Case Studies in Chronic Pain Case Formulation Pain Types by ...
Case Studies in Chronic Pain Case Formulation Pain Types by ...
Case Studies in Chronic Pain Case Formulation Pain Types by ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Case</strong> <strong>Studies</strong> <strong>in</strong> <strong>Chronic</strong> Pa<strong>in</strong>‐‐<br />
Objectives<br />
<strong>Case</strong> <strong>Studies</strong> <strong>in</strong> <strong>Chronic</strong> Pa<strong>in</strong><br />
Miles Belgrade, MD<br />
Fairview Pa<strong>in</strong> Management Center<br />
• Carry out a physiologic pa<strong>in</strong> assessment that <strong>in</strong>forms<br />
treatment<br />
• Dist<strong>in</strong>guish chronic pa<strong>in</strong> from acute pa<strong>in</strong> and recognize the<br />
dangers <strong>in</strong> confus<strong>in</strong>g them<br />
• Flare recognition and management<br />
• Opioid management vignettes and the DIRE Score<br />
• Understand the need for a biopsychosocial approach to<br />
chronic pa<strong>in</strong> syndrome<br />
<strong>Case</strong> <strong>Formulation</strong><br />
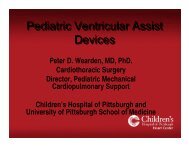
Pa<strong>in</strong> <strong>Types</strong> <strong>by</strong> Physiology<br />
• Name the type of pa<strong>in</strong><br />
• Identify the acuity:<br />
– Acute<br />
– <strong>Chronic</strong><br />
– Recurrent<br />
– Term<strong>in</strong>al<br />
• Identify contribut<strong>in</strong>g factors and barriers<br />
• Assess disease burden<br />
• What treatments are <strong>in</strong>dicated<br />
• Are <strong>in</strong>terventional approaches warranted<br />
• Is this patient a candidate for long‐term opioids<br />
Neuropathic<br />
Inflammation<br />
Mechanical<br />
Bone<br />
Psychogenic<br />
Muscular<br />
Acute, <strong>Chronic</strong>, Recurrent, Term<strong>in</strong>al Pa<strong>in</strong><br />
• Acute Pa<strong>in</strong> is pa<strong>in</strong> that has a beg<strong>in</strong>n<strong>in</strong>g, a middle<br />
and a predictable end<br />
• <strong>Chronic</strong> Pa<strong>in</strong> is pa<strong>in</strong> that persists beyond<br />
expectation and exists <strong>in</strong>dependent of the<br />
orig<strong>in</strong>al cause<br />
• Recurrent Pa<strong>in</strong> is pa<strong>in</strong> that re‐occurs <strong>in</strong><br />
stereotyped acute episodes over a long period of<br />
time<br />
• Term<strong>in</strong>al Pa<strong>in</strong> is pa<strong>in</strong> at the end of life that is<br />
related to the term<strong>in</strong>al illness<br />
Identify Contribut<strong>in</strong>g Factors and Barriers<br />
• Contribut<strong>in</strong>g factors amplify or perpetuate pa<strong>in</strong> but are<br />
not the orig<strong>in</strong>al cause<br />
– Posture<br />
– Stress<br />
– Occupational factors<br />
• Barriers are factors that prevent mak<strong>in</strong>g a complete<br />
pa<strong>in</strong> assessment or render<strong>in</strong>g optimal treatment<br />
– Insurance non‐coverage<br />
– Low motivation<br />
– Language barrier<br />
– Transportation/limited resources<br />
– Chemical dependency
Assess Disease Burden<br />
D.I.R.E. Score: Patient Selection for <strong>Chronic</strong> Opioid Analgesia<br />
For each factor, rate the patient’s score from 1-3 based on the<br />
explanations <strong>in</strong> the right hand column<br />
core Factor Explanation<br />
1 = Benign chronic condition with m<strong>in</strong>imal objective f<strong>in</strong>d<strong>in</strong>gs or no def<strong>in</strong>ite<br />
