estramustine<br />
phosphate sodium capsules), Idamycin ® (idarubicin hydrochloride<br />
for injection, USP), Inlyta ® (axitinib) tablets, Neumega ® (oprelvekin),<br />
Sutent ® (sunitinib malate), Torisel ® (temsirolimus) injection, Xalkori ®<br />
(crizotinib) capsules, Zinecard ® (dexrazoxane for injection)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.pfizerhelpfulanswers.<br />
com<br />
Pfizer Helpful Answers<br />
Pfizer Helpful Answers is a family <strong>of</strong><br />
assistance programs for people who have<br />
no insurance, or who do not have enough<br />
insurance <strong>and</strong> need help getting their<br />
Pfizer medicines. Programs may provide:<br />
●●<br />
●●<br />
Pfizer medicines for free or at a savings<br />
to patients who qualify<br />
<strong>Reimbursement</strong> support services to<br />
insured patients.<br />
If your patient is uninsured or underinsured<br />
<strong>and</strong> would like more information<br />
about Pfizer Helpful Answers<br />
assistance programs, call us toll-free at:<br />
1.866.706.2400, or view all assistance<br />
programs online at: www.pfizerhelpfulanswers.com/pages/Find/FindAll.aspx.<br />
PATIENT ASSISTANCE<br />
Uninsured <strong>Patient</strong>s<br />
Pfizer First Resource ® <strong>of</strong>fers reimbursement<br />
support services <strong>and</strong> patient<br />
assistance to help patients gain access to<br />
Pfizer oncology medicines. If the patient<br />
qualifies, the program can also provide<br />
co-pay assistance for certain medicines.<br />
A Pfizer First Resource counselor will<br />
help confirm if a patient is eligible for<br />
assistance, <strong>and</strong> can guide the provider<br />
<strong>and</strong> patient through the enrollment process.<br />
Download the Pfizer First Resource<br />
brochure (pfizerhelpfulanswers.com/<br />
files/First%20Resource%20Brochure_<br />
Sutent%20PI_Final%20File_9_27_11.<br />
pdf) for more information on how this<br />
program can help you.<br />
To receive free medicines, patients must:<br />
●●<br />
Have no prescription coverage or not<br />
enough coverage<br />
●●<br />
Meet specific income guidelines,<br />
adjusted for family size<br />
●●<br />
Live in the United States, the U.S.<br />
Virgin Isl<strong>and</strong>s, or Puerto Rico<br />
●●<br />
Be treated by a licensed doctor in the<br />
United States or Puerto Rico.<br />
The following medicines are available<br />
through the First Resource program:<br />
Aromasin (exemestane tablets)<br />
Bosulif (bosutinib) tablets<br />
Camptosar (irinotecan HCI<br />
injection)<br />
Ellence (epirubicin hydrochloride<br />
injection)<br />
Emcyt (estramustine phosphate<br />
sodium capsules)<br />
Idamycin (idarubicin hydrochloride<br />
for injection, USP)<br />
Inlyta (axitinib) tablets<br />
Neumega (oprelvekin)<br />
Sutent (sunitinib malate)<br />
Torisel (temsirolimus) injection<br />
Xalkori (crizotinib) capsules<br />
Zinecard (dexrazoxane for injection).<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Enrollment Instructions<br />
To apply to First Resource:<br />
●●<br />
Download First Resource IV application<br />
online in English (www.pfizerhelpfulanswers.com/files/9565_FirstResourceIV_rev8.pdf)<br />
or Spanish<br />
(www.pfizerhelpfulanswers.com/<br />
files/14634_FirstResource2IV_Sp.pdf)<br />
or call 1.877.744.5675 to begin the<br />
enrollment process. First Reach counselors<br />
are available Monday through<br />
Friday, 9:00 am to 8:00 pm EST <strong>and</strong><br />
<strong>of</strong>fer assistance in English or Spanish.<br />
●●<br />
Download First Resource oral<br />
application online at: www.pfizerhelpfulanswers.com/files/FirstResource_English%20Oral%20App.<br />
●●<br />
pdf or call 1.877.744.5675 to begin the<br />
enrollment process.<br />
The provider <strong>and</strong> patient must fill out<br />
<strong>and</strong> fax or mail the completed application,<br />
along with pro<strong>of</strong> <strong>of</strong> income for<br />
continued assistance (if approved),<br />
to 1.800.708.3430, or to: Pfizer First<br />
Resource PO Box 220582 Charlotte,<br />
NC 28222-0582. Pro<strong>of</strong> <strong>of</strong> income<br />
includes copies <strong>of</strong> one <strong>of</strong> the following<br />
documents that show a patient’s<br />
total gross annual household income:<br />
current paycheck stub; federal tax<br />
return for the prior tax year (Form<br />
1040 or 1040EZ); wage <strong>and</strong> tax statements<br />
(W2 form); Social Security,<br />
pension, or railroad retirement<br />
statements (SSA-1099 or similar); <strong>and</strong><br />
statements <strong>of</strong> interest, dividends, or<br />
other income (1099-INT, 1099, 1099-<br />
DIV, or other forms).<br />
Pro<strong>of</strong> <strong>of</strong> income includes copies <strong>of</strong> one <strong>of</strong><br />
the following documents that show total<br />
gross annual household income:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Current paycheck stub<br />
Federal tax return (Form 1040 or<br />
1040EZ) for the prior tax year<br />
Wage <strong>and</strong> tax statements (W-2 forms)<br />
Social Security, pension, or railroad<br />
retirement statements (SSA-1099 or<br />
similar)<br />
Statements <strong>of</strong> interest, dividends,<br />
or other income (1099-INT, 1099,<br />
1099-DIV or other forms).<br />
If you do not have any pro<strong>of</strong> <strong>of</strong> income,<br />
please call us at 1.866.706.2400.<br />
Insured <strong>Patient</strong>s<br />
For patients with prescription drug<br />
coverage, First Resource can provide the<br />
following benefits:<br />
●●<br />
●●<br />
●●<br />
<strong>Reimbursement</strong> support services. A<br />
First Resource counselor will research<br />
<strong>and</strong> verify patient benefits for the<br />
medicine needed, explain coverage<br />
options <strong>and</strong> policies, <strong>and</strong> investigate<br />
<strong>and</strong> explain the prior authorization<br />
process.<br />
Alternate funding assistance. First<br />
Resource can help providers <strong>and</strong><br />
patients find alternate sources <strong>of</strong><br />
funding if necessary. These may<br />
include state pharmaceutical assistance<br />
programs, Medicaid, Medicare<br />
Part D, low-income subsidies, <strong>and</strong><br />
charitable foundations.<br />
Appeals process information. If a<br />
67<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
68<br />
●●<br />
●●<br />
claim is underpaid or denied, First<br />
Resource will investigate <strong>and</strong> explain<br />
the appeals process.<br />
Specialty pharmacy referral. If<br />
patients are insured <strong>and</strong> have been<br />
prescribed Xalkori or Inlyta, First<br />
Resource will refer them to an appropriate<br />
specialty pharmacy that can fill<br />
the prescription.<br />
Hardship assistance. If patients have<br />
prescription coverage but are experiencing<br />
significant financial hardship<br />
(e.g., cannot afford their co-pay or<br />
coinsurance), they may be eligible to<br />
receive their Pfizer medicine for free,<br />
or obtain a Co-Pay Card that will<br />
cover the full cost <strong>of</strong> their co-pay.<br />
Pfizer Pfriends<br />
Regardless <strong>of</strong> age <strong>and</strong> income, if patients<br />
qualify, a Pfizer Pfriends card can<br />
<strong>of</strong>fer savings on many br<strong>and</strong>ed Pfizer<br />
medicines at participating pharmacies.<br />
To receive a savings on Pfizer medicines<br />
through the program, patients must:<br />
●●<br />
●●<br />
Have no prescription coverage<br />
Live in the United States, Puerto<br />
Rico, or the U.S. Virgin Isl<strong>and</strong>s.<br />
To apply to Pfizer Pfriends:<br />
1. Download an application online at:<br />
www.pfizerhelpfulanswers.com/files/<br />
PP_English.pdf (English) or www.<br />
pfizerhelpfulanswers.com/files/PP_<br />
Spanish.pdf (Spanish). Providers <strong>and</strong><br />
Lake Region Healthcare, Cancer Care<br />
<strong>and</strong> Research Center, Minnesota<br />
patients can also request applications<br />
by calling 1.866.706.2400.<br />
2. Complete the application, which covers<br />
the entire family. Pro<strong>of</strong> <strong>of</strong> income<br />
is not required.<br />
The application will be processed in two<br />
to three weeks. If approved, patients will<br />
receive a welcome kit in the mail. This<br />
kit includes the Pfizer Pfriends savings<br />
card(s). <strong>Patient</strong>s can begin using their<br />
savings card(s) at participating pharmacies<br />
when filling their prescriptions for<br />
Pfizer medicines. To find a participating<br />
pharmacy, go to: www.pfizerhelpfulanswers.com/pages/Programs/PharmacyLocator.html.<br />
To continue receiving Pfizer Pfriends<br />
program benefits, patients must reapply<br />
each year.<br />
●●<br />
●●<br />
●●<br />
REIMBURSEMENT ASSISTANCE<br />
Pfizer First Resource<br />
Through Pfizer’s First Resource Program,<br />
providers can access the following<br />
services:<br />
●●<br />
<strong>Reimbursement</strong> support services.<br />
A First Resource counselor can help<br />
patients <strong>and</strong> healthcare pr<strong>of</strong>essionals<br />
underst<strong>and</strong> coverage <strong>and</strong> reimbursement<br />
options. This includes benefits<br />
verification, in which the counselor<br />
will review patients’ benefits to see<br />
how they are covered for the medicines<br />
they need. They’ll also explain<br />
coverage options <strong>and</strong> policies, as well<br />
as investigate <strong>and</strong> explain the prior<br />
authorization process.<br />
Alternate funding assistance. First<br />
Resource can help patients find<br />
alternate sources <strong>of</strong> funding if they<br />
need them. These may include state<br />
