SCCO Medical History Form
SCCO Medical History Form
SCCO Medical History Form
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
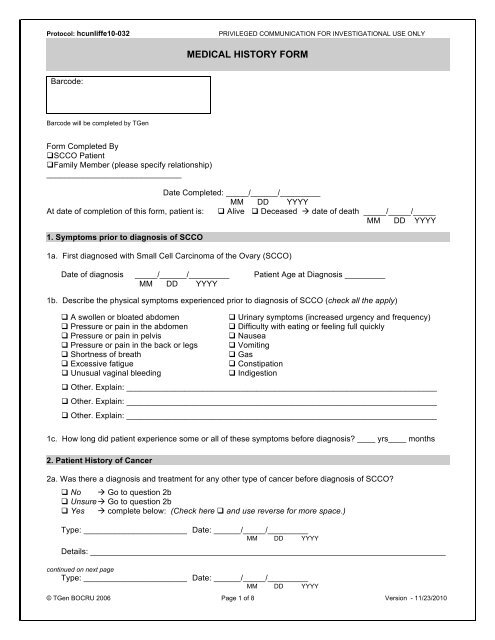
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
<strong>Form</strong> Completed By<br />
<strong>SCCO</strong> Patient<br />
Family Member (please specify relationship)<br />
______________________________<br />
Date Completed: _____/______/_________<br />
MM DD YYYY<br />
At date of completion of this form, patient is: Alive Deceased date of death _____/_____/_____<br />
MM DD YYYY<br />
1. Symptoms prior to diagnosis of <strong>SCCO</strong><br />
1a. First diagnosed with Small Cell Carcinoma of the Ovary (<strong>SCCO</strong>)<br />
Date of diagnosis _____/______/_________ Patient Age at Diagnosis _________<br />
MM DD YYYY<br />
1b. Describe the physical symptoms experienced prior to diagnosis of <strong>SCCO</strong> (check all the apply)<br />
A swollen or bloated abdomen<br />
Pressure or pain in the abdomen<br />
Pressure or pain in pelvis<br />
Pressure or pain in the back or legs<br />
Shortness of breath<br />
Excessive fatigue<br />
Unusual vaginal bleeding<br />
Urinary symptoms (increased urgency and frequency)<br />
Difficulty with eating or feeling full quickly<br />
Nausea<br />
Vomiting<br />
Gas<br />
Constipation<br />
Indigestion<br />
Other. Explain: _____________________________________________________________________<br />
Other. Explain: _____________________________________________________________________<br />
Other. Explain: _____________________________________________________________________<br />
1c. How long did patient experience some or all of these symptoms before diagnosis ____ yrs____ months<br />
2. Patient <strong>History</strong> of Cancer<br />
2a. Was there a diagnosis and treatment for any other type of cancer before diagnosis of <strong>SCCO</strong><br />
No Go to question 2b<br />
Unsure Go to question 2b<br />
Yes complete below: (Check here and use reverse for more space.)<br />
Type: _______________________ Date: ______/_____/_________<br />
MM DD YYYY<br />
Details: _______________________________________________________________________________<br />
continued on next page<br />
Type: _______________________ Date: ______/_____/_________<br />
MM DD YYYY<br />
© TGen BOCRU 2006 Page 1 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
Details: _______________________________________________________________________________<br />
Comments: _______________________________________________________________________________<br />
_________________________________________________________________________________________<br />
2b. Was a genetic test performed to determine whether patient had an abnormality in either the BRCA1 gene or<br />
the BRCA2 gene<br />
No Go to question 2c<br />
Unknown Go to question 2c<br />
Yes Check here if BRCA1 mutation test was positive<br />
Check here if BRCA2 mutation test was positive<br />
2c. Were other genetic or DNA tests performed to evaluate possible genetic alterations for this patient<br />
No Go to question 3<br />
Unknown Go to question 3<br />
Yes Explain: (Check here and use reverse for more space.)_______________________<br />
__________________________________________________________________________________<br />
3. Patient Family <strong>History</strong> of Cancer (First-Degree Relatives)<br />
3. Do any of the patient’s first-degree relatives, for example, parents, siblings, or children have a history of<br />
cancer of any kind Yes No Unknown<br />
If yes, complete all below.<br />
(Check here and use reverse for more space.)<br />
