Continuous Validity of Pedicled Myocutaneous and Myofascial ... - NCI
Continuous Validity of Pedicled Myocutaneous and Myofascial ... - NCI
Continuous Validity of Pedicled Myocutaneous and Myofascial ... - NCI
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
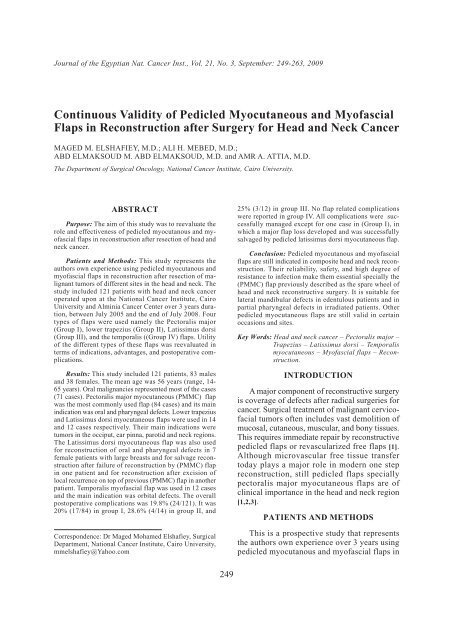
Journal <strong>of</strong> the Egyptian Nat. Cancer Inst., Vol. 21, No. 3, September: 249-263, 2009<br />
<strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> <strong>and</strong> My<strong>of</strong>ascial<br />
Flaps in Reconstruction after Surgery for Head <strong>and</strong> Neck Cancer<br />
MAGED M. ELSHAFIEY, M.D.; ALI H. MEBED, M.D.;<br />
ABD ELMAKSOUD M. ABD ELMAKSOUD, M.D. <strong>and</strong> AMR A. ATTIA, M.D.<br />
The Department <strong>of</strong> Surgical Oncology, National Cancer Institute, Cairo University.<br />
ABSTRACT<br />
Purpose: The aim <strong>of</strong> this study was to reevaluate the<br />
role <strong>and</strong> effectiveness <strong>of</strong> pedicled myocutanous <strong>and</strong> my<strong>of</strong>ascial<br />
flaps in reconstruction after resection <strong>of</strong> head <strong>and</strong><br />
neck cancer.<br />
Patients <strong>and</strong> Methods: This study represents the<br />
authors own experience using pedicled myocutanous <strong>and</strong><br />
my<strong>of</strong>ascial flaps in reconstruction after resection <strong>of</strong> malignant<br />
tumors <strong>of</strong> different sites in the head <strong>and</strong> neck. The<br />
study included 121 patients with head <strong>and</strong> neck cancer<br />
operated upon at the National Cancer Institute, Cairo<br />
University <strong>and</strong> Alminia Cancer Center over 3 years duration,<br />
between July 2005 <strong>and</strong> the end <strong>of</strong> July 2008. Four<br />
types <strong>of</strong> flaps were used namely the Pectoralis major<br />
(Group I), lower trapezius (Group II), Latissimus dorsi<br />
(Group III), <strong>and</strong> the temporalis ((Group IV) flaps. Utility<br />
<strong>of</strong> the different types <strong>of</strong> these flaps was reevaluated in<br />
terms <strong>of</strong> indications, advantages, <strong>and</strong> postoperative complications.<br />
Results: This study included 121 patients, 83 males<br />
<strong>and</strong> 38 females. The mean age was 56 years (range, 14-<br />
65 years). Oral malignancies represented most <strong>of</strong> the cases<br />
(71 cases). Pectoralis major myocutaneous (PMMC) flap<br />
was the most commonly used flap (84 cases) <strong>and</strong> its main<br />
indication was oral <strong>and</strong> pharyngeal defects. Lower trapezius<br />
<strong>and</strong> Latissimus dorsi myocutaneous flaps were used in 14<br />
<strong>and</strong> 12 cases respectively. Their main indications were<br />
tumors in the occiput, ear pinna, parotid <strong>and</strong> neck regions.<br />
The Latissimus dorsi myocutaneous flap was also used<br />
for reconstruction <strong>of</strong> oral <strong>and</strong> pharyngeal defects in 7<br />
female patients with large breasts <strong>and</strong> for salvage reconstruction<br />
after failure <strong>of</strong> reconstruction by (PMMC) flap<br />
in one patient <strong>and</strong> for reconstruction after excision <strong>of</strong><br />
local recurrence on top <strong>of</strong> previous (PMMC) flap in another<br />
patient. Temporalis my<strong>of</strong>ascial flap was used in 12 cases<br />
<strong>and</strong> the main indication was orbital defects. The overall<br />
postoperative complications was 19.8% (24/121). It was<br />
20% (17/84) in group I, 28.6% (4/14) in group II, <strong>and</strong><br />
Correspondence: Dr Maged Mohamed Elshafiey, Surgical<br />
Department, National Cancer Institute, Cairo University,<br />
mmelshafiey@Yahoo.com<br />
25% (3/12) in group III. No flap related complications<br />
were reported in group IV. All complications were successfully<br />
managed except for one case in (Group I), in<br />
which a major flap loss developed <strong>and</strong> was successfully<br />
salvaged by pedicled latissimus dorsi myocutaneous flap.<br />
Conclusion: <strong>Pedicled</strong> myocutanous <strong>and</strong> my<strong>of</strong>ascial<br />
flaps are still indicated in composite head <strong>and</strong> neck reconstruction.<br />
Their reliability, safety, <strong>and</strong> high degree <strong>of</strong><br />
resistance to infection make them essential specially the<br />
(PMMC) flap previously described as the spare wheel <strong>of</strong><br />
head <strong>and</strong> neck reconstructive surgery. It is suitable for<br />
lateral m<strong>and</strong>ibular defects in edentulous patients <strong>and</strong> in<br />
partial pharyngeal defects in irradiated patients. Other<br />
pedicled myocutaneous flaps are still valid in certain<br />
occasions <strong>and</strong> sites.<br />
Key Words: Head <strong>and</strong> neck cancer – Pectoralis major –<br />
Trapezius – Latissimus dorsi – Temporalis<br />
myocutaneous – My<strong>of</strong>ascial flaps – Reconstruction.<br />
INTRODUCTION<br />
A major component <strong>of</strong> reconstructive surgery<br />
is coverage <strong>of</strong> defects after radical surgeries for<br />
cancer. Surgical treatment <strong>of</strong> malignant cervic<strong>of</strong>acial<br />
tumors <strong>of</strong>ten includes vast demolition <strong>of</strong><br />
mucosal, cutaneous, muscular, <strong>and</strong> bony tissues.<br />
This requires immediate repair by reconstructive<br />
pedicled flaps or revascularized free flaps [1].<br />
Although microvascular free tissue transfer<br />
today plays a major role in modern one step<br />
reconstruction, still pedicled flaps specially<br />
pectoralis major myocutaneous flaps are <strong>of</strong><br />
clinical importance in the head <strong>and</strong> neck region<br />
[1,2,3].<br />
PATIENTS AND METHODS<br />
This is a prospective study that represents<br />
the authors own experience over 3 years using<br />
pedicled myocutanous <strong>and</strong> my<strong>of</strong>ascial flaps in<br />
249
250<br />
<strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
reconstruction after resection <strong>of</strong> malignant tumors<br />
<strong>of</strong> different sites in the head <strong>and</strong> neck.<br />
The study included 121 patients with head <strong>and</strong><br />
neck cancer operated upon at the National Cancer<br />
Institute, Cairo University <strong>and</strong> Alminia<br />
Cancer Center over 3 years duration, between<br />
July 2005 <strong>and</strong> the end <strong>of</strong> July 2008.<br />
One hundred <strong>and</strong> 2 cases receieved no previous<br />
treatment while 19 cases presented with<br />
recurrent or persistent disease after previous<br />
treatment by surgery alone in 3 cases, combined<br />
