Policy Roundtable Abstracts - AcademyHealth
Policy Roundtable Abstracts - AcademyHealth
Policy Roundtable Abstracts - AcademyHealth
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
evisit the topic for at least a decade, maybe two or<br />
three. Meanwhile, Baby Boomers will be able access<br />
home care more readily, but for the real catastrophe,<br />
nursing home care costs, they will still be waiting for an<br />
answer. And so will state Medicaid budgets. Dr. Ng will<br />
focus on HCBS. He observes that over the past two<br />
decades state Medicaid programs have greatly<br />
expanded HCBS although considerable interstate<br />
variation in access to services remains. The PPACA has<br />
three important provisions to expand HCBS. First, the<br />
Community First Choice Option allows states to provide<br />
attendant care services with enhanced federal matching<br />
assistance. Second, HCBS can be offered as an optional<br />
benefit instead of a waiver at a financial eligibility level of<br />
300% of SSI. Third, the State Balancing Incentive<br />
Payments Program provides five years of enhanced<br />
federal matching to eligible states to increase HCBS.<br />
Although these provisions are valuable, the law does not<br />
set minimum standards for HCBS benefits. Moreover,<br />
the new incentives may not be sufficient to encourage<br />
major changes in light of ongoing state budget<br />
difficulties. Wide variations in access to HCBS can be<br />
expected to continue while HCBS competes with<br />
mandated institutional care for funding. Dr. Stone will<br />
focus on the LTC workers. She argues that the PPACA<br />
will impact the development and sustainability of the LTC<br />
workforce in several ways. Specific programs designed<br />
to support and strengthen the elder care workforce<br />
include financial incentives to encourage individuals to<br />
pursue geriatric careers across professions, the<br />
expansion of the Geriatric Education Centers program,<br />
and the development of core competencies and curricula<br />
for direct care workers. Indirectly, the PPACA will<br />
influence the LTC workforce through provisions<br />
designed to shift LTC from a primarily institutional to<br />
HCBS system. Promulgation of new payment<br />
methodologies designed to improve quality and<br />
efficiency in Medicare and an array of demonstration and<br />
pilot projects designed to promote person-centered care<br />
will further impact its size and structure. Ultimately, the<br />
type of education and training and practice patterns<br />
required will need to be altered to successfully achieve<br />
the goals inherent in these provisions. Dr. Phillips will<br />
focus on the provision of nursing home care. He argues<br />
that those portions of the PPACA most likely to have<br />
direct effects on nursing home quality are the Nursing<br />
Home Transparency Act and the Elder Justice Act.<br />
Potential advantages of these programs include an<br />
emphasis on quality assurance, performance<br />
improvements, abuse prevention, standardization of<br />
complaint processes, and strengthening enforcement<br />
remedies. By contrast, it is likely that the PPACA’s<br />
emphasis on shifting LTC services from nursing homes<br />
to HCBS will have indirect effects on nursing home<br />
quality. This is because successful implementation of<br />
such a shift will depend heavily on significant institutional<br />
restructuring; increases in human capital in the LTC<br />
sector; and the identification of funding sources for the<br />
provision of high quality care, both in the community and<br />
in nursing homes.<br />
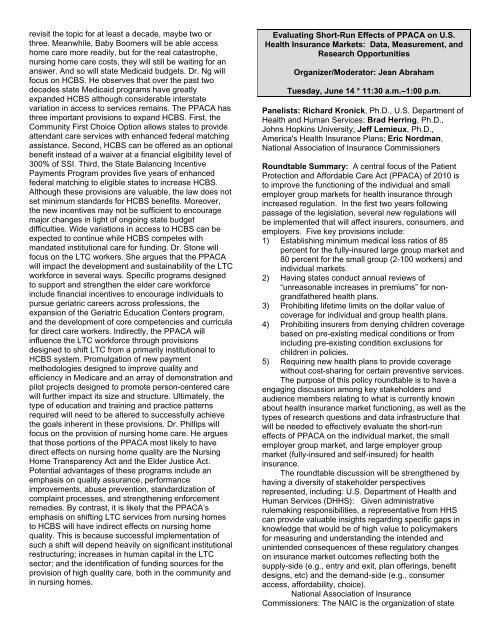
Evaluating Short-Run Effects of PPACA on U.S.<br />
Health Insurance Markets: Data, Measurement, and<br />
Research Opportunities<br />
Organizer/Moderator: Jean Abraham<br />
Tuesday, June 14 * 11:30 a.m.–1:00 p.m.<br />
Panelists: Richard Kronick, Ph.D., U.S. Department of<br />
Health and Human Services; Brad Herring, Ph.D.,<br />
Johns Hopkins University; Jeff Lemieux, Ph.D.,<br />
America's Health Insurance Plans; Eric Nordman,<br />
National Association of Insurance Commissioners<br />
<strong>Roundtable</strong> Summary: A central focus of the Patient<br />
Protection and Affordable Care Act (PPACA) of 2010 is<br />
to improve the functioning of the individual and small<br />
employer group markets for health insurance through<br />
increased regulation. In the first two years following<br />
passage of the legislation, several new regulations will<br />
be implemented that will affect insurers, consumers, and<br />
employers. Five key provisions include:<br />
1) Establishing minimum medical loss ratios of 85<br />
percent for the fully-insured large group market and<br />
80 percent for the small group (2-100 workers) and<br />
individual markets.<br />
2) Having states conduct annual reviews of<br />
“unreasonable increases in premiums” for nongrandfathered<br />
health plans.<br />
3) Prohibiting lifetime limits on the dollar value of<br />
coverage for individual and group health plans.<br />
4) Prohibiting insurers from denying children coverage<br />
based on pre-existing medical conditions or from<br />
including pre-existing condition exclusions for<br />
children in policies.<br />
5) Requiring new health plans to provide coverage<br />
without cost-sharing for certain preventive services.<br />
The purpose of this policy roundtable is to have a<br />
engaging discussion among key stakeholders and<br />
audience members relating to what is currently known<br />
about health insurance market functioning, as well as the<br />
types of research questions and data infrastructure that<br />
will be needed to effectively evaluate the short-run<br />
effects of PPACA on the individual market, the small<br />
employer group market, and large employer group<br />
market (fully-insured and self-insured) for health<br />
insurance.<br />
The roundtable discussion will be strengthened by<br />
having a diversity of stakeholder perspectives<br />
represented, including: U.S. Department of Health and<br />
Human Services (DHHS): Given administrative<br />
rulemaking responsibilities, a representative from HHS<br />
can provide valuable insights regarding specific gaps in<br />
knowledge that would be of high value to policymakers<br />
for measuring and understanding the intended and<br />
unintended consequences of these regulatory changes<br />
on insurance market outcomes reflecting both the<br />
supply-side (e.g., entry and exit, plan offerings, benefit<br />
designs, etc) and the demand-side (e.g., consumer<br />
access, affordability, choice).<br />
National Association of Insurance<br />
Commissioners: The NAIC is the organization of state