pharmaceutical assistance programs,<br />
Medicaid, Medicare Part D, lowincome<br />
subsidies, <strong>and</strong> charitable<br />
foundations.<br />
Appeals process information. If a<br />
claim is underpaid or denied, First<br />
Resource will investigate <strong>and</strong> explain<br />
the appeals process.<br />
Specialty pharmacy referral.<br />
Xalkori (crizotinib) capsules or Inlyta<br />
(axitinib) tablets will be available only<br />
through select specialty pharmacies.<br />
A First Resource counselor can help<br />
patients who have been prescribed<br />
Xalkori or Inlyta get connected to the<br />
specialty pharmacy appropriate for<br />
their insurance plan. The specialty<br />
pharmacy will then conduct a benefits<br />
verification to determine coverage<br />
options <strong>and</strong> the process to receive<br />
Xalkori or Inlyta. Note: Services vary<br />
by product <strong>and</strong> eligibility.<br />
Pfizerpro.com<br />
PfizerPro (www.pfizerpro.com) provides<br />
access to current product information as<br />
well as patient education <strong>and</strong> assistance<br />
programs for Pfizer’s prescription<br />
medicines. When providers register with<br />
PfizerPro.com they gain access to pr<strong>of</strong>essional<br />
resources, including:<br />
●●<br />
Epocrates ®<br />
●●<br />
●●<br />
●●<br />
●●<br />
The 5-Minute Clinical Consult<br />
MedPage Today ® Medical News<br />
Journal Reprints<br />
Pfizer Medical Information.<br />
Note: Some restrictions may apply.<br />
Providers also gain access to patient<br />
education <strong>and</strong> assistance, including:<br />
Pfizer Samples for Eligible Health<br />
Care Pr<strong>of</strong>essionals<br />
A.D.A.M. Quicksheets<br />
Printed Literature Requests<br />
Pfizer Helpful Answers.<br />
●●<br />
●●<br />
●●<br />
●●<br />
Plus, additional product-exclusive<br />
programs <strong>and</strong> other <strong>of</strong>ferings that may<br />
help you better serve your practice <strong>and</strong><br />
patients.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
ProStrakan<br />
www.prostrakan-usa.com<br />
Oncology-related <strong>and</strong> supportive care products: Fareston ®<br />
(toremifene citrate); Sancuso ® (granisetron transdermal system)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.patientrxsolutions.com<br />
<strong>Patient</strong> <strong>Assistance</strong><br />
Uninsured <strong>Patient</strong>s<br />
Our <strong>Patient</strong> <strong>Assistance</strong> Program was<br />
designed to assist uninsured individuals<br />
<strong>and</strong> those who have no public or private<br />
prescription coverage (e.g., Medicaid,<br />
Medicare prescription drug coverage,<br />
other charitable organizations). All<br />
applications are reviewed on a case-bycase<br />
basis. If your patients do not have<br />
prescription coverage, our team can help<br />
them explore their options. To qualify,<br />
patients must:<br />
●●<br />
Not be eligible for or have prescription<br />
drug coverage through any<br />
private or public prescription coverage<br />
program, including Medicaid <strong>and</strong><br />
Medicare.<br />
●●<br />
●●<br />
●●<br />
Have an annual income at or below<br />
300% <strong>of</strong> the current Federal Poverty<br />
Level.<br />
Submit a recent federal tax return<br />
along with the application. If the<br />
patient does not file taxes, an alternate<br />
pro<strong>of</strong> <strong>of</strong> income will be required.<br />
Be a legal resident <strong>of</strong> the U.S. or its<br />
territories.<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
income values on your application.<br />
Acceptable documents include:<br />
■■<br />
W2 forms<br />
■■<br />
Pay statements<br />
■■<br />
Social security, pension, or retirement<br />
statements<br />
■■<br />
Bank statements<br />
■■<br />
Statements <strong>of</strong> interest, dividends,<br />
or other income.<br />
Sign the Applicant Declaration<br />
section.<br />
Complete the Therapy <strong>and</strong> Physician<br />
Information sections <strong>of</strong> the application<br />
in their entirety.<br />
Sign the Physician Certification (no<br />
stamped signatures will be accepted).<br />
Note: Physician must have completed<br />
the enrollment form <strong>and</strong> received a<br />
denial for coverage.<br />
Sign the separate <strong>Patient</strong> Authorization<br />
to Share Health Information<br />
form (no stamped signatures will be<br />
accepted).<br />
Fax or mail both forms to: <strong>Patient</strong> Rx<br />
Solutions, PO Box 8203, Somerville,<br />
NJ 08876, Phone: 1-866-325-8231,<br />
Fax: 1-866-694-2546.<br />
Sancuso Example: Co-pays per Fill<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
sending as no documents will be<br />
returned.<br />
Attach current pro<strong>of</strong> <strong>of</strong> income<br />
(tax return, W2, pay stub) for all in<br />
household.<br />
<strong>Patient</strong>’s signature <strong>and</strong> date is<br />
required on the application.<br />
Prescriber’s signature <strong>and</strong> date is<br />
required on the application.<br />
Provide a copy <strong>of</strong> Medicare card or<br />
letter <strong>of</strong> Medicaid <strong>and</strong>/or Social<br />
Security denial, if applicable.<br />
Fax or mail both the completed<br />
application <strong>and</strong> documentation<br />
to: <strong>Patient</strong> Rx Solutions, PO Box<br />
8203, Somerville, NJ 08876,<br />
Phone: 1-866-325-8231,<br />
Fax: 1-866-694-2546.<br />
Questions Call 1.866.325.8231, 9:00 am<br />
to 5:00 pm EST.<br />
Sancuso Co-pay <strong>Assistance</strong> Card<br />
Program<br />
Each card can save your patients up to<br />
$2,200 over 11 Sancuso prescription<br />
fills; in no case will the monthly benefit<br />
exceed $200. Here’s how the program<br />
works: 1) patients can save up to $200 on<br />
each prescription after paying the first<br />
$30 <strong>and</strong> 2) each card is good for 11 fills,<br />
4 patches per fill, subject to prescription<br />
coverage.<br />
Out-<strong>of</strong>-Pocket Cost <strong>Patient</strong> Pays Co-pay Card Pays<br />
$75 $30 $45<br />
$230 $30 $200<br />
$300 $100 $200<br />
For Sancuso, download the patient<br />
assistance program application at www.<br />
patientrxsolutions.com/pdf _ files/<br />
<strong>Patient</strong>_<strong>Assistance</strong>_Application.pdf <strong>and</strong><br />
then follow the directions below.<br />
✔✔<br />
✔✔<br />
Complete the Applicant Information<br />
section <strong>of</strong> the application in its<br />
entirety.<br />
Complete the Financial Information<br />
section <strong>of</strong> the application in its<br />
entirety. Include a copy <strong>of</strong> a recent<br />
federal tax return. If you do not file<br />
taxes, the documentation support submitted<br />
should match with the selected<br />
Please be sure the physician section is<br />
completed before submitting your<br />
application. Incomplete applications<br />
will be returned as denied. Questions<br />
Call 1.800.6.SOLUTIONS, 9:00 am to<br />
5:00 pm EST.<br />
For Fareston, download the patient<br />
assistance application at www.patientrxsolutions.com/pdf<br />
_ files/Fareston_<br />
<strong>Patient</strong>_<strong>Assistance</strong>.pdf <strong>and</strong> then follow<br />
the directions below.<br />
✔✔<br />
Ensure all sections <strong>of</strong> the application<br />
are completed. Make a copy before<br />
Download the free Sancuso co-pay assistance<br />
card at www.sancuso.com/patient/<br />
copay/loyaltyRX.php <strong>and</strong> follow these<br />
easy steps:<br />
1. Show this prescription card <strong>and</strong> your<br />
valid prescription each time you pay<br />
for your prescription.<br />
2. Pay the initial $30 <strong>of</strong> your co-pay; any<br />
remaining out-<strong>of</strong>-pocket costs will be<br />
reduced by up to $200 per month.<br />
3. Save your co-pay assistance card—<br />
this card can be used once a month for<br />
up to 11 prescriptions or 44 patches<br />
69<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
St. Mary Corwin Regional Medical Center,<br />
Dorcy Cancer Center, Pueblo, Colorado<br />
70<br />
per patient, whichever comes first.<br />
Maximum 4 patches per fill. In no<br />
case will the monthly benefit exceed<br />
$200.<br />
Fareston Co-pay <strong>Assistance</strong> Card<br />
Program<br />
Each card can save your patients up to<br />
$2,400 over 12 Fareston prescription<br />
fills; in no case will the monthly benefit<br />
exceed $200. Here’s how the program<br />
works: 1) it <strong>of</strong>fers co-pay savings <strong>of</strong> up to<br />
$200 toward each prescription after paying<br />
the first $30 for up to 12 prescriptions<br />
per year for eligible patients <strong>and</strong> 2) each<br />
Fareston Example: Co-pays per Fill<br />
card can be used once a month for up to<br />
12 prescriptions.<br />
Download the free Fareston co-pay assistance<br />
card at www.patientrxsolutions.<br />
com/fareston-copay <strong>and</strong> follow these<br />
easy steps:<br />
1. Show this co-pay assistance card <strong>and</strong><br />
your valid prescription each time you<br />
pay for your prescription.<br />
2. Pay the initial $30 <strong>of</strong> your co-pay.<br />
Any remaining out-<strong>of</strong>-pocket costs<br />
will be reduced by up to $200 per<br />
month.<br />
3. Save your co-pay assistance card—<br />
this card can be used once a month for<br />
up to 12 prescriptions. In no case will<br />
the monthly benefit exceed $200.<br />
Sancuso Patch Replacement<br />
Program<br />
If your patient’s chemotherapy is<br />
delayed or canceled, the Sancuso Patch<br />
Replacement Program may be able to<br />
help receive a replacement patch. The<br />
application is available online at www.<br />
patientrxsolutions.com/pdf _ files/Patch_<br />
