Classification of dental cements - VoWi
Classification of dental cements - VoWi
Classification of dental cements - VoWi
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
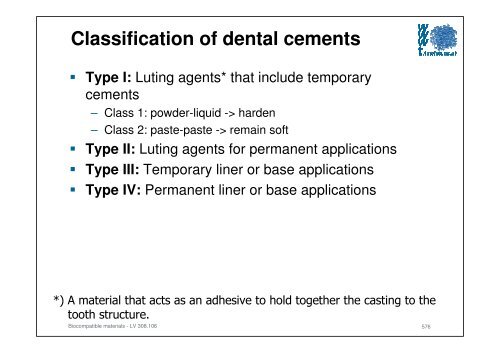
<strong>Classification</strong> <strong>of</strong> <strong>dental</strong> <strong>cements</strong><br />
Type I: Luting agents* that include temporary<br />
<strong>cements</strong><br />
– Class 1: powder-liquid -> harden<br />
– Class 2: paste-paste -> remain s<strong>of</strong>t<br />
Type II: Luting agents for permanent applications<br />
Type III: Temporary liner or base applications<br />
Type IV: Permanent liner or base applications<br />
*) A material that acts as an adhesive to hold together the casting to the<br />
tooth structure.<br />
Biocompatible materials - LV 308.106<br />
576
Applications <strong>of</strong> <strong>dental</strong> <strong>cements</strong><br />
• Underfilling or liner<br />
(materials for protection<br />
<strong>of</strong> <strong>dental</strong> pulp against mechanical and chemical )<br />
· Temporary filling<br />
· Cover filling (inserted into a prepared cavity in a<br />
tooth = Filling in general)<br />
· Temporary or long-life anchorage<br />
for coronas or filling in root channels<br />
· Healing <strong>cements</strong>, e.g. <strong>dental</strong> zinc oxide eugenol<br />
cement which is used as temporary sealing material<br />
having a anodyne , sedative and antiphlogistic<br />
effect upon oral disease<br />
Biocompatible materials - LV 308.106<br />
577
Requirements for <strong>dental</strong> <strong>cements</strong><br />
Good thermal, chemical and bacterial isolation<br />
No or low toxicity<br />
Low or no tissue irritating effects<br />
Mechanical strength<br />
Chemical resistance<br />
Good sealing and adhesion properties<br />
No or low electrical conductivity<br />
Low film thickness<br />
Adaptable colour, haze ...<br />
Good processability<br />
x-ray opacity<br />
Biocompatible materials - LV 308.106<br />
578
ROOT CANAL FILLING MATERIALS<br />
Root canal filling materials consist <strong>of</strong><br />
– tapered gutta-percha (right root) or<br />
– silver (left root) (or titanium or polymer coated gutta-percha)<br />
points<br />
in standard sizes that match the size <strong>of</strong> the files used.<br />
The points are cemented in place with root canal sealer<br />
that is usually a zinc oxide and eugenol preparation.<br />
Root canal filling materials are used to fill previously<br />
prepared root canals. They are a part <strong>of</strong> root canal, or<br />
endodontic, therapy.<br />
www.free-ed.net/sweethaven/MedTech/Dental/DentMat/lessonMain.aspiNum=fra0208<br />
Biocompatible materials - LV 308.106<br />
579
GUTTA-PERCHA POINTS<br />
Gutta-percha points are made from the refined, coagulated, milky exudate <strong>of</strong><br />
trees in the Malay peninsula. Gutta-percha is pink or gray in color. It is<br />
s<strong>of</strong>tened by heat and is easily molded. When cool, gutta-percha maintains its<br />
shape. Gutta-percha points are used as a root canal filling material.<br />
Advantages<br />
(1) They have a high thermal expansion.<br />
(2) They do not shrink unless used with solvent.<br />
(3) They are radiopaque, conduct heat poorly, and<br />
are easy to remove from the root canal.<br />
(4) They may be kept sterile in antiseptic solution, are<br />
impervious to moisture, and are bacteriostatic<br />
(prevent the growth or multiplication <strong>of</strong> bacteria).<br />
www.synca.com<br />
Disadvantages<br />
(1) They shrink when used with a solvent.<br />
(2) They are not always easy to introduce into the root canal.<br />
www.free-ed.net/sweethaven/MedTech/Dental/DentMat/lessonMain.aspiNum=fra0209<br />
Biocompatible materials - LV 308.106<br />
580
SILVER ROOT CANAL POINTS<br />
The dentist has the option to use silver root canal points in<br />
filling a root canal.<br />
Advantages<br />
(1) They are more easily inserted than gutta-percha points<br />