Diagnosis<br />
medical diagnosis. Examples: fibromyalgia, migra<strong>in</strong>e headaches, nonspecific<br />
back pa<strong>in</strong>.<br />
2 = Slowly progressive condition concordant with moderate pa<strong>in</strong>, or fixed<br />
condition with moderate objective f<strong>in</strong>d<strong>in</strong>gs. Examples: failed back surgery<br />
syndrome, back pa<strong>in</strong> with moderate degenerative changes, neuropathic pa<strong>in</strong>.<br />
3 = Advanced condition concordant with severe pa<strong>in</strong> with objective f<strong>in</strong>d<strong>in</strong>gs.<br />
Examples: severe ischemic vascular disease, advanced neuropathy, severe<br />
sp<strong>in</strong>al stenosis.<br />
1 = Few therapies have been tried and the patient takes a passive role <strong>in</strong><br />
Intractability<br />
his/her pa<strong>in</strong> management process.<br />
2 = Most customary treatments have been tried but the patient is not fully<br />
engaged <strong>in</strong> the pa<strong>in</strong> management process, or barriers prevent (<strong>in</strong>surance,<br />
transportation, medical illness).<br />
3 = Patient fully engaged <strong>in</strong> a spectrum of appropriate treatments but with<br />
<strong>in</strong>adequate response.<br />
Risk<br />
(R= Total of P+C+R+S below)<br />
Psychological: 1 = Serious personality dysfunction or mental illness <strong>in</strong>terfer<strong>in</strong>g with care.<br />
Example: personality disorder, severe affective disorder, significant<br />
personality issues.<br />
2 = Personality or mental health <strong>in</strong>terferes moderately. Example: depression<br />
or anxiety disorder.<br />
3 = Good communication with cl<strong>in</strong>ic. No significant personality dysfunction or<br />
mental illness.<br />
Chemical Health: 1 = Active or very recent use of illicit drugs, excessive alcohol, or prescription<br />
drug abuse.<br />
2 = Chemical coper (uses medications to cope with stress) or history of CD <strong>in</strong><br />
remission.<br />
3 = No CD history. Not drug-focused or chemically reliant.<br />
Reliability:<br />
1 = History of numerous problems: medication misuse, missed appo<strong>in</strong>tments,<br />
rarely follows through.<br />
2 = Occasional difficulties with compliance, but generally reliable.<br />
3 = Highly reliable patient with meds, appo<strong>in</strong>tments & treatment.<br />
Social Support: 1 = Life <strong>in</strong> chaos. Little family support and few close relationships. Loss of<br />
most normal life roles.<br />
2 = Reduction <strong>in</strong> some relationships and life roles.<br />
3 = Supportive family/close relationships. Involved <strong>in</strong> work or school and no<br />
social isolation.<br />
1 = Poor function or m<strong>in</strong>imal pa<strong>in</strong> relief despite moderate to high doses.<br />
Efficacy score<br />
2 = Moderate benefit with function improved <strong>in</strong> a number of ways (or<br />
<strong>in</strong>sufficient <strong>in</strong>fo- hasn’t tried opioid yet or very low doses or too short of a<br />
trial).<br />
3 = Good improvement <strong>in</strong> pa<strong>in</strong> and function and quality of life with stable<br />
doses over time.<br />
_____Total score = D + I + R + E<br />
Score 7-13: Not a suitable candidate for long-term opioid analgesia<br />
Score 14-21: Good candidate for long-term opioid analgesia<br />
<strong>Case</strong> Vignettes<br />
• A pt has burn<strong>in</strong>g pa<strong>in</strong> down the posterior leg to the calf after<br />