surgery <strong>and</strong> radiotherapy in 4 cases <strong>and</strong> radiotherapy<br />
alone in 12 cases.<br />
Preoperative medical assessment included<br />
routine complete blood picture, liver <strong>and</strong> kidney<br />
functions, fasting blood sugar, bleeding <strong>and</strong><br />
coagulation pr<strong>of</strong>ile <strong>and</strong> cardiological assessment.<br />
All the patients were biopsied before<br />
surgery <strong>and</strong> pathological diagnosis was obtained.<br />
The stage <strong>of</strong> the disease was evaluated by<br />
clinical assessment, locoregional (CT or MRI),<br />
routine CXR <strong>and</strong> other metastatic workup as<br />
indicated.<br />
The extent <strong>of</strong> surgical resection <strong>and</strong> the<br />
technique <strong>of</strong> reconstruction with its potential<br />
complications were discussed preoperatively<br />
with the patient with combined signed consent<br />
by the patient <strong>and</strong> the surgeon performing the<br />
operation.<br />
Four types <strong>of</strong> pedicled flaps were used for<br />
reconstruction namely the Pectoralis major<br />
myocutaneous (PMMC) flap (Group I), lower<br />
trapezius myocutaneous flap (LTMC) flap<br />
(Group II), Latissimus dorsi myocutaneous flap<br />
(Group III) <strong>and</strong> the Temporalis my<strong>of</strong>ascial flap<br />
(Group IV). Immediate reconstruction after<br />
resection was done in 110 cases while delayed<br />
reconstruction <strong>of</strong> anterior pharyngeal defects<br />
after total laryngectomy was done in 11 cases.<br />
In one case in (Group I), major flap loss developed<br />
<strong>and</strong> was successfully salvaged by pedicled<br />
latissimus dorsi myocutaneous flap.<br />
Patients were followed-up in the outpatient<br />
clinic for detection <strong>of</strong> local or distant recurrences<br />
by clinical examination <strong>and</strong> radiological assessment<br />
as indicated <strong>and</strong> for assessment <strong>of</strong> the<br />
final functional <strong>and</strong> aesthetic results.<br />
Data regarding the type <strong>of</strong> tumor, site <strong>of</strong><br />
tumor, stage <strong>of</strong> the disease, the type <strong>of</strong> myocutaneous<br />
flap used, postoperative complications<br />
<strong>and</strong> the total hospital stay were collected <strong>and</strong><br />
analyzed. Utility <strong>of</strong> the different types <strong>of</strong> these<br />
flaps was reevaluated in terms <strong>of</strong> advantages,<br />
indications, <strong>and</strong> morbidity.<br />
RESULTS<br />
This study included 3 types <strong>of</strong> repair in head<br />
<strong>and</strong> neck region using 4 different types <strong>of</strong> pedicled<br />
myocutaneous or my<strong>of</strong>ascial flaps ( repair<br />
<strong>of</strong> mucosal defects, repair <strong>of</strong> composite mucosal<br />
& skin defects <strong>and</strong> repair <strong>of</strong> skin only defects).<br />
Most <strong>of</strong> the cases were associated with bulky<br />
s<strong>of</strong>t tissue <strong>and</strong> bone defects. In cases with combined<br />
mucosal & skin defects (29 cases) the<br />
myocuteous flaps mainly the (PMMC) flap<br />
(used in 28 cases) were used for one <strong>of</strong> the<br />
following purposes:<br />
1- Replacing the inner mucosal layer <strong>and</strong> using<br />
the deltopectoral fasciocutaneous flap for<br />
skin closure (17 cases).<br />
2- Replacing the outer skin layer, while the<br />
inner mucosal defect was not reconstructed<br />
(2 cases) after maxillectomy.<br />
3- Replacing both the inner mucosal <strong>and</strong> outer<br />
skin layers using long skin territory which<br />
was folded on itself (bipaddle skin flap) in<br />
9 cases.<br />
Primary sites <strong>of</strong> malignancy <strong>and</strong> types <strong>of</strong><br />
defects left after excision are represented in<br />
Table (1). Oral carcinoma represented most <strong>of</strong><br />
the cases (71 cases) <strong>and</strong> the majority were at<br />
advanced stage (T3 & T4) representing 40.8%<br />
(29/71) <strong>and</strong> 33.8% (24/71) respectively.<br />
Different types <strong>of</strong> flaps used in our study<br />
are represented in Table (2). The overall postoperative<br />
complications was 19.8% (24/121).<br />
It was 20% (17/84) in group I, 28.6% (4/14) in<br />
group II, <strong>and</strong> 25% (3/12) in group III. No flap<br />
related complications were reported in group<br />
IV. The mean hospital stay was 14 days (range,<br />
8-27 days) in group I, 11 days (range, 8-15<br />
days) in group II, 12 days (range, 8-16 days)<br />
in group III, <strong>and</strong> 8 days (range, 5-11 days) in<br />
group IV.<br />
The (PMMC) flap was the most commonly<br />
used flap (84 cases ). Figs. (1-9) show different<br />
operative views. The postoperative common<br />
complications in group I were mild infection
Maged M. Elshafiey, et al. 251<br />
(15 cases), minor fistulae (11 cases), partial<br />
skin sloughing <strong>of</strong> the skin isl<strong>and</strong> with the underlying<br />
muscle healthy (3 cases), minor dehiscence<br />
<strong>and</strong> retraction (4 cases). All were properly<br />
managed by antibiotics, skin debridement <strong>and</strong><br />
ryle feeding <strong>and</strong> oral hygiene in mucosal fistulae.<br />
One case with circumferential reconstruction<br />
<strong>of</strong> the pharyngeal defect after total laryngopharyngectomy<br />
developed pharyngeal stenosis <strong>and</strong><br />
required repeated pharyngeal dilatation. In one<br />
case severe infection <strong>and</strong> major sloughing <strong>of</strong><br />
the flap developed that was successfully salvaged<br />
by pedicled latissimus dorsi myocutaneous<br />
flap reconstruction.<br />
Table (1): Primary sites <strong>of</strong> malignancy <strong>and</strong> type <strong>of</strong> defect after excision in patients with head & neck cancer.<br />
Primary site <strong>of</strong> tumor<br />
No. <strong>of</strong><br />
cases<br />
Skin<br />
defect only<br />
Mucosal<br />
defect only<br />
Combined mucosal &<br />
skin defects<br />
Bone<br />
defect<br />
Oral cavity:<br />
Tongue<br />
Alveolar margin<br />
Retromolar<br />
Buccal mucosa<br />
Mouth floor<br />
Lip commisure<br />
71<br />
24<br />
18<br />
11<br />
9<br />
6<br />
3<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
58<br />
24<br />
15<br />
10<br />
4<br />
5<br />
–<br />
13<br />
–<br />
3<br />
1<br />
5<br />
1<br />
3<br />
71<br />
24<br />
18<br />
11<br />
9<br />
6<br />
3<br />
Larynx<br />
Scalp over occipital region<br />
Maxilla<br />
Parotid<br />
Conjunctiva & lids<br />
Cheek<br />
Ear pinna<br />
Neck region<br />
External auditory meatus<br />
Post cricoid<br />
13<br />
9<br />
9<br />
7<br />
4<br />
