Policy Roundtable Abstracts - AcademyHealth
Policy Roundtable Abstracts - AcademyHealth
Policy Roundtable Abstracts - AcademyHealth
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
COST: Panelist Michael Chernew, PhD, from<br />
the Harvard Medical School will summarize his research<br />
on differing mechanisms to control healthcare spending<br />
growth while maintaining quality of care. Specifically, Dr.<br />
Chernew will highlight the challenges in collecting and<br />
standardizing cost data, discuss consumer incentives<br />
and value-based insurance design, and discuss how<br />
alternative payment models may align with the goals of<br />
IHI’s Triple Aim initiative.<br />
PATIENT EXPERIENCE: Panelist Elliott Fisher,<br />
MD from The Dartmouth Institute for Health <strong>Policy</strong> and<br />
Clinical Practice will briefly summarize the many lessons<br />
learned from three decades of variation research on<br />
patient outcomes and the patient experience. Dr. Fisher<br />
will give special attention to his landmark findings<br />
illustrating the disconnect between utilization volume and<br />
patient outcomes and the implications of unwarranted<br />
variations for patient safety and quality of care. He will<br />
conclude by discussing the potential of newly proposed<br />
initiatives to stimulate and support accountable delivery<br />
systems.<br />
POPULATION HEALTH: Panelist David Kindig,<br />
MD, PhD from the University of Wisconsin School of<br />
Medicine and Public Health will draw on his experience<br />
as co-director of CountyHealthRankings.ORG and the<br />
Mobilizing Action Toward Community Health (MATCH)<br />
project to discuss measurement of the social and<br />
environmental determents of health and their interaction<br />
with the healthcare system when quantifying the health<br />
of a population. He will also discuss the synergies and<br />
conflicts between conceptualizations of population health<br />
in the Triple Aim and MATCH models.<br />
PERFORMANCE MEASUREMENT: Panelist<br />
David Radley, PhD, is a measurement expert at the<br />
Institute for Healthcare Improvement and The<br />
Commonwealth Fund. Dr. Radley will draw on real-world<br />
examples (based on IHI collaborations with<br />
organizations currently pursuing improvement activities<br />
around the Triple Aim concepts) to discuss the unique<br />
challenges of simultaneously measuring performance<br />
across the three dimensions of the Triple Aim. He will<br />
describe his experience creating locally representative<br />
health system performance scorecards and will discuss<br />
the collection and use of systematically defined ‘local’<br />
data to measure health system performance and<br />
motivate improvement.<br />
Healthcare system design and re-design should<br />
simultaneously aim to improve population health,<br />
enhance the patient experience, and reduce per capita<br />
healthcare spending. Proposed and legislated<br />
healthcare reforms can go a long way to achieving better<br />
performance on each of these dimensions. However,<br />
success also requires the development of data systems<br />
and carefully defined metrics that are accessible to<br />
evaluators, a recognition of and commitment to<br />
addressing the community-based determinants of<br />
population health, a common purpose and the adoption<br />
of mechanisms to control per capita cost, and most<br />
importantly, engagement from motivated local entities<br />
that are willing and able to support a defined population<br />
and ensure the existence of systems that align<br />
healthcare services with individual’s needs.<br />
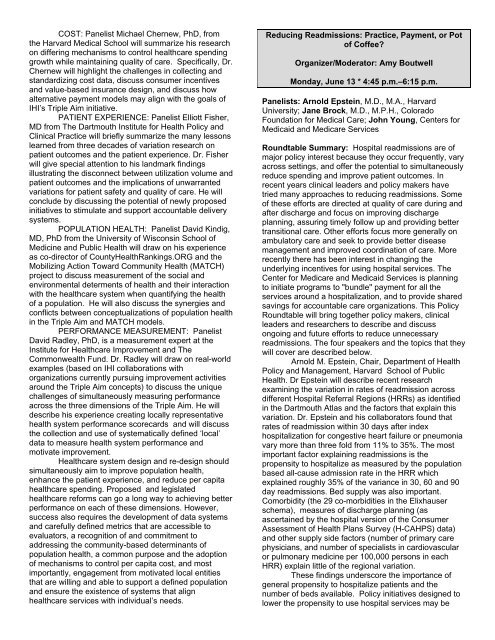
Reducing Readmissions: Practice, Payment, or Pot<br />
of Coffee<br />
Organizer/Moderator: Amy Boutwell<br />
Monday, June 13 * 4:45 p.m.–6:15 p.m.<br />
Panelists: Arnold Epstein, M.D., M.A., Harvard<br />
University; Jane Brock, M.D., M.P.H., Colorado<br />
Foundation for Medical Care; John Young, Centers for<br />
Medicaid and Medicare Services<br />
<strong>Roundtable</strong> Summary: Hospital readmissions are of<br />
major policy interest because they occur frequently, vary<br />
across settings, and offer the potential to simultaneously<br />
reduce spending and improve patient outcomes. In<br />
recent years clinical leaders and policy makers have<br />
tried many approaches to reducing readmissions. Some<br />
of these efforts are directed at quality of care during and<br />
after discharge and focus on improving discharge<br />
planning, assuring timely follow up and providing better<br />
transitional care. Other efforts focus more generally on<br />
ambulatory care and seek to provide better disease<br />
management and improved coordination of care. More<br />
recently there has been interest in changing the<br />
underlying incentives for using hospital services. The<br />
Center for Medicare and Medicaid Services is planning<br />
to initiate programs to "bundle" payment for all the<br />
services around a hospitalization, and to provide shared<br />
savings for accountable care organizations. This <strong>Policy</strong><br />
<strong>Roundtable</strong> will bring together policy makers, clinical<br />
leaders and researchers to describe and discuss<br />
ongoing and future efforts to reduce unnecessary<br />
readmissions. The four speakers and the topics that they<br />
will cover are described below.<br />
Arnold M. Epstein, Chair, Department of Health<br />
<strong>Policy</strong> and Management, Harvard School of Public<br />
Health. Dr Epstein will describe recent research<br />
examining the variation in rates of readmission across<br />
different Hospital Referral Regions (HRRs) as identified<br />
in the Dartmouth Atlas and the factors that explain this<br />
variation. Dr. Epstein and his collaborators found that<br />
rates of readmission within 30 days after index<br />
hospitalization for congestive heart failure or pneumonia<br />
vary more than three fold from 11% to 35%. The most<br />
important factor explaining readmissions is the<br />
propensity to hospitalize as measured by the population<br />
based all-cause admission rate in the HRR which<br />
explained roughly 35% of the variance in 30, 60 and 90<br />
day readmissions. Bed supply was also important.<br />
Comorbidity (the 29 co-morbidities in the Elixhauser<br />
schema), measures of discharge planning (as<br />
ascertained by the hospital version of the Consumer<br />
Assessment of Health Plans Survey (H-CAHPS) data)<br />
and other supply side factors (number of primary care<br />
physicians, and number of specialists in cardiovascular<br />
or pulmonary medicine per 100,000 persons in each<br />
HRR) explain little of the regional variation.<br />
These findings underscore the importance of<br />
general propensity to hospitalize patients and the<br />
number of beds available. <strong>Policy</strong> initiatives designed to<br />
lower the propensity to use hospital services may be