lumbar surgery. How would you classify it<br />
• A 71 yr old man is admitted to hospital with a CVA. He has a<br />
long hx of chronic low back pa<strong>in</strong> and DDD. How do you treat<br />
the low back pa<strong>in</strong> <strong>in</strong> the hospital<br />
• A pt calls you on the phone because their chronic neck pa<strong>in</strong><br />
has been worse after he helped his sister move. He has been<br />
on SR morph<strong>in</strong>e for over a year at the same dose, and is<br />
ask<strong>in</strong>g for a boost <strong>in</strong> the dose. What is your response<br />
• A chronic pa<strong>in</strong> patient has lost 2 Rxs. Name two actions you<br />
can take besides stopp<strong>in</strong>g the opioids<br />
<strong>Case</strong> Vignettes<br />
• Neck pa<strong>in</strong> is ach<strong>in</strong>g 2 years after a rear‐end collision.<br />
It hurts with flexion of the neck. Pressure over the<br />
trapezius causes referred pa<strong>in</strong> <strong>in</strong>to the occipital area.<br />
What is the physiological type of pa<strong>in</strong><br />
• The above patient has a newborn. Pa<strong>in</strong> is worse<br />
when she carries the <strong>in</strong>fant. What do you call that<br />
component of the pa<strong>in</strong><br />
• True or False: It is reasonable to try to get the chronic<br />
pa<strong>in</strong> patient to a pa<strong>in</strong> level that is < 4/10<br />
<strong>Case</strong> vignette<br />
Verne<br />
• Three years after a car accident, a patient is still not<br />
able to return to work due to pa<strong>in</strong>. She has been<br />
through chiropractic, medication, exercise. She is<br />
gett<strong>in</strong>g depressed and feels like her life is taken from<br />
her. What is most likely to help restore her<br />
function<strong>in</strong>g<br />
– A. Neuront<strong>in</strong><br />
– B. A chronic pa<strong>in</strong> management program<br />
– C. A long‐act<strong>in</strong>g opioid<br />
– D. Acupuncture
Verne (cont.)<br />
• 77‐year‐old man with PD and type 2 DM; he has burn<strong>in</strong>g and<br />
shoot<strong>in</strong>g pa<strong>in</strong> <strong>in</strong> both feet; his jo<strong>in</strong>ts ache—especially his hips<br />
and knees; pa<strong>in</strong> is bad at night, but can flare up first th<strong>in</strong>g <strong>in</strong><br />
the morn<strong>in</strong>g and also when he walks any distance<br />
• He was widowed <strong>in</strong> the past year and moved to an assisted<br />
liv<strong>in</strong>g i apartment; he has fll fallen a few times, susta<strong>in</strong><strong>in</strong>g i soft<br />
tissue <strong>in</strong>juries, but no fracture<br />
• Ibuprofen and acetam<strong>in</strong>ophen with code<strong>in</strong>e<br />
were <strong>in</strong>effective; hydrocodone/APAP made<br />
him confused and constipated<br />
• He jokes, “Might as well put me <strong>in</strong> the p<strong>in</strong>e<br />
box right now”<br />
Verne’s Exam<strong>in</strong>ation<br />
• Affect discordant with his depressed mood<br />
• Gait is shuffl<strong>in</strong>g and wide‐based with postural<br />
<strong>in</strong>stability<br />
• Jo<strong>in</strong>t deformities <strong>in</strong> the hands and knees<br />
consistent it twith OA<br />
• Sensory loss to p<strong>in</strong> and vibration <strong>in</strong> the feet and<br />
distal legs; positive Romberg’s sign; absent DTRs<br />
at the Achilles tendons;<br />
feet are sensitive to light touch<br />