Replacement_Application.pdf. Providers<br />
must work with patients to complete the<br />
Out-<strong>of</strong>-Pocket Cost You Pay Co-pay Card Pays<br />
$75 $30 $45<br />
$230 $30 $200<br />
$300 $100 $200<br />
application as information is needed from<br />
both the patient <strong>and</strong> the physician. The<br />
provider must also sign the application.<br />
Completed applications, along with a<br />
receipt for pro<strong>of</strong> <strong>of</strong> purchase, should be<br />
faxed to: 1.866.258.7480.<br />
REIMBURSEMENT ASSISTANCE<br />
Prior Authorization <strong>Assistance</strong><br />
Program<br />
If your patient has prescription insurance<br />
coverage, our experienced staff will<br />
make it easier to gain access to Sancuso<br />
<strong>and</strong> Fareston by working directly with<br />
him or her on coverage-related questions.<br />
The prior authorization assistance<br />
program:<br />
✔✔<br />
✔✔<br />
✔✔<br />
Uses all available discounts <strong>and</strong> assistance<br />
programs to make Sancuso <strong>and</strong><br />
Fareston more accessible.<br />
Works with retail pharmacies <strong>and</strong><br />
physician dispensing pharmacies to<br />
provide Sancuso <strong>and</strong> Fareston.<br />
Can connect patients to mail order<br />
resources that will ship product<br />
directly to the patient’s home.<br />
The prior authorization takes between<br />
24 <strong>and</strong> 72 hours; however, the average<br />
response or status update time is less than<br />
24 hours. For the quickest service, fill out<br />
the prior authorization assistance applications<br />
below <strong>and</strong> fax the application <strong>and</strong><br />
the prescription to 1.888.705.7852 or<br />
call 1.888.705.7851. Be sure to have the<br />
following information available when<br />
faxing or calling:<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
<strong>Patient</strong> information<br />
Prescription<br />
<strong>Patient</strong>’s prescription drug insurance<br />
card<br />
Physician Information.<br />
Download the Sancuso prior authorization<br />
application at www.patientrxsolutions.com/pdf<br />
_ files/Prior_Authorization.<br />
pdf <strong>and</strong> the Fareston prior authorization<br />
application at www.patientrxsolutions.<br />
com/pdf _ files/Fareston_Prior_Auth.pdf.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
San<strong>of</strong>i Oncology<br />
www.san<strong>of</strong>ioncology.com<br />
Oncology-related products: Elitek ® (rasburicase), Eloxatin ®<br />
(oxaliplatin), Jevtana ® (cabazitaxel), Leukine ® (sargramostim),<br />
Mozobil ® (plerixafor), Taxotere ® (docetaxel), Thymoglobulin ®<br />
(anti-thymocyte globulin [rabbit]), Zaltrap ® (ziv-aflibercept) a<br />
collaboration between San<strong>of</strong>i <strong>and</strong> Regeneron Pharmaceuticals, Inc.<br />
●●<br />
●●<br />
<strong>and</strong>
72<br />
To qualify for the free drug program:<br />
Household income for non-oncology<br />
products <strong>of</strong>
Seattle Genetics<br />
www.seagen.com<br />
Oncology-related products: Adcetris ® (brentuximab vedotin)<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.seagensecure.com<br />
PATIENT ASSISTANCE<br />
SeaGen Secure <strong>of</strong>fers a <strong>Patient</strong><br />
<strong>Assistance</strong> Program for uninsured <strong>and</strong><br />
underinsured patients who have been<br />
prescribed Adcetris. Once an enrollment<br />
form (www.seagensecure.com/assets/<br />
pdfs/3850_sgnmm_ fa1_ss_ form.pdf) has<br />
been completed, fax it to: 855.557.2480.<br />
It is important that each field is filled<br />
out completely <strong>and</strong> accurately to ensure<br />
timely processing <strong>of</strong> the application.<br />
If you have any questions, please call<br />
855.4SEAGEN (855.473.2436), option 1,<br />
to speak with a reimbursement counselor.<br />
Benefits Investigation<br />
Once the enrollment form is received,<br />
a benefits investigation is conducted to<br />
determine an individual patient’s coverage<br />
for treatment. It is our priority to<br />
make sure providers have patient-specific<br />
coverage information before starting<br />
patients on therapy with Adcetris, so<br />
we will fax providers a summary <strong>of</strong><br />
the patient’s Adcetris-related benefits<br />
within two business days <strong>of</strong> receiving the<br />
completed request. If patient coverage for<br />
Adcetris is confirmed:<br />
●●<br />
●●<br />
Refer to sample claims form (http://<br />
seagensecure.com/assets/pdfs/Sample_CMS_1500_ADCETRIS.pdf)<br />
for<br />
billing guidance.<br />
If the patient needs help paying coinsurance,<br />
he or she will be assessed<br />
for eligibility for the SeaGen Secure<br />
Co-Insurance <strong>Assistance</strong> Program<br />
or referred to an independent foundation.<br />
Note: To be eligible for the<br />
Co-insurance <strong>Assistance</strong> Program,<br />
patients must have coverage for<br />
Adcetris through a commercial<br />
insurer, be at least 18 years old, <strong>and</strong><br />
be seeking treatment for a labeled<br />
indication.<br />
If patient does not have coverage for<br />
Adcetris:<br />
●●<br />
If the patient is insured, SeaGen<br />
Secure will assist with an appeal. If<br />
the appeal is unsuccessful, the patient<br />
will be assessed for eligibility for<br />
patient assistance.<br />
●●<br />
Skagit Valley Hospital Regional<br />
Cancer Care Center, Washington<br />
If the patient is uninsured, the patient<br />
will be assessed for eligibility for<br />
SeaGen Secure <strong>Assistance</strong> program.<br />
Co-Insurance <strong>Assistance</strong><br />
SeaGen Secure <strong>of</strong>fers an Adcetris<br />
Co-Insurance <strong>Assistance</strong> Program for<br />
commercially-insured patients who have<br />
trouble affording their co-insurance.<br />
Once an enrollment form has been completed,<br />
fax it to: 855.557.2480. It is important<br />
that each field is filled out completely<br />
<strong>and</strong> accurately to ensure timely processing<br />
<strong>of</strong> the application.<br />
If you have any questions, please call<br />
855.4SEAGEN (855.473.2436), option 1,<br />
to speak with a reimbursement counselor.<br />
REIMBURSEMENT ASSISTANCE<br />
SeaGen Secure reimbursement services<br />
include:<br />
●●<br />
Billing <strong>and</strong> coding support. Trained<br />
reimbursement counselors provide<br />
payer-specific billing <strong>and</strong> coding<br />
requirements to assist with the billing<br />
process.<br />
●●<br />
●●<br />
●●<br />
Prior authorization assistance. If it<br />
is determined that Adcetris treatment<br />
requires prior authorization, SeaGen<br />
Secure can determine which forms<br />
<strong>and</strong> processes are needed to secure<br />
the authorization. Additionally, Sea-<br />
Gen Secure can track the prior authorization<br />
claim once it is submitted.<br />
Appeal assistance <strong>and</strong> claims tracking.<br />
If an Adcetris prior authorization<br />
or claim is denied (or partially<br />
paid), SeaGen Secure will work to<br />
determine the reason for the denial<br />
<strong>and</strong> the steps for an appeal. SeaGen<br />
Secure will also provide a sample<br />
Letter <strong>of</strong> Medical Necessity (www.<br />
seagensecure.com/assets/pdfs/Adcetris_Sample_Letter_<strong>of</strong><br />
_Medical_<br />
Necessity_20120302.pdf). Medical<br />
Information may be able to assist with<br />
any additional data requests. After<br />
SeaGen Secure assists with an appeal<br />
<strong>and</strong> the documentation is submitted to<br />
the payer, we <strong>of</strong>fer claims tracking to<br />
ensure the payer receives the appeal<br />
<strong>and</strong> addresses it. Claims tracking<br />
ensures that the provider is aware<br />
<strong>of</strong> claims payment <strong>and</strong>/or any payer<br />
delays in processing.<br />
General payer <strong>and</strong> policy research.<br />
Many payers have established<br />
Adecetris policies. SeaGen Secure<br />
can provide a copy <strong>of</strong> the requested<br />
policy or assist with navigating the<br />
Adcetris Payer Map. The Adcetris<br />
Payer Map allows providers to find<br />
payer policies based on their state <strong>and</strong><br />
their patient’s specific payer.<br />
73<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
TEVA Oncology<br />
formerly Cephalon Oncology<br />
www.tevausa.com<br />
Oncology-related therapeutic products: Tre<strong>and</strong>a ® (bendamustine HCl)<br />
for Injection, Trisenox ® (arsenic trioxide) for Injection<br />
Oncology-related supportive care products: Actiq ® (oral transmucosal<br />
fentanyl citrate) [C-II], Fentora ® (fentanyl buccal tablet) [C-II]<br />
Oncology<br />
<strong>Patient</strong> <strong>and</strong> <strong>Reimbursement</strong><br />
<strong>Assistance</strong> Website<br />
www.cephalononcologycore.<br />
com<br />
PATIENT ASSISTANCE<br />
CORE <strong>Patient</strong> <strong>Assistance</strong> Program<br />
Cephalon supports patients <strong>and</strong> providers<br />
through programs for eligible patients<br />
treated in the United States who do not<br />
have insurance, cannot afford their out<strong>of</strong>-pocket<br />
co-pay costs, or need assistance<br />
with reimbursement issues.<br />
The CORE <strong>Patient</strong> <strong>Assistance</strong> Program<br />
provides FDA-approved products<br />
free <strong>of</strong> charge for patients who qualify.<br />
Cephalon also engages with groups like<br />
the Leukemia <strong>and</strong> Lymphoma Society<br />
that have programs designed to help<br />
patients access the treatments they need.<br />
For complete details <strong>and</strong> eligibility<br />
requirements, contact the CORE Hotline<br />
toll-free at 1.888.587.3263.<br />