Relative 1: _______________ Cancer type: ___________________ Age at Diagnosis if known: _____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Relative 2: ______________ Cancer type: ___________________ Age at Diagnosis if known: _____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Relative 3: _______________ Cancer type: ___________________ Age at Diagnosis if known: _____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Check here if additional first-degree relatives have a history of cancer and use reverse. Continued on next page.<br />
4. Patient Family <strong>History</strong> of Cancer (Second-Degree Relatives)<br />
© TGen BOCRU 2006 Page 2 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
4. Do any of the patient’s second-degree relatives, for example, grandparents, aunts, uncles, or cousins, have a<br />
history of cancer Yes No Unknown<br />
If yes, complete below: (Check here and use reverse for more space.)<br />
Relative 1: ____________<br />
Maternal<br />
Paternal Cancer type: ______________ Age at Diagnosis if known: ____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Maternal<br />
Relative 2: ______________ Paternal Cancer type: ______________ Age at Diagnosis if known: ____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Maternal<br />
Relative 3: ______________ Paternal Cancer type: _______________ Age at Diagnosis if known: ____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Maternal<br />
Relative 4: ______________ Paternal Cancer type: _______________ Age at Diagnosis if known: ____<br />
Details: _______________________________________________________________________________<br />
_____________________________________________________________________________________<br />
Check here if additional second-degree relatives have a history of cancer and use reverse.<br />
5. Risk Factors - Hormonal<br />
5a. What was the patient’s age at her first period (Menarche) ________ Unknown<br />
5b. Was patient pregnant at any time<br />
No Go to question 5c<br />
Unknown Go to question 5c<br />
Yes How many pregnancies ________ Unknown<br />
Patient age at first pregnancy ________ Unknown<br />
How many children did patient give birth to ________ Unknown<br />
How many miscarriages or abortions did patient have ________ Unknown<br />
continued on next page<br />
5c. What was patient’s menopausal status at time of diagnosis of <strong>SCCO</strong>: Unknown Unsure<br />
© TGen BOCRU 2006 Page 3 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
Pre-pubescent<br />
Pre-menopausal<br />
Peri-menopausal<br />
Post-menopausal<br />
Menstruation not yet started. No menopausal symptoms.<br />
No menopausal symptoms<br />
Going through menopause* (see below for common symptoms)<br />
Menopausal symptoms have finished.<br />
*Common symptoms of going through menopause (the beginning of menopausal symptoms typically occur in women ages<br />
45-55 but some women show symptoms in their 30s.<br />
• Changes in pattern of periods (can be shorter or longer, lighter or heavier, more or less time between periods)<br />
• Hot flashes (sudden rush of heat in upper body)<br />
• Night sweats (hot flashes that happen while you sleep), often followed by a chill<br />
• Trouble sleeping through the night (with or without night sweats)<br />
• Mood changes. Irritability. Trouble focusing, feeling mixed-up or confused,<br />
• Hair loss or thinning on your head. More hair growth on your face<br />
• Vaginal dryness.<br />
5d. Did patient use contraceptives for birth control at any time<br />
No Go to question 6<br />
Unknown Go to question 6<br />
Yes Did patient use hormonal contraceptives Y N Unknown<br />
Does patient currently use hormonal contraceptives Y N Unknown<br />
Did patient stop using hormonal contraceptives 10 or<br />
more years ago Y N Unknown<br />
5e. List any names or types and duration of contraceptives you recall were used by patient:<br />
Type Used Previously Currently Use Total Use in Years or Months<br />
Oral (“the pill”) ____ Years ____ Months Unknown<br />