• Sacral decubitus ulcer<br />
DM=diabetes mellitus. PD=Park<strong>in</strong>son’s disease.<br />
APAP=acetam<strong>in</strong>ophen.<br />
OA=osteoarthritis.<br />
DTRs=deep tendon reflexes.<br />
Pa<strong>in</strong> <strong>Types</strong> <strong>by</strong> Physiology<br />
Inflammation<br />
Bone<br />
Neuropathic<br />
Muscular<br />
Mechanical Psychogenic<br />
Cl<strong>in</strong>ical Features of<br />
Neuropathic Pa<strong>in</strong><br />
• Cl<strong>in</strong>ical sett<strong>in</strong>g<br />
– DM, MS, PD, HZV, sp<strong>in</strong>e surgery, CVA, HIV<br />
• Distribution<br />
• Quality and tim<strong>in</strong>g<br />
– Burn<strong>in</strong>g, freez<strong>in</strong>g, sear<strong>in</strong>g<br />
– Jabb<strong>in</strong>g, shock‐like, shoot<strong>in</strong>g<br />
– Spasm<br />
– Worse at night<br />
• Physical signs<br />
– Allodynia, hyperalgesia, cooler temperatures, pa<strong>in</strong><br />
with numbness<br />
MS=multiple sclerosis.<br />
CVA=cardiovascular accident.<br />
HIV=human immunodeficiency virus.<br />
HZV=herpes zoster virus.<br />
Contribut<strong>in</strong>g Factors and Barriers<br />
• Contribut<strong>in</strong>g factors amplify or perpetuate pa<strong>in</strong><br />
– Depression or anxiety<br />
– Posture<br />
– Intercurrent illness<br />
• Barriers <strong>in</strong>terfere with pa<strong>in</strong> assessment or with<br />
implement<strong>in</strong>g appropriate treatment<br />
– Insurance noncoverage/resource access<br />
– Low motivation<br />
– Chemical dependency<br />
– Language or communication difficulty<br />
– Conflict<strong>in</strong>g medical therapies<br />
Distribution of Neuropathic vs<br />
Nonneuropathic Pa<strong>in</strong><br />
A B C<br />
D E F G H<br />
Distribution (shaded areas) of neuropathic (A‐E) vs nonneuropathic (F‐H) pa<strong>in</strong> as depicted <strong>by</strong> patients <strong>in</strong> a pa<strong>in</strong> diagram.<br />
A=peripheral polyneuropathy. B=ulnar mononeuropathy. C=thoracic radiculopathy. D=lumbar radiculopathy. E=myelopathy.<br />
F=arthropathy. G=muscular pa<strong>in</strong>. H=mechanical low back pa<strong>in</strong>.<br />
Belgrade MJ. Postgrad Med. 1999;106(6):127-140.
Assess Disease Burden<br />
Verne’s <strong>Case</strong> <strong>Formulation</strong><br />
Priority<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Goals of Pa<strong>in</strong> Management <strong>in</strong><br />
Palliative Care vs <strong>Chronic</strong> Pa<strong>in</strong><br />
Return to work<br />
Self‐care<br />
Patient assumes responsibility for symptom management<br />
Increase activity<br />
Functional restoration<br />
M<strong>in</strong>imize healthcare utilization<br />
Comfort<br />
Support<br />
Ease pa<strong>in</strong>/suffer<strong>in</strong>g<br />
• Pa<strong>in</strong>ful diabetic neuropathy<br />
• Muscular dysfunction/pa<strong>in</strong> due to PD<br />
• OA<br />
• Inflammatory pa<strong>in</strong> due to decubitus ulcer<br />
• Contribut<strong>in</strong>g factors:<br />
– Grief and loss<br />
– Depression<br />
• Barriers<br />
– Bradyk<strong>in</strong>esia<br />
– Risk of falls<br />
– Intolerance to analgesics<br />
• Disease burden: fairly high—take mostly<br />
palliative approach<br />
Neuropathic Pa<strong>in</strong>—Treatment<br />
Neuropathic Pa<strong>in</strong><br />
Disease‐Specific Measures<br />
Glucose control<br />
Infection management<br />
MS treatment<br />
PD treatment<br />
CBT=cognitive behavioral therapy.<br />
Symptom<br />
Management<br />