and they have all the same advantages.<br />
(2) Sight selection <strong>of</strong> silver points is easy because they come<br />
in the same sizes and tapers as standard<br />
root canal broaches and reamers.<br />
Disadvantages<br />
(1) They are more expensive than gutta-percha.<br />
(2) They do not adapt to contours <strong>of</strong> the root canal.<br />
(3) They tend to corrode if subjected to body fluids.<br />
www.free-ed.net/sweethaven/MedTech/Dental/DentMat/lessonMain.aspiNum=fra0210<br />
Biocompatible materials - LV 308.106<br />
581
Dental impression<br />
Impression<br />
materials<br />
rigid<br />
flexible<br />
irreversible<br />
reversible<br />
irreversible<br />
reversible<br />
ZnO-Eugenol<br />
paste,<br />
Plaster<br />
Thermoplastic<br />
compositon mass<br />
e.g. Guttapercha,<br />
Stent's, Kerr, Waxes<br />
Elastomers<br />
Alginate<br />
Hydrocolloids<br />
Polysulfide<br />
(Thiocols)<br />
Polyether<br />
Silicones<br />
condensation<br />
crosslinked<br />
addition<br />
crosslinked<br />
582
Processing <strong>of</strong> Elastic<br />
Impression Materials – Volume Effects<br />
Curing shrinkage<br />
Thermal shrinkage<br />
Storage time dependent shrinkage<br />
Biocompatible materials - LV 308.106<br />
583
Processing <strong>of</strong> Elastic<br />
Impression Materials – Volume Effects<br />
Biocompatible materials - LV 308.106<br />
(R. Marxkors/H. Meiners, 1993)<br />
584
Artificial teeth<br />
www.trubyte.dentsply.com<br />
Biocompatible materials - LV 308.106<br />
585
Artificial Teeth<br />
Waxs model<br />
Metal cuvette<br />
Hard plaster<br />
Functioning model<br />
Cut through a two-sectioned cuvette with embedded wax model on the functioning<br />
model<br />
Biocompatible materials - LV 308.106<br />
(R. Marxkors/H. Meiners, 1993)<br />
586
Artificial Teeth<br />
State <strong>of</strong> a thermoplastic material in dependence on the polymerisation<br />
grade<br />
degree <strong>of</strong> polymerisation<br />
Biocompatible materials - LV 308.106<br />
(R. Marxkors/H. Meiners, 1993)<br />
587
Artificial Teeth<br />
Processing<br />
Powder-liquid-technique: Pearl polymer: Monomer 2 : 1<br />
Micrograph (grinded) <strong>of</strong> a Powder-Liquid Technique Polymerised Acrylate, Etched (75x)<br />
Biocompatible materials - LV 308.106<br />
(R. Marxkors/H. Meiners, 1993)<br />
588
Artificial Teeth<br />
Hot polymerisation<br />
<br />
<br />
<br />
Initiation by temperature increasing<br />
Heating by a water bath<br />
Residue monomer!<br />
– Short time procedure:<br />
30 min heating, 30 min holding time at 100 °C<br />
– Medium time procedure:<br />
60 min at 75 °C, 30 min at 100 °C<br />
– Long time procedure:<br />
12 h at 50 °C, 2 h at 120 °C<br />
Biocompatible materials - LV 308.106<br />
(R. Marxkors/H. Meiners, 1993)<br />
589
Artificial Teeth<br />
Auto polymerisation<br />
Initiation by reduction agent<br />
Faster than hot polymerisation procedure<br />
Use <strong>of</strong> very fine grained powder<br />
Continuous change in residual monomer content<br />
Biocompatible materials - LV 308.106<br />
(R. Marxkors/H. Meiners, 1993)<br />
590
Dental Implants<br />
worl<strong>dental</strong>.org/images<br />
Biocompatible materials - LV 308.106<br />
591
Conditions<br />
„Biological system“<br />
– State <strong>of</strong> the bone and the s<strong>of</strong>t tissues<br />
i.e., height and width <strong>of</strong> the jaw bone: the higher and<br />
thicker the better the conditions for a successful<br />
implantation<br />
Width < 5 mm and height < 8 ... 10 mm are critical<br />
dimensions because bone volume (mass) is to small<br />
for holding an implant<br />
Biocompatible materials - LV 308.106<br />
592
Conditions<br />
Sufficient bone density<br />
Gums (or Gingiva) state:<br />
– Healthy s<strong>of</strong>t tissue support for the implant<br />
and the supra construction<br />
Position <strong>of</strong> the upper jaw in relation to the<br />