2<br />
2<br />
2<br />
1<br />
1<br />
–<br />
9<br />
–<br />
7<br />
4<br />
2<br />
2<br />
2<br />
1<br />
1<br />
–<br />
–<br />
6<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
13<br />
–<br />
3<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
9<br />
9<br />
3<br />
1<br />
2<br />
2<br />
–<br />
1<br />
–<br />
Total<br />
21<br />
28<br />
64<br />
29<br />
98<br />
Table (2): Primary sites <strong>of</strong> malignancy <strong>and</strong> type <strong>of</strong> the used flap in patients with head & neck cancer.<br />
Primary site <strong>of</strong> tumor<br />
No. <strong>of</strong><br />
cases<br />
(PMMC) flap<br />
(Group I)<br />
(LTMC) flap<br />
(Group II)<br />
Latissimus dorsi<br />
myocutaneous flap<br />
(Group III)<br />
Temporalis<br />
my<strong>of</strong>ascial<br />
flap (Group IV)<br />
Oral cavity:<br />
Tongue<br />
Alveolar margin<br />
Retromolar<br />
Buccal mucosa<br />
Mouth floor<br />
Lip commisure<br />
71<br />
24<br />
18<br />
11<br />
9<br />
6<br />
3<br />
64<br />
22<br />
15<br />
11<br />
8<br />
6<br />
2<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
8<br />
2<br />
4<br />
–<br />
1<br />
–<br />
1<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
–<br />
Larynx<br />
Scalp over occipital region<br />
Maxilla<br />
Parotid<br />
Conjunctiva & lids<br />
Cheek<br />
Ear pinna<br />
Neck region<br />
External auditory meatus<br />
Post cricoid<br />
13<br />
9<br />
9<br />
7<br />
4<br />
2<br />
2<br />
2<br />
1<br />
1<br />
12<br />
-<br />
3<br />
4<br />
-<br />
-<br />
-<br />
-<br />
-<br />
1<br />
–<br />
9<br />
–<br />
2<br />
–<br />
–<br />
1<br />
1<br />
1<br />
–<br />
1<br />
–<br />
–<br />
1<br />
–<br />
–<br />
1<br />
1<br />
–<br />
–<br />
–<br />
–<br />
6<br />
–<br />
4<br />
2<br />
–<br />
–<br />
–<br />
–<br />
Total<br />
121<br />
84*<br />
14<br />
12*<br />
12<br />
* Two flaps were used in the same patient.
252<br />
<strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
Table (3): Postoperative complications in different groups according to type <strong>of</strong> reconstruction.<br />
Complication<br />
No.<br />
Group I<br />
%<br />
No.<br />
Group II<br />
%<br />
No.<br />
Group III<br />
%<br />
Infection:<br />
Mild<br />
Severe<br />
15<br />
1<br />
17.8<br />
1.2<br />
1<br />
–<br />
7<br />
–<br />
2<br />
–<br />
16.6<br />
–<br />
Sloughing:<br />
Partial<br />
Major<br />
3<br />
1<br />
3.6<br />
1.2<br />
1<br />
–<br />
7<br />
–<br />
1<br />
–<br />
8.3<br />
–<br />
Flap dehiscence & retraction:<br />
Minor<br />
Severe<br />
4<br />
1<br />
4.8<br />
1.2<br />
2<br />
–<br />
14<br />
–<br />
1<br />
–<br />
8.3<br />
–<br />
Fistula:<br />
Minor<br />
Major<br />
11<br />
1<br />
13<br />
1.2<br />
–<br />
–<br />
–<br />
–<br />
2<br />
–<br />
16.6<br />
–<br />
Wound dehiscence at donor site<br />
Seroma at donor site<br />
Hematoma at donor site<br />
Pharyngeal stenosis<br />
–<br />
–<br />
-<br />
1<br />
–<br />
–<br />
–<br />
1.2<br />
2<br />
–<br />
1<br />
–<br />
14<br />
–<br />
7<br />
–<br />
1<br />
2<br />
–<br />
–<br />
8.3<br />
16.6<br />
–<br />
–<br />
The (LTMC) flap was used in 14 patients.<br />
The most common pathology was squamous<br />
cell carcinoma diagnosed in 6 patients. Other<br />
types <strong>of</strong> pathology included parotid carcinoma<br />
(2 cases), recurrent basal cell carcinoma (2<br />
cases), basosquamous cell carcinoma (one case),<br />
sebaceous adenocarcinoma (one case), fibrosarcoma<br />
(one case) <strong>and</strong> malignant peripheral<br />
nerve sheath tumor (one case). The occiput was<br />
the most common site for reconstruction (9<br />
cases). Other sites included the parotid region<br />
(2 cases), the ear pinna (one case), the external<br />
auditory meatus (one case) <strong>and</strong> the posterior<br />
neck (one case). All wounds were closed primarily<br />
<strong>and</strong> preservation <strong>of</strong> the superior fibres<br />
<strong>of</strong> the trapezius enabled almost normal abduction<br />
<strong>of</strong> the arm. Only (1 case) developed partial<br />
distal sloughing <strong>of</strong> the skin isl<strong>and</strong> for which<br />
debridment was done. Minor dehiscence occurred<br />
in 4 cases (the recipient area in 2 cases<br />
<strong>and</strong> the donor site in 2 cases. All cases were<br />
properly managed conservatively by repeated<br />
dressings. Figs. (10-14) show different operative<br />
views.<br />
The latissimus dorsi myocutaneous flap was<br />
used in 12 cases. It was used for reconstruction<br />
<strong>of</strong> oral defects in 8 patients <strong>of</strong> whom 6 cases<br />
were females with large breasts, one case presented<br />
with local recurrence on top <strong>of</strong> previously<br />
used (PMMC) flap for reconstruction Figs.<br />
(15A-C) <strong>and</strong> one case was properly salvaged<br />
after failure <strong>of</strong> previous reconstruction by (PM-<br />
MC) flap. Other indications included major<br />
defects after excision <strong>of</strong> advanced parotid carcinoma<br />
(one case), advanced epithelioma <strong>of</strong> the<br />
ear pinna (one case), synovial sarcoma <strong>of</strong> the<br />
neck (one case) Figs. (16A-C) <strong>and</strong> anterior<br />
pharyngeal defect after salvage laryngectomy<br />
in a case <strong>of</strong> laryngeal carcinoma that had failure<br />
<strong>of</strong> treatment by radiotherapy. Only one case<br />
developed minor sloughing <strong>of</strong> distal skin isl<strong>and</strong>.<br />
Other complications with this flap was seroma<br />
at the donor site (2 cases), minor fistulae (2<br />
cases), minor dehiscence at the recipient site<br />
(one case) <strong>and</strong> at the donor site (one case). All<br />
were properly treated conservatively with aspiration<br />
in seroma cases <strong>and</strong> repeated dressings<br />
in the latter.<br />
The temporalis my<strong>of</strong>ascial flap was used in<br />
(12 cases). In 6 cases it was used to reconstruct<br />
the orbital floor after total maxillectomy for<br />
maxillary carcinoma. In 2 cases it was used to<br />
reconstruct the lateral <strong>and</strong> floor <strong>of</strong> the orbit<br />
after excision <strong>of</strong> epithelioma <strong>of</strong> the cheek invading<br />
the zygomatic arch. It was used for<br />
reconstruction after orbital exenteration in 4<br />
cases. In one case it was used to fill the orbital<br />
cavity <strong>and</strong> internal eye prosthesis was put, in<br />
another case it was used to cover the dura in a<br />
defect in the orbital ro<strong>of</strong> <strong>and</strong> in the other 2 cases<br />
it was used to cover the orbital cavity anteriorly<br />
with overlying skin graft <strong>and</strong> external eye prosthesis.<br />
There was no flap related postoperative<br />
complications.