●●<br />
●●<br />
●●<br />
is available online at: www.<br />
cephalononcologycore.com/includes/<br />
pdf/Sample_Medical_TRISENOX.pdf.<br />
A sample letter <strong>of</strong> medical necessity<br />
for Tre<strong>and</strong>a is available online at:<br />
www.cephalononcologycore.com/<br />
includes/pdf/Sample_<br />
Medical_TREANDA.pdf.<br />
Personalized support through the<br />
claims process.<br />
Requested information needed to support<br />
claims submission.<br />
Appeal support. A sample appeal<br />
When calling about patient-specific reimbursement<br />
issues, providers should have<br />
the following information available:<br />
●●<br />
●●<br />
●●<br />
<strong>Patient</strong>’s name, address, telephone<br />
number, date <strong>of</strong> birth, Social Security<br />
number, diagnosis, therapy start date,<br />
<strong>and</strong> expected course <strong>of</strong> treatment<br />
Name <strong>and</strong> telephone number <strong>of</strong> payer<br />
plan(s), policy number(s), <strong>and</strong> name <strong>of</strong><br />
subscriber<br />
Provider’s name, address, <strong>and</strong><br />
telephone number.<br />
For coverage verifications <strong>and</strong> prior<br />
authorization or appeal support, patients<br />
will need to review <strong>and</strong> sign a brief<br />
enrollment form <strong>and</strong> fax or mail it to the<br />
CORE Hotline. The enrollment form<br />
is online at: www.cephalononcologycore.com/includes/pdf/CORE_Enrollment_Form_20100930.pdf.<br />
When<br />
REIMBURSEMENT ASSISTANCE<br />
74<br />
CORE—Cephalon Oncology<br />
<strong>Reimbursement</strong> Expertise<br />
CORE is a convenient reimbursement<br />
resource that provides a support program<br />
along with online tools to help providers<br />
<strong>and</strong> patients better underst<strong>and</strong> the<br />
reimbursement process. <strong>Reimbursement</strong><br />
consultants provide assistance with the<br />
following:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Benefit verification <strong>and</strong> coverage.<br />
Policy benefits <strong>and</strong> limitations.<br />
Pre-certifications.<br />
Drug <strong>and</strong> services coding information.<br />
Coverage guidelines <strong>and</strong> payer claim<br />
requirements. A sample letter <strong>of</strong><br />
medical necessity for Trisenox<br />
letter for Trisenox is available online<br />
at: www.cephalononcologycore.com/<br />
includes/pdf/Sample_Appeal_<br />
TRISENOX.pdf. A sample appeal<br />
letter for Tre<strong>and</strong>a is available online<br />
at: www.cephalononcologycore.com/<br />
includes/pdf/Sample_Appeal_TRE-<br />
ANDA.pdf.<br />
Presbyterian Cancer<br />
Center, North Carolina<br />
complete, the form should be faxed to:<br />
1.866.676.4073 or mailed to: CORE,<br />
6900 College Blvd., Suite 1000,<br />
Overl<strong>and</strong> Park, KS 66211.<br />
<strong>Reimbursement</strong> counselors are available<br />
by phone Monday through Friday,<br />
from 9:00 am to 8:00 pm EST. Simply<br />
call 1.888.587.3263.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Other <strong>Patient</strong> <strong>Assistance</strong> Programs<br />
<strong>and</strong> Resources<br />
BenefitsCheckUp ®<br />
www.benefitscheckup.org<br />
BenefitsCheckUp is a free, confidential,<br />
online service <strong>of</strong> the National Council<br />
on Aging (NCOA). The online service<br />
will ask a series <strong>of</strong> questions to help<br />
adults over 55 who need help paying<br />
for prescription drugs, healthcare, utilities,<br />
<strong>and</strong> other basic needs <strong>and</strong> identify<br />
programs <strong>and</strong> benefits that could help.<br />
After answering the questions, patients<br />
will receive a personalized report that<br />
describes the programs or benefits that<br />
may <strong>of</strong>fer support. <strong>Patient</strong>s can apply<br />
for many <strong>of</strong> the programs online or<br />
print an application form. Here are<br />
the types <strong>of</strong> expenses patients may<br />
get help with:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Medications<br />
Food<br />
Utilities<br />
Legal<br />
Healthcare<br />
Housing<br />
In-home services<br />
Taxes<br />
Transportation<br />
Employment Training.<br />
If patients have Medicare <strong>and</strong> have<br />
limited income <strong>and</strong> resources, they may<br />
be able to get help paying for prescription<br />
drug costs if:<br />
●●<br />
●●<br />
Their income is less than $16,755 if<br />
single <strong>and</strong> $22,695 if married. If they<br />
live in Alaska or Hawaii, they may<br />
still get help even if their income is<br />
higher than these limits.<br />
<strong>Patient</strong>s have resources less than<br />
$13,070 if single <strong>and</strong> $26,120 if<br />
married.<br />
If patients meet the guidelines, they<br />
will have low or no deductible, low or<br />
no premiums, no coverage gap (also<br />
called the “donut hole”), <strong>and</strong> will pay<br />
much less for their prescriptions. At<br />
the same time, patients can start the<br />
application process for the Medicare<br />
Savings Programs that could increase<br />
patients’ monthly income by $99.90.<br />
<strong>Patient</strong>s will also find out if there are<br />
other benefit programs that can save<br />
them money. Apply online at: https://<br />
www.benefitscheckup.org/cf/continue.<br />
cfm. For more information: www.<br />
benefitscheckup.org.<br />
Co-Pay Relief<br />
www.copays.org<br />
The <strong>Patient</strong> Advocate Foundation<br />
(PAF) Co-Pay Relief Program (CPR)<br />
provides direct financial support for<br />
pharmaceutical co-payments to insured<br />
patients, including Medicare Part D<br />
beneficiaries, who financially <strong>and</strong><br />
medically qualify.<br />
The program <strong>of</strong>fers innovative<br />
technology tools for patients, providers,<br />
<strong>and</strong> pharmacy representatives, including<br />
24-hour web-based application portals,<br />
electronic signature, document upload,<br />
<strong>and</strong> bar code fax routing capabilities,<br />
increasing the speed with which an<br />
approval can be granted <strong>and</strong> expenditures<br />
can be paid. The program also <strong>of</strong>fers<br />
individualized service to all patients<br />
through the use <strong>of</strong> call counselors—<br />
personally guiding patients through the<br />
enrollment process.<br />
CPR currently assists insured patients<br />
who are financially <strong>and</strong> medically<br />
qualified <strong>and</strong> are being treated for the<br />
following:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Breast cancer<br />
Non-muscle invasive bladder cancer<br />
Non-small cell lung cancer<br />
Hormone suppression therapy<br />
Cutaneous t-cell lymphoma<br />
Multiple myeloma<br />
Myelodysplastic syndrome (<strong>and</strong> other<br />
pre-leukemia diseases)<br />
Renal cell carcinoma<br />
Pain.<br />
CPR <strong>of</strong>fers a secured website for medical<br />
providers to enroll electronically for the<br />
CPR Program on behalf <strong>of</strong> their patients.<br />
Should you wish to access this provider<br />
resource, go to: www.copays.org/providers.php<br />
to obtain information on how<br />
to register <strong>and</strong> submit an application on<br />
your patient’s behalf. You will receive an<br />
email to confirm your registration <strong>and</strong><br />
create your password. You will need to<br />
provide your provider tax Identification<br />
Number (EIN), National Provider Identifier<br />
(NPI), <strong>and</strong> a valid email address to<br />
complete the registration process.<br />
To register now go to: https://sx2035.<br />
unicentric.com/cprportal/ForProviders.<br />
aspx. If you have already registered with<br />
CPR, log in at: https://sx2035.unicentric.<br />
com/cprportal/Login.aspx to start the<br />
application process.<br />
Note: CPR provides assistance to patients<br />
on a first-come first-served basis <strong>and</strong><br />
processes applicants in the order in which<br />
their completed applications are received.<br />
A thorough review <strong>of</strong> the completed<br />
application packet, in its entirety, is<br />
necessary before a final determination<br />
<strong>of</strong> acceptance for assistance can<br />
be made. Questions Contact CPR at:<br />
1.866.512.3861.<br />
HealthWell Foundation<br />
www.healthwellfoundation.org<br />
The HealthWell Foundation provides<br />
financial assistance to eligible individuals<br />
to cover coinsurance, co-payments,<br />
healthcare premiums, <strong>and</strong> deductibles for<br />
certain medications <strong>and</strong> therapies. If your<br />
patient has been prescribed a medication<br />
<strong>and</strong> his or her insurance company covers<br />
it, but the patient still cannot afford the<br />
co-insurance or co-payment required,<br />
HealthWell may be able to help by paying<br />
for part <strong>of</strong> the costs associated with the<br />
medication. Also, if your patient is eligible<br />
for health insurance, but cannot afford the<br />
insurance premium, HealthWell may be<br />
able to help with the insurance premium.<br />
Providers <strong>and</strong> patient advocates can<br />
apply on behalf <strong>of</strong> a patient in two ways:<br />
●●<br />
Apply online at: https://www.healthwellfoundationsupport.org/secure/<br />
Default.aspx<br />
●●<br />
Apply by phone at: 800.675.8416.<br />
Before beginning the application process,<br />
please have the following information<br />
h<strong>and</strong>y:<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
<strong>Patient</strong> contact information (name,<br />
address, telephone number, Social<br />
