Continuous Validity of Pedicled Myocutaneous and Myofascial ... - NCI
Continuous Validity of Pedicled Myocutaneous and Myofascial ... - NCI
Continuous Validity of Pedicled Myocutaneous and Myofascial ... - NCI
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
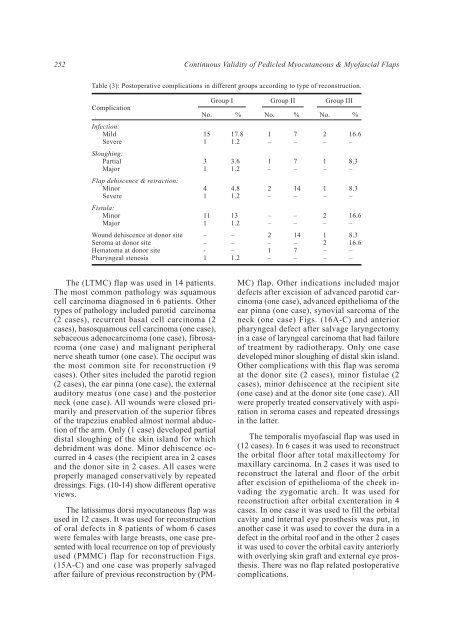
252<br />
<strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
Table (3): Postoperative complications in different groups according to type <strong>of</strong> reconstruction.<br />
Complication<br />
No.<br />
Group I<br />
%<br />
No.<br />
Group II<br />
%<br />
No.<br />
Group III<br />
%<br />
Infection:<br />
Mild<br />
Severe<br />
15<br />
1<br />
17.8<br />
1.2<br />
1<br />
–<br />
7<br />
–<br />
2<br />
–<br />
16.6<br />
–<br />
Sloughing:<br />
Partial<br />
Major<br />
3<br />
1<br />
3.6<br />
1.2<br />
1<br />
–<br />
7<br />
–<br />
1<br />
–<br />
8.3<br />
–<br />
Flap dehiscence & retraction:<br />
Minor<br />
Severe<br />
4<br />
1<br />
4.8<br />
1.2<br />
2<br />
–<br />
14<br />
–<br />
1<br />
–<br />
8.3<br />
–<br />
Fistula:<br />
Minor<br />
Major<br />
11<br />
1<br />
13<br />
1.2<br />
–<br />
–<br />
–<br />
–<br />
2<br />
–<br />
16.6<br />
–<br />
Wound dehiscence at donor site<br />
Seroma at donor site<br />
Hematoma at donor site<br />
Pharyngeal stenosis<br />
–<br />
–<br />
-<br />
1<br />
–<br />
–<br />
–<br />
1.2<br />
2<br />
–<br />
1<br />
–<br />
14<br />
–<br />
7<br />
–<br />
1<br />
2<br />
–<br />
–<br />
8.3<br />
16.6<br />
–<br />
–<br />
The (LTMC) flap was used in 14 patients.<br />
The most common pathology was squamous<br />
cell carcinoma diagnosed in 6 patients. Other<br />
types <strong>of</strong> pathology included parotid carcinoma<br />
(2 cases), recurrent basal cell carcinoma (2<br />
cases), basosquamous cell carcinoma (one case),<br />
sebaceous adenocarcinoma (one case), fibrosarcoma<br />
(one case) <strong>and</strong> malignant peripheral<br />
nerve sheath tumor (one case). The occiput was<br />
the most common site for reconstruction (9<br />
cases). Other sites included the parotid region<br />
(2 cases), the ear pinna (one case), the external<br />
auditory meatus (one case) <strong>and</strong> the posterior<br />
neck (one case). All wounds were closed primarily<br />
<strong>and</strong> preservation <strong>of</strong> the superior fibres<br />
<strong>of</strong> the trapezius enabled almost normal abduction<br />
<strong>of</strong> the arm. Only (1 case) developed partial<br />
distal sloughing <strong>of</strong> the skin isl<strong>and</strong> for which<br />
debridment was done. Minor dehiscence occurred<br />
in 4 cases (the recipient area in 2 cases<br />
<strong>and</strong> the donor site in 2 cases. All cases were<br />
properly managed conservatively by repeated<br />
dressings. Figs. (10-14) show different operative<br />
views.<br />
The latissimus dorsi myocutaneous flap was<br />
used in 12 cases. It was used for reconstruction<br />
<strong>of</strong> oral defects in 8 patients <strong>of</strong> whom 6 cases<br />
were females with large breasts, one case presented<br />
with local recurrence on top <strong>of</strong> previously<br />
used (PMMC) flap for reconstruction Figs.<br />
(15A-C) <strong>and</strong> one case was properly salvaged<br />
after failure <strong>of</strong> previous reconstruction by (PM-<br />
MC) flap. Other indications included major<br />
defects after excision <strong>of</strong> advanced parotid carcinoma<br />
(one case), advanced epithelioma <strong>of</strong> the<br />
ear pinna (one case), synovial sarcoma <strong>of</strong> the<br />
neck (one case) Figs. (16A-C) <strong>and</strong> anterior<br />
pharyngeal defect after salvage laryngectomy<br />
in a case <strong>of</strong> laryngeal carcinoma that had failure<br />
<strong>of</strong> treatment by radiotherapy. Only one case<br />
developed minor sloughing <strong>of</strong> distal skin isl<strong>and</strong>.<br />
Other complications with this flap was seroma<br />
at the donor site (2 cases), minor fistulae (2<br />
cases), minor dehiscence at the recipient site<br />
(one case) <strong>and</strong> at the donor site (one case). All<br />
were properly treated conservatively with aspiration<br />
in seroma cases <strong>and</strong> repeated dressings<br />
in the latter.<br />
The temporalis my<strong>of</strong>ascial flap was used in<br />
(12 cases). In 6 cases it was used to reconstruct<br />
the orbital floor after total maxillectomy for<br />
maxillary carcinoma. In 2 cases it was used to<br />
reconstruct the lateral <strong>and</strong> floor <strong>of</strong> the orbit<br />
after excision <strong>of</strong> epithelioma <strong>of</strong> the cheek invading<br />
the zygomatic arch. It was used for<br />
reconstruction after orbital exenteration in 4<br />
cases. In one case it was used to fill the orbital<br />
cavity <strong>and</strong> internal eye prosthesis was put, in<br />
another case it was used to cover the dura in a<br />
defect in the orbital ro<strong>of</strong> <strong>and</strong> in the other 2 cases<br />
it was used to cover the orbital cavity anteriorly<br />
with overlying skin graft <strong>and</strong> external eye prosthesis.<br />
There was no flap related postoperative<br />
complications.