Maged M. Elshafiey, et al. 253<br />
Fig. (1-A): Sq.C.C. <strong>of</strong> the alveolar margin.<br />
Fig. (1-B): Skin paddle <strong>of</strong> the (PMMC) flap was sutured to<br />
the tongue.<br />
Fig. (2-A): Bipaddle (PMMC) flap, the upper one was<br />
used for mucosal replacement <strong>and</strong> the lower<br />
one was used for skin replacement.<br />
Fig. (2-B): Composite oral defect with mucosal<br />
<strong>and</strong> skin defects replaced with bipaddle<br />
(PMMC) flap.<br />
Fig. (3-A): Late postoperative view <strong>of</strong> bipaddle (PMMC)<br />
flap seen from outside.<br />
Fig. (3-B): Late postoperative view <strong>of</strong> bipaddle (PMMC)<br />
flap seen from inside.
254 <strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
Fig. (4-A): Early postoperative view after resection<br />
<strong>of</strong> advanced maxillary carcinoma <strong>and</strong><br />
reconstruction by (PMMC) flap.<br />
Fig. (4-B): Inner fold <strong>of</strong> the (PMMC) flap replacing the<br />
mucosal defect.<br />
Fig. (5): Central m<strong>and</strong>ibular defect<br />
replaced by Titanium plate<br />
<strong>and</strong> (PMMC) flap.<br />
Fig. (6-A): Lt. parotid carcinoma.<br />
Fig. (6-B): Reconstruction by (PMMC) flap.<br />
Immediate postoperative view.
Maged M. Elshafiey, et al. 255<br />
Fig. (7-A): Vascular pedicle <strong>of</strong> the (PMMC) flap.<br />
Fig. (7-B): Reconstruction by (PMMC) flap after<br />
excision <strong>of</strong> Rt parotid carcinoma. Immediate<br />
postoperative view.<br />
Fig. (8-A): Pharyngeal fistula after total laryngectomy.<br />
Fig. (8-B): Skin paddle <strong>of</strong> the (PMMC) flap was<br />
used to replace the pharyngeal mucosal<br />
defect <strong>and</strong> the deltopectoral flap was<br />
used to replace the skin defect.<br />
Fig. (9-A): Salvage laryngectomy after failed treatment<br />
by radiotherapy.<br />
Fig. (9-B): Operative view after laryngectomy <strong>and</strong> primary<br />
pharyngeal T shaped closure.
256 <strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
Fig. (9-C): <strong>Pedicled</strong> (PMMC) flap was used as a<br />
buttress to the pharyngeal closure <strong>and</strong><br />
for skin defect replacement.<br />
Fig. (10-A): Fibrosarcoma <strong>of</strong> the occiput.<br />
Fig. (10-B): Reconstruction by (LTMC)<br />
flap. Late postoperative<br />
view.<br />
Fig. (11): Reconstruction by (LT-<br />
MC) flap (Early postoperative<br />
view).<br />
Fig. (12): Reconstruction by (LT-<br />
MC) flap. Late postoperative<br />
view.<br />
Fig. (13): Reconstruction by rotational<br />
full paddle (LT-<br />
MC) flap. Early postoperative<br />
view.<br />
Fig. (14): Partial sloughing <strong>of</strong> the<br />
distal end <strong>of</strong> the (LTMC)<br />
flap.
Maged M. Elshafiey, et al. 257<br />
Fig. (15-A): Recurrent Sq.C.C. <strong>of</strong> the buccal mucosa.<br />
Fig. (15-B): Scar <strong>of</strong> previously used Rt. (PMMC)<br />
flap for reconstruction.<br />
Fig. (15-C): Skin paddle <strong>of</strong> the latissimus<br />
dorsi myocutaneous flap is<br />
sutured to the tongue.<br />
Fig. (16-A): Synovial sarcoma <strong>of</strong> the neck.<br />
Fig. (16-B): The latissimus dorsi myocutaneous flap<br />
is passing superficial to the pectoralis<br />
minor <strong>and</strong> deep to the pectoralis major.<br />
Fig. (16-C): Early postoperative view.
258 <strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
Fig. (17-A): Operative view showing lateral <strong>and</strong><br />
lower orbital defects.<br />
Fig. (17-B): The temporalis flap was used to reconstruct<br />
the lateral <strong>and</strong> lower orbital walls <strong>and</strong> a<br />
piece <strong>of</strong> the Lt. ear cartilage was used to<br />
reconstruct the lower eyelid tarsus.<br />
Fig. (18-A): Operative view <strong>of</strong> radical maxillectomy with<br />
lower orbital defect.<br />
Fig. (18-B): Lt. temporalis flap was used<br />
to reconstruct the Lt. lower<br />
orbital defect.<br />
Fig. (19-A): Operative view after excision <strong>of</strong><br />
advanced recurrent B.C.C. with<br />
defect in the orbital ro<strong>of</strong>.<br />
Fig. (19-B): The temporalis flap was used to cover<br />
the exposed dura in the orbital ro<strong>of</strong>.