Security number, date <strong>of</strong> birth)<br />
<strong>Patient</strong> insurance <strong>and</strong> prescription<br />
information <strong>and</strong> ID (i.e., insurance<br />
<strong>and</strong> pharmacy card)<br />
<strong>Patient</strong> income information (total<br />
household income, total household<br />
size)<br />
Prescribing physician information<br />
(name, address, telephone number,<br />
fax number, contact name)<br />
Whether the patient is applying for<br />
co-payment or premium assistance.<br />
(<strong>Patient</strong>s can receive only one or the<br />
other.).<br />
If the patient is pre-approved, providers<br />
75<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
or advocates must submit the following<br />
required documentation within 30 days:<br />
✔✔<br />
Complete Statement <strong>of</strong> Treatment<br />
with the prescribing provider’s<br />
signature.<br />
✔✔<br />
✔✔<br />
A copy <strong>of</strong> the patient’s insurance <strong>and</strong><br />
pharmacy card(s), front <strong>and</strong> back.<br />
If requesting premium assistance,<br />
also include: documentation from the<br />
patient’s insurer or employer confirming<br />
the portion <strong>of</strong> the health insurance<br />
premium the patient is responsible<br />
for paying <strong>and</strong> documentation that<br />
the patient’s insurance will cover the<br />
medications for the disease state. We<br />
accept any <strong>of</strong> the following: 1) letter<br />
from insurer, Explanation <strong>of</strong> Benefits<br />
(EOB) form (must include patient<br />
name, insurer name, drug name,<br />
<strong>and</strong> co-pay amount), or 3) recent pharmacy<br />
receipt (must include patient<br />
name, insurer name, drug name, <strong>and</strong><br />
co-pay amount).<br />
HealthWell must receive all the required<br />
documentation within 30 days <strong>of</strong><br />
approval or the patient’s grant will<br />
be closed. The patient can re-apply,<br />
however, the approval date will reset.<br />
Dates <strong>of</strong> service <strong>and</strong> costs incurred prior<br />
to the most recent approval date will not<br />
be eligible for reimbursement. We will<br />
not call or send letters requesting any<br />
missing required documentation. It is the<br />
responsibility <strong>of</strong> the patient <strong>and</strong> provider<br />
to ensure we received the required documentation<br />
within 30 days <strong>of</strong> the approval.<br />
For fastest service, fax these items to<br />
HealthWell at: 800.282.7692. Providers or<br />
advocates will receive an automatic fax<br />
back confirmation, which includes the<br />
number <strong>of</strong> pages received. To check on<br />
the status <strong>of</strong> a grant, providers can register<br />
<strong>and</strong> use our secure online provider portal<br />
at: https://healthwellfoundation.secure.<br />
force.com. Providers can also use our<br />
automated system by calling: 800.675.8416<br />
<strong>and</strong> following the instructions.<br />
The Leukemia &<br />
Lymphoma Society<br />
www.lls.org<br />
The Leukemia & Lymphoma Society<br />
(LLS) Co-Pay <strong>Assistance</strong> Program helps<br />
patients pay their insurance premiums<br />
<strong>and</strong> meet co-pay obligations. LLS can<br />
also help providers <strong>and</strong> patients find<br />
additional sources <strong>of</strong> financial help. The<br />
LLS Co-Pay <strong>Assistance</strong> Program <strong>of</strong>fers<br />
financial help toward:<br />
●●<br />
Cancer treatment-related co-pays<br />
●●<br />
Private health insurance premiums<br />
●●<br />
Private insurance co-pay obligations<br />
●●<br />
Medicare Part B, Medicare Part D,<br />
Medicare Supplementary Health<br />
Insurance, Medicare Advantage<br />
premium, Medicaid spend-down, or<br />
co-pay obligations.<br />
Prescription insurance coverage is<br />
required to qualify for this program.<br />
Prescription drugs covered under this<br />
76<br />
Sutter Cancer Center, California<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
Financial Specialists as Part <strong>of</strong> the<br />
Multidisciplinary Cancer Care Team<br />
program include those supplied to the<br />
patient by a pharmacy or administered in<br />
an <strong>of</strong>fice or hospital by a healthcare provider.<br />
To receive assistance, patients must<br />
maintain insurance coverage at all times<br />
<strong>and</strong> the requested assistance must be<br />
covered by the patient’s insurance carrier.<br />
The program cannot provide financial<br />
assistance for drugs or treatments that are<br />
not included on the patient’s insurance<br />
plan or drug formulary. Providers must<br />
confirm the diagnosis <strong>and</strong> that the drugs<br />
or treatment received during doctor visits<br />
for which patients have applied for copay<br />
or premium assistance are being used<br />
to treat a blood cancer currently covered<br />
in LLS’s Co-Pay <strong>Assistance</strong> Program.<br />
To be eligible for Co-Pay <strong>Assistance</strong>,<br />
patients must:<br />
✔✔<br />
✔✔<br />
Have a household income at or within<br />
500 percent <strong>of</strong> the U.S. Federal<br />
Poverty <strong>Guide</strong>lines as adjusted by<br />
the Cost <strong>of</strong> Living Index (COLI).<br />
Reside in the United States or<br />
Puerto Rico <strong>and</strong> be medically<br />
✔✔<br />
✔✔<br />
<strong>and</strong> financially qualified<br />
Have prescription insurance coverage<br />
Have an LLS Co-Pay Programcovered<br />
blood cancer diagnosis<br />
confirmed by a provider.<br />
The following expenses are covered by<br />
the LLS Co-Pay <strong>Assistance</strong> program:<br />
●●<br />
Blood <strong>and</strong> marrow stem cell<br />
transplantation<br />
●●<br />
Blood cell boosters <strong>and</strong><br />
erythropoietin-stimulating agents<br />
●●<br />
Blood transfusions<br />
●●<br />
Chemotherapy<br />
●●<br />
Intravenous preparation <strong>and</strong>/or<br />
maintenance procedures<br />
●●<br />
Iron chelation therapy<br />
●●<br />
Kyphoplasty<br />
●●<br />
Photopheresis <strong>and</strong> UV light therapy<br />
●●<br />
Prescription drug co-pays related<br />
to the covered co-pay diagnosis or<br />
treatment<br />
●●<br />
●●<br />
●●<br />
Take this online course <strong>and</strong> learn how<br />
to incorporate this staff member <strong>and</strong><br />
financial assistance services into your<br />
existing cancer care team. An experienced<br />
financial advocate explains how<br />
to develop a staffing model that will<br />
produce the best outcome for patients,<br />
providers, <strong>and</strong> program by:<br />
■■<br />
■■<br />
Clarifying <strong>and</strong> defining staff roles<br />
<strong>and</strong> responsibilities for providing<br />
financial assistance services to<br />
patients <strong>and</strong> families.<br />
Process mapping. Flow chart<br />
your financial assistance services<br />
<strong>and</strong> the staff that perform these<br />
functions. Look for ways to<br />
reduce duplication <strong>and</strong> improve<br />
or streamline your process.<br />
Public or private insurance premiums<br />
Radiation therapy<br />
Radioimmunotherapy.<br />
Apply online at: www.lls.org/#/diseaseinformation/getinformationsupport/financialmatters/copayassistance/<br />
providers (providers) or www.lls.org/#/<br />
diseaseinformation/getinformationsupport/financialmatters/copayassistance/<br />
patients (patients).<br />
You can also apply or get more information<br />
about the LLS Co-Pay <strong>Assistance</strong><br />
Program, by calling 877.557.2672<br />
<strong>and</strong> speaking with a co-pay specialist<br />
who will provide personalized service<br />
throughout the application process.<br />
■■<br />
Explore models for how these<br />
staff members fit into an organizational<br />
chart. Who do these staff<br />
members report to How are they<br />
supervised How is job performance<br />
measured<br />
Register at: www.accc-cancer.org/education/FinancialCounseling-Courses.<br />
asp. This course is part <strong>of</strong> ACCC’s<br />
Financial Information <strong>and</strong> Learning<br />
Network educational program.<br />
Needy Meds<br />
www.needymeds.org<br />
<strong>Patient</strong> assistance programs (PAPs) are<br />
usually sponsored by pharmaceutical<br />
companies <strong>and</strong> provide free or discounted<br />
medicines to low-to-moderateincome,<br />
uninsured, <strong>and</strong> underinsured<br />
people who meet the guidelines. Eligibility<br />
<strong>and</strong> application requirements vary<br />
from program to program. Here are four<br />
easy steps to find PAPs on this website:<br />
1. Search by name <strong>of</strong> the drug. PAPs are<br />
found by searching for the name <strong>of</strong><br />
the medicine.<br />
2. Click on the Br<strong>and</strong> Name Drugs link<br />
at: www.needymeds.org/drug_list.taf.<br />
Click on the first letter <strong>of</strong> the drug’s<br />
name in the alphabet bar. An alphabetical<br />
listing <strong>of</strong> all the drugs <strong>of</strong>fered<br />
through a PAP are listed. If it is not<br />
there, then click on the Generic Name<br />
Drugs link at: www.needymeds.org/<br />
generic_list.taf <strong>and</strong> follow the same<br />
procedure.<br />
3. Click on the name <strong>of</strong> the medicine.<br />
This will open a program page with<br />
contact information, medication dosages,<br />
application if available, eligibility<br />
criteria, <strong>and</strong> other details <strong>of</strong> the PAP.<br />
4. Call the program. Please do not call<br />
NeedyMeds with specific program<br />
questions. Some programs will make<br />
exceptions to their eligibility criteria.<br />
The drugs <strong>of</strong>fered <strong>and</strong> the program<br />