Local/Regional Treatment<br />
Topical capsaic<strong>in</strong><br />
Topical lidoca<strong>in</strong>e<br />
Orthotics<br />
Assistive devices<br />
Epidural/<strong>in</strong>trathecal drug adm<strong>in</strong>istration<br />
Nerve root blocks<br />
Sympathetic blocks<br />
Systemic Treatment<br />
Drugs<br />
Behavioral<br />
Treatment<br />
Relaxation<br />
Hypnosis<br />
Meditation<br />
CBT<br />
Systemic Drugs<br />
for Neuropathic Pa<strong>in</strong><br />
• Anticonvulsants<br />
– Gabapent<strong>in</strong><br />
– Pregabal<strong>in</strong><br />
– Lamotrig<strong>in</strong>e<br />
– Topiramate<br />
• SNRIs<br />
– Duloxet<strong>in</strong>e<br />
– Venlafax<strong>in</strong>e<br />
• TCAs<br />
– Amitriptyl<strong>in</strong>e, nortriptyl<strong>in</strong>e,<br />
desipram<strong>in</strong>e<br />
• Opioids<br />
– Oxycodone<br />
– Tramadol<br />
– Methadone<br />
• NMDA blockers<br />
– Ketam<strong>in</strong>e<br />
– Amantad<strong>in</strong>e<br />
– Memant<strong>in</strong>e<br />
• Dopam<strong>in</strong>e agonists<br />
– Pramipexole<br />
• Alpha‐2‐adrenergic<br />
agonists<br />
– Clonid<strong>in</strong>e<br />
– Dexmedetomid<strong>in</strong>e<br />
• N‐type calcium<br />
channel blocker<br />
– Ziconotide<br />
NMDA=N-methyl-D-aspartate. SNRIs=seroton<strong>in</strong>-norep<strong>in</strong>ephr<strong>in</strong>e reuptake <strong>in</strong>hibitors.<br />
TCAs=tricyclic antidepressants.<br />
This <strong>in</strong>formation <strong>in</strong>cludes a use that has not been approved <strong>by</strong> the US FDA.<br />
Verne’s Plan of Care<br />
• For DPNP<br />
– Optimize glucose control<br />
– Duloxet<strong>in</strong>e or venlafax<strong>in</strong>e*<br />
– Recommend a walker<br />
– Check and optimize<br />
shoe wear<br />
– Tramadol for pa<strong>in</strong> flares<br />
• For OA<br />
– Glucosam<strong>in</strong>e supplement<br />
– Scheduled acetam<strong>in</strong>ophen<br />
or NSAID<br />
– Acupuncture<br />
• For muscular pa<strong>in</strong><br />
– Pool therapy<br />
*Duloxet<strong>in</strong>e and venlafax<strong>in</strong>e are the choice for this patient,<br />
but other neuropathic pa<strong>in</strong> medications may also substitute for these choices.<br />
DPNP=diabetic peripheral neuropathic pa<strong>in</strong>.<br />
NSAID=non-steroidal anti-<strong>in</strong>flammatory drugs.<br />
• For decubitus ulcer<br />
– Topical morph<strong>in</strong>e<br />
– Local wound care<br />
– Evaluation of sleep surface<br />
• For contribut<strong>in</strong>g factors:<br />
grief/loss/depression<br />
– Duloxet<strong>in</strong>e or venlafax<strong>in</strong>e* lf – Pool therapy <strong>in</strong> group sett<strong>in</strong>g<br />
– Grief group if Verne<br />
is amenable<br />
• Manage barriers:<br />
– Manage PD (pramipexole)<br />
– (Walker)<br />
– Choose <strong>in</strong>termediate analgesic<br />
(tramadol)<br />
Summary<br />
• Assess for the 4 card<strong>in</strong>al physiologic types of<br />
pa<strong>in</strong>: nociceptive, neuropathic,<br />
muscle, bone<br />
• Determ<strong>in</strong>e disease burden to pick goals of<br />
treatment on the spectrum of restorative<br />
to palliative<br />
• Identify and manage contribut<strong>in</strong>g factors and<br />
barriers<br />
• Choose neuropathic pa<strong>in</strong> treatments that attend<br />
to the comorbidities
Nikki<br />
• Ms. N is a 27‐year‐old female with systemic lupus erythematosis<br />
and renal osteodystrophy with a history of multiple fractures and<br />