IUD (“Mirena/Progestin”) ____ Years ____ Months Unknown<br />
IUD (“Paraguard/Copper”) ____ Years ____ Months Unknown<br />
Implant (“Implanon”) ____ Years ____ Months Unknown<br />
Skin patch (“Ortho Evra”) ____ Years ____ Months Unknown<br />
Injection (“Depo-Provera”) ____ Years ____ Months Unknown<br />
Vaginal ring (“NuvaRing”) ____ Years ____ Months Unknown<br />
Other: _________________ ____ Years ____ Months Unknown<br />
If known, names: _______________________________________________________________________<br />
6. Risk Factors – Lifestyle<br />
6a. Did patient gain weight since turning 18 years of age and before diagnosis of <strong>SCCO</strong><br />
No Go to question 6b<br />
Unknown Go to question 6b<br />
Yes What was the amount of weight gain (in pounds)<br />
0-15 16-30 31-50 More than 50 Unknown<br />
continued on next page<br />
6b. At the time of diagnosis, did patient smoke<br />
© TGen BOCRU 2006 Page 4 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
Unknown Go to question 6c<br />
Yes How many packs per week ___ Unknown<br />
How long did patient smoke for ___ Months or ___ Years Unknown<br />
No<br />
Did patient smoke at any time previously<br />
No Go to question 6c.<br />
Yes How long ago did patient quit ___ Months or ___ Years Unknown<br />
How long did patient smoke for ___ Months or ___ Years Unknown<br />
How many packs per week ___ Unknown<br />
6c. At the time of diagnosis, did patient drink alcohol<br />
No Go to question 7<br />
Unknown Go to question 7<br />
Yes Average number of drinks: _____ per Day Week Unknown<br />
Month Year<br />
7. Risk Factors – Other<br />
7a. Did patient at any time have a diagnosis of one of the following (check all that apply).<br />
Human papillomavirus (HPV)<br />
Hepatitis B Virus (HBV)<br />
Hepatitis C Virus (HBV)<br />
Epsein-Barr Virus (EBV)<br />
Human T-lymphotropic Virus (HTLV) Kaposi's sarcoma-associated herpesvirus (KSHV)<br />
Merkel cell polyomavirus (MCPV) None I am aware of.<br />
7b. List all possible vaccinations you can recall for this patient and approximate year if known.<br />
Vaccine: _________________________<br />
Vaccine: _________________________<br />
Vaccine: _________________________<br />
Vaccine: _________________________<br />
year _______<br />
year _______<br />
year _______<br />
year _______<br />
Check here and list additional vaccine information on reverse.<br />
7b. Are there any unusual environmental exposures for the patient you would like to include<br />
For example, exposure to nuclear fallout or significant levels of radiation, work with toxic/carcinogenic<br />
substances, exposure to unusual pathogens, etc.<br />
Describe: _____________________________________________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
Check here if additional details on environmental exposures and use reverse.<br />
continued on next page<br />
© TGen BOCRU 2006 Page 5 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
8. Treatment<br />
8a. Did patient have surgery to remove the ovarian cancer<br />
No<br />
Did patient receive chemotherapy or any other treatments to shrink the cancer<br />
No Go to Question 8e.<br />
Yes Go to Question 8c.<br />
Yes Date of Surgery (MM/DD/YYYY): ______/______/_______<br />
Name of Doctor: __________________________________________<br />
Hospital or clinic name: ____________________________________<br />
Is a copy of the pathology report available Y N<br />
Is a copy of the cytology report available Y N Report not ordered<br />
Note: TGen will require a de-identified copy of the patient’s final pathology report(s) and cytology report (if<br />
cytology was requested by the surgeon). Patient personal identifying information can either be blanked out by<br />
you, or the TGen Research Coordinator will do this for you before it reaches the Researchers for this study.<br />