requirements change, so it may pay to<br />
call back from time to time.<br />
If your medicine is not on either list or<br />
77<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
<strong>2013</strong> Federal Poverty <strong>Guide</strong>lines<br />
78<br />
is not available through a PAP at this<br />
time go to: www.needymeds.org/indices/<br />
cantfindmeds.htm.<br />
Providers <strong>and</strong> patients can also access<br />
other services, such as:<br />
●●<br />
●●<br />
Size <strong>of</strong><br />
48 Contiguous<br />
Family Unit States <strong>and</strong> D.C. Alaska Hawaii<br />
1 $11,490 $14,350 $13,230<br />
2 $15,510 $19,380 $17,850<br />
3 $19,530 $24,410 $22,470<br />
4 $23,550 $29,440 $27,090<br />
5 $27,570 $34,470 $31,710<br />
6 $31,590 $39,500 $36,330<br />
7 $35,610 $44,530 $40,950<br />
8 $39,630 $49,560 $45,570<br />
For each additional<br />
person, add $4,020 $5,030 $4,620<br />
Source: Federal Register: January 24, <strong>2013</strong>.<br />
Applications <strong>Assistance</strong>: www.<br />
needymeds.org/local_programs.taf.<br />
Many local programs <strong>and</strong> individuals<br />
assist providers <strong>and</strong> patients to<br />
use patient assistance programs. For<br />
a small fee, they can help with such<br />
things as finding a program, completing<br />
the forms, <strong>and</strong> working with<br />
physicians who must sign the forms.<br />
Click on your state to bring up a list<br />
<strong>of</strong> local programs. Click on the name<br />
<strong>of</strong> the program for more information.<br />
Diagnosis-Based <strong>Assistance</strong>: www.<br />
needymeds.org/copay_branch.taf.<br />
This database <strong>of</strong> programs helps<br />
with costs associated with specific<br />
diagnoses. They may cover many<br />
types <strong>of</strong> expenses, including drugs,<br />
insurance co-pays, <strong>of</strong>fice visits,<br />
transportation, nutrition, medical<br />
supplies, <strong>and</strong> child or respite care.<br />
Some cover one specific diagnosis,<br />
while others cover whole categories<br />
(such as all types <strong>of</strong> cancers) or<br />
even all chronic medical illnesses.<br />
These programs are funded by<br />
either private or government<br />
organizations. Some programs are<br />
national in scope, while others are<br />
limited to people in specific states.<br />
Most have some type <strong>of</strong> eligibility<br />
requirements, usually financial<br />
ones. It’s best to search by the type<br />
<strong>of</strong> diagnosis. Other ways to search<br />
for assistance are by looking for<br />
programs that serve a specific<br />
geographical area. Note that this<br />
method will only show programs<br />
●●<br />
that are limited to a state or region;<br />
national programs are not included<br />
in these lists. If you know the name<br />
<strong>of</strong> a specific program about which<br />
you want more information, you can<br />
also search by name <strong>of</strong> program.<br />
<strong>Assistance</strong> with Government<br />
Programs: www.needymeds.org/<br />
indices/government_programs.htm.<br />
Every state has programs to help<br />
needy families <strong>and</strong> individuals with<br />
the cost <strong>of</strong> healthcare. NeedyMeds<br />
has compiled a database <strong>of</strong> these<br />
State Programs. The programs can<br />
be found by clicking on a state, the<br />
District <strong>of</strong> Columbia, Puerto Rico, or<br />
Guam. Programs <strong>and</strong> their guidelines<br />
vary from state to state. NeedyMeds<br />
also has a list <strong>of</strong> Medicaid Sites: www.<br />
needymeds.org/indices/medicaid.<br />
htm. Other helpful links include the<br />
Federal Poverty <strong>Guide</strong>lines: www.<br />
needymeds.org/indices/povertyguidelines.htm,<br />
<strong>and</strong> a Tax Return Request<br />
Form: www.needymeds.org/indices/<br />
forms.htm.<br />
At this time, NeedyMeds.org does not<br />
have a phone helpline. All NeedyMeds<br />
information is available on its website.<br />
Providers or patients who need help<br />
using the website can email: info@<br />
needymeds.com.<br />
Partnership for<br />
Prescription <strong>Assistance</strong><br />
www.pparx.org<br />
The Partnership for Prescription <strong>Assistance</strong><br />
(PPA) helps qualifying patients<br />
without prescription drug coverage<br />
receive the medicines they need for<br />
free or nearly free. PPA <strong>of</strong>fers a single<br />
point <strong>of</strong> access to more than 475 public<br />
<strong>and</strong> private programs, including nearly<br />
200 pharmaceutical patient assistance<br />
programs. To learn more, download the<br />
brochure at: www.pparx.org/sites/default/<br />
files/PPA_brochure.pdf.<br />
Here’s how PPA works:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Step 1: Tell us what medicines your<br />
patient takes. Go to: www.pparx.org/<br />
en/gethelp/select-meds to search for<br />
<strong>and</strong> pick out the medicines. Type the<br />
name <strong>of</strong> the medicine into the box<br />
<strong>and</strong> click the search button. Once<br />
the search is complete you can add<br />
one or more prescription drugs from<br />
your search to the My Medicines list,<br />
which appears on the right side <strong>of</strong> the<br />
page. Repeat this process until you<br />
have entered <strong>and</strong> selected all <strong>of</strong> the<br />
medicines.<br />
Step 2: Tell us about your patient.<br />
Provide basic information about the<br />
patient <strong>and</strong> the type <strong>of</strong> drug coverage<br />
(if any) he or she currently has.<br />
Answer short questions, such as the<br />
patient’s residency, age, <strong>and</strong> household<br />
income, to see which patient<br />
assistance programs the patient<br />
may qualify for. You must answer<br />
all questions on this page for your<br />
patient to be considered. If you need<br />
assistance, please call 1.888.477.2669<br />
Monday through Friday, from 9:00<br />
am to 5:00 pm EST.<br />
Step 3: Get your results. See which<br />
prescription assistance programs<br />
your patient may be eligible for <strong>and</strong><br />
select the ones you would like to<br />
apply to.<br />
Step 4: Complete the application process.<br />
Print, complete, <strong>and</strong> mail your<br />
applications to each program you are<br />
applying to.<br />
PPA <strong>of</strong>fers other resources, including:<br />
A list <strong>of</strong> co-pay programs at: www.<br />
pparx.org/en/prescription_assistance_programs/co-payment_programs.<br />
●●<br />
●●<br />
A list <strong>of</strong> discount drug card<br />
programs at: https://www.pparx.org/<br />
en/prescription_assistance_programs/discount_cards.<br />
Information about Medicare drug<br />
coverage at: https://www.pparx.org/<br />
en/prescription_assistance_programs/medicare_drug_coverage.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
<strong>Patient</strong> Access Network<br />
Foundation<br />
www.panfoundation.org/<br />
PAN is an independent non-pr<strong>of</strong>it organization<br />
that provides assistance to underinsured<br />
patients for their out-<strong>of</strong>-pocket<br />
expenses for life-saving medications.<br />
Providers <strong>and</strong> their patients can apply for<br />
assistance by calling: 1.866.316.7263 or<br />
start the application online at: www.<br />
panfoundation.org/fundingapplication/<br />
index.php9.<br />
In order for patients to qualify for<br />
co-payment assistance with the <strong>Patient</strong><br />
Access Network Foundation, they must<br />
meet the following eligibility criteria:<br />
<strong>Patient</strong> is insured <strong>and</strong> insurance<br />
covers the medication for which the<br />
patient seeks assistance<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
The medication must treat the disease<br />
directly<br />
<strong>Patient</strong>’s income must be below a<br />
designated percentage <strong>of</strong> the Federal<br />
Poverty Level, depending on individual<br />
fund requirements<br />
<strong>Patient</strong> is prescribed a high-cost drug<br />
for the disease, depending on individual<br />
fund requirements<br />
<strong>Patient</strong> must reside <strong>and</strong> receive treatment<br />
in the U.S.<br />
<strong>Patient</strong>s applying for financial assistance<br />
for their co-payments need to have access<br />
to the following information:<br />
✔✔<br />
Step 1. Select the disease for which<br />
you are seeking assistance, the<br />
patient’s insurance type, <strong>and</strong> the<br />
medication(s). If the patient is commercially<br />
insured <strong>and</strong> has selected<br />
a medication for which the manufacturer<br />
program has a co-pay card<br />
program, you will be made aware<br />
under the alternative programs box.<br />
Please research these other programs<br />
as manufacturer programs may be<br />
more generous than what PAN has<br />
to <strong>of</strong>fer.<br />
✔✔<br />
Center for Cancer Care<br />
& Research, Florida<br />
tion.org or 202.347.9273 for more<br />
information.<br />
Step 3. You will need to have access<br />
to the following information for the<br />
patient:<br />
Demographic Information<br />
■■<br />
First <strong>and</strong> last name<br />
■■<br />
Social Security number or Alien<br />
Number<br />
■■<br />
Date <strong>of</strong> birth<br />
■■<br />
Gender <strong>and</strong> marital status<br />
■■<br />
Employment status<br />
■■<br />
Phone number<br />
■■<br />
Street address <strong>and</strong> email address<br />
■■<br />
Language the patient speaks <strong>and</strong><br />
underst<strong>and</strong>s<br />
■■<br />
Residency status.<br />
Income Information<br />
■■<br />
Number <strong>of</strong> people in the household<br />