mechanical abnormalities contribut<strong>in</strong>g to multiregional jo<strong>in</strong>t, bone,<br />
and muscular pa<strong>in</strong>.<br />
• She is on chronic hemodialysis for end‐stage renal disease. She has<br />
chronic pa<strong>in</strong> <strong>in</strong> her shoulders, back, hips, and both legs <strong>in</strong> addition to<br />
daily headaches. She has severe hear<strong>in</strong>g impairment and is bl<strong>in</strong>d <strong>in</strong><br />
one eye from <strong>in</strong>fection.<br />
• She lives with her mother, sister, and niece and spends most of her<br />
time at home watch<strong>in</strong>g television. She receives social security<br />
disability <strong>in</strong>come.<br />
• Communication is also difficult because she is hostile toward the<br />
cl<strong>in</strong>icians. She has been unreliable with adher<strong>in</strong>g to physician<br />
recommendations <strong>in</strong> the past.<br />
Nikki<br />
• Ms. N’s primary physician prescribes hydrocodone/acetam<strong>in</strong>ophen 5<br />
mg/500 mg every 4 h as needed. She says she takes about six to<br />
eight tablets per day but it is not controll<strong>in</strong>g the pa<strong>in</strong>.<br />
• The physician suspects she is abus<strong>in</strong>g opioids because of lost<br />
prescriptions and requests for early prescriptions and for<br />
“someth<strong>in</strong>g stronger.”<br />
• She uses doses of hydroxyz<strong>in</strong>e hd for uncontrolled itch<strong>in</strong>g regularly. l She<br />
had previously tried nonsteroidal anti<strong>in</strong>flammatory drugs (NSAIDs),<br />
antidepressants, and diazepam without relief.<br />
• She tried biofeedback, chiropractic care, Transcutaneous Electrical<br />
Nerve Stimulation (TENS), and counsel<strong>in</strong>g, but she is currently only<br />
utiliz<strong>in</strong>g medications.<br />
• She has moderate lip read<strong>in</strong>g ability and limited hear<strong>in</strong>g. Her<br />
mother is present and appears to be an exhausted caregiver and<br />
advocate.<br />
Nikki<br />
• On physical exam<strong>in</strong>ation, Ms. N presents as a young<br />
woman of short stature, her physician has to repeat<br />
th<strong>in</strong>gs over and over before she understands.<br />
• She is completely bl<strong>in</strong>d <strong>in</strong> the right eye. Her sk<strong>in</strong> is<br />
excoriated <strong>in</strong> places where she scratches. There are<br />
deformities of the long bones at sites of healed old<br />
fractures. She has multiple tender po<strong>in</strong>ts on the neck,<br />
back, and limbs.<br />
• She can walk <strong>in</strong>dependently. She has peripheral<br />
neuropathy with a stock<strong>in</strong>g distribution loss of p<strong>in</strong>prick<br />
and vibratory senses and absent deep tendon reflexes.<br />
Nikki’s Pa<strong>in</strong> Assessment<br />
• What is/are the physiologic types of pa<strong>in</strong><br />
• What is the temporal type of pa<strong>in</strong><br />
• Identify contribut<strong>in</strong>g factors and barriers<br />
• Determ<strong>in</strong>e the disease burden<br />
• Develop a treatment strategy<br />
• Is Nikki a candidate for long‐term opioid<br />
analgesics What is her DIRE Score
D.I.R.E. Score: Patient Selection for <strong>Chronic</strong> Opioid Analgesia<br />
For each factor, rate the patient’s score from 1-3 based on the<br />
explanations <strong>in</strong> the right hand column<br />
Score Factor Explanation<br />
Diagnosis<br />
Intractability<br />