Maged M. Elshafiey, et al. 259<br />
DISCUSSION<br />
Radical head <strong>and</strong> neck surgery may leave<br />
mucosal or skin defects <strong>and</strong> sometimes with<br />
exposed large vessels, dura mater, cartilage or<br />
bones. It should be coupled with good reconstructive<br />
surgery [4]. An ideal flap should provide<br />
high success rate, few complications, low<br />
morbidity, short hospitalization <strong>and</strong> the greatest<br />
potential for best aesthetic <strong>and</strong> functional outcome<br />
[5].<br />
Local neck skin flaps <strong>and</strong> fasciocutaneous<br />
flaps as forehead flap described by Mc Gregor<br />
(1963) [6] <strong>and</strong> deltopectoral flap described by<br />
Bakamjian (1965) [7] were the only method for<br />
head <strong>and</strong> neck reconstruction in the 1960s <strong>and</strong><br />
1970s although they have many disadvantages.<br />
They have been markedly replaced by the pedicled<br />
myocutaneous flaps in the early 1980s<br />
since the pedicled pectoralis major flap was<br />
first described by Ariyan in the late 1979 [8].<br />
Many myocutaneous flaps were described<br />
for head <strong>and</strong> neck reconstruction including<br />
pectoralis major, latissimus dorsi, trapezius,<br />
sternomastoid, temporalis <strong>and</strong> platysma [9].<br />
The use <strong>of</strong> pedicled myocutaneous flaps <strong>and</strong><br />
free microvascular flaps in head <strong>and</strong> neck reconstruction<br />
started early in our institute in the<br />
early 1980s <strong>and</strong> late 1980s respectively [4,10,11].<br />
Choice <strong>of</strong> reconstructive options depends<br />
on various factors such as site <strong>of</strong> the defect,<br />
type <strong>of</strong> tissue required, functional <strong>and</strong> cosmetic<br />
implications <strong>of</strong> the defect, associated co–morbidity<br />
<strong>and</strong> availability <strong>of</strong> resources [9].<br />
A major advantage <strong>of</strong> pedicled flaps over<br />
free flaps is their simple <strong>and</strong> st<strong>and</strong>ardized surgical<br />
technique requiring no further surgical<br />
qualification compared to micro vascular free<br />
flaps. Also they are reliable, safe <strong>and</strong> have high<br />
degree <strong>of</strong> resistance against infection <strong>and</strong> so<br />
can be used in irradiated patients. Free flaps<br />
are also associated with some drawbacks like<br />
the need for vigorous monitoring <strong>and</strong> reexploration<br />
if required [3]. However, all these<br />
flaps have limitations. Firstly, they have a limited<br />
reach because <strong>of</strong> which there are more<br />
chances <strong>of</strong> distal flap failure <strong>and</strong> wound gap<br />
due to tension by the downward pull <strong>of</strong> the<br />
flaps. Secondly, the type <strong>of</strong> tissue in the flap,<br />
its bulk <strong>and</strong> pliability does not always suit the<br />
defect to be reconstructed. Thirdly, it may not<br />
be possible to contour the flap to the defect in<br />
different planes. Another advantage <strong>of</strong> the (PM-<br />
MC) flap is filling the emptied side <strong>of</strong> the neck<br />
due to concomitant block neck dissection thus<br />
preserving the normal cervical contour <strong>and</strong><br />
protect the major vessels <strong>of</strong> the neck [4].<br />
The use <strong>of</strong> pedicled flaps is still indicated<br />
for patients in whom microsurgery is contraindicated<br />
due to the general condition <strong>of</strong> the<br />
patient or in cases <strong>of</strong> unsuccessful microsurgical<br />
flaps [1].<br />
Despite the increasing use <strong>of</strong> microvascular<br />
reconstruction, the (PMMC) flap continues to<br />
be the most universal major flap in head <strong>and</strong><br />
neck reconstruction [3,12].<br />
The (PMMC) flap dimensions can be varied<br />
from a small isl<strong>and</strong> to a large one overlying the<br />
whole medial two thirds <strong>of</strong> the muscle, depending<br />
upon the site <strong>and</strong> size <strong>of</strong> the defect to be<br />
repaired [4].<br />
Some modifications were described that<br />
maintains maximal donor-site function <strong>and</strong><br />
morphology <strong>of</strong> the (PMMC) flap. Musclepreserving<br />
procedure was described taking the<br />
pectoralis major as an isl<strong>and</strong> flap with no muscle<br />
around the vascular pedicle <strong>and</strong> preserving the<br />
nerve supply to the clavicular <strong>and</strong> the upper<br />
sternocostal parts <strong>of</strong> the muscle [13,14].<br />
When large skin paddle is needed some<br />
modifications were done to preserve blood<br />
supply to the skin isl<strong>and</strong>. Inclusion <strong>of</strong> nippleareola<br />
complex on the skin paddle stabilizes<br />
the blood circulation in the skin isl<strong>and</strong> [15]. The<br />
pectoralis minor muscle can be divided to preserve<br />
the lateral thoracic artery <strong>and</strong> its blood<br />
supply to the lateral distal skin isl<strong>and</strong> <strong>of</strong> (PM-<br />
MC) flap without compromising the pedicle<br />
length [16].<br />
With large full thickness cheek defects. The<br />
modification adopted in bipaddling the flap was<br />
based on anatomical location <strong>of</strong> perforators to<br />
ensure good blood supply to both paddles <strong>of</strong><br />
the flap. Placing the flap horizontally with<br />
inclusion <strong>of</strong> nipple <strong>and</strong> areola increased the<br />
reach <strong>and</strong> size <strong>of</strong> available flap. Precautions<br />
should include proper assessment <strong>of</strong> reach <strong>of</strong><br />
the paddle, placing not more than one-third <strong>of</strong><br />
the paddle outside the muscle <strong>and</strong> securing the<br />
skin paddle to the muscle to avoid shearing <strong>of</strong><br />
perforators during flap raising [17].
260<br />
<strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
In our study (PMMC) flap was used in 84<br />
cases with a very high success rate (98.8%),<br />
whether this success was primary without any<br />
complications (79.8%) or secondary to successful<br />
management <strong>of</strong> minor complications that<br />
delayed healing (19%). Major flap loss requiring<br />
salvage reconstruction by latissimus dorsi flap<br />
occurred in only one case. Different series had<br />
reported varying incidences <strong>of</strong> complications,<br />
63% [18], 58% [19], 36.1% [2]. Fewer complications<br />
were reported when using the my<strong>of</strong>ascial<br />
flap only [18,20]. The incidence <strong>of</strong> major or total<br />
flap loss was varying from 0% [21], to 1.5% [4],<br />
to 2.4% [2,18].<br />
The main indications in our study were oral<br />
<strong>and</strong> partial pharyngeal defects.<br />
In an old series done in the Egyptian <strong>NCI</strong><br />
in 1985 [4], pedicled (PMMC) flap was used<br />
for pharyngoplasty after total laryngopharyngectomy<br />
in 50 patients <strong>and</strong> in another series<br />
done in 1986 [10], latissinus dorsi myocutaneous<br />
flap was used for the same purpose in 28 cases.<br />
In our study, pedicled (PMMC) flap was used<br />