■■<br />
Income received from wages,<br />
tips, or salaries<br />
■■<br />
Income from IRA distributions,<br />
pensions, or annuities<br />
■■<br />
Social Security benefits, including<br />
the amount <strong>of</strong> the benefits<br />
received<br />
■■<br />
Any other income (child support,<br />
alimony, rental income, etc.).<br />
✔✔<br />
✔✔<br />
■■<br />
■■<br />
insurance for his or her medications<br />
Does the patient receive assistance<br />
from any other co-pay or<br />
co-insurance assistance organizations<br />
How did the provider or patient<br />
first hear about the <strong>Patient</strong> Access<br />
Network<br />
Step 4. You will need to access to<br />
the following information for the<br />
provider:<br />
■■<br />
■■<br />
■■<br />
■■<br />
■■<br />
■■<br />
First name<br />
Last name<br />
Phone number<br />
Fax number<br />
Email<br />
Address.<br />
Step 5. Review the application to<br />
make sure the information entered is<br />
correct <strong>and</strong> then submit the application<br />
online at: www.panfoundation.<br />
org/fundingapplication/patientEnrollment.php.<br />
Applications <strong>and</strong> supporting<br />
documents can also be mailed to:<br />
PAN Foundation, PO Box 221858,<br />
Charlotte, NC 28222-1858 or faxed<br />
toll-free to: 1.866.316.7261.<br />
✔✔<br />
Step 2. You will need to select the use<br />
type. As a provider, click the “I am<br />
applying for someone else” box. If the<br />
patient is applying, he or she will click<br />
the box “I am applying for myself.”<br />
If you are from a specialty pharmacy,<br />
you will need to undergo training<br />
with the PAN Foundation. Contact<br />
Korab Zuka at: kzuka@panfounda-<br />
Insurance <strong>and</strong> Co-payment<br />
Information<br />
■■<br />
Primary insurance carrier<br />
■■<br />
Policy ID number<br />
■■<br />
Group number<br />
■■<br />
Telephone number<br />
■■<br />
Secondary insurance carrier<br />
<strong>and</strong> contact information<br />
■■<br />
What is the patient’s co-pay or co-<br />
<strong>Patient</strong> Advocate<br />
Foundation<br />
www.patientadvocate.org<br />
The <strong>Patient</strong> Advocate Foundation<br />
(PAF) is a national non-pr<strong>of</strong>it organization<br />
that serves as an active liaison<br />
between the patient <strong>and</strong> his or her<br />
79<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
80<br />
insurer, employer, <strong>and</strong>/or creditors to<br />
resolve insurance, job retention, <strong>and</strong>/<br />
or debt crisis matters relative to the<br />
patient’s diagnosis through case managers,<br />
physicians, <strong>and</strong> attorneys. PAF<br />
seeks to safeguard patients through<br />
effective mediation, assuring access to<br />
care, maintenance <strong>of</strong> employment, <strong>and</strong><br />
preservation <strong>of</strong> their financial stability.<br />
PAF <strong>of</strong>fers services by telephone,<br />
email, or web chat to patients in need<br />
that fall under the scope <strong>of</strong> our services.<br />
Our pr<strong>of</strong>essional staff members<br />
intervene by making conference calls<br />
when needed, assisting with appeals<br />
to insurance companies or the Social<br />
Security Administration, negotiating<br />
with providers in medical debt situations,<br />
or securing access to care. Our<br />
staff strives for positive resolutions<br />
whenever possible <strong>and</strong> provides the<br />
following services:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Case Management<br />
Co-Pay Relief<br />
MedCareLine<br />
Outreach<br />
Prevention Resources.<br />
PAF’s <strong>Patient</strong> Services provides patients<br />
with arbitration, mediation, <strong>and</strong> negotiation<br />
to settle issues with access to care,<br />
medical debt, <strong>and</strong> job retention related to<br />
their illness. <strong>Assistance</strong> is available in the<br />
following areas:<br />
Access to Care. PAF <strong>of</strong>fers direct<br />
guidance for patients seeking access to<br />
pharmaceutical agents (drugs), devices<br />
that help with certain functions as medically<br />
necessary, <strong>and</strong> procedures, such<br />
as surgeries. Frequently, insurers deny<br />
these types <strong>of</strong> requests because certain<br />
conditions are usually not met. PAF’s<br />
pr<strong>of</strong>essional case managers will be the<br />
liaison between you <strong>and</strong> the insurer (your<br />
insurance plan or policy) to ensure that<br />
you are getting the very best possible<br />
care <strong>and</strong> access according to your policy.<br />
Financial <strong>Assistance</strong>. PAF has developed<br />
a list <strong>of</strong> resources for patients<br />
seeking assistance with accessing their<br />
medications or help with the out-<strong>of</strong>pocket<br />
expenses for their medications.<br />
Prescription assistance programs that<br />
cater to uninsured or underinsured<br />
patients can be found at: www.patientadvocate.org/index.phpp=775.<br />
Other<br />
financial services include assistance<br />
with: the disability process, the medical<br />
debt crisis, <strong>and</strong> co-pay assistance.<br />
Insurance <strong>Assistance</strong>. PAF <strong>of</strong>fers assistance<br />
with the following patient issues:<br />
●●<br />
Insurance appeals process<br />
●●<br />
Pre-authorization(s)<br />
●●<br />
Coding <strong>and</strong> billing<br />
●●<br />
Debt crisis assistance<br />
●●<br />
Medicare <strong>and</strong> Medicaid<br />
●●<br />
Clinical trial barriers.<br />
Job Retention <strong>Assistance</strong>. PAF case<br />
managers help patients with issues<br />
regarding reasonable accommodation in<br />
the workplace (in accordance with the<br />
Americans with Disabilities Act <strong>of</strong> 1990).<br />
Case managers also serve as a liaison<br />
between patients <strong>and</strong> employers for<br />
issues related to FMLA <strong>and</strong> help assist<br />
with employment rights for disabled<br />
individuals. <strong>Patient</strong> Advocate Foundation<br />
case managers make referrals to<br />
the EEOC for patients who feel they are<br />
being discriminated against <strong>and</strong> desire to<br />
file a formal complaint.<br />
Questions Contact the <strong>Patient</strong> Advocate<br />
Foundation at: help@patientadvocate.<br />
org or call: 800.532.5274.<br />
RxAssist<br />
www.rxassist.org<br />
The RxAssist database contains eligibility<br />
information <strong>and</strong> applications for<br />
more than 150 pharmaceutical company<br />
patient assistance programs. The<br />
database can help you find out whether a<br />
drug is available, which pharmaceutical<br />
company program <strong>of</strong>fers the drug, <strong>and</strong><br />
how to apply for the medication. In order<br />
to use the database, you must register<br />
either as a provider or patient.<br />
Using RxAssist<br />
Step 1: Go to www.rxassist.org <strong>and</strong><br />
click “Learn More” under either the<br />
Provider Center or <strong>Patient</strong> Center.<br />
✔✔<br />
✔✔<br />
✔✔<br />
Step 2: In the database search box,<br />
type in either the drug name or company<br />
name. If you would like to search<br />
for multiple drugs, click the advance<br />
search button. Then, enter the items in<br />
the search boxes that pop up.<br />
Step 3: After you have entered<br />
information in the search box, if the<br />
✔✔<br />
✔✔<br />
✔✔<br />
database finds a match, a Search<br />
Results page will appear. (If there<br />
is only one program available for a<br />
medication, you will be taken directly<br />
to the Program Details page.)<br />
Step 4: Click the underlined hyperlink<br />
<strong>of</strong> the medication you want in the<br />
Search Results page, <strong>and</strong> you will be<br />
taken to the Program Details page.<br />
Step 5: The Program Details page<br />
includes eligibility criteria <strong>and</strong><br />
information on how to apply to the<br />
program. If an application is available<br />
for a program, you will see “Application<br />
Forms <strong>and</strong> Instructions” to<br />
the right with links to download the<br />
application.<br />
Step 6: If an application is available<br />
online, you can either open (download)<br />
the application, type information<br />
directly onto the application on<br />
the screen <strong>and</strong> print it out, or print out<br />
the application <strong>and</strong> fill it out by h<strong>and</strong>.<br />
If there is no application online, use<br />
the phone number provided at the top<br />
<strong>of</strong> the Program Details page to call<br />
the company for information on how<br />
to get an application.<br />
The RxAssist Learning Center is where<br />
healthcare advocates <strong>and</strong> safety net<br />
providers find the information they need<br />
to manage the challenges <strong>of</strong> our changing<br />
healthcare world. If you are a provider<br />
working with patients with chronic diseases<br />
<strong>and</strong> medication assistance needs,<br />
the Learning Center <strong>of</strong>fers the following<br />
resources:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
Browse the library <strong>of</strong> carefullyselected<br />
resources related to medication<br />
assistance, healthcare access,<br />
patient resources, <strong>and</strong> program tools.<br />
Read healthcare reform highlights.<br />
Explore virtual learning with<br />
webinars. Webinars are hosted by<br />
RxAssist staff, include guest speakers<br />
<strong>and</strong> welcome audience participation.<br />
Webinars are free, but registration is<br />
required.<br />
Join RxConnects, a listserv discussing<br />
issues related to medication<br />
access.<br />