lower jaw<br />
– Deflection against ideal position can lead to<br />
loadings that can not be compensated by the<br />
materials and/or the design<br />
Biocompatible materials - LV 308.106<br />
593
Caution!<br />
– Implantation site in the upper jaw<br />
The bone <strong>of</strong> the upper jaw flanks the<br />
maxillary sinus that is connected with<br />
the nose<br />
-> inflammation and implant loss if the<br />
implant penetrates the mucous<br />
membrane <strong>of</strong> the maxillary sinus<br />
Nervus<br />
mandibularis<br />
Biocompatible materials - LV 308.106<br />
- Implantation site in the lower jaw<br />
N. mandibularis locates along the side<br />
<strong>of</strong> <strong>of</strong> the lower jaw<br />
-> numbness in the lower lip and the<br />
chin if this nerve is injured during the<br />
operation<br />
Maxillary sinus<br />
594
Dental implants - Types<br />
Transosseous implants:<br />
– Only used in mandibles<br />
– These implants are inserted in the jawbone, and penetrate the<br />
whole jaw -> anchoring at the bottom <strong>of</strong> the chin by means <strong>of</strong> a<br />
pressure plate<br />
– Disadvantage: general anaesthesia owing to the extraoral surgical<br />
approach for placement -> longer hospitalisation; bone degradation<br />
around the posts<br />
– Materials: CoCr-alloys, CP Ti and gold<br />
Biocompatible materials - LV 308.106<br />
595
Dental implants - Types<br />
Subperiostal implants:<br />
– These implants are inserted between the top <strong>of</strong> the jawbone (onthe-bone)<br />
and the gum<br />
– Long-time behaviour: the implants have to be replaced after some<br />
years (in most <strong>of</strong> the patients) 5 years upper jaw, 10 years lower jaw<br />
– Cause: chronic inflammation around the implant posts and<br />
loosening over time<br />
Inflammation -> bone degradation + support removal by surgery -><br />
crater shaped damage <strong>of</strong> the jaw -> afterwards problems with<br />
removable denture<br />
Biocompatible materials - LV 308.106<br />
596
Dental implant - Types<br />
Endosteal (endosseous) implants:<br />
– The implants are completely integrated in the jaw (feel and function<br />
like natural teeth)<br />
– proper conditions <strong>of</strong> material selection, design and use -><br />
Osseointegration = bone tissue grows around the implant and<br />
provides anchorage<br />
– most frequent <strong>dental</strong> implants today<br />
Blade, disc, cylinder or screw implants from titanium or metal<br />
alloys with ceramic coating, ceramics<br />
Biocompatible materials - LV 308.106<br />
597
Osseintegration<br />
Biocompatible materials - LV 308.106<br />
(J.B. Park, Bioceramics, 2008)<br />
598
Endosteal Implant Types<br />
Lower jaw without teeth and applied<br />
blade implant<br />
Screw and cylinder implants (Ti)<br />
www.3d-machining.com/3dmedicalspeciality.html<br />
www.implantat-wissen.de<br />
disc implant<br />
www.implantat-wissen.de<br />
Biocompatible materials - LV 308.106<br />
osseosource.com/<strong>dental</strong>-implants<br />
Customised ZrO 2 <strong>dental</strong> implant in comparison<br />
with a conventional implant. Dental Tribune<br />
Austrian Edition, 12/2008, pp 9-12<br />
www.bioimplant.at/index-<br />
Dateien/BioImplantSurgeryVideos.htm<br />
599
Implant Components<br />
Biocompatible materials - LV 308.106<br />
www.<strong>dental</strong>clinicdelhi.com/implants.htm<br />
600
Implantation<br />
2 steps<br />
– 1. Anchorage <strong>of</strong> the implant in the jaw followed by a healing phase<br />
(≈ 4 month lower jaw, 6 month upper jaw)<br />
www.implantat-wissen.de<br />
– 2. Application <strong>of</strong> the superstructure system: crown, bridge, denture<br />
Biocompatible materials - LV 308.106<br />
www.implantat-wissen.de<br />
601
Implant solutions<br />
Biocompatible materials - LV 308.106<br />
www.commerceimplants.com/<strong>dental</strong>-implant-solutions.html<br />
602