in only one case for reconstruction after this<br />
kind <strong>of</strong> surgery in a patient with poor general<br />
condition that could not withst<strong>and</strong> neither free<br />
jejunal flap nor gastric pull up.<br />
<strong>Pedicled</strong> myocutaneous flaps are rarely used<br />
nowadays to reconstruct the pharynx after total<br />
laryngopharyngectomy as this method has many<br />
disadvantages that includes development <strong>of</strong><br />
fistula <strong>and</strong> stenosis <strong>and</strong> due to the evolution <strong>of</strong><br />
gastric pull up <strong>and</strong> free jejunal flaps <strong>and</strong> their<br />
established use in such cases.<br />
Gastric transposition is more commonly<br />
used after pharyngolaryngo-oesophagectomy<br />
in our institute, owing to increased multidisciplinary<br />
experience in this form <strong>of</strong> surgery <strong>and</strong><br />
in relation to the advanced pathological stage<br />
<strong>of</strong> hypopharyngeal carcinoma at presentation<br />
in which total esophagectomy is needed to<br />
obtain proper lower safety margin [22].<br />
In our study the (PMMC) flap was used to<br />
reconstruct the anterior wall <strong>of</strong> the pharynx<br />
after total laryngectomy in 12 cases receiving<br />
prior radiotherapy (In 2 cases the mucosa was<br />
closed primarily & the muscle flap was used as<br />
a buttress to augment the suture line <strong>and</strong> replace<br />
the skin defect, <strong>and</strong> in 10 cases the skin isl<strong>and</strong><br />
was used to repair the mucosal defect). In the<br />
latter group, intentional pharyngostomy was<br />
done after resection in 7 cases, <strong>and</strong> 3 cases<br />
developed major fistulae after trial <strong>of</strong> primary<br />
closure. In these 10 cases, the skin isl<strong>and</strong> <strong>of</strong> the<br />
(PMMC) flap was used to reconstruct the mucosal<br />
defect <strong>and</strong> the skin defect was reconstructed<br />
by deltopectoral fasciocutaneous flaps. The<br />
latissimus flap was used for this purpose in only<br />
one case in a female with large breast.<br />
Iginio Tansini in 1896 [23] was the first<br />
surgeon who performed the pedicled latissimus<br />
myocutaneous flap. He used it in reconstructing<br />
skin defects after surgery <strong>of</strong> breast cancer.<br />
However, this procedure was put to rest when<br />
Halsted started his radical mastectomy using<br />
thin skin flaps instead <strong>of</strong> removing wider skin<br />
area. Olivari in 1976 [24] rediscovered this flap<br />
<strong>and</strong> since then it gained its popularity in reconstruction<br />
<strong>of</strong> major defects that occurred after<br />
radical surgery for malignancies in the breast,<br />
chest wall <strong>and</strong> head & neck areas.<br />
Its blood supply is based on the thoraco<br />
dorsal vessels that run 8-14cm before entering<br />
the muscle just above the mid point <strong>of</strong> its free<br />
border. Its cranial vascularity allows it to have<br />
wide arc <strong>of</strong> rotation that it can cover any defect<br />
from the sternum anteriorly to the midline posteriorly<br />
<strong>and</strong> it can reach to the upper border <strong>of</strong><br />
the ear [10].<br />
When the donor site is less than 10x12 cm,<br />
it can be closed primarily but wider defects will<br />
need skin grafts. The largest reported size <strong>of</strong><br />
this flap was 35x20 cm [25]. Olivari 1979 [26]<br />
proved the presence <strong>of</strong> 27 perforating arteries<br />
going between the muscle <strong>and</strong> the overlying<br />
skin.<br />
One <strong>of</strong> the greatest advantages <strong>of</strong> the latissimus<br />
dorsi flap over other regional myocutaneous<br />
flaps as the pectoralis major flap is that<br />
one can control the thickness <strong>of</strong> the muscle due<br />
to the anatomical fact that the main arterial<br />
supply runs along the lateral thin border <strong>of</strong> the<br />
muscle <strong>and</strong> gives its branches to the bulk <strong>of</strong> the<br />
muscle medially [10].<br />
Elevation <strong>of</strong> the skin isl<strong>and</strong> overlying the<br />
latissimus dorsi muscle <strong>and</strong> dissecting the dominant<br />
perforating vessel, permit independent<br />
positioning <strong>of</strong> the skin isl<strong>and</strong> in relation to the<br />
muscle (razor flap) thus decreasing the donor<br />
site morbidity [27].
Maged M. Elshafiey, et al. 261<br />
The indications <strong>of</strong> this flap in our study were<br />
those cases in whom the bulky (PMMC) flap<br />
were not satisfactory (8 cases), the (PMMC)<br />
flap was previously used <strong>and</strong> the patient developed<br />
local recurrence (1 case), the (PMMC)<br />
flap was used <strong>and</strong> the patient developed major<br />
fistula <strong>and</strong> retraction that needed salvage reconstruction<br />
(1 case) or the defect was out <strong>of</strong> the<br />
reach <strong>of</strong> the (PMMC) flap (2 cases).<br />
The inclusion <strong>of</strong> osseous parts had been<br />
described in pedicled myocutaneous flaps to be<br />
used in m<strong>and</strong>ibular reconstruction including<br />
the pectoralis major osteomusculocutaneous<br />
flap including full thickness anterior bony part<br />
<strong>of</strong> the 5 th rib [11,28] <strong>and</strong> the sternocleidomastoid<br />
clavicular osteomusculocutaneous flaps whether<br />
ipsilateral [29-30] or contralateral in cases necessitating<br />
radical neck dissection [31]. The main<br />
disadvantage <strong>of</strong> the above mentioned osteocutaneous<br />
flaps is osteonecrosis <strong>of</strong> the bony part<br />
reaching 40-50% [11].<br />
Myoosseous flaps <strong>and</strong> osteocutaneous flaps<br />
whether pedicled or free vascularized have<br />
several advantages when compared with other<br />
methods <strong>of</strong> m<strong>and</strong>ibular reconstruction. M<strong>and</strong>ibular<br />
deviation <strong>and</strong> temporo-m<strong>and</strong>ibular joint<br />
ankylosis can be prevented in contrast to techniques<br />
in which s<strong>of</strong>t tissue replacement only is<br />
used. Also the functional <strong>and</strong> cosmetic deformity<br />
can be avoided when m<strong>and</strong>ibular symphysis is<br />
included in resection [11,31]. Central complete<br />
m<strong>and</strong>ibular defects should be immediately reconstructed<br />
by osseous flaps [9]. Free vascularized<br />
fibular graft is the mostly used flap for this<br />
purpose nowadays in our institute. One disadvantage<br />
<strong>of</strong> the fibula free flap is the limitations<br />
<strong>of</strong> the s<strong>of</strong>t tissue component <strong>of</strong> the flap, however<br />
in anterior oral cavity defects, less tissue volume<br />
replacement is desired.<br />
In our study, we had only one case with<br />
central m<strong>and</strong>ibular defect that was reconstructed<br />
with titanium plate <strong>and</strong> (PMMC) flap. It was a<br />
case <strong>of</strong> advanced carcinoma <strong>of</strong> the alveolar<br />
margin invading the lower lip <strong>and</strong> floor <strong>of</strong><br />
mouth. Partial lateral m<strong>and</strong>ibulectomy <strong>and</strong> primary<br />