8b. What chemotherapy did patient receive (check all that apply): Weeks Cycles<br />
Paclitaxel (taxane, taxol) _____ _____<br />
Cisplatin (cisplatinum, or cis-diamminedichloroplatinum(II) or CDDP) _____ _____<br />
Carboplatin _____ _____<br />
Cyclophosphamide (Endoxan, Cytoxan, Neosar, Procytox, Revimmune) _____ _____<br />
Bleomycin (Blenoxane, Bleocip) _____ _____<br />
Doxorubicin (Adriamycin, hydroxydaunorubicin). _____ _____<br />
Etoposide (Eposin, Etopophos, Vepesid, VP-1) _____ _____<br />
Vinblastine (vincristine) _____ _____<br />
Unsure _____ _____<br />
Other________________________________ _____ _____<br />
Other________________________________ _____ _____<br />
Not applicable<br />
Additional details: (Check here and use reverse for more space.)______________________________<br />
Date chemotherapy started : _____/______/_______ Unknown<br />
MM DD YYYY<br />
Date chemotherapy completed: _____/______/_______ Unknown<br />
MM DD YYYY<br />
continued on next page<br />
© TGen BOCRU 2006 Page 6 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
8c. Was there a diagnosis of ‘hypercalcemia’ Hypercalcemia is a high level of calcium in the blood.<br />
Y N Unknown<br />
If yes, did hypercalcemia symptoms (typically nausea and / or vomiting) lessen or disappear following<br />
surgery Y N Unknown<br />
Not Applicable<br />
8d. Is (or was) patient receiving any other kind of treatment other than surgery and chemotherapy (like<br />
radiation)<br />
No Go to question 8e<br />
Unsure Go to question 8e<br />
Yes Please explain, including dates of treatment: (Check here and use reverse for more space.)<br />
______________________________________________________________________________<br />
______________________________________________________________________________<br />
______________________________________________________________________________<br />
8e. Is (or was) patient receiving any other prescribed medications as part of her care<br />
Yes<br />
complete below. (Check here and use reverse for more space.)<br />
No<br />
Go to question 8f<br />
Unknown<br />
Go to question 8f<br />
Prefer not to answer Go to question 8f<br />
Drug Name Indication # months<br />
Comments: _______________________________________________________________________________<br />
_________________________________________________________________________________________<br />
continued on next page<br />
© TGen BOCRU 2006 Page 7 of 8 Version - 11/23/2010
Protocol: hcunliffe10-032<br />
PRIVILEGED COMMUNICATION FOR INVESTIGATIONAL USE ONLY<br />
MEDICAL HISTORY FORM<br />
Barcode:<br />
Barcode will be completed by TGen<br />
8f. Is (or was) patient diagnosed with any other medical conditions or co-morbidities (examples listed below)<br />
Myocardial infarct Congestive heart disease Peripheral vascular disease Hemiplegia<br />
Cerebrovascular disease Chronic pulmonary disease Moderate or severe renal disease AIDS<br />
Connective tissue disease Diabetes type 1 or type 2 Diabetes with end organ damage type 1 or type 2 Lymphoma<br />
Mild liver disease Moderate or severe liver disease Any tumor (not ovarian cancer) Leukemia<br />
Ulcer disease<br />
Dementia<br />
Yes complete below. (Check here and use reverse for more space.) No Unknown NA<br />
<strong>Medical</strong> Condition<br />
Date of Diagnosis<br />
Comments: _______________________________________________________________________________<br />
_________________________________________________________________________________________<br />
Data Collection <strong>Form</strong> Receiving - To be completed by TGen staff:<br />
Copy received at TGen by: _________________________________________ Date: ______/______/______<br />
Name (Printed) MM DD YYYY<br />
Comments: _______________________________________________________________________________<br />
© TGen BOCRU 2006 Page 8 of 8 Version - 11/23/2010