Join RxUpdates to receive regular<br />
notification <strong>of</strong> changes in pharmaceutical<br />
company <strong>and</strong> other medication<br />
assistance programs.<br />
Questions Contact RxAssist at: info@<br />
rxassist.org.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
RxHope<br />
www.rxhope.com<br />
Here’s how this web-based patient<br />
assistance program works. The provider<br />
enters the site <strong>and</strong> clicks on the<br />
<strong>Patient</strong> <strong>Assistance</strong> Application link.<br />
Providers then choose from the available<br />
products, fill in the application,<br />
<strong>and</strong> depending on the manufacturer,<br />
either print <strong>and</strong> fax the application<br />
for signature verification or mail the<br />
printed application to the appropriate<br />
address. Some products do not require<br />
a fax or mail; they may be completed<br />
electronically. All information is sent<br />
to the pharmaceutical manufacturer for<br />
final approval <strong>and</strong> shipping.<br />
Healthcare providers <strong>and</strong> their staff<br />
can set up accounts online to order free<br />
medications for their patients through<br />
our automated patient assistance online<br />
system. If you would like to create a<br />
free account for one healthcare provider,<br />
please read the instructions below. If<br />
you would like to create a free account<br />
for multiple healthcare providers, call<br />
RxHope at 1.877.267.0517 <strong>and</strong> a customer<br />
service representative will<br />
assist you.<br />
To set up your free account <strong>and</strong> place<br />
orders online for individual <strong>and</strong> multiple<br />
provider accounts, the following criteria<br />
is required:<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
✔✔<br />
You must be a healthcare provider or<br />
their staff<br />
A valid state license number for the<br />
healthcare provider<br />
An email address (this will become<br />
your login)<br />
The medication for which the patient<br />
is applying<br />
The patient’s first <strong>and</strong> last name.<br />
Once you have the above information<br />
available, go to: www.rxhope.com/<br />
Prescriber/Register.aspx <strong>and</strong> follow the<br />
instructions. You will be setting up your<br />
free account <strong>and</strong> creating an order for<br />
your patient all at the same time.<br />
RxHope provides this service to<br />
physicians <strong>and</strong> patients free <strong>of</strong> charge.<br />
RxHope is available to assist providers<br />
<strong>and</strong> patients Monday through Friday,<br />
from 8:00 am to 7:00 pm EST by calling<br />
1.877.267.0517. You can also contact<br />
RxHope by emailing: CustomerService@RxHope.com.<br />
Rx Outreach ®<br />
www.rxoutreach.org<br />
<strong>Patient</strong>s can use Rx Outreach regardless<br />
<strong>of</strong> age or if they use another discount<br />
medicine program or patient assistance<br />
program. To use Rx Outreach, the<br />
patient’s income needs to be less than a<br />
certain amount <strong>of</strong> money each year. This<br />
amount differs, depending on the number<br />
<strong>of</strong> financially dependent people living in<br />
the house:<br />
●●<br />
●●<br />
●●<br />
●●<br />
●●<br />
1-person household: Less than<br />
$33,510/year. (Alaska: less than<br />
$41,910/year; Hawaii: less than<br />
$38,580/year).<br />
2-person household: Less than<br />
$45, 390/year. (Alaska: less than<br />
$56,760/year; Hawaii: less than<br />
$52,530/year).<br />
3-person household: Less than<br />
$57,270/year. (Alaska: less than<br />
$71,610/year; Hawaii: less than<br />
$65,880/year).<br />
4-person household: Less than<br />
$69,150/year. (Alaska: less than<br />
$86,460/year; Hawaii: less than<br />
$79,530/year).<br />
More than 4-person household: For<br />
each additional person in the house,<br />
add $11,880/year. (Alaska: add<br />
$14,850/year; Hawaii: add $13,650/<br />
year). For example, if six people<br />
are in the household, the patient’s<br />
income must be less than $92,910 a<br />
year ($69,150 + $11,880 + $11,880 =<br />
$92,910).<br />
Providers <strong>and</strong> patients can enroll in the<br />
program by following these four steps:<br />
✔✔<br />
Determine patient eligibility using<br />
criteria above.<br />
✔✔<br />
See if the patient’s drug is listed on<br />
the RxOutreach Medication’s List:<br />
www.rxoutreach.org/medications.<br />
✔✔<br />
✔✔<br />
Obtain a prescription from the provider.<br />
Prescriptions may be written<br />
with refills available for up to one<br />
year. Ask your doctor about a 180-day<br />
supply with one refill or a 90-day supply<br />
with three refills.<br />
Create a simple web account then<br />
enroll/re-enroll online at: https://<br />
remote.rxoutreach.org/login/auth;jse<br />
ssionid=30465B636751F923960A6B1<br />
BA8F99C2F.<br />
Completed applications, along with<br />
your prescription <strong>and</strong> payment, can be<br />
mailed to: Rx Outreach, PO Box 66536,<br />
St. Louis, MO, 63166-6536. For more<br />
information, go to: www.rxoutreach.org<br />
or call 1-800.769.3880, Monday through<br />
Friday, 7:00 am to 5:30 pm CST.<br />
Together Rx Access ®<br />
Card<br />
www.togetherrxacess.com<br />
To qualify for a Together Rx Access<br />
Card, individuals must:<br />
●●<br />
Not be eligible for Medicare<br />
●●<br />
Have no prescription drug coverage<br />
<strong>of</strong> any kind<br />
●●<br />
Have a household income that is<br />
equal to or less than: $45,000 for a<br />
single person; $60,000 for a family<br />
<strong>of</strong> two; $75,000 for a family <strong>of</strong><br />
three; $90,000 for a family <strong>of</strong> four;<br />
$105,000 for a family <strong>of</strong> five. (Families<br />
<strong>of</strong> six or more <strong>and</strong> residents <strong>of</strong><br />
Alaska <strong>and</strong> Hawaii should contact<br />
the Together Rx Access Program at:<br />
1.800.444.4106.)<br />
Applying for the Together Rx Access<br />
Card is free <strong>and</strong> takes just a few minutes.<br />
<strong>Patient</strong>s may apply:<br />
●●<br />
●●<br />
●●<br />
Online using the checklist at:<br />
www.togetherrxaccess.com/p/<br />
prescription-savings/about-togetherrx-access/enroll.aspx.<br />
By downloading, printing, <strong>and</strong> filling<br />
out the application at: www.togetherrxaccess.com/App_Controls/Enrollment/pdf/TRx_Access_Enroll_English.pdf.<br />
The completed application<br />
should be mailed to: Together Rx<br />
Access, LLC, P.O. Box 9426, Wilmington,<br />
DE 19809-9944.<br />
Over the phone by calling:<br />
1.800.444.4106.<br />
<strong>Patient</strong>s who enroll online or by phone<br />
can use their member ID number at<br />
participating pharmacies within two<br />
hours <strong>of</strong> enrollment. To use the card,<br />
patients show it to their pharmacists<br />
when purchasing br<strong>and</strong>-name prescription<br />
medicines. Savings on generic drugs<br />
are also available <strong>and</strong> vary by pharmacy.<br />
Participating pharmacies can be found<br />
online at: www.togetherrxaccess.com/p/<br />
prescription-savings/about-together-rxaccess/pharmacies.aspx.<br />
81<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
The <strong>Association</strong> <strong>of</strong> Community Cancer Centers<br />
gratefully acknowledges its <strong>2013</strong><br />
Industry Advisory Council<br />
Amgen, Inc.<br />
Astellas Pharmaceuticals<br />
Bayer Healthcare<br />
Bristol-Myers Squibb<br />
Celgene Corporation<br />
Eisai<br />
Eli Lilly <strong>and</strong> Company<br />
Genentech, Inc.<br />
GlaxoSmithKline<br />
Janssen Biotech<br />
Merck<br />
Millennium<br />
Novartis<br />
Pfizer Oncology<br />
san<strong>of</strong>i-aventis<br />
TEVA Oncology<br />
Emerging Companies Council<br />
Ariad Pharmaceuticals<br />
Boehringer Ingelheim<br />
EMD Serono<br />
Genomic Health<br />
Onyx Pharmaceuticals<br />
Seattle Genetics<br />
Technical Advisory Council<br />
ION Solutions<br />
Philips Healthcare<br />
Veridex<br />
for their support.<br />
We want to hear from ACCC members. If your community cancer center knows <strong>of</strong> any<br />
additional patient assistance programs or you have suggestions for improving this guide<br />
for 2014, please contact us. If you know <strong>of</strong> any changes to an existing patient assistance<br />
program <strong>and</strong>/or reimbursement program or find an incorrect form or broken link in this<br />
publication, please let us know. Email all comments <strong>and</strong> feedback to ACCC’s managing<br />
editor at: mmarino@accc-cancer.org.<br />
Managing Editor: Monique J. Marino, Associate Editors: Jillian Kornak, Am<strong>and</strong>a Patton, Designer: Constance D. Dillman<br />
Cover Photograph courtesy <strong>of</strong> The Michael <strong>and</strong> Dianne Bienes Comprehensive Cancer Center at Holy Cross Hospital, Florida.<br />
82<br />
©<strong>2013</strong>. <strong>Association</strong> <strong>of</strong> Community Cancer Centers. Although every effort has been made to ensure the accuracy <strong>and</strong> completeness <strong>of</strong> this guide,<br />
ACCC is not responsible for any errors or omissions contained within. Inclusion <strong>of</strong> companies within this publication does not serve as<br />
an endorsement by ACCC <strong>of</strong> the company, its products, or its services.<br />
<br />
ACCC <strong>2013</strong> <strong>Patient</strong> <strong>Assistance</strong> <strong>and</strong> <strong>Reimbursement</strong> <strong>Guide</strong>
<strong>Association</strong> <strong>of</strong> Community Cancer Centers<br />
11600 Nebel Street, Suite 201<br />
Rockville, MD 20852<br />
www.accc-cancer.org<br />
Phone: 301.984.9496<br />
Fax: 301.770.1949