s<strong>of</strong>t tissue closure without osseous reconstruction<br />
is a satisfactory treatment in good<br />
h<strong>and</strong>s [32,33]. This is suitable for lateral defects<br />
especially edentulous patients as deviation <strong>of</strong><br />
the jaw is not a concern as there is no occlusion<br />
to be maintained. This is a safe, rapid <strong>and</strong><br />
reliable procedure that leads to rapid healing<br />
<strong>and</strong> does not delay the adjuvant radiotherapy.<br />
The trapezius myocutaneous flap was first<br />
described by Demergasso <strong>and</strong> Piazza [34]. Several<br />
variations <strong>of</strong> this flap had been described.<br />
One <strong>of</strong> these variations is the lower vertical<br />
trapezius isl<strong>and</strong> flap [35]. Although the superior<br />
fibers have been designed as the basis for a flap<br />
for head <strong>and</strong> neck reconstruction, this flap has<br />
limited arc <strong>of</strong> rotation. However, it is possible<br />
to use only the middle <strong>and</strong> inferior portions <strong>of</strong><br />
the trapezius as a musculocutaneous flap. This<br />
flap is based on the descending branch <strong>of</strong> the<br />
transverse cervical artery <strong>and</strong> associated veins.<br />
Further several detailed studies <strong>of</strong> the vascular<br />
anatomy <strong>of</strong> the human cadavers found that the<br />
trapezoidal branch <strong>of</strong> the dorsal scapular artery<br />
is a constant vessel to the lower trapezius muscle<br />
[5].<br />
Its location makes it frequently the flap <strong>of</strong><br />
choice for defects <strong>of</strong> the occipital, parotid &<br />
cervical spine areas. In addition it may be used<br />
for intraoral & anterior neck coverage but the<br />
main disadvantage is the need to change the<br />
position to the lateral decubitus [36].<br />
If an inadequate arc <strong>of</strong> the rotation is obtained<br />
after elevation <strong>of</strong> the trapezius to the<br />
level <strong>of</strong> the first thoracic vertebra, it is possible<br />
to divide the fibers <strong>of</strong> origin <strong>and</strong> insertion <strong>of</strong><br />
the superior portion <strong>of</strong> the trapezius muscle<br />
from the occiput <strong>and</strong> acromio-clavicular joint.<br />
This maneuver markedly increases the arc <strong>of</strong><br />
rotation [5].<br />
In our study, 14 cases were reconstructed<br />
by the lower (vertical) trapezius flap. The occiput<br />
was the most common site for reconstruction<br />
(9 cases). Other sites included the parotid<br />
region (2 cases), the ear pinna (one case), the<br />
external auditory meatus (one case) <strong>and</strong> the<br />
posterior neck (one case).<br />
In our current series the lower trapezius flap<br />
had many advantages. The donor site functional<br />
deficits were minimal <strong>and</strong> primarily closure<br />
was feasible in all cases. The resulting donor<br />
scar on the back had been favored over anterior<br />
chest scars by some female patients. The wide<br />
arc <strong>of</strong> rotation makes it suitable source for skin<br />
<strong>and</strong> muscle replacement for the entire neck,<br />
face <strong>and</strong> occipital region <strong>of</strong> the scalp. Its design<br />
could be the workhorse myocutaneous flap in
262<br />
<strong>Continuous</strong> <strong>Validity</strong> <strong>of</strong> <strong>Pedicled</strong> <strong>Myocutaneous</strong> & My<strong>of</strong>ascial Flaps<br />
regions not reached by the pectoralis major or<br />
in women in whom prevention <strong>of</strong> distortion <strong>of</strong><br />
the breasts is desirable. The main disadvantage<br />
<strong>of</strong> this flap is the need to change the position<br />
in some cases to the lateral decubitus position<br />
during surgery.<br />
The temporalis muscle was used in facial<br />
reconstruction for more than 100 years. Many<br />
surgeons use the temporalis muscle for various<br />
defects in the craniomaxill<strong>of</strong>acial region. It has<br />
some limitations because <strong>of</strong> its pedicle. It cannot<br />
reach the midline defects <strong>of</strong> the face, only a<br />
small volume <strong>of</strong> the muscle can reach the defect,<br />
<strong>and</strong> most <strong>of</strong> the muscle bulk is used in the<br />
pedicle [37].<br />
In our study the temporalis muscle flap was<br />
used in 12 cases. It was effective in reconstructing<br />
the lower or lateral orbital wall defects in<br />
8 cases to support the eye globe. Other effective<br />
indications was to cover the dura in the orbital<br />
ro<strong>of</strong> defect <strong>and</strong> to facilitate the use <strong>of</strong> eye<br />
prosthesis after orbital exenteration.<br />
Conclusion:<br />
<strong>Pedicled</strong> myocutanous <strong>and</strong> my<strong>of</strong>ascial flaps<br />
are still indicated in composite head <strong>and</strong> neck<br />
reconstruction. Their reliability, safety, <strong>and</strong> high<br />
degree <strong>of</strong> resistance to infection make them<br />
essential specially the (PMMC) flap previously<br />
described as the spare wheel <strong>of</strong> head <strong>and</strong> neck<br />
reconstructive surgery. It is suitable for lateral<br />
m<strong>and</strong>ibular defects in edentulous patients <strong>and</strong><br />
in partial pharyngeal defects in irradiated patients.<br />
Other pedicled myocutaneous flaps are<br />
still valid in certain occasions <strong>and</strong> sites. Surgeons<br />
must be acquainted with the different<br />
pedicled myocutaneous flaps that could be used<br />
for head <strong>and</strong> neck reconstruction. The proper<br />
choice <strong>of</strong> the type <strong>of</strong> flap that suites every case<br />
<strong>and</strong> the proper surgical technique got by experience<br />
will give the best functional <strong>and</strong> aesthetic<br />
results with the least morbidity.<br />
REFERENCES<br />
1- Croce A, Moretti A, D’Agostino L, Neri G. Continuing<br />
validity <strong>of</strong> pectoralis major muscle flap 25 year after<br />
its first application. Acta Otorhinolaryngol Ital. 2003,<br />
23 (4): 297-304.<br />
2- Vartanian JG, Carvalho AL, Carvalho SM, Mizobe L,<br />
Magrin J, Kowalski LP. Pectoralis major <strong>and</strong> other<br />
my<strong>of</strong>ascial/myocutaneous flaps in head <strong>and</strong> neck<br />
cancer reconstruction: Experience with 437 cases at<br />
a single institution. Head Neck. 2004, 26 (12): 1018-<br />
23.<br />
3- Milenovic ´ A, Virag M, Uglesic ´ V, Aljinovic –<br />
Ratkovic ´ NJ. The pectoralis major flap in head <strong>and</strong><br />
neck reconstruction: First 500 patients. Craniomaxill<strong>of</strong>ac<br />
Surg. 2006, 34 (6): 340-3.<br />
4- Abdel Mageed H, Mebed H, Amer F, Khafagy M,<br />
Ismail T, Gareer WY, et al. Further Experience with<br />
the use <strong>of</strong> the pectoralis major myocutaneous flap for<br />
reconstruction after radical head <strong>and</strong> neck surgery. J<br />
Egypt Natl Cancer Inst. 1985, 2 (2): 199-212.<br />
5- Attia AA. The lower trapezius myocutaneous flap for<br />
reconstruction after surgery for head <strong>and</strong> neck cancer:<br />
<strong>NCI</strong> experience. Journal <strong>of</strong> the Egyptian Nat Cancer<br />