Risk<br />
Psychological:<br />
Chemical Health:<br />
Reliability:<br />
Social Support:<br />
1 = Benign chronic condition with m<strong>in</strong>imal objective f<strong>in</strong>d<strong>in</strong>gs or no def<strong>in</strong>ite<br />
medical diagnosis. Examples: fibromyalgia, migra<strong>in</strong>e headaches, nonspecific<br />
back pa<strong>in</strong>.<br />
2 = Slowly progressive condition concordant with moderate pa<strong>in</strong>, or fixed<br />
condition with moderate objective f<strong>in</strong>d<strong>in</strong>gs. Examples: failed back surgery<br />
syndrome, back pa<strong>in</strong> with moderate degenerative changes, neuropathic pa<strong>in</strong>.<br />
3 = Advanced condition concordant with severe pa<strong>in</strong> with objective f<strong>in</strong>d<strong>in</strong>gs.<br />
Examples: severe ischemic vascular disease, advanced neuropathy, severe<br />
sp<strong>in</strong>al stenosis.<br />
1 = Few therapies have been tried and the patient takes a passive role <strong>in</strong><br />
his/her pa<strong>in</strong> management process.<br />
2 = Most customary treatments have been tried but the patient is not fully<br />
engaged <strong>in</strong> the pa<strong>in</strong> management process, or barriers prevent (<strong>in</strong>surance,<br />
transportation, medical illness).<br />
3 = Patient fully engaged <strong>in</strong> a spectrum of appropriate treatments but with<br />
<strong>in</strong>adequate response.<br />
(R= Total of P+C+R+S below)<br />
1 = Serious personality dysfunction or mental illness <strong>in</strong>terfer<strong>in</strong>g with care.<br />
Example: personality disorder, severe affective disorder, significant<br />
personality issues.<br />
2 = Personality or mental health <strong>in</strong>terferes moderately. Example: depression<br />
or anxiety disorder.<br />
3 = Good communication with cl<strong>in</strong>ic. No significant personality dysfunction or<br />
mental illness.<br />
1 = Active or very recent use of illicit drugs, excessive alcohol, or prescription<br />
drug abuse.<br />
2 = Chemical coper (uses medications to cope with stress) or history of CD <strong>in</strong><br />
remission.<br />
3 = No CD history. Not drug-focused or chemically reliant.<br />
1 = History of numerous problems: medication misuse, missed appo<strong>in</strong>tments,<br />
rarely follows through.<br />
2 = Occasional difficulties with compliance, but generally reliable.<br />
3 = Highly reliable patient with meds, appo<strong>in</strong>tments & treatment.<br />
1 = Life <strong>in</strong> chaos. Little family support and few close relationships. Loss of<br />
most normal life roles.<br />
2 = Reduction <strong>in</strong> some relationships and life roles.<br />
3 = Supportive family/close relationships. Involved <strong>in</strong> work or school and no<br />
social isolation.<br />
Efficacy score<br />
1 = Poor function or m<strong>in</strong>imal pa<strong>in</strong> relief despite moderate to high doses.<br />
2 = Moderate benefit with function improved <strong>in</strong> a number of ways (or<br />
<strong>in</strong>sufficient <strong>in</strong>fo- hasn’t tried opioid yet or very low doses or too short of a<br />
trial).<br />
3 = Good improvement <strong>in</strong> pa<strong>in</strong> and function and quality of life with stable<br />
doses over time.<br />
______Total score = D + I + R + E<br />
Score 7-13: Not a suitable candidate for long-term opioid analgesia<br />
Score 14-21: Good candidate for long-term opioid analgesia