Inst. 2002, 14 (3): 185-91.<br />
6- Mc Gregor IA. The temporal flap in intra-oral cancer:<br />
Its use in repairing the post-excisional defect. Br J<br />
Plast Surg. 1963, 16: 318-35.<br />
7- Bakamjian VY. A two-stage method for pharyngoesophageal<br />
reconstruction with a primary pectoral skin.<br />
Plast Reconstr Surg. 1965, 36: 173-84.<br />
8- Ariyan S. The pectoralis major myocutaneous flap. A<br />
versatile flap for reconstruction in the head <strong>and</strong><br />
neck.Plast Reconstr Surg. 1979, 63 (1): 73-81.<br />
9- Watkinson JC, Gaze MN, Wilson JA. Stell & Maran’s.<br />
head & neck surgery. Fourth eition. Butterworth-<br />
Heinemann. Oxford. 2000, 129-30.<br />
10- Manieh MA, Abou El Ella M, Bassiouny M, Ismail<br />
SA, Abou El Ella M. Use <strong>of</strong> latissimus dorsi myocutaneous<br />
flap in head <strong>and</strong> neck surgery. J Egypt Natl<br />
cancer Inst. 1986, 2 (4): 535-41.<br />
11- Bassiouny M, Gareer WY, Hweidi S, Abdel Mageed<br />
H, El Naggar H, Abou El Ella M. Selective variants<br />
<strong>of</strong> reconstruction <strong>of</strong> the oral cavity after radical surgery.<br />
J Egypt Nat Cancer Institute. 1992, 5 (3): 533-58.<br />
12- Chaturvedi P, Pai PS, Pathak KA, Chaukar DA, Deshp<strong>and</strong>e<br />
MS, D'Cruz AK. Simultaneous reconstruction<br />
<strong>of</strong> large skin <strong>and</strong> mucosal defect following head <strong>and</strong><br />
neck surgery with a single skin paddle pectoralis<br />
major myocutaneous flap. J Laryngol Otol. 2005, 119<br />
(4): 303-5.<br />
13- Corten EM, Schellekens PP, Bleys RL, Kon M. The<br />
nerve supply to the clavicular part <strong>of</strong> the pectoralis<br />
major muscle: An anatomical study <strong>and</strong> clinical application<br />
<strong>of</strong> the function-preserving pectoralis major<br />
isl<strong>and</strong> flap. Plast Reconstr Surg. 2003, 112 (4):<br />
969-75.<br />
14- Corten EM, Schellekens PP, Oey PL, Hage JJ, Kerst<br />
A, Kon M. Function <strong>of</strong> the clavicular part <strong>of</strong> the<br />
pectoralis major muscle after transplantation <strong>of</strong><br />
its sternocostal part. Ann Plast Surg. 2007, 58 (4):<br />
392-6.<br />
15- Coruh A. Pectoralis major musculocutaneous flap<br />
with nipple-areola complex in head <strong>and</strong> neck reconstruction:<br />
Preliminary results <strong>of</strong> a new modified method.<br />
Ann Plast Surg. 2006, 56 (4): 413-7.<br />
16- Po-Wing Yuen A. Preservation <strong>of</strong> lateral thoracic<br />
artery to improve vascular supply <strong>of</strong> distal skin without<br />
compromising pedicle length in harvesting pectoralis
Maged M. Elshafiey, et al. 263<br />
major myocutaneous flap. J Plast Reconstr Aesthet<br />
Surg. 2006, 59 (12): 1433-5.<br />
17- Ahmad QG, Navadgi S, Agarwal R, Kanhere H, Shetty<br />
KP, Prasad R. Bipaddle pectoralis major myocutaneous<br />
flap in reconstructing full thickness defects <strong>of</strong> cheek:<br />
A review <strong>of</strong> 47 cases. J Plast Reconstr Aesthet Surg.<br />
2006, 59 (2): 166-73.<br />
18- Kroll SS, Goepfert H, Jones M, Guillamondegui O,<br />
Schusterman M. Analysis <strong>of</strong> complications in 168<br />
pectoralis major myocutaneous flaps used for head<br />
<strong>and</strong> neck reconstruction. Ann Plast Surg. 1990, 25<br />
(2): 93-7.<br />
19- Huang RD, Silver SM, Hussain A, Parnes SM, Wing<br />
PD. Pectoralis major myocutaneous flap: Analysis <strong>of</strong><br />
complications in a VA population Head Neck. 1992,<br />
14 (2): 102-6.<br />
20- Righi PD, Weisberger EC, Slakes SR, Wilson JL,<br />
Kesler KA, Yaw PB. The pectoralis major my<strong>of</strong>ascial<br />
flap: Clinical applications in head <strong>and</strong> neck reconstruction.<br />
Am J Otolaryngol. 1998, 19 (2): 96-101.<br />
21- Lefebvre JL, Vankemmel B, Meynadier J, Castelain<br />
B, Coche-Dequeant B, Adenis L. The use <strong>of</strong> the<br />
pectoralis major myocutaneous flap in cervic<strong>of</strong>acial<br />
<strong>and</strong> particularly buccopharyngeal, surgery. Apropos<br />
<strong>of</strong> 42 cases. Bull Cancer. 1984, 71 (1): 35-9.<br />
22- Abdelaziz S, Anwar H, Ramzy S, Elshafiey MM,<br />
Mebed AH. Is gastric pull-up reconstruction still the<br />
versatile method in the surgical treatment for hypopharyngeal<br />
carcinoma. Kasr El Aini Journal <strong>of</strong> Surgery.<br />
2005, 6 (1): 3-11.<br />
23- Maxwell GP. Iginio Tansini <strong>and</strong> the origin <strong>of</strong> the<br />
latissimus dorsi musculocutaneous flap. Plast Reconstr<br />
Surg. 1980, 65 (5): 686-92.<br />
24- Olivari N. The latissimus flap. Br J Plast Surg. 1976,<br />
29 (2): 126-8.<br />
25- Maxwell GP, Stueber K, Hoopes JE. A free latissimus<br />
dorsi myocutaneous flap: Case report. Plast Reconstr<br />
Surg. 1978, 62 (3): 462-6.<br />
26- Olivari N. Use <strong>of</strong> thirty latissimus dorsi flaps. Plast<br />
Reconstr Surg. 1979, 64 (5): 654-61.<br />
27- Cavadas PC, Teran-Saavedra PP. Combined latissimus<br />
dorsi-thoracodorsal artery perforator free flap: The<br />
"razor flap". J Reconstr Microsurg. 2002, 18 (1): 29-<br />
31.<br />
28- Cuono CB, Ariyan S. Immediate reconstruction <strong>of</strong> a<br />
composite m<strong>and</strong>ibular defect with a regional osteomusculocutaneous<br />
flap. Plast Reconstr Surg. 1980,<br />
65 (4): 477-84.<br />
29- Conley J. Use <strong>of</strong> composite flaps containing bone for<br />
major repairs in the head <strong>and</strong> neck. Plast Reconstr<br />
Surg. 1972, 49 (5): 522-6.<br />
30- Siemssen SO, Kirkby B, O'Connor TP. Immediate<br />
reconstruction <strong>of</strong> a resected segment <strong>of</strong> the lower jaw,<br />
using a compound flap <strong>of</strong> clavicle <strong>and</strong> sternomastoid<br />
muscle. Plast Reconstr Surg. 1978, 61 (5): 724-35.<br />
31- Barnes DR, Oss<strong>of</strong>f RH, Pecaro B, Sisson GA. Immediate<br />
reconstruction <strong>of</strong> m<strong>and</strong>ibular defects with a<br />
composite sternocleidomastoid musculoclavicular<br />
graft. Arch Otolaryngol. 1981, 107 (11): 711-4.<br />
32- Huot LA, Larochelle D, Gagnon NB, Dupont SS.<br />
Reconstruction <strong>of</strong> the floor <strong>of</strong> the mouth following<br />
surgery for cancer. J Otolaryngol. 1977, 6 (5): 386-<br />
92.<br />
33- Leipzig B, Johnson JT, Rabuzzi DD. Composite<br />
resection without m<strong>and</strong>ibular reconstruction. J Otolaryngol.<br />
1979, 8 (1): 60-4.<br />
34- Demergasso F, Piazza MV. Trapezius myocutaneous<br />
flap in reconstructive surgery for head <strong>and</strong> neck cancer:<br />
An original technique. Am J Surg. 1979, 138 (4): 533-<br />
6.<br />
35- Mathes SJ, Nahai F. Clinical Atlas <strong>of</strong> Muscle <strong>and</strong><br />
Musculocutaneous flaps. St. Louis: Mosby. 1979: pp.<br />
303-5.<br />
36- Hagan KF, Mathes SJ. GRABB’S Encyclopedia <strong>of</strong><br />
flaps, head <strong>and</strong> neck. CH 123: Trapezius muscle <strong>and</strong><br />
musculocutaneous flaps. Lippincott-Raven. Philadelphia.<br />
New York. 1998, p. 461-466.<br />
37- Menderes A, Yilmaz M, Vayvada H, Demirdover C,<br />
Barutçu A. Reverse temporalis muscle flap for the<br />
reconstruction <strong>of</strong> orbital exenteration defects. Ann<br />
Plast Surg. 2002, 48 (5): 521-6.